A particular manner
Here and there physician friends have asked me about how I practice. But however much I have written about kidney stones, nowhere before have I told about how I practice because I feared my style might seem too odd. But it is not if you consider how narrowly I have chosen to focus.
My clinical life is based on several facts. One is that doctors send me their patients and expect that I will prevent recurrent stones. That is all they want from me. This means that I can depend on other physicians to do everything else, focus on the pathogenesis of kidney stones in a particular patient and fashion for that patient a program of prevention which will disrupt that pathogenesis and reduce or possibly abolish their illness.
In the title of this post, I say ‘art’ because physicians are makers. We make a treatment plan for every patient that will result, in this case, in less stones. In the making of such plans, I use only a few remedies, which most of you know about, but I probably use them a bit differently from most.
Time
Although I have seen about 6,000 stone patients, I still take a very long time with each one. New patients require an hour or more, and it might surprise you to know that many return visits can take as long or longer. Such lavishness would be unreasonable in the broad world of medicine, only in a world like mine, subsidized by a tolerant university and the willingness of our culture to support a few odd sojourners like me can someone lavish so much time on one task.
The time is partly to get the history right. Stones arise through a compound of inheritance, habit, accident, and chance, and no two patients are exactly alike in how they became stone formers. Although I have not written any proof of it, no two have the very same treatment programs if you consider not just superficial aspects of diet and drugs but the details of life and work and habit that need to be altered. It is in those details, in the thick of the brambles, I usually find the real reasons for stones and, having found them, fashion my treatment plan around them. This patient did some odd thing, that one something else, for a while or for a lifetime, and will not tell me right away. Some do not know what caused their stones. Some know very well but will not tell unless I stumble on it. That is where the variety hides, and where I spend a lot of time.
The rest of the long time I take is used in explaining and in finding ways to change things, for I must bring about a change in life. It sounds easy if you have not tried it, but most of you know it is not easy. Patients will always acquiesce on the moment, and then do as they desire. I must somehow change their desires or fail. And these desires are about important matters: How they work, how they eat, how they entertain themselves, how they strive to remain healthy. I know that much of general medicine concerns itself with healthy habits, but my work is not like that. It is not general, but so particular as to reach into the detailed reality of the lives as lived, and it is there one meets with beliefs and resistances, and desires, and habits.
What crystals know
Of course it is not behavior that makes crystals from, it is urine chemistry. I use the standard 24 hour urine to gauge the immediate forces that control crystallization and use my clinical history to understand what aspects of life have affected those forces and which of them might be alterable. Everyone does this, I simply do it with unusual focus as it is all I do.
Consider this patient.
A woman of 42 began forming stones at 32, not an unusual age. Her latest stone was in the past year, and in between the first and last she had 4 other episodes. For her stones she has had 3 SWL procedures, and one ureteroscopic removal. An early stone report showed calcium oxalate dihydrate with 15% hydroxyapatite. A more recent stone analysis reported 45% calcium oxalate dihydrate, 5% brushite, and the rest hydroxyapatite. A recent CT showed bilateral universal papillary and perhaps medullary calcifications varying from 1 to 5 mm. A brief trial of hydrochlorothiazide some years prior had resulted in hypotension and the drug was stopped within 3 months. She had been advised to maintain a high fluid intake, which she said was her habit.
Her mother, who had herself developed premenopausal osteoporosis, urged calcium supplements on her which she used from her early twenties. She became a nurse, and in her mid twenties specialized in orthopedic surgical work. She married and had two children at ages 33 and 35, which interrupted but did not stop her nursing career that continued through a combination of day care and willing grandparents. When stones began she stopped the calcium supplements, and went on a low calcium diet. Her husband is a skilled pipe fitter with steady work in a foundry.
As I do in all cases, I obtain the blood and urine laboratory results I will need in advance of the visit so they are available without needing yet another visit. So when I had finished with the initial history, I had the labs ready. Her blood chemistries were normal – in particular she was normocalcemic. Her 24 hour urine studies – I do three, not two as is more common – showed mild hypercalciuria, mild hyperoxaluria, a volume of above 2 liters, a pH of 6.5 on average, and only modest supersaturations with respect to both calcium oxalate and calcium phosphate. Urine sodium excretion averaged 175 mEq/day. Her urine calcium excretion varied with her urine sodium excretion in an obvious manner, as I commonly find. I made her a little graph to illustrate the point.
What life does
Of course, this is a patient with sodium dependent, genetic – idiopathic – hypercalciuria which may have been worsened by maternal advice and lessened by low calcium diet. As expected, she had modest osteopenia – I ordered a DEXA scan as any of you would do. The natural initial treatment would be low sodium, high calcium diet since thiazide had already proven troublesome and her calcium excretion was sodium dependent. But her work made me suspicious: how did she achieve her ample urine volumes being a surgical nurse? One of her three collections was on the weekend but I had insisted that two be during working days and the volumes at work and on the weekend matched reasonably well.
The answer, which took some time to get to, is that she drank after her long cases – one or two cases a day – and in the early evenings. The high sodium was from everywhere. Her husband and she were so busy that ‘food’ was ‘take out’ most of the week, and she, being in a hospital much of her day, snacked, as nurses do, on pretzels, chips, and peanuts. Willing as they were, the grandparents could not cook for them to any great extent, and, in fact, had high sodium food habits of their own. So, how can I treat her in a way that will work? How will she achieve constant high fluids, much reduced diet sodium, and much increased diet calcium?
What I did
This is a sophisticated nurse. She knew her fluid intake was variable to an extreme because of surgery and suspected the low extremes were promoting her stones. But she did not tell me. I had to ‘find out’ by going through her meals and what she drank with each, her work schedule, the nature of her cases, and even her snacks before the obviousness of the fluid problem led her to tell me she certainly knew daily intermittent dehydration was a problem.
She knew surgery was causing a dehydration problem, but she was the larger wage earner of the pair, so less surgery was not an option and she did not want it to come up with me. As for her diet, she did not know that high sodium intake would raise her urine calcium, or that combined with a low calcium diet would reduce bone mineral balance; but she did know the family ate badly. This latter she did not tell me until I had asked after all her meals; she knew there was no time to cook or shop properly but given the work she and her husband did what could be done about it?
Of course, making a way for her was not easy. It was all about the nearly impossible realities of two busy people. I did find ways, and her followup urines showed more calcium than at the beginning – higher calcium diet, somewhat less sodium, less oxalate – the low calcium diet and peanut snacks had raised her urine oxalate, and the same volumes. So on average her supersaturations were not better. But she assured me that the urine volumes were steadier throughout the working days. Over time she pushed the sodium down, the volumes up, and saturations fell more. Because of her many stones, and that she had converted from calcium oxalate to brushite and apatite, I added a very low dose of a long acting (23 hour 1/2 life) thiazide – chlorthalidone, 12.5 mg every other day – and achieved a reasonable result.
How, you might ask, did I get her sodium intake down and her urine flow up steadily yet she remain an operating room nurse? I talked to her about how she and her husband worked out their schedules and realized there was no time in the week for anything like cooking. So, I recommended they shop and do batch cooking on the weekends, freeze meals in proper sized containers, and use them for lunches and suppers. As for her water, I worked out her rotating in and out of scrub with several colleagues, which permitted fluids. She has been free of new stones for several years.
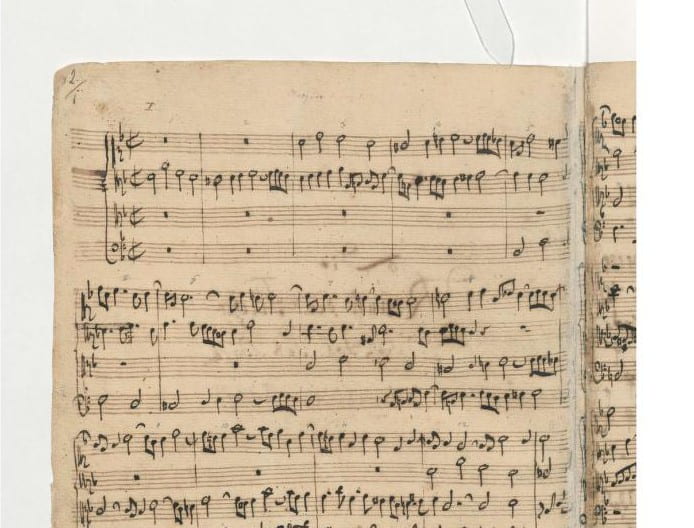
The manuscript score is said – on the web – to be an original by Bach. Perhaps a few of you who play classical keyboard music will have recognized the opening of the first fugue in d minor from ‘Art of Fugue’, his vast unfinished masterpiece. Bach is an immortal genius, and we are common folk, but the principle holds. He was a maker, as we are. Perhaps so much greater a maker that the comparison seems ridiculous, but I disagree. We make treatments out of the materials at hand and with what skills we can achieve. If we believe, as does the spiritus mundi of the West, that even one individual life is priceless, then what we do is, in its way, considerable under heaven. And, I might say, worth even my extravagances of time in the doing of it.
When I work
I see patients only one half day a week, because as a professor I do research which takes a lot of time and for which research grants provide support. Likewise, the writing of books, chapters, reviews, and papers takes up a lot of life. My meager clinical life is not odd for a university research profession; many I know do what I do. It is in fact the very smallness of the actual clinical time which permits me to be so specialized, and to have leisure to review what has happened to the patients I have seen so that past mistakes need not be repeated for a lifetime. My Google page is public; if you follow the link, and look, many of my papers have described what I have seen, and in the making of them I have made and remade the way I work with patients.
How I get paid
The only way that works is to bill by time. I keep track of how long I spend, and the university bills for that time. The documentation of the medical record for various levels of care is a distraction to me, and utterly unfit to what I do. What good is a stock review of systems, as an example, to someone who is after extreme details concerning the whole health and behavior of a patient? The basic assumption of my practice is that other doctors provide the broad range of care and have sent their patient to me for one special thing. I tell all patients about my specificity and the need to have proper primary care; to my knowledge they all do.
How I report
The computer formatted record is useless to me. I need to produce a consultant’s report, and do it in a way patients like and I find very effective. I use a blank report form in the EMR and share the screen with the patient by turning it at an angle where we both can see it. I tell patients we will write the record together and to correct any errors as we go along. I use up about a full single spaced page and when they leave patients get the report to take with them. We mail it out with all labs alter on to the physicians, and the patient. Incidentally, I have sent all my patients their entire record since I began in 1969, and have never encountered a single problem in doing it.
Something for later on
I haven’t told you everything. Nor can I. But I can bring some cases, as time goes on, and hope they show what I cannot tell. You might offer some, too. I am happy to have guests post a case. Let me know.
Bach was a teacher, incidentally. He wrote the 48 preludes and fugues partly for his gifted children to learn from. I believe the violin and cello suites, French and English suites, even the Musical Offering – though presumably made for Frederick II of Prussia – were also by way of education, perhaps his own. As for Art of Fugue why write 17 fugues in d minor on one theme if not by way of illustration; they make their way through every kind of fugal technique, and culminate in an unfinished fugue of such complexity no one has ever been able to fashion a reasonable ending for it.
Fredric L Coe MD
Return to Walking Tour on Supersaturation


Dr. Coe,
Can you please comment on how urine volumes affect the reported measures of substances on 24 hour studies? As substances such as calcium, oxalate, phosphate, uric acid etc. can cyrstallize and come out of solution if there isn’t enough water to keep them at or below their solubility product, how, for example, can we be sure that a patient does not have hypercalciuria when a 24 hour urine study reports out, say, 120mg of calcium, with only 1 liter of urine (as the lab can only report what is dissolved in solution, it will not be able to report any calcium that has come out of solution with an accompanying anion)? I have anecdotally found a direct correlation between certain substances in the urine (such as calcium, phosphorus, oxalate, and uric acid) and urine volumes (to a point) and believe that low urine volumes may reduce the specificity/predictive value of 24 hour urine studies to predict abnormally high values of certain substances in the urine. I appreciate your thoughts on this. Thank you.
Hi Steve, and thanks for the great question. It is true that as urine volume falls supersaturations rise steeply and in vitro crystallizations are not rare. I have often found 24 hour urine uric acid excretions of 300 mg/day in adult men with scanty and acidic urine which rises to 900 mg/day when I raise pH or volume or both. Likewise, I have observed urine calcium excretion rise in high pH CaP stone formers when the volume goes up. As a lab practice we can acidify an aliquot of urine to dissolve CaP crystals and raise the pH to dissolve uric acid, and that can help. But if you do not have the 24 hour urine container a lot can be lost in it unless patients rotate it about so aliquots sent to central labs have some of the crystals. Put simply when I find low volumes I raise them and always recheck everything on the higher volumes to be sure nothing is missed. For uric acid excretion and SS in acidic urines, I have no confidence until pH goes up and volume, too. Warm Regards, Fred
Dr. Coe,
I apologize if this topic is discussed in another section of your website., but I wonder if you could tell me what you have heard about Phyllanthus Niruri, or point me to the area where this is discussed. This plant, also called Chanca Piedra, has been touted as an aid in preventing or resolving kidney stones, but this could just be a marketing ploy to sell herbal cures that are worthless, and maybe even dangerous. I am intrigued, though, by articles mentioned on the National Institutes of Health website as to its potential. Thank you!
Hi Michael, I do not know about this plant but I’ll tell you what. Send along the link and I will read it and say what I can about the article from NIH. If it is interesting I will write an article about it and credit you for putting me on to it. Regards, Fred Coe
Hi Dr. Coe! Here are two links: http://www.ncbi.nlm.nih.gov/pubmed/21176271 and http://www.ncbi.nlm.nih.gov/pubmed/12010223 It seems some of the studies mentioned are fairly old. Makes you wonder if research is continuing. Thank you, Mike Williams
Hi Michael, I reviewed these two abstracts. I know this group, which is excellent, and believe they do fine research. About the plant itself, they are careful in their claims, and I likewise have little more to say. I have saved a PDF of the review – the first abstract – and will update the article on stone matrix and inhibitors with it. Thank you very much, Regards Fred Coe
Thank you, Dr. Coe. If something sounds too good to be true, it probably is. One caveat is this study (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3252221/) on Phyllanthus amarus, which appears to be another name for the same plant.
Hi Michael, So far as I can tell they are either the same or related. This article suggests the plant extract is not so safe, and therefore it may not be worth putting up the work on the site. Regards, Fred
I have been a patient of Dr. Coe’s clinic for many years. Initially, I saw Dr. John Asplin. He learned from the best. Everything Dr. Coe has written about working with patients, Dr. Asplin did, too. I was quite impressed at my initial and follow-up visits. Eventually, Dr. Asplin left to spend his time at Litholink, providing us a great service with 24 hour urine analysis. Dr. Anna Zisman took over, another terrific kidney stone specialist. As the clinic is a 2 hour one way commute, I see a local nephrologist and a urologist annually. Along with Litholink’s 24 hour urine testing, I get an annual CT Scan. I’m always afraid to go on vacation without knowing size and location of stones. This works for me. The high dose of radiation is worth it for my peace of mind. I go to Dr. Coe’s clinic every 3 years or so. Thankfully, my nephrologist (Dr. Donald Cronin) has great respect for Dr. Coe and follows his guidelines.
Drinking upwards of 3 liters a day can be quite daunting early on. It becomes easier and 2nd nature within weeks. Adding fresh lemon juice to the water helps to keep citrates in a healthy range for kidney stone patients.
I highly recommend any patient reading Dr. Coe’s blog entries, take this information to his/her own Nephrologist or Urologist. Prevention is certainly key!
I have considered trying to form kidney stone patient support groups in the Chicago metropolitan area. It would be a beneficial service, with Urologists and Nephrologists referring their patients to the program. I believe a quarterly gathering and an online forum would be sufficient. The involvement of a Nutritionist or Dietician, educated about the different stone type dietary guidelines, would be important. This would have been very beneficial to me in the late 1990’s when I began the struggle with stones too large to pass. At that time, my local Urologist handed me a short 1/2 page dietary restriction, based more on oxylate stones, when unknown to him, my stones were phosphate. Thankfully, the internet was growing and I found Dr. Coe’s clinic.
Here’s to no stones to large to pass and continued research identifying metabolic reasons for this disease – Cheers!
many plants extract use to treat kidnet stone. Is it safe and effetive enough?
Hi Rumah, I know plants have been mentioned but I also know we have inadequate studies so far for me to recommend any. Regards, Fred Coe
Dr. Coe, my name is Shams Zia and I’m a nephrologist. I have started a kidney stone center along with the urologists and dietician in our program. As expected, our major population has calcium oxalate stones and NC is a known stone belt. I wanted to ask if you generally use urine pH sticks for home use on patients with hypocitraturia and low urinary pH to maintain a urinary pH of 6-7. I’ve a couple of patients who have been using these and several of them are interested to use them now. Thanks in advance.
shams
Hi Dr Zia, I do not use them. To me overall 24 hour urine pH will more or less determine overall uric acid crystal formation over the day, and it is for uric acid stones we raise urine pH. As an example, suppose urine pH rises after eating – as it may – and some uric acid dissolves. But later on the pH dips and more crystals form. As for low urine citrate, urine pH is misleading in my observations. For example in RTA urine pH can be very high and citrate below detectable. Plots of urine citrate vs. urine pH taken in the CRC hour by hour show only a weak correlation. So, I think it is more stable to just measure 24 hour urine pH and citrate to monitor treatment. Regards, Fred Coe
Thank you so much Dr. Coe, this really helps. I may have more questions for you in future.
shams
I have had Oxalate stones since I was born – I use many strategies to control the production of.. and the pain of course when
Hi Jon, So long a time of calcium oxalate stones makes me wonder why. I hope you have had 24 hour urine studies with especial care for the urine oxalate level – primary hyperoxaluria can be like that. Be sure. Regards, Fred Coe
Good day Dr. Coe,
Like the patient you describe in your article, I first presented with my stones in early adulthood. I had my first stone in my twenties and have been producing them ever since. My father had one stone at 25 and never presented again. Now, as a father of two I find myself wondering if my children will one day suffer from stones as well. To that effect, I have 2 questions.
1) Why is it common for first time stones to occur between the ages of 20 & 30?
2) What should I do if anything for my children?
Thank you very much and warm regards,
Stavros
Hi Stavros, I do not know why the age of onset. But I do know that given many stones you would benefit from prevention efforts. Here is a nice plan. Given the ideal diet for stone prevention is the US healthy diet I would follow it in the family. Regards, Fred Coe
Thank you very much for all the research and resources you have made available here. I have learned a lot.
Dear Dr. Coe,
I had been a stone former for over 30 years but only having stones every two or three years. However, stone formation increased significantly in late 2013-2016. I contacted you over a year ago (Jan 2016). At that time I provided you (online) with my lab tests, CT scans and KUB, and medication list, and you provided recommendations. I also had some concerns regarding my own MDs, procedures to remove stones, and lack of dietary education. I had already had a PNL that had complications…adm 9 days, two ureteroscopies, and two lithotripsies all since 2013. After having four stones from Jan to April of 2016, I started on your low oxalate diet in mid-April 2016. I used the Harvard list on this website to avoid all foods with very high and high levels of oxalate six days of the week plus also paired foods with calcium to those with oxalate. I did not drink anymore fluids that I had been drinking. I am very happy to report that I have not had any kidney stone attacks this past 12 months! Also, I have had wnl lab work plus a recent KUB shows no new formation of kidney stones! Although I still have fragments/dust/particles from a lithotripsy the area has not grown or moved. This is the first time since 2013 that I have not had any kidney stones! It now appears that my healthy eating diet (2013) in which I lost 25 pounds and exercised more both contributed to my significant increase in kidney stones. My nephrologist agreed that I no longer need to be on HCTZ or K Citrate as I taken myself off of it after 9 months after having normal lab work and KUB at 6 months. Thank you so much for all your help and for this wonderful educational interactive website. I have no doubt that you and you alone were responsible for preventing new kidney stone formation this past 12 months. I am now trying to determine how to lose weight and still have a low oxalate diet. I am very excited that I can now travel without worrying about having a kidney stone attack. Again, thank you so much.
Sincerely,
Judy C of St. Louis, MO
Hi Judy, I am glad that everything has gone well. Be careful. CHeck out this later article that has a lot of details in it. Regards, Fred
Dear Dr. Cole.
I’ve had recurring incidents of kidney stones for 45 years now. I got my first one when staioned on Guam, “the kidney stone capital of the world.” where there is super high calcium in the water. Better than getting nuked by the North Koreans, I suppose. I get calcium oxalate stones, one every 3-4 years. Like most stone-formers, I’ve been told to drink more water which I try to do but Ugh and is it enough? Based on your great site info, I will have my urine analyzed to see if I’m avoiding that supersaturation level. Regardless, is there a “better” type of water to be drinking? The water where we live tastes terrible and we only drink carbon-filtered and reverse-osmosis water that we buy in 5G jugs. From what I glean, the water should be slightly alkaline. Is that correct? Can I add something to it to increase the citrate? How about adding lemon juice, which, of course would make it more acidic? I plan on getting my urine tested fro citrate too, Anecdotally, my brother who USED to have recurring oxalte stones too hasn’t had one in maybe 20 years now since he started taking a tablespoon of natural apple cider vinegar in a glass of water every morning. If it really does help. I could handle that. Not so sure about the pureed asparagus stone-reducing treatment though…
All that said, I’m currently passing a 5.5mm stone which is stuck (I’ve never passed one that big.) so currently have it “stabilized (?)” with a stent while I’m scheduled for some more of that costly surgery in two weeks. I’m not sure what procedure they are planning but heard something about the stent possibly expanding the ID of the ureter enough where the stone might pass. I guess I’ll find out in two weeks.
Anyway, for different reasons my wife has me taking a concentrated packet of “GreenTea HP” every day. http://www.greenteahp.com/ Allegedly, it is equivalent to 30 glasses of geen tea but they are not very definitive on how much ECGC it has. Interestingly, and of course anecdotally, since I’ve started taking the stuff, I’ve passed a number of small stones (~1-2mm) and I had never done that before.
So it would appear that green tea helps?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855614/
https://www.ncbi.nlm.nih.gov/pubmed/16724910
Then there’s Oxalobacter formigenes,,,”is an anaerobic bacterium that colonizes the intestinal tract, where it metabolizes oxalate to formate and carbon dioxide. Absence of O. formigenes colonization predisposes persons to oxalate stones. Preliminary studies of O. formigenes ingestion in healthy patients and in patients with primary hyperoxaluria demonstrated up to a 90 percent decrease in urinary oxalate levels. Larger studies of this potential therapy are ongoing.”
http://www.aafp.org/afp/2011/1201/p1234.html
If so and true, is there a test for that?
Your comments on any of this would be most appreciated.
Best regards,
Peter Wagner
.
Hi Peter, Be sure and analyse this stone coming and be sure the stones really were all calcium oxalate and not highly admixed with calcium phosphate. The 24 hour urine package for stones includes citrate, so you will have it. As for all the other stuff, without the data and a plan you will get confused and be confused. Follow this plan, as it works. The bacteria has had its day. You cannot give it to people, so maybe some have it and are lucky. It is not worthwhile as a test. You do not even know if your urine oxalate is high. Get tested, check out the stone, ignore all the noise around you, and follow on your own track – from your own data and all will go well. Best, Fred Coe
Dear Fredric,
Is there a way to schedule an appointment with you? I don’t see that anywhere on this site.
I think all of my trunk and kidney pain and much of my pelvic pain (though I do have pelvic floor dysfunction) is coming from small stones that have not changed or moved (according to the reports of the CT scans done) in 4 years. If I even suggested that they be taken out, I believe any doctor (at least, that I have seen) would argue that it is totally unnecessary. For the past 4 months I have (at times gross) blood in my urine (at least 3+ and sometimes filling the toilet with red), trace protein and more recently leukocytes (for which I have just received antibiotics) and pain that wakes and keeps me awake at night unless I get up and take tylenol.
Thanks,
Rebecca in MA
413-230-3102
Hi Rebecca, Of course I can see anyone who wishes. But I would ask my physicians beforehand if they think I could be of use to you as it is a long way off and costly of time and even money. If the main issue is benefit to removal of small stones in relation to bleeding and pain, a urological expert might be more valuable than I could be. Let me know, and I can arrange whatever is best for you. My office secretary – in About Us – is 773 702 1475: Kathleen Dineen. Regards, Fred Coe
Dr. Coe, I am curious if you feel I might be a good patient for you. I am now 36 and started passing stones at age 20 (spent almost half my life with kidney stones). I’ve had 5 or 6 lithotripsies (losing count now) and felt that these only exacerbated my stone formation since the fragments always dropped to the base of my kidneys and didn’t pass. Some of the CT scans I’ve had the radiologists actually stop counting the stones and stated so in the report because there were so many. I have them in both kidneys. I just passed another stone yesterday and was anxious because I haven’t been to the urologist in a while so I have no idea on the current size of my stones. I tend to just pass the stones on my own at home because I figure there isn’t much point going to a hospital since I suspect the only thing they’d be able to do is confirm stone size and help manage the pain. I now only have a lithotripsy if a stone is too large to pass. My mom and sister both have a history of a few kidney stones, but nothing even close to the number I have.
I suspect that food allergies may be a contributor to my stone formation. I suspect that I retain fluids when I’m exposed to a food allergen and that decreases the fluid available for urine. When I was pregnant, I gained 50 pounds the first time and 30 pounds the second time. Within a week of birth, I had lost almost all of the weight gained during pregnancy because it was water weight. I didn’t discover my food allergies until after my second pregnancy at around age 30. When I first discovered my food allergies, I lost 60 pounds in about a year. I’ve suffered from these food allergies for most of my life without realizing it. One of my major difficulties is that I really cannot avoid all of my food allergens. One is corn and it is literally in everything so my only hope with this one is to keep the level low enough that I don’t have bad reactions.
Since trying to avoid my allergens, I had much reduced frequency of passing stones. However, I’ve been busy professionally and have reverted back to a bad diet of eating out too much. I am convinced this is why I started passing stones again. I also had to gain weight because after losing 60 pounds I was underweight. So I resorted to eating some things that I shouldn’t to avoid being skin and bones. Now I am overweight and need to lose weight again. I feel like the doctors I’ve seen in the past just use the same old formula they’ve always tried and hope it works. It sounds like you are different and different is very welcome at this point. If you have the ability to work with me remotely or help me locate a colleague in Texas with a similar focus on stone prevention and finding the root of the stone formation cause, then that would be ideal since I am not sure if travel would be possible (would depend upon required frequency). Thank you in advance for any thoughts you may care to share. Regards, Julie
Hi Julie, Indeed at UT southwestern, Dallas, I know three outstanding kidney stone experts. Dr Peggy Pearl, Dr Orson Moe, and Dr Sakhaee. All three are famous for their work, and good friends of mine. Surely one or another will resolve your problems and prevent more stones. I would pick one, let them know I sent you, and perhaps choose which of the three will be most efficient for you. Let me know, Regards, Fred Coe
Hi Dr. Coe,
I’m a 45 year old male and have just had my second lithotripsy procedure – two years in a row!
Given my recent history and the latest CT scan showing another stone developing in the the kidney now, it is pretty clear I’m a “stone grower.”
I’m looking for any recommendations for doctors or facilities with kidney stone experts who can help me reverse my stone growing.
I was considering traveling to the Cleveland Clinic or Columbia’s Kidney Stone Center, but I’m wondering if there are any experts you recommend who are closer to my residence in charlotte, NC?
Thanks in advance for any help/suggestions.
Regards,
Mike
Hi Michael, You mention two excellent centers. If you have to fly, you can also come to us – we never say so in this site, by choice – but do help many who fly here. I am not familiar with stone prevention in Charlotte. Regards, Fred Coe
Thank you for all the information you provide on here! I enjoy reading everything. I wanted to let you know how I got rid of 4 kidney stones in 2 months as confirmed by ct scan with contrast and ultrasound. In Dec I had an emergency ultrasound for pain radiating from my ovary (it was discovered I had a ruptured cyst) but coincidentally the tech saw 4 stones (3 in left kidney and 1 in right) all around 4-6mm on average on ultrasound. Needless to say I was dismayed as my last kidney stone was 5 years ago and it was 1cm which was surgically removed and a temporary stent put in my ureter. I have been taking daily 300mg of magnesium citrate for years and if I had colicky pain I started Chancra piedra right away and the pain resolved. With my new finding a I did a google search on anything new coming out in the urology field concerning kidney stones and came upon new promising research on hydroxycitrate. I looked and looked but only could find one product that was hydroxycitrate (I did not want a garcinia Cambodia product for weight loss). My ultrasound was Dec 8, after this time I started drinking much more fluid during the day and started hydroxycitrate on Jan 5, I took 500-750mg daily until Feb 28 (1.5 months) and stopped. Yestrday March 8 I had an abdominal CT with contrast as my urologist wanted to see how large the stones were and what the next plan was. I am happy to say I received results today and no renal calculi was noted at all. All I can attribute this to is the hydroxycitrate. Even my urologist was stunned that all of them are completely gone with no trace and asked to see the product I was taking. Just wanted to share this somewhere and say that maybe, just maybe this might be a new way to help stone formers. The product I was taking was hydroxycitrate by Solgar.
Hi Sarah, hydroxycitrate is a readily available commercial weight loss product that can affect crystals. I have remained silent about it pending some trial evidence. But a CT with contrast worries me- one cannot see stones through contrast. Be sure views were taken before contrast was given else they may be there, still. Regards, Fred Coe
Hi Sarah! Your information sounds promising! I have been taking Chanca Piedra now for a month but haven’t been in to the doctor to get another CT scan. I’m considering switching to the hydroxycitrate after hearing your story and reading about it from http://news.doccheck.com/en/5218/hydroxy-citrate-can-kidney-stones-just-melt-away/#comment-744
Do you know for sure it was HCA or do you think the Chanca Piedra helped?
Hi Heather and Sarah, I am putting this up on the site but need to add that no evidence supports either treatment. The Chanca Piedra is a remedy based on almost no real data. Hydroxycitrate was studied by a close colleague of mine, Dr Asplin, but there is no evidence concerning human stone prevention. Since it is a common health food – diet supplement – I see no harm in it. But I do not want people to think that because posted here these things are of any proven benefit. I should write about both, and apologize it has not yet happened. Regards, Fred Coe
hello Dr. Coe, I sure wish I had discovered you 40 years ago. 60 year old male here, with first passing of kidney stone at age 26, and 6 since then. Also first recorded hypertension about the exact same time. A couple of times the stones were clearly related to eating spinach and swiss chard and beet greens, because I did not know at the time that those foods are very high in oxalate, and they were my favorite foods one summer in my 30s. I continue to form stones, depite adhering to a low oxalate diet, adequate H20, and daily dosing with K Citrate. I take Verapamil, Losartan, and Flomax. I am going to ask a simple question. I have three siblings, and none of them have ever had a kidney stone, neither do any of them have hypertension. Another difference between me and my siblings is I have Ehlers Danlos Syndrome, which affects many aspects of my life, notably chronically dislocating joints with pulled tendons and ligaments, orthostatic hypotension with hundreds of dangerous instances of syncope, and aortic arch enlargement on echo. The question is: is the kidney stone forming possibly related to connective tissue issues in the kidney? Second question, if I may have a second one, is do you have any recommendations for my regimen. Thank you.
Hi Arno, I know of no associations between EDS and kidney stones. I have found uncommon associations with hypertension, but this seems rare. You might want to determine your genotype – well established by now and possibly consult with experts in this disease. Here is a rare disease link – one of many – you might find useful. It centers on EDS. Regards, Fred Coe
Dear Dt. Coe
Reading this has been fascinating, I also am curious to find a prevention method. So far, my stones have been extremely small. I have passed three with minimal discomfort I j just have a week or two of bloating , then about a half hour of pain, then pain is gone. The stones have been so small. I did have a ct scan. There are two stones, one 7 mm and one 8 mm. On Tuesday, the doctor will go over this and probably recommend lithotripsy.. My father had stones also.
I also have cysts in my right kidney.
I do like spinach and Kale!!!! I would love to find a kidney specialist in my area. I live in the Washington/Baltimore area, and am sure there is someone you can recommend here.
I have been taking a minimal amount of Chanca Piedra (Stone Breaker).its probably not in your toolbox, as it is an alternative product.
The doctor also found blood in the urine about a month ago. I felt as though I was passing a stone in her office at that moment .
Any contact in my area, would be greatly appreciated.
Sincerely, Nan
Hi Nan, Spinach is a big risk factor for calcium oxalate stones, kale is free of oxalate and has no stone risk. If you have two stones, perhaps your urologist might consider ureteroscopy as a way to insure a stone free kidney result. Chanca Piedra is on my list for articles; it is probably not a fraud nor panacea. As for a stone expert, Brian Matlaga at Hopkins, is brilliant and I can recommend him without hesitation. He is a surgeon of considerable skill and also knows about prevention. We are friends so do not hesitate to say I sent you his address. Regards, Fred Coe
Hello, my husband had stones for the first time earlier this month. We are both plant based and eat a lot of fresh fruit and veg, mostly organic. He had a CT scan and urine sample after having bloody urine and severe pain. The CT scan came back negative, but the doctor was still sure they were there. He passed 3 or 4 in the hospital room toilet, and the doctor sent him home. He still had a lot of pain for awhile after. I have bought chancapietra for him. Would you know if anything we can do or avoid to stop this happening again? His work is very high stress, could that be a contributing factor? Thank you so much!
Hi Mary, He would benefit from an organized workup and treatment based on what is causing his stones. Here is a good place to start. Any stones passed are best collected and analysed, by the way. Regards, Fred Coe
Hello, my husband had stones for the first time earlier this month. We are both plant based and eat a lot of fresh fruit and veg, mostly organic. He had a CT scan and urine sample after having bloody urine and severe pain. The CT scan came back negative, but the doctor was still sure they were there. He passed 3 or 4 in the hospital room toilet, and the doctor sent him home. He still had a lot of pain for awhile after. I have bought chancapietra for him. Would you know if anything we can do or avoid to stop this happening again? His work is very high stress, could that be a contributing factor? Thank you so much! Any help would be so appreciated!
Hi Mary, he needs a proper evaluation, and treatment based on the results. Take a look here. Regards, Fred Coe
Hello Dr. Coe,
In 2006 my urologist gave me a list of vegetables that are high in oxalate like spinach, beets, almond etc. I passed calcium oxalate stone in 2011. I’ve gone to a different urologist and they gave me a list of things to avoid and this time it’s focused on high red meat, sodium consumption. They also recommend taking magnesium as a supplement. What are your thoughts on these? Also, I’ve watched Dr. Oz episode how you can still eat vegetables high in oxalate as long as you eat something which calcium to bind the oxalate. Just want to get your thoughts. Thanks!
Hi Mike, You have more or less found out why I have put up this site. In fact, none of the physicians are wrong, but they are not coordinated in terms of an overall prevention strategy. Here is a very good place to start. Follow it and its links and you will have a workable prevention strategy. Regards, Fred Coe
Hi Dr. Coe,
I’m a 59 yer old male with a 9mm stone in the L lower kidney and an 11mm stone in the right lower kidney. I’m scheduled for ESWL this Friday. My urologist measured the density of one of the stones at 3 x that of bone using a roll on the imaging CD. I’m having reservations based on my research on success rates of ESWL for hard stones located in the lower kidney. Any thoughts, and can you recommend a urologist near Ft. Lauderdale, Florida?
Hi Gary, the choice of surgical modality is complex and I am far away. First, I am not sure why the stones need removing. WIthout pain, infection, bleeding, or obstruction, the only reason is concern for eventual passage; but surgery is already a major procedure. As for hardness and SWL, and location, everything is in the details. I do not know of urologists in the region you mention for whom I have special knowledge. Whatever you do, ask if it is necessary. For sure, evaluation and treatment to prevent more stones – that is certainly important as you already have formed two. The whole site is about prevention; you can start here. Regards, Fred Coe
I had trace urine, trace leukocytes, and few bacteria initially, trace blood and trace leukocytes a couple of weeks later, and the last urinalysis was normal. I’ve had no symptoms. I did pass 3 stones 3 years ago without pain. These recent stones were found following up on the back to back urinalysies showing trace blood and trace leukocytes. My diet was crazy high in oxylates, lots of raw spinach, nuts, beans, dates, cashew milk (I was following a vegan diet). My first of two 24 hr urine tests revealed high calcium (336), high oxylate (59), high calcium oxylate(3.64), and slightly elevated brushite (2.14). Everything else was normal, as was my bloodwork. Started the 2nd 24 hour urine this morning.
Hi Gary, The high urine calcium is almost certainly genetic and needs treatment. The high oxalate is diet. Be sure you know what the passed stones were made of – calcium oxalate vs calcium phosphate. The trace blood does not require stone removal, which is entirely elective. Of course it does require your urologist be sure it is from the stones and not something else – that is part of urological surgery practice and outside of my specialty. Regards, Fred Coe
Hi Again, Dr. Coe,
My calcium intake has almost certainly been low, as I don’t consume dairy. I have a couple more numbers for your consideration if you’re willing. My serum calcium was 9.8 and PTH was 28. I’ve been wrestling with intractable insomnia which is what initially led me on this path. Recent life events could be the culprit, but I’ve suspected that it was possibly biochemical rather than psychological.
Hi Gary, Your calcium and PTH are normal. Not problems. Regards, Fred Coe
Hi Dr Coe,
I am the Mother of an 18 year old son that has had 4 kidney stones this year. All bit the current One that hasn’t passed yet have been analyzed. The first one was made up of primarily uric acid, the next two and I suspect the one coming out have all been 100% ammonium your One that hasn’t passed yet have been analyzed. The first one was made up of primarily uric acid, the next two and a suspect the one coming out have all been 100% ammonium urate. He has a primary diagnosis of autism which is moderate to severe, so articulation is very difficult for him and his pain threshold is ridiculous! We typically don’t know that he even has a stone until he’s in trouble. He has multiple comorbid conditions, Specifically seizure disorder. He takes a large amount of Depakote but it is coupled with corner tour to help reduce the ammonia. He’s been on it for over 10 years and has just started developing stones in the past year. I’ve put him back on Flomax in hopes of being able to pass the 5 mm stone in his left kidney, the others have been 5.5mm, 3.8mm and 4mm, so he doesn’t make little stones. Any thoughts or ideas please? I’ve been researching chance piedra and wonder what you think of it please? Thank you so much!
Hi Laura, The ammonium acid urate stones are probably due to the high ammonia production which raises the urine pH and ammonia together. I do not know what ‘corner tour’ is as a counterpoise to the Depakote. I doubt the initial stone was uric acid because these require a very acid urine not likely in your son. I would advise 24 hour urine testing so we know what the chemistries are, and if it is high pH and ammonia what else is present. Chacha piedra is a trash remedy widely promoted by hucksters – rare for me to be so blunt. An excellent scientist did some initial work on it, but the results certainly did not warrant mass marketing as a stone crusher. Levocarnitine has some evidence as an agent to reduce ammonia production. Perhaps that is what your ” meant. If not, perhaps your physician might want to consider it. Regards, Fred Coe
Thank you for responding Dr Coe! That was a typo and es sir he has been taking carnitore (levocarnitine) for the same amount of time he has been on Depakote… specifically to keep ammonia down. We have done a 24 hour urine collection… his output was low, sodium and phosphorous and sulfate were elevated. Uric acid was normal.
Additionally the first stone results were :
60% ammonium acid urate
10%. Calcium phosphate
20% oxylate
2nd and 3rd stones analyzed were. 100%. Ammonium urate
4th stone was surgically removed this morning so we are awaiting results on its composition.
So my question is, do you think the levocarnatine that is supposed to reduce the ammonia is not working or that it’s got to be excreted through his kidneys this causing these?
Thank you Sir!
Hi Laura, You do not present the urine ammonia so we cannot tell if the drug is working or not. Do you have that measurement?? Regards, Fred Coe
Dr Coe, My sons ammonia levels are always within normal range. Don’t have the specific number but it’s never been outside of the normal range sir.
Hi Laura, if they are then the drug is presumably working, but the normal range is wide. Be sure ammonia is about 2/3 of the sulfate. The next step may be adding alkali – potassium citrate – enough to lower the urine ammonia further to stop the ammonium acid urate stones. This is complex and your physicians have to attend to the details. Regards, Fred Coe
I’ve read conflicting info about coffee in regards to kidney stones.
Some advise to stay away from coffee and caffeinated drinks, other reports say coffee drinkers have a lower risk of stones.
what is your opinion on coffee? assuming I’m drinking enough water and am not dehydrated.
Hi Paul, The data on coffee are encouraging- reduced stone risk in prospective epidemiological studies. Regards, Fred Coe
On July 1, 2019 I had a 5 mm. stone that had been lodged in the proximal portion of my ureter since, at least, May 1, 2018, move down to the distal portion of my ureter. Other than the pain felt on July 1 during its’ movement and the occult blood produced for a few days coincident with that movement, I have had no further symptoms of pain or occult blood. My Urologist order a KUB x-ray which showed the stone in the distal portion of the ureter on July 24th. Is there any reason to have this constantly x-rayed every few weeks and/or the stone removed by ureterscopy IF IT IS PRODUCING NO SYMPTOMS, whatsoever? Thank you, very much, for any advice, on this matter….of which I am in disagreement with my Urologist on what I see is an excessive prescription of testing on his part.
Hi Kurt, Here is the problem. It is precisely this kind of stone that can silently obstruct your kidney and cause irreparable damage, so in this case no amount of surveillance is too much – low risk, but of catastrophic outcome. If I were she/he I would be doing ultrasounds or flat plates and worrying about kidney loss. Likewise, after a while I would want the stone out altogether, and URS would be a first choice. Here is a rare case where an outsider with no real knowledge of your medical details can still weigh in – your physician is right and he/she is protecting you. Do it. Regards, Fred Coe
Hello Dr. Coe,
I am a 53 yr. old male, had 4 stones that required medical attention since i was 32. The last stone was in Aug. 2018 that was on the right side that 5.7mm that blocked the kidney and required Lithotrypsy and stent placement. The one in 2010 was on the left side and it was 6.4mm caused hydronephrosis and pylonephritis, required surgical intervention.
The stones were mixed.
The most current 24hr collection test showed: high SSCAOX, as well as Urine Oxalate, the PH 6.118, with moderate uric acid at 0.875.
What would you recommend, is there a specialist in NY to see?
Thank you,
Hi Yuri, Dr David Goldfarb practices in NY at NYU and is an expert in these matters. He will want to know what the stone was a mix of. I can recommend him highly. Regards, Fred Coe
Thank you Dr. Coe
Will b sharing your presentation with my Endocrinologist, Dr. Wayne Enron.
He has offered to help, where others have failed. Please tell me that there is DNA testing that can solve the kidney stone mystery, or fat malabsorption research that can unlock the mystery of bile salts.
Ever grateful,
Suzanne Plesha from Pennsylvania
P.S. Do you work with a colleague named Rita McGill? She was my kidney doctor in PA
Hi Suzanne, DNA has not been of much help so far. Fat malabsorption is a factor in people which small bowel malabsorption, from bowel resection, obesity surgery, or inflammatory bowel disease or pancreatic insufficiency. Rita and I do work together, and she is a wonderful colleague. Regards, Fred Coe
Thank you Dr. Coe,
for your prompt reply.
I see my Endocrinologist tomorrow, Dec. 3, I will be sharing your reply.
I had a RNY surgery in 2000. There is no history of stones in my family. I had one small stone in the upper folds of my right kidney which was removed in 2015. I have had small ones in the left that have passed on their own. This past Sept had a large ugly CaOX stone that was stuck in the top of my right ureter removed. There was no urine coming out of the right side noted in surgery. The Xrays and CT showed the stone but didn’t mention it was in the ureter just on the bottom of the kidney. I had no real symptoms and planned to get it done in November. Luckily circumstances of losing insurance happened and I had the surgery in Sept. My right kidney is much thinner than my left which looks normal. I do not know how long no urine was able to pass on the right side. My GFR was normal until 5 years ago and began going down.(I am 62) The last values were 38, now 42. Naturopaths have given me Kidney Korrect to try, I do a monthly IV to get more fluids and B vitamins. I am thinking to ask to switch from Lisinopril (been on for 10 years) to one with a diuretic if it helps with the stones. My fluid intake is low. I putout 1-1.2L/day and I have to push to get that. For fourty years I was a lab tech and not allowed to drink at work except during my 30 min lunch on an 8-12 hr shift. I’ve lost my natural ability to be thirsty. My diet has been chocolate and ice tea with very little water, supplemented with hi protein food because of the RNY. Between the RNY and the stones, many of the foods to eat conflict. My 24hr urine oxalate is extremely hi and citrate low. I’ve dropped the ice tea, still drink a cup of hot tea in the AM), drink some herbal teas, and trying to cut down on the chocolate. I’m trying to drink more as I am now retired and can drink freely for once, I am taking CitriCal twice a day. I had a sample of UriCit-KCit but the 15mg size is way too big for me to swallow so we are trying diet, more water and Citircal first. I will try now to follow a low oxalate diet and drink more water. AM I destined to have kidney failure at some point and continue to have stones? When the stent came out after 2 weeks there were visible crystals on the end of the stent.
Dear Lorri, You have a very serious problem. Some function is lost on the right from obstruction and overall kidney function is reduced a low and urine oxalate is very high. Your risks are partly from more stones, which can be improved with fluids and reduced diet oxalate, and with increased diet calcium to lower oxalate absorption. But crystals can form inside the kidneys and cause progressive renal failure. I would discuss this latter with your physicians, and consider the possibility of reversion to a gastric sleeve. The Roux en Y procedure drives your high urine oxalate, and it is hard to reduce it. Be sure and discuss this matter with your physicians sooner than later. Regards, Fred Coe
Can you recommend a surgeon in San Francisco who can help me with my stones. I am in so much pain. I am a 53yr old male and my last urologist Dr Kahn had retired and I desperately need a great recommendation as I have extreme pain on my right side from new stones
Hi Milo,
Dr. Marshall Stoller is a prominent doc in your area at UCSF
Best, Jill
Dr. Coe, I appreciate the information you share with us! So far, I have never passed a kidney stone, but I have heard stories from an aunt. I have had quite a lot of joint pain, and that pain moves around a lot including to my back. Sometimes it is just a stiff neck, other times it is pain in my achilles tendon, pain in my knee, or pain in my back. I suspect some of the pain has been in my kidneys. While I work I try to find time to drink water and coffee. It is difficult to find the time. In the past, I ate green vegetables daily including spinach, asparagus, or broccoli. That has been stopped, because of the oxalates. In the past, I occasionally took calcium supplements, but I’ve noticed the calcium supplements and vitamin D have been associated with my increased pain. Now I think you would suggest that we consume dairy products, and maybe you would suggest they be combined with the cocoa or coffee we crave. I snack on salted peanuts, and maybe I should stop. I have tried potassium citrate, and I noticed it relieved my back pain. Simultaneously, it seems to change the dull joint pain into intermittent stinging in random spots under my skin. Maybe you can shed some light on what I am experiencing. And is it likely that my joint pain is related to calcium oxalate? https://www.nutritionist-resource.org.uk/memberarticles/oxalates-a-possible-cause-of-pain-and-illness
Hi Richard, Since you do not have known stones, much of what we write here does not apply to you. Oxalate is a rather modest offender in people with normal kidneys and not likely to cause systemic pain despite the occasional hype in the press. I would strongly suggest leaving well enough alone and not doing serious changes in diet or taking supplements without your physician’s help. If you are concerned about stones, ultra low dose CT scanning poses minimal radiation risk and can settle the matter. Regards, Fred Coe
Dr. Coe, I appreciate the information you share with us! So far, I have never passed a kidney stone, but I have heard stories from an aunt. I have had quite a lot of joint pain, and that pain moves around a lot including to my back. Sometimes it is just a stiff neck, other times it is pain in my achilles tendon, pain in my knee, or pain in my back. I suspect some of the pain has been in my kidneys. While I work I try to find time to drink water and coffee. It is difficult to find the time. In the past, I ate green vegetables daily including spinach, asparagus, or broccoli. That has been stopped, because of the oxalates. In the past, I occasionally took calcium supplements, but I’ve noticed the calcium supplements and vitamin D have been associated with my increased pain. Now I think you would suggest that we consume dairy products, and maybe you would suggest they be combined with the cocoa or coffee we crave. I snack on salted peanuts, and maybe I should stop. I have tried potassium citrate, and I noticed it relieved my back pain. Simultaneously, it seems to change the dull joint pain into intermittent stinging in random spots under my skin. Maybe you can shed some light on what I am experiencing. And is it likely that my joint pain is related to calcium oxalate? https://www.nutritionist-resource.org.uk/memberarticles/oxalates-a-possible-cause-of-pain-and-illness
Hi Richard, Since you do not have known stones, much of what we write here does not apply to you. Oxalate is a rather modest offender in people with normal kidneys and not likely to cause systemic pain despite the occasional hype in the press. I would strongly suggest leaving well enough alone and not doing serious changes in diet or taking supplements without your physician’s help. If you are concerned about stones, ultra low dose CT scanning poses minimal radiation risk and can settle the matter. Regards, Fred Coe
Dear Dr. Fred
Back with a doubt. I did analysis to my vit D and although i go and walk in the sun during summer months and eat a varied diet, now in the winter months, my endocrinologist told me to take vit D, one pill a month. She told me it is only maintenance, not treatment. Is it OK? She told me it wont increase my risk of stones. Thanks
Hi Maria, Routine vitamin D supplements do not raise kidney stone risk. Regards, Fred Coe
Dear Dr. Fred
Back with a doubt. I did analysis to my vit D and although i go and walk in the sun during summer months and eat a varied diet, now in the winter months, my endocrinologist told me to take vit D, one pill a month. She told me it is only maintenance, not treatment. Is it OK? She told me it wont increase my risk of stones. Thanks
Hi Maria, Routine vitamin D supplements do not raise kidney stone risk. Regards, Fred Coe
Your website is by far the most informative I have found and I thank you in advance for any insight you may have. I am 62 have passed a 7mm stone in 2006 and another 4mm in 2018. (calcium oxalate) I currently have 3 stones in each kidney- I have no pain, no abscess etc. I follow up yearly and each time they find 1-3 stones but this is the first time that 2 stones measure over 4mm. I have faithfully taken B6 and magnesium and drink at least 2.5 L fluids daily. But in hindsight, I see that I eat way too many green leafy vegetables, nuts, and dark chocolate and possibly not enough calcium (either 1/2 cup of milk or 1 container yoghurt and a bit of cheese every day). Do I have to schedule a shock wave lithotripsy per my doctor’s recommendation or can I wait and make some drastic changes in my diet and possibly reduce the stones?
Hi Sandra, You have calcium oxalate stones that are ongoing, and you do not know why. I would strongly suggest testing 24 hour urine and blood to find out and focus treatment on what is the cause of your stones. Changing diet without knowledge can be futile. Regards, Fred Coe
Your website is by far the most informative I have found and I thank you in advance for any insight you may have. I am 62 have passed a 7mm stone in 2006 and another 4mm in 2018. (calcium oxalate) I currently have 3 stones in each kidney- I have no pain, no abscess etc. I follow up yearly and each time they find 1-3 stones but this is the first time that 2 stones measure over 4mm. I have faithfully taken B6 and magnesium and drink at least 2.5 L fluids daily. But in hindsight, I see that I eat way too many green leafy vegetables, nuts, and dark chocolate and possibly not enough calcium (either 1/2 cup of milk or 1 container yoghurt and a bit of cheese every day). Do I have to schedule a shock wave lithotripsy per my doctor’s recommendation or can I wait and make some drastic changes in my diet and possibly reduce the stones?
Hi Sandra, You have calcium oxalate stones that are ongoing, and you do not know why. I would strongly suggest testing 24 hour urine and blood to find out and focus treatment on what is the cause of your stones. Changing diet without knowledge can be futile. Regards, Fred Coe
Honorable Dr. Coe,
After going through numerous doctors/urologists/nephrologists, i am stuck in the position of having little to no hope of prevention of these recurrent stones. At one point, I had passed 6 in a month with the biggest being 1.4 cm.
I have the returned results of supersaturation profiles as well as serum results but as a layman, these are little or no use to me without the expertise. Having received the results, my doctor’s just prescribe the regular – “drink lemon water route”. As I know how beneficial the lemon water can be in prevention of my oxalate and phosphate oxalate stones I have continuously utilized these guidelines as well as the guidelines of increased calcium/limited sodium to no avail. It seems hopeless. I am constantly at a point of having a stone in my ureter at any given time. I have gone through numerous doctors who offer no help in prevention or cause but of course opt for treatment of current stones via surgery (understandably so). The follow up is scarce or lacking even after pushing.
As background, I am not an overweight individual at 6’0, weighing 180 lbs, living a semi sedentary life at an office job.
My supersaturation profiles come up normal with the below heavy discrepancies:
Citric acid : 15 mg/24 hr
Urine sulfate : 32 mEq/24hr
Calcium Oxalate ratio : 6.41
Brushite Ratio : 4.21
Monosodium urate : 6.49
I know a lot of these are a “hodge-podge” of ingredients and the perfect storm for stone formation.
Please note – ph levels of urine always indicate the 7-7.5 range.
My blood levels at this point come up with high creatinine content at ~1.68 range.
Blood urea nitrogen also comes up as ~24 mg/dL
A recent test of pth function came up as the pth intact value of 98.9 pg/mL.
My first stone attack was 2015-2016 and I am a 27 yo make.
I take escitalporam oxalate 7.5 mg – and I see in the very rare side effects is stone formation but have been told numerous times this is not the cause.
I do not know what to do and need true expertise in the field.
Thank you kindly doctor.
Hi Paul, You do not mention what your many stones are made of. I suspect they are hydroxyapatite given the shocking urine pH of 7-7.5. You have reduced kidney functions (creatinine in serum 1.68) and the high PTH of 98 could be from that or from primary hyperparathyroidism – you do not mention your serum calcium level as being high; is it? The high urine pH and almost negligible urine citrate suggest a form of renal tubular acidosis. I have also seen this in phosphate stone formers whose blood levels of total CO2 are normal. The drug is not a stone risk despite the menacing name – a search of PubMed shows no cases of the drug causing renal tubular acidosis. I think you need a very skilled stone expert to figure out what is wrong. If you tell me where you live I could try to identify someone near enough. Regards, Fred Coe
Honorable Dr. Coe,
After going through numerous doctors/urologists/nephrologists, i am stuck in the position of having little to no hope of prevention of these recurrent stones. At one point, I had passed 6 in a month with the biggest being 1.4 cm.
I have the returned results of supersaturation profiles as well as serum results but as a layman, these are little or no use to me without the expertise. Having received the results, my doctor’s just prescribe the regular – “drink lemon water route”. As I know how beneficial the lemon water can be in prevention of my oxalate and phosphate oxalate stones I have continuously utilized these guidelines as well as the guidelines of increased calcium/limited sodium to no avail. It seems hopeless. I am constantly at a point of having a stone in my ureter at any given time. I have gone through numerous doctors who offer no help in prevention or cause but of course opt for treatment of current stones via surgery (understandably so). The follow up is scarce or lacking even after pushing.
As background, I am not an overweight individual at 6’0, weighing 180 lbs, living a semi sedentary life at an office job.
My supersaturation profiles come up normal with the below heavy discrepancies:
Citric acid : 15 mg/24 hr
Urine sulfate : 32 mEq/24hr
Calcium Oxalate ratio : 6.41
Brushite Ratio : 4.21
Monosodium urate : 6.49
I know a lot of these are a “hodge-podge” of ingredients and the perfect storm for stone formation.
Please note – ph levels of urine always indicate the 7-7.5 range.
My blood levels at this point come up with high creatinine content at ~1.68 range.
Blood urea nitrogen also comes up as ~24 mg/dL
A recent test of pth function came up as the pth intact value of 98.9 pg/mL.
My first stone attack was 2015-2016 and I am a 27 yo make.
I take escitalporam oxalate 7.5 mg – and I see in the very rare side effects is stone formation but have been told numerous times this is not the cause.
I do not know what to do and need true expertise in the field.
Thank you kindly doctor.
Hi Paul, You do not mention what your many stones are made of. I suspect they are hydroxyapatite given the shocking urine pH of 7-7.5. You have reduced kidney functions (creatinine in serum 1.68) and the high PTH of 98 could be from that or from primary hyperparathyroidism – you do not mention your serum calcium level as being high; is it? The high urine pH and almost negligible urine citrate suggest a form of renal tubular acidosis. I have also seen this in phosphate stone formers whose blood levels of total CO2 are normal. The drug is not a stone risk despite the menacing name – a search of PubMed shows no cases of the drug causing renal tubular acidosis. I think you need a very skilled stone expert to figure out what is wrong. If you tell me where you live I could try to identify someone near enough. Regards, Fred Coe
Dear Dr. Coe:
I have been diagnosed with a bladder infection of Morganella Morganii 100,000 CFU/ml. This type of bladder infection is typically associated with catheters and bladder stones. The urologist did not do any tests for bladder stones and I clearly am not catheterized. She said that bladder stones generally don’t occur in women because our ureters are short and large diameter. My symptoms are frequent urination of small volumes and on infrequent occasions some dull aches in my lower abdomen which I interpret to be emanating from my bladder. I am post menopausal and have a BMI of 25.
Alb/Cr Ratio, Random 8 mcg/mg Cr (0 – 29 mcg/mg Cr)
U Albumin Conc, Random 7.2 mg/L
U Creatinine 87 mg/dl
My eGFR has ranged from 59 to 70 mL/min/1.73 m² over the last 5 years
Here is a little history – I started a ketogenic diet when diagnosed with diabetes almost 5 years ago. Although diagnosed as Type 2 initially, it was later determined to be Latent Autoimmune Diabetes of Adults (LADA), Type 1. My diabetes is well controlled my HbA1c was 5.6 at last testing. The ketogenic diet was able to allow me to avoid starting insulin for 4 years, but I was consuming foods that were high in oxalates (particularly almonds, almond milk, and almond flour, as well as spinach). About 1-1/2 years ago I developed bladder pain that sometimes was bad enough to keep me awake at night. After researching on the internet I came to the conclusion that it might have been caused by high oxalates, so I cut way down on high oxalate containing foods. The bladder pain essentially went away, but I was left with the symptoms of more frequent urination of small volumes which the urologist attributed to being older (65) and incomplete emptying of my bladder. So my question is this: might I be an unusual case of a women with bladder stones and that the stones are potentially creating a welcoming environment for the Morganella bacteria and also making complete emptying of my bladder difficult? I have not been treated for the bladder infection, as the antibiotic offered had nasty side effects, so I declined to take it. The urologist did not think having the infection was a concern. None of my doctors have been concerned with my somewhat low eGFR, but it makes me wonder if it could be related to the oxalates. I have read research on hydroxycitrates (before seeing the post on your website) and recently started taking some to see if it would make any difference. Would you recommend pursuing any additional testing based on my history?
Hi Betty, I would think a CT of the bladder area would disclose any stones. I would ask my urologist why your bladder does not empty completely given that the female urethra is indeed short. A (very) brief review of M Morganii on PubMed yielded many hits. Here is a recent review. The organism has urease so it can transform urea into ammonia and promote struvite infection stones. This is why it is very important to look for stones in your bladder – or perhaps crystals. It is a pathogen and highly resistant to antibiotics, and increasing in prevalence world wide. I am concerned that if it is producing crystals using urease it can persist in your bladder, cause your symptoms by irritating the bladder lining, and possibly reach into the kidneys. I would start with ways to look for crystals. Antibiotics are not very effective given its remarkable resistance elements. I wonder how it got there – in you. On PubMed you will find a lot of articles like this one. Regards, Fred Coe
Dear Dr. Coe:
I have been diagnosed with a bladder infection of Morganella Morganii 100,000 CFU/ml. This type of bladder infection is typically associated with catheters and bladder stones. The urologist did not do any tests for bladder stones and I clearly am not catheterized. She said that bladder stones generally don’t occur in women because our ureters are short and large diameter. My symptoms are frequent urination of small volumes and on infrequent occasions some dull aches in my lower abdomen which I interpret to be emanating from my bladder. I am post menopausal and have a BMI of 25.
Alb/Cr Ratio, Random 8 mcg/mg Cr (0 – 29 mcg/mg Cr)
U Albumin Conc, Random 7.2 mg/L
U Creatinine 87 mg/dl
My eGFR has ranged from 59 to 70 mL/min/1.73 m² over the last 5 years
Here is a little history – I started a ketogenic diet when diagnosed with diabetes almost 5 years ago. Although diagnosed as Type 2 initially, it was later determined to be Latent Autoimmune Diabetes of Adults (LADA), Type 1. My diabetes is well controlled my HbA1c was 5.6 at last testing. The ketogenic diet was able to allow me to avoid starting insulin for 4 years, but I was consuming foods that were high in oxalates (particularly almonds, almond milk, and almond flour, as well as spinach). About 1-1/2 years ago I developed bladder pain that sometimes was bad enough to keep me awake at night. After researching on the internet I came to the conclusion that it might have been caused by high oxalates, so I cut way down on high oxalate containing foods. The bladder pain essentially went away, but I was left with the symptoms of more frequent urination of small volumes which the urologist attributed to being older (65) and incomplete emptying of my bladder. So my question is this: might I be an unusual case of a women with bladder stones and that the stones are potentially creating a welcoming environment for the Morganella bacteria and also making complete emptying of my bladder difficult? I have not been treated for the bladder infection, as the antibiotic offered had nasty side effects, so I declined to take it. The urologist did not think having the infection was a concern. None of my doctors have been concerned with my somewhat low eGFR, but it makes me wonder if it could be related to the oxalates. I have read research on hydroxycitrates (before seeing the post on your website) and recently started taking some to see if it would make any difference. Would you recommend pursuing any additional testing based on my history?
Hi Betty, I would think a CT of the bladder area would disclose any stones. I would ask my urologist why your bladder does not empty completely given that the female urethra is indeed short. A (very) brief review of M Morganii on PubMed yielded many hits. Here is a recent review. The organism has urease so it can transform urea into ammonia and promote struvite infection stones. This is why it is very important to look for stones in your bladder – or perhaps crystals. It is a pathogen and highly resistant to antibiotics, and increasing in prevalence world wide. I am concerned that if it is producing crystals using urease it can persist in your bladder, cause your symptoms by irritating the bladder lining, and possibly reach into the kidneys. I would start with ways to look for crystals. Antibiotics are not very effective given its remarkable resistance elements. I wonder how it got there – in you. On PubMed you will find a lot of articles like this one. Regards, Fred Coe
Hi Doctor,
I had 5 kidney stones (4-6 mm) removed, and I did a 24hrs urine analysis right after. The urine oxalate was high (63.6 mg/day) and low citrate (196 mg/day). My urine output was 4.9 l (I drank a lot).
I am concerned about my oxalate levels, are they dietary or due to loss of good bacterias during the surgery? I am a vegetarian, but I have moderate oxalate level food, though low calcium intake. My urologist did not mention Primary hyperoxaluria saying it has around more (100 or more) oxalate levels. My age is 25.
I never had any GI issues as well, so not sure if it is for Secondary hyperoxaluria.
Also concerned about my citrate levels.
I just want to know if this are dietary or some underlying issues?
Thank you!
Hi Trusha, Your urine oxalate is very high and I would repeat the study. Citrate is very low and it is not clear why as you do not give me all of the data. As a vegetarian you might have raised urine oxalate by diet, or by low calcium intake along with food oxalate. Or you might indeed have a form of primary hyperoxaluria. Do it again, make note of what you ate – all of it – and supplements and see if this is consistent. Regards, Fred Coe
Hi Doc!!
I apologize for not giving all of the data, as my doc ordered only some of it. The rest like urine magnesium, calcium and rest were all in normal range.
I redid the test again last week after one year, and to my happiness, my oxalates levels are back to 16mg/day as well as citrates have increased to 460mg/day
Here’s the latest report
Timed Urine Chemistry
Total Volume
Urine volume: 3800
Collection date start: 27-MAR-2025
Collection time start: 0730
Urine Creatinine
Urine Creatinine 24h
A
4.6
5.0-16.0
mmol/d
Urine Urate
Urine Urate 24h
1.5
<5.9
mmol/d
Urine Calcium
Urine Calcium 24h
3.91
1.0-7.0
mmol/d
Urine Citrate
Urine Citrate 24h
2.5
0.7-4.9
mmol/d
Effective Feb. 27, 2023, this test is
performed on a new analyzer.
Urine Oxalate
Urine Oxalate 24h
186
40-340
umol/d
For one year, I managed a low to medium oxalate level food and increased my calcium intake with taking chanca peidra.
Hi Trusha, Things look rather good. I would expect stones should be sparse or not at all. Fred