Kidney stone types
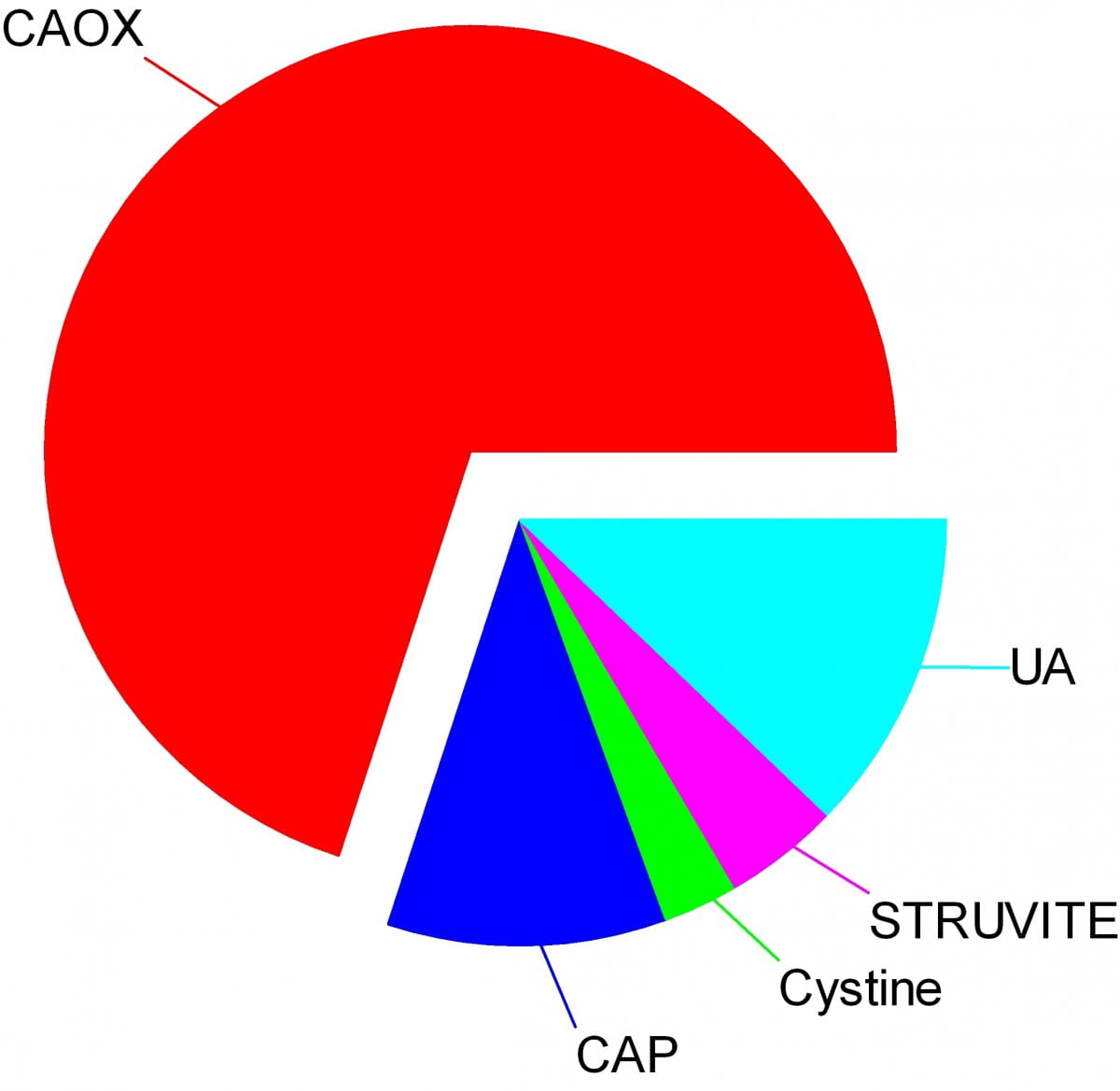
Crystals make stones and their names signify the kidney stone types. Here are the names of the crystals that make the stones: CAOX, Calcium Oxalate; CAP, Calcium phosphate; UA, Uric Acid; Cystine; Struvite.
The wedges on my pie chart show the relative abundances of stone types in our large population of stone forming patients. Calcium oxalate stones predominate by a wide margin in our clinic and in all others I know of.
The names, matter because the whole science of stone prevention focuses upon stone crystals. Each kidney stone crystal creates its own unique illness and requires specific treatment. That is why we name stones by the names of their crystals and why when stones are analysed the results are reported by these very same names.
Being a bold and rather large graphic, the featured picture does what I intended, brings the main facts into view as, at a circus, the great animals and the small animals circle the ring by way of an introduction. Come. I will show you all the common stones, like at a fashion show, or a circus parade. You can watch as they go by and remind yourself, or wonder, which ones might have been yours.
Here they are.
Which type do you have?
You might think your doctors know what stones you have formed, but don’t rely on it. People move, doctors move, health records are far from ‘all electronic’. That stone report from 4 years ago could lie in a dusty filing cabinet, your new doctors unaware it exists. Worse, it could hide in a dresser drawer and you forgot it you put it there. Perhaps even more worse, the stones might stay in that drawer, never analysed at all. Find the stones, find missing reports, urge analysis by your physicians. They can help you most if they know your stone analysis.
When they do not know, physicians can still mount prevention efforts but with less focus and probably less effect than when guided by a knowledge of the crystals. So always seek treatment. If a stone comes along the way, make every effort to get it analysed.
Why should you care to know all this?
Because you will conduct much of your own treatment, and over many years.
Since stones tend to recur, prevention requires treatment over long periods. These treatments work by altering urine chemistry in a direction that minimizes the risk of forming crystals. Such altering of urine chemistry requires control of fluid intake, lifestyle, and diet, and sometimes additional use of medications.
Just as the sailor who aims along a chosen track against the random, misdirecting, confusing sea and air maintains a constant way in proportion to that skill which comes from knowing the way of the boat, patients who aim to keep a certain kind of condition in their urine despite the demands and temptations of the world do so, I believe, in proportion to skills that come from knowing how their work and lives and foods affect their bodies, and how those crystals form which they so much desire to prevent.
Put another way, knowledge is power.
Why is this article so long?
I wanted to put all five main types of kidney stones. That makes a long story. But probably you will care to read about only your own type.
I should mention here, to save a lot of confusion, that stones often contain mixtures of crystals.
The pie chart refers to the most common crystals in a stone, for which the stone is usually named. Much of the time, minor crystal components are not crucial, but sometimes – to jump forward a bit – they are. Even a trace of struvite or cystine, for example, can have great diagnostic importance.
Calcium stones
Calcium Oxalate Crystals
In the great circle atop this page article, the calcium oxalate stone, being most common, occupies a lion’s share of the space. 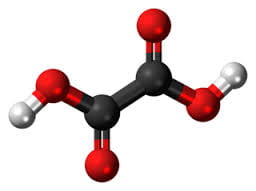
The calcium oxalate crystal forms when calcium combines with oxalic acid. Oxalic acid (at left), a dead end waste product that the kidneys remove, contains two carbon atoms (the large black spheres), four oxygen atoms, and two hydrogen atoms (silver).
At the acidity of urine, the positively charged hydrogens leave their negatively charged oxygens. As a result the oxalate molecule carries two negative charges. In the figure at right one negatively charged oxygen attracts the hydrogen of a nearby water molecule (H – O -H) while another attracts a positively charged calcium atom.
You can imagine how another oxalate ion (the name for a charged molecule in water) could attract the same calcium, or another calcium atom attract the bottom oxygen on the oxalate molecule so the chain extends and makes a crystal. You can see more about this in a video I made. Broadly speaking – though my more expert colleagues may bridle at such a simplification – the calcium atoms and oxalate molecules combine by the attraction of their opposite charges.
The calcium oxalate kidney stone comes in two varieties, calcium oxalate monohydrate and calcium oxalate dihydrate. The former are harder and therefore more resistant to fragmentation by lithotripsy. Likewise, the former appear more often when elevated levels of urine oxalate are present.
Calcium oxalate stone formers
From Systemic Diseases
Sometimes this kidney stone arises from a systemic cause, like bowel disease, primary hyperparathyroidism, or primary hyperoxaluria. Only physicians can establish that a known disease – like bowel disease – is the cause of stones. Only physicians can discover underlying primary hyperparathyroidism as a cause of stones. Patients cannot do much for themselves except provide as complete a medical record as possible.
Idiopathic
Most of the time this kidney stone arises simply from the interplay between inheritance, diet, and aspects of daily living. We call such patients idiopathic calcium oxalate stone formers, from Greek ἴδιος idios “one’s own” and πάθος pathos “suffering”.
Even though physicians discover the links between daily living and stone production, and select those changes that can prevent new stones, patients themselves must create and maintain those changes. I believe patients can so this in proportion to how well they understand what is needed, and why. When changes in daily life are not enough, physicians add medications, so even then patients remain active therapists for their own disease.
Stones usually form on kidney surfaces
About one million nephron units make up a normal adult kidney. The calcium oxalate kidney stone type does not grow in the tubules of the nephrons but ‘outside’ them, on the surfaces of the renal pelvis where final urine collects and drains through the ureter to the bladder. Here is a video that shows how they can form.
Calcium phosphate crystals
Phosphate ion and urine pH
Calcium phosphate stone crystals form when calcium atoms combine with phosphoric instead of oxalic acid and produce the calcium phosphate kidney stone.
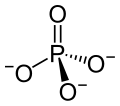 Phosphoric acid is simply a phosphorus atom (shown as the ‘P’ in the line drawing to the left) with 4 oxygen atoms bonded to it. One oxygen atom has two lines for its bond to phosphorus; this oxygen cannot provide any charge with which to bond calcium atoms to make a crystal. The other three have ordinary bonds that are shown by a line, and a dashed and solid arrow. These two arrows mean simply that the oxygens lie above and below the plane of the paper – so if you built the molecule with sticks and balls it would have a three dimensional shape.
Phosphoric acid is simply a phosphorus atom (shown as the ‘P’ in the line drawing to the left) with 4 oxygen atoms bonded to it. One oxygen atom has two lines for its bond to phosphorus; this oxygen cannot provide any charge with which to bond calcium atoms to make a crystal. The other three have ordinary bonds that are shown by a line, and a dashed and solid arrow. These two arrows mean simply that the oxygens lie above and below the plane of the paper – so if you built the molecule with sticks and balls it would have a three dimensional shape.
One of the three negatively charged oxygens never has a hydrogen on it in urine but only in exceedingly acidic solutions. A second charged oxygen is always occupied by a hydrogen atom in urine.
This makes the third oxygen, variably occupied by a hydrogen in urine, a tie breaker.
In a urine of average normal acidity (pH around 6), most of the tie breaker oxygens have their hydrogen leaving the phosphate ion only one negative charge. Not enough to make a crystal.
When the urine is abnormally alkaline (pH above 6.3 or 6.5), the variable oxygen becomes charged so the ion has two negative charges that can combine with calcium to make crystals. For this reason the calcium phosphate kidney stone tends to occur in people who produce a more alkaline urine than those who produce calcium oxalate kidney stones.
Brushite vs. hydroxyapatite
Much like calcium oxalate, calcium phosphate crystals begin simply as one to one pairings of doubly negative phosphate ions with doubly positive calcium atoms. This initial crystal is named brushite. Brushite, which is an equal mixture of calcium and phosphate ions, can convert to hydroxyapatite (HA), which has a more unbalanced proportion of calcium to phosphate. Hydroxyapatite crystals make bones hard.
Because less soluble than brushite, hydroxyapatite cannibalizes brushite. The organic molecules in urine modify this process.
Calcium Phosphate stone formers
From Systemic diseases
Primary hyperparathyroidism and renal tubular acidosis raise average urine alkalinity (higher urine pH) and foster calcium phosphate kidney stones. Many uncommon genetic diseases do the same.
Idiopathic
Idiopathic calcium phosphate stone formers share a common set of traits. Perhaps because urine contains far more phosphate than oxalate, they form more frequent and larger stones than idiopathic calcium oxalate stone formers. Often the stones originate as crystal plugs at the terminal ends of the kidney tubules. More crystals deposit over the end of the plug open to the urine, to make the final stone. Crystal plugs damage the cells that line the tubules and cause local scarring.
Uric acid stones
Uric acid crystals
Structure and charged sites
A breakdown product of DNA and RNA, uric acid forms crystals in abnormally acidic (low pH) urine. Obese and diabetic people, those with gout or kidney disease typically produce abnormally acid urine. I know how the urine becomes acid, but leave it for elsewhere on the site.
Uric acid, the molecule we are interested in here (shown to the far right), has two linked rings made of carbon atoms (they are at the angles where lines join), with  interposed nitrogen (N), oxygen (O), and hydrogen (H) atoms.
interposed nitrogen (N), oxygen (O), and hydrogen (H) atoms.
This molecule has only two charged sites, the nitrogen atoms at the bottoms of the rings. In urine of pH 6 or so, one nitrogen lacks its hydrogen and therefore carries a single negative charge. In more alkaline solutions both nitrogens lack hydrogens, but urine does not normally achieve such alkalinity (pH>8).
When urine pH is low (<5.5) and both nitrogens have their hydrogens, the molecule lacks any charged site, so water can no longer find a hold on the molecule. It crystallizes. It simply leaves the water as water droplets themselves form from the high and vaporous late afternoon clouds and fall from the air as the warm rains of springtime.
Relation to water
Water molecules are each a single oxygen atom (large ball) bonded with two hydrogen atoms (small balls) as in this picture from Wikipedia. The hydrogen side has a positive, the bare side of the oxygen a negative charge. So water molecules link to each other, 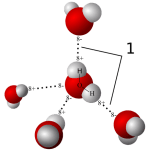 positives to negative surfaces, to make up the clear and seemingly continuous fluid we drink, swim in, and hold up umbrellas to keep off of us when it rains. They link by charge at angles, shown by the number ‘1’ so as to make up a three dimensional macrame.
positives to negative surfaces, to make up the clear and seemingly continuous fluid we drink, swim in, and hold up umbrellas to keep off of us when it rains. They link by charge at angles, shown by the number ‘1’ so as to make up a three dimensional macrame.
To be ‘in solution’ means to have some charge to which water molecules can link up with by attraction. Calcium atoms are positive and become surrounded by a shell of water molecules facing it with their bare negative surfaces. Oxalic and phosphoric acids have negative charges and are surrounded by water molecules pointing their positive or hydrogen sides to them.
Uric acid at neutral pH has its one negatively charged nitrogen water can grasp. But when pH falls, and neither nitrogen has any extra charge for water to bind with, how can the molecule remain among the water molecules? It cannot. The molecules stack into solid crystals and fall from solution.
Uric acid stone formers
The stones can be orange – red, large, and numerous
The stones can be red or orange because uric acid crystals absorb hemoglobin breakdown products that are red – orange pigments in urine. Sometimes uric acid crystals pass in urine as a red orange gravel.
Uric acid does not have to connect itself to some other atom or molecule to make a crystal, in the way that calcium must bond with oxalate or phosphate ions to make calcium oxalate or calcium phosphate crystals. When pH is low enough to extinguish its charge, uric acid can crystallize very fast, in seconds, and pass as an orange gravel in the urine. If retained, such crystals can grow rapidly into large stones. Because there is much more uric acid in urine than there is oxalic acid, uric acid stones can grow very large and rapidly. Some fill up the entire collecting system of the kidney.
Urine pH controls stone formation
But because the whole process depends almost completely on the acidity of the urine, uric acid stones are very easy to treat. Just a modest amount of supplemental alkali will make the urine of almost any patient alkaline enough that the hydrogen atoms are removed from the one crucial charged nitrogen. Water can bond there so uric acid remains in solution. Because so simple, treatment prevents stones with certainty. Relapse need never occur.
Mixed stones require special care
Unfortunately, however, stones commonly contain uric acid mixed with calcium oxalate. In this case, one needs to track down the cause of the calcium oxalate stones as well as make the urine alkaline enough to stop uric acid stones from forming. Calcium phosphate crystals mix with uric acid only rarely, because it takes a rather alkaline urine to remove the hydrogen atoms from phosphate so it has two negative charges and can bind efficiently with calcium atoms. At that higher pH, uric acid will have its charge site and remain in solution.
Struvite stones
Urea and the planet
Kidneys cannot make struvite. Bacteria make it. Not all bacteria, either. It takes bacteria that normally thrive in the soil, and they do it for ancient and compelling reasons. These bacteria produce the kidney stone named Struvite after Heinrich Christian Gottfried von Struve (1772–1851).
Animals deposit urea (at left) all over the planet when they urinate. Plants cannot use it.
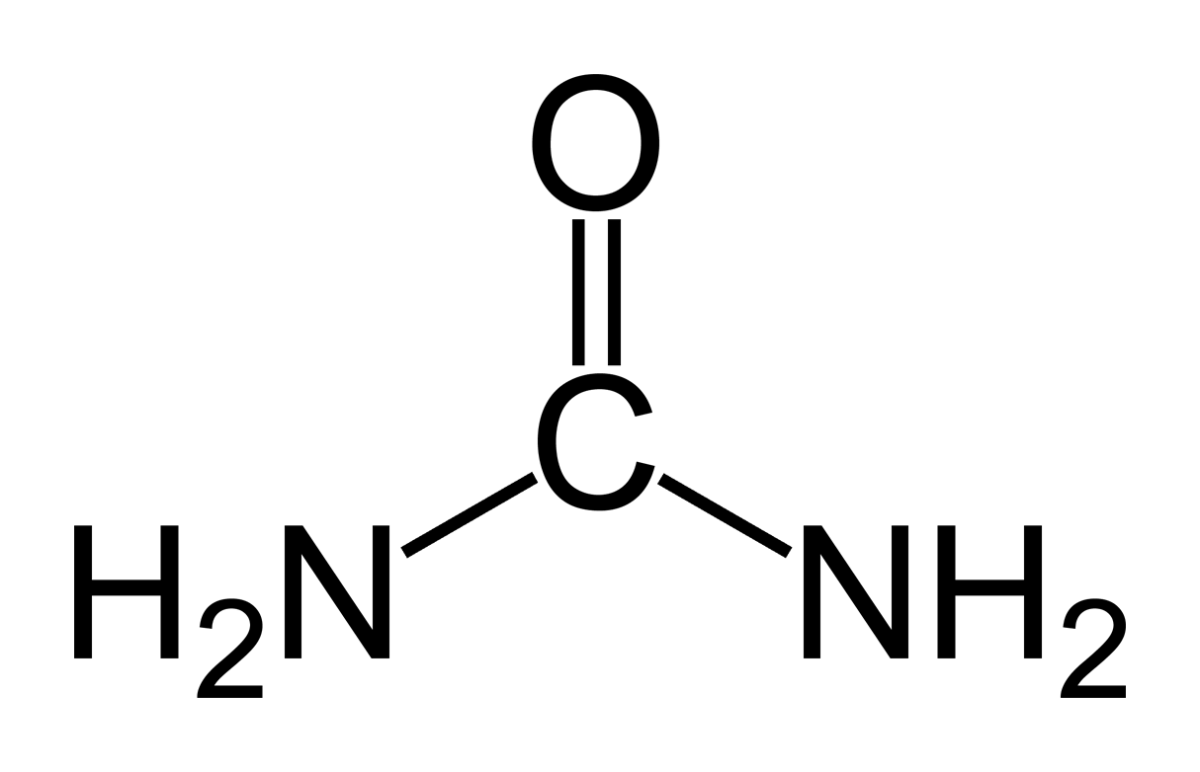 Like oxygen, nitrogen is an essential for life yet dangerous. It is integral to proteins, DNA and RNA. As these molecules are broken down and remade, some of their nitrogen slips by and can form poisonous compounds unless caught up in safe waste products. Of these, the main one, urea, contains 2 nitrogen atoms bound to a single carbon atom (‘C’ in the picture to your left).
Like oxygen, nitrogen is an essential for life yet dangerous. It is integral to proteins, DNA and RNA. As these molecules are broken down and remade, some of their nitrogen slips by and can form poisonous compounds unless caught up in safe waste products. Of these, the main one, urea, contains 2 nitrogen atoms bound to a single carbon atom (‘C’ in the picture to your left).
Uric acid contains 4 nitrogen atoms (look back at the picture of it). Birds and reptiles excrete most of their nitrogen as uric acid; mammals like us excrete nitrogen mainly as urea.
As the animals of the world urinate on the soil, their urea brings nitrogen to plant roots, but the plants cannot use it. They cannot release the nitrogens from the carbon atom that holds them. Those soil bacteria that make struvite crystals have an enzyme, called urease, that can release the nitrogen for plants to use as their nitrogen supply.
So, soil bacteria with urease maintain the nitrogen cycle of the earth.
Struvite crystals
As they release nitrogen from its carbon in urea, the nitrogen takes up a proton making ammonia (NH3). Ammonia is a powerful alkali and takes up another proton.
As it does so, the working bacteria surround themselves with spheres of very alkaline fluid enriched with ammonium ion (NH4) that carries one positive charge. Soil magnesium ( an atom with two positive charges) and phosphate sans all of its protons (an ion with three negative charges) spontaneously form their triple salt: three negative phosphate charges, two positive from magnesium, one positive from NH4).
The crystals anchor the bacteria and help create a porous nitrogen rich soul good for plants to grow in
The struvite kidney stone
Why they start
Because urine is filled with urea, soil bacteria that get into the urinary tract can break it down to ammonia and create struvite from the magnesium and phosphate urine always contains.
You might wonder how soil bacteria get into the urinary system.
Because we eat them, with foods that are not cooked, and they become part of the intestinal bacterial population from an early age. In us and around us, they find a way into the urinary system, especially in women whose shorter urethra makes entry easier. No matter how skillfully used, any instrument put into the bladder can carry our personal soil bacteria with it.
What they do
Because they live among molds and fungi, soil bacteria easily mount resistances to antibiotics, so antibiotics given for a urinary tract infection will tend to kill sensitive bacteria and select out those that can resist them.
Soil bacteria can produce struvite stones de novo, or infect calcium stones to produce a mixed stone. Either way, struvite stones are infected by their very nature. They can become huge. Their bacteria can injure the kidneys, even enter the bloodstream and cause sepsis.
Treatment is a mix of thoughtful surgery and selection of antibiotics after such surgery to kill bacteria that remain. If the stones are a mixture of struvite and calcium crystals, new calcium stones need to be prevented.
Cystine stones
Inherited kidney abnormality
 Lemon yellow with a sugary coating these form only in people who have an inherited kidney disorder called cystinuria.
Lemon yellow with a sugary coating these form only in people who have an inherited kidney disorder called cystinuria.
Although the kidneys function well, they permit abnormal amounts of four amino acids to enter the urine. Three do not matter that we know of. The fourth makes crystals and the cystine kidney stone type.
Cystine
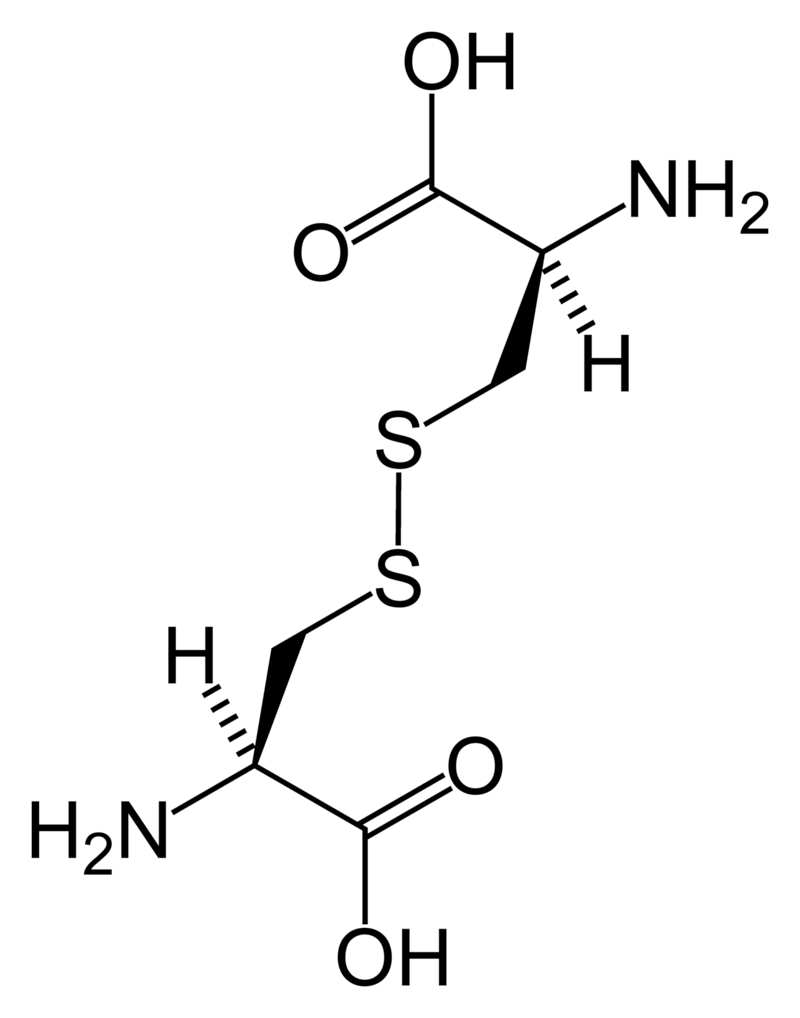
Cystine (left) forms through the coupling of two identical amino acids – called cysteine – through their sulfur atoms (‘S’ in the line drawing).
Each cysteine contains two carbon atoms – not shown except as corners – bonded together (shown by the single long line that connects the two corners) as in oxalic acid.
One carbon atom has 2 oxygens bonded to it; the other has one nitrogen (which makes it an amino – nitrogen containing – acid), a hydrogen atom, and a sulfur atom. As for phosphate, the dashed and solid arrows simply mean the hydrogens and sulfurs lie above and below the plane of the page and a stick model would have a three dimensional shape.
Cystine Crystals
Cysteine itself is very soluble because the sulfur atom has an appreciable negative charge.
But the big, long cystine molecule has very little charge because the sulfurs bind to each other. So, like uric acid, cystine loses intimacy with water molecules and simply leaves the solution as crystals. Also like uric acid, the process is fast.
Cystine stones
Because people with cystinuria lose large amounts of cystine in their urine stones readily grow large, and fast.
Stones probably form in the urine itself. But cystine crystals can plug the ends of kidney tubules, as calcium phosphate crystals do, causing cell damage.
Since cystinuria is an inherited disease, stones may begin in childhood.
Effective treatment always requires very large amounts of fluids to dilute the urine. The few effective drugs resemble cysteine. Their sulfur groups bond with cysteine to form a ‘mixed disulfide’ more soluble than cystine. But their side effects can limit use.
Rare stones
Here and there we find patients who make uncommon crystals and require very special care.
Uric acid, as an example, can form odd crystals such sodium or ammonium acid urate, especially in people with bowel disease and chronic diarrhea.
Anti-viral drugs can crystallize in urine and form stones only recognized for what they are through stone analysis.
Very rare disorders of metabolism can produce molecules which crystallize in the urine, for example 2-8 dihydroxyadenine.
Although it can take a while before the right answer emerges, stone analyses will put physicians on the right track for these special cases.
The end of a very long post
That’s my parade.
The common animals and the rarer animals have gone by, and you have glimpsed the main ones, big and small.
The one point is what it was at the beginning. Each kind of kidney stone has its own ways, and treatment requires we know which one you have.
Likewise, for whatever that one may be, it is good to know as much about it as you can know. For long term prevention of stones is hard to come by and ultimately what the patience and and consistency of patients themselves matters most.
If you don’t know which stones you have made, find out.
Track down old reports and pull them together.
Keep copies and send everything to the doctors who care for you.
Fred Coe MD


Dr. Coe, I was a patient of yours in 2007. You determined that my stones were caused when my kidneys were low on fluids, which was common in my lifestyle of being on the road a lot. You felt that if I kept my kidneys flush and drank constantly all day, I would not continue to produce stones. I am reporting in that 7 years later, after having a couple incidents of passing small stones, my last MRI showed no signs of additional stone production. You can imagine that I have endured (though not strenuously) comments about my constant glass-in-hand lifestyle, but I am used to the regular bathroom visits and the constant hydration. It is just fine!! When I brag about being stone-free, some say, “that is because you are the only person on the planet who actually listened to your doctor!” And they may be right. Anyway, keep up the good work, I am looking forward to reading your posts.
Dear Nancy, On reading back over some of the site – I am forever editing it – I noticed you mentioned an MRI used to number your stones. I think you must have meant CT scan as MRI scans do not generally show stones. Let me know, Fred Coe
I just found out the my kidney stones were a mix of Calcium Phosphate and Struvite stones. I do not have an UTI so how did I get a struvite stone and how can I prevent future struvite stones? Thank you!
Dear Leanne, A common way to get an infection is during stone removal procedures, and these can be silent. If your stone is indeed struvite, even in part, it is almost certainly due to infection. The calcium phosphate component is not from infection, and indicates you have some primary underlying stone forming problems that would benefit from diagnosis and treatment – if this has not already happened. Of concern, stone analysis labs have had some of their worst difficulties in ascertaining struvite in stones HOW BAD IS KIDNEY STONE ANALYSIS? so perhaps your physician might want to be sure the laboratory is confident. Urine cultures for bacteria that can produce struvite are important – they possess the enzyme urease. If stones have been removed perhaps they were cultured. Fred Coe
Hello. I am having more stone problems the past few days. I am trying a home treatment of equal parts lemon juice and EVOO. I peed about an hour ago and strained it. I had 6 chunks in my pee, larger than my last episode. I will take them into my Dr. to have them analyzed. Stupid question: How “fresh” do they have to be. I don’t want to take in my stones to have tested and get a false reading. Thank you!
Hi Leanne, Stones will keep for years. Just send them in and have them analysed. Likewise, be sure you collect 24 hour urines to find out the cause of the stones and stop forming them. Regards, Fred Coe
Hi Dr. Coe, I am writing to ask for any suggestions for my son. He is 20 and he has a burning sensation when he urinates, now a year later, also when his bladder is full and he urinates. We are now at our 2nd Urologist trying to find the root of the problem with, so far no luck. A friend of mine (who is a nurse practitioner) said he remembered a patient with similar symptoms 20 years ago coming into the ER and it turned out that he had Cystine stones. We have just had a CT scan yesterday and are waiting for the results to be called into the doctors office. My son has had a syscoscopy and been checked for all std’s in the book, all coming back clear. Our recent Urologist has given my son a second course of medicine to calm the bladder and see if this helps. He has no visible blood in his urine and no pain any where else, only the burning. I am writing to see if you have any other suggestions as I truly believe 2 heads are better than 1! or if you think it could be one of the stones you have mentioned above. Thank you in advance for any help or suggestions.
Dear Natalie, of course my remarks are of a general nature as I have no real knowledge of your son’s actual medical situation. The very thoughtful nurse you mention observed similar symptoms in a patient with cystinuria because such patients can form crystals which are not detected easily but produce urinary tract symptoms much like infection. In fact, many of the more common calcium stone conditions do the same: produce masses of crystals which mimic infection and are very hard to detect. The lack of bleeding is a bit against the idea of crystals which typically cause slight bleeding. Even so, I suspect your son’s urologists are very aware of what crystals can do and have looked for them in the urine during what must have been many microscopical examinations of his urine. An alternative is what has been called ‘non – specific’ urethritis, an entity all urologists have encountered and presumably does not fit the picture your son presents. If there are no crystals identified and the symptoms persist, one can measure a 24 hour urine and look for obvious high supersaturations from high urine calcium, abnormally high or low urine pH, or even high urine oxalate. Some people who have high stone risk begin with crystals and symptoms and later begin to form stones.
Hello Dr. Coe,
I am a 21 years old female who has been getting known kidney stones since I am 15 and they just seem to be getting worse. I have been to several urologist and so far we have no answers as to why. February and March of 2015, I had a total of 5 surgical procedures including a couple of stents, lithotripsy, and stent removals. About 3 weeks after the final procedure I ended up with a severe infection and was placed on Cipro 750 for 15 days. After completing the antibiotics the infection returned again and was placed on Augmentin 500 for a few day, which was interrupted by a numerous kidney stones causing hydronephrosis. I passed 2 rather large stones, 1 being 12 mm. I still had a stone blocking so I ended up going back in for another stent and the doctor removed all the other stones. 24 hours after the stent was placed, I ended up with a 103 temp and was admitted into the hospital for lots more antibiotics and after 6 days of IV antibiotics I was sent home, only to find out a few days later, the infection was still there, so I was placed on 3 other antibiotics orally. Finally after a month with the stent, it was removed and it was reported that I already have stones crowning. I have been on antibiotics for 52 days now and have another week to go before I can stop taking them. The infection was enterococcus facalis. Now, I finally got the report of my stone analysis and it came back UNKNOWN!! (that was from the 12mm stone) I am at lost for what to do next and am desperate for help! Do you have any idea what an unknown kidney stone could be? Do you suggest a specific type of doctor in the PA,NJ,NY surrounding areas?? I need to get these stones to stop and get back to being a normal 21 year old pain free again!
I should also include, I eat all natural foods and drink TONS of water. atleast a gallon a day!!
Dear Catherine, This sounds like a terrible and frustrating experience. Sometimes stone analysis does come back without identification of the crystal types, and such results pose real difficulties in prevention. I am sure your physicians are doing what they can under these difficult conditions which are not rare – recurrent stones, infections, stents and the like. It is most important to maintain contact with them and preserve continuity of care. The specific type of doctor you need is a urological surgeon who is experienced with stones, and it sounds like you already have one who has performed your procedures. Fred Coe
Dr. Coe,
My first incident with stones was in 1975, ( I was 22) and was told that I deeded to stay away from anything that had soy products in them. The best I can determine is I probably have always been producing the calcium oxolate type. I have made changes in my life by dropping as much calcium (milk, cheese, ice cream) as is humanly possible in today’s world, but I seem to be plagued by having a stone at least every other week. There was aerial of about 10 years I did not have a noticeable recurrence, but they returned. I am going to be discussing this with my primary physician on my next visit, but the last stone analysis ( June 30) reported calcium oxalate mono hydrate : 75%, calcium oxalate dihydrate: 25%. I worked for 18 years as a medical center chaplain, so along the way I picked up a lot of info for life, and a desire to by proactive in my health, so I have been exploring everything from magnesium to thiazides to potassium citrate to add to my diet. Give me something, please to discuss with my doc. Thanks ever so much!
Hi Mark, I gather that you have about 25 stones a year and have been forming them at this rate for some time. Given the stone composition I think you may have idiopathic hypercalciuria (genetic high urine calcium) partly treated with low calcium diet and the diet is increasing your urine oxalate. You need to review the results of your 24 hour urine studies. If you have hypercalciuria the low calcium diet poses a risk for bone mineral loss and later life fracture, and so it is not a good idea. The site has a lot of material on how these studies are used, although the hypercalciuria parts are just being written. Take a look at the latest ‘walking tour’ which is pretty good as a review. So, it is not just any treatment but proper diagnosis you need, which, if it is done right will lead to effective treatment. Best, Fred Coe
I did not tell you I have been dx with osteoporosis in my spine (inherited from my mother) . I never thought that this could be a factor in kidney stone production.
Further I am a diabetic, no treatment using only diet. Cholesterol is fantastic however. I am “O” negative with a negative Lewis factor, which I believe is a benefit to cholesterol issues. I have high blood pressure however, taking benazepril 20 mg, BID. I also take 2400 mg of ibuprofen daily for the pain associated with the back issues.
Hi Mark, This is in reply to both additional comments. From the osteoporosis diagnosis I am more sure that you have idiopathic hypercalciuria and that low calcium diet is not the proper treatment. You need to review your 24 hour urine values and get proper treatment along with a high calcium diet and something for your bone disease. There may be other factors as well. Diabetes is a cause of bone disease, for example and sorting out the effects from my presumed hypercalciuria and from diabetes is what your personal physicians must do. I am sure they have already thought about virtually everything I have said, incidentally, and urge you review all this with them so they can get you proper treatment. Regards, Fred Coe
Dr. Coe,
Thank you for the very interesting post and taking time to respond to so many of the comments.
I was wondering if you know of any proven correlation between cloudy urine (not caused by UTIs, blood, etc.) and later development of kidney stones. I know cloudy urine can be a symptom of kidney stones, but that’s not really what I’m interested in.
I have calcium oxalate stones, which raises my concern about kidney stones, but my concern is actually about my daughter who has fairly frequent cloudy urine. I had cloudy urine occasionally before I knew about my stones and started drinking about a gallon of fluids a day. It seems much less common now. It has always seemed likely to me that, if whatever was making the urine cloudy was a crystaline substance, it could probably also form larger crystals and eventually kidney stones. Can cloudy urine be a real danger sign for later development of kidney stones and would a standard urine test reveal what substance was making the urine cloudy? If it was calcium oxalate or calcium phosphate, I would be pretty concerned.
Of course, I’m already nagging her to drink more water and we will also discus this with her pediatrician.
Thanks for any response you can offer.
Hi Domenico, What a wonderful question! So far as I am concerned cloudy urine in stone formers is usually crystals, and the crystals are more often than not calcium phosphate. A very common reason in children and young adults is genetic (familial) hypercalciuria, a condition of high urine calcium excretion which leads to stones and can cause crystal formation in even children. Pain and hematuria are common with crystal passage, as well. Now that I think about the matter, I have never put up an article on this topic and will do so when I get the chance. High fluids are great, but if there is indeed hypercalciuria there is more to consider. Such people are at risk for loss of bone mineral so diet calcium needs to be ample – 1000 mg from food – and high fluids, and low sodium intake (1500 to 2000 mg daily to lower urine calcium most advisable. Her pediatrician will know about hypercalciuria. I presume you have it as well, and probably are being treated. The site has not as yet gotten so far as hypercalciuria but soon will. Thanks, Fred Coe
Fred,
Thanks so much for your quick and thoughtful response.
I’m actually not sure if I have hypercalciuria. My last 24-hour urine test showed a total calcium during the test of 148 mg, but that same lab result showed a total sample size of 1856 ml, which I know to be wrong. The roughly 1-gallon collection jug was essentially full. I understand the sample volume is calculated form the concentration of a tracing compound that is added to the jug. I have no idea how the lab could have gotten the concentration of this compound wrong, but I have no doubt that it did. My sample was far in excess of 2 liters.
But even if I assumed a sample size of 3.75 liters (almost a full gallon), if the concentration of calcium, was measured correctly (8 mg/dl), that would translate to 300 mg of calcium, which I understand to be the high-end limit of what is considered normal. So, I’m not certain what my calcium output was on that test.
I have had at least one prior 24-hour urine test, but I don’t have the results of that test at hand. My current treatment is potassium citrate, lots of water, and dietary adjustments to avoid dietary oxalate.
I will talk to my daughter’s pediatrician and ask that he test her urine for hypercalciuria. I don’t want to project my health issues onto my daughter, but my history does make me concerned that I may have passed on a hypercalciuria or some other trait that may give her a propensity for stones.
If nobody has ever studied the relationship between cloudy urine containing crystals of calcium phosphate, calcium oxalate, etc. and later development of kidney stones, it would seem worth studying as a possible early warning sign to detect people who may need to take steps to avoid stone formation. I certainly would have appreciated some warning before my first episode with passing a stone, which was very painful and pretty scary when I didn’t know what was going on.
Perhaps testing for urine calcium levels serves much of the same purpose, but I did have cloudy urine previously and asked a GP about it. I was told to drink more, but not to worry about it and, if anyone ever tested calcium levels in my urine, I never heard that they were abnormal before my first stone. If the cloudy urine I first noticed about 20 years earlier could have served as a warning, that would have been very helpful for me.
I guess we’ll never run out of medical questions to research and this may not be the most important unanswered question out there, but it’s certainly one I’d like to see answered.
Thanks again for your helpful response to my questions. This site is a wonderful resource for people with stones. I was particularly intrigued by your colleague Jill’s post indicating that tea consumption correlates with a lower stone risk. I have been told to avoid tea because of its oxalate content, which is a shame because iced tea was one of the drinks I had been using to break up the monotony of all the water I drink.
Nico
Hi, You are hypercalciuric; values of 300 mg/day are quite high. Older criteria such as above 300 mg/day are passing out of use. Crystals in the urine are a famous clue to stones, and crystalluria with hematuria a commonplace childhood syndrome, so my first reply was perhaps not clearly worded. The very same supersaturations that produce crystals can produce stones. You should have your bone mineral density measured as hypercalciuria can lead to reduced bone mineral and long term bone disease. Regards, Fred Coe
Thanks again. I just got the 300mg number off of the test report as the high end of the normal range. I appreciate your advice that 300 mg is actually problematic.
I wish the GP I saw decades ago had warned me of kidney stone risks or checked my urine calcium levels when I came to him to ask about my cloudy urine, but that’s water under the bridge. I’m glad I now know to treat this as a danger sign in my daughter and can have urine testing done to see if any further steps are needed to help minimize her risks.
As for my bone density, I believe that was checked and the results were not troubling, but I will confirm that with my doctors.
You and your colleagues should be proud of this site. Making this information available really does help make the world a somewhat better place.
Hi, I am glad your bone density is normal, but be sure that it is not reduced. Your daughter should be checked; for a start the urine can be looked at under a microscope to determine if the cloudiness is indeed crystals and what the crystals are> Crystals have characteristics one can identify. As for the site, I am happy to know people benefit from it. The goal was to make information at a high scientific standard available to anyone who want it. Best wishes, Fred Coe
I too had cloudy urine, and back in March I was told it was nothing, and cloudy urine is insignificant. However, when I brought a cloudy sample to my urologist, he confirmed there were calcium phosphate crystals ++. Litholink showed me what other doctos said about my cloudy urine was wrong, because apparently I have 329mg/d of calcium in my urine and my CaP SS is 1.17. If it weren’t for the warning from the cloudiness and help from Litholink I would never have known. I agree, cloudy urine without UTI should be considered to be caused by crystals.
Now, I’ve noticed, when drinking plenty of fluids and maintaining a urine ph <7 I don't ever have crystals. Does this mean the stones will likely be prevented?
And do you think my daily urine calcium would be problematic for my bone density?
I also notice that many things I have read regarding urine calcium state that values are for a normal calcium diet. During my testing time I definitely ate well over 1,200mg daily of calcium. Could this affect results?
Thank you Dr Coe for everything you do, and I thank Litholink for all the information and education!
Joe
Hi Joe, Yes you do have hypercalciuria and with a high pH are forming phosphate crystals. Keeping fluids high throughout the 24 hour day and night is helpful; reducing diet sodium is an additional help. The high calcium intake from food is a good idea, and I would continue that habit. If you notice the Curhan data for stones vs. urine calcium were collected over a range of people and presumably diets, and above 200 mg/day seemed to increase risk. As for bone, I would have a mineral density measured; it could be reduced. The site will take up sodium as a treatment for IH, and later on the drug trials, but for the moment I am afraid the pace is a bit slow – mostly just me writing these. Regards, Fred Coe (PS By the way, I founded Litholink in 1995 and we sold it to LabCorp in 2006.)
Sir, I have stones from past 4 years. I recently removed one of them through URS . And tests showed that the stone was 90% calcium monohydrate and 10% calcium dehydrates. What all should I avoid eating…
Hi Sushil, 90% COM is not a rare stone, and compatible with high urine calcium or oxalate, or low volumes; you would need 24 hour urine testing, which is advisable. Your personal physicians may have already done this, or surely could. Regards, Fred Coe
Dear Dr. Coe – I am a 46 year old female diagnosed with MSK. I have numerous stones in both kidneys. In 2008 I passed a 5mm stone, and in early 2010, I had lithroscopy with a stent for a 10mm stone. I most recently passed a 6mm stone (on 12-August-15) and still have some discomfort in the right flank area. All 3 of the mentioned stones were in the right kidney, and caused moderate to severe hydronephrosis. All stones were Calcium Phosphate. I currently have a 8mm in the right renal pelvis. My questions are: Since all of my attacks have been acute and extremely painful, is there anything more proactive that I can do about this systemic condition? (My urologist has not suggested any dietary changes, or medications, or any surgeries). I feel like I am just sitting around waiting for the next urgent trip to the ER. Thank you in advance for any counsel/suggestions you may be able to provide.
Dear Catherine, you are certainly right in asking, and I am happy to tell you that prevention of recurrent stones is why I put up this site and what I have devoted my professional career to the fostering of. The central problem in stones is the crystals, and your crystals are calcium phosphate. That means your urine is too saturated with respect to calcium phosphate. Very high fluids – throughout the day and even overnight – are a start. If your urine calcium is high, reduced salt intake is valuable, and medications are also available – your personal physicians surely can provide these for you if fluids and reduced sodium are insufficient. Regards, Fred Coe
Hi,
I am so impressed with your articles and the fact that you take time to respond to questions. It is much appreciated!
Over the past year, I have had a relentless UTI. I had been on six different antibiotics, some of them twice. I had surgery right before they started, and the doctor thought that I had a hospital acquired UTI because cultures showed that it was resistant to most antibiotics. A few months ago, my doctor put me on a strong dose of ampicillin for 10 days. I use test strips at home, and since then, it has been much better. The leucocytes never clear up entirely, but they are now much lower and I rarely have symptoms.
A few weeks ago, my doctor referred me to a urologist because we thought I had a kidney stone. I have had 8 or so of them over the past 20 years. In the meantime, a CT scan showed that I did have a kidney stone, but it was high up in the kidney and non obstructive. They also found a cyst on my ovary, which appears to be the cause of the pain.
When I went to the urologist, I told him that I have had blood in my urine. He did find trace amounts that day, and he did a 24 hour urine collection. The abnormal ranges were total urine volume (7.1), calcium oxalate (3.1), brushite (4.87), and sodium urate (2.89). Since then, I continue to have blood in my urine. For the past several days, it is cola colored about 50% of the time.
I appreciate any advice you can give me.
Thanks!
Sorry, just noticed an error in my post. PH urine is 7.1, total urine volume is 1.08.
Hi Colleen, I guess you have high SS with respect to calcium phosphate (3.1 is quite high), and in part this arises from the high pH of 7.1 and the remarkably low urine volume of 1.08 liters. You do not mention stone composition but that is important as your urine is also supersaturated with respect to calcium oxalate. You also do not mention urine calcium or oxalate levels. Certainly the bleeding can reflect crystals and stones, and even more certainly you need a urine volume above 3 liters a day. That alone should benefit you greatly. But the other issues – stone type, other urine abnormalities, and also very important. Likewise for your serum calcium level. Regards, Fred Coe
Thanks for your response. I have not had any stones analyzed, so I don’t know their composition. Urine Calcium was 176, Urine Oxalate was 28. Both of these were listed as in range. Other results listed that were also in range were Uric Acid Urine (495), Citrate Urine (555), Sodium Urine (76), Sulfate Urine (407), Magnesium Urine (89), Potassium Urine (26), Creatinine Urine (1187), and Uric Acid (.19). Would you be able to venture a guess as to stone composition from these numbers so I can hopefully make dietary changes to help? I know that I do not drink enough. I try and try, but cannot seem to do it.
Hi Colleen, Your urine sodium is in a good range, your urine calcium is just under the stone risk threshold of 200 mg/day, so high urine volume – above 3 liters a day – would be an excellent alternative. Your urine potassium is low, incidentally, suggesting you could use more potassium rich foods. The urine sulfate looks wrong – can you be sure? What are the units? As for the stones, calcium phosphate is a good guess. If high volume – with some attention to overnight – is not enough to stop stones, your physicians might want to consider medications. Regards, Fred Coe
Thanks for the info. You are right – Urine Sulfate is 6, Phosphorus urine was 407. I appreciate your help!
Hi Colleen, I thought so. Given your creatinine, phosphate, potassium and sulfate, you might bring to your physician the question of whether your diet is ideal; rather low values for potassium, phosphate and sulfate may indicate some value in re-adjusting your proportions of protein, carbohydrates, and fats. This requires your own physicians, who know your entire medical situation. Regards, Fred Coe
Thank you again. It is obvious that you are a doctor who really cares, and it is much appreciated.
Dear Dr. Coe,
Thank you for this very helpful and interesting article. I think I have already told you that I do have Comindation of calcium phosphate (brushite) and calcium carbonate-phosphate (apatite). What exactly does the brushite and apatite mean? I had an endo once tell me that one of them are older stones and one is just formed? Is there any truth to this? Also I have had 9 litho and my urologist is now telling me that litho is not viable for me any longer that only ureteroscopies will be best. He did go into the calyx last two times and said it was very very successful and he removed 20 calcifications in each kidney. Now I am wondering if it would be worthwhile to investigate if he could go into the belini. I have had him as my only surgeon since my msk was diagnosed. Thank you for your consideration.
Yours,
Laura
Hi Laura, Brushite is a specific form of calcium phosphate, and hydroxyapatite is another form, just like in the article. CLinically brushite is a special problem because the stones are very hard and do not fracture well with lithotripsy. What you have is typical of our published experience with brushite stone formers: Lots of stones, hypercalciuria, an alkaline urine pH. We have some reasons to believe lithotripsy itself may foster more brushite stones, but have not proven it; so I agree with your urologist about the value of ureteroscopy as an alternative. Unroofing plugged bellini ducts is purely experimental, there are no trials, and it is an invasive procedure because you are damaging papillary tissue. It is not taken lightly here at CHicago or Indianapolis our sister institution. The key is proper prevention and the site has a lot about that already: Really high and steady fluids above 3 liters a day. lowering of urine calcium aggressively using low sodium diet and medication. Potassium citrate is a questionable treatment right now as it could improve or worsen things. From prior comments you have sent I am not convinced that all elements of prevention are in place and being pursued to their maximum and I urge they be. Incidentally I am virtually certain you do not have medullary sponge kidneys. We found a very different picture in our cases. You have nephrocalcinosis from calcium phosphate stones. For example, tubule plugging as you have described is uncommon in MSK. Instead there are the massive numbers of tiny round micro-stones in dilated ducts. Take another look at the MSK article. Regards, Fred Coe
Dear Dr. Coe,
I am trying to increase my water intake everyday but I normally can only get two litres in I will shoot for higher amounts. I am going to investigate with my surgeon next visit (Sept. 21st) the MSK/tubular plugging. I also need to add that I have chronic perpetual infections and chronic flank and back pain. My family doctor is now having me do urine catches frequently he wants to see if what I say is actually what is going on. I believe I have an ongoing infection that never goes away. I have been on antibiotics more on than off during the last 8 years. I have become septic about 5 times or more over the years. I was also on Macrobid for about 3 or 4 years but it stopped working and my bug changed from ecoli to enterococcus. Then I went on an estring (my endourologist put me on this) and for two whole years the worst of the infections was kept at bay. Now that stopped working also. My endourologist does not want me to go on prophylaxis again. Now I am on and off amoxicillin constantly. It does not seem to be killing this bug. So my doctor wants me to do repeaded urinalyisis before and after each episode. He gave me a standing order years ago for urinalysis, stone analysis, and KUB. So if I feel the need for any of those I am able to just scoot off to the hospital. Big time saver. As you can imagine this is a very time consuming disease. Please tell me what is the strongest one thing that gives you the opinion that I do not have msk? And have you seen patients and given them a different diagnosis than msk? Can you have chronic pain with tubular plugging and nephrolcalcinosis?
Thank you very much for your time,
Best regards,
Laura
Hi Laura, The infections are such a problem and hard to control once stones themselves become infected – which sounds like what has happened to you. The MSK issue was raised by Celia, and it is this: MSK is not just calcium in the kidneys but a developmental abnormality of the kidney in which tubules are not often plugged as they are intrinsically dilated because never made properly. They fill with huge numbers of fantastically tiny stones that are not at all like what is found in ordinary calcium phosphate stone formers. The very shape of the papillum is abnormal. The source paper has great pictures some of which we copied into the article linked above. My focus would be on preventing more stones. If you have infected stones your surgeon might want to remove them via ureteroscopy if possible, but that may be inappropriate – as I have no real medical knowledge of your situation I cannot comment intelligently about the proper choices. Regards, Fred Coe
Hi Fredric, the fact that Laura’s stones are both apatite and brushite, could this mean that the brushite stones are formed on top of Randall’s plaque made of apatite where brushite crystals form on top? As in calcium oxalate stones that form on top of plaque made of apatite? According to studies by G. Gambaro and team on The Origins of Nephrocalcinosis, Randall’s Plaque and Renal Stones (published Sept 2009) “Randall’s plaques are frequently observed with idiopathic calcium oxalate stones, plaques are apatite structure, we propose they are an example of nephrocalcinosis” a phenomenon that has existed since the beginning of medicine, Egyptian and prehistoric times and which when you think of it, actually means calcifications of the kidneys (nephro for kidney is Greek; calcinosis for calcifications). Laura was definately diagnosed with nephrocalcinosis as well as MSK. Considering that stones are also a form of calcifications, in your opinion, could all parallel forms be caused by the same mechamisms? All due to some sort of initial cell damage? And if Laura has already had two ureteroscopy procedures, the ureteroscope also used to provide video images, would the Urologist not have been able to establish whether Laura actually does have MSK dilated tubules or not? We have not seen the images ourselves so have no way of knowing! If we could see the images, would this help somehow to understand? Thank you Fredric!
Hi, Celia; as usual you have outstanding questions. Brushite and apatite stones are the two common kinds of calcium phosphate stones we see, and we have published our work on both. Neither forms on plaque to any extent. Plaque is a form of calcium deposit in the renal interstitium, and therefore a calcium deposit in the kidney tissue. Strictly speaking it is therefore nephro (kidney) calcinosis (calcium) but the word has no real meaning. Plaque does not seem to cause inflammation or damage, although that point remains a research interest, whereas tubule plugs surely do so. Both are calcium in kidneys. All of the CaP stone formers we have studied have some plugging but no one has to date proven the stones grow on the plugs – that too is an open research question. Laura does not have MSK, I am sure, because it produces an odd and recognizable shape of the papillum and the bellini ducts are not plugged but higher up, in the inner medullary collecting ducts you find not plugs but myriads, hoards of microscopic round stones that just roll out when the ducts are opened. It is perhaps a lot to ask of urologists who are not ensconced inside university research institutes to make the kinds of distinctions that are in our paper, but with new instruments I believe that most will be doing so soon. Most important, the old fashioned diagnosis of MSK by x ray is not credible. The issue for Laura is prevention, and if pursued aggressively it can reduce new stones greatly and therefore the miseries of such stones. I would focus there. Prevention of calcium stones is not overly difficult. All the best, Fred
Hi Dr Coe,
I have had recurring stones since my 30’s. Sometimes I pass them with ease and of course some are associated with extreme pain. I average one stone every 1 to 2 years. Recently, I had a lithotripsy to break up a 3 mm stone in my right kidney. However, I could not pass the pieces. So, the doctor went back in and removed the stuck piece from my right ureter and another stone in my left kidney. He put a stent in each kidney. Very painful. The stents were removed two weeks ago and I still have discomfort in my back. 3 days ago they did another CT scan and could see nothing abnormal. So, the regime is ibuprofin and fluids and the discomfort seems to be subsiding. I finally received the analysis of one of the stones. It says the following: Nidus: No Nidus visualized. Calculi: Calcium oxalate dihydrate (Weddellite) 10 %, Calcium oxalate monohydrate (Whewellite) 85%, Calcium phosphate (Apatite) 5%. Surface crystals, Calcium oxalate dihydrate (Weddellite). The size was 4x3x2mm wt 20.2 mg. I will admit that I don’t drink a ton of water. However, I avoid salt, no tea, one cup of coffee in the morning. I read on a web site that nuts and caffeine can be stone formers. I eat a lot of peanuts and eat peanut butter and jelly sandwiches for breakfast a lot. Do you have any suggestions for me? Thanks for any help. Robert
Hi Robert, It is true that nuts can contain oxalate and help form your stones. It is not true that coffee promotes stones, in fact coffee drinking is negatively associated with stones. My suggestion to you is proper 24 hour kidney stone risk factor urines with at least one blood to screen for systemic diseases that can cause stones. With all your stone activity you will have some abnormalities that cause them, and selective treatment should lead to prevention. Regards, Fred Coe
Hello Dr. Coe,
I am a grade 12 student writing an essay on how kidney stones are formed. This article helped me tremendously in understanding the different types of kidney stones and how they form. I would love to reference your article in my paper, but I need the date of publication. Could you help me out? Thank you so much! Marie
Hi Marie, I am so glad you found the article helpful. The publication date is: Jun 20, 2014 @ 20:40. All the best, Fred Coe
Dear Doctor,
I am suffering from last 5 years from kidney stone, i have controlled my diet in every means. I am trying to control my body weight also. I just want to get rid of this stone. Please suggest a way if any. It will be help full if you can share the picture of type of stones. My whats app contact is +918806074161.
Regards,
Anike Tambe
Dear Anike, Your type of stone needs to be determined by a laboratory as appearances are not very specific. WHatever the crystals in the stones, you need to prevent their forming. TO do this you need 24 hour urine testing to discover what in your urine is promoting the crystals and then aim your diet changes and even medications specifically there. Nothing else is known to work well. So, that is the way, and I hope it works for you. Fred Coe
Dear Dr. Coe,
I was hospitalized over the Thanksgiving holiday in acute renal failure due to a 5 mm kidney stone that was stuck in the proximal left ureter x 3 days. The urologist tried to remove the stone via ureteroscopy and laser, but was unable to get a clear shot at the stone due to swelling of the ureter. He put in a stent and called it a day. Renal function returned to normal within 24 hours. A KUB showed that the stone is currently back up in the lower pole of the left kidney. The urologist wants to use lithotripsy to break up the stone. We are not sure what kind of stone I currently have, but I did have a kidney stone 20 years ago (on the same side) that was calcium oxalate; I was never told whether it was monohydrate or dehydrate; it is assumed that this stone is probably the same type. 1) Would you recommend lithotripsy over ureteroscopy for a calcium oxalate stone, and 2) is it true that lithotripsy can cause hypertension? I am a 57 y/o female in otherwise good health. Thank you for considering my questions.
Hi Meg, I am concerned about acute renal failure from a left sided ureteral stone; I presume you have only one kidney as the right kidney should otherwise have maintained normal overall renal function. This means you have stones in a solitary kidney. For the stone, considering your acute renal failure and my suspicion that your right kidney is not functional – or present – I would favor ureteroscopy. SWL of a single functioning kidney is not ideal. Hypertension from SWL is a vexed issue – no definitive proof. If there are two functioning kidneys, I guess SWL of the single stone is alright. But then why did you have acute renal failure? You should find out about why you had acute renal failure – is it indeed one functioning kidney, were you septic? Regards, Fred Coe
I have both kidneys, and to my knowledge both were working before this happened. My creatinine has always been about 0.6 or 0.7. My GFR has always been over 60. My creatinine had gone up to 1.3 on admission and the GFR down to 45. CT showed mild hydronephrosis on the left side. So are you saying that the kidney function tests should have remained normal even if only one kidney is in trouble? I think I have some more questions for my internist.
Hi Meg, Thanks for the clarification. What you experienced is best referred to as possible mild acute kidney injury but more likely it was pre-renal azotemia – simply functional reduction of filtration from dehydration, or other factors associated with the stone episode. THis kind of reduction of filtration does not actually imply any renal damage at all. Acute renal failure as a phrase evokes a sense of marked reduction of filtration posing significant risk and concern which what you had did not. The 45 is a calculated – so called eGFR – which is not ideal in acute settings. When I said kidney function should have remained normal I meant as compared to serious kidney failure – where creatinine levels rise to 4 or 5, serum potassium can rise to threatening levels, urine flow rates fall markedly. That is what I surmised was meant by acute renal failure. The white cell increase is also compatible with dehydration, which I suspect. Given all this, your surgeon should certainly do what is most feasible given what he encountered at the first surgery, as you are a routine instance of a single stone in an otherwise healthy person. I suspect you will do well. Be sure and analyze the stone, and perhaps it is time to undertake prevention against any more of these. Regards, Fred Coe
Dear Dr. Coe,
The diagnosis of acute renal failure was on my discharge summary and took me by surprise. Thank you for clarifying that issue. Prevention is key. After the last stone I asked about prevention and was told just to drink plenty of water, that dietary restriction of oxalates was unnecessary. I live in the southwest, so staying hydrated can sometimes be a challenge. I have been looking into the dietary sources of oxalates and realized that lately I have been eating very high oxalate foods, especially nuts and nut butter, so-called “healthy” snacks, and tis the season for chocolates! I will be sure the stone is fully analyzed. I want to thank you for answering my questions. I appreciate your generosity in sharing your knowledge in this forum. Also your website has been particularly helpful and now bookmarked. Thank you again.
Thanks, Meg; for prevention check out the article on the five steps. Fred
Hi Dr. Coe,
My lithotripsy was cancelled at the last minute. I was in pre-op when the results of that morning’s KUB showed the stone was gone. The KUB done 3 weeks prior clearly showed the stone in the lower pole of the left kidney. I had no symptoms of passing the stone at all. The urologist said he’s seen stents do weird things, and perhaps it facilitated the stone’s exit. I asked him about prevention and he did not think a low oxalate diet was useful, but just suggested staying hydrated. Thoughts?
Thank you.
Hi Meg, I am glad the thing is gone. As for prevention, staying hydrated is fine but certainly we can do better. Have you read my article on the five steps to prevention?? There is a lot to do and that lot can prevent stones and reduce all the miseries of surgery. There will be more on the same subject as prevention is the main purpose of the site. Warm regards, Fred Coe
One more thing to add: my WBCs were 9,000. I told the ER doctor that number was high for me, as my normal count is closer to 3,000. He countered that the differential was normal. One week later the WBCs were 3,700; kidney function continues to be normal.
Happy New Year, and thank you for your response. Yes I have been reading your website on prevention in earnest, and I have connected with Jill Harris. I must say that I was a little surprised by the response from the urologist. My thinking (as a nurse and as a patient) is that hydration is good, but dietary changes might give me some extra protection should I get a bit dehydrated in the future. Why tempt fate by eating spinach salads with almonds, when there are so many healthy low oxalate food alternatives from which to choose. The first stone I had twenty years ago resolved in two hours. This stone took one month to to resolve. I am committed to do what I can to prevent a third episode. Thank you for this website.
Excellent articles! I have been dealing with kidney stones for 35 years, and I am always open and eager to learn more about what I can do to prevent the next stone having had hundreds by now. The lab results for my left side stones is different than the labs on my right side stones. Is it unusual to make different stone types in each side?
Dear Lisa, Yes it is, and of research interest, too. A common pattern is calcium oxalate from one side and a calcium phosphate from the other – apatite or brushite. Likewise common is struvite from one side because of infection. What is not unusual enough is forming stones for 35 years without effective enough treatment to make an end of them. Since you read the site, take a look at the one on prevention – why keep making stones? Regards, Fred Coe
Hello,
I had my fifth uteroscopy with lithotripsy almost 3 weeks ago. I hadn’t had this done in almost 5 years. I had two stones, the larger being 6mm which was partialy obstructing my kidney. I always have trouble after the surgery with the stent but usually I am better after the stent is removed. Not this time. the stent was removed two weeks ago tomorrow and I am continue to ave pain and spasms in the bottom part of the ureter and in my bladder with some flank pain now and then. I am going back to the urologist tomorrow. These stones were in the kidney but I have had stones travel almost to the bladder and just sit there, causing this same type of pain. I have medullary sponge kidneys so I make stones. I don’t want to any more. This last time I had one of each of the calcium oxilate types. I hope we can find a way to stop these stones from forming. I have been dealing with them for over 23 years. I just can’t go through anymore uteroscopies. I hope this pain isn’t going to be something permanent. Thank you for this information! Anne
Hi Anne, MSK patients form two kinds of stones. In their cystic dilated ducts they form masses of microscopic almost dust like stones. They also form common stones like yours. Prevention is like all stone formers. What were your 24 hour urine test results? What have you been doing for durable prevention? Whatever your urine supersaturations they are too high and need to be lowered. This will prevent a majority of recurrences in most cases if followed diligently. GIven your frequent stones, you need more than you are getting. Regards, Fred Coe
Hi
I have just gotten the results back from stones I passed last week. They are calcium phosphate. I am going to be doing a urine collection, but had a few questions. What is the main concern with this type of stone and how can I prevent more.
Hi Julie, The main concern is more rapid growth than calcium oxalate and accumulations of crystals within the kidneys. Prevention is very valuable and important. Regards, Fred Coe
Hello Dr Coe
I have kidney in both my kidneys. the left kidney is an ectopic kidney with a 18 mm stone. the right has a 8 mm stone.
i was advised for RIRS procedure. This may be in two stages. It will be only for the left ectopic kidney using stent in the procedure.
Kindly advise should I go for an open surgery as one urologist suggested so.
Some have also advised me get the treatment by Ayurvedic medicine which helps to dissolve the stone.
Please let me what treatment to follow.
Many Thanks
Kumar
Hi, I do not know what the RIRS procedure is – the abbreviation is not familiar. Can you tell me more? As for dissolving stones, I know of no real evidence that this can happen for calcium oxalate stones although it is routine for uric acid stones. Perhaps you might write back with more information and I will try to help. Regards, Fred Coe
I’ve been struggling with kidney stones for about 20 years. I’ve had three surgeries to have them removed and countless trips to the ER. I feel like I’m getting the runaround when it comes to having them tested. These are my results from the last hospital stay in November. Would you please tell me what this all means? What kind of stones am I producing? And how do I prevent them?
Thank you!
Stone Weight 83.6
Stone Calcium Oxalate Dihydrate 20
Stone Calcium Oxalate Monohydrate 10
Stone Calcium Phosphate 02
Stone Calcium hydrogen Phosphate 68
Dear Danielle, Your stone analysis is crucial in that you are forming stones that contain brushite – calcium monohydrogen phosphate – at 68%. In general stones contain no brushite so patients with this kind of stone are a special case. The stones are hard and fragment poorly with shock wave lithotripsy. The are often very recurrent and hard to stop. The kidneys themselves can accumulate calcium deposits in them so the CT picture become confusing and resembles nephrocalcinosis. You are someone who must have medical prevention, and I would try to get that done in an orderly way. As a rule brushite stone formers have high urine calcium excretion levels due to idiopathic hypercalciuria which is treated with low sodium diet and high fluid intake and, if that is not enough, thiazide diuretic agents. In general most require both fluids and low sodium diet and also thiazide. Prevention is most important for you, and the benefits are remarkable. Regards, Fred Coe
Dr. Coe,
My husband has been suffering for about 8 years now with calcium phosphate stones. He has had so many surgeries that we have lost count. He currently is taking hctz and potassium citrate. He has seen 2 urologist which he is still in the care of one of them and he is also seeing a nephrologist. The 2 Dr’s he sees now do now agree on his care. His stones actually seem to be getting worse if you ask me. He usually passes a few each month if not more.
I found your article very informative. We have never had it told to us like this before. My question is, do you see patients or look over their records. We are just on our last string and we just feel like the Dr’s don’t really listen and try to really help him.
Any help will be greatly appreciated. Thanks for the article.
Dear Jonna, I am sorry about your husband; calcium phosphate stones are very recurrent and can be extremely serious. I am a professor at University of Chicago and would be pleased to see him and be helpful, but you should discuss this matter with his physicians, who seem very involved, and be sure they think there is some way that I could add something. Should this seem reasonable, it would be best to email me directly as personal health care is best discussed in a less public medium. Regards, Fred Coe
My 23 year old son is severly handicapped ans has had a sandy substance in his urine. The lab results say the specimens are 100% dahllite. Please teach me more. Is it serious? Thank you!
This mineral is carbonate apatite and forms in alkaline urines. It usually means the urine pH is very high – over 7 – and urine calcium and phosphate are high enough to form this material. Renal tubular acidosis, some drugs that can cause renal tubular acidosis, abnormalities of the urinary tract, all of these can cause this kind of crystal to form. Massive crystalluria can lead to stones. To understand what is wrong would require a knowledge of all that is wrong, and that is the role of the physicians who take care of him. Perhaps they might not be aware of the special issue of highly carbonated apatite stones and might be able to stop the crystallization and head off stones if they saw this note. Perhaps they already know everything and just cannot stop the process. Also – commercial labs vary in quality with respect to these less common crystals, and perhaps a sample should be sent to another lab for verification. Regards, Fred Coe
Thank you for your insight! We.have captured multiple samples that are thick and gooey but they dry to a white color. They didn’t show up on a kub image. Would a different imaging method be better to evaluate the extent of the problem? My son is non verbal with global delays. He takes tegretol,baclofen and valium. For the most part he is healthy. He was injured by the whole cell pertussis vaccine. Should we see an urologist or nephrologist? Our General Practioner doesn’t seem to be concerned because of the lack of fever. Thank you very much for your time! We will have a sample sent to a different lab as well.
Hi Kelly, In the absence of symptoms and surety if these are crystals I would just try to find out what the material is. It sounds a lot like protein, and may not be a real problem. If he is having pain attacks that seem to coincide with passage of this material crystals would be a higher likelihood. Let me know, Regards, Fred Coe
Thank you sooo much Dr. Coe! I will be looking also into a possibility of Lesch Nahan syndrome. I will try to get my son to tolerate an ultrasound. Can you give me ideas for antibiotics useful for infection stones? I truly appreciate your help!
How do I give you a 5 star rating?
Dear Kelly, You just did. Regards, Fred
If he is indeed infected, his physicians need to identify the organisms. With what appear to be apatite crystals, he may indeed have stones, and they can become infected. That can complicate things. The best course it to verify if there are stones – ultrasound will do – and have more samples of the white material tested: It may be protein. The crystal material you have so far need not be infection based, it may be from some other cause as it did not contain struvite. This is a situation so complex my own help is very limited and your physicians remarkably central to everything. They seem to be doing very well. Best, Fred Coe
I have calcium oxalate dihydrate and monohydrate stone pl give suggetion to remove it
Hi Vitthal, Here is my best overview on stone prevention. As for surgery, here is a good article about modern techniques. Just being there does not mean stones need to be removed. Pain, bleeding, infection and obstruction are proper indications – otherwise why have a surgery? Regards, Fred Coe
Hello Dr. Coe,
I’m a environmental engineer and currently put me a question about the benefits / detriments of alkaline water for human consumption. Initially responded to an increase in pH would disrupt the natural balance of water system -> carbon dioxide – bicarbonate-carbonate, favoring the appearance of the H+ ion and acidifying the urine promoting the appearance of uric acid kidney stones. My question is if we have way to relate alkalinity in water intake with the appearance of Calcium Oxalate Stones?
Best Regards,
Amarilis
Hi Amarilis, Thanks for the interesting question. Generally the buffering capacity of even alkaline water is so low it has only modest effects on urine pH, but if it had any it would be to raise it. Calcium oxalate crystals are pH independent over the range of pH in human urine (4.5 7.9) because oxalic acid has a very low pKa for its second proton and is entirely ionic in urine. Warm regards, Fred Coe
Thank you for your feedback,
During the university years I remember a water treatment teacher mention the fact that the temporary hardness associated with counter ions (carbonate / bicarbonate) is related to alkalinity and be harmful to human health for those who have tendency to form kidney stones . I always had this idea, but the problem is to explain it more detailed.
Best Regards,
Amarilis
Hi Amarilis, I think your explanation is fine, but that the buffer capacity of water is very low. I suppose in some cases the water is so filled with carbonates that urine pH will rise; it is a matter worth studying. Regards, Fred Coe
Dr. Coe,
I have been battling kidney stones for about 8 years now (multiple lithotripsy’s, and 2 PCNL’s). I was told just recently that I have a Medullary Sponge Kidney. Over the last 3 1/2 years the stones that I have pasted have been Calcium Monohydrogen Phosphate Dihydrate (Brushite) 100% stones. I did have one that was Carbonate Apatite (Dahllite) 100% and one that was Calcium Monohydrogen Phosphate Dihydrate (Brushite) 80% and Calcium Oxalate Monohydrate (Whewellite) 20%. Water pills make my potassium levels really low so I have been taken off those. I try to push the fluids but sometimes have difficulty due to kidney fullness and not urinating well during the day. I am back to watching my sodium intake. Any other ideas? I know that with MSK I will probably always have stones but any ideas to maybe help slow them down?
Thank you for taking a moment to read this. Have a great day!
Betsy Weiss
Hi Betsy, I am rather sure this is not MSK but rather brushite stone disease which is very unusual in MSK patients. Brushite stones are a special kind of problem. The stones are hard and fracture poorly with shock waves. They almost always are driven by idiopathic hypercalciuria and I suspect you have that because you have been placed on a diuretic. A low sodium diet – 1500 mg daily will lower urine calcium in IH and if needed thiazide can be used in a very tiny dose. A potassium blocker like amiloride can be added, to reduce potassium losses. Take a look at how a prevention program can be constructed. It begins with fluids and low sodium, the latter checked by 24 hour urine to be sure. We have treated a lot of brushite stone formers, and they can be managed very well. I am sure your physicians would want precisely what I am writing to you about; perhaps you could bring this to their attention. The best drug may be chlorthalidone, which can be used in very low doses and has a long half life. Warm Regards, Fred Coe
Dr. Coe,
Thank you so much for your reply. I will definitely talk to him about the amiloride, thiazide, and chlorthalidone (which I have been on in the past-potassium level around 3.4 on them all even with taking potassium citrate or potassium chloride). Yes high calcium levels in 24 hour urine. I am not sure how they determined the MSK-no special xray just said it. I will do my best to lower the sodium even more and push fluid.
Thank you so much for your time. You have helped a lot.
Betsy
My daughter had her first kidney stone at age 16. She has had two more episodes of pain and microscopic hematuria (presumed passed a stone) one and two years later. The stone required retrieval and stent placement and the analysis showed 3 constituents, 50% calcium phosphate (apatite), 40% calcium oxalate dihydrate and 10% calcium oxalate monohydrate. Our urologist told us she did not need any dietary modifications and just to drink alot of water daily. Can you suggest any other preventative (dietary, medications) for her profile.
Hi Jane, Your daughter almost certainly has idiopathic hypercalciuria, and needs a low sodium high calcium diet – the low sodium to lower her urine calcium, the high calcium to protect her bone mineral stores. The high fluids your physician recommended are indeed a good idea. But in order to get proper treatment she needs to have 24 hour urine testing – my guess about hypercalciuria is just that until she is tested, and screening for the uncommon systemic diseases that can cause stones in young people. Read this article which helps put everything together. That her stones are 50% phosphate is not too surprising because this is the common pattern in young women, but the phosphate increases the urgency of prevention as phosphate stones can grow rapidly and also because kidney tubules can become plugged with crystals. If diet and fluids are not sufficient to prevent more stones, she may require medication. Good luck, Regards, Fred Coe
Hello,
I am 47 and I am on stone 93 (that I have actually seen). I had a few in my teens(calcium oxalate), 30 while pregnant (containing oxalate and phosphate), I am now 47 and pass calcium oxalate stones often.
I would please appreciate any feedback.
Kidneys – healthy (no signs of sponge) Numerous Stones in both
All blood and 24 hour urine levels normal
No parathyroid issue
Normal cystine levels
Exercise 5 times a week
Weight-in proper range
BP LOW
Cholesterol -normal
Diet healthy Avoiding high oxalate including spinach, kale and black pepper,
No tea soda, or coffee
Water intake high (clear,very light color urine)
Tried Hydroclorthiazide discontinued since ultrasound showed no improvement
Tried Allopurinol discontinued since ultrasound showed no improvement
Currently trying Thera Lithium XR Vitamins
Stones passed size 1mm- 8mm
Rarely painful in kidneys
Can almost pinpoint location in left and right ureter
Pain tolerance high
Pain relievers don’t work, so I don’t use them
Is there anything I could be missing?
Thank you for your time.
Julie R
I forgot to mention never had stents, and only one lithotripsy which was horrible because the 8mm stone turned out to be in a T-shape so I passed the gravel and an additional 8mm Stones piece. It was awful and I hope I never have to get it again. I felt very awake during the procedure in terrible pain.
Thanks again.
Hi Julie, How high is the phosphate content in your stones? One percent, 10 percent? The higher, the more likely the problem is in your urine pH and calcium. What does normal mean for your 24 hour tests? If you are forming stones, the supersaturations in the urine you form is too high in relation to the crystals in the stones you are forming, and need to be lowered. So take a closer look.
Thank you for the reply. I am going to have my latest stone analyzed, mainly because it looks different than my other 90 plus stones. It is an odd black color with strange white pieces.
I will get the exact numbers. The phosphate was only during pregnancy which was 10 years ago.
I will check back when I get the result.
My 24 hour collection shows all levels in normal rangeaccording to my nephrologist.
I will investigate the “super saturation”.
Dear Dr Coe,
I have MSK and have suffered recurrent Calcium Oxalate kidney stones since I was 16 yrs (now 45). I have always managed to pass them but have just been released from hospital after having surgery to remove a 9mm stone and have a stent in place for the next few weeks. I am interested in your opinion of the use of Potassium Citrate for prevention of stone formation in MSK patients specifically. Can you get a similar result through diet alone or is it recommended to change diet and take potassium citrate at the same time in MSK patients? Can you overdo Oxalate reduction?? Regards Rowena
Dear Rowena, It is not possible to overdo oxalate reduction per se because oxalate is irrelevant as a food substance. But the foods with it are worthwhile, so check out good ways of lowering oxalate. In fact, what do your 24 hour urine studies show is wrong with you? Citrate is not unreasonable but we like to focus treatment on what we find is abnormal. Regards, Fred Coe
In the fall season of 2013, I had my first and only kidney stone attack, which involved pain only on my left side. I think that I triggered it by, for some reason, not drinking enough water over a weekend. I guess I just wasn’t thirsty. The CT scan and follow-up KUB revealed an approximately 11 mm stone in the lower pole of my right kidney. The stone analysis showed a composition of 20% Calcium Oxalate Dihydrate, 40% Carbonate Apatite, and 40% Ammonium-Magnesium Phosphate Hexahydrate (Struvite). A 24-hour urine test was performed and I was told that everything was normal. A small stone that I passed at the urologist’s office two days after I first saw my regular doctor was found to be a uric acid stone. A subsequent KUB in the fall season of 2014 and Ultrasound in January, 2016, showed that the stone in the right kidney had not grown. My urologist wants me to undergo an ESWL treatment, even though his partner (who has now retired) thought in 2013 that a scope procedure performed by a younger doctor with a steadier hand than his was what was recommended, if I decided to do anything at all. The ESWL procedure is scheduled for 062216, but I am not convinced that this is the right thing to do. As you said in an earlier post ,”… Just being there does not mean stones need to be removed. Pain, bleeding, infection and obstruction are proper indications – otherwise why have a surgery?” Also, the Johns Hopkins Kidney Stone Glossary (website) describes the lower pole as “the bottom-most part of the kidney’s collecting system. Stones in this location tend to not respond as well to ESWL and ureteroscopy, as fragments often persist in this location following treatment, promoting the formation of new stones.”
My urologist says that I should try ESWL because it is the least invasive procedure and that if it doesn’t work, we could consider another procedure or do nothing. He says that the overall success rate for ESWL is 80% and that the stone is a calcium stone because it shows up on a KUB. He says that if the stone were to move and block a ureter, I would be in a very painful emergency situation.
I know that the stone is too large to pass without being broken into smaller pieces. My concerns are that we do not the know the chemical composition or hardness of the stone, that it is in a difficult location to treat, and that I have no pain or other symptoms. If the stone does, indeed, need to be removed, I don’t know that I should start with ESWL in this situation, even though it is the least invasive treatment procedure. There probably isn’t “a best solution,” but I would appreciate any insight that you can provide.
Hi Dan, as I am not a urologist and only know what you have said I can only offer a few thoughts. First, the stone analyses do not really make sense. Struvite is only from infection, but uric acid is altogether another matter. Are the analyses accurate? As for the stone, being without symptoms one could leave it alone, as you mentioned. Perhaps the most definitive approach would be ureteroscopy but not dusting – rather the more definitive procedure which requires a ureteral sheath. Dusting could indeed leave a residue at the bottom of the kidney. If there has been struvite, then SWL or dusting would be a bad idea in that it might spread infected particles. I would suggest perhaps asking your urologist’s opinion about these additional matters, and, of course, seeking a second opinion which is always prudent. Regards, Fred Coe
Dear Dr Coe,
My kidney stone analyses resulted in 80% cystine and 20% struvite. As I understood the formation of that stone types require very different levels of pH in urine. How that can be explained?
Regards,
A.
Hi an, The cystine means you have cystinuria and require specialized treatment for it. The struvite means that your upper tract has been infected with an organism that hydrolyses urea to ammonia and produces the struvite crystals in situ. This can and does happen. Your situation is complex and requires a lot of expertise – for the cystinuria and for what is presumably an infection localized to stones. Regards, Fred Coe
Dear Dr Coe,
Have a great day. Great article about Kidney Stones. My kidney stone analyses resulted in Ammonium Hydrogen Urate 50% and Carbonate Apatite (Dahllite) 50%. Can you explain me? Thank You.
Regards,
John.
Hi John, AMmonium acid urate occurs in settings of potassium depletion and bowel disease. It is otherwise unusual. Do you have bowel disease or a cause of diarrhea or potassium depletion? Regards, Fred Coe
Hi Dr. Coe,
So far I know I don’t have any bowel disease or cause any diarrhea or have any pain in my stomach I’m overweight 235Lb but never feel I have problems to going bathroom or any weird color of my feces very normal for the color. My story in the last year since November 2015 I been almost sedentary, ate junk food and a lot of cola and sugar. In June 10, 2016 I thought I had UTI infections for the symptoms cloudy urine, smelly and pain in the tip of the penis but I took home remedies to cure myself I never went the doctor because the symptoms I was feeling better and gone but In June 30 I was in ER because I had a great flank pain right side kidney, the doctors found I had a massive UTI in the kidney and bladder infection plus 4mm stock in the uretra right side took 30 hours to passing the stone when I was in the hospital they give antibiotics for UTI, Morphine 2mg and 4mg, flomax and I took pills to going the bathroom for going to number 2. The doctors told me I have pre-diabetes, B12 deficiency and 2mm kidney stone left side. After I was discharged I had 2 fallow ups one July 13 with primary doctor and July 16 an Urologist.
I had a fallow up with a primary doctors July 13 and I got the urine test showed Ketones 15mg the doctor told me if I’m drinking enough water I told her I’m drinking 8 to 12 Oz of water every day plus oatmeal with water 1Lt, she felt might something wrong going with my kidney isn’t process the water.
I spoke with an urologist in July 16 I had an appointment he showed the CAT when ER took it, my right kidney was 2.5 bigger than the normal size he said was very much inflammation pushing everything inside. When I got the results of the kidney stone 3 days ago July 21 he told if I had problems of diarrhea because I was drinking medicine to going the bathrooms for the constipation, I told when I was in ER the doctors give pills to going to number 2 because I was stock. Also I told him I been almost sedentary, ate junk food and a lot of cola and sugar since Nov 2015. The urologist told me July 16 in the coming week I will get a 24 hour urine test and in July 7, I will have an Ultra Sound to see my kidneys are working correctly and how is going on with the stone of 2mm.
Dr. Coe I feel nervous about my situation right now my symptoms are having trouble with memory, in some nights not every night I have very little pain when I going to pee in the tip of penis, some pain in the left side kidney when I walk more of 30 min, my eyes hurt me, my leg shin/calf part hurts me in the night and I feel thirsty.
I told the urologist this he says this will be pass no worry but will take time and he don’t know when.
Thanks for following up my case, appreciate it any advice from you Doctor Coe.
Hi John, this is complicated. I wonder if your stones are really related to infection and the stone analysis is not correct and you have struvite and carbonate apatite. Errors are especially bad for struvite. Have your physicians determine as best they can. Regards, Fred Coe
Hello Dr. Coe,
Three wks ago had pcnl for a 2.3 cm staghorn stone that had been within the kidney for 6 years. I have had multiple complications since surgery including hemorrhage, infections and fever. The physician was expecting struvite and I have had Proteus mirabilis pyelonephritis. The stone analysis, however, showed:
Brown portion of calculi composed of calcium oxalate monohydrate.
Tan portion of calculi composed primarily of 80% calcium oxalate dihydrate and 20% calcium phosphate (hydroxy- and carbonate- apatite).
Can you give me any insight on this type of stone. I certainly want to avoid going through this again if I can!
Thank you for your time.
Hi Mary, these constituents are from calcium and oxalate disorders and you would want a standard evaluation for them. Try this general approach. But the proteus and the size makes me suspicious that some struvite was in the stone and either the fragments in the stone that were analysed did not happen to have those crystals or the lab was not accurate. Struvite is the least accurate analysis in labs. I would have hoped the stone was cultured, and also that the PCNL left you free of all fragments. If there are any residual fragments your physician might want to consider a few month course of acetohydroxamic acid – a blocker of the urease enzyme that permits proteus to produce struvite, so permit dissolution of any residual struvite. As this drug has lots of side effects and significant hazard he/she may not want to use it, understandably. But overall I am very suspicious there was some struvite there. In any event prevention is to be directed against the calcium oxalate stones as in the Five Steps article. Regards, Fred Coe
Dear Dr Coe,
My kidney stone analysis resulted in Calcium Oxalate Monohydrate (Whewellite) 60% and Calcium Oxalate Dihydrate (Weddellite) 40%. Can you explain this to me? It is the first time I have ever experienced kidney stones. I had my gallbladder removed in 2003. I developed a boutique of H. Pylori and, as a result, I suffer from IBS. Any information would be helpful. Thank You.
Hi Michelle, You have formed the most common kind of stone. Possibly your gallbladder surgery has resulted in some malabsorption and your urine oxalate has risen. But that is speculation. The right approach is to obtain an organized prevention program. Try this approach to organizing things, it works. Regards, Fred Coe
Hi Dr. Coe,
In 2007 I had the wave surgery to remove kidneys stones a month ago I had passed a stone and kept it for the doctor all they said was “compostion, calculus, infrared spectroscopy hydroxyl apatite with moderate portion of calcium oxalate”. What does that mean?
I was in a lot of pain when they were in the verge of passing and now realize I have had a number of them pass through the years without realizing what it was.
Gloria
Hi Gloria, The stone seems to be primarily calcium phosphate so you probably fit the pattern of idiopathic calcium phosphate stone formers. Prevention is very practical and should reduce the numbers of new stones. Take a look at a practical way to go about the matter. Regards, Fred Coe
Good Morning Dr. Coe,
On May 30, 2016 I was diagnosed with a 1.4cm stone cluster in my rt kidney, and kidney infection (after an ER visit for extreme rt lower back pain). During that visit, thanks to a CT of my abdomen, I also found out that I had aortic valve stenosis (1.3 opening) from calcium build up. After many tests and procedures to obtain a cardiac clearance, I finally had lithotrypsy and a stent placed in my right kidney. As previously stated, the cluster was 1.4cm, a month later it was seen on KUB to be a 1 cm cluster, and subsequently seen on a CTA Runoff 2 weeks after to be a 1.5 cm solid stone. The lithtrypsy was successful. The stone report just came back and the stone was 15% Whewellite (calcium oxylate monohydrate) and 85% Dahllite (carbonate apatite). I am a 37 yr old female with no previous hx of kidney stones but have a maternal family hx of CKD at a young age. I do not take any supplements including nothing with calcium. When I asked my urologist what I can do to prevent them, he had nothing to offer (which was extremely disheartening). Can you help me understand what this type of stone is from and how I can try to prevent further stones. Thank you so much for your help.
Hi Rebecca, Your stone was mainly calcium phosphate. Most likely you have your stones without systemic disease, so called idiopathic stones. Prevention is best based on a plan, and here is one I favor. But your family history is odd in having chronic kidney disease on one side. This suggests the possibility of Dent’s disease or renal tubular acidosis or other such which your physicians might want to consider seriously and exclude – something one should do. Most likely there are not the cause and prevent will go well. Regards, Fred Coe
Thank you for the information. I am going to have my urologist order fasting labwork and a 24 hour urine (as neither have been ordered yet. I will also have my doctor check into Dent’s and RTA. This site has been a amazing resource for information and helping me to understand this situation that I now find myself in. Thank you again!
My daughter (20 yo) had stones consisting of Ammonium Hydrogen Urate 90% and Uric Acid 10%. What causes this type of stone and what can she do to minimize chances of future stones?
Hi Lois, This is a very interesting and important question. Such stones require the combination of a modestly high urine pH and very high urine ammonium ion, and that usually occurs because of diarrhea, either from bowel disease or laxative use. It can also occur with potassium depletion. Here is a case where 24 hour urine testing is absolutely necessary for understanding. Let me know. Regards, Fred Coe
She does have IBS, so that part makes sense. The doctor didn’t mention 24 hour urine testing, so I’ll tell my daughter about that. I have IBS and never had stone, so why does she have them and what can she do?
Hi Lois, Stool electrolyte losses are the key, and these can vary a lot. 24 Hour urine testing and serum as well are crucial to see what is going on. Often serum potassium will be slightly low, as well. That you have what she has may be a matter of degree – the worse the losses the higher the risk of these special kinds of stones. Regards, Fred Coe
What category does a 100% Mucin kidney stone fall under & what causes these?
Hi Charity, It is a stone in which no crystals were found. Usually that means it is not a stone at all. Regards, Fred Coe
Hello Dr. Coe! Nice article great info! Ive had a history of stones going back 9 years. Both times it started with pregnancy. The first incident i had a couple lithotripsys done and i finally got rid of them. But now Ive had stones in both kidneys for 6 years, they havent been too bothersome until recently. My major concern is frequent uti’s but also just a general discomfort…bloating, nausea, irregular urination. So i have a procedure scheduled for the Dr to go in and get a sample of the stone. Based on your article it sounds like its struvite or mixed, i dont know. I was wondering what i can do in the meantime to help with discomfort, i feel as if they prescribe me antibiotics for a uti, an i feel better while im taking it, but as soon as i stop i feel like the uti is right back?
Hi Bethany, I am sure your urologist is not going in to get a sample but to render your kidney as stone free as possible. Presumably this will be flexible digital ureteroscopy or perhaps percutaneous nephrolithotomy. Analysis will be crucial. Your stones may be infected whether struvite or not. Be sure and get a full evaluation beside the stone analysis. Regards, Fred Coe
Dr. Coe,
I have a long history of kidney stones. I read an article many years ago about apatite having significance and you mention it here briefly. Can you explain it in more detail please. I have seen that element in a few reports. For example I passed a 5mm stone–not so easy!– and the composition was reported:
50% hydroxy and/or carbonate apatite
40% calcium oxalate mono hydrate
10% calcium oxalate dehydrate
I was diagnosed with osteoporosis at 44yrs old and have felt my kidney stones and bone loss are correlated. Can you offer any insight based on the composition of this one stone? Thanks
Hi Lisa, You do indeed have phosphate stones – 50% is enough for me, and I presume a combination of idiopathic hypercalciuria and low calcium diet. I suggest you follow an orderly plan of evaluation and if it is what I think then it is possible to prevent stones and also help with the bone problem. But diagnosis comes first. Regards, Fred Coe
Thank you for your time and guidance Dr. Coe. I will find a skilled physician and follow up in the near future. Bless you!
Let me know how things turn out. Regards, Fred Coe
Dr. Coe,
I have a total of 12 stones that have been deposited over the years from both kidneys. I have read most of the comments but have seen none with my concentration of stone make-up. 90% WHEWELLITE 10% WEDDELLITE. Why is the Calcium Oxalate Monohydrate so high and what causes it to be so?
Hi Rod, a perceptive question. High COM usually means oxalate abundance is high in relation to calcium, so I would guess your urine chemistries show a moderately high urine oxalate and perhaps also calcium and a low pH around 5.9. Be sure and get evaluated completely as there have been a lot of stones. Regards, Fred Coe
Hi Dr. Coe – I posted this in the low oxalate diet page but I wanted to post it here too as I am interested in learning about the potential connection between IBS, diarreah and dehydration. I was diagnosed with IBS (with diarreah) 30 years ago. I have without a doubt been seriously dehydrated for periods of time when suffering with bouts of IBS attacks. And then I can go months with no incident. Ironically I’ve actually noticed an improvement in my IBS since learning of my kidney stone and increasing my water intake – which doesn’t really make much sense to me and maybe it is a coincidence. I’ve mentioned my IBS and a connection to the kidney stone to my Gastroenterologist as well as to my Urologist but neither seemed too convinced. I’m posting the rest of my story here – in case anyone has any comment.
Hi – I am a 50-year-old healthy female (5’7, 120 pounds) who experienced what I believe to be kidney stone pain on June 23. I had pain in my left flank that radiated to the front and down into my groin area. I got up for work and the pain was very intense so I drove myself to the ER. As soon as I walked in to ER and showed them where my pain was – the nurses and ER doc all said kidney stone. They did a catscan and found no hyronephrosis or ureteral dilatation. But did find a 7mm non-obstructing calculus in the midportion of the left kidney, (“probably in an upper pole infundibulum). No other renal, ureteral, or urinary bladder calculi identified. I had microscopic hematuria and was sent for an ultrasound of abdomen which found nothing. I was loaded up with IV fluids, Dilaudid (which after the first dose made me extremely nauseated) and Toradol. A Urologist examined me and said your pain is not coming from the stone. They kept me for observation and sent me home following day. From start of the intense pain to finish I’d say it lasted about 48 hours or so. It would come in waves and was like nothing I’ve ever felt before. I will also mention that many years ago a former doctor ran a catscan on me (I forget why) and saw a tiny stone, he said I’d likely pass it without ever knowing. That is my only history with a stone. My older brother had a uric acid stone 20 years ago, he is now 55.
I saw a Urologist after I was discharged from hospital (2 days later) and the blood in my urine continued. He also believed the 7mm stone was not the issue but discussed the small possibility that I had passed a tiny stone without it being picked up on catscan by the ER. He ordered an xray and the report said “a 7 mm calcification overlies the medial aspect of the left renal outline. A questionable tiny calcification overlies the lower portion of the left renal outline, no calcifications are noted overlying the right renal outline.” Based on the blood in the urine I had a Cystoscopy performed 2 weeks later – and nothing was found, though he did have to dilate my urethra (I was sedated) as he could not get the scope in. Next we did a 24-hour urine collection via Litholink with the following results:
Urine volume: 2.70
SS CAOx: 1.50
Urine Calcium: 109
Urine Oxalate: 17
Urine Citrate: 782
SS CaP: 0.58
24 Hour Urine pH: 6.751
SS Uric Acid: 0.08
Urine Uric Acid: 0.520
Interpretation: High urine ph. High urine pH can promote calcium phosphate stones. When coupled with low urine citrate consider distal renal tubular acidosis. When using alkali supplements (citrate or bicarbonate) manage urine volume and urine calcium to maintain SS CaP less than 2.0.
Stone Risk Factors/Cystine Screening – Negative
Dietary Factors:
Na24: 147
K 24: 53
Mg: 59
P 24: 0.555
Nh4 24: 20
CI 24: 141
Sul 24: 23
UUN 24: 7.04
PCR: 1.0
Normalized Values:
CR 24: 1210
Cr 24/kg: 21.9
Ca 24/kg: 2.0
Ca 24/ Cr 24:
90
I returned to my Urologist who was not concerned about the mention of distal renal tubular acidosis. He’s had me order a supplement called Theracran (cranberry supplement) to take twice day for a few months to try to acidify my urine. And I will take another 24-hour urine test end of October.
Lastly – I had an ultrasound done of my kidneys last week as I was asked to fly/travel for work and I’m concerned about the stone moving. The results are confusing though! It says “There is no hyronephrosis bilaterally. There is a small right extra renal pelvis measuring 1.5cm AP dimension. There is a small echogenic focus in the lower pole of the left kidney measuring 5 mm. Demonstrates variable shadowing. Impression: Suspected small calculus lower pole left kidney. Suggest CT or KUB imagining for conformation if not performed previously.
My questions are: Due to my low urine oxalate content, should I still be vigilent about low oxalate foods all the time? Is my urine oxalate level only indicative of what I ate in the past 24 hours or is more cumulative?? I’ve increased my water intake – which is obvious due to my test results. I never watched my salt previously but had no reason to and rarely salt my food – nonetheless I have cut back on salt. I am not a big red meat eater, eat small portions of animal protein. My doctor really hasn’t advised me on any main dietary factor to prevent stones – and doesn’t even recommend removing the stone.
But the latest ultrasound concerns me. I know they are not as accurate as catscan – but is it possible I now have a 5mm stone in my lower kidney and they did not pick up the 7 mm stone in the upper pole? Or is it possible the 7mm stone dropped and the size reading is off?
I’m so concerned about having a kidney stone attack. And I swear I always have this lingering dull ache in my lower flank and sometimes I get a sharp pain. Docs say it can’t be the non-obstructing stone. I’m seeking a 2nd opinion at the end of the month. I want to consider lithotripsy – but if the 7mm stone is now in the lower pole – I have read that can be more of a challenge to blast and then pass the fragments?
I am told it is unlikely I can pass stone of that size – so I just wait for it to cause me all this excruciating pain people talk about? That isn’t really something I think I can do. But the other concern for me is do I now have TWO stones? I really don’t want the radiation of another catscan. Can MRI pick up on the stone just as well? Do I get a KUB?
I’d appreciate any feedback you can provide.
Hi Beth, I imagine you passes a small stone and have at least one more in your kidney. The CT is far more sensitive than the ultrasound so I would use the former as my guide. Your 24 hour labs are normal, so I imagine you have it about right. Your formed stones during episodic dehydration and that is not presently a problem but will be when your GI disorder becomes active again. You have no oxalate problem, and as for the urine pH it is not important. I and John Asplin wrote the litholink algorithms, so I understand why it says what it does but I also understand to ignore it for you. Your issue is to avoid dehydration as you can form stones – many people do you despite dehydration. Be sure and analyse the stone if it passes or is removed. MRI does not visualize stones. As for surgery, I would think I might wait – surgery is also a problem. If the stone comes part way own the ureter is an easier target for the surgeon – marginally so with modern instruments. Regards, Fred Coe
i Dr Coe, thanks so much for responding. Regarding my 24-hour collection results, don’t you think it would be wise to test it again once or twice since one collection only – might not show any other variables? Regarding opting out of ESWL — do you think it might not be successful or just not worth potential complications/pain as its easier to remove once it starts to pass? Aren’t there others like me who fear the pain of such an episode of a stuck kidney stone in the ureter as well as the potential of it happening during an inconvenient time such as while traveling etc? Every time I have a pain in my back I fear it’s the stone.
Why do you think the cat scan did not show a stone passing while I was in hospital with the pain? Was it too small to see possibly? Would there have been other indications of the passing stone such as inflammation? I still have microscopic blood in my urine, is that likely from the stone I still have?
Lastly the cat scan in June said stone was in mid to upper pole. But last weeks ultrasound says lower pole. It’s possible the stone dropped right?? My doc said the ultrasound was more reliable than cat scan and that this was same stone but now moved. That didn’t make much sense to me as I thought the CAT scan was much more accurate than an ultrasound based on all the reading I’ve done. How often should I monitor a 7mm stone – as I’d assume if it got much bigger it should come out?
Thank you again for your time, it is sincerely appreciated!
Beth
Hi Beth, Repetition is always prudent. Stones in the kidney that are not doing anything – obstructing, causing pain or bleeding or infection – it is unclear to me why one would undertake a preemptive surgery on their behalf. Surgery is itself burdensome. But if anxiety overcomes you, go ahead. Be rid of it, so long as your physician believes that is a reasonable and safe undertaking. As for the mysterious attack I think it might have been a tiny stone or a lot of crystals. Either way be sure you have a good prevention program in hand. Regards, Fred Coe
Thanks! I’d love to have a good prevention program in place – if someone would provide it to me! 🙂 Right now – all I can come up with is continuing to stay hydrated and managing my gastro issues to prevent dehydration. I will be seeing another doc for a 2nd opinion and will see if he recommends anything additional. Thank you again!
Hi Beth, Here is a plan that I think is very useful. Here is an overview, too. Here is a way to get the most out of your visit with the physician. Warm regards, Fred Coe
Hello Dr Coe,
I have within the last 1.5-2yrs been dealing with kidney stones. I have not been able to get a clear understanding of what is causing these or what I should be doing to prevent them, and wonder if you could help clarify? I have had four pregnancies and each pregnancy has had complications of UTI during. My first pregnancy I was hospitalized for 3 days due to UTI leading to kidney infection, was prescribed antibiotics for length of pregnancy, only blood and urine collected no further diagnostics done. 2nd pregnancy was put on antibiotics on/off for length of pregnancy after first signs of UTI. 3rd pregnancy saw dr told of history was put on antibiotics, started seeing midwife told her history and she referred me to a urologist. Urologist showed signs of uti and did renal ultrasound, didn’t hear back for length of pregnancy. thought things were normal, except did have blood in urine 1 time, increased fluid intake. 40wks passed 1 large stone and a 2nd smaller stone. went to urologist after baby was born and has x-ray done found stone stuck in right tube and a few more in kidney. Had lithotripsy done on stone in ureter. not long after this pregnancy I became pregnant again, began seeing different doctor, started having symptoms again ended up having large amount of blood in urine on multiple occasions. was put on antibiotic after hospital visit for 2 weeks. Passed 3 kidney stones during pregnancy, and had one sent to lab, also had ultrasound done and they send things looked fine. This is the info from the test result on the kidney stone: WEIGHT, STONE 0.0650 g, CALCULI COMPOSITION Result: Carbonate Apatite (Dahllite) 100%.
Thank you in advance,
Kortney
sorry for typos, holding baby typing one handed!!
Hi Kortney, You seem to be forming calcium phosphate stones, which are indeed most common in younger women and an important problem. When you are not pregnant or nursing you should have a proper evaluation to find the cause of your stones and take steps to prevent more. Here is a good outline of how to proceed. I am sure the bleeding with pregnancy was small stones or crystals themselves. Do not accept the idea that pregnancy or its associated vitamins caused the stones, it is that you are prone to them and need evaluation and long term prevention. Regards, Fred Coe
Hello Dr Coe,
I have been suffering with kidney stone around 6 yrs. Few days back I was able to catch 5mm X 5mm brownish color stone through urine. After lab analysis it appears to be made of
1st constituent:- Calcium oxalate monohydrate
2nd constituent:- Calcium oxalate dihydrate .
Can you please advise which kind of specific foods causes this stone I had? I do not eat any kind of meat. It would be really helpful to find out where I need to make changes in my daily diet.
Thanks in Advance
Nilay
Hi Nilay, These are the common calcium stones and their prevention is well described here. Regards, Fred Coe
My 14 year old has had kidney stones for years. No doctor has helped us. These are the analyzed stones – although she gets stones often.
ANALYZED KIDNEY STONES
2009 Calcium Oxalate kidney stone (Cedar Sinai Medical Center Andrew L. Freedman, M.D. – Urologist)
May 2014 CHLA Urologist Roger E. DeFilippo, M.D. – Dr. DeFilippo confirmed (after visual inspection of Hannah’s urine) that Hannah is passing sediment and kidney stones in urine; pressure in vaginal area is from passing sediment and kidney stones; Dr. DeFilippo said that kidney stones are like pearls and keep accumulating material and get bigger, but fortunately Hannah passes sediment and kidney stones before they get big
May 2014 – Kidney stone – 80% Uric Acid Dihydrate and 20% Calcium Oxalate Monohydrate – Whewellite; weight 0.0040 – CHLA
June 2014 – Kidney stone – Calcium Oxalate Dihydrate (Weddellite) 65% and Carbonate Apatite (Dahlite) 35%; stone weight 0.0010 – CHLA
Some of them look like little sticks. She is in pain so often. It seems like she gets a lot of sand and “tissue” like material in her urine. Any suggestions?
Hi Nanci, It would appear that the stones are 80% uric acid admixed with 20% calcium oxalate in May, and just a month later 65% calcium oxalate and 35% calcium phosphate. Frankly that seems odd in that uric acid and calcium phosphate stones do not usually coexist. The one crystal – uric acid – is stable in acid urine, the other – calcium phosphate – is stable in alkaline urine. The exception to this general rule is when urine volumes are very low or excretion rates for calcium are very high. Put another way, if you have transcribed the reports correctly and if the laboratory has analysed the stones correctly, this is an unusual and very complicated problem. One main approach is the 24 hour urine testing, which is absolutely needed here. Likewise she needs blood measurements to exclude systemic causes of stones. Here is an outline of what one needs. You physician knows all this but perhaps having the outline in hand will help keep things together. The links in the article go to more detailed articles which fill in details. Given the testing and the stone analyses perhaps some sense may be made of what has happened here and what can be done to stop it. Because of the variability of the stone compositions I would gather more of her stones and have many more analysed so as to get a perspective on what are the main crystals forming. Regards, Fred Coe
My 14 year old has had kidney stones for years. No doctor has helped us. These are the analyzed stones – although she gets stones often.
ANALYZED KIDNEY STONES
2009 Calcium Oxalate kidney stone (Cedar Sinai Medical Center Andrew L. Freedman, M.D. – Urologist)
May 2014 CHLA Urologist Roger E. DeFilippo, M.D. – Dr. DeFilippo confirmed (after visual inspection of Hannah’s urine) that Hannah is passing sediment and kidney stones in urine; pressure in vaginal area is from passing sediment and kidney stones; Dr. DeFilippo said that kidney stones are like pearls and keep accumulating material and get bigger, but fortunately Hannah passes sediment and kidney stones before they get big
May 2014 – Kidney stone – 80% Uric Acid Dihydrate and 20% Calcium Oxalate Monohydrate – Whewellite; weight 0.0040 – CHLA
June 2014 – Kidney stone – Calcium Oxalate Dihydrate (Weddellite) 65% and Carbonate Apatite (Dahlite) 35%; stone weight 0.0010 – CHLA
Some of them look like little sticks. She is in pain so often. It seems like she gets a lot of sand and “tissue” like material in her urine. Any suggestions?
Hi Nanci, It would appear that the stones are 80% uric acid admixed with 20% calcium oxalate in May, and just a month later 65% calcium oxalate and 35% calcium phosphate. Frankly that seems odd in that uric acid and calcium phosphate stones do not usually coexist. The one crystal – uric acid – is stable in acid urine, the other – calcium phosphate – is stable in alkaline urine. The exception to this general rule is when urine volumes are very low or excretion rates for calcium are very high. Put another way, if you have transcribed the reports correctly and if the laboratory has analysed the stones correctly, this is an unusual and very complicated problem. One main approach is the 24 hour urine testing, which is absolutely needed here. Likewise she needs blood measurements to exclude systemic causes of stones. Here is an outline of what one needs. You physician knows all this but perhaps having the outline in hand will help keep things together. The links in the article go to more detailed articles which fill in details. Given the testing and the stone analyses perhaps some sense may be made of what has happened here and what can be done to stop it. Because of the variability of the stone compositions I would gather more of her stones and have many more analysed so as to get a perspective on what are the main crystals forming. Regards, Fred Coe
I have 3 stones 11mm, 12mm, 9mm in the left ureter & 2 stones 5mm, 7mm in the right ureter. Stone analysis: 50% Calcium oxalate monohydrate, 30% Calcium oxalate dihydrate, 20% Calcium phosphate (apatite). I have had lithotripsy on the left that didn’t work, I am scheduled for a Flex URS, holmium lasertripsy on the right. What are the chances of this working? Also what I diet should I follow to prevent these stones and would I need medication for prevention?
Thank you.
I have bilateral urethral stents that were placed 10/6/2016 through nephostomy tubes which I needed for severe hydronephrosis (nephostomy tubes were removed before I left the hospital). The are painful and I would like removed ASAP…ugh
Hi Wendy, Having many calcium oxalate stones surely means that prevention is of the highest importance. The plan for URS is very sound and you should expect excellent results. That you had hydronephrosis on both sides is unusual and speaks for a high stone rate. The 20% CaP in your stones is also important, in that gradual conversion from calcium oxalate to predominantly calcium phosphate is common and also not ideal as CaP stone disease is often more active and involves calcifications inside the kidney tubules. Take a careful look at this overview of prevention. Also, this more focused five step article. Most of all, you probably fit into the idiopathic calcium stone former category, and this article speaks directly to them. But, the five steps and putting it altogether are basic first steps because sometimes there are special problems, and underlying systemic diseases lurking that need special treatment. Let me know, regards, Fred Coe
I have 3 stones 11mm, 12mm, 9mm in the left ureter & 2 stones 5mm, 7mm in the right ureter. Stone analysis: 50% Calcium oxalate monohydrate, 30% Calcium oxalate dihydrate, 20% Calcium phosphate (apatite). I have had lithotripsy on the left that didn’t work, I am scheduled for a Flex URS, holmium lasertripsy on the right. What are the chances of this working? Also what I diet should I follow to prevent these stones and would I need medication for prevention?
Thank you.
I have bilateral urethral stents that were placed 10/6/2016 through nephostomy tubes which I needed for severe hydronephrosis (nephostomy tubes were removed before I left the hospital). The are painful and I would like removed ASAP…ugh
Hi Wendy, Having many calcium oxalate stones surely means that prevention is of the highest importance. The plan for URS is very sound and you should expect excellent results. That you had hydronephrosis on both sides is unusual and speaks for a high stone rate. The 20% CaP in your stones is also important, in that gradual conversion from calcium oxalate to predominantly calcium phosphate is common and also not ideal as CaP stone disease is often more active and involves calcifications inside the kidney tubules. Take a careful look at this overview of prevention. Also, this more focused five step article. Most of all, you probably fit into the idiopathic calcium stone former category, and this article speaks directly to them. But, the five steps and putting it altogether are basic first steps because sometimes there are special problems, and underlying systemic diseases lurking that need special treatment. Let me know, regards, Fred Coe
Hi, what a beautifully written article, fun to read even. I couldn’t see what black stones usually are? Waiting in the analysis – had it out surgically today. You put in some really important information. I want to send it to all Dr’s and say, please get your patients to read this and find out about their stones. I for one don’t want anymore.
Hi, what a beautifully written article, fun to read even. I couldn’t see what black stones usually are? Waiting in the analysis – had it out surgically today. You put in some really important information. I want to send it to all Dr’s and say, please get your patients to read this and find out about their stones. I for one don’t want anymore.
Thank you, Joanne; be sure and get a copy of the actual analysis, not word of mouth. When you have it get prevention. Here is a good overview with links to the details. Regards, Fred Coe
Hello 🙂
here are my recent stone results.
Calcium Phosphate 05
Ca Oxalate Monohydr. 70
Ca Oxalate Dihydrate 25
Weight 215.5
Size Specimen received as fragments. (broken up from lithotrypsy)
Color Brown
I am 46, have suffered with stones off and on since 2011, this is the first that has needed stents and litho for removal.
Thanks for any advice on how to prevent 🙂 Cathy
Hi Cathy, You have done the right thing by getting your stone analysed and keeping a copy of the results. Your stone is the common calcium oxalate stone. Here is a good article on how to do prevention. Here is an overview that includes this article and other ones as well. Here is the whose approach but more as the underlying science. You will prevail. Regards, Fred Coe
Hello 🙂
here are my recent stone results.
Calcium Phosphate 05
Ca Oxalate Monohydr. 70
Ca Oxalate Dihydrate 25
Weight 215.5
Size Specimen received as fragments. (broken up from lithotrypsy)
Color Brown
I am 46, have suffered with stones off and on since 2011, this is the first that has needed stents and litho for removal.
Thanks for any advice on how to prevent 🙂 Cathy
Hi Cathy, You have done the right thing by getting your stone analysed and keeping a copy of the results. Your stone is the common calcium oxalate stone. Here is a good article on how to do prevention. Here is an overview that includes this article and other ones as well. Here is the whose approach but more as the underlying science. You will prevail. Regards, Fred Coe