
A Good Place to Start
The videos review the chapter and emphasize the main points. I would start with them.
Salt Ponds
The featured image shows salt harvesting from evaporation ponds.
The sea is salty and like our blood holds its salts in solution. But if you channel the sea into ponds, and balance things so the sun evaporates water faster than new water can enter, the remaining water overloads with sodium chloride. It crystallizes out of solution as sea salt. Workers collect it for us to season our food with.
Is it not an apt picture?
Our Blood is the Sea, our Kidneys Make the Pond
Mostly the Salts Stay in Solution
Our kidneys filter the salts and water of our blood into their millions of fine tubules. Like the sun they take back the water, unlike the sun they also take back much of the salts.
Mostly they are balanced, these takings back, so the final urine can dissolve its salts.
Stones Arise from Imbalances
If you ask me to say what makes stones form, I must answer that something has disturbed the balance, leaving not enough water to dissolve the salts, as in the ponds drying out under the sun.
Which salts, you might ask? After all, we are not ponds and our kidneys remove many small molecules.
Those salts, I would answer, that have made the stones.
Precisely those. Usually calcium oxalate and calcium phosphate.
The 24 Hour Urine is Our Pond
In it we measure losses of salts that can become stones, and the volume of water to dissolve them. We need the full day because things vary, with sleep and food, and all of what we do in life. Each is snapshot of our pond for one day. Which salts, how much imbalance, all this comes from our daily samples.
Abnormal Excretions Cause Stones
In our urine, excesses of calcium or oxalate excretion, or insufficiency of citrate excretion or of water are proven independent risk factors
that predict new onset of stones. Since stones cannot cause these abnormal excretions, and the abnormal excretions can cause stones, this association is equivalent to cause.
By independent I mean that the effect of each is significant when the effects of the other factors are adjusted for mathematically using common statistical techniques.
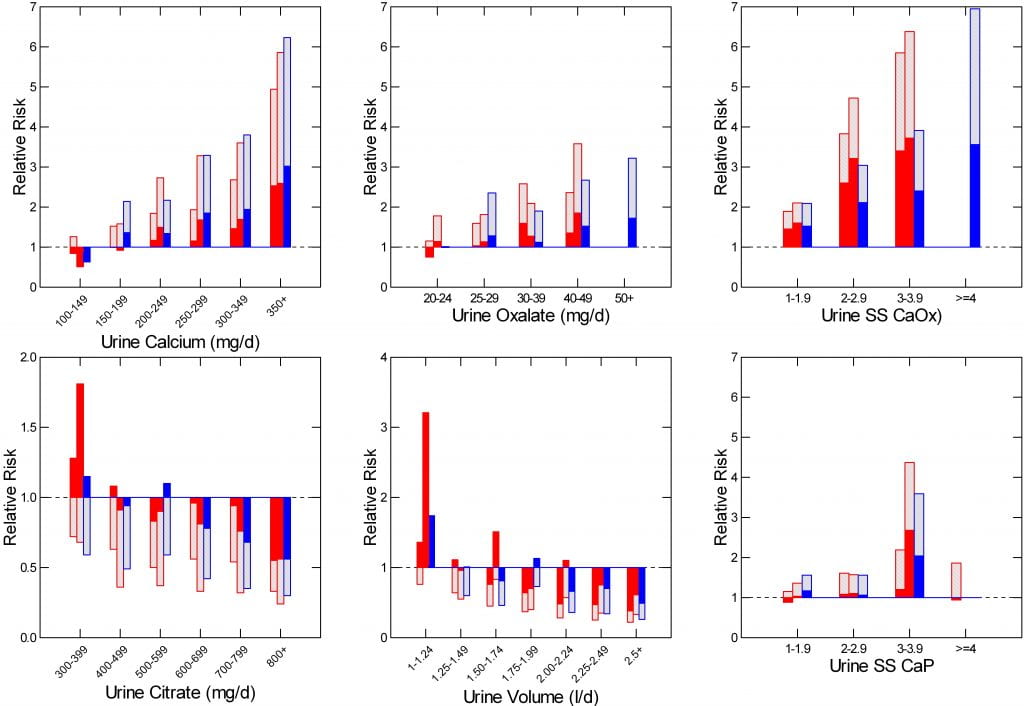
In cohorts of women (red) and men (blue) followed over decades, risk of forming stones rose smoothly with urine calcium or oxalate (upper left and upper middle panels), and fell with increasing citrate and urine volume (lower left and middle panels).
The mechanisms causing high urine calcium and urine oxalate are well known. Means for lowering them, likewise, and such lowering is known to reduce new stone formation.
Risk from low urine volume is most obvious below 1.25 liters per day (lower middle panel), a scanty volume. By 2 liters a day risk from low volume is gone.
Supersaturation is the Word for Overloading the Pond
Crystals produce kidney stones, and supersaturations produces the crystals. Modern laboratories can measure the supersaturations in 24 hour urine collections along with the key components in the urine that control the supersaturations.
As you might expect, supersaturation is a powerful predictor of whether people will become stone forming patients. The two right panels of the graph show how supersaturation with respect to calcium oxalate (top) or calcium phosphate relate to risk of stones. (Note that common supersaturation urines for calcium oxalate are 3.3 times higher than these older style supersaturation ratios. Your report will almost always use the newer units. So risk begins above 3 and rises smoothly up to 12 or more).
Given the stone crystals and the supersaturations you can gauge treatment goals from a simple maxim: In a patient who is producing new stones, urine supersaturation with respect to the crystals in the stones forming is too high.
Ideally one will lower supersaturation by improving all factors that raise it. But one must avoid a common and obvious fallacy. Water alone can lower urine supersaturation – think about rain and the pond. But water alone, without proper testing and as a sole remedy is a poor idea under all circumstances and to me anathema.
Ideal Treatment Improves All Abnormalities
Given a patient may have any one of these four abnormalities, and that they act independently, the ideal treatment strategy will attempt to improve each one to achieve synergy. It is often more practical to partly reverse multiple abnormalities than to rely on improving only one. For example, possibly extremely high urine volume might reduce stones even if urine calcium and oxalate remain high. But lesser volume would be sufficient if these two excretion rates were each moderately reduced.
When treating hypertension, as an example, one tries to achieve some weight loss, some increase in exercise, some reduction in sodium intake, and some increase in potassium intake, and then use medications as needed. The alternative, medications alone, or just exercise, would create a potential for side effects – too tired from exercise, or drug side effects in this case – which synergy would avoid.
Proper Testing Is Essential for Proper Practice
All Stone Formers Deserve Serum and 24 Hour Urine Testing
It is obvious that the only documented risk factors for stone are found in 24 hour urine, so this measurement is the bedrock of stone prevention. Systemic diseases that cause stones often alter serum chemistries, and they must be diagnosed from those alterations.
Inadequate Testing Can be Dangerous
A few causes of stone disease, such as severe hyperoxaluria can destroy kidneys. Others like primary hyperparathyroidism or renal tubular acidosis can do the same. Other rare but dangerous inherited diseases lurk in any kidney stone population. They require both serum and 24 hour urine testing.
Consider that idiopathic hypercalciuria can be very severe and lead to both stones and bone disease. One cannot know without a 24 hour urine collection. Elevated serum calcium can mark for primary hyperparathyroidism, or simply benign familial hypocalciuric hypercalcemia. So one needs a 24 hour urine here as well. Low urine citrate as a cause of stones is simply unknowable without a urine collection.
Arguments Against 24 Hour Urine Testing are Specious
Cost, difficulty, and futility are all common arguments against urine testing, and none of the three convince me. Add to this that all people fear and detest surgery. Surgery is a nightmare one hopes to avoid. If testing can reduce surgery by even a small amount, testing is a virtue.
Surgical Costs Dwarf Those of Proper Testing
A common 24 hour urine with fasting blood sample costs a few hundred dollars – say three hundred for an upper end estimate. A kidney stone surgery, ureteroscopy for example, costs – about eight to ten thousand dollars, to which one must add lost work and the debilitating effects of general anaesthesia, postoperative pain, stents, infections, and postsurgical visits to physicians. Shock wave lithotripsy costs as much or more as shown in the same reference. At these rates, 30 to 40 24 hour and blood testing panels match one surgery discounting the personal losses.
Difficulty of Collection Stops Few Patients
In my decades of managing patients with kidney stones almost none have demurred to collect – pilots, surgeons, busy and successful business people, teachers. I could also point out that modern commercial vendors all provide convenient collection kits and instructions. But no one could make the case better than my partner Jill Harris did in her spirited article on this topic.
Personalized Kidney Stone Prevention
Stone Analysis is Crucial
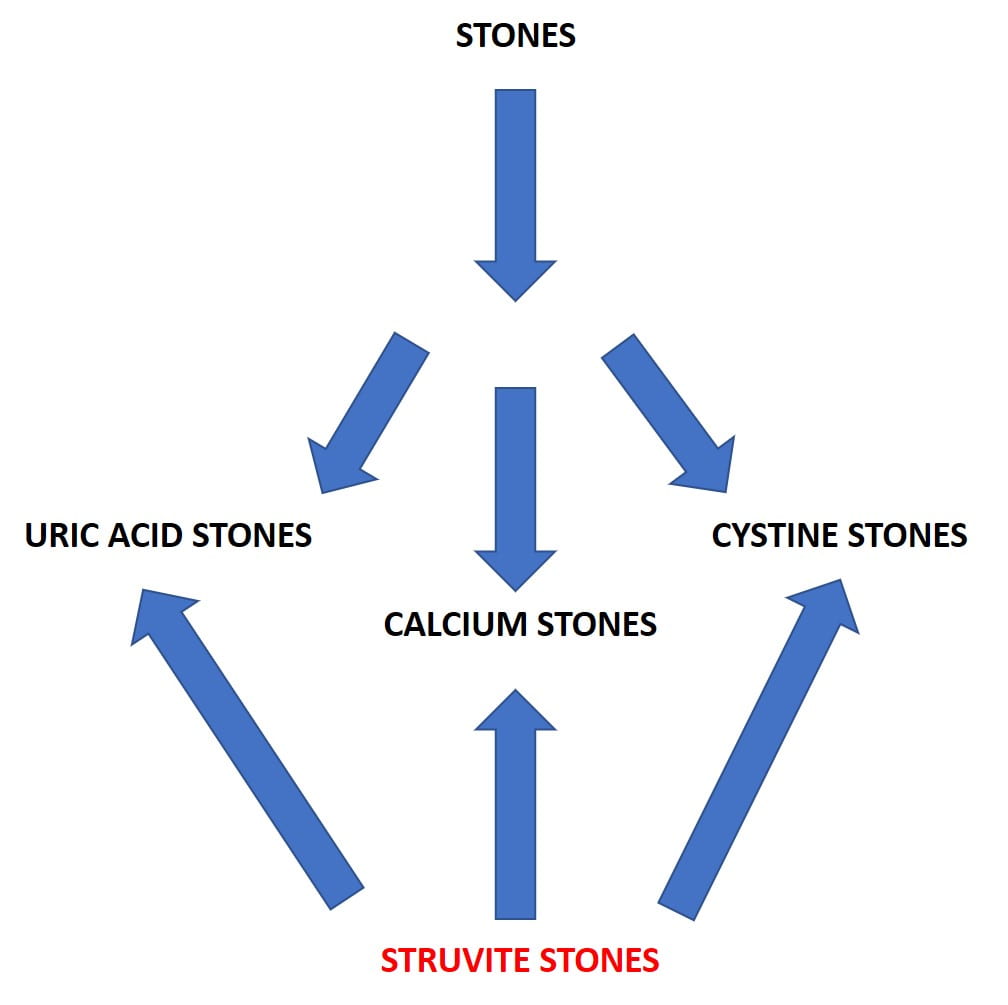 Assuming stones are forming or have formed, everything branches off of stone analysis.
Assuming stones are forming or have formed, everything branches off of stone analysis.
Uric Acid in Stones
Uric acid stones form mainly because an overly acid urine raises supersaturation so powerfully nothing can reliably prevent more stones but alkali to raise pH and make the urine less acid. Uric acid stone can be pure or admixed with calcium oxalate crystals. In either event, treatment must include alkali to prevent more uric acid. If your stones contain uric acid, follow this link.
Cystine in Stones
Cystine stones form only when genetic abnormalities of renal cell transporters allow a vast excess of this amino acid into the urine. Treatment is high specialized. Stones can grow very large and rapidly. Supersaturation can be measured but only in a few laboratories. Like uric acid stones, cystine stones can contain calcium phosphate crystals, but prevention of cystine crystallization is paramount and takes primary importance. If your stones contain cystine, follow this link.
Struvite in Stones
Struvite, magnesium ammonium phosphate, forms in humans only because of infection with organisms that hydrolyse urea to ammonia and carbon dioxide. Struvite can be the only stone crystal or can become part of any stone. Treatment has nothing to do with diet or the usual stone medications. Struvite stones are essentially infected foreign bodies within kidneys, and cure requires a mixture of thoughtful surgical management and use of antibiotic drugs.
Calcium Stones
The mass of patients will form calcium stones unmixed with uric acid or struvite. Out of this mass physicians – patients cannot do this

themselves -must cull the small fractions with systemic diseases that cause stones but produce illness beyond stones and require special and often very complex management.
Serum and Urine Testing
The tubule disorders are recognized from serum abnormalities, sometimes paired with specific 24 hour urine findings. Renal tubular acidosis and primary hyperparathyroidism are particularly related to stone disease. Both require both serum and 24 hour urine abnormalities for diagnosis.
Primary hyperoxaluria, and hyperoxaluria from bowel diseases, dangerous diseases that can cause kidney failure, are diagnosed from high 24 hour urine oxalate excretion and cannot be otherwise recognized. Bowel disease is recognized clinically, but 24 hour urine testing is required to assess both urine oxalate excretion and other secondary abnormalities that can cause stones and kidney disease.
Idiopathic Calcium Stones
Evaluate 24 Hour Urine and Treat Abnormal Risk Factors
Urine Calcium
High urine calcium in these patients arises from idiopathic hypercalciuria, and can be controlled with reduced diet sodium intake, avoidance of excessive diet protein intake, perhaps reduction of refined sugar intake, and, when needed, thiazide diuretic agents. Adequate diet calcium is needed to reduce risk of bone mineral loss.
Urine Oxalate
Urine oxalate above 25 mg/d can be treated with adequate diet calcium, that reduces oxalate absorption, and reduction of diet oxalate intake to below 200 mg/d using lists of high oxalate foods. Of these, spinach, rhubarb, nuts, seeds, and pepper are common offenders. If diet calcium increase does not bring urine oxalate into the desired zone (<25 mg/d is ideal, <30 is acceptable), limiting diet oxalate to below 100 mg/d is a proper strategy.
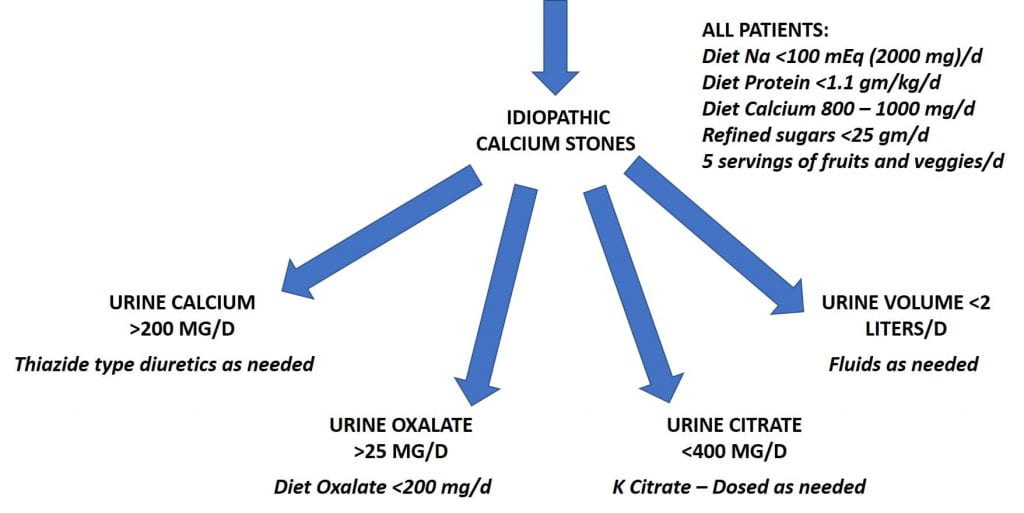 Urine Citrate
Urine Citrate
Low urine citrate, below 400 mg/d raises stone risk because citrate binds urine calcium in a soluble complex and directly inhibits formation and growth of calcium oxalate and calcium phosphate crystals. Five servings of fruit and veggies provides about 120 mEq/day of potassium alkali that can raise urine citrate. If needed, potassium citrate can be added as a specific treatment.
Urine Volume
One hardly need mention that urine volume below 2 – 2.25 liters a day needs extra fluids to achieve that goal.
The Kidney Stone Diet
The elements common to the three main risk factors beside urine volume are reduced diet sodium, sugar, and protein – to permit adequate diet calcium without raising urine calcium, adequate diet calcium for bones and to block diet oxalate absorption, and fruits and veggies to provide diet potassium alkali. These are highlighted in the large upper box.
These five diet elements all correspond to present healthy diet recommendation for all US citizens, and should be advocated by all physicians for all patients unless otherwise limited by underlying diseases. Since idiopathic calcium stone formers are almost by definition free of systemic disease, it is a desired diet in general. The diet has been tested in one prospective trial and more trials are much needed.
Online help with the kidney stone diet is available from my colleague Jill Harris.
Specific treatments, thiazide like diuretics, potassium citrate pills, and low oxalate diet are noted under their respective abnormalities. A strategy for beginning treatment with diet and adding drugs as needed is outlined here.
More is Wrong Than Just Stones
Having stones is burden enough, especially the dreaded surgery they can entail. But epidemiologists have discovered links between stone formation and risk of hypertension, bone disease, stroke, heart attack, and kidney disease including even renal failure and dialysis. The links between stone forming and these other major diseases are not as yet obvious, but the message obvious. Physicians need to treat the patient, nor just focus on preventing stones.
The kidney stone diet, being in line with best present recommendations for all US citizens, is a reasonable choice for all stone formers because aimed at reduction of risk for all of the above mentioned disorders. Even if the problems of stone formers transcend those of normal people, so that a healthy diet does not suffice, it can do no harm, and may do some element of good.
Why Not Just Lots of Water?
Consider the least threatening possible scenario, an idiopathic calcium stone former who has had only one stone – a kind of baseline kidney stone disease. Being such a common and large group why not simply treat them with lots of fluids, do a single 24 hour urine for safety, and save more refined treatment if water fails?
That Has Been Tried
Before you read what follows brush up on supersaturation.
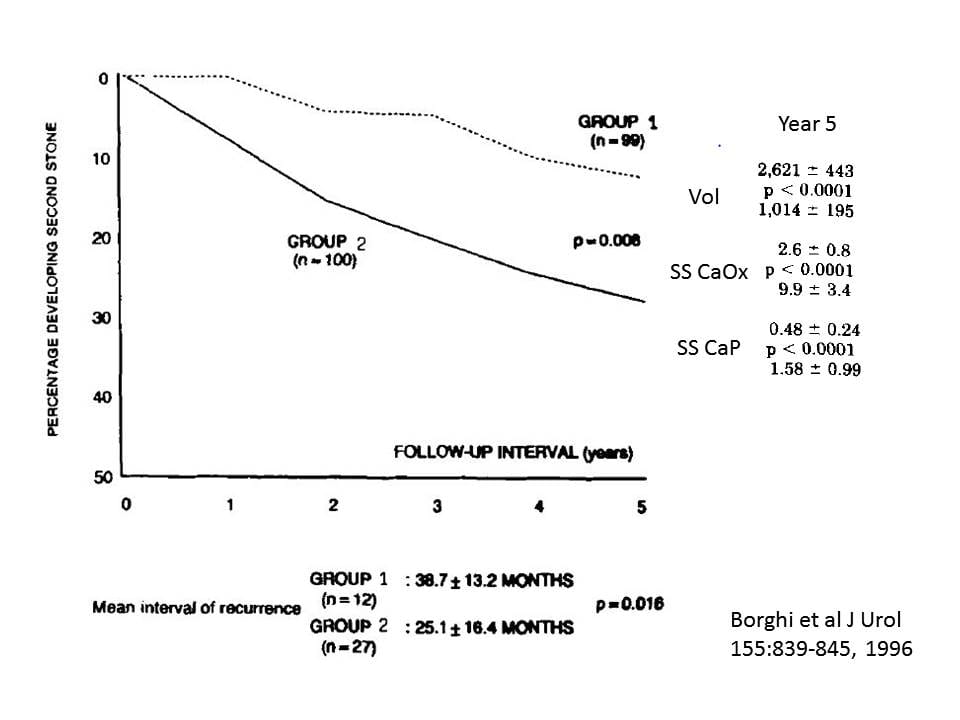
Of ninety nine people who formed one calcium oxalate stone and drank so much they produced 2.6 liters a day of urine, 12 formed one or more new stones in five years (Group 1). Among one hundred more just like them who produced only 1 liter of urine daily 27 formed one or more new stones during the same time.
As expected water reduced supersaturations. SS CaOx was 9.9 in the low flow and 2.6 in the high flow group. SS CaP was 1.58 in the low and 0.48 in the high flow group. Excellent and predictable results.
In passing the authors note that before the trial, at baseline, patients had lower urine volumes than their non stone forming subjects. One might surmise from this that habitual low urine volume played a role in causing their stones. But that is observation, not hypothesis testing.
Water Is Not Enough
Surely water works. Stones were less with lots of it.
But why so many stones? Of one hundred random people 12 people will not make one or more new stones in five years drinking so much water as to achieve a urine volume of 2.6 liters daily. This would be 2.4 percent per year or 24 percent per decade. Even if limited to adult years this would produce stone rates approaching 75 percent in a population of high fluid drinkers.
For the controls, who drank less, the numbers essentially double.
More is wrong than water could right. Given the risk factor studies I have already presented, this is an expected outcome.
In fact, in Table 4 of the water treatment article in the link above, hypercalciuria was at least one of the reasons for higher relapse. Baseline, before anything was done, the urine calcium levels of those destined to relapse was higher than those who did not 233 vs.336 mg/d and 249 vs. 313 in the high fluid and low fluid groups, respectively; p<0.001 for those into statistics. So those destined for a bad outcome had idiopathic hypercalciuria, a well known personal risk factor.
This Was Water Under Ideal Conditions
Above all else, these patients were supervised so that water treatment was as good as it can ever be. The cost of such supervision was underwritten by the grants that supported this trial. Outside the umbra of a subsidized program, adherence to such high fluid intakes will be less ideal.
Multiple Stones Predict Higher Relapse on Treatment
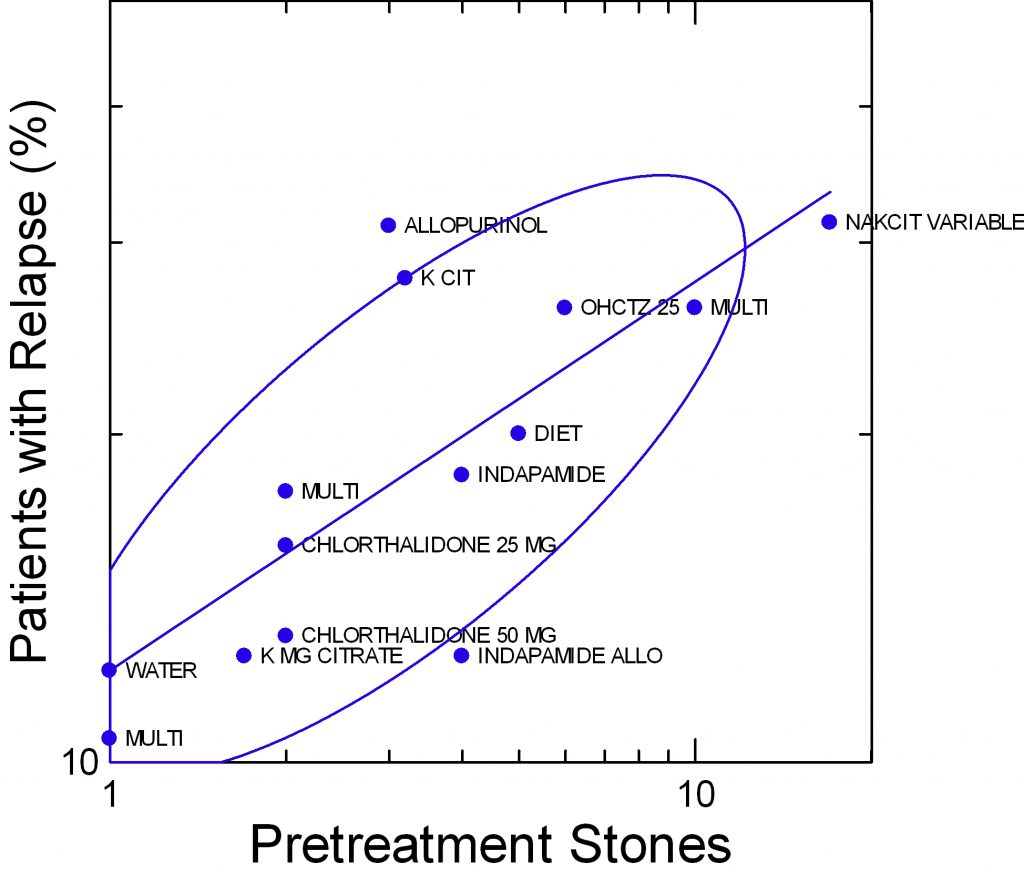 This figure shows the treated patients in a number of published trials. The details can be found in the parent article.
This figure shows the treated patients in a number of published trials. The details can be found in the parent article.
The abbreviations refer to the treatment modalities: K Cit means potassium citrate; chlorthalidone, indapamide are thiazide like diuretics, HCTZ is hydrochlorothiazide; Multi means several medications were used together; allopurinol lowers urine and serum uric acid and proved effective in one major trial against calcium oxalate stones.
As the number of stones produced before treatment goes up, from one to 10 or more (along the horizontal axis), the percent of patients who relapse during treatment rises from 10 – 12 percent to 20 to 30 percent. More or less, the percent who relapse increases proportionally to how many stones had formed before treatment.
Results for the water trial of single stone formers and my own published observations on patients who had formed a single calcium stone are at the lower left of the graph.
Stones Form Steadily Over Time
Waiting to treat a single idiopathic calcium stone former, either by the use of relatively ineffective high fluid intake alone or, in the worst
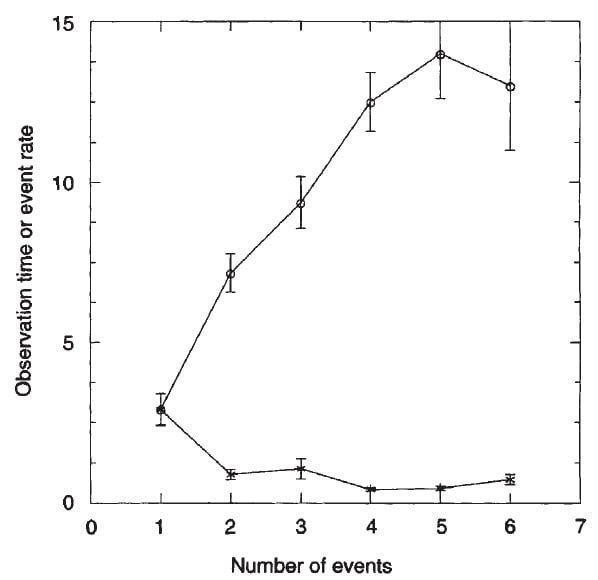
case, doing nothing at all, will on average lead to more stones. On this graph, detailed elsewhere, time is on the vertical axis and the number of countable stone events on the horizontal axis. Squares show the rate of stones per year, a rather constant number. Circles show the inevitable consequence: more time, more stones.
So time wasted, with water as a sole remedy, or no specific treatment, will tend to increase the number of stones, and as that number increases the successfulness of even highly supervised protocol treatment as used in trials will wane.
Never Use Water Alone
I will surely not treat any patients with just water unless 24 hour and serum testing shows me that nothing at all is wrong but low urine volume. Even then I am sceptical.
The reason I am so stubborn about water and waiting is that the main force of treatment for idiopathic calcium stones – those forming in the absence of systemic diseases – is diet change. Not only that, the diet change is in the direction considered most healthy for the US population. Why would anyone force fluids on patients when much of the disordered urine chemistry can be mitigated by a healthier diet?
Maintenance Treatment
Analyse Every Stone
One might think that once we know someone forms, for example, calcium oxalate stones more analyses add little or even nothing to successful treatment. But obvious problems make that thought a poor one.
New Struvite
Every surgery poses risk of infection. As foreign bodies in the kidneys stones themselves offer lodgment to bacteria that may be passing through the urinary system. So struvite can grow over older calcium stones, or even begin on their own. The person ‘converts’ from one type of stone crystal to another. Treatment no longer stops stone growth.
Because rapidly growing, large, and laminar in appearance by x ray, struvite stones will make themselves apparent over time. But larger size means more complex surgery, and perhaps kidney injury or even sepsis from stone infection. So early detection matters.
New Uric Acid
People age, gain weight, develop diabetes and with this urine pH falls. Treatment with alkali that might have stopped uric acid production begins late, when rapid stone growth or large stone size makes uric acid come to mind. But large means harder to dissolve, perhaps impossible. That means surgery. Early detection of uric acid in stones can save future surgery.
Calcium Oxalate to Calcium Phosphate
This happens and probably matters. CaP stones most often arise over tubule plugs which means cell injury in tubules and the tissues around them. By contrast, growth over plaque, how CaOx stones form, appears less invasive. Tissues seem less injured.
My imagination tells me calcium phosphate stones may cause more long term kidney problems than calcium oxalate stones. If this hypothesis were true then mere observation of patients well characterized in stone composition should disclose differences in kidney function, or perhaps urine albumin loss. Perhaps blood pressure rises more. Perhaps someone might have such information.
Quite possibly potassium alkali that work well to prevent calcium oxalate stones do poorly for calcium phosphate stones. After all, they raise urine pH and a higher pH will foster the phosphate stone. No trial addresses this obvious question; one should.
How Good is Kidney Stone Analysis
Less than ideal
What happens if you make a rigorous analysis of stones, divide the sample up into parcels and send them to different commercial laboratories. What will they tell you?
Ideally they will tell you what you already know. But in fact they under reported struvite and calcium phosphate – as hydroxyapatite. They also failed in to identify brushite.
Not Utterly Unreliable
My own work with Joan Parks compared kidney stone content of CaP – as hydroxyapatite to urine pH and supersaturations obtained by 24 hour urine samples. Unlike work from centers that performed their own kidney stone analyses we relied on a multitude of commercial lab reports obtained over decades. Even so urine pH and CaP supersaturations tracked will with these commercial lab results.
A Reasonable Conclusion
As an inexpensive and indispensable tool, all of us need and use commercial kidney stone analysis. What we know prompts wariness about missed struvite – a most important stone diagnosis. But perhaps that argues for multiple analyses – more tries lower likelihood of missing the diagnosis.
Make Followup 24 hour and Serum Measurements
It would seem unnecessary to say, but sometimes this obvious maxum goes unfulfilled. There is no use to changing diet – or trying to – or adding medications if one does not assure that the changes lead to a betterment of stone risk. I think followup urine collections for diet change should be when a patient believes the diet has changed and is tolerable enough to be used long term. With thiazide or potassium citrate, I favor 6 weeks initially. For all patients, followup with testing and a clinical visit should be yearly at least until stones become a thing of the pasts.
Aids for Patients Who Have Formed Stones
I have written several articles outlining the steps to prepare for and do testing, and for obtaining the most from physician visits.
This site has a large volume of articles. This page lists all of the articles by topic.
Chapters 2 – 6 of this book give a lot of background and links to related articles.
Chapters 7 – 12 concern specific stone forming systemic diseases.
Summary of Chapter One
The miserable fragments we call kidney stones have a complex origin in the kidneys. All but one kind contain crystals without which they could not exist. The exception, protein stones, occur rarely and I do not consider them here. Stone crystals form as all crystals form, from a solution overloaded with the crystal material – supersaturated with respect to the crystal of interest.
Many Paths to Stones
Kidneys can supersaturate urine by conserving water or by increasing the amounts of insoluble salt constituents such as calcium or oxalate. They can reduce the excretion of citrate, an inhibitor or change pH. The latter can be downward, fostering uric acid or upward fostering calcium phosphate crystals.
Treatment Synergy Requires Proper Testing
Although effective and obvious, extra fluids do not reduce new stone production completely to the baseline levels of average people. Moreover, above perhaps 2 to 2.5 liters a day of urine becomes difficult to maintain. So ideal treatments employ synergies – increase of fluids and changes in calcium, oxalate, citrate, or pH of urine as indicated in any one patient. Only blood and 24 hour urine testing can tell what is indicated in any one patient, and also what treatment has accomplished.
Stone Analysis is Crucial
Since all treatments but water relate to specific crystals, prevention depends on stone analysis whenever possible. Stone crystals can change over time and I see no reason to discard stones and good reasons to analyse them. Especially, infection or uric acid stones may complicate or even replace calcium stones and be missed without analyses. Likewise for stones from drugs.
Stone Prevention is Precision Personalized Medicine
Stone prevention exemplifies the best features of precision medicine. The crystals arise from specific supersaturations we measure in simple 24 hour urine samples and can reduce with healthy diet changes and a few medications that have proven their worth in trials. No two patients are quite the same, so each needs personalized care – stone analysis and 24 urine testing along with blood tests and clinical assessment to exclude systemic diseases.


Hello Dr Coe – this site has been very helpful to me, so thank you very much! I am hoping you can help me interpret my latest 24 hour urine calcium results. (53 yr old female, postmenopausal, healthy/active lifestyle and weight, diagnosed with osteoporosis, kidney ultrasound revealed 3 stones – 3mm, 4mm, and 1cm). After my first 24hr Urine Calcium test 5 months ago (which was 334) I have been eating a low sodium/high potassium diet and also eating 1000-1200 calcium/day. My latest results are as follows:
Calcium Oxalate Crystal Value = 1.00 (Normal value: Reference Mean= 1.59 DG)
Brushite Crystal Value = 1.00 *HIGH (Reference Mean = -0.11 DG)
Hydroxyapatite Crystal Value = 6.38 *HIGH (Normal value: Reference Mean = 3.62 DG)
Uric Acid Crystal Value = -3.66 (Normal Reference Mean = 0.89 DG)
Collection Duration = 24h
Volume Value = 2750 mL
Sodium = 83 (normal range 22-328 mmol/24h)
Potassium = 105 (normal range 16-105 mol/24h)
Calcium = 303 *HIGH (normal value <200 mg/24h)
Magnesium = 165 (normal range 51-269 mg/24h)
Chloride = 83 (normal range 34-286 mol/24h)
Phosphorus = 935 (normal range 226-1797 mg/24h)
Sulfate = 23 (normal range 7-47 mol/24h)
Citrate Excretion = 740 (normal range 385-1191 mg/24h)
Oxalate (U) = 0.22 (normal range 0.11-0.46 mol/24h)
Oxalate (mg) = 19.4 (normal range 9.7-40.5 mg/24h)
pH = 6.7 (normal range 4.5-8.0)
Uric Acid = 715 (normal range 250-750)
Creatine = 1073 (normal range 603-1783 mg/24h)
Osmolality = 318 (normal range 150-1150 mOsm/kg)
Ammonium = 25 (normal range 15-56 mol/24h)
Urea Nitrogen = 13.6 (normal range 7.0-42.0 g/24h)
Protein Catabolic Rate = 110 (normal range 56-125 g/24h)
Patient Surface Area = 1.73m(2)
Height = 163 cm
Weight = 50 kg
So as you can see my calcium only reduced a little. What type of stones do you suspect? Are oxalates a problem for me? Any advice on my next course of action?
THANK YOU for sharing your expertise to all of us!
JM
Hi Jennifer, Your urine shows isolated high calcium despite a modest sodium intake of 83 mEq/d. Oxalate is trivial for you being low – mid normal. So stones will be because of the high calcium. You could have idiopathic hypercalciuria which causes bone disease, postmenopausal bone loss which raises urine calcium especially at the outset, or both. I like the ample diet calcium for you, have no interest in oxalate, and if asked would try for even lower diet sodium. It will lower urine calcium a but more and is very good for bone mineral balance. With that, perhaps your might benefit from a bisphosphonate to stabile bone, and that might lower your urine calcium more. This is for your physicians to decide. Thiazide comes at the end of the list. I cannot say much more because I do not know the details of your medical situation and your physicians indeed do know them. But what I said is more or less commonplace and reasonable. Regards, Fred Coe
Hello Dr. Coe,
Your site has so much wonderful information – I can’t thank you enough. I had a kidney stone back in September 2023 which was lodged in my ureter and resulted in a lithotripsy. I am female, sixty-three, osteoporotic, 5’1 and about 105 lbs. I also take anti-seizure medication. My 24 hour urine collection showed that my urine citrite level was very low, less than 27 mg. My urine oxalate was 34 mg, my urine calcium was 159, ph was 7.148, sodium 67 mg and my phosphorus was 478. I follow a plant-based diet, so I don’t eat meat, I eat lots of fruits and vetables, so I can’t understand why my citrate level would be so low. Could it be pharmacological? I looked up the medication I am taking and it stated it only had a 4% increased risk of calculi. My urologist has put me on a low oxalate diet and advised me to purchase citrate beverage enhancers. Thank you!
Hi Theresa, The high urine pH and low citrate points to the seizure medication which probably inhibits carbonic anhydrase. Topiramate is the most famous of these. I am virtually certain it is the cause. Fred
Hi Dr Coe
New to this site but kidney stones for 20 yrs.
I had my last 24 hr urine test in August this year and although the results looked ok to me I am still forming stones. I’ve had to shockwave treatments on my left kidney in the last 3 yrs and the latest ultrasound was reported to have a 6mm stone in same kidney. I am 61 yrs old male, 145lbs and am an active person with a lawn service in this Texas heat during the summers. I’ve cut my salt and drink as much water as I can and somehow keep producing stones. My blood panel was all good and within positive ranges. Here are my results from my last 24hr urine test.
URINE VOLUME: (ml) 1,525
CALCIUM CLT TM (hr) value=24
CALCIUM,UR normal value: mg/dL Value=120
CALCIUM 24H UR normal value:100-300 mg/24hr Value:183
CREATININE CLT TM (hr) Value=24
CREATINE UR normal value:40-278mg/dL Value=80.67
CREATININE 24H UR normal value:1.0-2.2g/24hr Value=1.2
OXALATE UR -per volume mg/L Value=11
OXALATE 24H UR normal range: 16-49 mg/d Value=17
SODIUM CLT TM (hr) Value=24
SODIUM UR normal value:mmol/L Value=37
SODIUM 24H UR normal value:40-220 mmol/24hr Value=56
CITRIC ACID URINE PER VOLUME mg/L Value=56
CITRIC ACID URINE PER 24hr normal range:320-1240 mg/d Value=471
CREATININE URINE PER VOLUME mg/dL Value=78
CREATININE URINE PER 24hr normal range:800-2100mg/d Value=1190
CITRIC ACID/CREATININE RATIO,UR Value=396
URIC ACID CLT TM (hr) Value:24
URIC ACID UR normal value:mg/dL Value=21.1
URIC ACID 24H UR normal value:200-1000mg/24hr Value=322
POTASSIUM CLT TM (hr) Value=24
POTASSIUM UR normal value:mmol/L Value=33
POTASSIUM 24H UR normal value: 26-123 mmol/24hr Value=50
PHOSPHORUS CLT TM (hr) Value=24
PHOSPHORUS UR normal value:mg/dL Value=82.5
PHOSPHORUS 24H UR normal value:0.4-1.3/24hr Value=1.3
SULFATE 24H UR normal range:7-47 mmol/24h Value=13
PH URINE Value=5.98
Please help me make sense of what I may be lacking or excessive on
Also, the last ultrasound said I had simple cysts on my kidneys and that scares me a lot.
Thank you.
Chuck
Hi Chuck, I see nothing wrong and suspect the stones are from low urine volumes from your occupation and where you live. Your 24 hour urine volume is frankly low – risk begins below 2000 ml. The urine oxalate seems low and therefore I suspect this test was done by an inferior laboratory. A lot of information is not present. Your physician might want to use Litholink (a branch of LabCorp) that does a better job. Right now I have to guess it is a need for much more water when working. Regards, Fred Coe
Hello Dr Coe – this site has been very helpful to me, so thank you very much! I am hoping you can help me interpret my latest 24 hour urine calcium results. (53 yr old female, postmenopausal, healthy/active lifestyle and weight, diagnosed with osteoporosis, kidney ultrasound revealed 3 stones – 3mm, 4mm, and 1cm). After my first 24hr Urine Calcium test 5 months ago (which was 334) I have been eating a low sodium/high potassium diet and also eating 1000-1200 calcium/day. My latest results are as follows:
Calcium Oxalate Crystal Value = 1.00 (Normal value: Reference Mean= 1.59 DG)
Brushite Crystal Value = 1.00 *HIGH (Reference Mean = -0.11 DG)
Hydroxyapatite Crystal Value = 6.38 *HIGH (Normal value: Reference Mean = 3.62 DG)
Uric Acid Crystal Value = -3.66 (Normal Reference Mean = 0.89 DG)
Collection Duration = 24h
Volume Value = 2750 mL
Sodium = 83 (normal range 22-328 mmol/24h)
Potassium = 105 (normal range 16-105 mol/24h)
Calcium = 303 *HIGH (normal value <200 mg/24h)
Magnesium = 165 (normal range 51-269 mg/24h)
Chloride = 83 (normal range 34-286 mol/24h)
Phosphorus = 935 (normal range 226-1797 mg/24h)
Sulfate = 23 (normal range 7-47 mol/24h)
Citrate Excretion = 740 (normal range 385-1191 mg/24h)
Oxalate (U) = 0.22 (normal range 0.11-0.46 mol/24h)
Oxalate (mg) = 19.4 (normal range 9.7-40.5 mg/24h)
pH = 6.7 (normal range 4.5-8.0)
Uric Acid = 715 (normal range 250-750)
Creatine = 1073 (normal range 603-1783 mg/24h)
Osmolality = 318 (normal range 150-1150 mOsm/kg)
Ammonium = 25 (normal range 15-56 mol/24h)
Urea Nitrogen = 13.6 (normal range 7.0-42.0 g/24h)
Protein Catabolic Rate = 110 (normal range 56-125 g/24h)
Patient Surface Area = 1.73m(2)
Height = 163 cm
Weight = 50 kg
So as you can see my calcium only reduced a little. What type of stones do you suspect? Are oxalates a problem for me? Any advice on my next course of action?
THANK YOU for sharing your expertise to all of us!
JM
Hi JM, I think you are Jennifer as well whom I just responded to. As for your stones I cannot be sure but would suspect about 1/2 calcium oxalate half calcium phosphate – the latter perhaps may be more predominant. I have mentioned reasonable actions to consider in my prior note. Regards, Fred Coe
I am trying to find someone to manage a stone former in the Baltimore region. Do you have a recommendation for a referral?
Hello Doctor Helschien, Brian Matlaga, Hopkins. Brilliant surgeon and skilled at prevention as well. Fred
Thank you for continuing to help those of us whose urologists apparently don’t see the usefulness of interpreting the 24-hour test for patients—and the testing company doesn’t provide reference ranges for everything. So I don’t know where I stand with a Brushite of .56 DG—or the Citrate excretion of 653mg. My Hydroxyapatite is marked High at 5.37DG but I have no idea how high that is. My two oxalate tests are low moderate I think because there IS a ref range for that—15mg and .17mmol are my 24 hour values. I did have high calcium of 319 mg but before the test I was under the misapprehension from a superficial reading of your recommendations that I should be eating a very high calcium diet, so had been eating much more dairy than usual leading up to the test. Do you think I should get another test to determine whether high calcium is actually a problem for me? I also had been drinking large volumes so had a high urine 2900 mL volume. My sodium was 46 mmol and uric acid excretion was 435 mg. I now know I actually haven’t had a stone but was told I had one based on two X-ray and ultrasound readings by a radiologist, but my father was a repeat stone former and my grown daughter has also had one before age 35. So now that my consciousness has been raised I am taking this very seriously. Thank you for any insights and for your kindness in continuing this service.
Hi AManda, I think you have idiopathic hypercalciuria and so does your father and daughter. The low urine sodium should lower urine calcium a lot and if yours was 319 and sodium was only 46 mmol/d it may be a very active form of this disease. If you had such findings in your urine as I wrote, and if you were my patient, I would measure serum phosphate and calcium fasting in the morning, and also serum 1,25 vitamin D. If phosphate was low and the 1,25D high I would do gene testing. Best, Fred Coe
Oh my, thank you so much, Dr. Coe! I will actively pursue this with my urologist!
Hi Dr. Coe,
Thank you so much for the time you put into this great website.
I got my first stone surgically removed recently, and I was wondering if a small percentage of Calcium Phosphate in a stone’s composition makes it a Calcium Phosphate stone — or are only stones formed of a majority of CAP considered so? I just want to go down a prevention path, and I think your opinion on my stone “type” will provide a great foundation! My stone lab results, as they were sent to me, are:
80% calcium oxalate monohydrate
10% calcium oxalate dihydrate
10% calcium phosphate (hydroxy- and carbonate- apatite)
Thank you!
Hi Caroline, No. The 10% does not make it. But I would seek prevention – stones are nasty. Fred
Calcium Oxalate stone was removed. Have at least another in the making.
Litholink Test Results:
Cystine, Urine, Qualitative 01 Neg Negative
Urine Volume (Preserved) 01 2680 mL/24 hr 500-4000
Calcium Oxalate Saturation 01 2.64 Low 6.00-10.00
Calcium, Urine 01 190 mg/24 hr 450
Calcium Phosphate
Saturation 01 0.44 Low 0.50-2.00
pH, 24 hr, Urine 01 5.910 5.800-6.200
Uric Acid Saturation 01 0.42 <1.00
Uric Acid, Urine 01 461 mg/24 hr <800
Sodium, Urine 01 159 High mmol/24 hr 50-150
Potassium, Urine 01 45 mmol/24 hr 20-100
Magnesium, Urine 01 125 High mg/24 hr 30-120
Phosphorus, Urine 01 954 mg/24 hr 600-1200
Ammonium, Urine 01 44 mmol/24 hr 15-60
Chloride, Urine 01 156 mmol/24 hr 70-250
Sulfate, Urine 01 47 meq/24 hr 20-80
Urea Nitrogen, Urine 01 10.72 g/24 hr 6.00-14.00
Protein Catabolic Rate 01 1.0 g/kg/24 hr 0.8-1.4
Creatinine, Urine 01 1280 mg/24 hr Not Applic.
Creatinine/Kg Body Weight 01 16.3 mg/24 hr/kg 11.9-24.4
Calcium/Kg Body Weight 01 2.4 mg/24 hr/kg <4.0
Calcium/Creatinine Ratio 01 148 mg/g creat 34-196
PTH test were:
70.5 pg/mL
69.6 pg/mL
Not sure if I am to be worried or not.
Urologist only said to drink water with lemon.
I know there's more to it than that.
Hi Steve, THis is a second copy but I have another comment. The borderline PTH. IF your morning fasting blood calcium is normal, it is probably secondary increase of PTH from low calcium diet, perhaps, or slight reduction of kidney function common at your age. If blood calcium is at all increased one is concerned for primary hyperparathyroidism. Regards, Fred Coe
Dr. COE
You are a tremendous asset to the stone formers and a great human being. I did a 24 hour urine test and my Dr. said nothing other than my salt was high and handed me a contradictory pamphlet. I was crushed. He said I could see his Nephrologist, but soonest appointment was 9 months later! I’ve had 3 surgeries to remove stones and passed several others and currently have at least one in my kidneys. Can you decipher my urine test? Or give a recommendation on who could? All my stones were calcium oxalate. THANK YOU!
Component Sep 3, 2024
-Cystine, Ur
Normal Range: Negative Neg
-URIC ACID URINE
Normal Range: <800 mg/24 hr 693 mg/24 hr
-Sodium, Ur
Normal Range: 50 – 150 mmol/24 hr (high)
202 mmol/24 hr
-POTASSIUM, URINE
Normal Range: 20 – 100 mmol/24 hr 35 mmol/24 hr
-MAGNESIUM URINE
Normal Range: 30 – 120 mg/24 hr 109 mg/24 hr
-Phosphorus, Ur
Normal Range: 600 – 1,200 mg/24 hr 954 mg/24 hr
-AMMONIUM URINE
Normal Range: 15 – 60 mmol/24 hr 30 mmol/24 hr
-Chloride Urine
Normal Range: 70 – 250 mmol/24 hr 173 mmol/24 hr
-SULFATE URINE
Normal Range: 20 – 80 meq/24 hr 33 meq/24 hr
-Urea Nitrogen, Ur
Normal Range: 6.00 – 14.00 g/24 hr 8.84 g/24 hr
-Protein Catabolic Rate (low)
Normal Range: 0.8 – 1.4 g/kg/24 hr
0.7 g/kg/24 hr
-URINE VOLUME
Normal Range: 500 – 4,000 mL/24 hr 2,230 mL/24 hr
-Creatinine, Ur
Normal Range: Not Applic. mg/24 hr 1,727 mg/24 hr
-Creatinine/KG Body Weight
Normal Range: 11.9 – 24.4 mg/24 hr/kg 15.2 mg/24 hr/kg
Component Sep 3, 2024
-Calcium/Kg Body Weight
Normal Range: <4.0 mg/24 hr/kg 2.6 mg/24 hr/kg
-Calcium/Creat.Ratio
Normal Range: 34 – 196 mg/g creat 171 mg/g creat
-COMMENT Note
-Calcium Oxalate Calculation
Normal Range: 6.00 – 10.00 9.60
-Calcium, Ur (high)
Normal Range: 450 mg/24 hr 721 mg/24 hr
-Calcium Phosphate Saturation
Normal Range: 0.50 – 2.00 1.86
-pH, 24 Hr Urine. (high)
Normal Range: 5.800 – 6.200
6.398
-Uric Acid Saturation
Normal Range: <1.00 0.28
Hi Greg, I am having trouble getting your numbers straight: sodium 202 mEq/d; calcium ?; volume 2230 ml/d; mg calcium/gm creatinine = 171; creatinine = 1.727 gm/d; therefore total calcium per day = 171 mg/gm creat x 1.727 gm creat/d or 295 mg calcium/d – this is high enough to cause stones. Oxalate is not shown. pH is a bit high at 6.4; SS CaOx 9.6 – no oxalate posted, and CaP SS 1.86 this reflects the high calcium and pH. So you have high urine calcium and pH and can corm calcium oxalate or calcium phosphate stones – no analysis posted. As you have no access to physician help right now I would suggest the kidney stone diet which will tend to help. Probably you have idiopathic hypercalciuria, but that is a guess as I have incomplete information. Best, Fred Coe
Hi Dr Coe,
28yo male. I had my first stone about a year ago and recently had surgery to blast another stone that got stuck, they also cleared 4 stones from my kidney. The analysis has come back now at 65% phosphate and 35% oxalate.
The advice my urologist has given me is to just drink more water with lemons and I’ll have a CT in 6 months. He doesn’t want to do any other testing.
Should I be pushing for more testing?
(I live in the UK).
Thank you.
Hi James, Indeed I would suggest 24 hour urine testing to determine what is wrong, I would guess high urine calcium and low urine citrate and high urine pH, but that is mere guessing. Calcium phosphate stones are less common in men than women and worrisome so I would pursue a proper evaluation. In UK that is possible, though a bit harder than it should be. Best, Fred Coe