 Severe hyperoxaluria – always worrisome, never something to dismiss or even wait a long time thinking about.
Severe hyperoxaluria – always worrisome, never something to dismiss or even wait a long time thinking about.
The Vegetable Seller’ by Flemish painter Joachim Beuckelaer (c.1534-1574) seems a perfect image for this exercise in vegetable excess. He was never very famous but influential concerning food and kitchen scenes.
Jill Harris co-authored this article with me.
Kidney Stone History
This 47 year old woman had her first manifest stone 12 years before I first met her. It was removed by SWL. The second stone was about 6 years ago treated with URS. Stones were 90% calcium oxalate monohydrate, 5% calcium oxalate dihydrate and 5% calcium phosphate. Three years ago, and then one year ago, more stones were reported in her kidneys. One year ago URS was performed on one side. Her physicians determined that new stones were forming over the years. Her father, mother, and one of four brothers have stones, but none of her 2 sisters. Her three children 20, 19, and 16 have had no stones.
Long before, at age 20 she had an episode remembered as stone passage but without any specific documentation.
General Medical History
A full GI evaluation for Crohn’s or Celiac disease a month before we met was normal. Fatty liver and multiple stones were documented from that evaluation. In addition she had hypothyroidism of unknown cause treated with hormone replacement, and takes progesterone for perimenopausal symptoms. She has been anemic for reasons presumed to be dietary.
Detailed Diet History
Going back to age 18 through 31 she was vegetarian but ate considerable soy products and nuts. She also remembers constant snacking on dried apricots and almonds specifically during the 15 years between her first presumed stone and her first documented stone. She used dairy products but not very much. Note her stones became manifest at age 35 but there is history suggesting an earlier stone at around age 20. From 31 through 38 she incorporated small amounts of chicken and fish but with the same low dairy product use and her continued high vegetable and nut intake. The chicken and fish were used once to twice a week.
In 2008, at age 38, in response to her diagnosis of hypothyroidism she was evaluated for food intolerance which led her to avoid casein, meat, and dairy products, so that her low intake of calcium worsened. She resumed her vegan diet that now also excluded gluten and soy. These more stringent changes occurred three years after her first stone.
One year ago she added to these restrictions a very low sugar intake leaving only fruits, veggies, eggs, nuts and nut butters – the latter became extreme. She lost 15 pounds on this regimen – from 140 to 125. She then gained 17 pounds back just before the fatty liver diagnosis. Of note, the high fruit and vegetable diet produced the expected loose stools.
Initial Laboratory Findings
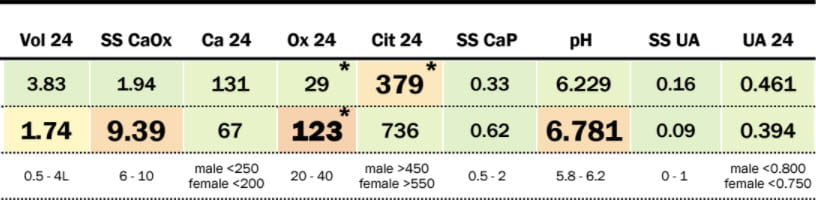
Remarkable Hyperoxaluria
![]() Her urine volume was
Her urine volume was 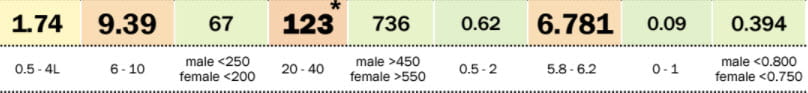
![]() reasonable, calcium frankly low, and oxalate excretion in the range of enteric and primary hyperoxaluria. As expected from her diet, urine
reasonable, calcium frankly low, and oxalate excretion in the range of enteric and primary hyperoxaluria. As expected from her diet, urine 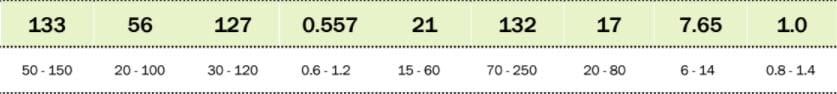 pH was high.
pH was high.
Otherwise Normal
Urine sodium was modestly higher than I prefer, potassium, magnesium, and phosphate unremarkable. LIkewise for urine NH4 and sulfate, and protein catabolic rate of 1 gm protein per kg per day.
Stone Risk
Because of the oxalate excretion, calcium oxalate SS was above 9 fold. From this I would have expected calcium oxalate stones, perhaps the monohydrate. Indeed that was her stone type as noted above.
Diet Treatment
Even though my first concern was primary hyperoxaluria, her diet was so remarkable I considered a single attempt at diet treatment reasonable before referring her to a primary hyperoxaluria research center. Accordingly, after studying her actual food intakes I recommended major changes. I counseled her on how to eat at least 1,000 mg of calcium with her meals. Obviously, I went through all of the highest oxalate foods and asked they be stopped. Because of the higher calcium intake and her stone disease being both familial and antedating her most remarkable diet changes, I also advised toward a lower sodium intake of 1500 mg. Likewise I asked she reduce her refined sugar intake to below 25 gm/day.
Followup Results
Stone Risk Factors
Of course, from her diet history, I suspected mere dietary hyperoxaluria, but also worried that being so severe I might be wrong.
In fact, her urine oxalate fell to 29. Probably because of higher calcium intake her urine calcium about doubled. SS for CaOx fell to below 2 meaning little or no serious stone risk.
The fall in urine pH was expected – we went from almost exclusively vegetable foods with their predictable high potassium alkali content to more milk and other products that would provide less GI anion uptake. The fall in urine citrate, however, seems a bit marked and makes one wonder if she tends to a low citrate but because she ate so much vegetation that trait could not become manifest.
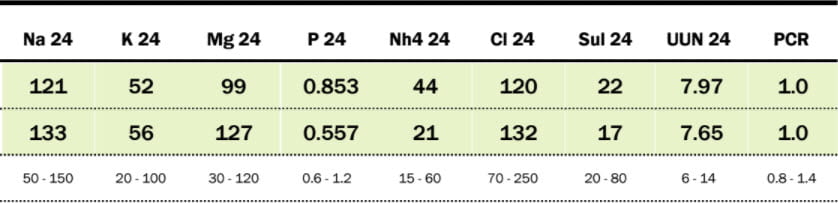
Diet Factors
She did not lower sodium intake very much but given her urine calcium I am not concerned. Perhaps as I expected her urine NH4 increased but sulfate was not changed. A crude calculation of GI anion uptake from just the sum of Na + K – Cl was not changed – 57 at the beginning and 53 mEq after treatment. Since sulfate went up by 5 mEq and net anion fell by 4 mEq I would have expected NH4 to go up by only 9 mmol not 23 mmol. Possibly a more refined calculation using Mg, Phosphate and calcium would give more reasonable estimates. As well, urine pH fell, so urine ammonia for any ammonia production rate would increase.
What We Can Learn
Leaving aside the arcana of urine ammonia and acid base balance for a moment, the main point is how high diet can drive urine oxalate and with what remarkable force one can lower it by diet change as happened here.
The clinical implications are few but significant.
When faced with a very high urine oxalate level, no time should be wasted. A complete diet history may direct one toward an attempt at diet treatment. If so that attempt should be vigorous and focused – high calcium, low oxalate all at once. If the urine oxalate falls, as it did here, chronic diet planning is a leisurely matter. If it does not, levels this high pose too much risk for protracted diet efforts. Other causes need be sought and reversed.
Diet history is a powerful clinical instrument. Here it not only disclosed the reason for the urine abnormality but provided a decent time correlation between diet changes and first stone manifestation – a likely high oxalate diet preceded the stone manifestations by some years. Given her many affected relatives, her diet could not be the only reason for stones – they are not likely to have done what she did. But her urine citrate is a clue – perhaps that trait of low urine citrate runs in her family.


I have diagnosed with hyperoxaluria and as to cause was told “No, the cause is unknown. You just have it. ”
*Is there a class of hyperoxaluria with no known cause?*
Age 61, stone history.
Diet restrictions did little; nor additional calcium; no symptoms of other disorders and now seen 2-3 metabolic experts, as well as regular urologist. No sign of genetic Primary Hyperaxaluria.
Since 2014, 24-hour urine UrOx:
162 | 160 | 668 * | 56 | 65 | 86 | 133** | 51 | 112 | 46
*668 is probable error
**133 is only one done with Litholink
All other urine/serum values normal, including Calcium and Citrate; uric acid controlled by Allopurinol.
Thanks for any thoughts.
Very useful information My grandfather also had 24 mm Kidney Stone. Ayurvedic medicines left his 24 mm stone in one and a half months. I am not yet sure how Ayurveda did miracles. Well my grandfather’s age is almost 75 years
Hi, I have left this on the site, but it is in a language I do not read. Because it seems to promote commercial medications, I would have normally deleted it. But out of respect for what I do not know I left it here. If any readers can help me understand the language, much appreciation. Fred Coe
Hello. Thank you for sharing all of the great information. A couple of things are confusing me though.
1. Since elevated Ca is known to cause deposits in all soft tissues dramatically increasing CVD mortality, Ca is a component of CaOx stones, and since magnesium is 70% as effective as Ca at binding with and lowering urine oxalate, and that most adults are chronically deficient in Mg why wouldn’t Mg be recommended to chelate dietary oxalate in the intestine instead of dangerously increasing Ca levels?
2. Along these same lines, what is the advantage of using potassium to deliver citrate vs magnesium?
3. Organic lemon juice contains almost no sugar and is very high in citrate. Wouldn’t this be a good choice for alkalinizing the urine and delivering even more citrate?
Thank you for your help. I’m really trying to piece this all together–well, as much as possible.
Hi Zack, About diet calcium; in the ranges recommended for all Americans, 1000 – 1200 mg/day from foods no evidence supports any disease risk whatever. It is in renal failure patients we find calcium deposits in soft tissues. Low calcium diets foster oxalate absorption and bone disease, especially in stone formers who have high urine calcium losses. Likewise, higher calcium intake reduces blood pressure. I think you refer to elevated blood calcium, or renal disease; of course if you do have such, your physicians would know and act accordingly. Magnesium loading is not well tested, and I have no comments. The potassium as counter ion is in place of sodium that would raise urine calcium and blood pressure; most US people have potassium deficient diets. Lemon juice has sugar, and tends to a low enough pH that much of the citrate can be in the form of citric acid – that would not benefit stone formers. Regards, Fred Coe
I’ve had 30+ stones since August 2018. They were tested last fall – oxalate. I tried a low oxalate diet – kept meticulous track without success in altering/lowering the number of stones.
Hi Luann, Diet oxalate alone is not much help. Here is a good stone prevention diet. But you also need proper evaluation for cause, as there are many reasons for stones. Regards, Fred Coe
Thank you for sharing all of the great information
Hello all
Can U please expand on how methylation or leaky gut may also contribute to oxalate sensitivities.
Hi JM, I have not studied this matter, and therefore cannot comment. Sorry, Fred
Hi Dr.Coe,
I’ve recently been diagnosed with hyperoxaluria (unknown if primary or secondary). I’ve passed a dozen stones every year for four years now and did present with stones and renal colic in my early 20’s. I have a good majority of my stones tested – they range from calcium Oxalate, calcium Oxalate mono hydrate, calcium phosphate (80%) and kidney matrix stone (protein with trace calcium oxalate). I’m currently 34. Unfortunately my high Oxalate result was not brought to my attention after completing a 24hr urine test in June of last year. That October I passed a large stone in ED and ultrasound showed I had medullary nephrocalcinosis. Finally, I was seen at a routine renal appointment and I was diagnosed last month with hyperoxaluria. Since my diagnoses, the 24hr Oxalate testing has been suspended in Ontario due to global shortage of the testing agent. Is there any place that I can get tested in the US? I live in a border town and can seek medical care in US.
PS: I posted on your matrix stone page and I appreciate your responses. Unfortunately the lack of knowledge in my hometown means I haven’t gotten through to specialists in my area but I will begin to see specialist at Mount Sinai and London Health Science Centre in the near future, of which I hope they can give insight.
All the best,
Hi Kasey, I have been very behind in answering people and regret that. You do not show the oxalate result but if there is any question of unexplained high urine oxalate you need intensive testing to be sure about how much and if it is from primary hyperoxaluria as that disease puts kidneys at serious risk. Looking at Google Earth London Ontario is within distance for Ann Arbor or Rochester NY, both have fine university health centers and especially Rochester has lots of stone expertise. Litholink is the US national kidney stone testing lab – a branch of LabCorp and I would be sure and get that in the US for 24 hour testing. They do not sell outside the US. As for evaluation for cause you need a wide range of testing which I an sure your physicians know about and certainly will be available in the US at the two places named. Until the diagnosis is established I would avoid dehydrating episodes, diuretic agents and low sodium diets – the latter two common in stone prevention – as they could cause kidney damage given primary hyperoxaluria. Regards, Fred Coe
Dear Dr fred Coe,
Please note that Iam writing this for my husband I am from Kerala, India he is a frequent kidney stone former,his father and brother also have.He is obes and diabetic .first stone at the age of 20. He has around 4 stones in a year.but they don’t have this frequency.Here in India stone analysis reports says it as calcium oxalate stone.by reading your article I went for 24 hour urin analysis twice.I don’t know how accurately they do the test here.all parameters were normal except oxalate ,first test showed a value of 112, and repeated test showed it as 40. In the first test ,lab people had not put any chemicals in the can for collecting the urin .second time they had put some chemicals ,each done in different lab.this was done in 2023 July.nephrogist over here told chances of having hyperoxalouria,so they gave high doses of pyridoxine tablet .And potassium citrate and formgene tablets .He was scared to have these many tablet ,so he discontinued it.he is strictly avoiding oxalate rich food and incorporating 1 glass milk. With coffe with breakfast and fish ,curd ,and some veggies as lunch.he avoids all rice bran .he frequently eat chicken and eat 2 eggs daily.Still he is making stones.
Any suggestions to improve his condition.
Looking forward for your kind words.
Thank you
Dhanya
Hi Dhanya, The widely varying urine oxalate may reflect diet or lab error. I would surely obtain another 24 hour sample with preservative to be sure. Given the family history I am surprised urine calcium is not high. But high oxalate can also be inherited and is dangerous as well as a cause of stones. Best, Fred Coe