Diagnosis of MSK is Increasing
Urologists and nephrologists specializing in the treatment of kidney stones seem to encounter patients with medullary sponge kidney (MSK) far more often than one would predict given the fact that this disease affects less than 0.5-1% of the general population.
One potential explanation is the high frequency of stones in such patients, nearly 70%. Stones call attention to themselves. Even so, referrals for MSK seem to be occurring at ever increasing rates, out of proportion to the prevalence of the disease.
Another explanation is that we can see more because of dramatic improvements in CT scanners and endoscopic equipment we use for stone removal.
Latest generation, thin slice CT scans can isolate tiny stones as small as a millimeter in size. Meanwhile, modern flexible endoscopes not only visualize every crevice of the renal collecting system but are able to do so in high definition. Consequently we can identify previously unrecognized variations in the appearance of stone forming kidneys, of particular interest here nephrocalcinosis on CT and tubular plugging on endoscopy.
But diagnostic capabilities may be progressing faster than our ability to comprehend the significance of what we see. As a result, one can misclassify patients as having MSK when the correct diagnosis is another more common finding such as nephrocalcinosis or tubule plugging.
For example, a urological surgeon performing ureteroscopy with a modern high resolution digital instrument notices “hundreds of tiny stones,”, “abnormal papillary architecture” or “stones located under the urothelium” and proceeds to label the patient with MSK. Or, a patient with urologic symptoms such as renal colic, recurrent urinary tract infections, or microhematuria has a CT scan showing ‘nephrocalcinosis’ and is labeled as having MSK.
In both instances, the true likelihood of actually having MSK is, by a recent small study, only 4/15 (25%), but physicians are not generally aware of the differences between MSK, nephrocalcinosis, and tubule plugging because these are new areas of knowledge which have not been proliferated widely.
This article is one way we hope to make the diagnosis of MSK, a unique and complex disorder of renal development, clearer for physicians and their patients.
What Is MSK?
Our collective understanding regarding the development and pathophysiology of MSK is rather sparse even though G. Lenarduzzi first described it in 1939.
The Cause of MSK
The exact mechanisms that produce MSK are unknown. It is believed to be a result of abnormal renal development in utero. More specifically, scientists believe the ureteric bud – which will give rise to the ureters – interacts abnormally with the metanephric blastema tissue in the embryo which will produce much of the kidney substance.
There appears to be a genetic component to the disease. Recent evidence is that about half of patients diagnosed with MSK will have at least one relative with some degree of similar affliction. This kind of familial clustering can suggest an autosomal dominant gene expression or the actions of multiple genes giving that impression. The review of the above link is an excellent recent treatment of the matter of development and genetics which we highly recommend.
The Anatomy of MSK
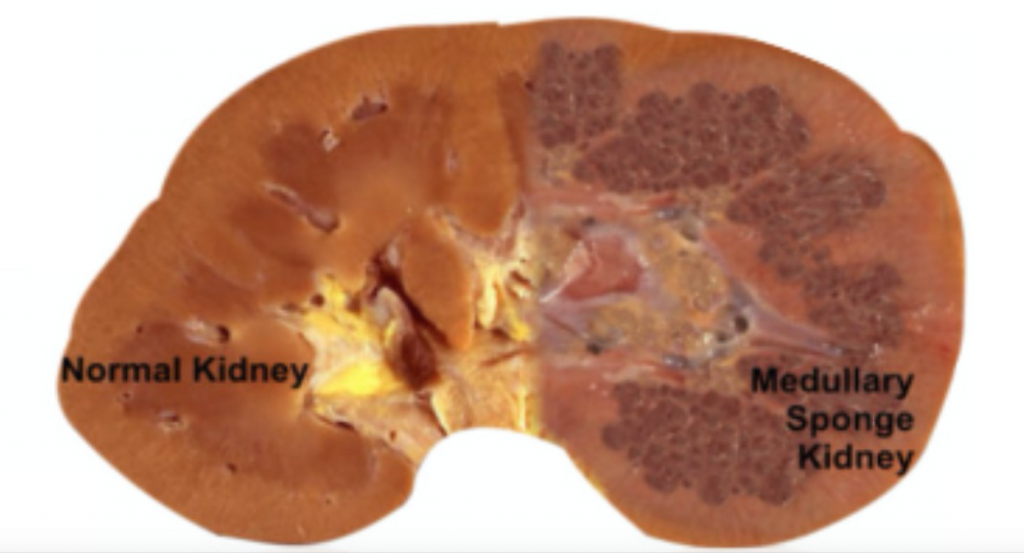
MSK, as its name implies, is characterized by sponge like, cavitary regions within one or both kidneys (Figure 1).
Figure 1 – A normal appearing kidney (left) compared to MSK kidney (right).
More specifically, the dilations occur in the inner medullary (precalyceal) collecting ducts. These collecting ducts are the terminal region of the nephrons, the individual functional units of the kidney.The inner medullary collecting ducts (IMCD) have the job of delivering urine to progressively larger ducts (ducts of Bellini) that deliver the final urine out of the renal papilla into the minor calyces (Figure 2) which connect into the renal pelvis and thence into the ureter to the bladder.
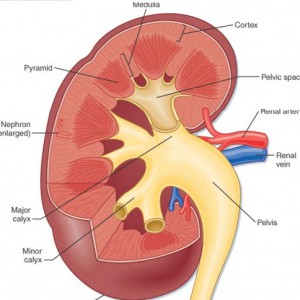
One way to think of the IMCD is as a collection of streams merging and forming a river (duct of Bellini) which leads to a delta (minor calyx) and then a lake (major calyx) and ultimately an ocean (renal pelvis) (Figure 2).
Figure 2 – Anatomic depiction of kidney and collecting system
The IMCDs are not visualized in Figure 2 but if you scan down to Figure 3 just below several human nephrons which were microdissected from an MSK kidney show what is really wrong with them.
In MSK, some IMCD are dilated markedly and have outpouchings (cysts): blind sacs which begin at the IMCD lumen but go nowhere – like a hallway someone walled off at one end. It is at the ends of these hallways one finds the stones, free floating and probably trouble. Other IMCD are not dilated and do not have cystic outpouchings.
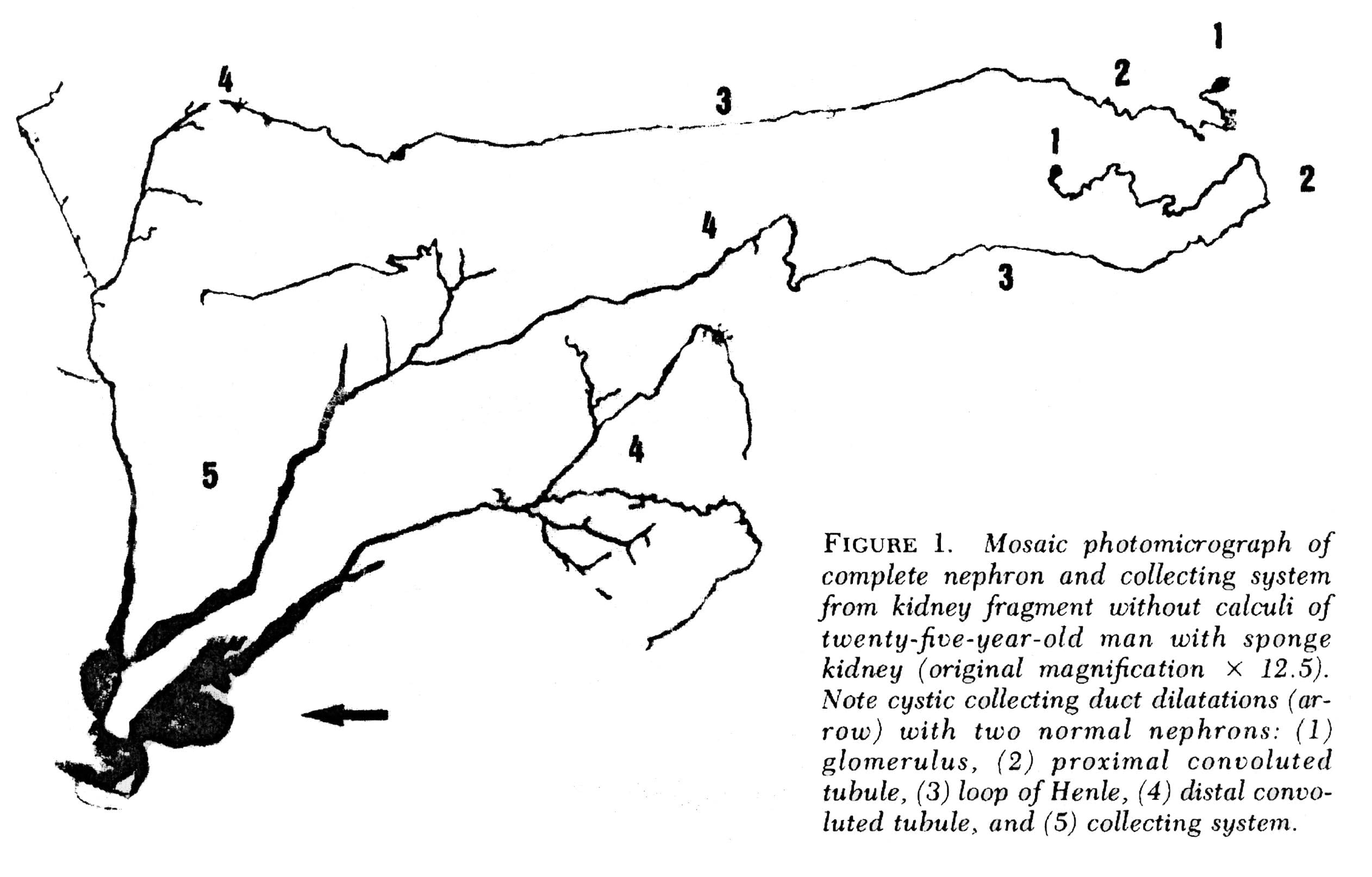 Figure 3 – Microdissection of complete nephrons from MSK. Irregular dilation of the IMCD is present. Cystic outpouchings are present, of varying sizes. The blind ends are obvious. It is in these cysts that tiny stones are found.
Figure 3 – Microdissection of complete nephrons from MSK. Irregular dilation of the IMCD is present. Cystic outpouchings are present, of varying sizes. The blind ends are obvious. It is in these cysts that tiny stones are found.
Quite apart from the IMCD dilatation and cysts, the kidneys of MSK have two other abnormalities which mark it as a specific disease. Those IMCD which are not dilated nor cystic have a multilayered epithelial lining, whereas a normal undilated IMCD lining is one cell layer thick. The interstitial cells of the renal papillum – the cells between the tubules and vessels – are more numerous than in normal kidneys, and have an immature appearance much like is seen in fetal kidneys.
Why Stones Form in MSK
Elsewhere on this site we have pointed out that supersaturation is a force, a source of energy directed at forming solid phases such as stone crystals. The kinetic retardants in urine, which include citrate, stave off crystallization but can never prevent it: A supersaturated solution will eventually collapse into two phases, crystals and a residual solution precisely at the solubility point, devoid of extra free energy.
The stagnant flow as a result of the dilated MSK IMCD, and particularly the static conditions in the fluid filled blind ended cysts, are the probable reason those innumerable tiny stones form which end up packing the ‘sponges’ with masses of crystals. How MSK patients produce larger stones, big enough to block the ureter is unknown. It is not true that MSK patients have remarkably high urine supersaturations or other physiologic abnormalities such as hypercalciuria and hypocitraturia. Possibly the tiny stones somehow leave their cysts and enter the urine where they act as nucleation centers.
Other Associations
Other common associations with MSK include urinary tract infection, microscopic and gross hematuria, and impaired renal function. Perhaps the stagnant flow in dilated IMCD and particularly in cysts, predisposes to infection. But since the papillae are abnormal in other ways it seems likely that these intrinsic abnormalities themselves must be clinically important, and more work needs to be done on the problem.
Making the Diagnosis of MSK
Of course, when we speak of what is wrong in the MSK kidneys, and how it affects people, we base everything on knowing that a given patient has MSK. If you have a kidney from such a patient and can show the dilated IMCD, the cysts, the tri-layered IMCD epithelium, and abnormal interstitial cells, diagnosis is certain. But what can we do when we are dealing with a patient?
Radiological Studies
Intravenous Urography
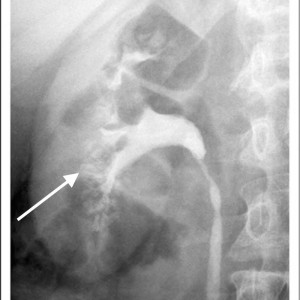
Historically, the diagnosis of MSK has been made on intravenous urography (IVU). Radiographic contrast is administered and x-rays of the kidneys, ureter, and bladder are taken periodically as the contrast is absorbed and later excreted by the kidneys through the urinary tract.
The delayed phase image is essential for diagnosis. This is when contrast material fills the masses of dilated IMCD and cysts which make up the sponge.
The masses of dilated IMCD filled with contrast material produce a characteristic ‘papillary blush’ which appears like flames on the outer edges of the papillae. When particularly large it can mimic a bouquet of flowers peripheral to the collecting system.
Figure 4 – IVU image of medullary sponge kidney. The arrow designates the papillary blush in the mass of dilated IMCD space.
CT Scans and Other Imaging
Over the past 10-15 years, noncontrast CT scans have replaced IVU as the imaging method of choice for stone formers. While these scans are more sensitive in detecting small stones, the lack of contrast limits the ability to accurately diagnose MSK and has raised concerns regarding the potential for under-diagnosis of this disease.
CT does have the capability of making this diagnosis when contrast is given and CT urography is performed; though this is not used as a first line choice for stone imaging and is generally reserved for specific indications such as hematuria and concern for urinary tract injuries.
Figure 5 – Demonstration of papillary blush (small arrows) on CT urography for patient with medullary sponge kidney.
Use of other imaging modalities have been investigated as well though they have proven suboptimal in their diagnostic capabilities. Ultrasound has poor sensitivity to detect dilation of the collecting ducts and MRI has the potential to delineate detailed renal anatomy but can not detect stones or calcification.
High Definition Endoscopy
State of the art high definition endoscopes have allowed investigators to make observations at the time of renal endoscopy correlating the appearance of the renal papillae and collecting system to specific types of diseases and metabolic derangements associated with stone formation. Because endoscopy is now being performed as a common and often preferred way to manage stones, this kind of detailed imaging of kidneys will be available more and more in the course of regular patient care and permit physicians to diagnose the exact kinds of disorders in the kidneys of stone formers.
Medullary sponge kidney in particular has an entirely unique appearance unlike any other type of stone related disease, making endoscopy a particularly exacting diagnostic procedure. Detailed anatomic descriptions from twelve such patients each with evidence of MSK on biopsy were recently described by Evan et al.
The Papillary Malformations Seen Via Endoscopy
In stone formers the papillae often appear abnormal, a concept that merits its own post and which we can only briefly summarize here.
Plaque
The renal 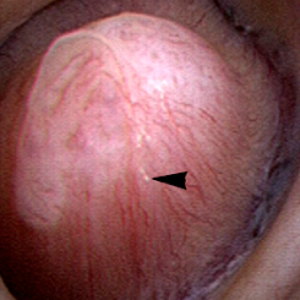 papilla is the anatomic subunit of the kidney where the IMCD merge together into the terminal Bellini ducts which empty into the minor calyx. Normally, it should have the appearance of a smooth walled mound or mountain without much if any calcification (plaque) along its surface. The link is to a detailed post about plaque by Dr Andrew Evan.
papilla is the anatomic subunit of the kidney where the IMCD merge together into the terminal Bellini ducts which empty into the minor calyx. Normally, it should have the appearance of a smooth walled mound or mountain without much if any calcification (plaque) along its surface. The link is to a detailed post about plaque by Dr Andrew Evan.
Figure 6 – Healthy appearing renal papilla with a minimal amount of Randall’s plaque (arrowhead).
Ductal Plugging
Another common abnormality identified in many papillae at the time of endoscopy are plugged ducts. The physiologic mechanisms for this process are currently unclear; 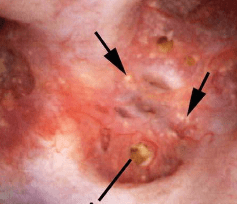 however, we believe it is a reflection of injury that begins a potentially disastrous chain of events for stone formers.
however, we believe it is a reflection of injury that begins a potentially disastrous chain of events for stone formers.
Figure 7 – Abnormal papilla in a patient with severe ductal plugging. Yellow mineral deposits (arrows) can be seen protruding from dilated ducts of Bellini.
Our present assumptions are that once crystals begin to form within a duct, they damage the lining cells and the duct loses its ability to make acidic urine. This in turn raises the local pH level and leads to the growth of more calcium phosphate mineral deposits which are favored by high pH.
Unclear is what begins this process. Since these ducts contain fluid which is very close in composition to the final urine, we suspect it is high supersaturation with respect to calcium phosphate. This occurs in those patients with both high urine calcium excretions (hypercalciuria) and higher urine pH levels – above 6.2. Such patients often form stones high in calcium phosphate composition and plugging is strongly associated with formation of such stones.
The mineral deposits subsequently grow and we believe can even act as a nidus for stone formation. The corresponding papillae can look markedly abnormal and the dilated ducts are easily evident. Remnant dilated ducts left behind after the mineral is spit out or surgically removed (Figure 8) show dilation without the mineral plug.
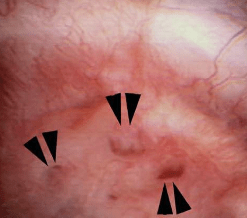 Figure 8 – Evidence of abnormally dilated ducts (arrowheads) at the surface of a papilla.
Figure 8 – Evidence of abnormally dilated ducts (arrowheads) at the surface of a papilla.
MSK
The findings in MSK are comparable in some ways to ductal plugging; however, rather than the papillae having one or several abnormally dilated ducts, the entirety of the papillum is markedly abnormal.
Therefore MSK and plugging type papillae look remarkably different.
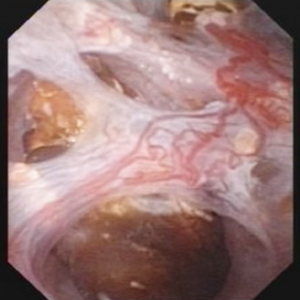
The MSK papillae are excessively round, enlarged, and billowy (Figure 9).
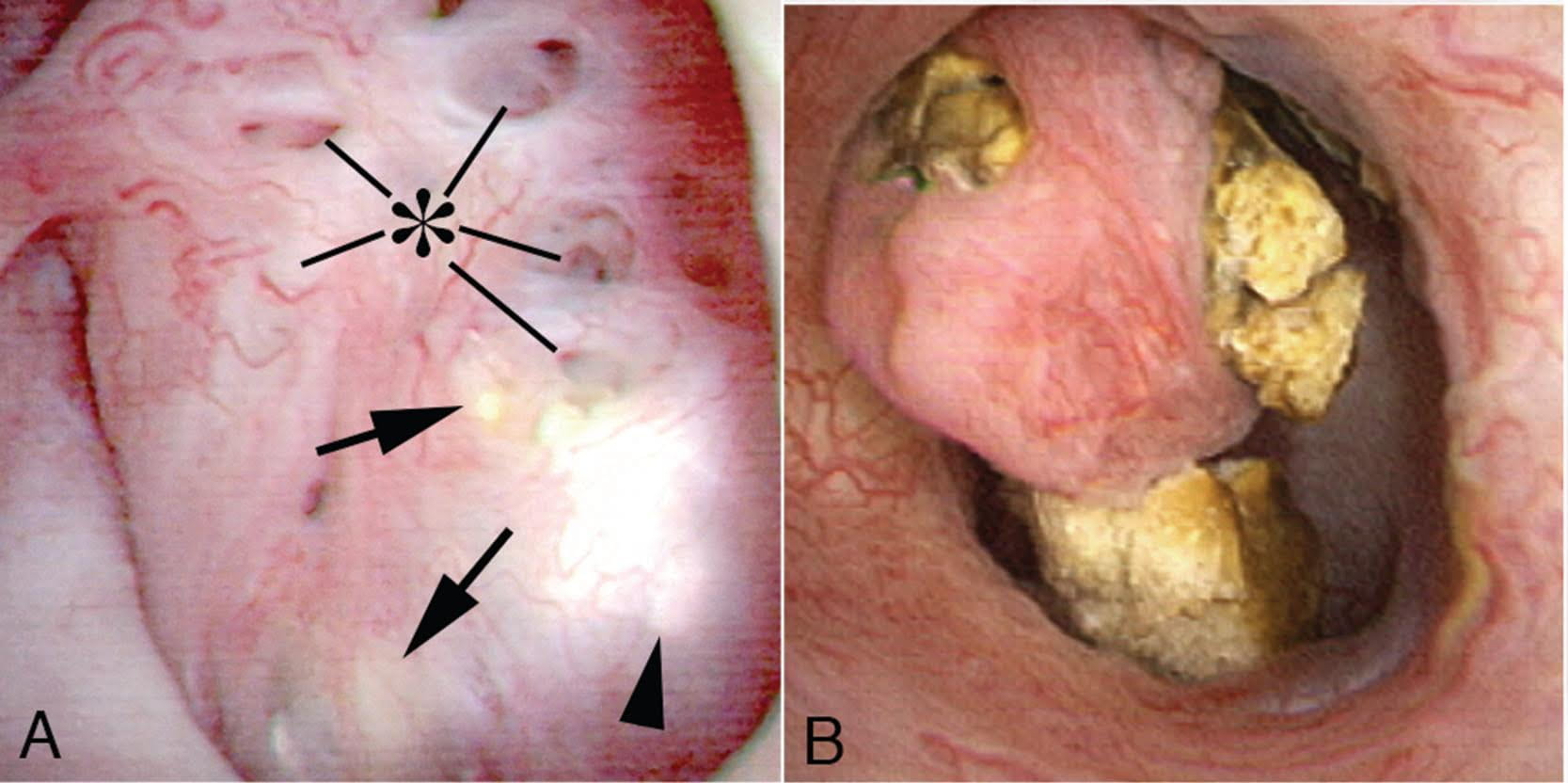 Figure 9 – A papillum in a patient with medullary sponge kidney. The papillae are rounded and enlarged with a billowy appearance. The papillary tips are blunted. No other kind of papillary disease is known to present this appearance which is therefore pathognomonic of MSK. Panel a shows dilated Bellini duct openings at asterisk; the arrows show yellow plaque – plugging of IMCD completely separate from the stones which fill dilated IMCD, the arrowheads show traces of white plaque. Panel b shows the billowy papillum with a blunted tip surrounded by calyceal stones.
Figure 9 – A papillum in a patient with medullary sponge kidney. The papillae are rounded and enlarged with a billowy appearance. The papillary tips are blunted. No other kind of papillary disease is known to present this appearance which is therefore pathognomonic of MSK. Panel a shows dilated Bellini duct openings at asterisk; the arrows show yellow plaque – plugging of IMCD completely separate from the stones which fill dilated IMCD, the arrowheads show traces of white plaque. Panel b shows the billowy papillum with a blunted tip surrounded by calyceal stones.
In the majority of such cases, these changes are seen diffusely throughout each kidney, though segmental sponge findings are present in a minority of patients.
The differences in appearance are well demonstrated in the post by Dr. Evan and the following video. With ductal plugging the bulk architecture of the papilla is intact though many ductal plugs are seen. Note the way the ductal plugs are adherent to the lumen.
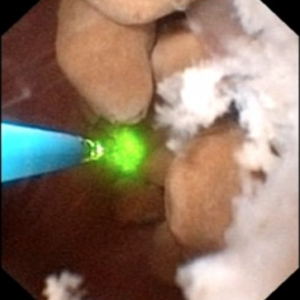
In MSK on the other hand, the papillary architecture has and unique, billowy appearance with massively dilated ducts and freely mobile stones within them. The following video is from a patient with MSK. A duct of Bellini is massively dilated and numerous tiny stones which are free floating pass out of it during the visualization as the opening is enlarged with a laser. You can see stones bouncing within the duct because of movement of the irrigation fluid.
Clearly neither papillum is “normal” and one can imagine the tendency to misdiagnose a plugging patient as a MSK patient unless the two patterns are clearly in one’s mind.
The ductal deposits themselves are an important clue. In all plugging diseases but cystinuria ductal mineral plugs are fixed within the ducts because the crystals adhere to the lining cells and often destroy them. As the lining cells are destroyed crystals fix themselves to the basement membranes, the collagen shell on which the lining cells once grew. Inflammation follows such injury with scarring and loss of the tubule segments. Deposits therefore never float free from a dilated duct except in cystinuria and in MSK. Cystinuria is usually diagnosed directly from stone analysis and urine cystine screening.
Perhaps because the tiny stones in MSK do not attach to the epithelium of IMCD there is no evidence of cell injury or inflammation, in marked contrast to all of the plugging diseases. Even in cystinuria injury occurs, not from the free floating distal cystine plugs but from calcium phosphate plugs which form in the IMCD.
Stones may cause pain in MSK despite the lack of ureteral obstruction and inflammation and cell injury. Possibly distention of the dilated ducts by masses of tiny stones could be a factor. Consequently, laser unroofing has been postulated as a potential treatment option in both disease states: those with plugging and MSK.
The video may not make it easy for everyone to visualize the stones and cavities of MSK. The 4 still pictures below show much the same thing for clarity.
Figure 10 (a-d) – Example of laser unroofing of sponge cavity full of freely floating stones. The massively dilated MSK bellini ducts are seen in Panel a; the white speckles at 9 o’clock are tiny stones in dilated IMCD or cysts. Panel b shows a holmium laser fiber being used to open dilated IMCD or cysts. Panel c shows masses of tiny stones free in dilated IMCD or cysts which float out as the surface is incised with the laser. In panel d, the remnant sponge cavity can be seen now free of stones.
Nephrocalcinosis and MSK
Strictly speaking, nephrocalcinosis refers to the presence of calcium deposits in the kidney tissue. Of course, this includes ductal plugging and the masses of tiny micro – stones inside cavities produced by numerous dilated IMCD in MSK. However, the word ‘nephrocalcinosis’ is also used as a radiological diagnosis which is far less specific.
Limitations of Radiology
When radiologists speak of nephrocalcinosis they can mean large numbers of calcifications within the collecting system or kidney tissue, because they cannot differentiate reliably between tissue calcifications and stones. When urologists speak of nephrocalcinosis seen during high resolution endoscopy they can specify if it refers to tissue calcifications, stones, or both, and will reserve the term for that component arising from tissue calcifications.
MSK is one of several disease states that is commonly associated with extensive nephrocalcinosis observed by radiologists. Other common conditions are stones caused by renal tubular acidosis and primary hyperparathyroidism. Calcium phosphate stone formers without any systemic disease can also produce sufficient combinations of ductal plugging and stones that nephrocalcinosis is diagnosed radiologically.
In a recent study of 67 idiopathic calcium stone forming patients undergoing percutaneous nephrolithotomy, rates of nephrocalcinosis ranged from 18-71% depending on the type of associated stone.
Figure 11- X-ray example of patient with MSK affecting the left kidney. Extensive nephrocalcinosis is seen.
Because radiographs cannot reliably distinguish tissue calcifications from stones adjacent to tissues, the very word ‘nephrocalcinosis’ needs to be re-defined.
In particular, the situation with respect to diagnosis of MSK has worsened as radiological techniques have changes. When IVU was the first line imaging modality for stones, contrast enhanced urographic phase imaging gave additional clues to MSK – the papillary blush illustrated in a prior section.
Nowadays since a single non-contrast CT series is all that is typically performed, the papillary blush effect cannot be seen, and diagnosis of MSK must rely more on the presence and pattern of nephrocalcinosis itself, which is not very specific to MSK. This means that the diagnosis of MSK by radiology has become unreliable.
The Power of Endoscopy
Differentiation of Nephrocalcinosis from Stones
During endoscopic procedures, stones and tissue calcifications can be directly identified and told apart. For example, in the images below, some of the calcifications were identified as stones. Others were tissue calcium deposits such as plugging or extensive plaque.
This has led to the notion that kidneys should only be labeled as having nephrocalcinosis once confirmed visually on endoscopy.

Figure 12 (A-C) – Evidence of increasing degrees of nephrocalcinosis confirmed visually at the time of percutaneous nephrolithotomy. In each image a nephrostomy tube (not calcification) is depicted by an arrow. The remainder of the images have increasing degrees of calcification (bright white) within the kidney. Ignoring the nephrostomy tube, one can clearly appreciate a minimal but very present degree of accessory brightness (calcification) in panel A, a moderate amount in panel B and a severe amount in panel C.
Diagnosis of MSK
Of course, all of the problems of nephrocalcinosis are compounded when it comes to MSK. Stones and tissue mineral are easily mistaken for one another in CT scans, and ‘MSK’ affixed as a label to patients who do not have it. Endoscopy will easily identify the remarkably abnormal papillary shapes and dilated sponges, so MSK patients are properly diagnosed.
Tips for diagnosing MSK
1) Confirmation with flexible renal endoscopy can make a definitive diagnosis in patients suspected to have MSK and can be diagnostic as well as potentially therapeutic in terms of stone removal.
2) Consider urographic phase imaging either with IVU or CTU to confirm MSK suspicion in cases where renal endoscopy is not clinically indicated.
3) MSK should not be confused with ductal plugging as these are distinct clinical entities.
4) Nephrocalcinosis is more common than previously appreciated and does not necessarily indicate systemic disease or the specific developmental disorder of MSK.
A Final Word on Treatment
MSK is a true disease and deserves more attention and research efforts to help clarify its etiology and optimize treatment strategies. Because diagnosis by CT scanning is unreliable, the condition is easily overdiagnosed, a problem which leads to many kinds of confusion, clinical and research.
Alternative diagnoses to MSK, such as severe ductal plugging, are not benign and require their own treatment in order to prevent progression. Very often patients with plugging have multiple and severe abnormalities of urine chemistry which can be treated with diet and medications. Proper classification of patients is therefore especially important as different disease states may require unique treatment strategies.
In the event that an accurate MSK diagnosis is made, the tendency to give up on treatment and surrender to the inherent challenges of the disease should be avoided. In fact, these are the patients where metabolic evaluations and attempts at stone prevention are most critical.
Moreover, just because many of these patients tend to have extensive nephrocalcinosis on imaging does not mean they can’t form symptomatic stones in the collecting system as well. In fact, for such patients the clinical history is especially important as visualizing new stones in the setting of extensive nephrocalcinosis can be quite challenging.
Oftentimes when there is a high index of suspicion based on clinical factors, the optimal approach is ureteroscopy as this can be both diagnostic and therapeutic.
That being said, realistic surgical goals should be established. Clearing all stones from such kidneys is rarely feasible, though unroofing those pockets closest to the collecting system or largest on CT imaging offers a good place to start.
MSK is a complex and poorly understood disease that can manifest uniquely from patient to patient. In that respect what works for one person may not be appropriate for another and treatment strategies should thus be organized on a patient to patient basis.







I want to thank for this article as I read this it was very informative.
Thank you, Dean, for the gracious remark. Regards, Fred Coe
Mike, this is really a great contribution. I have heard urologists say that they could diagnose MSK at endoscopy but I had not seen these sorts of terrific pictures of what the exactly looks like. Are there any studies correlating this endoscopic appearance with the radiographic manifestations of MSK seen with contrast administration? I think publishing a few cases showing that congruency would be worthwhile. Getting this discussion about nephrocalcinosis to the radiologists would also be useful as I agree that “MSK” is often cited as a likely diagnosis simply because some medullary calcium deposits are seen on CT without contrast. (I believe that Michael Grasso and I reported one of the first MSK cases diagnosed by CT-urogram: http://www.ncbi.nlm.nih.gov/pubmed/17591535). Fortunately I don’t think this potential over-diagnosis does any clinical harm but it’s not supportive of careful nosology. On the other hand, if a patient with radiographic nephrocalcinosis has a first degree relative with MSK, it’s possible that the imaged patient has some form of the disorder too, given Gambaro’s demonstration of the familial clustering: http://www.ncbi.nlm.nih.gov/pubmed/23223172; and my accompanying editorial: http://www.ncbi.nlm.nih.gov/pubmed/23364586 but the genetics remain unresolved.
Im so glad to hear you enjoyed the article. You raise some great points, I agree that a study correlating endoscopic and urographic phase contrast enhanced imaging would be a nice addition to the literature and further establish the link between endoscopic and radiographic diagnoses. One issue here is the general instinct in the medical community to suspect a stone and reflexively order a noncontrast CT. Sending some patients back for immediate urographic imaging would be somewhat controversial, especially in the event that they are ultimately going to proceed with ureteroscopy, a diagnostic procedure in its own right.
I also agree that at this point in time the potential for overdiagnosis is unlikely to cause a clinical harm; however, I think it raises a great point which is that we still don’t do a very good job as a field distinguishing stone formers from one another. Our most utilized clinical tools to do this (24 hour urine and stone analysis) are fraught with the potential for sampling bias and error. They do a sufficient job identifying some of the less common metabolic abnormalities and stone forming diseases; however, rarely distinguish common calcium stone formers from one another. Perhaps endoscopy might offer some clues in this regard? Image analysis is a routine part of GI endoscopy these days and in many cases the photos are saved and linked to the medical record. Maybe one of the reasons we don’t do this as commonly in urology is that we still don’t know what to do with that sort of information.
Im not sure if you have this sort of system in your clinic but would imagine you might have an interest. We would love to hear your opinion!
Sincerely,
Mike Borofsky
Thank you. I wi share this with my urologist as he has has experience with just a few patients and I can tell he is not up to date on MSK.
Dear Dr. Michael Borofsky M.D.
Thank-you, Thank-you, Thank-you. This is just what we in the Msk community have waited, and pushed for. I could never thank you enough.
Thank you for this article I was diagnosed with medullary sponge kidneys with nephrocalcinois in 2010 by IVP and then CT with contrast. I was so lost as to what all this means but there is a lovely group on facebook where we share our stories with one another. I am thankful to not pass stones daily or at all that I know of. However, the daily pain is what gets me. Doctors will say that unless there is an obstruction or a stone moving there is no pain, but I differ very strongly on this.
Thank you again for this article.
ashley_harradon@att.net
Thank you for bringing more notice to msk. This disease is a horrible one to live with and very hard as a patient to find doctors who understand.
Thank you for sharing this informing article on MSK. Many medical professionals I encounter ask, “What’s that?” when I share my diagnosis, so it’s encouraging to find someone so well informed sharing information with the public on this largely unheard of disease that can wreak havoc in the lives of those who have it. In addition to MSK, I have severe IC, which I think partially may have stemmed from all of the infections, stones, stone removals, even sepsis, creating constant inflammation. Do you know of anyone well versed in both diseases who can help me? I have to drink 1 gallon of water per day for stone prevention, but have a “micro bladder” that holds 1/2 teaspoon at this point, quite the conundrum! ANY suggestions on where to go for help would be appreciate. Again, THANK YOU for this helpful article!
Dear Meredith,
Thank you for your kind comments. One of the reasons we chose to go into detail regarding MSK is because it can be such a challenge to diagnose and we hope to help educate patient and providers alike. In regards to your MSK I would make sure you are working with someone on metabolic treatment and prevention of future stone events. MSK can be quite a challenge to treat and often the best solution is maximizing efforts to reduce stone activity through diet, fluids, and medications as needed. If you have not had a formal metabolic workup with blood tests and 24 hour urine testing I would recommend doing one. In regards to the IC, this too is an extremely challenging disease with controversial treatments and explanations for the primary symptoms. If you are having trouble finding someone specializing in both areas I recommend checking with a local academic center or major teaching hospital. The larger the hospital and affiliated university the more likely you will be to find someone with particular interests, research activity, and clinical experience in these areas.
Sincerely,
Mike Borofsky
My god I am going insane, I have been unable to drive,lost my job and in almost in constant pain with at times spasms that are like having a stone yet 3 urologists have told me there is nothing they can do and offer no pain medications but send me on my way. It has gotten so bad I carry my records now and the doc today didn’t even want to see them. I am so desperate is this what my life will be?
Dear Tina,
It sounds like you are going through quite a bit of suffering and I hope you are able to find some relief. As mentioned in our previous post, pain can be quite the challenge to to understand and treat. If you have a history of stones I would recommend at the minimum undergoing a metabolic evaluation with some bloodwork and a 24 hour urine analysis as well as a CT scan to see whether there are any stones or other abnormalities within the kidney. If there are stones in the kidney and you are having pain you might consider a diagnostic and potentially therapeutic attempt at stone removal. Clearly this is entirely dependent upon your history and the result of your tests. Also if you do pass any stones, make sure you have them analyzed to know what type of stone former you are. This can help your doctor tailer a prevention plan against future stone events.
Hope this helps,
Mike Borofsky
I am a 51 year old female who was diagnosed with MSK in my early 20’s after an IVP. I went through my entire adult life with constant urinary tract infections. I just got used to having them and managed them on my own. A month ago I ended up in the ER with Kidney stones. They found 2 masses on my liver (probably Hemangioma) and a mass in my kidney. I forgot to tell my doctor about my MSK diagnosis years ago. Is it possible that this is what they are seeing on the scan? I don’t really want to have any unnecessary tests.
Dear Eva, MSK is very difficult to diagnose, but does indeed foster urinary infections and kidney stones. Whether or not you have MSK the liver and kidney abnormalities need to be evaluated on their own. I gather the liver contains benign hemangiomas, and that should be that. The kidney mass needs to be resolved for what it is by appropriate imaging studies. Most incidental masses are benign yet even so some are not but are readily removed with prevention of later consequences. So the answer is: Have your physicians do as they need to, and be sure of what these two masses are, in the liver and kidney, even if the tests are expensive and time consuming. MSK is not a major issue one way or the other in this decision. Regards, Fred Coe
Hi Mike, I personally think that statistics in MSK patients needs to be updated considering that we have over 2000 members in the various MSK fb support groups who have all been diagnosed with MSK. You state that …
“”In both instances, the true likelihood of actually having MSK is, by a recent small study, only 4/15 (25%), but physicians are not generally aware of the differences between MSK, nephrocalcinosis, and tubule plugging because these are new areas of knowledge which have not been proliferated widely.””
And I understand this dilemma about “misdiagnosis” but the fact is that all our support group members HAVE been diagnosed with MSK based on scan results and reports that confirm MSK. We’ve seen many photos of scans in our group that all show the famous MSK dilated cystic tubules, bouquet of flowers and/or papillary blush marks. Many have participated in a recent research survey and were accepted based on their MSK diagnosis.
The genetic component you mention could be autoimmune and not necessarily the wellknown “abnormal renal developement” seeing as many of our members suffer from one of the various autoimmune disorders, not all have a family history of stones but members have other associated genetic diseases.
Most of our members also have nephrocalcinosis, many pass continuous recurrent stones, some do not pass stones at all, many have continuous recurrant UTI’s whether passing stones or not BUT all suffer from different degrees of daily chronic pain. Pain which most urologists/nephrologists cannot explain!
Not only do we need the medical community to know that this MSK causes chronic pain BUT how it affects patients’ mental health, daily lives and families, factors of which most doctors are oblivious! And that traditional treatments have not been helpful in slowing down this disease, if not for a handful of members who, thanks to treatment have less symptoms accept for chronic pain and fatigue.
Thanks Mike sorry for my ranting!
Hi Celia, Thanks for the very important note about how many of the people in the groups indeed have the specialized findings of MSK. I will leave it to Mike to make his own answers, but I suspect that the general problem of diagnosis may not apply to groups which have concentrated this one disease so completely as your’s have. Tomorrow morning we will have a new article up on nephrocalcinosis itself which is intended to clarify what it is at the kidney level and what problems are faced in evaluation. You will see MSK as a special form of nephrocalcinosis. About traditional treatment, the remark you make is very important. Perhaps it would be very valuable if the members might share which treatments they are getting. Maybe some members who have stopped making stones are being treated a bit differently. Warm Regards, Fred
And Fredric, another thing I forgot to mention is that we have new requests to join our group every day, from patients who were just recently diagnosed with MSK even though they’ve been suffering from stones and chronic pain for years.
Thanks, Celia, for all this information. I believe there are at least three MSK groups, or perhaps another MSK group and a stone group listed on your site. Is this more or less what you see on all of them? Given so many people so affected, there must be more we can do to help make things better. Fred
Yes there are several MSK support groups Fredric, I only belong to one other besides our group but am not active in that group. Each group will have to represent their own members and stories. You could request to join each group so that you can promote your fb page and website in the hopes that more and more MSK patients are aware of this great opportunity!
I am not sure how to do that Celia, perhaps Mike will do it for us. Best, Fred
Originally, in 1987 at the age of 20, I was sent to have an ultrasound, because I was having back or kidney pain, along with strong smelling urine and having to go a lot. I was told by the ultrasound Sonographer that my kidneys looked like “bouquets of flowers”.. But my doctor told me I had a “urine concentration defect” but nothing else. I finally learned I had MSK in 2000 when I got a lodged kidney stone. Since then I’ve had multiple CTs that all say “Nephrocalcinosis” .. But now that I’ve finally gotten a referral to a Nephrologist he denies that I have Nephrocalcinosis.. and had said he feels I could have Milki Alkali Syndrome.. lol So I give up.. every doctor and every CT/Utrasound and ultrasound says something different. My abnormal test results have been Hypovitaminosis D and abnormally high urine Calcium. I don’t pass stones very often but have quite a bit of flank pain. My Nephrologist has told me that it’s not possible for me to be having pain from my kidneys and that I should seek elsewhere for the cause. I have frequent urination with a strong smell at times. The urine sometimes has a slimy feel to it, with a film visible on top of it, with pieces of tissue floating in it. I have a lot of burning and urgency but have only ever had one UTI.
Hi Chrissy, From your comments you may have idiopathic hypercalciuria, a genetically determined, familial increase of urine calcium which is benign but can lead to numerous stones, depleted vitamin D stores, and bone mineral loss. The strong smelling urine could be ammonia, and this happens with certain kinds of bacteria. Do you know what kind of stones you have?? Some of your pain might be from crystals – tiny and cause bleeding and pain. Some may be from infection. Fred
This is a brilliant and very helpful reply. Thank you. I was not aware that idiopathic hypocalcuria could be the cause of my low Vit D and bone mineral issues. Thank you . That’s important information especially since I have already suffered a low impact compound fracture in my spine from a hug!
Dear Tasha, you need proper treatment for idiopathic hypercalciuria, if that is indeed what you do have. Your serum calcium would be normal, and your doctor would have to be sure there is no systemic disease causing the urine calcium to be high. If so, the treatment begins with as low a sodium intake as possible, at least 1000 mg of calcium daily to protect your bones, and if needed medication. I do not recognize the units of your urine calcium – it is usually mg/day and normals are less than 200 mg/day. Often family members will have had stones, or bone disease at an earlier age than one might have expected. Good luck, Fred Coe
Thank you for your reply! I have heard of Idiopathic Hypercalciuria. I will ask my Nephrologist about it at my appointment with him on the 29th.. see what he has to say. I have perfectly normal blood calcium levels.. and one thing that concerned me wayyy back 28 years ago.. was the very strong smell of ammonia! A doctor I saw once who filled in temporarily for my PCP put me on Vitamin D3 2,000 units per day, but when I got in to see the Nephrologist I’m seeing he immediately took me off of it and said he didn’t want me taking any additional Vitamin D, other than my daily multivitamin. My urine calcium level was 499 mg/day. I haven’t had any family members with early bone disease, except for some cousins with Ankylosing Spondylitis, who are positive for HLA-B27. My test for that was negative. My bone density test was good, except for some Osteoarthritis in my S1 joint. My kidney stones are not Oxalate.. they are potassium citrate or uric? It was a combination that surprised my nephrologist when he read it out loud.. he said, “Huh.. ?” lol
Thank you so much for sharing your time and your knowledge! 🙂
Hi Chrissy, you do indeed have idiopathic hypercalciuria and your stones are calcium phosphate – perhaps brushite. The level of urine calcium is very high. I will be putting up an article on hypercalciuria fairly soon as it is on the agenda for the site. The sodium article was a critical preliminary, because sodium intake controls urine calcium remarkably and low sodium diet is a major first step. This part is not published yet, but the main lines of sodium handling are – take a look. The ammonia smell may mean bacteria are present that possess the enzyme urease which splits urea into ammonia. Often this is harmless but such bacteria can actually make stones. The mineral they make is a triple salt of magnesium ammonium and phosphate called struvite. I doubt that is the name of your stones, but find out. Regards, Fred Coe
This is just fantastic. What an awesome opportunity for us to have the Kidney Doctors to bounce these questions off of. Is there any research on why some Mskers pass so many stones, verses one that makes a lot of stones but they don’t seem to pass. I am lithogenic but my stones (phosphate, apatite, & brushite) seem to get big 10mm then need to be surgically removed. I have always wondered why there are so many different forms/symptoms of MSK sufferers. Thank you in advance for your time and energy for this.
Hi Laura, apatite and especially brushite stones are nasty. The usual reason is high urine calcium losses and an alkaline urine pH. Do you know your urine calcium excretion? What are you taking for prevention? Best, Fred Coe
Dear Dr. Coe,
My pH is alkaline but my calcium output has varied over the years to high and not so high..I will find exact numbers today.
Laura, I am sure the urine calcium is indeed above safe limits and with the alkaline pH is fostering calcium phosphate stones. Take a look at some of the articles on supersaturation and on calcium phosphate that are on this site. Treatment is to lower the urine calcium with reduced salt intake and perhaps medications. Regards, Fred
Ok this article:) I posted it a while back. I was very impressed with it and I thought the author made some very good points. I have nephrocalcinosis, I do not pass many large stones at all. I pass mostly Sandy gravelly bits with a larger stone once or twice a year. Oddly my pain is not much worse passing a larger stone than it is regularly. I generally have bad aching kidneys and flank area. I also pass a lot of large chunks of tissue. Often I have pain in my kidneys before I pass the tissue. Other than being told to watch my salt I have not been told any other management techniques. Although my neph did Hydrochlorothiazide it was a fail as it caused gout. My Vit D is low and does not respond well to supplements but does cause debilitating kidney pain and loss of bladder control. So my nephrologist has said no to Vit d supplementation which is tough because the low Vit d cause intermittent secondary hyperparathyroidism. I pee out way to much calcium. Normal is 2.2-6.4 my last test result was 22.1. That four times more than I should be. My serum calcium is high normal. Absolutely no calcium supplement allowed or my serum calcium levels shoots to high. I do not know what kind if stones I make but my 24 tests have detected both oxalates and urate crystals. And I don’t have a clue what bicarbonate is but it is always high also. And my urine is also dark it cloudy even though my volume is excellent. I agree with Dr.Coe from Kidneystone Docs that we create lots of small stones. When ever I collect for 24 hour testing I see lots of gravel and also lots of tiny salt like crystals that I would never have noticed had I not got some of the urine on my hand. Oddly I also seems to have a lot of what looks like silt. Very strange.
Dear Dr. Coe,
I got my reports in order, you had asked me about my urine calcium levels well they used to be high and now they are low. So all of these are in compiled format so I can go back until 2008. All values are mmo/L. So calcium has being as high as 8.1 in 2010 and 2011 also those two years my sodium was 210, and 108 mmo/L. By 2013 my sodium was 42 mmo/L. My calcium that same year was 1.4. The last report I got from my nephrologist Dr. B McCormick in Ottawa, Canada. He also had my stones analyzed and I have done multiple 24’s.. So fast forward to this past winter he says Laboratory investigations from December show creatinine of 72, potassium 3.4, irate 236, calcium and phosphorus are within normal range. In regard to what preventative measures my doctor took is I take indapamide .0.625 mg daily, and a potassium saver Amiloride 20mg which seems to have resolved the low potassium. With high PH 7.0. Thank you for taking the time to consider this. I feel as though I may have changed stone from ox to phosphate, could that be possible? My urine calcium no longer high. Not sure what to make of these values. By the looks of things on paper I don’t seem to have any red flags..but yet am extremely lithogenic and this year formed four stones in 20 days on my stent. It’s all so puzzling. I also don’t pass to many stones but instead they get stuck and surgically need to be removed. Thank you..when you asked about my uri e calcium I thought I should give you a clear picture.
Perhaps the high pH is what may have fostered conversion from CaOx to calcium phosphate stones. Indapamide and reduced sodium intake is excellent treatment so your nephrologist is much to my taste. High urine volumes are very important, and I imagine he/she has recommended at least 3 liters daily given your active stone formation. Stents are a special problem; they may gather many crystals even when stone prevention is going well, and they are short term. You have a good physician, to my lights, just keep steady and expect things to smooth out. Warm Regards, Fred Coe
Thank you for this advice Dr. Coe!
Is there any correlation between MSK and phaeochromocytoma?
Thanks
I know of none. Regards, Fred Coe
I was just diagnosed with MSK. Is it better to see a urologist or a reno dr? I’ve been having constant Uti with absolutely no symptoms. They diagnose infection from urine cultures and every time it’s ecoli bacteria. So far I’ve been on 8 rounds of antibiotics. Dr believes it’s a stone infection and that I should have a urethroscopy with possible stent . I have absolutely no pain or symptoms except that I’m being told I have a urine infection. Any help or suggestions would be appreciated!
Hi Ramona, I presume your CT scan shows multiple small calcifications and that the name MSK has been suggested. This may or may not be true, as it is nearly impossible t diagnose MSK by CT scans. That you have e coli means that possibly the stones are themselves infected but that the organism itself cannot be helping to make the stones bigger. Ureteroscopy is helpful in that your urologist can tell which of the calcifications are indeed stones and which are calcifications in the kidney tissues themselves. The former can be removed, the latter cannot be removed. But in a larger sense, I am a bit uncertain about a procedure. You are without symptoms, the organism you have is not capable of producing stones, and your stones are without symptoms. What you have is colonization with an organism, possibly from the stones, possibly from elsewhere. I would discuss with my doctors what they would hope to accomplish from the procedure and how it will help you. Since you have no symptoms, and surely will have some after the procedure, how will you benefit? This is something they will certainly be able to address, and in doing so, help you to decide what to do. Regards, Fred Coe
I have medullary sponge kidney. I was diagnosed with osteoporosis at age 42. Now it is very easy for me to break bones and I’m having dental issues. I was told it was because of my kidney disease, but I can’t find any literature to back this up. Is this true or false?
Dear Nanette, I suspect you have idiopathic hypercalciuria and perhaps were following a low calcium diet. This genetic trait can cause a vicious fracturing bone disease in some people. Be sure your physicians have looked into this and are taking steps to protect your bones. There is a lot they can do and should do for you. Possibly there is another problem, and if so they need to discover what it is. Medullary calcifications are usually not medullary sponge kidney, and in any event do not lead to fracturing bone disease. Regards, Fred Coe
Hi Dr. Coe,
Sorry for story..tie together for question at end. DX’d MSK @ 36 after 8 years of stones. Frequency slowed from 1-2/year to 1 every other year (I throw up on only this pain). Rarely drink more than water since 25 (to help stones-told to add lemon years ago & to help new chronic uti’s last year, added not from concentrate cranberry juice).
At 46, after 6 years of many internal pains & issues, a test resulted in my “5 organ 2 surgeon surgery” (UroGyno & colorectal). No previous surgerical history, but 5 days after, I bled excessively bleed into legs. DXd w/ Hemo. C/Factor XI deficiency. Shortly after, DX’d w/ Ehlers-Danlos Syndrome type III. At EDNF conference, told MSK can be one of the issues for EDSers (collagen).
At 50 (now 53), stone blockage. on-call Uro used a stent procedure to unblock, but post procedural heavy bleeding & wouldn’t stop, so on-call Hemo. ordered plasma transfusion to stop bleeding (did).
I now take a temporary clotting med. prior & after EDS related procedures & minor surgeries, plus my 1st bleeding uti (told med. no guarantee tho).
Chronic Vitamin D def. past 5 years & given 50k D2 past 2 years. Began chronic uti’s last year (so, began organic non-concentrate Cranberry this year; seems to help).
After 2014 stone, radiologist said 0 stones & ER Dr. said no uti when asked. Online record said 2 small stones & a uti. So, it’s all tied together.
I have no Uro or Neph, but b/c of Hemo. C, etc, I want to understand how to best address my MSK & related key issues or concerns. I don’t know tho, if Uro or Neph is best & if finding one that really gets more than basics of MSK is necessary (haven’t found one yet) & the key “whys”. Thank you so much for having your site & taking time to answer questions. Sincerely, Kris
Hi Kris, You have a major medical issue, and are right to be concerned. Massive efforts at medical stone prevention are justified in your case as every stone is worrisome with respect to bleeding. Without a doubt someone as complex as you should receive her care at a university medical center that has the proper array of surgical and medical people. If that is already the case, I am sure that proper surgical and stone prevention care can be obtained. If not, you should transfer your care to such a center. It is unfair to you and – frankly – to physicians to expect that this kind of very complex multi – specialty problem can be handled outside of a center. Regards, Fred Coe
I have had MSK and nephrocalcinosis since birth but symptoms started showing when I was 15 and I am now 34. I have had in excess of 20 operations in my life due to renal colic and routine op’s to blast the stones.
I also have dangerously low Vit D that doesn’t respond to treatment.
I have to care for my family, house, pets and work all while suffering from this horrendous disease. I have no idea how I get through the days. I cry most days about it. It makes me very depressed and anxious.
Luckily I have a very supportive family, urologist that I have seen for 19 years and a world renowned nephrologist otherwise I don’t know what would happen to me 🙁
Hopefully a cure is found one day. I am in Australia.
Dear Jade, I am so glad that you have really fine physicians to help you. The very low vitamin D level that does not respond to vitamin D sounds odd. I wonder what your physicians think is wrong. I would have guessed that you are not absorbing the vitamin D that you are taking as a supplement. All the best to you, Fred Coe
Thanks Fred, it l’s great to see some people are really interested in this barely researched disease.
I will check back regularly to see if you have any updates 🙂
I am the same I have MSK symptoms started at 15 I am now 40 and it gets worse as u get older could I ask u who your urologist and nephrologist are as I am struggling to find a good one. I did have a good one but he retired 🙁
SAW 35 YEAR OLD WITH BECKWITH -WIEDEMANN SYNDROME PASSING 40+ STONES PER WEEK QUITE DISABLED HAVE THESE PATIENTS EVER HAD BILATERAL NEPHRECTOMIES AND RENAL TRANSPLANT?
Hi Dr Napier, I do not know. However, Dr John Lieske at Mayo Clinic runs their rare disease program and probably has contacts with people who have some personal knowledge about treatment options for this condition. I would contact him directly. Warm regards, Fred Coe
THANK YOU FOR YOUR HELP
I am searching for help with a good pain treatment protocol. My son (age 29 now), was diagnosed with MSK 5 years ago. He generally passes a stone or fragments once a month. They also seem to break loose in pairs, sometimes passing 2 within a couple of days of each other. He has yet to find a doctor who will set up a reasonable management plan. Every doctor takes the same approach as they would with a first time stone passer: urine test and radiology (cat scan). If a stone doesn’t show up, they won’t prescribe any medication for pain. He seldom passes blood and has left the doctors’ offices many times and passed a stone two days later. He has some doctors state that stones won’t always show up on scans or radiology, others treat it like it is a litmus test. As a result, he spends hours waiting for scans, for results, sitting in the doctors’ offices, waiting at the pharmacy – all the while being exposed to copious amounts of radiation and receiving sporadic pain relief. Isn’t there someone who understands that MSK patients like my son would desperately love to lead a productive and meaningful life if they could receive the management that they need. without fear of cancer or other complications from too many scans? He has been to two urologists at university hospitals as well as two in private practice. Their protocols are all the same- go to ER or radiology, get scan. wait, if it looks like a stone is passing and blocking, then we can prescribe. This, in spite of CT scans showing multiple stones in both kidneys. Any hope or suggestions from the practitioners in this field?
Hi PC, The article you are commenting on reviews this problem of pain from non obstructing stones. There are some urological surgeons who are attempting to treat this condition, but so far I cannot site any peer reviewed publications concerning their results. One critical issue for people with many stones is an organized program of prevention, and my observations have been that such prevention can reduce pain considerably. I know that parts of real prevention are often pursued by patients like your son, but very often the real approach – sustained reduction of supersaturation for the crystals in stones being formed – that kind of precise prevention, is not really in effect. So, I would urge prevention be tried in a very serious way in hopes that pain can be reduced. Fred Coe
Thank you for your prompt and thoughtful reply. It is true that prevention is crucial and also may be the hardest to adhere to, particularly in the diet. Long term, it is a common sense approach. In the meantime, MSK patients are forced to deal with the pain of passing stones with very little relief (as well as the continual pain within the kidney itself). Along with this pain, an ECSWL procedure caused nerve damage in my son’s abdomen- another possible complication of treating MSK The tighter restrictions of pain medications in our country has created a climate of worry, which impacts the quality of life for many MSKI sufferers. Most MSK patients speak of being made to feel like they are drug abusers at ERs, by medical professionals and pharmacies because they are asking for relief from debilitating pain from stones. I don’t normally post to articles, but appreciated your research and work in this area. I am hoping to one day see a safe pain treatment protocol accepted and taught within the American Urological Association that avoids excessive exposure to scans and recognizes the loss of productivity and quality of life created by the current popular approach of every stone being passed requiring a scan, urine test, hours of waiting and yet generally with the same prescribed outcome- flomax and nsids (which create their own health dilemmas). Again thanks for your time.
Hi PC, I find on Facebook literally thousands of people who say exactly what you say. As I understand it, when stones are actually passing ER staffs are reasonably prompt about pain management, as one would expect. Flowmax and NSAIDS are traditional and have some pretty good trial data showing pain relief as compared to narcotics. When there is pain and no stones passing, it is another matter altogether, and things are often as you describe them. I am impressed by the size of the problem, and personally have encountered many patients with pain, large kidney stone burdens, and no apparent reason why the stones should be causing pain – they are not obstructing. My comments about prevention being paramount were not intended as fey or utopian, because some pain is due to crystal passage which is not visible on scans and crystal attacks can be prevented reasonably well. The chronic pain, non obstructing stone problem needs more research. We said it in our article and I will say it here. The problem is what to do practically to bring about enough new data to then bring about change. Right now I confess to having no clear ideas. Regards, Fred Coe
Dr. Coe- Again, thank you for your reply. I am very appreciative of your work in this area, it is one that is sorely needed. The anecdotal evidence of pain from non-obstructing stones is there- especially, as you said, on the internet where MSK sufferers have a forum to compare notes. This makes the research you are doing for the medical profession, so valuable. I do not think your prevention is at all utopian- it is critical given the limited options for MSK treatment. As to the ER, if an association-wide protocol could be developed for MSK patients that was no longer based on a ‘single stone event’ approach, it could improve their quality of life enormously. MSK is not even close to being in the same category as a one time stone event, and yet pain treatment is still approached as if it were. Even when an ER may give a good response (relative to demographics in our experience), it is still hours lost in ER, exposure to scans and great expense. Many MSK patients are seemingly constantly passing gravel/crystals as well as stones. The practical reality of spending your life in the ER, doctor’s office or radiology center, as well as the expense- all with the same outcome- NSAIDS (or nothing if crystals or gravel don’t show up on scans) makes for a terrible quality of life. It seems that for many MSK patients, NSAIDS do not provide adequate pain management, are not great for kidneys and (as with my son), heavy use can cause stomach and intestinal erosion (which is exacerbated by stress and chronic pain). As I am sure you know, chronic pain can set up a nerve signal pathway that can be relentless after time. As many MSK sufferers express, since doctors know that there are multiple stones in the kidneys and that this is producing frequent or constant pain, why continue to treat each incident as if it were a single event? There are many more compelling reasons for why the AUA needs to come up with a comprehensive approach that makes sense for multiple stone pain management that takes into consideration time lost, exposure to dozens of scans each year, at times being viewed suspiciously by medical personnel and the unrelenting cycle of pain. That is why I am so grateful to you and others who are studying and contributing to the knowledge of this disease. Thanks again for listening and for your article!- PC
Dear PC, Your thoughts are echoed throughout the MSF groups though not, perhaps, in so eloquent a form as what you write. It is easy to dismiss one person as a drug seeker or neurotic but really when so many people all have the same complaints the problem is real and does need a response. Prevention is the ultimate response but the small stone pain issue is urgent. I am not a urologist, so I cannot speak about surgical approaches, nor am I a qualified pain management specialist, but perhaps people in those specialities need to try something more. Regards, Fred Coe
PC, you are spot on. Its like you are talking about me.. I too have MSK and suffer daily… Quality of life is pain then death… No relief. Very sad disease that needs hope! I’m sorry that your son goes through this, I pray none of mine inherit it. God Bless you.
I too suffer from MSK. No quality of life, pain daily, I have a special needs child who needs me so I take no pain meds. I’d this it for the rest of my life?? Pain then Death… Does kidney transplant cure this?
Hi Susan, You are indeed part of a vast group of people with pain from non obstructing stones. As I have said to all, proper surgery is in evolution and perhaps one might want to wait a bit before undertaking any surgical approach. Kidney auto transplant – moving the kidney downward toward the bladder – would be relevant if there were passage of many stones or of crystals; but in either event the better approach is to insist on prevention treatment to lower supersaturation and stone or crystal formation. I know I can sound repetitive as I say this all the time but I say it because it is so important a step in reducing pain from crystals. Regards, Fred Coe
I am 29 and was diagnosed with MSK 6 years ago. I have had at least 10 lithotripsy procedures. The last two I woke up in a lot of pain. The previous ones never hurt when waking up. My question is how safe is repeated lithos? Does it cause significant scaring? or effect kidney function in the long run?
Dear Kelly, shock wave treatments are probably less effective with numerous small calcifications- the usual reason for diagnosis of MSK – some of which are stones and some tissue calcium deposits. I would prefer ureteroscopy which is safer and more effective in removing stones. MSK or not proper prevention will reduce new stones and calcium deposits and is urgent in cases like yours. Try to get it accomplished. Regards, Fred Coe
Thank you for this thorough article on MSK. I was diagnosed more than 25 years ago, but this one article has educated me more than all of my consults put together! Thank you for you honesty in stating when you don’t have answers. You are right, this disease needs much more research. I know that many MSK patients would be willing to participate in any studies that might help future patients. I’ve posted the link to this article on an MSK Facebook group, encouraging the members to browse the rest of this site as well.
Dear Suzanne, I am glad you found the article worthwhile. MSK is a developmental disorder of the last portions of the nephron and indeed under studied. All I can think to do for patients with it is to reduce the risk of stone formation. Because stones form inside the dilated tubules one needs very low supersaturations even if the urine chemistry itself is not very abnormal. This latter is a point the article does not emphasize enough but I mean to edit it soon in that direction. Regards, Fred Coe
I am 33 and recently had a ultrasound done that is showing possible MSK, I have never had any stones or UTI’s, so my question is if I do happen to have MSK is it possible to live a normal life and never have any stones and UTI’s?
Hi Patricia, On ultrasound all that can be established is the presence of numerous small calcifications which could be from medullary sponge kidneys or simply another of the many causes of such deposits. Whatever the cause you can certainly lead a normal life. Of great importance is a program to reduce growth of the stones and also reduce the rate of new stone formation. Take a look at the Five Steps to Stone Prevention and try to follow through on getting this done. ALthough you may not have passed any stones from what you have said there are indeed calcifications in your kidneys and you do not want more of them. Regards, Fred Coe
Good Evening! I, too, was diagnosed with MSK shortly after the birth of my son in 2011. It explains why I spent my entire childhood with horrible kidney infections. My question is this……..what do you do when you are looked at poorly for expecting adequate pain relief even though you are clearly in agony, you tell the doctor you have MSK, the radiologists see the scans in front of them, and yet one still has to suffer the pain because so many addicts have made it to the point where those of us that actually need pain management CAN NOT get it?! I have never felt so hopeless. My marriage/family is falling apart because I stay in excruciating pain from this disease and have to fight from the depths of Hell to take care of everything and everyone I am responsible for.
Dear WV Girl, You are part of an unhappy crowd of people who are not being treated fairly. I presume you have many stones in your kidneys from the MSK and are perhaps infected. I would consider going to a center for consultation about better means of treatment. I do not know where you live, so I cannot be helpful in recommending a place. Regards, Fred Coe
Thank you so much for your response! I live in northeast Texas. I imagine there is a university medical center here (perhaps in connection with Baylor University). I am going to my PCP today to discuss pain management options. This will have to do until I can get in to see a nephrologist. I do sympathize with those suffering from this disease. I thought I was crazy in thinking this disease could be so painful, but, sadly, it is.
Hi WV, Baylor sounds like a good idea. I should mention Dallas – UT SW Medical School – has a stone center if it is not too far. Perhaps they might offer surgical options beyond the usual. Regards, Fred Coe
I did not ask this question before. How do I tell my doctor that I need pain relief without being labeled a drug seeker? So, so many have no idea how painful this disease really is, which leads me to believe that since my doctor doesn’t have the disease, I am clearly exaggerating the amount of pain I am truly in ( which as MSK sufferers know could not be further from the truth)
My daughter is 30 years old and was diagnosed with MSK 3 years ago while pregnant with her 5th child after moving to Ohio. She has had multiple UTI’s up to this point and was never diagnosed in Florida where she was born and grew up. They had never taken an xray to determine the cause of the UTI’s. She is in constant pain, runs a high temperature, has had extremely low potassium levels and cannot keep food down, therefore vomiting on a daily basis. She was referred by her urologist to one of the best nephrologists around who indicates that it is the “most impressive case” he has ever seen. He has informed her that there is absolutely nothing that can be done regarding this disease other than through daily diet and liquid intake, which obviously is difficult for her as she is continually vomiting daily. She’s been prescribed daily antibiotics on a continous basis and is seeing her urologist on a regular basis. I’m wondering what other options might be available for her. Is dialysis and/or a transplant optional or any other treatment that can be given to help her quality of life?
Dear gail, I imagine her low potassium is from vomiting. The cause of fevers and vomiting is unclear. If this is ongoing urinary infection despite antibiotics she has a major medical issue; likewise, but different in kind if the fevers are not urinary. I imagine her kidney function is normal, and such issues as transplant and dialysis are irrelevant to her. I gather there are no stones. If Cleveland Clinic is practical might I suggest she go there. Other alternatives might be Mayo Clinic. It sounds as though her problem is not being solved despite excellent intentions by those concerned about her health. Regards, Fred Coe
I was diagnosed with MSK when i was 21 years old, however experiencing symtoms since i was 15. I am at the point where now i have an ESBl infection (antibiotic resistant infection), and i keep getting this infection back. it is quite frustrating. I get so sick to the point i was hospitalized in sept & january for 2.5 weeks on dialysis. I get this infection every 4-8 weeks, and even though i get treated it comes back and im getting sicker and sicker. I have a 3mm left kidney stone that is stuck in one of my cyts which i think is harbouring the infection. Why is my specialist refusing to remove my stone? oh yea risk of infection and its too small. If im already infected with such a ESBL infection why arent they removing it, im suffering, missing work, and in insane pain sometimes to the point where i faint. is there any thing you can help me out with Doc?
Dear Rebekah,
Your situation is indeed serious and also quite complex. Given your history of recurrent, severe infections, if there is a stone that is in a surgically accessible location treatment should be considered. It is possible that the stone may be a source of the infections. As discussed in the article, many patients with MSK will have calcifications within the kidney that are not accessible (nephrocalcinosis) and will never be able to be fully cleared surgically. However, MSK patients commonly form stones within the accessible parts of the kidney as well which can be removed either using ureteroscopy or percutaneous nephrolithotomy.
Without being able to review the imaging myself it is hard to give advice on your current situation with the 3mm stone. The good news is that if it is the only stone that is visible on your x-rays/ultrasound/CT then there is hope that removing it may in fact help clear your infections. The tricky part may be if it is located within what we refer to as a calyceal diverticulum (similar to a cyst) which can be challenging to remove surgically and would likely require a percutaneous nephrolithotomy. These procedures are most commonly performed by endourologists who specialize in complex stone removal.
Sincerely,
Mike Borofsky
I am a 41 year old female with MSK. Recently I have been having high blood pressure. Not sure if it’s because I am sick or related to something else. My doctor has had me on 25 mg of Losartan and recently increased that dose to 100mg. As well as adding hydrochlorothiazide. I’ve been reading articles regarding these two medications. It says Losartan should not be taken if you have known kidney disease, but hydrochlorothiazide could be beneficial. I’m afraid that my doctor is not so familiar with MSK and I want reassurance that I’m not causing myself more harm by taking the prescribed medication.
Hi Norma, MSK itself is not strongly associated with hypertension which may be a separate problem in your situation. Losartan is an excellent choice for hypertension and combining it with a thiazide type diuretic is an excellent choice as well as their physiologies synergize nicely. Thiazide produces a fall in blood volume the way low sodium diet will do, and that is a main reason it lowers blood pressure. Losartan is used very frequently in patients with kidney disease and is thought to be helpful in prevention progressive loss of kidney function. Your situation is otherwise altogether from routine kidney disease in that almost all patients with MSK have normal overall renal function unless injury from stones or procedures or another disease have supervened. What may confuse people is that losartan and related sartan drugs reduce the filtration pressure in the kidney so blood tests can register a fall in kidney function. But that is like what happens when you turn down the voltage to a light bulb with a dimmer – the light is dimmer but the bulb lasts longer. So, your physician is doing well and you are being treated well, and should not expect any harm. Regards, Fred Coe
i have msk. Im always having protein and blood in my urine. I alway have kidney pain in the morning. Im wondering is there a time when the kidney will finally not be able to function. If so what are the symptoms that a msk patient gets.
Hi Crystal, The blood is from stones, I suspect and the protein is simply because of the blood. But your personal physicians will know exactly and you should ask them what you have asked me, here. Loss of kidney function from MSK is not expected. Regards, Fred Coe
if a pth calcium blood test is a 9.0 but the calcium in my 24 hour urine was 438mg could i still have something wrong with my parathyroid glands? I have msk disease and have trouble with continual calcium kidney stone. I have had pain in the front right side of my neck but my nephrologist isn’t concerned about the parathyroid since the blood test is in normal range?
I presume the 9 is your serum calcium level, and you do not show a PTH test. High urine calcium with normal serum calcium is idiopathic hypercalciuria most of the time and can be treated to prevent both stones and potential bone disease. Diet and thiazide diuretics are effective. Be sure your serum PTH is normal or even high but not suppressed – suppressed PTH means another kind of disease is present. Regards, Fred Coe
I also have another question:
I am 28 now…..why am i told that when my kidney stone is in my kidney i shouldnt be experiencing pain. Im finding this a load of crap!I have a stone stuck inside a cyst, and im experiencing the worst renal colic, to the point where i am throwing up at work. Why do patient with MSK have renal colic when a stone is not physically passing? I find that ER doctors look at me as though i am a “drug seeker” and ”cause with the amount of pain I am having, it cannot be associated with a kidney stone in the kidney. ” .
Rebekah
Hi Rebekah, You are part of a large cohort of patients who ask this question. Stones that obstruct interior passages within the kidneys may indeed cause pain, and the matter is considered a surgical controversy in terms of what to do. On the one hand there is the temptation to try to remove tissue mineral deposits, on the other there is no trial showing this is effective. So, every surgeon is in a way a pioneer until matters clarify. The behavior of ER personnel arises from the ‘war on drugs’ that has made physicians very worried about prosecution for excessive prescribing. It does not help that it is said that 17,000 deaths occurred last year from drug misuse. I am quite certain you are in no way a drug misuser, but a stone patient. Those prescribing are worried about being criticized or even prosecuted. It is a tough time with respect to pain control. Regards, Fred Coe
I am 33 and have suffered horribly over the past 3-4 years with colic and ER after ER have suggested I had psychological issues but I have just found a remarkable dr who is helping me with a diagnosis- I HOPE!! Do up still suffer? If so what do you do to relieve the pain? I go through a pain clinic and I find with the guidance of a pain specialist helps to get through day to day life!
Hi Danielle, It is very important to sort out the origins of the pain. If it is renal colic – meaning pain that comes in episodes, you may be having passage of crystals which cause pain but do not show up on radiographs. Often the crystals can be seen under the microscope and /or there is blood in the urine. This condition is prevented exactly as are stones themselves. I would pursue this with your physicians, and perhaps it will be possible to do something about the pain and not just have to rely on pain medications. Regards, Fred Coe
I’m 48 now but since the age of 4 was hospitalized a few times a year from severe UTIs, few times a year the contrast dye xray which one pees, holds on a table not pain free at 5yrs. Have a few rare congenital birth defects finally diagnosed in late 30s after decades of missed diagnosis or incorrect ones. MSK damn well hurts in the kidney and tubes, I’ve been to the endocronodist (sic) I eat well but with the different issues and now hypo thyroid it’s challenging, plus I create both types of stones many many each month. My urologist introduces me to his residences as a stone maker 🙂 My question is does it make sense that when a large one pops out of the kidney (ballooning) the kidney feels like its “ice cold” that burning pain which of course means I’m peeing every 10 mins. It’s just trying to accurately describe that pain. thanks
Hi Anna, The pain experience seems about what others have described. The frequent urination suggests the stones are obstructing at the junction of the ureter and bladder. But what is being done for you to stop the stones from forming? With many stones a month prevention is very important. Regards, Fred Coe
i have been going to the drs for about 18 months and have no diagnosis, but I think I may have MSK. I suffer from chronic moderate to very intense flank pain. It gets much worse during the night. I did have kidney stones (8, very small) about a year ago, and I feel like the pain has never completely gone away. My mother has MSK but is asymptomatic. My doctor says my urinalysis results were normal both times she tested, and that MSK does not cause pain, and is not hereditary. Therefore, she hasnt done any CT scans or additional testing. I feel so frustrated that I will never know what is wrong with me. Has any one else experienced anything like this?
Hi Kristine, MSK is not diagnosed by CT scan so I am not sure how yours was diagnosed. Like every stone former there are reasons you form your stones and prevention is usually feasible. Perhaps your 24 hour urines have been read with an eye to older upper limits of normal. Take a look yourself using my simplified questionnaire. MSK is not hereditary, it is developmental, but as I said there is no reason to believe you have it. As for pain from small non obstructing stones, urologists are beginning to believe it does occur. Overall, prevention is always preferable, and this site offers a lot of information about it that your physicians may fine useful. Regards, Fred Coe
Hi there, Im a little confused by the response.
The article states that: Recent evidence is that about half of patients diagnosed with MSK will have at least one relative with some degree of similar affliction. But you are saying that it is not hereditary, does that mean that the fact that my mother has it is irrelevant? Also you mention in your response to me that CT scan is NOT used for diagnosis of MSK, but the article states that: CT does have the capability of making this diagnosis when contrast is given and CT urography is performed. I have NOT been diagnosed with MSK, but have been suffering from constant pain and am looking for some kind of diagnosis. If not a CT scan, is there a different type of test I should be requesting in order to find out if i have MSK? Thanks again for your help & advice.
Hi Kristine, It is a developmental anomaly which means that there may indeed be genes that affect development and can lead to MSK but they are not directly causing MSK. CT scans cannot make the diagnosis without contrast infusion, and this is rarely done for stone patients unless there is a special desire to diagnose MSK. There rarely is such a desire because MSK or not does not change medical prevention efforts or surgery – at the present time. If you have constant pain, and multiple small stones in your kidneys you are in the very large group of patients with a problem for which surgeons have not as yet been able to come to a consensus about treatment. Some are attempting flexible ureteroscopic opening of dilated ducts in MSK or removal of tissue calcifications and stones in non MSK cases. Others are skeptical and concerned the risk of surgery is not balanced by surety of good outcome. I hope this answers your questions. If not feel free to email me directly and I can be more specific. Regards, Fred Coe
I am a 36 yo female who has suffered from approximately 15 stones in the last 15 years. During an ER visit, a radiologist diagnosed me with Renal Tubular Ectasia-is this connected to Medullary Sponge Kidney? Can you explain the difference between the two conditions and any possible treatments that may be available? I am allergic to Iodine contrast so CT scans have all been w/o contrast…
Hi Shelby, The two are the same and neither can be diagnosed without contrast. What was no doubt seen was multiple calcifications in the renal papillae – nephrocalcinosis. The calcifications themselves are not a basis for prevention. The best approach I could develop is here: I would certainly seek for a proper diagnosis for the cause of your stones or calcifications and a means for prevention of more. Regards, Fred Coe
Hi! In January I had 8 sones removed from the left kidney and one that was stuck on the way out and causing trouble. I did a 24 hour urine collection about a month later and it was totally normal. I drink a lot of fluids due to constant thirst from Sjogrens, so my fluid volume is excellent. The surgeon did not say I had MSK, but he did say there was something wrong with the anatomy of the kidney, that it has “deep pockets” that were difficult for him to navigate with the ureteroscope, and that no matter what I do or take I will probably form stones because of that (given my normal urine chemistry). Does this sound like MSK? Or is there some other kidney abnormality that would cause these deep pockets?
Hi Kate, Given you have Sjogrens syndrome you probably have renal tubular acidosis with consequent stones. I suspect your calcifications are plugs in the kidney tubules as are common in renal tubular acidosis. Bring this possibility to your physicians. I suspect they already know what you have, but perhaps they might want to consider treatment options. This is not a rare situation. Regards, Fred Coe
Thanks Fred. My urine ph is 6.3. Would that be consistent with renal tubular acidosis?
Hi Kate, It is rather a modest pH and not thrilling for the diagnosis if it is the 24 hour average. The diagnosis of RTA in Sjogren’s is made by reduced serum CO2 and a urine pH like yours. The diagnosis is pretty hard for me to progress for you as it is technically complex, and your physicians are in a lot better position to do it right. Just so long as they are thinking about the matter, they will figure out the best treatment. If they cannot, I could try to help but that would require a detailed look at all of the information. Regards, Fred Coe
I passed my first kidney stone at 21, and unfortunately it wasn’t my last. I was diagnosed in May of 2013 with MSK when I had to go in for a very thorough ultrasound. My urologist calls me “the Stone Queen”, and he doesn’t really know what to do with me. I am going to be 47 next month, and I had to have three surgical procedures in March 2016 alone. I have had a total of 11 ESWLs and 4 ureteroscopys just since July of 2013. I create two types of stones and I am on Uloric, Potassium Citrate ER, Tamsulosin HCL, and 5,000 IU of Vitamin D to try to slow down the production of stones. They have emptied my kidneys of stones with procedures and the next time I go in a few weeks later, I have already made quite a bit more. Is there anything that you can suggest that might help slow production? I am on a meat, and sugar free diet which seems to be helping the stones not “fuse together” and create large masses (which they were doing before). Thanks for any help you can offer.
Hi Jody, Stone prevention is one thing, and always about the same. Check out this summary; it links to other more detailed articles. All of them together outline a pretty good path to prevention that you can pursue with the help of your physicians. There are too many procedures, and not enough prevention; lets even things up. Let me know. Regards, Fred Coe
I have struggled with kidney stones and recurrent uti’s (3-4 a month) since I was 17. At 23 I was diagnosed with MSK and renal tubular acidosis after I was hospitalized for a severe kidney infection . I did the litholinks test and it showed a very high pH level and a shockingly low potassium level. I’m now on potassium citrate 15 Meq (2 pills twice a day). My urologist isn’t the best I don’t feel like I get the answers I want. After reading this article I’m considering getting a second opinion.
Hi Carly, If indeed you do have renal tubular acidosis the low potassium would be an expected finding and part of the abnormal physiology of that class of diseases. I presume that other causes of low potassium such as diuretics and vomiting or diarrhea have been excluded. RTA is indeed complex and another opinion is always a good idea. Regards, Fred Coe
Diagnosed with MSK years ago after episode of sepsis due to kidney stone. Later informed I have 2 small kidneys with each having 2 ureters. Last year I was told the top and bottom of kidneys do not communicate. Had many lithotripsys over the years (maybe 50 or so). Moved across state away from trusted urologist who has since retired. May 2015 became septic again due to multiple stones greater than 2 cm in size. Had neprostomy tube and multiple laser treatments on upper kidney with cyto to lower kidney to laser and retrieve stones. Took all summer for treatments. March 2016 began having occasional pain in right kidney. Occasional nausea and vomiting. Went to ER. KUB done. Told I had kidney stones and to follow up with urologist. Urologist who I saw last year, moved to another state. Other urologists to busy to see me. Saw NP. She ordered CT. CT showed multiple stones and stool. She told me there is no reason for pain and that I have one of two problems 1. back pain that needs physical therapy or 2. constipation and to take Miralax. I have not injured my back and I have no back pain. I had bariatric surgery 3.5 years ago. Side effect is multiple stools a day. I’m not constipated. (Although I will admit to not having a BM prior to that CT on that day.) I know kidney pain. I am having right kidney pain. By day, pain is about a 3 with momentary twinges that feel like getting kicked by a horse. By night, the pain increases when I try to sleep. I cannot sleep. It seems to help to urinate and put heat on right flank area and eventually doze in a sitting position. I have not had decent sleep in over a month now. I am exhausted. I have not asked for pain meds. I have not taken pain meds since Aug 2015. Yet I feel this NP has passed judgment on me. She tells me that I cannot have kidney pain with no stone in the ureters. Question: Is there a type of urologist that specializes in MSK patients? And how do I find him/her in my state? (Michigan)
Dear Peggy, You are part of a huge group of people with pain from small stones, and many of them write about this exact kind of problem. People are gradually coming to understand that you can indeed have pain from stones that are not obstructing. I think the department of Urology at the medical school at Ann Arbor would be my choice, given the complexity of your problem. Let me know if that works out for you. Regards, Fred Coe
What about in kansas? I wad diagnosed with MSK along with Nephrocalcinosis and stage 3 CKD back in January. Both my Urologist and Nephrologist just say my pain is back or gas pain because i do not have any obstructions or stone moving. I get a therapeutic massage monthly so i can pinpoint exactly where they pain is at and i also see a chiropractor 3 times a week right now that says its not back pain yet they do not believe me.
Hi, If your physicians cannot believe you, perhaps you need to seek others. The problem of small stone pain is by now rather well known, although far from solved. University of Kansas Medical center has excellent faculty in nephrology. Regards, Fred Coe
Thank you I will contact them.
I have suffered with MSK and RTA for years. Please pay close attention to your low potassium. I ended up passing out at 28 on my sons play ground and going into cardiac arrest. In the days after being hospitalized it was found my potassium was extremely low. Even with Potassium going in me both orally and IV I went into cardiac arrest 2 more times. I ended up needing a pacemaker to stay alive. Does anyone know of a good doctor in Las Vegas.
Dear Nicole, You sound as though you do indeed have renal tubular acidosis unless your potassium is low because of diuretics, vomiting, or diarrhea. That condition is very complex and I would advise you have consultation within a university hospital system. The University Medical Center has poor ratings and I personally know nothing about it. So this means you would need to make arrangements elsewhere. Certainly the very low potassium makes me concerned about what you really have, and that it was low enough to require a pacemaker even more so. The closest places that might work are Mayo Clinic in Arizona, UCLA, or UC Irvine where there is a good stone group. There are outstanding people in Dallas, if you can afford to fly there. Regards, Fred Coe
I passed my first kidney stone when I was 15 and then it seemed like every couple of months I was passing a stone. During the years I have suffered from chronic kidney pain to the point where even when I would inhale it hurt…long story short at 21 I had my appendix removed and the imagining revealed that I had MSK as well. 2 years ago I was hospitalized and had 19 kidney stones removed via bilateral ureterscopy with stent placement. After 2 weeks the stents came out and my urologist said he had gotten the majority of the stones out. So a couple months go by and I feel that flank pain again, I went to the hospital and they found that I had 13 more stones that had developed…I guess what I’m saying is that is this what my life is going to consist of…
Hi Sarah, You are making a lot of stones and really need proper prevention now. Take a look at the overview of how to get it done. I would begin at the beginning of the article, read the linked articles and get the testing, use it, and get on focused preventive treatment right away. I have seen many patients with rapid recurrence, and urge you do everything reasonable to interfere in that process. No, your life need not be all about stones, it is all about prevention of stones. Regards, Fred Coe
Hi all, my name is Theresa I am about to be 45, I passed my first stone at 19… (Actually went to ER where I was told that I needed surgery to remove a stone. What the heck I thought. When the Dr went in he noticed that I had other stones, which he thought may pass. I can’t tell you how many stones I have had removed, I was diagnosed many many years ago with MSK, RTA, CKD, Hypercalceuria (sp) I was only diagnosed back then with left sponge kidney. I was diagnosed in my right kidney.. For those of you who are new to this, it’s about having a great UROLOGIST! I now have a great one, he is very educated on our disease and I have never had a dr who treated me as if I wasn’t crazy and that I was truly in pain. Due to my past UROS not listening, and thinking I was crazy, I now have kidneys that are completely embedded with stones. The URO I have now listens, and if I have an episode I know I can call him and get in. I see him every six months. Unfortunately my daughter had kidneys stones during her first pregnancy, and has yet to have another. My niece is has been dealing with kidneys stones for a couple of years and she is 19. Thanks for having this page and being able to share and read others stories…
Dear Theresa, I am glad you have found someone to help you. I presume you are no longer forming new stones. Because it is so hereditary, idiopathic hypercalciuria may well be affecting your daughter and niece. I hope both are being checked for it and treated so they do not form so many stones. Regards, Fred Coe
Thank you for answering these questions so quickly. My urologist told me I have MSK…my first stone was in 2007, at 47 years old, and I have passed numerous stones since. Twice, I had to have them removed via ureteroscopy. X-rays show I keep making them, and they aren’t getting smaller. Have tried different diets to no avail. Most recently, I went on a Paleo diet for weight loss, etc, and my most recent 24 hour urine showed increase in both calcium, and now uric acid. At a loss. Not sure why lithotripsy is not indicated, or if there is some other procedure that can get rid of them all (or most), or what else to do. Had even tried a Chinese herb for a while that made the urine analysis numbers look much better but the stones themselves did not shrink. Perhaps I didn’t take them for long enough (it was four months). Not sure if there is a recommended specialist in my state (Florida), or another state, if necessary, but if you have any input at all I would be most grateful. Thank you so much.
Dear Debbie, With all these stones and hypercalciuria prevention is important and should be effective. Lowering urine calcium with low sodium diet and if necessary thiazide diuretics is effective. The high protein diet will predictably raise urine calcium and urine uric acid, so that diet is not advisable. Likewise high fluids. The point is to lower urine supersaturation and keep it low. Take a look at how prevention can work I am not familiar with a special prevention program in Florida, but if you can travel to other states let me know by separate email and I will try to help. Regards, Fred Coe
Thank you. I would be willing to travel, if there is better treatment. Any suggestion of where is best would be welcome!
Hi Debbie, I never make any comparisons or recommendations on the site. If you wish to email me flcoe#uchicago.edu – I will be happy to help you choose in terms of needs, travel issues and all. Regards, Fred Coe
Hello-
I was diagnosed with Medullary sponge kidney disease 2 years ago due to a high fever with an ecoli infection. I was told I had a urinary tract infection caused by ecoli. I’ve been prescribed 3 rounds of different antibiotics. However the infection/ ecoli was still persistent. I decided to see a urologist and after having urine cultures, a sonogram, an x-ray, a catscan and a litholink 24 hour test, I was told I have MSK. I have absolutely no pain, symptoms or discomfort of stones or UTI. I’ve taken 9 rounds of antibiotics and am currently taking hippurate/methanamine, potassium citrate. The prescribing urologist believes some of the stones are colonized and he would like to perform a urethroscopy to find out if the stones are in the funnel plus to perform lithotripsy and most probably insertion of stents (possibly multiple sessions). I was told he isn’t aware of how intense my situation is, until the urethroscopy is performed and at that time he might have to perform multiple lithotripsy and possibly have to access from my back.
I am asymptomatic no pain of kidney or complaints of UTI ever, however last month again I had high fevers which was admitted and received IV antibiotics due to sepsis. I’m not sure if having a procedure is going to help my case. I’m afraid it will open a can of worms and lead to pain that I don’t currently have.
I would love to hear your opinion & Im looking forward to hearing back from you.
Thank you very much,
Mona
Hi Ramona, The stones themselves do not appear to be causing pain infection or bleeding but you have had multiple infections which could be from MSK – if indeed you have this – or infected stones. The fact that repeated antibiotic treatments have failed makes me think there is infection within stones. Ureteroscopic inspection and removal of stones with stone culture is in fact a rather good plan – as best I can tell from this distance – and it is hard for me to argue against it. Shock wave lithotripsy does not seem a very good idea because of infection and because it sounds like there may be many tissue calcifications that will not respond to such a treatment. But perhaps your physician means laser lithotripsy during the ureteroscopy, which is a common practice. After ureteroscopy your physician will indeed know what is present, will have removed all movable stones, and have them cultured; hopefully their removal will help with preventing more infections. YOu do indeed have a very complex problem, and you might want a second opinion. Incidentally, with all the infection, dusting during ureteroscopy might not be as ideal as selective stone removal. Regards, Fred Coe
Hi Dr. Coe-
I am hoping you can guide me to the right path. My urologist believesthe reason I test positive for E Coli is due to some colonized stones. In October of 2016 he performed cystoscopy and laser lithotripsy on the stones he thought were suspicious. Two months later I again tested positive for E Coli. Currently, I am on another round of antibiotics and have become resistant to some.
I am losing hope and not sure what to do.
Any help you can give me will be greatly appreciated.
Thank you very much.
Sincerely,
Mona
Hi Mona, It would seem important to ask if all the stones were removed. If not perhaps more are infected than was thought. Alternatively you are colonized and creating resistant organisms. If you are treating symptomatic infections – fever, pain, and cannot control these episodes consider more infected stones. If you are not treating culture reports discuss with your physician if it is not better to stop and let the bacterial sort themselves out. Resistant organisms will be overgrown by non resistant ones in the absence of antibiotics. Regards, Fred Coe
I am from Long Island, NY. Please let me know if you know anyone who you would recommend for MSK patients for urologist or nephrologist.
Your help is greatly appreciated.
Mona
Hi Mona, I do not endorse physicians on the site apart from occasional references to university teaching centers – If you want to contact me personally I will try but not in a public place. My email is on the site. Regards, Fred Coe
Mona, I have a great urologist in NY… however don’t think posting of docs are allowed here.
You can write to her privately. Fred Coe
Carol- would you pls let me know how I can get intouch with you privately? Would really appreciate your help.
Thanks,
516-776-8892
Mona
Carol- would you please contact me and let me the dr’s name. I would greatly appreciate it. My contact: ramobrt@aol.com cell:516-776-8902. I thank you again.
I have some multiple cysts with stones on both of my kidneys. I’ve been taking potassium citrate and now my stones got smaller but did not totally pass. Can this possibly be a case of MSK, too? On my ultrasound, the impression is, focal ecstasia with cysts or cysts with nephrolithiases. Please advise.
Dear Anne, What you describe is complex and of course I cannot be sure about anything from such a distance. Given many stones and cysts I would seek at least one consultation with a physician who is an expert in the cystic renal diseases to be sure of what you really have. It is not likely to be MSK. Regards, Fred Coe
Hey I am from Canada and I have diagnosed with msk. I have been suffering with chronic pain and stones for 14 years. I am tired. It sure helps to hear other people’s stories because most of the time it just feels hopeless. I have chronic bouts of nausea and vomiting as well just wondering if this is a symptom of this or something else. I have had months where I can’t eat a meal with out vomiting. Between that and the stones it’s been a long hull. Any suggestions would be appreciated.
Thanks
Hi Sasha, The nausea and chronic pain always suggest infection or bouts of crystal passage. Your physicians know this, of course, but perhaps you might bring it to their attention once again. The main point is to head of crystal formation, and your vomiting and dehydration will create a possible vicious cycle in that regard. Be sure the causes of your stones are known, and you are on preventative treatment. Possibly a period of home IV fluids during vomiting spells will help ward of more crystals. Often this works and one can get back to more normal life. Regards, Fred Coe