LISTS – AND LISTS
I know you are all looking for THE list. Here is one from a reliable source I have have downloaded on my site to a separate document so it opens with one click.
The reliable source, as it turns out, needed some updating. Dr Ross Holmes, professor, School of Medicine, University of Alabama, was kind enough to review the work of Dr. Michael Liebman who is a professor of Human Nutrition and Food Option at University of Wyoming and determine which food entries on the Harvard list needed changing. We cannot change the original but we have updated our lists accordingly and annotated updates with *** marks. So the lists here are the most recently edited available at present.Fred Coe and I have updates and annotated the list for those with a tendency to perfectionism: Updated table of oxalate foods. Set it at 50% for easier reading. Get yourself acquainted with the lists. They will tell you much of what you need to know. A lot of it will even surprise you. You are not as restricted as you think you are or as you have been told.
A more dramatic list is the 177 high oxalate foods we distilled out of the big list. Here are culprits! Not on this list? Probably not very high in oxalate so far as we know – with perhaps a few exceptions. Note that quantity is critical. For example black pepper is high in oxalate but the amounts used are small enough that total oxalate intake from it is negligible.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
LET’S DIVIDE AND CONQUER
FOODS TO WORRY ABOUT
A List of Concerning Foods
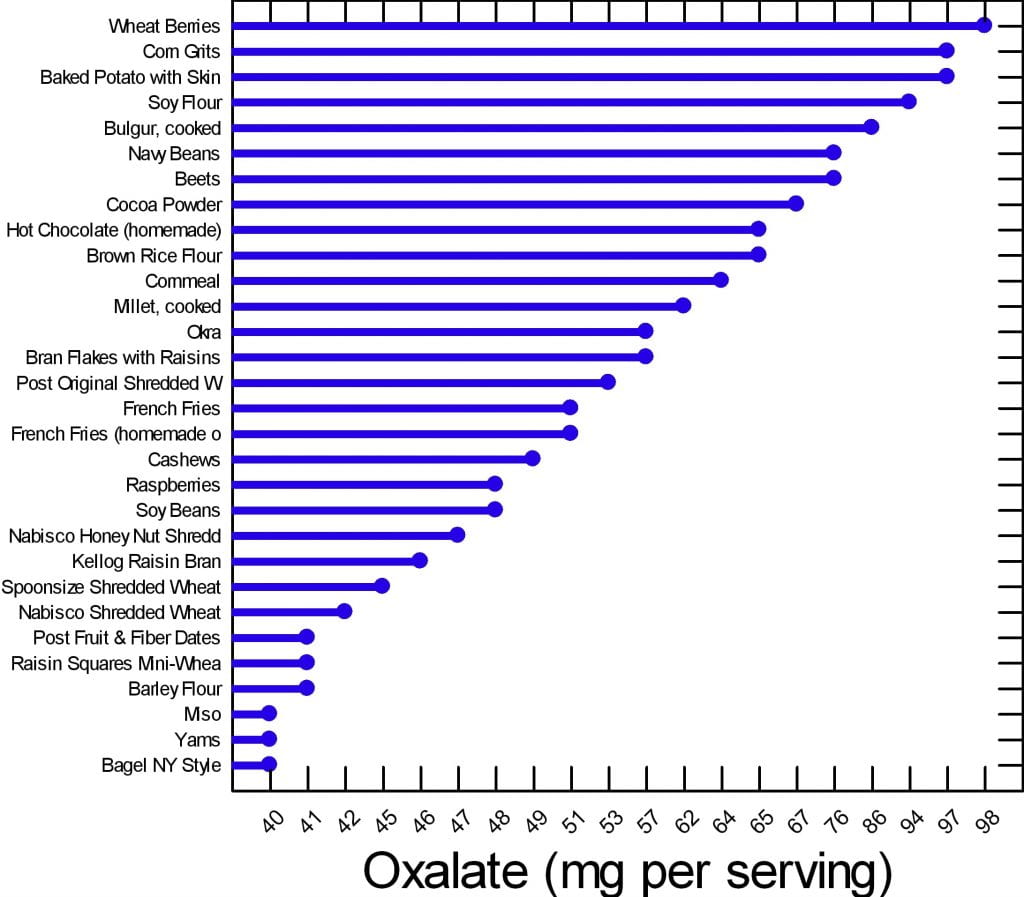
We have created two graphs for this article. Of the 177 foods on our master list, many are of concern but can be used in your diet if you control the portion size and how often you use them. There are 30 of them that are worrisome enough to deserve special attention.
Here are the 30. The graph shows mg of oxalate in a common portion. The details of the portions are in the complete list. The foods have in common that all contain at least 40 mg/serving. All other foods for which we have reliable data have less oxalate per serving.
Your budget is about 100 mg/day.
What does this graph mean? Does it mean you can never have chocolate, or a baked potato?
No.
It means if you want to use your whole budget on a treat, do it, but keep track and make sure you do not overspend in any meal or in any one day. Have your baked potato, but maybe share half with your partner. Or, have some hot chocolate but make it with milk because calcium helps reduce oxalate absorption. Eat your cashew nuts, but pay attention to how many. If one handful leads to ten, you cannot have them.
FOODS TO AVOID
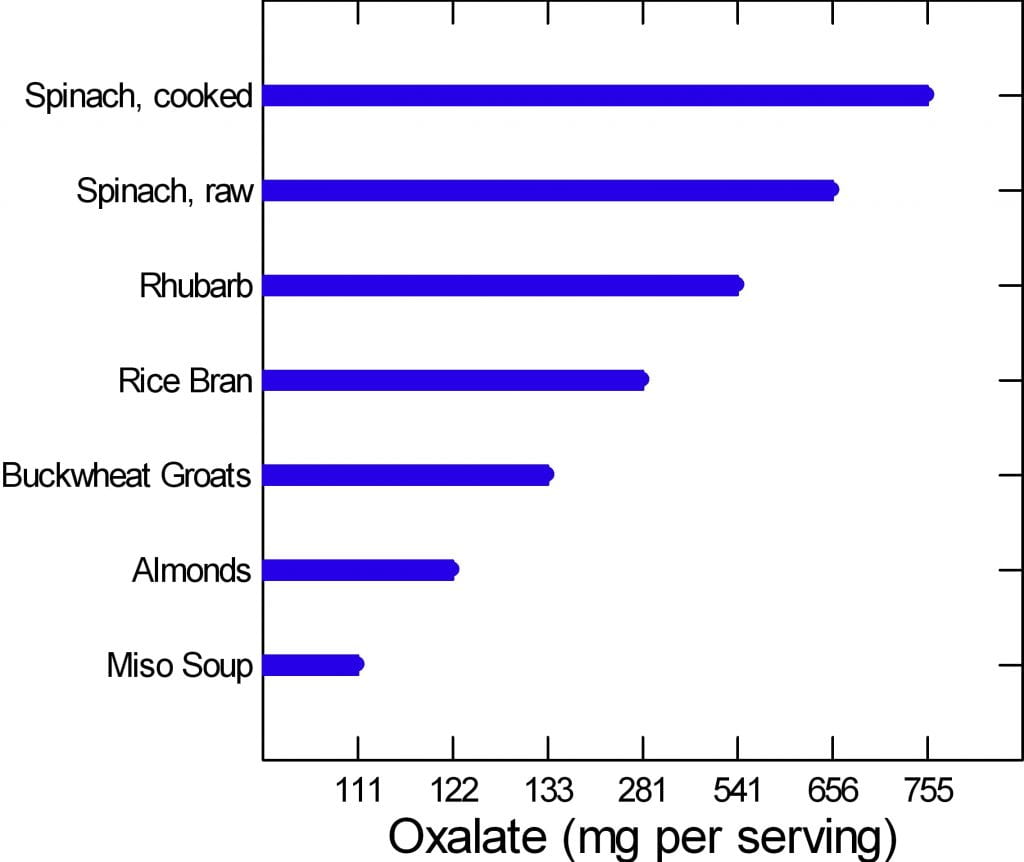 The graph to the left is of the very few dangerously high oxalate foods.
The graph to the left is of the very few dangerously high oxalate foods.
There are only six foods, but spinach, being worst of all, has two entries. Be careful of this plot because of its range. It begins at 100 mg/portion and rises to 755 mg/portion in only 7 steps, so the distance from miso soup to spinach is about a 7 fold increase.
Rhubarb and spinach are so high you just cannot eat them. Rice bran is something few will miss, the same for buckwheat groats.
People like almonds but have a hard time controlling portion size. If you can keep it to 11 almonds a day – the portion size that gives 122 mg of oxalate, alright. Otherwise stay away from them.
If you have to eat any of these foods, caution is hardly a strong enough word.
Are you sure you need to eat them?
Why?
WHAT ARE WE SAYING?
We are saying that oxalate is common in foods, and that you have to be careful, but care is a scarce resource. How much care can you give every bite? The graphs say if you eat moderately high oxalate foods – the first graph – be careful.
Watch portions.
If you are eating one of the six dangerously high oxalate foods, stop eating it.
It is too hard to be careful with those six foods. They have too much oxalate for most of you to handle. So, just say no.
WHY BELIEVE OUR DATA?
These data arose from a major effort at the Harvard School of Public Health. A world class expert has curated it twice. Harvard can be wrong and so can Ross Holmes, but both will tend to be wrong less often than the average persons who attempt to put complex data into the public domain. We have always appreciated comments, and if anyone has a peer reviewed publication with different food oxalate levels than ours, we will read the paper and see if it warrants our making a change.
Medical research is endlessly argumentative, and food oxalate is no exception. A recent paper contrasts findings from 6 websites and 2 applications and finds some wide variations. Of the sites, the Harvard site – used here as our reference, and the Wake Forest site – which is a legacy of an outstanding investigative group have most standing with me. Leaf through the comparisons between them in the 4 charts and in the large table at the very end. On the whole differences are modest. The hyperoxaluria and oxalosis list from the paper has been withdrawn from their site.
DO YOU NEED A LIST?
Sure, a list is nice. But we helping you here. Lists can run on to hundreds of foods. The picture is meant for focus. Here are the ones to focus on.
Many of you leave the doctor’s office thinking you will never be able to eat a fruit or vegetable again. If that wasn’t bad enough chocolate and nuts are gone, too. Some of this sadly is true, most of it is not. I am here to bring you good news: Almost everything, high oxalate or not, can be incorporated into your diet safely.
Do you need a low oxalate diet? You may if your stones contain calcium oxalate crystals and your urine oxalate is high enough to pose risk.
If you do need a low oxalate diet, what is your goal? Less than 100 mg of diet oxalate is good; less than 50 mg is ideal.
If you want to read some of the science about urine oxalate and risk of stones and about how we get to the diet oxalate goals, it is summarized at the end of this article.
Here we assume you do need to lower the oxalate in your diet.
CALCIUM FIRST
Low calcium diets can raise urine oxalate, and the solution may be as simple as a proper calcium intake. There is every reason for stone formers to eat 1000 mg of calcium daily to protect their bones. The common hypercalciuria of calcium stone formers puts bones at special risk when diet calcium is low.
Before changing your whole life around, ask yourself if you are avoiding calcium foods. If so, add them back and ask your doctor to check your urine oxalate again. It may fall enough that a low oxalate diet is not necessary.
If low calcium intake is not your problem, and you need a low oxalate diet, here is my take on how to do it.
WHAT IS THE DIET OXALATE GOAL?
Typical diets contain upward of 200 – 300 mg of oxalate. For stone prevention, a reasonable goal is below 100 mg of oxalate daily. An ideal would be about 50 mg daily if that can be accomplished.
To get there, consider the oxalate contents in common serving portions of all of the foods, and make up a plan for yourself.
FRUITS
FRESH
Everyone who comes to me is very unhappy thinking they can never have a berry again. This is Baloney. The only berry that is very high in oxalate is raspberries (look at the list). On the other hand, people do not realize avocado, oranges, dates, and even grapefruit and kiwi are very high and need caution.
This doesn’t mean you can never have these healthy treats. If you incorporate any of these high oxalate fruits into your morning yogurt you can reduce some of the effects of the oxalate content.
Also look at your portion sizes. You really cannot eat a lot at any one time. Dates are not a good bargain: One date is 24 mg!
CANNED OR DRIED
Canned pineapple is a problem.
Dried fruits have to be a worry because the water is taken out, so a ‘portion’ of dried fruit can be gigantic in oxalate content. Figs, pineapple and prunes are standouts. Just think: 1/2 cup of dried pineapple is 30 mg – not a lot of fruit for a lot of oxalate. If you want dried fruit, think about apples, apricots, and cranberry as lower oxalate options.
VEGETABLES
Spinach and rhubarb are standouts; stay away.
Other vegetables you need to be aware of are tomato sauce, turnips, okra, and yams (sweet potatoes) along with beans of different sorts.
I am not in the business of taking healthy foods away from people. But in the cases above you really must limit; there is just too much oxalate and these foods do not pair well with high calcium foods the way fruits can be mixed right into your yogurt or cereal and milk.
Many of you have been told to stay away from all green leafy vegetables. This is not true. Look at the list. There are plenty of salad options still available for you including kale. Even though tomato sauce is high in oxalate (see below) that is because of concentration. A whole medium tomato is only 7 mg and who eats more than one at a time?
Many of the salad vegetables are so low in oxalate they are freebies. Eat what you want.
POTATOES
These are Trouble! I put them into their own separate group even though they are vegetables.
From french fries to baked potatoes they are very high oxalate items. One ounce of potato chips has 21 mg of oxalate and who eats one ounce? Not I. Baked potatoes are terrible. One comes in at just under 100 mg of oxalate. Mixing sour cream into the potato will not help much; one tablespoon of sour cream contains only 14 mg of calcium. One ounce of cheddar cheese contains 200 mg of calcium, which could help, but it increases calories, salt and fat. But all in all, why struggle so hard? Potatoes are not ideal for stone formers.
DAIRY PRODUCTS
They have no oxalate. They are your main source of calcium. Use them. They can add a lot of salt – cheeses – and can be caloric. But they reduce oxalate absorption and preserve your bones.
For a stone former who has to watch salt intake, increase calcium intake, and lower oxalate intake, here is how to do that. You cannot have as much cheese as you want because of the salt. So portion sizes are very important. Yogurt, milk, even ice cream are good bargains – modest sodium and high calcium. These are a great place to add in a wee bit of chocolate – high oxalate foods – for those of you who cannot live without these high oxalate treats.
BREADS AND GRAINS
Some of the basic ingredients to make these foods are very high. White flour and brown rice flour are high in oxalate so everything you make from them will be high.
BREADS
Even so, as far as kidney stones go, breads are mainly alright because of portion size: not that much flour so one slice is 5-8 mg. French toast and New York style bagels top the list at 13 mg for two slices and 40 mg for one bagel – as much as anyone will eat of either food.
PASTA RICE AND GRAINS
Spaghetti, one cup cooked is 11 mg and most of us eat more than one cup.
Buckwheat groats, one cup cooked is 133 mg – I don’t see many of you saying ‘darn it’ or taking to your bed, but beware. Millet and bulger, wheat berries, rice bran, corn grits, and corn meal, these are widely used and are high. If you are using these, be thoughtful.
Here are some low oxalate options in this category: White rice, hummus, corn flour, corn bran, flax seed, and oat bran are popular and safe.
MEAT PRODUCTS
Since oxalate is only found in plant foods, all the meats are safe. Fish, too.
For our vegetarian friends, tofu and veggie burgers are very high.
NUTS AND SEEDS
These are just dangerous for two reasons.
Obviously they are very high in oxalate.
Secondly, I don’t know anybody who just has a few nuts at a time.
Just like chips no one eats one – the whole jar is more like it.
But, for one cup of pumpkin sunflower or flax seeds the highest is only 17 mg of oxalate and none for flax. For those of you who love foods in this category seeds are the better choice and they can be sprinkled on yogurt and ice cream.
SWEET STUFF
I have good news for my chocolate lovers. I know most of you have been sent home with a list and chocolate is high on it. But if you look at the numbers nuts are a lot worse than chocolate. Chocolate can be mixed in with dairy products, too, so as to reduce oxalate absorption.
Even so I do want to point out that half a brownie is on the high side, and who eats one half?
You can still satisfy your sugar craving but pay attention to your portion size.
Keep in mind, however, that sugar loads increase urine calcium loss which increases stone risk, so there are two reasons why this food group can be a problem.
But even without chocolate, you eat a lot of flour when you eat a piece of cake, so cake can be a problem – about 15 mg per piece, like french toast. Pies are half the risk because of their fillings – unless they are chocolate pies!
CRACKERS AND CHIPS
The big enemy here is potato chips. A one ounce serving contains a whopping 21 mg of oxalate. I repeat: A one ounce serving.
Your best bet in this category if you’re looking for something crunchy is corn chips – one ounce is 7 mg, popcorn – one cup is 5 mg, and pretzels, one ounce is 5 mg.
Crackers are OK mainly because they are small and the amount of flour is not that much.
BEVERAGES
PLANT SOURCES
Hot chocolate is the clear loser at 65 mg per cup; carrot juice is the runner up at 27 mg per one cup. Lemonade, tea, tomato juices, rice dream and the like are better but still high. The are 15 – 18 mg per serving. Lemonade – frozen concentrate – is 16 mg per 8 ounces so be careful about this as a source of citrate.
Soy milk, for those of you who prefer it, is not a good option. It is very high at 20 mg per cup. We have no data from standard sources for rice milk, cashew milk, and coconut milk; almonds are high in oxalate so the almond milk product will certainly be high.
Tea is so commonly used, here are the details. If you brew your own tea it is high in oxalate. The longer you steep your tea, the more oxalate it will have in it. If you use a sweetened instant iced tea one cup has 0 mg of oxalate.
Here are some juices that are low in oxalate and better substitutes: Apple juice, apricot juice, orange juice, grapefruit juice, grape juice. For all the lemonade drinkers, diet lemonade is low in oxalate.
Here is something very important: Coffee is oxalate free – almost, 1 mg for a cup (2 mg/cup for decaf). We already told you that coffee drinkers have a reduced stone risk, so lets debunk the coffee myth here: Drink it as you wish.
DAIRY SOURCES
Everything is good except chocolate milk. Even that is only 7 mg a cup for a sweet treat here and there.
ALCOHOL
What tops the list in this category is a can of beer: 4 mg of oxalate. All the rest are low and, frankly, the oxalate in a can of beer comes with a lot of fluid. This is not the problem area for stone formers.
WATER
If I didn’t say this to you I could not sleep well tonight. Water is the clear winner in this whole category. It is free of calories, sugar, and oxalate. Please use it as your main beverage and supplement with the items above.
SPREADS AND SAUCES
Chocolate, miso, peanut butter, and tahini are all high.
SOUPS
Miso soups is extremely high – 111 mg/cup. Lentil soup is high, and so is clam chowder – the potatoes.
BREAKFAST FOODS
This is a dangerous meal if you are a cereal lover. Many cereals are high in oxalate. I am afraid you need to look them up in the list by brand. Unfortunately the healthier cereals are highest in oxalate because they contain more plant based ingredients. Probably having milk in your cereal is wise, but we have no data to show.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
HOW DO WE MANAGE ALL THIS?
The first thing you need to do is to learn and remember what are the highest oxalate foods and beverages. Without this in mind it is impossible to shop and cook intelligently. Here is a short list of the highest oxalate foods all in one place.
BREAKFAST
For those of you who love cereal because it is quick and easy check out the list and see if the one you love is high in oxalate. If it is, choose the next best one with lower oxalate. Put milk in the cereal.
Alternatives to cereal that are also quick and easy: Yogurt or cottage cheese and fruit. The only fruits to worry about are raspberries because no one puts oranges on their yogurt. Bananas, peaches, blueberries and strawberries are perfect toppings.
More trouble, but no oxalate, eggs any way at all. Boil a batch on Sunday and have them for the week for breakfast, and snacks, too.
Your breakfast coffee is free and so is your water. For juices use orange, apple, pineapple, grapefruit – all great. If you want tea, don’t steep more than a minute and consider adding milk to it. Green tea is better than black.
LUNCH
Typically you are grabbing a salad or a sandwich for lunch, so what now? Many clients tell me they no longer eat salads because their physicians told them to stop all green leafy vegetables.
I’m bringing salads back to you.
Arugula, iceberg, romaine lettuces, and kale, are fine as your base. Stay away from spinach. Here are good toppings. Cauliflower, corn, cucumber, mushrooms, onions, peas, scallions, squash and zucchini are all fine. Tomatoes are fine, too; it is only the sauce that is high. Broccoli and green pepper are moderately high so watch the portion size.
Sandwiches will cost you between 12 and 16 mg of oxalate depending on the bread you are using – 2 slices. This doesn’t mean you can never have a sandwich, it just means you have to keep track of how much. You can have 50 to 100 mg daily. What goes inside between the two slices of bread is usually cheeses and meats which are oxalate free. So sandwiches are not something to be afraid of.
SUPPER
Beef, chicken and fish are all fine, and those the main courses for most of us. You will run into problems if you are a pasta or potato eater. If you are you need to limit the amount of times you have these foods each week and also the quantity each time you use them. Substitutes are a problem: White rice is a nice substitute for potatoes but there are few others. It is more veggies that have to fill in – very healthy but not as much fun.
Here is a recipe for cauliflower – ‘mashed potatoes’ you will like and even think, sometimes, is the real thing. There are many versions on the web, choose the one that makes you happy but be careful about the ingredients.
There is also quinoa which is not on our lists, but may well be high. A recent scientific article on this plant does not give oxalate contents which suggests they are not reliably known.
I have recently put together a private FB page called THE Kidney Stone Diet. It is a group that helps educate you on your physician prescribed treatment plans. As you can imagine, oxalate comes up in many posts. I moderate it to keep it clinically sound. Come on over and join the discussion!
URINE OXALATE AND RISK OF KIDNEY STONES
I promised you some science – here it is for those interested. It concerns only highlights from the food – urine oxalate research recently performed and seemingly germane to the problem of how stone formers should control oxalate intake.
The most useful data about urine oxalate we have so far is from three cohorts studied by Dr. Gary Curhan. Two are cohorts of nurses one a cohort of physicians. These people have kept track of many aspects of diet and health for decades, and among their records are onset of kidney stones.
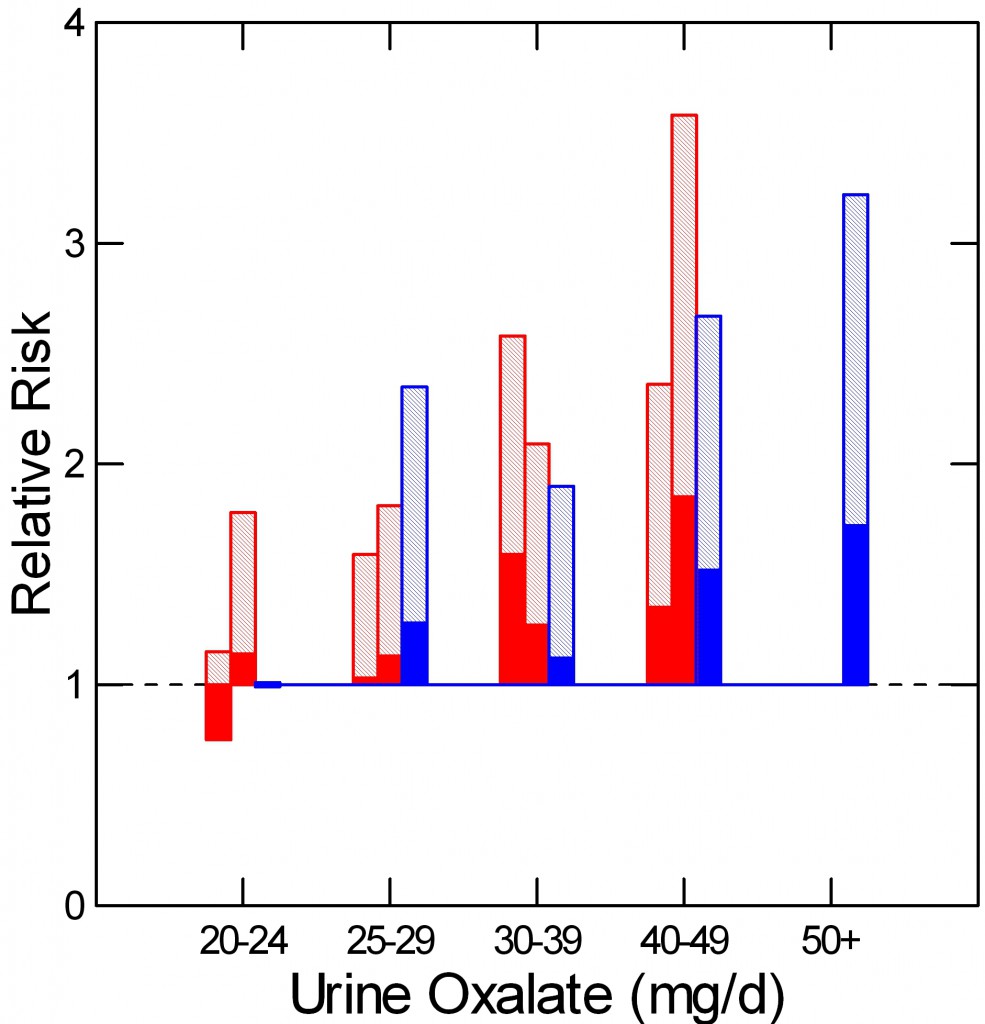 As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
The two nurse cohorts are red, the physicians – all men – are blue. The dotted line at 1 is the risk threshold: Above that line, risk is present.
The top of each crosshatched bar shows the mean relative risk for each of the five urine oxalate ranges. Clearly the mean goes up as urine oxalate goes up.
But the mean relative risk has a range of uncertainty around it. The bottom of the solid portion of each bar is the lower 95th percentile for that range of uncertainty. When that bottom lies above 1, risk is very likely to be present.
For both the women and men groups, that point is reached between 25 and 30 mg of urine oxalate a day. Therefore one wants to try to get urine oxalate below 30 mg daily and even lower, below 25 mg daily if possible. The average urine oxalate excretion among the women in this study was close – 26 and 28 mg/day for those who did not form stones and just a bit higher for those who did – 28 and 30 mg per day. The men are a problem: 39 and 41 mg/day for those who did not and those who did form stones.
This is not diet oxalate, it is urine oxalate. Urine oxalate is how much the body makes and how much is absorbed from foods. Mostly, we can control only the second part – how much is in the food.
HOW MUCH DIET OXALATE DAILY
All dietary advice depends on having a reasonable goal in mind for oxalate intake. My goal of 50 – 100 mg of oxalate from food daily is not unreasonable given the research that has been done in normal people and stone formers.
Holmes and colleagues found a urine excretion of oxalate of about 10 mg/gm urine creatinine in normal 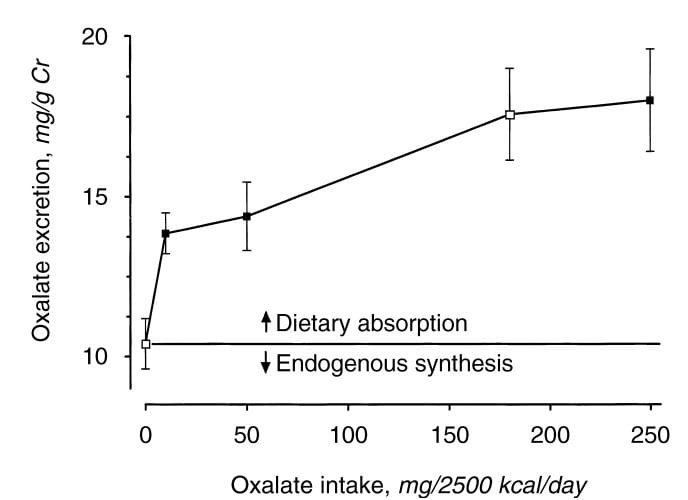 people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
From this work the percent oxalate absorption could be calculated as around 10 – 15% and the contribution of diet oxalate to urine oxalate excretion as around 25 – 40% when intake of oxalate was between 50 and 350 mg/2500 kcal. Therefore one can consider a whole food 1000 mg calcium 50 mg oxalate as a usable low oxalate diet, and a 150 – 250 mg oxalate diet as relatively high.
The balance between diet calcium and diet oxalate does not matter greatly if diet calcium is high. Among normal men and women eating 1000 mg/day of calcium and 750 mg/day of food oxalate, 24 hour urine calcium was about 110 mg/day and oxalate about 44 mg/day.
If the calcium oxalate balance is altered so calcium intake is 400 mg and 20 mg of oxalate at breakfast and lunch, and 200 mg of calcium and 710 mg of oxalate at dinner, as compared with simply 333 mg of calcium and 250 mg of oxalate in all 3 daily meals, urine oxalate is lower after the high calcium low oxalate meals, but only slightly higher after the high oxalate low calcium evening meal than when calcium and oxalate intakes were balanced. This means that when diet calcium is at least 1000 mg daily the balance of calcium to oxalate within any one meal is not likely to affect stone risk.
Seiner and colleagues make clear that stone formers are different from normal people. They divided male and female stone formers into 2 groups of 93 people each, one with urine oxalate above 0.5 mmol (~50 mg) of urine oxalate daily and the other with urine oxalate below 0.4 mmol (~40 mg) daily. They found virtually identical calcium and oxalate intakes: 845 vs. 812 calcium and 101 vs. 130 mg daily of oxalate respectively in the lower and higher urine oxalate groups. But the below 0.4 mmol group excreted only 27 mg of oxalate daily on average, whereas the high oxalate group excreted 64 mg daily. In other words diet was not responsible for the higher urine oxalate excretion, suggesting a difference of oxalate absorption. Those prone to high oxalate excretion seem, therefore, to most need diet modification.
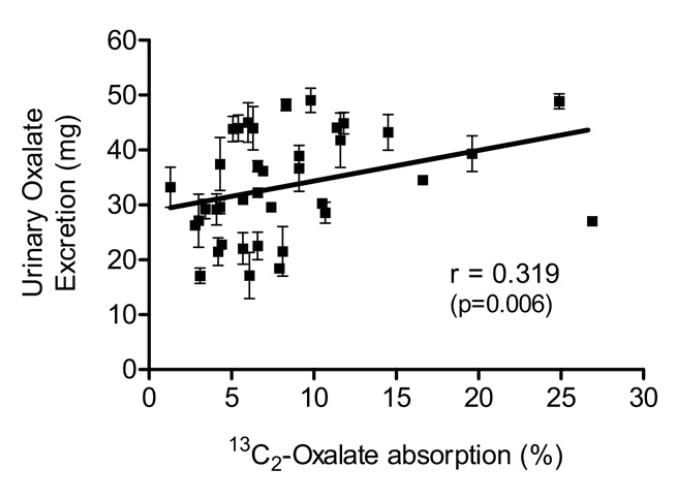 Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
PROTEIN AND GELATIN
Diet protein intake does not affect urine oxalate excretion. In 11 normal people fed a 1000 mg calcium, 51 mg oxalate, 3000 mg sodium fixed diet, varying protein intake from 0.6 to 1.6 gm/kg/day – a very wide range – did not alter urine oxalate appreciably (mean values were 23, 23, and 25 mg daily for the three protein intakes) even though oxalate precursors like glycolate rose markedly (25, 22, and 46, mg daily).
Jello is a source of hydroxyproline which converts to glycolate and oxalate, and oral loading with gelatin can raise urine oxalate. Ten normal people eating a 1000 mg calcium, 150 mg oxalate diet (typical normal level) were fed supplemental gelatin as one quarter of daily protein intake. Urine oxalate was 24 mg daily vs. 17 mg daily when the same diet was supplemented with whey protein – containing little hydroxyproline – as a control. So lots of jello is not an ideal plan for stone formers.
Where does this leave us about how much oxalate is alright for a day. If diet calcium is high, as it should be, at about 1000 mg, then one should try to limit diet oxalate below 100 mg daily. Perhaps this is most important in those patients whose baseline oxalate excretions are higher – in the range of above 40 mg daily.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life.
For those who need special help, I run an online course: The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.



What are the studies of adding Magnesium to ones diet through the way of Magnesium Citrate supplements? I hear they can help somewhat in preventing Calcium based stones.
Hi Tim, although I have not published them, there have been magnesium trials – negative I am afraid. It does not appear to work. Regards, Fred Coe
I have a question, does flax milk have less oxalate levels than almond milk?
Hi Roxanne, I hope Jill answers this one. I do not know. Regards, Fred Coe
Roxanne,
In our article on how to eat a low oxalate diet we speak of flax and that is is one of the safe seeds. Enjoy the flax milk. It is on the lower side, much lower than almond milk.
Jill
I’ve had 2 lithotripsy procedures in the last 2 months. I had a mini gastric bypass in 2001 and cruised along pretty good for 8 or 9 years. Then the stones kicked in and I’ve had so many I couldn’t begin to count them all. I just saw my first urinalysis test today and it reads like this. Volume 253, ss CaOx 749, urine calcium 94, urine oxalate 144, urine citrate585, sscap 0.47, 24 hour urine ph 6.258 ss uric acid 0.20 urine uric acid 0.419. For the last 5-6 years I’ve been passing a stone a month sometimes 2or3, Needless to say lots of pain and even more worry about when the next one might come. when I started the lithotripsy 2months ago I had 6 stones that were 7mm to 11mm (2 were 11mm). I’m not a drinker and have been making an effort to drink a lot more water, I’ve looked at high oxalate foods and other than potatoes and peanut butter maybe a few others on the list I don’t eat a lot of high oxalate foods. My urologist told me today to drink 2 glasses of milk a day and try to cut back on the higher oxalate foods. what are your thoughts on this, thanks Bob B
Hi robert, I guess the very high urine oxalate catches one’s eye. The volume you quote is surely incorrect, I imagine it is 2530 ml, and the ss CaOx looks odd but is probably 7.49. Your physicians must be very concerned about the oxalate and will surely want to lower it. Not only can it cause stones but also there is a real risk of kidney injury. It is not the foods it is the bypass procedure, surely, and there are approaches to treatment. Be sure the oxalate is lowered as much as possible. Regards, Fred Coe
Hi,
Thank you for this thoughtful and comprehensive post.
As often is the case I see discrepancies in online lists that are confusing.
Hummos LOW / Tahini – HIGH
“Here are some low oxalate options in this category: White rice, hummus, corn flour, corn bran, flax seed, and oat bran are popular and safe.” Hummos is made with tahini so I am confused. And I really want to have hummos. Blueberries and yogurt are mentioned here as a good breakfast – but I have a bewilderingly bad reaction to nice seasonal organic blueberries (listed elsewhere as confirmingly HIGH).
Any further thoughts on this?
Many thanks,
D.
Hi D. The lists here are by the best experts in the field – I am not one of them. Ross Holmes went over the oxalate contents and he is really the authority. I trust him and the list. The origin of the list was the Harvard Public Health people, and Ross made additions and corrections. So it is what it is, and I know many online lists differ – from us and from each other. This is an odd site; it is from a stone program at a university and I and those I work with are – if imperfect, certainly, at least careful and bound by the best science we can find. If better data become available, we will certainly seek to publish them. Regards, Fred Coe
Hi D,
I think you will be ok with hummus, as it’s mainly chickpeas…the reason tahini is high is because it’s just ground-up sesame seeds, which are very high. You could make your own hummus and just leave out the tahini altogether, there isn’t a lot of it in hummus anyway. I don’t know about the blueberries though :(.
Hi,
I just had lithroscopy last fall. Today went for a followup to my last week’s ulstrasound.-my procedure was done on my left with one left at the very bottom at 2mm. It appears I have 2 new stones in my right kidney, one at 3mm and one at 4mm. I know this is due to my high oxlate diet, however, I have been trying very hard to restrict some of the good foods that are high. I no longer eat spinach, kale, potatoes (any of the high items)! I love all fresh fruit and veggies, very little salt or process foods. I love coconut milk, greek yogurt as well for calcium intake. I am frustrated at what I can continue to eat without enlarging these stones. I am also trying to drink my 10 glasses of 10ounces of water!
Any other suggestions? I want to continue eating clean and healthy but feel I am at a point where I can not eat anything!
Thank you!
Hi Lisa,
There are plenty of fruits and veggies that you can eat and of course lean meats as well. Please look at the list in the article and use the high oxalate products sparingly, and the low oxalate products more. You can eat kale.
Have you had a 24 hour urine collection? If so how high was your oxalate levels. Let us know.
Jill
Dr Coe. What are your thoughts on chance piedra for kidney stones?
Hi Holly, I have been asked this before and looked. I can find no studies reported in PubMed – the national repository of science articles. So, no data. No data means could be good, could be bad, could be nothing at all. Take a look yourself, it is free to everyone. Let me know if you find anything. Regards, Fred Coe
Hi Tim, Jill,
Thank you for this great article and the wealth of information on this site. I passed my first stone last week, ouch! I put together a quick web app to make searching/viewing the list of foods you provided easier from a mobile phone, or desktop. I hope you and/or your viewers find it useful.
http://oxalates.site44.com
Best Regards,
Payam
Hi Payam, I am a bit confused. If you have copied the data from the tables on my site and made them into a web source, you have an obligation to make clear their provenance, which is mixed. The lists arose from the Harvard school of public health and were modified by Dr Ross Holmes. They are meant as a complement to the article Jill wrote on who should use them and why, and to what extent. To place them into an app of your own may be a nice service to others but it is not your work and it isolates the mere measurements from the cognitive source of the article with its references. Have you assured that you have copied the results without errors? Without a link to the original article, how will people know the best ways to use it and how to determine if these lists are important in their individual treatment? If, long term, results put up on a site like mine seem to wander off without proper links back, is it certain the site will remain available? Regards, Fred Coe
Diagnosed with ‘secondary oxolosis’ 4.7.16. Help! All information and suggestions gratefully recieved. Creatinne level 325 & climbing.
Dear Colleen, I do not understand the word secondary. Do you mean high levels of oxalate in the urine due to bowel disease? Is it instead primary hyperoxaluria? These are both very serious especially when kidney function is impaired. My suggestion is that you consult at the nearest medical school as these conditions are uncommon enough that even the finest practitioners are not likely to have managed very many patients. Regards, Fred Coe
Hi & thanks for responding.
Diagnosis from kidney biopsy. Creatinne levels from bloodtests. I’ve started low oxalate diet. 6 week pelvic radiation treatment begins 20.7.16, so I’m a bit of a challenge!
Hi Colleen, You really do have a very complex situation and I am sure your personal physicians are doing the right things. I gather the oxalate disease was diagnosed by kidney biopsy showing calcium oxalate crystals in your kidney tissue. Given the radiation there is clearly more wrong and I hope for a good outcome for you. It might be important to measure the amount of oxalate in the urine – routine kidney disease can cause some crystal deposits in kidneys but usually not large amounts of calcium oxalate crystals. Regards, Fred Coe
Yikes! Please help. I’ve seen a handful of lists rating oxalate amounts of foods and many are in contrast from this one. This lists looks very complete, which is wonderful, but for example, your list says blueberries are low, in moderation. The other lists I’ve seen place blueberries, along with other berries, as very high and to be avoided. Please help my confusion. Thanks!
Hi Lisa, These lists arose from the Harvard Public Health school and were then vetted and edited by Dr Ross Holmes who in fact made many of the measurements currently available. It is the best we can make of all of the available data. We know about the many divergent lists and believe they are simply not always based on reliable measurements. I am not myself a primary investigator measuring food oxalate but Ross is, and I don’t know how else to offer better right now. One list, from the Oxalosis Foundation was pulled down by them because it had faulty data, indicating a high level of responsible behavior from that organization. Others who offer lists should be sure their offerings are indeed accurate. We are not so sure they all are. Regards, Fred Coe
It seems that every 3 months I’m having 10mm and 11 mm stones shocked. My urologist tells me it’s just a “heredity” thing. I should drink lots of lemon water and cut out protein such as meat. I no longer believe this after reading your article. I have changed my diet according to your list, which I hope helps. My question is this: I am Type II diabetic, so I’m wondering how to incorporate a low oxalate diet, including 1000 mg of calcium per day, along with 10+ glasses of plain water, without messing with my sugar levels too much. Orange juice would be a prime example – low in oxalate, high in sugar. Any help you could offer would be greatly appreciated! Thanks so much for such a thorough, proven article.
Liz
Hi Liz, I guess my question would be whether you know what the stones are made of. Are they really calcium oxalate? Diabetics often make uric acid stones. If calcium oxalate, what do your 24 hour urine tests show. Diabetics often have very high urine calcium levels and oxalate is not the problem. Take a look at this plan and see if you have really had a full evaluation. If you have a high urine oxalate and need to lower it, and also to watch your sugar intake I think you might just contact Jill Harris – who wrote the article. She often speaks with people and helps them personally. Regards, Fred Coe
Hi Liz,
I get this question all the time. it is tricky but certainly very doable. I am happy to help. Write me at jharris1019@gmail.com and I can give you advice specific to you and perhaps you can hop on a call with me which might be easier.
Very Best,
Jill
You write that the goal is 50-100 mg of oxalate per day. How much for a child of 8 years?
Hi Natali, This is an important question because children do not usually require low oxalate diets. Is there evidence that your child has a high urine oxalate? If so, are your physicians sure it is from diet or is it from primary hyperoxaluria. Please be very careful about this matter. I do not know the correct figures for so small a child, and would suggest that your child be seen by someone very expert in this area if there is a urine oxalate elevation. Regards, Fred Coe
My daughter was in the hospital. She has been diagnosed with Tubulointerstitial Nephritis. She has a high urine oxalate. The doctor said that we need a low oxalate diet. But did not give clear recommendations. In this article I understand everything and I want to follow these recommendations. But I’m not sure what goal to deliver. Whether 50 normal goal for child?
Hi Natali, I am concerned your daughter may have primary hyperoxaluria which can cause what appears to be interstitial nephritis but is due to calcium oxalate crystals. I would contact the Mayo Clinic – Dr. John Lieske – and bring her to his attention. They have a rare disease consortium there and a vast experience with this specific disease. Regards, Fred Coe
Thanks for the Google sheet list of foods and oxylate content. It will be very useful but I did wonder how a serving of cake could have as much oxylate as a cup of AP flour. A typical layer cake takes 3 cups and makes 8-12 servings. Thanks.
Hi.
I see your confusion. I am afraid I do not have an answer for you. Who knows how big the piece of cake was, who exactly what kind of flour was used? Perhaps Dr. Coe has an insight.
Best-
JIll
im looking for a complete listing of all foods that are low in oxalate and high my niece 31 yrs old has had stents put in kidneys hospital twice surgery twice has major issues cause of kidney stones where can we find a complete listing at
The article and your website are very helpful. Can you tell me if sunflower lecithin or soy lecithin contain oxalates? They’re in a lot of protein powders. Thanks.
Hi Alex, here is the truth. What we know is on those lists. What is not on them is so far as we can tell not known. Oxalate contents of food materials are hard to come by and no one wants to pay for the measurements. Sorry I have not more for you. Regards, Fred Coe
Hi Alex,
Since we know that soy lecithin does indeed have soy in it, I think it is safe to say that protein powders made with it would be a higher oxalate item.
Warmly,
Jill
There’s no real way of knowing. However, given the fact that soy lecithin is tolerated by the majority of people with soy allergies, I would venture to guess that there’s probably very little actual soy in the protein powder and, therefore, very little oxalate per serving.
Frank: please don’t be sorry. Both comments were a big help.
At the end of this article you mention the study where gelatin raises urine oxalate. If there is gelatin (or kosher gelatin) in yogurt and a stone former eats two small Yoplait containers a day, can that raise urine oxalate also? Or would those amounts of gelatin be too small?
Thanks,
Alex
Hi Alex, it is possible if someone is very sensitive to food oxalate and absorbs a high fraction of it. But if the amounts are small, as you describe, it is unlikely to be a contributor. Regards, Fred
Sorry… Fred!
In the “useful table of oxalate foods”, my question is on pancakes. When listed under bread, the pancakes are listed as (mix), (home made), they are listed 10 mg and 11mg respectively, then lower on the list under Breakfast, they are listed at 37mg and 22mg. Could you please let me know which is accurate. Thank you.
Hey Mick-
Even though we stand by this list and know that it comes from the highest level of scrutiny, it can also be confusing. I assume that although they did not list what pancake mix they tested it was different in each case. Depending on the list of ingredients, it would vary. Not very helpful, huh?
Personally, pancakes are not the healthiest item in the world, so I would just eat them when I wanted a “treat”. I would also just consider them a higher oxalate product and if you are limiting oxalate, limit pancakes.
Also, just because something is on the high list doesn’t mean you can NEVER eat it. The easiest way to lower the oxalate is to just lower the quantity you are eating during a sitting.
Thanks for writing and I can only hope this wasn’t a dreadful reply.
Jill
This was very informative and written in a non-technical way AND the comments were recent. I just got thru my 2nd bout of stones within 2 yrs. This last one required 1 month off and on in the hospital and surgery. So yesterday I got the analysis of my stones back-the 2 similar but different oxalate stones. The diet boggles my mind that the doc included. While I am not a strict vegetarian, I’ll eat a burger maybe every couple months, my diet consists of mainly everything on the “avoid” list-requires me to drink “at least 2 glasses of milk a day” Ewww-I cannot stand milk. So milk, pop(specifically colas) and water and was told to limit water as it has no nutritional value. Most veggies are to be avoided-everything in my garden is to be avoided except small quantities of cukes.
The 1st time I had stones, my (now retired) urologist took me off calcium supplements, I had had another doc have me on 8K mg of Vit D a day. The uro doc took me off everything-then I understood the massive VitD may have played a role, also the parathyroid came into the pic. In the last less than 2 yrs, my calcium level is normal to slightly low, and my PHP (parathyroid) has been close to normal-down by almost 1/2 from when I had the 1st stone issue, and my Vit D is in the low range in the normal numbers.
So I am confused as to-why stones again? Or why the 1st time? All my numbers are normal now. The 1st time nothing was said about the low oxalate diet-although it was the oxalate stone then, too. They went off on the D and parathyroid. I am currently seeing an internist, urologist and endocronlogist, then they wanted me to see my family doc every week “just to check in” I feel they’re milking me and my insurance-no pun intended. But the difference in treatment/diet within the 2 yrs makes me wonder. Are there other causes for oxalate stones than high oxalate? Why was I told to limit calcium the 1st time and now have to drink 2+ glasses a day? I am more confused having gone thru this twice now. If this diet is correct-no way can I drink milk and eat meat like they suggest-are there any alternatives? I’ve eaten this way 40+ years and only had stones within the last 2-in my late 50’s. Sorry to ramble… Thanks
Hi Stoner, I fully understand the confusion, and hope I can be of help. Try this article and see if you can follow it from beginning to end asking the questions and lining up the answers. Likewise, as a second one, this summary. It is do hard to do prevention without a clear method, and this is mine – it will get you there. Regards, Fred Coe
Thanks for your prompt response. I do have a urine save and blood work coming soon. The internist got me into the endocronogist within days after my last hospital release-telling her I had extreme hypercalcemia, which confused her as my calcium had been low to normal in the hospital. I held up on the tests, as I was wiped from all the runaround (I had been initially admitted with septic shock, which they said was due to the stone blockage.) Besides the usual nausea, all they would give me was 7 up-which I can’t drink. The food was horrendous, no matter what you ordered-pop, cinnamon rolls, lunch meat sandwich etc. was what they brought. I was begging for something good-like veggies and was refused. They also push Flomax for passing stones, which my former retired uro doc said was nonsense. During urine saves/bloodwork and the PTH tests that my 1st endroconlogist ordered 2 yrs ago, on my return visit, when I asked the results, he told me “let me worry about it-you don’t understand” I wanted my PTH number-I know what normal range is and I had been in the 130 range. My DIL, who’s a nurse, suggested (other than that was wrong) to ask my family doc, who also refused “because he didn’t order the tests”, although he had sent me to his buddy the endro doc. Finally I went off on a rant at my ob-gyn’s nurse several months later, she talked to my ob-gyn, who accessed the “other hospitals” records and printed out my test results. As far as I can tell, everything looks reasonably normal, my PTH had dropped to the 80 range-although the 1st endro doc told me I needed surgery-either 1 Dr at Uof I, 1 in Madison, WI or Mayo-in that order. Yet my PTH dropped. They did all the tests in the hospital, but for a patient to get-it’s impossible. And I’m confused why I have been told to quit drinking so much water since there are no nutritional benefits. I had been under the impression that the parathyroid had caused the stones 2 yrs ago and to just finally hear about the oxalate-that wasn’t even brought up thru several weeks of in and out in the hospital.
Dear Stoner, I am as confused as you are. The serum PTH can be high because of low calcium diet, vitamin D deficiency and many other disorders. Primary hyperparathyroidism generally raises serum calcium above normal, and serum PTH is not suppressed below normal, and urine calcium excretion is not extremely low. I cannot tell what is wrong in your case, so much information missing. Perhaps you do indeed need to gather up all of your lab results from all sources and compile them by date as a help to your physicians. The university medical school in Madison WI and the Mayo Clinic deliver a very good level of medical case, so I also a bit uncertain as to why things are so uncertain. Try doing your own compilation and sharing all of the results with someone in these institutions who is taking care of you. As for stone prevention, which is your obvious goal, here is a good reference as to how to organize things to get it done. Regards, Fred Coe
first of all, thank you for this important site and your dedication to informing people about kidney stones.
i have two questions, and i’ll use another form for the second one. i remember reading some time ago, but have forgotten the source, that of the high oxalate foods, only several actually contribute to stone formation. perhaps this is due to how they are digested. do you know of this study and can you respond? thanks, terry
Hi Terry, You have asked a fine question in that it raises important issues. Oxalate is a risk factor for calcium oxalate stones – that is accepted medical information. But, why do we say so? The stones are made of it, so that makes the case, sort of. But oxalate makes calcium oxalate stones with calcium, meaning in some – perhaps many – people calcium is at fault. At fault seems a good way to put things: Stones can know about only supersaturation, which is – roughly speaking – the product of the calcium concentration multiplied by the oxalate concentration. The concentrations are the amounts of each in the urine daily divided by the volume of the urine. So if you eat more oxalate, and raise your urine oxalate – both are necessary, for any given amount of calcium in the urine and, by the way, any given urine volume, the product of the calcium by oxalate concentrations will be higher and therefore the supersaturation will be higher. This should put diet oxalate into some perspective. Three factors set urine calcium oxalate supersaturation – the only thing crystals can ever know about – urine volume, urine calcium excretion, and urine oxalate excretion. Urine citrate also plays a role, because citrate binds calcium so it cannot mate with oxalate. It should therefore come as no surprize that urine volume, and urine excretions of calcium, oxalate, and citrate are the four factors that are epidemiologically well linked to new stone onset. So, diet oxalate matters by indirection. No study has proven that diet oxalate itself causes calcium oxalate stones though it surely is important, and no trial has shown that reducing diet oxalate reduces new calcium oxalate stones – although common sense would make that point obvious. As for specific foods, given what I have said, I guess it is more or less that the foods with the most oxalate – spinach is a prime one – are the most risky. Also potentially risky is low calcium diet. Urine calcium may not fall so much as urine oxalate rises, so one can possibly make matters worse. Thanks for asking – warmest regards, Fred Coe
hi. concerning increased calcium consumption vs oxalates, which of the several calcium compounds available respond most effectively in tying up oxalates in the gut? and recent studies have suggested a correlation between calcium supplements and prostate problems. can you comment to that? thanks, terry
Hi Terry, Once again, thank you. It is not which calcium produce or high calcium food it is that the calcium be eaten when the oxalate is eaten. Just as calcium mates with oxalate in the urine, it mates with oxalate in the bowel lumen, and the result – calcium oxalate crystals, makes oxalate absorption go down and urine oxalate with it – or at least this is current teaching by my colleagues who study oxalate. My favorites are to use a high calcium food in every substantial meal, preferably within the meal. A calcium supplement 350 – 500 mg is probably alright but needs to be with the other food. As for prostate problems, I have never heard of a calcium supplement issue. Warm regards, Fred Coe
Hello Dr. Coe, I had my first bout of kidney stones in 2007. The urologist said that the stone analysis showed that it was a Calcium Oxalate stone made of about 98% Calcium. If I remember correctly, it measured somewhere between 4mm-5mm in diameter. He suggested drinking a couple of liters water, especially first thing in the morning and before bedtime. He also suggested taking ‘Citric K’, (not sure if that is the right name for the prescription, as I ended up not taking it). He said I could drink Lemonade and even a Coke to try and get some citric acid into my system. At that time, a clump of ‘kidney stone forming’ masses were detected resting in the bottom inner folds of each kidney. Nine years on, now 2016, I had an x-ray of my spine done by my chiropractor. Many white stones were seen in those x-rays in each kidney. Depending on the gray lines running between the white stones, there look to be about 8 stones in each kidney; the largest measuring 6mm in diameter. My question is should I return to the urologist or should I try and find a nephrologist? Secondly, until I find a doctor, could I continue to take supplemental Iron, (my recent blood work shows that I am slightly anemic), Magnesium Citrate, SAM-e, Glucosamine, and Zinc. Do these play a role in raising urine oxalate or promote stone formation? Thank you for your time.
Hi Heather, It sounds like you are an active stone former and have produced a number of stones silently over about 9 years. YOu need to pursue prevention in an organized way, and I suggest this route. The nature of the physician is not so critical as the manner of how you get yourself evaluated. I am sure physicians who are convenient for you will be happy to do the few things this approach requires. Iron for iron deficiency – if that is what you have – should always be supervised by your physician. Mg citrate, and the other agents you mention have no known role in prevention. Try to put together a good prevention plan using the article. This one is a kind of summary you might find useful as well. Regards, Fred Coe
Long time kidney stone sufferer. Since 1999, I’ve had 16 surgeries for stones. The stones continue to grow in size with the last 2 episodes producing stones 2-3cm each which are causing blocked ureters. I am trying yet another urologist due to insurance changes. The latest 24 hour urine test for stone risks show hyperoxaluria, marked hypocitraturia and mild hyperuricosuria. My urine citrate measures 450 for males, urine oxalates measure 69 (range 20-40)urine uric acid 0.867 (range ,0.800 males), sodium 335 (range 50-150), chloride 332 range 70-250) and urine creatinine 31.4 (range 18-24 males).
I make different stones. I have been advised to increase mu Urocit-K from 10 mEqs BID to 15mEqs TID, a low oxalate, low calcium, low sodium diet. I was advised NOT to drink lemonade to acidify my urine.
The conflicting information on what I should eat or dink is driving me crazy. Can you give me any guidance?
Hi Jerry,
Sorry to hear about all your trouble with kidney stones. They are a terrible thing. I can understand your frustration with diet and fluids. I would like to offer you the opportunity to have a complimentary call with me to help sort it out. Feel free to write me at jharris1019@gmail.com. You have much going on and it would be difficult to get all info needed to give best advice.
I will tell you this- with the right advice you do NOT have to suffer like this anymore.
Write me to set up the call if you like-
Jill
Hubby,67…stones since 29 years old…defy diets…stones anyway
Help,
Carole
Give me a bit more Carol. Has he had 24 hour urine collections done? Does he have any other medical conditions? What types of stones does he make? The more you give me, the better I am to you…
Talk to us!
Until then,
Jill
Hi Jerry, The high urine oxalate is probably dietary, and perhaps Jill Harris can help you with it. Certainly the low calcium diet will worsen the problem and is not advisable. But your stones – are they in fact calcium oxalate, or are they calcium phosphate? You do not mention a urine calcium; is it high? Your urine sodium is massive meaning you eat a lot of salt; this might be raising urine calcium losses in the face of a low calcium diet, which is not ideal. Take a look at a way to help you organize your care so you can fill in the missing pieces and make it easier for your physicians to reduce stone formation. Regards, Fred Coe
Husband (22) just came back from Dr after 24 hour urine analysis. Told to limit calcium, sodium, and red meats. What is he supposed to eat?! I feel like what I read is contradicting. His Dr. said to limit calcium, but lots of articles say that it’s okay?
Hi Micaela,
I know it sounds like a ton of information, but it is very doable. Calcium should NOT, I repeat, NOT be limited. Normal amounts of calcium, about 1,000 mg/day by food is best. Most adults come nowhere near that. Limiting sodium and meats (all animal meats) is not too hard to do if you have the right guidance (and of course discipline). If you need help just reach out. I am happy to give a complimentary call to start him off if you would like. Email me at jharris1019@gmail.com and we can set up a date and time.
Jill
I am 57 years old and have had kidney stones twice in the last 5 years. Both times were within 2 weeks of starting to take chewable tablets containing calcium. One was a fiber supplement that also contained calcium and the other was antacids. I have not read anywhere about a connection between chewable tablets and stones, but it sure seemed to be there for me. I have taken vitamins containing calcium for years and never had a problem. When I stopped taking the chewable tablets each time there were no more stone problems.
Hi Gary, If you have, as an example, idiopathic hypercalciuria, a sudden burst of calcium can raise urine supersaturation and promote crystals and stones. That seems likely. As for calcium supplements they are safer taken with meals, never alone. Be sure and get at least one CT so you know what is there. Regards, Fred Coe
This article is really helpful! The prospect of finding things to eat was daunting with the short list I got from my doctor, but your updated/more comprehensive list and all of the helpful hints about how to work things in makes the task much easier. Thank you!
Hi Gretchen,
Thanks for taking the time to write us. We know that eating a low oxalate diet can be -at the very least- a bit overwhelming. Let us know if you have any questions.
Enjoy the rest of summer-
Jill
I am curious to learn more about the oxalate content of stevia. In the section about sweets, you note that one teaspoon of stevia contains 42 mg of oxalates. Is that pure stevia leaf or something else? Stevia leaf and extract are so strong that it would be unusual to consume more than a pinch of crumbled stevia leaf, or a drop or two of extract; can you point me toward the primary data source for the oxalate composition of stevia so I can look into this? Thank you!
Hi Patsy, I looked on Pubmed and found nothing. I will write to my colleague Ross Holmes who is the real food oxalate expert and ask him where the number came from. Given the stevia alkaloids are themselves not likely to metabolise to oxalate – they do not, it must be leaf preparations, and leaves contain oxalate variably depending on the source. Thanks for the valuable question. Regards, Fred Coe
Professor Holmes shared the source with me: ‘The value for Stevia was included in the Low Oxalate Cookbook – Book 2, published by the VP Foundation. Assays performed by Mike Liebman. I noted quite a few Stevia products on the supermarket shelf. I imagine the oxalate load in a teaspoon (5 g) is around 150 mg, so it should be avoided. There are plenty of non-oxalate choices.’
Regards, again, Fred Coe
What about turmeric? I’ve read it’s very high in soluble oxalate, but it’s also meant to have many health benefits. Would you advise avoiding turmeric? Or perhaps taking it with a bit of calcium to form insoluble oxalate?
Hi Mark, I am going to leave this one to Jill. I don’t like turmeric much. Regards, Fred Coe
I hate to say it but yes, it is high in oxalate. Check out this link (http://ajcn.nutrition.org/content/87/5/1262.full)
I take turmeric as a supplement as I have had cancer and it a great anti-inflammatory agent. Eat it with some dairy product for the calcium. But, yes, if you are watching your oxalate consumption, I would go for lower doses of it.
Thanks for writing.
Jill
This is a very helpful article! I’ve suffered kidney stones for 25 years (very prone due to “sponge kidney” condition, per my nephrologist). I have had good success with maintaining calcium levels (as you recommend) with supplements while limiting oxalates. I also take vitamin B-6, per my nephrologist. However, I’ve had a spike in stones in the past few months that I think may be tied to adding Citrucel to my diet — with methylcellulose as the active ingredient. I’ve looked extensively for information on oxalate content for Citrucel and Metamucil, with no luck. Do you have any leads on this? Thanks — it’s always a challenge to find fiber sources that don’t have high oxalate content!
Hi Tom, I doubt the agent increased urine oxalate, but it may have affected urine volume by increasing stool water losses. I would consider getting a new 24 hour urine while on the agent to see if there is really any oxalate effect. See what your physician thinks. Regards, Fred Coe
Thanks so much, Dr. Coe!
Such a Marvelous Article!!! Many of us Kidney Stone Sufferers aren’t aware of the massive amounts of Oxalates waiting to sabotage us! You have brilliantly listed these offenders, so now I can shut them out. But something that would be of major help in this article is a day to day diet recommendation. Yes, you briefly touch on the positive foods to eat, but we need more specifics.
A detailed one week clear cut list showing what to specifically eat for Breakfast, Lunch and Dinner Sunday thru Saturday. From there, I can do variations on this theme. —- LET’S MAKE IT HAPPEN, DR. COE AND JILL.
Hi Steven, We will try. Regards, Fred Coe
Hi Steve,
One of the reasons I have not given a sample diet is bc many patients don’t like the same foods. So what I might say to you is not what I would say to perhaps a vegan. It is much more complicated than that. I don’t know if you eat meat or have diet restrictions, other medical conditions (like diabetes) or what you like and don’t like. Make sense?
Here is some generic advice: Meats and dairy do NOT have oxalate so you are safe with them. As far as fruits, veggies, and grains, look what is on the list and eat the ones that have less oxalate. When you eat higher oxalate foods, combine them with calcium containing products to absorb the oxalate.
In order to really give good advice I need specifics on each individual and then we can create a daily diet that works for each person.
I am afraid this reply is not going to make you happy so perhaps you might like to email me personally and I can be of better service. Just really tough to make a generic meal plan when there are so many other factors that are involved.
Very Best,
Jill
Are there calcium supplements you can take with meals to offset the oxalate in your meal? Something like the chewable Viactiv or calcium capsules etc? What and how can you do this? Please help !!!
Hi Brent, Calcium supplements can be taken with larger meals and can prevent oxalate absorption. Before doing all this be sure you know exactly what stones you have formed, and what is the reason you form them. This is an orderly plan for you that will assure safety and that you are doing what is actually of benefit. Regards, Fred Coe
First time suffering with Kidney stones…Terrible feeling..went to e.r..ran tests and found 2 mm…stone…Holy crap. ..something so small…so much pain..i can’t imagine the other guys pain…with cm size stones. ..As I’m in pain now looking for remedies…is there anything you can suggest to help me pass stone faster or home remedy for pain…I’m on hydrocodone…and ibuprofen..flomax? But…looking for more faster methods of relief…took pills this morning and just vomited them up along with water..ugh…heeeeelp.
Hi Michael, the acute attack is managed with fluids and with the drugs you are taking, so your physicians are doing what they can. When it passes the pain will go away. If it does not your physicians can go in and get it, but usually that is not needed. If there is persistent vomiting let your physicians know so they can arrange for hydration. The real problem is to prevent more. Take a look at a good plan. Regards, Fred Coe
hi, terry here again. this process of deciphering the multitude of sites and information, often conflicting, is perplexing. i joined the yahoo group and accessed the extensive and formidable oxalate food list, as well having its own contradictions. on the “how to read spreadsheet” instruction page it says:
“5. Column E – Total oxalate in mg (insoluble and soluble) per 100 g. Insoluble oxalate- oxalate that can be bound by the calcium/magnesium. Soluble oxalate- gets absorbed in the body and isn’t available for binding.”
either this is poorly or incorrectly written or i am misinformed about what soluble vs insoluble means. i think correctly stated it would read:
insoluble oxalates found in food sources are already bound to another atom and cannot be absorbed into the body. soluable oxalates are those that are available to be absorbed into the body and are available to bind with calcium to form an insoluble oxalate that will be excreted rather than absorbed.
am i on track with this? thanks.
Hi Terry, Are you referring to the lists on my site? If so, where did you find the confusing comment? I will fix it. If it is on another site, I would not know off hand. The issue of available food oxalate is complex scientifically. Insoluble oxalate in food is irrelevant as you appear to say. That which can be absorbed will be unless the amount is limited or diet calcium is provided to complex with it and prevent absorption. Let me know where the confusing text – if it is on this site. I agree there are a multitude of sites, and of variable reliability. This one tries to adhere to contemporary science and bases its articles on references from PubMed – the peer review literature. In general, we work at the same standards for the site as we would in a scientific paper or review. Even so there are a lot of confusing areas and I would like to improve them. Regards, Fred Coe
hi and thanks for the reply. no, not on your site, but on the yahoo oxalte group site that has a 180 page pdf of food oxalate contents by per 100 g samples and also by serving sizes. the list is composed of results from the *autism oxalate project* and the *vulvar pain foundation*. also, serving sizes are helpful, as they put things into a real world perspective similar to glycemic index vs glycemic load does.
Hi Terry, Yes I am familiar with these lists. I am not an expert on diet oxalate, my expert colleague is Dr Ross Holmes and he is not completely satisfied with these lists. You do make a good point about serving sizes, however, which are not perhaps as good as we could do. Our lists arose from the Harvard group and we modified them to bring the data up to best modern standards such as one can. Creating serving sizes may be too much work right now as this site has no support, and is simply run by a few of us volunteers. Regards and thanks for the thoughtful comments, Fred Coe
I need a diet that I can eat that does not form stones. I love cheese, eggs, and some bread. I was raised on meat, potatoes and veggies. This was a balanced diet for me. It is hard for me to cut out potatoes. I love tomatoes, green onions, pasta, meat and green beans, and all Mexican food. I am not a sweet eater but I do like ice cream. I have passed 9 stones in the past 6 months. I’m 76 years old and I’ve never had stones until now. I drink nothing but water and I drink 15 glasses a day. I am seditary and I don’t do much to exercise. What can I do to help myself and stay away from stones?
Hi Pat, You may indeed need a diet but stone prevention is very uncertain and cumbersome if one just tries to somehow avoid all possible factors that might cause stones. Every person has some few specific causes for stones, sometimes not amenable to diet. Take a look at a way to obtain rational prevention, rather than trying to do all things with diet alone. Regards, Fred Coe
Hi Pat,
The diets will work but only if you need to be on them and if you do it right. Have you done a 24 hour urine collection to see if your oxalate is high? If not, you should. That is a lot of stones in a short time and you don’t want to continue down this path.
Take a look at Dr. Coe’s link he shared with you. See what still needs to be done and then we can talk diets. If your oxalate has been tested and you know that it is high, then unfortunately you will need to limit the potatoes for sure. Doesn’t mean you can never eat them but in moderation is fine. Eat them less days and less quantity each time.
Great job with the water. No matter what you do with diet, won’t matter much if your’e not drinking enough water. So keep that up.
Hope this helps-
Jill
Just wanted to say Thank you. I have found this article very helpful and encouraging. I have passed 10 stones since March this year and I am currently working on number 11. The stones that have been captured and tested were all calcium. However, my current Doctor has not been helpful in respect to diet changes. And I have asked. I do understand that you are not offering a cure, you are offering me a path to improve my situation that is manageable and it gives me some hope for relief. I am also looking into the benefits of Magnesium Citrate. And will be dicussing or with a new Docter soon.
Sorry.. Last comment should read I am looking into the benifits of Potassium Citrate.
Hi Shari, I also found this very informative and was told I need to follow a low oxalate diet to pervent any other kidneys stones, I have past stones which are very painful! What deit is helping you? I need some advice from someone that can relate to what I am going through, I really appreciate your input and want to know do’s and don’ts !
Hi Marilyn, Along the way, be sure and read the article I mentioned to Shari as it applies to every stone patient who has all of the trouble I sense you have had. Prevention is the key and is practical. Let me know, Regards, Fred Coe
Hi SHari, Calcium can mean calcium oxalate or calcium phosphate and there is a world of difference. For example, diet oxalate is not so relevant for the latter as it is for the former type of stone. Treatment requires one know the reason for stones and I do offer a path, a rather good one; take a look. I would not advise trying this or that remedy until you know for sure what the stones really are and why you form them. Regards, Fred Coe
Hi Jill and Fred, thanks for the info. I was just wondering when you say lentil soup, which lentils are you referring to- yellow, red or something else? There are so many “daals” in Indian food. Which ones should be avoided? Do you have number as to how much oxalate is in the lentils or other daals? Also, oxalate stone patients are advised to reduce intake of dairy and meat products. What should one eat?
– Sunita
Hi Sunita!
No one should be told to avoid dairy when instituting a low oxalate regimen. That is wrong information as dairy does not contain oxalate, and it is good to get the calcium as it will LESSEN calcium oxalate stone formation! So, please eat dairy, but watch the sodium content when you do.
As far as the lentils they are high in oxalate. It is doubtful that every type has been tested, but in general, they are high. If this is a staple to your diet, please reduce the frequency and the portion size when you do eat it. Please remember that you need to know how high your oxalate level is before you go banning foods from your diet. Also, if you eat some dairy when you have the higher oxalate foods it will help lessen the amount of oxalate your body absorbs. Calcium is important to maintain normal levels of 1000 mg/day. More days than not.
Hope this helps-LMK if it doesn’t.
Jill
Hello! I am being put on a low oxalate diet for kidney stones and me physician said that this is a reliable list to base my diet off of, but there are some interesting, confusing things on this list. 1) It says I am allowed cornbread but i am not allowed cornmeal. 2) I am not allowed to eat oranges but I can drink orange juice 3) It says on the list that kale is low in oxalates but my urologist said to avoid eating kale. I am just extremely confused by all of this. Also, the list does not mention anything about pumpkin and coconut. I have been substituting flour for coconut flour and pumpkin is an all time favorite of mine. Please, if you could help me on some of these clarifications that would be wonderful. Thank you!
Hi Raeshae,
Unfortunately many doc bunch up the green leafy veggies and say that they are all high in oxalate. Not true. Kale is ok to eat. The other foods you mentioned are confusing but not really if you look into it. Orange juice vs one orange makes sense bc the juice is diluted with water and the corn meal also is more concentrated with corn than the corn bread. Make sense?
Pumpkin and coconut tend to be lower in oxalate.
Thanks for writing!
Jill
Thank you for your quick response! I do not buy oranges from concentrate, we buy simply orange juice which is just orange juice, no water. When you say “tend to be lower” do you mean they are lower or that certain varieties of pumpkin are lower in oxalates than others? I ask because I have been substituting anything I would eat with regular flour for coconut flour and I want to make sure that the coconut flour is ok so when the holidays come I can enjoy homemade coconut flour crust pumpkin pie.
Hi Raeshae-
Here is a piece I found about pumpkin seeds (http://www.ncbi.nlm.nih.gov/pubmed/3799495). I have no reputable or reliable information on what type of pumpkin.
Everything I have read on coconut and coconut flour indicates that it is low in oxalate. However, I do not have a reliable source on this information.
When I do not have definitive answers I like to caution patients that they use the product in moderation. I do not want to say that coconut flour is for sure low, because that generally means that patients will use it and eat it constantly. So, within moderation should be fine.
I cannot say this enough. Unless your oxalate levels are in crazy land, you can eat your favorite foods that contain oxalate. Just watch the portion size, eat high oxalate foods less frequently, and when able, pair them with calcium rich foods (almonds and yoghurt for example). You want to stay under the 50 mg/day level. It is very doable if you follow this advice.
In regards to eating your favorite foods that are high in oxalate, some people like the “within moderation” way. Some say they “can’t have it in the house”. You are all different, so do what works for you. All require discipline, and that is what is hard.
In all of this diet stuff, please know that none of you will be perfect. It is when we aim for perfection that we fall off the wagon. Eat and drink well most days and on the days that you don’t, get up the next day and start all over again.
Hope this helps-
Jill
Hi Jill and Fred,
I’m a stage 2 breast cancer survivor (5 years this December). I had surgery for kidney stones last week (my urologist removed two, one was 2cm, the other was 1cm). I try to stay away from dairy and soy in general but I like almond milk. I also like freekeh (and I know I need to stay away from bulger). Do you have any suggestions for an alternative to almond milk? Can I still eat freekeh?
Thanks,
Jade
Hi Jade, Jill will answer about the milk but allow me to add that prevention of more stones is really important and there is no reason to believe that a low oxalate diet is what you need or enough for you. Take a look at a path to prevention. Regards, Fred Coe
Hi Jade,
Being a stage 4 cancer survivor, I know how good it feels to write that, huh!!! Congrats to you!
Almond milk will be high in oxalate, as you know. Coconut milk is a good alternative and so it coconut yoghurt. I just ate some myself. Staying away from dairy might increase your stone risk, so unless you are lactose or casein sensitive I might ask you to add some dairy into your diet. LMK.
AHHHH, the new super grain Freekeh. It is wheat so assume it has a lot of oxalate in it, no studies on it but one can assume safely it is high in oxalate.
Congrats again on your remission. Here is to continued good health-
Jill
Thank you both for your quick responses…
Hi Jill, I’ll mix in some dairy here and there, stoneyfield actually makes a great non gmo plain yogurt. I’ll try coconut milk and yogurt too. Have you ever heard of tiger nuts (not a nut at all if you have)? I thought of using tiger nuts and tiger nut milk as well.
Hi Fred,
I was sent a 24 hour urine test yesterday, and I have an appointment with my urologist to figure out what my next move should be. The low oxalate, low sodium diet was given to me when I left the hospital.
I know about Tiger Nuts. Not sure about oxalate content as it is considered a root vegetable. I would assume it is most likely high. Let us know what your oxalate level is once you do the 24 hour urine collection. Write us when you know more about your 24 hour values.
Jill
Will do, thanks!
Hi Jill, It does feel good to say “survivor” it’s changed my life for the better. One other thing I wanted to mention, I’m taking vitamin D3, CoQ10, Women’s one a day, and a powder probiotic.
I have had two bouts with kidney stones; the first about 8 years ago and the second a year ago. MRI’s taken during each occurrence revealed I had multiple stones but, thankfully, each time, the largest stone passed on its own. I have done extensive research on identifying foods high in oxalates, but there is so much conflicting information. To compound my dietary restrictions further, I have celiac disease, osteoporosis and am lactose intolerant. Any help you can offer will be very much appreciated.
Hi!
Have you done a 24 hour urine collection? Is your oxalate high? Your conditions contradict each other so that is why it is so difficult. Let us know if you have done a urine collection to see if you really need to restrict your oxalate. Worth checking for your stone disease and with your already complicated diet restrictions.
The oxalate list in this article is reliable and one that I and Dr. Coe would use for ourselves and our families. Check it out, but again, please don’t limit oxalate if you have not been tested. Even when you make oxalate stones, high oxalate may not be the reason.
Please email me personally at jharris1019@gmail.com when you get those values. I can help you if you like, but it might take more than just one reply.
Thanks for writing-
Jill
Thank you!
My dilemma is that I have very severe lactose intolerance, IBS-D, a gut that is hyper sensitive to acidic foods and I am a teacher who has long stretches of the day without the possibility of a bathroom break, so I limit water intake for much of my day. I’ve had extensive difficulty with calcium oxalate stones and my 24 hour urine showed high levels of oxalate so I’ve been told to follow a low oxalate diet. I am anemic and have always eaten a fair amount of spinich each week to help with that. My favorite things are now taboo – black tea, peanut butter, spinach, sweet potatoes, carrots, etc. My list of foods I can eat is very short. I’ve had five lithotripsy procedures in the last ten years and have passed many stones. I also have a familiy history of kidney stones on both sides of my family. Any suggestions?
Oh Sandy, I am sorry that you are going through this but very happy you have found us.
So, yes. Your favorite foods are very high in oxalate so you will have to avoid them, but not totally give up on them. I, too, am lactose intolerant which is so annoying, but nowadays there are so many alternatives. Of course many of those alternatives are made with almonds and since you must watch for oxalate you cannot have them. I use coconut milk and coconut yoghurt for my dairy alternatives. Give those a try.
You can have some green tea to sub for black tea and less oxalate. Substitute kale for spinach.
Drink enough water to pass at least 2.5 liters of urine a day. This is tough with your job, I understand. The only thing I can say to this is it is worse to have to take off from work bc you are making more stones or having more lithos. I do not mean to sound glib, I realize that it is very difficult or nearly impossible to leave your classroom. But, there is not much of an alternative I can give you there.
Limiting your water is probably your biggest factor, not the oxalate. Give that some thought. Changing your diet won’t matter much WITHOUT increasing your water intake. The driving force of stone formation is super saturation. This means that if you don’t drink enough water your urine will be super saturated with stone forming crystals- in your case- calcium oxalate. When you drink enough fluids your urine becomes less saturated with crystals and you will form LESS stones. So although very hard, you really will have to concentrate on getting your urine less concentrated with these crystals. If you change your diet but don’t drink enough water you will still make stones.
Stay healthy and write if you have more questions-
Jill
I just recently had a kidney stone blasted and am now trying to figure out what to eat. Every one of my favorite foods (spinach, chocolate, raspberries, whole wheat everything, lots of tofu, and lots of raw nuts, etc.) is very high in oxalate, probably what caused the stone. I am a vegetarian, so leaving out tofu will be hard, but I can switch to milk from soy milk, and increase dairy food. One big question I have – are endive and escarole low in oxalate?? Thank goodness kale and romaine are low. Also, what is a good carbohydrate to eat? Is popcorn and corn on the cob o.k.? The list you have shows corn flour o.k. but corn grits and corn meal very high. How is that? Thanks for your help.
Hi Barbara, Your big issue is to figure out if you even need a low oxalate diet and, if so, how much of an oxalate problem is there. Save your anguish about lost foods until you know you really need to sacrifice. For this you need your stone analysis and 24 hour urine studies. Take a look at this and see what you think. Also, remember that a high calcium diet will lower urine oxalate and is always a first step. Regards, Fred Coe
Hi Barb,
Sorry to hear about your stone troubles. It is always hard to figure out what to eat and what to sub for your fav foods. I highly recommend you doing a urine collection so you can be sure of what the cause is. Perhaps you can eat your favorite foods without cutting them out entirely. Maybe it is more a hydration problem then oxalate. Problem is you don’t know what it is until you complete a collection.
From what I have read, endive is lower in oxalate and escarole is higher. The only answer I might suggest is that there are different levels of concentration in the corn products above, it is a good question and I do not have a good answer.
Ask for the collection, you might not have to put yourself through this!
Thanks for writing,
Jill
I also have hypothyroidism. If you read about diet restrictions for this, they suggest not eating cruciferous vegetables as well such as broccoli, cauliflower and kale. I am having difficulty balancing all the diet restrictions with what I can actually eat to avoid kidney stones AND to help my metabolism work…add Fibromyalgia into this recipe and I am confused what to eat!
Hi Lisa, Perhaps Jill can help with the diet. But please be sure about what it is you need for stone prevention. Please take a look here and see if you have followed all the steps. Regards, Fred Coe
Hi Lisa,
No need to worry about limiting cruciferous vegetables. Take a look at this
study-
http://www.ncbi.nlm.nih.gov/pubmed/?term=cruciferous+vegetables+and+hypothyroidism
You can safely eat broccoli, kale, and cauliflower without risk of stones or hypothyroidism. What led you to believe that this would be a problem?
Hope this helps in your confusion-
Jill
Since 1978, I’ve had nearly a dozen bouts of calcium oxylate kidney stones. Some have been removed, some passed. I conscientiously restricted my diet to very low oxylate intake, but continued to have stones. In 2011, I had a parathyroidectomy; one bad gland was removed. The surgeon said the other 3 were good, and that I would now feel better, have no more stones, and could eat whatever I want, which I have. I live in a hot dry climate, but do drink a lot of water. Since January, my doc has me on 5,000 units VitD daily and Calcium 600mg because my Vit D level is below normal and bone scan shows beginning osteopenia. Three days ago, another attack. CT shows 5 stones, all in the right kidney, largest 4.7mm, blocking the kidney. My question is, why why why after the surgery am I again making stones??? What should I do??
Hi Lara, You need repeat 24hour urine testing. Not rarely urine calcium stays high after cure of hyperparathyroidism. Also, are these five stones new or leftovers from when you had that disease?? Be sure and analyse all of these stones that pass, and take a look to be sure calcium oxalate is all that is there. I suspect more phosphate than you report. Regards, Fred Coe
Hi Lara,
First get blood and 24-hour urine samples done to see why you are forming stones. Have you done this yet?
Secondly, even though you had a partial parathyroidectomy doesn’t mean that you don’t have to watch what you eat and drink.
You may still have high calcium levels in your urine and this could be why you are still forming stones. But we don’t know until you do testing, right?
Do that and come back here and tell us what is going on if you wish. We are here!
Jill
I’ve started forming stones that are a mix of oxalate and phosphate. The 24-hour urine test revealed that I have hypercalciuria but my oxalate level was not even detectable. I’m also on the lower side of normal for citrate. I can justify cutting out high oxalate foods as a precaution, but do I really need to go down the road of a super restricted low oxalate diet?
Hi Jim, If you have hypercalciuria and little urine oxalate why bother with oxalate in your diet. How about treating what is wrong. Idiopathic hypercalciuric requires a low sodium reduced sugar, high calcium diet and the latter will lower urine oxalate all by itself. Be sure to cover all the bases in your evaluation. Regards, Fred Coe
Thank you for your reply–especially over a long weekend!
I wish I lived closer, as I am finding it hard to get proper advice/care up here in Canada (I’m an American transplant). The only thing the ER urologist tentatively suggested to me was possibly increasing the acidity of my urine and suggested either citrate tablets or just adding lemon juice to my diet. However, the problem is that I also suffer from severe acid reflux and lemon juice and/or citrate would be too harsh on my stomach. I’m beginning to wonder if being on a low acid these past few years for reflux/ GERD has somehow contributed to the stone formation. I’m also wondering if the kidney stones are at all related to having had bone loss for the past several years (i.e. osteopenia and even osteoporosis in some places) possibly due to either HIV disease or the HIV medications I take (I have previously been on Tenofovir, which has been implicated in bone loss). Also I read that stress can cause kidney stones, but who doesn’t have stress in life, right?
At this point, I am upping my dietary calcium through food (I’m not sure about calcium supplements and stone formation) and I am also restricting my sodium intake and really trying to limit my sugar. I’m not someone who eats fast food or lots of processed items. I also don’t drink soda or sugary drinks (or even alcohol), but I do have to watch the other sweet stuff i.e. cakes, cookies. After thinking I would have to also eliminate oxalate in my diet, I am now relieved, as it seems everything has oxalate in it.
Any other advice would be appreciated, as I am not really able to follow up with anyone here. Socialized healthcare might be free in Canada, but it often means wait lists of over a year to see a specialist.
Hi Jim, Here is a set of steps for evaluation, and a good wraparound article. The bone disease may well be from many causes, but one I know about is hypercalciuria – which is benefited by low sodium reduced sugar high calcium diet. But your other problems may well play a role, so you really need those physicians there who provide comprehensive care – Canada is famous for the quality of its health care research. Diet oxalate may not matter depending on your urine findings and stone crystals. Regards, Fred Coe
Hi there, i hope you don’t mind me commenting on here, i live in Wales – part of the United Kingdom. I was searching for information on diets for high Oxalate/Urate stones and came across your page.
I’ve had 2 occasions where i have been admitted to hospital because of stones, the first when i was 19 or so, which passed naturally. The second was in 2013 when i was visiting Disney land Florida, when i returned to the UK i had 2 operations – the first involved a stent insertion and the second to remove a large stone – approx 5-6 mil.
I’ve had no advice from my docs regarding diet, only to drink lots of water.
How much would diet affect the forming of stones? As i said the only advice i have received is to drink fluids.
I feel as though i’m just waiting for another episode.
I’m taking allopurinol tablets daily to reduce the uric acid build up.
Any advice would be greatly appreciated.
Regards
Ian Thomas
Hi Ian, Everybody is welcome. I gather the stones contain both calcium oxalate and uric acid. This latter is due to an unduly acid urine and potassium citrate is usually prescribed. Perhaps your physician might want to consider this. Allopurinol will not treat uric acid stones, and as I am the person who first suggested it for calcium oxalate stones I am free to say it is a minor and rare treatment alternative. So potassium citrate would be important. Likewise 24 hour urine testing is critical as we have no compass – just a map. Regards, Fred Coe
I’ve been reading the oxalate content of foods from the Harvard link you provided at the beginning of this article. On line 179 it states pancakes (4, from mix) have 10 mg oxalate. However, on line 507, it shows 37 mg oxalate for the same item. Could you please clear this up for me? Thanks!
Hi Kim,
Thanks for picking this up. The only plausible answer is that it was different mixes and unfortunately they did not clarify. Suffice to say pancakes do have some oxalate in them, eat them here and there and when you do try to eat with milk or another calcium rich food.
Thanks again,
Jill
ok, thanks for your help!
Thanks for all the info – I have been struggling to find answers; perhaps you have some ideas….
My situation is perhaps unique (?)
I began having occasional (calcium oxalate) kidney stone episodes 20+ years ago, after first using Imitrix (a vasoconstrictor for migraines)
I elected to continue the medication because up until that time I had suffered with severe debilitating migraines for 20+ years, increasing in number to the point where I literally was never without the pain, nausea, photophobia, etc….this constant pain lasted for approx. 12 years!
I tried everything! (ergotamines, narcotics, anti-inflammatories, muscle relaxers, beta blockers, calc channel blockers, etc., massage, PT, bio feedback, yoga, etc., …multiple anything! that multiple doctors and therapists suggested, I tried it….. add to that my own research and trial of various methods and herbs, etc…..)
The imitrix (and later similar meds such as Maxaalt) works! !!
(I only have 2-4 migraines a month now, lasting several days each, the meds take the edge off, allowing me to have a “normal” life.)
I have been more than willing to put up with kidney stone pain and/or passing now and then, in order to keep the migraines in tow.
HOWEVER – in the past 3 years, kidney stone production has increased drastically!
A year ago I ended up in the ER with malignant hypertension, due to severe pain of 5 stones….4 of which thankfully passed on their own (with help from fluids and muscle relaxers)
(And then it got worse…….3 weeks ago I underwent surgery on my kidneys for removal of 35 stones!, some very large, spread throughout R and L)
Since the surgery, I am drinking TONS of water, increased my dairy intake; have cut back on salt, pepper, and have eliminated all the high-oxalate foods; ….and stopped my vegetarian diet
(about 3 years ago I adopted a vegetarian diet, simply because of compassion for animals being treated so badly)…….I have now discovered Kosher meats (very compassionate processing)…..I am aware now that the veg diet could very well be the “culprit” for the drastic increase in stone production…
Minus multiple stones, I was feeling better… until this weekend …..I had a severe migraine…..I took the meds….and within 24 hours, experienced that all too familiar kidney pain.
I am sitting on a heating pad as I write this letter – my head feels better, but my left flank is miserable!
I can’t even imagine going back to the life of excruciating migraines every day! (if you have ever had even one, you can understand)….
On the other hand, 35 kidney stones!! I am concerned about the pain yes….but primarily my concern is that my kidneys will be eventually scarred, and damaged to the point of compromising not just my comfort, but all the possibilities that kidney damage might entail, including shortening my life expectancy.
I head back to the doc in 2 weeks…..she says medication may be necessary.
I am assuming she probably is talking about orthophosphates or thiazides…and I am beginning my research on those.
I am desperately looking for alternatives, ideas, insight, wisdom….anything to help me make a decision about what to do next
Hi Connie, I am sorry to hear about so much trouble. I did not find in your writeup anything about the causes of your stones – just a conjecture about your recent diet change. Why don’t you consider this approach – it is organized and will lead to the causes of stones in most cases and thence to efficient treatment. This site has a lot about treatment for idiopathic calcium stones – no systemic disease as a cause of stones – and thiazide is at the end of the list. Phosphate is not a proven treatment and I would not use it. Let me know, Regards, Fred Coe
Could you be sensitive to histamine. Too many histamine rich foods cause intense migraines for me. Surprisingly, high oxylate foods are also high histamine foods
Hi Stacey, I do not know about histamine from high oxalate foods. But I have no reason to believe histamine plays a role in stone production. Regards, Fred Coe
It’s so confusing. Some reputable sources say the tahini in hummus is super high in oxalates and to avoid it, while others don’t even include it on their list. Some list graham crackers and popcorn as being low in oxalates, while others say they are high. How can someone which to believe or go by?
Lee,
Darn right it is confusing. We use the list from Harvard and don’t bother with anything else otherwise we, too, would be pulling out our hair. We trust their list and also realize that none of these lists are perfect. Plants studied under different growing conditions might vary. Use the Harvard list and if you find your favorite food really high from a reputable source elsewhere (not many of those btw), then eat it with a calcium containing food, or drink with milk, to counterbalance the oxalate.
Hope that helps-
Jill
Hi – I am a 50-year-old healthy female (5’7, 120 pounds) who experienced what I believe to be kidney stone pain on June 23. I had pain in my left flank that radiated to the front and down into my groin area. I got up for work and the pain was very intense so I drove myself to the ER. As soon as I walked in to ER and showed them where my pain was – the nurses and ER doc all said kidney stone. They did a catscan and found no hyronephrosis or ureteral dilatation. But did find a 7mm non-obstructing calculus in the midportion of the left kidney, (“probably in an upper pole infundibulum). No other renal, ureteral, or urinary bladder calculi identified. I had microscopic hematuria and was sent for an ultrasound of abdomen which found nothing. I was loaded up with IV fluids, Dilaudid (which after the first dose made me extremely nauseated) and Toradol. A Urologist examined me and said your pain is not coming from the stone. They kept me for observation and sent me home following day. From start of the intense pain to finish I’d say it lasted about 48 hours or so. It would come in waves and was like nothing I’ve ever felt before. I will also mention that many years ago a former doctor ran a catscan on me (I forget why) and saw a tiny stone, he said I’d likely pass it without ever knowing. That is my only history with a stone. My older brother had a uric acid stone 20 years ago, he is now 55.
I saw a Urologist after I was discharged from hospital (2 days later) and the blood in my urine continued. He also believed the 7mm stone was not the issue but discussed the small possibility that I had passed a tiny stone without it being picked up on catscan by the ER. He ordered an xray and the report said “a 7 mm calcification overlies the medial aspect of the left renal outline. A questionable tiny calcification overlies the lower portion of the left renal outline, no calcifications are noted overlying the right renal outline.” Based on the blood in the urine I had a Cystoscopy performed 2 weeks later – and nothing was found, though he did have to dilate my urethra (I was sedated) as he could not get the scope in. Next we did a 24-hour urine collection via Litholink with the following results:
Urine volume: 2.70
SS CAOx: 1.50
Urine Calcium: 109
Urine Oxalate: 17
Urine Citrate: 782
SS CaP: 0.58
24 Hour Urine pH: 6.751
SS Uric Acid: 0.08
Urine Uric Acid: 0.520
Interpretation: High urine ph. High urine pH can promote calcium phosphate stones. When coupled with low urine citrate consider distal renal tubular acidosis. When using alkali supplements (citrate or bicarbonate) manage urine volume and urine calcium to maintain SS CaP less than 2.0.
Stone Risk Factors/Cystine Screening – Negative
Dietary Factors:
Na24: 147
K 24: 53
Mg: 59
P 24: 0.555
Nh4 24: 20
CI 24: 141
Sul 24: 23
UUN 24: 7.04
PCR: 1.0
Normalized Values:
CR 24: 1210
Cr 24/kg: 21.9
Ca 24/kg: 2.0
Ca 24/ Cr 24:
90
I returned to my Urologist who was not concerned about the mention of distal renal tubular acidosis. He’s had me order a supplement called Theracran (cranberry supplement) to take twice day for a few months to try to acidify my urine. And I will take another 24-hour urine test end of October.
Lastly – I had an ultrasound done of my kidneys last week as I was asked to fly/travel for work and I’m concerned about the stone moving. The results are confusing though! It says “There is no hyronephrosis bilaterally. There is a small right extra renal pelvis measuring 1.5cm AP dimension. There is a small echogenic focus in the lower pole of the left kidney measuring 5 mm. Demonstrates variable shadowing. Impression: Suspected small calculus lower pole left kidney. Suggest CT or KUB imagining for conformation if not performed previously.
My questions are: Due to my low urine oxalate content, should I still be vigilent about low oxalate foods all the time? Is my urine oxalate level only indicative of what I ate in the past 24 hours or is more cumulative?? I’ve increased my water intake – which is obvious due to my test results. I never watched my salt previously but had no reason to and rarely salt my food – nonetheless I have cut back on salt. I am not a big red meat eater, eat small portions of animal protein. My doctor really hasn’t advised me on any main dietary factor to prevent stones – and doesn’t even recommend removing the stone.
But the latest ultrasound concerns me. I know they are not as accurate as catscan – but is it possible I now have a 5mm stone in my lower kidney and they did not pick up the 7 mm stone in the upper pole? Or is it possible the 7mm stone dropped and the size reading is off?
I’m so concerned about having a kidney stone attack. And I swear I always have this lingering dull ache in my lower flank and sometimes I get a sharp pain. Docs say it can’t be the non-obstructing stone. I’m seeking a 2nd opinion at the end of the month. I want to consider lithotripsy – but if the 7mm stone is now in the lower pole – I have read that can be more of a challenge to blast and then pass the fragments?
I am told it is unlikely I can pass stone of that size – so I just wait for it to cause me all this excruciating pain people talk about? That isn’t really something I think I can do. But the other concern for me is do I now have TWO stones? I really don’t want the radiation of another catscan. Can MRI pick up on the stone just as well? Do I get a KUB?
I’d appreciate any feedback you can provide.
Hi, I believe this replicates your other comment, so I will just leave it as is. Regards, Fred Coe
Thanks Dr. Coe – was there a response? If so, I can’t locate it.
Hi Beth, YOu posted the same question to two different article and I answered one and did not answer it again. The other article was Types of Kidney Stones a Primer. I answered you in detail there. Take a look and let me know. Regards, Fred Coe
I had many kidney stones over the years with more than 20 surgeries in about 30 years! Each time the urologist gave me a list of things I not suppose to eat containing oxalate. I still the list on my refrigerator. I look at it and try to be careful but my wife does have practically the opposite diet that contain a lot of oxalate. She’s a better cook than me hence my many kidney stones OK my fault!
I’m now 67 and would like to be able to not make kidney stones anymore.
By the way this is the best ever report I red on the subject I’m glad I found it.
I do have a couple questions. There is no way I can shop for the right food each time and cook this recommended low oxalate meals for me each time.
So I’m asking if someone know a business that can prepare low oxalate meals that can be purchase online?
Why only my left kidney is making those stone called calcium/oxalate and not the right one?
Thank you
Jacques
Grants Pass, Oregon
Hi Jacques, Here is the issue. Many stone formers have no oxalate problem. Oxalate lists are embedded in medical stone practice but not always relevant. Take a look at this plan for evaluation of your kind of disease. Also take a look at the treatment trials for what you appear to have – plain calcium oxalate stones not due to a systemic disease. One treats by causes – causes of stones in a given person. Possibly urine calcium is your problem, citrate, volume, if oxalate is high perhaps diet calcium is low or misplaced. Because of the medical narrowness – common to find – about oxalate, you are driving yourself to distraction about what might not be your major problem or a problem at all for you. See what you think. Regards, Fred Coe
Thank you Dr. Coe for your prompt answer and the following link: http://kidneystones.uchicago.edu/treatment-of-idiopathic-calcium-stones/ Well looks like I need to follow-up with more attention on my new recent urine test from the lab. Great informative website with more emphasis on learning about my own case and prevention. While all my urologists surgeon over the years have done an excellent work on extracting the stones with new technology each time. I still have issue to be able to follow up on the prevention. Now that I’m retired I’ll spend more time on your website and hopefully find a solution. Best regards, Jacques
One more question: Is there a kit to test for oxalate in the urine that you can do your my self each day or one a week?
So I’ll know immediately if what I eat is OK.
No, it is too difficult. Regards, Fred Coe
Dr. Coe, I am a 77 year old male, and recently had a urine tract infection. I was given Ciprofloxacin500mg twice a day and Harnal 0.4mg before sleeping, and did a PSA test which resulted in a reading of 2.9. The doctor said it should be less than 4, but a week later had me take another PSA test and the reading was 3.3. He said that the increase was not a good sign, so he changed the medication to AMOKSIKLAV 1000mg twice daily plus the same Harnal dosage. I am supposed to get a 3rd PSA in a couple of days. Here are my questions:
1. Are the oxalates that cause kidney stones different from the oxalates that might cause prostate cancer?
2. I have read that a PSA reading of 0.0-6.0 is normal for men of my age, so is the doctor making me take PSA tests unnecessarily or is he looking for a trend?
3. While he did not give me a diet list, he told me specifically to stay away from dairy products and chicken because they have high oxalates. Yet, the tables on this web site show chicken as low in oxalates. Yes, it is confusing.
Hi Howiem, I gather you are not a stone former and your questions are about effects of oxalate on the prostate. There is no link between oxalate and cancer of any kind. Dairy products do not contain oxalate and neither do the meat products. It is true that oxalate is produced via amino acid metabolism but that is inconsequential for intakes of meat in the normal range. Your present drug is a combination of amoxicillin and clavulanic acid and presumably aims at your urinary infection. With respect to the PSA testing, I am not an expert and leave that to your physicians. Regards, Fred Coe
Thank you, Dr. Coe, Appreciate it.