Kidney stone types
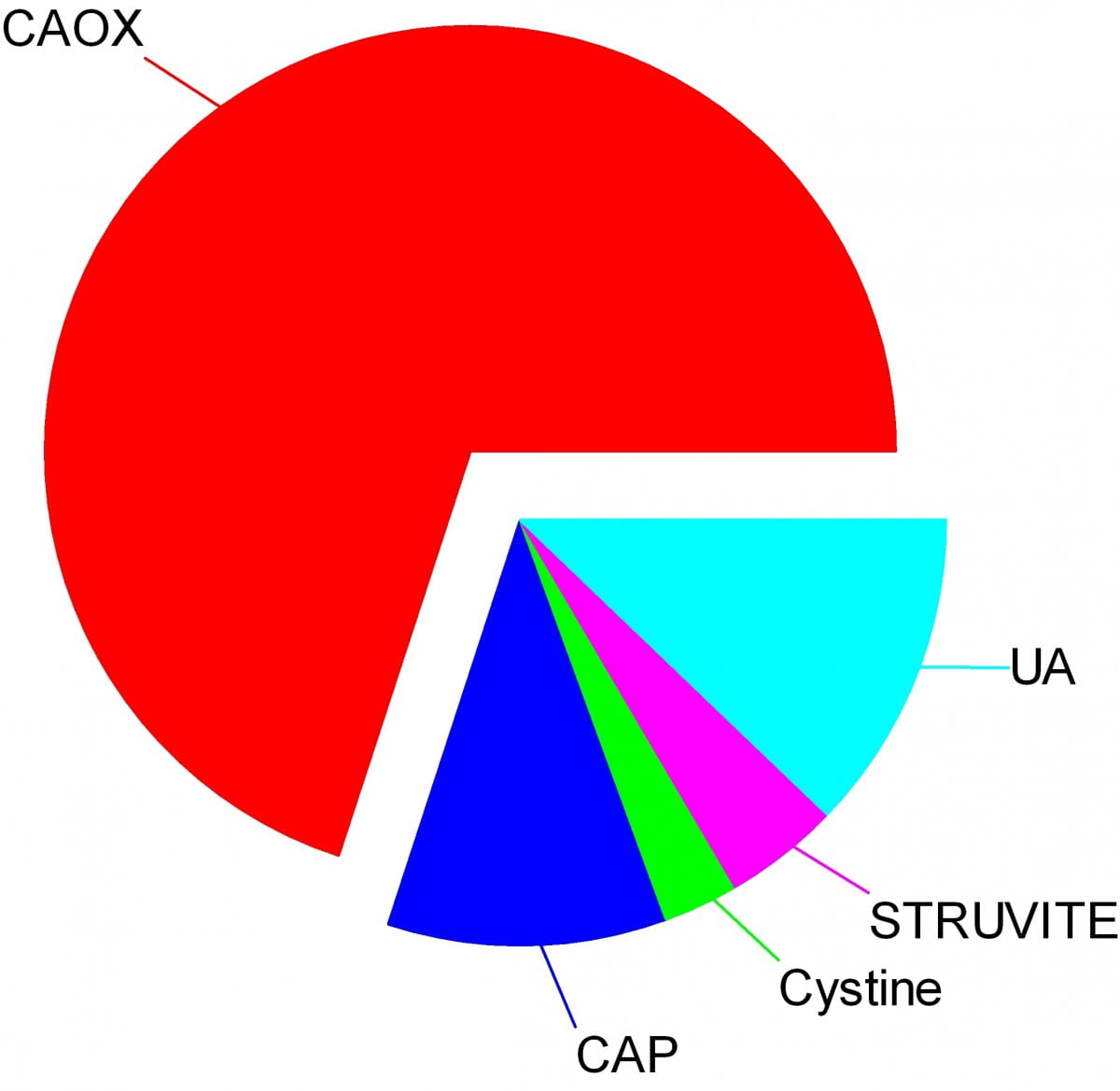
Crystals make stones and their names signify the kidney stone types. Here are the names of the crystals that make the stones: CAOX, Calcium Oxalate; CAP, Calcium phosphate; UA, Uric Acid; Cystine; Struvite.
The wedges on my pie chart show the relative abundances of stone types in our large population of stone forming patients. Calcium oxalate stones predominate by a wide margin in our clinic and in all others I know of.
The names, matter because the whole science of stone prevention focuses upon stone crystals. Each kidney stone crystal creates its own unique illness and requires specific treatment. That is why we name stones by the names of their crystals and why when stones are analysed the results are reported by these very same names.
Being a bold and rather large graphic, the featured picture does what I intended, brings the main facts into view as, at a circus, the great animals and the small animals circle the ring by way of an introduction. Come. I will show you all the common stones, like at a fashion show, or a circus parade. You can watch as they go by and remind yourself, or wonder, which ones might have been yours.
Here they are.
Which type do you have?
You might think your doctors know what stones you have formed, but don’t rely on it. People move, doctors move, health records are far from ‘all electronic’. That stone report from 4 years ago could lie in a dusty filing cabinet, your new doctors unaware it exists. Worse, it could hide in a dresser drawer and you forgot it you put it there. Perhaps even more worse, the stones might stay in that drawer, never analysed at all. Find the stones, find missing reports, urge analysis by your physicians. They can help you most if they know your stone analysis.
When they do not know, physicians can still mount prevention efforts but with less focus and probably less effect than when guided by a knowledge of the crystals. So always seek treatment. If a stone comes along the way, make every effort to get it analysed.
Why should you care to know all this?
Because you will conduct much of your own treatment, and over many years.
Since stones tend to recur, prevention requires treatment over long periods. These treatments work by altering urine chemistry in a direction that minimizes the risk of forming crystals. Such altering of urine chemistry requires control of fluid intake, lifestyle, and diet, and sometimes additional use of medications.
Just as the sailor who aims along a chosen track against the random, misdirecting, confusing sea and air maintains a constant way in proportion to that skill which comes from knowing the way of the boat, patients who aim to keep a certain kind of condition in their urine despite the demands and temptations of the world do so, I believe, in proportion to skills that come from knowing how their work and lives and foods affect their bodies, and how those crystals form which they so much desire to prevent.
Put another way, knowledge is power.
Why is this article so long?
I wanted to put all five main types of kidney stones. That makes a long story. But probably you will care to read about only your own type.
I should mention here, to save a lot of confusion, that stones often contain mixtures of crystals.
The pie chart refers to the most common crystals in a stone, for which the stone is usually named. Much of the time, minor crystal components are not crucial, but sometimes – to jump forward a bit – they are. Even a trace of struvite or cystine, for example, can have great diagnostic importance.
Calcium stones
Calcium Oxalate Crystals
In the great circle atop this page article, the calcium oxalate stone, being most common, occupies a lion’s share of the space. 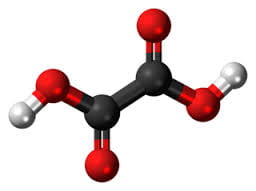
The calcium oxalate crystal forms when calcium combines with oxalic acid. Oxalic acid (at left), a dead end waste product that the kidneys remove, contains two carbon atoms (the large black spheres), four oxygen atoms, and two hydrogen atoms (silver).
At the acidity of urine, the positively charged hydrogens leave their negatively charged oxygens. As a result the oxalate molecule carries two negative charges. In the figure at right one negatively charged oxygen attracts the hydrogen of a nearby water molecule (H – O -H) while another attracts a positively charged calcium atom.
You can imagine how another oxalate ion (the name for a charged molecule in water) could attract the same calcium, or another calcium atom attract the bottom oxygen on the oxalate molecule so the chain extends and makes a crystal. You can see more about this in a video I made. Broadly speaking – though my more expert colleagues may bridle at such a simplification – the calcium atoms and oxalate molecules combine by the attraction of their opposite charges.
The calcium oxalate kidney stone comes in two varieties, calcium oxalate monohydrate and calcium oxalate dihydrate. The former are harder and therefore more resistant to fragmentation by lithotripsy. Likewise, the former appear more often when elevated levels of urine oxalate are present.
Calcium oxalate stone formers
From Systemic Diseases
Sometimes this kidney stone arises from a systemic cause, like bowel disease, primary hyperparathyroidism, or primary hyperoxaluria. Only physicians can establish that a known disease – like bowel disease – is the cause of stones. Only physicians can discover underlying primary hyperparathyroidism as a cause of stones. Patients cannot do much for themselves except provide as complete a medical record as possible.
Idiopathic
Most of the time this kidney stone arises simply from the interplay between inheritance, diet, and aspects of daily living. We call such patients idiopathic calcium oxalate stone formers, from Greek ἴδιος idios “one’s own” and πάθος pathos “suffering”.
Even though physicians discover the links between daily living and stone production, and select those changes that can prevent new stones, patients themselves must create and maintain those changes. I believe patients can so this in proportion to how well they understand what is needed, and why. When changes in daily life are not enough, physicians add medications, so even then patients remain active therapists for their own disease.
Stones usually form on kidney surfaces
About one million nephron units make up a normal adult kidney. The calcium oxalate kidney stone type does not grow in the tubules of the nephrons but ‘outside’ them, on the surfaces of the renal pelvis where final urine collects and drains through the ureter to the bladder. Here is a video that shows how they can form.
Calcium phosphate crystals
Phosphate ion and urine pH
Calcium phosphate stone crystals form when calcium atoms combine with phosphoric instead of oxalic acid and produce the calcium phosphate kidney stone.
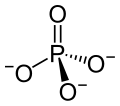 Phosphoric acid is simply a phosphorus atom (shown as the ‘P’ in the line drawing to the left) with 4 oxygen atoms bonded to it. One oxygen atom has two lines for its bond to phosphorus; this oxygen cannot provide any charge with which to bond calcium atoms to make a crystal. The other three have ordinary bonds that are shown by a line, and a dashed and solid arrow. These two arrows mean simply that the oxygens lie above and below the plane of the paper – so if you built the molecule with sticks and balls it would have a three dimensional shape.
Phosphoric acid is simply a phosphorus atom (shown as the ‘P’ in the line drawing to the left) with 4 oxygen atoms bonded to it. One oxygen atom has two lines for its bond to phosphorus; this oxygen cannot provide any charge with which to bond calcium atoms to make a crystal. The other three have ordinary bonds that are shown by a line, and a dashed and solid arrow. These two arrows mean simply that the oxygens lie above and below the plane of the paper – so if you built the molecule with sticks and balls it would have a three dimensional shape.
One of the three negatively charged oxygens never has a hydrogen on it in urine but only in exceedingly acidic solutions. A second charged oxygen is always occupied by a hydrogen atom in urine.
This makes the third oxygen, variably occupied by a hydrogen in urine, a tie breaker.
In a urine of average normal acidity (pH around 6), most of the tie breaker oxygens have their hydrogen leaving the phosphate ion only one negative charge. Not enough to make a crystal.
When the urine is abnormally alkaline (pH above 6.3 or 6.5), the variable oxygen becomes charged so the ion has two negative charges that can combine with calcium to make crystals. For this reason the calcium phosphate kidney stone tends to occur in people who produce a more alkaline urine than those who produce calcium oxalate kidney stones.
Brushite vs. hydroxyapatite
Much like calcium oxalate, calcium phosphate crystals begin simply as one to one pairings of doubly negative phosphate ions with doubly positive calcium atoms. This initial crystal is named brushite. Brushite, which is an equal mixture of calcium and phosphate ions, can convert to hydroxyapatite (HA), which has a more unbalanced proportion of calcium to phosphate. Hydroxyapatite crystals make bones hard.
Because less soluble than brushite, hydroxyapatite cannibalizes brushite. The organic molecules in urine modify this process.
Calcium Phosphate stone formers
From Systemic diseases
Primary hyperparathyroidism and renal tubular acidosis raise average urine alkalinity (higher urine pH) and foster calcium phosphate kidney stones. Many uncommon genetic diseases do the same.
Idiopathic
Idiopathic calcium phosphate stone formers share a common set of traits. Perhaps because urine contains far more phosphate than oxalate, they form more frequent and larger stones than idiopathic calcium oxalate stone formers. Often the stones originate as crystal plugs at the terminal ends of the kidney tubules. More crystals deposit over the end of the plug open to the urine, to make the final stone. Crystal plugs damage the cells that line the tubules and cause local scarring.
Uric acid stones
Uric acid crystals
Structure and charged sites
A breakdown product of DNA and RNA, uric acid forms crystals in abnormally acidic (low pH) urine. Obese and diabetic people, those with gout or kidney disease typically produce abnormally acid urine. I know how the urine becomes acid, but leave it for elsewhere on the site.
Uric acid, the molecule we are interested in here (shown to the far right), has two linked rings made of carbon atoms (they are at the angles where lines join), with  interposed nitrogen (N), oxygen (O), and hydrogen (H) atoms.
interposed nitrogen (N), oxygen (O), and hydrogen (H) atoms.
This molecule has only two charged sites, the nitrogen atoms at the bottoms of the rings. In urine of pH 6 or so, one nitrogen lacks its hydrogen and therefore carries a single negative charge. In more alkaline solutions both nitrogens lack hydrogens, but urine does not normally achieve such alkalinity (pH>8).
When urine pH is low (<5.5) and both nitrogens have their hydrogens, the molecule lacks any charged site, so water can no longer find a hold on the molecule. It crystallizes. It simply leaves the water as water droplets themselves form from the high and vaporous late afternoon clouds and fall from the air as the warm rains of springtime.
Relation to water
Water molecules are each a single oxygen atom (large ball) bonded with two hydrogen atoms (small balls) as in this picture from Wikipedia. The hydrogen side has a positive, the bare side of the oxygen a negative charge. So water molecules link to each other, 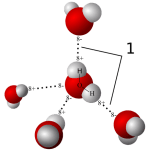 positives to negative surfaces, to make up the clear and seemingly continuous fluid we drink, swim in, and hold up umbrellas to keep off of us when it rains. They link by charge at angles, shown by the number ‘1’ so as to make up a three dimensional macrame.
positives to negative surfaces, to make up the clear and seemingly continuous fluid we drink, swim in, and hold up umbrellas to keep off of us when it rains. They link by charge at angles, shown by the number ‘1’ so as to make up a three dimensional macrame.
To be ‘in solution’ means to have some charge to which water molecules can link up with by attraction. Calcium atoms are positive and become surrounded by a shell of water molecules facing it with their bare negative surfaces. Oxalic and phosphoric acids have negative charges and are surrounded by water molecules pointing their positive or hydrogen sides to them.
Uric acid at neutral pH has its one negatively charged nitrogen water can grasp. But when pH falls, and neither nitrogen has any extra charge for water to bind with, how can the molecule remain among the water molecules? It cannot. The molecules stack into solid crystals and fall from solution.
Uric acid stone formers
The stones can be orange – red, large, and numerous
The stones can be red or orange because uric acid crystals absorb hemoglobin breakdown products that are red – orange pigments in urine. Sometimes uric acid crystals pass in urine as a red orange gravel.
Uric acid does not have to connect itself to some other atom or molecule to make a crystal, in the way that calcium must bond with oxalate or phosphate ions to make calcium oxalate or calcium phosphate crystals. When pH is low enough to extinguish its charge, uric acid can crystallize very fast, in seconds, and pass as an orange gravel in the urine. If retained, such crystals can grow rapidly into large stones. Because there is much more uric acid in urine than there is oxalic acid, uric acid stones can grow very large and rapidly. Some fill up the entire collecting system of the kidney.
Urine pH controls stone formation
But because the whole process depends almost completely on the acidity of the urine, uric acid stones are very easy to treat. Just a modest amount of supplemental alkali will make the urine of almost any patient alkaline enough that the hydrogen atoms are removed from the one crucial charged nitrogen. Water can bond there so uric acid remains in solution. Because so simple, treatment prevents stones with certainty. Relapse need never occur.
Mixed stones require special care
Unfortunately, however, stones commonly contain uric acid mixed with calcium oxalate. In this case, one needs to track down the cause of the calcium oxalate stones as well as make the urine alkaline enough to stop uric acid stones from forming. Calcium phosphate crystals mix with uric acid only rarely, because it takes a rather alkaline urine to remove the hydrogen atoms from phosphate so it has two negative charges and can bind efficiently with calcium atoms. At that higher pH, uric acid will have its charge site and remain in solution.
Struvite stones
Urea and the planet
Kidneys cannot make struvite. Bacteria make it. Not all bacteria, either. It takes bacteria that normally thrive in the soil, and they do it for ancient and compelling reasons. These bacteria produce the kidney stone named Struvite after Heinrich Christian Gottfried von Struve (1772–1851).
Animals deposit urea (at left) all over the planet when they urinate. Plants cannot use it.
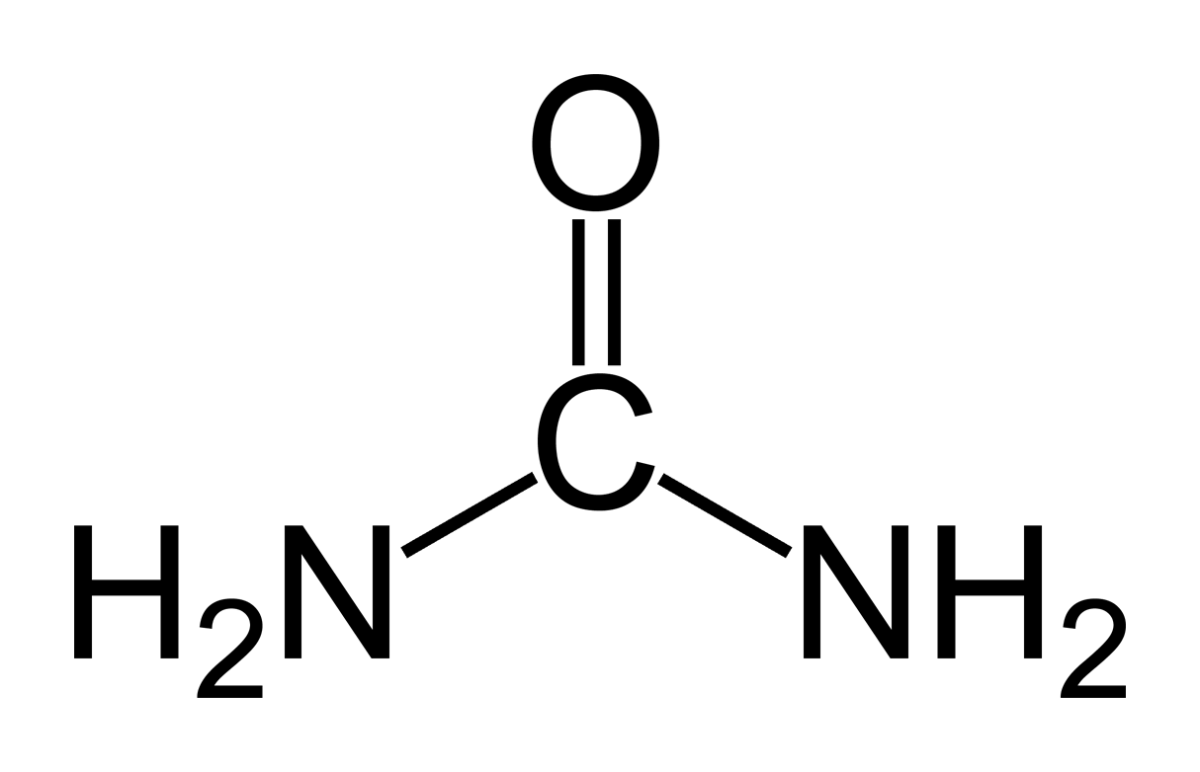 Like oxygen, nitrogen is an essential for life yet dangerous. It is integral to proteins, DNA and RNA. As these molecules are broken down and remade, some of their nitrogen slips by and can form poisonous compounds unless caught up in safe waste products. Of these, the main one, urea, contains 2 nitrogen atoms bound to a single carbon atom (‘C’ in the picture to your left).
Like oxygen, nitrogen is an essential for life yet dangerous. It is integral to proteins, DNA and RNA. As these molecules are broken down and remade, some of their nitrogen slips by and can form poisonous compounds unless caught up in safe waste products. Of these, the main one, urea, contains 2 nitrogen atoms bound to a single carbon atom (‘C’ in the picture to your left).
Uric acid contains 4 nitrogen atoms (look back at the picture of it). Birds and reptiles excrete most of their nitrogen as uric acid; mammals like us excrete nitrogen mainly as urea.
As the animals of the world urinate on the soil, their urea brings nitrogen to plant roots, but the plants cannot use it. They cannot release the nitrogens from the carbon atom that holds them. Those soil bacteria that make struvite crystals have an enzyme, called urease, that can release the nitrogen for plants to use as their nitrogen supply.
So, soil bacteria with urease maintain the nitrogen cycle of the earth.
Struvite crystals
As they release nitrogen from its carbon in urea, the nitrogen takes up a proton making ammonia (NH3). Ammonia is a powerful alkali and takes up another proton.
As it does so, the working bacteria surround themselves with spheres of very alkaline fluid enriched with ammonium ion (NH4) that carries one positive charge. Soil magnesium ( an atom with two positive charges) and phosphate sans all of its protons (an ion with three negative charges) spontaneously form their triple salt: three negative phosphate charges, two positive from magnesium, one positive from NH4).
The crystals anchor the bacteria and help create a porous nitrogen rich soul good for plants to grow in
The struvite kidney stone
Why they start
Because urine is filled with urea, soil bacteria that get into the urinary tract can break it down to ammonia and create struvite from the magnesium and phosphate urine always contains.
You might wonder how soil bacteria get into the urinary system.
Because we eat them, with foods that are not cooked, and they become part of the intestinal bacterial population from an early age. In us and around us, they find a way into the urinary system, especially in women whose shorter urethra makes entry easier. No matter how skillfully used, any instrument put into the bladder can carry our personal soil bacteria with it.
What they do
Because they live among molds and fungi, soil bacteria easily mount resistances to antibiotics, so antibiotics given for a urinary tract infection will tend to kill sensitive bacteria and select out those that can resist them.
Soil bacteria can produce struvite stones de novo, or infect calcium stones to produce a mixed stone. Either way, struvite stones are infected by their very nature. They can become huge. Their bacteria can injure the kidneys, even enter the bloodstream and cause sepsis.
Treatment is a mix of thoughtful surgery and selection of antibiotics after such surgery to kill bacteria that remain. If the stones are a mixture of struvite and calcium crystals, new calcium stones need to be prevented.
Cystine stones
Inherited kidney abnormality
 Lemon yellow with a sugary coating these form only in people who have an inherited kidney disorder called cystinuria.
Lemon yellow with a sugary coating these form only in people who have an inherited kidney disorder called cystinuria.
Although the kidneys function well, they permit abnormal amounts of four amino acids to enter the urine. Three do not matter that we know of. The fourth makes crystals and the cystine kidney stone type.
Cystine
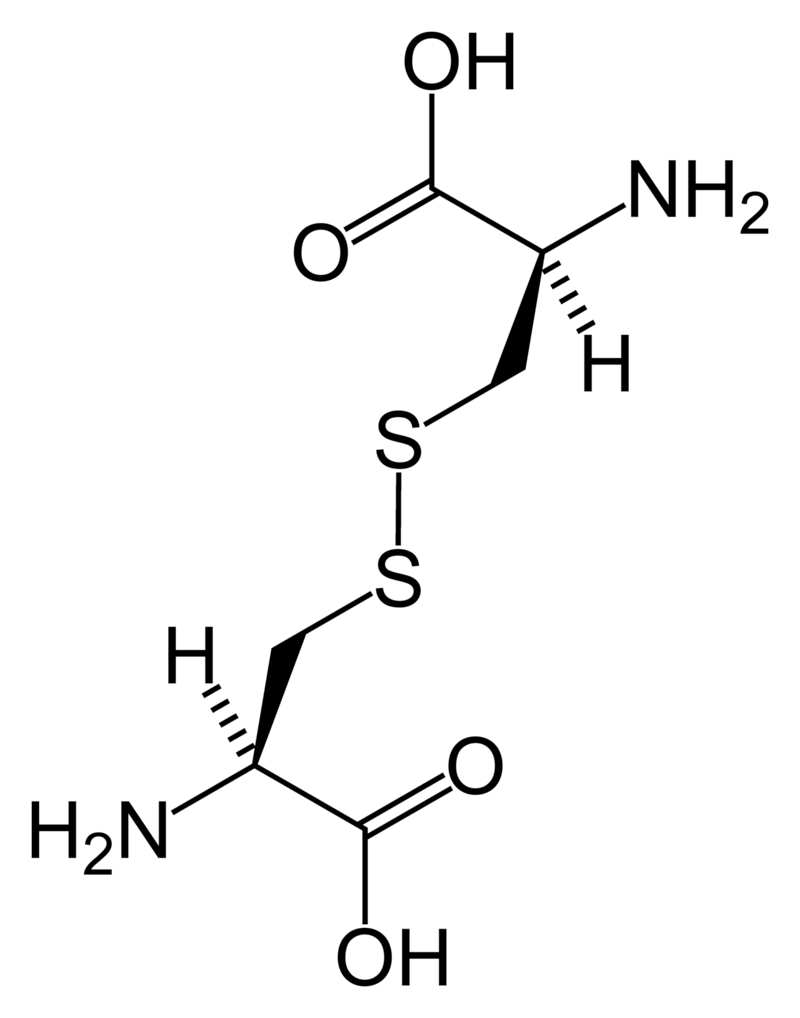
Cystine (left) forms through the coupling of two identical amino acids – called cysteine – through their sulfur atoms (‘S’ in the line drawing).
Each cysteine contains two carbon atoms – not shown except as corners – bonded together (shown by the single long line that connects the two corners) as in oxalic acid.
One carbon atom has 2 oxygens bonded to it; the other has one nitrogen (which makes it an amino – nitrogen containing – acid), a hydrogen atom, and a sulfur atom. As for phosphate, the dashed and solid arrows simply mean the hydrogens and sulfurs lie above and below the plane of the page and a stick model would have a three dimensional shape.
Cystine Crystals
Cysteine itself is very soluble because the sulfur atom has an appreciable negative charge.
But the big, long cystine molecule has very little charge because the sulfurs bind to each other. So, like uric acid, cystine loses intimacy with water molecules and simply leaves the solution as crystals. Also like uric acid, the process is fast.
Cystine stones
Because people with cystinuria lose large amounts of cystine in their urine stones readily grow large, and fast.
Stones probably form in the urine itself. But cystine crystals can plug the ends of kidney tubules, as calcium phosphate crystals do, causing cell damage.
Since cystinuria is an inherited disease, stones may begin in childhood.
Effective treatment always requires very large amounts of fluids to dilute the urine. The few effective drugs resemble cysteine. Their sulfur groups bond with cysteine to form a ‘mixed disulfide’ more soluble than cystine. But their side effects can limit use.
Rare stones
Here and there we find patients who make uncommon crystals and require very special care.
Uric acid, as an example, can form odd crystals such sodium or ammonium acid urate, especially in people with bowel disease and chronic diarrhea.
Anti-viral drugs can crystallize in urine and form stones only recognized for what they are through stone analysis.
Very rare disorders of metabolism can produce molecules which crystallize in the urine, for example 2-8 dihydroxyadenine.
Although it can take a while before the right answer emerges, stone analyses will put physicians on the right track for these special cases.
The end of a very long post
That’s my parade.
The common animals and the rarer animals have gone by, and you have glimpsed the main ones, big and small.
The one point is what it was at the beginning. Each kind of kidney stone has its own ways, and treatment requires we know which one you have.
Likewise, for whatever that one may be, it is good to know as much about it as you can know. For long term prevention of stones is hard to come by and ultimately what the patience and and consistency of patients themselves matters most.
If you don’t know which stones you have made, find out.
Track down old reports and pull them together.
Keep copies and send everything to the doctors who care for you.
Fred Coe MD


THANK YOU very much, Dr.Coe – for all the responses you provide. Just finished lithotripsy, first time, @ 70 y. Result: 90% calcium oxalate mono and 10% calcium ox dihydrate. Mostly normal blood panels…lots of water 70-90 oz. daily intake, no medication, watching oxalate food intake – as much as humanly possible. Would like to decrease uric acid naturally, how to do this please?
Hi Pia, I can see no reason to focus on uric acid. You formed stones late in life and need a proper evaluation as to the cause of stones. Regards, Fred Coe
What about carbonate apatite (dahllite) 100 stones? These kinds of stones are not mentioned.
Hi Kristi, It is calcium phosphate stone crystals but the crystals incorporate carbonate ions as part of their structure. Treatment is the same as for routine calcium phosphate stones. Best, Fred Coe
What does one do when the stone comes back 50% calcium oxalate monohydrate and 50% calcium oxalate dihydrate and you suffer from gout?
Hi Marsha, Gout patients form more stones than normal people, and often the stones are not uric acid but calcium based. What you must do is evaluate fully for causes of the stones. Go on from there. Best, Fred Coe
Is Calcium oxalate monohydrate associated with tubular injury and fibrosis over time, essentially is it a contributor to CKD?
Hi Jeremy, kidney stones are associated with increased risk for CKD, mechanisms are various. So you are right. Best, Fred
What do I do as my stone has come back Ammonium -Magnesium Phosphate Hexahydrate(Struvite) 80% Carbonate Apatite (Dahllite) 20%??
Hi Tina, This is a stone caused by infection and needs very expert urological and medical care.Best, Fred Coe
Hello Dr. Coe,
I am 23 years old and after my 4th bout of kidney stones in the last 3 years, they were finally able to test the stone they had extracted. It came back to be 40% Calcium oxalate dihydrate, 40% Calcium oxalate monohydrate, and 20% Calcium phosphate (apatite). I drink 120 ounces of water a day, I try to avoid soda, I am a dance teacher, and I eat very regularly.
I’m waiting for an appointment with the Urologist. Got any advice for the wait or the appointment?
Hi MK, You need a full evaluation to find the cause. I guess it is a combination of high urine calcium and low urine flow (perhaps in past years) given the COD and COM. Dance teachers can get dehydrated, can they not? Best, Fred Coe
Hi Dr. Coe, I am a 56 year old female who just had cysto/uretero w/lithotripsy and stent for a 10 mm stone – calcium oxalate monohydrate 95% / carbonate apatite 5%. I also passed 2 smaller stones in the hospital before having the procedure. I had no prior history of stones. Approximately 12 months ago, I completely changed my diet to lower my LDL cholesterol – and it worked! My LDL is down to 80. Unfortunately, my very healthy diet of daily bran, almonds and seeds, lots of beans, leafy veggies and dark chocolate, and eliminating cheese, is what I think caused my stones. I’m also experiencing daily menopause symptoms of hot flashes and sweating for the last 2 years. I was never a water drinker – most days only drinking around 20-30 ounces a day. I now drink 100 ounces of water a day. I know it’s impossible to predict, but in cases like mine, do you think if I eliminate all those “healthy foods” that I added last year, and increase my water intake, will that solve my kidney stone problem? Or is this just a new phase of life where I will continue to create stones?
Hi Karen, Maybe change of diet, but menopause can create high urine calcium losses that cause stones – and point to bone loss one might want to reduce. So I would go ahead and do a real evaluation – ‘Just in Case’. Regards, Fred Coe