MINIMALLY INVASIVE STONE SURGERY (Ureteroscopy)
(Images of surgical equipment featured in this article are for patient education only. They are not intended for promotional use or a reflection of personal preference. We accept no fees or other benefits from vendors or their agents.)
Evolution of Technique
The fascinating history of urology with its captivating depictions, texts and stories rivals any other field in medicine. In particular, the ancient past of lithotomy (treatment and removal of urinary stones) dates back to Mesopotamia (3200 BC), and descriptions and treatments for urinary stone disease have been identified from ancient cultures including Hindu, Greek, and Egyptian. The treatment of stones, which at the time most commonly occurred in the bladder, was very dangerous, often lethal. As such, it led to the development of one of the first medical subspecialists, the lithotomist, who opened the urinary tract and removed stones directly. Recognition of this unique set of skills earned a distinction in the Hippocratic oath, still recited by graduating students: “I will not cut for the stone, but will leave this to be done by practitioners of this work…”
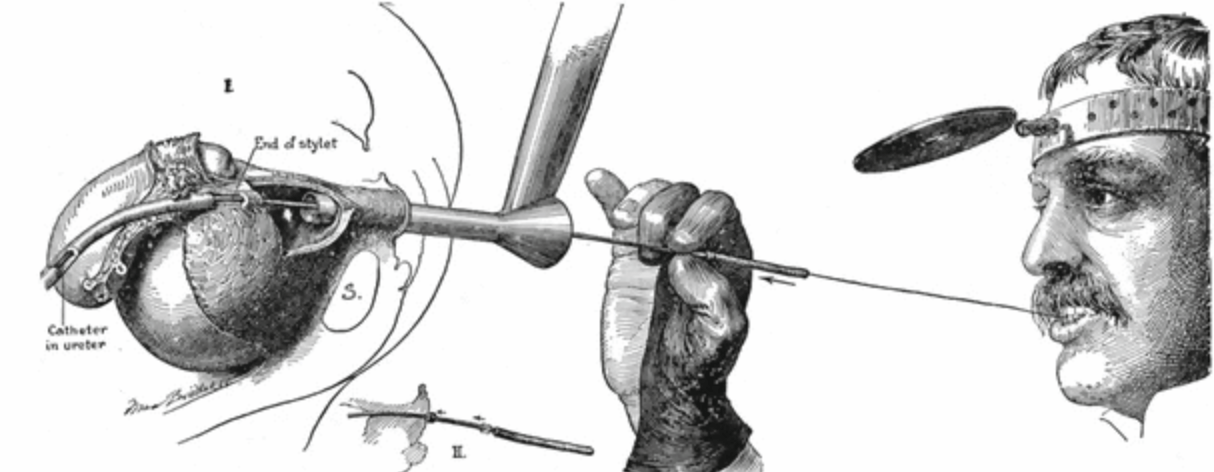
Today, “cutting for stone,” otherwise known as open stone surgery, has been replaced by alternative minimally invasive techniques. Critical to this change has been the introduction of the endoscope. Whereas early pioneers such as Howard Kelly (depicted above in the early 1900’s using a wax tipped catheter in the ureter to detect a ureteral stone) relied heavily on intuition, feel, and clinical suspicion, advances in endoscopy have made it possible to inspect all parts of the urinary tract directly.
The particular endoscope that has revolutionized our ability to treat kidney stones in a minimally invasive fashion is the ureteroscope. Incorporation of its use into urologic practice has led to the development of a unique subspecialty, endourology, that focuses on minimally invasive and endoscopic surgical treatments.
Modern Ureteroscopy
A ureteroscope, as its name implies, is an endoscope designed to visualize and work within the ureter. Other scopes commonly used by urologists and endourologists include the cystoscope (used in the bladder) and the nephroscope (used in the kidney).
Although such scopes now enable modern surgical stone treatment, they have only been routinely utilized for the past several decades. Minimally invasive kidney stone treatment began in the mid-1980’s with shock wave lithotripsy and percutaneous nephrolithotomy. Ureteroscopy for treatment of ureteral stones was not performed routinely until then as well, and it was not until the late 1990’s and early 2000’s that ureteroscopes could routinely access and treat stones in the kidney. In the United States we often take such technologies and treatment options for granted, but open stone surgery is still practiced in many parts of the world where modern technology remains limited.
There are two types of ureteroscopes, rigid and flexible. Rigid ureteroscopes, as their name implies, are firm and preferred for treatment of stones lodged in the lower ureter which can usually be accessed in a straight path. When stones are located in the upper ureter and/or kidney, they often require 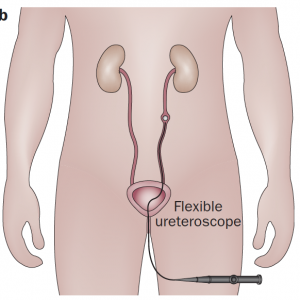
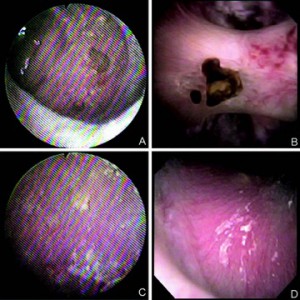
flexible ureteroscopes that accommodate to the shape of the ureter and renal collecting system (figure on right). Though more difficult to maneuver, flexible scopes allow the urologist to inspect nearly the entirety of the inner kidney to find stones, treat them, and remove them using a variety of techniques. Innovation this area is brisk and modern digital ureteroscopes offer increasingly superior image quality, lighting and wide fields of view.
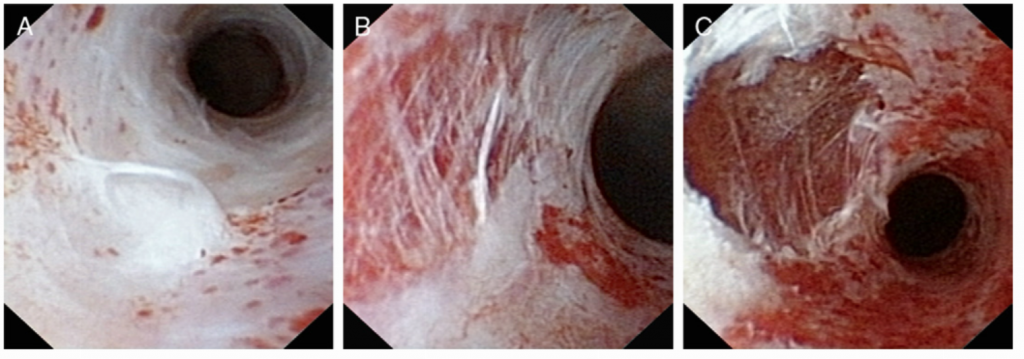
(Figure – Left ) Ureteroscopic image of the renal collecting system using older generation fiberoptic ureteroscope (left) and newer generation digital ureteroscope (right). Note the superior image quality, increased light intensity and wider field of view. Panels A and B feature small stones attached to a renal papilla. Panels C and D feature the endoscopic appearance of Randall’s plaque.
Irrigation and Access Sheaths
In order visualize anything at all, fluid must run continuously through the scope and into the kidney to wash away blood, debris, and crystals that impair visualization. To accomplish this, the fluid (most commonly saline) is hung from a bag and run through tubing directly into the body of the scope where it comes out the tip and into the kidney.
This inflow is harmless, but excess filling of the kidney because of high pressure inflow or an inability of the fluid to freely exit around the scope can overstretch the kidney and cause fluid absorption, leakage, bleeding, and small tears within the kidney itself, a term we call extravasation.
To prevent this, many urologists use a device called a ureteral access sheath. This can be thought of as a temporary tunnel from the bladder to the kidney which allows any fluid that is irrigated into the kidney to quickly wash out around the scope, optimizing visualization and decreasing the likelihood of extravasation. The scope can be passed back and forth without rubbing against and potentially damaging the lining of the ureter, which is generally around the same small diameter as the scope itself. When used appropriately, temporary sheaths are safe and decrease postoperative infections and sepsis. While the majority of urologists routinely use them during ureteroscopy, debate does exist within the community as to whether or not they are required in every case.
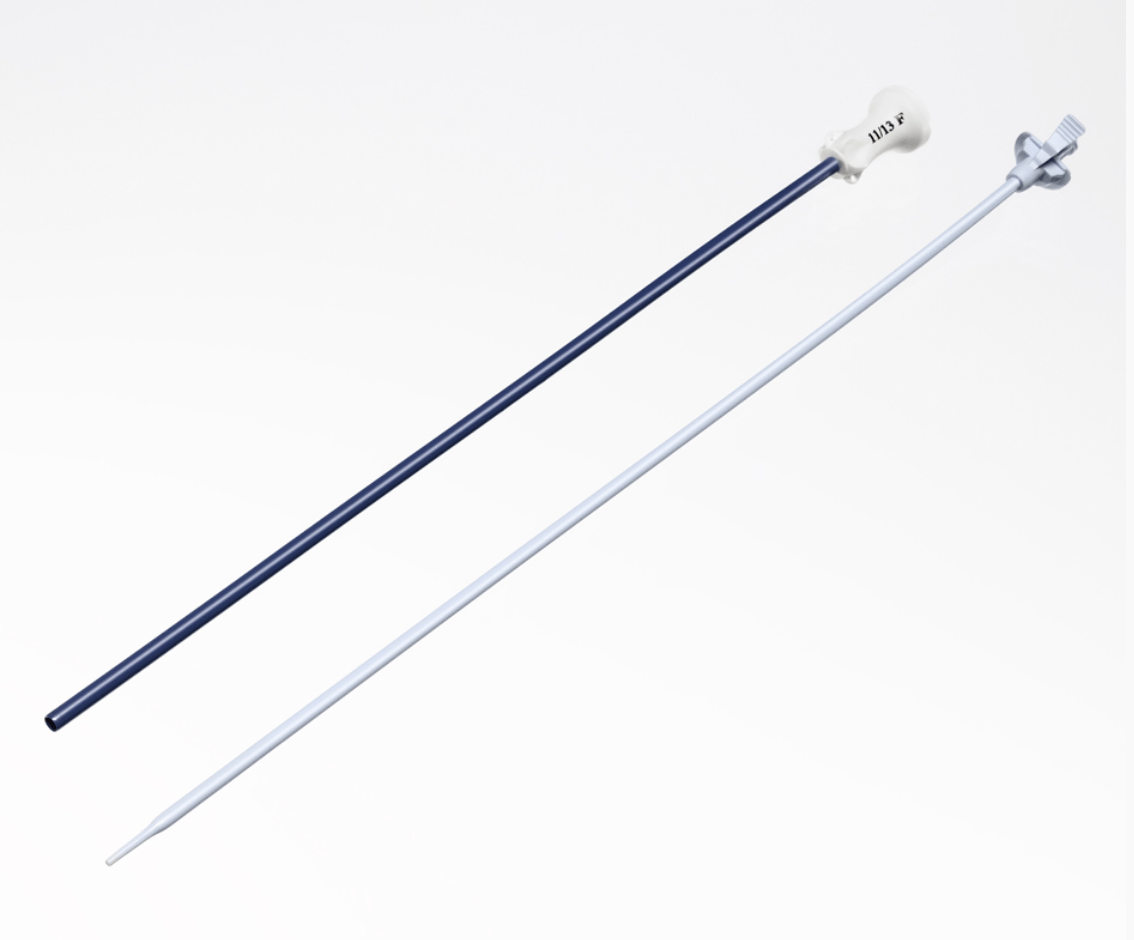 (Figure on Left – Boston Scientific Navigator HD TM, Marlborough, MA)
(Figure on Left – Boston Scientific Navigator HD TM, Marlborough, MA)
The concern with routine use of a sheath is trauma and injury to the ureter when the sheath is passed. Larger diameter sheaths are preferable for procedures, but the ureter is quite narrow and often will not accommodate a large sheath and sometimes any sheath at all. In such cases, surgeons have several options. If they deem a sheath necessary, they can place a temporary ureteral stent that lets the ureter passively dilate and facilitate sheath placement at a later time. Alternatively, they can dilate the ureter during the procedure using either balloon or serial dilators in order to get the sheath up.
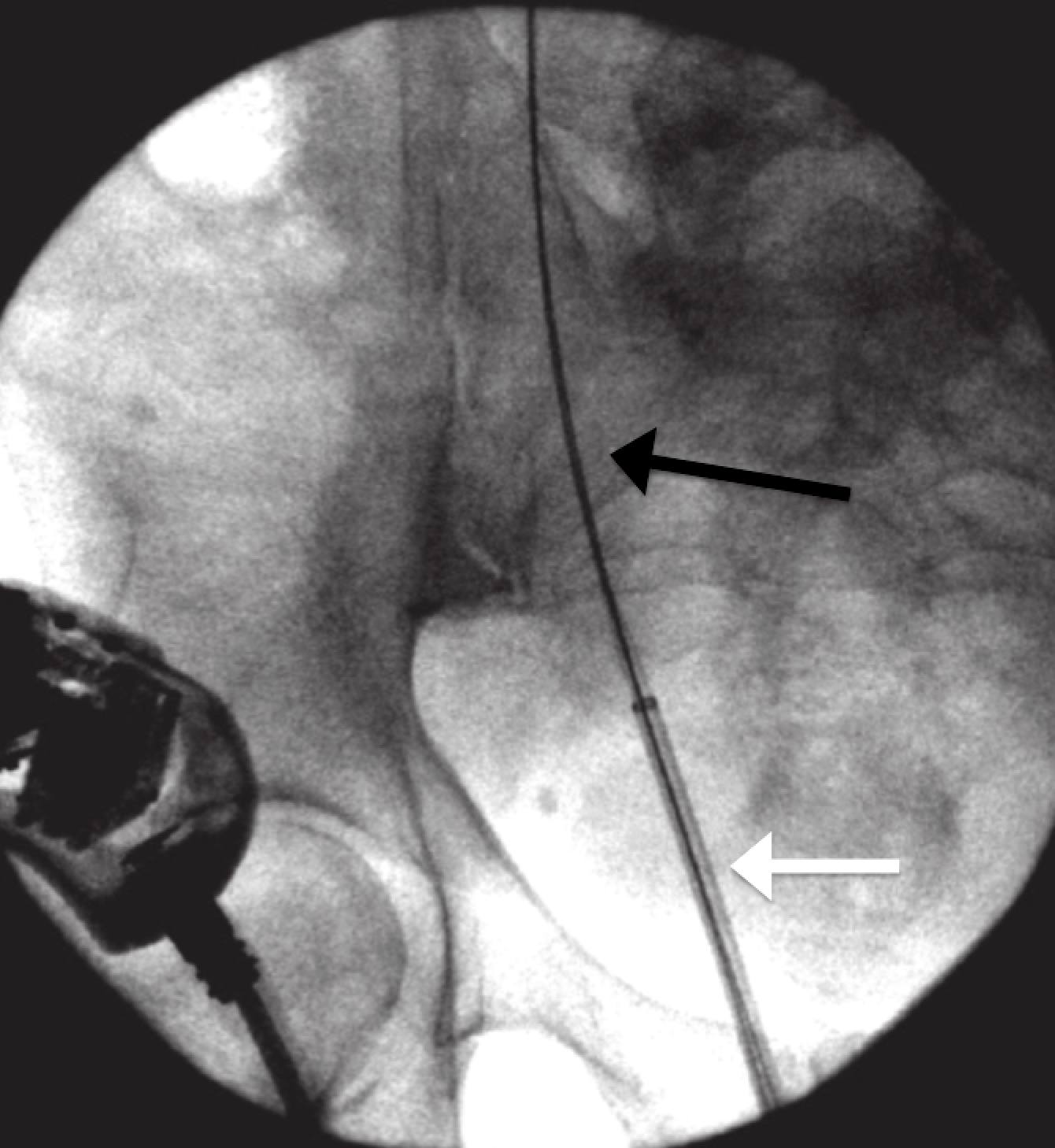
(The ureteral access sheath (white arrow) is passed under fluoroscopic guidance over a wire (black arrow) that is positioned from outside the body and extends through the ureter to the kidney.)
Because the ureter is delicate and easily torn and injured when overstretched, there is risk. In a recent publication by Traxer et al. that describes 359 consecutive cases of ureteroscopy where a ureteral access sheath was used, nearly half (46.5%) of the patients had some degree of ureteral injury. Most injuries were superficial, but severe injuries were found in 13.3%. The main figure (below) from this paper often presented at society meetings, particularly by those who do not favor sheath use.
While these images raise concerns, there is no evidence to date that when managed properly with placement of a temporary ureteral stent these injuries produce any long term consequence. For example, there is no published evidence of an association between ureteral access sheath use and ureteral stricture. Most studies have shown that intraoperative complication rates during flexible ureteroscopy are no different with or without an access sheath.
Alternatively, urologists have the option of performing ureteroscopy without using a sheath at all. One advantage of this approach is that the ureteroscopes themselves are thinner than the sheaths and thus more likely to be able to be passed up the naturally thin ureter without trauma or need for dilation. This approach does have limitations though including poorer visualization, higher potential for excess intrarenal pressure, and a limited ability to make multiple passes back and forth between the kidney and bladder to remove stones.
Lasers and Baskets
Many instruments, all are extremely thin, can be passed through the small working channel that runs from the back of the ureteroscope outside of the body, to the tip of the scope in the kidney. They are used to fragment and remove stones.
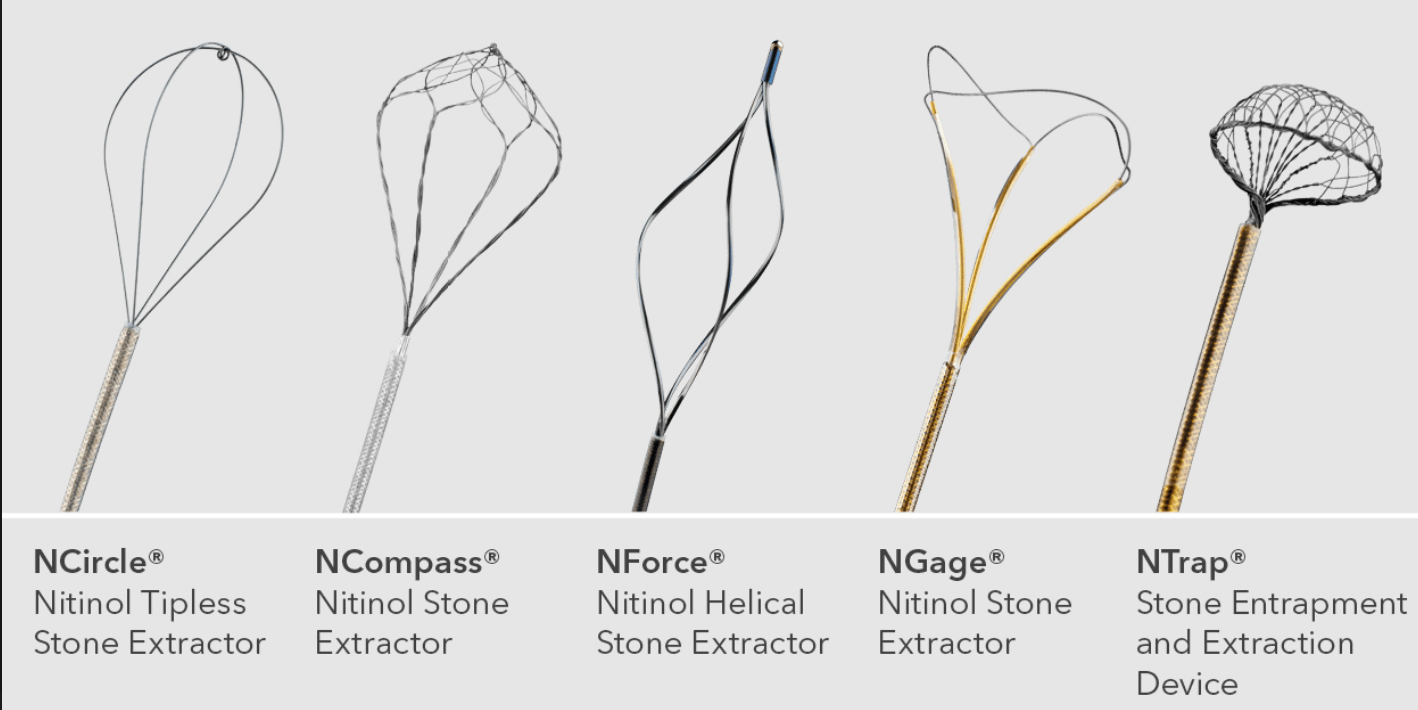
Stone retrieval baskets, pictured below, (Cook Medical, Bloomington, IN) are opened and closed by an assistant to ensnare stones and remove them from the kidney. They come in various shapes, sizes and configurations. When stones are roughly 2-4 mm the basket is able to remove them intact. When stones are larger, they must be fragmented into smaller pieces in order to be removed or pass.
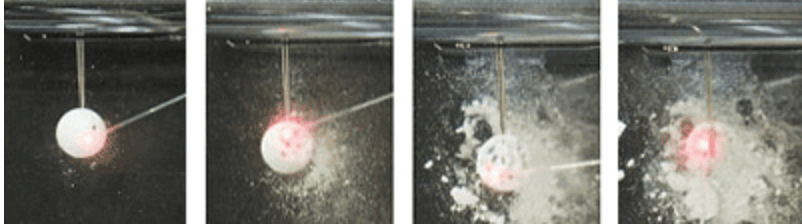
The most commonly utilized method to fragment stones during ureteroscopy is laser lithotripsy. Several lasers exist for the purpose but the most popular one by far is the Holmium laser. The Holmium laser can safely fragment any type of stone. The laser delivers short bursts of light energy through water that destroys the stone’s structure by creating a micro explosion of intense heat, pressure, and cavitation bubbles. Because the laser energy penetrates less than half of a millimeter deep it causes minimal damage to surrounding tissues.
(Dornier Medtech, Friedrichshafen, Germany)
Ureteroscopic Stone Treatment Techniques
As ureteroscopic technology and familiarity with this approach to treat stones continues to grow, the relative number of stones being treated in this fashion has been growing rapidly as well. The latest estimates of surgical practice from the past decade show that ureteroscopy has replaced shock wave lithotripsy as the most commonly performed treatment of kidney stones, accounting for 54% of upper urinary tract stone procedures. Along with the widespread adoption of this procedure, two main techniques have evolved into practice, the optimal one of which remains unclear.
Active Extraction
Active extraction means to remove every piece of stone from the kidney so that at the end of the procedure there are no remaining stones and patients do not pass any stones postoperatively. Critics raise concerns that this technique requires a ureteral access sheath, an assistant to operate the basket, and potentially increases the operating time. A video description of this technique prepared for this article can be seen below.
[youtube id=”gz_VK6qn2Fw”]
Stone Dusting
Stone dusting is conceptually different from active extraction because the goal of the procedure is not to remove all stones directly but rather fragment them into minute pieces (dust) that can then be passed after the procedure, painlessly and without consequence.
Because his technique needs no access sheath, being performed with single pass of the ureteroscope, it benefits patients with narrow ureters. The surgeon can dust with only a laser and avoid a basket with its cost of disposable equipment and need for a skilled assistant. Here is a video of the procedure prepared by Lumenis Ltd, Israel.
[youtube id=”ooj9d_f81MY”]
Which Technique is Best?
Urologists debate whether active extraction or dusting is the better treatment approach, and both sides have their staunch advocates. As is common, the intensity of debate reflects the paucity of studies that compare the two techniques.
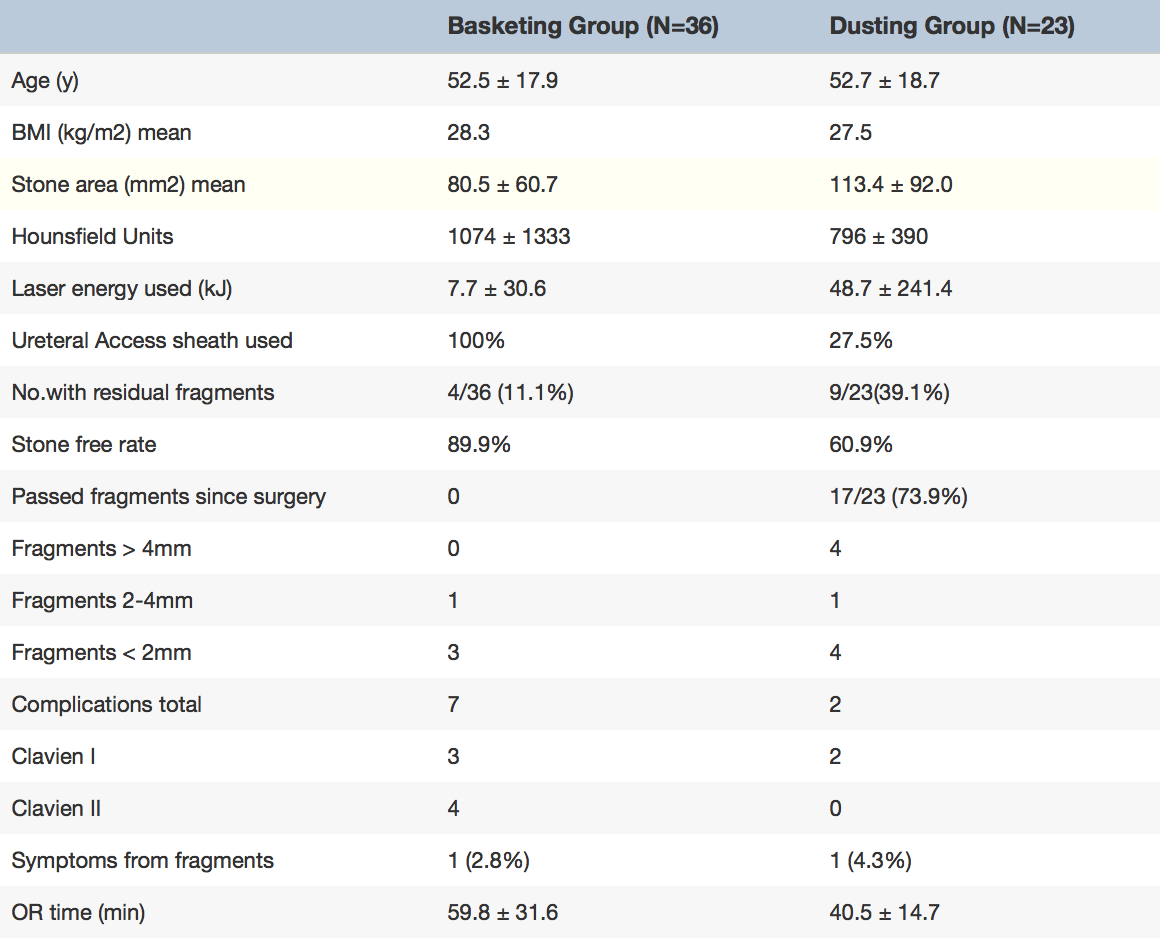
Interim results from an ongoing study by the Endourology Disease Group for Excellence (EDGE) comparing dusting to active extraction (table) indicate that dusting is associated with a shorter operative time (40.5 vs. 59.8 min) despite being used to treat larger stones (113 mm2 vs 81mm2).
On the other hand, a greater percentage of patients treated with a dusting had residual (leftover) stones after the procedure than those treated using active extraction (39.1% vs 11.1%).
These residual stones were not just dust; 44% of the stones were greater than 4 mm.
Despite the higher rate of residual fragments in the dusting group, only one patient in each arm suffered symptoms from a residual fragment at short term follow-up, raising the question of whether or not small residual stones are clinically significant.
But these ‘clinically insignificant residual fragments (CIRFs)’ may not be clinically insignificant.
In one recent study, the EDGE working group found that 44% of 232 patients who had ureteroscopic stone treatment and were found to have residual fragments experienced a “stone event” (defined as a composite of stone growth (at least 1 mm), stone passage, re-intervention or postoperative complications) at mean follow-up of nearly 17 months. Of these 29% required a surgical intervention.
The likelihood of stone events and reintervention were depended on the size of the residual fragment. Among patients with fragments greater than 4mm, reintervention was required 38% of the time and complications related to the fragment occurred 59% of the time. Second surgical procedures occurred sooner in patients treated with a dusting technique compared to those treated with active extraction but the statistical significance of this difference was uncertain.
Portis et al. found that among 218 patients treated with ureteroscopy and active extraction residual stones predicted need for retreatment. At a median follow-up of 4.1 years, patients with residual fragments less than 2mm in size required retreatment 2.4% of the time, compared to 19% among patients with residual fragments 2 to 4 mm in size, and 46% among patients with residual fragment greater than 4mm. Rebuck et al. found a nearly 20% likelihood of retreatment for residual fragments less than 4 mm after ureteroscopy at a mean of 1.6 years.
All in all, both sides in the debate can find reasons for their position. Active extraction leaves behind fewer fragments, but so far in a head to head trial need for less secondary surgery has not been documented. Dusting avoids the cost and complexity of the basket and the sheath, but in the long term may condemn patients to more followup surgery. Time and trial will tell, ultimately.
Follow-Up After Ureteroscopy
Oftentimes urologists will leave a temporary ureteral stent to prevent swelling of the ureter as a result of the procedure. This use of stents is a source of controversy worthy of a future post.
All agree one needs follow-up imaging of the kidneys to tell whether or not stones have been fully removed and whether or not a ureteral stricture (scar) has caused obstruction and kidney swelling (hydronephrosis), a complication that occurs 1-4% of the time.
Ultrasound Imaging
Ultrasound is relatively inexpensive, requires no radiation, and offers very detailed images of the kidney to determine whether or not there is hydronephrosis. But it is not very accurate at identifying residual stones, particularly small ones. It is also operator dependent and results can vary based upon the experience of the sonographer performing the examination.
KUB X-Rays
Ultrasounds are commonly combined with a kidney x-ray (commonly referred to as a KUB) which is also inexpensive and better at detecting stones with minimal radiation.The majority of published studies to date that have assessed stone free rate after ureterscopy have used KUB/US to determine the presence of residual fragments. Stone free rates using this imaging endpoint are commonly found to be in the mid 80-90%; even for large stones greater than 2 cm in size.
CT Scans
CT scans are the best test to identify stones, but are more expensive and are associated with higher degrees of radiation. Those studies that have used postoperative CT scans to identify residual stones demonstrate much lower stone free rates, commonly in the range of 50%. Interestingly the difference appears to be in the small stones <4 mm more likely to be seen on CT scan over KUB/US. If these stones are not taken into consideration, CT scan follow-up would otherwise be on par with that reported in the KUB/US series.
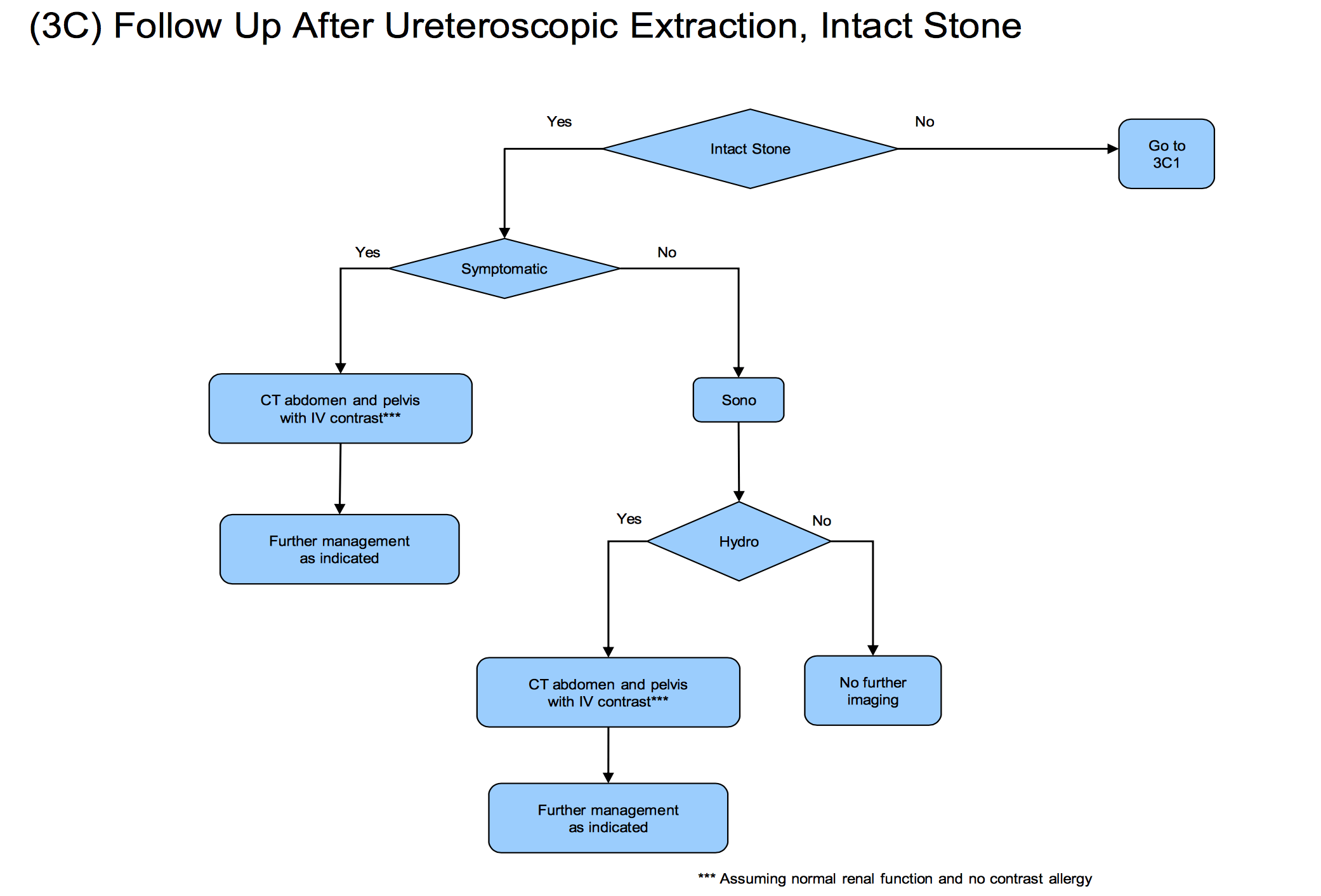
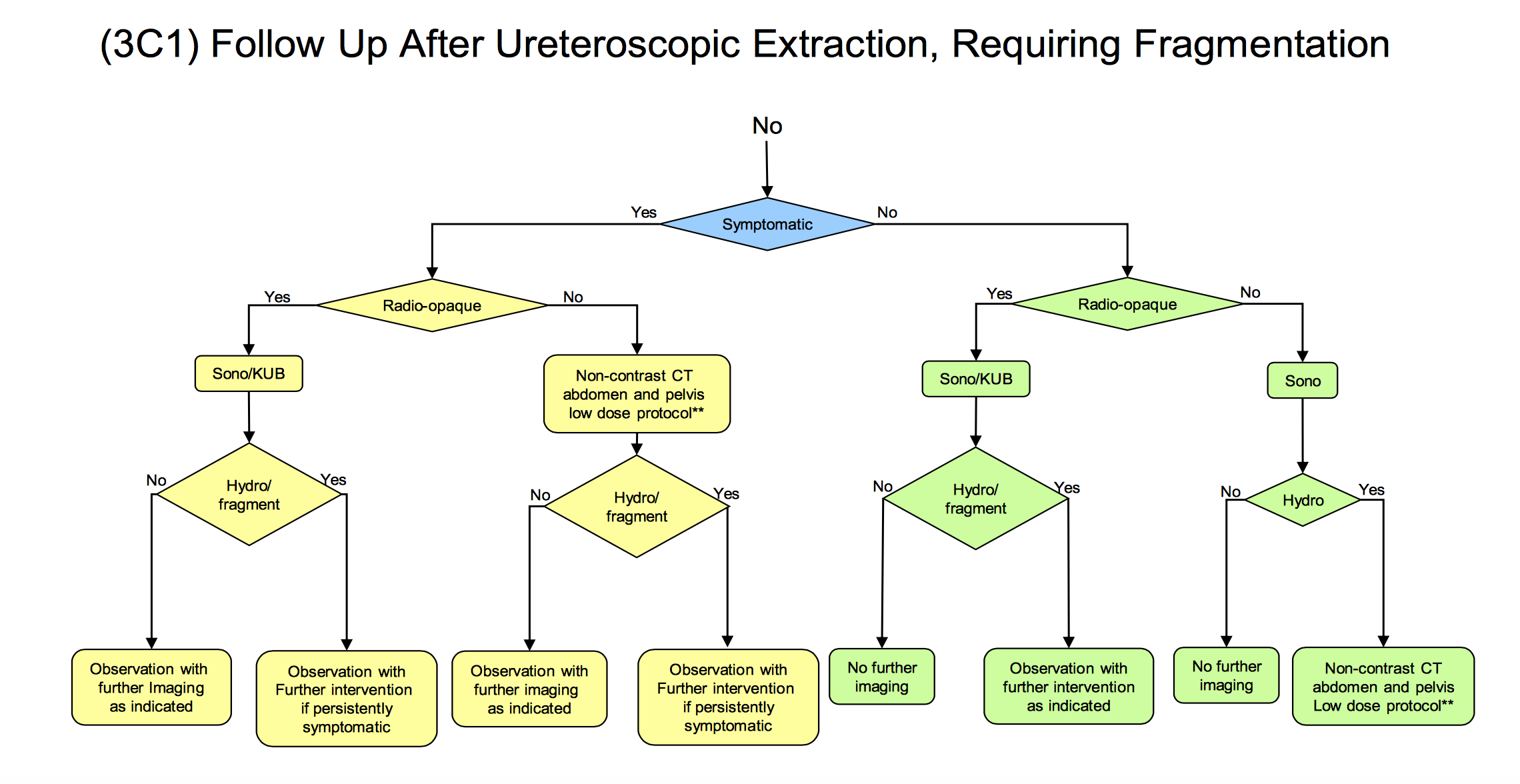
Although the question of whether KUB/US or CT is a better follow-up test is an important one, the more important question is whether or not routine imaging is being performed after the procedure at all. Despite recommendations by the American Urological Association that all patients should undergo at least a minimum of an ultrasound after ureteroscopy (see figure below) ,a recent study from the Cleveland Clinic found that fewer than half of all urologists routinely obtain any postoperative imaging whatsoever.
Take Away Messages
The goal of ureteroscopy should be to render the patient stone free
Regardless of the technique used, the ultimate goal of the procedure should be to leave the patient with no stones. Residual fragments are likely sources of future stone events. Therefore removing all stones should improve long term outcomes.
Urologists should be familiar with all ureteroscopic treatment techniques
Results of studies such as the EDGE group comparing dusting and extraction will determine the gold standard ureteroscopic treatment technique. In all likelihood though, we will come to realize that ureteral anatomy, width, and ability to pass an access sheath as well as the stone themselves will mandate one technique over another for any one patient.
Soft stones, for example, are more likely to fragment to true dust and thus may be more amenable to dusting. Harder stones are more likely to fragment into large pieces and thus benefit from active removal. Infection mandates complete stone removal, potentially harder to achieve with dusting. Alternatively dusting does not require an assistant and thus may be the only feasible option in instances where extra help is not available.
The ureteroscopy should not be the end of the story
Nephrolithiasis often manifests as an acute event ending in ureteroscopy; however, it is increasingly recognized as a chronic condition. As such, it is critical that surgery to remove the stone is not the end of the relationship with the patient.
Residual stones commonly lead to clinical events greater than one year from the time of the initial procedure including growth, passage, and need for retreatment.
Stone disease is chronic and recurrent, and the least desired outcome is formation of new stones after stones have been removed. As many as 50% of first time stone formers will recur within 10 years highlighting the significance and potential benefits to dietary counseling, metabolic testing, surveillance imaging, and other practices to prevent and detect stones over the long-run.
The main thrust of this entire site is toward prevention, before surgery is ever needed and with especial need after a successful surgery so that another need never be performed.


Hi Dr. Coe,
I had a ureteroscopy/cystoscopy yesterday to remove a 3mm ureter stone. The doctor did not find the stone, and said that I must have passed it without realizing it. I did not require a stent. I was given antibiotics through IV during the procedure, and sent home with a five day prescription for Levaquin (500 mg once a day). I am concerned about the side effects of this medication. Is there an alternate medications that I can request, or does this prescription sound reasonable to you? I am a 41 year old female, distance runner/weight lifter. The idea of rupturing a tendon due to this medication is scary.
Hi Janet, I can understand your concerns, as this drug has very significant warnings. I would simply ask my urologist for an alternative medication. Tendon ruptures are indeed an accepted consequence. Regards, Fred Coe
My mother in law is currently in the hospital for the third time with kidney stones. The first tome she got here they told her she had stones and had to follow up with a urologist. The 2nd time we were in the Er was a week or 2 later when the urologist canceled due to an emergency. They rescheduled her appt. but since she was in severe pain she headed to ER again. The 2nd time they placed a stent but recommended laser surgery. We scheduled another appt with urology and haven’t been seen yet. Now we are in the ER for the 3rd time. She was supposed to have surgery but now they are waiting on a urine culture as it seems she might have an infection. Can she still have surgery? She’s been in pain since last night and can’t bare the pain anymore and we are still waiting to hear back to see what the plan is. Is it true she can’t get surgery of culture comes back positive with it uti? Any other options for her so she can get the stones removed?
Hi Vorellana, The problem of surgery during infection is so specific to the individual patient situation I cannot say anything specific. I presume by this time – November 3 – everything has been taken care of. The stent can cause pain, infection can set in, and I agree with you that treatment needs to be completed. If it has not been, perhaps she needs transfer to an institution that is prepared to complete it. Regards, Fred Coe
Dr. Coe,
On January 8th, 2020, I was scheduled to proceed “Cystoscopy, ureteroscopy with biopsy and fulguration and placement of stent” because the findings of both CT dated 11/18/19 and MRI dated 12/02/19 have indicated a right renal pelvis mass suspicious for upper tract urothelial cancer.
However, my urologist was not able to complete the procedure because the ureteroscopy was not able to go through the area between the ureter/bladder and the kidney. The reason was because the diameter of the area is TOO NARROW. Therefore, I was discharged with a stent placement. And my urologist will see me again in two weeks.
Would you please tell me what alternative treatment could be done to remove the neoplasm completely and also get biopsy done successfully?
With warm appreciation,
Mei
Hi Mei, I am afraid this is outside my expertise. Given the situation I would ask my urologist about alternatives and about the wisdom of a second opinion from a urologist specializing in urological oncology preferably at a medical school. If the procedure cannot be done via ureteroscopy I would presume laparoscopy would be the default, but I have inadequate specialized knowledge to really be of value here. Best, Fred Coe
Hello, Dr. Coe:
I’m a 57 yo overweight female who was diagnosed in December with a first time stone, 9 mm. My Uro performed the laser lith with basket procedure, but was unsuccessful due to not being able to reach the stone, even though it was low, because my ureter was too small (1 mm). He place a stent & I’m scheduled for the same surgery in two weeks. Why would my ureter be too small & why would he think it will be larger next surgery? I’m so scared. This article was informative, thanks.
Hi Carol, sometimes ureters are small, and placing a stent is a way to dilate it. Your surgeon is doing what I would have expected, and I would hope for a fine outcome. Regards, Fred Coe
my mother had laser kidney surgery in march, she has a staghorn stone, after the surgery she is very sore when she sit on the couch, what can I do to make her more confortable
Hi Donna, I am afraid this is something only her surgeon can answer. Regards, Fred Coe
Dear Dr. Coe,
I had a 9 mm calcium oxalate stone on my left kidney. A stent was placed and ESWL scheduled. The ESWL session had to be cut short because of pain, but the stone was reduced to 5 mm. Now my doctor is refusing to send me again for ESWL and wants to do RIRS instead. The position of the stone is the same, top of the ureter. I am worried about the risks of this surgery, also considering that I have already passed stones this size myself. What is the main advantage of choosing RIRS over ESWL in my case? What about just removing the stent and trying to pass the stone with expulsive therapy?
thank you!
Hi Marc, This is really a complex surgical decision. I imagine she/he believes URS is the most efficient way to remove the remaining stone material, and I have often observed surgeons pursuing this same track. Multiple SWL are not a good idea, so I fully understand avoiding it. As for letting it pass, that may be forlorn idea – it could be adherent and also could pass and obstruct the kidney without your knowing. I would powerfully advise letting your surgeon do as he/she desires in this kind of case. Regards, Fred Coe
Dear Dr. Coe,
I am 30 years old male and discovered that I had UBJ obstruction and stones in 2015 in my left kidney . I had my first endopyelotomy but the surgery was not successful. In 2019, I decided to do a robotic laparoscopic pyeloplasty where the doctor was supposed to treat the UBJ obstruction and remove the kidney stones, to later find out the ubj obsuctration was fixed but the doctor did not remove the kidney stones.
in March 2020, I did a CT Scan to find that I now multiple obstructing left renal calculi measuring up to 7mm at the UBJ with moderate left hydronephrosis. I changed the doctor and seek advice from a different one (since he forgot to remove the stones) and he suggested that the best option for me is percutaneous nephrolithotomy to take out the stones. His second recommendation was ureteroscopy but said that it will probably leave dust that it could cause more problem and damage the kidney.
My question is : I am more toward doing the ureterscopy as it is less invasive- take less time and stay in the hospital? in general, would you recommend the ureterscopy over percutaneous nephrolithotomy for patients in my situation?
my current kidney functions are 26% (left) and 74% (right)
Thank you so much for your advice
Hi Sinnane, I am not sure what UBJ obstruction is but I presume you mean UPJ, at the junction of the ureter and renal pelvis. I gather stones formed behind it and were left in place during a lap repair. In March you have hydronephrosis, lots of apparently new stones, and greatly reduced function on the obstructed side. For choice of procedure, a complex decision that your surgeon needs to make. One big issue is how much kidney tissue has been lost – it will not come back. A PERC is rather invasive and you may lose more functioning tissue. URS done through a ureteral sheath allows removal of the stone without leaving dust behind, and might be ideal if your surgeon believes it is reasonable given the past UPJ repair. Regards, Fred Coe
Hi, I had a 14×12 mm kidney stone removed (dusted?) by laser surgery a month ago, with stent inserted. Up until yesterday I have have had blood in my urine every time i pee . Yesterday was more clear, almost normal. I have been drinking over a gallon of water a day, but still had several clumps of what looks like coagulated blood. Of course I have also had the urge to pee about 50 times a day EVERY day since the operation, and many of those are the rapid onset of urge. At the end of EVERY urination the burning pain has been very intense. It has worn me out. I did arrange to have the stent removed several weeks early after talking to my urologist. I have had two other stones, but over ten years ago, and this one was the largest by far. Last night I had what in my mind can only be seen as another kidney stone attack. I did not take myself to the hospital. The pain was as intense as when I went in for the surgery. I just could not believe it, and thought I must be wrong. So I stayed home. At 3 am I took two oxycodone for the pain, and passed out 45 min later. I don’t see my Dr. until Sept 1, and this is Sunday. I will call his office on monday and try and discuss. Any thoughts? Thanks, David in Delawawre.
Hi DEavid, Stents are often terrible! My main thought is prevention of more. Take a look and be sure you are giving yourself all possible benefits. Regards, Fred Coe
Hi Dr. Coe,
How often does extravasation of fluid around ureter and kidney occur? I had laser lithotripsy done and 10 mins after leaving the surgery facility had 9 pain score, soaked with sweat and nearly passed out. The next day I had extreme pain still, unable to use my left leg correctly (couldn’t lift foot off floor, had to physically lift left leg to move it etc), pain in upper thigh and groin. Long story short, eventually had CT followup which showed fluid build up around my peroneal nerve. Leg is slowly gaining function back (now 2 weeks post op). How long does it typically take for my body to resorb the fluid? And any long term damage from the nerve compression?
Thanks
VK
Hi V K, as I am not a surgeon, I cannot answer your question with perfect assurance, but I have never before heard of this happening. This link from the AUA suggests that this particular nerve injury comes from “Stirrup pressure on fibular neck • OR Table pressure on dependent leg” during the procedure. For more you would need to consult a surgeon. Regards, Fred Coe
Hi Doc , I had a Uretersocopy last September and the scope used came apart inside me and had to spend 6 days in the hospital to wait for the swelling to go down in the ureter tube above my bladder , my Dr removed it ok but the broken scope damaged the tube and a stint was later put in to expand it back to normal and that worked . This whole process lasted from September 2019 to January 10 2020 , quite the ordeal . I was told this had happened twice , my situation and once before. My question : is how common is this or is it for these scopes coming apart ? I’m still experiencing pain in my testicular area , my best Ron
Hi Ron, Oh my! Scope breakage is not common, but the instruments can be fragile. It sounds like your physician did all he could to get the part removed, and injury to the ureter is not surprising. A Google search (“ureteroscope breakage during surgery with retained parts scholar”) found this lengthy meta-analysis and it included breakage with retained parts – not very common. IN all URS seems to have a lot more hazards than our article implies. Regards, Fred Coe
Hi,
I had a ureteroscopy yesterday to remove a 4mm ureter stone. While the Stone was present in a CT scan taken in the ER two weeks ago, the surgeon did not find the stone and said that I must have passed it or dissolved it without knowing. However, he found some slight kidney and bladder inflammation and diagnosed me with Interstitial Cystitis. Even though no stone was found, he did place a ureter stent and my appointment to remove it is in 8 days. I am far more uncomfortable now than I was in the days leading up to my surgery (I was in no pain and taking zero pain meds for 5 days leading up to surgery). I am now experiencing pain that is making me unable to sleep, urinating is really the most painful (like a severe pain I need to actively breath through) and peeing seems to make my pain worse for about 30 minutes after as well. I’m wondering if this stent was necessary? And if so, is it necessary to have the stent for just as long as I would have if they did find the kidney stone? This Post-op appointment was made before my surgery and I’m worried it’s more due to convenience / availability. And what my options are? I was given antibiotics during surgery but sent home with no prescriptions and instructions to just take Tylenol. I’m planning to call the nurses line in the morning but wondering what your thoughts are.
This is my first kidney stone and I am an otherwise healthy, active 25 year old female.
Hi KP, Stents can and do cause horrid pain. Most surgeons try to keep them in to prevent ureteral narrowing after URS. I would suggest calling the physician or assistants and asking for as prompt removal as is safe. As for the stone, perhaps one might want to get a CT and see if the stone is still there. It may be. Regards, Fred Coe
hi, Dc, my Mom’s surgeon perforemed replacement of Double J stent for her without any assistance of any visualization equipment ,is this a common practice procedure to do this? Regards, Hao
Hi levis, I am not sure. Do you mean she/he removed a stent and put in a new one without an instrument? I do not know of that being possible. Stents are frequently removed without instruments, even by patients themselves. I am not a surgeon, however, so I cannot be absolutely positive here. Regards, Fred Coe
My father vomited and is running a fever after the procedure. Is this normal?
Hi Zoya, I presume a stone removal procedure. Some vomiting is common after surgery fever usually means infection that I am sure his physicians are treating. Regards, Fred Coe
Hi Dr. — I had a ureteroscopy w/ laser preformed to remove a 7mm stone, which I was told was successful. Had a stent in place for 3 days and was subsequently removed by my dr. Fast forward one month and I am experiencing frequent flank pain, sometimes shooting down my outer thigh — all on the side where the stone once was. I had a sonogram done recently and it came back entirely normal. I can’t understand why I am in such pain! Is it likely a residual fragment not picked up by the sonogram? If so, would a urine test detect this? I’d like to avoid a CT scan given the radiation. Appreciate your advice!
Hi Justin, Obstruction is so serious I would do a CT. US is very weak at detecting stones compared to CT. Regards, Fred Coe
After having blood in my urine and short-term back pain, I was recently told I have a 4mm cluster of small kidney stones in one kidney and they aren’t passing, possibly due to the anatomy of the kidney. (I clearly passed one or more stones, which is what caused the paid and bleeding). I have read numerous horror stories of ureteroscopy mishaps, mostly due to the stents perforating the ureter. This is terrifying and seems very prevalent. I have not had any pain since the first episode but was recently told there are small traces of blood in my urine. I’m wondering if this could be a case of watch-wait-and-see or if I absolutely need to have the stones removed. Is percutaneous surgery a viable option, given the very real risks with ureteroscop? Also, can asymptomatic kidney stones cause problems such as general malaise, etc.? Your feedback is appreciated.
Hi Scott, I presume the bleeding led to discovery of the stones. Ureteroscopy is overall reasonably safe but I can understand your not wanting surgery – no one wants to have it. Prevention of more stones is your most important approach. It will minimize the growth of those present. Start here, and plan an organized approach for yourself. Use yearly low dose CT scans to follow the ones you have. Regards, Fred Coe
Hi
I have multiple stones , some over 1 cm and parapelvic cysts. Can the parapelvic cysts be disturbed when they do a laser l. And Utererscopy? Some stones are inside the kidney and two are in the UPJ.
Anni
Hi Anni, I cannot say much in detail given just the few facts, but the cysts are not a problem during ureteroscopy. The procedure lets your surgeon remove stones inside the kidney and at the UPJ. Regards, Fred Coe
I have a history of kidney stones. Last scope over a year ago the Urologist said my ureter was damaged cause he had to dig a stone out that was embedded. Now I have a 7mm stone and went to scope last month but my ureter was strictured and he couldn’t reach the stone. He inserted a stent to help with the stricture which caused Pressure, terrible burning with urinating, spasms and frequency and urgency urination. I go back in tomorrow and he will try again to reach the stone and insert another stent. I am so nervous. Do you think things could turn out and he could reach the stone without any more damage to my ureter?
Hi Sharon, Surgical details are no specific an outsider has little of value to offer. If your present surgeon cannot manage things she/he should refer you to a specialized center where you can get more help. Regards, Fred Coe
I’m a patient of Dr Luke Reynolds (great Dr.)
I have 2.2 cm kidney stone in line for Ureteroscopy but I’m terrified with urosepsis Post. been running constant Klebsiela infections if it happens (sepsis)
What is the best treatment and best outcome also best prevention. Thanks I’m terrified and in trouble
Thanks much
Hi Fernando, Dr Reynolds is my partner, and I am sure that if he is aware of this problem he will attend to risk abatement. Be sure and let him know about the Klebsiella history if you have not already done so. Dr Reynolds will know the best approach for your surgery, and his practice is within a university medical center that has in it multiple experts in infection control. Best, Fred Coe
I had a ureteroscopy for a 9mm mid ureter stone causing severe hydronephrosis. I felt like I had a UTI all along. How do I know when I have hydronephrosis? Should I get renal ultrasounds done periodically?
Hi Elan, A very good question. Obstruction is not a good thing. Your urologist is responsible for assuring normal urine drainage and for surveillance aimed at that goal. There is no substitute as you cannot reliably know if obstruction is present or not. New obstruction after this episode usually causes pain or bleeding so you can seek care. Regards, Fred Coe
After ureteroscopy, I am having regular bladder control and frequency issues even after 4 days that the stent was removed? Is there a time frame on this issue and when to be concerned?
Hi Elan, the bladder symptoms are not rare. Only your urologist can help with control of them. Regards, Fred Coe
Hello Dr Coe,
I recently had a ureteroscopy to the right kidney, My surgeon explained that he took some small stones but he couldn’t access some as they are located inside the kidney. He said opening up to extract stones could damage the function,
My question is will the stones make there way out of renal pyramids so he can later access or can they just collect and cause me bigger problems down the road. I really thought this was my chance to be stone free and live without the stress, but once again I’ve been hit with more challenges. Is a pcnl or other means more effective. Thanks for your hard work ( incomplete RTA calcium phosphate stones )
Jonathan.
Hi Jonathan, calcium phosphate stones are a problem, and often recur and grow. The surgery left some behind, and I cannot from here comment on the wisdom or not of another right now. Most likely is that the residual stones may grow rather than pass, and time will tell. But evaluation of cause and directed treatment is crucial. Usually ‘incomplete RTA’ means urine calcium and pH are high, urine citrate below normal. Urine calcium can be lowered with diet and medications, and that sounds like the best course. I imagine your physicians pursue that course. Regards, Fred Coe