LISTS – AND LISTS
I know you are all looking for THE list. Here is one from a reliable source I have have downloaded on my site to a separate document so it opens with one click.
The reliable source, as it turns out, needed some updating. Dr Ross Holmes, professor, School of Medicine, University of Alabama, was kind enough to review the work of Dr. Michael Liebman who is a professor of Human Nutrition and Food Option at University of Wyoming and determine which food entries on the Harvard list needed changing. We cannot change the original but we have updated our lists accordingly and annotated updates with *** marks. So the lists here are the most recently edited available at present.Fred Coe and I have updates and annotated the list for those with a tendency to perfectionism: Updated table of oxalate foods. Set it at 50% for easier reading. Get yourself acquainted with the lists. They will tell you much of what you need to know. A lot of it will even surprise you. You are not as restricted as you think you are or as you have been told.
A more dramatic list is the 177 high oxalate foods we distilled out of the big list. Here are culprits! Not on this list? Probably not very high in oxalate so far as we know – with perhaps a few exceptions. Note that quantity is critical. For example black pepper is high in oxalate but the amounts used are small enough that total oxalate intake from it is negligible.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
LET’S DIVIDE AND CONQUER
FOODS TO WORRY ABOUT
A List of Concerning Foods
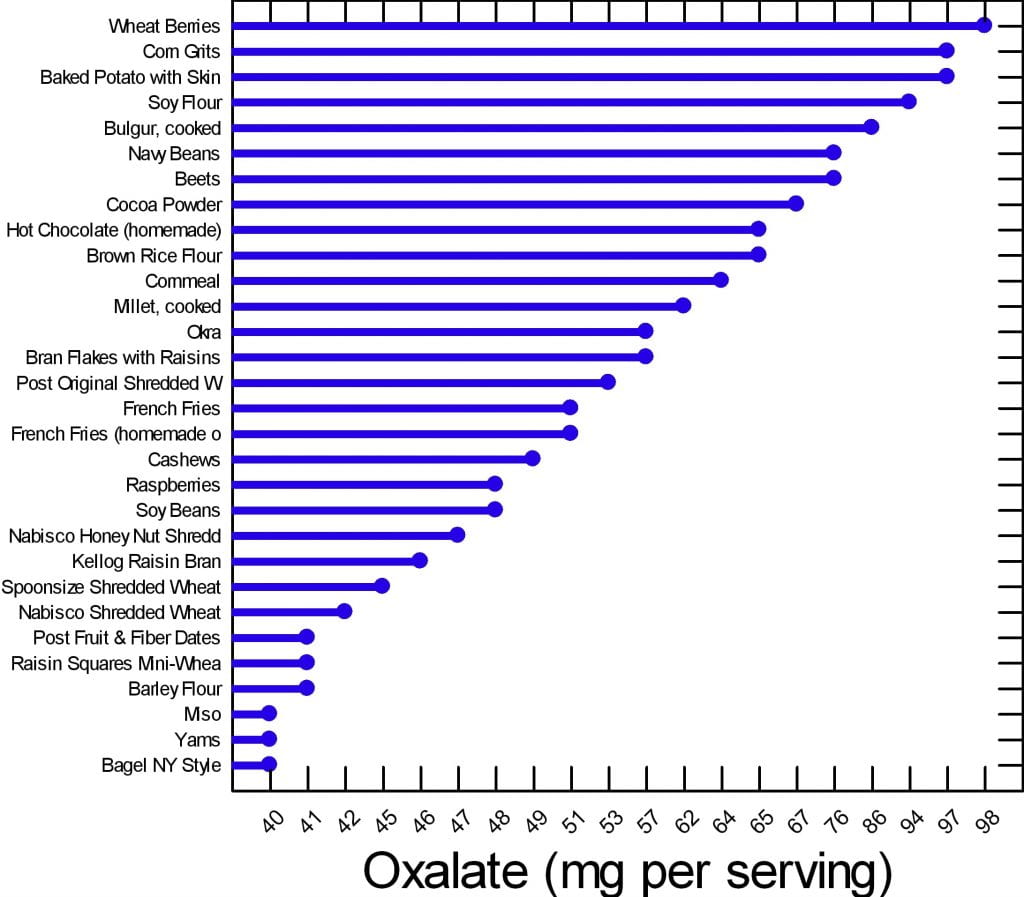
We have created two graphs for this article. Of the 177 foods on our master list, many are of concern but can be used in your diet if you control the portion size and how often you use them. There are 30 of them that are worrisome enough to deserve special attention.
Here are the 30. The graph shows mg of oxalate in a common portion. The details of the portions are in the complete list. The foods have in common that all contain at least 40 mg/serving. All other foods for which we have reliable data have less oxalate per serving.
Your budget is about 100 mg/day.
What does this graph mean? Does it mean you can never have chocolate, or a baked potato?
No.
It means if you want to use your whole budget on a treat, do it, but keep track and make sure you do not overspend in any meal or in any one day. Have your baked potato, but maybe share half with your partner. Or, have some hot chocolate but make it with milk because calcium helps reduce oxalate absorption. Eat your cashew nuts, but pay attention to how many. If one handful leads to ten, you cannot have them.
FOODS TO AVOID
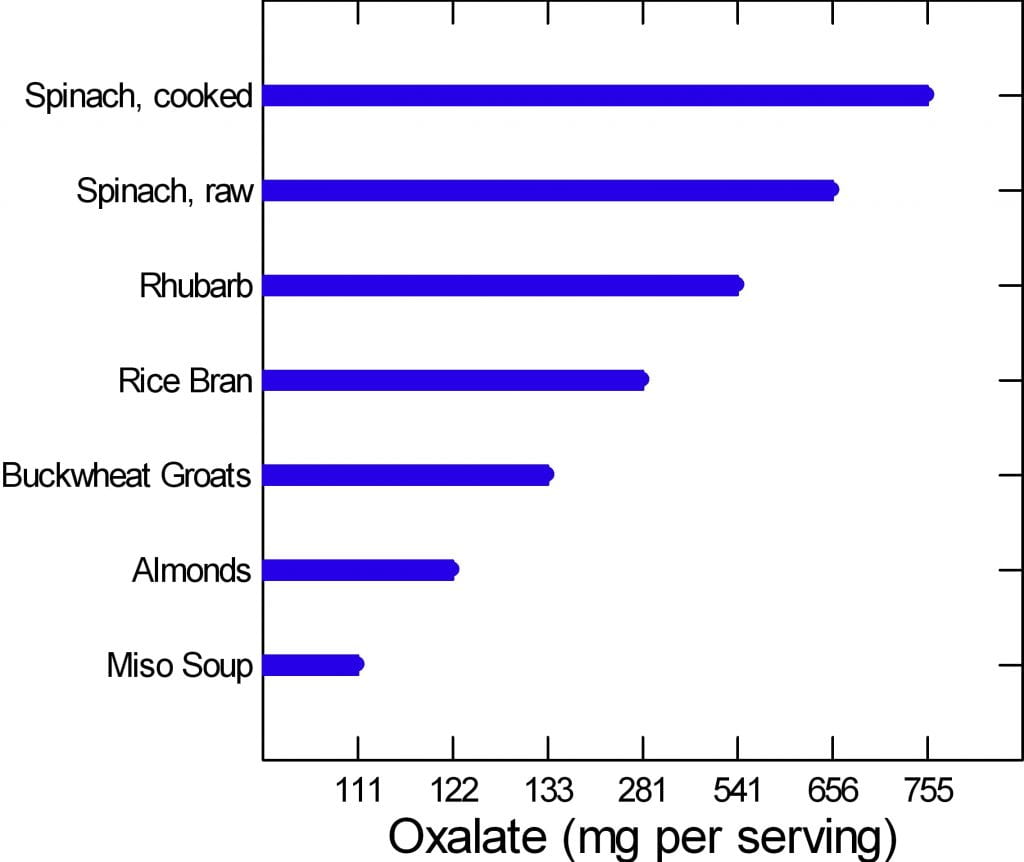 The graph to the left is of the very few dangerously high oxalate foods.
The graph to the left is of the very few dangerously high oxalate foods.
There are only six foods, but spinach, being worst of all, has two entries. Be careful of this plot because of its range. It begins at 100 mg/portion and rises to 755 mg/portion in only 7 steps, so the distance from miso soup to spinach is about a 7 fold increase.
Rhubarb and spinach are so high you just cannot eat them. Rice bran is something few will miss, the same for buckwheat groats.
People like almonds but have a hard time controlling portion size. If you can keep it to 11 almonds a day – the portion size that gives 122 mg of oxalate, alright. Otherwise stay away from them.
If you have to eat any of these foods, caution is hardly a strong enough word.
Are you sure you need to eat them?
Why?
WHAT ARE WE SAYING?
We are saying that oxalate is common in foods, and that you have to be careful, but care is a scarce resource. How much care can you give every bite? The graphs say if you eat moderately high oxalate foods – the first graph – be careful.
Watch portions.
If you are eating one of the six dangerously high oxalate foods, stop eating it.
It is too hard to be careful with those six foods. They have too much oxalate for most of you to handle. So, just say no.
WHY BELIEVE OUR DATA?
These data arose from a major effort at the Harvard School of Public Health. A world class expert has curated it twice. Harvard can be wrong and so can Ross Holmes, but both will tend to be wrong less often than the average persons who attempt to put complex data into the public domain. We have always appreciated comments, and if anyone has a peer reviewed publication with different food oxalate levels than ours, we will read the paper and see if it warrants our making a change.
Medical research is endlessly argumentative, and food oxalate is no exception. A recent paper contrasts findings from 6 websites and 2 applications and finds some wide variations. Of the sites, the Harvard site – used here as our reference, and the Wake Forest site – which is a legacy of an outstanding investigative group have most standing with me. Leaf through the comparisons between them in the 4 charts and in the large table at the very end. On the whole differences are modest. The hyperoxaluria and oxalosis list from the paper has been withdrawn from their site.
DO YOU NEED A LIST?
Sure, a list is nice. But we helping you here. Lists can run on to hundreds of foods. The picture is meant for focus. Here are the ones to focus on.
Many of you leave the doctor’s office thinking you will never be able to eat a fruit or vegetable again. If that wasn’t bad enough chocolate and nuts are gone, too. Some of this sadly is true, most of it is not. I am here to bring you good news: Almost everything, high oxalate or not, can be incorporated into your diet safely.
Do you need a low oxalate diet? You may if your stones contain calcium oxalate crystals and your urine oxalate is high enough to pose risk.
If you do need a low oxalate diet, what is your goal? Less than 100 mg of diet oxalate is good; less than 50 mg is ideal.
If you want to read some of the science about urine oxalate and risk of stones and about how we get to the diet oxalate goals, it is summarized at the end of this article.
Here we assume you do need to lower the oxalate in your diet.
CALCIUM FIRST
Low calcium diets can raise urine oxalate, and the solution may be as simple as a proper calcium intake. There is every reason for stone formers to eat 1000 mg of calcium daily to protect their bones. The common hypercalciuria of calcium stone formers puts bones at special risk when diet calcium is low.
Before changing your whole life around, ask yourself if you are avoiding calcium foods. If so, add them back and ask your doctor to check your urine oxalate again. It may fall enough that a low oxalate diet is not necessary.
If low calcium intake is not your problem, and you need a low oxalate diet, here is my take on how to do it.
WHAT IS THE DIET OXALATE GOAL?
Typical diets contain upward of 200 – 300 mg of oxalate. For stone prevention, a reasonable goal is below 100 mg of oxalate daily. An ideal would be about 50 mg daily if that can be accomplished.
To get there, consider the oxalate contents in common serving portions of all of the foods, and make up a plan for yourself.
FRUITS
FRESH
Everyone who comes to me is very unhappy thinking they can never have a berry again. This is Baloney. The only berry that is very high in oxalate is raspberries (look at the list). On the other hand, people do not realize avocado, oranges, dates, and even grapefruit and kiwi are very high and need caution.
This doesn’t mean you can never have these healthy treats. If you incorporate any of these high oxalate fruits into your morning yogurt you can reduce some of the effects of the oxalate content.
Also look at your portion sizes. You really cannot eat a lot at any one time. Dates are not a good bargain: One date is 24 mg!
CANNED OR DRIED
Canned pineapple is a problem.
Dried fruits have to be a worry because the water is taken out, so a ‘portion’ of dried fruit can be gigantic in oxalate content. Figs, pineapple and prunes are standouts. Just think: 1/2 cup of dried pineapple is 30 mg – not a lot of fruit for a lot of oxalate. If you want dried fruit, think about apples, apricots, and cranberry as lower oxalate options.
VEGETABLES
Spinach and rhubarb are standouts; stay away.
Other vegetables you need to be aware of are tomato sauce, turnips, okra, and yams (sweet potatoes) along with beans of different sorts.
I am not in the business of taking healthy foods away from people. But in the cases above you really must limit; there is just too much oxalate and these foods do not pair well with high calcium foods the way fruits can be mixed right into your yogurt or cereal and milk.
Many of you have been told to stay away from all green leafy vegetables. This is not true. Look at the list. There are plenty of salad options still available for you including kale. Even though tomato sauce is high in oxalate (see below) that is because of concentration. A whole medium tomato is only 7 mg and who eats more than one at a time?
Many of the salad vegetables are so low in oxalate they are freebies. Eat what you want.
POTATOES
These are Trouble! I put them into their own separate group even though they are vegetables.
From french fries to baked potatoes they are very high oxalate items. One ounce of potato chips has 21 mg of oxalate and who eats one ounce? Not I. Baked potatoes are terrible. One comes in at just under 100 mg of oxalate. Mixing sour cream into the potato will not help much; one tablespoon of sour cream contains only 14 mg of calcium. One ounce of cheddar cheese contains 200 mg of calcium, which could help, but it increases calories, salt and fat. But all in all, why struggle so hard? Potatoes are not ideal for stone formers.
DAIRY PRODUCTS
They have no oxalate. They are your main source of calcium. Use them. They can add a lot of salt – cheeses – and can be caloric. But they reduce oxalate absorption and preserve your bones.
For a stone former who has to watch salt intake, increase calcium intake, and lower oxalate intake, here is how to do that. You cannot have as much cheese as you want because of the salt. So portion sizes are very important. Yogurt, milk, even ice cream are good bargains – modest sodium and high calcium. These are a great place to add in a wee bit of chocolate – high oxalate foods – for those of you who cannot live without these high oxalate treats.
BREADS AND GRAINS
Some of the basic ingredients to make these foods are very high. White flour and brown rice flour are high in oxalate so everything you make from them will be high.
BREADS
Even so, as far as kidney stones go, breads are mainly alright because of portion size: not that much flour so one slice is 5-8 mg. French toast and New York style bagels top the list at 13 mg for two slices and 40 mg for one bagel – as much as anyone will eat of either food.
PASTA RICE AND GRAINS
Spaghetti, one cup cooked is 11 mg and most of us eat more than one cup.
Buckwheat groats, one cup cooked is 133 mg – I don’t see many of you saying ‘darn it’ or taking to your bed, but beware. Millet and bulger, wheat berries, rice bran, corn grits, and corn meal, these are widely used and are high. If you are using these, be thoughtful.
Here are some low oxalate options in this category: White rice, hummus, corn flour, corn bran, flax seed, and oat bran are popular and safe.
MEAT PRODUCTS
Since oxalate is only found in plant foods, all the meats are safe. Fish, too.
For our vegetarian friends, tofu and veggie burgers are very high.
NUTS AND SEEDS
These are just dangerous for two reasons.
Obviously they are very high in oxalate.
Secondly, I don’t know anybody who just has a few nuts at a time.
Just like chips no one eats one – the whole jar is more like it.
But, for one cup of pumpkin sunflower or flax seeds the highest is only 17 mg of oxalate and none for flax. For those of you who love foods in this category seeds are the better choice and they can be sprinkled on yogurt and ice cream.
SWEET STUFF
I have good news for my chocolate lovers. I know most of you have been sent home with a list and chocolate is high on it. But if you look at the numbers nuts are a lot worse than chocolate. Chocolate can be mixed in with dairy products, too, so as to reduce oxalate absorption.
Even so I do want to point out that half a brownie is on the high side, and who eats one half?
You can still satisfy your sugar craving but pay attention to your portion size.
Keep in mind, however, that sugar loads increase urine calcium loss which increases stone risk, so there are two reasons why this food group can be a problem.
But even without chocolate, you eat a lot of flour when you eat a piece of cake, so cake can be a problem – about 15 mg per piece, like french toast. Pies are half the risk because of their fillings – unless they are chocolate pies!
CRACKERS AND CHIPS
The big enemy here is potato chips. A one ounce serving contains a whopping 21 mg of oxalate. I repeat: A one ounce serving.
Your best bet in this category if you’re looking for something crunchy is corn chips – one ounce is 7 mg, popcorn – one cup is 5 mg, and pretzels, one ounce is 5 mg.
Crackers are OK mainly because they are small and the amount of flour is not that much.
BEVERAGES
PLANT SOURCES
Hot chocolate is the clear loser at 65 mg per cup; carrot juice is the runner up at 27 mg per one cup. Lemonade, tea, tomato juices, rice dream and the like are better but still high. The are 15 – 18 mg per serving. Lemonade – frozen concentrate – is 16 mg per 8 ounces so be careful about this as a source of citrate.
Soy milk, for those of you who prefer it, is not a good option. It is very high at 20 mg per cup. We have no data from standard sources for rice milk, cashew milk, and coconut milk; almonds are high in oxalate so the almond milk product will certainly be high.
Tea is so commonly used, here are the details. If you brew your own tea it is high in oxalate. The longer you steep your tea, the more oxalate it will have in it. If you use a sweetened instant iced tea one cup has 0 mg of oxalate.
Here are some juices that are low in oxalate and better substitutes: Apple juice, apricot juice, orange juice, grapefruit juice, grape juice. For all the lemonade drinkers, diet lemonade is low in oxalate.
Here is something very important: Coffee is oxalate free – almost, 1 mg for a cup (2 mg/cup for decaf). We already told you that coffee drinkers have a reduced stone risk, so lets debunk the coffee myth here: Drink it as you wish.
DAIRY SOURCES
Everything is good except chocolate milk. Even that is only 7 mg a cup for a sweet treat here and there.
ALCOHOL
What tops the list in this category is a can of beer: 4 mg of oxalate. All the rest are low and, frankly, the oxalate in a can of beer comes with a lot of fluid. This is not the problem area for stone formers.
WATER
If I didn’t say this to you I could not sleep well tonight. Water is the clear winner in this whole category. It is free of calories, sugar, and oxalate. Please use it as your main beverage and supplement with the items above.
SPREADS AND SAUCES
Chocolate, miso, peanut butter, and tahini are all high.
SOUPS
Miso soups is extremely high – 111 mg/cup. Lentil soup is high, and so is clam chowder – the potatoes.
BREAKFAST FOODS
This is a dangerous meal if you are a cereal lover. Many cereals are high in oxalate. I am afraid you need to look them up in the list by brand. Unfortunately the healthier cereals are highest in oxalate because they contain more plant based ingredients. Probably having milk in your cereal is wise, but we have no data to show.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
HOW DO WE MANAGE ALL THIS?
The first thing you need to do is to learn and remember what are the highest oxalate foods and beverages. Without this in mind it is impossible to shop and cook intelligently. Here is a short list of the highest oxalate foods all in one place.
BREAKFAST
For those of you who love cereal because it is quick and easy check out the list and see if the one you love is high in oxalate. If it is, choose the next best one with lower oxalate. Put milk in the cereal.
Alternatives to cereal that are also quick and easy: Yogurt or cottage cheese and fruit. The only fruits to worry about are raspberries because no one puts oranges on their yogurt. Bananas, peaches, blueberries and strawberries are perfect toppings.
More trouble, but no oxalate, eggs any way at all. Boil a batch on Sunday and have them for the week for breakfast, and snacks, too.
Your breakfast coffee is free and so is your water. For juices use orange, apple, pineapple, grapefruit – all great. If you want tea, don’t steep more than a minute and consider adding milk to it. Green tea is better than black.
LUNCH
Typically you are grabbing a salad or a sandwich for lunch, so what now? Many clients tell me they no longer eat salads because their physicians told them to stop all green leafy vegetables.
I’m bringing salads back to you.
Arugula, iceberg, romaine lettuces, and kale, are fine as your base. Stay away from spinach. Here are good toppings. Cauliflower, corn, cucumber, mushrooms, onions, peas, scallions, squash and zucchini are all fine. Tomatoes are fine, too; it is only the sauce that is high. Broccoli and green pepper are moderately high so watch the portion size.
Sandwiches will cost you between 12 and 16 mg of oxalate depending on the bread you are using – 2 slices. This doesn’t mean you can never have a sandwich, it just means you have to keep track of how much. You can have 50 to 100 mg daily. What goes inside between the two slices of bread is usually cheeses and meats which are oxalate free. So sandwiches are not something to be afraid of.
SUPPER
Beef, chicken and fish are all fine, and those the main courses for most of us. You will run into problems if you are a pasta or potato eater. If you are you need to limit the amount of times you have these foods each week and also the quantity each time you use them. Substitutes are a problem: White rice is a nice substitute for potatoes but there are few others. It is more veggies that have to fill in – very healthy but not as much fun.
Here is a recipe for cauliflower – ‘mashed potatoes’ you will like and even think, sometimes, is the real thing. There are many versions on the web, choose the one that makes you happy but be careful about the ingredients.
There is also quinoa which is not on our lists, but may well be high. A recent scientific article on this plant does not give oxalate contents which suggests they are not reliably known.
I have recently put together a private FB page called THE Kidney Stone Diet. It is a group that helps educate you on your physician prescribed treatment plans. As you can imagine, oxalate comes up in many posts. I moderate it to keep it clinically sound. Come on over and join the discussion!
URINE OXALATE AND RISK OF KIDNEY STONES
I promised you some science – here it is for those interested. It concerns only highlights from the food – urine oxalate research recently performed and seemingly germane to the problem of how stone formers should control oxalate intake.
The most useful data about urine oxalate we have so far is from three cohorts studied by Dr. Gary Curhan. Two are cohorts of nurses one a cohort of physicians. These people have kept track of many aspects of diet and health for decades, and among their records are onset of kidney stones.
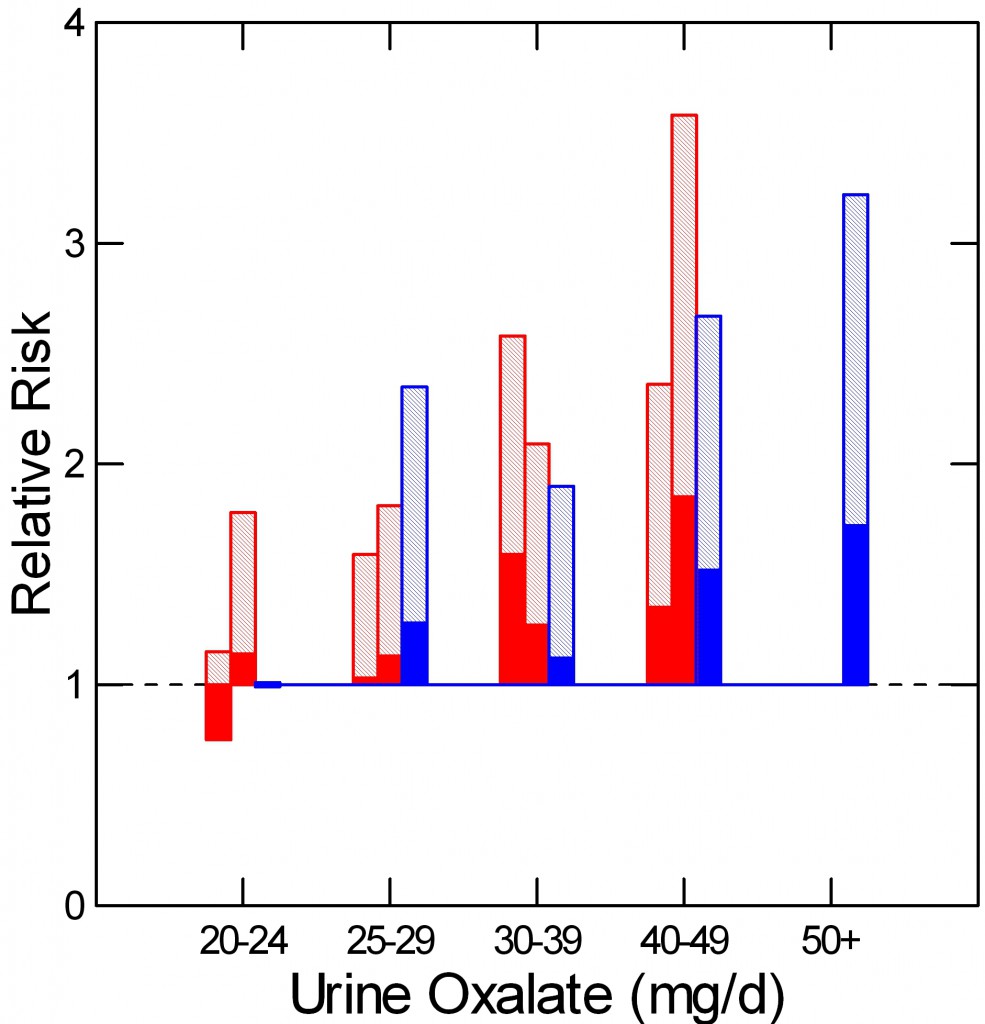 As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
The two nurse cohorts are red, the physicians – all men – are blue. The dotted line at 1 is the risk threshold: Above that line, risk is present.
The top of each crosshatched bar shows the mean relative risk for each of the five urine oxalate ranges. Clearly the mean goes up as urine oxalate goes up.
But the mean relative risk has a range of uncertainty around it. The bottom of the solid portion of each bar is the lower 95th percentile for that range of uncertainty. When that bottom lies above 1, risk is very likely to be present.
For both the women and men groups, that point is reached between 25 and 30 mg of urine oxalate a day. Therefore one wants to try to get urine oxalate below 30 mg daily and even lower, below 25 mg daily if possible. The average urine oxalate excretion among the women in this study was close – 26 and 28 mg/day for those who did not form stones and just a bit higher for those who did – 28 and 30 mg per day. The men are a problem: 39 and 41 mg/day for those who did not and those who did form stones.
This is not diet oxalate, it is urine oxalate. Urine oxalate is how much the body makes and how much is absorbed from foods. Mostly, we can control only the second part – how much is in the food.
HOW MUCH DIET OXALATE DAILY
All dietary advice depends on having a reasonable goal in mind for oxalate intake. My goal of 50 – 100 mg of oxalate from food daily is not unreasonable given the research that has been done in normal people and stone formers.
Holmes and colleagues found a urine excretion of oxalate of about 10 mg/gm urine creatinine in normal 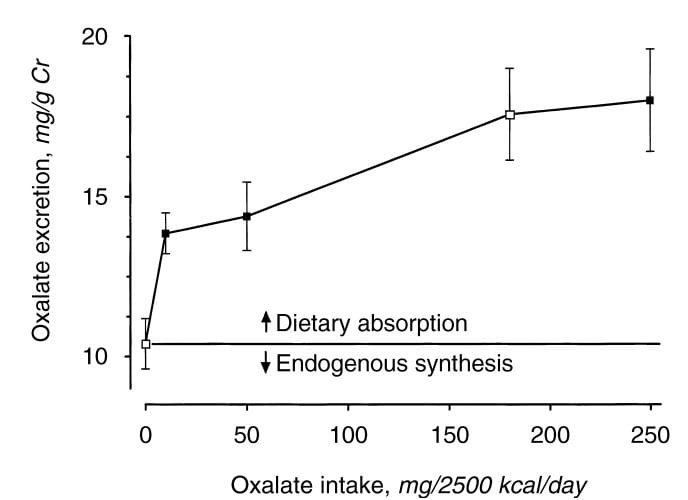 people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
From this work the percent oxalate absorption could be calculated as around 10 – 15% and the contribution of diet oxalate to urine oxalate excretion as around 25 – 40% when intake of oxalate was between 50 and 350 mg/2500 kcal. Therefore one can consider a whole food 1000 mg calcium 50 mg oxalate as a usable low oxalate diet, and a 150 – 250 mg oxalate diet as relatively high.
The balance between diet calcium and diet oxalate does not matter greatly if diet calcium is high. Among normal men and women eating 1000 mg/day of calcium and 750 mg/day of food oxalate, 24 hour urine calcium was about 110 mg/day and oxalate about 44 mg/day.
If the calcium oxalate balance is altered so calcium intake is 400 mg and 20 mg of oxalate at breakfast and lunch, and 200 mg of calcium and 710 mg of oxalate at dinner, as compared with simply 333 mg of calcium and 250 mg of oxalate in all 3 daily meals, urine oxalate is lower after the high calcium low oxalate meals, but only slightly higher after the high oxalate low calcium evening meal than when calcium and oxalate intakes were balanced. This means that when diet calcium is at least 1000 mg daily the balance of calcium to oxalate within any one meal is not likely to affect stone risk.
Seiner and colleagues make clear that stone formers are different from normal people. They divided male and female stone formers into 2 groups of 93 people each, one with urine oxalate above 0.5 mmol (~50 mg) of urine oxalate daily and the other with urine oxalate below 0.4 mmol (~40 mg) daily. They found virtually identical calcium and oxalate intakes: 845 vs. 812 calcium and 101 vs. 130 mg daily of oxalate respectively in the lower and higher urine oxalate groups. But the below 0.4 mmol group excreted only 27 mg of oxalate daily on average, whereas the high oxalate group excreted 64 mg daily. In other words diet was not responsible for the higher urine oxalate excretion, suggesting a difference of oxalate absorption. Those prone to high oxalate excretion seem, therefore, to most need diet modification.
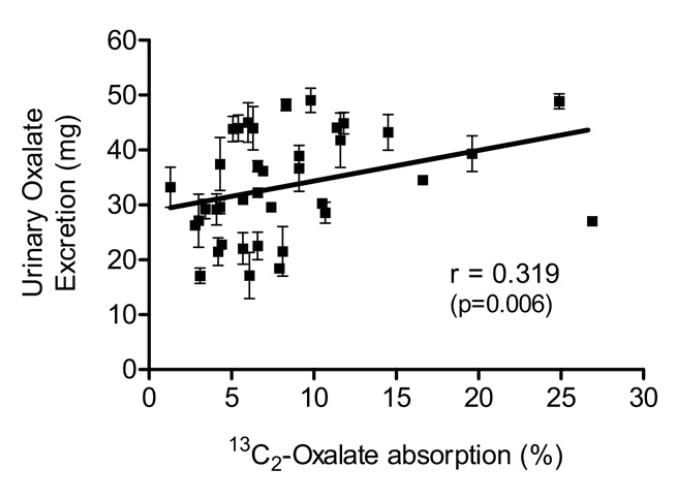 Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
PROTEIN AND GELATIN
Diet protein intake does not affect urine oxalate excretion. In 11 normal people fed a 1000 mg calcium, 51 mg oxalate, 3000 mg sodium fixed diet, varying protein intake from 0.6 to 1.6 gm/kg/day – a very wide range – did not alter urine oxalate appreciably (mean values were 23, 23, and 25 mg daily for the three protein intakes) even though oxalate precursors like glycolate rose markedly (25, 22, and 46, mg daily).
Jello is a source of hydroxyproline which converts to glycolate and oxalate, and oral loading with gelatin can raise urine oxalate. Ten normal people eating a 1000 mg calcium, 150 mg oxalate diet (typical normal level) were fed supplemental gelatin as one quarter of daily protein intake. Urine oxalate was 24 mg daily vs. 17 mg daily when the same diet was supplemented with whey protein – containing little hydroxyproline – as a control. So lots of jello is not an ideal plan for stone formers.
Where does this leave us about how much oxalate is alright for a day. If diet calcium is high, as it should be, at about 1000 mg, then one should try to limit diet oxalate below 100 mg daily. Perhaps this is most important in those patients whose baseline oxalate excretions are higher – in the range of above 40 mg daily.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life.
For those who need special help, I run an online course: The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.



I love peanut butter with my oats in morning 😞 what can I substitute for that ?
Can I use NUT FREE peanut butter which is made out of toasted Soya and Soy oil.
Or is soy no good also ??
I have to reduce my Oxalate levels. Please suggest something
Hi Evan,
Make sure you go to my site where you can find all your answers about the kidney stone diet. But you can certainly have PB. Two tablespoons is 26 mg of oxalate. The problem is people just get a spoon and eat right from the jar without getting their calcium needs met and they do this for years. That is what can contribute to stones. Also, this is so much more than just oxalate. The kidney stone diet includes lowering sodium, added sugar, meat protein, increasing your daily calcium and of course fluids. Go here for your oxalate stuff which includes a free oxalate calculator. kidneystonediet.com
Best, Jill
Is Anything with Soy high in oxalate??
Hi Evan,
Be careful of soy products, they tend to be on the higher side. This doesn’t mean that you cannot eat foods like tofu, it just means to not overeat it and watch portion size. Get your daily amounts of calcium per day by food whether non dairy or dairy.
best, jill
Hi Jill. The materials you provide are really helpful. I was so confused finding resources that were simply contradicting each other. Your list seems to be a good indicator and it makes me readjusting my diet little by little. Your explanation has also helped. Could I please take this opportunity and ask about a few products that I’m not really sure about?
– how about cinnamon? (some sources claim that it’s high in oxalates)
– olive oil and vinegar (incl. balsamic); (olive oil seems to be low; saw confusing info about vinegar, how about that
vin+lemon+water mix?)
– nuts-based oils (walnut, hazelnut); nuts are high, what about oils?
– pomegranate (any info?)
Kind regards!
Hi Martin,
Oils have no oxalate. Cinnamon is high, but portion not perfection. I have a video on pomegranate on my YouTube channel.https://www.youtube.com/watch?v=1lLQW5-HnKQ
Best, Jill
How to I add calcium without consuming dairy?
Hi Shauna,
I have an excellent article for people that do not use dairy as a calcium source. Go here:https://kidneystonediet.com/16-non-dairy-calcium-sources-for-kidney-stone-formers/
Best, Jill
Calcium and oxalic acid form calcium oxalate which are water insoluble and difficult to excrete by the kidneys. This is valid for most calcium and organic acid salts (citric, malic acid). Do I understand you correctly that you recommend to consume calcium with oxalic acid rich foods to promote the excretion of calcium oxalate? I think adding sodium bicarbonate to oxalic acid rich foods would be a wiser choice. Sodium bicarbonate keeps ocalates in solution and facilitates excretion by the kidneys. Good luck!
Hi Arnold, Thanks for the thoughtful analysis. You are right of course, but the system I am describing is in the intestine. Higher diet calcium will reduce absorption of oxalate into the blood and thereby reduce its level in the urine so crystals will have less supersaturations to drive their nucleation and growth. Regards, Fred
Hi, Jill. Is there an oxalate value available for lentils? (I only see lentil soup on the list.) Thanks.
Hi JC,
You can certainly have them. Harvard didn’t study them, don’t overeat them, get your calcium each day and my patients do just fine.
jill
Oxalates are only in plant foods…..then why have I seen sardines and liver listed as moderate oxalate foods? I don’t know about your lists. I’m talking about ones I found on upmc.com
It’s endlessly frustrating to find conflicting information. Sweet potatoes are high oxalate, no they’re not. Potato skins have the most oxalates, the flesh is “fine”.
Hi Jodie, meats have no oxalate, they have precursors from which oxalate can be made but that is a tenuous reason to list them as oxalates – wrong, to me. My lists are not mine, they arose from the Harvard school of Public Health, and were curated by an expert in the science of food oxalate. Much data for food oxalate came from that expert, and in this article he gives the (modest) amount of oxalate (29 mg/100 gm) in a sweet potato. In the same article he gives a value of 24 mg/100 gm for potato. I show this article because it was an early – founding almost – article in the field. The lists here are the accumulation of data to about 4 or more years ago. As for other sites, I cannot comment – too many, life is too short. Regards, Fred Coe
I am looking for a protein shake option with no whey, soy, or gluten. I’ve found a pea protein called Naked Pea. Do you think this would be a low oxalate food?
Hi Ashley,
See what I say about protein shakes here:https://kidneystonediet.com/are-your-smoothies-causing-kidney-stones/
Jill
I’ve been consuming a meal product called Huel. The company reports that the testing lab they use cannot test for oxalate because there isn’t any in the product. There may be some for the chocolate flavor though.
Dear A.
I am not a fan unless this product is for once in awhile. I don’t think that these drinks and powders teach people how to eat healthy. But we all know I am a pain in the tush! As far as oxalates no company tests for them as it is very expensive to do so and also hard. But to say that there are no oxalates in their products? Not so sure about that as they do use brown rice and brown rice is HIGH in oxalate. I am guessing they don’t know much about oxalate at all and just told you that.
But again, I am a pain in the tush,
Jill
Hey A. Matulich, they did an oxalate test on some of their products: mg of oxalic acid per 100g of Huel product.
v3.0 UU – 40mg/100g
v3.0 Peanut Butter – 50mg/100g
v3.0 Chocolate – 80mg/100g
Black Edition Vanilla – 90mg/100g
Black Edition Chocolate – 100mg/100g
H&S Thai Green Curry – 40mg/100g
What about millets.
Can share how much oxalates in millets.
Hi Sneha,
Harvard did not study so listen to this when a food you want to eat has not been studied. I have a youtube channel that will help:https://www.youtube.com/watch?v=5fM4hO4dA9s&t=16s
Jill
Thank you. Your information is so helpful. I have a couple questions.
Do Diet Arizona Green Tea or Diet Snapple peach ice tea have high oxalate?
Today my Dr said I need to lower my oxalate. I had 3 stones last year. Just today, reading about this, I’ve been eating everything high in oxalate! So much to learn!
Thank you!
Hi Cindy,
Have them as an occasional treat. They have not been studied so not sure. An even more important goal is to get your daily calcium needs met each day to help rid your body of the excess oxalate.
Jill
I got 19.4mm left middle calyx kidney stone so PCNL surgery was done to removed and now I have higher chance to reoccurring kidney stones so please suggest me diet plan and instructions accordingly, thanks
Hi C R, It is not so easy, alas. Here is a reasonable approach to evaluation, which will lead to the right changes in diet and perhaps use of medications. Regards, Fred Coe
That’s the biggest stone I’ve ever heard of. Mine was only 8mm.
Hi – As someone who loves chocolate, I’m definitely struggling with me new diet. Is there a portion size of solid dark chocolate, that eaten with milk daily is safe? Also, is chocolate ice cream a good solve because of the dairy content?
Hi Dave.
Watch what I say about oxalate here on my youtube channel:https://www.youtube.com/watch?v=5fM4hO4dA9s&t=16s
Jill
From the sounds of it, milk chocolate is a safer bet than dark chocolate.
Yes, milk chocolate is somewhat safer because it’s been diluted. What a travesty! It pains me to be a chocolate aficionado now that I must restrict my chocolate intake. I consider milk chocolate as inferior, having too much sweetness with hardly any actual chocolate flavor. I believe it was invented just to save production costs while fooling an unsuspecting public, because cacao is an expensive ingredient while milk is cheap. In wine-connoisseur terms, milk chocolate is to real chocolate as white Zinfandel is to real Zinfandel. One is light and cloying, the other is dark and rich.
The first person to figure out how to remove oxalic acid from cacao will make a fortune. A similar thing was done with decaffeinated coffee, why not chocolate?
Hi Alex, thanks for the information about milk chocolate – I happen to like it, which shows a lack of proper taste. Nablu is a commercial site and I usually do not allow them, but it appears scientific and reasonable. Fred
I was hoping you could help me with two specific products. The first is White chocolate made with cocoa butter, the second is soybean spaghetti. The links below will get you to the nutrition labels:
https://pool.netrition.com/choc-zero-chocolate-squares.html
https://pool.netrition.com/zeroodle-organic-soybean-spaghetti.html
Thank you.
Hi Scott,
You can have white chocolate. It is more about sugar than oxalate here. Make sure you remember that too much sugar in your diet is not advisable. The kidney stone diet is much more than lowering oxalate. Kidneystonediet.com
Jill
This is the first that I have heard that meat, seafood, and eggs are ok to eat. Most low oxalate diets recommend a plant-based diet.
Hi Kim,
Oxalate are only found in plants.
Jill
Hi Kim,
Oxalates are found in plant food.
Best, Jill
You’re thinking of purines. Not oxylates. Purines are the cause of gout as well but they also cause another type of stone. Oxylate stones however, are the most common at 70%.
Hello, we would like to create patient education materials for our institution based on your research and the content found on this page. Would it be possible to obtain permissions to utilize this information for patient care? Thank you!
Hi Rachel, We are planning to send permissions. Regards, Fred
The tables have confusing information. For example, cornmeal and corn grits are “very high” in oxalate, but foods made from them (cornbread, corn chips, corn flakes) are low to moderate. How can 1 cup of cornmeal be very high while 1 cup of corn flour be low? They come from the same corn! It’s hard to make sense of this.
My urologist who removed a kidney stone advised me to avoid cranberry juice (which isn’t listed at all), and while I see scientific literature saying cranberry juice increases the risk of forming calcium oxalate stones, the table lists cranberry sauce as “low”.
And there is a lot of conflicting information – from reliable sources – so that it’s hard to know what to believe. For example, the University of Pittsburgh Medical Center lists lentils as “low” in oxalate – see http://www.pkdiet.com/pdf/LowOxalateDiet.pdf – but the table linked on this page lists lentil soup as “very high”. Why should I trust one reliable source that contradicts another reliable source?
Hi again A,
Please go to my website as I explain all the things you ask about: kidneystonediet.com/start
jill
It is very important to mention, in order to avoid confusion, that not all kidney stones are formed from oxalate crystals. However, oxalate stones are the most common kidney stones in most nephrolithiasis patients. Obviously, the oxalate crystaluria should be targeted in those patients with a comprehensive oxalate minimized diet. And yes, it is correct to mention that oxalic acid is present in plants only. Most oxalic acid sources are fruits and vegetables. Also, it is important to mention that mannitol rich vegetables and fruits (i.e. cauliflower, celery, plums, nectarines and yellow squash are rich in mannitol). Vitamin E in minimum daily requirement doses (MDR doses) are needed to supplement this benefit of mannitol as protectant of kidney tubules in oxalate crystalluria. In summary, my point is to make emphasis in the intake of mannitol rich vegetables and fruits in oxalate forming patients. Supplemental calcium in MDR doses is also a “chemical antidote” (in fact, the only one) for oxalate stone formation in the kidneys. Remember that vitamin E and calcium supplements in combination with intake of mannitol rich fruits and vegetables are a most in oxalate stone formation (oxalate stone nephrolithiasis) in order to protect kidneys from oxalate cristaluria and hematuria.
Hi Dr Perera, I have put this comment up as a courtesy. I do not subscribe to the remarks about mannitol as a protection against oxalate crystals, as you do not put up the evidence and I know of none. Regards, Fred
Is it ok to drink Ensure?
Hi tmbrown,
If your doc has suggested it then use it. If you are drinking this for some other reason, I wuold be careful of the added sugar. These drinks are not the healthiest options for anyone much less kidney stone formers.
Jill
hai, is coral lettuce high on oxalate as compared to iceberg lettuce and romaine lettuce which is low near to none oxalate? thanks for the reply
Hi Anwar, Lettuce is not high in oxalate. Fred Coe
What can one eat? Y’all talk about what not to eat. Please give a menu for a week. Thanks 😊
Hi Ann,
Pretty much everything else. Go to my website for kidney stone safe recipes and much more: kidneystonediet.com
jill
Hi, Ann, I believe menus are available. RECIPES FOR KIDNEY STONE PATIENTS Jill Harris also has many. Regards, Fred Coe
What is your opinion of TheraLith XR? Does using this supplement give one any kind of leeway? It’s so well regarded that you can get a discount with a physician or provider code. I had my first stone at age 64. No others yet. Had to have lithotripsy no stent in May off this year. Just turned 65 I’m primarily vegetarian of the ovolacto variety. Adding more Greek yogurt to my diet. The oxylate diet is so restrictive it’s no wonder most stone former’s relapse.
Hi Tom, TheraLith has a modest amount of magnesium – 180 mg – as the citrate or oxide (50% each) salt, and trivial amounts of potassium citrate – about 1 mEq. It is meaningless for stone prevention unless many are taken a day, and even then that would be an excess of magnesium. I have no idea why such a product exists, from a scientific perspective, nor why anyone would want it apart from a magnesium supplement. Regards, Fred Coe
Hi! There are many fiber rich foods low in oxalate, but can you recommend a commercial fiber supplement to trial or those to avoid?
Hi Jamie,
I have a free resource on my website with a low oxalate and high fiber shopping list:https://kidneystonediet.com/high-fiber-low-oxalate-grocery-list/
Jill
This article is really wonderful, and very helpful. But I am confused about one thing.
You wrote: “Here are some juices that are low in oxalate and better substitutes: Apple juice, apricot juice, orange juice, grapefruit juice, grape juice.”
Previously in this article, you stated that grapefruit are high in oxalates. Is the whole fruit worse than the juice? That would be the opposite of tomatoes vs tomato juice.
Hi gardencast,
you can certainly have grapefruit. Go here for you oxalate list: kidneystonediet.com/start
Jill
I agree with GardenCat that this is truly a great article and will help me make diet choices that will help me not to get more stones. I also didn’t know I was at higher risk of bone problems. And I appreciated how you told us how to use dairy to counteract the oxalate foods.
However, I don’t feel you answered her question which I had too as I read through the article.
In the Fruits section above you state “On the other hand, people do not realize avocado, oranges, dates, and even grapefruit and kiwi are very high and need caution.”
In the Beverages section you state “Here are some juices that are low in oxalate and better substitutes: Apple juice, apricot juice, orange juice, grapefruit juice, grape juice.”
In the Foods List it states “Grapefruit 1/2 fruit Very High 12mg”
So our question is, “Why is Grapefruit juice okay but not the fruit?”
For other people with kidney stones, specialists presented this seminar within the last month. Free. Covers all the info I could ever think to ask, including diet. This is how I learned about Oxalate Foods.
http://stonecentrevgh.ca/ucla-ubc-kidney-stone-patient-information-webinar-2021/
Hi gardencat,
you can certainly have grapefruit. Go here for you oxalate list: kidneystonediet.com/start
Jill
hai, is coral lettuce is classified as low in oxalate? thanks for the reply
So green decaf tea is just fine correct?
I believe that is true. Fred
If tomatoes are fine why is tomato sauce a problem?
Hi Linda,
It is the concentrated form of tomatoes. And that doesn’t mean you can never have sauce again, go to my site to learn about my mantra, “portion not perfection.” kidneystonediet.com
Jill
Can a 4mm some in lower pole of kidney cause pain?
Hi Joni, Theoretically no. But many with small non obstructing stones complain of pain. I always check for infection, the only reason I can think of. Regards, Fred Coe
I wish I could find an answer regarding red sweet onions, whether low or high in oxalates
Hi Valdine,
Onions are low. All of them.
Jill
Male,74yrs no kidney stones ever. Within last 2 yrs have had bladder stones removed twice and will need another the size of a golfball removed before end of 2021. Been on low oxalate diet last 6mos. Taking calcium citrate supplements daily. Still growing bladder stone. What else can I ask doc to look for??
Hi Tony, A common cause of bladder stone is outlet obstruction from prostatic obstruction, and that usually needs remedy to prevent more stones. What the stones are is a major issue. If uric acid, then raising urine pH will prevent them, so stone analysis is crucial. I would pursue both possibilities. Regards, Fred Coe
First oxilate stone at 58. This, suspiciously, is after six years of using almonds (and other nuts) as the staple in my diet due to type 2 diabetes, which is ‘well managed’ with stable a1c at 5.9. Im not happy to work in another level of restriction, but I will as the stone, scope removal and stent has been HELL. I wish diabetic management had a source of information as good as this – I might have been forewarned a bit… namely, you also have to mind your substitutions as well as blood sugar.
Hi Jeff, Stone surgery is horrid despite the brilliance of new instruments, and the very high skill level of modern stone urologists. It is just that no one wants any surgery, if possible. I would get fully evaluated as to the real reasons for the new onset of stones. Often urine calcium is high from diabetes, for example. Are you sure the stone is calcium oxalate? Uric acid stones are frequent in diabetes. Measure twice, cut once – old carpenter’s saw. Regards, Fred Coe
Thank you for the article, it’s helping to understand lo diet. How is corn flour low in oxalate but corn meal is very high? I understand cornflour is corn meal grinder to a fine texture. Also is oat flour (made from grinding either rolled or steel cuts ) low in oxalate?
We are trying to find flours that are low in oxalate for everyday.
I have a few foods I have questions on: chia seeds, garbanzo beans, rice noodles, rice cakes, gluten free oatmeal, and what about hard alcohol like whiskey or vodka?
Hi Diana,
Harvard has not studied all foods. Other sources say chia seeds are very high, so be careful. Hard liquor is not high in oxalate. Rice (white) little oxalate. Brown rice higher. For all things oxalate including an counter you can put on your phone, go to my website at kidneystonediet.com/start
Jill
How can pure miso be have less oxalate content than “ miso soup” , which is miso and water?
Hi Iris,
This has plagued me forever. Not sure. Harvard would be the one to ask.
Jill
I guess it’s because mido soup also has other ingridients, such as tofu, that are high in oxalate
Dilution
Hey this website is a lifesaver! Recently diagnosed with a load of tiny stones in both kidneys.
How much oxalate per gram does pumpkin, garlic, ginger, guava & bitter gourd have?
Hi Mohammad,
Harvard did not study all foods. When you find a food that they didn’t study have the food once or twice per week in normal portion sizes. It is when we overeat foods in everyday along with not getting any calcium in our diet that we run into higher urine oxalate levels. I have given this advice to my patients for over 22 years and it has never proven it wrong.
Jill
Does it help most or some people to take 500-1000mg of Vitamin C daily?
Hi Tony, for stone formers, vitamin C can increase oxalate production, so keep it to the amounts in a multivitamin. Fred
Hi.. thanks for this comprehensive article.. im on a low oxalate low lectin diet for my severe osteoporosis. So much research and leg work to find foods low in both.. do you have any suggestions? Any info would be sooo helpful.. thank you Karen
Hi Karen, I presume you eat a low oxalate diet because of calcium oxalate kidney stones. No evidence supports nor any medical theory suggests diet oxalate has anything to do with osteoporosis. Osteoporosis is not the main thrust of this site, but idiopathic hypercalciuria a main cause of calcium stones, may contribute to bone mineral loss. I am not familiar with any link between lectin intake and osteoporosis, either, and doubt the association exists. So perhaps your efforts may not be ideally directed at the moment. Regards, Fred Coe
Thank you for all the information.
How much lower is the oxalate count of backed potatoes without the skin?
Thank you.
Hi Michael,
Not sure. But you can certainly still keep them in your diet here and there. Skin and all. Find out by getting your free oxalate info here: kidneystonediet.com/start
Jill
It is informative website. I like it, but here I am having issue that whom to believe and whom not to believe. who is right and who is wrong. In your website you mentioned that meat is free from oxalate and the website of HARVARD MEDICAL HEALTH SAYING ANIMAL PROTEIN IS BAD AND CAUSING KIDNEY STONE. here is their website. https://www.health.harvard.edu/blog/5-steps-for-preventing-kidney-stones-201310046721
The people like me who do so much research and trying to find out the real fact about ever day life problems, how I can trust then who is telling the truth, causing so much confusion on mind.
Hi Normandy, I know the Harvard work on protein and can help here. First, there is no oxalate issues with meats – animal protein. Here is my analysis of the paper from there about diet protein and stones. As I know the authors, I asked Dr Taylor to read my analysis and put his answer at the end. Briefly, they could not find an effect of diet protein on stone risk – even though they would want to find it. As for meat and oxalate, they do not consider it as oxalate in meat is very minute indeed. Regards, Fred Coe
How do i cross this data with the requirements of dealing with heart disease? I’m a 61 year old male who had a triple bypass at age 51, and I’ve also had 4 kidney stones.
Hi Jack, Diet oxalate is massively overdone in the US, and may not even apply for you. Here is my best effort on that question. If indeed after reading this you feel a need to restrict diet oxalate, here is a better way – a more integrated plan that is also ideal for cardiac disease. I hope this helps, Regards, Fred Coe
Highly helpfull info.
I am drinking water with half a fresh lemon squeezed in every day to keep stones from forming as I have read online. Is this good or bad ?
Hi Chuck, I think the verdict is ‘unproven’. No trials for lemon. Lemons are supposed to be a way to get potassium citrate cheaper than in pills, and the excessive pricing of medicinal K citrate has pushed people into this kind of ad hoc remedy. Some people with calcium oxalate stones have low urine citrate, and will benefit (trials here) from added potassium citrate. Some form uric acid stones, and it is not citrate that matters but too acid a urine pH. For them the potassium citrate works by raising urine pH. Some have calcium phosphate stones and have a high urine pH (alkaline) and low citrate; added alkali has never been tried and is likely to worsen things. So, about the lemons, I suspect they matter not at all, having too little alkali, and real treatment needs to match the problem. Here is my best intro to that. Regards, Fred Coe
I have been diagnosed with a large kidney stone that showed up on CT scan but not on Xray so they have determined it is more than likely NOT a calcium stone. However, I have celiac disease and history of gastric surgery and I feel like I am THE perfect candidate for hyperoxalate issues (and all of my favorite foods are on this list). Is it possible to have a stone composed of something other than calcium when you have hyperoxalates? Or maybe they just didn’t have the right resolution on the xray and will find that it actually IS calcium once removed via cystoscope (as opposed to sound waves). Thank you, Shelley
Hi Shelley, If your physician would measure the Hounsfield units of the stone on CT you could get a fair idea of what it is made of. The best (overwhelming) bet is uric acid stones because of your GI disorders. A full workup for cause of stone is important for you as oxalate could be a problem, but calcium oxalate stones are usually very easy to see. Regards Fred Coe
I had calcium oxalate shards brake loose from my kidney stones do to a fall from a ladder while cleaning my oldest sisters’ gutters. Blood in my urine and extreme pain sent me to the ER ,who gave me a shot and pills and sent me to a urologist. (a saint named Dr.Stackpoll) He took an X-ray and explained what I had to do and why and my options if I needed sergery. He told me to read the JAMA report on 100,000 people over two decades done by Harvard Medical School on diet and illness. So I did. I passed the
shard one day before lazer sergery by drinking tons of hot tea with lemon. This was 30 yrs ago and I’m still drinking hot teas and doing maintenance.
Hi Ron, Lovely story, and I am happy for you. Gary Curhan authored those papers, and I have his work everywhere on this site. Fred
I thought tea was bad, high oxilate? What kind of tea?
Hi Brenda,
Learn more about oxalate from my website- kidneystonediet.com/start
j
This list has been somewhat helpful. But as I have CKD and have to watch my phosphorous, potassium, sodium, & protein it has me spinning. I wish I could find a list with all these values listed together. Do you know of one?
Hi Linda, stones are very uncommon given CKD sufficient to influence diet. If you indeed form calcium oxalate stones and have abnormal urine oxalate and have significant CKD there may be a serious underlying disease for which diet is irrelevant. Please consider if this is the case. Regards, Fred Coe
This is such great information! Thank you SO much for publishing.
Curious, what is the oxalate levels of lupin or lupini beans and flours? I cannot find this anywhere.
Also, is there a recommended calcium supplement to take to maintain about 1000mg of calcium daily? Or a certain type to look for?
Thank you!
Hi Amy,
Go get your free resources from my website that will address calcium (no we do not recommend supplements in pill form) and what to do when you are not sure how much oxalate is in a food. kidneystonediet.com/start
Jill
Thanks so much, Jill! Final question: does monolaurin impact oxalates or kidney stone formation?
Hi Amy, It does not. But a recent scholarly review shows that there is no evidence that the material has any benefits. Regards, Fred Coe
Do you know of an oxalate list that can be copied and pasted? I have benefited greatly from the list you sent me but want to take from it with the foods I like. Will type from scratch but prefer this faster way
Hi Diana, Sorry I overlooked this. Jill Harris has such a list, I think, and free, too. Best, Fred
Trying to navigate the turbulent waters of Oxalate kidney stones, IBS and diabetes. For the latter two, proteins are good with a 80-120gm daily intake. How will that fare with someone like me who has had Calcium protein oxalate stones 4 years back??
Hi Ajay, Oxalate is often a minor issue for calcium oxalate stone formers. Here is a better article to organize your stone prevention. Here is a more balanced one about the role of diet oxalate. Here is something about the protein /stone story – hint, protein has a very modest role. I wish I had the time and resources to make this morass of a site more obvious, so people could see what is in it. Regards, Fred Coe
Wow! Thanks for sharing this information. I’ve been attempting to reduce or rid myself of high candida which I’ve battled for some time, by ingesting the monolaurin pellets. I may have to look for an alternative with better evidence. Please let me know if you have any suggestions! Cheers!
Hi Amy, A good review found no evidence for monolaurin as a systemic treatment for anything, including fungi. Vaginal use may be effective – see the linked review. As for diet oxalate, no evidence supports a role in cause or treatment of candida. Regards, Fred Coe
Thanks for the good information. What about meat consumption? You suggest it is not an issue but what do you think of studies such as this: https://pubmed.ncbi.nlm.nih.gov/24518789/ ? Since the subject here is oxalates perhaps I’m confusing mitigating Uric acid-based stone formation.
Hi Jim, This paper is not very powerful as it merely shows that eating purine loads from meat alters urine uric acid – an oxide of purine metabolism. Here is a good article I summarized showing what you really want to know. Meat is weak indeed as a stone risk. Regards, Fred Coe
Hello,
Thank you so much for your article!! My husband has the kidney stone health problem. Both of us became pretty discouraged on what to avoid and what you are allowed to eat! So many articles were old and contradicted each other! Being the cook in the family I was so overwhelmed and discouraged But alas you gave us light at the end of the tunnel and with humor ! Thank You So Much!
Hi Judy, Do not fall into the oxalate trap – there is a lot more to do and oxalate intake is not always the most important. Most important is full evaluation so you know what are your goals. Then diet is multifaceted; here is a good overview. Regards, Fred Coe
I have struvite stones what is the difference ,what for diet do I have to take!
Hi Hendrika, These stones are produced by bacteria and are special. I have never written an article about them – about time! Diet is usually not the most important matter – they are essentially infected foreign bodies in the kidney that need surgical removal and treatment thereafter to avoid more growth from bacteria. I am afraid this one is for your surgeon, but I will write about the matter when I get the time. Regards, Fred Coe
So are you saying that if my stones are Calcium Oxalate I do not need to reduce my Oxalate intake? You said in a comment above that Oxalates are often a minor issue for Calcium Oxalate stone formers. Can you please clarify?
Thank you
Hi Gail, If your stones are calcium oxalate, diet oxalate is one thing to consider, among others. The link is to my best attempt at an overview of stone prevention. If the stones are mainly calcium phosphate (calcium oxalate 15% or less) the emphasis is certainly not on diet oxalate but usually on urine calcium and pH. If stones are mainly uric acid, urine pH is more or less all that matters. I hope that makes things clearer. Regards, Fred Coe