 Agonizing, intolerable, miserable, excruciating, stabbed with a knife, worse than childbirth.
Agonizing, intolerable, miserable, excruciating, stabbed with a knife, worse than childbirth.
As a urologist specializing in the treatment of patients with kidney stones I have learned a new lexicon exclusive to stone formers describing bouts of renal colic.
Pain, the hallmark symptom of stone disease, accounts for over one million emergency room visits by such patients in the United States each year.
Over the past several decades considerable progress has been made gaining insight into the physiology of renal colic and optimizing methods to treat it. However, despite improved scientific explanations we as clinicians still lack a perfect understanding of why it occurs.
PAIN FROM STONE PASSAGE
Patients have been suffering from renal colic secondary to stone disease for over two thousand years. As a matter of fact, it is remarkable how little has changed in its clinical presentation over this time period. In 400 B.C. Hippocrates referred to it as first disease of the kidneys. He was one of the initial observers to comprehend the association between urinary obstruction and pain, writing:
An acute pain is felt in the kidney, the loins, the flank and the testis of the affected side; the patient passes urine frequently; gradually the urine is suppressed. With the urine, sand is passed; as the sand passes along the urethra, it causes severe pain which is relieved when it is expelled; then the same sufferings begin again.
We have since come to appreciate the complex physiologic basis for this relationship at a much deeper level.
How Pain Begins
 The first step in this process is acute obstruction, most commonly from a stone. But in stone formers masses of crystals can create obstruction, as can blood clots if bleeding is particularly brisk.
The first step in this process is acute obstruction, most commonly from a stone. But in stone formers masses of crystals can create obstruction, as can blood clots if bleeding is particularly brisk.
Urine from the kidney can no longer pass to the bladder and as a result builds up and stretches the proximal – closest to the kidney – ureter and renal collecting system. This stretch activates nociceptive nerve fibers – fibers which sense injury – within an entire neuronal network located submucosally in the renal pelvis, calyces, capsule and ureter.
Figure 1 (left) – Example of obstructing proximal ureteral stone with dilation and stretch of the collecting system above the level of obstruction.
These fibers then transmit afferent signals to the T11 – L1 spinal cord which the body interprets as pain at the corresponding level of neuronal activation. As the stone migrates from the kidney down the ureter and towards the bladder, pain usually shifts downward as well. It is commonly sensed as high as the upper flank when the stone is lodged in the proximal ureter and as low as the labia/testicle when down near the uretero-vesical junction at the entry to the bladder.
Patients passing stones may experience other symptoms in addition to pain. Many of the nerves involved in the process of obstruction are intimately linked to innervation of adjacent organs, for example the gastrointestinal tract. Cross activation of these associated nerve fibers has been proposed as an explanation for the nausea and vomiting which so often occurs in the setting of an acute episode of renal colic.
In rare instances patients may even have alternative symptoms without any pain at all. In some cases, particularly when the stone is at the uretero-vesical junction, urinary symptoms predominate and the only appreciable symptoms are urinary frequency, urgency and discomfort while voiding. These symptoms mimic urinary infection and often result in temporary mis-treatment with antibiotics until the correct diagnosis is made.
What Happens Later
Increasing renal pelvis pressure from persistent obstruction causes a release of prostaglandin E2. This chemical mediator of injury response produces a perfect storm.
It causes ureteral hyperperistalsis (increased intensity of the waves of coordinated ureteral contractions which normally drive urine down to the bladder) and eventually even ureteral spasm. It also leads to dilation of the afferent arterioles – those tiny resistance vessels which control the flow of blood into the capillaries of the kidneys.
The arteriolar dilation increases blood flow to the kidney and promotes a temporary diuresis just as ureteral smooth muscle hyperperistalsis and ultimately spasm tighten the ureter around the stone and worsen obstruction. Spasm leads to lactic acid build up, as occurs when any muscle is over-exercised, and sets off an inflammatory cascade that itself can worsen pain.
With time, blood flow to the affected kidney falls, even though the arterioles which let blood into the renal capillaries remain dilated. It falls because the efferent arterioles, which let blood out of the capillaries where filtration occurs, begin to constrict and raise filtration by the renal glomerulae. The increased filtration maintains and can even raise pressures.
Figure 2 – Diagram of blood flow to the nephron. Blood enters through the afferent arteriole and is then filtered within the glomerulus, producing urine in the process. Blood exits through the efferent arteriole. Both the afferent and efferent arteriole are able to dilate and constrict in order to regulate pressure and ultimately filtration via urine production.
In many ways, this complex system is analogous to the soaker hoses many people use to water their lawns. The afferent arterioles are the faucet the hose is connected to and the efferent arterioles are the opening at the end of the hose which can be closed or left open into a sprinkler.
Filtration is the many tiny flows of water all along the hose which keep the grass growing.
When working appropriately, the faucet and the end are both open and water (urine) is produced at a slow, constant rate (Figure 4 – left). With an obstructing stone the faucet – so to speak – is opened more and the end clamped more so more fluid – water – is filtered out along the length of the hose at high pressure (Figure 4 – right). In the kidney this filtration is into the nephrons and raises pressure. When the clamp is tightened, the total amount of flow through the hose can fall just as the amount of water filtered out along the hose rises.
Figure 4 – Soaker Hose Analogy to Renal Blood Flow and Filtration. On the left, there is little pressure in the system and water (urine) seeps out slowly from along its length. On the right, the inflow is much higher than the outflow and water (urine) shoots out from along the hose at exceedingly high pressure.
Three Phases of Pain in more Detail
The Physiology
No discussion regarding ureteral obstruction would be complete without the work of E. Darracott Vaughan, who characterized the physiology of urinary obstruction in the 1970’s.
Assuming two functional kidneys, the physiologic effects of acute unilat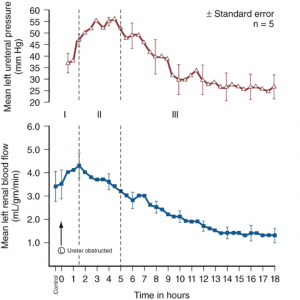 eral ureteral obstruction can be marked by three distinct phases.
eral ureteral obstruction can be marked by three distinct phases.
In phase one, the effects of the inflammatory cascade described above cause a progressive rise in renal blood flow and renal pelvis and ureteral pressure. This phase lasts for approximately one to one and a half hours. This is the portion where the afferent arteriole – the faucet – is maximally opened.
Phase two is marked by efferent arteriolar vasoconstriction which causes a decrease in overall renal blood flow but an increase in ureteral pressure for up to five hours. The faucet is opened and the end clamp is tightened.
Phase three is marked by a further decrease in renal blood flow to the affected kidney and ultimately decreased ureteral pressure. The end clamp is progressively tightened so blood flow to the kidney is reduced enough that filtration and urine production begin to fall, and pressure with it.
Measurements of ureteral pressure (red) and renal blood flow (blue) after onset of acute unilateral ureteral obstruction. (Courtesy Campbell-Walsh Urology, Tenth Edition, Elsevier Inc.)
The fall in blood flow is not injurious during an acute attack, but over time it can be. This means that relief of an obstructing stone is an important matter. Commonly stones pass of themselves. But stone attacks need medical attention because if the stone continues to obstruct it must be removed.
The Symptoms
It is easy to conjecture how these three distinct phases correlate clinically to the symptoms experienced during an acute episode of colic.
The onset of pain classically correlates to phase one and the inciting obstructive event. It is at this point that the patient commonly seeks care in the emergency room or physician’s office.
The pain classically persists at a severe level for several hours (phase two) but ultimately subsides, at least partially (phase three).
In many instances pain comes in waves, potentially a sign of intermittent obstruction activating the above pathway each time urinary flow is obstructed. This occurs through a combination of the stone moving and the tensions of the ureter with increases or decreases of muscle spasm.
THE CONUNDRUM – Pain Without Obstruction
Opinions of Urologists in General
Though the physiologic basis of pain in the setting of obstruction is clear, it does not provide an explanation for one of the most commonly encountered conundrums in stone disease – the symptomatic non-obstructing stone. These can be actual free stones that have not passed, stones attached to plaque, or actual plugs in the kidney tubules that are massed together enough to show up on a CT scan as ‘stones’ though actually tissue calcifications.
There is perhaps as much variation in clinical opinion in such instances as any other clinical scenario in the field.
If one were to ask a group of urologists whether they believed that small nonobstructing stones could cause renal colic, opinions would range from absolute certainty to complete dismissal of the concept altogether.
What Happens to Patients
As a result, there is no standard of care regarding how to optimally manage such patients. In all cases it is first imperative to rule out other potential sources of pain; however, such workups often end with the same result – a patient with bothersome flank pain and evidence of one or more nonobstructing stones on imaging.
Lacking a physiologic explanation to explain their symptoms, patients with pain and non obstructing stones are often sent for detailed workups, secondary and tertiary consultations and referral to pain specialists and even psychiatrists. However, in an age where flexible ureteroscopy can be performed quite safely and on an outpatient basis one must wonder whether such patients are being treated appropriately.
A Specific Example
As an example, I recently met a patient who had been referred from several hours away seeking a fourth opinion regarding her chronic flank pain. For months she had suffered from a severe ache in her left flank that had limited her ability to work and live her normal life.
She had attributed the pain to a 7 mm lower pole nonobstructing renal stone on that side which was discovered on a CT scan during her initial presentation to an outside emergency room (Figure 3). However, none of the physicians she had seen agreed with her self diagnosis.
scan during her initial presentation to an outside emergency room (Figure 3). However, none of the physicians she had seen agreed with her self diagnosis.
Figure 3 – CT image of left lower pole nonobstructing stone (red arrow). There is no evidence of obstruction or inflammation around the kidney.
In the ER she was given narcotic pain medication and sent home to follow-up with a urologist.
The first urologist she saw told her that while the stone was visible, its location within the kidney meant that it could not possibly be causing her pain. He refilled her prescription for pain medication and sent her to see a pain specialist.
The pain specialist tried physical therapy for what he thought may be a musculoskeletal source but ultimately this did not prove effective and she was given more pain medication.
She later sought care from a second urologist who also told her that the stone could not possibly be causing her pain in the absence of obstruction. This time however she was accused of having an agenda and seeking care specifically to get pain medication. Similar visits to a variety of emergency rooms elicited more CT scans as well as accusations of seeking pain medications. Each CT result was the same though, all demonstrating a 7 mm non obstructing left lower pole stone.
On one instance a treating practitioner even admonished her, saying that nonobstructing stones don’t cause pain and he should know since he too had been diagnosed with such stones incidentally on a CT scan.
Ultimately she made her way to the clinic for consultation at which point she was offered a ureteroscopy and stone removal. The procedure went well and she was discharged with a stent for one week. She was last seen back 5 weeks after the procedure and reported complete resolution of her pain. She was no longer taking any pain medication whatsoever and there was no evidence of any stone or hydronephrosis on follow-up imaging.
What is Known to Date
Such patients are frequently encountered. Despite a lack of physiologic explanation as to why these non-obstructing stones may cause pain, there is emerging evidence that they do and therefore that removal can cure it.
In 2006 Taub et al. described outcomes of twenty such patients who had chronic flank pain as well as radiographically evident calcifications within their papillae without obvious collecting system stones. Ureteroscopy with laser papillotomy to unroof and remove all evident stone was performed on twenty seven kidneys. Pain improvement was seen in 85% of cases with a durable improvement for greater than one year in nearly 60% of cases.
This study was then repeated on a multi-institutional level with 65 patients undergoing similar procedures over a ten year period. Overall there were 176 procedures performed in this cohort with patients reporting less pain after the procedure 85% of the time. The mean duration of response was 26 months with 60% of patients having sustainable improvements in their pain levels for over one year.
Finally, this clinical scenario is seen commonly enough that it garnered its own nickname at Massachusetts General Hospital where it has been described as “small stone syndrome”. In a retrospective review of patients treated there with ureteroscopic removal of small nonobstructing stones (<4mm) for reasons related to chronic pain, 11/13 patients reported being pain free after the procedure with the other two noting a partial response.
What I think
We still do not completely understand the physiologic explanation for pain in these patients. However, much like Hippocrates over two thousand years ago, clinical observation often precedes scientific understanding. In this regard it is unfair to dismiss the notion that small non obstructing stones can elicit legitimate renal colic.
Physiologic breakthroughs in the understanding of pain signaling and inflammation are currently happening at a rapid rate and it is likely that in time we may be able to better decipher which non-obstructing stones are truly responsible for symptoms. However, until then, such scenarios will continue to be a commonly encountered clinical complexity for urologists.
For the time being I would still advocate consideration of alternative causes of pain in such situations including urinary infection, obstruction and malignancy. A careful history is critical to rule out non-urologic sources such as pathology within the musculoskeletal, pulmonary, gynecologic and gastrointestinal systems. Another important element of the history is whether the patient has previously passed a stone and if the current symptoms are similar to that experience.
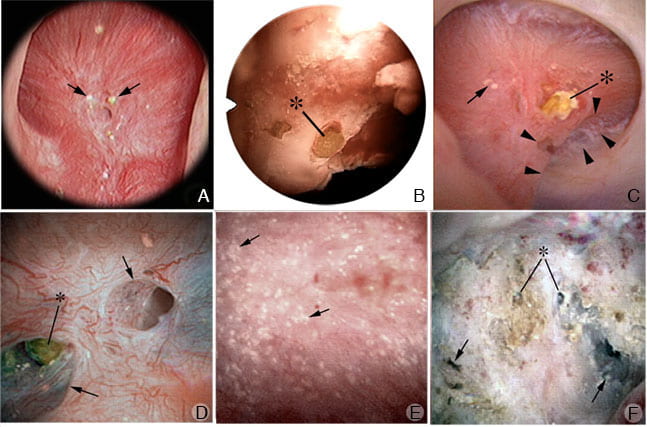
Once other explanations have been ruled out, offering stone removal is entirely reasonable. This not only has the potential to improve pain but may also decrease the risk of future stone growth or spontaneous passage at a later date. In such instances, I prefer flexible ureteroscopy with stone removal to shock wave lithotripsy. First, ureteroscopy maximizes the likelihood that all stones can be identified and removed which is especially important in the event that pain persists after the procedure. Second, with ureteroscopy one can inspect the inside of the kidney in high definition which has the potential to offer information not readily available on x-rays and CT scans such as embedded stones, tissue calcifications, and other pathology (Figure 4).
Figure 4 – High definition images obtained during renal endoscopy demonstrating tubular plugging (stones embedded in the kidney) (Courtesy: AE Evan, IMCD and BD plugs: Do they have a role in stone formation).
Finally, it is critical to establish realistic expectations before surgery in regards to pain control. Our understanding of this concept is in evolution and the published literature suggesting a treatment response is limited to relatively few patients. However, as science and history have shown us, just because we don’t fully understand the connection doesn’t mean it doesn’t exist.
More You Might Like
What Kidney Stones Are
Types of Kidney Stones
Do We Need to Analyse All Those Stones?
How Kidney Stones Form
When Crystals Plug The Kidneys
Medullary Sponge Kidneys


Thank you. 24 hour urine test coming up soon.
Over the past 4 years as well as during all 3 of my pregnancies, I have been on a very painful and often frustrating journey very similar to the story recounted of the woman with nonobstructing stone and pain. I’ve researched this topic quite a bit in an effort to better understand my pain, and had to become my own health advocate. Having finally been diagnosed with Medullary Sponge Kidney this past year, my urologist performed a papillotomy on my affected kidney. The pain relief was very notable, but only lasted about 1 month before my symptoms cropped up again. My urologist, while very understanding, tends to be of the camp who believe that nonobstructing stones cannot cause pain. It has only been since I started a regimen of lemon juice in my diet that the pain has mostly disappeared and I’ve been able to get my life back.
Dear Ashley, Thank you for sharing your experience. I am glad things seem to have improved. Fred Coe
Thankful for this article! I have chronic pain associated with small stones. I have medullary sponge kidney and hope to see research for people like myself struggling to making it through each day with the pain I experience with this disorder. I can’t even tell you how much it means to me that you have validated pain with non obstructing stones. It’s real and doctors need to understand this.
This is a great article! Thank you 🙂 I have MSK and pain without obstruction has been a huge part of my life
Hi Ivelisse, I am glad the article is valuable. See the comment to Celia, which is above. You may have MSK or tubule plugging. It is hard to tell except at stone surgery. Good luck with your treatment, and I hope your pain condition is under good control. Fred coe
May I ask why you do not mention Medullary Sponge Kidney in your article on chronic pain,? although you do talk about calcifications, embedded stones, in the link to “For Scientists” there’s an article entitled “Tubule Plugging” which talks about plaque, but nowhere do I see mention of MSK? As far as I know, these are all characteristics of MSK!
Hi Celia, Medullary sponge kidney is a developmental anomaly of the most distal – last parts – of the nephrons, and a special kind of disease. It is true there are calcifications seen on radiographs but in fact the correct diagnosis is not made not that way but during ureteroscopic examination of the kidney during stone removal. The calcifications are mostly dilated cystic collecting ducts filled with innumerable tiny microscopic round ‘stones’ each perhaps a millimeter or so in diameter. If the surgeon unroofs such a duct with a laser they come rolling out like tiny marbles on a table top. They are not embedded in the tissue. The tubule plugging Andy Evan describes is something very different. Patients who form calcium phosphate stones acquire this kind of plugging, which is not a developmental abnormality of how the kidney is formed but a damaging collection of crystals inside the kidney tubules. I am sorry we do not have an article on MSK on the site as yet. This site is in evolution, being built in public one might say, and I nor any of my colleagues has as yet written such an article. Here is a link to our recent publication on MSK. As you can see from the abstract is is quite new so we are just ourselves becoming clear about the disease. Thank you for the very thoughtful question, Fred Coe
“Another important element of the history is whether the patient has previously passed a stone and if the current symptoms are similar to that experience.”This is the most important part of your article…ask your patient. Let them describe their pain and history. Observe them for signs of fatigue or paleness, clammy skin, etc. And remember that they may have their pain under control while they are in front of you. I had some relief with bucket loads of Advil.
I am currently waiting for laser lithotripsy for a 1.5CM stone. I had horrid pain and nausea starting on May 15. My previous 2 stones caused me several hours of pain and then the stone moved and I passed them without incident. This one..the pain was unrelenting and causing nausea. I went to the ER day 2. All they did was a urinalysis. I had to jump through hoops all week long to finally land in a urologists office who recognized how ill I was and who did an urgent stent placement. My pain absolutely was not the same as my other stones…it was worse and it wouldn’t stop. It was because this large stone wasn’t moving and my kidney was working hard to pass urine and to move the stone. No wonder! I got lousy care at the ER, and had to go through my PCP for the necessary testing, wait 2 days for results…all this time I was very sick. Here is my blog about my experience. I can’t wait to have this behind me. http://mcclearymrsaprevention.com/?p=1594
Hi Kathy, You are correct, in my opinion, that one should ask anyone who has had a stone if the new attack is like the other ones. I think patients always know stone pain, and are an ideal source of insight. As for your unfortunate experience, I am very sympathetic and sorry you had such an ordeal. You are very kind to share your blog with others. Fred Coe
Thank you very much for getting back to me Fredrick Coe and thanks for the useful information! I belong to one of the fb MSK support groups, altogether in the various groups, there are over a thousand MSK patients most of whom suffer from daily chronic pain and fatigue not to mention many other common symptoms.
Dear Celia, I had not until now known about the large numbers of patients with chronic pain from stones that are not obstructing the urinary tract. It is indeed a very important matter, and I will do everything I can to make this issue clear to the stone research community in hopes of furthering better treatment. Regards, Fred Coe
I appreciate your article and I too have MSK. Its a disease that gets played down as just kidney stones. I have had 24 kidney surgeries with various types of stone removal. Hopefully you will find an accurate publication about MSK. It’s a disease that isnt given the credit it deserves. Debilitating, well thats just the start of the MSK nightmare. I would love to see a study about the possibility that MSK is more autoimmune than exclusively kidney. The symptoms shared by other MSKers are so great its hard to not pay attention to it. There may not be very many with MSK, but I can promise you there is a screaming need for more research. Thank you for your research so far. I hope you will hear enough pleas from the msk community and decide to dive in deeper into the lonely msk world. Thank you
Dear Jaime, Our group published a recent paper on MSK which details its rather specific anatomy and points out how it is via modern digital ureteroscopy that MSK can be distinguished from other diseases which resemble it on radiographs but are in fact different in their character. A link to the paper is in my response to Celia MacDonald just below. We are planning an article for one week from this coming tuesday on the MSK anatomy and surgical appearance and how it differs from other diseases with many stones and tissue crystals. Regards, Fred Coe
Thank you for your work and articles on the physiology of pain. I have MSK, nephrocalcinosis, incomplete RTA, and chronic uti’s & chronic pain. Although this article speaks of pain
with unobstructed stones, it also indicates this pain is resolved with
removal. The pain I have is daily. I
have had 9 lithotripsy, and about six
ureteroscopies. The last two were
to remove embedded calcifications in the calyx. Which do
you think is the most likely cause of pain that is daily and for years. The
surgeries?, possibly traumatizing the
kidneys? Or nephrocalcinosis?
If nephrolithiasis can cause pain would
it stand to reason nephrocalcinosis
could be the cause of the chronic pain. All this being said because the medical books claim MSK does not
cause pain. Then where is it coming from? I make calcium phosphate (apatite & brushite) stones. Could it be that there are two types of MSK? One that is simply MSK and one with added complications? Also, is it possible to misdiagnose MSK when it is plugged tubules? We have about 800 people in our MSK support group and half if not more have pain, fatigue, and complications. Thank you again in advance for any light you can shed on this complicated and misunderstood disease. Best regards, Laura
Dear Laura,
Thank you for sharing your history, your situation sounds quite distressing and I hope that ultimately you are able to find relief. Your questions are excellent and honestly I am not certain we as a field are able to provide the answers you seek at this moment in time. The entire concept of pain from non obstructing stones is very controversial; though clearly given the number of people who share stories similar to your own there must be something to the matter that we do not yet understand.
One thing you mention that caught my attention was the fact that you make brushite stones. This in its own right can be a clinical challenge as these stones tend to be more difficult to treat, faster to recur, and have associations with metabolic abnormalities. There also seems to be an association between these stones and abnormal appearing kidneys on endoscopy, though not necessarily MSK. Your point about differentiating tubular plugging from MSK is important and I would encourage you make sure that you are being followed by a provider specializing in the metabolic aspect of kidney stones to make sure your risk of forming more stones is minimized.
Sincerely,
Mike Borofsky
Thank you for the article and the efforts to understand pain with non-obstructing stones . If a patient has msk, nephrocalcinosis, incomplete distal renal tubular acidosis, nephrolithiasis, chronic uti’s and chronic flank/back pain, along with having had multiple lithotripsy and multiple ureteroscopies. In your opinion, since non-obstructing stones can cause pain could you say where the chronic pain might be coming from? Trauma from many surgeries? Could it be the nephrocalcinosis since that is non-obstructing and always present? Also, as far as the health of the kidneys go do you believe that more surgeries would be beneficial or detrimental, to try to remove more calcifications embedded? It would be awesome to have msk included in future studies as many suffer from it and are in daily pain with non-obstructing stones. Also, to link msk with nephrocalcinosis instead of it being said that msk is considered harmless, I think it is so important to have all urologists and nephrologists start to understand in the way that Dr. D. Goldfarb and Professor Giovanni Gambaro do that Msk can have many symptoms and be a very painful and debilitating disease. Thank you for your time and best regards. Most of the various kidney foundations have outdated information regarding Msk. This should be changed. Laura
Dear Laura,
Your concerns are well noted, have faith that there are many people within the kidney stone community who share such interests and are currently trying to better understand this challenging situation. I am hopeful to touch on some of the issues you raise in an upcoming post on specifically on MSK. I believe the term is MSK is often used to describe a variety of challenging clinical findings among stone formers including ductal plugging, nephrocalcinosis, and high stone burdens, when in fact these all may be separate entities that require tailored treatment strategies. In regards to whether or not more surgeries would be beneficial, this is something that must be addressed between you and your urologist on the basis of pain relief, evidence of stones on imaging, and other clinical issues.
Sincerely,
Mike Borofsky
Is there also a theory for the phenomena of ‘silent’ ureteric stones found on routine imaging with variable degrees of obstruction.
Hi Derek, certainly we have all seen ‘silent’ stones in the ureter, often not obstructing and sometimes having lodged in the ureter wall. Partially obstructing stones are also sometimes without symptoms, and most ominously a kidney can be obstructed with loss of the organ and symptoms did not lead to early discovery. The main message is watchfulness. New pain, new bleeding, or any other suspicion surely warrants a call to one’s personal physician. Ultrasound is without radiation risk and often will identify a stone or obstruction. Fred Coe
Anything new on cystine kidney stones.
Hi Cathy, I am sure you saw Anna’s introductory article. I wish there was some new treatment hoving up on the horizon, but…not right now. A quick check of PubMed came up empty, too. Regards, Fred Coe
I think I might have a “small stone”story. I am a 55 yo in good health on no meds and recently passed my first kidney stone. I still have a 6 mm non-obstructing stone on CT scan. I have had moderately severe intermittant right back /flankpain for the past year and occasional bouts of nausea. I thought the back pain was MSK in origin as it got better with hot packs and motrin. It also seemed to get worse when I was doing a shift in the ED (no breaks, usually dehydrated, main source of nutrition Bare Naked juice which incidentally gave me 20-40x RDA of vitamin C). Pain bad enough that I’ve needed to take motrin 1.8 grams daily on and off for past year. The nausea I figured was due to peri-menopause.
Since passing the stone, I have no back pain if I hydrate but get nagging flank pain if I don’t drink adequete fluid. I haven’t had any more nausea, I also have lost 4 pounds in a week without trying- by far the most I have ever lost. I am wondering if the constant inflammation increased my insulin resistance or impacted my weight in some other way.
Hi Holly, Thank you for the story which is very instructive. All of us wonder about ‘non obstructive’ stones, whether there is inflammation, papillary surface injury, or other, and about the role of pre-emptive surgery. Frankly I think a surgical trial is reasonable and likely to be organized. Until then the matter is a bit moot; will surgeons and patients want to take the chance of doing a procedure without some strong reason to believe the benefit is likely and substantial? If I may add a small point, now that the stone has passed, please avoid dehydration and maintain a high fluid intake. New ones can form. Best wishes, Fred Coe
I am a 24 year old who has been to the doctor and emergency department for a small stone….. i dont know if it’s obstructive or not but let me tell you, the pain has been ridiculous. They had me on a morphine drip for the fact I couldn’t handle the pain and something for nausea due to the fact of throwing up everything I put in my system….. they then refused to tell me which junction the stone was at but just said it was at a junction and that’s why I was so miserable. The stone is 2 mm and I’ve honestly been hurting so bad I almost asked my room mate to cut my kidney out that’s how painful this is. I’m shaking tired and frustrated at the fact it’s been over 3 months and I haven’t passed it and just been in pain dealing with night sweats, sleepless nights, vomiting, nausea, and severe dehydration because I can’t keep fluids down.
Dear Brandon, It would seem that this has gone on too long and it is time to do a urological procedure to remove the stone even if it is not obstructing the ureter. I would insist on it, if I were you. Three months of pain is too much. Fred Coe
Brandon; my stone is also 2mm and causing me similar amounts of pain plus the sleepless nights, sweats, nausea etc. Anti-biotics have helped a little with the referred infection but today I feel bloated and was in so much pain at work I had to lie down. Let’s hope we both get our situations sorted out so we can lead happier lives!
Thanks for this information; so interesting to read the article and the comments especially about small, non-obstructive stones. I’m a 31 year old female who has always been very healthy. In the past 2 months I’ve been getting pain, predominantly on my right-hand side. It is mostly flank pain with some referred pain down to my lower back/groin area. I’ve also had a low fever, shakes, sweats and just generally feeling run-down. I ended up in emergency twice. They tested me for EVERYTHING and all they can find is a 2-3mm non-obstructive stone in my right kidney plus a small one (I think 1-2mm) in my left kidney. I’ve been referred to a urologist and a nephrologist. The urologist said I have a virus and the nephrologist diagnosed me with pylonephritis and put me on an antibiotic. I think I did have a bit of nephritis as the antibiotics have helped with a lot of the referred symptoms (shakes, sweats, nausea etc.) but I have still got the pain after all this time! I have a feeling the pain is from the stone as they can’t find anything else….but the problem is convincing a doctor that this is the case! Not ONE doctor I’ve spoken to whether specialist or otherwise has believed that the stone would be the cause of my problems. Any ideas about where to go next or what to do? How do I find a doctor who will actually listen?!
Hi Anna, Of course, at this distance I cannot tell you what is wrong, but the fever and shaking are compatible with infected stones or infection behind a stone that is partly obstructing within the kidney. The stone pain from small stones that Mike described in his article did not include fever or what appears to be chills. Surgeons differ about the pain of non obstructing stones, and I am not a surgeon, so my advice is this: If the pain goes on too long, write directly to Mike Borofsky who wrote the article and ask him about surgeons who share his opinion and might be reasonable consultants for you. If the fever and chills come back, that is another matter and your personal physicians will no doubt treat you for infection and need to track it down to its source, wherever that may be. Fred Coe
Thanks so much for your prompt reply! You’re right in that i definitely had an infection on top of the stones; it’s just a matter of which came first. Now the infection has cleared up but I’m left with the flank pain. What would be the best way for me to get in touch with Mike Borovsky?
Dear Anna,
Thanks for sharing your story. As Dr. Coe stated it is always somewhat of a challenge to give medical advice in such a forum as the remainder of your history, lab work, physical exam and medical imaging are essential to guiding the most appropriate treatment. That being said we see many patients like you so I am happy to share my thoughts on a general level. In my opinion, if other potential sources of flank pain have been considered and ruled out including musculoskeletal and gynecologic sources and all that you are left with is evidence of a stone then it is reasonable to consider a ureteroscopy to remove it. This procedure also allows your surgeon to take a detailed look around your kidney which can be quite diagnostic in its own right as detailed elsewhere on this site. Another reason to consider removing the stone is your history of infection. Stones are foreign bodies and in the presence of infection often become seeded with bacteria which is hard to clear with antibiotic therapy alone. This is especially true if you are suffering from recurring infections, particularly with the same bacteria which would indicate that the stone may in fact be the source. Of course, ureteroscopy is an invasive procedure and is carries with it its own risks, but that will have to be discussed and considered further with your treating urologist. I hope you find this information useful and wish you the best.
Sincerely,
Michael Borofsky
Thanks so much for you thoughtful comment, Dr. Borofsky. I will print this article and our conversation and will try to find a urologist that shares your opinions. To answer your question, yes, I’ve had an ovarian/uterine ultrasound which shows everything in that area is working perfectly and muscoskeletal sources were also ruled out whilst in one of my emergency room stays. On top of that I have a history of childhood nephritis which I’ve told multiple doctors who still claim the stone could not possibly be causing my constant infections. Hopefully I’ll find the right urologist to share your sentiments.
Thanks so much for your thoughtful reply. I will print this article as well as our conversation trail and hopefully try to find a urologist who will share your sentiments! To answer your query, yes, I have visited a gynecologist who gave me a uterine/ovarian scan which showed everything is functioning perfectly in that area. Musculoskeletal factors were also ruled out whilst in one of my hospital stays. On top of this I have a history of childhood nephritis which I’ve told doctors to no avail (I thought maybe this would mean I’m more at risk of infections from a stone). Hopefully I’ll have some better luck with finding someone to help me. Thanks again!
This may be a long shot but you don’t know the names of any good urologists in the Asia/Pacific region, do you? If not I’ll just do my own investigation. I’m in Australia (a long way away)!
Hi Anna, I do not. But, Mike Borofsky probably does in that urologists travel a lot and tend to know one another. He has been on the site a lot and is easy to find. Regards, Fred Coe
I was curious as to the best way to contact Dr. Borofsky regarding this article?
Hi Jenny, I am a bit hesitant to put email addresses of others on the site, but Mike is at Indiana University Indianapolis (IUPUI) and easily located on the web. Likewise we have a facebook site kidneystone docs with him on it. I suppose I am being squeamish, so forgive me. Best, Fred Coe
I’m a 28 y/o, female. I had my first kidney stone in Aug 2011. It was 10mm, obstructing, wbc 26, in renal failure. Immediate surgery for stint placement, contacted a super-bug in my lungs and 36 hours later was back in the hospital with a o2-38%- spent over a week in ICU and then on the floor for about a week. A month later, I had lithotripsy. Since then, I’ve had at least 17 surgeries for kidney stones and had one urologist go in and empty out all of the stones in 2013. I have kidney stones in both kidneys. My kidneys hurt all of the time. I went from being a full-time student and employee to no life whatsoever. I haven’t worked since Aug 2011 and there’s no way I could be relied upon to even run an errand. I’m not sure I’ve been without an infection since this first began. I’ve been on antibiotics on and off the entire time. In fact, they rarely even have an effect big enough to knock out the infections completely. I’ve seen 6 specialist and the one who retired is the only one who gave me any sense of hope. He was the one who emptied out my kidneys and believed that it truly does cause pain. *note: he retired.
Back to square one.
I’m entirely too young to be laid up on the couch or in the bed or even in any kind of discomfort that would keep me from living like a 28 y/o should. Then, to have anyone tell you that there’s no way you could hurt- because, the stones are inside of the kidney. Have mercy on them, Lord; because, I surly do not.
I would rather pass kidney stones all day long as to have them in my kidneys. It’s a pain that doesn’t ever truly go away. It’s always there. When I bend, turn, lift…sometimes, with every step that I take. It is awful.
I understand, the pandemic with narcotics. I do. It’s hard for me to feel ashamed of needing the only thing that knocks the pain out enough for me to even sometimes make it just walking through my house. It is sad that any human with a heart and conscious would refuse to write a prescription for someone to have some sort of quality of life…and instead…be the reason someone, like myself, has to suffer from day to say and see no light at the end of the tunnel. It takes a huge toll on you. Believe me. The way I see it, if you aren’t willing to help find a solution; rather- you run test, can’t find any answers and throw your hands up, refuse pain medication- because, you’ve been told for years and years that there’s no pain to accompany stones that are of passing size… Well, you have been lied to. Not everyone is looking for pain medication to get a “buzz”. Some of us are just trying to get by with the only fix to our kidney pain.
I apologize for the rant. It’s been going on for years, now, and I’m at my wits end. I just need someone who will help me. Because, it hasn’t happened in Arkansas. Please, if there is anyone who I could be referred to, who is willing to help me figure out how to overcome this pain and these kidney stones- I would gladly accept it. My email is brittneydollins@gmail.com
Dear Brittney, This sounds simply horrible. The main problem is to stop making new stones. Do you still form them or is the pain altogether from stones in the kidneys? The former is not hard to treat, the latter is what Mike Borofsky was writing about. Let me know, Regards, Fred Coe
Thank you for this website!! I’ve been a “chronic” sufferer of kidney stones and infections for the past 20 years. It started with recurring kidney infections, treatment with antibiotics, and then kidney stones. I had a large stone surgically removed 7 years ago, and last June when I had a scan done (Viascan) the doctor found a stone “as big as his head”. Clearly it’s too large to pass, which is a blessing because I’ve been through that pain! But I now have chronic flank pain. What is the prognosis for something like this? Does it just continue to get bigger until I decide to have it removed? The pain isn’t unbearable, I’ve gotten used to it for the most part. But I worry that it’s getting bigger every day!
Dear Eileen,
If you do in fact have a large stone in your kidney at the moment that would be a very likely explanation for the reason you are having pain. It sounds like something that should be removed. Obviously the remainder of your medical history is critical to this sort of decision but the stone is likely to continue to grow over time and I would not expect the pain to improve without the it being treated. Additionally since this is now the second large stone you have developed in your kidney over the past several years you should consider undergoing formal blood and urine testing to try and figure out why you are forming these recurrent stones and what if anything can be done to prevent them in the future. We wish you well.
Sincerely,
Mike Borofsky
Thank you so much for this much needed article! I am a 38 year old female. I found out that I had over a dozen non-obstructing stones in each kidney in May, 2015. Since then, I have passed 33 stones (that I have collected – there may have been more) and had one procedure to remove an obstructing stone in my upper ureter. I have been to the ER on multiple occasions, often told “you have multiple calculi in both kidneys and a few in your bladder, but none are obstructing and you shouldn’t be having pain”. As of the last CT done a few weeks ago, I had 16 stones in my left kidney and 15 in my right. The stones in my left haven’t done a thing and aren’t growing, but my right kidney is making them faster than I’m passing them and they are all growing. I had a 24 hour urine done in the beginning of July, showing high levels of calcium and low citrate, so I was placed on potassium citrate and chlorthaladone to help reduce the stone making process. So far, no results. I went to the Cleveland Clinic last week to figure out why this is happening and don’t have any answers – I go back in November to see a urologist who specializes in stone disease. During the past year, I have also fractured multiple bones in my feet and teeth (15 all together) most of which were spontaneous. The one that wasn’t a spontaneous fracture in my foot was precipitated by hopping. The endocrinologist I saw at Cleveland said it’s not osteoporosis as they are small bones, plus I had a normal bone density. I feel like something metabolic is going on with my system. I have another endocrinologist appointment next month and am hoping they will run the right tests. Oh, my parathyroid and serum calcium are both normal, along with my D3. Have you ever heard of anyone presenting with bone disease along with kidney stones? Also, when will the treatment of potassium citrate and chlorthaladone start working? Do you agree that there has to be some sort of condition that’s causing this many stones? I can’t imagine this continuing for years, as it has been a nightmare! The urologist I saw at Cleveland Clinic, who didn’t specialize in stone disease, said there were a few surgical options if this continues with no solution. I could replace my ureters with intestines (so the stones wouldn’t get stuck) or move my right kidney next to my bladder, as that is my problem kidney. My life as I have known it has changed due to this and I feel like I’m suffering.. a lot! I’m still working full time, but have had to call off intermittently due to this. Thanks again and thanks in advance for my questions!
Dear Rachel, You seem to have high urine calcium loss and presumably idiopathic hypercalciuria. It is an hereditary condition in which bone disease is very well described, sometimes rather severe and not at all necessarily like routine osteoporosis. Your physicians presumably know this already, and are taking steps to prevent more fractures. The chlorthalidone is certainly a reasonable drug and I prefer it for my own practice. The potassium citrate depends. If the stones are calcium phosphate, there are no trials to be sure it is beneficial; if the stones are calcium oxalate, it has been shown to be beneficial. So analysis of all those stones is important. I suspect they are calcium phosphate. The drugs are not enough or you would stop forming stones. I would think a very high urine volume would be important. This site has a lot about fluids. Likewise about kinds of fluids. The chlorthalidone works best with a reduced sodium diet – be sure your urine sodium is on the low wide. I have never found it necessary to resort to extreme surgical measures such as replacing ureters with intestinal segments. I am sure your physicians are doing all they can for you, and hope these few additions will make the needed difference and result in stoppage of stones. Incidentally the main stone urologist at Cleveland Clinic is excellent, and someone I know personally. All the best, Fred Coe
Thank you so much for responding!! That’s incredibly kind of you. Very good information regarding the association of kidney stones and fractures. The make up of a stone I had analyzed was 65% calcium oxalate dihydrate and 35% Carbonate apatite. Does that change anything? I’m doing another 24 hour urine this weekend to see if the medication has had an effect. If you don’t mind me asking, who is the Dr at Cleveland Clinic you know? I’m scheduled with Dr Noble, but have heard good things about Dr Monga as well.
I know Dr. Monga, but that is not to say Dr. Noble is not of the same quality. The dihydrate composition of the stone is compatible with high urine calcium driving crystal formation, and the carbonate apatite means your urine pH is higher than in the usual calcium oxalate stone former. The higher phosphate concentration would mean to me a great emphasis on prevention, so your medications should be bolstered by as low a diet sodium as possible and as high a urine volume – especially overnight. Your goal is eradication of new stones, which is certainly a reasonable goal. The bone disease may well be related to idiopathic hypercalciuria, a matter I have not as yet taken up on this site but is very well known. It is familial, by the way, both IH and its bone disease. Best wishes for a successful visit to Cleveland Clinic, and my regards to Dr. Monga should you encounter him. Fred Coe
I have sponge kidneys and have passed hundreds of stones over the past 25+ years. Dr. Monga was my Dr for 25 years and I was heartbroken when he moved from the U of M to Cleveland. You will be in good hands………….Jane
Thank you so much for replying Dr. Coe!! You gave me valuable information. 🙂 I was going to see what openings Dr Monga had that week as the date/time of Dr Noble’s appointment may not work for me. I take the chlothaladone at night, so I definitely have a higher urine volume overnight..I often have to wake up in the middle of the night at least once. I have already increased liquids and am watching sodium, but will be more mindful now that I know. I’ll find out the results of my 24 hour urine this week and I’m hopeful the calcium has gone down and citrate up. My father had a severe form of kidney stone disease. I remember him going through several procedures and mentioning calcium build up or something in his ureters. Thank you again!! I realize how kind it is to take your time to reply. You have been very helpful!!
I passed my first 7 kidney stones on my husband’s 40th birthday, (he’s 10 yrs. & 6 wks. older than me), 6 hrs. prior to the surprise party to begin. I had been planning this for 4 mths., and I had been having severe pain the prior 9-10 days with nausea, vomiting, horrible diarrhea, sweats, fever, bloody urine and often felt very light headed. I honestly thought it was my Crohn’s Disease flaring up and I was just miserable. I was diagnosed at age 22 that I inherented from my Nanny, (Mom’s Mom & 2 female cousins.)
After being admitted to the hospital from the ER on 8/29/2000, it took a week to diagnose at ‘U of M’ in Ann Arbor, MI. I was tested with all the following: Blood, Urine, 24 & 48-hr collections, along with X-rays, CT Scans and an IVP. I was told that I have Medullay Sponge Kidneys and the most stones in both my kidneys! Since 8/27/00, I have passed over 19,685+ stones! In just over 15 years, I’ve had only 1 – day, each year that I didn’t pass any stones, which is when I had to have them removed surgically!
In an average 24 hr day, I pass between 50-100, (best day=7•worst day=157.) I was just about to be scheduled for ESWL Surgery, but then we moved to Las Vegays, NV. I have had a heck of a time trying to convince BOTH my Urologist and Nephrologist to preform the ESWL! They feel and have told me, “it could cause damage to my other organs, because of the sheer amount of stones they would need to ‘blast’!”
Since diagnosed, I see a Nutritionist that has me on a very specific and healthy Diet, for BOTH my MSK & Crohn’s Disease, which is a very delicate balancing act! I drink 2 gallonsof bottledwater daily & a 1/2 gallon of Lemon and /or Lime water, a low protein diet and see my Internist every 3 mths and both my kidney MD’S every month, along with my pain doctor.
At this point, I am passing ALL forms of kidney stones and over the last 18-20 mths, the are fusing (bonding) together, which of course makes this even more painful!
I lead a very healthy lifestyle: don’t smoke don’t drink alcohol, caffeine (of any kind), no nuts, chocolate, lots of organic healthy foods and for do water arobics 3-4x/wk, and light forms of yoga.
I would like to know your opinion and any suggestions that you may have, after everything I’ve described to me over the past 15+ years.
Thank you in advance for your input!
Respectfully, Suzy Williams
☆ Dr. Fredric Coe, you can see my Facebook info. under the legal name I provided to you.
Hi Susie, It sounds like you have stone disease complicated by bowel disease, which is indeed a difficult treatment situation. We have observed and published series of accelerated stone disease like yours and found that they are not so difficult to prevent. I agree with your surgeons that shock wave lithotripsy is potentially harmful and should not be used very often, and mention that medical prevention is the proper approach. Youe physicians at Ann Arbor are likely to be outstanding specialists, and have, I am sure, thought carefully about treatment options for preventing recurrence. From your description I do not detect what I might have expected by way of treatments, and there may be good reasons why not. I do not know why a low protein diet would be helpful. If you are really drinking 2 gallons of water daily and do not have diarrhea which would otherwise dissipate that water then your urine volume would approach 2 gallons per day; at that level of flow I cannot imagine any supersaturation would be present to drive crystal and therefore stone formation. For this reason, I would be concerned that the urine chemistries are abnormal in unusual ways which I do not know about. Perhaps your physicians are indeed already working to correct matters. Whatever, prevention of such numbers of stones should certainly be possible at a major university center and no doubt will be achieved. Fred Coe
Wow Suzie! And I thought I was having issues when I passed 27 stones last Sunday after 14 agonizing hours of pulsing wave pain. Hot baths really helped. Never hurts expelling them..only the path down the ureter. Left side for me. I hope someone figures out why diluting urine with large quantities of water isn’t helping you. Because I haven’t had a stone since age 23 (I’m now 63), I wonder why all of a sudden I passed a mass of these suckers! Since Sunday, I’ve begun a daily regimen of 500 mg of magnesium, 75 mg of B6 (in a balanced-B vitamin), and trying to take in 1200 mg of calcium. I’ve never been big on calcium & I now read that studies show that people who produce calcium oxalate stones are usually low on calcium and magnesium. I have no clue what these latest stones are made of, but I’ve saved them. I don’t go to doctors anymore & try to self-treat via research. The stones are smooth & round & various sizes but small enough to pass at this point. For what it’s worth, I’m a chocolate addict (very high in oxalate) & I began to eat unsalted nuts by the handful a few times/day. Bad combo apparently when not taking in calcium & magnesium. I hope some of this might strike a chord with you as sounds like we have something here in common, but I’m on the minor edge while you’re off the charts! Good luck! -Lynn
I should add that I drink more than 1 quart of water daily & have just begun to add the juice of one lemon to that. I’d sure like to hear what Dr. Coe thinks about all that I’m doing. I know I must drink more water! (and that first stone at age 22 had to be removed surgically as it was 1975) I guess I should try to find a way to have the 27 stones analyzed but hate to have to pay a doctor just to hand them over! Is there another way to have them tested? tks!
Hi Lynn, a quart of water is not much in this league – 3 would be good protection. The lemon thing is mostly nonsense, if you need potassium citrate – which is what lemons are presumed to supply – you need a lot of lemons and are better off with medication. See what I wrote below. As for paying, stone analyses are not expensive. Regards Fred Coe
Hi Lynn, I gather you had stones in your youth and none since age 23, then – all of a sudden?? – passed 27. Firstly you should have the stones analysed. It really matters. Given so many, you should get a CT scan and see what is in your kidneys. As for diet calcium, many stone formers have genetic hypercalciuria and will lose bone mineral in their urine if they do not eat enough calcium with their meals. The calcium needs to be with food. If necessary one can take a calcium supplement but with the meal. The lower the diet sodium, the lower the urine calcium, so low sodium diet is a big help. The magnesium and B vitamins have no proven role in stone prevention. Regards, Fred Coe
Mike Bornofsky you say “The pain classically persists at a severe level for several hours (phase two) but ultimately subsides, at least partially (phase three)”. Some of our MSK group members when passing stones experience these same symptoms of extreme renal colic, not for hours, but for days, weeks and even months on end! Trying their best to avoid ER for the millionth time this year for obvious reasons (same attitude, same treatment, same dirty looks, same insinuations, accusations for seeking unjustified pain relief!) Many of our members are living their lives in dialy chronic pain due to MSK, when renal colic hits from passing yet another stone, their pain is multiplied, never ending relentless pain, till they finally pass that darned stone (days, weeks or months later!) Once this episode has passed, they’re blessed with … what? a week? a month? 2 months of colic free symptoms until … the next stone, and all this pain hits again, for days, weeks, or months at a time!
This article was very informative, my only wish is that this information be made more widely available to E.R. and family doctors. To many times I see doctors get stuck in the rut of believing only what a text book says, or be handicapped by what an insurance company will pay for. The part that gets me is do E.R. doctors really believe we as kidney stone patients are that stupid ??? For us that have had to deal with real kidney pain, we know the drill you go the E.R. first thing they do is order the gold standard, C.T.. If they don’t see any obstructing stones they say it shouldn’t hurt, next if their nice they will give you tordol which does help, but doesn’t relieve the majority of the pain. Do doctors really think we want to subject ourselves to C.T. after C.T. only to be told we shouldn’t be having pain? I work as a Diesel Mechanic, and have seen trucks come in the shop that have been to 5 other shops and bills as high $3,000 for stupid things that should have be caught. After fixing the problem, the customers always ask the same thing why was it that I took it to all the other places and they couldn’t figure out the problem but you did, or someone else in my shop did. My response is usually always the same, because the answer the problem wasn’t is in a book, or technical service bulletin. We had to but 2 and 2 together and realize the manual was wrong, or the diagram was printed wrong. Here is a good example, customer says check engine light comes on mostly when going around corner. Other shops said sorry you don’t have any codes, customer gets mad the light comes on again, he takes it to another shop and the same thing repeats itself, customer comes to our shop and he tells us everything he has been through at the previous shops. So we start off with the customer is correct and not lying, after a few diagnostic steps we find that yes there is no codes and yes there is a rubbed through wire that is grounding out the check engine light. Errors in programming are found everyday, and we are used to it. Heck the idiom we are only human, confirms it. Ok I’m done with my rant now, please keep up the good work and continue to think outside the box, not many people believed Einsteins ideas but the atomic bomb left a literal explanation point that he was right.
Hi Travis, I love the analogy. To me physicians are all diesel mechanics, but we do not get a users manuals for our engines (bodies), circuit diagrams, or code – we need to work them out ourselves – called biomedical research – and somehow distribute the results to the folks fixing the engines (physicians) – called medical education. I am convinced that pain without obstruction must be common and I know it is not an accepted phenomenon. This is a real research problem as nothing else can fix the ER problem, and make life better for people with this pain. Great note, thanks, Fred Coe
Just saw this comment, Travis, and it is 100% spot on. Doctors are spouting off what they read in a medical textbook but not actually opening their minds and seeing what happens in the real-world and using real-life examples to changes their views. Due to doctors’ closed-mindedness I’ve suffered for a long time with my non-obstructive stone. Funnily enough, I recently went to Indonesia for a work trip where I happened to attend a training session at a hospital with a group of doctors. In Indonesia (a developing country) all the doctors were taught that non-obstructive kidney stones CAN cause pain and this seemed to be general knowledge amongst all the doctors I met. i got a prescription for Flomax over there which although hasn’t eradicated my pain has REALLY helped and I have a lot more energy now. Not sure what exactly it’s done but seems to be doing something right. If nothing happens after a few weeks on Flomax I’ll investigate into finding a doctor to perform surgery for me (I still haven’t found one here yet). Why the thinking that was common knowledge with the doctors I met in a developing country is NOT common knowledge in first world countries, I’ll never know. Good luck and I hope you and I BOTH stop suffering soon 🙂
Lovely interesting letter Travis!!
Grace
Hi..
since I hv 3 kidney stones frm last 5 months so during starting 3 tyms I suffered frm severe pain so mah urologist suggested fr operations so I request you to ans meh dat nw a days I feel totally fyn n there is no pain but stones r still present so is it ok? If
I take sos wen needed..n is it ok if I do aerobics every evening?
Hi Priya, I take it that you have three stones in your kidneys, you have had severe pain presumably from one of the stones but are not free of pain. It is OK to do nothing if – a very important if – your urologist is sure there is no obstruction being produced by any of your stones. Stones that are not causing obstruction, infection, bleeding or pain can be left in place. You would know about severe bleeding and pain and could guess about infection but obstruction can be silent – so be sure of this. As for aerobics, not a problem. Stay well hydrated so as not to form more stones! Fred Coe
if it is smaller than 5mm you should drink 3-4 ltr water in a day it can pass from urin and if it is bigger than 5 mm concern with doctor bkz lasour operation cannot successful stone dissolve for few time after that u have problem again
hi sir i am shubham mishra i have 7 stones size 5,6,7 mm and both are kidneys its very painfull what can i do please suggest me
Hi Shubham, Seven stones is a lot, and given the pain I would guess one of more of them is obstructing the kidney. There is nothing you can do about this; you need a skilled urologist who can take care of this matter. I would suggest you get the proper physician and let him or her resolve things for you. Regards, Fred Coe
After reading this article I feel hope for the first time in years. I have been seeing my family doctor for some time now regarding the exact same thing you are talking about which is pain in what seems to be my right kidney. He sent me to a urologist and they found nothing. They did a CT scan and found 2 stones in my right kidney but they all said that they are not the cause of the pain. I’ve had my gallbladder removed after having that tested and was told that it was performing below the “normal” levels and that didn’t solve anything. They sent me to a pain specialist where he did a procedure where the myelin sheath is severed believing that it was nerve pain in my lower back and once again nothing. They sent me for a colonoscopy and then an endoscopy and yet again was given what seemed to me as bad news as there was nothing detected as to what was causing the pain. I just scheduled an appointment with my doctor to talk to him about this article and I’m really worried about what his response will be. Any suggestions before I go as to what I should say to him to make him possibly believe me?
Hi Janette, I am afraid that the only thing we have to offer is the article itself. Small stones do seem associated with chronic pain, but surgical procedures for such pain are presently in the province of surgical research centers as there are no prospective randomized trials. If pain is so severe as you describe, and there are stones present, it would not be remarkable to remove them, especially via ureteroscopy so that the papillae can be visualized. The unsolved problem is crystal deposits within the kidney tissues. Your physician can distinguish these from stones at the time of the procedure. Regards, Fred Coe
Hi thank you so much for this article!
I was in the ER last night after a sharp horrible pain in my right mid flank for kidney stones but the doctor said there were no stones present in the CT scan as it probably had past. They found samples in my urine and that for them was the evidence that I indeed had stones. I was treated horribly by the doctor I felt like he saw me as a patient just looking for pain medication but I really was in the most horrible pain in my life. I got to a UC school far from home full time so I cannot see my primary doc and am also an athlete and I am now very scared the stones will come back as the doctor said they are in my kidneys. I don’t want to have to go to the ER again and have the doctor give me the dirty “your a druggie” look. Any advice is much appreciated.
Hi Venus, It sounds like you passed some crystals; they can cause pain and bleeding but are not seen on CT scans. Being an athlete means potential for dehydration, and I wonder if this attack followed a particularly strenuous event. I gather there are stones in your kidneys and that you are young. You need a full evaluation for causes of stones and a proper prevention program. This would require referral to a skilled physician. Do this, as especially women – I am guessing – who form stones early in life are prone to form many and also have distinctive abnormalities that can be effectively treated. Regards, Fred Coe
Dear Dr. Coe,
Thanks for your thoughtful explanation about non-obstructive kidney stones, their ability to cause pain and the significant disagreement within the field. After reporting mild right side pain where I have a small stone (3mm) in the lower pole and questioning if it could be causing pain and hematuria (the latter symptom I’ve had x 6 months) I was told categorically that the stone could not be causing this pain and that the pain was probably from the UPJ obstruction pyeloplasty sequelae. I pointed out that the pyeloplasty was performed on my left side and my pain was on the right. Also, I was informed that urology had performed every test to determine the cause of the hematuria and the results were negative. I was very clear that I was not claiming that the stone was passing, that the pain was dull and intermittent and tolerable. Obviously Dr. Coe, I have omitted many of the details in order to focus on the current bothersome symptoms. The pain I can live with unless the stone is not only causing the pain, but more importantly the stone is somehow causing the daily gross hematuria (I have read that non-obstructive stones cause cause hematuria but I am not clear as to how).
Thanks for any feedback and for your appreciation that as medical knowledge evolves patients can have a rough go of it depending on the practitioner’s beliefs and whether the patients can be relentless in getting answers.
Thank you for your time and thoughts,
Karen
Dear Karen, You are certainly in a large group of people which this kind of symptom, and not a few people in the field are concerned about what is causing the problem and how best to treat it. As for hematuria, so long as important other causes have been eliminated by your urologists it is presumed from the stones and is itself not of especial concern per se nor an indication for s surgical procedure. Regards, Fred Coe
Hi,
My father has been hospitalized for 1 month now with flank pain and ‘too small to cause this pain’ kidney stones. They have run all sorts of tests, CT, ultrasound, echo-cardiogram, bonescan, etc, not finding anything. I have asked and asked for a urologist to do a ureteroscope but they insist it’s not indicated. What can I do? Thanks so much!
Hi Chris, It seems unusual to be hospitalized for a month for flank pain. I doubt that small stone pain would lead to a month of inpatient care however so much it can be burdensome. If it really a whole month then I would suspect more than stones. Possibly you mean he has had hospital associated pain episodes; perhaps you might clarify this so I could be more helpful. Regards, Fred Coe
Hello sir
Yesterday i got pain and got an ultrasound done
It says 5.6 mm calculus in left kidney in lower pole
And in the right kidney mild prominence of pelvicalyceal system and right ureter not visualised. What is your opinion. I am having nausea too. My urine is acidic Ph 6
I am taking uralyt u granules
Please reply
Hi Zoya, Your medication, URALYT-U® is a preparation of sodium and potassium citrate about equivalent to two US potassium citrate tablets in citrate content but having half sodium and half potassium as the cation. It is for uric acid stones. For calcium stones, the sodium component would be less ideal as sodium will raise urine calcium. Your present attack is unclear as your pain is not specified as to which side. The left kidney has a stone in it that could have transiently blocked urine flow and caused pain. The right side does not seem abnormal. What to do here is a matter of surgical judgment for your personal physicians. Regards, Fred Coe
Hello sir
Pain was localized to right lower abdomen radiatng from back and coming in waves
Can a 5.6 mm stone pass via urine. I am prescribed good hydration
Dietary changes
Tamuolosin aplha blocker to dilate ureters for ten days
Dear Zoya, the right sided pain could be a stone. But the stone you mentioned was on the left. I presume there are two stones or else you have the stone and pain mixed as to the side. In any event management of stones seems right – from your description of your meds – and a 5.6 mm stone can pass. You doctors seem to be doing all the right things. After the stone has passed and you are well you should have the stone analysed so you know what it is, and have blood and urine testing to determine the causes of the stones. Regards, Fred Coe
Hello sir
I have been prescribed tablet uricare two tablets three times after meals by doctor for 1 month. Its an ayurvedic medicine. Will it affect my kidneys in a bad way? . I have a 5.6 mm stone in my left kidney. Please reply
Thanks
Uricare tablet is also known as cystone. Waiting for your opinion
See below Fred Coe
Hi Zoya, I found one study of this drug which was resoundingly negative. It did not lower urine supersaturations. The total burden of stones in the kidneys did not decrease over one year, and in fact increased. It seems worthless based on this trial. Of course it was a short trial and perhaps a longer one might be positive, and might not be. If you have significant stones, why not pursue more established prevention: 24 hour testing to find out what is wrong; stone analysis to find out what crystals we are trying to prevent; diet changes and meds if needed to reverse supersaturations for the crystals in your stones. Regards, Fred Coe
Hello sir
Recently my doctor diagnosed a fibre size kidney stone in my right kidney I am taking medicine since four days but I am feeling a mild pain continuously on right side abdomen
I am drinking 3 litres of water daily but pain is hurting when I touched or exercises
Hi Vishal, If you are passing a stone, your personal physician needs to keep track of its progress and be sure it leaves your urinary tract. Be sure and follow up with him. Otherwise the fluids sound like a good idea. If your physician gave you medication take it as directed. Regards, Fred Coe
Facinating article, I have had kidney stones(oxalate) since age 23, had lithotripsy then and again 17 yrs later and again 5 yrs later due to medullary sponge kidney. The stones are always rattling around and this year for the first time they have decided to move on their own and hurt. My urologist says the stones are too small for the lithotripter at 6mm but they hurt moving or just staying. Thanks for your article.
Hi Deb, You are part of the small stone dilemma. Certainly shock wave lithotripsy is not likely to do much good. Whether people with pain and small stones benefit from ureteroscopic treatment to remove the stones and tubule plugs is a matter of controversy. A lot depends upon how much pain and therefore whether it is worth your undertaking surgical treatment not as yet tested in any trials. Fred Coe
Very nice Article, For the first time, I Suddenly had pain in groin which I thought might be pain in testes due to sleeping injury or might be urinary infection. So, I tried antibiotics and tablets for pain killers without any relief . Pain was constant for around 4 hours with increasing urge to pass the urine but I was unable to do that. Then pain started increasing with spasm in abdominal area, urge for urinating was causing hell lot of discomfort. Slowly, pain increases more and my jaws, face muscles got spasm, also both hand and feet muscles were undergoing contraction. Condition was much like Tetanus. For once I thought It might be Paralysis attack because upper part of body was loosing the sensation. Pain was so high I was afraid of pass out. After lots of medication on time, I got some relief and kidney stone moved out. So, my observation is, “extreme pain” may cause symptoms like “tetanus” and “loss of sensation” in body parts. Thanks!!
Hi Raj, Thanks for the comment. I suspect you were hyperventilating and lowered your blood calcium ion concentration which caused the spasms. Good luck in preventing more stones! Fred Coe
Hello sir
I have posted earlier regarding my 5.6 mm stone in my left kidney. I have been prescribed uralyt u granules, but the taste is bitter causing nausea. Because of nausea i m skipping this drug. Is there any tablet of potassium sodium hydrogen citrate. Can you please elaborate on medical expulsive therapy for renal calculus. I took Tamuolosin for 10 days but nothing happened, the stone is still there. I have appointment with Dr after 2 weeks
Please reply
Thanks
Hi Zoya, potassium citrate has nothing to do with stones that are already formed. Those are surgical problems, unless they pass on their own. Potassium citrate and all other prevention measurements are to prevent more stones. At this point your urologist needs to deal with the stone. Thereafter you need to have proper prevention so there are no more to cause trouble later on. Fred Coe
Hello sir,
Three days ago, I had pain in my lower left stomach and when I went to the hospital, I was diagonised with with 7 mm kidney stone. The doctor said the stone is on the way to the bladder and gave me pain medications and Flomax. But so far I am not feeling any pain for the past two days. I am concerned as to what is going on. Please any advise would be much appreciated.
Thanks
Hi Guna, Usually physicians want to know if pain changes, as yours has done, so it is important to let your physician know. Perhaps the stone has passed, or perhaps it is lodged in the ureter. Either way, your physician needs to know and make a new evaluation. Regards, Fred Coe
I have two herniated discs in my lower spine. It has caused sciatica pain in my left leg, I have been having back pain for about a month now which I dismissed as pain associated with my back issues. I then started my monthly cycle and dismissed the cramps in my stomach as menstrual pains. The pain increased so much that I went to the ER. They did a CT scan and said I have a 2 mm stone, sent me home with pain meds and something for being nauseous. Now the pain is so bad I can’t get up out of bed. I need to know if this is normal and if I should seek further treatment. How long should this last? I drink about a gallon of water a day, I have tried fresh lemon juice and olive oil, cranberry juice and water with lemons. The pain never fully leaves but it does increase to unbearable levels then back down to being tolerable. When I walk it hurts, I can’t bend over and I can’t sit up on my own. My left leg has pain at times then the pain completely goes away. Please let me know what you think.
Hi Stephanie, I guess the question is whether it is the stone causing your pain or your disc disease. Is the 2 mm stone obstructing the ureter? If it is, that can cause terrible pain which should go away when the stone has passed. The new pain, in your stomach, may well have been from the stone as stones rarely cause sciatic pain. So there are two pains of perhaps differing origins. From the stone, the pain will not improve or worsen with motion, position, bending or any other physical means. So what you describe at the end of your note is presumably from your back and may require physical medicine care. Nausea and abdominal pain is usually not from a disc and could be from the stone. The fluids are a good idea, the lemons of dubious value, and the cranberry juice likewise. I would wait for the stone to pass and seek care for the disc problem. When things get better, be sure and have your physicians figure out why you formed the stone so you can take steps to avoid more of them. Regards, Fred Coe
I’m 28 weeks pregnant and was diagnosed with Kidney stones. However, the pain is in my left flank where 2 CT scan did not pic anything up. A stone was found on my right. Due to being pregnant, I was finally sent home after 3ER visits with pain med (Dilaudid). Tonight the pain is worsened even over the meds. I’m confused what to do! My options for pain relief is limited due to pregnancy. The Er/OB basically told me to let it run its course…a course that cannot be found and I’m in pain! What are my options? It’s been 5 long days and no results. I’m so scared
Dear Jamie, Your’s is an odd situation. I gather the right stone is not obstructing your ureter, and there is nothing at all on the left side. The CT scans are normal apart from the stone on the right. Firstly, it is not acceptable to have narcotic level pain during an otherwise normal pregnancy and it is also not reasonable to ascribe pain of such magnitude to stones on a side that shows no stones. So there must be another reason for the left sided pain. I would think your personal OB physician needs to figure this out. What if the pain on the left is not from stones? Is it possible there was a small left stone – missed on CT – which is now obstructing; if so an ultrasound- no radiation- can be helpful. By all means to not let this simply do what it is doing without your personal OB physician closely monitoring things and figuring out the nature of the problem and a medically proper solution. Fred Coe
Can anyone offer some advice my wife has been diagnosed with a large kidney stone and is awaiting surjury to have it removed however the pain she is going through is unbearable I have had her to the er twice before we found out about it watching her go through this is driving me crazy knowing there is nothing I can do any suggestions on how we can lessen the pain
Hi Wayne, I take it the stone is obstructing the urinary system and that is the cause of her acute pain. When severe enough narcotics are not unreasonable presuming NSAIDS have been ineffective. This is a complex surgical issue, and no one at a distance can make any useful advice apart from this: Acute pain from a stone can be very severe, short term narcotics are entirely justified to control pain until the stone can be managed surgically, and one is justified in speaking the the personal physicians involved to assure short term pain management until the episode has been resolved. Regards, Fred Coe
I am reading this and I need help! This is one of the first articles and doctor that I have found that actually might understand what im going through. Like the lady in the article, I have too been told I am med seeking and that I shouldnt be in this much pain. Please, if anyone knows how to contact this urologist or has any advice, PLEASE respond. This is my 10th or 11th stone within eight months. I cant work because of the pain. Ive had this current stone for five days. Lots of pain, vomiting anf chills. I need to help fifuring out how to avoid making these in the first place. They keep dropping into my uritur. Some only one or two days apart. Thank you.
Dear Johanna, I am very sorry to hear about so much trouble. Firstly, having 8 – 9 stones in 8 months means that prevention is very urgent. Before embarking on a search for other physicians, be sure and speak with those who already care for you and bring up the importance of prevention. Prevention of stones is very practical and usually effective. If your present physicians cannot stone these stones perhaps they can arrange a referral for you to a center where it can be accomplished. The physician who wrote the article works at the Methodist Stone Center at Indiana University, Indianapolis, and would, I am sure, be pleased to speak with you or email. Let me know, Regards, Fred Coe
My daughter (6 years old) was diagnosed with 5-6mm kidney stone last week. She had a couple of days of severe pain, but the pain seems to have gone away completely. I have collected and strained all of her urine and she has not passed a stone. Is this normal?
Hi Tamara, I would be sure and speak with her physician. The stone may have passed or perhaps is obstructing her ureter. It is important for her physician to be sure. As for stones at 6, this is a serious matter and the cause of the stones must be ascertained so that prevention can be accomplished. Childhood stones are often due to common genetic hypercalciuria but can also be from a serious systemic disease, so be sure the cause is determined. Regards, Fred Coe
Hello sir
2 weeks ago I have a severe pain then the physician adviced me to go through ultra sonography, there its found to be one 4mm stone in left kidney and a 6.5mm in ureters. I was asked to go through medicines, then for 5 days I don’t have pain now. Now today I again have gone for sonography, now it detects a stone in right kidney of 5.8 mm. Was it already there or what??? Please can anyone explain.
Hi Rittu, One possibility is that the stone in the ureter on the right has moved back up into the kidney – I gather it is no longer in the ureter and you have without pain. The size difference of 6.5 to 5.8 is well within the error from measurement using ultrasound. Regards, Fred Coe
My wife has 3 stone of 10 mm in ureter. She has not feel pain since 2 week. Blood and urine report suggest no clinical complications. Please suggest is it necessary to go through surgery
Hi Tejas, surgery is needed if stones obstruct the ureters whether pain is present or not. I presume if her physicians want to operate it is because the stone is lodged in the ureter and is or may well begin obstructing the ureter. That would be a serious risk for loss of function in that kidney. If the stone was merely in the kidney and not obstructing, then surgery or not is a much more nuanced decision. Regards, Fred Coe
I have medullary sponge kidney disease, and both of my kidneys are full of stones, calcifications, and cysts. I was diagnosed when I was 11 years old and am now 61 years old. I have had many urologists and nephrologists since my diagnosis, and I have never had one acknowledge that non-obstructing kidney stones can cause flank pain. I have always suffered with chronic flank pain, and as I’ve gotten older, it had worsened. I pass kidney stones several times during a year, and also pass crystals in my urine on a daily basis. Thank you so much for writing this article! I really wish that I could find a urologist who would recognize that my pain is real and not from my spine, back, muscles, etc.
I have little doubt that these calcifications can cause pain; the problem is that proper surgical approaches have not as yet become established. Of special importance is the crystals passing; they are absolute proof that urine supersaturation is too high and needs to be lower. Lowering it and therefore abolishing the crystal passage may not end your pain but might possibly lessen it considerably. I strongly suggest your take steps with your physicians to lower urine supersaturation with respect to calcium phosphate- -the crystals surely are calcium phosphate – in hopes of lessening symptoms. Regards, Fred Coe
Thanks so much for your reply! I will definitely talk with my urologist about urine supersaturation during my next appointment. I drink only bottled water, and try to drink at least 2 liters per day (more during the summer when I sweat a lot). I’m taking 25 mg of hydrochlorothiazide per day. I have been prescribed potassium citrate through the years, but it causes me to have severe stomach pain. My last 24 hour urine collection was two years ago. How often do you think this needs to be done? Whenever I wake up in the morning, my kidneys ache, cramp, and feel very heavy. It takes several hours for them to calm down. What do you think could cause this? Also, why do I always have blood in my urine? Almost every urine specimen that I’ve ever had taken has shown trace amounts of blood. (Of course, when I’m passing a stone, I pass larger amounts of visible blood.) My doctors have never been concerned about it, so I’m assuming that it must be associated with my medullary sponge kidney disease. I appreciate your time in answering my questions!
You should have your past studies reviewed with respect to calcium phosphate and calcium oxalate supersaturations, if these crystals are calcium crystals, as I assume. If they were uric acid they would generally have an orange red tint which you did not mention. Surely the crystals have been analysed as you are always passing them, and the key supersaturation is the one that corresponds to your crystals. Blind treatments do not work- they must be directed at the relevant supersaturation. Regards, Fred Coe
A very interesting article and I thank you for it. I live in the UK and began experiencing severe left flank pain in February 2015. I had MRI to check my muscular skeletal issues that came back clear except for fair wear and tear. A partial colonoscopy and a CT scan.
I then came off Statins (Simvastin). My pain greatly reduced but I still have occasional severe pain. I have now been informed that I have a Staghorn Calculi in my right kidney but the right side has never been an issue. Plus 2 small stones (3 and 5mm) in my left kidney. I believe these must be giving me non obstructive pain, I have never passed a stone I my 63 years,
Is this a typical presentation?
Hi Richard, No this is not very typical but it is in a way also reasonably straightforward. The left staghorn needs to be removed by a PERC. While under anaesthesia perhaps the left stones could be removed via URS. The analysis of the stones is critical; the staghorn could be from infection and a host of other causes. The small ones likewise need to be analyzed. Given all this you should have 24 hour urine and serum testing to find out what is causing all the stones. Regards Fred Coe
Hi Richard, yes I completely agree with Dr. Coe. Staghorn calculi can be quite serious stones with high likelihoods of longterm kidney damage, infection, and other medical problems. Despite the fact that the right side is not bothering you I would consider it the side of greater concern at this point in time. I recommend trying to meet with a urologist, ideally someone who routinely performs percutaneous nephrolitotomy (PCNL or PERC), for consideration of stone removal. In some cases the side with smaller stones can be treated simultaneously, in other cases they can be treated at a separate setting. Regardless, your situation certainly merits consultation with a surgeon.
Regards,
Mike Borofsky
Thank you Fredric and Mike for your replies. The unfortunate thing in the UK is that although our National Health scheme is free, it is slow. I have an appointment with a consultant but not until 10th March. I will keep you posted. Just to throw something else into the mix, the pain last February began after an allergic reaction (sickness, Diarrhea, sweats etc) to Shellfish through cross contamination in a restaurant. I am now white fish intolerant as well but thankfully this is not immediate (2 – 3 hours)
Many Thanks Richard
Thanks again
I am one of the patients that have been told there is no reason for me to be having pain. I am on my 5th stone issue right now. The first 2 were not diagnosed as stones at all. One of which I was pregnant and had urgency and stabbing pain in my urethra. It lasted for 2 months approximately. I had blood in my urine but nothing showed up in my cultures. My 3rd stone I had the same symptoms. I had a CAT scan done and was told repeatedly that while they could see the stone, it was not in a location that would cause pain. By the time I made it to the urologist visit, I was actually passing the stone on the way to the office. I felt like I was having a baby, having the urge to push. Then all of a sudden out of nowhere, I was fine. A week later I collected the stone from my urine. It was calcium oxclate. In 2012, the exact same thing occurred again. I informed my general doctor that it WAS a stone, gave her the info from the previous experience. Again, I was told there were stones, but NONE would be causing me pain. Blood in urine and stabbing in my urethra and urgency. After 2 months of going to the ER repeatedly she finally referred me to a urologist. By the time I made it to that appointment, I had the stone in hand. Size of the stone was 36mg. Again calcium oxalate. I asked her why they all keep saying there is not a stone when there is. She said I do not present typically. She even wrote on a prescription pad information to give to future doctors. ( It states that I do no have hydronephrosis, no pheboliths in my pelvis.) Not one time have I been prescribed any medication to help me with the pain, I am instructed to take Ibprohine. Now here I am again in 2015 November and am having severe stabbing pain in my urethra, my bladder aches, and blood in my urine. Now they say I have lots of little stones, but none should be causing me pain. I am at a complete loss. My abdomen is sore, I have stints of flank pain, but the urgency and stabbing is killing me. I have an appointment with a urologist in Feb 9th. I just want to cry. No pain meds and go to the ER if it gets too bad. *Also as soon as the stone passed previously there is NO pain what so ever. And I have NO history of drug use what so ever.
Dear Tamara, I am sure that the pain you are having is from stones as there is no pain between them and you pass stones eventually. I wish that the contemporary craze over pain medications would abate. Your note speaks about 11/15 so the episode is no doubt resolved. Did you pass another stones? I might ask why you keep having stones. Can you get prevention? See the article and get what you most need – an end to new stones.
hello sir,
i have stone in my left kidney..approx 2 mm. i am on a treatment…but few days before i suffered pain in my left testicle..cn u tell me is this pain normal??should i do something to cure this??
Hi Prateek, the left testicular pain is from the stone and is simply referred there because of shared nerves between the ureter bladder and testicle. It has nothing to do with the testicle and will vanish when the stone passes. Regards, Fred Coe
Hello. I went to the ER for sharp pains in my lower right back and mild pain in my stomach. Got a CT done and they found a 2mm stone in my left kidney. Shouldn’t I be having back pain on my left side where the stone is instead of my right side?
Any help would be appreciated!
Can you email me your response?
Thank you kindly!
Joni
Hi Joni, I guess we take what we get. The stone on the left is your primary issue. Sometimes CT scans can get mislabeled right to left, although given the anatomy this should be easily recognized. SOmetimes there are two stones, and only one is seen. This means your physicians will no doubt we wary. Regards, Fred Coe
I am 75 and I have now passed 6 kidney stones in the past few months. I have never had one before this year. I have read all I can about what causes them, etc. I have tried to do all I can to not have them but they keep coming. What can I do to prevent them because they are no fun. I must pass them by drinking lots of water because they go away after about two days. I have never been to a doctor about them. What can Doctor do that I haven’t done already, other than tell me I have kidney stones? Thank you.
Hi Pat, The composition of the stones is crucial. A common reason for late age stones is a fall in urine pH with uric acid stones as a consequence. What are your stone made of? If you have never had them analyzed what do they look like – especially what color? There is no reason to have so many and not know why they form and get treatment to stop them from forming. Regards, Fred Coe
Hello, I am currently 12 weeks pregnant. 2 weeks ago I was awaken at 2am with severe lower left back pain. I’ve never had a kidney stone before. The pain came in spasms and I honestly thought I was having a miscarriage. We went to the ER, and I was told I have a UTI. Being pregnant, they couldn’t do a CT, so they did an ultrasound. They couldn’t see a stone and said there wasn’t any hydronephrosis. I was told to take antibiotics and pain meds. Being pregnant, I can’tell take anti-inflammatory drugs. The pain is horrible. My obgyn wants me to go to my psychiatrist. (I do have schizoaffective disorder, but it is thankfully under control) he finally agreed to send me to a urologist but I have to see a high risk pregnancy doctor first. No appointments have been made. I can’t make him stop dragging his feet and take me seriously. I don’t know what to do. I am exhausted and so sick of the pain.
Hi Victoria, I think your physicians are doing the right things but perhaps the pace is not ideal. The high risk pregnancy physician is key here and I would try to get seen as soon as possible. This kind of pain sounds like something that should be taken care of one way or another. Obviously from this distance I would have no idea what it might be. Regards, Fred Coe
Hi Dr. Arizona, USA here. As I read this is felt I was reading my own story. I was diagnosed with my first 9mm stone in my ureter near my kidney at the ER and admitted for laser ureteroscopy with a stint amd revealed it being a calcium oxalate stone. 2 days later while home I had profuse vomiting and pain that I went back to the ER, admitted and had surgery again to have the stint removed. 4 days later at home I had vomiting again but less pain, but still renal colic pain and day my urogist. He ordered a 3d ct scan and there are two 3mm stones in the pocket (lower pole) of my kidney which are stones left over from the 9mm stone he lasered. I begged hik to do a repeat suegery and remove the stones and he said no they will pass. They never have. I was upset and he said this is not the cause of my pain which I did not believe. The ct ruled out any swelling in my ureter or kidney but my frustrations of being in pain were still there. I went to another urologist who was adamant in the stones not causing my pain and sent me home. After researching on my own I found forums where other people had pain from stones in their kidneys like myself. I feel so lost and helpless and I shouldn’t be in pain everyday and I miss working out daily. What does someone in my situation do?
Hi Lacey, A reasonable approach would be flexible ureteroscopy to remove those stones. It sounds technically feasible if you are having enough pain to make it a worthwhile effort. That judgment is between you and your surgeons, of course, as the pain must be enough to take on the risks of anaesthesia and another procedure. Regards, Fred Coe