LISTS – AND LISTS
I know you are all looking for THE list. Here is one from a reliable source I have have downloaded on my site to a separate document so it opens with one click.
The reliable source, as it turns out, needed some updating. Dr Ross Holmes, professor, School of Medicine, University of Alabama, was kind enough to review the work of Dr. Michael Liebman who is a professor of Human Nutrition and Food Option at University of Wyoming and determine which food entries on the Harvard list needed changing. We cannot change the original but we have updated our lists accordingly and annotated updates with *** marks. So the lists here are the most recently edited available at present.Fred Coe and I have updates and annotated the list for those with a tendency to perfectionism: Updated table of oxalate foods. Set it at 50% for easier reading. Get yourself acquainted with the lists. They will tell you much of what you need to know. A lot of it will even surprise you. You are not as restricted as you think you are or as you have been told.
A more dramatic list is the 177 high oxalate foods we distilled out of the big list. Here are culprits! Not on this list? Probably not very high in oxalate so far as we know – with perhaps a few exceptions. Note that quantity is critical. For example black pepper is high in oxalate but the amounts used are small enough that total oxalate intake from it is negligible.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
LET’S DIVIDE AND CONQUER
FOODS TO WORRY ABOUT
A List of Concerning Foods
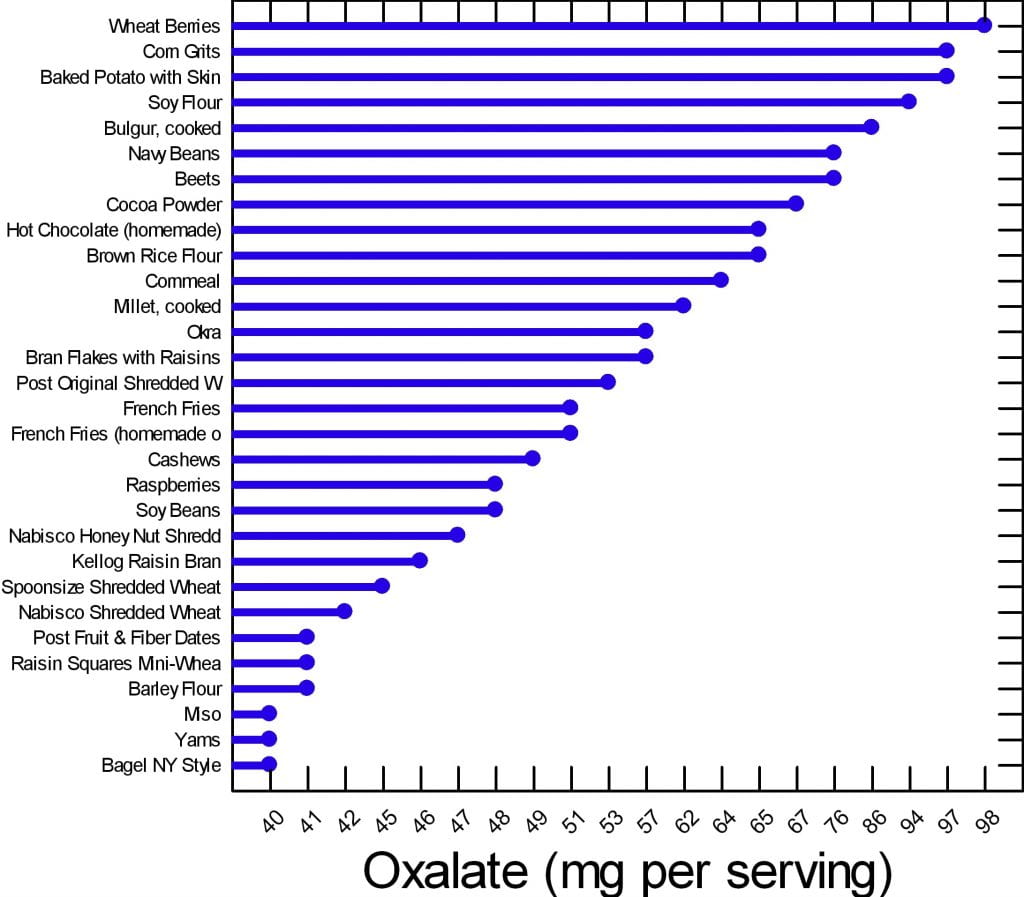
We have created two graphs for this article. Of the 177 foods on our master list, many are of concern but can be used in your diet if you control the portion size and how often you use them. There are 30 of them that are worrisome enough to deserve special attention.
Here are the 30. The graph shows mg of oxalate in a common portion. The details of the portions are in the complete list. The foods have in common that all contain at least 40 mg/serving. All other foods for which we have reliable data have less oxalate per serving.
Your budget is about 100 mg/day.
What does this graph mean? Does it mean you can never have chocolate, or a baked potato?
No.
It means if you want to use your whole budget on a treat, do it, but keep track and make sure you do not overspend in any meal or in any one day. Have your baked potato, but maybe share half with your partner. Or, have some hot chocolate but make it with milk because calcium helps reduce oxalate absorption. Eat your cashew nuts, but pay attention to how many. If one handful leads to ten, you cannot have them.
FOODS TO AVOID
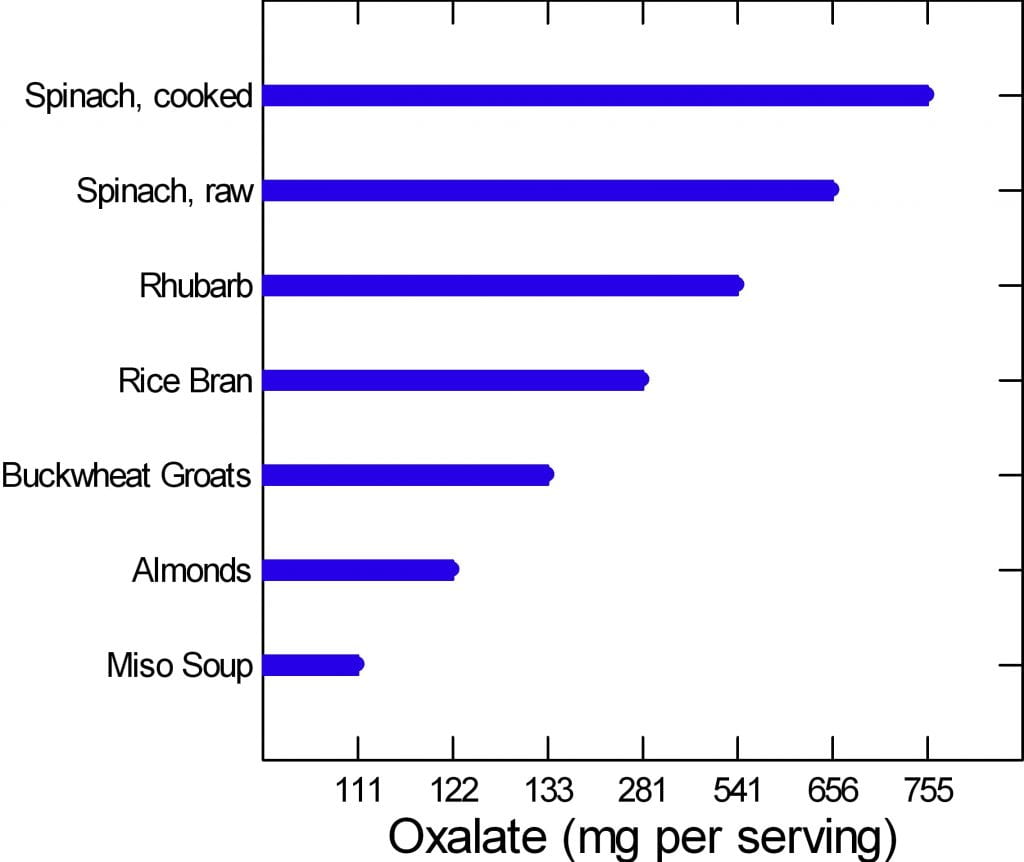 The graph to the left is of the very few dangerously high oxalate foods.
The graph to the left is of the very few dangerously high oxalate foods.
There are only six foods, but spinach, being worst of all, has two entries. Be careful of this plot because of its range. It begins at 100 mg/portion and rises to 755 mg/portion in only 7 steps, so the distance from miso soup to spinach is about a 7 fold increase.
Rhubarb and spinach are so high you just cannot eat them. Rice bran is something few will miss, the same for buckwheat groats.
People like almonds but have a hard time controlling portion size. If you can keep it to 11 almonds a day – the portion size that gives 122 mg of oxalate, alright. Otherwise stay away from them.
If you have to eat any of these foods, caution is hardly a strong enough word.
Are you sure you need to eat them?
Why?
WHAT ARE WE SAYING?
We are saying that oxalate is common in foods, and that you have to be careful, but care is a scarce resource. How much care can you give every bite? The graphs say if you eat moderately high oxalate foods – the first graph – be careful.
Watch portions.
If you are eating one of the six dangerously high oxalate foods, stop eating it.
It is too hard to be careful with those six foods. They have too much oxalate for most of you to handle. So, just say no.
WHY BELIEVE OUR DATA?
These data arose from a major effort at the Harvard School of Public Health. A world class expert has curated it twice. Harvard can be wrong and so can Ross Holmes, but both will tend to be wrong less often than the average persons who attempt to put complex data into the public domain. We have always appreciated comments, and if anyone has a peer reviewed publication with different food oxalate levels than ours, we will read the paper and see if it warrants our making a change.
Medical research is endlessly argumentative, and food oxalate is no exception. A recent paper contrasts findings from 6 websites and 2 applications and finds some wide variations. Of the sites, the Harvard site – used here as our reference, and the Wake Forest site – which is a legacy of an outstanding investigative group have most standing with me. Leaf through the comparisons between them in the 4 charts and in the large table at the very end. On the whole differences are modest. The hyperoxaluria and oxalosis list from the paper has been withdrawn from their site.
DO YOU NEED A LIST?
Sure, a list is nice. But we helping you here. Lists can run on to hundreds of foods. The picture is meant for focus. Here are the ones to focus on.
Many of you leave the doctor’s office thinking you will never be able to eat a fruit or vegetable again. If that wasn’t bad enough chocolate and nuts are gone, too. Some of this sadly is true, most of it is not. I am here to bring you good news: Almost everything, high oxalate or not, can be incorporated into your diet safely.
Do you need a low oxalate diet? You may if your stones contain calcium oxalate crystals and your urine oxalate is high enough to pose risk.
If you do need a low oxalate diet, what is your goal? Less than 100 mg of diet oxalate is good; less than 50 mg is ideal.
If you want to read some of the science about urine oxalate and risk of stones and about how we get to the diet oxalate goals, it is summarized at the end of this article.
Here we assume you do need to lower the oxalate in your diet.
CALCIUM FIRST
Low calcium diets can raise urine oxalate, and the solution may be as simple as a proper calcium intake. There is every reason for stone formers to eat 1000 mg of calcium daily to protect their bones. The common hypercalciuria of calcium stone formers puts bones at special risk when diet calcium is low.
Before changing your whole life around, ask yourself if you are avoiding calcium foods. If so, add them back and ask your doctor to check your urine oxalate again. It may fall enough that a low oxalate diet is not necessary.
If low calcium intake is not your problem, and you need a low oxalate diet, here is my take on how to do it.
WHAT IS THE DIET OXALATE GOAL?
Typical diets contain upward of 200 – 300 mg of oxalate. For stone prevention, a reasonable goal is below 100 mg of oxalate daily. An ideal would be about 50 mg daily if that can be accomplished.
To get there, consider the oxalate contents in common serving portions of all of the foods, and make up a plan for yourself.
FRUITS
FRESH
Everyone who comes to me is very unhappy thinking they can never have a berry again. This is Baloney. The only berry that is very high in oxalate is raspberries (look at the list). On the other hand, people do not realize avocado, oranges, dates, and even grapefruit and kiwi are very high and need caution.
This doesn’t mean you can never have these healthy treats. If you incorporate any of these high oxalate fruits into your morning yogurt you can reduce some of the effects of the oxalate content.
Also look at your portion sizes. You really cannot eat a lot at any one time. Dates are not a good bargain: One date is 24 mg!
CANNED OR DRIED
Canned pineapple is a problem.
Dried fruits have to be a worry because the water is taken out, so a ‘portion’ of dried fruit can be gigantic in oxalate content. Figs, pineapple and prunes are standouts. Just think: 1/2 cup of dried pineapple is 30 mg – not a lot of fruit for a lot of oxalate. If you want dried fruit, think about apples, apricots, and cranberry as lower oxalate options.
VEGETABLES
Spinach and rhubarb are standouts; stay away.
Other vegetables you need to be aware of are tomato sauce, turnips, okra, and yams (sweet potatoes) along with beans of different sorts.
I am not in the business of taking healthy foods away from people. But in the cases above you really must limit; there is just too much oxalate and these foods do not pair well with high calcium foods the way fruits can be mixed right into your yogurt or cereal and milk.
Many of you have been told to stay away from all green leafy vegetables. This is not true. Look at the list. There are plenty of salad options still available for you including kale. Even though tomato sauce is high in oxalate (see below) that is because of concentration. A whole medium tomato is only 7 mg and who eats more than one at a time?
Many of the salad vegetables are so low in oxalate they are freebies. Eat what you want.
POTATOES
These are Trouble! I put them into their own separate group even though they are vegetables.
From french fries to baked potatoes they are very high oxalate items. One ounce of potato chips has 21 mg of oxalate and who eats one ounce? Not I. Baked potatoes are terrible. One comes in at just under 100 mg of oxalate. Mixing sour cream into the potato will not help much; one tablespoon of sour cream contains only 14 mg of calcium. One ounce of cheddar cheese contains 200 mg of calcium, which could help, but it increases calories, salt and fat. But all in all, why struggle so hard? Potatoes are not ideal for stone formers.
DAIRY PRODUCTS
They have no oxalate. They are your main source of calcium. Use them. They can add a lot of salt – cheeses – and can be caloric. But they reduce oxalate absorption and preserve your bones.
For a stone former who has to watch salt intake, increase calcium intake, and lower oxalate intake, here is how to do that. You cannot have as much cheese as you want because of the salt. So portion sizes are very important. Yogurt, milk, even ice cream are good bargains – modest sodium and high calcium. These are a great place to add in a wee bit of chocolate – high oxalate foods – for those of you who cannot live without these high oxalate treats.
BREADS AND GRAINS
Some of the basic ingredients to make these foods are very high. White flour and brown rice flour are high in oxalate so everything you make from them will be high.
BREADS
Even so, as far as kidney stones go, breads are mainly alright because of portion size: not that much flour so one slice is 5-8 mg. French toast and New York style bagels top the list at 13 mg for two slices and 40 mg for one bagel – as much as anyone will eat of either food.
PASTA RICE AND GRAINS
Spaghetti, one cup cooked is 11 mg and most of us eat more than one cup.
Buckwheat groats, one cup cooked is 133 mg – I don’t see many of you saying ‘darn it’ or taking to your bed, but beware. Millet and bulger, wheat berries, rice bran, corn grits, and corn meal, these are widely used and are high. If you are using these, be thoughtful.
Here are some low oxalate options in this category: White rice, hummus, corn flour, corn bran, flax seed, and oat bran are popular and safe.
MEAT PRODUCTS
Since oxalate is only found in plant foods, all the meats are safe. Fish, too.
For our vegetarian friends, tofu and veggie burgers are very high.
NUTS AND SEEDS
These are just dangerous for two reasons.
Obviously they are very high in oxalate.
Secondly, I don’t know anybody who just has a few nuts at a time.
Just like chips no one eats one – the whole jar is more like it.
But, for one cup of pumpkin sunflower or flax seeds the highest is only 17 mg of oxalate and none for flax. For those of you who love foods in this category seeds are the better choice and they can be sprinkled on yogurt and ice cream.
SWEET STUFF
I have good news for my chocolate lovers. I know most of you have been sent home with a list and chocolate is high on it. But if you look at the numbers nuts are a lot worse than chocolate. Chocolate can be mixed in with dairy products, too, so as to reduce oxalate absorption.
Even so I do want to point out that half a brownie is on the high side, and who eats one half?
You can still satisfy your sugar craving but pay attention to your portion size.
Keep in mind, however, that sugar loads increase urine calcium loss which increases stone risk, so there are two reasons why this food group can be a problem.
But even without chocolate, you eat a lot of flour when you eat a piece of cake, so cake can be a problem – about 15 mg per piece, like french toast. Pies are half the risk because of their fillings – unless they are chocolate pies!
CRACKERS AND CHIPS
The big enemy here is potato chips. A one ounce serving contains a whopping 21 mg of oxalate. I repeat: A one ounce serving.
Your best bet in this category if you’re looking for something crunchy is corn chips – one ounce is 7 mg, popcorn – one cup is 5 mg, and pretzels, one ounce is 5 mg.
Crackers are OK mainly because they are small and the amount of flour is not that much.
BEVERAGES
PLANT SOURCES
Hot chocolate is the clear loser at 65 mg per cup; carrot juice is the runner up at 27 mg per one cup. Lemonade, tea, tomato juices, rice dream and the like are better but still high. The are 15 – 18 mg per serving. Lemonade – frozen concentrate – is 16 mg per 8 ounces so be careful about this as a source of citrate.
Soy milk, for those of you who prefer it, is not a good option. It is very high at 20 mg per cup. We have no data from standard sources for rice milk, cashew milk, and coconut milk; almonds are high in oxalate so the almond milk product will certainly be high.
Tea is so commonly used, here are the details. If you brew your own tea it is high in oxalate. The longer you steep your tea, the more oxalate it will have in it. If you use a sweetened instant iced tea one cup has 0 mg of oxalate.
Here are some juices that are low in oxalate and better substitutes: Apple juice, apricot juice, orange juice, grapefruit juice, grape juice. For all the lemonade drinkers, diet lemonade is low in oxalate.
Here is something very important: Coffee is oxalate free – almost, 1 mg for a cup (2 mg/cup for decaf). We already told you that coffee drinkers have a reduced stone risk, so lets debunk the coffee myth here: Drink it as you wish.
DAIRY SOURCES
Everything is good except chocolate milk. Even that is only 7 mg a cup for a sweet treat here and there.
ALCOHOL
What tops the list in this category is a can of beer: 4 mg of oxalate. All the rest are low and, frankly, the oxalate in a can of beer comes with a lot of fluid. This is not the problem area for stone formers.
WATER
If I didn’t say this to you I could not sleep well tonight. Water is the clear winner in this whole category. It is free of calories, sugar, and oxalate. Please use it as your main beverage and supplement with the items above.
SPREADS AND SAUCES
Chocolate, miso, peanut butter, and tahini are all high.
SOUPS
Miso soups is extremely high – 111 mg/cup. Lentil soup is high, and so is clam chowder – the potatoes.
BREAKFAST FOODS
This is a dangerous meal if you are a cereal lover. Many cereals are high in oxalate. I am afraid you need to look them up in the list by brand. Unfortunately the healthier cereals are highest in oxalate because they contain more plant based ingredients. Probably having milk in your cereal is wise, but we have no data to show.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
HOW DO WE MANAGE ALL THIS?
The first thing you need to do is to learn and remember what are the highest oxalate foods and beverages. Without this in mind it is impossible to shop and cook intelligently. Here is a short list of the highest oxalate foods all in one place.
BREAKFAST
For those of you who love cereal because it is quick and easy check out the list and see if the one you love is high in oxalate. If it is, choose the next best one with lower oxalate. Put milk in the cereal.
Alternatives to cereal that are also quick and easy: Yogurt or cottage cheese and fruit. The only fruits to worry about are raspberries because no one puts oranges on their yogurt. Bananas, peaches, blueberries and strawberries are perfect toppings.
More trouble, but no oxalate, eggs any way at all. Boil a batch on Sunday and have them for the week for breakfast, and snacks, too.
Your breakfast coffee is free and so is your water. For juices use orange, apple, pineapple, grapefruit – all great. If you want tea, don’t steep more than a minute and consider adding milk to it. Green tea is better than black.
LUNCH
Typically you are grabbing a salad or a sandwich for lunch, so what now? Many clients tell me they no longer eat salads because their physicians told them to stop all green leafy vegetables.
I’m bringing salads back to you.
Arugula, iceberg, romaine lettuces, and kale, are fine as your base. Stay away from spinach. Here are good toppings. Cauliflower, corn, cucumber, mushrooms, onions, peas, scallions, squash and zucchini are all fine. Tomatoes are fine, too; it is only the sauce that is high. Broccoli and green pepper are moderately high so watch the portion size.
Sandwiches will cost you between 12 and 16 mg of oxalate depending on the bread you are using – 2 slices. This doesn’t mean you can never have a sandwich, it just means you have to keep track of how much. You can have 50 to 100 mg daily. What goes inside between the two slices of bread is usually cheeses and meats which are oxalate free. So sandwiches are not something to be afraid of.
SUPPER
Beef, chicken and fish are all fine, and those the main courses for most of us. You will run into problems if you are a pasta or potato eater. If you are you need to limit the amount of times you have these foods each week and also the quantity each time you use them. Substitutes are a problem: White rice is a nice substitute for potatoes but there are few others. It is more veggies that have to fill in – very healthy but not as much fun.
Here is a recipe for cauliflower – ‘mashed potatoes’ you will like and even think, sometimes, is the real thing. There are many versions on the web, choose the one that makes you happy but be careful about the ingredients.
There is also quinoa which is not on our lists, but may well be high. A recent scientific article on this plant does not give oxalate contents which suggests they are not reliably known.
I have recently put together a private FB page called THE Kidney Stone Diet. It is a group that helps educate you on your physician prescribed treatment plans. As you can imagine, oxalate comes up in many posts. I moderate it to keep it clinically sound. Come on over and join the discussion!
URINE OXALATE AND RISK OF KIDNEY STONES
I promised you some science – here it is for those interested. It concerns only highlights from the food – urine oxalate research recently performed and seemingly germane to the problem of how stone formers should control oxalate intake.
The most useful data about urine oxalate we have so far is from three cohorts studied by Dr. Gary Curhan. Two are cohorts of nurses one a cohort of physicians. These people have kept track of many aspects of diet and health for decades, and among their records are onset of kidney stones.
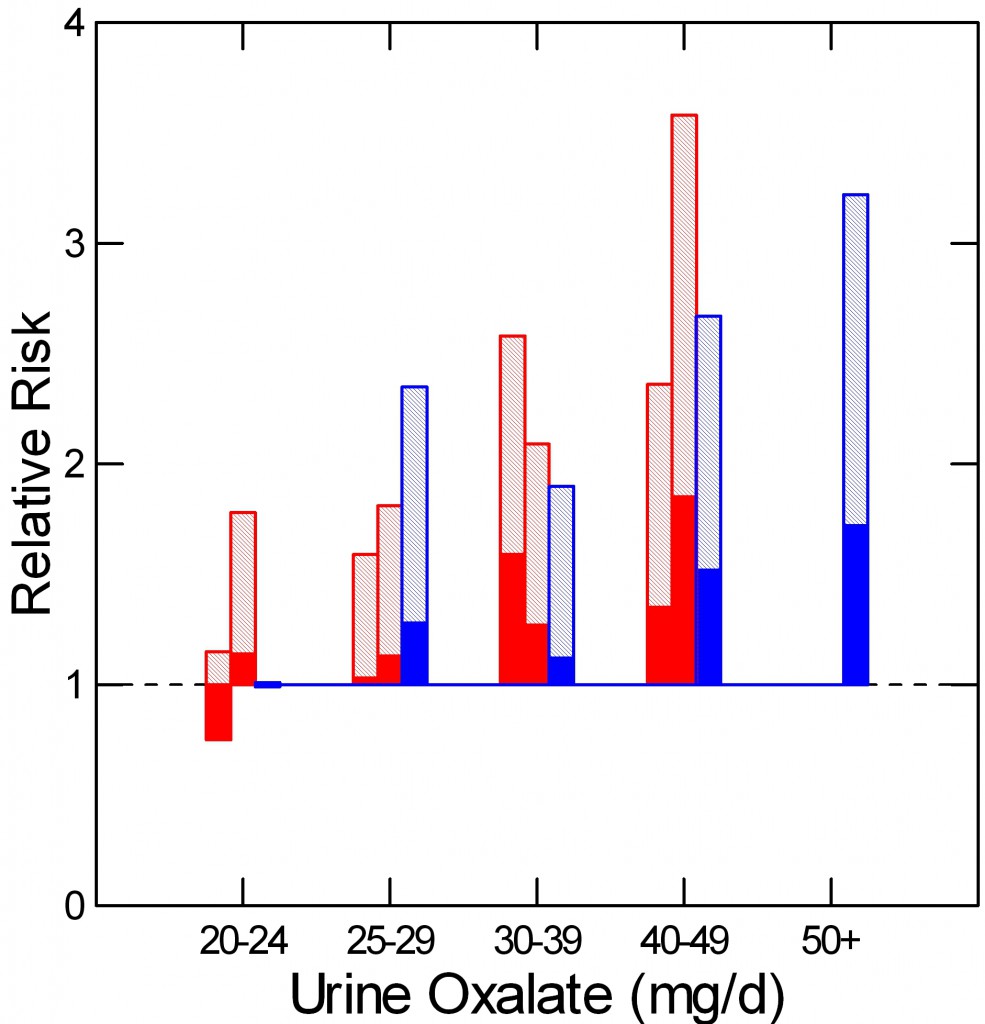 As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
The two nurse cohorts are red, the physicians – all men – are blue. The dotted line at 1 is the risk threshold: Above that line, risk is present.
The top of each crosshatched bar shows the mean relative risk for each of the five urine oxalate ranges. Clearly the mean goes up as urine oxalate goes up.
But the mean relative risk has a range of uncertainty around it. The bottom of the solid portion of each bar is the lower 95th percentile for that range of uncertainty. When that bottom lies above 1, risk is very likely to be present.
For both the women and men groups, that point is reached between 25 and 30 mg of urine oxalate a day. Therefore one wants to try to get urine oxalate below 30 mg daily and even lower, below 25 mg daily if possible. The average urine oxalate excretion among the women in this study was close – 26 and 28 mg/day for those who did not form stones and just a bit higher for those who did – 28 and 30 mg per day. The men are a problem: 39 and 41 mg/day for those who did not and those who did form stones.
This is not diet oxalate, it is urine oxalate. Urine oxalate is how much the body makes and how much is absorbed from foods. Mostly, we can control only the second part – how much is in the food.
HOW MUCH DIET OXALATE DAILY
All dietary advice depends on having a reasonable goal in mind for oxalate intake. My goal of 50 – 100 mg of oxalate from food daily is not unreasonable given the research that has been done in normal people and stone formers.
Holmes and colleagues found a urine excretion of oxalate of about 10 mg/gm urine creatinine in normal 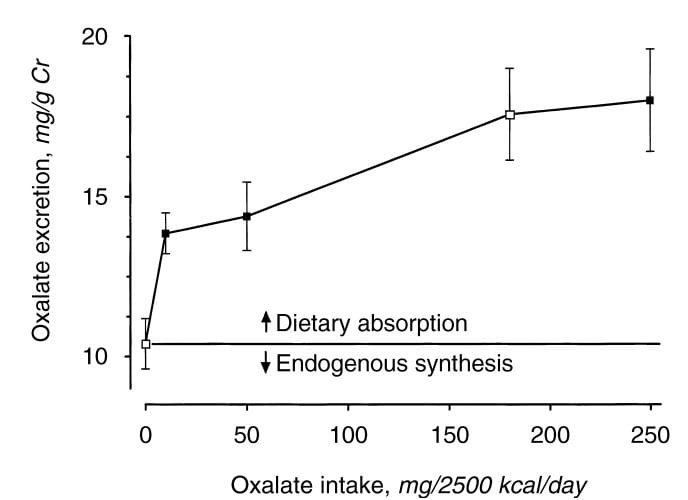 people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
From this work the percent oxalate absorption could be calculated as around 10 – 15% and the contribution of diet oxalate to urine oxalate excretion as around 25 – 40% when intake of oxalate was between 50 and 350 mg/2500 kcal. Therefore one can consider a whole food 1000 mg calcium 50 mg oxalate as a usable low oxalate diet, and a 150 – 250 mg oxalate diet as relatively high.
The balance between diet calcium and diet oxalate does not matter greatly if diet calcium is high. Among normal men and women eating 1000 mg/day of calcium and 750 mg/day of food oxalate, 24 hour urine calcium was about 110 mg/day and oxalate about 44 mg/day.
If the calcium oxalate balance is altered so calcium intake is 400 mg and 20 mg of oxalate at breakfast and lunch, and 200 mg of calcium and 710 mg of oxalate at dinner, as compared with simply 333 mg of calcium and 250 mg of oxalate in all 3 daily meals, urine oxalate is lower after the high calcium low oxalate meals, but only slightly higher after the high oxalate low calcium evening meal than when calcium and oxalate intakes were balanced. This means that when diet calcium is at least 1000 mg daily the balance of calcium to oxalate within any one meal is not likely to affect stone risk.
Seiner and colleagues make clear that stone formers are different from normal people. They divided male and female stone formers into 2 groups of 93 people each, one with urine oxalate above 0.5 mmol (~50 mg) of urine oxalate daily and the other with urine oxalate below 0.4 mmol (~40 mg) daily. They found virtually identical calcium and oxalate intakes: 845 vs. 812 calcium and 101 vs. 130 mg daily of oxalate respectively in the lower and higher urine oxalate groups. But the below 0.4 mmol group excreted only 27 mg of oxalate daily on average, whereas the high oxalate group excreted 64 mg daily. In other words diet was not responsible for the higher urine oxalate excretion, suggesting a difference of oxalate absorption. Those prone to high oxalate excretion seem, therefore, to most need diet modification.
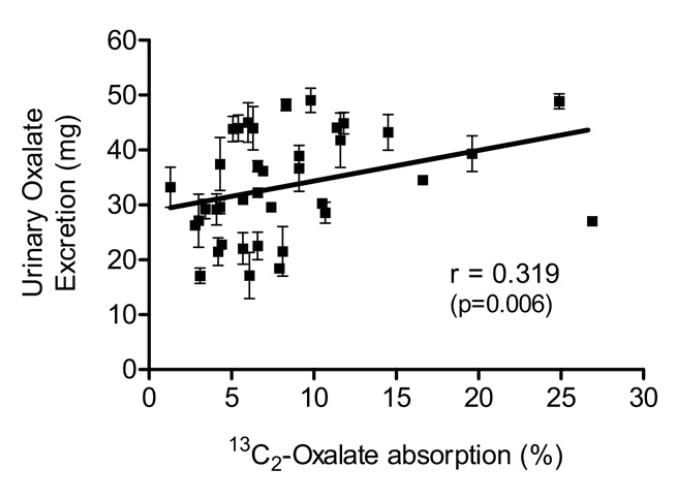 Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
PROTEIN AND GELATIN
Diet protein intake does not affect urine oxalate excretion. In 11 normal people fed a 1000 mg calcium, 51 mg oxalate, 3000 mg sodium fixed diet, varying protein intake from 0.6 to 1.6 gm/kg/day – a very wide range – did not alter urine oxalate appreciably (mean values were 23, 23, and 25 mg daily for the three protein intakes) even though oxalate precursors like glycolate rose markedly (25, 22, and 46, mg daily).
Jello is a source of hydroxyproline which converts to glycolate and oxalate, and oral loading with gelatin can raise urine oxalate. Ten normal people eating a 1000 mg calcium, 150 mg oxalate diet (typical normal level) were fed supplemental gelatin as one quarter of daily protein intake. Urine oxalate was 24 mg daily vs. 17 mg daily when the same diet was supplemented with whey protein – containing little hydroxyproline – as a control. So lots of jello is not an ideal plan for stone formers.
Where does this leave us about how much oxalate is alright for a day. If diet calcium is high, as it should be, at about 1000 mg, then one should try to limit diet oxalate below 100 mg daily. Perhaps this is most important in those patients whose baseline oxalate excretions are higher – in the range of above 40 mg daily.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life.
For those who need special help, I run an online course: The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.



Dr.Coe, I just had a total work up. My Urologist says my levels are fine. I have two stones, 1mm and 2mm that have not changed size or moved in the two years since the CAT. I had one other stone, at 1mm that passed out two
years ago. I had an ultrasound and an x-ray this time. The only issue I could see from the 24 hr urine was my urine ph was 6.7 which is not surprising considering the trouble I have getting enough water or liquids.
So if I email you the lab results from the 24 hr urine and the blood test, and the screenings, could you see what you might see as an issue ? I would certainly be willing to pay for it. Rose F.
Hi Rose, I would be pleased to help, but your physician needs to be involved. Here is the issue; answering questions here is not the practice of medicine – just advice and information. But if I look at your results and tell you things to do as a specific to your condition, it is, and I do not know all about you – so I would be practicing medicine badly. To really prevent stones I need to know all about someone. This means I can surely tell you and your physician what the numbers mean, qua numbers, but she/he is responsible for you. Regards, Fred Coe
Hello Dr. Coe, just yesterday I had a bladder scan and CT pelvic scan without contrast which revealed a new focal calcification of 1.7 cm at the posterior right bladder. The catylsy to my going to the ER was bright red urine followed by total blockage. I was told this is a very prominent bladder stone at 1.7 cm ( not mm). I now have a catheter in and am waiting to see Urologist for cysto and assumed plan to wave or laser the large mass. My pH score is 6 and glucose, bilirubin and ketones were all negative. Any thoughts on how to attack this massive stone beast? Thanks-
Hi Tom, The large bladder stone can be removed and will be. The common cause is usually twofold: some outlet obstruction from prostate and some cause of excess crystal formation. The former is urological. The latter is standard 14 hour testing for causes of stones. Here is a good plan. Regards, Fred Coe
I have Crohns disease and have had two feet of my small bowel removed. This includes the ileocical valve which makes absorption an issue. I have done the 24 hour urine collection and my oxalate level was 121! I just passed my 4th stone in 5 years and they aren’t small. I hardly eat anything on the Harvard list except potatoes which are now out. I eat lots of cheese, yogurt, pudding and ice cream so I think I get a lot of calcium in my diet. I receive iron infusions and B-12 shots because of the bowel loss and poor absorption. I am low in Vitamin D always. Taking supplements helps slightly. I was told that the loss of that important part of my bowel may be contributing to my high oxalate because my bowels are not absorbing it and it makes its way into my kidneys. Have you heard this before in post surgery Crohns patients? If so, do you have any advice?
Hi Liz, I am afraid I have heard of it all too often. Oxalate is being absorbed in your colon because of the short bowel. Treatment is complex, but a good starting place is high calcium diet planned so high calcium foods are eaten WITH your larger meals. The timing is crucial. If high calcium foods are not tolerated, one can use supplements but the timing needs to be very accurate – the calcium will prevent oxalate absorption when present with the food oxalate. I try to get the best I can from calcium, and then add something more if I need to. I am sorry I have not as written a proper article on this. Warm regards, Fred Coe
Whew. 75 y/o cause. female just passed calcium oxalate stone on Christmas! I have primary immunodeficiency and do weekly infusions of 7 gm. Hizentra. Advised to d.c. calcium/VitD supplements. 24 hr urine calcium 9.2 on basically calcium free diet seven days prior to test. Plan to adapt contents of this paper into my life. Any other suggestions?
Hi Patt, Your treatment is wrong. Calcium oxalate stones are never treated with low calcium diet because that can cause bone disease and raise urine oxalate. You need a complete evaluation and treatment directed from what is actually wrong. The urine calcium of 9.2 is not clear to me – is that 9.2 mmol/d 360 mg? or is it a blood calcium – normal value. If you have a high urine calcium loss low calcium diet is particularly bad. Take a look here, and see if you can get a better fix on what is wrong and what to do.
I am a student of Jill’s Kidney Stone Prevention Course and an avid reader of your work. In 2017 I had 13 kidney infections with 15 rounds of antibiotics, kidney stones, 3 surgeries, have a tiny duplex kidney with duplex ureters so tiny the surgeon barely could get stents in which I promptly enjoyed for 3 months. So naturally I am very interested in NOT making any more kidney stones!
Through my research, I have come across the term “oxalate dumping”. Oxalates are not just feared by calcium – oxalate kidney stone formers as the most common condition associated with excessive oxalates in the diet, but the inability to bind them with calcium in the “gut” and flush them out can causes excess to go back into the blood through the kidneys). I have also read that our body makes oxalates by “endogenesis”.
Tell me if I am wrong, but our bodies can also store oxalates in the liver when we become overwhelmed with them as we only can pass so many at a time. So just eating enough a LOD and dietary calcium is NOT always just enough for many (with compromised gut flora). Must heal the gut so the process of eliminating oxalates can work like it should.
So, when someone goes on a LOD (too quickly vs lowering oxalates slowly) is it possible that the liver might “dump oxalates”?
I appreciate any thoughts that you have on this subject.
Hi Janene, The liver produces oxalate, and does not store it. Kidneys remove the net of what the liver produces and is absorbed by the bowel, minus that is secreted by the bowel from blood. Here is a review of the process. Dumping of oxalate from low oxalate diet is not a real phenomenon – it is nonsense. The idea of liver storage of oxalate is nonsense. Low oxalate diet and high diet calcium safely lowers urine oxalate. Regards, Fred Coe
Thank you Dr Coe, for your clarification about oxalate dumping. I am on a LOD and find it very difficult to get 800-1200 mg of dietary calcium. I purchased a liquid calcium citrate (600 mg), with magnesium citrate(300 mg) and vitamin D3(500 IU). I took this the day before and the day of my last 24 hr urine test in December 2017. My LabCorp results for calcium went up to 284 from 167 in October 2017). I stopped taking this product as I am now very supplement shy. My cit 24 went down fro 519 to 413. My nephrologist recently put me on Potassium Cit 1620mg per day. However, I am a CHF patient with a Medtronic pacemaker, so I also take 40mg of Lasix twice per day. (was on Potassium Chloride for 10 years) With that much Lasix I am afraid that there won’t be enough Potassium Citrate left at the end of the day. I am scheduled to do another 24 hr test after 6 weeks. Some days I just feel “broken” but I won’t stop trying to do my best to keep stones from forming. Thank you for all your research and year of helping those who suffer from kidney stones.
Hi Janene, You are a much more complex case than is usual in the stone world, and what we usually do cannot be applied in a simple way. Lasix itself raises urine calcium drastically. The dose is quite high, so I suspect your CHF is very significant. Perhaps the best approach is to speak with your cardiologist. Could your CHF be managed with chlorthalidone in place of lasix?? It would lower urine calcium and in full dose is a powerful diuretic. He/she might feel is a possible way out for you. Regards, Fred Coe
I have a dime size kidney stone lodged deep inside my kidney. I’ve had pain but no worse than any kidney stone I’ve ever had, which is only been one.
The physician’s assistant I saw this weekend told me that she called the doctor, at another hospital, and he told her I needed to have my kidney removed. An over the phone recommendation stunned me.
I have a friend who is a paramedic. She had a 3 in Staghorn kidney stone and was able to have lithotripsy and flomaxx using no stent.
Any response to that story?
Hi Karie, I am not so sure it is a good idea – we rarely remove kidneys because of stones. Please seek an opinion at a university hospital. Do not have a kidney removed without multiple opinions by some expert people. If it is for a stone, do not have a kidney removed at all. Regards, Fred Coe
Hi Dr. Coe,
From what I have read, certain bacteria and enzymes are able to break oxalates down. The problem as I understand it, is whether these bacteria and enzymes can survive the gut environment. What the is the research on this?
I found one product that claims to lower oxalates. See link below
https://www.nephure.com/
Have these been proven to work? Are there other commercially available products that have been proven to work in lowering oxalates? Why can’t food be treated with these bacteria and enzymes prior to food been consumed?
Thanks
Tom
Hi Tom, Enzymes do exist. This one has no decent trials so I cannot recommend it. As for treating foods, frankly oxalate is not so important as to warrant such a complex intervention. I presume you have stones disease and a high 24 hour urine oxalate level. Most high urine oxalate in stone formers comes from both high use of high oxalate foods and inadequate diet calcium. The latter is a bad thing of itself so one needs to add at least 1000 mg calcium as foods. And, the high calcium foods need to be where the oxalate is – larger meals. Likewise, we need to avoid high oxalate snacks – away from the diet calcium; nuts and chocolate come to mind. These simple steps will work and one does not need much else. Regards, Fred Coe
Hi Dr. Coe,
Thanks for the response. It sounds like from your statement that there are indeed proven enzymes and/or bacteria that work. Can you list some that have decent trials and are commercially available, so that I can look into it?
I travel a lot and it is not always easy to get the right amount of calcium with meals. I don’t have to tell you about the difficulty of being on a lowl sodium diet while traveling. Even when I did try a high calcium low oxalate diet, my urine oxalates were just above 50. So I am guessing if I were to go to a high oxalate diet, things might get even worse. And I do miss a lot of my favorite foods which are high in oxalates. In my view every little tool that I can add to my toolbox will help me not form stones.
Thanks
Tom
Hi Tom, there are no decent trials at all. For the moment, do not try to rely on alternative measures but use high calcium diet and oxalate moderation. If we ever get a proven version I will be the first to promote it. Regards, Fred Coe
Dr. Coe,
I was recently hospitalized for a creatinine of 3.8 and GFR of 15. I have never had a kidney stone, yet my biopsy showed healthy tissue loaded with oxalate crystals. I have changed my diet, increased my fluids and have had a lot of IV fluid, yet there are never any oxalate crystals detected in my urine. It seems like no matter what I do, the crystals are not flushing out. How do I get the crystals out? The tissue is healthy, I want to recover before there is damage.
Thank you,
Michele
Hi Michele, Unless you have some other cause, the diagnosis is primary hyperoxaluria, a very dangerous cause of kidney failure. You need special care, and right away, as it does not sound as though your present caregivers are familiar enough with this rare entity. Do something immediately. This is a very urgent problem. If you tell me where you live, I can try to find a place for you. The best is Mayo Clinic because they have a PH program. Dr John Lieske, there, is ideal. Fred Coe
Hi Dr. Coe,
I live in Oswego IL. I’ve been receiving care at Rush-Copley in Aurora. My doctor did tell me that she has never seen a case like mine before. Although she did mention at some point maybe Mayo, I did not feel the urgency projected in your response. I will not take that lightly and will address this right away.
Thank you Dr. Coe
Hi Michele, if Mayo is not practical, you live not far from us. Please do not tarry. I know what you have, and have considerable concern. While waiting, heep up high fluids and – almost the only time you will see me write this – an ample sodium intake to protect your kidneys. Do not use over the counter pain meds – NSAIDS – like Motrin or any related version. Do not use any diuretic agents. Let me know what happens. My secretary is Kathleen Dineen 773 702 1475 if you need anything while waiting for Mayo. Regards, Fred Coe
Hi Dr. Coe,
Mayo responded to me right away and I have a tentative appointment for Feb 20th. Thank you again for your help and direction.
~Michele
PS
My biopsy was sent to UofC. You’re welcome to look at it if you’d like.
Hi Michele, good. Do what I said: high diet sodium, no OTC NSAIDS, no diuretics, avoid dehydration. Give Dr Lieske my regards. Let me know how things turned out. It can be via personal email. Best, Fred
Hello Dr. Coe,
First off, thank you for all the valuable info you’ve shared.
I’ve got a question about dietary calcium. From what I understood, adequate dietary calcium “neutralizes” oxalates. Does it matter if Cal-rich foods are taken in the same meal as high-oxalate foods, or can cal-rich foods be spread out during the day? E..g., one meal has oxalates, the next meal/snack is high in calcium etc?… because dairy being the primary source of calcium, it’s hard to combine dairy products with some high-to-mod oxalate veggies.
Question #2: i’ve heard that too much calcium can lead to deposits and/or stones, too. I”ve also read that only about 50% of the consumed dietary calcium is absorbed, e.g., if I consume 250ml of milk which is, say, about 30mg of calcium, only about 15-20 will be absorbed. Is there any truth to that?… should one aim at more than 1000mg of cal per day to ensure that one actually absorbs 1000mg?… but then – how to avoid consuming too much calcium? … this whole cal situation is very confusing.
Question #3 – is oatmeal high in oxalates? steel-cut and old-fashioned?… I’ve gone through several “oxalate” content lists and some put it in high group, others – in moderate. So, where does it stand?… and in general, different lists of oxalate content from different sites often vary significantly. Where is the truth?
Thank you!
Hi Laura, diet calcium combines with oxalate in your intestines so the oxalate cannot be absorbed into the blood. Diet calcium far exceeds diet oxalate, so oxalate makes to difference to how much diet calcium is absorbed. The fraction of diet calcium absorbed is controlled by your hormone systems and ranges from 20 – 35% of what you eat. IN people with hypercalciuria – common in stone formers – the fraction is high. So all of the calcium in milk is available to block oxalate absorption. Given this, it is obvious that the diet calcium needs to go with diet oxalate – to bind it and prevent absorption. Finding a way to match oxalate to calcium is not so hard. Jill Harris – who wrote the oxalate article with me – is an ideal source and consults via internet. She might be able to find ways for you to eat more happily and also prevent stones. Finally, high calcium intake is only part of the treatment; the other is low diet sodium, which keeps that extra calcium out of the urine and in your bones. The ideal is 1500 mg sodium daily. So you need both high diet calcium and low diet sodium, together, as well as timing. Regards, Fred Coe
Thank you very much for the prompt and detailed reply, Dr. Coe!
I am going to check out all the links you’ve provided and, perhaps, will contact Jill Harris.
Thank you again!!
Hi Laura,
My patients do indeed eat oatmeal and continue to lower their urine oxalate. Have it with milk and you will be fine. Or any non-dairy milk like coconut or flax seed milk.
Thanks for writing- Jill
Thank you for all of the helpful info! I am on my 17th (yes, I said SEVENTEENTH) kidney stone. I had a couple prior to gastric bypass surgery, but since my surgery in 2006 I have been a stone producer. I realize my diet is not the greatest, but now seeing a kidney specialist and he has recommended a low-oxalate diet. It’s hard enough to stay on my GB diet, much less a new diet. My GB doc says I need more calcium, yet my KS doc says more uric – my body doesn’t know what to think. He also suggested 3 liters of water each day (as anyone with bariatric surgery knows, even if you LOVE cold water as much as I do, drinking that much is tough to do as you can’t just chug it!), so it’s tough. I am doing my best to get though everything (also type 2 diabetic, non-medication).
Anyways, thanks for all the good info! 🙂
Hi Hopester,
As you are a perfect example, many times people are juggling many different issues. You need someone well versed to help you sort this all out. If you need help let me know at jharris1019@gmail.com. It is what I do for a living.
Jill
Hi Hopester, I presume the bypass has raised urine oxalate and perhaps made other changes that promote calcium oxalate stones. I general high diet calcium will lower urine oxalate so a low oxalate diet is not so crucial. Given diabetes, you might also form uric acid stones, because diabetes makes for acid urine. Perhaps you make both kinds – you do not say. In any event prevention is not difficult so much as tedious. Very high fluids may be less critical, depending on stone type and 24 hour urine results. Regards, Fred Coe
Okay, this is my challenge, I’m a vegan and trying to recover anorexic. I’m a vegan for humanitarian purposes ONLY. For the first time EVER since I have had “Ana”, have I ever been frustrated at the things I can not eat or restricted to. I am allergic to soy protein, and extremely careful with gluten due to IBS.
HELP.
I had two 9mm stones in my ureter last March. I had been bleeding so much they thought it was my needing a hysterectomy but I DID my own research…nope and then it went back three months later to a crappy mean dr in the ER that stated I had hematherma in my urine, gave me a pamphlet w/o talking further. When I asked if she would break it down for me because this scared me, she seriously asked me , “why, can’t you read”? and left the room. three months later I was in emergency surgery and almost totally had bled out with an additional 12 kidney stones in my kidney stones (plus the ones that were trapped in my ureter) . So for the first time, with what I can and can not have and trying to not get stuck in a all-too-familiar rut where I only eat a few foods and don’t try new things because of the apparent limitations, its hard for this southern woman to cook recipes, or God help me go out with my new awesome boyfriend. HELP!!!!
Dear Leigh,
I am sorry for the “crappy doc” you had and your terrible ER experience. Having anorexia is a very hard thing to deal with and I hope you are getting the support you need for that. So to me, you are dealing with two separate issues. I can certainly help with the kidney stone part of it and you should get the proper testing you need. A 24 hour urine collection to help see what is going on. Until then, follow our kidney stone prevention diet, get the counseling you need and if I can be of personal assistance let me know – jharris1019@gmail.com
My Urologist talked about eating a less acid diet and gave me medication to raise my Ph. So I found that Buckwheat was better than Oatmeal in terms of Ph but now I find that Buckwheat is bad in terms of Ocalates so just when I thought I was moving in a good direction I fell like I am back to Square One and starting all over again. Sigh! My doctor has been so totally unhelpful.
Hi Lee,
It is hard when you have not been given much advice. Read the article here on Dr. Coe’s site on The Kidney Stone Diet. It will be helpful to you. I also run a FB page called The Kidney Stone Diet and Prevention Course. You can learn lots there as well!
Jill
How about just a long list of foods that are low in oxalate so a person can make a diet out if the list and stay out of harms way. It seems simpler to me than listing all the foods that are high in oxalate.
Hi Joe,
I once had a private client that asked me to make him one. I have it if you would like it please write me at jharris1019@gmail.com and I will send it to you.
jill
I would like that list as well. Thanks!
I am confused. Another site stated Avocados were low in Oxalate and safe to eat. You state otherwise.
Hi Karin.
Here is the thing. Harvard lists them as high, but you see they are only 19mg for a whole fruit. You have 100 mg/day to eat. You can easily fit them into your diet. Please go by the portion size of food and the amount of oxalate listed. Not by the adverb that is used to describe it.
Hope that helps,
Jill
Hi Karin, I have the same query but am still confused.
In the XLS it says 19 mg per fruit
avocados range in size a lot – up to twice in size
also the grain weighs a lot!
IS THE 19 mg CONTENT FOR THE FLESH ONLY AND FOR WHICH SIZE OF AVOCADO?
in other sites Avocados lists as LOW OXALATE PER SERVING where low they define as 5-10 mg.
Thanks a lot ♥
Aliza,
The content is for the fruit itself, not the shell. There will be some variance from food to food. We trust the Harvard list that we teach from. You must learn how to use your list and you must really know if you need to have a low oxalate diet. Don’t forget to get the right amount of calcium too.
Jill
Hi Karin, In the XLS it says 19 mg per fruit
avocados range in size a lot – up to twice in size
also the grain weighs a lot!
IS THE 19 mg CONTENT FOR THE FLESH ONLY AND FOR WHICH SIZE OF AVOCADO?
in other sites Avocados lists as LOW OXALATE PER SERVING where low they define as 5-10 mg.
Thanks a lot ♥
I HAVE A CONGENITAL DISEASE AND HAVE BEEN ADVISED TO FOLLOW AN ALKALINE PLUS LOW OXALATE DIET,HOWEVER,MANY LISTS DO NOT AGREE WITH EACH OTHER there IS NO DUPLICATION IN THIS COMMENT!
Hi Carol, Not knowing what disease you are speaking of I have little to say. Lists do not agree because many are wrong. Our own has a good lineage, from Harvard and then curated by Dr Ross Holmes, a recognized authority on oxalate. Regards, Fred Coe
I would like to know if the content and absorption of calcium in the piece of food matters, because oranges are high in oxalates but high in calcium so may be is not that bad
Hi Toni, Yes it does. Often, oxalate is stored in plants as calcium oxalate crystals – for packing efficiency, and neither is well absorbed. In fact, because we eat an orange, not 5 or 10 the amount of oxalate is low. Orange juice in quantity can be a problem, but many are calcium supplemented so oxalate cannot be absorbed at all. Regards, Fred Coe
I had been on this diet on yours for almost two years. Was making calcium oxilate stones 6 to 9 mm every 6 months for 7 years. Thank you for this infor. My question….I drink 1 cup of full fat raw milk with my three meals. That is the only calcium i take. Could i drink my milk 3 cups for one of my meals…..then my water with my other 2 meals and get the same results? Now that i am not “eating Healthy foods” the milk has made me gain at least 15 lbs and a stomach in two years. Very active and walk at least 4 to 5 miles a day.
Thank you for all your work!!
To everyone else. ….USE THIS SITE FOR OXILATE AMOUNTS. They havr it figured out!!
Hi Jeannie, You can use low fat milk with less calories in it and get the same calcium. Regards, Fred Coe
I have been adding lemon juice (fresh squeezed, no sugar) to my water. Is this helpful to prevent stone formation?
Hi Shirley, In general, no. Like most casual nostrums it is likely to do nothing. Here is a very good article all about the subject, and perhaps will help you point to better approaches. Warm regards, Fred Coe
On this list (https://docs.google.com/spreadsheets/d/1nbDZPxhAW4It-m2-c460w6eGr4dMSIeDiQdqg3MaRgQ/edit#gid=1354389148 ), you have soy milk listed twice:
Soy Milk 1 Cup Very High * 20mg (under Beverage)
Soy Milk 1 cup Low 4mg (under Dairy Beverage)
Which one is good? My husband is lactose intolerant and likes to eat cereal in the morning. Also please list best granola bars, which might be a solution or a good recipe.
Hi Deb,
We are aware of the discrepancy and are looking into it. Please know that soy is HIGH and should not be used in The Kidney Stone Prevention Diet. You can use flax milk that has been fortified with calcium or coconut milk if he has ok cholesterol. Hope this helps-
Jill
Thanks, Jill. I was thinking rice milk might be an alternative, also.
Hi Deb, Thank you. I will ask Jill Harris to check and remove the incorrect one. But possibly the amount indeed varies from product to product as this is not a natural but synthetic material. About low oxalate diet, be sure of your needs and do not spend extra energy on oxalate unless you have reason. Take a look here. And here. Regards, Fred Coe
Thanks. Read links, great advice. He is in the process of 24 hr. evaluation.
I have had kidney stones in the past and I am looking for a “valid”, proven list of good and bad foods when it comes to kidney stones. There are a lot of different lists out there that are conflicting. One says pumpkin seeds help prevent kidney stones and another says they are high in oxalates. One list says drink all the cola you want but other reports state cola can cause the stones. I would like to find a good, accurate list that I can follow of what I should or should not eat. Please help. Thank you.
Hi Jason,
So many of our patients come to us saying the same thing. You can trust the list we use. It is from Harvard and one of the highest authorities in oxalate study, Dr. Ross Holmes. Our patients do indeed lower their urinary oxalate levels using it, but also remember that you need to follow all the other guidelines we post in The Kidney Stone Diet. Lower sodium, get fluids up, and perhaps most importantly, eat enough calcium.
Hope this helps,
Jill
I am 76 yrs old and had my first kidney stone in 2015; in 2016 I had another 6 mm stone that was a few cm from the UVJ and causing moderate hydronephrosis. Laser lithotripsy was done on both. (In 2014 my husband had a cardiac arrest following neck surgery resulting in a long hospitalization and rehabilitation; in 2016 he was again seriously ill with septicemia necessitating care in ICU, etc, over a period of time.) So my first question is ‘can stress trigger changes that affect the formation of kidney stones?’ Or, do stones just appear late in life and the timing is just a coincidence?
I then went to a kidney stone clinic where not only do I have another stone in the lower lobe of the right kidney, but the results of a 24 hr urine showed a Ox24 of 52 and Na24 of 169; ss CaOx was 3.73 and SS CaP was 0.18 altho the dr wasn’t concerned about these flagged values. Four months ago I began a low oxalate, low sodium diet. I lost 5 lbs and quit having bloating. I am scheduled to return in 2 months after having another imaging test to see the status of the stone. The dr. said he wasn’t going to order another 24 hr urine; wanted to see about the stone.
My second question has to do with this plan. I think a 24 hr urine would tell if what I”m doing is working (low oxalate, low sodium, 2.5-3 liters of water daily, and increased dietary calcium.) so I’m planning to call and request another 24 hr urine. Does this seem logical? This eating plan has not been easy and if it’s not working, I’d prefer not to continue, at least to the degree of effort that’s gone into it.
The last question has to do with oxalobacter formigenes, specifically Oxazyme. Not sure if it’s available or being tested. Please comment.
Thank you.
Hi Marian, You need followup testing, of course. High diet calcium and reduced diet oxalate will lower urine oxalate; low diet sodium will keep urine calcium from rising and may also benefit bones. But you cannot tell if you have done anything without repeated testing. Get it, and if you have not achieved your goals try harder. It will work. Always lower the sodium first, then raise the calcium, check; if needed, then bother with diet oxalate. The bacteria do not work right now. Regards, Fred Coe
Hi and thanks for this helpful article.
I have one kidney and fibromyalgia so I keep a low oxalate diet & studied the XLS list of foods high oxalates carefully (1st link in the article).
It’s very good but I see something there that MAY be a mistake…
Avocado appears as low oxalate food in all the lists I see in the internet including the one I got from a medical inst.
HELP PLEASE !!! I HAVE BEEN EATING 2 AVOCADO EVERY WEEK FOR A WHILE AND AM WORRIED.
All the best, keep up the good work ♥
Hi Dorit, I will ask Jill Harris to answer this one. Regards, Fred Coe
Hi Dorit,
You can easily eat your avocados. Not a problem. Go by the amount of oxalate in foods and portion size. Most of you are to lower your oxalate to 100 mg/day. You can see how eating avocados can be eaten. No problem!
Make sure you need to actually do a low oxalate diet too.
Best,
Jill
I have idiopathic hyperoxaluria and went from Stage IV kidney disease to Stage III by only eating low oxalate food (from the Harvard site) along with taking B3 and Potassium Citrate. I have a few stones, but I’ve never passed one or had to have intervention. My crystals were primarily small and blocked the tubules in my kidneys and deposited in my joints. I only eat salt free or extremely low salt products and limit meat to fish and fowl. I have a milk product with every meal. I limit spices to basil, garlic, chives, and onions.
1. I would like to know if there are other herbs and spices that I can safely add back into my diet.
2. My nephrologists said to avoid any product with caffeine, but from your site, I am wondering if it is OK to have decaffeinated coffee?
3. My primary snacks have been unsalted corn ships, popcorn, or rice rollers. Why does popcorn made with oil have a moderate oxalate status while air popped is low? And why is corn low but corn chips moderate? I thought olive oil was low in oxalate? Does frying release additional oxalates?
4. Since the onset of the hyperoxaluria I’ve had severe constipation and I take iron daily because of anemia caused by the kidney disease. I currently eat l/3 cup of Bob’s Red Mill oat bran cereal with 1 cup of skim milk for breakfast. I’d like to double this amount, but do not even know what the oxalate count is for the one serving I now have. Do you have that information or other suggestions for foods that would address this problem? None of the fiber supplements, stool softeners, or medications doctors have suggested have worked.
Your help could greatly improve my quality of life. Thank you.
Hi Christy, By primary do you mean primary hyperoxaluria?? Do you actually mean that calcium oxalate crystals are depositing in your joints? IF so, this is a very serious condition with advanced treatment needs and you should be cared for at a center specializing in this disease. In the US, Mayo clinic is best, and Dr John Lieske the director of their rare disease consortium. Diet is of little avail per se. Let me know. Regards, Fred Coe
Thank you for responding. I was seen by Dr. Lieske’s predecessor at Mayo in 2014. She said I had hyperoxaluria, but I didn’t have any of the 3 genetic forms of the disease. She thought I might have a form that was unknown. I don’t have any of the health issues that might otherwise lead to secondary hyperoxaluria. However, I asked in your forum on hypercalciuria if a 24-hour urine lab finding from two years ago of “marked hypercalciuria” was just part of having hyperoxaluria. I haven’t had a 24-hour urine in two years, and I’m curious if this should be watched more closely. My kidney function has improved from Stage IV to Stage III over the last 3.5 years. It is difficult financially to travel to Minnesota. If you think I should be going there regularly, please let me know. If so, how often?
Hi Christy, No; urine calcium has nothing to do with primary hyperoxaluria. If you have been at Mayo and have none of the three forms of high urine oxalate, and have high urine calcium and kidney disease, then you have something important that I cannot figure out here with only a few sketchy materials at hand. I can offer to see you, if you can come to Chicago. Otherwise, I want to avoid getting in the way of treatment as an incompletely informed outsider. But whatever is really wrong sounds very unusual to me, and I wonder if you should not be back at Mayo or somewhere else like that. Regards, Fred Coe
Thank you. I will rethink my approach.
I’ve been eating Brussel sprouts because I was told that I could eat any cruciferous vegetable. Now I see that frozen Brussel sprouts are high in oxalate. I always eat fresh Brussels, does this make a difference? Is there a reason why everything else in the cruciferous family is OK, but Brussels are not? It is sad to give up yet another food.
Hi All-
I am going to address this for everyone. One needs to learn how to use this list. Although it may say “very high” please look at the serving size and the amount. If you all have 100 mg of oxalate to use each day, then you can easily use these foods. You pick and choose how to withdraw from your oxalate bank. If you want avocaodo, then have them. Some may be higher or lower on other lists bc not every food will measure exactly alike. Also, the size of the food matters as well. But you can eat all the things you are talking about easily. Also, whether frozen or not, the oxalate will be around the same number.
Hope this clears it all up!
Jill
Your advice is good. However, my disease is severe, and I can only have 50 mg of oxalate each day, so I’ve found it simplest just to avoid high oxalate foods. I’d rather have a a normal portion of cabbage than a tiny portion of a Brussel Sprouts.
I am limited to 50 mg of oxalate by my doctor.
Hi Christy, I understand, and continue to be worried on your behalf. Regards, Fred Coe
Hi,
Are Garbanzo beans (chickpeas) high in oxalate? Can you provide me a number for mg of oxalates per 100g of chickpeas?
Thanks
Tom
Hi, Looks like this one might have slipped through the cracks. Normally a question doesn’t get posted without there being an answer, but this one did get posted. Can you please provide a response?
Thanks
Tom
Hi Tom, We did indeed miss it. I will text Jill Harris and ask her to answer you – it is her area. Sorry! Fred
Hi Tom,
Sorry, did miss this. We don’t have good numbers for garbanzo beans, and when this is the case we say to eat in normal portion size and a couple times a week.
Thanks,
Jill
I’ve read this with great interest, as I’m also on a low oxalates diet and have had kidney stones for going on 30 years- for the most part I’ve had few problems with them. My nephrologist advised to also take 3-4 Tums with every meal – each being 1000mg calcium carbonate. Is there information on this approach having positive results? I’ve not yet had tests since starting this regime.
Thank you
Hi Iris, there is indeed. Calcium in food, or if needed by pills much reduces urine oxalate. But the dose seems well out of line – you say 3 to 4 1000 mg CaCo3. The MW of calcium carbonate is just about 100 mg/mmol, and a mmol is 40 mg of calcium. So 1000 mg of the calcium carbonate gives 400 mg of calcium. Three to 4 of these is 1200 to 1600 per meal meaning 3600 to 4800 mg of calcium for three meals a day. Surely this is a vast excess of calcium, and I doubt your physician so intended. A more likely idea was 1 such pill with each meal giving 1200 mg of calcium daily, itself quite a bit. More; with such an increase in calcium intake you should recheck your urine calcium, which may have much increased, and if so take steps such as low sodium diet as an offset. Discuss this with our physician who is responsible for your care. Regards, Fred Coe
Hi. I am 56 years old and postmenopausal. I have been taking Topamax for migraines since October 2017. I already had osteopenia and I began having severe bone pain shortly after beginning it and had a bone density test and had osteoporosis. I take Vitamin D3 and calcium daily. The last few weeks I have had pain in my right kidney off and on but no fever. Several times I have passed what looked like small stones. Is there any reason I would need to go to the doctor and have tests done or can I just continue to drink more water (enormous amounts seem to help) and try to figure out this diet puzzle? My kidney has been connected laparoscopically (it was loose and hydronephrotic after a car accident 25 years ago) so I feel kidney pain in my front right abdominal side, not in my back and whenever I tell a doctor my kidney hurts and point there, they tell me that’s not my kidney and I just prefer not to have to try to go through the whole agony of trying to convince them and go through other tests before they settle on believing that it’s my kidney. So is it really necessary to see a doctor for kidney stones?
Hi, Oxalate is very likely irrelevant for you. Your drug is notorious for calcium phosphate stone formation. If you see what appear to be stones, get them analysed to be sure. If they are indeed calcium phosphate crystals you need to take steps with your physicians. As for your main question, indeed yes. Stone are merely a sign of something wrong that is causing them, and they can cause trouble ranging from pain and inconvenience to serious disease. A CT and analysis of passed material would help. Here is an introductory article about the quandary you are in. Please move forward and get things resolved. Regards, Fred Coe
As a calcium oxalate kidney stone person who has had a lithotripsy and 2 kidney stone removal surgeries, my urologist recently suggested taking “potassium citrate” which is readily available through Amazon other sites, cutting back on animal protein and have more fruit and veggies. The natural supplement “Chanca Piedra” which I started on my own for several months did nothing to dissolve the stones. I love nuts, bulgur and healthy breakfast cereals among other items on ‘the list’, so that’s going to hurt, but perhaps occasionally in moderation might be ok. Am putting off another ‘lithotripsy’ until the next kidney x-ray in Aug. ’18. . A big part of the problem is a narrow section of the right ureter which hinders stones from passing. The urologist said it can corrected by ‘robotic surgery’, an option I’ve so far declined.
Hi Ed,
I can address the diet issues, and yes, some of the foods you enjoy are high oxalate so eating them in moderation would be best. More importantly is to be eating foods with calcium when you are eating foods high in oxalate. Getting the diet right, low sodium, normal calcium, low oxalate, and high fluids will be your prescription most likely. It takes work, but is very doable and not getting new stones I am sure is on your high priority list. Dr. Coe can speak about the robotic surgery-
Be well,
Jill
Hi Ed, Ureteral narrowing is a complex problem. My best advice is simply to obtain multiple surgical opinions before making a final commitment. Each case is a bit different, each surgeon, and the first surgery usually the best chance for a good outcome. Fred Coe
Hi,
What about high dose IV vitamin c?
My joints are hurting badly.
Hi Michelle, high dose vitamin C is not a good idea as it can raise urine oxalate. It has no known benefits. Regards, Fred Coe
I am so overwhelmed. So I was told to eat a low protein diet as well. I don’t know what to substitute for protein. Dr told me animal protein at most only twice a week.
Hi Julie, Your physician does not know as yet but new work has more or less ended the business of low protein diets for stones. Wait a bit and the new article will be up on the site. Be sure you need a low oxalate diet. Regards, Fred Coe
Hi Jill,
I have a question regarding the food list. 🙂
I was looking at the crackers/chips/misc. category and noticed that most items are measured in ounces or cups, yet the saltines, Triscuits, and Wheat Thins are measured as “1 cracker.”
The 1 cracker was listed in the “little to none” category for oxalate as 1mg. However, in the same category, the tortilla chips, and other snacks, are measured as “1 oz” and in the “moderate” category with 7mg.
If the Triscuits, or Wheat Thins, were listed in ounces, that would equate to approximately 16 Wheat Thins or 8 Triscuits. With one cracker equating one mg of oxalate, that would put Wheat Thins at 16 in the “very high” range, and Triscuits in the “moderate” range with 8.
I understand that all of these listings can have conversions based on serving size. This one just stuck out to me because of the discrepancy in measurement consistency within the category which, at first, was misinterpreted. I bought the crackers thinking it could be a safe choice, yet when I realized that it was measured per cracker, as opposed to per ounce, they didn’t seem like it was worth the “cost” of the item any longer.
Which then led me to wonder if the “per cracker” listing was an error and perhaps maybe they were meant to be listed as a one ounce serving?
I know this seems like a tedious question, however the list on your site is the same as the list I received when I went to Mayo last week. Given my newly diagnosed hyperoxaluria, I am living by this list and trying hard to learn, plan, execute, and track everything I put in my mouth.
Thank you for your input. 🙂
Michele
Hi Michele,
We can only assume they meant what they wrote. There are a couple things for you to think about. Most people depending on their urine oxalate level can eat about 100mg/oxalate/day. As long as you are able to eat your calcium as well, you will be fine typically. You can still eat 20 crackers and only get 20 mg of oxalate. Not too bad really. Make sure you have done a urine collection to see how high your oxalate level is and let me know if you have any questions.
Be well,
Jill
Hi Michele,
We can only assume they meant what they wrote. There are a couple things for you to think about. Most people depending on their urine oxalate level can eat about 100mg/oxalate/day. As long as you are able to eat your calcium as well, you will be fine typically. You can still eat 20 crackers and only get 20 mg of oxalate. Not too bad really. Make sure you have done a urine collection to see how high your oxalate level is and let me know if you have any questions.
Be well,
Jill
What about chia seeds? I have been eating everything they tell us that are “Super foods” like avocados, coconut. I read things are high on one site then low one another.
I just cleaned out my pantry and sobbed uncontrollably. I have no income and have to give it all away now. All the things I love. All that’s left is olive oil and sugar. I have been doing things right by eating things in moderation. And the right proportions for several years. And now I can’t eat any of it.
I was tested for diabetes and I have high cholesterol even though I ate well and ate hardly any bad fats. I thought … well I’ll just eat bark, but read even that has high oxalates. I don’t like yogurt. I rarely drink milk. Always bothered my stomach. I give up!
Hi Kathy,
I don’t have to read between the lines too hard to hear how frustrated you are and I totally understand. I hope you did a urine collection to confirm that you need a low oxalate diet. What seems more important for you (bc you said that you ate your food in moderation) is that you don’t get enough calcium. Please try some flax milk or coconut milk that has been fortified with calcium. There are other nondairy sources, like salmon too, that might help.
You can eat many, many fruits and veggies without any increase oxalate if you get the recommended amount of calcium into your diet. Chia seeds are fine when eating in normal portion sizes.
Keep reading the articles here and hang in there. It is doable once you have the right info, testing, and of course, tenacity!
Be well,
Jill
What about a low oxalate, low cholesterol diet?
Go vegan and watch oxalate content of the fruits and veggies? No dairy
Hi Peg,
You still need to get your calcium. You can eat many fruits and veggies on a low oxalate diet, esp if you are getting your daily requirement of calcium. Do you want to go vegan? Let me know this first before I continue on.
Jill
I have just begun the kidney stone ordeal. Passed my first one in Sept 17. Had Lithotripsy on both kidneys in October because of stones too large to pass. Now, I’ve learned that my urine oxalate level is 116mg. My urologist started to put me on the potassium supplement,but tested my blood and found that my potassium level there is already high. He is sending me to a nephrologist – whom I have not yet met. I have the usual concerns about the state of my kidneys, but complicating this is the fact that I have had gastric bypass surgery (2007) and need to maintain a high protein diet and I am concerned about that need as well. I appreciate your list of High Oxalate foods. Do you know any protein supplements that are low oxalate? I currently use Unjury products which are extremely good tasting and nourishing. I feel like I’m between a rock and a hard place. I’m 74 years old, and relearning how to eat for optimum health is confusing.
Dear Diana, The high urine oxalate and the bypass mean you have developed stones – almost certainly – from the bypass itself that has seriously increased your urine oxalate. The nephrologist will know how to prevent kidney damage and stones. Do not use supplements or anything else until you see him/her. High urine oxalate like yours can lead to acute kidney injury so your appointment is rather more urgent than most. Be sure and get in as soon as possible. Regards, Fred Coe
Do you mean no calcium or protein supplements? I want to fully understand you and closely follow instructions based on your knowledge and experience. I have not yet heard from the nephrologist’s office (only referred last Friday), but I will see him/her ASAP. Thank you for your advice.
Hi Diana, Protein supplements are not necessarily a good thing. Calcium supplements with main meals can lower urine oxalate as well as food calcium can, though the latter is always preferable. Here is a good general reference. Regards, Fred Coe
Dr. Coe,
You have provided me with a wealth of information that will aid my preparation for my coming first appointment with a local nephrologist. I intend to reread your article and make notes prior to seeing him/her. Sincere thanks for your help.
Seems odd, corn meal is high in oxalate, white flour is high, both are used in cornbread, but cornbread isn’t considered high.
Hi Chris, It is all about portions; the final amount of oxalate in corn bread as eaten is not high whereas the individual materials are high for the amounts used in preparing – as an example – a batch of such. It is a plague of these lists, and we have never been able to get rid of the inconsistencies. Regards, Fred Coe
Hello,
My father had a calcium oxalate stone removed in the 1980’s and my brother has had kidney stones. What’s your view on whether people can inherit the tendency to develop calcium oxalate kidney stones?
Hi Chris, stones are very hereditary. Given your father and brother you have a higher risk. But many with such risk remain well. So, hope for the good side. Regards, Fred Coe
I’m a vegan, and doing the low-oxalate diet is life-ruining, especially given that every source of information is contradictory, so the tendency (mine at least) is to avoid all the foods that ANY research institution feels are moderate to high in oxalate. If you’re trying to eat anti-inflammatory as well, you’re limiting fruits of all kinds. The anti-inflammatory, low-oxalate vegan is basically left with peas and cucumbers, which perhaps explains why I am now anemic and my hair is falling out. I recently saw a nutritionist hoping for clarification, and he only confused me more. I feel like you basically have to (1) pick one source of information and stick with it, and (2) try not to think about the fact that you may be suffering for no reason if the source you’ve chosen isn’t accurate. And I know it’s all about portion control, but when the pool of foods you can eat is so limited, you’re going to eat more of what’s left — and eat it more often. I feel like there is no winning the food game.
Dear Holly,
I understand and hear your frustration. You do have to stick with one source, here we use the Harvard list and have had great success with lowering patients urine oxalate. You need to work with someone who can help you with both. I certainly can. I usually don’t direct people to me, but if you need help I am happy to work with you to figure your diet out. My email is jharris1019@gmail.com. You will see by looking at the list that there are many foods you can eat if you do watch the portion size. And getting your calcium intake in- which I know might be hard as you are vegan, but I work with many vegans who are doing it!
Be well,
Jill
I had several kidney stones over the passed 20 years, but I was prescribed K-lyte 25meq 2x daily (potassium citrate) and I longer had stones. I stopped taking it to see what would happen and I’ve passed some tiny stones but I feel I can control it somewhat through diet & exercise. The problem now is I have Gallstones and discovered on a site called ‘ehealthme’ (Potassium citrate and Gallstones – from FDA reports) that potassium citrate can cause gallstones. The best thing for Gallstones are bitter high oxalate foods. I was hoping I could start taking K-lyte again but … Any truth to this, or have I misunderstood?
Thanks,
Domenic
Hi Domenic, a search of PubMed under ‘gallstones AND potassium citrate’ turned up not one publication, so I do not believe they are causally linked. If you have an FDA report could you post it? Regards, Fred Coe
Tea is listed as high in oxilate, does this include herbal teas (i.e. peppermint, rooibos, camomile)?
Hi Cheryl, I will ask Jill Harris to answer this one. Fred Coe
Hi Cheryl,
Not all have been tested. When drinking teas, have a cup, don’t steep it long, and if you can, drink it with milk!
Be well,
Jill
What is your recommendation regarding salt substitutes?
Also, any recommendations on bread? Most are made from wheat or potato, which are on “the list” of do not eat.
Thanks, Peggy
Hi Peggy, salt substitutes are mainly potassium chloride. I have no problem with them. Some are half sodium however, so read the labels. Wheat and potato are not problems, though listed as high, because of amounts. Bread has so little oxalate per slice it does not matter. A potato likewise, even though many eaten at once are a problem. Do not limit either below a standard portion per meal. Regards, Fred Coe
Hello,
Thanks a lot for the very helpful information on your website. Going through the list of foods classified according to their oxalate content, I noticed that orange has a very high oxalate content, while orange juice is considered to have a ‘low’ oxalate concentration. How can this apparent inconsistency be explained? On other places on your website, orange juice is indeed recommended as help to reduce the risk on kidney stones, while oranges are mentioned as fruits to be eaten with ‘caution’. Our nephrologist generally recommended to eat a lot of citrus fruits, because of the high citrate level. Is this correct? Is the high oxalate content in orange compensated by the high citrate level? Will complexation of dietary Ca with citrate lead to lower formation rate of Ca oxalate in intestines and thus higher absorption of oxalate? To what extent will the additional citrate absorbed in urine (leading to higher pH) level out the higher urine oxalate level with associated risk on kidney stone formation?
A 24-hr urine sample analysis of my son revealed low citrate levels and myself, I have also been suffering from kidney stones during the last months (although type of stone not yet confirmed).
Thanks in advance for any clarification you can give on this.
Kind regards,
Wim
Hi Wim, Oranges have a lot of oxalate but one orange has little – it is all portion. You can eat 100 – 200 mg of oxalate a day safely if you eat calcium. Take a look at how this works. Fruits and veggies provide potassium coupled with many anions like citrate. They are effective in reducing stones. But for you and your son the proper response is not one food but the whole diet – here is the kidney stone diet. Stone prevention is a complete system, of which diet is a part; take a look. Regards, Fred Coe
Thanks for your response.
I am aware I should consider my diet as a whole and not focus on one single food and I keep on reading on your website . However, the recommendations about orange and orange juice seemed somewhat contradictory to me. I understand that it is important to reduce salt, (animal) protein and sugar in the diet. Anyway, I have stopped eating meat (except fish) more than 10 years ago and eat quite a lot of vegetables (and nuts). Nevertheless, analysis of my 24-hr urine sample now revealed severe hypocitraturia (only 29 mg/24h), which is bothering me. Stone analysis outcome is not yet known, but my urologist recommended me to take Dacitrin (which is a commercial preparate of potassium citrate, if I understand well). However, a check of blood K-levels (check for hyperkalemia) was not ordered. Isn’t this always necessary after starting intake of potassium citrate (in the form of medecins)? I am also wondering why animal protein is to be avoided (or limited) and vegetable protein not. What is the logic behind this?
Thanks in advance for your advice.
Kind regards,
Wim
Hi Wim, orange juice is high in citrate but high in sugar and I have not much recommended it. Meat is not a stone causing food – see the new article I put up on this very topic. The very low urine citrate makes my concerned that something is very wrong – do you have bowel disease, diarrhea, do you vomit, take laxatives, or drugs that are known to cause stones. The cause of the low citrate needs to be discovered, and from here I would be unable to help much – so many causes! As for animal protein, it is of no concern as I just said above. I cannot find your prior comment, so if I have repeated myself or contradicted myself let me know and I will try to find it. Regards, Fred Coe
hi Jill
Thank you for this very informative website. I’m wondering about avocados…I think your site lists them as very high whereas I’ve seen them on lowoxalate.info (which is also cited as a very reliable website I think) as ‘very low’.
Also, I’ve seen constrasting results for Quinoa (either no result or high)…perhaps you would be able to advise/clarify on these two as they are a mainstay of my lunch most days…and I want to try a low oxalate diet because of achey joints and chronic tendonitis in my hip flexor.
Thanks
Best regards, Mary
hi again Jill…
No need to respond, I saw the answer further down…portion size being the one to watch…thanks a mill, Mary
what about peanut butter?
Hi Joyce.
It is high. But if you spread it thinly across your bread (not glob it on) and drink a cup of milk with it, you could get away with it. Although peanut butter is indeed high, it is the portion people tend to use that makes it a problem. That and not pairing it with a calcium product to absorb the extra oxalate it produces.
Be well,
Jill
I’m a 74 yo female who just had a nephrolithotomy to remove an oxalate calcium stone. My urologist wants me to follow a low oxalate diet. A year ago I changed my diet to a Whole Food Plant Based Diet with no oil. The thought of adding back all the problem foods is causing me distress. With the WFBP diet I am off my blood pressure meds and pain free. I am able to walk for exercise again. I have lost 30 lbs. Do you have any recommendations that will help me increase calcium and remain plant based?
Hi Anne, You know the stone, but do you know if urine oxalate is high? Here are the right steps to choose a diet and other treatments. This one is specially about low oxalate diet. See if this helps. Regards, Fred Coe
When I read and hear to boil kale I ask myself, are we suppose to throw out the water that it was boiled in?, Or do the oxalates evaporate?, Or does it change the chemical composition without the need to evaporate and without throwing out the water it was boiled in?,
I remember they made baked kale on the Dr. Oz show, but I don’t remember what was said on that show. Do we use oil to bake kale if we bake kale?
Is the oxalate lower when boiling or baking kale? And if one method is better than the other, what is the temperature for how long for the best in home method used?
Hi Kenny, kale has almost no oxalate at all, so it poses no dangers. So just use it any way you want. Regards, Fred Coe
Hello; I’m 63 years old and just found out that I have Osteoporosis and also kidney stones, one in each kidney. It has been very difficult for me to decide what to eat and what not. The kidney stones are not giving me any symptoms so far, so my priority is to take care of my bones. I’ve been doing a lot of research to be able to improve my diet and where ever I search the alkaline diet is most recommended to improve your bone density including Almond milk which I’ve been drinking with my coffee to reduce acidity. I only drink one cup of coffee in the morning. My question is, in your opinion should I switch back to drink regular milk ( 1%) and I can still enjoy my Gouda and Brie cheese, aren’t dairy products too acidic for my bones.
Thank you so much, best regards.
Hi Carmen, Dairy products are an ideal calcium source. Dairy protein, even animal protein has no bad effect on bone – calcium absorption rises with protein intake so bone balance is not reduced. Excess protein can raise urine calcium and promote stones however. Given stones and bone disease I suspect you have idiopathic hypercalciuria and your best bet is combined high calcium / low sodium diet. Extra alkali has not been proven to improve bone mineral. For your stones you should have proper evaluation and prevention, and in all cases what we do for stone prevention also benefits bones. Take a look and see what you think. Regards, Fred Coe
Thanks a lot for the advice.
I recently had calcium oxalate kidney stones. I did 24 hour urine collection and the results said high uric acid, high oxalates, and high sodium. Quite honestly, I don’t know what I can eat now. Things that are ok for oxalates are not ok for uric acid.
Any suggestions
Hi Rick, It is confusion, so I wrote this article to tie together all of the materials on the site you need. You already know your stone, so just skip down the page and you will find your place. The oxalate matters, I think, the uric acid may not. Let me know, Regards, Fred Coe
I recently had calcium oxalate kidney stones. I did 24 hour urine collection and the results said high uric acid, high oxalates, and high sodium. Quite honestly, I don’t know what I can eat now. Things that are ok for oxalates, are not ok for uric acid.
Any suggestions I am also a diabetic type 2.
I’m forming what my doc calls oxalate stones (his experience says that’s what they are though I don’t think there was a an actual test on any of them). I’m going on my 6th lithotripsy tomorrow and am working on changing my diet. I’ve read much regarding diet and am finding it’s a crazy balance sometimes
I’m often finding that lists of low oxalate and high oxalate foods are sometimes contradictory. While most are very similar, there are some glaring differences. A handout from my doctors office says kale is a high oxalate food while Dr. Fred Coe, replying to a question on here says it is not. There doesn’t seem to be a definitive list. I realize it’s a balance thing and I can roll with that but I will still look for that elusive list. Perhaps I will have to create my own…maybe I’ll share.
Thanks
Hi Matthew, just because the stone name includes ‘oxalate’ diet oxalate may be your least concern. If your stones have been analysed and they are indeed calcium, here is my best article on treatment – including the proper diet. That latter has a lot in it, oxalate perhaps the least important part. Regards, Fred Coe