 At the end of it all, the science, the medical visits, the surgeries, what we really want is to prevent new stones. That is the main goal. Modern surgery is a blessing for those with stones. But no surgery is far better than even the most skilled and effective surgery.
At the end of it all, the science, the medical visits, the surgeries, what we really want is to prevent new stones. That is the main goal. Modern surgery is a blessing for those with stones. But no surgery is far better than even the most skilled and effective surgery.
Prevention of stones is orderly and occurs only over time.
Here is how to do it.
This article is designed to go with my other one which tells how to organize your medical visits so as to achieve these steps.
What is the Science of the Five Steps?
Supersaturation drives crystal formation and growth – this is a physical law that must always apply.
Supersaturation measurements are widely available from commercial vendors.
Because people who are actively forming stones are forming crystals their supersaturations are too high – crystals are forming – with respect to those crystals.
Lower the relevant supersaturations and you must lower formation and growth of those crystals in their stones.
With respect to the most common stones, calcium oxalate and calcium phosphate, and uric acid, supersaturation in urine depends mainly on volume, calcium, oxalate, citrate, and pH. You can lower supersaturation by altering any or all of these in a given person and so far as crystals are concerned the effects are much the same.
1. Know the Stone Crystals
Stones are made of crystals: No crystals no stones. Prevention is prevention of crystals.
Analyze Stones
The proper way to know the crystals is analysis of stones and their fragments. Stone analysis is not expensive. If imperfect, it is the best we have, so use the service liberally. Stone crystals can change, and therefore prevention can need to change direction. There is no reason to discard a stone without analysis just because we think we know the answer.
Uric acid stones are remarkably easy to treat by raising urine pH and require little more discussion.
Cystine stones arise from hereditary kidney transport disorders and require special management.
Struvite stones arise from infection and require special combined surgical medical management.
Drug stones, ammonium acid urate stones, and rare stones – eg. 2,8 dihydroxyadenine stones require special management.
The vast proportion of kidney stones are calcium oxalate and calcium phosphates and uric acid, and this article refers mainly to them.
Guess if You Have To
Red or orange stones probably contain uric acid. Likewise, stones that do not show up on simple abdominal flat plate x rays are probably uric acid. These are easy to prevent, and recurrences are unnecessary.
Allow me to elaborate on this. Pure uric acid stones are almost all due to an excessively acid urine pH, and will stop if you raise that pH. Potassium citrate tablets, 10 mEq size, 2 twice daily is almost always enough. Sometimes it takes 2 tabs 3 times a day. Crystal light lemonade has in one liter about the same amount of alkali as two of the tablets. I could say that there is little excuse for another uric acid stone.
If stones contain uric acid and other crystals, those other crystals need to be dealt with on their own. They may not respond to higher urine pH, and could be worsened.
Yellow stones are probably cystine, and due to cystinuria, a complex disease with its own special treatments. Because almost all kidney stone panels include a cystine screening test, cystinuria is almost never missed. A positive test, however, can reflect cystine trait and the stones can be something else. So it is the negative test that is fully informative.
Small black stones are probably calcium oxalate, and large very homogeneous hard stones are probably brushite. But one cannot be sure.
Big stones that fill up the interior of the kidney are usually cystine, struvite – from infection, or calcium phosphates from alkaline urine and hypercalciuria.
But guessing is not a good way to achieve prevention. Find out whenever possible what crystals you are trying to prevent. Any stone fragment can be analysed. Never pass up an chance to be sure.
2. Obtain Proper Blood and 24 Hour Urine Measurements
I prefer two 24 hour urine kidney stone risk panels as a minimum along with at least one set of fasting blood measurements.
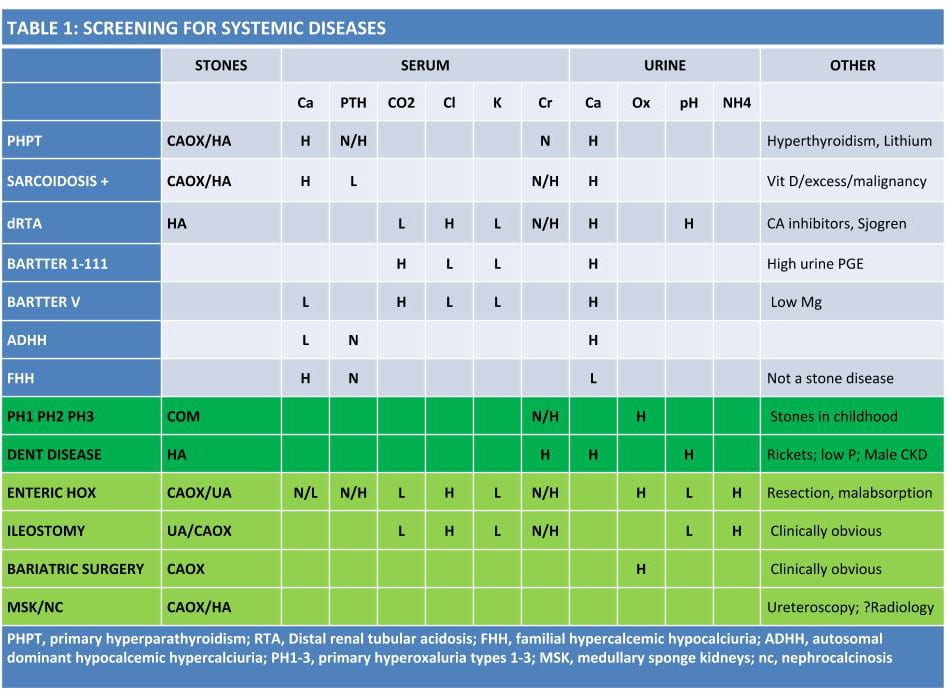
Screen for Systemic Diseases
Here is a table of systemic causes any physician can follow using the blood and 24 hour urine testing. This is not something a patient can do anything about except see that it is accomplished.
The bowel diseases that cause enteric hyperoxaluria – small bowel resection, malabsorption, are usually obvious, as are ileostomy and bariatric surgery.
Medullary sponge kidney and nephrocalcinosis are complicating features physicians need to deal with. Medullary sponge kidneys actually form tiny micro crystals in their dilated ducts. Whether these grow to become clinically important is not clear.
Nephrocalcinosis simply means many crystals are present on x ray images. During ureteroscopy these crystal deposits can be sorted out into real stones and plugs within the terminal ducts of the kidneys. Pain without obstruction is widely described in both of these conditions which complicates management.
Measure Urine Supersaturations of the Stone Crystals
Standard 24 hour urine kidney stone risk panels give supersaturations along with the urine chemistries that control those supersaturations. These are the keys to prevention. Supersaturations control crystallization and can be measured reliably in people. If crystals are being formed the supersaturation is too high and we need to lower it.
Read Your 24 Hour Urine Reports
Your physician will take care of you but a prepared and educated patient can make that care vastly more effective and reliable.
You can understand your 24 hour urine tests and follow along with your physician during your visits and when treatment has been introduced and your urine chemistries change as a result. The details of interest are different for calcium stones and uric acid stones, so I have put them in two separate articles. Do not be put off by all the numbers. Follow the articles with your test panel in hand and you will find things are not so difficult.
Stone prevention is long term and involves changes in diet and behavior and, often, medication use. If you can read your own report you will have a first hand sense of why your treatments are good for prevention and whether your treatments have achieved what they were designed to achieve.
3. Lower By Half the Supersaturations for the Crystals in Stones
There is no one way to reduce supersaturations. Every patient will have a characteristic pattern of abnormalities and supersaturation can be lowered by changing any number of those abnormalities present. Below is my general strategy, but it may not apply to you. If your urine volume is already very high, for example, to raise it would be silly. So consider my ‘strategy’ a general set of rules, easily modified to fit the individual situation.
Raise Urine Volume as High as is Practical
Above 2.5 liters daily is ideal. The site is very rich in advice for fluid treatments. How to drink more. How to get variety. How to avoid low flow periods. Being without cost or risk, fluids are always my first choice.
Reverse Urine Abnormalities Raising Supersaturations for the Crystals in Stones
 Identify the factors in the 24 hour urine beside volume that are raising supersaturations for the crystals in stones, and act so as to reverse them toward normal. Common ones are high urine calcium, high urine oxalate from diet, low urine citrate, and low urine pH – for uric acid stones. High pH is a risk factor for calcium phosphate stones but one cannot lower urine pH under most circumstances.
Identify the factors in the 24 hour urine beside volume that are raising supersaturations for the crystals in stones, and act so as to reverse them toward normal. Common ones are high urine calcium, high urine oxalate from diet, low urine citrate, and low urine pH – for uric acid stones. High pH is a risk factor for calcium phosphate stones but one cannot lower urine pH under most circumstances.
Bang For the Buck
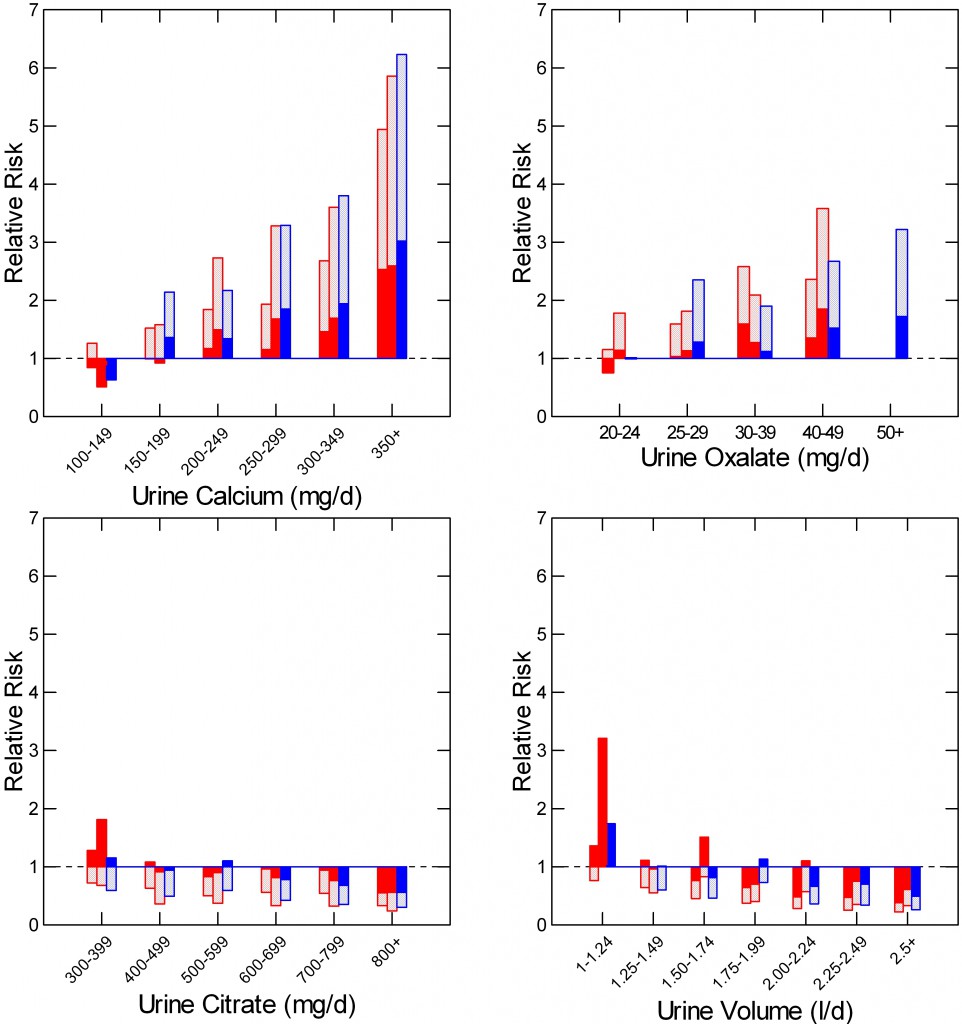
A vulgar phrase, if you think about it. Here are the relative risks of becoming a stone former in the three cohorts of nurses (red) and physicians (males, blue) Dr. Gary Curhan followed. You might say relative to what. For each risk factor it is different: Calcium – less than 100 mg/day; Oxalate – less than 20 mg/day; Citrate – less than 300 mg/day; Volume, less than 1 liter.
The average relative risk is at the end of the crosshatched bars. The ends of the solid bars are the 95th percentiles. When the solid bars are above one risk is certainly present, so you can see the safe ranges for calcium, oxalate, citrate, and volume. Because the plots all have the same risk ranges you can compare these four risk factors. Calcium has the widest effect range. Oxalate is next and increases risk at even 25 mg/day. Citrate causes risk only when below 400 mg/day, and volumes above 2 – 2.24 liters lower all three cohorts into a low risk range.
Although urine volume confers relative risk equivalent to high urine calcium and oxalate only when below 1.25 liters daily (see graph at left), one always wants to raise it as much as is possible because such treatment is without risk or cost. Above 2.25 liters daily is ideal. The site is very rich in advice for fluid treatments. How to drink more. How to get variety. How to avoid low flow periods.
Obtain New 24 Hour Urines to be Sure Supersaturations Have Fallen
There is no point to changing diets or medications without proper follow up to determine if what was done had the desired effects. Six weeks is a good time for the first follow up measurement. Continue measurements until the supersaturation goals have been achieved.
4. Obtain more 24 Hour Urines if New Stones Continue
Crystals follow physical laws and supersaturation is what drives them to form and grow. Continued stones with reduced supersaturations means either supersaturations need to be lower, the 24 hour samples are not being taken on representative days, or the days themselves have periods of low urine flow or other breaks in treatment.
Crystals do not sleep nor do they make mistakes. Any chances they get, they use.
Physicians are trained to ferret out the details of a patient’s history that matter here. It is my main clinical expertise.
Patients are not trained but they are the ones sitting up close at the 50 yard line. So they know more than anyone else. They just may not know what is important for stone prevention.
5. Follow Up Every Year Thereafter Even If Free of New Stones
OH, you might say, those urine measurements cost money.
They do, hundreds of dollars for each one.
The merest surgery can cost near to or even above ten thousand dollars when you consider the total of medical, operating room, anesthesia, and pre and postoperative imaging costs, and the inevitable emergency room visits that provoke the surgery in the first place. This is not to mention lost time from work.
And, did I speak about pain, misery, infections?
It it time for blunt talk. Lab measurements are the compass and altimeter. Flying blind is silly.
A Good Way to Get All This Done
You cannot do the five steps alone, your physician is crucial. He or she cannot do them either; you are crucial. In case you missed it, here is my view on how a patient and physician can best partner for stone prevention.
That’s It
This site is far from complete but it already has a lot of what one needs to carry out these five critical steps. Do them and new stones will cease altogether or at least greatly reduce in frequency. If it does not work, one or more of the steps need correcting. After nearly 45 years preventing stones, I have become bold enough to say this, and mean it.
Good Luck, Fred Coe


3 weeks ago I had a ureteroscopy which removed a 6mm calcium oxalate stone. I continue to get intermittent flank pain on the affected side but only when I urinate. Is this another stone that wasn’t picked up on CT or just residual reflux from the hydroureter caused by the original stone?
Hi Joe, I cannot be sure which is the cause, but if it continues your urologist will want to look into that cause and be sure things are alright. If you are a physician, which I suspect, indeed there may be residual hydroureter; but sometimes there are residual fragments, and sometimes the hydro has not resolved because of residual obstruction. So I would be sure. Regards, Fred
I am trying to figure out my test results. I do not see my urologist until 2 months from now, but would love to get a kick start on whatever I need to do. Can I send you the results?
Hi Ginger, I would be remiss if I did this as it were practicing medicine for someone I do not know. If you want to post the results I can comment technically on what the numbers show – many have done this – and being public commentary I would be within proper bounds. Regards, Fred Coe
Hello! Thank you for all the information you have given through the web. It helped me make sense of the test results I just received. I had a kidney stone test to test the crystals that are consistently in my urine – causing cloudy urine. My crystals are 20% ammonium hydrogen urate and 80% struvite. Ironically, it looks like the treatment for either of these individually is exactly the opposite of the other. I was wondering if you would be willing to comment on the test results. Thanks for considering this :).
Hi Kathryn, Struvite is formed by bacteria colonized in your urinary system. The ammonium acid urate is uncommon with infection but could occur. Your physicians need to culture the organism and consider how to treat the condition. If you have bowel disease or diarrhea from laxatives, that could promote the ammonium acid urate. Given so little information I cannot offer more. I deleted the repeat of your query. Regards, Fred Coe
I suffer from calcium oxalate stones and ulcerative colitis. From what I have read, UC suffers should avoid dairy. Doing so would make it difficult to acheive a high calcium diet. What do you suggest?
Hi Douglas, Alas I have not as yet put up an article on ulcerative colitis, just on bariatric surgery and ileostomy. Stones from UC involve fluid loss from diarrhea – variable from person to person, acid urine pH from the same fluid loss, but urine oxalate is not usually high. I would advise pursuing a full evaluation as in the article to see what your urine findings are and get those treated. Diet calcium, as an example, may have nothing remarkably to do with your individual situation. Regards, Fred Coe
Hi! Thank you for your informative website. Doing my own research brought me with you 🙏🏿😍 I have 4 mm calculus w/in the calyx upper pole of Right Kidney, noted incidentally in CT scan lungs in 2010, old TB contracted when young, Phils . I Did 24 hr urine once, Nephro prescribed Urocit & Allopurinol, taking them regularly. In 2015 another CT urogram off base was done due to hematuria, my PCP referred me to a Urologist. Every year I have X-rays & ultrasound done. Findings are the same, unchanged. Have you passed them? always asked , every three months of visits. No advice., to dissolve, No proper blood testing, or urine urinalysis. Occasionally I felt flank pain on Left back side down my groin. It’s an unexplained pain?? So he order anotherCT & KUB. I risk my general health of radiation, I refused. On my regular check up I complained to my PCP re: my chronic fatigued due to my Levo Meds, not taking in effect yet, did exercises for IIiotibial syndrome( felt better ) . I have signs symptons of UTI did a urine test/dipstick and was given Cipro. My new DO urology surgeon , felt my risk injury to my kidney by waiting and heard I want to be
treated, discussed treatment options of ESWL and ordered to get preoperative Labs and scheduled me for Oct, yes that soon?? Now I making a second thought and getting chicken out, getting scared of pains after the procedure, the passing of fragments through my uterus, the stents , healing. I am afraid of more radiation, CT’s ( I’ve undergone bi -lateral lumpectomy in 2014 ) Are there any alternatives. How do you pass stone w/o intervention? Are there any medical theraphy, to pass , dissolve, dissipate with the help of medicines. If the stones are small and are non -obstructing ( my 1st CT says so) is it usually best to left it alone. I read about to just be watchful and wait for stone will pass on its own but 😂I am a worried of CKD, dialysis. My brother recently died of kidney failures. I read if untreated it can cause kidney blockage( poor kidney function) can cause serious infection. I am very careful, watch my oxalate diet , on purines ( Uric Acid ) . I have to see a dietician, nephrologist re: my hypothyroid & Kidney,very confusing. I am 5 feet; 125 lbs. My eGFR non African is 78 & 91 African ; BUN 11; Creatinine .78; I believe I have systemic diseases that may also cause my stone. If ever I will have my procedure 🙏🏿 I prefer Ureteroscopy laser and baskets, stone dusting where fragments into small pieces (dust) w/o consequences to pass after, painless. I pray not to form any new stones. . I do appreciate and will heed all your advices , steps to stone prevention. Your websites, your love and care for us patients , are God-sent. Thank you very much for any advice you can give me and for taking time to read my long message. Sincerely, Rosie
PThank you you very for your advice
Hi Rosalinda, I believe this is a duplicate, and my original answer is complete. Let me know, Regards, Fred Coe
Hi! Thank you for your informative website. Doing my own research brought me with you 🙏🏿😍 I have 4 mm calculus w/in the calyx upper pole of Right Kidney, noted incidentally in CT scan lungs in 2010, old TB contracted when young, Phils . I Did 24 hr urine once, Nephro prescribed Urocit & Allopurinol, taking them regularly. In 2015 another CT urogram off base was done due to hematuria, my PCP referred me to a Urologist. Every year I have X-rays & ultrasound done. Findings are the same, unchanged. Have you passed them? always asked , every three months of visits. No advice., to dissolve, No proper blood testing, or urine urinalysis. Occasionally I felt flank pain on Left back side down my groin. It’s an unexplained pain?? So he order anotherCT & KUB. I risk my general health of radiation, I refused. On my regular check up I complained to my PCP re: my chronic fatigued due to my Levo Meds, not taking in effect yet, did exercises for IIiotibial syndrome( felt better ) . I have signs symptons of UTI did a urine test/dipstick and was given Cipro. My new DO urology surgeon , felt my risk injury to my kidney by waiting and heard I want to be
treated, discussed treatment options of ESWL and ordered to get preoperative Labs and scheduled me for Oct, yes that soon?? Now I making a second thought and getting ,chicken out, getting scared of pains after the procedure, the passing of fragments through my uterus, the stents , healing. I am afraid of more radiation, CT’s ( I’ve undergone bi -lateral lumpectomy in 2014 ) Are there any alternatives. How do you pass stone w/o intervention? Are there any medical theraphy, to pass , dissolve, dissipate with the help of medicines. If the stones are small and are non -obstructing ( my 1st CT says so) is it usually best to left it alone. I read about to just be watchful and wait for stone will pass on its own but 😂I am a worried of CKD, dialysis. My brother recently died of kidney failures. I read if untreated it can cause kidney blockage( poor kidney function) can cause serious infection. I am very careful, watch my oxalate diet , on purines ( Uric Acid ) . I have o see a dietician, nephrologist re: my hypothyroid & Kidney,very confusing. I am 5 feet;p 125 lbs. My eGFR non African is 78 & 91 African ; BUN 11; Creatinine .78; I believe I have systemic odiseases that may also cause my stone. If ever I will have my procedure 🙏🏿 I prefer Ureteroscopy laser and baskets, stone dusting where fragments into small pieces (dust) w/o consequences to pass after, painless. I pray not to form any new stones. . I do appreciate and will heed all your advices , steps to stone prevention. Your websites, your love and care for us patients , are God-sent. Thank you very much for any advice you can give me and for taking time to read my long message. Sincerely, Rosie
Hi Rosalinda, I am not quite sure but you seem to describe a single 4 mm stone in one kidney unchanged for years. Given that one small stone, surgery is completely elective: Pain, bleeding, infection, obstruction. Perhaps I do not have all the facts, however. But with even one stone, and no recurrences, you should review your 24 hour urine and serum findings with your physician concerning at least a proper diet to reduce risk of more. This article speaks about diet, here is a longer one. Regards, Fred Coe
Hello sir I want your contact number if possible to you.
Hi Shwete, my university email is flcoe@uchicago.edu. Regards, Fred Coe
Plz give me your contact number.
Hello Mr Coe,
I have had calcium stones since I was 18. I am now 48 and my stone problem seems to be getting worse. Anytime I eat sugar high sugar foods, I get stones. Furthermore, I sometimes have coughing fits (it also seems to affect my lungs). I know that sounds weird but I have tried to avoid sugars completely. Although it is really hard to do. Your explanation is something no urologist has been able to help me with.
Hi Tiffany, THis article you are posting on is a good guide to proper evaluation and treatment. Avoiding refined sugar is just wise, for a lot of reasons. I did it, and was a sugar lover. By now you should have been on a stone prevention regimen for years; finish your evaluation and get treated. Regards, Fred Coe
Hello Dr. Coe. I’ve followed your articles for some time now. I’ve been searching for an underlying cause to my kidney stones since I first became aware back in the fall of 2017 and prior imaging on record showed evidence back to 2014. Hypercalciuria and borderline hypercalcemia, low/normal PTH. Recent 24 hour collection now recommends treating hypercalciuria with thiazide diuretics. I am possibly sarcoidosis but lung/mediastinal lymph node sample was negative (ace positive and seem to be sensitive to vitamin d supplements). No cancer after 5 scans in last year, but possibility of lymphoma exists with stable lymphadenopathy and mild splenomegaly (going back for another eval). Hospitalized with hypercalcemia and acute kidney failure last summer (aki in 2014 also). Currently on prednisone and plaquenil to keep it all in check. GFR is borderline stage 3a. That’s my background and my question is simply this: are thiazide diuretics safe for someone in the double hyper calcium category? Would also love to see a write up on sarcoidosis and associated vitamin d complications because I have around 15 specialists and no one has a clue what is wrong with me.
Hi Chad, You have something far more complex than routine stones. Thiazide is not a good idea. If the prednisone /[plaquenil control your hypercalcemia and hypercalciuria – presuming this is sarcoid – that is the best direction. Thiazide can cause significant hypercalcemia and another bout of kidney damage. The report is no doubt from Litholink, and I and Dr John Asplin wrote the code that generated it – I founded Litholink and sold it to LabCorp. I do need to write more about the hypercalcemic vitamin D excess states. Promise. Regards, Fred Coe
Dr. Coe. Thank you for thoughtful and thorough response. Interestingly enough, I did my 24 hour collection after 7 weeks off of prednisone. Wish I had done it when I was on. Went back on prednisone when my serum Ca/Cr started to creep back up right after. Concerning that 2 months of plaquenil alone wasn’t cutting it and disheartening because the ocular side effects I have with prednisone are very bad. Hopefully on a less harsh dose now. I’ve done everything else for stone prevention there is for me to possibly do so hopefully my relatively young body can hang in there. Best. CLW
Hi Chad, Discuss with your physicians if you really have Sarcoid or perhaps CYP24a1 mutation that is treated with fluconazole. Gene studies are now practical and rather more direct. Regards, Fred Coe
Hi Dr. Coe. I am researching how to get tested for the CYP24A1 genetic mutation, and keep coming up empty. My doctor is happy to write the order for me, but she does not know where to go to run the lab. I reached out to my urologist and no response. I called Children’s Hospital, and came up empty. I’ve tried LabCorp, and have come up empty. I will call Quest next, but am not hopeful. Might try Ohio State. They are looking for a test code which I don’t have. I found this information, but do not know how to use it. https://www.ncbi.nlm.nih.gov/gtr/all/tests/?term=1591%5Bgeneid%5D
i thought someone would just be able to do the lab draw and send it to Mayo like they do for every other weird test I’ve had. Sigh. Do you have any further advice here?
Thanks again,
Chad
Hi Chad, I am answering questions tonight and have the eerie feeling I did them already and WordPress has either lost them or somehow made the questions seem unanswered. I know I mentioned Mayo to you and especially Raj Kumar, there, who is the world expert and a good friend. Regards, Fred Coe
Hello again. I reached out via email through this website at Mayo (http://www.rarekidneystones.org/) and got an immediate response. They can test this at no charge as part of their research if I meet the criteria. I think I have everything I need. Thanks again for your generosity and time! Chad
Hello again Dr. Coe.
Happy to report that my urinary calcium is down from 555 to 313. I’m on 7.5 mg of prednisone and 400mg plaquenil daily. Still a little ways to go but that is lowest reading I’ve ever had. Can these drugs contribute to this improvement in addition to my serum levels?
Sadly, my citrate went back down despite being on 20 meq K-Citrate. Wondering if I have a drug interaction. Still waiting to hear back from Mayo on results from CYP24A1 draw in May.
Kind regards,
Chad
Hi Chad, Your treatment is as if aimed at Sarcoid, and I am glad it is helping. It would not do much for CYP24A1 deficiency. Regards, Fred Coe
Hi Dr Coe, thank you for your wonderful website. Do you have the name of a doctor in the San Francisco Bay Area you could recommend? I had one large Uric stone that was removed through lithotripsy about ten years ago and I don’t want to go through that again. I have been put on six 1080 mg pills of potassium citrate per day and was trying to get another opinion if this is the best solution. It is a bother and will be very expensive when I go on Medicare later this year. Thank you for your anticipated courtesies and your wonderful work.
Hi RObert, I do; Dr Marshall Stoller at UCSF. He is terrific and a friend of mine. Do not hesitate to say I recommended you. As for uric acid stones, I am amazed that you got a second one; 6 k citrate pills should have prevented all recurrences. These stones are caused entirely by low urine pH and that much alkali surely would have raised your pH above the threshold for crystallization. Regards, Fred Coe
Hello! I was hoping you could refer me to a doctor in MI for my gf.
Hi Jeremiah, I can try. I presume your gf (girl friend) has stones. Can you tell me where in MI she lives so I can get the closest for her? Regards, Fred Coe
I just had my first kidney stone and developed Septic Shock, Flash Pulmonary Edema, and Takotsubo Cardiomyopathy because of it. I was in ICU twice and on a ventilator. I almost died twice. I am terrified that I am going to get another stone. I need to find another Urologist since the one I have only told me to eat healthy, lose weight, and exercise and he would see me again in 3 months. I just had my stent removed 2 days ago after having it in for almost 2 months. Do you know a good Urologist in the metro Detroit Michigan area?
Hi Susan, What a terrible event. In Detroit Wayne State has no urology faculty I recognize. U MIchigan at Ann Arbor has a large urology department and likely higher quality. Dr Roberts in that department lists himself as an expert in endourology and must be their main stone surgeon. I do not know him, but I would make inquiry if I were you. Regards, Fred Coe
Susan… I just saw an amazing urologist in he Detroit area. I have been plagued with kidney stones most of my life and she is one of the first Drs who has done a thourough work up and has advised me on prevention. Dr. Shiva Miralania
I have had 4 stones in the last 4 years….my doctor has not put me on anything to stop these stones – just had another analysis and my SS CaOx 9.86 and SS CaP 2.84 — is there anything I can take to prevent them>
Hi Lisa, Do you know what the stones are made of? The SS are the outcome of the various urine chemical imbalances, but I cannot tell which ones matter to you. Here is an article that details a bit more, see if you can find yourself in it. Here is another to help with your lab report. I am guessing your stones are calcium, but if they are uric acid, read this. Regards, Fred Coe
Hi Dr. Coe,
I had my first kidney stone 2 years ago and have had 6 others that I may or may not have passed and currently have 12 between my 2 kidneys, the majority being in my right side. My CT scan in November showed these stones, with the one I was trying to pass at that time being 6mm. Since then, I have had 3 other “major” pain sessions, but go in and out of pain, sometimes several times a week. I will be fine and then boom 💥 I start hurting. On top of that, my blood pressure has gone up and is now staying around 140-150 over 98-101 most days. My primary DR is Internal Medicine but hasn’t really been able to help me much. I went to s kidney doctor and they really didn’t help either. At this point, im being told to see a urologist. I am in Texas, a little north of Houston… know anyone in the area that I can actually get some help from?
Thank you!
Stephanie
Hi Stephanie, you seem to have a complex problem and need real experts. My choice is UT Dallas, that has a wonderful mineral center and specializes in kidney stones and bone disease. Dr Sakhaee or Dr Orson Moe would both be excellent choices. Please feel free to say I sent you. Regards, Fred Coe
I wondered if you ever thought about toothpaste as a main re-occuring cause of stones. My dentist was telling me I need to brush to re-mineralize my teeth; I often enjoy the taste and used to just ingest a portion of it brushing. Combined with the fact I noticed a special toothpaste with the warning to rinse out numerous times to avoid ingesting the minerals??
I also read your piece on supersaturation and 24 hour urine collections. I have disordered sleeping patterns due to a sleeping disorder and a neurovascular condition that requires I sleep during the day. I have been known to sleep for as long as 22 hours at a time. And be awake just as long. Of course I cheated when they had me do a 24 hour urine I just did it when I was awake to impress them with a gallon of urine – I’m waiting on the Citrate levels, they didn’t get any of the concentrated morning urine void. The labs instructions fail to plan for people that are not on a 24 hour sleep cycle, and there are many of us. Your supersaturation theory sounds plausable, But I also have imagined that after sleeping for about 8 hours it is possible that since no more sodium or minerals are going in. That perhaps with nothing going into the kidney there is no supersatuaration. The only way to find out would be to collect a 24 hour urine from someone that is sleeping for about 20 hours. This might prove or disprove your supersaturation theory. The next time I do my 24 hour urine I will only give them concentrated urine. However, a normal person could probably duplicate this by just giving them only nighttime urine and 2 first morning voids(over 48 hours), without drinking water before going to bed. This would prove, or disprove, the supersaturation theory.
BTW, I haven’t had a stone in 5 years with 10 Meq potasium Citrate 3x or 4x per day. I also drink those 0 calorie “clear” diet citrus drinks that have citric acid, and potasium citrate. Pre Kidney stones I used to consume 6000-8000 mg sodium from junk food and I am slender with a belly.
Hi Jon, We have no data on altered sleep cycles, as you point out. But we have good data that SS is highest at night even though excretion rates are low because urine volume falls drastically with sleep. Possibly you have very high SS while sleeping. But since no new stones have formed, perhaps things are alright. As for toothpaste, it is not ideal to eat much of it because it contains fluoride and that can stain tooth enamel. Regards, Fred Coe
Hello Dr. Coe, as an information seeker, I am so grateful I have found this website. After reading 50 different sites about “oxalate content”, I’ve found your “how to eat a low Oxalate diet” especially valuable! On 9/30/2016 an ultrasound revealed 1. Few parenchymal echogenic foci measuring less then 0.5 CM, bilateral kidneys, consistent with localized fat, prominent vessels or calcifications (calculi). 2. Minimal collecting system dilation and/or subcentimeter parapelvic cysts, right kidney. 3. Prominent column of bertin, right kidney (normal). I read stones of 5cm (if they were) could just pass naturally so I increased my liquid consumption to 75-90 oz/day. Using a sieve, I think I did collect a 1ml stone I bagged up ( tan colored) but never got it analyzed. I live in Glendale, CA and have many options to care, but wondered if you know of a doctor on the more conservative treatment side? I think CedS is a wonderful place, had 1 surgery there, excellent results, but also have declined 3 others with excellent results. My gynecologist sent me for the ultrasound in 2016 & said yesterday I should have followed up it could be a 10cm by now. I am going to get another ultrasound so that’s why I am asking if you have a referral. Thank you for your valuable time
Hi Ann, Dr Nguyen is a urologist who is skilled in stone disease and also a good scholar. I know him, and you can feel free to mention that I suggested him – he is at USC. I looked around and he is about the best of those not too far from you. As for your note, ultrasound is so weak for stone counting I never rely on it. Ultra low CT is excellent and has minimal radiation risk. If you do indeed have stones, you need a proper evaluation as in this article and treatment can indeed be with diet. Regards, Fred Coe
Dr Coe – I had my first lithotripsie and stone last year June/2018. I had horrible back pain before I had the lithotripsie procedure on my left kidney. I had a follow up appointment in April to see if I was developing any more stones, I was told everything was great. My back started hurting on my right side this time and my urine was dark so I called their office in July to see what I needed to do. I went in for a urine test and it was positive for e-coli bacteria. I learned that my results from April showed that I had had bacteria in my urine and that I had a kidney stone in my left kidney again. I was upset since no one ever follow up with me after my official results came in to their office (radiologist reading and lab results) I had no other side effects of infection except dark urine and severe back pain that I was feeling on my left side since there was no stone present in that kidney. It took two rounds of antibodies to get rid of the bacteria and the third test was negative of that bacteria but positive of Lactobacillus species which they indicated they don’t treat. I think that original bacteria has come back again since my back is starting to hurt again on my left side. I am prone to UTI’s. It seems I had bacteria in my urine last time I had kidney stones too. I was able to finally see my doctors partner since she was out of town.I indicated to him at that time I was also passing black pepper like specks and settlement, I also mentioned my concerns of the bacteria being present with the stone since it was there constantly last time I had stones but he was not concerned and did not seem to think there was a correlation. He said it would be a different bacteria that caused them. He ordered a 24 hour urine test. My results came back as SS CaOx 6.11 Urine Calcium 223 Urine Oxalate 39 The interpretation of lab results: *Urine Calcium borderline elevated *Borderline Hyperoxaluria *Mild CaOx stone risk. I have been reading it might be my parathyroid having issues. I also read that I should take calcium. Do you know what I should do about stones? Do you know what I should do about UTI’s and bacteria? They maybe two separate issues but I need both addressed. Since I have absolutely no faith in my current Urologist or their office staff, do you know anyone in the Atlanta area that would be able to help me? Thanks in advance!
Hi Michelle, It sounds like you have two problems, E Coli infections and a recurrent stone. The former can be from surgery or worsened by it, and stones can become infected and perpetuate infection. Lacto bacillus is harmless and not treated. The recurrent stone may be indeed new or perhaps it is a residue from the surgery – not everything was removed. If the post surgery image was a CT and there was no residual stone, then this is truly new. If it was just a flat plate or ultra sound after surgery, a retained fragment could be overlooked. Your labs offer treatment possibilities – here is a good article about it. As for Atlanta, I looked at Emory online under kidney stones and found only a vague looking prochure in PDF format, so I cannot identify any faculty person for you. Regards, Fred Coe
Thanks for your artice. I have passed one huge stone 2 years ago. I have been drinking more water and not had another stone. Ultrasound shows a cortcal stone in one kidney, but I am always told not to worry about it. Any ideas?
Also what is a good target ph for stone prevention? I will use Uralyt-U. I am in Thailand.
Hi Marcus, so you have had one stone without recurrence. I always vote for serum and 24 hour testing to figure out what is wrong – just as in this article. Then depending on results, you can take rational action, perhaps nothing more than fluids or more if abnormalities are marked. You are taking potassium citrate, I presume, and being safe I see no reason not to do this. If Thailand has no 24 hour urine testing, perhaps you can get tested when visiting other countries. Regards, Fred Coe
HI Dr. Coe. I’m new to the stone world. I think I passed a kidney stone two years ago; went to the ER for discomfort but nothing special was done afterwards. This past July I had over a 1 cm stone in my left kidney with infection. I had the laser procedure to remove it 2 weeks later in after the infection cleared up. Teh problem is I do not know officially what the stone was made of- my urologist keeps telling me it sometimes takes weeks to get a result back; I checked again with him last week but he says he still doesn’t have any results. My 24 hr urine test was somewhat botched because I went to the ER for extreme pain near my left hip during collection time (so IV, urine collection, and throwing up from the pain meds- passed a 2 cm blood clot and a 5 mm stone about a day later). Regardless, I do understand I need to increase my fluids, lower my protein and sodium intake, watch my sugar (also newly diabetic) and am following your Low Oxalate Diet. I just have a feeling I am frustrated that I may never know my stone composition at this point, but keep hoping something comes in. I am also thinking about finding a new urologist and would like to ask you for any recommendations for one in the far western suburbs of Chicago. Thank you.
Hi D., The stone analysis is crucial to planning treatment, and if the 24 hour urine was botched just do another one as it is equally essential. Low oxalate diet is not always important, so wait for the urine results. I am afraid that even though I work in CHicago I am not familiar with urologists in the far Western suburbs; the university of Chicago is far east. Regards, Fred Coe
Hi all. I noticed a question about the MTHFR polymorphism. As a genetic engineer (NOT a physician) with a family that has the C677T polymorphism I know this definitely leads to kidney stones especially in males. I have 100 years of family data. Those that are homozygous for this polymorphism- in my family – ALL have horrible stone issues. Luckily it can be treated effectively. My homozygous son began forming stones at age 8. Appropriate probiotic and methyl B-12 and methyl folate (B-9) supplements completely solved the problem. A good and experienced functional medicine physician will be able to help. If possible obtain the services of a doctor that suffered/s from this same problem and overcame it!!!
Hi Becca, Thank you for responding about this gene variant. On the OMIM site, I could not find kidney stones in this genetic disease complex. Likewise for the NIH Rare Disease site. Can you point me to a reference about kidney stones and this variant so I can post it for others? Thanks very much, Fred
Hi Dr. Fred,
My son’s kidney stones are the result of a mitochondrial disorder of the liver. He has hyperoxaluria – three types of PH have been elucidated but unfortunately we have yet to determine the exact genetic difference/defect that is at play in our family. The heterogeneity of mitochondrial disorders is astonishing- even within my family. Given his MTHFR polymorphism – a poor methylator- we bypass the metabolic gridlock by giving him methyl-B12 injections SubQ and L-methylfolate PO. In addition I apply magnesium sulfate cream tid to support sulfation metabolism that is critical for oxalate detox. I give him probiotics and keep him on a special anti-inflamatory diet to ensure that his gut is sealed so that dietary oxalates do not escape out into his bloodstream as he is already overburdened with oxalates- Many professionals studying this think that the MTHFR gene drives the mtDNA damage/dysfunction in a complex epigenetic way. Initially my son was Dx with “autism” that was actually hepatoencephalopothy. Many of these autistic kids have extremely high levels of oxalate in their urine wether or not they get stones. Scientists are just now beginning to look at these kids and see that in a quite large subset of autistic kids there is a true biological metabolic illness at work & these kids are NOT just mentally defective. So far since the installation of the above medical interventions, he has remained stone free for five years although his urinary oxalate is always high. I know my family’s situation is rare and probably doesn’t apply to your patients but I just wanted to let everyone with a MTHFR polymorphism know about what we’re doing in case it might help.
Hi Rebecca, Primary hyperoxaluria is a serious disease. Can you say how high his urine oxalate level is? I do not know about high urine oxalate in autistic children; can you please provide a reference so I can read it and put it up on the site. That would be very valuable. Fred
Fred,
It would be so wonderful to have a urologist with your experience and desire to really help others study renal disease in these children. They suffer so much! I am just now figuring out how to help my children. If you can direct me to any research you think could help- I will be eternally thankful!
https://www.sciencedirect.com/science/article/abs/pii/S1090379811001541
Hi Rebecca, Thanks for the reference. I cannot get the full paper as it is protected by copyright and my institution does not participate in the consortium. This paper is later and does some more serious work on what high serum oxalate might do about iron binding, which may also be abnormal in autism. But it is about serum, not urine oxalate. I will try to get access to the full article you mention, if possible. Regards, Fred Coe
Hello Rebecca, I would to have contact with you as our son have diagnosis CHD8 (related to autism en mental retardation) but I believe that he have also like kidney stone disease, please send me mail where I can find you on FB and than we could talk about this.
I found a very rare stone in our son his bed, 100% mucopolysacharides, nobody knows until today what this stone means.
Did your son had also genetic test for CHD8?
Hi Ellen, Thanks for commenting. Protein stones are in fact well known, though not common. They are the glycoprotein matrix of stones with so little crystal as to often be unmeasurable. One should still look for crystallization potential using 24 hour urine testing as lowering that may put an end to the protein stones. Regards, Fred Coe
Hi Dr Coe:
Thanks for the excellent website and for all of your work on kidney stones. I’ve had multiple CaOx stones… 68 y.o. radiologist with ileostomy (colon Ca 40 years ago), low urine citrate and low urine pH. I take Tricitrates solution (Kcitrate/NaCitrate/citric acid) 15 cc (15mEq) twice daily (Kcit tabs don’t seem to get absorbed) and 2 liters of water daily (trying for 2.25!). Also CaCarbonate (750 mg) heartburn chew daily. Have Stage 3 CKD (Cr=1.7, BUN=24), mild DM2 (taking 500mg metformin daily), borderline anemia and hyperlipidemia (on rosuvastatin 40 mg and lovaza 1 g). HBP controlled with metoprolol (25 mg) and lisinopril (20 mg). K has been gradually rising since beginning ACE inhibitor (now 5.4). I’m considering taking CaCitrate instead of Tricitrates (to avoid K intake and horrible tasting solution) since HBP meds seem to be working well otherwise (I’ve read that ARBs may cause less K rise and could be better for CKD?). I see cardiologist and nephrologist at JHU but few folks have such specific interest and knowledge as you. Do you have opinion re: CaCitrate or other advice? Thank you.
Hi Dr Rosenbaum, With ileostomy, sodium loads are usually irrelevant – large sodium losses – so I use sodium alkali with abandon. Your 24 hour urine studies can confirm if this is true. If so, you would need neither calcium or potassium as a counter ion. Sodium bicarbonate tablets work, too, and are easy to use for many. Take a look at the article I wrote on this topic. I like Arbs more than ACEs, as a rule, but suspect the rising K is partly from the diabetes. Even so, there is no need to potassium loading. The article shows our published renal pathology in ileostomy, the plugging of tubules is significant and probably contributes to reduced kidney function. So effective reduction of supersaturations is really important. Regards, Fred
If you have uric acid stones that are 80% uric acid and 20% calcium oxalate can you still get them to dissolve with potassium citrate?
Hi Mary, Uric acid will dissolve when urine pH is above 6 so K citrate is for you. I find the calcium oxalate part is often fine grained and passes – but you do need 24 hour urine and serum testing to figure out why you form that as well as uric acid. Regards, Fred Coe
Hi Dr. Coe,
I’ve been forming stones my entire life. I had a lithotripsy when I was nineteen (1986). I currently have a collection of eight or more stones in my left kidney (lower lobe). I usually pass a stone every two-four years. The last one caused months of pain, but was small enough to go undetected on CT scan. I had one of my stones analyzed years ago, but the records are no longer accessible and I can’t remember the results. I recently had 24 hour urine collection test/blood serum. All was normal except urine calcium was borderline elevated and urine high pH was high (7.417). I read in your article “High pH is a risk factor for calcium phosphate stones but one cannot lower urine pH under most circumstances.” Does this mean I’m unable to lower my pH with dietary changes, etc? Thanks very much for your help!
Hi Lisa, High pH and abnormal urine calcium are common causes of stones and the latter is easy to correct. What you need to do is lower urine calcium – how is in the article you posted on – and raise urine volume, using Calcium phosphate supersaturation as your guide. It needs to be below 1. Here is an article on phosphate stones. Regards, Fred Coe
Dr. Coe,
I have a history of developing 100% calcium oxalate stones. My urine output is about 2.2 Liters. My 24 hour urine showed: calcium oxalate crystals at 1.47 DG, within the normal range, but Hydroxyapatite Crystals were elevated at 5.71 DG. Can these crystals lead to 100% Calcium Oxalate stones? My urine oxalate was 30.8mg/24h, and oxalate concentration was 0.35. The only other abnormal results were: urine sulfate- 6, and Urine Urea Nitrogen- 6.4g/24h. Thank you for any feedback and knowledge you may be able to provide.
Hi Jennifer, Your urine oxalate seems quite ordinary, so I wonder if your urine calcium might be high or, possibly, your urine volume a lot lower much of the time from work or play. Yes, calcium phosphate crystals do initiate calcium oxalate crystals, but you have only the latter which means usually volume is low – or calcium high: Take another look. Regards, Fred Coe
Dear Dr. Coe, I would like to know, if there is a meal in front of me that I know somewhat high in oxalate (say 50mg) and I consume the meal with plenty of lemonade (stevia sweetened, no sugar) and a 250 mg calcium citrate supplement, would that effectively “cancel” some of that oxalate in the food, provided I drink plenty of fluid throughout the day also?
Hi Alex, I presume you form calcium oxalate stones, and your urine oxalate is above normal so that diet oxalate is a serious issue for you. In that case, the better approach is to just use the US normal amount of diet calcium – 800 – 1000 mg/d from foods – so that meals with oxalate in them have calcium containing foods as well. The lemonade is irrelevant to oxalate. This article focuses on the calcium, oxalate axis. Diet sodium is crucial in many patients to control urine calcium. Just to be safe, here is my best on evaluation so you can be sure the causes of your stones are fully defined. Regards, Fred Coe
Hello Dr. Coe
I am 57 & never had stones knowingly until recently, when I had pain that was mis-diagnosed as possible prostate inflammation, then 3 months later a CT showed maybe 20 Caox stones between the 2 kidneys.
3 surprisingly punishing ureteroscopies in less than a month (those stents are fun aren’t they), and I’m clear for now.
For years leading up to this I had been trying to get in shape & do the right things as I headed towards the big 60, so a shake a day with spinach, rolled oats + soy & pea protein powder; Fruit’n’Fibre for breakfast; 70% dark chocolate rather than other sweet stuff, yadayada.
As many others, had never heard of oxalates but was clearly caning them unknowingly.
Am due to do the 24 hour urine & follow up in the new year.
My question therefore is this. Can a person who is overloading on oxalates develop stones because of this & not necessarily be a “Stone former”?
It would be nice to think that I could get back to a normal life & not worry too much about future episodes. I have of course cut out the uber oxalate stuff, and have no family history regarding stones.
Your site is absolutely top drawer by the way, and I’m sure I speak for many by saying thank you for your time, energy & experience.
Hi Kevin, It may be that you just did too much oxalate. The 24 hour urine testing will help decide this. Be sure and get fasting blood for calcium and that should be normal, below 10 mg/dl. Perhaps the urine will show other abnormalities, or even higher oxalate despite your changes. Measurement is the only way to guide treatment. Good luck, Fred
Hello Dr Coe, my name is mutarr I’m from The Gambia west Africa, last year I realize I had a 1 cm stone stock in my ureter, I did Ureteroscopy stone fragmentation and I had 16 small fragments in my kidneys and i have passed all of them expect 4 and they seems to be getting bigger and am at risk for another surgery, we don’t have the facilities for test likes 24 hour urine collecting and sadly our urologist aren’t quipped enough to help us stone former’s to prevent new stones and currents stones from get bigger, I’ve no idea of knowing what kind of stones I’m forming, few days ago I did a urine and serum profile but wasn’t a 24 hour urine collection and my serum results were fine but my urine result were all high, i fell lost and helpless, I’d really appreciate an advice from you, thank you mutarr from Africa..
Hi Mutarr, I believe I have answered this – belatedly! – in subsequent notes. Sorry for the delay. Fred
Dr Coe
Do you recommend or have any thoughts about a product called Rowatinex? It has gotten 1000’s of good reviews for stone breakup. I currently have 3 stones, 3mm, 5mm and 9mm and am looking for ways to eliminate these from my life. Thank you for all you do!
Hi Greg, I have not studied this material but in general all those I have studied lack convincing evidence for efficacy. Regards, Fred Coe
Hello. I was diagnosed May 2023 with a 4mm stone and told to f/u in 6 months. In November I ended up in the ER with severe pain and hematuria. The CT scan showed a 1.2 cm stone and a 2 mm stone. I had a serum Ca level of 10.3, and the u/a showed 2+ calcium oxalate. One week later I had a CRULS procedure. I saw my urologist post-op and there were no stones noted on KUB, but a “gas cloud” over the kidney. He had me come back in one month for an u/s, and there was no hydronephrosis but but there was a 6mm stone that had already formed. At this point I reminded him I had a slightly elevated serum calcium level in the ER, and asked for testing to determine what was causing me to make stones so quickly. I am a nurse so I have a wee bit of knowledge. I did ask if we could check a PTH while awaiting the 24 hour urine, that was 23. He did not order a serum Ca level at that time, but coincidentally I had f/u labs by another provider that I needed drawn which included a CMP, so I had them all done at the same time. My Ca was 9.3. The 24 urine results are as follows:
Urine Volume- 2.36
SS CaOx- 10.16
Urine Ca- 583
Urine Oxalate- 44
Urine Citrate- 1474
SS CaP- 2.80
pH- 6.331
SS Uric Acid- 0.41
Urine Uric Acid- 0.929
Na- 281
K- 24
Mg- 24
P- 1.026
Nh4- 4.24
Cl- 279
Sul- 37
UUN- 13.42
PCR- 0.9
Cr 24- 1805
Cr 24/kg- 15.9
Ca 24/kg- 5.1
Ca 24/Cr 24- 323
Hi Megan, From the urine your calcium loss is massiv. Partly that might reflect the high sodium intake of 281 mEq/d. Your weight seems to be 113 kg (creatinine 1805 mg.day, creatinine /day per kg body weight 15.9) si part if the high calcium is size, but it is very high per gm creatinine. Your serum calcium is uncertain as you have high and normal values, and a normal PTH. The NH4 is a type at 4.24, the value must be 42.4. Your high citrate perhaps reflects insulin resistance, your low urine magnesium of 24 and potassium of 24 are remarkable and suggest a major kind of diet issue I cannot say more about, or even perhaps some bowel issue for their absorption or excess prior losses from diuretics, proton blocker use for GIRDS, or even alcohol. In other words the data point to complexities I cannot know about but your physicians need to sort out for you. Regards, Fred Coe