I have pointed out that the recommended US diet specifically seeks to correct all five of these risks and we should recommend it to all of our stone patients unless contraindicated by some specific problem.
But I have not as yet shown to what extent we as a nation eat a diet deficient in calcium and potassium and excessive in refined sugar, sodium, and protein. In other words I have not as yet quantified the extent of the problem that stone forming patients face.
Here is evidence from a large body of expert scientists.that we do in general eat an unsatisfactory diet.
The painting ‘Peasant Wedding’ by Pieter Brueghel the Elder (1526/1530–1569 – Google Art Project) hangs in the Kunsthistorisches Museum, Vienna. I chose it to reflect not gluttony, which is almost a cliche in 16th century art, but fullness or richness of means and possibility.
It presents a lavishness like our excesses of sodium and sugar and protein, and a paucity – this is a scene of multiple classes of people and a gradient of wealth – as we are poor in calcium and potassium.
WHERE WE GET THE INFORMATION FROM
The National Health and Nutrition Examination Survey (NHANES) describes itself so perfectly, I merely quote their blurb:
“The National Health and Nutrition Examination Survey (NHANES) is a program of studies designed to assess the health and nutritional status of adults and children in the United States. The survey is unique in that it combines interviews and physical examinations. NHANES is a major program of the National Center for Health Statistics (NCHS). NCHS is part of the Centers for Disease Control and Prevention (CDC) and has the responsibility for producing vital and health statistics for the Nation.
The NHANES program began in the early 1960s and has been conducted as a series of surveys focusing on different population groups or health topics. In 1999, the survey became a continuous program that has a changing focus on a variety of health and nutrition measurements to meet emerging needs. The survey examines a nationally representative sample of about 5,000 persons each year. These persons are located in counties across the country, 15 of which are visited each year.”
The NHANES 2007 2010 survey is the most recent, and from it I have brought here the main results concerning kidney stone and bone disease.
A REVIEW OF THE IDEAL STONE FORMING DIET
In this article, I simply state the scientific conclusions about key diet factors that concern stones and bone disease in stone formers. The data are summarized in a prior article.
LOW CALCIUM INTAKE
Because idiopathic hypercalciuria (IH) is highly prevalent among stone formers, and because people with IH are in negative calcium balance – losing bone calcium – on diets with more than sufficient calcium to support bone balance in people without IH, a low calcium diet can deplete bone mineral and predispose to fractures.
Urine oxalate is strongly dependent on diet oxalate content when diet calcium is low, but when diet calcium is high urine oxalate falls. For this reason, a low calcium intake will raise urine oxalate excretion.
HIGH SODIUM DIET
Urine calcium rises with urine sodium in both normal people and those with IH, but far more briskly in those with IH than normal. So a high sodium diet is ideal to raise urine calcium, thereby increasing urine supersaturation and stone risk.
Although not studied in IH as yet, high sodium intake prevents even high calcium intake from achieving positive bone mineral balance at least in perimenopausal women. We lack a trial of diet sodium and calcium in IH bone disease.
HIGH SUGAR INTAKE
In everyone, but especially in people with iH, sugar loads raise urine calcium abruptly and markedly. The spikes of high urine calcium will raise urine supersaturations and foster crystal formation. Habitual sugar use has an excellent potential to help deplete bone mineral because calcium is not usually present in highly sugared foods and beverages.
LOW POTASSIUM INTAKE
Diet potassium is largely from fruits and vegetables, and comes not as the chloride salt but mainly as the counterion to organic molecules whose metabolism produces bicarbonate – such as citrate. Bicarbonate production down regulates the renal citrate transporter in normal people so urine citrate rises. Citrate inhibits stone formation by binding calcium thereby reducing supersaturations, and by directly interfering with nucleation and growth of calcium crystals.
HIGH PROTEIN INTAKE
Diet protein raises urine calcium. How it does so may be via the net acid load produced by oxidation of sulfur in cystine and methionine but recent evidence suggests it is the protein itself. Whichever way protein acts, the higher urine calcium can promote stones. Whether protein loads reduce bone mineral is a contested issue to date.
WHAT DO I MEAN BY LOW AND HIGH?
MUCH SCIENCE YIELDS REASONABLE ESTIMATES OF HEALTH NEEDS
With great expense of effort and skill the 2015 Dietary Guidelines Advisory Committee derived from available science to date optimal intakes of these and all other relevant nutrients for promotion of the health of the American people. I will not review evidence concerning the 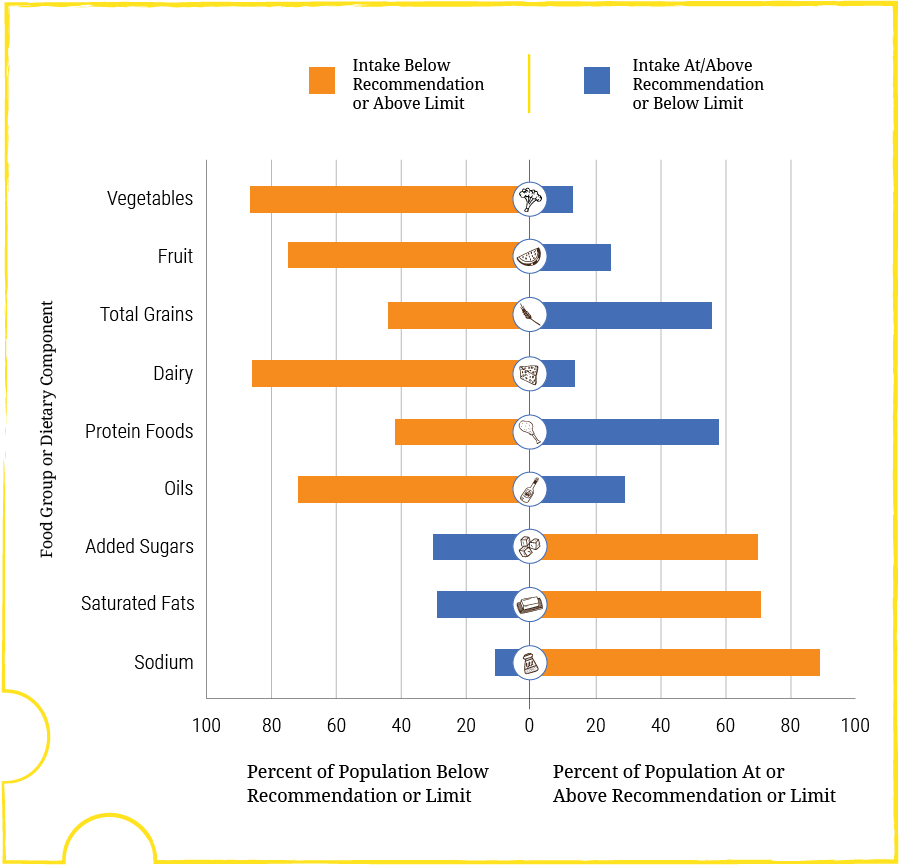 qualities of the people involved in that work, but simply accept that they were numerous and expert, and probably have provided about the best and balanced interpretation of the science possible.
qualities of the people involved in that work, but simply accept that they were numerous and expert, and probably have provided about the best and balanced interpretation of the science possible.
By high and low I mean in relation to the findings of that group. In the graphs here and to follow the upper and lower bounds of the optimal intakes are shown by bars.
This and all other graphs are from the 2015 – 2020 diet guidelines.
GENERAL SUMMARY
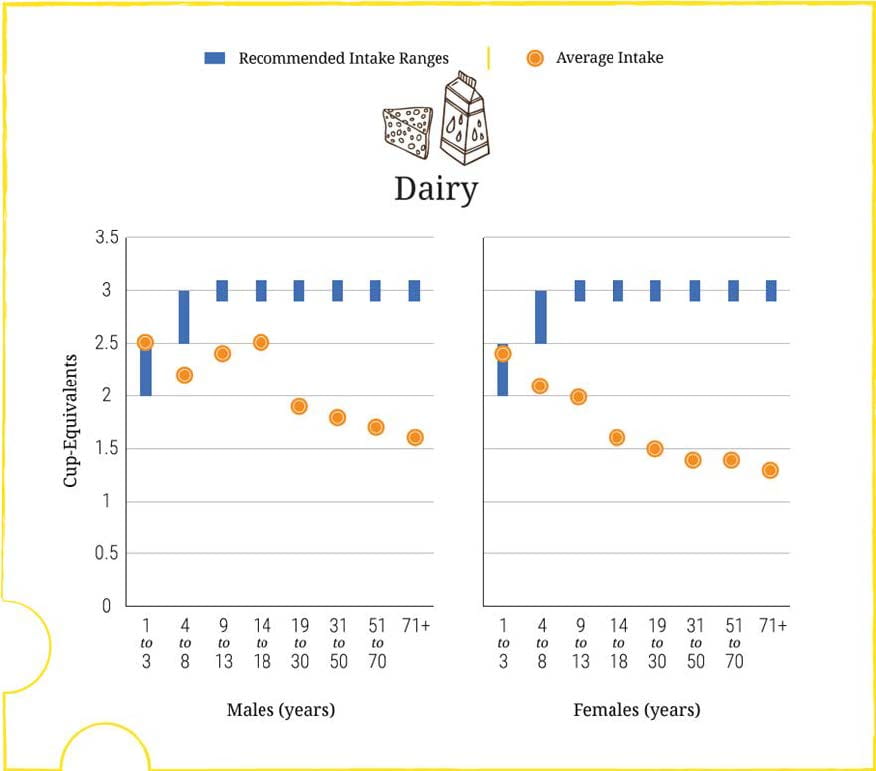
Dairy products (Dairy) are the chief source of calcium, and over 80% of Americans eat less than (orange bar) the recommended amount (1,000 to 1,200 mg/d depending on age and size).
Sodium is chiefly from additives, and over 80% of Americans eat more than the tolerable upper limit of 2,300 mg/d.
Added sugars are those that raise urine calcium, and about 70% of Americans eat more than the recommended amount (<10% of total carbohydrates/d).
Diet potassium is mainly from vegetables and fruits, and about 80% of Americans eat less than the recommended about of these foods and therefore less than the recommended 4,300 mg/d of potassium with its accompanying organic anions.
Diet protein is not so unbalanced as the rest, with only 55% of people eating more than ideal.
Oils and saturated fats may affect vascular disease but are irrelevant to stones and bone disease so I dismiss them here.
OUR DIET FOSTERS STONES AND BONE DISEASE
i hardly need to comment or repeat myself. Compared to what we need for health we eat too little calcium and potassium, and too much added sugar, and sodium. We also, in some subgroups, eat too much protein.
ANALYSIS BY AGE AND SEX
In this and the following graphs, all from the same 2015 – 2020 diet guidelines, the blue bars are the range of recommended intake.
CALCIUM
In both sexes, calcium intake is low almost throughout life, but increasingly so with age. Three cup equivalents of dairy products are estimated to provide the needed 1,000 to 1,200 mg of calcium, meaning that most adults, eating half of that or less, get about 500 to 600 mg/d of calcium.
Bone mineral balance is not well maintained in IH at even 1,000 mg/d of calcium. At lower levels, negative calcium balance would be the general rule. Urine oxalate will be higher at low compared to high calcium intake, a major factor in stone risk.
SODIUM
Among men, more than women, intakes soar with age, to over twice the upper limit (Graph below). That upper limit itself is hardly an ideal. For middle age people, those with high 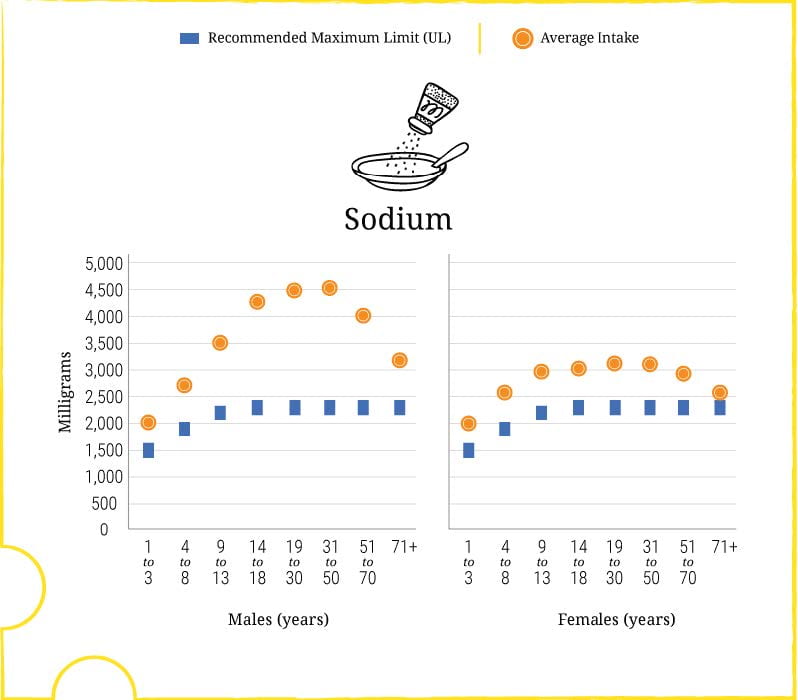 blood pressure, and others specially sensitive to sodium the ideal is 1,500 mg/d.
blood pressure, and others specially sensitive to sodium the ideal is 1,500 mg/d.
The high sodium is from additives. Creatures that walk on the earth, or swim in the salt sea, or in the lakes and running rivers have some sodium in them for us to eat, but little enough that if we add none from salt mines our daily intake would be below the ideal of 1,500 mg/d.
Most plants contain so little sodium that an all plant diet with no milk products would provide just enough.
Massive trial data have gradually pushed back all reasonable doubt that it is sodium excess and potassium deficiency more than any other factors that account for the rise in blood pressure with age. High blood pressure is a massive and remediable risk factor for stroke, heart attack, heart failure, and kidney disease.
SUGAR
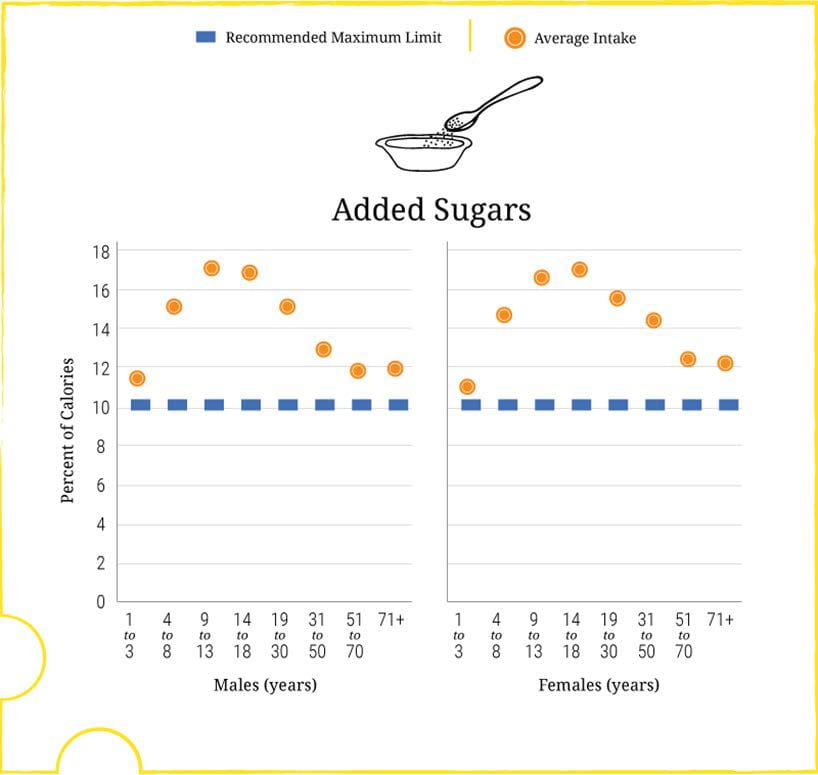 Experts have concluded that refined sugar is a main cause of obesity and diabetes. For us, it is a problem of hypercalciuria.
Experts have concluded that refined sugar is a main cause of obesity and diabetes. For us, it is a problem of hypercalciuria.
Men and women are equal in their sugar excess. From ages 4 – 8 on, and through into late middle age and old age we eat added sugar, as a percent of total carbohydrates, at nearly twice the levels we should.
FRUITS
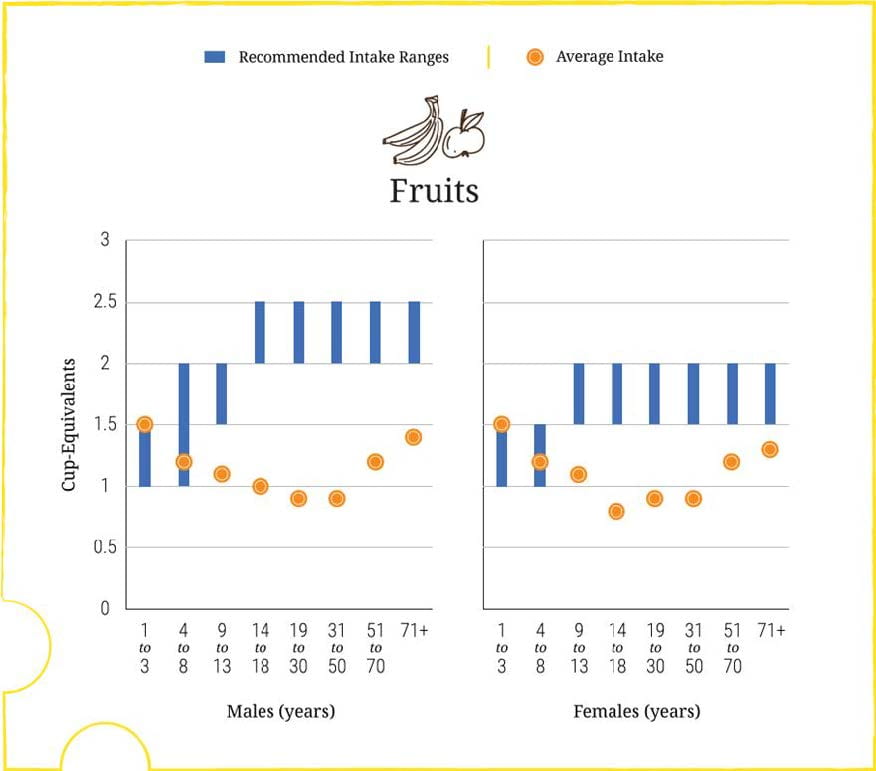 Because the two sexes eat about the same amounts of fruit but men are larger and should eat more, men are relatively more deficient.
Because the two sexes eat about the same amounts of fruit but men are larger and should eat more, men are relatively more deficient.
Fruits have virtuous molecules that experts say protect against diseases such as hypertension and perhaps cancer.
From the point of view of stones, their high content of potassium would be valuable because their potassium is mostly with organic molecules that are like citrate in being metabolizable, and their metabolism produces an alkali load that raises urine citrate.
PROTEIN
In general we eat protein mostly in line with recommendations. Men are perhaps high, 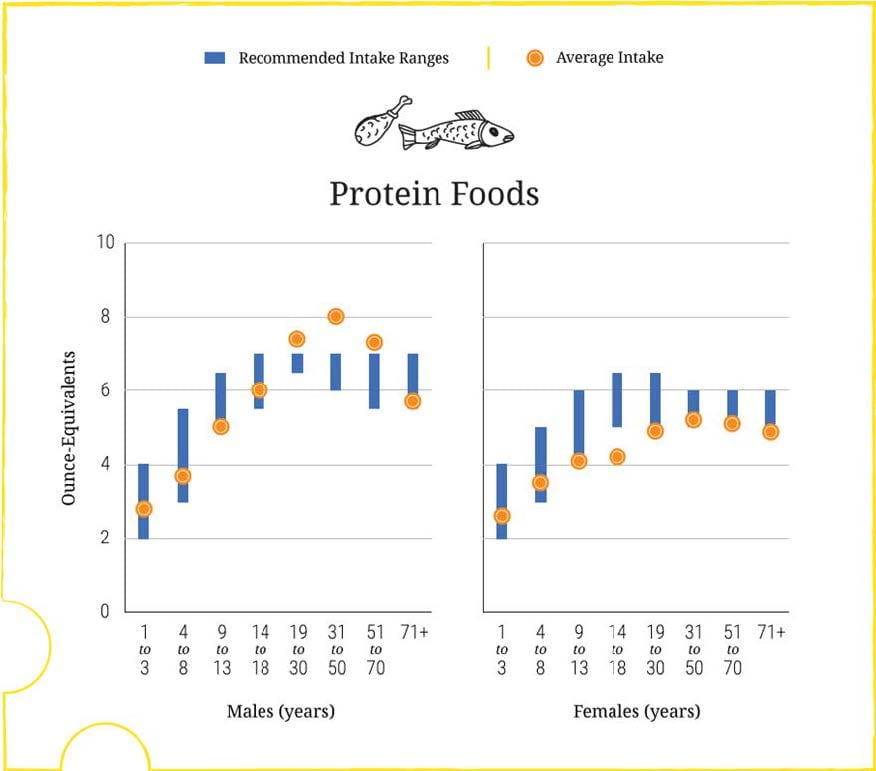 women are perhaps a bit too low. Experts maintain that too much of the protein is from land animals rather than fish or from plants, but from a kidney stone point of view I have no reason to make this distinction.
women are perhaps a bit too low. Experts maintain that too much of the protein is from land animals rather than fish or from plants, but from a kidney stone point of view I have no reason to make this distinction.
HOW GOOD IS THE EVIDENCE?
THAT OUR DIET FOSTERS STONES AND BONE DISEASE
I have exhausted myself parsing the data on calcium, sodium, sugar, anions, and protein and can do no more. This linked article reviews what is detailed in many other articles on this site, and the latter are linked out to the primary peer reviewed literature.
Nothing is certain in this world, this life. Even so we have to act based on reasonable evidence. The evidence is reasonable. Read it for yourself and make your own evaluation.
The ideal levels that the guideline committee proposes for calcium, sodium, potassium, calcium, and protein are in line with what the science of stone disease says would reduce kidney stone risk and risk of bone loss in patients with IH.
THAT OUR PRESENT DIET IS AS DEPICTED
I have no expertise in the kind of massive population sampling that drives NHANES and no ability to judge the quality of the NHANES scientists or the work they present. The sheer numbers of qualified scientists involved, and the longevity of the project, make me satisfied to some extent. Because salt and sugar are contentious matters in the US expert critics abound who would by now have unearthed and publicised defects in the work. I accept it as reliable. I might add that in my clinical experience stone formers commonly have many of the poor dietary habits reported in NHANES.
MY CONCLUSION
We eat and have long eaten in a way as if designed to cause stones and bone disease.
The diet for stone prevention and the bone disease of idiopathic hypercalciuria is more or less the diet for everyone. Physicians should foster the US diet recommendations for stone formers, and stone formers should adopt the diet for their own benefit.
Given the quality of the science that drives NHANES and the diet guideline committee, we all might be better off following the US diet recommendations, stone formers or not.


Dr. Coe, your research is so appreciated. And since I have moved to the West part of the country over the last
5 months, I realize have valuable your research is. I have followed your advice of low sodium, higher calcium now
for two years. I also realize now that I have new doctors, sometimes I have to tell them about this diet. Thank you
for continuing your research.
Hi Midge, Thanks for the note. I take it things are going well, and I am happy for that. Regards, Fred
Could you comment on oxalates? These should be reduced specifically, shouldn’t they? And should supplemental calcium be avoided, such as calcium citrate? I am especially wondering with milk if calcium cysts on kidneys. Thanks.
Hi Deborah, The article left oxalate out because it is about the current US diet as a cause of stones and diet oxalate excess is not a general US diet issue. High calcium intake is – I know this is counter intuitive – important for stone prevention and prevention of bone disease. High calcium intake with meals – not between meals – lowers urine oxalate excretion, and makes it possible to eat a wider range of foods. Supplements are workable if taken with meals. Ideally we would just use calcium containing foods. Avoiding calcium is not a good idea. Regards, Fred Coe
Thanks for this info
Dr. Coe, What an absolute joy it is to meet such a heartful, generous M.D. You’ve elevated my spirit. I’ve exhaused myself researching “How to prevent Kidney stones” because I had one about 9 years ago that was very frigntening as well as painful and a costly ER visit. It passed with out surgery thankfully~~~but I am beyone confused because I’ve seen soooo many articles on “Reducing Oxalates Dieting” i.e. spinach, potatoes, sweet potatoes being prohibited. Others say forget this and just pay attention to akaline/acid ratio. Please clarify because I can’t afford another “Kidney Stone”. I trust you more than any of the zillions of other sites on this subject. Thank you!
Hi Reina, Oxalate is a minor player if you do things correctly. Here is my suggestion. Begin here, and read through the first few chapters. They will take you to all the right places for prevention. Regards, Fred Coe
Dr. Coe: thank you for the continued information! I, too, moved away from the Chicago-land area last summer; however, the medical advice/assistance you gave me prior to moving has sure helped. As a teenager, I was unfortunately on a cycle of multiple stones every 6-9 months PRIOR to seeing you and since then I can happily report that is no longer true. I have learned, along with my parents, to do a lot of cooking from scratch and a lot of substituting as well. Thanks much~
Dear Kassidy, Thanks so much for writing. Stay on your treatment and lets hope there will be no more stones. Regards, Fred Coe
Fred,
I very much enjoyed reading your recent posts about diet and stone disease, and about the recommendations of the 2015 Dietary Guidelines Advisory Committee. I did have a couple of questions and comments about these recommendations. I’m sure you know and have already considered these issues, and I am interested in your thoughts.
With respect to calcium intake, you point out that, according to the guidelines, “Three cup equivalents of dairy products are estimated to provide the needed 1,000 to 1,200 mg of calcium.” Many people, either because of lactose intolerance or because of cultural or personal aversions to milk, do not consume this much dairy food. What should these people eat to get the recommended amount of calcium? Dairy products provide vitamin D as well as calcium. Should people who do not consume dairy products be concerned about their vitamin D intake, and if so, what should they do about it?
Understandably, the Dietary Guidelines say very little about exercise. Nonetheless, we can’t think about diet without also thinking about exercise. I don’t know the relationship between exercise and kidney stones, but exercise is certainly important for bone and general health. People should not think that following the dietary guidelines will absolve them of the need to exercise.
Governmental bodies such as the Dietary Guidelines Advisory Committee have to issue “one size fits all” guidelines. I don’t know if these guidelines are meant to be sufficient for 97–98% of the population (the mean ± 2 standard deviations) or if they are meant to provide an optimal balance between benefit and risk. Governmental committees can tailor their recommendations to age and sex, but not to other sources of variation among individuals. We have to remain mindful, however, of the ubiquitous variation in all aspects of our physiology and metabolism. This variation is part and parcel of our evolutionary heritage and of the variety of environments in which we develop and live. I was glad to see you point out “The US recommendations will hardly suffice for the most marked hypercalciuria.” Should we be alert to other sources of individual variation that might make different dietary goals appropriate for some people?
I agree that the members of the Guidelines Committee seem to highly qualified scientists, and their guidelines seem extremely sensible. While I do not want to undermine the quality of these guidelines, I do think it is worth remembering that nutritional guidelines have been plagued by misinformation and outright fraud. Many eminent nutritionists, including people who have been influential in drafting previous nutritional recommendations, were funded by the food industry and produced reports that benefitted their commercial patrons. The best reason to accept and follow these new guidelines is that they conform so well with the dietary guidelines to prevent or ameliorate kidney stones and bone disease that you have developed on the basis of your physiological expertise and clinical experience. These guidelines also conform well to our understanding of our evolutionary history. We and our evolutionary ancestors are omnivores, and over the millions of years since the human lineage diverged from the lineage leading to chimpanzees, our ancestors must have survived on a wide range of diets. Until recently, however, we did not consume refined sugar or large amounts of salt. The sugars our ancestors ate were fructose and sucrose in fruits, and glucose derived from starch in vegetables and grains; refined sugar became a significant part of the human diet only in the last two or three thousand years. Similarly, although people who lived near salt water had access to ample amounts of salt, until the advent of salt mining most people lived in salt-poor environments. As a result of our evolutionary history, our metabolic processes are not adapted to diets that contain large amounts of refined sugar or of salt. It is not surprising that diets rich in sugar and salt are risk factors for many diseases. A return to diets that comport more closely with our evolved physiology has got to be good both for individual health and for the health of our communities.
Bob
Hi Bob, Much thanks for gracing the page with such astute remarks. The lactose problem can be gotten around via alternative sources – lactose free as an example, or products not made from cow milk. A common alternative is the yogurt family of products. The vitamin D supplements are harmless being usually 25 hydroxy D or just D3 which are substrates for the active 1,25 vitamin D. With regards to variability, it is a real issue. The approach I have taken is to recommend diet changes and if they do not achieve clinical goals either do more or add medications. But the key is to begin with diet. The history of the guidelines is indeed stained by industry bias, especially with regard to salt and sugar. What pleases me and I am sure you, too, is that the new ones aim for very decent levels of both. I think that laudable.
That the guidelines reflect the physiology of stones and bone disease is indeed a crucial point in their favor. Likewise they accord with large numbers of trials concerning the effects of sodium intake on blood pressure, and even with the one major trial of sodium effects on bone mineral balance.
The idea that evolution could not prepare us for refined sugar and high sodium loads is so important your review of it adds greatly. These are foreign foodstuffs, not even real foods, and limiting them is crucial.
Thank you so much for contributing your thoughtful and elegant comments,
Fred
Dr. Fred Coe,
I am a desperate mother of a now 8 year old boy. Without getting into too much detail about my boy’s medical problems on a public site he has millions of crystals in his urine especially in the fall months. We went to a urologist at Seattle Children’s after he had what I call milk urine in which he then had a grand mal seizure and the urologist said he had never since a urine like it. We allowed him to have the picture for his professor colleague to show his students. He also has a mirade of other symptoms which I would be happy to share with you and I have all of his records as well. Could please help me or point me in the right direction. It is all beginning again and I am terrified. I am a pediatric ICU nurse myself of 12 years and have some theories myself. I have gone to multiple doctors, who I feel think I am being paranoid as well as my dear husband but both my mommy and nurse instincts are on high alert. I will give you anything in return money, study rights and etc.
Hi Sarah, All I can offer is to review all of the records for you and try to help. Seattle Children’s is a very fine place. The problem sounds like hypercalciuria with high urine pH – renal tubular acidosis perhaps. Anyway, I am a professor and can do the review. There is no charge – no way to bill anyway. If this will help, call Kathleen at 773 702 1475 and let her know about this note. She can arrange for a proper record transfer via fed ex. Regards, Fred
Thank you so much Dr. Coe. I will definitely be contacting. It seems to really be exacerbated by sugar which definitely supports your article. He has been tested for diabetes about 5 times. His results always seem to be the high end of normal. Thank you, you give this old mom hope. P.s. I bought his Halloween candy from him.
Dr Coe,
I understand the article left out oxalate as it is addressing more of the current American diet. What about someone who has adopted more healthy diet by incorporating vegetable juice, should they be worried about oxalate level? Specifically with carrot juice. Can it be offset by adding lemon?
Hi Kathy, the juices are always a problem being concentrates. I would worry about oxalate loading especially because the juice is not likely to be accompanied by calcium that would normally reduce oxalate absorption. Lemon would be of no use. Better to eat food than emulsify it into juice. Regards, Fred Coe