Here is my ‘bottom line’ on salt: The more you eat, the higher will be your urine calcium and – from what trial data I  can find – the higher your risk of forming stones and losing bone mineral. The big articles, on salt and on idiopathic hypercalciuria have put into place the structure I need to make this simple generalization acceptable. That is part of the reason I wrote them – to be a structure I can rely on and work off of.
can find – the higher your risk of forming stones and losing bone mineral. The big articles, on salt and on idiopathic hypercalciuria have put into place the structure I need to make this simple generalization acceptable. That is part of the reason I wrote them – to be a structure I can rely on and work off of.
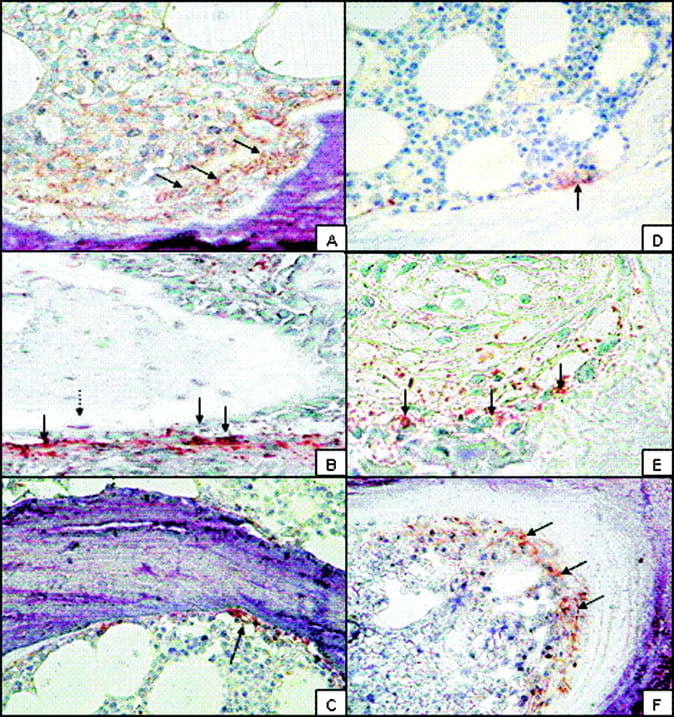
The large image is from a recent publication about the bone disease of idiopathic hypercalciuria. The full report is available and I recommend it.
So here is a new kind of article, from me to you, a call to consider action on your own behalf.
SALT AND STONES
Professor Loris Borghi and his colleagues, who performed the only prospective trial of reduced salt intake on actual stone formation wrote a fine review in 2014 that can be obtained in PDF form without charge. The review is a powerful argument for restraint, and well referenced.
Salt and Urine Calcium
The main point is that higher sodium intake raises urine calcium. The mechanisms are essentially that the way the nephrons get rid of salt force them to lose calcium more or less in due proportion.
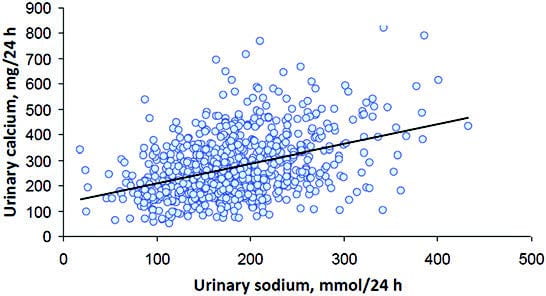 Here is their graph of urine sodium – which faithfully mirrors sodium absorption from diet – on urine calcium in men. I have already introduced millimoles in th
Here is their graph of urine sodium – which faithfully mirrors sodium absorption from diet – on urine calcium in men. I have already introduced millimoles in th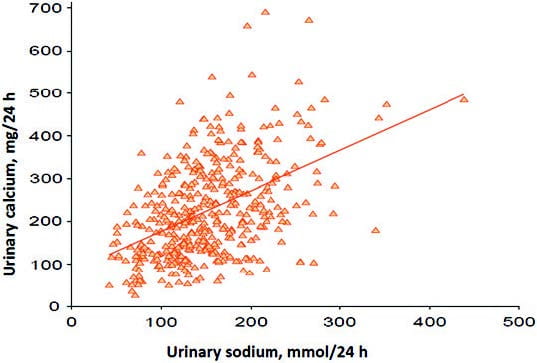 e sodium article so you can review the matter there. Women are the same. The graphs look different because the top of the vertical axis for men is higher than that for women, so the slope is higher for women. I would have prefered equivalent axes but take what I can get.
e sodium article so you can review the matter there. Women are the same. The graphs look different because the top of the vertical axis for men is higher than that for women, so the slope is higher for women. I would have prefered equivalent axes but take what I can get.
You already know about urine calcium and stone risk from the big hypercalciuria article: Above 200 mg/day is the beginning of increased risk. Take another look at these graphs. To get under that number you need to lower sodium intake below 100 mmol/day in men and about the same for women.
 I have made a graph just like theirs, from all of the data I could collect in which salt intake was deliberately varied in a trial setting and changes in urine calcium measured.
I have made a graph just like theirs, from all of the data I could collect in which salt intake was deliberately varied in a trial setting and changes in urine calcium measured.
Here, prospective trials are circles, observational data are triangles. Blue points are from people with idiopathic hypercalciuria, red points are from normal people. This graph is perhaps more generalizable than those shown above because it comes from many separate trials from different laboratories.
It shows that IH involves an increased slope dependence of urine calcium on urine sodium, which latter reflects diet sodium intake. At urine sodium levels below 100 mEq/d the curves begin to overlap. The newest FDA guidelines for US people is an upper limit of 100 mEq/d and an optimal value of 64 mEq/day.
Curhan has already shown that in observational data more urine calcium means more risk of stones. All that is missing so far is to prove that less sodium leads to less stones, and that is what Borghi did some time ago.
Salt and Calcium Kidney Stones
Borghi’s trial was not strictly a lower salt trial because several changes were made at once, and it lacked some of the trappings of an ‘ideal’ trial in that no one can not know what they are eating – so double blinding about treatment is an absurd notion. But it was a trial of considerable importance and generated some insights that, I believe, are perhaps not fully appreciated.
What He Did and Why
My article on idiopathic hypercalciuria reviews the complex evolution of thought concerning pure ‘absorptive’ vs. ‘renal’ mechanisms and eventually comes to rest on a not unexpected consensus: High absorption and reduced renal calcium conservation both seem present. As a result people with IH will not in general – though there may be specific exceptions – tolerate low calcium diets without incurring risk of bone mineral loss. Until recently, in the absence of compelling evidence for a wide spread renal mechanism for hypercalciuria, low calcium diet was a common means for reducing calcium stone recurrence.
It is against that background that the Borghi trial needs to be analysed. The trial set out to compare ‘…the traditional low calcium diet with that of a diet containing a normal amount of calcium but reduced amounts of animal protein and salt’ in terms of new calcium stone formation in patients with IH – unfortunately only men. One stated reason for the trial was data from Curhan showing that high calcium diets seemed protective against stones – inverse statistical association between diet calcium intake and onset of stones (I have referenced his later paper (2004) which shows effects of age on the calcium – stone link; his earlier paper was in 1993). Another was the large body of data available even then linking high salt intake with high urine calcium excretion. A third was the established fact that low calcium diet can increase urine excretion of oxalate which would balance the fall in urine calcium so lower urine calcium would not effectively lower urine calcium oxalate supersaturation.
His diets were of Italian cuisine and therefore not necessarily transferable to the US. But the key compositional differences are certainly simple enough: High calcium low sodium reduced protein – Calcium 30 mmol (1,200 mg), sodium 50 mmol (1150 mg sodium), protein 93 gm. Low calcium diet – Calcium 10 mmol (400 mg), avoidance of highest oxalate foods (walnuts, spinach, rhubarb, parsley and chocolate). Both diets included advice to maintain good hydration.
His male patients all had IH using the research criterion of 300 mg of urine calcium daily and at least two documented kidney stone passage events in the absence of any named systemic cause of stones or hypercalciuria. From 354 candidate cases, they excluded 234 and were left with 120, 60 in each of the two diet groups into which patients were enrolled using a random allocation system. Both groups were eating a lot of salt before the trial – above 200 mmol (4600 mg) daily.
What He Found and Why
WHAT
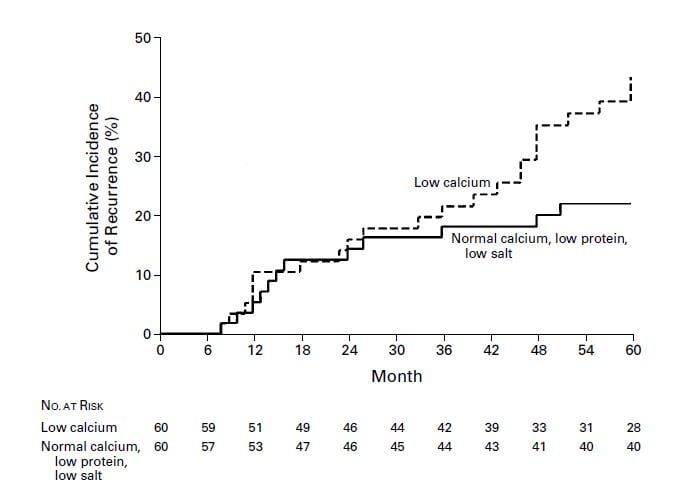
This famous graph simply shows the life tables of the two groups. After about 2 years, the normal calcium, low sodium reduced protein diet patients formed many less stones than did those eating the ‘traditional low calcium diet’.
The numbers in the table below the graph show how many people were ‘at risk’ over time – made it that far into the trial and did not drop out. They are comparable, and adequate for the one big conclusion: Low sodium high calcium reduced protein diets work better than low calcium diets and given what we know know about IH are a lot safer for bones.
WHY
But why did the numbers of stones fall.
Supersaturation. Everything on this site should point to a greater fall in supersaturation as the mechanism, so let’s look there. Calcium oxalate supersaturations (rounded without variance estimates) were 10, 8.1, 7.3, 6.8, 6.7, 4.8, and 4.7 for baseline, 1 week, and years 1-5 inclusive in the low calcium diet group. Corresponding values for the reduced sodium, protein and high calcium diet were 9.6, 4, 5.1, 4.7, 4.5, 3.7, and 3.5. Bolded means lower than low calcium diet by a variety of comparisons. One would have liked the calcium phosphate supersaturations given that they may be even more important than those for calcium oxalate, but we do not have them.
Urine Calcium. The low calcium diet and the high calcium reduced sodium and protein diet gave about the same levels of urine calcium, about 6 – 7 mmol (240 – 280 mg) daily with no differences between the groups.
Urine Oxalate. Because high calcium intakes reduce urine oxalate, and low calcium intakes raise it, the low calcium diet group consistantly excreted more oxalate: baseline, 1 week, and years 1-5 inclusive: 357, 422, 422, 411, 422, 433, 411 mmol/day vs. 411, 322, 344, 322, 333, 333, 333 mmol for the lower sodium high calcium reduced protein group – bolded means significantly lower. It is this, the lower oxalate excretion, that lowered the calcium oxalate supersaturation; urine volumes were the same.
Urine sodium. How well did people follow the diet? As expected, the low calcium diet group continued to lose above 200 mmol/day of sodium. The low sodium group with a goal of 50 mmol/day actually excreted between 110 and 130 mmol, except for week one which was indeed 51 mmol/day. So the outcome was double the goal. The urine calcium was, however, no higher despite the high calcium intake, meaning that the low sodium overcame the effects of the higher intake.
What I say
The trick is this: If sodium and protein are controlled one can eat a lot of calcium – 1200 mg – and yet keep urine calcium oxalate supersaturation reasonably low because the high calcium intake will lower urine oxalate and the low sodium will lower urine calcium.
The protein effect is not simple. Protein imposes an acid load and was thought to raise urine calcium because of the acid loading which would mobilize bone mineral. But more modern studies have shown this is not the case. Protein increases calcium absorption and urine calcium excretion even when enough alkali is given to offset the acid production from protein. A decent literature indicates that protein probably promotes bone mineral retention, not the opposite.
I have deliberately not referenced this last paragraph as I mean to deal with the protein effect in another article and do not want to bog us down.
Let us say that 93 grams of protein would be about 1 – 1.2 gm/kilogram body weight, not really very low. They used more from milk, breads and pastas than US people usually do, but the Italian cuisine favors that approach.
Perhaps for the moment I can say – though I will be criticized – that if we achieve reduced salt intakes of about 100 mmol (2300 mg sodium) daily and keep protein intake around 0.9 – 1.1 g/kg (all routine 24 hour kidney stone urine tests report a protein catabolic rate (PCR) value which gives an estimate of protein intake in gm/kg) we can eat 1200 mg of calcium in the diet and achieve protection against new calcium stones if we are men with IH. A women study is important here, and one in the US.
SALT AND BONES
I already reviewed the bone story in kidney stone formers. I know my article is long and difficult but it is accurate and brings together material from other sources that are also difficult.
Bone disease follows stone disease like a shadow. It is hidden among our patients until the first fractures. Often we can be so focused on the stones we forget about the silent but perhaps even more serious problems that are developing in bone and will become obvious enough years later.
We not only do not have bone oriented trials for stone formers, we do not even have a deep enough knowledge of the mechanisms producing bone disease, which is probably in large part from idiopathic hypercalciuria and from intentional or unintentional reduction of diet calcium intake combined with high sodium diets.
But at least one really wonderful bone trial points to low diet sodium and high diet calcium as a promising treatment to maintain bone mineral balance in IH and perhaps prevent fractures.
Bone Balances
There is every reason why reduced salt intake coupled with high calcium intake should benefit bone mineral balance. Trials are few indeed. This one is so elegant and convincing I have selected it.
Birgit Teucher pointed out in 2003 that salt loading should impair bone mineral balance, and that direct proof of such a link was wanting in humans. Her review is worth a careful read, as to me it seems a preliminary to her massive balance study in women testing the effects of high and low calcium and salt intakes. If her review is adequate, as I believe, her balance study seems to stand alone up to its publication, and to the present time – as best I can tell.
In my last paragraph and the following analysis of the main research I refer to Teucher as if she did the work alone. I mean no disrespect to her many coauthors but detest the passive voice and the tedious refrain of ‘and colleagues’.
Her own study is a crossover randomized trial of low and high sodium (70 and 191 mmol) and low and high calcium (518 and 1284 mg/day) calcium diets in a square design: low calcium and sodium, high calcium and sodium, low calcium high sodium and high calcium low sodium, each consumed for 40 days with at least 4 weeks washout in between. Sixteen postmenopausal volunteers entered the study and 11 finished all four dietary interventions.
The way she did the diets is of interest, to me at least. She constructed a ‘basal’ low sodium low calcium diet to which she added amounts of sodium in meal preparation and as supplements, and calcium exclusively as calcium carbonate. The supplements were taken with the meals, so far as I can tell.
She measured calcium balance two ways. Urine and fecal calcium were measured directly on days 30-40 of each meal cycle, and could return a classical estimate of overall systemic calcium balance. Her key approach went further. She used a complex calculation made from two stable calcium isotopes, one (calcium 42) orally the other (calcium 43) intravenously. This latter double isotope technique permits an estimate of net calcium absorption and bone mineral balance.
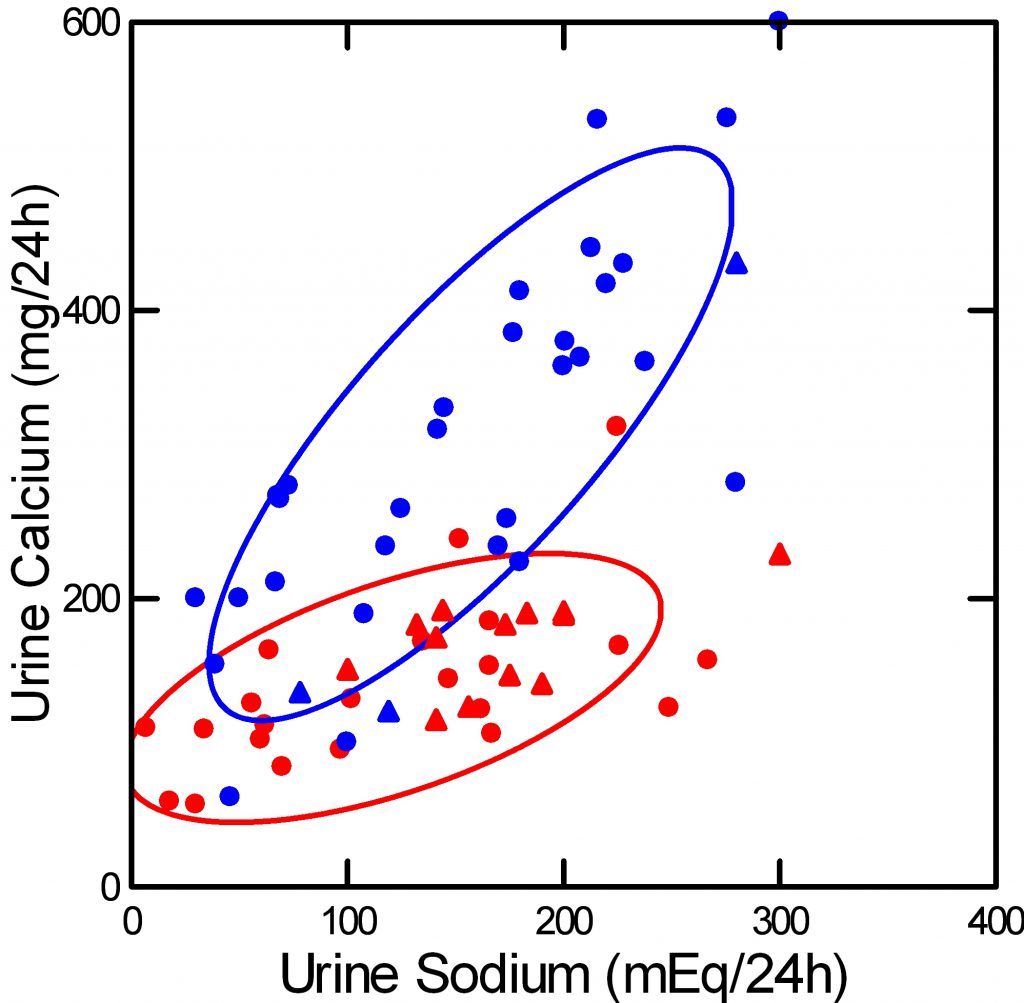
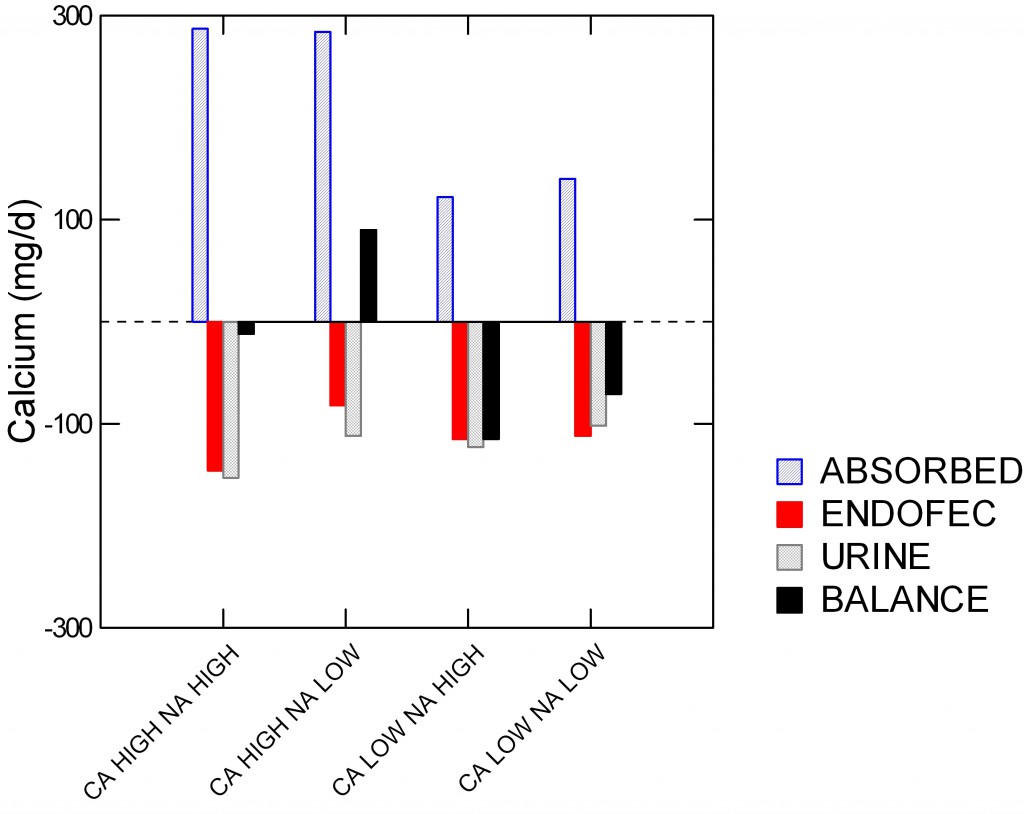 She published her results in a group of tables, but I have graphed the main findings for clarity here. My source is her Table 2.
She published her results in a group of tables, but I have graphed the main findings for clarity here. My source is her Table 2.
The vertical axis shows calcium in mg/day. The horizontal axis shows the four diet periods.
The crosshatched blue bars show calcium absorbed from diet. It is lower, of course, with the low calcium diet.
The next bar to the right is secretion of calcium from blood back into the intestinal lumen by pancreas, liver, and other transporters; it is a net loss of absorbed calcium from the body and can be determined only using the isotope studies.
The third bar, counting from the left, is simple urine calcium excretion, which is loss from the body.
The fourth bar is net bone mineral balance.
Positive balance occurred only with the high calcium low sodium diet and resulted from a fall in endogenous fecal (endofec) calcium secretion and urine calcium combined, even though in her statistical analysis only the urine loss difference was significant between high and low sodium periods on the high calcium diet.
Implications for Present Stone Treatments
Does this mean that stone formers with IH who restrict their daily sodium intakes below 100 mmol (2300 mg) and add calcium supplements to their diets to achieve 1,200 mg/day will avoid bone disease?
No, it does not.
We have no comparable study on female hypercalciuric stone formers and no study of men. Notice how low were the urine calcium levels in her women – 112 and 153 on the low and high sodium, high calcium diets. Perhaps hypercalciuric stone formers would benefit greatly, perhaps not. Perhaps men, hypercalciuric or not, would behave differently. Likewise for premenopausal women with IH vs. those who are postmenopausal.
But – that word again! – reduced sodium high calcium diet seems to protect at least Italian men with IH from more calcium stones. It is a good diet alternative. And, it just so happens it is more or less the same diet that Teucher used for her women.
It is also in line with modern general health recommendations. I have already referenced the CDC and American Heart recommendations for reduced diet sodium. The diet calcium recommendation of 1,200 mg is well known.
We need more trials. But while those of us on the sidelines wait, I think low sodium high calcium diets are right for IH stone formers, men and women, and will use them, as I do use them, with enthusiasm and persistence.
As a practical point, Teicher taught us that supplements can be taken with meals and the calcium will go into bone. So perhaps it is not so critical that all the calcium comes from food alone.
Implications for Those Who Fund and Perform Stone Trials
What We Need
We need more trials like her trial. How about IH men and women?
We need more trials like his trial. How about women, how about a US cuisine?
Teucher used supplements with meals in place of food calcium and got good bone results. What happens with IH stone formers? Is this not grounds for a good trial?
It is diet sodium, calcium, and protein that we need to sort out, following the wonderful work by Borghi and Teicher.
What We Do Not Need
Why nibble at straw when surrounded by sweet delights?
Need we prove again that thiazide or potassium citrate work? I say no.
Do we need to test again if high fluids are a good thing for stone prevention? I say perhaps, but with minimal enthusiasm.
Borghi did a fine trial of fluids years ago. It was among the first items I put up on this site. In a randomized but of course not double blind trial, 12 of 99 first time calcium oxalate stone formers with a daily urine volume averaging 2.6 liters formed a second stone over 5 years vs. 27 of 100 well matched patients whose urine volume averaged about 1.1 liters. If we were to do this again, how likely is it the results would be different?
What Might Hold Us Back from Really Worthwhile Trials?
Why not tackle the the less well studied issue of diet sodium, calcium, and protein in US men and women? It bears not only on stones but on bone disease, and is alternative and in addition to fluids which, quite frankly, every reasonable physician freely recommends because without cost and without risk.
I have thoughts about why diet sodium and protein, and effects on bone, have not been studied.
What Borghi and Teucher did is hard to do.
Her study was heroic.
His was long, arduous, and risky – who knew what might be the final answer.
We cannot redo his study as he did it. No one would use low calcium diet as a contrast anymore, so the contrast would have to be an active drug like thiazide or potassium citrate.
Both studies were done outside the US; our cuisine is distinctive and perhaps US citizens might not adhere to diets as well as Italians.
Is it not time to climb higher, breathe a thinner if more invigorating air?

Dr. Coe,
All I can say is WOW. I have struggled alone and with sporadic visits to my urologist without knowing my urine oxalate levels or other details, much less any idea of how to interpret and apply research to my own diet. I am so thankful to have found your site. You are truly helping people far beyond your university practice.
I find your site very useful. I am a 33 y/o male with a history of chronic stones since age 19. I have been flexitarian for 10 years. Prior to that I was a vegan for 5. As a stone former (calcium phosphate) I have tried just about everything. Currently I drink roughly 3.5 L of water a day. I eat a lower/ish ( I try!) sodium diet and take no calcium supplements.
I have low testosterone and take testosterone cypionate. I am worried about bone loss due to the calcium excretion and low testosterone levels I experience. I have been prescribed both thiazide or potassium citrate which I am not taking now. Thiazides helped control my blood pressure but dropped my potassium level.
I cannot take potassium due to having interstitial cystitis, which flares up severely with even small amounts of potassium rich foods or medications. Without the potassium I cannot take the thiazide anymore due to having dangerous potassium levels on that thiazide. My urologist declined to use Spirinolactone as a diuretic but I don’t really know why.
My question is what do you recommend for someone like me, in order to prevent stones when water and lower sodium diets are not enough? Thank you in advance. My lab info is below. My results have mostly remained the same with the exception of calcium which has risen from 199 about 6 mos ago (while on thiazides).
6.854 Urine PH
24 Hr Calcium 238
24 Hr Uric Acid 0.689
24 Hr Citrate 200
24 Hr Oxalate 38
Urine Volume 2.62
Supersaturation Caox 4.76
Supersaturation Uric Acid 0.10
Supersaturation Cap 3.06
24 Hr Potassium 87
24 Hr Sodium 153
24 Hr Creatinine 2326 mg/d
24 Hr Creatinine Per Kg Body Weight 27.0
24 Hr Calcium Per Kg Body Weight 2.8
24 Hr Calcium 102
Just realized this part was missing:
24 Hr Sulfate 44
24 Hr Ammonium 66
24 Hr Chloride 158
24 Hr Magnesium 178
24 Hr Phosphorus 1.506
24 Hr Urea Nitrogen 10.34
Protein Catabolic Rate 0.9
Hi Jacob, of course your situation is very complex, but I offer these comments for you and your physician to consider. You form calcium phosphate stones and have idiopathic hypercalciuria, accelerated bone loss from testosterone deficiency, or both, and your urine study shows a very high CaP supersaturation of 3 because of high pH, extremely high urine phosphate, modestly high urine calcium and fair to middling urine volume. Urine ammonium is very high suggesting your potassium stores are depleted despite a high urine potassium level. Urine sodium is high at 150 meq/day. Perhaps you might want to discuss with your physician another liter of urine volume, marked reduction of diet sodium to 65 mEq/d which is 1,500 mg sodium, and perhaps you might want to figure out the source of the high urine phosphate – this is usually soda or sports drinks, but you would have to be the judge. With very low sodium and high urine volume you might do well. A small dose (12.5 mg) of chlorthalidone – with the low sodium diet! should be usable if you remain saturated for CaP above 1. These are complex notes, I know, but your physician and you might want to think about them. Incidentally amiloride can spare potassium loss, and is not so complex as spironolactone. Given how complex your situation is, my ideas may be completely unworkable, and if so, my regrets. Let me know, Regards, Fred Coe
Dr. Coe, thank you for all of your articles on this site, it helps me understand a lot even though I feel like I get lost sometimes in the science.
I always drank lots of water to avoid kidney stones as my father had them (not sure of which type; also, he died of bladder cancer at age 56). In my 40s I entered osteopenia and last year my DEXA showed my left hip slipped into osteoporosis at age 56. (I should tell you I have Hashimoto’s and had breast cancer and bilateral mastectomy at age 53 but am okay now, not taking Tamoxifen because it made me sick.)
I worked hard since last year’s DEXA scan to build bone (lots of weight-training and jumping exercises, eating calcium rich foods, silica and calcium supplements, affirmations that spoke of my left hip getting stronger, yada yada.)
This year I had to take a 24-hour calcium test with my DEXA. So stopped all calcium supps 6 prior to the test. Results showed calcium excretion at 472mg/24 hours. (PTH intact was 57). So now I’m IH, too.
My doc told me to drop all calcium supplements immediately to prevent kidney stones and to start a diuretic because excessive calcium excretion is depleting my bones.
Then she checked this year’s DEXA, which showed that in one year (at age 57) I increased bone density in all areas:
* 6.4% in left hip (yay for affirmations!)
* 5.7% in right hip
* 2.9% in my spine
So I’m no longer in osteoporosis but the osteo doc still wants me to go on a diuretic to prevent further bone loss — even though I gained bone density this year (and I intend to gain more next year.) She also wants me to stop all calcium supps to prevent kidney stones.
Three questions for you:
1) If I am successfully rebuilding bone density without a diuretic, do I really need a diuretic?
2) If I must take a diuretic, should I be concerned about potassium loss? Should I also take potassium citrate?
3) As I understand some of your articles, a low sodium and low protein diet despite a reasonable calcium supplementation program might help prevent kidney stones. I’d like to try that and would take half of my typical calcium supplementation (maybe 800 mg calcium daily) would that be within recommended parameters?
Some lab numbers I am being so presumptuous to add for your review… I understand that I must make all decisions with my doctor’s advice and your response is not a medical diagnosis.
BLOOD PANELS
PTH Intact 57 pg/mL
Glucose 97 mg/dL
BUN 14 mg/dL
Creatinine 0.66 mg/dL
GFR >60 mL/min
Sodium 142 mmol/L
Potassium 3.9 mmol/L
Chloride 103 mmol/L
Bicarbonate 26 mmol/L
Anion Gap 13 mmol/L
Calcium 9.1 mg/dL
Total Protein 6.6 g/dL
Albumen 4.5 g/dL
Bilirubin total 0.30 mg/dL
AST (SGOT) 18 U/L
ALT (SGPT) 16 U/L
Alkaline Phos 65 U/L
Phosphorus 3.0 mg/dL
C-Telopeptide, Beta-Cross-Linked, Serum 313 pg/mL
URINE-24 Hour
Calcium Concentration 29.3 mg/dL
Calcium Total 24 hr 472 mg/24 hr
Volume 1610 ml (I was told to drink less than I normally do, so I cut my fluid intake in half)
Creatinine Concentration 104 mg/dL
Creatinine Total 24 hr 1674 mg/24 h
Hi Bonnie, I see no urine sodium. I am sure your physician will want the lowest possible diet sodium intake – 1500 mg or less – so as to lower your urine calcium as much as possible while permitting a more liberal calcium intake from food or supplements. Remember the calcium supplements need to be with the meals, never by themselves. If you use a diuretic, the lower the diet sodium the less potassium wasting and the lower the dose you need. I prefer long acting agents like chlorthalidone and the dose can be 12.5 mg a day or even every other day – 23 hour half life – especially with little diet sodium. In the one bone trial, high calcium low sodium produced positive bone mineral balances. Regards, Fred Coe
Thank you so much for your response!
I do always take supplements with my chow, so no worries there. Also am keeping the sodium intake below 1500 mg now that I know about it. My doc said nothing about sodium, I just learned it here (thank you for this resource!) I’m making plenty of notes for my next visit with her.
But do you think I could skip a diuretic if I am not losing bone density (but rather gaining it in substantial amounts without pharmaceuticals) while having IH? Especially if I keep my sodium low?
I mean, let’s assume that I was excreting too much calcium all those years that I was sliding into osteoporosis. Now I’ve shown I can successfully rebuild bone density with proper exercise and diet even though I am IH.
So couldn’t I forego a diuretic if I keep my sodium low? Or am I risking kidney stones?
Can you tell that I hate to take pharmaceuticals? 🙂
You are so kind to answer everyone’s questions on this site like you do. I very much appreciate your time.
Hi Bonny, The only bone trial this definitive concerning diet calcium and sodium showed positive balances – more bone mineral – with high calcium low sodium diet. So if that works for you a drug may not be necessary. Show the article to your physician and see what she says. Regards, Fred Coe
Hi Dr. Coe, I have been reading the site and came across this thread. In the post above by Bonnie, she mentioned her doctor suggested she immediately stop calcium supplements fearing they would cause kidney stones. I’m confused by this as I thought calcium supplement, specifically calcium citrate for oxalate stones, would help with prevention by binding to the oxalte, as discussed on this site. Or am I misunderstanding the information? Calcium oxalate stones run in my family and I was planning to start calcium citrate supplements and diet modification.
…and a few follow up questions, Dr. Coe… Our 24 yr old was just dx with two 8mm stones on the left. One in the lower pole and one in the renal pevis, and a 2mm on the right. He has been passing blood since 3/27/18, but so far no pain, which leads me to believe they have not yet entered the ureter. His reg doc prescribed Flomax, but he has problems with balance due to CP, and since dizziness is one of the side-effects, I did not want to start the meds until he started showing more symptoms. He passed a stone in Sept ’17 which was 100% calcium oxalate, and one prior in May ’17 that sent us to the ER. Finally, my questions: Should we see a urologist for removal? Is it possible to reduce the size of these stones with copious amounts of lemon water and a calcium supplement? Thank you.
Hi Andrea, Flomax is just a convenience med to aid in stone passing. But his urologist needs to be sure that obstruction is not present as it can injure kidneys. As for prevention, it is a process and here is my best on the subject. Size of stones, sorry to say, is not amenable to treatment, but prevention of more is very feasible; thence this whole site. Regards, Fred Coe
Thanks for your time, Dr. Coe, and for the time you put into this site. It is much appreciated. The urologist said I made the right decision not to give the Flomax since the stones are still inside the kidney. Our son is scheduled for laser surgery to remove the two 8mm.
Hi Andrea, confusion is an easy thing. A 1000 mg calcium diet will lower urine oxalate very well, but also raise urine calcium – and stone risk – unless (there is that key word!) unless you also lower sodium intake below the US tolerable upper limit (2300 mg) and ideally below 1500 mg. So it is the proper diet is never one thing but a manifold of things and all go together – for stone prevention and good health. Take a look at this article. When one item – like calcium – comes up in isolation, physicians and their patients can indeed suffer confusion. Regards, Fred Coe
Dear Doctor Coe,
Excellent site! My question is, can low diet sodium (<1500mg) lead to hyponatremia in people who take thiazides chronically? How can you deal with that? I am scared to lower my salt intake due to that.
Secondly, to avoid adverse effects of thiazide therapy, do you do any time breaks in chronic use? I read somewhere that after 2 years they lose part of their actions and they need a break. Do you see that from your experience?
Thank you!
Hi Demetrius, Indeed on thiazide and low sodium diet there is risk of hyponatremia, but managed properly that should not happen. One should achieve low sodium diet per se, then observe the urine calcium level – I presume this is all in treatment of stones due to idiopathic hypercalciuria and no systemic diseases are present. If the urine calcium level is not below the risk level, or if more stones form, then one adds a minimal amount of long acting thiazide like diuretic to lower urine calcium further. Here is the way I have followed. I have no evidence that thiazide effect varies over time. Regards, Fred Coe
I am very sorry for the double post. Please delete one of the two, as they didn’t appear right away in my monitor.
What would the impact be of calcium citrate as the supplemental calcium? If calcium with food binds oxalates in the digestive tract and increased citrate is good for lowering stone production, would usage of calcium citrate be a good option?
Hi Chuck, calcium citrate will work for binding oxalate. All calcium supplements are alkaline and will raise urine citrate. The citrate in calcium citrate is metabolized to the same alkali as in Tums. So choice is for price and ease of use. Remember that food calcium surpasses supplements, so use as much of it as you can and then add supplements if needed. Center the calcium where the oxalate is, and be sure to limit sodium so the extra calcium stays in bone not in the urine. Regards, Fred Coe
Dear Dr. Coe,
Your web site and private coaching with Jill Harris has been such a blessing! So much so that I am now participating in half marathons and mountain racing. Do you have general recommendations for electrolyte replenishment during and following endurance efforts? Thank you!
Hi Linda, Given the fluid and electrolyte losses of exercise, there is no reason a stone former would not follow the same fluid replacement as other athletes. I realize that low sodium is important for stone prevention, but sweat sodium losses and water alone can result in falling serum sodium, so with mountain racing do as all the other do to keep safe. During the runs, urine sodium will be low because of sweat losses. Since you race only sometimes, keep the diet sodium low. Regards, Fred Coe
Thank you so much Dr. Coe!
Dear Dr.Coe,
I am 79, 73 when diagnosed with hyperpqrathyroidism, 75 when operated on.
I have been reading your website, and I’m very impressed with the knowledge you share on it. I have a question for you:-
I was diagnose with HPT disease in 2013 and operated on in 2015. The aberrant glands were never found, and 6mths later I was given Cinacalcet. 30mg tabs. I was prescribed 2 but only took one, which was very effective in reducing my calcium/PTH levels to currently normal levels. Last year (2019) I was diagnosed with 10 (!!) kidney stones.
I am thinking – it seems kidney stones are a risk with HPT, so should I have been given an ultrasound scan or CT scan on diagnosis, to check for stones? Or at the very least a warning of this risk, and advice on diet? Because of a heart condition diagnosed at the same time as I was operated on – given a pacemaker, I had included more heart friendly veg etc. in my diet, all of which turn out to be high in oxalates. Beetroot, soy, sweet potatoes, nuts, kale, peanut butter, dark chocolate, all of which I love! I have never added salt to my cooking, or to my food for years, so that is a positive. I am currently trying to eat foods that are low in oxalates, very limiting and a bit dreary.
The stones are in both kidneys, 2 are largish 10 and 5mm, the others 3x3mm, 3x2mm, 1x1mm. I am wondering if the rash of smaller stones are due to the high oxalate changes I have made to my diet over the past 5 years
Kind regards
Patricia
Hi Patricia, Cinacalcet will lower serum calcium but can raise urine calcium. Given stones, your physicians need to measure 24 hour urine calcium, which may be quite high. If it is, neither low sodium nor thiazide will lower it, as far as I know. Oxalate is not the likely cause of stones, but proper 24 hour testing will show what the causes are. So, get 24 hour testing and then treatment as needed. Regards, Fred Coe
Dr. Coe,
The information you have published here is a breath of fresh air! Scientific and credible, but understandable to the layperson. Thank you!
I am writing for a bit of confirmation. For eight years I have been trying to rebuild bone I discovered at age 50, was already lost. At that time I embarked on a 2 year journey with a nutritionist who recommended a high-quality calcium supplement, that included of course magnesium & other wonderful things. At the end of 2 years the DEXA revealed I had lost 13% of my bone density! At that point I began to be terrified to ingest any calcium by supplement. Even when several docs over the years tested the urine calcium the results were within the ‘normal’ limits – likely due to low calcium intake. Finally my bones have become so fragile, I submitted to Fosomax. At that time I felt it was ‘safe’ to increase my calcium intake and did so for several months before the next 24 hour urine calcium check.
Interesting new number: 877.1. Recheck two weeks later to rule out human error. Result: 451.4.
Most recent result: 833. The most recent labs were taken after three weeks on 2 meq./day Potassium Citrate.
My gums are receding dramatically and previously only stopped receding when I stopped the calcium.
Yes, my doctor recommended I eat low sodium ( under 2 g./day ) and take in – by food & supplement, 1200mg. calcium. She also wanted me to take HCTZ, but I understand I should not take it because I am allergic to penicillin. However, I am still terrified to take and/ or ingest additional calcium.
Potassium 4.7
PTH within range
I share only other labs that are out of reference range:
Phosphorus 4.8
Until I read your post, I had no idea why I was doing Potassium or low sodium, or that increasing calcium at this point might not decrease my bone density. Yet, I still hesitate. How can I be sure that if I increase my calcium intake, it will result in the desired end result of building bone rather than taking it away? ( By the way, I have only ever had one kidney stone. )
Thank you so much for your posts, your time and for sharing your expertise.
Hi Ruth, I suspect you have idiopathic hypercalciuria and probably peri or postmenopausal bone loss as well. Your massive hypercalciuria can be the combine of the genetic hypercalciuria and rapid bone mineral loss. I presume your serum calcium level is normal – primary hyperparathyroidism can do this. I presume your serum PTH level is not suppressed; some uncommon conditions suppress PTH and promote bone loss. You are an uncommon kind of patient and should seek help from a university mineral center, as what you have is not clear and poses very complex issues of treatment. Regards, Fred Coe
Dear Dr. Cole,
I am a 65 year old woman who has been diagnosed with severe osteoporosis .I am not taking any meds for it as yet. I’ve never had kidney stones and hav never broken a bone. I am in excellent physical shape (5’1″ 94 lbs.).
My endocrinologist has run a series of blood tests, all of which came back normal. She did a 24 hour urinalysis ….the timed UR Calcium is 296 mg. She wants to put me on chlorthalidone. I do not have high blood pressure and I am concerned about the side effects of this drug.
Rather than go on the medication, shouldn’t I try to lower my sodium intake for a month and then do the UR test again?
I’ve heard that high levels of vitamin D can contribute to calcium in urine. My vitamin D level was 70.
What do you suggest Dr. Coe, that I should do? PLEASE respond to my email assign as you can! Thanks so much.
Hi Caryl, I presume you have idiopathic hypercalciuria – a familial and presumably genetic trait that promotes bone mineral loss. A key element in saying this is presumed normal blood calcium. Low sodium high calcium diet – as in the linked article – promotes bone mineral gain, and thiazide like diuretics (chlorthalidone as an example) do the same, so the diet is certainly a good step and the drug not at all unreasonable. THe diet might be tried first and the drug added (low dose is best, 12.5 mg/d). If bone disease is severe enough to pose serious fracture risk, many advise bone directed treatments such as bisphosphonates. Very high vitamin D intakes can injure bone, and your level is a bit high (70) but not quite in the range with proven bone disease. Regards, Fred Coe
Is there a rapid test covered by insurance since the key to reducing the risk of calcium oxalate stones is to have my urine tested frequently.
Hi Jacques, No. But Litholink pricing has usually been very reasonable and insurance coverage for stone formers the same. Regards, Fred Coe
Dr. Coe
I ordered a Vitamin panel on myself from Quest (provider order not required) and it included Iodine level and mine was low. Here it is:
IODINE, SERUM/PLASMA
Desired Range: 52-109 mcg/L
40 LOW
I believe this result is low because I’ve been following a low sodium diet for my kidney stones for several years around 1500mg/day and without extra iodized salt I believe it’s causing this, what are your thoughts? Will this low value affect anything else in my body? I did read a person can form a goiter if it’s too low or other thyroid issues. Would it be safe to take an iodine supplement so I don’t get extra sodium added back into my diet to bring the level up or is this something not to worry about?
Thank you!
Hi Diane, How clever! I wonder how many more people are showing this given US sodium consumption is falling for general health reasons. I see no reason one cannot take an iodine supplement. My multivitamin (Centrum Silver) contains 150 micrograms of iodine (100% of daily requirements) so I presume anyone on the market will do. I am not an expert on iodine. I looked up daily iodine requirements on Google and found that same value but there are foods that interfere with absorption. Here is a link to the list. Regards, Fred Coe