For Scientists
Content Collections
Guide Book
Video Collection
New Book
Articles For Patients
PUTTING IT ALL TOGETHER
Well, here it is, the last pillar in the foundation. My goal is to enable patients to achieve successful stone prevention and I believe this requires a partnership with their physicians, a partnership in which they play a very active individual role. Patients after all are the ones who can manage diet, fluid intake, and life demands, only they can assure that 24 hour urine collections are representative of normal life, and, frankly, only they can decide on a life of long term prevention. Stones being rarely fatal and usually not a cause of progressive kidney disease, patients can elect prevention or not, and their physicians are in a role more like attorneys and accountants than authoritarian directors of events. But as in Eden, one can expect proper choices only if one has provided full knowledge, which I have set out to accomplish. By proper I mean most suitable to patients given full knowledge, for some may not care to exercise themselves so much as I think they must to be successful, whereas others may consider the work of prevention slight indeed compared to the consequences of continued stones. In any event, this article is the end of that cycle of enablement I can manage, and I put it here, as in all writings, as the chef puts out her best effort – to face the indifferent judgement of the gourmet.
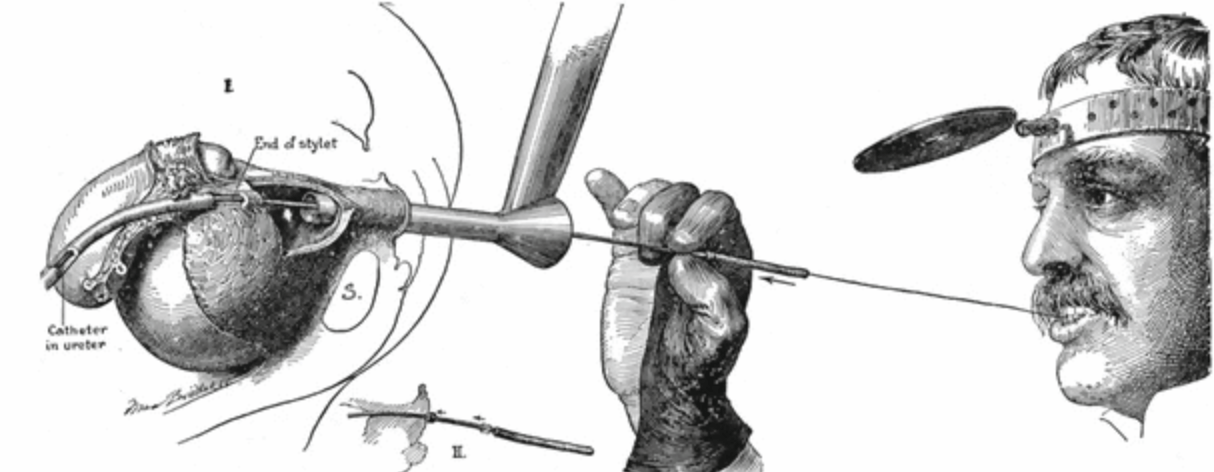
Ureteroscopy: Background and Current Controversies
Dr. Mike Borofsky authored a favorite article on this site – Pain from Kidney Stones. Now, he has authored our first article on stone urology, meaning the urological surgeries used for treatment of stones in the kidneys and urinary tract. Ureteroscopy is fast becoming the preferred approach, outstripping shock wave lithotripsy and percutaneous lithotripsy. This is because the instruments for ureteroscopy offer superior optics and are flexible and small enough to get from the urethra up into the kidneys and into all of the crevices of the kidneys where stones form and lodge. Armed with tiny but powerful laser fibers, the new ureteroscopes permit surgeons to fracture stones in the kidneys and turn them into mostly harmless dust that passes silently for days or weeks thereafter, or into small fragments they take out during the procedure leaving not a speck behind. It is a brilliant time to be a young urologist and use these marvelous instruments to do what would otherwise require a far more complex and risky procedure (percutaneous nephrolithotomy) or depend upon an indirect and often incompletely effective one (shock wave lithotripsy).
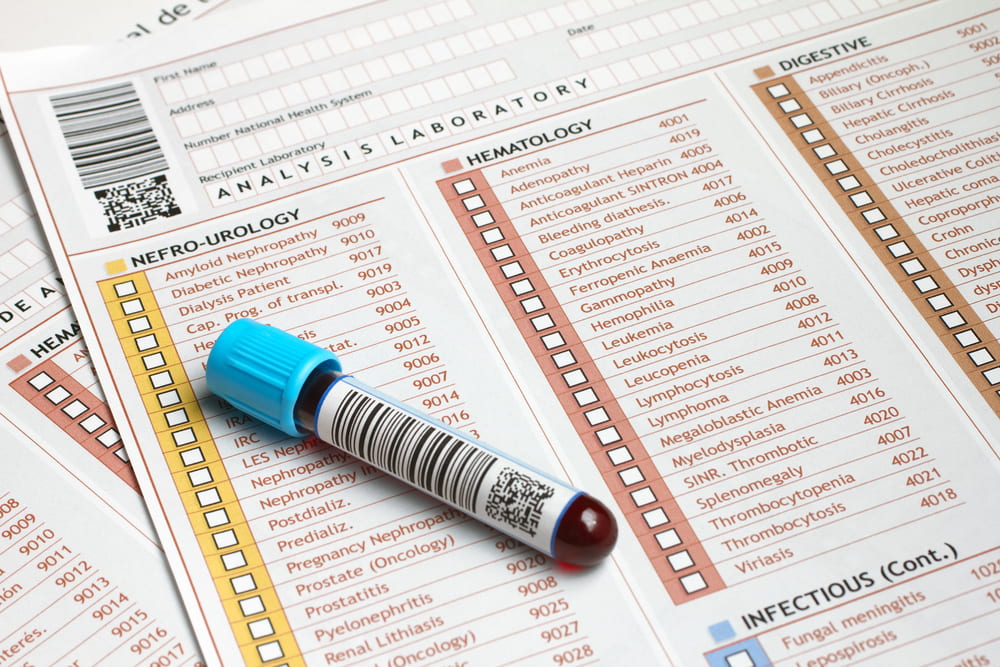
HOW TO READ YOUR KIDNEY STONE LAB REPORT – Uric Acid Stones
These two articles cover the main stone types, and this new one on uric acid parallels the prior one on calcium stones. Like the calcium stone article it is meant for patients, although physicians might like some of the nuances. The purpose is not to make patients into their own physicians but to enable them to understand their own stone forming abnormalities. My ruling hypothesis is that patients want prevention, and will embrace and implement the changes needed with more enthusiasm and endurance if they fully understand the goals. LIkewise if they can themselves follow the effects of their efforts on stone risk factors they will believe that what they are doing has real meaning. I know that hypotheses are for disproving, and I know someone may well do a prospective double blind randomized trial, some day, to test mine. Right now, I believe in the idea because of Eden whose resident twosome were not just told about the tree but exactly why they should not eat of its fruit. I know it is an unfortunate comparison, given the outcome, but much effort was expended on education. My source for the details, apart from the Hebrew Bible, is Milton, J: Paradise Lost; Books V – Viii.
HOW TO READ YOUR KIDNEY STONE LAB REPORT – Calcium stones
This site is meant to promote prevention and my current hypothesis is that enabling patients to read their own 24 hour urine tests with a professional eye will help achieve that aim. It is not an easy task. Lab reports, even the best of them, are dazzling arrays of numbers in often mysterious units. Even physicians have some work to do. But numbers are numbers and people can read them if they have the code. Here I have parsed out the main numbers for the calcium stones: Volume, calcium, oxalate, sodium, citrate and pH. Because this is the first article on reading this kind of report I also discuss collection quality, conversion of units – some labs report, as an example, calcium in mg/24 hour, others in mmol/24 hour, even mEq. So I introduce the simple conversions needed to use what I have written for a report with different units. Likewise I introduce how urine creatinine can be used to estimate collection quality. The supersaturation come at the end, as they should, being the final summary of everything. The tone is about that for trainees in nephrology or urology I have often worked with but with jargon elided and a focus on lab results per se. Those interested can follow the links into the thickets of the site which hold enough to satisfy most appetites. The main purpose is to enable patients to cast a cold eye on their own problems and on the results of treatment efforts so that in the event saturations can be effectively reduced and stone recurrence with them.
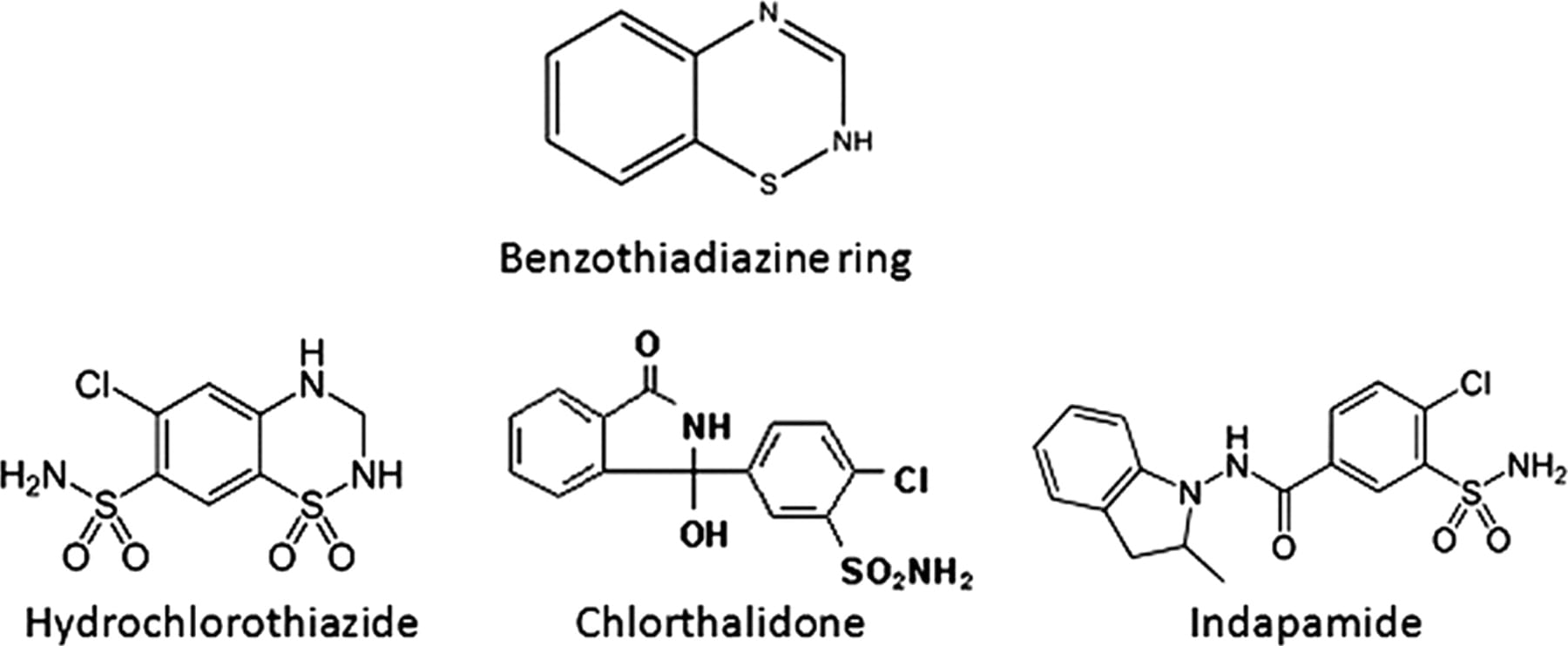
THIAZIDE DIURETICS FOR STONE PREVENTION
The thiazide type diuretics are able to reduce new stone formation and are an important part of stone prevention regimens. Here is all about these drugs: The trials that show they work; How they work; What they do for bone: Certain precautions in their use. To give a pill to someone is to throw a seed on unprepared ground – it is a sterile and doomed enterprise. All the features of prevention from diet and fluids and lifestyle come first, so that what one can do with them is being done. Then the drug will be most useful. And, you will know by the fall in urine supersaturation achieved. Whatever it was when stones were forming is too high, and real treatment means it has been reduced. After all that can be done without thiazide has been done, there will no doubt be residual supersaturation lowering needed, or one would not use the drug. The marginal benefit of the pill can be assessed by the extra fall in supersaturation it produces. Which supersaturations? Those related to crystals in the stones forming.
Five Steps to Stone Prevention
THE FIVE STEPS TO STONE PREVENTION
Ultimately we want to prevent kidney stones. Trial data, and my own large experience correspond in this one point: Prevention is a reasonable objective that can be successfully accomplished. Here is my own approach, simplified into five steps. They correspond to the overarching theme of this entire site: Stones require crystals; crystals follow the laws of physics; the force that drives crystallization is supersaturation; commercial vendors in the US provide supersaturation measurements in 24 hour urines at a reasonable price. So the steps are indeed simple: Know the stone crystals; measure the urine supersaturations; lower those urine supersaturations for the crystals in the stones being formed; keep them low. If stones persist, lower them more. It takes physicians to initiate this process, and there are complications such as the occasional systemic diseases which must be detected and treated in special ways. But it takes motivated patients to carry out the long term changes in fluids, diet, lifestyle needed, and to take the medications provided. It is time to focus here: Prevention is better than surgery. To help, I wrote a companion article several months ago about how to organize your medical stone prevention visits so as to get the most out of them.
How To Eat A Low Oxalate Diet
As part of a series, Jill offers this long and critical article on restricting diet oxalate. The problem is very complicated because oxalate is in a lot of plant foods and these are foods we need and often like. Using the Harvard oxalate list with cross referencing with another list from an excellent academic institution, Jill finds her way between the problems of too much oxalate and too little to eat. She offers a whole day meal plan outline people can fill in with their own preferences. Some key scientific papers are reviewed at the end to show the basis for her advice.
How To Eat a Low Sodium Diet
Jill Harris offers another of her amazingly useful and popular articles, this one on the how of low sodium diets. As she has done for fluids, Jill takes you into her own kitchen and dining room and shows you how to limit salt intake and yet fully enjoy your meals. She has had years of experience coaching patients about exactly this kind of crucial life management, and it shows. Her articles are the most popular on this site, and this one is destined to join her others in helping thousands of people actually do what their physicians ask them to do: Eat less salt to stop making stones.
Control Your Salt for Fewer Stones and Stronger Bones
Two good trials support lower sodium diets as a way of reducing new calcium stone formation and of protecting bones from calcium loss. The physiology behind these trials is detailed in the articles on idiopathic hypercalciuria and salt. In Italy at least, and in men with calcium stones and idiopathic hypercalciuria, a diet low in sodium, moderate in protein, and high in calcium leads to less stones than low calcium diet alone, and in fact to a rather low new stone recurrence rate. Among postmenopausal women, a high calcium low sodium diet brings bone mineral balance into the positive range: Bones add mineral. Neither trial is comprehensive in covering men and women, young and old, US vs. Italian cuisine, but they are the only ones we have of this quality, they are consistent with the science we have, and convincing. To me they are enough to recommend low sodium diet, moderation of diet protein, and high diet calcium for calcium stone formers with idiopathic hypercalciuria, recommend this kind of diet without reservation pending what I hope will be more trials which cover a wider range of patients and of ages. It is this kind of additional trial we really need in the US right now, substantial, bearing on really important diet interventions, and arising out of a sound scientific base.
IDIOPATHIC HYPERCALCIURIA (IH)
Idiopathic hypercalciuria may well be the most complex and important issue in all of medical management of calcium kidney stones. It arises within the elaborate systems that regulate calcium metabolism and produces both a risk of stone formation and of bone disease with fractures. IH is strongly familial, almost certainly genetic in origin, and present in children as well as adults. Treatments used include high calcium – moderate protein – reduced sodium diet, moderation of dietary sugar loads, and potassium citrate, and thiazide type diuretics, each of which act through different and reasonably well characterized pathways which cannot be understood without a knowledge of how IH works in the first place. Unlike stones themselves, supersaturation, or citrate, each a very large and important topic, IH cannot be presented well – at least by me – in separated linked articles but only in one article that carries its many intersecting physiologies along side by side and uninterrupted. Being a long and comprehensive article, foundational for this site and – to me at least – for comprehension of the whole topic of pathogenesis and treatment of nephrolithiasis, this article is not necessarily meant to be read all at once but rather used as a resource. I will cover the treatments of IH later on, in separate articles.