MINIMALLY INVASIVE STONE SURGERY (Ureteroscopy)
(Images of surgical equipment featured in this article are for patient education only. They are not intended for promotional use or a reflection of personal preference. We accept no fees or other benefits from vendors or their agents.)
Evolution of Technique
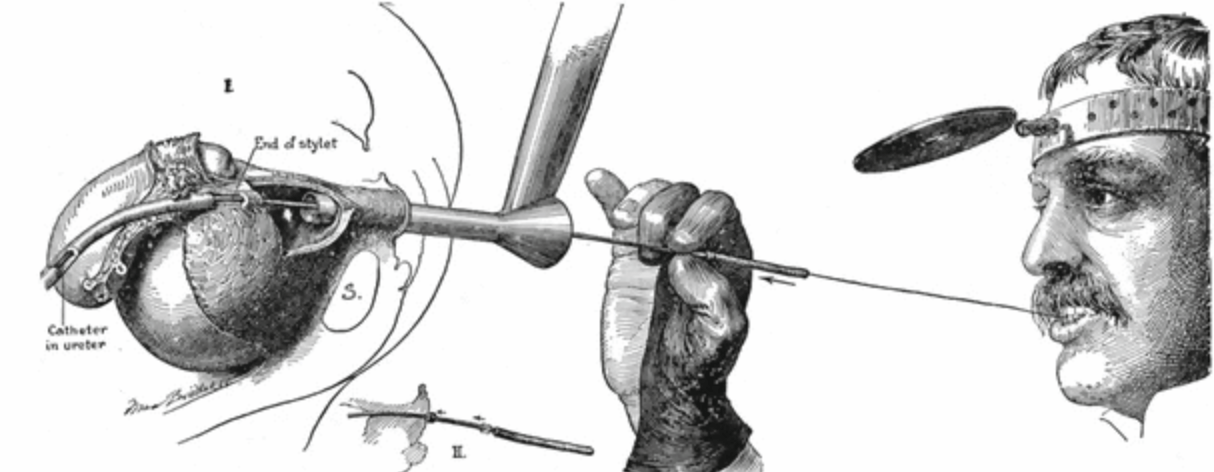
The fascinating history of urology with its captivating depictions, texts and stories rivals any other field in medicine. In particular, the ancient past of lithotomy (treatment and removal of urinary stones) dates back to Mesopotamia (3200 BC), and descriptions and treatments for urinary stone disease have been identified from ancient cultures including Hindu, Greek, and Egyptian. The treatment of stones, which at the time most commonly occurred in the bladder, was very dangerous, often lethal. As such, it led to the development of one of the first medical subspecialists, the lithotomist, who opened the urinary tract and removed stones directly. Recognition of this unique set of skills earned a distinction in the Hippocratic oath, still recited by graduating students: “I will not cut for the stone, but will leave this to be done by practitioners of this work…”
Today, “cutting for stone,” otherwise known as open stone surgery, has been replaced by alternative minimally invasive techniques. Critical to this change has been the introduction of the endoscope. Whereas early pioneers such as Howard Kelly (depicted above in the early 1900’s using a wax tipped catheter in the ureter to detect a ureteral stone) relied heavily on intuition, feel, and clinical suspicion, advances in endoscopy have made it possible to inspect all parts of the urinary tract directly.
The particular endoscope that has revolutionized our ability to treat kidney stones in a minimally invasive fashion is the ureteroscope. Incorporation of its use into urologic practice has led to the development of a unique subspecialty, endourology, that focuses on minimally invasive and endoscopic surgical treatments.
Modern Ureteroscopy
A ureteroscope, as its name implies, is an endoscope designed to visualize and work within the ureter. Other scopes commonly used by urologists and endourologists include the cystoscope (used in the bladder) and the nephroscope (used in the kidney).
Although such scopes now enable modern surgical stone treatment, they have only been routinely utilized for the past several decades. Minimally invasive kidney stone treatment began in the mid-1980’s with shock wave lithotripsy and percutaneous nephrolithotomy. Ureteroscopy for treatment of ureteral stones was not performed routinely until then as well, and it was not until the late 1990’s and early 2000’s that ureteroscopes could routinely access and treat stones in the kidney. In the United States we often take such technologies and treatment options for granted, but open stone surgery is still practiced in many parts of the world where modern technology remains limited.
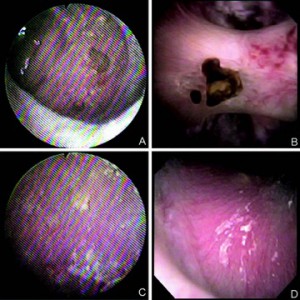
There are two types of ureteroscopes, rigid and flexible. Rigid ureteroscopes, as their name implies, are firm and preferred for treatment of stones lodged in the lower ureter which can usually be accessed in a straight path. When stones are located in the upper ureter and/or kidney, they often require 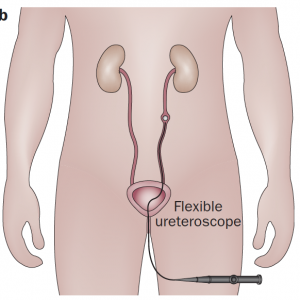
flexible ureteroscopes that accommodate to the shape of the ureter and renal collecting system (figure on right). Though more difficult to maneuver, flexible scopes allow the urologist to inspect nearly the entirety of the inner kidney to find stones, treat them, and remove them using a variety of techniques. Innovation this area is brisk and modern digital ureteroscopes offer increasingly superior image quality, lighting and wide fields of view.
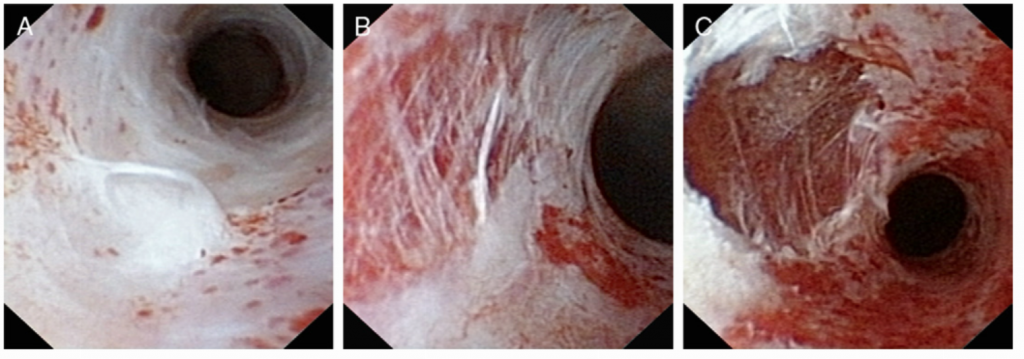
(Figure – Left ) Ureteroscopic image of the renal collecting system using older generation fiberoptic ureteroscope (left) and newer generation digital ureteroscope (right). Note the superior image quality, increased light intensity and wider field of view. Panels A and B feature small stones attached to a renal papilla. Panels C and D feature the endoscopic appearance of Randall’s plaque.
Irrigation and Access Sheaths
In order visualize anything at all, fluid must run continuously through the scope and into the kidney to wash away blood, debris, and crystals that impair visualization. To accomplish this, the fluid (most commonly saline) is hung from a bag and run through tubing directly into the body of the scope where it comes out the tip and into the kidney.
This inflow is harmless, but excess filling of the kidney because of high pressure inflow or an inability of the fluid to freely exit around the scope can overstretch the kidney and cause fluid absorption, leakage, bleeding, and small tears within the kidney itself, a term we call extravasation.
To prevent this, many urologists use a device called a ureteral access sheath. This can be thought of as a temporary tunnel from the bladder to the kidney which allows any fluid that is irrigated into the kidney to quickly wash out around the scope, optimizing visualization and decreasing the likelihood of extravasation. The scope can be passed back and forth without rubbing against and potentially damaging the lining of the ureter, which is generally around the same small diameter as the scope itself. When used appropriately, temporary sheaths are safe and decrease postoperative infections and sepsis. While the majority of urologists routinely use them during ureteroscopy, debate does exist within the community as to whether or not they are required in every case.
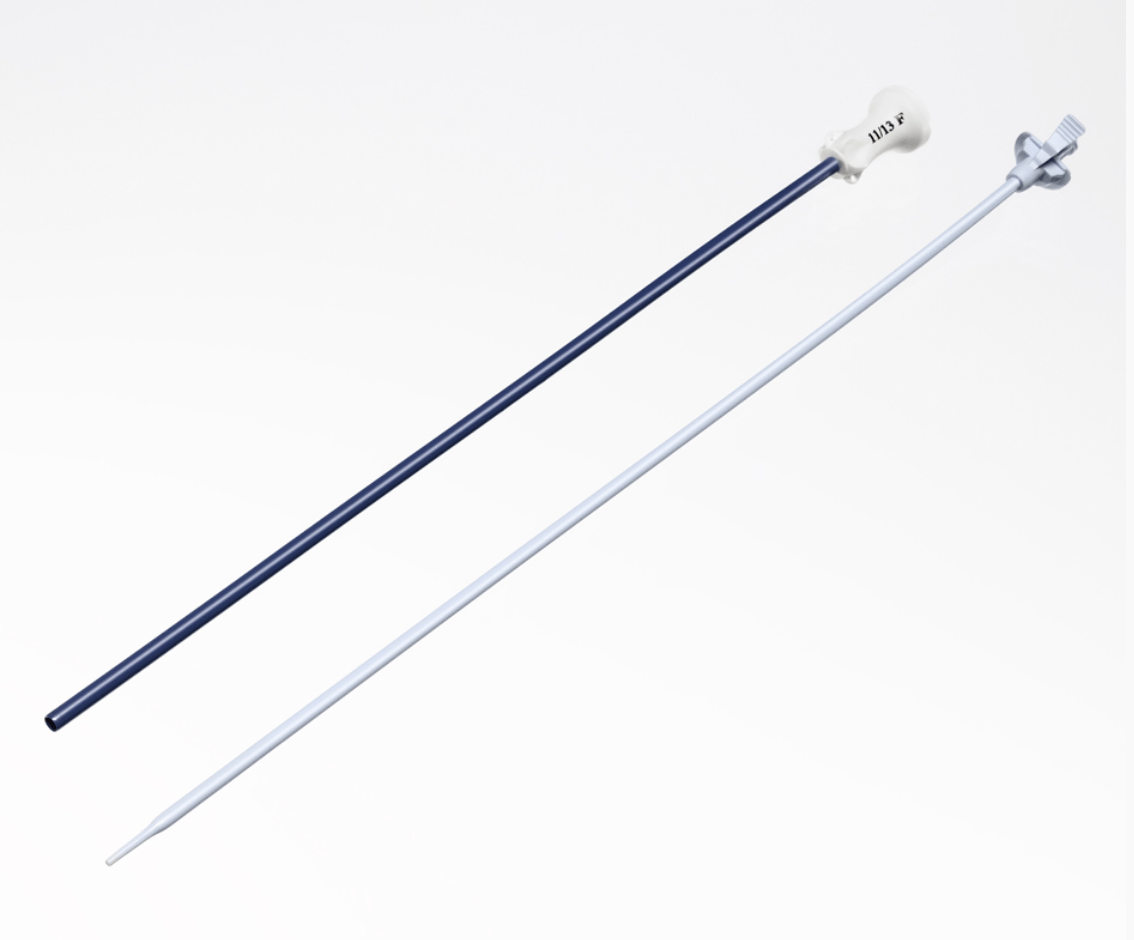 (Figure on Left – Boston Scientific Navigator HD TM, Marlborough, MA)
(Figure on Left – Boston Scientific Navigator HD TM, Marlborough, MA)
The concern with routine use of a sheath is trauma and injury to the ureter when the sheath is passed. Larger diameter sheaths are preferable for procedures, but the ureter is quite narrow and often will not accommodate a large sheath and sometimes any sheath at all. In such cases, surgeons have several options. If they deem a sheath necessary, they can place a temporary ureteral stent that lets the ureter passively dilate and facilitate sheath placement at a later time. Alternatively, they can dilate the ureter during the procedure using either balloon or serial dilators in order to get the sheath up.
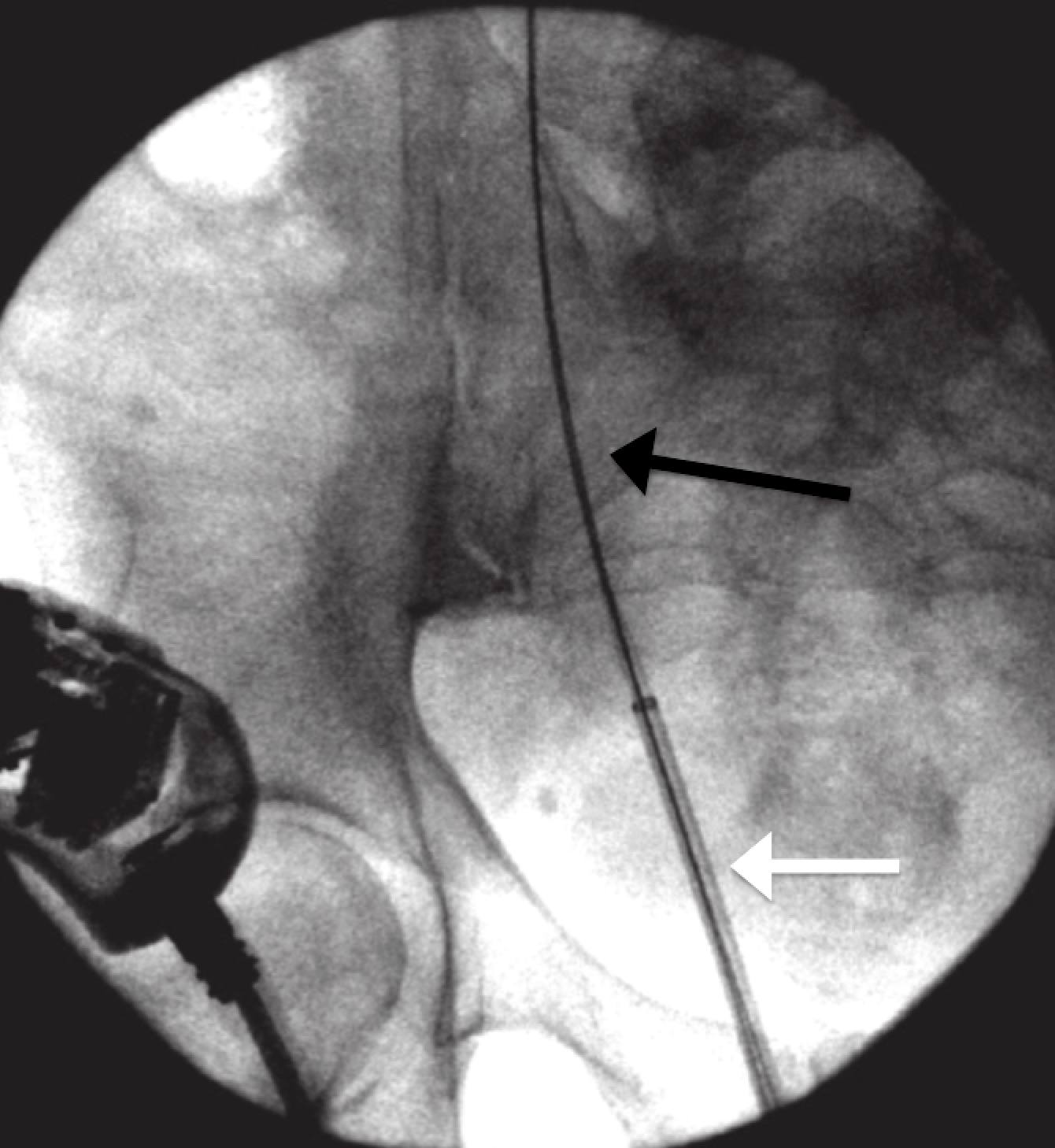
(The ureteral access sheath (white arrow) is passed under fluoroscopic guidance over a wire (black arrow) that is positioned from outside the body and extends through the ureter to the kidney.)
Because the ureter is delicate and easily torn and injured when overstretched, there is risk. In a recent publication by Traxer et al. that describes 359 consecutive cases of ureteroscopy where a ureteral access sheath was used, nearly half (46.5%) of the patients had some degree of ureteral injury. Most injuries were superficial, but severe injuries were found in 13.3%. The main figure (below) from this paper often presented at society meetings, particularly by those who do not favor sheath use.
While these images raise concerns, there is no evidence to date that when managed properly with placement of a temporary ureteral stent these injuries produce any long term consequence. For example, there is no published evidence of an association between ureteral access sheath use and ureteral stricture. Most studies have shown that intraoperative complication rates during flexible ureteroscopy are no different with or without an access sheath.
Alternatively, urologists have the option of performing ureteroscopy without using a sheath at all. One advantage of this approach is that the ureteroscopes themselves are thinner than the sheaths and thus more likely to be able to be passed up the naturally thin ureter without trauma or need for dilation. This approach does have limitations though including poorer visualization, higher potential for excess intrarenal pressure, and a limited ability to make multiple passes back and forth between the kidney and bladder to remove stones.
Lasers and Baskets
Many instruments, all are extremely thin, can be passed through the small working channel that runs from the back of the ureteroscope outside of the body, to the tip of the scope in the kidney. They are used to fragment and remove stones.
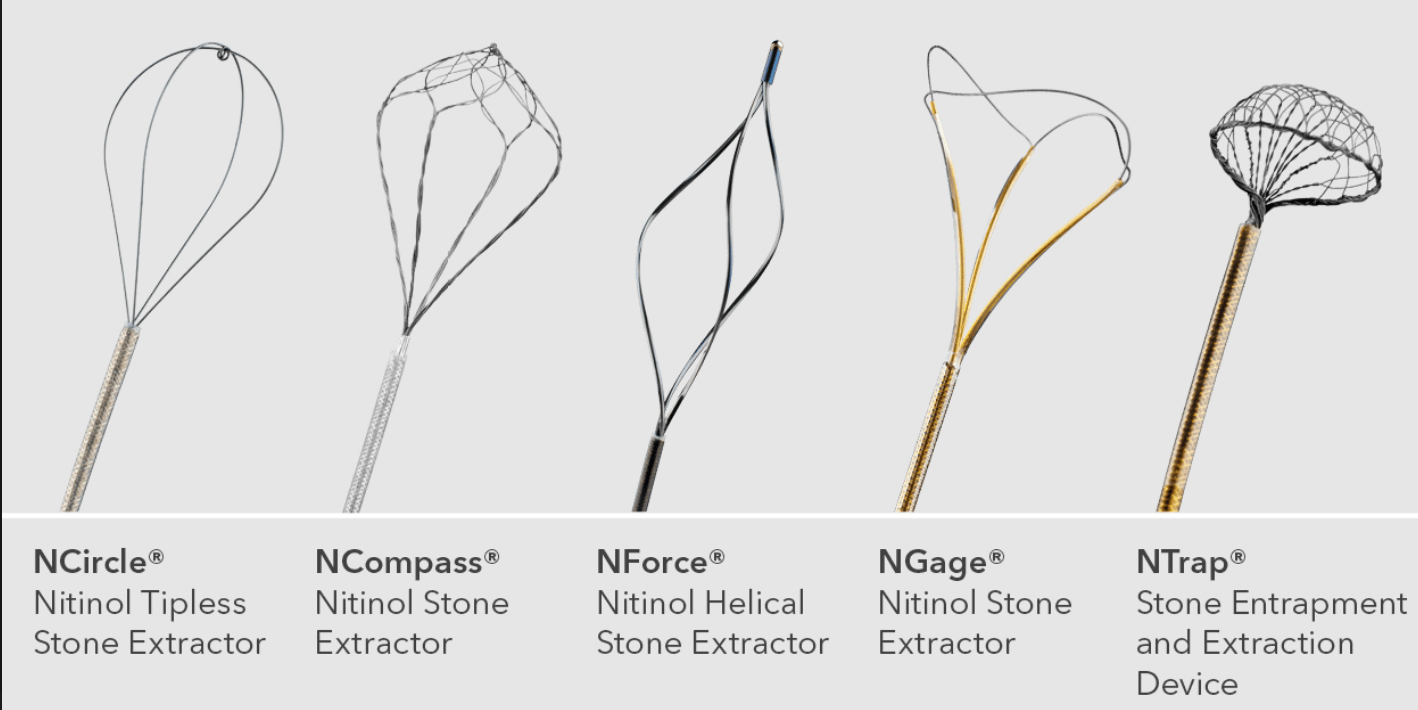
Stone retrieval baskets, pictured below, (Cook Medical, Bloomington, IN) are opened and closed by an assistant to ensnare stones and remove them from the kidney. They come in various shapes, sizes and configurations. When stones are roughly 2-4 mm the basket is able to remove them intact. When stones are larger, they must be fragmented into smaller pieces in order to be removed or pass.
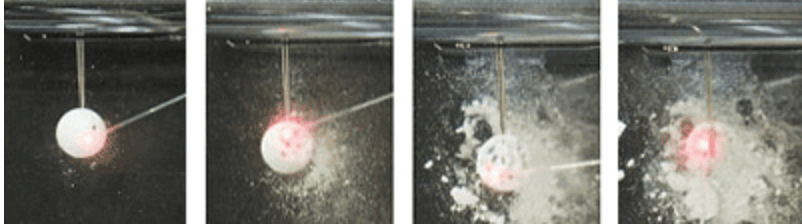
The most commonly utilized method to fragment stones during ureteroscopy is laser lithotripsy. Several lasers exist for the purpose but the most popular one by far is the Holmium laser. The Holmium laser can safely fragment any type of stone. The laser delivers short bursts of light energy through water that destroys the stone’s structure by creating a micro explosion of intense heat, pressure, and cavitation bubbles. Because the laser energy penetrates less than half of a millimeter deep it causes minimal damage to surrounding tissues.
(Dornier Medtech, Friedrichshafen, Germany)
Ureteroscopic Stone Treatment Techniques
As ureteroscopic technology and familiarity with this approach to treat stones continues to grow, the relative number of stones being treated in this fashion has been growing rapidly as well. The latest estimates of surgical practice from the past decade show that ureteroscopy has replaced shock wave lithotripsy as the most commonly performed treatment of kidney stones, accounting for 54% of upper urinary tract stone procedures. Along with the widespread adoption of this procedure, two main techniques have evolved into practice, the optimal one of which remains unclear.
Active Extraction
Active extraction means to remove every piece of stone from the kidney so that at the end of the procedure there are no remaining stones and patients do not pass any stones postoperatively. Critics raise concerns that this technique requires a ureteral access sheath, an assistant to operate the basket, and potentially increases the operating time.
Stone Dusting
Stone dusting is conceptually different from active extraction because the goal of the procedure is not to remove all stones directly but rather fragment them into minute pieces (dust) that can then be passed after the procedure, painlessly and without consequence.
Because his technique needs no access sheath, being performed with single pass of the ureteroscope, it benefits patients with narrow ureters. The surgeon can dust with only a laser and avoid a basket with its cost of disposable equipment and need for a skilled assistant.
Which Technique is Best?
Urologists debate whether active extraction or dusting is the better treatment approach, and both sides have their staunch advocates. As is common, the intensity of debate reflects the paucity of studies that compare the two techniques.
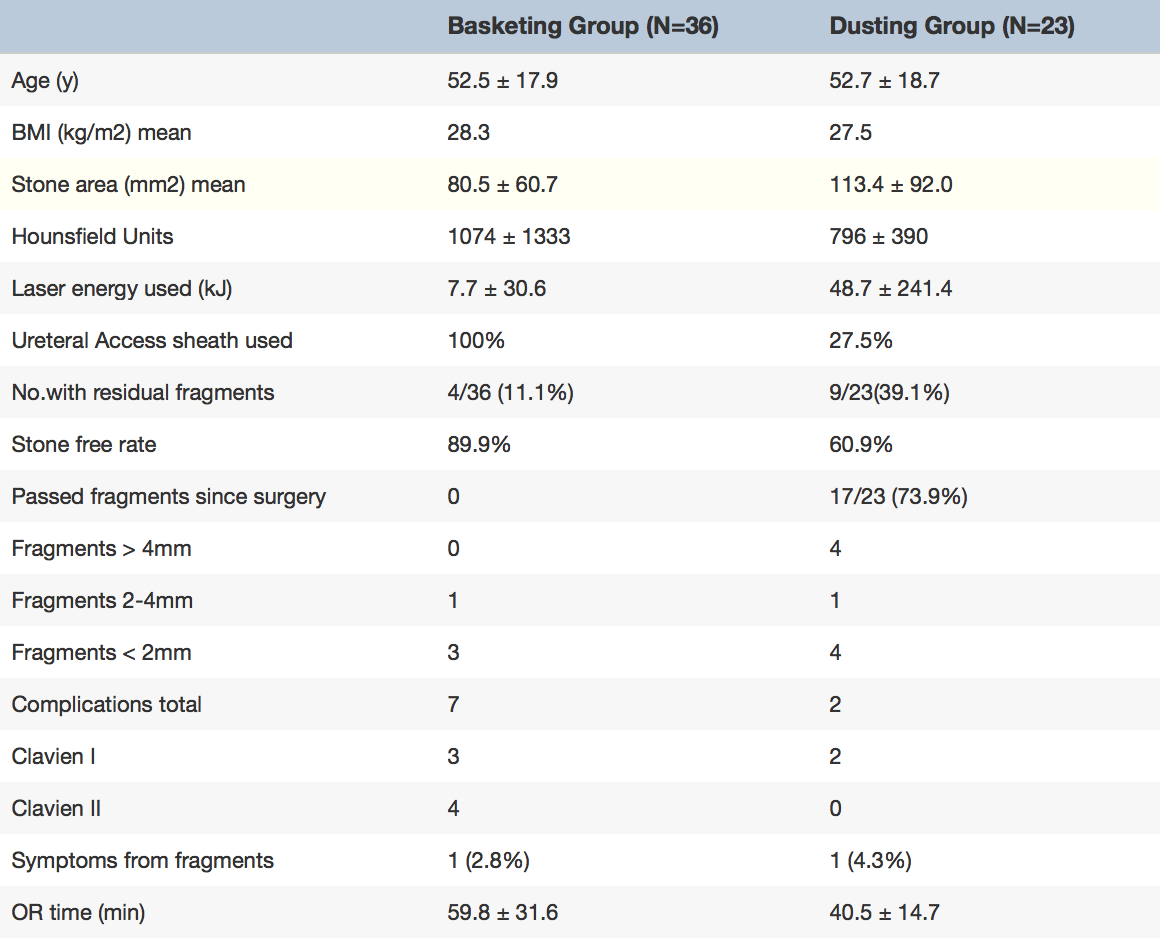
Interim results from an ongoing study by the Endourology Disease Group for Excellence (EDGE) comparing dusting to active extraction (table) indicate that dusting is associated with a shorter operative time (40.5 vs. 59.8 min) despite being used to treat larger stones (113 mm2 vs 81mm2).
On the other hand, a greater percentage of patients treated with a dusting had residual (leftover) stones after the procedure than those treated using active extraction (39.1% vs 11.1%).
These residual stones were not just dust; 44% of the stones were greater than 4 mm.
Despite the higher rate of residual fragments in the dusting group, only one patient in each arm suffered symptoms from a residual fragment at short term follow-up, raising the question of whether or not small residual stones are clinically significant.
But these ‘clinically insignificant residual fragments (CIRFs)’ may not be clinically insignificant.
In one recent study, the EDGE working group found that 44% of 232 patients who had ureteroscopic stone treatment and were found to have residual fragments experienced a “stone event” (defined as a composite of stone growth (at least 1 mm), stone passage, re-intervention or postoperative complications) at mean follow-up of nearly 17 months. Of these 29% required a surgical intervention.
The likelihood of stone events and reintervention were depended on the size of the residual fragment. Among patients with fragments greater than 4mm, reintervention was required 38% of the time and complications related to the fragment occurred 59% of the time. Second surgical procedures occurred sooner in patients treated with a dusting technique compared to those treated with active extraction but the statistical significance of this difference was uncertain.
Portis et al. found that among 218 patients treated with ureteroscopy and active extraction residual stones predicted need for retreatment. At a median follow-up of 4.1 years, patients with residual fragments less than 2mm in size required retreatment 2.4% of the time, compared to 19% among patients with residual fragments 2 to 4 mm in size, and 46% among patients with residual fragment greater than 4mm. Rebuck et al. found a nearly 20% likelihood of retreatment for residual fragments less than 4 mm after ureteroscopy at a mean of 1.6 years.
All in all, both sides in the debate can find reasons for their position. Active extraction leaves behind fewer fragments, but so far in a head to head trial need for less secondary surgery has not been documented. Dusting avoids the cost and complexity of the basket and the sheath, but in the long term may condemn patients to more followup surgery. Time and trial will tell, ultimately.
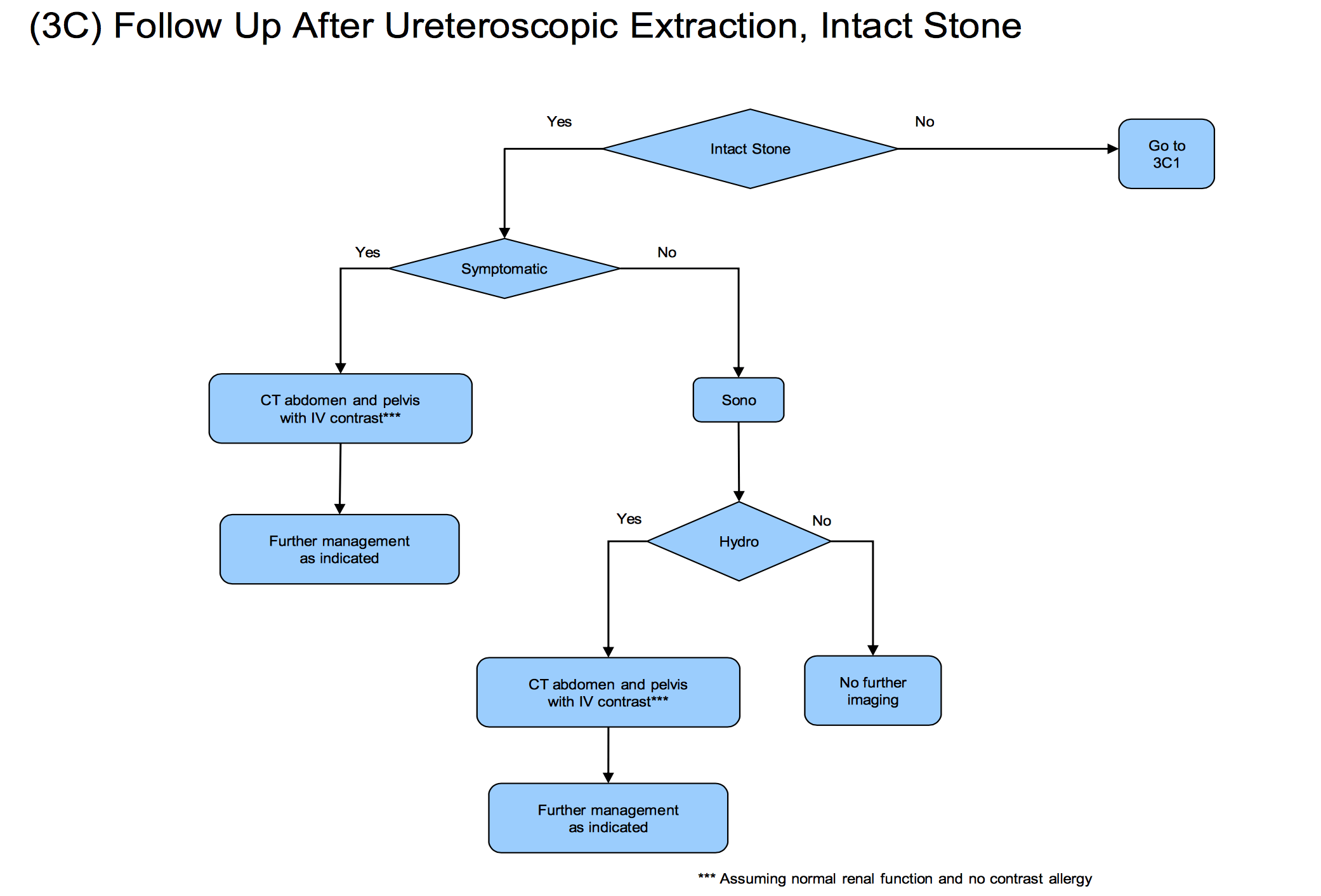
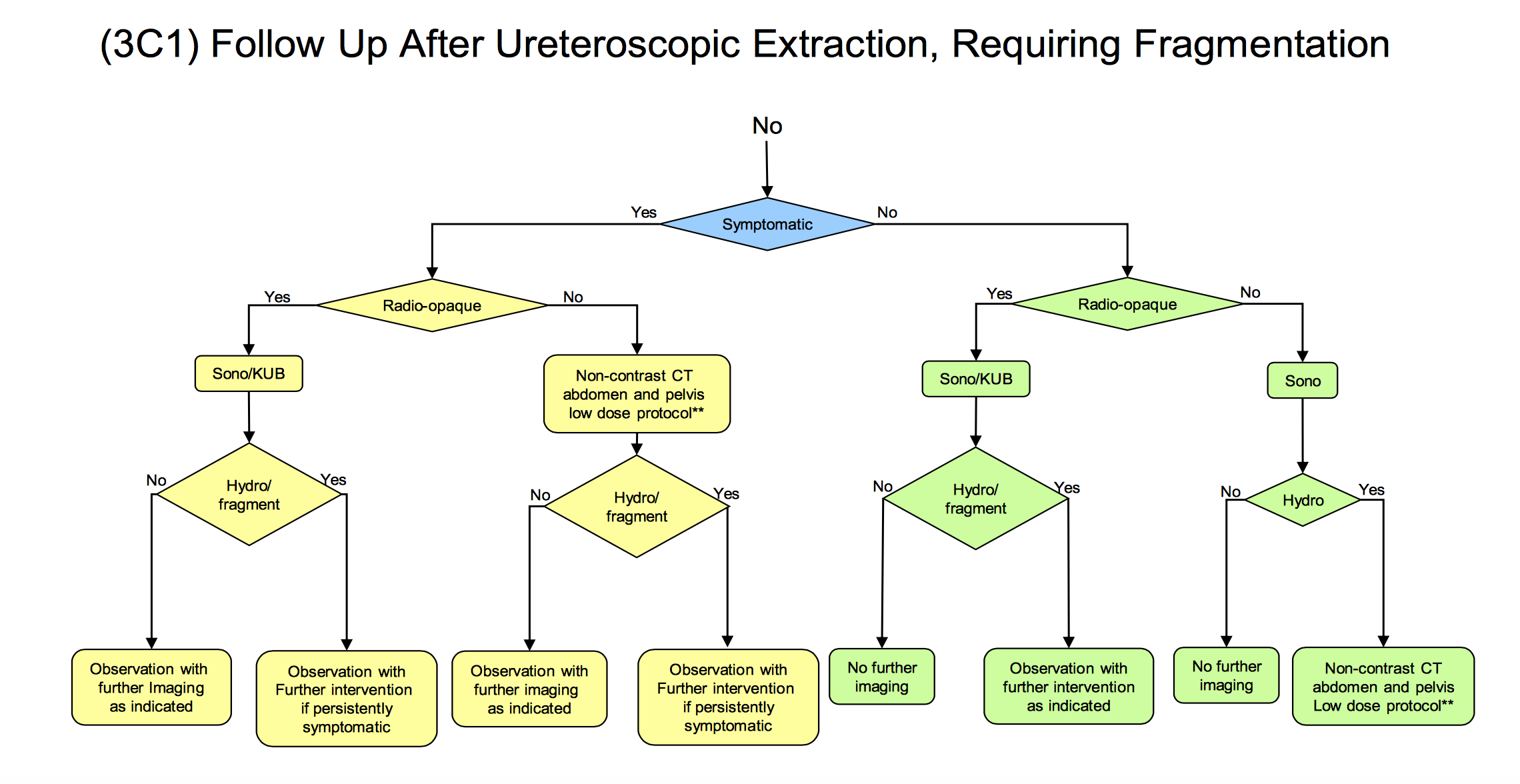
Follow-Up After Ureteroscopy
Oftentimes urologists will leave a temporary ureteral stent to prevent swelling of the ureter as a result of the procedure. This use of stents is a source of controversy worthy of a future post.
All agree one needs follow-up imaging of the kidneys to tell whether or not stones have been fully removed and whether or not a ureteral stricture (scar) has caused obstruction and kidney swelling (hydronephrosis), a complication that occurs 1-4% of the time.
Ultrasound Imaging
Ultrasound is relatively inexpensive, requires no radiation, and offers very detailed images of the kidney to determine whether or not there is hydronephrosis. But it is not very accurate at identifying residual stones, particularly small ones. It is also operator dependent and results can vary based upon the experience of the sonographer performing the examination.
KUB X-Rays
Ultrasounds are commonly combined with a kidney x-ray (commonly referred to as a KUB) which is also inexpensive and better at detecting stones with minimal radiation.The majority of published studies to date that have assessed stone free rate after ureterscopy have used KUB/US to determine the presence of residual fragments. Stone free rates using this imaging endpoint are commonly found to be in the mid 80-90%; even for large stones greater than 2 cm in size.
CT Scans
CT scans are the best test to identify stones, but are more expensive and are associated with higher degrees of radiation. Those studies that have used postoperative CT scans to identify residual stones demonstrate much lower stone free rates, commonly in the range of 50%. Interestingly the difference appears to be in the small stones <4 mm more likely to be seen on CT scan over KUB/US. If these stones are not taken into consideration, CT scan follow-up would otherwise be on par with that reported in the KUB/US series.
Although the question of whether KUB/US or CT is a better follow-up test is an important one, the more important question is whether or not routine imaging is being performed after the procedure at all. Despite recommendations by the American Urological Association that all patients should undergo at least a minimum of an ultrasound after ureteroscopy (see figure below) ,a recent study from the Cleveland Clinic found that fewer than half of all urologists routinely obtain any postoperative imaging whatsoever.
Take Away Messages
The goal of ureteroscopy should be to render the patient stone free
Regardless of the technique used, the ultimate goal of the procedure should be to leave the patient with no stones. Residual fragments are likely sources of future stone events. Therefore removing all stones should improve long term outcomes.
Urologists should be familiar with all ureteroscopic treatment techniques
Results of studies such as the EDGE group comparing dusting and extraction will determine the gold standard ureteroscopic treatment technique. In all likelihood though, we will come to realize that ureteral anatomy, width, and ability to pass an access sheath as well as the stone themselves will mandate one technique over another for any one patient.
Soft stones, for example, are more likely to fragment to true dust and thus may be more amenable to dusting. Harder stones are more likely to fragment into large pieces and thus benefit from active removal. Infection mandates complete stone removal, potentially harder to achieve with dusting. Alternatively dusting does not require an assistant and thus may be the only feasible option in instances where extra help is not available.
The ureteroscopy should not be the end of the story
Nephrolithiasis often manifests as an acute event ending in ureteroscopy; however, it is increasingly recognized as a chronic condition. As such, it is critical that surgery to remove the stone is not the end of the relationship with the patient.
Residual stones commonly lead to clinical events greater than one year from the time of the initial procedure including growth, passage, and need for retreatment.
Stone disease is chronic and recurrent, and the least desired outcome is formation of new stones after stones have been removed. As many as 50% of first time stone formers will recur within 10 years highlighting the significance and potential benefits to dietary counseling, metabolic testing, surveillance imaging, and other practices to prevent and detect stones over the long-run.
The main thrust of this entire site is toward prevention, before surgery is ever needed and with especial need after a successful surgery so that another need never be performed.


I found your site very helpful. I just had a ureteroscopythis afternoon and am very interested in follow up care. With so much conflicting information on the Internet these days, I feel that your site contains solid, objective information which helps kidney stone sufferers learn more about their condition
Hi Emil, The main thing is prevention. The stone should be analysed and you want to get proper evaluation and then treatment. This overview article is a reasonable introduction. Regards, Fred Coe
This is a very informative article and explains what sick people really need to know. I might add, Dr. Portis has a
You Tube video showing a utererscopy
I know he is one of the top endourologists in the US and is respected by his colleagues.
Trish
Thanks, Trish; I am sure he is. Regards, Fred
A recent CT shows two “tiny” fragments remain from a recent dusting I the right kidney. And a 3 x 9 mm stone in the left which has moved since the CT done three months ago and is causing hydronephrosis. I am very concerned about the remaining fragments and what can be done to prevent another such painful procedure.
But I also concerned about the shock wave lithotripsy scheduled in ten days. I have a lap band in place. I have asked if this is a problem and the answer is no. But considering the shock wave technique and the lap band position is there a reliable answer? Is damage a real possibility?
Hi M, Dusting has the virtue of no sheath, but remnants are not rare. Perhaps URS could be an alternative for the left stone if you are concerned about SWl, but I know of no instances in which SWL has interacted badly with banding. To be sure, perhaps you should speak with the surgeon who did your banding, as that person should know if SWL is a risk. As for the fragments, very often they are small enough to pass, and will. Several of the trials have shown that potassium citrate can reduce fragment growth. Regards, Fred Coe
I had ureteroscopy done twice in a 4-week span and I am deeply regretting it. The first procedure was aborted when the doctor perforated my ureter…oops! butterfingers! The second procedure just shattered the stone and left me passing out huge chunks and in pain. The only way to be absolutely sure the whole stone is removed is to do the actual percutaneous surgery.
Dear Jim,
I am sorry to hear that your recent surgical experience did not go as planned. You are correct that in general a percutaneous approach does have a higher success rate in complete removal of large and complex stones; however, this approach is typically more complex as well and does carry with it higher potential for bleeding and other complications. As our experience with ureteroscopy evolves, both in technology and technique, we are hopeful that we may one day be able to achieve complete stone removal each time in the most minimally invasive of fashions. For the time being however, a unique strategy must be determined for each patient and each stone to balance the risks and benefits of each approach we have to offer (shock wave lithotripsy, ureteroscopy, and percutaneous nephrolithomy). Choosing the best approach depends on several factors including overall health, the size, shape and location of the stone, and the comfort level of the surgeon performing each technique. Perhaps this would be a good topic to discuss in a future article.
Hopefully you are through the worst. Make sure you save a piece of stone for analysis if one has not already been performed and please wander through the rest of the website to learn how to best prevent a new stone from forming in the future.
Sincerely,
Mike Borofsky
I underwent ureteroscopy for the first time September 8 2016. This after having done ultrasonic lithotripsy in August 2015. I have a 9mm stone plugging my right ureter, and severe hydronophrosis. The doc was unable to get to the stone the first time, and he put a stent in to allow my kidney to drain for three weeks. Going in for a second time on Sept. 29th. Not looking forward to it at all, the pain afterwards when you wake and need to pee is intense, to say the least. Feels like you’re peeing razor blades. Sucks. Hate having to do it a second time, dreading it to the NTH degree. And the stent has caused me to practically live in the bathroom the last three weeks, pissing my insides out. Occasionally, it still hurts, even after almost three weeks, and I still get bloody urine after almost three weeks. I hate this!
I have a vial with a bunch of stones I passed in 2015, most are dark in color. Showed them to my urologist, and was surprised he did not want to take them from me to have them analyzed. You would think he would want to do that, so I can figure out what strategies to use to stop them in the future. Been making stones since 2001, when I had my first occurrence. Had none again until 2009, but had no insurance and had to live with them. When he gets this large one out of my ureter, I certainly hope he tries to determine what kind of stone it is. After the ultrasonic lithotripsy in 2015, wouldn’t they have had the ability to get some samples of the fragments since they had a catheter inside me throughout the procedure?
I’m reaching the end of my rope here. At 55 years of age, I do not want to have to have this procedure done on me again, it’s a horrible experience. If I have to look forward to stone removal every year or so, I may not desire to go on for much longer. It’s painful, even after three weeks. Disrupts your life for the entire time the stent is in place. Looking at six weeks now, since he will probably stick another damn stent in me after the procedure on the 29th. And what if he still cannot get the stone the second time? I’m frightened even contemplating that!
Hi Robert, You are right. Analysis of the stones is crucial as is an organized approach to stone prevention. I would have your personal physician get them analysed and help you through the steps in the link or refer you to someone who can. Urologists are busy surgeons and often do not have enough time to deal with the prevention problems. Given the numbers of stones and procedures you do need to insist on proper prevention efforts and stone analysis is essential. Regards, Fred Coe
Well, went in for a second ureteroscopy yesterday. Once again, my doctor was unable to gain access to the stone with a laser to break it up. This is really hard on me. He is going to try ultrasonic lithotripsy through my belly, since he will not be able to get it from the side. Says it’s been done before, and is hit or miss if it will work.
Told me my options if he cannot get it out, are pretty limited. I could just forget about it, let the kidney die, and go on with my life, it would cause no risk. Told me they could surgically remove the part of my ureter that the stone resides in, but it is a very tricky surgery repairing such a small internal organ such as a ureter. And told me the best option is to remove the kidney and go on with life.
I’m torn. My left kidney has never had a stone, always my right. But, my urine has the ingredients for stones, obviously. So, remove my right kidney, the stone problem goes to my left kidney, and I have no further backup. Scary. The stone plugging my right kidney gave no really bad indications it was this bad. Thought it was just another stone that would pass. Ended up with Severe Hydronophrosis, and a really damaged kidney. It has, because of the stent, returned to normal size. And I believe, due to the urine color after the stent was installed, I believe it is functioning normally.
I really hate to lose my kidney because my doctor is unable to get the stone out. I’ll give the Ultrasound a try, I’ve no other choice.
Doctor Coe, will this work?
Hi Robert, Given that stones fill form on both sides I would not readily accept loss of a kidney and would immediately seek another urological expert. Perhaps your urologist might know about possibilities in your part of the world. I do not know where you live of if you can travel, but perhaps you might want to email me directly – this kinds of matters are perhaps no longer ideal in a public space. Regards, Fred Coe
My doctor has been doing this for many years. He came highly recommended. He said something about scar tissue from previous stone passage blocking his ability to get the laser on the stone. It is an almost 3/8 inch stone, and one has to wonder how that cannot be found.
I cannot find your email address on the site. I would gladly do that.
I’m in Midwest City Oklahoma, just east of Oklahoma City.
Obviously your personal physician is excellent and I am too far from the situation to say anything more than the most general of statements. Regards, Fred Coe
The Doctor you recommended called me last night, we spoke for about 10 minutes. He is going to try and obtain my CT scans and medical records from my physician here. I also have the CT scans available on two CD’s, one dated August 15 2016 and the other September 27 2016.
Hi, THanks for writing. I know as he copied me on his email. Good luck with the kidney. I hope you can keep it in good shape. Regards, Fred Coe
Dear Robert,
It sounds like you are in a challenging situation. Situations such as the one you describe are quite complex and while I am unable to definitively comment on your current treatment without your medical records I would certainly not jump to have your kidney removed unless this is an absolute last option. Whereas removing kidneys for stones was once common, modern techniques both in stone removal and urinary reconstruction have made the need for this very rare anymore. I would strongly advise you to seek a variety of opinions from regional experts, specifically those at an academic teaching hospital or with subspecialty training in endourology prior to considering this approach.
Sincerely,
Mike Borofsky
Doctor Coe has provided me with the email address of a Dr. Lingeman. I have sent him a pretty detailed email of my situation as it currently stands. Yes, I do not want to lose my kidney, not being the stonemaker I am. So, currently I am awaiting a reply from Dr. Lingeman. I’ll see what transpires after that.
Anyhow, my doctor is Stanford Law. His practice is in Midwest City Oklahoma. He has many CT scans of my kidneys, dating back to July 2015.
http://www.alliancehealthmidwest.com/physician/361186/G.%20Stanford+Law
Thank you for your reply. I appreciate it greatly.
Dr. Coe. On Friday the 21 October, the stone was broken using ESWL. Been passing lots of little teeny pieces since then. I have 3 ultra sound images, taken at various times during the process. In those, the dark spot in the cross hairs is there in image 1, smaller in image 2, and gone in image 3. This ESWL was done through my abdomen instead of the side. And it appears to have worked well. My sister, who took me to the place, said my doctor was only in the surgery room about 20 minutes. I’m kind of amazed it took so short a time to break that large of a stone.
Still have a stent in place, and don’t understand how the pieces are getting out, since the urine flow is entirely through the stent? How could pieces midway in the ureter be getting out with a stent still in place?
Hi Robert, I am glad it worked. Usually the fragments are small and pass though the lumen of the stent. Regards, Fred Coe
Yes, I’m am getting many many teeny pieces that you need a magnifying glass to see. Yet there are enough of them to make a stone about half the size of the one that was in me, so far. Some are whitish, some black or reddish.
Question: I know we have crystals in our urine. Could some of these pieces I am seeing be those crystals? Or are the crystals too small to see, even with a magnifying glass?
If my doctor is looking out for me, he should want me to get some “after” CT scans? Because the images I’m seeing on the three ultra sound shots he gave me, are really not convincing to me. But then, I’m no expert on reading ultra sound images either. 😉
Hi Robert, BE sure and get the material sent for stone analysis. Modern instruments will identify the crystals easily and that is crucial for ongoing prevention. An after low radiation CT is a good approach, and invaluable for monitoring prevention. Regards, Fred Coe
Stent was removed today after 8 weeks of having one in me. Hurt like hell when he pulled the strings and took it out. Anyhow, I’m experiencing some side pain, nothing too terrible, but I don’t want to feel this for two more days. Also passing larger stone fragments now that the stent is out of the way. I’m confident from that, the stone is gone and my right kidney must be functioning normally.
Hi Robert, thanks for adding this. I hope things are just going to resolve perfectly. When they do, be sure you have a good prevention program in place as soon as possible. Here is a good plan in case you have not seen it before. Regards, Fred Coe
Hello. Great article. I am working on a research report and it involves the number of ureteroscopy procedures performed every year. Do you have any idea how many ureteroscopy procedures are done every year in the USA? Are there other types of procedures (besides kidney stone removal) that either treat the ureter/kidney that is done minimally invasively through the urethra?
Hi Nick, For that kind of detail, I would contact the primary author who is a urologist – Mike Borofsky. He is now at U Minnesota in Urology.
Thank you! I’ve reached out to him directly via email.
Dr Coe – Also, the project I am working on is with a large hospital in Miami. Please let me know if you would be interested in a summary on our idea and I can reach out to you directly via email.
Hi Nick, Sure, but I am not a urologist – Mike is. Regards, Fred
Hello Doctor,
I recently had a ureteroscopy performed for a supposed kidney stone. It turned out to be a pelvic phlebolith and they stopped the procedure. I am a young and healthy female, yet ever since the procedure I have experienced numbing pain on my clitoris and labia. Is is medically possible for a procedure such as this to cause nerve damage or lasting damage of any kind in those areas?
I greatly appreciate the help!
Hi Maria, I am afraid I am not a surgeon and not properly trained to answer your question. Possibly, being so close to where the scope enters you may be having some local and hopefully short lived symptoms. If they persist the first person to discuss this with is your surgeon who is most likely to be helpful. Regards, Fred Coe
Dear Dr. Coe.
First, thank you for your making such a wealth of information available to kidney formers like myself. I passed several small stones 18 months ago that were determined to be primarily Calcium Phosphate. Recently I passed a Calcium Oxalate stone and had a number of other stones removed that are being analyzed as I write this note. A CAT scan shows a remaining stone in my left kidney (approximately 4mm) that I would like removed via the flexible uteroscopy technique. It is not yet available in my rural area. I can travel to San Francisco or Los Angeles area with equal ease. Can you recommend surgeons capable of providing a flexible ureteroscopy procedure to remove the remaining stone? I have joined Jill’s Facebook group and will enroll in her next stone formers education class. Many Thanks for all you have done, and are doing, to help. Regards, William Bailey email: swbailey3@gmail.com
Hi Shelfield, UCSF has a superb surgeon, his name is Marshall Stoller. I would advise you call him. Feel free to say I personally recommended him to you – he is not only superb surgically he is a friend and colleague of mine in kidney stone research. Regards, Fred Coe
I have been diagnosed with a 7mm stone in my Right kidney (CT scan showed between renal pelvis and lowest calyx). I am weighing my options as to whether to do a ureteroscopy or SWL. I know SWL lithotripsy is less invasive but I am a little worried about the damage it might do to my kidney and or other organs, especially pancreas. I read some article which said there could be some long term damage to organs. I have type II diabetes and even the notes handed out to me by the Dr’s office about SWL said there could be 30-40% increase in the risk for diabetes. I certainly don’t want my diabetes to get worse and or have any long term damage to my kidneys, pancreas or any other organ as a result of SWL. Then there is the question of the efficacy of SWL due to the location of the stone and well as the fact that they can’t seem to spot the stone in a Xray. Due to the above reasons I am leaning towards ureteroscopy. Can you comment on the effects of SWL in terms of long term damage to organs (especially pancreas and kidney)?
Hi Nihal, A single stones that size can be disrupted by SWL or removed via URS. From a single treatment little evidence supports important disease in the pancreas. Overall, URS may be preferable if the stone is hard to see. This is an area where the surgeon doing the work is the best authority. Regards, Fred Coe
Dear Dr. Coe.
Thank you for the response. Like the concept of ureteroscopy, but dreading the stent aspect of it.
1. Are there techniques to better visualize stone during ESWL? I’ve heard terms like intravenous pyelogram. Can this be used during the ESWL to target the stone?
2. I took a closer look at CT. in the coronal view I see one bright spot (~7x7mm , 450 average HU) and in the adjacent plane, very close to the first one another bright spot (4x4mm, 350 average HU). In the axial view, it is one long, thin bright spot (11×2.5mm, 330 average HU) . So I am guessing one stone, long and thin in the axial view and much wider in the coronal view. Based on the above, how small do you think the average stone fragment sizes be after ESWL? 1mm, 2mm, 3mm or bigger or even smaller?
3. Location of the stone is another concern, CT scan shows it is between renal pelvis and lowest calyx (more biased towards the latter). I feel that the stone fragments after ESWL will fall into the lowest calyx. Would they come out on their own or would I have to do a subsequent ureteroscopy anyway to get these stone fragments out?
Thank you very much for the great service your are providing
Nihal
Hi Nihal, You are asking me things I cannot answer as I would have to see the images themselves. Even so, your surgeon is the key person, and I would bring these issues directly to him/her. With ESWL fragments do often lodge in the lower pole. I like ureteroscopy more because a stone free kidney is the usual outcome, but once again your surgeon wants a stone free kidney for you and may well have reasons to choose the modality, reasons I cannot know from so far away. Regards, Fred Coe
Dear Dr. Coe,
Thanks for the response. Based on the average HU density of the stone – 450 HU for part of the stone and 350 HU for other part of the stone (see more details above), can you say whether this is very likely to be an Uric Acid stone or not?
Thanks
Nihal
Hi Nihal, Low density like this is likely to be uric acid, but when very small stone density can become uncertain. The issue does matter. If uric acid it can dissolve and that would make surgery unnecessary. Have you done 24 hour urines? If so, is your average urine pH below 5.5? This latter is crucial for it not below 5.5 uric acid is most unlikely. Regards, Fred Coe
Dear Dr. Coe,
Thanks for the response. I haven’t done a 24 hr urine yet, but will get one done soon. Urine pH seems to be below 5.5 from the spot checks I am doing at home, plus I am a type 2 diabetic.
Let me introduce a twist. What about if there is blood in the urine? I have had visible blood in the urine in the recent past, but lately the urine has a yellow tinge (in spite of all the water I am drinking), so I am pretty sure there is some blood in the urine. Would this skew the urine pH? Do I need to subtract the pH effect from the blood (I am not sure if there is even a way to do this), or is it the composite urine pH with blood that I need to worry about? I would assume that the stone formed before it started bleeding, so if we were looking for a root cause we would have to subtract that effect. The confusion arises if the composite pH value were to come above 5.5. If the composite pH came below 5.5, then I would think the pure urine pH would be below 5.5 as well.
If I need to compensate for the blood effect, is there some extra parameter I need to request in the 24 hr urine test in order to do some calculation to subtract that effect?
Thanks
Nihal
Hi Nihal, diabetes will lower urine pH and famously causes uric acid stones. Blood has so little buffer capacity in the amounts present in urine you can ignore it totally. Just do the urine and see what is there. Regards, Fred Coe
Hi Nihal, diabetes will lower urine pH and famously causes uric acid stones. Blood has so little buffer capacity in the amounts present in urine you can ignore it totally. Just do the urine and see what is there. Regards, Fred Coe
Hi,
I was just hoping to post numbers from recent 24-urine test and see if Dr. Coe sees anything that jumps out. I am scheduled to have a ureteroscopy on Thurs. to remove about 10 stones from my left kidney – several of which are in the 9 mm range. I’ve had these for at least four years. Tried lithotripsy four years ago – which didn’t work well. (biggest stone wsa 5 mm back then). Then decided to leave it alone until discomfort in recent weeks. We don’t know what kind of stones other than likely calcium (according to my urologist because they show up on the xray.) Does anything look odd here? The doctors I’m seeing don’t see anything obvious. I notice my ss caOx is LOW and Creatine slightly high but that’s all I see that raise questions. Any help you can offer is appreciated.
Component Results
Component Your Value Standard Range
VOLUME, URINE 2.17 L/day 0.50 – 4.00 L/day
SS CAOX, URINE 2.40 6.00 – 10.00
CALCIUM, URINE 77 mg/day 0 – 199 mg/day
OXALATE, URINE 27 mg/day 20 – 40 mg/day
CITRATE, URINE 941 mg/day >=551 mg/day
SS CAPHOS, URINE 0.20 0.50 – 2.00
PH, URINE 5.895 5.800 – 6.200
SS URIC ACID, URINE 0.69 0.00 – 1.00
URIC ACID, URINE 0.598 gm/day 0.000 – 0.749 gm/day
CREATININE, URINE 1445 mg/day mg/day
SODIUM URINE 115 mmol/day 50 – 150 mmol/day
POTASSIUM, URINE 64 mmol/day 20 – 100 mmol/day
MAGNESIUM, URINE 49 mg/day 30 – 120 mg/day
PHOSPHORUS, URINE 0.724 gm/day 0.600 – 1.200 gm/day
WEIGHT 54.4 kg kg
CREATININE/KG 26.6 mg/kg 15.0 – 20.0 mg/kg
CALCIUM/KG 1.4 mg/kg 0.0 – 3.9 mg/kg
CALCIUM/CREATININE 53 mg/g 0 – 139 mg/g
AMMONIUM, URINE 31 mmol/day 15 – 60 mmol/day
CHLORIDE, URINE 129 mEq/day 70 – 250 mEq/day
SULFATE, URINE 30 mEq/day 20 – 80 mEq/day
UREA NITROGEN, URINE 7.65 gm/day 6.00 – 14.00 gm/day
PCR 1.1 gm/kg/day 0.8 – 1.4 gm/kg/day
CYSTINE SCREENING, URINE Negative Negative
Hi Raquel, These numbers and your story are consistent. The stones slated for removal have been present for 4 years or more and your lab data are all normal with low stone risk. I suspect your stones formed in the past when your urine chemistries were quite different. I am not sure why surgery is now being done, but be sure all material removed is analysed to find out what you are forming – or have formed. Possibly much of what is seen is in the kidney tissue. Regards, Fred Coe
Thank you for the response, Dr. Coe. So it turns out I had the procedure yesterday. Urologist was able to remove seven of the 10 stones in my left kidney. THREE remain imbedded deep in the kidney tissue. Can I expect these will cause problems there? Thanks again.
Hi Raquel, The imbedded stones are probably either plaque or tubule plugs. Your urologist knows which. IN neither case will the material itself migrate. But if plaque new stones may form in it; likewise if plugs. Your surgeon could not have removed these without damaging kidney tissue. Regards, Fred Coe
Dear Dr. Coe,
So on the Feb 28 reply, you had recommended I do a 24 hour urine to check my pH (among other things). My urologist says he will order 24 hour urine, only after surgery. I would like to see if I can melt this before doing any surgery, because my average HU densities are 350 and 450 HU (see earlier post) and my home pH measurements are below 5.5. So I got my family Dr. to order the 24 hour urines. I have some doubts as to whether he ordered the right ones to get all the info that is needed for a full evaluation. Following are the tests he ordered. Can you confirm that this covers everything including pH, SS values, and any other data that is needed for a full evaluation for any kind of stone? If these are not the right ones what should he have ordered? I would appreciate if you can respond quickly since I would like to start the collection process as soon as possible. I am in Illinois USA.
1. UR 24 hour Calcium
2. UR, oxalate 24 hour, MAYO OXU
3. UR 24 hour uric acid QUANT
4. UR 24 hour creatinine
Thanks
Nihal
Hi Nihal, No they are not related to uric acid stones as there is no pH. Likewise, most physicians order kidney stone panels – complete arrays of testing that bundle pricing so as to get the most from what you pay. Quest and LabCorp offer these. You do not know the stone type either, because HU are only approximate. More: I am far from your care as I know nothing except what you have sent, and I fear becoming an intruder. Might I recommend that before the surgery you seek a second opinion at a recognized university based kidney specialty program, just to be sure of everything. Regards, Fred Coe
Dear Dr. Coe,
Thanks for the response. Is the following the right test from Labcorp?
http://www.labcorp.com/test-menu/30091/kidney-stone-urine-test-combination-with-saturation-calculations
With regard to a recognized university based kidney specialty program, would you be able to recommend a Dr. in the Bloomington, IL, Decatur, IL, Peoria, IL, Champaign/Urbana, IL, Peoria, IL, Springfield IL. areas?
Thanks
Nihal
Hi Nihal, If it is LabCorp you want their Litholink product. It is more polished and priced the same. I looked on the map and you live in an unfortunate place. You are about equal distance – and considerable – from our center in Chicago and the other center in Indianapolis – but the INDY one looks easier to get to. One or the other would be right for you. If it is INDY, let me know and I can help make an introduction. If Chicago is not too hard, the same. Regards, Fred Coe
Dear Dr. Coe,
Actually Chicago is closer to me. Whom do I contact to setup something? Do I get to see you or someone else? As you might understand, I would have to investigate the affordability, since I am pretty sure my insurance won’t cover the bulk of it, since you would be considered “out of network”.
Thanks
Nihal
Hi Nihal, Kathleen Dineen can make all arrangements: 773 702 1475. She can also help with the financial issues. I would see you myself. Regards, Fred Coe
Thank you, Dr. Coe. So what might that mean for my diet? Any specific plan I should adhere to at this point?
Hi Raquel, As I remember your lab data results were normal and it seemed your stones might have formed in the past. I would have a new 24 hour urine when you are recovered from surgery and of course have the removed stones analysed. If results of the urine remain normal merely maintain a high fluid intake. But it is your physician who is in charge and what I say is from a great distance and merely commentary. Regards, Fred Coe
I had a ureteroscopy with laser 12 days ago. Doctor said they had to blast the stone first ( 5mm x 4 mm) and remove the pieces. This was my 2nd ureteroscopy as my first was 6 years ago from which I had a quick recovery. This time I am having a MUCH tougher time. Stent was removed after two days which was the most painful and horrifying two minutes of my life and I have been through 40 stones in my life so I know pain well. Since then, I have periodic but brief sharp pain when sitting on hard surface or bending over. Also have pain every single night for last 10 days when the area of the surgery “wakes up and stretches out”. Any attempt at activity with my wife is also painful. My urologist last week just said “give it time” and I should be fine. Is such pain normal for some patients or should I see a new urolologist ? I’m fearful of this never healing if something happened during surgery.
Hi, I suspect your urologist is right and things will gradually heal up. But 40 stones is so many, you should really push at prevention. If you have not seen it, here is a good plan. You should not need to make so many stones – even any is too much. Regards, Fred Coe
I have a 10mm kidney stone on my left kidney towards the bottom of the kidney… scheduled to have lithotripsy… so I have anything to worry about? I am healthy otherwise… just worried about trauma that might be caused from the shockwaves, Afterwards the Dr. told me to drink lots of water and stand on my head! for awhile so that the stones flow upwards and leave the kidney.
Hi Maria, with one 10 mm stone SWL is certainly reasonable and damage from a single treatment is not considered an important drawback. As for standing on your head, that is pretty athletic! Some risk there. Be sure to analyse the stone material, and be sure to pursue prevention so more do not form. Regards, Fred Coe
My wife had a kidney stone removed via ureteroscopy but the Urologist neglected to remove 2 other stones 5mm in size that he informed my wife may or may not cause issues in the future and that he could do the procedure again to remove them. I have developed a major anxiety as a result of this and wanted to accompany my wife into her next procedure to remove them. So far I have been stonewalled to the extent my wife doesn’t even want to try. Is there a facility in North America that will allow a family member (spouse) to observe the procedure thereby significantly reducing the stress on the patient and the spouse. We live in Edmonton, Alberta, Canada but are willing to travel anywhere in North America to have the process done with me ( her spouse) in attendance. Thank-you
Hi Kerry, In general the OR is not a good place for spouses. But also, if one asks for all stones to be removed one can expect that to happen. If you can travel in the US and get care, I can help you find very high quality surgeons who will render kidneys stone free. Just let me know. By the way be sure she is getting preventive care; nothing is more unnerving than new stones to replace the old ones. Regards, Fred Coe
Is it possible to arrange for a spouse to go into the OR under certain circumstances. Lithotripsy is also an alternative but it has also been moved into the OR in Canada further restricting my access. I have been present for a lithotripsy 30 plus years ago when it was first introduced. I have been looking at numerous studies and medical papers as of recently and have found that have a family member present during the procedures is healthier for the patient and their family member, significantly reducing stress on both parties and reducing recovery times. The main caveat on this is that Physicians are uneasy having a family member present which has be identified as the prime reason procedures have been placed behind the facade of the OR. It is this reason that the battle currently exists between patient’s rights to choose who is in attendance and the Physician’s personal feeling of angst. There have been many comments of anxieties of spouses that have made the procedures more difficult for the patient. I thank you for your response to my query. It appears that I have a long road ahead of me in my search. I have started searching in the UK where some of the family presence studies have been conducted. Patients and their families shouldn’t have to undergo this pain for a procedure that has no clinical bearing on who is in the room.
Hi Kerry, You raise an interesting question. Having been in many OR sessions as a physician with my own patients, I can offer a few ideas. They are busy and crowded places, and the staff needs to speak to each other and work with as little friction as possible. If there is anaesthesia, the patient will not know who is there. With lithotripsy it is perhaps less of a problem. How about as a compromise you might ask to watch the live video? Of all my concerns the worst might be distraction of surgeons that lengthens OR time and anaesthesia time for the patient. Most surgeons, by the way, and proud of their technical abilities and all to happy to demonstrate and converse. Good Luck, Fred Coe
I have been in my wife’s lithotripsy in the past and 3 colonoscopies and the surgeons that provided the procedures had no issues in me being there and exuded a great deal of confidence in their abilities. In each case my wife and myself were both relaxed prior to, during and after the procedures as we weren’t anxious with the support given to each other. Having a surgeon feel distracted while performing a procedure with a spouse present would have me questioning their confidence in their own abilities. Coming from an Engineering career scenario (I am not a professional Engineer), the best engineers I have found welcomed the presence of an observer of their work as it provided them the ability to present their capabilities. Those that didn’t like having an observer generally felt they were being tested and were generally the ones that made the most errors of which I had to go in after to correct. As far as my ability to manage the activity on my wife which would possibly be an issue, I would have to say that strengths in that area could match any nurse or physician in the OR as I have seen some major blood and gore on family members in a hospital ER’s over the years.
I would like to thank you for listening to my comments and providing input. My wife has decided at this point to do nothing and hope for the best.
Hi Kerry, I hope everything works out just fine. Best, Fred Coe
I am a 60 year old female, overweight, but generally in good health, low cholesterol (170), no diabetes, excellent blood pressure, I do water aerobics several times a week, more in the summer. I have had a seizure disorder since I was small child controlled by medication, no seizures in 30 years. In 2009 my neurologist switched me from dilantin to topiramate 400 mg daily. One of the side effects of topiramate is the formation of kidney stones and I believe this is because it seems to suppress my thirst. I have to force myself to drink. I am never thirsty, I don’t drink soda, coffee, much of anything. In 2011 I developed my first kidney stone, 6mm, which was dusted and removed with the ureteroscopy and stent procedure. I became a regular customer, every 2 years 2013, 2015 and now just yesterday, Sept 20, 2017! I have a new urologist who told me that I need to change my diet because my stone is an oxalate stone. I “thought” I was eating healthy-lots of whole grains, dark leafy greens, fruits and vegetables, nuts, all of which seem to be full of these oxalates! After reading this article I still plan on changing my diet but I wonder if I am just the perfect storm for these stones. The topiramate, the lack of liquids, the residual from the dusting, the previous diet. My last stone was 9mm. I have no family history of these at all but would appreciate any insight.
Thanks
Jan
Hi Janet, I am afraid the cause of stones with Topiramate is not reduced fluids but inhibition of renal carbonic anhydrase leading to renal tubular acidosis and calcium phosphate stones. It is the drug and the drug must go. All the diet changes will not protect you. Change the drug. Regards, Fred Coe
Hello Dr. Coe,
I am a 67 year old male in good health. I have asked my urologist to remove my
kidney stones 5mm lower pole,2mm mid pole right kidney and 3mm midpole, 2mm
and 1 mm in left kidney midpole. I am being proactive because I let a 3 mm fragment from a
previous lithotripsy grow to 1.2 cm back in 2008 and the removal in 2009 was difficult.
However, my Urologist wants to do both simultaneously and I am concerned that the
post operative stents could be an intolerable experience – one is difficult enough – any
studies on bi lateral ureteroscopy success rates compared to single.
Hi John, I am not a urologist so I cannot provide the statistics. My conjecture is that success rates will not be influenced by one or both sides. About discomfort, your urologist can be perfectly clear. The advantage is one anaesthesia session. Regards, Fred Coe
Five years ago I had lipotripsy which did not break stone small enough to pass. As a result, my urologist had to do uretoscpy surgery, seven times in seven month to retrieve them.
I now have been informed that that kidney has atropic iced and shrunk in size to the size of
Of a bean. I am now being told I have stage 3 kidney disease. Do you think all those Ureterscopt surgeries back to back have caused this.
Hi Charles, I cannot make any judgement of this without reviewing all of the images and operative reports – that is not possible outside the purview of actual clinical care. But I can say that having one kidney greatly increases the importance of stone prevention, so I would pursue it with vigor. Here is my best suggestions. Regards, Fred Coe
Hi Dr. Coe
I’m 53 yo male. Diagnosis showed there’re 3 stones in the right kidney(no symptoms but some blood traces in urine lead to the finding). My Urologist recommended SWL first and performed it on Jan. 2017(maximum force , 1 hr duration) but showed no impact. Prior to this procedure, creatinine is 0.88, eGFAR is 108. Than he recommended Laser lithotripsy and performed on Feb. ( I think he’s using dusting method, it lasted about one hr from the x-ray time stamp). He’s not able to get all stones and some stones moved after break up that he’s not able to catch. Stent being left for 5 days and removed. No follow up image being performed and he refer me to see his colleague who is more stone specialized. 6 weeks after the procedure, my family doctor ordered lab report and showed that the creatinine is 1.48, eGFAR is 55. Further ultra sound showed severe hydronephrosis. ( I felt few times the lower right flank pressure/pain for 2-3 days after the stent removed , the Dr. office stated it’s normal and advised to take Motrin). The colleague Dr. not able to get trough the ureter due to the blockage( he’s not sure it’s stone or scar tissue). He referred me to see local medical school faculty and identified cluster of stones fragments embedded in the ureter and UPJ area. Nuclear image showed 20%/80% split function. I like to know your opinion about how is this possible happened ? Have you seen a clinical case like this ? Thanks. -Sherman
Hi Sherman, Of course we all have seen obstruction from stones lead to loss of function of the obstructed kidney and therefore reduced total kidney function. I am sure the university urologists will clear up the obstruction as soon as possible in hopes of preserving that kidney. Unfortunately given what appears to be an interval of many weeks of obstruction that kidney may not regain its original function. Let’s hope for the best possible outcome. Regards, Fred Coe
Hi Dr. Coe
Thanks for the prompt reply. As you indicated that the university faculty urologist remove a lot of stone fragments from the ureter through PCN back in June. The function stay as it is now from nuclear image and keep monitoring it. The question is how’s that possible of a common laser lithotripsy turned into fragments embedded in the ureter and cluster on UPJ ? If I had known the risk, I’d either go for PCN or leave as it is. Neither able to google out a case like this.
From the laser lithotripsy to the nuclear image function check is about 14 weeks. Can the kidney function really degrade that much from the obstruction? Odd is that I did not have symptom. If not because of a regular annual physical lab checkup, worse even could happen. Thanks.
-Sherman
Hi SHerman, Sometimes fragments occlude the ureter without pain and kidneys are obstructed and lost. You were lucky your physicians found it. Regards, Fred Coe
Dear Dr. Coe,
As a result of an incident where a significant amount of blood was discovered in my urine (witnessed by me 5am in the morning – about 1pm in the afternoon of the same day when I would urinate) my urologist has recommended a Ureteroscopy be done to more fully reveal an abnormality discovered in a CT scan for my left kidney. After her and two radiologists looked at the scan, it was difficult for them to determine if the abnormality they saw in the scan was simply a cyst or possibly a tumor. For background, in reaching this point, so far I have given urine (normal), a blood panel was done (normal) a CT scan of my bladder, urethra & kidneys (all clear except what I mentioned above) and today a cystoscopy (done today.. all clear). Though I have no detection of kidney stones, does the ureteroscopy seem like a reasonable procedure to have done to help reveal a partial unknown seen in the CT scan of my left kidney? BTW, the visible blood in my urine has not returned except for that one day (about a month ago). About 6 hours prior to the blood being visible, I had exerted myself jogging… not far.. just enough to be winded. Thanks – John H.
Hi John, Given unexplained bleeding, URS seems reasonable to look for a cause along the ureter or in the renal pelvis. Your physicians seem eminently reasonable and cautious about an important matter. I would do as they recommend. Regards, Fred Coe
Fantastic Site.
I’d appreciate your input.
I was recently diagnosed with a kidney stone; fully obstructing the left kidney; it took 6 months from diagnosis to operation (uteroscopy) (UK NHS) and post op, a stent was inserted for a week after.
Everything appeared fine, but, a month later, back and abdominal pain (akin to the start of a kidney stone episode), bearable, but, always there. Appears to be compounded by weigh bearing (e.g. walking, standing, etc).
Are there long term effects from such procedures?
Clinical team have suggested that kidney function test is pointless, as, what can you do if you find they are not working well…..
Hi Brian, I am sorry it took 6 months to cure an obstructing stone. Does that kidney still function? Usually one acts much more rapidly. As for this new pain, it could be just muscular, but given all of what has happened I would advise your physicians might want to do another CT scan and be sure about that kidney. Is it draining? Infected? As for kidney function, I am sure they measure overall function and it is adequate, and reading between the lines I suspect the obstructed kidney may not be so good. Regards, Fred Coe
Hello,
I’m 27 and I had my first kidney stone over the holidays. For the month of December I had lower back pain on my right side, which I ignored until the pain took a very sharp turn that sent me to the emergency room while on vacation. I was diagnosed with a stone, it was surgically removed, and a stent was put in place for about a week. After the stent was removed everything seemed fine; however, the backache that accompanied the earlier stages of my stone resumed a day or two after stent removal. It has now been a couple weeks and the pain is still there – somewhat similar to what the above poster expressed – bearable, but constant. I was very paranoid that I had another stone, the pain was just so similar to those early weeks (before it morphed into the hell that directly preceded my surgery). I’ve seen a urologist for followup and he ordered a CT scan that came back totally normal. I suppose my question is… could this possibly be just residual soreness/pain from the procedure and stent even after a month? My doctor doesn’t think so and at this point we are both at a loss.
P.S. Thank you so much for this site, it has helped assuage some of my worry. My mom has had an absurd number of stones (like, 30) and I am anxious I will be burdened in a similar fashion.
Hi Marissa, Given the family history and yours, I would worry about crystal attacks- pain but nothing seen. You need 24 hour urine and serum measurements, and stone analysis to know exactly what is wrong with you and fashion rational prevention. Here is a good article to help with that. If it is crystals, proper treatment will end them. Regards, Fred Coe
Dr. Coe: My daughter, 46, had a kidney stone removed which resulted in damage to the ureter. The Dr. told her about it, apologized, said there could be future complications but suggested nothing further. She HAS had to have several surgeries, the latest taking cheek skin from the inside of her mouth and sewing it on the ureter after laying it open. She was told today that this has also failed and her options would be to POSSIBLY move the kidney or REMOVE the kidney. We need VERY expert advice and information and don’t know where to go or how to go about it. We are in NM but will travel. She is scheduled for March 6th so we have no time to waste. Where would you go for help?
Hi Darla, The best surgeon I know for this is Dr James Lingeman at Indiana University in Indianapolis. Call him and see if he can fix it. Please use my name as we are friends and colleagues. We must not lose a kidney. Let me know by email if necessary, Regards, Fred Coe
Just had the same thing happen to my husband. Curious to know your updates on your daughter?
Dr. Coe.
My husband is 48. Just had routine 1st kidney stone removal from ureter.
The collection basket ripped the bottom 2/3 of ureter on exit. He was unaware of it until too late.
Waiting for answers.
1. Move kidney
2. Move bladder
3. Try to use ureter left and drain into other kidney. Risk of other stones…and ability to ever remove
4. Use bowel to reconstruct. But 50 % chance of having to cath 4 times a day.
And risk of alot of infections.
Almost seems best to remove kidney!
Ever heard of this?
Any other options?
Thanks for your feedback!
Hi, This is a serious and unfortunate outcome. I would ask your urological surgeon for advice concerning a second opinion from a specialist perhaps at a university medical school. Possibly such a person might have more experience with this kind of repair, or at least offer a second point of view. As I am not a surgeon, I cannot comment, but to move a kidney, drain into the other kidney, or use bowel are large changes in biology and one should be as sure as possible before moving forward. Regards, Fred Coe
I’m a 42 yr. old female. On December 7th, 2017, I had acute abdominal pain which sent me to the doctor on December 8th. The doctor could not figure out what was causing the pain, so I was wheeled down to the ER. In the ER they did an x-ray, and discovered that I had a “complete” Staghorn Calculus in my left kidney. I also had a UTI, of which I had no symptoms previously (which they told me is odd, considering the stone is typically formed by re-occurring UTI’s). I had an abundance of abdominal pain that didn’t make sense, so they did a CT scan as well. I had some ureteral swelling, but nothing else was abnormal. I had no flank pain at the time. I was observed overnight because of the inability to control the pain, and then discharged the following day. A couple days later, I started getting flank pain, and the abdominal pain lessened, other than in the area on front side of my kidney. A subcostal left percutaneous nephrolithotomy was performed on December 28th. The surgery was challenging as my urologist had to enter from the bottom of the kidney because it was impacted and he was unable to get in from the top where he initially made an incision. I knew prior to the surgery that he would most likely need to do a follow up surgery. A post op x-ray, which they did because they made an incision above my lowest rib, showed mild atelectasis in both lobes. I ended up getting a post op infection, was discharged prematurely (after a 4 day stay rather than the 1 day expected), ended up back in the ER the following day with pneumonia. I saw my urologist, had my stent removed, and a follow up surgery was scheduled for February 1, 2018. A urethoscopy with laser lithotripsy was performed on an outpatient basis and I was sent home with a self removable stent, to be taken out on February 5th. Recovery was going as planned, however the stent was much more painful this go around. The stent was removed without any problems, I had quite a bit of pain and cramping for the day that I took pain meds for. That night at 11pm I started getting the chills, took some ibuprofen and went to bed. The following morning I ended up going by ambulance to the ER because my fever was 103.1, I had altered vision, was shaking all over, whole body ached, and I was extremely nauseated. Sat in the ER waiting room for 7 hours (that’s a whole other story), and when I was finally seen I was diagnosed with pyelonephritis and sepsis and was hospitalized for 2 nights (pretty much 3 full days). I was extremely sick. While I was in the ER they did a CT, and is showed residual stone fragments. I was told I would need surgery again, but not immediately as they were not blocking anything. After talking with my urologist, he wants to take a wait and see approach because he says that sometimes the fragments appear bigger than they actually are on a CT because they like to clump together. He is hoping they will pass on their own. He is going to run a complete metabolic test, do ultrasounds, etc for the time being. This whole situation has been one disaster after another. When I left the hospital my symptoms had all subsided, but now the left flank pain is back, along with the nausea and now I’m having chest pain on the left side (which I’ve never had in my entire life). I do have some atelectasis still in my left lung, though it has improved. An ekg and chest x-ray came back normal other than the atelectasis. No fluid around my heart. The chest pain doesn’t correlate with breathing, so we’re not sure what’s causing it. Having surgery again is the last thing I want to do, however I’m concerned that my symptoms are back. What is your opinion of this treatment plan? My doctor is a well regarded stone surgeon and affiliated with a highly respected university hospital.
Hi Sarah, you did not say but implied the stone was struvite – made by infection, and your story suggests recurring infection. From this distance I can form no opinion about your proper surgical course as I have not read your CT scans, and know essentially nothing about your situation. If you have surgery no doubt it will be ureteroscopic stone removal. There is a risk of sepsis but given the excellence of your physician and the institution I am sure they can minimize that risk. An alternative is to consult at another center simply to obtain perspective before another surgery. No doubt your physicians will be delighted to help as all university physicians are when so asked and usually make proper referrals to peers. Regards, Fred Coe
Hello Dr. Coe,
I had lithrotripsy for a 5 mm stone Jan 14,2018. Four days later, I reverted to feeling as sick as I was prior to the procedure. I felt that a stone was travelling and then became stuck. My Dr did kub post of 1 week later,and due to MSK he dismissed my condition by telling me I would always have stones. I switched Drs,had a CAT done with findings of another stone in same side at 6mm. Dr wants to do ureteroscopy despite not able to clearly know it’s location in the kidney,if he can get to it or if it’s in the meat of the kidney. I was asymptomatic,and decided to wait. Now I feel that a stone is stuck close to bladder as my labia hurts,pressure,and urgency. When I turn or move gently,I feel a pinch on the treated side near the bladder. No ureteral stones were seen on CT. Could it be a fragment trapped in the juncture? If small,could it be missed on CT? Is ureteroscopy the only way to know?
Hi Elan, indeed it could be where you say. The choice of approach is for your surgeon but I imagine he/she will want to do ureteroscopy. Given your many stones, be sure and achieve prevention. Try starting here, as you made no mention of it. Regards, Fred Coe
Thank you Dr. Coe,
Yes, I have finally found a Dr that has put me on a stone prevention plan. It has taken 13 years, and for the first time I am feeling hopeful that it is possible. I have taken Jill Harris’s class which was most helpful. As I am a calcium oxalate stone factory from MSK and a pre diabetic, I felt challenged with meal planning. A dietician consult was very helpful with that. Most helpful has been the addition of a nephrologists who is very enthusiastic about stone prevention. He has put me on a low oxalate diet, continued the thiazide,added allapurinol,continued lemon juice in water, and added 325 mg ferrous sulfate at each meal.we will repeat 24 hour urine in 1 month after implementation of these changes. My last collection was : urine volume 2.47 , SS CaOx 10.98 urine calcium 296 urine oxalate 49 urine citrate 538, SS CaP 1.74 , pH 6.266, SS uric acid .53 urine uric acid .856. I do realize now that I’ve been eating all wrong , lots of whole grains and green high oxalate veggies though I was told a few years ago not to eat spinach,rhubarb,and watch sodium. My dietary sodium is good. What would be the reason for the ferrous sulfate other than I have cut my protein down to 5 1/2 oz daily? I understand that the ferrous sulfate helps prevent anemia.
Hi Elan, low oxalate diet is always a secondary thing – calcium is the first. Low protein diet is not important, the article is not quite ready but recent excellent research has greatly reduced interest in it. Your urine calcium is quite high and you are taking thiazide, so I suspect your urine sodium is far above ideal of below 100 mEq or better below 65 mEq. As for the iron, I do not know your details, you may have modest anemia or another sign of iron deficiency. Regards, Fred Coe
Hello Dr. Coe,
I am having almost the same problem as Marissa, but for some reason, I am unable to read your response. I went to the ER on February 28 knowing I had a kidney stone. I saw a urologist the next day who scheduled me for a ureteroscopy the following day. I’ve constantly had pain in my right kidney down to my bladder since surgery. I had to make another trip to the ER because the pain was so bad Sunday night. I also still have a lot of blood in my urine. My follow-up appointment was supposed to be for four weeks but now the earliest I can be seen is Wednesday. Any idea what may be causing the pain? Should I still have a lot of blood in my urine? Any suggestions to help deal with this pain?
Hi Maegan, If you have pain like this your physician needs to figure out why and fix the problem. It could be retained fragments, as an example. So the appointment is the right idea, as soon as possible. The blood and pain together would be common with fragments of stones. Regards, Fred Coe
Hi, Dr. Coe,
I am a 56 year old female. After 2 days of extreme pain went to the ER; found a stone 7 x 4.5 x 4 mm and say surgery was required for that size of a stone. Yesterday, they did a Left ureteroscopy and put in a stent. Tomorrow I’ll go back for surgery and hoping they remove the stone. After reading comments here and another place, I’m a bit worried. Are there any success stories? Thanks.
Hi Paula, Indeed I would not have devoted by life work to this disease, nor written this site, if stone prevention were a false hope. Here is a very good place to start – It will take you everywhere you need to go on this site to help find a way to prevention. Write back after a while and let me know. Regards, Fred Coe
Hello
Thank you very much for writing this.
My brother have had a uteroscopic removal of stones that were in the distal ureter two days ago, now he has more pain than before the procedure and is bleeding a lot half a litter a day he said, the doctor said he is going to be fine and will be ok in two days but he is so tired right now I think due to blood loss, what could be wrong or what can we do to prevent further problems?
Hi Zee, Given this was an acute problem I apologize for the late answer – out of town. I hope the bleeding stopped! Weakness can indeed come from blood loss. Hopefully all is not well. Regards, Fred Coe
I am travelling by plane and my doctor wants to do a kidney stone retrieval 2 weeks before. I am worried that if anything goes wrong or I need a stent, that my trip will be ruined. Should I postpone til after vacation?
Hi Robbin, It is a matter of judgement. A stone can always pass and cause pain or real urological interventions. Your particular stone may pose special problems. I would ask your physician if the latter is the case; if it is a routine precaution, perhaps you can judge if the risk balances the unpleasantness of a procedure. Regards, Fred Coe
My husband had a 11.7 mm kidney stone; a surgeon performed ureteroscopy to break up and remove the stone. Immediately after surgery, the surgeon told me that he was able to remove nearly all of the stone, that my husband may pass a 2 or 3 granules, but other than that everything went well. He placed a ureter stent to allow for healing.
The following day, my husband started experiencing severe pain and elevated white blood cells. He ended up being hospitalized for 9 days, and it wasn’t until the eighth day that a different surgeon explained to us that the ureter had been perforated and that there was a portion of stone remaining. He told us that my husband would need to have his stent removed, the stone removed, and a new stent put in place. We are currently awaiting this procedure, planned for 3 weeks from first surgery.
My question is why the original surgeon did not disclose this even though it is noted in two post-op ct scan reports. My husband was also seen each day by a hospitalist, infectious disease doctor, and a physicians assistant from the urology practice each day that he was in the hospital. The perforated ureter was never disclosed to us by any of these medical professionals. They acted as though they did not know why his white cells were elevated, or why he was in so much pain.
I am quite concerned about his follow-up surgery after this experience. It is to be performed by the original surgeon
Hi Angie, What a bad experience. Of course from this distance I cannot answer your questions well, but if you no longer have confidence in the original surgeon feel free to select another. Perhaps the one who pointed out the problem might be fine. Alternatively, ask your present physicians for a referral. This is your husband, and you have every right to do whatever is necessary to get him the best possible outcome. Ureteral perforation is not rare, incidentally, and may have been managed quite well despite the confusions; I cannot tell. Regards, Fred Coe
I was out of town and Experienced pain on my right side. Two CT scans found had two 4 mm stones lodged one in each tube. They eventually passed after I was given morphine during 2 back to back ER visits. There were small stones found in the kidneys. One urologist recommended surgery and another did not for one stone that passed soon after.
I returned home and just saw a urologist who told me Part of the stone the size of a pencil point is lodged in the bladder near the urethra opening and he is concerned about infection. He said he is not doing surgery but will use a scope with a camera and maybe a laser to remove it. Said I might have a stent that I can remove myself. Will have 3 day recovery. I am concerned as this sounds like surgery and he also assured me I could climb 3 flights of stairs after this procedure which would take 30 minutes. I have been drinking lemon water and watching my diet which I think helped dissolve the other stones. After reading the risks I am wondering if I should have this reportedly nonsurgical procedure.
Hi Linda, your urologist has made a good recommendation and you should take it. Digital scopes work well, what he said sounds about right to me. I am not there, so it is a guess, but he/she seems perfectly reasonable. Regards, Fred Coe
Passed my first stone within the last three weeks. Only symptom was blood in my urine. CT showed a 3mm stone in ureter and slight inflammation in kidney. Today’s x-ray showed all clear. Dr. still wants to do a ureteroscopy procedure because there was blood in my urine when I had the stone over a month ago. He said he does this anytime there is visible blood.
I’m concerned to have such an invasive procedure when I’m currently stone free. If it wasn’t for the reddish urine, I wouldn’t have known I ever had a stone. Is it always a mandatory procedure or should I seek a second opinion to possibly avoid a ureteroscopy. It seems like such a risk.
Hi H.J., It is; given blood urological guidelines call for URS to be sure nothing more is present than a stone. Your physician is correct. Be sure and pursue prevention; more can form and you can prevent them. Regards, Fred Coe
I had my first surgery two days ago to remove several stones from left kidney. No one mentioned to me how difficult the post-op period could be. The day before surgery, I weighed 187. The day after surgery, I weighed 199! Is that kind of water retention normal? (They did make sure I drank like a fish and I had three hanging bags of solution) I also have extreme abdominal soreness, not localized. I do, of course, have a stent and have been told it will be there for a few weeks. I am shocked and dismayed at the aftermath of what is called a noninvasive procedure. And I am to have another surgery on right side in near future. Is the post-op period normally this challenging?
Hi Bob, You are not alone. No surgery is minor, and after effects commonly very troublesome. So prevention is a premium. As for your particular course, I think you are about in the middle of what I see. Of course I am not a surgeon, and perhaps see patients with more problems than average. Regards, Fred Coe
My daughter has been diagnosed with a 1.5cm kidney stone. She has blood in her urine and in pain. She seen a Urologist yesterday and he gave her option to do the Lipotripsy or the Laser Dusting procedure. She needs to decide by tomorrow and we are just not sure which is the better route with such a large stone. Please help us decide . She is 31 and has a 3 year old and an 18 month old baby at home . She is very scared as she has never been sedated for a surgery before. Thank you for your guidance.
Hi Cindy, I vastly prefer ureteroscopy with laser dusting to SWL. Your urologist is excellent to offer both! Sorry I am a bit late in writing this, but you wrote just yesterday. Regards, Fred Coe
Dr. Cole, I have spent many hours reading your wonderful articles. I must also add that I appreciate all the art and the backstories that you have taken time to share. Thank you in advance for taking the time to read about my concerns.
I was an active 63 yr old woman three years ago when I developed a 6mm stone (mid pole in the left side) that was never collected. No further testing was done at that time because within a few weeks I had a series of back, leg, and foot ailments after being prescribed the antibiotic Cipro by my urologist. I believe that particular antibiotic resulted in my being partially disabled (using a walker) and in unbelievable pain for over eight months. I still, and may always, have daily discomfort and limitations. I have since found out that I have an MTHFR gene variant that makes me sensitive to some medications. Thousands of people have reported the horrible side effects of Cipro, Levaquin, and other similar antibiotics. I will NEVER take another antibiotic in the Fluoroquinolone family again!
Three years went by and I have not had any kidney stone symptoms until eight weeks ago. So back to the ER for a CT scan. This time it is a 5mm stone that is lower down the same left pole. I had mild discomfort and passed a very small amount of debris one month prior to being diagnosed with this stone. Could this be the same stone that just chipped away and moved farther down? Thank goodness there is no infection this time. Hopefully, I can get the answers I need to feel comfortable in moving forward.
My urologist wants to go in and break it up with a laser and pull out the pieces but I am not wanting to have general anesthesia because of my MTHFR issues. I would also like to first know if the stone is still there without having another CT scan so soon, and also because when I had this last CT scan (with contrast) in the ER I had a reaction to the dye resulting in painfully swollen salivary glands, so I prefer not to do that again. My urologist ordered an ultrasound and x-ray one week after my ER visit and saw no stone, however, the left kidney is moderately swollen. The report says there is uniform and symmetrical blood flow in each kidney and both kidneys are jetting.
7/17 Right kidney- 9.5 x 3.9 x 5.5——Left kidney- 10.4 x 6 x 5.7
The second month’s ultrasound results are that both kidneys are still jetting, but mentions that the left renal pelvis and proximal ureter is dilated. No stone was seen either time.
8/17 Right kidney- 10.0 x 4.5 x 5.4—–Left kidney- 9.8 x 5.4 x 5.9
I am confused as to why my right kidney has gone up and my left kidney appears to have gone down. I was told by my urologist that the variation in numbers all depend on the tech doing the test. I hate to have surgery when no stone can be seen. The x-ray did show two phleboliths, low center.
I asked for referrals to a nephrologist and internist because I feel my urologist is focusing on the “mechanics” and possibly not my whole body and health issues. Last month (July) I saw the Internist and asked for a parathyroid test as stones run in my family after middle age. Parathyroid was 98.5 which I think might be high for a 66yr old woman. My calcium random urine was 12.5. No, follow up after test results. However, the tests showed borderline high blood pressure, cholesterol, and pre-diabetes, BMI 26.60. I did not get any advice on these health issues. The paperwork just said to come back in one year. This month (Aug.) I saw the nephrologist and asked for the 24hr urine test that you have said is important. The nurse called to say everything is normal. No mention about what kind of stones I may be making or what is causing them. I was hoping for information on what foods to avoid for the type of stones I am making, but was only told to avoid salt, spinach and drink lots of water! Beyond that, I have to get my test results online.
24hr urine test for calcium, phosphorus, and uric acid:
Timed urine volume was 3,200ml.
Calcium Timed Urine- 3.2, Calcium Urine Excretion- 102,
Phosphorus Timed Urine- 14.3, Phosphorus Urine Excretion 0.5,
Uric Acid Timed Urine- 15.1, Uric Acid Urine Excretion- 483
I am becoming very concerned about the fact that my kidney may be damaged (or I may need antibiotics again!), but at the same time, I don’t feel like I have been given enough information for making a decision in this matter. My urologist hasn’t heard of MTHFR and I get no real answers about my concerns over surgery, only that my kidney is being damaged and surgery is necessary.
The reason I am concerned about having general anesthesia is my mother’s rapid mental decline immediately after having a hysterectomy at 85. She lived the next 12 years in private homes and finally a secured Alzheimer’s facility. I believe my mother also had this MTHFR gene variant which could have been a factor. I have also done research on anesthesia in the elderly and found it often affects their mental abilities. I have noticed that over these past two months I have been having difficulties with recalling names and also crankiness. I’m not sure if this is from the contrast dye, or possibly the kidney inflammation. Maybe it’s just the stress from my frustration over all of this but it only adds to my concerns about general anesthesia.
It all boils down to the fact that I don’t want unnecessary surgery if there is no stone. Is there another way besides a CT (with contrast) scan to see a stone. Any other test I should take? Should I delay this any longer by getting a second opinion?
I appreciate your consideration in reading this and value any insight you may be able to share.
Thank you, Margie
Hi Margie, A CT without contrast should help here. Stones are very evident. The high PTH could reflect kidney disease, low calcium diet, low vitamin D levels or perhaps primary hyperparathyroidism. The key test is your serum calcium; if it is normal than the PHPT is not reasonable. Your urine calcium of 102 mg/d is actually low so I suspect low calcium diet, reduced kidney function or low vitamin D. Let me know, Regards, Fred Coe
Hi Dr. Coe, After two months of trying to pass this 5mm stone I am having the ureteroscopy and laser lithotripsy done tomorrow. Because of my MTHFR reductase deficiency, my major concern is still the effect of the anesthesia and other drugs. I will not allow nitrous oxide and will share my other concerns with the anesthesiologist before surgery.
Once this is over I will concentrate on why I am forming these stones. My surgeon plans to retrieve the stone particles and have them analyzed. Hopefully, this will tell me what kind of stones I have and what diet to follow.
Vitamin D 25-Hydroxy level is 41 ng/mL,
Vitamin D 1,25-Dihydroxy is 43.0 pg/mL,
Serum Calcium is 10.0 mg/dL.
The chart says they are all within the normal range. So does that mean I need more calcium in my diet, and/or to take calcium supplements, or could that mean my kidney function is impaired because of the stone and I should be retested after recovery?
Should I also have another 24 hr urine test (or more) after recovery? I’m thinking that drinking more water than normal during the first test may have skewed the results. Thank you, Margie
Hi Margie, The stone analysis is important as are the 24 hour and serum data. But the approach is a bit detailed. Here is my favorite article on how to proceed. See if this helps. Regards, Fred Coe
Recently has ureteroscopy and was told am now stone free. Went in today for stent removal and was asked to return in several weeks for intravenous PYelogram to check for a stricture. Is this necessary?
Hi Joyce, Your surgeon seems to have concerns about stricture and I would do as s/he says. They do occur, and if present need early treatment. Regards, Fred Coe
Hello, Over the summer I had a few giant stones that were removed via URETEROSCOPY COMPLEX W LASER LITHOTRIPSY and URETERAL STENT REPLACEMENT. This was the most painful thing I have ever experienced and surely do not want to go through it again! As instructed, I had a few follow-up tests, sonograms, X-rays and there is another stone that’s developed. They are now suggesting observation or extracorporeal shock wave lithotripsy. What are your thoughts about this type of procedure, also is there a medication they can prescribe me to prevent stones from occurring in the future? I have completely changed my diet per their recommendations and I still got one. Its a calcium oxalate kind of stone.
Hi Lori, I am sorry your procedure either did not leave you stone free or was followed by new stones. The whose site is about prevention, and here is a perfect way to begin reading about how to do it. Regards, Fred Coe
Your website and the Q&A have been so helpful for me with my stone issues, I am now having to make a decision as to which procedure for removing my stones. I know your website is very much about prevention but thought you might have some insight on options.
I have a history of passing some kidney stones, and for years multiple stones have always shown up on any imaging I’ve had as well. No one has ever really addressed prevention or dealing with them until now, when not quite a year ago I began experiencing hematuria. I was not experiencing any other issues at the time so chose to deal with them conservatively. In the spring, I developed RUQ pain for a few months which I believe was stone related, although unsure. I decided maybe it is time to do something about the stones.
I am receiving different opinions about what procedure to go with to remove the stones, between ureteroscopy and the percutaneous approach, at least for the large stone. I think the perc suggestion is coming from trying to avoid a stent and multiple procedures. The other physician thought ureteroscopy would take care of it (and he seemed to think that he could get them all out in at least one kidney with one procedure, although with the latest CT perhaps he might change his thoughts about it). One also suggested that the smaller ones could then be addressed later with SWL.
A recent CT shows that at least one stone has enlarged from about 7 mm to 1.4 cm within about 9 months or so. I would guess that is probably the one causing the continued hematuria (and possibly the pain or discomfort I still occasionally experience). It seems I’m left to make the decision about the approach and I’m at a loss. I’d like to avoid more invasive procedures but also totally dread a stent.
I understand that you can only generalize, but do you have any thoughts about different approaches and making a decision, or at least what I need to consider? I have been putting off doing anything about this because I just don’t know what to do. Thank you so much for any insight.
Hi Carole, I have not seen your images and am not your physician, so my remarks are rather general. Certainly a PERC is large surgery and if URS will do it, by all means elect it. If the URS is done with a ureteral sheath permitting multiple passages of the instrument I imagine your surgeon will be able to remove your stones, but that is a complex surgical decision I certainly cannot make from here. As for prevention, it is certainly time! Take a look here, and read right through the first few chapters, and into the key links. By all means pursue prevention aggressively as you have formed many stones – by report. Get all stone material analysed. When URS is performed your surgeon can see inside the kidney; ask if stones are forming on plaque or plugs. You can read about their significance in the chapters I have pointed you to. Regards, Fred Coe
Thank you so much for your insight. I appreciate it. The other urologist that initially recommended ureteroscopy or possibly PCNL although less preferred (rather than SWL) has just reviewed the more recent CT and is now also recommending PCNL for the right kidney with the multiple and larger stones (with ureteroscopy or watching on the left with small multiple stones). I believe the PCNL thought is because of the size and number of them on the right, although I’ve yet to speak with him in person about it. This physician is part of the kidney stone institute at a nearby world-renowned medical facility and deals with these this daily, so I am inclined to think I’m going to hear “perc” regardless of whom I see for those right stones. I would definitely prefer to avoid it and am reluctant to do anything surgically, so will have to think on it.
In the meantime, I definitely plan on working toward preventing even more with diet modifications! Thank you for the links and questions to ask. It’s a bit of a challenge as I have other dietary health issues that conflict with stone diets, so will have to try to work with this. I have not had any stones analyzed since 20+ years ago, and the results from that one are unavailable now (although I do recall a calcium reference), but was finally able to catch some tiny fragments during the last bout of hematuria and hope to hear about the composition of them soon.
Thank you again for this service and for sharing your knowledge with researchers and readers. It certainly helps to know what and how to ask what is needed to be asked.
Hi Carole, PERC is indeed right for large amounts of stones. Although a subtle matter, at any one renowned center, among the excellent stone surgeons practicing it is usually only one who has the finest skills for PERC. Do not be afraid to ask if your surgeon is that surgeon. Usually the PERC person has done many, and among the best ones a majority (though not all of course) do their own access into the kidney, a point of refinement you might pursue in a tactful way. This is not to say that among the surgeons all cannot do the work well, they undoubtedly can, but among them, as among chefs, pilots, and hair stylists there is a range from excellent up. Regards, Fred Coe
Thank you so much for your suggestion. Who or how exactly do I ask about this? Am I looking at urologists within the stone department, other surgeons? I do indeed have some concern about who performs it, partly because of some other mild health concerns and few prior surgical experiences of my own.
I’m not sure if I can say here – if not, please edit and remove – but I am in Ohio and have seen someone most recently at the Cleveland Clinic stone clinic as well as another urologist in northeast Ohio. They both recommend perc now for the right kidney. There are so many physicians in this region who are excellent, but this is new territory for me with these most recent stones and I’m not really sure how to fish around for info due to the sheer number of doctors. (I am, though, fortunate to live within a state that has some fine medical care and the option to utilize it throughout.)
Hi Carole, At Cleveland Clinic is Manoj Monga, a superb stone surgeon and a friend of mine. I would use him without hesitation. Regards, Fred Coe
Dear Dr. Coe,
I am writing to you from my hospital room as I await discharge (hoping!). I am a 40 year old female and have had recurrent kidney stones for the last 6 years. The first one caused hospitalization and stent placemement. I believe I passed the second on my own with help from some pain meds and the third, a 14mm stone, was treated with lithotripsy and stent placement with a 5 day hospital stay. I am very sensitive to anesthesia as well as to pain meds. My respiration slows significantly. I have a wonderful primary care physician as well as a pain specialist. The current situation is what I am writing about. I have been having significant discomfort in both sides and after some imaging it was found that I had an 8mm stone in my left kidney as well as a 3mm stone in my right kidney. Neither was obstructing at the time of the imagining. My urologist insists that the stones in my kidneys could not be causing my discomfort but felt that it was appropriate to treat the stone in my left kidney. I was scheduled for lithotripsy on Oct. 23. Before the surgery, he told me that if he had trouble visualizing the stones on the X-ray, he woul use uterescopy and laser to treat the stone as well as placing a stent if necessary. The latter was the case. I woke up in recovery in intense pain. My PCP’s PA order a CT scan and when my pain had continued throughout the day with no relief, they found that the stent had not made it to my kidney and had caused a perforation of my ureter. As my urologist had left for vacation already, his associate proceeded to remove the stent, attempt to place a new one and after he was unsuccessful, another procedure was done to place the stent through my kidney leaving a nephostomy in place. I spent a few days in ICU after the procedures and today is my 8th day in the hospital. All imaging and tests are looking good right now although I still have a 4mm stone in my left kidney and the 3mm one in my right kidney.
What has not been able to be answered for me yet is why they did not know that the stent had perforated my ureter when it was originally placed? From everything that I have gathered from the surgeon who did the second procedure, he checks to confirm current placement of the stent.
Dear Beth, I am so sorry. Whatever the sequence of causes, you have had a very bad time. I am sure your surgeons would want to consider helping you obtain a second opinion at a medical school stone center given possible future problems with that ureter. I say medical school center not because physicians in practice are not an able group but centers tend to support physicians so they can develop special skills for problems like you now have. Regards, Fred Coe
Dear Dr. Coe,
Thank you so much for your reply. Yesterday was the conclusion of this ordeal (I hope) with the removal of the nephrostomy tube. I have had two hospital stays since the initial, one with an infection and the other with a large amount of sediment in my nephrostomy and high lactic acid levels. Fortunately, it was not sepsis and I have been home since Thanksgiving.
I have been looking for a second opinion through the universities near me, as you suggested and haven’t had much success. I was wondering if you could point me in the right direction? I’m in the LA area so I’ve looked through USC and UCLA.
I was also wondering if you could point me toward any information available regarding the standard procedure for placing a kidney stent. I’m not sure if the procedure is the same for all surgeons or if there is some variation. The two surgeons involved in my case seem to have different procedures, one uses contrast at the completion of the placement to ensure that the stent is correctly placed, the other (the one who performed the initial surgery) does not.
The surgeon who took over my case did a cystoscopy when removing my stent and assured me that I had healed well. Do you think there is still reason to be concerned about future problems with the injured ureter?
Thank you again for your kind concern and for your reply. I am sure that the people of the Chicago area really appreciate the expertise of the program at the University of Chicago. Thank you also for the information that the website provides for those of us dealing with kidney stones.
Beth T.
Hi Beth, High lactate levels are worrisome and do suggest sepsis has been present. Procedures for placing stents are far within surgical urology, where I am not a citizen. As for physicians at UCLA and USC many are fine. I would enquire which ones at each place specialize in stone urology – they self identify – and meet one or two. All of the surgical urology faculty at these centers will be high level, and the stone specialists able to do what you need. Regards, Fred Coe
Hello there again Dr. Coe!
You have been so generous with your time and advice in the past, I am hoping that you might have some suggestions for my current situation.
Just to refresh your memory – I had a 8 mm stone in my left kidney removed in late Oct. with a complication of a urethral perforation. After a re-stent and nephrostomy, I healed but was continuing to have right flank pain. They found a ~3mm stone in my right kidney and my NEW (UCLA) urologist suggested that she remove it and analyze it before it grew larger and caused more issues. The removal was uneventful, she used a basket and was able to remove the stone whole. She also indicated that there were no more stones. I did end up back in the hospital with stent issues. (This was January). At the beginning of March, I returned to the ER with severe right flank pain again. They determined after a renal scan that I still had mild to moderate hydronephrosis in my right kidney and that it was draining with a t 1/2 time of 17 minutes (the left was 8 minutes). Another stent was placed and I went about my life, the plan being to remove the stent in a few weeks. After a few days, I was leaking urine, had pain, urgency and continued frequency. The doctor trimmed the string from the stent to see if that would help. Symptoms improved slightly. But this past Wednesday pain in my left flank, more toward the front, woke me from sleep. I tried to “shake it off,” but ended up in the ER again. A does of IV morphine didn’t touch the pain, but after they administered dialaud and admitted me, the pain resolved after a day but my right sided flank pain flared up again. They treated me for a UTI with vancomycin but the Urinalysis culture eventually showed yeast, a resistant type, so antifungal treatment began. It’s Monday and I’m still in the hospital. The doctors don’t know what to think and are puzzled. Psychological pain was brought up as well as chronic pain. Here are a few fact that might be useful:
1. My urine albumin:creatine was recently 215 mcg/mg (it has always been within normal range in the past – note I have Type II Diabetes well under control, my A1C is 6.3)
2. Creatine was 97 mg/dL (urine)
3. eGFR was 108 mL/min/1.73m2 (blood)
4. Blood Creatine was 0.70 mg/dL
5. Urine Bacterial culture was negative
6. CT scan showed improved mild hydronephrosis in rt. kidney and no changes in left.
7. 24 hr urine stay showed:
Volume 1 L
SS CaOx 7.53
Urine Ca 401 mg/day
Urine Oxalate 14 mg/day
Urine Citrate 295 mg/day
SS CaP 1.67
Urine pH 5.496
SS uric Acid 3.42
Urine Uric Acid 0.761 g/day
8. Parathyroid blood test – normal
Any suggestions on a direction we should go?
I appreciate anything. This is very frustrating and is seriously impacting my life. i do not want to continue to take narcotic pain meds (norco is helping at the moment with the pain). And I need to get back to work!
Thanks,
Beth
Hi Beth, At UCLA you have reliable physicians, so I am not so sure I can add anything. You did not say what the stone was made of, so I am a bit limited there, too. The 24 hour urine shows a terribly low volume and a low pH so uric acid crystals can form at any time. Likewise your urine calcium is very high so calcium crystal formation is at high risk. Perhaps the attack of left pain was crystals, perhaps a tiny stone. The fungal infection surely reflects diabetes + procedures. The increased urine albumin could reflect blood from the various above mentioned, and that would elevate urine protein without implications for kidney disease. I think potassium citrate to raise the urine pH and a vast increase of 24 hour urine volume may prevent another attack, while your physicians sort out the infection treatment and drainage problem. But I am far away, UCLA is a great place, and anything I am writing may be utterly out of touch given the complexity. Regards, Fred Coe
Beth Kidney stones can be very tricky even for the best urologists. No one knows why your doctor did not check your stent placement. You should ask him. What Dr. Coe said is correct, often urologists/professors at medical schools have skills that most doctors in private practices don’t. ( in many metro areas) The difference is these places are all educational institutions and non profit. Many have teaching hospitals as well. Most have either urology or nephrology residency programs. So doctors/professors keep up with the latest advancements in their specialty or subspecialty. Treatment seems the same to patients but it is not… as the treatment model is different.
Thanks, Patricia, for your thoughtful comment. Fred
Thank you Patricia. I’m still plugging along. My new urologist is a UCLA doctor.
I am currently having intermittent severe pain in my right kidney/hip area after having laser lithotripsy and stent removal a week ago. I had a previous shock wave lithotripsy a month ago. Initially after recovery I was pain free, but within two days I had developed severe pain (Level 8-10) mostly at night, and could not sit for very long during the day. Currently on hydrocodone with apap which only sometimes alleviates the pain. Mostly confined to bed at home. Went to see my urologist today, and he did not know what was causing the pain unless a stone fragment was blocking the ureter, so I got a KUB xray. Won’t know the results of that until a few days later. My question is, how unusual is it to have severe pain like this after a laser lithotripsy, and could the fact it was done within a month of the other lithotripsy have contributed to the pain now, as perhaps my kidney/ureter had not recovered yet.
Hi Pam, I most suspect stone fragments or crystal plugging of the ureter. With such pain I would consider an ultra low dose CT to be sure. A KUB is not so sensitive. Regards, Fred Coe
Thanks Fred, today I did go in to the ER due to the unrelenting pain and a CT was done that showed multiple stone fragments in the right kidney, and a one inch stone at the end of the right ureter, which is the source of my litany of pain. Going to schedule another surgery Monday to get that out ASAP, with a stent to keep the ureter open. Interestingly despite all the trauma my right kidney has gone through, it appears to be working fine.
Hi Pam, stones there cause endless misery. Glad they are gone. Now, be sure about their cause and about prevention. Regards, Fred
I have been diagnosed with multiple bilateral non obstructive kidney stones, the largest being 10mm pursuant to a CT scan. Although the urologist stated that the a Ureteroscopy Lithotripsy is elective and that it should not cause pain, i have experienced pain in my left flank. I have a history of kidney stones with 2 prior procedures for obstructions. Is there a particular risk for multiple procedures? Do multiple procedures increase the risk of ureter injury or kidney stone development? And is there any downside to just leaving the stones in place?
Hi Ralph, Your urologist is right to say the surgery is elective. If you do not have significant pain, bleeding, obstruction, or infection the stones can be left where they are. No surgery is without some risk, and if elective perhaps that would be a good idea – elective if needed. Regards, Fred Coe
Hello there,
I’m researching options to remove a non-obstructive 7mm stone that is currently in the mid-portion of my right kidney. I had some blood in my urine, saw a urologist, and underwent several tests, including a CT Scan which showed the stone. All other tests are negative and I am a healthy, active 50-year-old. The doctor has given me 3 choices: to wait and see if the stone passes on its own, ureteroscopy or SWL. I’m traveling out of the country in a few months and I’m a bit worried about the possibility that I’d need some sort of intervention abroad. But I also generally prefer a wait and see approach. Doesn’t sound like SWL is desirable, especially if there’s still potential for pain/passing fragments after the procedure. Mostly, I’d rather not undergo surgeries, either planned or of the emergency variety! My urologist has said that the stone has a 50-50 chance of passing on its own–and this makes me think ureteroscopy is the way to go. Is it possible that the stone will never move at all? Looking forward to your thoughts. : )
I forgot to mention that I’m a woman, in case that matters!
Hi DK, You do have a dilemma – the gambler’s dilemma. The stone can stay put forever, pass on its own, or pass and cause trouble, and no one can predict if or when. Given the size, however, pass on its own is not so likely as pass and cause trouble. It is like any single event – a probability applies poorly = not at all – to any one person and stone. If your travel is far away and you are a cautious soul, URS is your best choice, and a ureteral sheath with exact removal of all fragments better than ‘dusting’ and letting the dust pass on its own. If you are brave, let it be. You do not know how long it has been there. Perhaps years. There is no calculation can help. Regards, Fred Coe
Many thanks for your reply, Dr. Coe!
Dr. Coe I have a question regarding unsuccessful Ureteroscopy for stone removal. I am a stubborn RN who feels she can treat things at home and self diagnosis. For 3 days with increasing pain I diagnosed myself with possible constipation to lower back pain and by night 3 it hit me it was severe kidney pain and my urine out put was nothing compared to my input. I made the dreaded ER trip on a Monday morning and it was confined I had my first kidney stone obstructing at the renal pelvis that was 5mm in size. I am a 40 yr old female with no prior major heath issues. I was given flomax and pain medication with advice to see a urologist sooner than later. By 2 am that night I was back in the ER in uncontrollable pain. They kept me over night on IV dilaudid and toradol and had me an appt with a urologist before the clinic even opened Tuesday morning. I was scheduled the following day at noon for uteroscopy with possible laser, extraction, and stent placement if needed. That night before the procedure I was back in the ER is uncomfortable pain. The procedure was unsuccessful and the stone remained and was unable to be broken up. A stent was placed to drain my kidney which I know had helped bc I put out of 3 liters of urine in 24 hours and lost over 10lbs. As of now I am I showing no signs of infections and was placed on antibiotics. I see pain control due to a traumatic cervical herniation with spinal cord compression. When I woke up the urologist told me the horrible news. I go back on Monday to “try again” and was told even if it was removed this painful stent will remain. My main question is: if this second Ureteroscopy is unsuccessful what is the next plan of care. I’m losing hours at work, I can’t manage to move out or med. my pain medicine wears off hours before the next does alternating it with Motrin and Levsin. I had to go 24 hours after the first scope without pain medicine bc the urologist said that since I had a pain management dr he could not prescribe (first I’ve heard as an RN for account treatments) but I didn’t get in till today to get it.
I am curious what my outcomes could possible be. I’m so nauseated from the pain that I know my intake isn’t on par but I also know my out put is decreasing based on what’s going in. I’m even keeping an I&O to see if I’m fluid over loading again. Any advice is appreciated.
Thank you,
Crystal
Hi Crystal, Sorry I took so long to answer you. Your urologist needs to remove the stone. If S/He cannot do it one needs to bring in another surgeon who can. In general URS is effective for almost all stones in the ureter so perhaps you have a special anatomical issue. Either way, if the second try is not helpful, get someone else for the third. When all this is done, seek prevention – stones recur. Regards, Fred Coe
how is the temporary stint removed after 4-10 days
Hi Jerry, Some stents are designed for self removal, others for physicians to remove. You need to check with your physician which is your situation. This is in answer to both of your questions. Regards, Fred Coe
how is the temporary stint removed after surgery
Hello – I had severe abdomen pain for a year. A CT scan showed a 7mm kidney stone still in kidney. I elected a Ureteroscopy to have it removed since it was on the bigger side. They might have to make an incision in my kidney to remove the stone – it appears to be stuck. Should I be requesting antibiotics after the procedure? My doctor doesn’t typically prescribe antibiotics but I feel that if an incision is made in my kidney, I should be given antibiotics. What are your thoughts?
Hi Patricia, Post operative antibiotics is a complex choice, and your surgeon needs to decide. I suspect she/he will give you some short term. Regards, Fred Coe
I’ve had stones since I was 12, some 45 year i currently have 2 or 3 in my left (6mm each) which recently caused a blockage & had me in hosp. They have to be addressed. My stones began from infection. They were bilateral but surgeries on each back in the 70’s removed 1 from left and all from right. No reoccurrence of stoned in my right kidney ever. Left is another story. 14 eswl’s and I don’t pass all the fragment which remain and grow. A viscous cycle. Now laser lithotripsy is available but all I ever hear is how great it is. But I also only hear “for stones in the ureter”. Not only is it easy to damage a ureter, but the kidney itself can be easily scarred. I will need a stent but one my doctor will place and remove, passing fragments and sand can cause blockages. But can the laser go INTO the kidney to pulverize the stone, or must the stone be at the junction of kidney and ureter or in the ureter for use of the laser technique? It sounds too good to be true. As I age, I have more fears, recuperation is a little longer, days or a week instead of hours or a day, Also, I get violently I’ll from anesthesia, which feeds the fear and apprehension.
Hi Maria, Ureteroscopy with laser lithotripsy is indeed usual in the kidney and seems ideal for you, but your surgeon has the real say as she/he is the one doing the work. Are these struvite stones? If not, it would seem that prevention might be better. Why are the stones coming back so frequently? Regards, Fred Coe
Hi Dr. Coe,
I just had laser lithotripsy for 2 4mm stones in my left kidney. After the surgery I ended up in the ER for excruciating pain (similar to when I passed a stone 19 year ago). Nobody knows why so they put me on Cipro for possible infection and gave me IV dilautid. The next day I ended up in the ER for fluid retention (my eyes, cheeks & abdomen were swollen. I was put on Lasix for 5days. I just had a CT w/ contrast which showed:
1.8cm region of decreased relative cortical perfusion, suspect a small renal contusion at site of previously seen 4mm stone. And residual 1mm & 2mm stone fragments.
Was my kidney “bruised” from the surgery and is this normal?
Thank you!!
Hi Tracy, I suspect you have some kidney tissue injury from the lithotripsy and that was why you had so much pain. I suspect you had a reaction to Cipro or Dilaudid causing the swelling. SWL causes some kidney tissue injury so this is a common problem. I am sorry you have retained fragments, and hope they all pass. Given all this, you should pursue prevention. Regards, Fred Coe