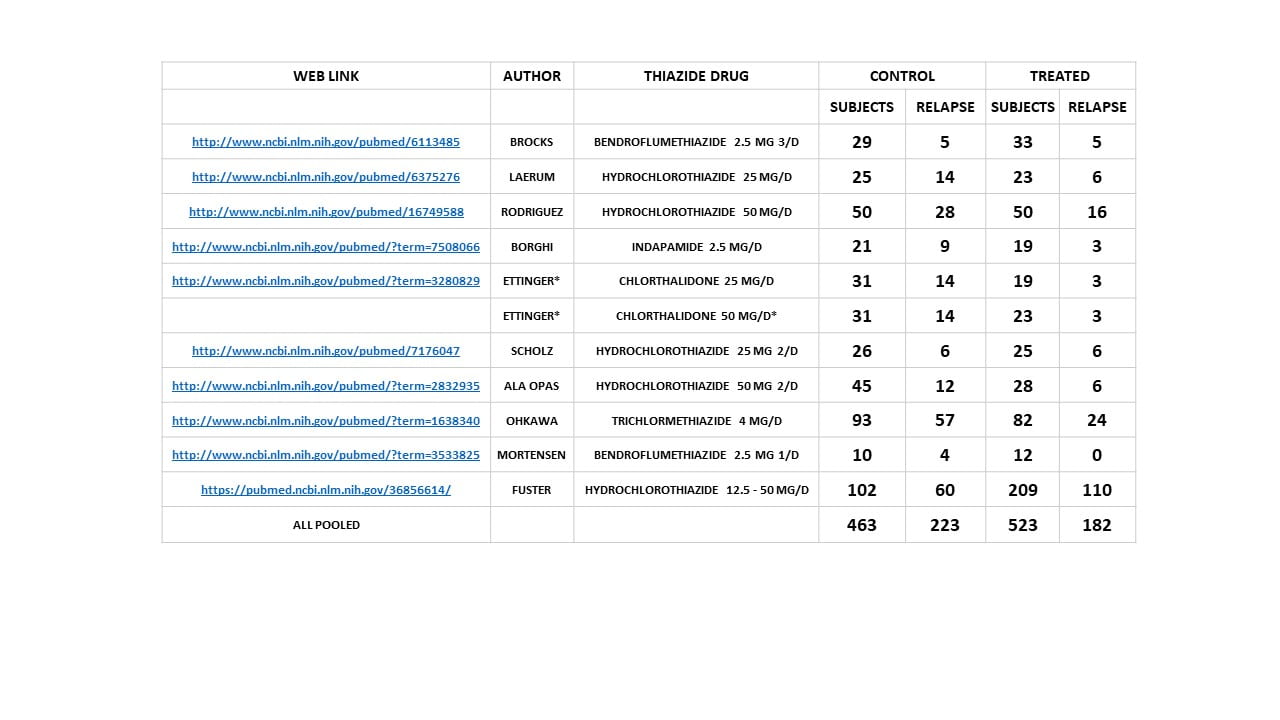
 I picture a younger me on this article because the long line of thiazide trials stretches back decades in time to when I looked just like the photograph. The large picture that heads this article depicts my spreadsheet of all of the trials I have reviewed, and this link will take you to that sheet. It is a nice place to go because it has links to each of the trials in case you want to take a look at them yourself.
I picture a younger me on this article because the long line of thiazide trials stretches back decades in time to when I looked just like the photograph. The large picture that heads this article depicts my spreadsheet of all of the trials I have reviewed, and this link will take you to that sheet. It is a nice place to go because it has links to each of the trials in case you want to take a look at them yourself.
Of course the reason I am writing this article is the new trial by professor Fuster and his colleagues. You can see at a glance it is much larger than the rest, and it is negative – meaning those who took the drug did no better than those who did not.
ABOUT TRIALS
Of all the branches of biomedicine trials should seem most intuitive and simple to almost anyone who lives in modern times. Medical trials are not different from trials of refrigerators, or cars, or sunscreen potions. They are what they say, practical demonstrations concerning the extent to which something in the real world accomplishes those tasks we desire accomplished. For good reasons modern trials use fancy statistics, fancy meaning beyond common intuition and using techniques that someone like myself, who is not at all unfamiliar with statistics, finds baffling – or, better said, dense enough in meaning one might hope someone else does the work.
Their valuable enhancement of precision tends to screen the coarse realities of a trial behind the gossamer of a shimmering mathematic. In service to the assumptions of the mathematics things about the trial are arranged as in a ballet – done this way, not that way, from start to end. At the end the magicians step before their shining curtain and pronounce their verdict. We are suitably awestruck.
But behind the curtain is just folks who form stones, some of whom take an active medication and some a lookalike placebo. After a while, we can count them – so many on the drug made a new stone, so many on the placebo made a new stone. From that fleshy and highly medical labor of counting the mathematicians can conclude if the difference departs in a meaningful way from what might occur by chance alone. For chance is the devil in the room. Unlikely things do happen. A useless drug might just by chance’s whim be taken by people whose stone disease was in a temporary decline and we are mislead. It is in the estimate against chance that we need our mathematicians, their glorious equations and punctilious manner of proceeding. They can save us from false belief.
Because I know nothing about these high affairs, and because we have had a lot of trials for thiazide over decades, going back to when I looked more young and winsome, I have taken what could be called a dumb view of the topic. I just accumulate all the people tried on the drug or off, and how many made another stone (relapsed is the common medical term). As for chance I do only a simple counting statistic. To my accumulation I have added the new numbers. They have a powerful effect being so large as they are. This seemingly witless approach is not bad if there are a lot of trials. For, after all, what is uncommon is – well – uncommon, so trial after trial will more or less give us a crude idea of how the world works. Is that not not untrue?
THE NEW TRIAL
Objective(s)
Like all science, we start with the objective: What did the investigators seek?
I would have thought is was merely if thiazide reduced new stone production, but it was more: “Thus both the efficacy of thiazide in the prevention of the recurrence of kidney stones and the dose-response effect remain unclear.” So they wanted two things. For the one it was just the usual – drug or not, new stones or not. For the other it was to use a range of doses to look for a dose response. Two objectives.
Research Plan
What They Did
The drug: hydrochlorothiazide, the doses 12.5, 25, and 50 mg once daily vs. placebo. So, four groups of roughly equal size, three for the drug doses, one for the placebo. The measure: number of patients in each group who passed a stone OR had one removed OR showed a new stone on CT, OR showed the enlargement of a prior stone on CT. Any ‘OR’ yes = ‘Recurrent Stone’. The final score is number of recurrent stone formers thus defined in each of the 4 groups during the 3 year trial. My little table included precisely these four numbers.
The analysis is far more sophisticated. Mathematicians abounded and I will not scruple to question or even try to describe their particular form of magic. We have to allow for time of exposure to the drugs, how many stones each person had formed (an estimate of their propensity to stone forming), the two major ‘OR’s were analyzed separately (passage OR removal) and radiographic new stone OR growth of old stone(s).
My Reservations
Their null hypothesis (no effects of drug) was odd: “that there would be no relation (i.e., no significant linear trend) between the hydrochlorothiazide dose and the symptomatic or radiologic recurrence of kidney stones”. As a physician this seems overly stringent. After all no one cares about the linear regression, just whether the drug reduces stones.
I have another worry. Those of us who work with patients know the hydrochlorothiazide is relatively short acting so we use longer acting drugs. We also know that at such a low dose as 12.5 mg once a day the drug is unlikely to work – experiments are planned a bit from practical wisdom even if analyzed with the scrupulous eye of a mathematician. So the lowest dose had little a priori likelihood of doing any good.
I have a third worry. Stone passage or removal can be from old stones or new ones. The latter requires on read the CT and count to show that the stone that left the person was not one already in the kidney. They attempted to correct for this by analyzing separately patients with no stones at baseline, and those events that occurred within 6 or 12 months of entry into the trial – present stones might washout in those early intervals. But I am not so sure they need to do this – why not pass at any random time during the trial. Why not count the stones?
Finally, a forth. Stone growth differs from new stone appearance. The latter requires nucleation of crystals the former merely addition of atoms and molecules to a completed crystal/protein matrix ensemble. The saturation needed for nucleation exceeds that needed for growth. The drug, so far as we know, acts by lowering urine calcium and thence saturation, and thence stone forming propensity. The two are different so their merge is to add dissimilars.
I Am Not Ungracious
This could seem carping and negative, but not so.
Quite opposite.
I know some of these investigators and think so highly of them that I am offering my best thoughts. They have performed a very large trial in a sophisticated and rigorous manner, and deserve the best I one offer intellectually.
Results
The drug did not reduce stone events (passage OR surgery) but the two higher doses did reduce the CT recurrence estimates of combined growth OR new stone; odds ratio vs placebo were 0.49 (CI=0.27 to 0.87) and 0.54 (CI=0.29 to 0.98) for 25 and 50 mg/d doses respectively. In a fancier ‘corrected’ model this effect disappeared.
Urine calcium was not reduced beyond chance by any of the drug doses (Table S15). So the main action of thiazide to prevent stones was not in evidence in the 24 hour urine samples. But although not significant as against chance values did fall by about 40-50 mg/d at the two higher drug doses and by about 25 mg/d in the lowest dose group.
As expected from the weak effect on urine calcium, hydrochlorothiazide did not lower urine saturation with respect to calcium oxalate or calcium phosphate. Even so, the highest dose did lower SS CaOx from 8.1 to 6.8 a change of -1.23 (CI=-2.49 to 0.02) nearly significant as against chance. For CaP SS the lowest dose was least ineffective, but none of the doses lowered CaP SS. Although stones were predoinantly calcium oxalate, initial CaP phases may play in important role in nucleation and stone disease.
What Does it Mean?
We Need More Trials of this Fine Quality
Certainly this study is the first really large and scrupulous trial for thiazide in stone formers, and the only proper response is for the stone research community to get itself together and do more trials with more promising agents like chlorthalidone or indapamide. Both seemed effective in trials that had many inherent defects and I suspect fine trials with them will be stunningly positive.
I would hope future trials jettison dose response ranging and use their available power to compare placebo to a common clinical dose of 25 or 50 mg (I favor the former) chlorthalidone or the equivalent for indapamide. I would also be more conservative concerning clinical recurrence. Passage or removal of a stone is not recurrence, and stone counting by CT is very difficult so perhaps one would want to focus on patients with low stone burdens.
Hydrochlorothiazide is Not A Good Drug Against Stones
I have shunned hydrochlorothiazide for stone prevention life long, and will certainly continue to do so. It is short acting and just as much a nuisance as longer acting drugs with regard to potassium loss and changes in glucose tolerance. I never saw any good in it.
I Will Not Change My Practice
I will continue to use long acting thiazide drugs to prevent calcium stones and use them in the way that seems most effective. The weight of all trials combined makes me doubt profoundly that thiazide does not reduce stones depsite the evident weaknesses of number and design that abound among them. It is too precious to contend that although the summary of all cases ever tried points to an effect the drug is nevertheless without an effect. There is just too much imbalance on the side of stone reduction. I have added the present study numbers but only for the 25 and 50 mg doses as the lowest dose had little chance of working. The sum total of all the data remain biased in favor of a thiazide effect.
I do not use thiazide by itself but only with diet management. I have always advocated for diet first, meaning lower diet sodium and sugar as a way of lowering urine calcium, high fluids, and adequate diet calcium to reduce urine oxalate and for bone health. To me, thiazide is an addition to diet. In that context this trial is no reason to stop using long acting thiazide like drugs.
But withal, should trials of this quality discredit my thinking and prove the longer acting drugs ineffective I will drop them on the moment. Likewise for diet in that we have only one find diet trial after all these years of NIH funding for stone research.
As I was long a beneficiary of such NIH funding some might ask why I did nothing to advance the cause of stone trials. I would answer that I have no taste for such work and a poor kind of mind as well. Trials are for people with certain talents I lack utterly, being too caught up in imagination’s whorles. Too unworldly, impractical, and easily confused.

Dr Coe; I am a stone former (Hypercalciuria). I started taking 25 mg of Hydroclorothiazide a couple years ago. My 24 hour collection (and CT scan) done once per year have indicated no new stones and no supersaturation since starting on the Thiazide. However, at the same time, I took your advice and lowered my daily sodium to 1,200 mg or less per day, started drinking more water (2.5 liters per day) and added citrate capsules three times per day (Potasium/magnesium Hydroxycitrate) so not sure which of these did the trick or a combination. Do you think I should just stay with the Hydrochlorothiazide or switch to something like Indapamide or one of the other longer acting Thiazides?
Hi Doctor Coates, The new trial does not really apply to you as you have used multiple modalities – fluids + low sodium diet + potassium alkali and you have been free of new stones and have presumably lowered urine calcium and supersaturations. The trial, by nature, could not include all of this. For this reason, I would not change things. But if a new stone does occur I would switch to a longer acting drug. Best, Fred
Dr. Coe, I appreciate all your helpful articles and all you do for stone formers!
Am I understanding correctly that this study would not apply to Chlorthalidone ( which is what I am taking)? I t has successfully lowered my urine calcium ( dose 25 mg daily) into normal range when low sodium low sugar diet did not . I also have osteoporosis so am very concerned about high urine calcium for that reason as well. ( I haven’t had a stone in 5 years). Thanks.
Hi Nancy, You are right. The longer acting drugs will work better. As well, this trial is not negative as CT stone counts fell even with a weaker drug. Regards, Fred
Dr. Coe,
I have passed a few oxalate stones..but thanks to Jill’s education had my bone density tested due to high urine calcium reports. I am active (normal weight) 40 year old man and but unfortunately, I have been diagnosed with bone disease and Hypercalciuria. Changed to the kidney stone diet right away.
When I did the change, lowered by Urine Calcium from 419 to 341 and Urine Sodium from 103 to 40. PCR dropped from 1.8 to 1.1. Ox went up a bit from 19 to 24. Citrate went from 661 to 658.
I was rechecked for thyroid issues recently and all looks normal with those levels: PTH 39, blood calcium at 9.3, ionized calcium 5.1 while on the kidney stone diet. Vit D level at 38.
My doctor has started me on Chlorthalidone (12.5 mg/once a day) but while my blood pressure seems to stay in a normal range, after 3 days I found the side effects quite difficult (headaches, lethargic, fogginess, some dizziness, some muscle tightness) so I stopped. Did i simply not give it enough time for my body to normalize to it (maybe I need to give it a week or more?)
Upon these reports doctor had my potassium and Sodium checked, both look to be normal levels.
My thinking was if I asked to move to Hydroclorothiazide 12.5 mg/twice a day with good compliance, might this reduce the power of the side effects but still give me results despite your reluctance for this drug?
I also saw you mentioned someone taking 12.5mg Chlorthalidone every other day and with its half life of 23.5 hours, they would effectively be getting a lower dose that way. I worry if I would still feel a similar side effect the day I consume that 12.5 mg dose of Chlorthalidone.
Clearly I need more help than diet alone, but am stressed wondering about potential side effects. Do i have a sound theory for asking to switch to Hydroclorothiazide 12.5mg twice a day if I can perhaps tolerate that better while lowering urine calcium?
I will also add. My first stone passage was in 2018, and had my first litholink done then and had it checked yearly several more times. It was first reported in 2018 at 552, then 505 in 2019, then 419 in 2021. I was under the care of three urologists over the time period and not one every expressed concern for bone health or that I might have a serious issue going going until I chatted with Jill this summer. You can imagine my anger and disappointment knowing that perhaps I could have taken action much sooner if the Urologists I saw were more informed to the high danger of bone loss. I had no idea until now.
Thanks for all you and your staff do.
Hi Sam, You have a high urine calcium and bone mineral loss, and your physician has – not unreasonably – offered CTD at a dose I would have chosen myself. Given the bone disease and stones, might I ask if your serum phosphate has been measured? Some cases like yours arise from gene defects and treatment is not conventional. Likewise is your serum PTH in the normal range? Sometimes PTH is very low = also reflecting a genetic cause. Perhaps your physicians might want to consider bone active medication, if the above ideas do not work out. This is a complex decision. As for the diuretics, they are bone friendly. Perhaps 12.5 mg every other day might be effective for you as some people are very sensitive to the drug. Having very little information about you, that is about what I can say. Your physicians are responsible and seem to be doing the right things. Regards, Fred Coe
Hi Dr. Coe,
I recently started on hydrochlorothiazide, with my urologist prescribing 50mg once a day. I’m a bit discouraged to see this new study and wondering if there’s a better drug that I can request. Even with strict sodium/sugar intake, my urine calcium is still around 300, so clearly I need more help than just diet alone. All blood tests came back normal, so it seems it’s IH. Thanks to you and Jill for the wonderful information and research.
Hi Austin, Given so high a urine calcium on 50 mg of OHCTZ I wonder if the urine sodium is still high. You do not give the value. Or perhaps you mean urine calcium is 300 with diet and no drug. If the latter this high a dose of OHCTZ should lower urine calcium by about 70 mg more. In the study the highest dose of the drug was clearly effective. Regards, Fred Coe
Hi, Dr. Coe
Sorry it took so long to reply. I meant to say that my urine calcium was high before the drug (303 on my last test). However, after a few days on hydrochlorothiazide I passed out several times at work, and was advised by my doctor to immediately discontinue the drug. My natural urine calcium is still high, so I clearly need help, but I was keeping sodium low (under 1,000mg a day) and the drug took me off my feet. Is there any other natural remedy? Low salt and sugar hasn’t been enough, yet these drugs come with lethal side-effects and I’m uncertain how to proceed. Is there another drug besides hydrochlorothiazide that might work better? Thanks for your help.
Hi Austin, I looked back to your first comment and now. Perhaps your physicians need to look into the cause of your high urine calcium. I do not see any information about that. Perhaps you have some underlying issues, or genetic causes that might affect treatment. I do not even know your age. These are just thoughts but your physicians might want to look more into cause than continue to use treatments that do not work well for you. Best, Fred Coe
Hi Dr. Coe,
Hoping this comment reaches you and you still actively monitor this site. I have a nephrology appt at Emory Medical University in two months, and your input here would be greatly appreciated while we wait.
I am a 21 year old male, I first started passing kidney stones when I was 12. For years after that I experienced chronic kidney pain, and several doctors refused to acknowledge the possibility of kidney stones, until I finally found a doctor willing to perform an ultrasound when I was 19. This revealed a 0.7cm stone and 1.2cm stone next to each other in right kidney. Urology performed a 24hr urine collection, suggested potassium citrate (refused) and to wait and observe, and was never removed. The most recent checkup CT scan at age 21 has showed one stone in right kidney, 1.6 cm, suspected of fusing together. Another 24hr collection recently has showed much different and numerous issues.
[1] The first 24hr collection (11/09/21): Vol 24 = 2.13, SS CaOx = 5.20, Ca 24 = 188, Ox 24 = 34, Cit 24 = 278, SS CaP = 1.27, pH = 6.408, SS UA = 0.24, UA 24 = 0.550
(The issues of note from this collection were high SS CaOx, low citrate, high ph, high SS CaP, high ph)
[2] The second 24hr collection (1/19/24): Vol 24 = 3.16, SS CaOx = 4.42, Ca 24 = 319, Ox 24 = 37, Cit 24 = 364, SS CaP = 2.19, pH = 7.012, SS UA = 0.05, UA 24 = 0.655
(The issues noted from this collection were significantly higher calcium excretion, significantly higher Cap, and significantly higher pH. However, citrate and CaOx were improved)
Interestingly, as mentioned previously, the stone appears to have not grown much at all between these collections which is confusing. We have no info as to stone makeup, but I assume CaOx was the predominant issue. From 2021 onward, I have been consuming much more protein and sodium, which I hypothesize to have caused the calcium increase.
A couple questions:
-should the most recent collection results (however bad they may be), be invalidated due to the fact the stone hasn’t grown?
-I have read your articles claiming that diet is not a reliable treatment to lower pH, why is this? I have read several published studies showing that citrus fruits/vegetables raise urine pH (which I consume a lot of), and animal protein lowers it. Other than this, is there any way the prolonged urine pH can be treated? Would dRTA be suspected here?
-could medication that lowers urine calcium effectively make the high pH a non issue, if Ca levels falls into ideal range?
There seems to be a paradoxical solution here, where previously citrate needed to be increased, which I have accomplished through fruit intake. However, this appears to have pushed the pH further, potentially creating the new issue of calcium phosphate stones.
Other potentially helpful notes: from age 12 to around 15 bloodwork showed a significant vit D deficiency. Blood calcium was highest at 10.2 but has normalized. More details from recent 24hr collection: Sodium 167, Potassium 62 mmol, Magnesium 173 [High], Phosphorus 970mg, Ammonium 37 mmol, Sulfate 40
Thanks in advance for any input
Hi Evan, High urine pH with modest urine citrate is common among people who form calcium phosphate stones. The high urine calcium probably reflects idiopathic hypercalciuria. The urine calcium will vary with diet sodium more than in normal people and the new higher value may well reflect that. I suspect your stones will have a significant proportion of calcium phosphate in them. Stones beginning as early as yours usually reflect idiopathic hypercalciuria. To me you seem a rather commonplace kind of stone former and will no doubt be an easy problem for your nephrologist. Regards, Fred Coe
Hi Dr. Coe and thanks for the reply and insights. Your expertise is invaluable.
Another 24 urine collection has been completed. Urinary sodium was successfully reduced greatly to 60. Protein dropped to 1.3 g/kg. These were the two recommendations to help control the high calcium excretion. Unfortunately urinary calcium went even higher to 341 this time. Citrates dropped further to 316.
Oxalates, SS Caox are normal. SS cap and ph remain elevated. Serum calcium and potassium both normal. PTH normal. Serum co2 is slightly elevated at 30.
I am under care of a nephrologist at a university medical center. He currently has no ideas and we are doing more and more tests. Genetic testing on the way.
I am completely baffled how such a drastic drop in sodium produced zero beneficial results. Treatment is difficult because medicine to control calcium will make ph even worse/higher.
Thanks in advance for any ideas or input.
Hi Evan, Perhaps you have a more complex cause for high urine calcium. I do not know your medical situation nor all of your results, so I cannot go further. But I would be sure about all blood testing and perhaps look for clues to genetic causes that might have specific treatments. The link is just an illustration of one such pair of causes. Regards, Fred Coe
Dr. Coe,
Wanted to say thanks again for your help. I am waiting on genetic testing to be complete.
In the meantime, we have all blood work back. 1,25 dihydroxyvitamin D came back as elevated, at 85. PTH came back as normal. Serum calcium normal.
My last question for you: is it worth pursuing further parathyroid analysis? I have read publications stating that elevated 1,25 D can suppress PTH levels. In your opinion, could parathyroid still be causing the IH even if levels appear to be normal, due in part to the elevated 1,25?
Thanks so much.
Hi Evan, I do not think you have PHPT. The high 1,25D will drive hypercalciuria. Gene testing is very valuable here as you may find a specific cause for the high 1,25 D (NaPi defects, CYP 24, other) which could refine treatment. Obviously your situation is complex and may benefit from referral to a university program at a geographically suitable medical school. Regards, Fred Coe
First, thank you for this wonderful resource. I’ve been directing any patient with a history of kidney stones here.
I have an odd combination of abnormal lab values that don’t seem to align with any single diagnosis.
Polyuria 6000 ml
Urinary calcium 650
Urinary phosphorus 3660
Urinary Uric acid 1590
Persistent Hypocalcemia, hypophosphatemia and hypouricemia
Elevated 1,25 vit. D 105 (20-80)
Normal PTH 31.6 (15-65)
Normal Mg, Na, K, Cl, C02
In 2005, at the age of 32 I was found to have osteoporosis and IH. My case was reviewed by a think tank at Mayo. Was Rx HCTZ 25 mg and told to take up a sedentary existence. Didn’t like that advice and continued testing. Found to have very low IGF-1 and began HGH at dose to get my IGF-1 into mid range. By 2008 was osteopenia, today my T-score is above 0. The HCTZ and HGH have kept my labs normal all these years (I test 2-3x/ yr) until recently.
From Aug-Nov I got very strict with my diet and dropped 15 lb. During that time these symptoms gradually increased-
Urinary frequency & urgency, fatigue, insomnia, loss of libido, muscle cramping especially in feet, gas, constipation, reduced exercise tolerance
By mid-Nov I ran labs and was shocked by these results. I am scheduled with a nephrologist but the soonest was in 3 months (June17).
I experienced rhabdomyolysis on 2-26, 9-fold elevated CK, liver enzymes and LDH. Currently recovering from a second, albeit lesser, case of rhabdo.
Trying to desperately help myself until I am seen. I stopped HCTZ thinking this may aggravate the hypophosphatemia. Started K-Phos neutral, restricting salt and I don’t eat sugar. Taking a moderate amount of supplemental calcium. I tried Dipyrimadole for the calcitriol lowering effects but found the headaches unbearable. I’m suspecting my clean diet with no processed food meant my phosphorous intake went down aggravating a genetic renal phosphate leak. Likely also a calcium sensor defect. I’m currently awaiting genomic test results.
Also of interest, the hormone Leptin reduces urinary calcium by blocking 25-d alpha hydroxylase. I ran a Leptin test on myself and there is none that could be detected. Another consequence of fat loss.
Hi, Apart from the low serum calcium you fit the pattern seen with gene variants in the sodium /phosphate cotransporter(s). The high 1,25D mediates high urine calcium, and increases kidney tubule calcium receptor activity worsening calcium loss. Bone disease is related to osteomalacia and bone scans underestimate its severity. Here is a link to at least one form of this general set of conditions. Phosphate supplements reverse the syndrome by lowering 1,25D. Thiazide is not desirable. The low serum calcium is odd for this condition, indeed for any high serum 1,25D normal PTH situation with high urine calcium. But the path here is genetic – find which variant(s) you have and work from there. By all means do not self experiment. Serum phosphate can get low enough to cause serious diseases. You need your care from a university based program because your condition is not common. Regards, Fred Coe
Hi Dr Coe – I am a 57 yr old male and 40 yr weight lifter and athlete that was recently diagnosed with osteoporosis. 24 hr urine over 500 and diagnosis of idiopathic hypercaciuria (2 of my brothers also just received same diagnosis). No hx of kidney stones. I have reduced sodium intake and am now taking a thiazide. I have read that after 2 yrs that thiazides can lose their efficacy. Have you found this to be the case, and if so how do you manage tx at this point. Thank you.
Hi Paul, male osteoporosis and such high urine calcium and a family history point to possible genetic causes. Your physicians might want to explore this possibility as it could affect treatment. As for thiazide they do not lose effectiveness over time so far as I can tell from available studies. Apart from gene studies your physicians might want to measure serum phosphate, 1,25 vitamin D, serum calcium, PTH, and bone markers to clarify the underlying causes of your bone disease. Likewise thiazide might not be sufficient or necessary – perhaps hone directed medications would be more so depending on the above. In other words, I think what you have is complex and arising from an underlying disease, not simple idiopathic hypercalciuria. Regards, Fred Coe
Hi Paul, male osteoporosis and such high urine calcium and a family history point to possible genetic causes. Your physicians might want to explore this possibility as it could affect treatment. As for thiazide they do not lose effectiveness over time so far as I can tell from available studies. Apart from gene studies your physicians might want to measure serum phosphate, 1,25 vitamin D, serum calcium, PTH, and bone markers to clarify the underlying causes of your bone disease. Likewise thiazide might not be sufficient or necessary – perhaps hone directed medications would be more so depending on the above. In other words, I think what you have is complex and arising from an underlying disease, not simple idiopathic hypercalciuria. Regards, Fred Coe
Dr. Coe,
Would indapamide possibly be more effective than thiazide in lowering the amount of calcium in the urine? I was originally prescribed potassium citrate, but, after seeing a recent 24 hr urinalysis (with a relatively higher amount of calcium than the previous analysis), my doctor decided to try this diuretic. I haven’t actually taken it yet because I’m concerned about possibly urinating all day. I am 76 yrs old with an enlarged prostate, so I’m already urinating fairly frequently. But, it the idapamide is truly worth a try, then I’ll put up with that inconvenience.
Thank you,
Carl Kalwaitis
Hi Carl, indapamide is excellent for reducing urine calcium in calcium stone formers with high urine calcium excretion. Ideally one lowers diet sodium as much as possible so the dose can be low. Because long acting this drug does not change urine volume – does not cause sudden increases that are followed by troughs. Regards, Fred Coe
Good Afternoon Dr Coe,
Ive asked some questions before and its been very useful when speaking with my Nephrologist. So thanks a lot for that. I’ve tried to bring my sodium excretion down to under 100mmol/24hr and my urine calcium still is a stubborn 7mmol /24hr. I then got prescribed indapamide 2.5mg which I take half of the dose at 1.25 once a day with 4g of potassium chloride over the 24 hour period. here are my results before taking the indapamide.
Result – 30/11/2024
PH 6.7
Collection Period[Hours 24
Urine Volume (mL] 2582 mL
Urine Phosphate-17.3 mmol/24 hr
Ur. Phosphate conc -6.7 mmol/24 hr
Urine Calcium- 7.0 mmol/24 hr
Ur. Calcium conc -2.7 mmol/L
Unne Magnesium 4.1 mmol/24 hr
Ur. Magnesium conc.1.6 mmol/L
Citrate non detectable
Here are the results after 3 months of indapamide:
Sample BB382271A (URINE) Collected 01 Jan 2024 09:00 Received 02 Jan 2024 09:00
Urine Volume 3.791
Urine Stone Former Profile
Creatinine Concentration 3.6 mmol/L
Creatinine Excretion 12.6 mmol/d 7 – 13
Urine Calcium Concentration 2.28 mmol/L
Calcium Excretion * 8.0 mmol/d 2.5 – 7.5
Urine Phosphate Concentration 4.97 mmol/L
Phosphate Excretion 17.41 mmol/d 15 – 50
Citrate excretion – Non detectable
Indapamide 6 months 1.25mg
Sample BB382507F (URINE) Collected 10 Jun 2024 09:00 Received 10 Jun 2024 13:55
PH – 6.7
Calcium Excretion
Collection Period 24 h
Volume 3.607 L
Urine Calcium Concentration 2.19 mmol/L
Calcium Excretion * 7.9 mmol/d 2.5 – 7.5
Citrate excretion: Non detectable
From these numbers would you say the indapamide is having any effect. Ive tried to keep my sodium regular throughout this period at under 1.5g of sodium and just over 1g per kg of protein per day. I was really praying for a huge reduction but the only improvement I see is my urine concentration.
I haven’t had the reduction in my urine PH which I was hoping for based on your information above which is unfortunate.
I have increased my urine volume as much as I possibly can to mitigate any stone burden. Due to the huge increase in urine volume should I be happy with this calcium excretion or maybe seek guidance from my nephologist to maybe consider chlorthalidone to try and decrease my urine calcium. I see that I’m still over the 200mg that you recommend. At this point Im trying everything in my power to resolve my lifelong illness. Any comments or points I can take to my doctor will be hugely grateful. They don’t have much experience with my RTA issue even the very best here in the UK.
Thank you Dr Coe
Jonathan ( possible heterozygous RTA)
Hi Jonathan, I do not think your urine calcium fell with the drug. But you do not give urine sodium values. I suggest you make a graph of urine calcium (y axis) urine sodium (X axis) using all points before and after indapamide with different symbols. Urine calcium will vary linearly with urine sodium. Are the indapamide points below the control at any given urine sodium? Right not it is hard to tell as you do not give all the data. I think the RTA is causing the low citrate and high pH. A few papers have suggested that SLGT2 inhibitors may lower urine pH. No data on RTA. Your nephrologist might try it – off label and likely to fail. I have used it in one CaP stone former, results not in yet. regards, Fred Coe
Hello Dr Coe, unfortunately with the urine profiles from the UK NHS provider, I cannot get my urine sodium excretions. I followed a fairly strict diet which is mostly the same consisting of calorific intake of animal foods(moderate) and whole foods with minimal salt under 1.5G sodium per day( I count the salt intake on foods)
I appreciate the recommendation on the SLG2, I will pass this to my Nephrologist for consideration. For your patients (rta or no rta) with no lowering of calcium with Indapmide, have you seen any success with switching to chlorathaldone. I have limited options left at my disposal. I’m hoping your preferred diuretic could give me hope.
Any information is so much appreciated. Thank you.
Hi Jonathan, thiazide drugs generally lower urine calcium, and can prevent new stones. But it is like enough to indapamide one cannot expect much difference. I do not know the details of your blood chemistries. Is your phosphate low, perhaps, as a clue as to the cause of the high urine calcium (I do not have ready access on this site to your past posts). Have your physicians considered phosphate? Best, Fred Coe
Thanks again for your reply. Here are some of serum phosphate levels over the years.
13 Jun 2024 – Inorganic Phosphate 1.02 mmol/L 0.8 – 1.5
08 Aug 2023- Inorganic Phosphate * 0.72 mmol/L 0.8 – 1.5 (Low)
26 May 2021- Inorganic Phosphate 1.11 mmol/L 0.8 – 1.5
19 Dec 2022- Inorganic Phosphate * 0.73 mmol/L 0.8 – 1.5
08 Aug 2018- Inorganic Phosphate * 0.67 mmol/L 0.8 – 1.5
07 Sep 2018- Inorganic Phosphate 1.33 mmol/L 0.8 – 1.5
I tried to see if there was a correlation with high urine calcium and low serum phosphate but as I do these tests on different times I couldn’t do this.
It seems they swing from low to normal. My physician is really out of answers and told me that its something that I will have to deal with and not stop the stone burden. I try and push him some of your work which we have been in the process trying (indapamide). I would even consider booking a consultation with yourself if this would give any insight. I spoke to Cinthia a year back and explained, Id see how thiazides will do and come back to her. Gene testing is unavailable here in the UK.
Thank you so much
Hi Jonathan, I am afraid that you have complexities I cannot fathom except as a real consultant. That is legally possible between US and UK. If you wish to pursue that route I could try and help. Our renal clinic is 773 702 6134. The nurses there have contact with coordinators to set something up. Best, Fred Coe
I might be in a situation where I’m going to have to engage in some medical self-advocacy. Due to a career change I was in and out of health insurance plans and things hadn’t been taken care of as they should have for the last 4 or so years. I’m a very frequent stone former (currently have ~6-7 in my left kidney and 2-3 in my right kidney from what I could see of the CT scan they showed me; radiologist did not bother to count and I don’t have personal access to the imagery to go step through myself and count) and have yet to have a metabolic workup done on potential causes of stone formation. I am obviously very interested in exploring stone prevention. A recent kidney stone incident has landed me with a new urologist, but when I inquired about 24 hour urine drops blood work for PTSH, Phosphorous, and etc there was little interest and an insinuation that this should be the purview of my PCP. My PCP when I brought this type of workup up a year ago seemed uninterested and unsure (did not seem to be aware what a 24 hour urine analysis was).
Given that I have a history of hyperuricemia and gout (but I do not appear to be making urate stones based on 2 analyzed stones) I was wondering if I should even try a thiazide diuretic if the topic comes up. I haven’t computed any statistics on the numbers above, nor did I see any presented here, but I didn’t find the data to look particularly strong here (but you noted study limitations and this is far from an area where I have any real expertise). Particularly, given that my gout is not necessarily well controlled yet (after a particularly severe set of flares I had to push for my PCP to consider starting allopurinol). My flare rate is on the order of once every 1-2 years, but the last flare took a couple months before it really stopped.
My two analyzed stones were predominantly calcium oxalate. The first was about 50/50 mono and dihydrate (this was an incomplete stone recovery from a ureteroscopy and lithotripsy so I don’t know if any nidus that may not have been calcium oxalate would have been recovered) the most recent one was 95% calcium oxalate monohydrate and 5% calcium phosphate. I’d have to imagine from this that there is either some hypercalciuria or hyperoxaluria at work here. I’m just in the seemingly ridiculous situation where I’m having to push really hard with my doctors that, given that I’m making and passing more than one stone a year, drink more water and see what happens is an inadequate answer at this point. Kind of just trying to explore what options I have to see if I can get one of my doctors to pursue for prevention (and hopefully avoid having to shop around for another doctor which takes months in my area right now).
Hi Matthew, You have a problem and presently no real information apart from the stone analyses. I cannot imagine why 24 hour urine testing and appropriate serum testing as well is not in the works. Here is my best about how to procede.Treatment sans knowledge of cause is commonly done and as commonly futile so I advise against it. With so many stones testing is the obvious approach and indeed you should advocate strongly for it with your physicians. Best, Fred Coe
Hi Dr. Coe,
Does Thiazides not work in some people to lower high urine calcium? I have been taking Chlorthalidone 12.5 to 25mg for over 3 years. My urine calcium levels vary from 400-500. My urine pH is around 6.3 and my urine citrate is in the 300s. My serum potassium and bicarbonate are normal. I follow the kidney stone diet: 3-4 liters of water daily, 1,500 to 2,000mg of sodium daily, I watch the protein, sugar and oxalates and consume 1,200mg of calcium daily from food sources only. My PTH and phosphate levels are normal. My vitamin D level is around 50 and the 1,25 Dihydrox is 46. I’m 56 years old and have osteopenia that’s getting worse with each dexascan. My nephrologist says there’s nothing else to do for my treatment? Do you think I have RTA? My nephrologist won’t prescribe potassium citrate because of my high urine pH. Lowering the sodium to 1,200mg hasn’t helped to lower the urine calcium (ex. One urine study I had a sodium level of 56 (1,288mg) with a calcium level of 470). Any help you can give me would be greatly appreciated!!!
Hi JoAnn, Very high urine calcium despite low sodium and other precautions, osteopenia – at a glance one think of post-menopausal osteoporosis in its rapidly progressive phase. Perhaps a bone directed drug like a bisphosphonate might benefit bone and also lower urine calcium losses. Of course I know nothing about your medical situation so this is a mere suggestion. Regards Fred Coe