Kidney stone types
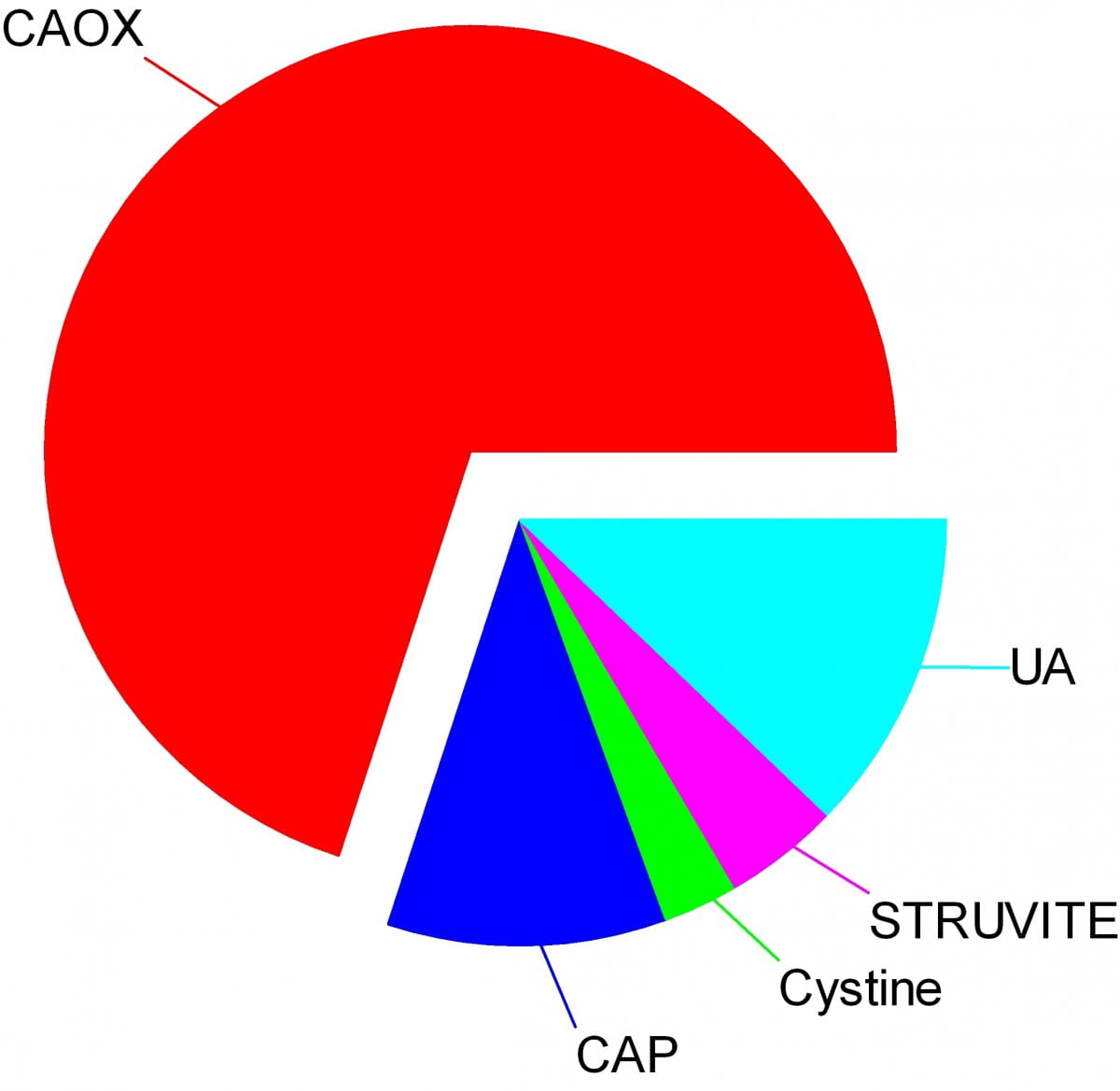
Crystals make stones and their names signify the kidney stone types. Here are the names of the crystals that make the stones: CAOX, Calcium Oxalate; CAP, Calcium phosphate; UA, Uric Acid; Cystine; Struvite.
The wedges on my pie chart show the relative abundances of stone types in our large population of stone forming patients. Calcium oxalate stones predominate by a wide margin in our clinic and in all others I know of.
The names, matter because the whole science of stone prevention focuses upon stone crystals. Each kidney stone crystal creates its own unique illness and requires specific treatment. That is why we name stones by the names of their crystals and why when stones are analysed the results are reported by these very same names.
Being a bold and rather large graphic, the featured picture does what I intended, brings the main facts into view as, at a circus, the great animals and the small animals circle the ring by way of an introduction. Come. I will show you all the common stones, like at a fashion show, or a circus parade. You can watch as they go by and remind yourself, or wonder, which ones might have been yours.
Here they are.
Which type do you have?
You might think your doctors know what stones you have formed, but don’t rely on it. People move, doctors move, health records are far from ‘all electronic’. That stone report from 4 years ago could lie in a dusty filing cabinet, your new doctors unaware it exists. Worse, it could hide in a dresser drawer and you forgot it you put it there. Perhaps even more worse, the stones might stay in that drawer, never analysed at all. Find the stones, find missing reports, urge analysis by your physicians. They can help you most if they know your stone analysis.
When they do not know, physicians can still mount prevention efforts but with less focus and probably less effect than when guided by a knowledge of the crystals. So always seek treatment. If a stone comes along the way, make every effort to get it analysed.
Why should you care to know all this?
Because you will conduct much of your own treatment, and over many years.
Since stones tend to recur, prevention requires treatment over long periods. These treatments work by altering urine chemistry in a direction that minimizes the risk of forming crystals. Such altering of urine chemistry requires control of fluid intake, lifestyle, and diet, and sometimes additional use of medications.
Just as the sailor who aims along a chosen track against the random, misdirecting, confusing sea and air maintains a constant way in proportion to that skill which comes from knowing the way of the boat, patients who aim to keep a certain kind of condition in their urine despite the demands and temptations of the world do so, I believe, in proportion to skills that come from knowing how their work and lives and foods affect their bodies, and how those crystals form which they so much desire to prevent.
Put another way, knowledge is power.
Why is this article so long?
I wanted to put all five main types of kidney stones. That makes a long story. But probably you will care to read about only your own type.
I should mention here, to save a lot of confusion, that stones often contain mixtures of crystals.
The pie chart refers to the most common crystals in a stone, for which the stone is usually named. Much of the time, minor crystal components are not crucial, but sometimes – to jump forward a bit – they are. Even a trace of struvite or cystine, for example, can have great diagnostic importance.
Calcium stones
Calcium Oxalate Crystals
In the great circle atop this page article, the calcium oxalate stone, being most common, occupies a lion’s share of the space. 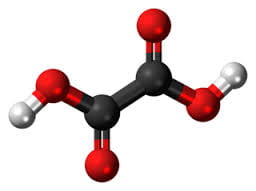
The calcium oxalate crystal forms when calcium combines with oxalic acid. Oxalic acid (at left), a dead end waste product that the kidneys remove, contains two carbon atoms (the large black spheres), four oxygen atoms, and two hydrogen atoms (silver).
At the acidity of urine, the positively charged hydrogens leave their negatively charged oxygens. As a result the oxalate molecule carries two negative charges. In the figure at right one negatively charged oxygen attracts the hydrogen of a nearby water molecule (H – O -H) while another attracts a positively charged calcium atom.
You can imagine how another oxalate ion (the name for a charged molecule in water) could attract the same calcium, or another calcium atom attract the bottom oxygen on the oxalate molecule so the chain extends and makes a crystal. You can see more about this in a video I made. Broadly speaking – though my more expert colleagues may bridle at such a simplification – the calcium atoms and oxalate molecules combine by the attraction of their opposite charges.
The calcium oxalate kidney stone comes in two varieties, calcium oxalate monohydrate and calcium oxalate dihydrate. The former are harder and therefore more resistant to fragmentation by lithotripsy. Likewise, the former appear more often when elevated levels of urine oxalate are present.
Calcium oxalate stone formers
From Systemic Diseases
Sometimes this kidney stone arises from a systemic cause, like bowel disease, primary hyperparathyroidism, or primary hyperoxaluria. Only physicians can establish that a known disease – like bowel disease – is the cause of stones. Only physicians can discover underlying primary hyperparathyroidism as a cause of stones. Patients cannot do much for themselves except provide as complete a medical record as possible.
Idiopathic
Most of the time this kidney stone arises simply from the interplay between inheritance, diet, and aspects of daily living. We call such patients idiopathic calcium oxalate stone formers, from Greek ἴδιος idios “one’s own” and πάθος pathos “suffering”.
Even though physicians discover the links between daily living and stone production, and select those changes that can prevent new stones, patients themselves must create and maintain those changes. I believe patients can so this in proportion to how well they understand what is needed, and why. When changes in daily life are not enough, physicians add medications, so even then patients remain active therapists for their own disease.
Stones usually form on kidney surfaces
About one million nephron units make up a normal adult kidney. The calcium oxalate kidney stone type does not grow in the tubules of the nephrons but ‘outside’ them, on the surfaces of the renal pelvis where final urine collects and drains through the ureter to the bladder. Here is a video that shows how they can form.
Calcium phosphate crystals
Phosphate ion and urine pH
Calcium phosphate stone crystals form when calcium atoms combine with phosphoric instead of oxalic acid and produce the calcium phosphate kidney stone.
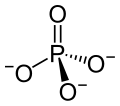 Phosphoric acid is simply a phosphorus atom (shown as the ‘P’ in the line drawing to the left) with 4 oxygen atoms bonded to it. One oxygen atom has two lines for its bond to phosphorus; this oxygen cannot provide any charge with which to bond calcium atoms to make a crystal. The other three have ordinary bonds that are shown by a line, and a dashed and solid arrow. These two arrows mean simply that the oxygens lie above and below the plane of the paper – so if you built the molecule with sticks and balls it would have a three dimensional shape.
Phosphoric acid is simply a phosphorus atom (shown as the ‘P’ in the line drawing to the left) with 4 oxygen atoms bonded to it. One oxygen atom has two lines for its bond to phosphorus; this oxygen cannot provide any charge with which to bond calcium atoms to make a crystal. The other three have ordinary bonds that are shown by a line, and a dashed and solid arrow. These two arrows mean simply that the oxygens lie above and below the plane of the paper – so if you built the molecule with sticks and balls it would have a three dimensional shape.
One of the three negatively charged oxygens never has a hydrogen on it in urine but only in exceedingly acidic solutions. A second charged oxygen is always occupied by a hydrogen atom in urine.
This makes the third oxygen, variably occupied by a hydrogen in urine, a tie breaker.
In a urine of average normal acidity (pH around 6), most of the tie breaker oxygens have their hydrogen leaving the phosphate ion only one negative charge. Not enough to make a crystal.
When the urine is abnormally alkaline (pH above 6.3 or 6.5), the variable oxygen becomes charged so the ion has two negative charges that can combine with calcium to make crystals. For this reason the calcium phosphate kidney stone tends to occur in people who produce a more alkaline urine than those who produce calcium oxalate kidney stones.
Brushite vs. hydroxyapatite
Much like calcium oxalate, calcium phosphate crystals begin simply as one to one pairings of doubly negative phosphate ions with doubly positive calcium atoms. This initial crystal is named brushite. Brushite, which is an equal mixture of calcium and phosphate ions, can convert to hydroxyapatite (HA), which has a more unbalanced proportion of calcium to phosphate. Hydroxyapatite crystals make bones hard.
Because less soluble than brushite, hydroxyapatite cannibalizes brushite. The organic molecules in urine modify this process.
Calcium Phosphate stone formers
From Systemic diseases
Primary hyperparathyroidism and renal tubular acidosis raise average urine alkalinity (higher urine pH) and foster calcium phosphate kidney stones. Many uncommon genetic diseases do the same.
Idiopathic
Idiopathic calcium phosphate stone formers share a common set of traits. Perhaps because urine contains far more phosphate than oxalate, they form more frequent and larger stones than idiopathic calcium oxalate stone formers. Often the stones originate as crystal plugs at the terminal ends of the kidney tubules. More crystals deposit over the end of the plug open to the urine, to make the final stone. Crystal plugs damage the cells that line the tubules and cause local scarring.
Uric acid stones
Uric acid crystals
Structure and charged sites
A breakdown product of DNA and RNA, uric acid forms crystals in abnormally acidic (low pH) urine. Obese and diabetic people, those with gout or kidney disease typically produce abnormally acid urine. I know how the urine becomes acid, but leave it for elsewhere on the site.
Uric acid, the molecule we are interested in here (shown to the far right), has two linked rings made of carbon atoms (they are at the angles where lines join), with  interposed nitrogen (N), oxygen (O), and hydrogen (H) atoms.
interposed nitrogen (N), oxygen (O), and hydrogen (H) atoms.
This molecule has only two charged sites, the nitrogen atoms at the bottoms of the rings. In urine of pH 6 or so, one nitrogen lacks its hydrogen and therefore carries a single negative charge. In more alkaline solutions both nitrogens lack hydrogens, but urine does not normally achieve such alkalinity (pH>8).
When urine pH is low (<5.5) and both nitrogens have their hydrogens, the molecule lacks any charged site, so water can no longer find a hold on the molecule. It crystallizes. It simply leaves the water as water droplets themselves form from the high and vaporous late afternoon clouds and fall from the air as the warm rains of springtime.
Relation to water
Water molecules are each a single oxygen atom (large ball) bonded with two hydrogen atoms (small balls) as in this picture from Wikipedia. The hydrogen side has a positive, the bare side of the oxygen a negative charge. So water molecules link to each other,  positives to negative surfaces, to make up the clear and seemingly continuous fluid we drink, swim in, and hold up umbrellas to keep off of us when it rains. They link by charge at angles, shown by the number ‘1’ so as to make up a three dimensional macrame.
positives to negative surfaces, to make up the clear and seemingly continuous fluid we drink, swim in, and hold up umbrellas to keep off of us when it rains. They link by charge at angles, shown by the number ‘1’ so as to make up a three dimensional macrame.
To be ‘in solution’ means to have some charge to which water molecules can link up with by attraction. Calcium atoms are positive and become surrounded by a shell of water molecules facing it with their bare negative surfaces. Oxalic and phosphoric acids have negative charges and are surrounded by water molecules pointing their positive or hydrogen sides to them.
Uric acid at neutral pH has its one negatively charged nitrogen water can grasp. But when pH falls, and neither nitrogen has any extra charge for water to bind with, how can the molecule remain among the water molecules? It cannot. The molecules stack into solid crystals and fall from solution.
Uric acid stone formers
The stones can be orange – red, large, and numerous
The stones can be red or orange because uric acid crystals absorb hemoglobin breakdown products that are red – orange pigments in urine. Sometimes uric acid crystals pass in urine as a red orange gravel.
Uric acid does not have to connect itself to some other atom or molecule to make a crystal, in the way that calcium must bond with oxalate or phosphate ions to make calcium oxalate or calcium phosphate crystals. When pH is low enough to extinguish its charge, uric acid can crystallize very fast, in seconds, and pass as an orange gravel in the urine. If retained, such crystals can grow rapidly into large stones. Because there is much more uric acid in urine than there is oxalic acid, uric acid stones can grow very large and rapidly. Some fill up the entire collecting system of the kidney.
Urine pH controls stone formation
But because the whole process depends almost completely on the acidity of the urine, uric acid stones are very easy to treat. Just a modest amount of supplemental alkali will make the urine of almost any patient alkaline enough that the hydrogen atoms are removed from the one crucial charged nitrogen. Water can bond there so uric acid remains in solution. Because so simple, treatment prevents stones with certainty. Relapse need never occur.
Mixed stones require special care
Unfortunately, however, stones commonly contain uric acid mixed with calcium oxalate. In this case, one needs to track down the cause of the calcium oxalate stones as well as make the urine alkaline enough to stop uric acid stones from forming. Calcium phosphate crystals mix with uric acid only rarely, because it takes a rather alkaline urine to remove the hydrogen atoms from phosphate so it has two negative charges and can bind efficiently with calcium atoms. At that higher pH, uric acid will have its charge site and remain in solution.
Struvite stones
Urea and the planet
Kidneys cannot make struvite. Bacteria make it. Not all bacteria, either. It takes bacteria that normally thrive in the soil, and they do it for ancient and compelling reasons. These bacteria produce the kidney stone named Struvite after Heinrich Christian Gottfried von Struve (1772–1851).
Animals deposit urea (at left) all over the planet when they urinate. Plants cannot use it.
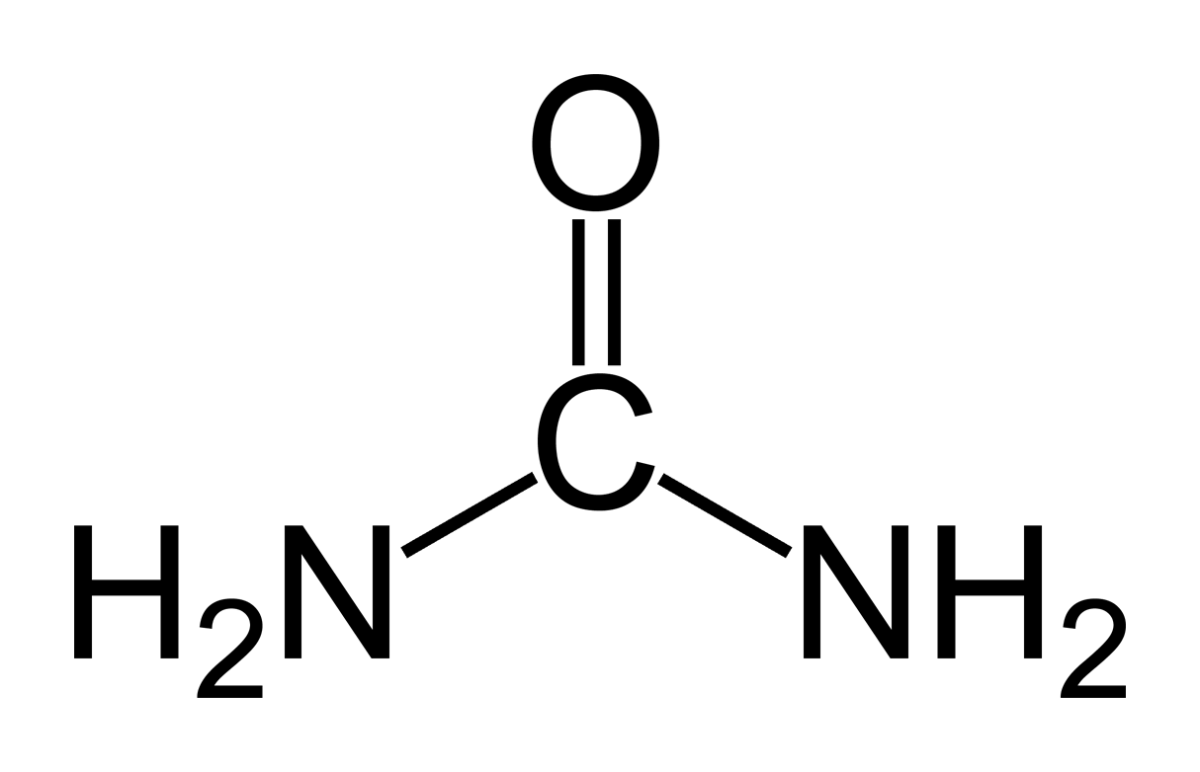 Like oxygen, nitrogen is an essential for life yet dangerous. It is integral to proteins, DNA and RNA. As these molecules are broken down and remade, some of their nitrogen slips by and can form poisonous compounds unless caught up in safe waste products. Of these, the main one, urea, contains 2 nitrogen atoms bound to a single carbon atom (‘C’ in the picture to your left).
Like oxygen, nitrogen is an essential for life yet dangerous. It is integral to proteins, DNA and RNA. As these molecules are broken down and remade, some of their nitrogen slips by and can form poisonous compounds unless caught up in safe waste products. Of these, the main one, urea, contains 2 nitrogen atoms bound to a single carbon atom (‘C’ in the picture to your left).
Uric acid contains 4 nitrogen atoms (look back at the picture of it). Birds and reptiles excrete most of their nitrogen as uric acid; mammals like us excrete nitrogen mainly as urea.
As the animals of the world urinate on the soil, their urea brings nitrogen to plant roots, but the plants cannot use it. They cannot release the nitrogens from the carbon atom that holds them. Those soil bacteria that make struvite crystals have an enzyme, called urease, that can release the nitrogen for plants to use as their nitrogen supply.
So, soil bacteria with urease maintain the nitrogen cycle of the earth.
Struvite crystals
As they release nitrogen from its carbon in urea, the nitrogen takes up a proton making ammonia (NH3). Ammonia is a powerful alkali and takes up another proton.
As it does so, the working bacteria surround themselves with spheres of very alkaline fluid enriched with ammonium ion (NH4) that carries one positive charge. Soil magnesium ( an atom with two positive charges) and phosphate sans all of its protons (an ion with three negative charges) spontaneously form their triple salt: three negative phosphate charges, two positive from magnesium, one positive from NH4).
The crystals anchor the bacteria and help create a porous nitrogen rich soul good for plants to grow in
The struvite kidney stone
Why they start
Because urine is filled with urea, soil bacteria that get into the urinary tract can break it down to ammonia and create struvite from the magnesium and phosphate urine always contains.
You might wonder how soil bacteria get into the urinary system.
Because we eat them, with foods that are not cooked, and they become part of the intestinal bacterial population from an early age. In us and around us, they find a way into the urinary system, especially in women whose shorter urethra makes entry easier. No matter how skillfully used, any instrument put into the bladder can carry our personal soil bacteria with it.
What they do
Because they live among molds and fungi, soil bacteria easily mount resistances to antibiotics, so antibiotics given for a urinary tract infection will tend to kill sensitive bacteria and select out those that can resist them.
Soil bacteria can produce struvite stones de novo, or infect calcium stones to produce a mixed stone. Either way, struvite stones are infected by their very nature. They can become huge. Their bacteria can injure the kidneys, even enter the bloodstream and cause sepsis.
Treatment is a mix of thoughtful surgery and selection of antibiotics after such surgery to kill bacteria that remain. If the stones are a mixture of struvite and calcium crystals, new calcium stones need to be prevented.
Cystine stones
Inherited kidney abnormality
 Lemon yellow with a sugary coating these form only in people who have an inherited kidney disorder called cystinuria.
Lemon yellow with a sugary coating these form only in people who have an inherited kidney disorder called cystinuria.
Although the kidneys function well, they permit abnormal amounts of four amino acids to enter the urine. Three do not matter that we know of. The fourth makes crystals and the cystine kidney stone type.
Cystine
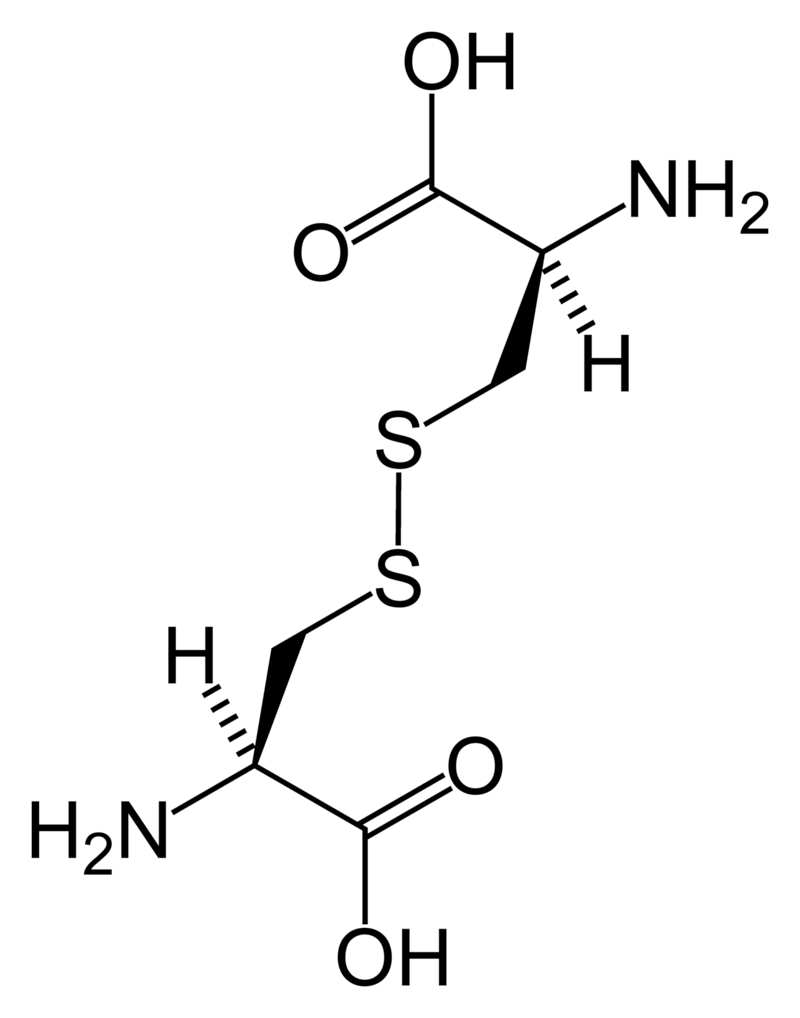
Cystine (left) forms through the coupling of two identical amino acids – called cysteine – through their sulfur atoms (‘S’ in the line drawing).
Each cysteine contains two carbon atoms – not shown except as corners – bonded together (shown by the single long line that connects the two corners) as in oxalic acid.
One carbon atom has 2 oxygens bonded to it; the other has one nitrogen (which makes it an amino – nitrogen containing – acid), a hydrogen atom, and a sulfur atom. As for phosphate, the dashed and solid arrows simply mean the hydrogens and sulfurs lie above and below the plane of the page and a stick model would have a three dimensional shape.
Cystine Crystals
Cysteine itself is very soluble because the sulfur atom has an appreciable negative charge.
But the big, long cystine molecule has very little charge because the sulfurs bind to each other. So, like uric acid, cystine loses intimacy with water molecules and simply leaves the solution as crystals. Also like uric acid, the process is fast.
Cystine stones
Because people with cystinuria lose large amounts of cystine in their urine stones readily grow large, and fast.
Stones probably form in the urine itself. But cystine crystals can plug the ends of kidney tubules, as calcium phosphate crystals do, causing cell damage.
Since cystinuria is an inherited disease, stones may begin in childhood.
Effective treatment always requires very large amounts of fluids to dilute the urine. The few effective drugs resemble cysteine. Their sulfur groups bond with cysteine to form a ‘mixed disulfide’ more soluble than cystine. But their side effects can limit use.
Rare stones
Here and there we find patients who make uncommon crystals and require very special care.
Uric acid, as an example, can form odd crystals such sodium or ammonium acid urate, especially in people with bowel disease and chronic diarrhea.
Anti-viral drugs can crystallize in urine and form stones only recognized for what they are through stone analysis.
Very rare disorders of metabolism can produce molecules which crystallize in the urine, for example 2-8 dihydroxyadenine.
Although it can take a while before the right answer emerges, stone analyses will put physicians on the right track for these special cases.
The end of a very long post
That’s my parade.
The common animals and the rarer animals have gone by, and you have glimpsed the main ones, big and small.
The one point is what it was at the beginning. Each kind of kidney stone has its own ways, and treatment requires we know which one you have.
Likewise, for whatever that one may be, it is good to know as much about it as you can know. For long term prevention of stones is hard to come by and ultimately what the patience and and consistency of patients themselves matters most.
If you don’t know which stones you have made, find out.
Track down old reports and pull them together.
Keep copies and send everything to the doctors who care for you.
Fred Coe MD


I have suffered with several kidney stones, had several lithotripsy procedures and just recently had my 2nd PCNL (?) stone removal. I just received the analysis report and the latest stone is 70% calcium phosphate (apatite), 10% calcium carbonate 10% calcium phosphate (brushite) 10% calcium oxalate dihydrate.
Presently I take allopurinol and calcium citrate as prescribed by my urologist. What lifestyle/diet changes do I need to make to prevent future stones?
Hi Lisa, Your stones are calcium phosphate – apatite with some brushite – and a bit of calcium oxalate. Allopurinol is not appropriate for such stones, and I am sure when your urologist has had a chance to review the stone crystal composition she/he will want to stop it. These stones occur because of high urine calcium excretion and an alkaline urine pH. Be sure to get a full evaluation including 24 hour urine studies. The main treatment is to lower urine calcium via low sodium diet – 1500 mg of sodium daily is ideal. High urine volume of at least 2.5 liters daily – 3 liters of fluid – is important. Potassium citrate is a questionable approach because on the one hand it will raise urine pH more but also will tend to lower urine calcium. If between low sodium intake and high volume your urine supersaturation with respect to calcium phosphate is not below 1 then a long acting thiazide type drug is ideal. Regards, Fred Coe
I have suffered with several kidney stones, had several lithotripsy procedures and just recently had my 2nd PCNL (?) stone removal. I just received the analysis report and the latest stone is 70% calcium phosphate (apatite), 10% calcium carbonate 10% calcium phosphate (brushite) 10% calcium oxalate dihydrate.
Presently I take allopurinol and calcium citrate as prescribed by my urologist. What lifestyle/diet changes do I need to make to prevent future stones?
Hi Lisa, Your stones are calcium phosphate – apatite with some brushite – and a bit of calcium oxalate. Allopurinol is not appropriate for such stones, and I am sure when your urologist has had a chance to review the stone crystal composition she/he will want to stop it. These stones occur because of high urine calcium excretion and an alkaline urine pH. Be sure to get a full evaluation including 24 hour urine studies. The main treatment is to lower urine calcium via low sodium diet – 1500 mg of sodium daily is ideal. High urine volume of at least 2.5 liters daily – 3 liters of fluid – is important. Potassium citrate is a questionable approach because on the one hand it will raise urine pH more but also will tend to lower urine calcium. If between low sodium intake and high volume your urine supersaturation with respect to calcium phosphate is not below 1 then a long acting thiazide type drug is ideal. Regards, Fred Coe
What a great article(s)! Thank you! I read thru all the comments and didn’t see anyone with my type of stones. I recently had cholecystitis attack & was hospitalized overnite. The ultra sound, CT scan and X-ray also showed stones in my left kidney which was no surprise to me as 40 years ago, at age 23, I had (old-fashioned open) surgery to remove a very large stone that caused my kidney to become blocked with urine. Horrible time! That stone was said to be calcium oxalate (nothing else reported back then – 1977). Fast forward to last month’s gall bladder attack & imaged kidney stones in same kidney that had stone in 1977. The see a cluster of small stones & a significant single stone – none of which are blocking. I did pass small stones several times over a year ago (40 yrs later!) after adding nuts (almonds) to my diet, not knowing they are very high in oxalate. In Oct 2015 I passed 27 stones in one bathtub sitting & saved them. I passed a few at a time over about a month. I save those too. Research suggested drinking water with lemon juice & adding B6 supplement & increasing calcium. I’ve been drinking 70 oz of water highly juiced up with fresh lemon juice (with no added sugar or anything else) since passing those 27 small stones, and nothing has passed since that I know of. I have no clue why they now see that small cluster but I also had a horrible diet up until a month ago when I changed it due to the gallbladder attack. I was eating huge amount of chocolate daily and daily carrots & celery, all of which are high in oxalate. For about 18 months, I was drinking a daily powdered chocolate Slim Fast shake made with powdered non-fat milk in which I increased the milk powder thinking the calcium would bind with the chocolate in my intestines & pass out thru my stool. There have been no stones passed since & after increasing water, lemon & adding the B6 and calcium supplement, BUT I ended up messing up my gallbladder! To make a long story end quicker, I dropped the 27 stones passed in 2015 to the urologist who consulted in the hospital last month during gallbladder attack & got the stone analysis today. I have no idea how many of them they analyzed but the report says Uric Acid Dihydrate 80% Calcium Oxalate Monohydrate (Whewellite) 20%. I was surprised by the Uric Acid part because my blood tests from last month’s hospitalization said my Uric Acid level was 4.4 ml/dl. Perhaps that means nothing when it comes to stones, but could you please suggest what I should eliminate or do now besides staying hydrated and keeping oxalate below 50 mg/day & the lemon, B6 (via a balanced B vitamin supplement)? Should I keep taking calcium supplements as I’m not to eat daily with the gallstones issue & I’m dairy intolerant, never having liked milk since a toddler, so any milk I had a child was forced & I often gagged. I later found that chocolate milk was better tolerated, but I think I’ve had dairy issues since early on & not having much dairy since a teen and able to refuse milk, might have caused my original stone in 1977 at age 23. Sorry this was so long! Tks!
Hi Lynn, Mixed uric acid calcium oxalate stones are not at all uncommon. Blood uric acid itself is not directly relevant to formation to such stones. Uric acid stones form when urine is too acidic – low pH, and that is the only important cause. Treatment is always simply to raise urine pH with potassium citrate, a common dose is 10 – 20 mEq twice daily with 24 hour urine followup to assure successful results. The pills are expensive and one can get equivalent alkali from certain beverages. As for the calcium oxalate part, there is something more in your urine chemistries and you should be properly evaluated. Here is a good plan you and your physician can implement. Regards, Fred Coe
What a great article(s)! Thank you! I read thru all the comments and didn’t see anyone with my type of stones. I recently had cholecystitis attack & was hospitalized overnite. The ultra sound, CT scan and X-ray also showed stones in my left kidney which was no surprise to me as 40 years ago, at age 23, I had (old-fashioned open) surgery to remove a very large stone that caused my kidney to become blocked with urine. Horrible time! That stone was said to be calcium oxalate (nothing else reported back then – 1977). Fast forward to last month’s gall bladder attack & imaged kidney stones in same kidney that had stone in 1977. The see a cluster of small stones & a significant single stone – none of which are blocking. I did pass small stones several times over a year ago (40 yrs later!) after adding nuts (almonds) to my diet, not knowing they are very high in oxalate. In Oct 2015 I passed 27 stones in one bathtub sitting & saved them. I passed a few at a time over about a month. I save those too. Research suggested drinking water with lemon juice & adding B6 supplement & increasing calcium. I’ve been drinking 70 oz of water highly juiced up with fresh lemon juice (with no added sugar or anything else) since passing those 27 small stones, and nothing has passed since that I know of. I have no clue why they now see that small cluster but I also had a horrible diet up until a month ago when I changed it due to the gallbladder attack. I was eating huge amount of chocolate daily and daily carrots & celery, all of which are high in oxalate. For about 18 months, I was drinking a daily powdered chocolate Slim Fast shake made with powdered non-fat milk in which I increased the milk powder thinking the calcium would bind with the chocolate in my intestines & pass out thru my stool. There have been no stones passed since & after increasing water, lemon & adding the B6 and calcium supplement, BUT I ended up messing up my gallbladder! To make a long story end quicker, I dropped the 27 stones passed in 2015 to the urologist who consulted in the hospital last month during gallbladder attack & got the stone analysis today. I have no idea how many of them they analyzed but the report says Uric Acid Dihydrate 80% Calcium Oxalate Monohydrate (Whewellite) 20%. I was surprised by the Uric Acid part because my blood tests from last month’s hospitalization said my Uric Acid level was 4.4 ml/dl. Perhaps that means nothing when it comes to stones, but could you please suggest what I should eliminate or do now besides staying hydrated and keeping oxalate below 50 mg/day & the lemon, B6 (via a balanced B vitamin supplement)? Should I keep taking calcium supplements as I’m not to eat daily with the gallstones issue & I’m dairy intolerant, never having liked milk since a toddler, so any milk I had a child was forced & I often gagged. I later found that chocolate milk was better tolerated, but I think I’ve had dairy issues since early on & not having much dairy since a teen and able to refuse milk, might have caused my original stone in 1977 at age 23. Sorry this was so long! Tks!
Hi Lynn, Mixed uric acid calcium oxalate stones are not at all uncommon. Blood uric acid itself is not directly relevant to formation to such stones. Uric acid stones form when urine is too acidic – low pH, and that is the only important cause. Treatment is always simply to raise urine pH with potassium citrate, a common dose is 10 – 20 mEq twice daily with 24 hour urine followup to assure successful results. The pills are expensive and one can get equivalent alkali from certain beverages. As for the calcium oxalate part, there is something more in your urine chemistries and you should be properly evaluated. Here is a good plan you and your physician can implement. Regards, Fred Coe
My 9 year old son has had a very bright white, chalk-like residue in his underwear for several months. It is usually dried when I find it, and when I flake it off, it becomes powdery. He has had this once every week or so for 4-5 months, and I am now noticing that on days when he has it he often has an episode of stomach pain, which is pretty painful. He has never before complained of stomach pain so this made me pay attention and I noticed the correlation. At his doctor’s request, I was recently able to scrape some off to take in to the lab, and the stone analysis came back as 65% calcium oxalate dihydrate (weddellite) and 35% carbonate apatite (dahilite) Additionally, a 24 hour urine test indicated a calcium/creatinine ratio of 245 (normal 30-20-) and an elevated creatinine level of .81 (normal 0.11-0.68). The doctor said for him to follow a low oxalate diet and follow-up with a pediatric nephrologist, which we will. Is it important to find the cause of the high creatinine and calcium rather than just treat the symptom? This doesn’t seem normal for a child his age – he does not consume an unhealthy diet at all, and is not dehydrated. Is there any particular test I should request? Thank you – your insight is much appreciated.
I forgot to include a bit of family history in my original question. My aunt (would have been my son’s great aunt), died of nephritis at age 7. I don’t know if that’s anything to consider as far as possible hereditary/genetic factors, but thought it’s worth mentioning.
Hi Natalie, Genetic diseases with female renal failure and stones are not very common, and given it was labeled nephritis and led to death I suspect it was really an intrinsic kidney disease unrelated to stones. Regards, Fred Coe
My 9 year old son has had a very bright white, chalk-like residue in his underwear for several months. It is usually dried when I find it, and when I flake it off, it becomes powdery. He has had this once every week or so for 4-5 months, and I am now noticing that on days when he has it he often has an episode of stomach pain, which is pretty painful. He has never before complained of stomach pain so this made me pay attention and I noticed the correlation. At his doctor’s request, I was recently able to scrape some off to take in to the lab, and the stone analysis came back as 65% calcium oxalate dihydrate (weddellite) and 35% carbonate apatite (dahilite) Additionally, a 24 hour urine test indicated a calcium/creatinine ratio of 245 (normal 30-20-) and an elevated creatinine level of .81 (normal 0.11-0.68). The doctor said for him to follow a low oxalate diet and follow-up with a pediatric nephrologist, which we will. Is it important to find the cause of the high creatinine and calcium rather than just treat the symptom? This doesn’t seem normal for a child his age – he does not consume an unhealthy diet at all, and is not dehydrated. Is there any particular test I should request? Thank you – your insight is much appreciated.
I forgot to include a bit of family history in my original question. My aunt (would have been my son’s great aunt), died of nephritis at age 7. I don’t know if that’s anything to consider as far as possible hereditary/genetic factors, but thought it’s worth mentioning.
Hi Natalie, Genetic diseases with female renal failure and stones are not very common, and given it was labeled nephritis and led to death I suspect it was really an intrinsic kidney disease unrelated to stones. Regards, Fred Coe
Hi Natalie, Given the CaOx and HA crystals it is likely he is indeed forming excessive stone related crystals. His tests show marked hypercalciuria which could be simply idiopathic – genetic, or perhaps some more uncommon genetic disease that involves the kidney as well as urine calcium losses – such as Dent disease. He does need a skilled pediatric nephrologist to be sure about the serum creatinine. Low oxalate diet will be of only minimal value compared to measures that lower urine calcium, and your nephrologist will surely resolve that matter. Of course I assume urine oxalate has been measured and is normal. Regards, Fred Coe
Thank you. He has a repeat 24 hour urine test this week. He has had 2 episodes of burning during/after urination, and I wonder if that’s related. A spot urine test showed no UTI. He also had an ultrasound which showed :
1. Mild right pelviectasis in the prone position only (7 mm).
2. Otherwise normal sonographic appearance of the kidneys. No definite calcifications are
seen.
In the prone position only, there is mild right pelviectasis (SFU grade 1 bordering on 2) with
AP diameter of the pelvis measuring 7 mm.
I assume the pelviectasis isn’t serious since she the nurse didn’t bring it up on the phone, but never having heard the term before, I tried to research it. The only references I can find refer to fetal pelviectasis, and I can’t find anything about this condition in a 9 year old child. I’m also curious about it only being seen in the prone position. Does this point to the possibility of some sort of blockage, or is it likely just a physiological finding? Is it unusual in a child his age?
Hi Natalie, the dysuria with lack of obvious infection could well be crystals or a tiny stone at the junction of the ureter and bladder. The dilation of the renal pelvis could be from brief obstruction by the stone. If he has not had a CT he should have at least one to be sure about tiny stones in the kidneys. Certainly he needs complete evaluation and some prevention program. His one stone analysis was calcium oxalate and calcium phosphate, and he had high urine calcium. Regards, Fred Coe
Thank you!
This was immensely informative and entertaining. I would love to read more of your writing; you might consider expanding your bibliography to cover other unconventional physical afflictions for the benefit of the ailing public.
Thanks, Chris; I am afraid I do not know much else. Fred
This was immensely informative and entertaining. I would love to read more of your writing; you might consider expanding your bibliography to cover other unconventional physical afflictions for the benefit of the ailing public.
Thanks, Chris; I am afraid I do not know much else. Fred
Hi Fred,thank you so much for your article. It was very informative. I was diagnosed with a horseshoe kidney and several large kidney stones in November of 2015. Since then I have had stints put in and 3 lithotripsys. Not including the multiple rounds of anti-biotics for infections. The discovery of my horseshoe kidney was a shock but a relief to finally know as I have always had issues with pain and infections since I was a child. I’m just surprised that the doctors never found it when I have had three children, a tubal ligation, an appendectomy, and polycystic ovation syndrome. Needless to say I have had numerous MRI’s, CT scans, ultrasounds, sonograms and various other procedures, surgeries and tests. But I guess with a condition that is somewhat rare, the docs didnt always know to look for it. According to my very wonderful urologist, The horseshoe kidney isn’t what is creating my stones but it exasperates the problem. An analysis of the stones came back as being carbonate apatite(hope i spelled that right) which I guess is like struvite stones that are caused by infections. And here I thought the stones were creating the infections. I was hoping to get more information on that type of stone but am having no luck. I am 37 years old and hopefully a lifetime ahead of me and would like to live it without the constant pain, procedures,antibiotics and fatigue. One ER doctor told me it was very common for patiences to go in for lithotripsy every few months. One doctor told me I need to wipe front to back, as if I was a child and didn’t know proper hygiene. But I am about to start collecting my urine for 24 hours so hopefully that will give me some answers. My most recent lithotripsy was November 18,2016 and an X-ray today showed some stones still in my left kidney. I guess what I’m asking is for any additional information you could provide me regarding horseshoe kidneys and the type of stones I have. I have a great urologist but I would like to know more about my condition so that I can be more proactive regarding my own health. Thank you
Hi Lorena, The horseshoe shape does make urology harder but crystals are crystals and stopping them is otherwise much the same. The stones are just calcium phosphate, common type, with a fancy name. Your stones are not at all like struvite and are not caused by infection but from the composition of the urine with is too alkaline and probably too high in calcium. You need 24 hour urine studies and the usual prevention approaches. That you get infections is not a surprise, and that stones and multiple procedures will make them more frequent likewise, but these kinds of stones are not due to infection. Take a look here and be sure you have been properly evaluated. WHen the correct cause is known, reverse it. Regards, Fred Coe
What is the meaning of a very dark colored kidney stone, almost black. Thank you.
Hi Olivia, You cannot tell by color. Have it analysed so you know what it is you are trying to get rid of. Regards, Fred Coe
Hi Fred,thank you so much for your article. It was very informative. I was diagnosed with a horseshoe kidney and several large kidney stones in November of 2015. Since then I have had stints put in and 3 lithotripsys. Not including the multiple rounds of anti-biotics for infections. The discovery of my horseshoe kidney was a shock but a relief to finally know as I have always had issues with pain and infections since I was a child. I’m just surprised that the doctors never found it when I have had three children, a tubal ligation, an appendectomy, and polycystic ovation syndrome. Needless to say I have had numerous MRI’s, CT scans, ultrasounds, sonograms and various other procedures, surgeries and tests. But I guess with a condition that is somewhat rare, the docs didnt always know to look for it. According to my very wonderful urologist, The horseshoe kidney isn’t what is creating my stones but it exasperates the problem. An analysis of the stones came back as being carbonate apatite(hope i spelled that right) which I guess is like struvite stones that are caused by infections. And here I thought the stones were creating the infections. I was hoping to get more information on that type of stone but am having no luck. I am 37 years old and hopefully a lifetime ahead of me and would like to live it without the constant pain, procedures,antibiotics and fatigue. One ER doctor told me it was very common for patiences to go in for lithotripsy every few months. One doctor told me I need to wipe front to back, as if I was a child and didn’t know proper hygiene. But I am about to start collecting my urine for 24 hours so hopefully that will give me some answers. My most recent lithotripsy was November 18,2016 and an X-ray today showed some stones still in my left kidney. I guess what I’m asking is for any additional information you could provide me regarding horseshoe kidneys and the type of stones I have. I have a great urologist but I would like to know more about my condition so that I can be more proactive regarding my own health. Thank you
Hi Lorena, The horseshoe shape does make urology harder but crystals are crystals and stopping them is otherwise much the same. The stones are just calcium phosphate, common type, with a fancy name. Your stones are not at all like struvite and are not caused by infection but from the composition of the urine with is too alkaline and probably too high in calcium. You need 24 hour urine studies and the usual prevention approaches. That you get infections is not a surprise, and that stones and multiple procedures will make them more frequent likewise, but these kinds of stones are not due to infection. Take a look here and be sure you have been properly evaluated. WHen the correct cause is known, reverse it. Regards, Fred Coe
What is the meaning of a very dark colored kidney stone, almost black. Thank you.
Hi Olivia, You cannot tell by color. Have it analysed so you know what it is you are trying to get rid of. Regards, Fred Coe
This article is one of its kind, i have gone through different sites and centers, but you have explained everything in depth. I was too having stones back and tests were 50% calcium monohydrate, but it is all fine now. Thank you Fredric for the great info.
Dear Alena, Thanks for the nice words. Be sure about the other 50% – that it was not something with special implications for treatment. Regards, Fred Coe
This article is one of its kind, i have gone through different sites and centers, but you have explained everything in depth. I was too having stones back and tests were 50% calcium monohydrate, but it is all fine now. Thank you Fredric for the great info.
Dear Alena, Thanks for the nice words. Be sure about the other 50% – that it was not something with special implications for treatment. Regards, Fred Coe
Dear Dr. Fredric Coe:
Really aooreciate for your comprehensive article, also all the others at this very appreciated informative website. Since I am living in Iran, so when I have any medical problem, I check a lot at internet. Since many years I had a left kidney stone problem. It started with 2 stones about 15mm, and ended with 4 stones the biggest 45 mm. After final consulation in Germany I decided to go through PCNL operation and I did it 14 days ago. After the operation I found this website and your article and others helped me a lot. Next week also I have to pass an ESWL, because after PCNL a KUB showed me two 15 mm stones are still left there. After another thanks from you and your colleagues, I have two Q’s:
1- Is the ESWL is ok with me?
2- Am I allowed to translate this article and the related chart Farsi and convert it to a 120 x 70 cm banner for the use of the patients and surgeons?
Really thanks: Ali
Hi Ahmad, Be sure the stones removed are analysed so your physicians know what the crystals are. This is very important to prevent more stones. Whether to use ESWL or flexible ureteroscopy for the stones is a matter of surgical judgement – made by your surgeons. As for the article, this site is free and open to the world. It is good courtesy in making your chart to also make clear where it came from. Regards, Fred Coe
I suffer with kidney stones for the last 8 years Right now I have couple stones in each kidney I have been in pain for last couple weeks starts in my back around my kidneys then moves toward lower stomach I have seen serval doctors they keep they telling me the kidney stones in my kidney shouldn’t be hurting me because they are not moving I have had my stone sent off and they came back Calcium Oxalate Dihydrate (Weddellite) 65%
Carbonate Apatite (Dahllite) 35%
Hi Jennifer, They can cause pain but research on the matter is slow in coming. You have mixed calcium oxalate calcium phosphate stones and really need proper evaluation and a treatment plan. Take a look. Regards, Fred Coe
Thank you I am still dealing with lots of pain can not find a doctor that will help all of Urlogist either thinks it’s in my head or something else and refer me to another doctor so I went and they return me to my urlogist I keep showing blood in my urine with the test deep down I feel it is something to do with my kidney I had some blood work done and the only thing that came back high was liver enzymes and high cholesterol still have kidney stone in both kidneys the urlogist says they are only 2mm in size a lot smaller than my others ones any insight will be great I am mentally drain I am always hurting
Hi Jennifer, The problem is no one yet knows what to do for small stone pain. The blood in the urine surely comes from those small stones and that indicates they are doing enough to produce bleeding. But surgical removal is a procedure with considerable issues and surgeons hesitate to do them for fear of worsening things. One factor may be active crystal formation. So be sure and do everything you can to prevent more crystals and stones. Here is a good routine to follow. You might find the pain improves over some weeks of proper prevention treatments. Regards, Fred Coe
Dear Dr. Fredric Coe:
Really aooreciate for your comprehensive article, also all the others at this very appreciated informative website. Since I am living in Iran, so when I have any medical problem, I check a lot at internet. Since many years I had a left kidney stone problem. It started with 2 stones about 15mm, and ended with 4 stones the biggest 45 mm. After final consulation in Germany I decided to go through PCNL operation and I did it 14 days ago. After the operation I found this website and your article and others helped me a lot. Next week also I have to pass an ESWL, because after PCNL a KUB showed me two 15 mm stones are still left there. After another thanks from you and your colleagues, I have two Q’s:
1- Is the ESWL is ok with me?
2- Am I allowed to translate this article and the related chart Farsi and convert it to a 120 x 70 cm banner for the use of the patients and surgeons?
Really thanks: Ali
Hi Ahmad, Be sure the stones removed are analysed so your physicians know what the crystals are. This is very important to prevent more stones. Whether to use ESWL or flexible ureteroscopy for the stones is a matter of surgical judgement – made by your surgeons. As for the article, this site is free and open to the world. It is good courtesy in making your chart to also make clear where it came from. Regards, Fred Coe
Dear Dr.: Thanks for your fast response. My stones are; Hard, Brown and Rough in surface apperance. They are made of Phosphate (5%), Oxalate (40%), Magnesium (5%), Calcium (10%) and UA (40%). Please be informed that the whole operation (till now) has cost me about 50 $, for ESWL (next week) will be about 40 $ and for final removal of DJ stent (March 2nd) will be about 35 $, in total about 125 $ including medicines and hospital take cares. The ESWL has been advised before my physician could check the stones’ analyisis. Should I advise him forb thisbanalysis? I really bappreciate all the time you spent for us. Ali
Hi Ahmad, Uric acid stones are not ideal for SWL; mention this to your surgeon and get his opinion. Uric acid stones occur because of too acid a urine, and treatment is very efficient. The prices you quote astound me; in the US an SWL treatment can cost $12,000 or more. Warm regards, Fred Coe
I suffer with kidney stones for the last 8 years Right now I have couple stones in each kidney I have been in pain for last couple weeks starts in my back around my kidneys then moves toward lower stomach I have seen serval doctors they keep they telling me the kidney stones in my kidney shouldn’t be hurting me because they are not moving I have had my stone sent off and they came back Calcium Oxalate Dihydrate (Weddellite) 65%
Carbonate Apatite (Dahllite) 35%
Hi Jennifer, They can cause pain but research on the matter is slow in coming. You have mixed calcium oxalate calcium phosphate stones and really need proper evaluation and a treatment plan. Take a look. Regards, Fred Coe
Thank you I am still dealing with lots of pain can not find a doctor that will help all of Urlogist either thinks it’s in my head or something else and refer me to another doctor so I went and they return me to my urlogist I keep showing blood in my urine with the test deep down I feel it is something to do with my kidney I had some blood work done and the only thing that came back high was liver enzymes and high cholesterol still have kidney stone in both kidneys the urlogist says they are only 2mm in size a lot smaller than my others ones any insight will be great I am mentally drain I am always hurting
Hi Jennifer, The problem is no one yet knows what to do for small stone pain. The blood in the urine surely comes from those small stones and that indicates they are doing enough to produce bleeding. But surgical removal is a procedure with considerable issues and surgeons hesitate to do them for fear of worsening things. One factor may be active crystal formation. So be sure and do everything you can to prevent more crystals and stones. Here is a good routine to follow. You might find the pain improves over some weeks of proper prevention treatments. Regards, Fred Coe
Hi Dr. Coe! I am one of the Medullary Sponge Kidney group members. I have a couple of questions and I have a feeling you can help me. First I want to thank you so much for your work and for all of the information you have for us. I really appreciate it. Secondly, are my issues.
I found out 13 years ago that I had MSK when a Calcium Oxalate stone became stuck in my ureter. Since then I have been treated for the usual CO stones. About a year and a half ago my stones started to change. First phos. cal. started to add to the already Co stones. My nephrologist said he had no idea how to help me but to keep on the kidney stone diet. At the next 6 month 24 hr urine it hadn’t changed and he said he still didn’t know how to help me. Then at my last visit, I now have Calcium/Oxalate/uric acid/phos stones. My nephrologist said there is no point in coming back to him, he has no way of treating me. He also did not give me any referrals to another nephrologist, so I will begin researching them. Can you tell me why my body has changed the stones so much? I am 42 now and I no longer seem to pass stones on my own. I used to pass massive amounts. I have had to do a yearly clean out of my kidneys for the last 2-1/2 years. I am in daily pain, which I am working with pain management on a non-narcotic treatment plan, but it is not helping like it has in the past. I would love any of your insight or even referrals to nephrologists in central Texas area. Thank you so much!
Hi Sarah, Stones can convert from calcium oxalate to calcium phosphate. Calcium phosphate stones form in alkaline urine and perhaps your urine chemistries have changed in that direction. Of most importance is proper evaluation and prevention. There is an excellent kidney stone group at University of Texas Dallas; if it is not too far, I would recommend you go there for an opinion. Prevention is crucial to reduce pain and need for so many surgeries. Regards, Fred Coe
Hi Dr. Coe! I am one of the Medullary Sponge Kidney group members. I have a couple of questions and I have a feeling you can help me. First I want to thank you so much for your work and for all of the information you have for us. I really appreciate it. Secondly, are my issues.
I found out 13 years ago that I had MSK when a Calcium Oxalate stone became stuck in my ureter. Since then I have been treated for the usual CO stones. About a year and a half ago my stones started to change. First phos. cal. started to add to the already Co stones. My nephrologist said he had no idea how to help me but to keep on the kidney stone diet. At the next 6 month 24 hr urine it hadn’t changed and he said he still didn’t know how to help me. Then at my last visit, I now have Calcium/Oxalate/uric acid/phos stones. My nephrologist said there is no point in coming back to him, he has no way of treating me. He also did not give me any referrals to another nephrologist, so I will begin researching them. Can you tell me why my body has changed the stones so much? I am 42 now and I no longer seem to pass stones on my own. I used to pass massive amounts. I have had to do a yearly clean out of my kidneys for the last 2-1/2 years. I am in daily pain, which I am working with pain management on a non-narcotic treatment plan, but it is not helping like it has in the past. I would love any of your insight or even referrals to nephrologists in central Texas area. Thank you so much!
Hi Sarah, Stones can convert from calcium oxalate to calcium phosphate. Calcium phosphate stones form in alkaline urine and perhaps your urine chemistries have changed in that direction. Of most importance is proper evaluation and prevention. There is an excellent kidney stone group at University of Texas Dallas; if it is not too far, I would recommend you go there for an opinion. Prevention is crucial to reduce pain and need for so many surgeries. Regards, Fred Coe
Dr. Coe, I was a member of jill’s kidney stone prevention course and she recommended I contact you.
The first 24hr urine analysis I did back in January at the beginning of the class showed low citrate and high ammonia (56.6 mEQ/24 hrs) as increased stone risk factors.
After balancing my diet citrate levels are now normal but my urine ammonia level is still showing up as an increased risk factor (52 mEQ/24 hrs). The test cites 50 mEQ/24 hrs as the “normal” risk threshold.
The test said likely causes of high ammonia were: urinary tract infection, excessive laxative use, and eating disorders. I was screened for a UTI and the results were negative. Laxatives and eating disorder are not a problem.
Do you have any thoughts on how to lower urine ammonia levels back into the normal, or reduced risk range?
Hi Greg, Urine ammonia indexes to urine sulfate. If the ammonia is just a bit below sulfate that is normal. When ammonia is above sulfate the usual causes are potassium depletion – diuretics?? – or something else. Let me know. Regards, Fred Coe
Dr. Coe, I was a member of jill’s kidney stone prevention course and she recommended I contact you.
The first 24hr urine analysis I did back in January at the beginning of the class showed low citrate and high ammonia (56.6 mEQ/24 hrs) as increased stone risk factors.
After balancing my diet citrate levels are now normal but my urine ammonia level is still showing up as an increased risk factor (52 mEQ/24 hrs). The test cites 50 mEQ/24 hrs as the “normal” risk threshold.
The test said likely causes of high ammonia were: urinary tract infection, excessive laxative use, and eating disorders. I was screened for a UTI and the results were negative. Laxatives and eating disorder are not a problem.
Do you have any thoughts on how to lower urine ammonia levels back into the normal, or reduced risk range?
Hi Greg, Urine ammonia indexes to urine sulfate. If the ammonia is just a bit below sulfate that is normal. When ammonia is above sulfate the usual causes are potassium depletion – diuretics?? – or something else. Let me know. Regards, Fred Coe
Dr. Coe,
My sulfate level was 22 mmol/24 hrs, ammonia was 52.0 mEq/24hrs. Would you recommend I increase my potassium intake via diet? Over the counter supplements? Prescription?
I’m not sure what you mean by diuretics.
Thanks in advance,
Greg
I just read a bit more on potassium depletion. If you’re asking if I’m currently taking any diuretics – I’m not on any prescription medicine.
Could it be that I’m drinking too much water? My urine volume was 7.5 liters / 24 hours. Jill told us flushing the kidneys out was the most important thing we could do – so I have been a LOT of water.
Not sure where to go from here..
also, I just noticed potassium was one of the values on the 24 hr urine analysis. mine measured 134.1 mmol/24hr
Hi Greg, Let me try to respond to all three questions at once. The ammonia you quote is very high in relation to the sulfate. Lots of water will not cause potassium depletion nor raise urine ammonia excretion. Your urine potassium excretion is certainly high. The ammonia is not a stone risk factor but rather a measurement that points to something wrong in overall acid base metabolism – or infection with bacteria that hydrolyze urea. Since Dr Bushinsky already reviewed your data I am sure he determined if your urine pH was high or low; I do not recall seeing that value. I remember your citrate was low but now is high. What was the pH in the urine with the high ammonia? Since you are not on diuretics nor have been on any and, I presume, diarrhea and vomiting do not occur the pH will be helpful. Regards, Fred Coe
Dr. Coe,
I am not under the care of a Dr. Bushinsky. Perhaps you have me confused with someone else?
I am going to include all values from both 24 urine tests for your reference. The first test was taken in early January at the beginning of Jill’s class. The second was taken just a few weeks ago to measure progress:
Test 1: Urine volume 2.3 L/24hrs, ph range 5.6, Calcium 124.2 mg/24hrs, sodium <20mmol/L, citrate 193mg/24hrs, magnesium 69.9mg/24hrs, oxalate 14.2 mg/24hrs, uric acid 418.6 mg/24hrs, phosphorous 805 mg/24hrs, sulfate 18.4 mmol / 24hrs, ammonia 56.6 mEq / 24hrs, qualitative cystine negative, potassium 27.4 mmol / 24hrs, chloride <20 mmol / L, urine creatinine 1334 mg / 24hrs
Test 2: Urine volume 7.33 L/24hrs, ph range 7.1, Calcium 205 mg/24hrs, sodium <20mmol/L, citrate 652mg/24hrs, magnesium 107 mg/24hrs, oxalate <.03 mg/24hrs, uric acid 506 mg/24hrs, phosphorous 1026 mg/24hrs, sulfate 22 mmol / 24hrs, ammonia 52.0 mEq / 24hrs, qualitative cystine negative, potassium 134.1 mmol / 24hrs, chloride <20 mmol / L, urine creatinine 1906 mg / 24hrs
Diarrhea and vomiting do not occur.
I was screened for a urinary tract infection last week but that came back negative. Are there other infections or manners of testing I should request from my urologist to be screened for?
I do not have any of the burning or pain associated with a urinary tract infection, although I do feel a bit of pressure or almost a very mild cramping in the bladder / pubic area. So mild, that I didn't really think of it until bacteria infection was mentioned but I do feel *something.
Hi Greg, I do; I found the other person; apologies. In test one the urine sodium is <20 mmol/liter – remarkable low sodium intake or extra renal sodium losses. The pH is 5.6. Urine potassium is low. Urine chloride is <20 mmol/liter. In test 2 urine sodium is again <20 mmol/l and urine Chloride the same, oxalate is unmeasurably low – this actually cannot be correct. Urine potassium is not over 100 mEq/day. Urine pH is now very high 7.1. I will write to you via email and tell you what I think is happening as this is medically complex and should not be public. Regards, Fred Coe
Dr. Coe,
Test 1 (early January) – sulfate 18.4 mmol / 24hrs, Ammonia 56.6 mEQ / 24hrs, PH 5.6 PH range
Test 2 (a few weeks ago) – sulfate 22 mmol / 24hrs, Ammonia 52 mEQ / 24hrs, PH 7.1 PH range
No diarrhea or vomiting.
I was screened for a urinary tract infection last week and it came back negative. Are there other bacteria infections or types of screening I should request from my urologist?
sorry for the multiple responses. It looked like my first draft didn’t go through so I resubmitted – then saw that it did. My apologies.
Greg
Hi Greg, I believe these are the same as the prior ones you mentioned so I will comment there. Regards, Fred Coe
Dear Dr. Coe,
Jill Harris recently reviewed my two 24 hour urines and recommended diet modifications at the request of Dr. David Goldfarb. She said she discussed my case with you because I have a very unusual stone – ammonium acid urate. I would greatly appreciate if you would answer a few questions I have:
1. The main modifications Jill recommended for my diet were: stop eating 150 peanuts/day which I’ve been doing so that I decrease my elevated oxalate; increase fluid intake to 2.5L/ day; increase calcium to 1000mg/day. Do these changes actually address the ammonium acid urate stone?
2. Do we have an idea why I’m forming that (actually I’ve been having orange gravel but never a stone)? She said she discussed with you and she replied in her email that it is seen in laxative abuse, diuretic abuse, and ileostomy. But none of those apply to me.
3. My urine pH is 6.69. I guess that’s protective of forming a uric acid stone as you say in the article. Do we know why the pH is abnormally elevated? I guess that’s a good thing but I wouldn’t want to make change to the diet which would end up decreasing my pH which is so protective of the uric acid stone.
Ok, let me know if you need me to send you a copy of my 24 hour urines or my daily diet. Will you reply to my email or do I need to check this website for your reply?
Thank you very much for your expert opinion!
Perry Cohen
Hi Perry, Ammonium acid urate stones form when pH is not low but indeed like your pH and when urine ammonium ion is high as I suspect it must be to form such stones. High urine ammonium from bowel disease in general lowers urine pH but when potassium depletion becomes worse ammonia production rises, this in turn raises urine pH and you get this stone. I would suggest you and Dr Goldfarb – who is very excellent indeed at kidney stone work – look at your urine ammonia level. If it is high – above urine sulfate, there is a reason for him to figure out. Another alternative is lab error – have several labs analysed stones for you? Is your urine potassium low, your serum potassium? Regards, Fred Coe
Dear Dr. Coe,
Jill Harris recently reviewed my two 24 hour urines and recommended diet modifications at the request of Dr. David Goldfarb. She said she discussed my case with you because I have a very unusual stone – ammonium acid urate. I would greatly appreciate if you would answer a few questions I have:
1. The main modifications Jill recommended for my diet were: stop eating 150 peanuts/day which I’ve been doing so that I decrease my elevated oxalate; increase fluid intake to 2.5L/ day; increase calcium to 1000mg/day. Do these changes actually address the ammonium acid urate stone?
2. Do we have an idea why I’m forming that (actually I’ve been having orange gravel but never a stone)? She said she discussed with you and she replied in her email that it is seen in laxative abuse, diuretic abuse, and ileostomy. But none of those apply to me.
3. My urine pH is 6.69. I guess that’s protective of forming a uric acid stone as you say in the article. Do we know why the pH is abnormally elevated? I guess that’s a good thing but I wouldn’t want to make change to the diet which would end up decreasing my pH which is so protective of the uric acid stone.
Ok, let me know if you need me to send you a copy of my 24 hour urines or my daily diet. Will you reply to my email or do I need to check this website for your reply?
Thank you very much for your expert opinion!
Perry Cohen
Hi Perry, Ammonium acid urate stones form when pH is not low but indeed like your pH and when urine ammonium ion is high as I suspect it must be to form such stones. High urine ammonium from bowel disease in general lowers urine pH but when potassium depletion becomes worse ammonia production rises, this in turn raises urine pH and you get this stone. I would suggest you and Dr Goldfarb – who is very excellent indeed at kidney stone work – look at your urine ammonia level. If it is high – above urine sulfate, there is a reason for him to figure out. Another alternative is lab error – have several labs analysed stones for you? Is your urine potassium low, your serum potassium? Regards, Fred Coe
Hy Dr. Coe! I am glad to read the article about kidney stones. I am a stone former, two years back in 2015 I have a Uretoscopy and ESWL in this way my stones were removed but in 2016 a stone itself passes through my urine, now once again I got to know I have two stones one in the ureter and one in kidney (by CT SCAN and I.V.U + Ultrasound tests), the one in ureter blocks my kidney and causes hydronephrosis now Dr suggests again the Uretoscopy for as a solution because due to stones my urine passes too much blood in it. I have examined my last stones and came to know the type of my stones which was of Calcium Oxalate. Now I would like to know how can I get rid of stones how I stop them to form again and again in my kidnies I would be greatful for a better solution. Thank you!
Hi Asim, Prevention is not hard. Take a look here. Likewise, for more, here as well. Regards, Fred Coe
Hy Dr. Coe! I am glad to read the article about kidney stones. I am a stone former, two years back in 2015 I have a Uretoscopy and ESWL in this way my stones were removed but in 2016 a stone itself passes through my urine, now once again I got to know I have two stones one in the ureter and one in kidney (by CT SCAN and I.V.U + Ultrasound tests), the one in ureter blocks my kidney and causes hydronephrosis now Dr suggests again the Uretoscopy for as a solution because due to stones my urine passes too much blood in it. I have examined my last stones and came to know the type of my stones which was of Calcium Oxalate. Now I would like to know how can I get rid of stones how I stop them to form again and again in my kidnies I would be greatful for a better solution. Thank you!
Hi Asim, Prevention is not hard. Take a look here. Likewise, for more, here as well. Regards, Fred Coe
I am a producer of rare silica calcium carbonate kidney stones. No doctors have let alone heard of them or tell me I am crazy and I did not produce them. I have had a least 6 stone tested and they all come back as 98% silica and 2% calcium carbonate. I have done a lot of research on my own and found one doctor who started a study, but the patient dropped out and ended the study. I have followed her advice and stopped taking any man made meds that have silica into them. It reduced the pain significantly and stopped the stones from forming for awhile. Now, the stones are coming more often and I have no idea why. Any ideas or suggestions. I am at Cleveland Clinic right now and they told me there is no such thing. Looking for any information possible. Thank you.
Hi Linda, Silica in stones is uncommon but not at all unknown. Here is a link to a comment by Jim Williams about a report of them. Here is a link to the parent article about such stones as common in Africa. Here is an old report of a man who had used a magnesium trisilicate antacid for a long time and formed such stones. So, there is indeed such things though not very common. And, for every stone there is a reason. Regards, Fred Coe
Hello, Back in July 2007 I had a kidney stone that was 70% Calcium Phosphate and 27% Calcium Oxalate. It was so big I had to have it surgically removed. When they took x-rays I was told it looked like there might still be a small one in my right kidney. Now 10 years later I am starting to have pain in my back at my kidney level. Its been going on for a few days now. I take lots of tums due to heartburn and feel I may have been feeding this stone. What can I do to help this pass without having to have surgery again? What can I do to dissolve it, if possible? What can I do to prevent it? Any information would help. I am terrified of the pain that is about to follow. 10 years ago the pain was about the same as giving birth to my 3 children. Help!
Hi Crystal, Tums are a good way to produce a calcium phosphate stone – lots of alkali and calcium together. But there is confusion – is there a new stone? How big. It will not dissolve if it is calcium phosphate. Here is a good place to read right now to help sort things out. Regards, Fred Coe
Hello, Back in July 2007 I had a kidney stone that was 70% Calcium Phosphate and 27% Calcium Oxalate. It was so big I had to have it surgically removed. When they took x-rays I was told it looked like there might still be a small one in my right kidney. Now 10 years later I am starting to have pain in my back at my kidney level. Its been going on for a few days now. I take lots of tums due to heartburn and feel I may have been feeding this stone. What can I do to help this pass without having to have surgery again? What can I do to dissolve it, if possible? What can I do to prevent it? Any information would help. I am terrified of the pain that is about to follow. 10 years ago the pain was about the same as giving birth to my 3 children. Help!
Hi Crystal, Tums are a good way to produce a calcium phosphate stone – lots of alkali and calcium together. But there is confusion – is there a new stone? How big. It will not dissolve if it is calcium phosphate. Here is a good place to read right now to help sort things out. Regards, Fred Coe
Hello Dr. Coe,
Thanks so much for this highly informative website. My three year old son recently passed a stone: Stone weight = 0.0040 g, Component: Calcium Oxalate Dihydrate (Weddellite) 20%
Calcium Monohydrogen Phosphate Dihydrate (Brushite) 80%. The stone seemed to be surrounded by a brown stringy mucous.
We were lucky enough to catch the stone in his potty. Prior to this we had noticed blood in his urine and had seen his pediatrician on several occasions, as well as a nephrologist. Several urinalyses have been done as well as an ultrasound of the kidneys. Below are the test results:
9/20/2017 (Urinalysis from the collection that included the stone)
PH = 7.5
Glucose, negative
Protein, negative
RBC 0-2 HPF
CALCIUM/CREATININE RATIO (QUEST) 160 mg/g creat
CALCIUM, RANDOM URINE (QUEST) 4.0 mg/dL
CREATININE, RANDOM URINE (QUEST) 25 mg/dL
August 3, 2017
PH = 6.0
Glucose, negative
Protein = 30mg/dl
RBC = 82/hpf
Urine Mucous = 1+/lpf
CREATININE, URINE, RANDOM 84.9 mg/dL
CALCIUM, URINE, RANDOM 19.6 mg/dL
PROTEIN, TOTAL, URINE, RANDOM 17 mg/dL
July 26, 2017 – Urine Dipstick
Glucose, negative
Protein, negative
RBC = small
PH = 7.0
July 17, 2017
Urine Dipstick:
RBC = Trace
PH = 7.5
Glucose, negative
URINE PROTEIN, DIPSTICK 30. mg/dl
PROTEIN, TOTAL, URINE, RANDOM <4 mg/dL
CALCIUM, URINE, RANDOM 5.5 mg/dL
CREATININE, URINE, RANDOM 9.7 mg/dL
Ultrasound on this date showed: "Question of either prominent column of Bertin, or possible renal duplication. Normal thickness"
July 7, 2017
PH = 7.5
Glucose, negative
Protein, trace
RBC = 10-20/HPF
We would really appreciate any impressions you may have on this case (i.e.implications for diet, important follow-ups). We have a follow-up with the nephrologist in the coming weeks and are hoping to be as informed as possible at the appointment.
Thank you so much!
Hi Anna, Brushite is an uncommon form of phosphate stone. The urine data you show gives high values for urine calcium – 160, 231,560 mg per gram of creatinine so I presume he has idiopathic hypercalciuria. Childhood primary hyperparathyroidism or other causes for high urine calcium all need to be explored by the nephrologist who sees him. Most of the urine samples have an alkaline pH which could indeed promote calcium phosphate stones. Idiopathic hypercalciuria is the final default diagnosis presuming all other causes of high urine calcium have been eliminated. If that is the cause, low sodium high calcium diet is a reasonable approach to discuss with his physician and thiazide type diuretic agents can be used as a next step. Of course, all of what I say is contingent and theoretical. Be sure and analyse all stones as brushite is uncommon and the stone was small. Continued brushite makes prevention perhaps more urgent than usual. Likewise this is a general comment your physician may elaborate on if appropriate. Best, Fred Coe
Hello Dr. Coe,
Thanks so much for this highly informative website. My three year old son recently passed a stone: Stone weight = 0.0040 g, Component: Calcium Oxalate Dihydrate (Weddellite) 20%
Calcium Monohydrogen Phosphate Dihydrate (Brushite) 80%. The stone seemed to be surrounded by a brown stringy mucous.
We were lucky enough to catch the stone in his potty. Prior to this we had noticed blood in his urine and had seen his pediatrician on several occasions, as well as a nephrologist. Several urinalyses have been done as well as an ultrasound of the kidneys. Below are the test results:
9/20/2017 (Urinalysis from the collection that included the stone)
PH = 7.5
Glucose, negative
Protein, negative
RBC 0-2 HPF
CALCIUM/CREATININE RATIO (QUEST) 160 mg/g creat
CALCIUM, RANDOM URINE (QUEST) 4.0 mg/dL
CREATININE, RANDOM URINE (QUEST) 25 mg/dL
August 3, 2017
PH = 6.0
Glucose, negative
Protein = 30mg/dl
RBC = 82/hpf
Urine Mucous = 1+/lpf
CREATININE, URINE, RANDOM 84.9 mg/dL
CALCIUM, URINE, RANDOM 19.6 mg/dL
PROTEIN, TOTAL, URINE, RANDOM 17 mg/dL
July 26, 2017 – Urine Dipstick
Glucose, negative
Protein, negative
RBC = small
PH = 7.0
July 17, 2017
Urine Dipstick:
RBC = Trace
PH = 7.5
Glucose, negative
URINE PROTEIN, DIPSTICK 30. mg/dl
PROTEIN, TOTAL, URINE, RANDOM <4 mg/dL
CALCIUM, URINE, RANDOM 5.5 mg/dL
CREATININE, URINE, RANDOM 9.7 mg/dL
Ultrasound on this date showed: "Question of either prominent column of Bertin, or possible renal duplication. Normal thickness"
July 7, 2017
PH = 7.5
Glucose, negative
Protein, trace
RBC = 10-20/HPF
We would really appreciate any impressions you may have on this case (i.e.implications for diet, important follow-ups). We have a follow-up with the nephrologist in the coming weeks and are hoping to be as informed as possible at the appointment.
Thank you so much!
Hi Anna, Brushite is an uncommon form of phosphate stone. The urine data you show gives high values for urine calcium – 160, 231,560 mg per gram of creatinine so I presume he has idiopathic hypercalciuria. Childhood primary hyperparathyroidism or other causes for high urine calcium all need to be explored by the nephrologist who sees him. Most of the urine samples have an alkaline pH which could indeed promote calcium phosphate stones. Idiopathic hypercalciuria is the final default diagnosis presuming all other causes of high urine calcium have been eliminated. If that is the cause, low sodium high calcium diet is a reasonable approach to discuss with his physician and thiazide type diuretic agents can be used as a next step. Of course, all of what I say is contingent and theoretical. Be sure and analyse all stones as brushite is uncommon and the stone was small. Continued brushite makes prevention perhaps more urgent than usual. Likewise this is a general comment your physician may elaborate on if appropriate. Best, Fred Coe
My question: I’m supposed to catch my stone but besides urine and pubic hair , I have no idea what I am looking for – at?
1. I passed a stone a couple years ago. Though a painful experience, I don’t know when I did it. I did not hear a kerplunk in the toilet or anything, it was just gone. At the time I was told I had another stone and I wouldn’t have to worry about because of it’s location.
2. I am currently attempting to pass the second stone now… and catch it.
a. Will it be a ball like structure or can it be oblong?
b. Will it be hard, ceramic type or can it be crumbly to touch, like sand?
3 The stone is 2mm or .08″ in real measurement or just bigger than a 1/16 of an inch.
I don’t need anything in depth. Maybe just directions to information with pictures and layman descriptions of what I am looking for. You would think looking for something solid in a liquid wouldn’t be that difficult but here I am.
Regards,
Rob Ross
Hi Rob, Often, physicians provide a funnel device with a filter so that solid objects get caught. Stones are small hard and often black objects. I would consider urinating through a funnel with some gauze in it in hopes of catching the object because the crystal type is very valuable to know. Regards, Fred Coe
My question: I’m supposed to catch my stone but besides urine and pubic hair , I have no idea what I am looking for – at?
1. I passed a stone a couple years ago. Though a painful experience, I don’t know when I did it. I did not hear a kerplunk in the toilet or anything, it was just gone. At the time I was told I had another stone and I wouldn’t have to worry about because of it’s location.
2. I am currently attempting to pass the second stone now… and catch it.
a. Will it be a ball like structure or can it be oblong?
b. Will it be hard, ceramic type or can it be crumbly to touch, like sand?
3 The stone is 2mm or .08″ in real measurement or just bigger than a 1/16 of an inch.
I don’t need anything in depth. Maybe just directions to information with pictures and layman descriptions of what I am looking for. You would think looking for something solid in a liquid wouldn’t be that difficult but here I am.
Regards,
Rob Ross
Hi Rob, Often, physicians provide a funnel device with a filter so that solid objects get caught. Stones are small hard and often black objects. I would consider urinating through a funnel with some gauze in it in hopes of catching the object because the crystal type is very valuable to know. Regards, Fred Coe
I passed a almost round stone less than 5mm. (Black in color) do you have an Idea of which of the five it could be? How long do stones take to pas of this size normally?
God Bless
Pastor Don
Hi Pastor, the black stones are usually calcium oxalate. But I would favor your getting it analysed to prevent confusion about prevention. Best wishes for the holidays, Fred Coe
I passed a almost round stone less than 5mm. (Black in color) do you have an Idea of which of the five it could be? How long do stones take to pas of this size normally?
God Bless
Pastor Don
Hi Pastor, the black stones are usually calcium oxalate. But I would favor your getting it analysed to prevent confusion about prevention. Best wishes for the holidays, Fred Coe
I went to the ER one week ago from extreme pain , seemingly, stemming from my urethra. After the pain and burning appeared to spread to my abdomen and then my kidney I began passing blood clots. The blood clots scared me quite a bit and finally got me to head to the hospital. Urine came back clean (other than than lots of blood) so there was no infection. A CT scan was done and confirmed a stone (5mm). I have a history of previous kidney stones going back as much as 20 years ago. This is the first time I am aware of that I had a stone in my right kidney so I was kind of surprised when the ER doctor told me my other kidney was full of stones! They gave me a shot for pain and prescriptions for a pain med and also Flomax. This morning I finally passed the stone so all is well, for now. I’m wondering if there is anything that can be done to “dissolve” all the many stones still in my kidney or will I just have to wait for them to start to move.
Hi Pam, Prevention of more is what this whole site is about. Here is an article that gives a good plan. See if it works for you. Here is another that is perhaps too basic for you in that you know you have stones. Regards, Fred Coe
I went to the ER one week ago from extreme pain , seemingly, stemming from my urethra. After the pain and burning appeared to spread to my abdomen and then my kidney I began passing blood clots. The blood clots scared me quite a bit and finally got me to head to the hospital. Urine came back clean (other than than lots of blood) so there was no infection. A CT scan was done and confirmed a stone (5mm). I have a history of previous kidney stones going back as much as 20 years ago. This is the first time I am aware of that I had a stone in my right kidney so I was kind of surprised when the ER doctor told me my other kidney was full of stones! They gave me a shot for pain and prescriptions for a pain med and also Flomax. This morning I finally passed the stone so all is well, for now. I’m wondering if there is anything that can be done to “dissolve” all the many stones still in my kidney or will I just have to wait for them to start to move.
Hi Pam, Prevention of more is what this whole site is about. Here is an article that gives a good plan. See if it works for you. Here is another that is perhaps too basic for you in that you know you have stones. Regards, Fred Coe
Hi, my stone was analyzed as (Ammonium-Magnesium Phosphate Hexahydrate (Struvite) 90% Cabonate Apatite (dahlite) 10%
Whew !!!! My question is what the heck does it mean and how do I fix it ??????
Thanks for any help on this!!!!!!
Hi, my stone was analyzed as (Ammonium-Magnesium Phosphate Hexahydrate (Struvite) 90% Cabonate Apatite (dahlite) 10%
Whew !!!! My question is what the heck does it mean and how do I fix it ??????
Thanks for any help on this!!!!!!
Hi Andrew, Struvite stones are produced by bacteria that hydrolyse urea in urine to ammonia. They are a product of infection. Management is complex and involves clearing the kidney of infected stone material, brief but potent antibiotic treatment as an attempt to sterilize the urinary tract and – hopefully – that will do it. Because the stones are themselves infected through and through surgery is challenging. Regards, Fred Coe
Hi Doctor, great information. My stones were analyzed at 90% uric acid and 10% monohydrate calcium oxalate. I get it about reducing flesh in my diet to less than 6oz. a day. How important is it to lower the oxalates that are in so many vegies?
Hi Frodo, Uric acid stones have more or less one cause and one treatment – low urine pH and potassium alkali. Diet change is too weak to matter. As for oxalate, we treat it when urine oxalate is high – 24 hour urines needed. Here is a reasonable article about your problem. See if it does not help your physicians in getting you treated. Do not wait long: stones can form rapidly, treatment is more or less perfect. Regards, Fred Coe
Hi Doctor, great information. My stones were analyzed at 90% uric acid and 10% monohydrate calcium oxalate. I get it about reducing flesh in my diet to less than 6oz. a day. How important is it to lower the oxalates that are in so many vegies?
Hi Frodo, Uric acid stones have more or less one cause and one treatment – low urine pH and potassium alkali. Diet change is too weak to matter. As for oxalate, we treat it when urine oxalate is high – 24 hour urines needed. Here is a reasonable article about your problem. See if it does not help your physicians in getting you treated. Do not wait long: stones can form rapidly, treatment is more or less perfect. Regards, Fred Coe
I’m tired passing stones for 2 yrs now, they are orange, uric acid, but no one even my urologist explains me Why? If for 50 yrs I never had none and know is like every 3 month I’m getting this pains and there’s orange sedimentacion and then it comes the stones, Please help.Im diabetic,
Hi Marta, Thanks for tossing me an easy catch. Diabetes lowers urine pH and promotes uric acid (orange red) stones. Treatment with potassium citrate prevents them more or less perfectly. So, just get treated and no more stones. Regards, Fred Coe
I’m tired passing stones for 2 yrs now, they are orange, uric acid, but no one even my urologist explains me Why? If for 50 yrs I never had none and know is like every 3 month I’m getting this pains and there’s orange sedimentacion and then it comes the stones, Please help.Im diabetic,
Hi Marta, Thanks for tossing me an easy catch. Diabetes lowers urine pH and promotes uric acid (orange red) stones. Treatment with potassium citrate prevents them more or less perfectly. So, just get treated and no more stones. Regards, Fred Coe
Dr Coe, I was excited to see a familiar face when I came across this site. I was a pt. of yours back in the 80’s at good old Michael Reese. I had a stone discovered at 8mo pregnant in the ureter that ultimately had to be surgically removed post partum. Was found to be struvite and was on low dose Bactrim for several years. I also had a small, atrophied,scarred R kidney that was speculated to have been from a reflux nephropathy in childhood. Over the years I have had uro work ups for that as well as chronic microscopic hematuria with no significant findings other than a small stone in upper pole of R kidney that has been there for at least 5 yrs. The current issue is I went to urgent care 3days ago for presumed UTI. Burning pain with urination, low abd pain and R flank pain. Urine dip was grossly positive for blood and leukocytes and started on Cephalexin and pyridium. Now today collected some urine to examine if it looked clearer etc and low and behold passed a small black stone. Presumably Calcium oxalate from your article. My question is ,first did I really have a Uti or was the blood, pain and WBCs just from passing a stone ? Also although it appears to be Ca Ox can it also be struvite as well especially considering my past hx of those ? So where do I go from here? I will finish my 5 days of antibiotics but do I need to pursue this further. Can I bring the stone somewhere for analysis without a doctors order or do I need to see an MD first. Thank you for reading this somewhat long saga, any info will be greatly appreciated.
Hi Tina, Sorry about what sounds like a new calcium oxalate stone. We are still here but at University of Chicago. If that is still convenient, Kathleen Dineen can simply take care of things, arrange for me to see you, get the stone analysed. If I cannot – perhaps you now live far away, you will need a physician who can get your stone analysed and also do new 24 hour urines as I did long ago. The stone almost certainly caused your new symptoms. Warm regards, Fred
Dr Coe, I was excited to see a familiar face when I came across this site. I was a pt. of yours back in the 80’s at good old Michael Reese. I had a stone discovered at 8mo pregnant in the ureter that ultimately had to be surgically removed post partum. Was found to be struvite and was on low dose Bactrim for several years. I also had a small, atrophied,scarred R kidney that was speculated to have been from a reflux nephropathy in childhood. Over the years I have had uro work ups for that as well as chronic microscopic hematuria with no significant findings other than a small stone in upper pole of R kidney that has been there for at least 5 yrs. The current issue is I went to urgent care 3days ago for presumed UTI. Burning pain with urination, low abd pain and R flank pain. Urine dip was grossly positive for blood and leukocytes and started on Cephalexin and pyridium. Now today collected some urine to examine if it looked clearer etc and low and behold passed a small black stone. Presumably Calcium oxalate from your article. My question is ,first did I really have a Uti or was the blood, pain and WBCs just from passing a stone ? Also although it appears to be Ca Ox can it also be struvite as well especially considering my past hx of those ? So where do I go from here? I will finish my 5 days of antibiotics but do I need to pursue this further. Can I bring the stone somewhere for analysis without a doctors order or do I need to see an MD first. Thank you for reading this somewhat long saga, any info will be greatly appreciated.
Hi Tina, Sorry about what sounds like a new calcium oxalate stone. We are still here but at University of Chicago. If that is still convenient, Kathleen Dineen can simply take care of things, arrange for me to see you, get the stone analysed. If I cannot – perhaps you now live far away, you will need a physician who can get your stone analysed and also do new 24 hour urines as I did long ago. The stone almost certainly caused your new symptoms. Warm regards, Fred
Hi, please help I pass two to three kidney stones every year three already this year they are all black but my doctor said there cholesterol I don’t see any mention of cholesterol stones? What are they
Hi Richard, If coming from your urinary tract I imagine they are calcium oxalate stones. I would have them analysed. Here is a reasonable article to help you move things along. Regards, Fred Coe
Hi, please help I pass two to three kidney stones every year three already this year they are all black but my doctor said there cholesterol I don’t see any mention of cholesterol stones? What are they
Hi Richard, If coming from your urinary tract I imagine they are calcium oxalate stones. I would have them analysed. Here is a reasonable article to help you move things along. Regards, Fred Coe
Radheshyam. Hi ,This is mahesh from India. I have kidney stones since ten years. So many stones have passed from urine. Please tell me type of stones, treatment and diet thanks
Hi Mahesh, Here is reasonable starting place. You need to collect a lot of information to achieve success. Regards, Fred Coe
Radheshyam. Hi ,This is mahesh from India. I have kidney stones since ten years. So many stones have passed from urine. Please tell me type of stones, treatment and diet thanks
Hi Mahesh, Here is reasonable starting place. You need to collect a lot of information to achieve success. Regards, Fred Coe
Hello Dr,
I have had many stones through the years. All have been a light tan in color. I just passed a black stone this morning. Is the sudden change in color anything to worry about ?
Hi Mike, In a way yes and no. You are best off having the stones analysed so you know what crystals you are trying to prevent. If you have had many stones, prevention matters as there is always risk and concern. So analyse, and start prevention more.
Hello Dr,
I have had many stones through the years. All have been a light tan in color. I just passed a black stone this morning. Is the sudden change in color anything to worry about ?
Hi Mike, In a way yes and no. You are best off having the stones analysed so you know what crystals you are trying to prevent. If you have had many stones, prevention matters as there is always risk and concern. So analyse, and start prevention more.
I am dealing with a number of stones but 3 are impassable at 1.7, 1.5 and 0.8cm each. I did manage to pass a small 5mm stone and had it reviewed in lab. It came back comprised of all 4 crystal types. Where do I go from here?? I don’t have insurance so I’m waiting to get surgery to remove the big stones. Thanks Rich
Hi Rich, Four types is a lot – you did not mention which ones. Surgery is important, but evaluation for cause and prevention more so as they can come back. I would strongly advise you get this latter, and hopefully some insurance – stones are expensive and can be chronic. Good Luck and regards, Fred Coe
Per my doctor’s office:
“It showed mixed hexagonal cystine crystal, rectangular uric acid crystals and mixed
calcium oxalate crystals.”
Hi Rich, cystine crystals might mean you have cystinuria – has that been checked? Uric acid crystals mean an acid urine, and calcium oxalate crystals might mean high urine calcium or oxalate. @4 hour urine testing and cystine screening might be a good next step. Regards, Fred Coe
I am dealing with a number of stones but 3 are impassable at 1.7, 1.5 and 0.8cm each. I did manage to pass a small 5mm stone and had it reviewed in lab. It came back comprised of all 4 crystal types. Where do I go from here?? I don’t have insurance so I’m waiting to get surgery to remove the big stones. Thanks Rich
Hi Rich, Four types is a lot – you did not mention which ones. Surgery is important, but evaluation for cause and prevention more so as they can come back. I would strongly advise you get this latter, and hopefully some insurance – stones are expensive and can be chronic. Good Luck and regards, Fred Coe
Per my doctor’s office:
“It showed mixed hexagonal cystine crystal, rectangular uric acid crystals and mixed
calcium oxalate crystals.”
Hi Rich, cystine crystals might mean you have cystinuria – has that been checked? Uric acid crystals mean an acid urine, and calcium oxalate crystals might mean high urine calcium or oxalate. @4 hour urine testing and cystine screening might be a good next step. Regards, Fred Coe
Fix your typos