I do not know if Edvard Munch (1863 – 1944) had Lot’s wife in mind, but I do and thought this an apt image.
She crystallized, perhaps into calcium carbonate, hence my putting her here at the beginning of our sojourn into the vast territories of calcium metabolism and the hypercalciuric states. If I were to single out one condition that dominates stone disease prevention because of sheer commonness and reliable means of treatment it would be this one.
I have put off the crucial topic of hypercalciuria for the first year of this site because I wanted to build a proper foundation.
We now have good materials about stones and stone crystals, supersaturation, and certain critical treatments such as potassium citrate and high fluid intake.
It is time to tackle the problem of high urine calcium itself, what happens when it is high, why it might be high, what levels pose stone risk, and how it is best treated so far as we know.
This article lays out the relationships between urine calcium and stone risk, names the important causes of high urine calcium in stone forming people, and the other problems high urine calcium may be related to.
It is an introduction: Long, but brief in comparison to what is a major component of stone disease and its clinical management.
What is Hypercalciuria?
Stone Risk
To me the most immediate definition is about stones: At what level of urine calcium is the risk of new stone onset increased?
The best information to date arises from long term longitudinal data contributed by two cohorts of nurses and one of physicians exploited by Dr. Gary Curhan. In each cohort, some people became stone formers, and most did not. Gary obtained 24 hour urines in a cross section from all three cohorts, and was able to relate the level of urine calcium excretion to the risk of forming stones.
 Along the horizontal axis urine calcium excretions are groups into 6 bins; above each bin the relative risk of becoming a stone former is presented for the two nurse cohorts (all women, and in red bars) and the physician cohort (all men and in blue bars). The dashed line is at 1, meaning the baseline of risk for the population which was at taken at <100 mg/day of urine calcium loss.
Along the horizontal axis urine calcium excretions are groups into 6 bins; above each bin the relative risk of becoming a stone former is presented for the two nurse cohorts (all women, and in red bars) and the physician cohort (all men and in blue bars). The dashed line is at 1, meaning the baseline of risk for the population which was at taken at <100 mg/day of urine calcium loss.
The relative risks are given in the manuscript as an average (mean) value and an upper and lower 95% confidence limit. But I am showing only the lower 95% confidence limit (solid bars) and means (lighter bars).
For example, in the 100-149 bin the mean relative risk for the first of the two female (red) cohorts is 1.26 (plotted up from 1 as a light bar), the lower limit is 0.84 (plotted down from 1 in a solid red bar) and the upper limit is 1.91 (not plotted).
I am after a measure of risk that is robust: In which bin is it very likely that risk is increased above the 100 mg/day baseline?
For me, that is when the lower limit for the relative risk is above 1.
For example, the value of the lower 95% risk confidence limit of the 100-149 bin, in the first of the two nurse cohorts – 0.84 – does not connote a high likelihood of significant risk compared to 100 mg/day of urine calcium.
On the other hand, risk is very likely present above 200 mg/day of urine calcium, because the lower 95% limit is above 1 in all three cohorts. Of interest, women and men do not seem to differ, so this one criterion applies to both sexes equally.
Also of interest and great importance, there is a dose response.
Higher and higher urine calcium levels are associated with higher and higher relative risk. This is good supportive evidence of a causal connection and best seen by the position of the means which are at the tops of the bars..
The direction of causality is not determinable from observation, but I vote for higher urine calcium causing stones not that being a stone former somehow raised urine calcium.
My vote is because of the other science.
This site has belabored the point that supersaturation drives crystallization, and stones are made of crystals. In preparation for this new series of articles on urine calcium I have gathered the main articles on the stones themselves and on supersaturation into a pair of ‘walking tours’ which present them in context and with with commentary. These are the foundational articles upon which the effects of urine calcium and other urine constituents can be assembled to produce a reliable picture of how stones form and how they can be prevented.
Here, I simply note that higher urine calcium loss will increase average urine calcium concentration for any given urine flow rate, and higher calcium concentrations will in general produce higher SS values for calcium phosphate and calcium oxalate and therefore higher risk of stones. So hypercalciuria, to me, and for good reasons, is almost certainly a cause of calcium stones via increase of SS which is the prime measure of the energy that drives crystallization.
Upper End of the Normal Range
A valid and alternative definition of hypercalciuria is that it consists in very high urine calcium excretion, and a way to gauge the meaning of ‘very high’ would be values at the upper end of the normal range. This idea of the ‘upper end’ is usually taken as above the upper 95% of values encountered in surveys of people without known diseases.
The Curhan data actually give a reasonable measure of this ‘upper end’ from the means and 95% limits of the non stone formers in the three cohorts. The lower dot marks the position of the lower 95th percentile of 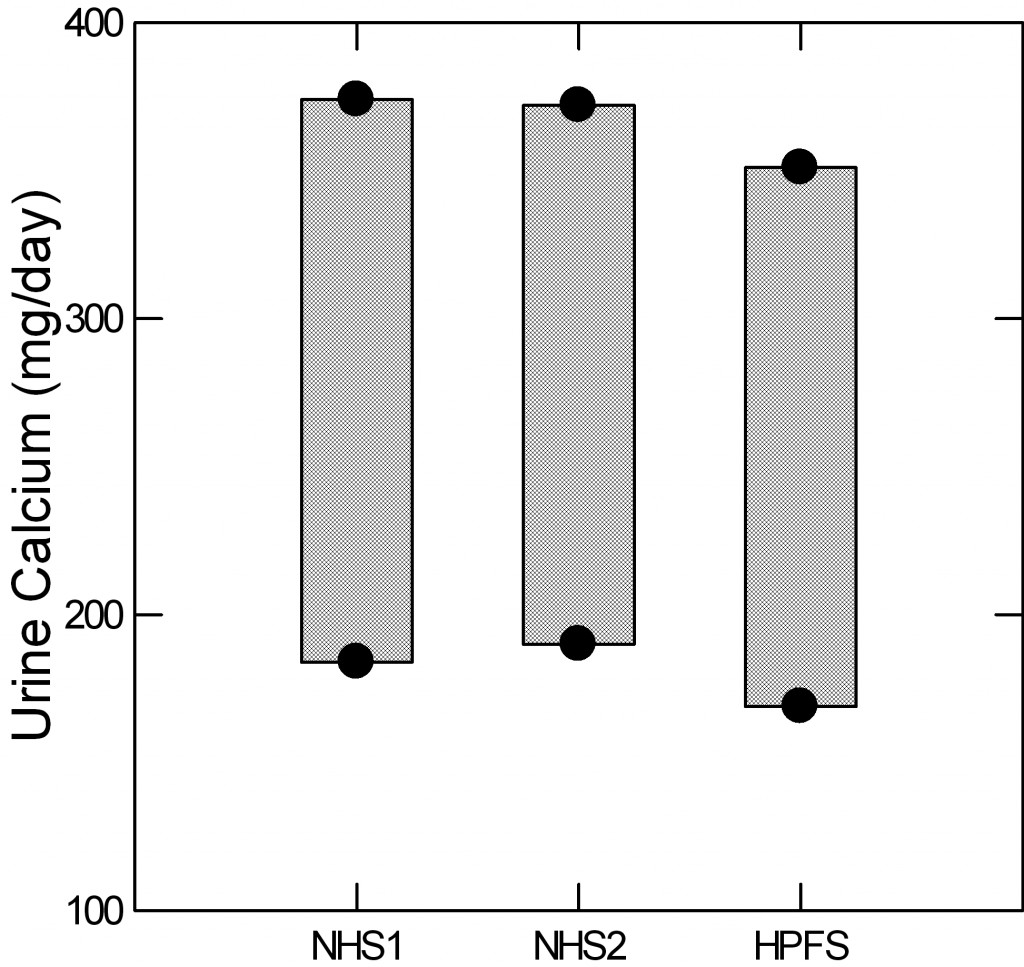 urine calcium for the two nurse cohorts and the physician cohort. The upper dot gives the upper 95th percentile (two standard deviations above the mean for those technically inclined). The intervening bars are for visual effect.
urine calcium for the two nurse cohorts and the physician cohort. The upper dot gives the upper 95th percentile (two standard deviations above the mean for those technically inclined). The intervening bars are for visual effect.
For those who want to study hypercalciuria, as an example, and want a reliable gauge of who is ‘really high’ the three figures are 374 372 and 351 mg/day for the three groups.
Older Conventions
Using smaller and less well selected populations, many investigators have derived somewhat different upper limits for defining hypercalciuria. For example urine calcium excretions above 250 mg/day or above 4 mg/kg body weight are common as in this typical kind of research publication. In our own reviews we have frequently used 250 mg/day for women, 300 mg/day in men, and 4 mg/kg body weight either sex as upper limits to define hypercalciuria.
Overview
I think that the Curhan values are ideal for clinical practice. People with calcium stones and urine calcium levels above 200 mg/day have increased risk from their urine calcium and one aspect of their treatment can be to reduce urine calcium.
That is to say, physicians look at all possible factors that may be increasing risk in a patient, sort them out and select for treatment those most promising and practical to treat. Among them will often be urine calcium and Curhan has given us good targets and criteria.
For research, I am more flexible. Strictly speaking the 95% upper limits are a kind of ideal, but if you want to understand mechanisms that raise urine calcium one might be better served by selecting cohorts with a range from high normal to very high. These are research design decisions, and all I mean to say here is we have decent ideas about normal ranges and stone risk, and it is possible from them to derive appropriate approaches to clinical research on hypercalciuria.
Diseases That Cause Hypercalciuria in Stone Formers
Let me be clear about goals here. Each of these diseases will get its own articles, or perhaps many articles, so this is not meant to be a proper exposition but merely an introduction.
For this reason referencing is light and I mainly make assertions which are commonplace and can be found in any textbook or review article. When I get to the diseases one by one I hope to offer considerably more than is commonplace.
Primary hyperparathyroidism (PHPT)
About 3 – 5% of calcium stone formers have this curable disease, on average, so its detection is crucial for proper patient care. As a reference I have used my own publication because it contrasts patients with this disease to ordinary stone formers, is available as a free pdf, and, perhaps, because I wrote it.
One or more of the parathyroid glands enlarges and produces an excess of parathyroid hormone (PTH). PTH signals kidney cells to retain calcium by reabsorbing a higher fraction of calcium that is filtered by the glomeruli. It stimulates production of the active form of vitamin D (calcitriol) and that in turn increases the efficiency of GI absorption of calcium from foods. Finally PTH increases bone turnover so more calcium than normal leaves the bone and can be lost in the urine.
The increased bone calcium loss and increased GI calcium absorption are balanced by increased urine calcium losses, and these can be very impressive. The high urine calcium losses raise urine supersaturation with respect to calcium oxalate and calcium phosphate so stone risk rises and patients with this disease not uncommonly present themselves as stone formers.
High rates of mineral loss from bone cause bone mineral depletion, and bone disease is well known to occur. If the disease is cured in a timely way bone healing is expected.
The action of PTH to increase the fraction of filtered calcium that is reabsorbed causes blood calcium to rise. The increase is often modest.
Being rarely malignant, the enlarged parathyroid glands can be removed surgically with expectation of a cure, so this disease is a curable cause of kidney stones and bone disease.
The diagnosis depends upon finding high urine calcium excretion, a serum calcium concentration above normal for the laboratory making the measurement, and a serum PTH value which is not suppressed below the normal range.
However, there are a few cautions that must be considered always. Even if everything I have just said is true, there are artifacts that lead to mistakes in diagnosis and could lead to unnecessary surgery. All thiazide type diuretics can raise serum calcium, so testing needs to be done after 2 weeks off the drug. Lithium can raise both serum calcium, serum PTH and even urine calcium, so is a real fooler. Hyperthyroidism, including that induced by too much thyroid hormone replacement, can raise serum and urine calcium although it does suppress serum PTH. The serum for PTH must be the one for the calcium – same blood draw for both, and must be drawn fasting overnight.
The relationship between PTH and serum calcium is often misunderstood. The calcium balance systems are elaborate and tend to be self regulating, so increased PTH secretion leads to increases in serum calcium and calcitriol both of which, through negative feedback on the glands, bring PTH down toward or even to normal, but never below normal. Therefore PHPT is diagnosed when the serum calcium is above normal and the PTH is not below normal.
Here are the serum and urine calcium values from the PHPT cases in our publication – all proven surgically – shown in large dots, normal people (medium dots) and thousands of points from stone formers without any systemic disease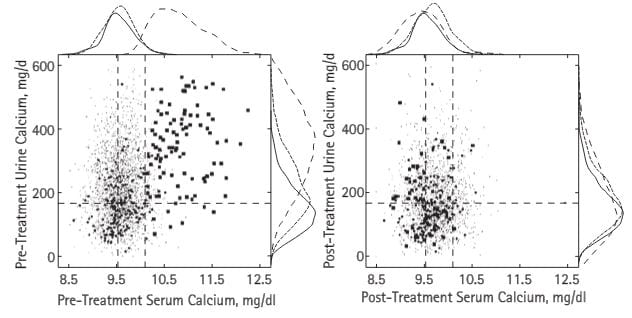 – fine spray of tiny dots (common stone formers). The vertical dashed lines are the normal range for blood calcium in our kidney stone laboratory, the horizontal line is just below the level where stone risk from urine calcium begins (200 mg/day).
– fine spray of tiny dots (common stone formers). The vertical dashed lines are the normal range for blood calcium in our kidney stone laboratory, the horizontal line is just below the level where stone risk from urine calcium begins (200 mg/day).
The patients all had serum calcium values above normal but many were just slightly high. Urine calcium was a lot higher than in ordinary stone formers, but even in those the plume of fine dots rose far above 200 mg/day. Note that some normal people had values above 200 mg/day.
After surgical cure (right panel) the PHPT cases, normals, and treated common stone formers who had no systemic disease all contracted into a small region, but not a few urine calcium values were above the fateful 200 mg/day limit still.
The curves outside the boxes show the distributions; see how the hyperparathyroidism points (dashed lines) spread out far above those for normals and ordinary stone formers, then fall back with surgical cure.
Normocalcemic Primary Hyperparathyroidism
Properly speaking this would be high urine calcium excretion, normal blood calcium, and reasons to think that an abnormality of parathyroid gland function was responsible for the high urine calcium – which is the only abnormality. One such reason could be an elevated level of serum PTH, and such levels are encountered from time to time. Another could be blurring of the true upper limit for serum calcium; not all laboratories are equally crisp. A third could be, and this is speculative, that along the course of PHPT glands might lose their normal CaSR responsiveness, so that PTH levels are no longer down regulated normally by serum calcium. In another article I will explore this problem. Right now, I believe it is wiser to wait for hypercalcemia before committing to neck surgery in hopes of cure and treat the hypercalciuria as if it were idiopathic hypercalciuria – see below. PHPT will ultimately declare itself in most cases. The reference in the link above is supportive of my suggestions because the authors expect elevated serum calcium in PHPT, as I do.
Secondary Hyperparathyroidism
Being so caught up in the maintenance of a normal serum calcium, the parathyroid glands will react to any threat with increased or decreased PTH secretion as required to restore that normal value. Low calcium diet, vitamin D deficiency, GI diseases with calcium malabsorption for any reason, chronic kidney disease with its odd form of calcium aberrations, all these will and do cause increase of PTH secretion and raised serum PTH levels. None of these are hypercalcemic states, and most have a low urine calcium loss. Stones may be present but for reasons other than parathyroid abnormalities, and often other than level of urine calcium. For example, acid urine pH from kidney disease can cause uric acid stones; high urine oxalate from bowel disease can cause calcium oxalate stones. All I mean to say here is that isolated increase of serum PTH with low or even normal urine calcium and normal or low serum calcium levels are usually not an occasion for parathyroidectomy, but call for a diagnosis of their own. As I have by said to excess, this is an issue that deserves more than an introduction. The link for normocalcemic primary hyperparathyroidism is useful for this topic and the one below.
Familial Hypocalciuric Hypercalcemia (FHH)
High serum calcium with low urine calcium excretion – below 100 mg/day is common – is almost never primary hyperparathyroidism but rather a mutation of the PT gland CaSR that raises its sensitivity so serum calcium can be low, serum PTH normal, and urine calcium quite low. When FHH patients have stones the stones are not due to high urine calcium but some other cause, and most importantly parathyroid surgery is a mistake.
Sarcoidosis
In my long experience I have seen far less than 1% of calcium stone formers present with this condition. A reputable source of information about Sarcoidosis fails to mention kidney stones so far as I could see.
Briefly, sarcoidosis is a disorder of the immune system and the cells which proliferate and enlarge lymph nodes, liver, spleen and other tissues produce calcitriol. So the physiology is that of unbalanced high calcitriol production.
As I have mentioned above, calcitriol increases GI calcium absorption, so food calcium entry into the blood increases. I have not mentioned but say now that calcitriol increases net bone mineral losses mainly by reducing bone production. Calcitriol is a steroid hormone and like many steroids acts on the nuclei of cells. It acts on parathyroid cells to shut down production of PTH so tubule reabsorption of filtered calcium is reduced as compared to primary hyperparathyroidism.
The increases in bone mineral loss and GI calcium absorption raise urine calcium excretion as in hyperparathyroidism. Because PTH is suppressed below normal, serum calcium may not rise or when it does so rises only slightly at first.
This means that in many instances suppressed serum PTH may be the only laboratory clue to sarcoidosis as a cause of hypercalciuria and stones. Clinically sarcoidosis is often diagnosed from its signs and symptoms, as noted in the reference from the National Heart and Lung institute. I have had cases which I diagnosed de novo being without obvious signs otherwise because of suppressed PTH with very high urine calcium and even elevated serum calcium.
Serum calcium rises when the flows of calcium from bone and GI absorption are very marked or when the efficiency of renal calcium removal falls.
This latter can occur because of calcium itself. It can reduce water and salt conservation and therefore reduce the blood volume and therefore filtration. Any reduction will tend to increase serum calcium, and increases in serum calcium will reduce filtration and water losses, so a kind of unhappy cycle begins. How calcium acts to reduce calcium reabsorption and that it also acts on filtration itself comes later, not in this article but in those perhaps months from now.
CYP24A1 Deficiency
Vitamin D3 is made in the skin or consumed in pills, and in the liver converted into 25 hydroxy (OH) vitamin D (25(OH)D3). The enzymes responsible for the conversion are called CYP2R1 and CYP27A1.
25(OH)D3 circulates and is itself biologically active, but has a larger fate. Some is converted by kidney cells into 1,25(OH)2D3 (calcitriol for ease of writing and reading) and it is this molecule which more powerfully activates tissue responses in the GI tract, kidneys, bone, and – as already mentioned – parathyroid cells. The enzyme which activates 25(OH)D3 to calcitriol is called CYP27B1.
CYP24A1 is a general purpose inactivator of 25(OH)D3 and calcitriol. It converts the former into inactive molecules in liver. In kidney it converts calcitriol into other inactive molecules. If this degrading enzyme is deficient because of mutations, calcitriol levels increase as in Sarcoidosis, and one gets a similar picture of high urine calcium suppressed serum PTH and high normal to high serum calcium, with kidney stone formation as a consequence of the high urine calcium.
This is a rare condition; in my lifetime of practice I have encountered only 2 cases I know of.
Vitamin D and Calcium Supplement Excess
Certainly, these OTC materials are associated with increases of urine and even serum calcium, especially noted in menopause when their use is prevalent. Causality is not certain. For example, serum 25(OH)2D3 levels between 20 (a low number) and 100 (a high number) were not associated with kidney stones in a small sample of 2012 people. However in a large trial, it appeared that calcium supplements, not food calcium, might be specifically a risk for stones. Calcium supplements might be a particular hazard in people prone to high urine calcium excretion by their genetics.
Distal Renal Tubular Acidosis
I have referenced our paper not out of community pride but because it is the only one which describes the papilla and separates stones from nephrocalcinosis. In a massive surgical practice at the Kidney Stone Center at Indiana University we could find only 5 cases on whom we have operated and obtained research information about the papillary tissues.
All five had the expected reduction of serum bicarbonate with increased serum chloride (no elevated anion gap), alkaline urine pH, and reduced serum potassium – from the obligatory bicarbonate driven kaluresis. Several were hypercalciuric.
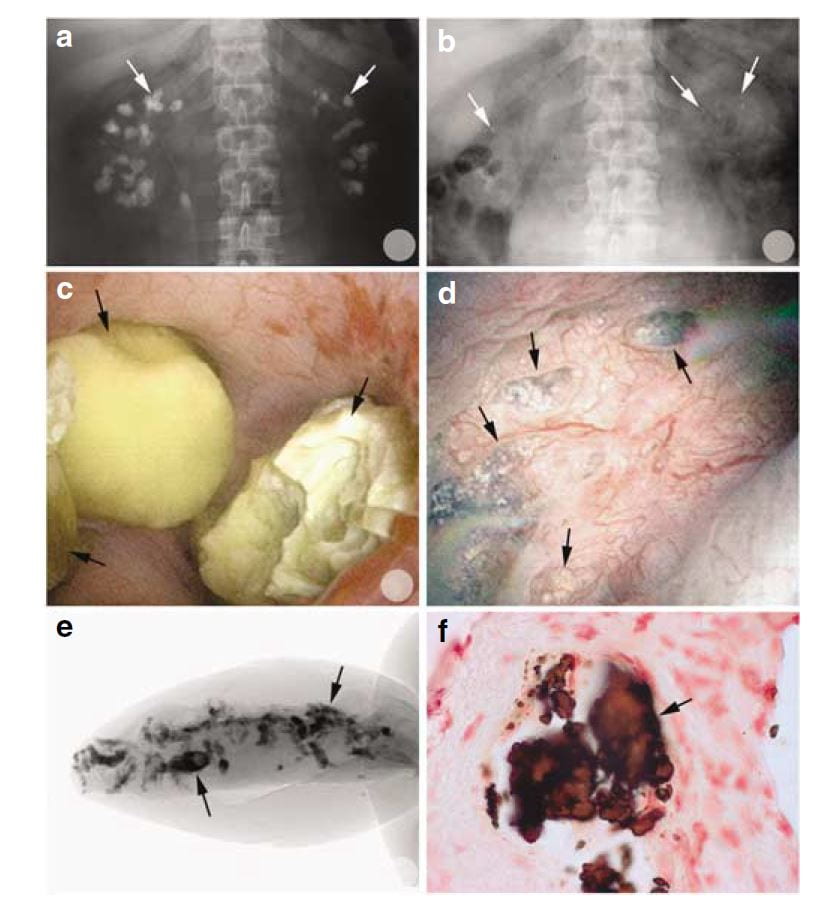 Of interest, most of the calcifications seen on radiographs were, at surgery, removable stones as opposed to crystals embedded in the renal tissues.
Of interest, most of the calcifications seen on radiographs were, at surgery, removable stones as opposed to crystals embedded in the renal tissues.
You can tell this from the x rays in the upper two panels. Before percutaneous nephrolithotomy nephrocalcinosis was dramatic; afterwards, few calcifications were present.
In the middle left panel you can see stones in the calyces during surgery, and in the right middle panel you can see the papilla after the stones were taken out. It has some calcifications in the tissue which are plugs in tubules. These plugs are shown by a micro – CT of a tiny biopsy from the papilla (lower left) and in a histological section (lower right)
Stone cultures were positive, perhaps because these patients had many prior procedures for multiple stones.
Deposits of calcium phosphate crystals affected virtually all of the Bellini ducts and though each deposit was small plugging on average replaced much of the papillary tissue. Despite this, kidney function as measured clinically was not remarkably abnormal, and the cortex of the kidneys not remarkably damaged.
In 1980 I presented our only 6 patients with stones and distal RTA out of over 1,000 stone formers to date, of whom 4 were from one family. They all had low bicarbonate and high chloride in their serum, as expected, an alkaline urine pH, and were unable to lower the urine pH with an acid load. Only one was convincingly hypercalciuric.
The essence of dRTA in stone formation is this: By inheritance or because of Sjogren’s syndrome, SLE or other immune mediated diseases the ability of the collecting ducts to lower urine pH normally is diffusely impaired, not in the patchy way one might expect from tubule plugging with crystals but throughout the medulla and papillae. High tubule fluid pH and, when present, hypercalciuria raise supersaturation with respect to calcium phosphate and diffuse plugging occurs with considerable damage and loss of tissue.
Perhaps because of its diffuse nature, dRTA does appear to lead to overall reduction of renal function if enough cases can be found and comparisons made to other forms of stone disease. In this study we had 1,856 patients with stone analyses and renal function, as well 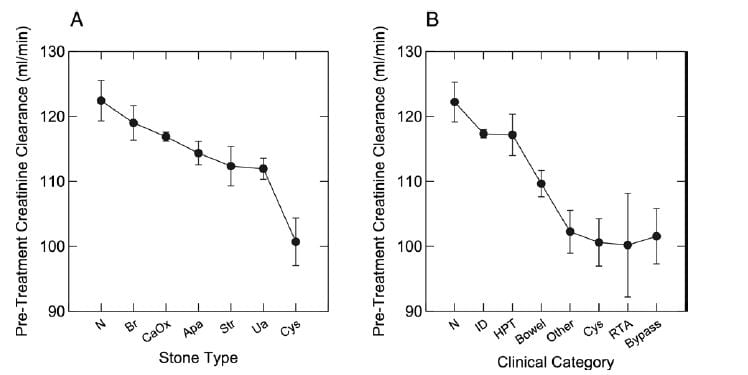 as diagnoses, all from our Kidney Stone Prevention Program at University of Chicago – the program that brings you this website.
as diagnoses, all from our Kidney Stone Prevention Program at University of Chicago – the program that brings you this website.
Measured creatinine clearances are shown as means with standard errors for all stone types on the left, and by diagnostic category on the right. Note that RTA, cystinuria, obesity bypass patients, and a miscellany of other rare disorders (like sarcoidosis and CYP 24A1 defects) shared a distinct reduction of renal function, whereas the common calcium stone types without systemic diseases, and even primary hyperparathyroidism (HPT), had no reduction compared to normal (N). ID refers to idiopathic hypercalciuria, people who have high urine calcium losses without obvious disease.
What does all this mean?
Distal RTA is very uncommon, colorful, easily diagnosed by blood abnormalities, family history of like diseases, and the presence of immune diseases. The label RTA may be misapplied to patients with many calcium phosphate stones because they produce an alkaline urine pH; that is not true RTA, but how phosphate stone formers are.
More Rare Genetic Mutations
These conditions are almost always evident in childhood, very rare, and not what a clinician in the practice of stone prevention expects to encounter. However every once in a while they do show up. The best reading source for all of the genetic hypercalciurias is OMIM, the wonderful online library that is free to everyone. In reading the tiny blurbs below keep in mind that almost no stone formers have these rare diseases, that those who have them present typically as ill children, even infants.
Bartter Syndromes 1-3
These are gene defects of transporters in the thick ascending limbs of the loops of Henle (In case you forgot or never knew the nephron segments this article has a nice picture). There is hypercalciuria but also a picture that resembles lasix use because lasix acts on this segment. Urine losses are high for sodium, potassium, and chloride, and people with these diseases are prone to low blood pressure if they do not get enough sodium replacement. The blood bicarbonate is high, potassium is low.
Bartter Syndrome 5.
There is excessive signalling of the cell surface calcium receptor (CaSR) which produces a lasix like picture but because of the specific problem serum calcium is low and so is serum magnesium. The parathyroid glands are regulated by serum calcium via via the CaSR which is the reason for the low serum calcium level.
Autosomal dominant hypercalciuric hypocalcemia
The CaSR is altered genetically but the specific alteration causes a more marked change in serum calcium than in thick ascending limb function, so the serum potassium and bicarbonate can be normal. These two diseases BS 5 and ADHH are essentially on a spectrum and resemble each other.
Dent Disease
A genetic mutation in a chloride transporter leads to hypercalciuria and, in males especially, progressive kidney disease. The serum values are normal apart from reduced kidney function.
Medullary Sponge Kidney
Given the nephrocalcinosis and many stones, one might think MSK is a cause of extreme hypercalciuria, but that is not the case. Among our 12 cases that were proven to be MSK during surgery and with papillary biopsy, the average urine calcium was 250 mg/day, just above the Curhan threshold for significant risk. SS values for calcium oxalate averaged 7 and for CaP 1.3, values scarcely above those encountered within normal populations or among common uncomplicated calcium stone formers.
We noticed the same in our much earlier paper on MSK diagnosed in the era of intravenous pyelography. We have already mentioned that among our two MSK series serum levels showed none of the abnormalities of renal tubular acidosis (low bicarbonate and potassium) and urine pH was not high (6.1 in our recent series). Ductal and clinical stones were on average calcium oxalate, not calcium phosphate. We believe the stones form in the stagnant recesses of the collecting duct cysts, abetted by a very modest bias of urine calcium excretion above the normal median value. This is what one expects when supersaturated urine is trapped in place, and supersaturation inevitably expresses itself in gradual crystallization.
Idiopathic Hypercalciuria (IH)
What is It?
In those two words you can find the major preoccupation of my life as a clinical investigator. To the mechanisms responsible for this common abnormality I have devoted my energies since I first began, in 1969.
The reference in the link above is to a review by my colleague Dr. Elaine Worcester whose brilliant research has clarified how the kidney goes about raising the urine calcium in this condition.
IH is not a disease.
It is a stone risk.
And that risk can be ascertained in any given person from the Curhan data in the first figure in this article.
People with high urine calcium excretions who do not have any of the diseases I have mentioned, or any of the others I have not – for pity and reasonable length of this article – mentioned thus far, have hypercalciuria that is ‘idiopathic’, of or from themselves or itself if you wish. They are the top of the mark among normals.
No red or green line separates IH from normal. Just as high blood pressure is a risk factor for stroke and heart disease, hypercalciuria is risk factor for disease – stones and bone disease, which is why I have devoted to its study so much of my life.
Being one end of the human distribution, IH may be found in your next door neighbor, or even your spouse and you would not know unless they are tested. And they will not be tested unless they get stones, or bone disease, or their family members get these diseases. If testing is done nothing will be found but high urine calcium, enigmatic, distinctive yet bland, but bespeaking a complex physiology.
Where Does the Extra Calcium Come From?
In the named diseases, hypercalciuria comes from bone and food calcium, and the same is true for IH. It has to be so, there are no other sources. But IH is not a disease, so we are seeing in IH a magnification of the usual losses of bone and diet calcium in urine, meaning that one or both of these must be increased. Certainly, as I will show in other articles, diet calcium is absorbed more efficiently in IH than in normal people. But bone mineral can be lost in excess, and bone disease can result.
It is for this reason, Dr. David Bushinsky, a distinguished bone and mineral investigator and internationally recognized authority in calcium metabolism, has proposed that every stone clinic is a bone clinic. Stone formers have the potential to develop bone disease if not properly cared for. Though their stones are an immediate reason for attention and a prime focus of care, bone health is also an inescapable concern.
How Can The Urine Calcium Be Lowered?
Toward the lowering of urine calcium and consequent prevention of stones – and preservation of bone mineral – we have some useful trials using thiazide diuretic type drugs. Likewise, some trial evidence favors reduction of diet sodium intake, to which I have alluded without presenting evidence.
Why Are We Ending Here?
It could seem ungracious to end here, without more details about IH or the many named hypercalciuric diseases, but this article is already very long, and what remains is a massive amount of information. I plan for many articles on hypercalciuria, the named diseases that cause it, and especially on IH itself because of its central role in stone disease and because it is a personal interest of mine and of those I work with.
Here I mean merely introductions, as at a cocktail party.
It seems probable to me that in doing right by this topic the articles on this site could double in number, although that may be an overestimate.
Check by from time to time, and you will find more.
Regards, Fred Coe


I enjoy reading your articles rekidney stone formation. Very informative. Thank you!
Dear Marguerite, thank you very much for your comment; it is encouraging that people find this site useful and enjoy it. Best, Fred Coe
I agree with you Fredric, a massive amount of info but hopefully our MSK members will find the time to read! You list many different causes of hypercalciuria, some of each may be present in our MSK support group members, in particular RTA and autoimmune diseases, also diagnosed with MSK!
In your paragraph on MSK you say, in your study with 12 patients (we have thousands of MSK members!) “none showed abnormalities of RTA, low potassium or high pH”, although we do have many members with all these lab results, some with very severe hypokalemia! We have both members who make calcium phosphate/brushite stones (which need to be surgically removed) and members who make, not frequent, BUT rapid daily, weekly, monthly calcium oxalate stones. All diagnosed with MSK.
I have a feeling we are dealing with much much more than MSK as though “just” MSK was an underdiagnosis? Maybe we should be renaming this new disease? With MSK Plus or Hyper MSK? Each patient different, with different symptoms, thus different causes.
In your paragraph on IH Idiopathic Hypercalciuria, you say “it is not a disease but a stone risk”. How do we know if some of our MSK members suffer from IH? And if they do, have been diagnosed with MSK and nephrocalcinosis, have been making stones for years, have continuous uti’s/kidney infections, IC, hematuria, have been reduced to a very low quality of life due to chronic pain, fatigue, depression, anxiety, reason for which they were forced to give up their jobs, in these cases (so many of them!) I would call it a disease! A very serious one which their doctors are not taking seriously enough! As always, thank you for listening Fredric!
Dear Celia, You are a very thoughtful and valuable voice, so thank you for your helpful comments. Of course we have reported few cases of MSK, but these are surgically proven, so we are sure that MSK is present. In that tiny sample we found what we found. Our group has spent the past 15 years – and considerable of your taxpayer dollars via NIH – gradually defining the various types of stone formers using a combination of intra-operative imaging, histology of tiny biopsies, and physiological studies. Brushite stone formers, for example, can have nephrocalcinosis and look like MSK on CT scans; so can RTA. But at surgery they do not have MSK. Accelerated stone formers, with vast numbers of stones, are uncommon but we have reported on them. What I plan to do is gradually write up all of these kinds of stone formers, for everyone who reads this site, with references, as always, and hope that things sort out. That there are so many patients in your group is important because as the site gets more details – it takes a lot of time to write these things up!! – perhaps patients and their doctors will be able to sort themselves out, even contribute to our work, if possible. As for IH, it causes diseases, lot of them, in kidney and bone, but it is itself just one end of the distribution of values found among people. Those with the highest urine calcium losses are prone to develop stones, often severe, nephrocalcinosis, and all of the miseries you have amply documented. But you would be surprised how many normal people have IH and never know it. Strictly speaking, 5% of all people have urine calcium excretions far above 300 mg daily, but only a small fraction get stones. How many get bone disease, and how much IH is part of postmenopausal osteoporosis are presently controversial issues and of research interest. Thank you so much for your thoughtful writing and your contributions to this site. I appreciate both very much. Regards, Fred Coe
Dear Dr. Coe,
Thank you for your latest educational and entertaining article on hypercalciuria. I thoroughly enjoyed reading it, and your witty and fun writing style. My I just add that Celia is my sister, and her intelligence and thoughtful inquisitiveness has been a godsend to me and all of us in our MSK group.
My question is twofold. Does citrate diminish stone crystalization in all types of stone formers’? So even me with calcium phosphate?
Next, I do not have high urine calcium. But I am hypokalemic, and have high urine pH. I have nephrocalcinosis, and RTA. How is this even possible if I dont even have high urine calcium? I used to but do not any longer. Thank you for this site, these articles and mostly your kind answers.
Dear Laura, Well, I guess between you and Celia we have a powerful family force! Citrate has never been tried formally in calcium phosphate stone formers, a matter I have repeatedly brought to the attention of my research colleagues: It is time! But the NIH is not usually willing to spend precious and limited research money on trials, which can be very costly. Industry will not because potassium citrate, though pricey, is a kind of commodity. As for your urine calcium, I gather it is below 200 mg/day, the lower level of risk in the Curhan data I just put up in my last article. Be sure this is true. If it is above 200 mg, an easy way to lower it is reduced sodium – check out your 24 hour urine sodium. Now, the low serum potassium. I gather you are not taking any form of diuretic for stone prevention; all of them reduce potassium levels. If you are not, and your blood level is low, is there enough potassium in your urine – at least 40 mEq/day? If so, you really are wasting potassium. If not, there may be other reasons. All patients with calcium phosphate stones have alkaline urine pH – that is how to make such stones. But RTA is when the blood bicarbonate is below normal and the urine is alkaline – both at the same time. Is your blood bicarbonate low? Ask yourself – and your test results – the answers, and if you like put up another comment with the numbers, so we can try to be helpful. Warm regards to you and Celia, Fred Coe
Thank you for the insightful article Dr Coe.
Thank you very much for your thoughtful and helpful insights. I believe in my last 24’s my urine levels were low, and am working to get them up daily. I do have potassium citrate at home but will ask doctor if he also thinks perhaps potassium chloride would be better. I understand what you are saying when you say that without clinical knowledge this may be of limited value but it is of great value to me. You are right my doctor did put me on amiloride to help potassium wasting. I do form calcium phosphate and my doctor thinks I am very lithogenic he called it. I do have a very good nephrologist and also urologist. I just appreciate this so much as a confirmation of minds. Thank you again for taking your time and answering in such good detail.
Best Regards,
Laura
I found this article to be extremely informative. Sadly since being ill my cognitive abilities have suffered so I will need to read it again. I struggle with to high calcium output in my urine and sometimes high in my serum. My PTH is all over the place. The PTH issues and high Urine calcium out put have been on going for a couple years but only recently I have had a couple tests showing higher serum calcium. My nephrologist said he suspects idiopathic but after reading this I’m a little confused. Once again thank you very much for your very informative article and I will be certain to read it again. I have also given my GP the information to join as she was very interested as was the student doctor with her last appt.
Dear Tasha, If your serum calcium is elevated above the normal values for the laboratory, and your serum PTH values are not suppressed below normal, and – very importantly, your urine calcium is clearly elevated, and you are NOT on drugs that can raise the serum calcium such as thiazide type diuretic drugs or lithium, then you may well have primary hyperparathyroidism. But if these specific features are not all met, I would not be satisfied with that diagnosis. I imaging your physicians already know all this and are acting in accord with what they know. Whatever the underlying diagnosis, if you are forming new stones, stones not present on prior CT scans, then your urine has too high a supersaturation for you and the supersaturations with respect to the crystals in your stones need to be lower. Regards, Fred Coe
Thank you:) I don’t take any diuretics. They gave me gout. Do other than ranitidine for the terrible heart burn I take pain medication and recently started Synthroid. I’m not a big stone maker. I pass lots of sand and have nephrocalcinosis. I pass larger stones only once or twice a year yet my kidneys are on agony always. I don’t understand. It and wish I could feel better. I appreciate you taking your time to help to educate us. Thank you
Dear Tasha, The sand means your urine is supersaturated with respect to the crystals in the sand. Have you had the sand analysed? You should. If diuretics give you gout perhaps the sand is not calcium but uric acid. The latter has an orange color sometimes. Passage of sand can cause kidney pain and back pain, and needs to be stopped. The borderline serum calcium and PTH levels need to be clarified. I would begin by analysing the sand, and I would raise my urine volume a lot until the sand is never present. A target is my favorite of over 3 liters of urine until you have abolished all sand and crystal passage. None of this needs to occur. Crystals are predictable. Has your 24 hour urine chemistry been determined? Best, Fred Coe
Dear Dr. Coe,
I myself cannot make heads nor tails out of these results. I can read them of course but to write them all out I no longer have the length of concentration that would take. You asked me about a few of my levels so I sent my labs all to Celia and she has written them all down. Some (the first set) are from 2013 and earlier. The second batch from 2014, 2015. I know that my sodium has gone way down but I am missing some values that you asked for.
Values Chart of 2013:
13/10/27 24 HR URINE
Calcium 3.6 mmol/d – ref. <3
Sodium 108 mmol/d – ref. < 100
13/10/28 Serum
K 3.3 mmol/L – ref 3.5-5.1
CI 102 mmol/L – ref 96-107
HCO3 31 mmol/L – ref 21-32
CA ++ 2.28 mmol/L – ref 2.2-2.5
Na 139 mmol/L – ref 136-145
14/09/15
pH Urine 7.5
14/12/07
Volume 24 hr 1.38 L
Citrate Urine 3.3 mmol/d – ref 0.8-6.0
CO2 31 mmol/L – ref 21-32
CA Urine 2.34 mmol/d – ref 2.12-2.52
Oxalates 287 mmol/d – ref <320
K 3.4 mmol/d – ref 3.5-5.1
15/02/05
CA Ionized 1.14 mmol/L – ref 1.15-1.32
K 3.5 mmol/L – ref 3.5-5.1
CA 238 mmol/L – ref 2.12-2.52
CI 100 mmol/L – ref 98-107
CO2 30 mmol/L – ref 21-32
AnionGap 8 mmol/L – ref 5-12
Na 137 mmol/L – ref 136-145
SO what you have above is all nice and organized by Celia. I hope you will be able to tell me something about this.
Very Best Wishes
Laura Bousada
Dear Laura, Thank you for sharing your information so others can perhaps benefit from thinking about the implications of the results. Let me make clear that my analysis is strictly technical, in that your physicians are responsible for your care and anything I say is from the numbers plus a few facts I know in addition: you are taking amiloride and indapamide and might be taking potassium citrate, and your stones are calcium phosphate – I do not know if the form is apatite or brushite. On 10/27/13 your urine calcium was mildly increased despite your diuretics and well controlled sodium of 108 mmol/day; your blood showed reduced potassium and increased CO2 content because of indapamide and despite amiloride. Calcium was normal. These are common results in treated idiopathic hypercalciuria; the potassium depletion is a problem because it will lower urine citrate. On 9/14/15 the urine pH is very high at 7.4. On 12/7/14, the volume very low at 1.38 liter/day, the blood remains essentially the same, and surprisingly urine citrate molarity and excretion exceeds calcium meaning I suspect you were taking potassium citrate. Urine oxalate is unremarkable. On 2/5/15 the blood is essentially unchanged – calcium is missing a decimal = 2.38 – and the slight reduction of [Ca] is from the metabolic alkalosis – high blood pH – from potassium depletion and diuretics. The urine is not provided. You seem to have a common condition which is being treated in the way I would favor but you are making stones actively, as I understand it. There are no supersaturations, perhaps because your health system does not provide them, but the one pH and the low urine volume make me quite sure your urine is supersaturated with respect to calcium phosphate as brushite. I would think that you would be better served with potassium chloride which might allow the urine pH to fall a bit, and by vastly more water – 3.5 to 4 liters – so that stones can stop. I see no alternatives provided you are indeed still forming stones. The serum potassium should be brought up – it is too low. I am sure your physicians have said all this already and will find my remarks of little value, but if they encourage you to raise your urine volume greatly I suspect stone activity will fall. Fred Coe
I appreciate your input very much. I am going to start taking potassium chloride, after speaking with my doctor. No I have never taken potassium citrate only at the very very beginning but stopped as it caused a lot of discomfort. I do make both brushite and apatite stones they are both (phosphate) listed in my stone analysis of 2013 I believe. I will try to have them looked at again. Thank you again you are an amazingly generous person and really a wonderful person.
best wishes,
Laura
Hi Laura, Given brushite and apatite stones, and proper use of drugs, there will be only one reason for more new stones: Inadequate urine volume. Ask your physician, if possible, to measure supersaturations and use the amounts of fluids needed to reduce the SS for calcium phosphate below 1. If SS cannot be measured, go for a maximum urine flow of about 4 liters daily – steady as possible – which will almost always be sufficient. There is no reason for new stones. You do not have RTA, that is certain. I doubt you have MSK: It is probable you have exactly what we have described for brushite and apatite stone formers. It can look like MSK but is not. Warm regards, Fred Coe
Dr Coe
I was wondering if you were going to talk about RTA in infants
And children. I found out infants a year old and under were being diagnosed
Also the parents did not have kidney disease in their families. I thought RTA
Was inherited or the result of the conditions you mentioned. I was not aware it was idiopathic. AlSo these parents are being told there children may grow out of it. Is that even possible? They are going to give them Polycitra in an effort to reduce or stop stone formation. I know pediatric nephrology is another subspecialty I don’t understand this . Also these parents want to have more children I would be terrified I would have another child with RTA. Is there. Genetic testing that can help. Them? Is it costly
Trish
Tpl Th’ve Are. Thin Ist
Hi Trish, I will be writing about RTA somewhat later on. It is hereditary, in multiple forms, and therefore can begin in childhood. There are forms that can wane with age. RTA affects growth and therefore treatment in children is very important. IN general genetic testing is not widespread but many of the genes are known and can be sampled in individuals on a research basis. Diagnosis of RTA is generally obvious, and the condition is very uncommon. Regards, Fred Coe
Very informative article…I am an ongoing stone maker and have been doing blood work for the last 5yrs at U of M. Dr’s are baffled because I continually have high PTH which they thought in the beginning was cause from my Vitamin D being so low(9) they put me on prescription vitamin D got my level up and my PTH went up so they no longer will put me on the high dosage of vitamin D. In Dec 15, my urine calcium tested at 501 so they suspected Primary Hyperparathyroidism and sent me for an Ultrasound, Sestamibi Scan and 4D Cat scan all of which were negative. U of M surgeon said thats not uncommon to see negative scans so he ordered 3 consecutive days of blood work testing my ionized calcium, PTH and regular calcium..everything came back normal except my PTH was in the 90’s. My question is does could I possibly have a renal calcium leak and would this cause my PTH to be elevated? Also, could I my body be excreted calcium out through my urine in order to keep my blood levels normal? Thank You for your help.
Hi Margaret, So you have a high PTH normal blood calcium levels, and very high urine calcium levels. I also believe your may be an active stone former from what you have said. All idiopathic hypercalciuria has an element of reduced renal calcium reabsorption, so the old idea of a ‘renal leak’ which may have originated with me long ago, no longer matters. What does matter is your treatment. I would think very low sodium diet proved by very low urine sodium would come first – try for 65 meq or 1500 mg. That may bring your urine calcium down. Be sure and maintain a high diet calcium – 1000 mg is ideal. If thiazide is needed one uses it with low sodium. The goal is to lower supersaturation, which will reduce stones. The High PTH is interesting but not my main concern given the normal blood calcium levels – if you have primary hyperparathyroidism under it all that will become obvious with time. Regards, Fred Coe
I have recently been diagnosed with IH non stone former. I have osteopenia according to DEXA scan. Have had hip replacement surgery and cervical neck fusion both orthopedic surgeons said I have soft bones. Had PE after hip replacement surgery currently on warfarin. Dr recommendsaid 25mg of hydroclorothiazide.Apprehensive?
Hi Amy, Very low diet sodium and 1200 mg diet calcium would help as would protein intake no higher than 1 gm/kg/day = 24 hour urine PCR gives this figure – and avoidance of sugar loads are a good base. The diuretic – I prefer chlorthalidone 12.5 mg – is on top of that so the dose can be low and potassium wasting minimal. You should consult a bone expert – bone directed drugs may he helpful – outside the scope of this site right now. Regards, Fred Coe
I studied your great article. it was very interesting to me while I’m not in medical field.
My 3 years and 8 months old girl has recurrent kidney stone ( 3 times up to now after dissolving stones by poly citrate). we tested her TSH, T4,IGFI, 25OH D3 in blood and urine calcium/creatinine ,uric acid/ creatinine . T4(9.63 microg/dL),TSH(0.86 mIU/L) results was normal but she’s got deficient 25OH vitamin D3 ( 21.62 ng/ml in one lab and 17.6 in another lab) and both Calcium/cr(0.31) and uric acid/cr(2.15) are high in urine random test. Our doctor prescribed hydrochlorothiazide and polycitrate latter to dissolve two 1.4 mm stones in her kidney.
Also Endocrinologist doctor prescribed around 900 IU/day Vitamin D3 supplement(3 types of syrops) .
I asked from her nephrologist doctor whether vitamin D3 defficiency can lead to higher calcium in her urine or not and he replied there is no relation between the two.
please help us to find our daughter recurrent stone root cause .
Best Regard
Hi Mousa, It sounds like your daughter has hypercalciuria and the drug is not inappropriate. Did they check the urine oxalate? What were her stones made of? Was she screened for cystinuria? It is important to be sure about everything. If the stones are calcium oxalate they will not dissolve, and probably that is also true for calcium phosphate. As for vitamin D levels, low ones to not play a role in stone production. Regards, Fred Coe
With recurrent bladder stones 60% CAOX-COM and 40% CAOX-COD, what are the likely causes and prevention?
Hi David, Prostate obstruction with residual urine is a common part of bladder stones, and often there are urine abnormalities as well. So the solution is both improvement in bladder emptying – your urologist, and evaluation as in any stone former. regards, Fred Coe
Hi Dr. Coe,
My son (8 years old) was diagnosed with hypercalciuria. I have been reading and following your site since his diagnoses trying to inform myself to best help my son. It has been very helpful and informative for me. His most recent labs show no vitamin D deficiency, normal PTH levels, but low blood calcium levels. Prior to his diagnoses he has reached a halt in growth and we have seen a rise in some unusual behaviors/moods. I am worried the “stunt” in growth we have seen is because his body is not absorbing much calcium at all, especially since limiting due to his diagnoses. I was curious about supplementing with calcium orotate. He is a very active boy and we just want to know the best ways to help him get the nutrients his body needs but not put him at risk for harm now or in the future due to this condition.
Hi Casey, Childhood hypercalciuria is common as idiopathic hypercalciuria is genetic. But such children have normal growth and normal blood calcium levels. Absorption of food calcium is above normal in such children, not low. Given normal PTH and low blood calcium levels with high urine calcium excretion perhaps he has a genetic abnormality of the calcium sensing receptor. Bring this idea to his physician – I realize I have no real data and am far away so this could be a silly notion. Even so, ask. Regards, Fred Coe
So, since this initial posting we have also received a diagnosis of developing hypothyroidism. We have seen our nephrologist and and an endocrinologist and both have mentioned high sodium levels. We already eat a healthy, mainly balanced diet not high in sodium. Could all these be related or influencing each other in some way?
Hi Casey, I presume your physicians mean high urine sodium levels – I have not seen these data. Likewise do they mean hypothyroidism or hypoparathyroidism? Frankly the low serum calcium and normal pth and high urine calcium make me think of genetic disorders of the calcium receptor. I do not have enough information to offer you or his physicians any real suggestions. If they like and want to send more details I would be happy to take a look. Regards, Fred Coe
Hi Fred
Am i glad i found this article!!! thank you!!! I am 33 and have had ureter dilation starting at 8 years old, and blood in my urine since i was born. Over the years they would test my urine and just give me antibiotics because of the blood, but many times i indeed did not have a infection. Anyhow i have had my ureter rebuilt a few years ago, and now am forming multiple stones in 3 months time, with a low salt intake still… my stones are 70% calcium phosphate (brushite) 20% Calcuim Oxalate monohydrate and 10% constituent Calculus calcium phosphate apatite… with many embedded stones. Im feeling very sick at this point , i can give you more info soon, but would love to here from you!!! Thanks Angela
Hi Angela, Brushite stones are a major problem indeed. Prevention of more is much the same as for all calcium stone diseases. Surgical management of stones is made difficult by confusions between stones and tissue calcifications that are not stones but show up on CT scans. I would begin by reviewing the article to be sure you are using all available methods. If not, I advise it to reduce new stones. Low sodium is a good thing, but there is more you can do. If you want to send more information, I am pleased to try to help. Regards, Fred Coe
Hi Dr Coe,
I am a chronic Lyme Disease sufferer. I treated with doxycycline, Zithromax and a combination of herbals and homeopathy for over 6 months. That was 2 years ago.
Since then I have been a total mess. I started with a UTI, but antibiotics didn’t help me – turns out I had a stone too. For the whole 2 years I have passed tons of little specks, gravel, sand and maybe the biggest was 2 or 3mm. I brought one in and it was calcium oxalate. Nothing shows on CT scan. I had a 24 hr urine study which showed high calcium and uric acid. My doctor said I have IH. She wanted me on hydrochlorothiazide but I’m fearful to try because I have low blood pressure. I then saw a nephrologist who suggested repeating the test through Litholink. I’ve not done it yet.
What do you suggest I do as I am always either in pain, burning or frequenting the bathroom. I really can’t stand much more
Thanks,
Lynn
Hi Lynn, I would suggest you follow a plan for your evaluation – not just the urine test. Here is a reasonable one. Gather all of the stones for a while and get them analysed to be sure you know what you are producing. I would obtain 2 24 hour tests with blood samples for each to be sure about systemic causes of stones. Perhaps the nephrologist would be your best choice. OFten meds are not needed. If you indeed have calcium oxalate stones without systemic disease – idiopathic calcium oxalate nephrolithiasis, then here is a good treatment approach. FLuids and diet are primary, drugs an addon if needed. Regards, Fred Coe
Wow thank you!
What are you referring to when you say “systemic causes”. I want to bring all up to my doc. Thank you!
Hi Lynn, The list is in this article. Here is one about how to organize everything for your physician visit. Regards, Fred
Your website has given me my first real understanding of hypercalciuria. I was diagnosed with osteoporosis last fall and was given my first 24-hr urine test ever: Calcium 365 mg, 7 mg/kg body weight, Volume 1800ml, Creatinine level normal. No other urine measures taken. No personal or family history of kidney stones. Blood tests indicated Calcium 9.7 mg/dl, Intact PTH 47 pg/ml. Subsequently I was infused with Reclast (zoledronic acid) to address the calcium loss. I have now had two further urine test: 315mg and 345mg on volumes marginally above 2000ml. I am suppose to be starting hydroclorathiazide 12.5mg. Does my situation warrant further testing, such as a kidney stone risk panel?
Hi Paula, I suspect you have idiopathic hypercalciuria, a hereditary trait that does cause stones and bone disease. Obviously the bisphonates did nothing for your calcium losses. Hydrochlorothiazide is a mediocre drug for hypercalciuria because short acting- I prefer chlorthalidone 12.5 mg/day but potassium wasting can be a problem and require potassium supplements or a sodium channel blocker like amiloride. But a better approach is low sodium high calcium diet; you may be able to eat quite a proper calcium intake of 1000 mg or so and with low sodium diet 65 mEq or 1500 mg/day lower urine calcium and do something for your bones – at least in principle. Against a really low sodium diet chlorthalidone will work best and with minimal potassium loss. Regards, Fred Coe
dear sir,
my daughter now 5yrs old.she had hematuria with no pain on 27/05/16.nearly 5 episode she had.then v approached a nephro doc and he asked to take low salt and more fluids.but again after six months she had hematuria with no pain for 3 episodes.now from 10/06/17 to 13/16/17 she had the same..v took her for urine test and blood test.shall i share them ?? ill u help me to clarify actually wt is happening with my girl.i feel my life is dark because of her health status.plz reply me
Hi Sharmila, I presume your daughter has idiopathic hypercalciuria that is causing crystal formation and bleeding. Low sodium and high fluids work but only if you assure the sodium is really low using 24 hour urine collections – it is impossible to estimate diet sodium otherwise. The treatment is sound. But perhaps she does not adhere closely to it. This disorder can produce stones in later life so low sodium is important. Diet calcium should always be high in children, it is the low sodium that will control calcium losses into the urine. Regards, Fred Coe
Dear Dr Coe,
Thank for this very informative website. I am 63 year old female with mild PHPT and mild PKD. I have hypercalciuria but was recently taken off thiazide as it drove up my serum levels. My urine levels have now risen to 680mg/day. Although my recent kidney US showed no stones, I am worried that at these high levels I will develop stones. I am following your fluid and diet recommendations. How long do I have before a stone precipitates?
My endocrinologist is uncertain as to whether my urine calcium levels is from the PKD or HPT and is not rushing the surgery until we get more info from scans. Meanwhile I am walking around with these high levels in my urine and am interested in preventative methods.
Thank you so much!
Hi Anne, I have forwarded your question to my colleague Dr Arlene Chapman – sans your name – who is an expert in PKD. For my part, do you have PHPT or just high serum PTH? I mean is your serum calcium high when you do not take thiazide or other drugs that would raise serum calcium?? Here is a lot about PHPT diagnosis. If it is just renal disease with high PTH that is secondary hyperparathyroidism. The high urine calcium may reflect PKD and that is what I asked Dr Chapman to comment on. Regards, Fred Coe
Thank you Dr Coe. After I went off thiazide in January, my serum calcium was measured at 10.6 in March, 59 PTH and 407 urine calcium. In May serum calcium was down to 9.7, but 68 PTH and 662 urine calcium. Thank you for referring my question to Dr Chapman. (p.s. I am in her ADPKD study). I now understand why my endocrinologist is being careful about surgery. I will review the link you sent me.
Thanks!!
Hi Anne, Dr Chapman did not know your name as I kept it confidential. She answered me: “Hi Fred she certainly is atypically hypercaluric from a PKD standpoint. If she had PKD and she is 63 she should have decreased her urine calcium excretion by now. Does she have a family history of ADPKD? Does she have a serum creatinine level? Happy to help.” Since you know her from the group perhaps you should speak with her directly. As for your hyperparathyroidism I am suspicious. Was the high serum calcium while you were on thiazide? Perhaps you might speak with your physicians about the value of multiple fasting serum calcium values off meds that might falsely elevate it. Your urine calcium is very high and there is a reason and therefore a proper treatment. Regards, Fred Coe
Hello, my 3 years old boy recently been diagnosed with nephrocalcinosis and hypercalciuria. Genetic tests revealed SLC34A3. Blood Ca is normal, PTH normal, P is normal both in blood and urine. Ca/creatine urinare is 0.4 (normal must be less than 0.2). Please tell me if anywhere in this world this disorder can be treated. Thank you so much!
Hi Alexandra, This is a phosphate transporter and defects lead to low serum phosphate, high levels of serum calcitriol. The normal blood phosphate is surprising and serum PTH should be decreased. So perhaps the gene alterations are not such as to reduce phosphate transport and are therefore incidental. If so he has idiopathic hypercalciuria which is multigenic and should be medically controllable. Given the above discrepancies perhaps his physicians might want to discuss with you what they believe is the main problem and treatment. Regards, Fred Coe
Thank you very much for your answer!
Is there any treatment to correct this disorder or it’s a problem that he will have all his life?
Thanks again,
Alexandra
Hi Alexandra, as I tried to say, his gene abnormality may not have functional meaning as his serum phosphate is not low nor his PTH. He may have an abnormal DNA pattern but normal functioning transporter function. Discuss this with his physicians. If he has mere idiopathic hypercalciuria it is managed in children with low sodium high calcium diet – the latter for bones – and low doses of thiazide type diuretic agents. This complex treatment needs management by fairly skilled peds renal or endocrine physicians. If it is mere idiopathic hypercalciuria, life long problems are easy to manage and the condition is very common. If he really has a transport disorder, that is very complex but manageable. Regards, Fred Coe
Thank you so much for your help!
Best regards,
Alexandra
Greetings. I have this male patient with FHH/ and renal calculi. The diagnosis is certain from biochemistry and it seems all siblings have the same…although geneteic analysis has not yet been done. Had been subjected to parathyroidectomy for supposed parathyroid hyperplasia in 2012 and has been almost continuously on Mimpara despite having normal range PTH. The urine does not show hypercalciuria, hyperoxaluria or hypocitraturia. In this case can he be considered as symptomatic FHH because of the renal calculi and be recommended Mimpara. He has no musculoskeletal symptoms/ no history of pancreatits
Hi Dr Rangel, Because FHH is heterozygous inactivation of the CaSR, one expects the high serum calcium with normal or perhaps elevated serum PTH and very low urine calcium excretion due to loss of function of the thick ascending limb CaSR. At surgery glands can be enlarged but usually because of the very low urine calcium level surgery is not performed. A CaSR agonist like Cinacalcet is not needed as the elevated serum calcium has no known effects. Because your patient had hyperplasia at surgery I presume some PT tissue was removed so the drug seems altogether unnecessary. My concern is about the primary diagnosis. The urine calcium needs to be very low for any confidence in the Dx. If it is even normal, I would suspect perhaps primary hyperparathyroidism, presumably familial given the siblings. THeir urine calcium values would be helpful. So about the drug, I would not use it. About the Dx, family 24 hour urine studies and if they are not low proceed to genes. MEN Type 1, 2a and 4 all may fit. HPT-JT seems most unlikely as you would have seen the jaw abnormalities. Uncommon but not unheard of, familial isolated PHPT. All these matter if urine calcium is not really very low. I hope this is of some use. I have had stone patients with FHH, and of course given the low urine calcium the cause is usually low volume and high oxalate. Best, Fred
Hi Dr. Coe. I am a 54 y/o woman. My doctor diagnosed me with Idiopathic hypercalciuria, and I have a 8 x 8 x 12 mm stone in my kidney. Blood serum results: Calcium 8.9, PTH Intact 39.2, uric acid 5.1. 24 hour Litholink urine collection results: volume 3.85, SS CaOx 2.03, Urine calcium 227, Urine Oxalate 21, Urine Citrate 945, SS CaP 0.31, 24 Hour Urine pH 5.911, SS Uric Acid 0.32, Urine Uric Acid 0.492. After reviewing your articles, I reduced salt and stopped eating sugar altogether. I would greatly appreciate it if you would let me know if I should go on a low calcium diet because of this. I am afraid to do this because it would not be good for my bones. Also, how much protein am I allowed to eat now? Should I be drinking lemon juice too? Thank you.
Hi Lois, No! You need the same high calcium diet as all US people do, 1,000 to 1,200 mg daily. The urine sodium will control how much gets into the urine. Try for 1500 mg of sodium. Be sure to get a followup urine and prove to yourself the sodium is indeed low and urine calcium reasonable. Also, bone mineral density is in order. Here is a good treatment protocol. Regards, Fred Coe
Thank you Dr. Coe– you are a lifesaver! I have one more question. It is my understanding that 30% of people never have pain with a stone, 30% have excruciating pain, and the last 30% have elective surgery removing the stone. Please let me know whether you think I should have elective removal of the stone or whether I should just hope I’m in the 30% that never has a problem and just keep monitoring the stone. I now do not have any pain or problems urinating. Thank you.
Hi Lois, the decision to intervene or not gets us into the details of your surgical care, and I lack enough information to say much. In general stones are removed that cause obstruction and fail to pass promptly. Likewise if they are large, or failing to progress. But in real life the rules are applied to someone with a lot of details, like you have, and that requires the surgeon who takes care of you. Just be sure to keep in touch with your surgeon who is in a position to protect against obstruction that could injure a kidney. Regards, Fred Coe
Thank you Dr. Coe. Your help is very much appreciated.
Hi Dr. Coe,
I have had multiple kidney stones on my left side only, for the past 8 years. All have come back as Calcium Oxalate. I am 46 years old and have a family history of stones. For the past 6 months I have kept to a whole foods ketogenic diet to help control migraines (with good success). Have been told by previous doctor to increase fluids and avoid high oxalate foods, however the stones kept forming.
My new urologist ordered a 24 hr. urine test and bloodwork and I’ve been sent a copy of the results to review before my follow-up appointment next week. Two values came back out of range and I’m curious if there is a link between them.
On the urine test the Calcium was 624 mg (pH 6.4, volume 4L, citrate 1276mg, sodium 156, mag 228, Ox 21.1, Uric acid 436, phos 880, Creatinine 1080).
On the blood work my-out-of-range value was Eosinophils at 2.8 x10E3/uL (mag 2.1, PTH 30, Phos 3.3, WBC 7.6, RBC 4.36, Neutrophils 2.3, Lymphs 2.1, Baso 0.0, Granulocytes 0.0, Uric Acid 4.7, Creatinine 0.55, sodium 140, potassium 4.2
chloride 96, calcium 9.2).
I have read elevated eosinophils could be related to Sarcoidosis, however I have no physical concerns/complaints beside trying to figure out my recurrent stone issues. I also understand that Sarcoidosis is relatively rare.
Thanks for any insights and for your wonderful, educational work. Best regards!
-Shannon
Hi Shannon, your urine calcium is stupendously high. Given your normal serum calcium and PTH I presume you have severe idiopathic hypercalciuria. Sarcoidosis reduced PTH to low values – not you. Treatment is via diet and if needed medication. This article on idiopathic calcium oxalate stone formers seems to fit your situation. Regards, Fred Coe
Thank you so much Dr. Coe. Looking at my diet, which I track for Keto maintenance, I can see my sodium and protein intake is very high compared with the recommended amounts. The information here is very helpful to making helpful adjustments!
Hello,
I have been treated for Vitamin D deficiency for 6 months and only now have tested my 24hour urinary calcium, serum calcium and PTH. Urinary calcium came back at 15.21mmol/d (High), along with high PTH (8.1mmol/L), but normal calcium (2.28mmol/L) [it might possibly be even a bit lowish]. My serum creatinine was in the normal high range and urinary creatinine was high.
Could it be consistent with still-being-treated Vitamin D deficiency to still have high PTH, high 24hr urinary calcium and lowish normal serum calcium. Those 3 simultaneously seem paradoxical.
Hi Joe, The urine calcium is majestic. But a high urine creatinine for your body weight means overcollection may have inflated the value. One possibility – assuming all other tests are normal – is idiopathic hypercalciuria with vitamin D deficiency showing up as vitamin D is repleted. YOu do not mention your vitamin D level. I would get it measured as well as your 1,25 d level which I imagine will be high. The other possibility is that you have primary hyperparathyroidism with incompletely treated vitamin D deficiency and as the latter is fully corrected serum calcium will rise above normal. Regards, Fred Coe
My daughter is special needs at age 50, and is post menopausal. In 2015, I took her to the ER, and found she had three kidney stones. She has never had kidney problems or stones prior to that time. They dissolved with 0.4mg of Tamsulosin. No other stones have been identified. Since 2015, she has had three 24 hour urine tests, which shows high urine calcium counts above 300, and drop in Urine PH at 5.369. Latest test was done in Sept. 2017. She is hypercalcuric, and has been showing she is hypercalcuric since the first test in 2016. In Oct. 2013, she had a count of 9 on a D3 test. The doctor prescribed 4,000IUs of Vitamin D3 supplements. She was re-checked in January 2014 and her D3 level had risen to 29. She was told to continue on the 4,000 IUs a day of Vitamin D3, and was not re-checked until recently in June 2017. Her level of D3 was measured at 97 even though she has had no Vitamin D3 supplements during at least the last 6 -10 months. She has been referred over to a Nephrologist, who has placed her on a low dose of Hydrochlorot 12.5MG, lemon or lime water and a Mediterranean diet. She has been on low sodium since 2015, water has been increased from 64 oz. of water per day, and now upwards of that amount to 2.5 liters, and low oxalate foods as well. I am not questioning the current Nephrologist’s method of treatment, But I do feel such a large dosage of Vitamin D3 supplements prescribed by her primary doctor over a year and a half without followup is what led to the stones and current high uric acid levels leading to hypercalcuria. The urologist or nephrologist are not the doctors who prescribed the vitamin supplements. Could I be wrong about the high dosage of Vitamin D3 supplements over a year and half as being the culprit for the hypercalcuria?
Hi Donnie, Your daughter had high urine calcium since 2016, but all we know is that her vitamin D level was 29 in 2014 and 97 in 2017. I gather her D level is now 93 which is very high. I presume blood calcium levels are normal. I assume the stones occurred in 2015 and led to the urine testing. So: 2013, D was 9; placed on 4000 units of D. 2014, D level was 29. 2015 three kidney stones, urine calcium high. 2016 and 2017 I presume high urine calcium found; 2017 vitamin D measured at 97. Possibly the high vitamin D caused the high urine calcium, possibly it was high anyway. The best approach is much like what your physician is doing: low sodium, chlorthalidone, water, and wait for the D to go back down. When it does, one will know what it contributed to the high urine calcium. Regards, Fred Coe
Just would like to add, she has tested negative for hyperthyroidism, malignant neoplasm and sarcoidosis. Thank you for your review of my comments.
I gather by this her serum calcium is not high and her PTH is not suppressed. Regards, Fred Coe
My daughter who is 8 recently had blood in her urine with no other physical symptoms of a uti. We ended up at a nephrologist who did a 24 hour urine and said she is spilling a lot of calcium in her Urine. She said she will need to be on meds rest of her life. Dr believes it’s a genetic cause as I have had kidney stones many times and my mom and grandma. Me, my mom and grandma all had other alarming physical symptoms as well and have not found a diagnosis. Have you found any autoimmune diseases that cause hypercaluria? What type of doctor should we all see now to find if there is a genetic cause,,a geneticist?
Hi Kerri, Likely your daughter has idiopathic hypercalciuria. It is genetic but has no relationship to autoimmune diseases. There is risk of bone disease. Children and all others benefit from low sodium high calcium diet to protect bones. Your physician sounds correct in what he/she said, so let him/her treat you – all of you? But read this, first, for perspective. Regards, Fred Coe
Dear Dr. Coe
I had so many kidney stone that I can not remember anymore. I am 53 years old and had my first stone at the age of 14 years with many fractures over the years before and after 14 years of age. 5 years ago I was diagnosed with osteoporosis and low Vit D with a slightly lowered kidney fuction and polyarthritis. I drink Calcifirol once a week and my Vit D is in the normal range. I was also diagnosed with the HLA B27 gene due to the joint pain that I had. Everybody thought that this was the problem dispite that the inflammation counts were normal. About a year ago, I was diagnosed with renal calcium and potassium leak after insiting on a test, and put on thiazides. I was also diagnosed with Metabolic Acidosis and Idiopathic Polycythemia. For the last few months, I had venesections, which I was told that it would relieve the pain. I was initially on Fosavance but for the last year on Aclasta. My PTH is normal and so are the minerals in my blood. I use Caltrate Plus and from time to time Slow-K when I am getting cramps. I have bone pains and kidney pain everyday and I find that a bit of exstra magnesium relieves the pain for a while but not always. Bone pain is in the upper long bones and in the lower distal third of the bone. All of them can sometimes pain but in most cases it is just one of them, alternating to the others from time to time. The most frequent bone that pain, is the left femur. The sacrum also pain constantly. NSAID’s does not make any differensce to the pain. I excersice regular through my whole life and I avoid to much protein and salt. I also don’t eat sugar and very little starch and I eat a lot of assorted raw vegetables everyday. My mass is 85 kg and I am 1.8m tall. My homone levels are in normal rage for my age. My recent Bone Density scan showed little improvement in my left femur neck and lumber vertebra, but a 6.8% decrease on my right femur neck from a year ago. From what I see from my own research, is that metablic acidosis, joint pain, bone pain, polycythemia, renal calsium and potassium leaks, low vit D and magnesium all interplay with each other. None of the specialist that I visited made any connection between them. If this is a chain reaction and is a true inverance by me, how do you break the chain. I have spend a lot of money on my problem, without benifit. I would appreciate it if you could give me some pointers on what the problem might be and what to do about it. I understand that you have not examined me and it would be difficult to make a proper informed diagnosis. At the moment I am desperate as the interventions that I had, don’t seem to work.
Kind regards,
Pieter
Hi Pieter, You have what sounds like something with a name but there is not enough detail for me to try to place that name. If you would like to send all of your results I would try to interpret them for your physicians and you, not on the web but in a private note. As I am a university professor, I can do this as a courtesy. I may not be successful. Regards, Fred Coe
Hi Dr. Coe,
I am 39 years old and 4 years ago I started to get kidney stones.I have had many calcium oxalate stones on my left side and laser lithotripsies. My pth came back extremely low and my vitamin d 125 was high. My urine calcium is also high but i have managed to get it down with chlorthalidone and potassium citrate to 330. I am being seen at the yale kidney stone clinic. My ace level was normal as was my chest x ray so im guessing sarcoidosis is ruled out. My doctor said my high vitamin d is causing my intestines to absorb too much calcium which i then pee out. My blood calcium is normal. My doctor thinks it is probably some genetic thing going on causing my d 125 to be high. Do you have any insight into this?
Hi Amy, I do indeed. Given your thoughtful physicians, we have high urine calcium, no doubt normal serum calcium, high 1.25D, and no reason for the latter. This is the very make and mark of genetic – or so called idiopathic – hypercalciuria as first described in 1936 by professor Flocks. It has been a lifetime study for me. You do indeed absorb calcium efficiently – by prediction – but if your diet is low in calcium you will lose bone calcium in the urine. You have a distinct risk of bone disease with time. And, you are easy to treat. The chlorthalidone is good, but better if your much reduce your diet sodium – to below 1500 mg (65 mEq) daily. The potassium citrate will give you an additional fall in urine calcium to the thiazide. Diet calcium should be adequate – 800 to 1000 mg, and a bone mineral scan would be a good idea. Here is a reasonable article on IH. Here is a reasonable one about a treatment plan for someone like you. Idiopathic hypercalciuria is the overwhelmingly most common trait seen in kidney stone clinics. There exists an uncommon genetic cause of high urine calcium like yours beside IH; it is known by a suppressed serum PTH; if you have that, treatment is special and more complex. At Yale everyone knows about this. Regards, Fred Coe
Thank you so much for your quick and kind reply. It is much appreciated as I am trying to navigate all of this. Would you mind telling me the rare condition. My pth is supressed. I know it is rare but i would like to have all the information possible. I also remember reading an artice about fish oil being able to lower urine calcium. Have you heard of this or is there any merit to it?
Hi Amy, The best known one is CYP24a1 deficiency. This link is embedded in the hypercalciuria article. Everyone in nephrology knows about it, and I am sure your Yale physicians will find my response beneath boring as they have already considered the idea in their care of you. But feel free to share anyway just in case. I offer it as it is well known to suppress serum PTH and raise urine calcium quite a lot. Here is a more technical and recent review in case anyone needs it. Drugs that affect hepatic hydroxylase function have been discussed as a treatment – I have no personal experience. As for fish oil, I have no special knowledge. Regards, Fred Coe
Hi Dr Coe, I am not sure if you can offer me any advice or not as we are from Scotland, but I found your artical very informative. My daughter (now 16) has been suffering from kidney stones from both sides since she was around 11 yrs old. The doctor in the uk only found this out after exhausting every other avenue for her suffereing intermittently but no less that 4-5 times a year from severe abdominal pain and blood in the urine and finally submitting to giving her a ct scan. She had up until that point had ultra sounds that had shown nothing. The original CT scan found her at that time to have 6 stones 2 in one kidney and 4 in the other. These stones were ranging from just millimetres to the largest at 4cm at the time. The doctor at that point was still reluctant to do anything about this because in their opinion she will pass these naturally. This my daughter has had to do for those 6 stones and several more since then but the passing of the stone can have her in agony for weeks at a time. Since the first finding of stones my daughter has had other tests done on her blood any urine and they did discover she shows high calcium output in her urine and very slightly above average in her blood. But they didn’t offer us any explanation as to what this means. They did put her on a restricted calcium diet, a lower intake of protein and to avoid foods like green leaf veg, nuts, high caffeine etc. She was also to watch her sodium intake as up her fluid intake. This is now all in place for a few years but the stones keep forming. They then said she showed a slightly low vitamin D reading so they put her on supplements for that for a year. I was worried about giving her this as the label clearly stated do not take if prone to kidney stones but the dr said it would be fine. As said before my daughter is now 16 and is at present in agony with another stone. Her urine is bright red with blood and when I took her to the local out of hours doctor as it started at night I was told it looks like it will be another stone and as always she will pass it eventually so not to worry but they will sent her urine off to make sure it’s not an infection. I am at a loss what to do next as the dr here doesn’t seem interested in trying to find answers or interested in understand the impact this is having on my child’s life. My daughter dad did suffer from kidney stones though I am no longer with him and he has no contact with us to ask if he still does and I did ask the doctor could this be genetic but they said no. My daughter is small for her age and would be classed as underweight for her age though she does eat a good healthy diet and only drinks water.
Hi again Dr Coe, I would like to amend my previous comment in the sense that I do not mean that my daughters Dr is not interested (forgive me as I am a frustrated parent desperate for answers or a solution to stop my daughter suffering like this) My daughters Dr is lovely and is doing the best she can but appears to be at a loss as to what to do herself to help, this may be because she is a paediatric renal Dr not a stone specialist and although she has tried in a few letters to get Drs with more knowledge of this involved, as yet no one seems willing to take on her case . I have now looked back all my daughters letters from tests done and the most recent which was in may 2017 states that my daughters urine biochemistry confirms a degree of hypercalciuria and her right kidney appeared at the time a little widened in the middle measuring 6mm across, there is however no explanation as to what this means. The urine test done around that time showed excessive amounts of calcium in the urine and her blood test showed a slightly high level of urate. This letter doesn’t give specific amounts. As stated in my first comment my daughter is on a controlled diet and has upped her fluid intake to be drinking over 3ltrs of water a day. The dr has then said she wanted to discuss my daughters case with a Nephrology team at another hospital but to this date I have not heard from or seen our original doctor or any other. No one is sure if this is linked but My daughter also suffers from a bit of voiding disfunction and has had issues with constipation since she was a baby. She is on movical to help with this. There has been tests done on this which has ruled out things like chron’s, coeliac and IBD. I am maybe being impatient as a parent and this amount of time to wait to be seen by doctors about this type of case is normal and that the fact my daughter can pass these stone natuarly without needing admitted to hospital is a good thing. It is just hard to see your child in so much pain for long periods of time and not be able to help them.
Hi Fiona, I gather she is hypercalciuric, and am quite sure it is the common genetic variety I have worked on for the past 40 years. My ideas about treatment are commonplace, too, and I would hope her physicians might agree with me. Let me know, Regards, Fred Coe
Hi Fiona, Of course, information is free to travel. Your daughter probably has genetic hypercalciuria and should be treated for it. The other causes of hypercalciuria also need consideration – in the article – by her physicians. In general this idiopathic hypercalciuria (IH) arises from renal losses of calcium and is treated with very low sodium diet, high calcium diet – for her bones, together. If urine calcium does not come down with proper diet calcium and low sodium, one uses very low doses of thiazide diuretics – chlorthalidone 12.5 or even 6.25 mg daily – as the drug increased renal calcium reabsorption. Childhood stones from IH is very common and needs treatment. Perhaps your physicians may want to consider my remarks, and act on them if I seem reasonable to them. Best wishes, Fred Coe
Thank you Dr Coe for your quick response, I had never heard of hypercalciura until I came across your artical online, but after reading it I began to see the similarities to what my daughter is going through. I would agree it will likely be the idiopathic hypercalciura than the others you have mentioned but I would like the others to be ruled out. I was then even more surprised to see the word hypercalciura used in the last letter from the Dr which obviously when I read it at the time, I had assumed it was just a word used by Drs and not important as the Dr had never mentioned it when last we had spoken during my daughters hospital appointment back in May 2017. I see you have suggested that people should be on a higher calcium intake diet rather than a restricted one? At present my daughter has been told she can only have her recommended daily allowance of calcium or less but not to exceed the amount at all. As for sodium intake we have got that down as low as humanly possible with her only eating that in food that we can’t make ourselves but she knows to still find the salt content on the pakaging or ask the person making it to make sure she doesn’t go over the amount she is allowed. No one has mentioned the possibility of her bones being affected by the calcium loss is this something I need to be asking about? I need to call my daughters GP tomorrow anyway as her urine is still red (usually the red blood part only lasts a few hours) plus my daughter has been in agony all weekend which to me indicates this stone is on the larger size and for the first time might need help. I will however also ask the GP to contact the renal Dr to arrange an appointment so we can see her as soon as she can(this could still be over a month before she can see us though) but at least then I can discuss everything you have written about. My daughter and I also pleased to hear you say that stones are common in childhood with this condition as every Dr we have seen up until now had never come across a child having stones before and this made my daughter feel slightly isolated as she though no one understood what she was going though and that some people were accusing her of lying for attention.
Hi Fiona, Bone mineral loss is commonplace in IH when diet calcium is inadequate. One cannot tell sodium intake, so you need successive 24 hour urine collections to correlate sodium loss – it equals diet intake – and calcium loss. The latter faithfully parallels sodium. I have placed graphs of this on the site. Read this, as I am sure it relates to your daughter. I failed to mention children but should have. When urine sodium has fallen – a good number is below 65 mEq (1500 mg) sodium, urine calcium should be much lower; should bleeding and crystals persist, the thiazide I mentioned is quite effective. Being genetic 1/2 of her immediate blood relatives will have this trait. Regards, Fred Coe
Hi my name is beau,
I have had Calcium oxalate stones since I was 18 and am now 29 with the last attack a few weeks ago passing 2x 5mm stones and 1x 2mm stone. My blood levels and kidney function came back perfect, but my urine levels showed high calcium excretion again (I already knew this for quite a while) the dr said the levels should be between 2-8 normal levels and the last two 24hr urine collections show mine at 13.0 &13.4 with urine output approx 2.5ltrs
They have recommended a thiazide which I’m about to commence but I was wondering if you have any thoughts on it as there is a lot of calcification in my kidneys and it’s not something I want for the rest of my life. It’s seems they have ruled out anything else in their mind. But as far as dieting they have just recommended more water.
Would appreciate your thoughts
Beau
Hi Beau, You do indeed have hypercalciuria and given normal blood values it is surely genetic. Treatment begins with lowering diet sodium and that will lower urine calcium – see the article in the link. Bone disease can occur in IH, so you need 800 to 1000 mg of calcium from foods. When diet sodium = urine sodium – is below 100 mEq (2000 mg) or even lower (ideal is 1500 mg) and if urine calcium is still high, then one uses a very low dose of a long acting thiazide like diuretic like chlorthalidone or indapamide. Ask your physician about these alternatives and remember I am just voice from far away and she/he is responsible for your care. Regards, Fred Coe
All you write are very fascinating! I have a question for you.
Approximately, how big would the changes be in 24h urinary calcium in non-IH people and in IH patients when they increase their dietary calcium from 800mg/day to 1200mg/day?
Just because the intestine blocks calcium absorption after a certain limit in normal individuals can we expect to have minimal changes in urinary calcium?
Thank you very much.
Just got my 24 urine test back, confused! Urine oxalate is down to 23, Urine calcium went up to 324, Ugh!!, Ph, is 7.321. I have increased my calcium and I’m still loosing alot in my urine. I must also add my sodium is 91, and protein is 1.2. so the conclusion is that calcium loss is not from sodium or protein. What would you recommend ? Getting most of my calcium from coconut milk, veg, only take a calcium citrate supplement if I think I need more for the day, and take 500 mg with a meal. I can’t do dairy. I have has my parathyroid glad checked and all seems normal. I do have osteoperosis, so that’s a real concern. Also if I have to go on some kind of meds, what is the best kind and will that be long term?
Hi Vickie, your urine oxalate fell because you added diet calcium. Your urine calcium rose because you did not lower your urine calcium anyway near enough. 90 mEq/d is near the US tolerable upper limit – you need to go down to 1500 mg/d of sodium or less until you begin to retain the calcium you are taking in instead of losing it in the urine. A protein intake of 1.2 gm/kg/day is high; 1 is the upper needed. High will raise urine calcium. No meds until you have really lowered diet sodium; if you cannot control the urine calcium with sodium restriction, then a small dose of chlorthalidone would be good to add to the diet. Your physician is entirely responsible for this decision. But always do the sodium first. Regards, Fred Coe
Thank you so much for the information, very helpful. I thought bringing sodium down to 90 was good., I did lower my protein from last test, but will work on that as well. I will work on the diet and really keep track of the sodium content, and retest. How long should I wait before a retest?
This is what the Litholink said in the summary that I got back. This is why I was confused on all of this, but I will take your advice.
Urine calcium is high and has risen (was 236 and now is 324 mg/d). Our records do not show the use of
calcium supplements, confirm clinically as calcium supplements can cause hypercalcuria. High urine calcium
cannot be ascribed to high sodium (91 mmol/d) or protein intake (PCR = 1.2 g/kg/d). Our records do not report
that thiazide has been prescribed. Consider use of thiazide. If prescribed recheck at 6 weeks. Monitor serum
potassium as appropriate.
Sorry, but one more question. I’ve really been watching the oxalates in food. So could that also be the reason for my lower oxalates and not just adding more calcium? It went from the last test being 38 down to 23 on this latest urine test.
Hi Vickie, Indeed the higher calcium is most likely the reason. To go as low as 23 almost always means calcium effects. That increase of diet calcium raised your urine calcium because your diet sodium and protein are too high. Neat. Regards, Fred Coe
Hi Vickie, I infer you raised your diet calcium, and see your diet sodium and protein intakes are high enough to cause the higher urine calcium. The Litholink algorithms were written by me and John Asplin when I owned that company, and I would no longer write them in the same way. Lower your diet sodium more, and your protein intake, and see if that fixes things. Regards, Fred Coe
Thank you so much for taking the time to help me understand all of this. Very much appreciated. I will work on lowering my sodium and protein.
Thanks again
Hi Dr. Coe, this is my last urine test. I value your opinion and was wondering if you think this means I should consider taking thiazide? My sodium dropped from 91 to 71, and my protein went from 1.2 to 0.9. I just needed another opinion before I discuss this with my doctor. I listed the last report and the one before for comparison. Seems like there is improvement , I also feel like I should up my calcium, I can’t tolerate dairy, so get most from coconut milk. around 900 mg from that and try to get the rest from other food. Maybe I should also take a supplement. Can you share your thoughts on this? Urine Calcium did improve some. Thank you Much!
07/03/18 03/16/18
Vol 24 – 3.53 2.92
SS CaOx – 3.82 3.95
Ca 24 – 243 324
Ox 24 – 31 23
Cit 24 – 695 892
SS CaP – 1.12 1.61
pH – 7.319 7.321
SS UA – 0.02 0.02
UA 24 – 0.439 0.529
Sodium – 71 91
PCR – 0.9 1.2
Hi Vickie, your urine calcium is still a bit high but lower, and your SS value for calcium phosphate is lower. I fear your diet calcium is lower as oxalate is up. If you can maintain the high volume, and there are no new stones, you might just stay as is and keep thiazide if new stones come. Otherwise, keep the diet as is and use a tiny amount of thiazide – I use very low doses. But your physician is in charge here, I am far away, and s/he is responsible for you. Regards, Fred Coe
I have been diagnosed with hypercalciuria, calcium oxalate kidney stones, and osteopenia. My PTH and Calcium levels in blood are normal; however my Bun/Creat is high 27, my liver function tests have also been high numerous times, and have a cyst on my kidney which they say is nothing. Vit D has always come back low but came back normal on my last time. I have recurring bouts with what appears to be kidney stone pain but have only caught one or found one on a scan. I have had a couple of UTIs but the majority of my UAs come back clean. I have had a complete hysterectomy 15 yrs ago and stopped hormone therapy a few years ago. Also I have inappropriate sinus tachycardia, there seems to be concern if HTCZ could make it more symptomatic and have told me to hold off on taking it.
I am getting completely conflicting treatment plans between Endocrinologist, Urologist and GP in regards to not to or to take Calcium & how much, take or not take HTCZ, and how to proceed. As of right now they have told me to reduce calcium and dairy intake to a minimal and have never mentioned sodium as you have.
Thank you for any insights you might be able to share with me!!
Hi Karol, I gather your urine calcium is high, serum calcium normal, and bone mineral density low. The liver complications seem outside the mainstream here. If you indeed have idiopathic – genetic – hypercalciuria, and bone disease, decades of work lead to high calcium 1000 to 1200 mg/d diet, and very low diet sodium – to prevent loss of the diet calcium in the urine. The thiazide only works ideally when diet sodium in very low – below 1500 or even 1000 mg/d. One can say that by now low calcium diet is never a good choice. Of course, do not make up your own treatments from what I say as your physicians may know things I do not; simply ask their opinion. Regards, Fred Coe
Hi Dr. Coe,
Would you please comment about the level at which vitamin D exacerbates hypercalciuria? Is there an optimal level to shoot for with IH, particularly for those who have osteoporosis but do not want to contribute to stone risk?
Thank you,
Mary
Hi Mary, serum vitamin D – 25 hydroxy D – has no known effect on urine calcium over the range from 20 to 50 so you can feel free to use it. Above 50 or 60 possibly active vitamin D (calcitriol) might rise, but the evidence for this is scant. So use enough for your bones. Remember, low sodium diet is the prime way to lower urine calcium, then thiazide if needed. Diet calcium needs to be 1000 mg or more for bones. Given osteoporosis, you may benefit from bone directed meds – a matter of complexity for your physicians. Regards, Fred Coe
Thank you so much for this fascinating article! I have idiopathic hypercalciuria. I am in my early 30s and experienced a miscarriage shortly before discovering this diagnosis. After a year of treatment with my endocrinologist, my 24 hour urine only showed minimal improvement. I’m on calcitonin, Vit D, calcium and HCTZ. When I first saw my endocrinologist, I told her I was following the ketogenic diet for weight loss, which she recommended, but it is high in sodium and I see that you recommend a diet low in sodium. Do you know of any side effects of the ketogenic diet on idiopathic hypercalciuria? I was hoping to try to conceive again, but it doesn’t look good unless I can normalize my numbers. Any suggestions? Thank you kindly!
Hi Kelly, idiopathic hypercalciuria is complex and in essence is an excessive sensitivity of kidney calcium loss to diet sodium; as diet sodium rises, urine calcium rises far more in IH than in normal people. Here is an article on your exact problem. Low sodium diet is the base of all treatment; high diet calcium is important for bones; the diuretic will do no good if diet sodium is high, so it is best used if low diet sodium does not control urine calcium. A sodium ideal is 60 mEq/d *1500 mg/d in common units. Regards, Fred Coe
Hi Dr. Coe,
Hmm – my 2 endocrinologists recommended that my D to be around 35 since they feel that as it rises, so can urine calcium loss in IH. My nephrologist wants my sodium intake, which to date has been about 1500 with no urine calcium reduction – still in the 300 range – after a year (on a bisphophonate), to be 2000 or so since I will be starting HCTZ 12.5 to try to reduce the calcium loss AND my BP tends to run on the lower side. Any thoughts? I’m a bit confuzzuled. Thank you!
Hi Mary P, I do not want to insinuate myself into your care between you and your real physicians, so my remarks are of a very general nature and need not apply to your specific case. In general, diet sodium and thiazide drugs interact this way: Urine calcium rises and falls with diet sodium (urine sodium marks diet sodium very closely) in a regular way that is more steep in hypercalciuric vs. normal people. In fact the central abnormality of idiopathic hypercalciuria is an undue rise in urine calcium for a given increment of diet sodium. At any given level of diet sodium, thiazide lowers urine calcium, in other words the drug displaces the whole curve of urine calcium vs. diet sodium downward. This means that one achieves as low a diet sodium as possible and if urine calcium remains high enough to pose a stone risk one uses a tiny and fractional dose of thiazide like drugs to achieve the final goal. Diet protein when high can raise urine calcium for any given diet sodium, as can high calcium diet – needed for bones. Perhaps your calcium intake increased, for your bones. Given the physiology, that is general, your treatment remains the responsibility of your physicians. Regards, Fred Coe
Thank you so much for this helpful article! I have had kidney stones since 2001 and recently had a ESWL procedure to break up a large (9 mm) stone. Prior to the procedure, I underwent a 24-hour urine supersaturation, and I have just now received the results. Here is what my doctor told me:
*I had an elevated urinary calcium level (hypercalciuria) of 284 mg
*I had an elevated urinary oxalate level (hyperoxaluria) of 53 mg
*I have low urinary citrate (hypocitraturia) of 346 mg
*My urine pH is slightly alkaline [number not given]
She has recommended keeping up water intake, increasing citrus, avoiding excess calcium supplementation, and reducing sodium intake. Would these be your recommendations as well?
I am definitely reluctant to take a thiazide diuretic because my blood pressure tends to run low, and I am already prone to dizzy spells. I have an upcoming follow-up appointment to my ESWL procedure next month, and at that time, I will bring in captured kidney stone fragments to be analyzed. Might that change the treatment recommendations? I would also note that at the time of my last blood test earlier this month, both my sodium and calcium levels were within normal limits (140 and 9.5, respectively).
Finally, would it be important to discover the causes of my supersaturation urine abnormalities? I also suffer from chronic migraines and wonder whether low magnesium levels might be a factor. I do not believe I have ever been tested for this, although I do take magnesium supplements.
Thank you for any help you can provide.
Hi Beth, Your urine calcium does seem high, and I suspect your diet calcium is low – high urine oxalate is usually a tip off. Treatment is based on low diet sodium high diet calcium etc – here is how it works. Supersaturation arises from the high oxalate and calcium, and that can be improved by diet. The low citrate maybe inadequate fruits and veggies – part of the kidney stone diet. Let me know, Regards, Fred Coe
Thank you Dr, Coe,
I’m thinking maybe adding more calcium, keep my volume up and hope for no new stones. If I was to start on a low dose of thiazide, does that mean I would have to take it for life? Also is there a danger with low potassium with a low dose of thiazide? I appreciate all your feed back. Wish I did live closer, I would definitely be making an appointment. Thanks again
Hi Vickie, Thiazide is not for life, so if your physicians wants to use it go ahead. S/He will monitor your serum potassium if you use the drug and take steps to keep it normal. Regards, Fred Coe
Hi Dr. Coe,
I have extremely high levels of Calcium in my urine with high PTH LEVELS and kidney stones that I live with in my kidneys. I have been to many doctors and there has been no explanation or treatment. I consider myself a healthy 55 year old, work out regularly and eat well. I don’t drink alcohol and I have always maintained a low sodium diet. I have noticed when I sweat it’s extremely salty. My 2 sisters have cystic fibrosis. One just died from the disease. Their sweat was overly salty as is mine. I am a gene carrier of cf. I think sodium also has something to do with cf. I’m concerned about my kidneys due to the several stones in my kidneys and occasional blood in my urine but only pains in my lower right side. I’m not sure what to do. Do I just go about life with these abnormal levels of high calcium in urine and PTH levels that have reached as high as 180. No doctor has suggested any form of treatment. I have had several 24hr calcium urine tests, all results abnormal. Perhaps you may shed some light on the situation. Thank you,
Gina
Hi Gina, In one study hypercalciuria seemed frequent among CF patients. Another study showed no relationship. The high PTH could be from the malabsorption one sees in CF. You do not mention it but is your serum calcium even slightly high – primary hyperparathyroidism is certainly an important alternative. This is a complex problem, and your physicians are the only ones who can figure it out as I have too little information. Regards, Fred Coe
Hi Dr.Coe, My doctor put me on a low dose of chlorthalidone, 1/2 of 25 mg, On day 5 I had some bad side affects, rapid heart beat, chills, weakness, restlessness, moody. I also have increased my potassium, with low sodium v8, bananas, orange juice, and other fruits with potassium. Could it be from low potassium that early on? I feel I just can’t take this medicine, and if not what other options? Or will they all have the same side affects. My last 24 hr urine test wasn’t that bad. I still have a 3 mm stone left from the last lithotripsy , but no new ones as of yet. This is the last 2 urine test for comparison:
07/03/18 – 03/16/18
Vol 24 – 3.53 – 2.92
SS CaOx – 3.82 – 3.95
Ca 24 – 243 – 324
Ox 24 – 31 – 23
Cit 24 – 695 – 892
SS CaP – 1.12 – 1.61
pH – 7.319 – 7.321
SS UA – 0.02 – 0.02
UA 24 – 0.439 – 0.529
Sodium – 71 – 91
PCR – 0.9 – 1.2
column on the left is the last one I had.
What do you think about trying another medicine or is my diet doing an ok job ?
Thank you in Advance
Vickie
Hi Vicki, Your last test looked pretty good and it sounds like the drug does not work well for you. Perhaps your physician may want to go on without it. S/he might try indapamide 1.25 mg/d instead. Some people feel better with it. Regards, Fred Coe
All tests normal except urine calcium at 251mg. Passed a calcium kidney stone, 2 stones remaining. I’m 57, early menopause at 47, diagnosed with osteoporsis 5 years ago. Increased calcium and D with supplements. Diagnosis is Hypercalciuria nephrolithiasis. Otherwise healthy. I don’t see this as a diagnosis, but rather a definition of a symtom. I know the osteoporsis and stones are related, and afraid to decrease calcium supps. Not sure what to do now.
Hi Cherie, You are a very clear minded person. Genetic – idiopathic – hypercalciuria is a complex derangement that fits your findings and can cause both bone and stone disease. Here is the better article. High calcium low sodium diet is ideal, low doses of long acting thiazide is often added when needed. The low sodium will reduce urine calcium losses and permit high diet calcium, but low sodium is hard to achieve. Food calcium may be preferable to supplements. Regards, Fred Coe
I wound up in the ER with a kidney stone– upon further evaluation, a CT showed several stones (some 5-6 mm) in both kidneys. Passed stone eventually– had analysis completed and showed composition of stone was 80% calcium phosphate. Had lithotripsy procedure– my post-op CT showed there are still stones in both kidneys, most smaller, some unchanged in size. Had 24-hour urine study done– urine calcium was 511 mg/24 hour. Tested PTH– levels were normal. Was started on chlorthalidone, however, it dropped my potassium significantly and quickly. Was started on a potassium supplement and was taking 100mEq/day and still was not enough to counteract how much the chlorthalidone dropped my potassium levels. Decided to discontinue chlorthalidone (and potassium supplements.) My urine calcium at 511 is quite high– should I be concerned about this? Should I go back on the medication?
Hi Paige, You have multiple calcium phosphate stones and very marked hypercalciuria. Be sure your serum calcium – fasting, off the chlorthalidone – is normal. Chlorthalidone is best used with low sodium diet and in a very low dose. The ideal diet is 1500 mg sodium, the dose 12.5 mg of the drug. That often works. See if your physician considers this a worthwhile variation that might help. Given so marked a hypercalciuria I am sure s/he has ruled out any systemic diseases as a cause. Regards, Fred Coe
I have been diagnosed with renal leak hypercalciuria. I have been given triam/thiazide 25 mg once a day and it has reduced my Ca24 from 454 to 253. Seems like it is getting better. I was wondering if it ever gets better and stays better or is the thiazide going to be needed from now on?
Hi Jim, All hypercalciuria is due to reduced renal calcium reabsorption, so you will need long term treatment. Very often, lower sodium diet – 1500 mg/d will do as well as thiazide. You might mention this to your physician. Here is an article about treatment of a condition like yours. Regards, Fred Coe
Hello and thanks for reading!
I had two stone episodes 15 years apart. In 2003 I had two stones in each kidney. I had EWSL on both kidneys but it did not break up the stones in the left kidney, so one was removed and one was left there. 15 years went by and I ended up in the ER with a 6mm, 9mm, and 2mm calcium oxalate/phosphate stones. I had a stent and then uteroscopy, lithotripsy and basket removal of the two larger stones. The 2mm remains in the left kidney.
I had two 24 consecutive 24 hour collections done. My volume on day 1 was 2.49 and it was 2.82 on day two. Other results were:
Day 1
Vol 24 SS CaOx Ca 24 Ox 24 Cit 24 SS CaP pH SS UA UA 24
2.49 4.31 276 23 388 0.63 6.010 .41 0.508
Vol 24 SS CaOx Ca 24 Ox 24 Cit 24 SS CaP pH SS UA UA 24
2.82 3.31 174 26 506 0.60 6.381 0.20 0.585
All of my dietary factors were within normal range and the only normalized value that was out of range was ca/cr 24 of 265 on the first day.
In June my blood calcium was 10.1, which I understand may be high for my age of 52.
My question is about possible hyperparathyroidism, as I have other symptoms that lean in that direction. I am unsure though of the next steps to take in the investigation. I did have a negative ultrasound notwithstanding the remaining small stone.
Thank you for any advice.
Hi Laura, I gather you have calcium phosphate stones and that it is unclear if you are making new ones because a stone was left behind 15 years ago after SWL; SWL scatters crystals about the kidneys that can grow into larger stones. Let’s assume new ones are forming, and you have a borderline high urine calcium and serum calcium. The best course is repeated fasting morning serum calcium measurements each with a PTH measurement – I favor at least 2 of these. If they remain at 10.1 and PTH is normal or high, PHPT is indeed a possibility. The negative ultrasound despite a CT proven stone is commonplace as ultrasound is not so sensitive. Feel free to share these thoughts with your physicians, and if they agree get the proper testing. If you do not have PHPT yet have made more stones, the increased urine calcium can be treated with low sodium diet as noted in the article and in this one as well. Regards, Fred Coe
Hello, and thanks so much for your response. My primary doctor is in agreement that this should be investigated further, although my urologist felt that my values were OK, which leads me to a follow up question:
On the second day of the 48 hour collection my values were better than the first day, and those seemed to be the ones that my urologist focused on in his interpretation of the results. However, my water intake was also better that day compared to the first day, specifically because the nurse in his office told me to push fluids throughout the collection.
I think my question / concern about this is that the amount of fluids I pushed both days is not sustainable on a daily basis, unless I want to quit my job/life and do nothing but drink water and urinate all day and night long. So that makes my think that its not viable to expect the same results under more normal conditions with a more reasonable amount of drinking and voiding, and that the results I got from this collection are not really an indicator of how my kidneys are functioning or my risks of future stone formation.
Did I make a mistake by increasing my fluids during the collection to an unsustainable amount? Could that have made the results less reliable? I ask because although my primary doctor is keen on looking further into this I was concerned that my urologist accepted the results as good indicators of my overall kidney function. Any light you can shed would be helpful as I decide how to proceed.
Thanks again!!
Hi Laura, Indeed it was a bad mistake to distort everything just when you were testing to figure out how stones formed. How better to miss everything than make changes while testing then go back to what you do every day. Get repeat studies while at work and find out what is really causing stones. Regards, Fred Coe
Dr. Coe.
I have been reading into these issues for years and your name keeps popping up. I am running out of ideas with my own issues.
I’ve had 110 calcium oxalate stones in the last 7 years. 2-3 a month. Serum Calcium is always normal. PTH is always normal 25-40 range. Vitamin D is deficient around 13. Urine Calcium is always high in the 400s. I have all the symptoms of pHPT, but always have to argue with Endocrine that as long as PTH is never suppressed below normal range it is HPTH. Even on HCTZ for a year my PTH never dropped. It gets worse every year and I am tired of fighting the Doctors. Do you think it could be something else or is it safe for me to assume hyperparathyroidism.
Hi Dustin, I gather your serum calcium is always normal, PTH normal, urine calcium high – this is not primary hyperparathyroidism. It is probably idiopathic hypercalciuria and incompletely treated. Surgery for PT disease is NOT an option. Regards, Fred Coe
I just reread my statement and I didn’t fully explain the serum calcium, sorry for the confusion. I’m in my late 30s. My serum calcium has been jumping all over the place but the majority are 10.1 to 10.4. Sometimes it drops to the mid 9s but pth is always steady. I am otherwise healthy, I have been active duty Army for 16 years now and this all started after a deployment to Balad, Iraq. The last two years it has been getting worse and I am fighting chronic fatigue, headaches, and have been spacing out mentally. I told my Doctor that it feels like I am slowly dying and I just the kidney stones to stop so I can get my life back. I don’t feel that it is as simple as IH.
Hi Dustin, So serum calcium has been both high and normal. Here is the best strategy: Gather all of your serum PTH and calcium values. Discard all those not drawn fasting and in the morning, as fasting morning bloods are the basis for the normative standards. If in that subset of values serum calcium has been high, get some more – morning and fasting – with PTH and calcium in the same blood. Diagnosis of PHPT is based on increased serum calcium, fasting, and a normal or high PTH in the same samples as the calcium + a urine calcium that is not low. Regards, Fred Coe
Hi
In March 2011, I was diagnosed as Osteoporosis patient. I am male and 51 years of age as of toady. Results of BMD was: Left Hip T Score -1.9, Z Score -1.6 (femoral neck T Score -2.8 & Z Score -2.2) SPINE: T Score -3.4 and Z Score -3.2.
I was given the treatment of Aclasta Injection (once every year) during last five years to strengthen the bones.
To investigate the reason for osteoporosis, examination of parathyroid scintigraphy with sestamibi was done June 2013 and the results was as follows:
“radionuclide parathyroid scintigraphy with sestaMIBI revealed no evidence of functioning parathyroid adenoma in neck or mediastinum.
Te results of recent (Nov 2018) Dexa Scan revealed further deterioration in bone and the result was as follows:
Left Hip T Score -1.9, Z Score -1.6 (femoral neck T Score -2.6 & Z Score -1.9) SPINE: T Score -3.6 and Z Score -3.3.
( Please note that in Feb 2015, results of Femoral neck was T Score -1.7 and Z Score -1.0)
Now recently (Dec 2018) doctors have advised me to undergo the following lab tests:
Result
Urine calcium 679
Urine creatinine 2.4
Creatinine clearence 166.8
Serum Creatinine 0.8
Serum Phosphorus 4.0
Serum TSH 0.345
Plasma PTH 66.2
Serum 25- Hydroxy Vitamin D 24.2
Plasma Glucose Fasting 136
Whole blood Hb1C 7.4
Please review my case and advise me best treatment for my Osteoporosis problem. Pl suggest if you think that I should do more tests in the diagnostic process
Thanks
M Khalid
Hi Khalid, You certainly have extreme elevated urine calcium and may have bone disease from idiopathic hypercalciuria – a familial condition. I cannot review your case and advise as that is to practice medicine for someone I have never met – illegal in the US and not a good idea either. For hyperparathyroidism the key is your serum calcium which you do not mention. I presume it is normal, fasting in the morning. The scans are not helpful for primary diagnosis. Speak with your physicians about serum calcium results and if there is some known reason for your very high urine calcium. If it is otherwise unexplained idiopathic hypercalciuria might be correct and treatment is reasonably well defined. Your high serum glucose and Hba1c indicate diabetes, a cause of bone disease and hypercalciuria – overall that may be the main issue for your physicians to manage. Perhaps both IH and diabetes are important here. Your physicians need to decide all this. Regards, Fred Coe
Hello Dr. Coe, My wife has repeatedly had calcium oxcalate stones and I’m musing on the subject. I’m wondering, do you know of any link between circulating calcium and high-impact exercise (like running)? I’m wondering if there’s any signaling that would alter the uptake or release of calcium from the bones, or from dietary calcium to the bones. Thanks!
I am a 79-year old Caucasian female with a history of corticosteroid use for polymyalgia rheumatica (for 18 months, starting at 80 mg) and osteoporosis. I have been treated with Fosamax 70 mg for 2 years (2006-08) followed by Reclast infusions in 2009, 2010, 2017, and 2018. (I refused to have it from 2011-16). I am scheduled for another Reclast infusion on March 29. A 3-mm kidney stone was noticed on a CT scan in 2002, 2003, and 2004 when looking for a cause to RBCs in my urine. Because of the stone, I was selected for a 24-hour urine test in the Nurses Health Study (I’m a member of the 1976 cohort). It showed a calcium level of 328, with a comment of “Hypercalciuria. Suspected problem is hypercalciuria nephrolithiasis.” Despite treatment, my osteoporosis seems to worsen and my fracture risk is now at 51%. In preparation for the next Reclast infusion, I had a 24-hour urine test, which showed a calcium level of 424. Blood vitamin D level was 61.9, PTH 15.0, albumin 3.7. This was nonfasting and I was taking my usual medications and supplements. Blood work showed a Tandem-R Ostase of 5.5, down from 6.5 two years earlier. I assume this means my bone turnover is low because of the Reclast; so I keep old bone but don’t make new bone? My osteoporosis is managed by a rheumatologist. I seems that the local endocrinologists don’t treat it or don’t take Medicare. Because the hypercalciuria hasn’t been addressed and my osteoporosis is worse despite treatment, I made an appointment to go to the Mayo Clinic in MN for consultation with an endocrinologist who does treat osteoporosis. My question is this: Do you think I should postpone the Reclast infusion until I have been seen by the endocrinologist? It seems to me that I have other issues contributing to bone loss and may need a different type of intervention. For that reason I believe I should wait. Thank you.
Hi Jan, You have hypercalciuria with a very low serum PTH. Idiopathic hypercalciuria famously causes bone disease, but there are other causes as well. Mayo is excellent in general. Dr Raj Kumar is a remarkably brilliant physician scientist there and I would try to get him to see you. He towers over most other people in the field. You can say I said this, and perhaps that will help. Regards, Fred Coe
Thank you!
This is very interesting article, doctor Coe. Thank you.
I am a year and a half post parathyroid adenoma surgery, 45 year old female, lost two glands and a half of the thyroid. I also have Hashimotoe and on thyroid medication (T3 + T4). It took 5 months to bring my serum Ca to normal after the surgery and hypocalcemia symptoms were severe. Now, after 6 months of normal life the symptoms have returned (mostly tingling and cramps) with low serum Ca (2.05 -2.09 mmol/L), normal PTH (shows activity, but doesn’t get above midrange), and at this time very high urine Ca. I was taking 1500mg of Ca citrate and 5000 IU of D3 for the last 6 months daily, feeling great, but when hypocalcemia symptoms returned my GP advised to raise the dose to 3000 mg with no improvement (this is when he tested 24hr urine and found out that Ca is x2 from the highest number in range (14.8 mmol/day with low phosphate). There are thoughts that the supplements just not being absorbed and I may have kidney issues and/or remaining parathyroid’s activity is not sufficient, even though it tests as “normal”. I reduced Ca supplements to 600 mg a day and retested in few days, so urine Ca dropped to 8.75 mmol/day, but serum Ca is still low ( but did get up from 2.08 to 2.12 mmol/L with PTH 3.4 pmol/L), vitamin D is in midrange. My GP wants to put me on thiazide, but my blood pressure is already on the lower side and I don’t consume much sodium. Serum Mg, K, phosphate and sodium are normal, bone scan last year – normal. Is there any known way to bring serum Ca up other than this medication? What other tests are recommended to confirm whether I may or may not have a renal reabsorption problem? I want to make sure I am diagnosed correctly. Thank you.
Hi Natalia, I suspect that perhaps some PT tissue was removed with your thyroid or that during the surgery blood supply to one or both of the remaining glands was compromised. That there is some PT hormone in your blood is a very good thing. I imagine the low urine phosphate is because the high oral calcium load is blocking phosphate absorption. The inadequate PTH prevents normal renal conservation of calcium, of course. With time – perhaps a lot of time – the remaining PT tissue may enlarge so you have a better balance between oral calcium intake and renal losses. Now your main risk is stones from the high urine calcium. You and your physicians are doing the right thing: use supplements only as needed, try to lower diet sodium to the maximum possible, measure urine sodium – do not guess – and strive for <50 mEq (1500 mg Na) or even less. I would move supplements away from meals so you are sure to absorb phosphate better – cells need it. Here is some additional PT physiology for you. Regards, Fred Coe
Hello Dr Coe, I am a patient with osteoporosis and idiopathic hypercalciuria (hx of stones in the past)… I also happen to be a radiologist. In addition, I’ve had a problem with obesity for many years, with many episodes of significant weight loss and weight gain. I’m about to undergo bariatric surgery (sleeve gastrectomy). I have seen many docs for opinions on how to treat my osteoporosis and hypercalciuria; and recommendations have varied from evista to bisphophonates to prolia (as well as thiazides, which I cannot tolerate due to hypokalemia). I’m confused as to best course of treatment; especially since I expect to lose more weight after surgery (hurting my BMD); AND I will have to take PPIs for some period of time after surgery (?hurting my BMD as well). I have sought opinions from nephrologists, endocrinologists, and rheumatologists, from UPenn and Columbia (where I saw John Bilezikian, whom I remember from when I was at P&S). Can you weigh in with any opinion; and/or could you recommend someone who could address BOTH my bone and kidney issues? (PS I also have psoriatic arthritis, on Humira, but I don’t *think* that has any bearing on this problem). THANK YOU. -Julie Cole
Hi Dr Cole, This article on idiopathic hypercalciuria is complex but well within your reach as a physician. The bone disease appears to arise from reduced renal tubule calcium reabsorption and bone mineral lability – some from increased tissue vitamin D effects. High calcium diet coupled with low sodium – 50 – 60 mEq/d is ideal – to increase renal calcium reaborption is the only diet regimen that can bring bone balance to neutral in perimenopausals and by extension – no trials – in IH. Very low doses of thiazide like drugs – I like chlorthalidone 12.5 mg daily – also promote bone mineral retention. Hypokalemia is minimal when diet sodium is low as I mentioned, otherwise it is very annoying. The PPI drugs are not ideal for bone, but perhaps their use can be transient. If needed bone active drugs are best on a background of high diet calcium low diet sodium and therefore added not in place of diet. Of course the diet + CTD will lower urine calcium (and oxalate) and is well known as a way to reduce stones. Regards, Fred Coe
Dear Dr. Coe,
I am a 56 year old female with osteoporosis and a history of calcium oxalate kidney stones. I first consulted with an endocrinologist for my osteoporosis early in 2016. He had me do a 24h urine collection and found my calcium excretion was too high at 284 mg on a reference range of <=199 mg. He started me on chlorthalidone 25 mg and Potassium CL ER 20 MEQ. Since 2016 I’ve had six 24h urine calcium tests ranging from 190 mg to 258 mg with an average of 221mg. My serum potassium has decreased from a pretreatment level of 4.4 mmol/L (range 3.5 mmol/L to 5.2 mmol/L) to an average value of 3.6 mmol/L despite the potassium supplement and my efforts to increase potassium consumption in foods. In addition, the osteoporosis has worsened significantly with my spinal T-Score going from -1.9 in Oct 2015 to -3.2 in Aug 2019 (-16%) despite concurrent treatment with raloxifene for nearly 2 years.
My questions are these:
1 Is potassium chloride the best form of potassium for someone with osteoporosis or would a different form such as citrate would be better?
2) In a situation with low serum potassium levels, would it be beneficial to lower the chlorthalidone to 12.5 mg or perhaps stop all together? It’s my understanding that low potassium levels can create an acidic environment which would be detrimental to bone health.
3) I’m trying to follow the high calcium/low sodium diet you outlined for bone mineralization but find it very hard to track the actual sodium consumption I’m getting. Are there lab tests that can be done to determine if I’m achieving the low sodium goal?
I’m trying to educate myself on this as much as possible and your informative articles have been a blessing to me. Thank you for sharing your wealth of knowledge!
Best regards,
Cori L.
Hi Cori, I assume you have idiopathic hypercalciuria, and it is fomenting bone mineral loss. Thiazide is effective in maintaining bone mineral, but only if diet sodium is not high – the only way to know diet sodium is to measure urine sodium, guessing never works. If you have a low urine sodium and decent diet calcium and use chlorthalidone and bone mineral loss progresses you should be taking a bone directed medication. The choice of such medication is beyond this site, but a simple bisphosphonate usually works as a first agent. As for potassium, both the chloride and citrate forms are fine, and the choice depends on the urine citrate and pH. If the citrate is low, potassium citrate may be the better choice, but it will raise urine pH and risk for calcium phosphate stones. Citrate is lowered by potassium depletion, so take enough potassium to raise serum levels to normal for at least several months before making the 24 hour urine measurement. Regards, Fred Coe
Dear Dr. Coe,
Thank you for your response, it is much appreciated. I will work with my endo to get the potassium levels up to normal and then test the citrate. I had tried alendronate for the OP back in 2017 but had a severe allergic reaction so bisphosphonates are off the table for me which limits the choices significantly. My U24 sodium was 107 mmol/day (range 41-227). If I did the math right that’s 2461 mg of sodium vs. 1500 mg recommended. So I need to address that with dietary changes. I don’t add a lot of salt but I’m thinking a salt substitute is potassium chloride, that would help with reducing sodium and increasing potassium – both of which I need. Thanks again for helping me understand!
Cori L.
Hi Cori, If your bone mineral falls below a safe level your physicians have a much larger array of medications to stabilize it beyond bisphosphonates. Just be sure to follow up with them and I am sure they will do what is needed to prevent fractures. Potassium chloride salt substitute is not a bad idea so long as the taste is reasonable for you. Regards, Fred Coe
Dr. Coe, Thank you again for your response. I tried the salt substitute and it’s really not too bad. I’m hoping it will help to raise my serum potassium level. I really had no idea how much sodium was in my diet but I see now from reading labels that some foods have a tremendous amount. I’m glad to have a path forward and very much appreciate your help in understanding this complex subject.
Cori L.