 In my very long and complicated article I detailed primary hyperparathyroidism (PHPT) like a good scientist should. With all my heart I tried to make it plain enough for people in general to get a sense of how things work, but looking back on it, I doubt many will. Anyway, this book structure makes a place for summary and synthesis.
In my very long and complicated article I detailed primary hyperparathyroidism (PHPT) like a good scientist should. With all my heart I tried to make it plain enough for people in general to get a sense of how things work, but looking back on it, I doubt many will. Anyway, this book structure makes a place for summary and synthesis.
Is this PHPT lite?
Not really.
It is PHPT practical, devoid of all but assets material to evaluation and treatment. Even so, in those areas I go into perhaps greater depth than in the parent article. The two articles complement each other as best I can arrange.
Alabama Grist Mill Dam by Beverly Hammond catches the sense of how PTH works on serum and urine calcium and phosphate. Also, it is beautiful.
A Disease of Misrule
PHPT arises because the parathyroid glands produce their hormone – parathyroid hormone (PTH) in excess of need and out of harmony with the mineral system within which PTH is the central regulator.
One could say through the actions of PTH the parathyroid glands rule the calcium kingdom, so powerful are its effects. And like the ruler of a well structured nation they are, in turn, held in check as were the ruling kings and queen of England by their royal subjects and their parliament.
But like those rulers of an earlier time might take to rampage that imperils their very kingdom, against which no force prevails to bring them back into the proper order of their world, like that is this disease. And as what only revolution – even regicide – could cure, so comes the surgeon in this case, to do that very deed.
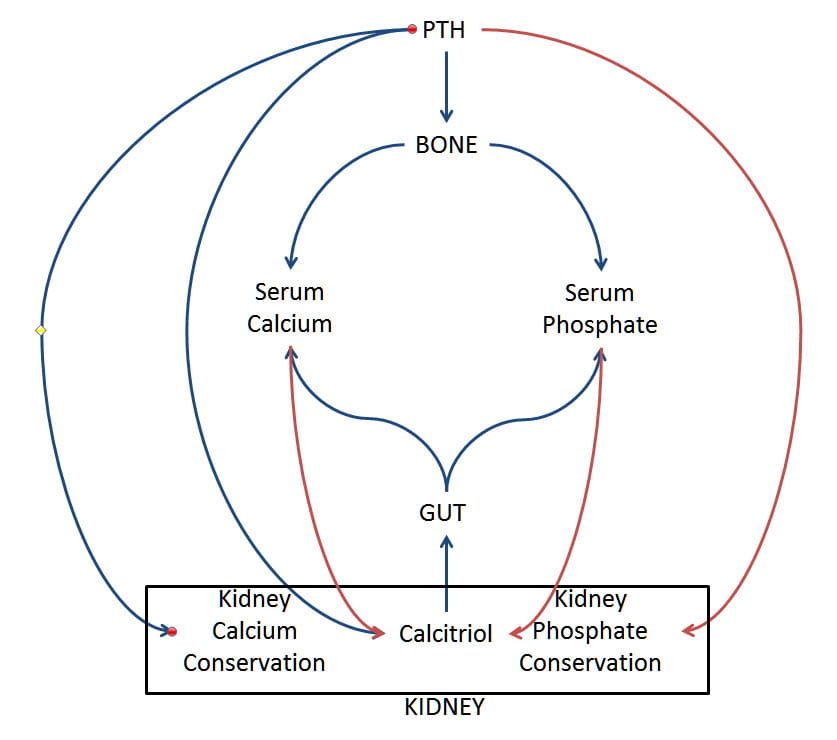 Now, let me tell about the agent of this ruler, the imperial hormone, PTH, principle among peers. I have drawn a simple picture of its rule. See where it stands – above the rest, prime, enacting the will of the crown royal.
Now, let me tell about the agent of this ruler, the imperial hormone, PTH, principle among peers. I have drawn a simple picture of its rule. See where it stands – above the rest, prime, enacting the will of the crown royal.
Kidney and GUT
Look first at calcitriol, active vitamin D, at the bottom in the kidney rectangle. PTH orders kidney cells to increase calcitriol production – blue lines mean stimulation. Calcitriol in turn signals gut cells to absorb more calcium and phosphate from food. So through calcitriol, PTH raises the amount of both minerals entering the blood which would tend to raise their concentrations.
Bone
PTH does the same for bone. It causes bone cells to break down its calcium phosphate mineral phase so that extra calcium and phosphate enter the blood. The red line means bone mineral goes negative – is lost.
Opposing Actions on Ca and Phos
Calcium
To raise serum calcium more, PTH signals kidneys cells to conserve calcium. Remember, calcium is filtered out of blood in large amounts, but only 1% to perhaps 7% of what is filtered escapes into the urine – the rest is reclaimed back into the blood.
Phosphate
But unlike for calcium, PTH signals kidney cells to lower the fraction of filtered phosphate reclaimed back into blood. So serum phosphate is under opposing influences: More comes in from food and bone, kidneys conserve less. Serum phosphate level falls.
Why should it fall when the flow of phosphate in from food and bone increases? Why don’t the two effects balance out the third?
It is like the milldam. Let the stream run as it will, yet the dam adjusts the height of the pool behind – upstream of it. Lower the dam, and as soon as the pool empties down to the new dam level the flow downstream – urine phosphate losses here – is what it was when the dam was higher. Even if the stream flow is increased – more phosphate in from food and bone, the height of the pool remains low because the dam is set low. No flow can keep the pool above the dam for very long.
A Disordered Kingdom
Think of it. The serum calcium, over favored, so to speak, too high. And serum phosphate, normally calcium’s equal, now too low. All out of balance. Both of them move in excess through the body. Into blood from bone and in from food. And both go out through the kidney narrows, those long thin nephron tubes that on their way through they put in jeopardy. Being both in excess, how can calcium and phosphate fail to crystallize from time to time and block the tubules or form the stones we write about?
Feedback Loops
I said through this hormone, like the monarch of well run kingdom, the parathyroid glands rule within the check and balances of watchful peers and parliaments. Call them feedback loops, if you like.
Of them I illustrate only three.
Serum Calcium on PTH
Foremost, serum calcium controls PTH secretion through the calcium sensing receptor on the surfaces of parathyroid cells. LIke – if I might once again harken back to an earlier time, king and archbishop, the serum calcium controls and is controlled by the parathyroid glands. Calcium acts directly on the gland whereas PTH acts to influence serum calcium indirectly through reordering the actions of kidney, gut, and bone as I showed in my drawing.
Serum PTH, Calcium, and Phosphate on Calcitriol
Serum calcium and serum phosphate both suppress kidney production of calcitriol – red lines from them to calcitriol. So as serum calcium rises it reduces calcitriol production. But fall of serum phosphate further stimulates calcitriol production by taking its foot off the brake. Since PTH and low serum phosphate stimulate calcitriol production and only higher serum calcium offsets them, it is two to one: the net effect is that it rises.
Calcitriol on PTH
In the full article, I point out that calcitriol itself suppresses PTH. Calcitriol increases expression of the calcium receptor gene so the abundance of the receptor increases; this makes any calcium signal stronger by virtue of there being more signallers. That effect lowers PTH secretion by the glands for any given serum calcium level. Calcitriol inhibits the expression of the genes for the precursor molecule of PTH – pre pro PTH. This acts in concert with the signaller effect.
Failure in PHPT
But in PHPT the parathyroid glands produce PTH outside of normal regulation. They make too much hormone whatever the serum calcium or calcitriol. What should be an elaborate conversation turns into a lecture: PTH production rises and drives the system out of the normal bounds causing disease.
What Makes the Glands Rampage
They grow.
Just as learned historians peer into distant times seeking the inner causes of misrule so do scientists into the genes and interior behaviors of the glands. And there they find the many reasons that explain why the glands should throw off their obligations and pursue the expansion of their own powers to the general deterioration of their domain – bone disease, stone disease, damage from high calcium to vessels, to brain function, stomach acid production, pancreatic function.
Main Abnormalities Produced by PHPT
When we come upon it, PHPT has already progressed to that kind of deterioration. Serum and urine are abnormal. But taken one by one, almost all of the abnormalities could have other causes. It is the pattern of those abnormalities that allows us to diagnose PHPT as their cause. And because the cure is surgery, to recognize that pattern and shun false diagnoses is for all physicians an imperial responsibility.
Hypercalciuria
PHPT raises urine calcium, a lot because extra calcium is absorbed from food and liberated from bone. That alone probably accounts for the kidney stones. But as a group, calcium stone formers also excrete more calcium in their urine than would a group of otherwise unselected men and women without stones, and that extra calcium arises from idiopathic hypercalciuria (IH).
So, just a high urine calcium need not mean PHPT – in fact in most cases it is due to IH.
Low Serum Phosphate
We just spoke about the low milldam and the stream. More phosphate flows through from food and bone into the urine but PTH has lowered the dam. So PHPT lowers serum phosphate.
But low serum phosphate occurs in many kidney stone formers. Some have IH and therefore high urine calcium and low serum phosphate.
Low serum phosphate, therefore, even with a high urine calcium need mean nothing more than IH and certainly does not diagnose PHPT.
High Serum (or plasma) PTH
Should one even measure PTH in a routine calcium kidney stone former? I do not.
But say you did, or your physician did, and the value exceeds normal. Low calcium diet can raise PTH, so can low vitamin D. Even the most modest reduction of kidney function, a level common among older people, raises PTH despite adequate calcium intake and vitamin D. Some say IH raises it, sometimes.
High serum PTH by itself, and even with high urine calcium and low serum phosphate do not diagnose PHPT.
Reduced Bone Mineral or Nephrocalcinosis
PHPT reduces bone mineral but so does low calcium diet, especially in IH. Even all of hypercalciuria, and low serum phosphate, and high PTH and low bone mineral density together, even this fourfold complex is not PHPT all by itself.
The same for nephrocalcinosis. An antique term of art suitable for an earlier period in medical history, multiple kidney calcifications in no way adds to the diagnosis of PHPT.
High Serum Calcium
Here – the talisman, the very make and mark of PHPT – this one finding sets PHPT apart from all the rest.
PHPT Raises Serum Calcium Three Ways
When the parathyroid glands themselves produce PTH in excess, not in response to something else but on their own accord, by themselves so to speak, the hormone directly or indirectly raises kidney calcium retention, bone mineral loss, and intestinal calcium absorption – all three together.
Serum calcium rises as the water pool behind a rising dam, and here the stream flows with more abundance – from bone and food. So the urine calcium is high even though calcium retention by the kidney is high: The dam wall is higher and the stream is flowing faster, too.
High Serum Calcium Cannot Force PTH Below Normal
The PTH level itself if in the normal range is too high. That normal range is for a normal serum calcium.
Remember, the primary controller of PTH is serum calcium. If low calcium diet or vitamin D deficiency lowers serum calcium even slightly, PTH will rise to correct it back. If serum calcium should rise from, as an example, very high vitamin D intake or very high calcium intake, serum PTH will fall to correct it. So the high serum calcium, were it primary – something on its own – would suppress PTH to its lowest level.
Therefore, a high serum calcium without suppressed PTH means it is the glands themselves that are raising PTH – that is PHPT.
The Diagnosis of PHPT
Thus it is, the diagnosis rests on an elevated serum calcium and a PTH level either in or above the normal range – not low.
The Urine Calcium Must Be Not Low.
There is a genetic defect of PTH regulation, not rare, in which serum calcium is high, PTH normal or even high, but urine calcium very low. That defect, familial hypocalciuric hypercalcemia, runs in families and one must pass it by for it needs no treatment. Stones, if present, have some other cause.
It may be that bone mineral is low, or kidneys have many stones or calcifications in them, or serum phosphate is low, or all or none, and still the prime combination of high serum calcium, and not suppressed PTH with adequate – not low – urine calcium is almost enough.
I say almost because there are four more steps.
No Drug or Disease Causes The Abnormalities
Thiazide Diuretics
Because these drugs lower urine calcium and prevent calcium stones, many patients take them. They raise blood calcium levels perhaps because they enhance renal calcium conservation – raise the milldam. A patient with idiopathic hypercalciuria taking a thiazide diuretic and who still excretes even a normal amount of calcium will seem to have PHPT because serum PTH levels will be normal and urine calcium not abnormally low.
Every physician knows this, but every stone patient needs to know it, too. Physicians may not know what their patients took when blood was drawn. Although in almost every case they will discover the drug as culprit, time and money get wasted for no reason. As a safe interval, one should stop the drug a week before drawing blood for the initial evaluation of any patient.
But what about follow up evaluations? Stopping the drug a week before won’t work. We want to know how well treatment has controlled urine calcium. So 24 hour urine and blood testing must coincide with drug use.
PHPT may appear during treatment and manifest as a rising serum calcium level, but thiazide can make it seem as if that has happened. What can we do?
The secret: tolerate slight increase of serum calcium. If seemingly too high too often, or rising over time, then stop the drug for a week and re-measure.
Lithium
This ion, used for bipolar disorders, reprises the physiology of PHPT: high serum calcium and not suppressed PTH. But urine calcium has generally been low – as in familial hypercalcemia. Case reports document PHPT in some patients long after the drug has been stopped. Though not a likely cause of stones, lithium can cause massive confusion during evaluation of stone formers.
Hyperthyroidism
Whether primary or from excessive thyroid hormone replacement, states of systemic hyperthyroidism can include high serum calcium. PTH levels tend toward the low or even suppressed side. Be sure about thyroid status when evaluating for PHPT.
Low PTH Conditions
High serum calcium with low PTH – suppressed below normal – do not concern us here. Some stone forming states like sarcoidosis, and CYP24 deficiency cause this, as do malignancies and other disorders.
Normocalcemic Primary Hyperparathyroidism
Does It Exist?
Given all I have said and the many factors that can raise PTH levels apart from PHPT, this diagnosis never fails to baffle and almost amuse me. Of course we can see normal serum calcium with increased PTH in low calcium diet or vitamin D intake, and any level of reduced kidney function. Just being older makes exclusion of mild kidney function loss difficult indeed.
Even so, some people do have high PTH for no apparent reason, and every one of us has a few cases that went on to raise their serum calcium levels. The big article links to long reviews of this topic by respected authorities who say more or less what I have just said, but say it better.
What Do We Do?
Who are these people and what do they look like?
They look like IH with elevated serum PTH levels.
I see no approach but to treat them like IH and wait. If they indeed have an early parathyroid disorder they will gradually raise their serum calcium levels and warrant surgery. Surgery in advance seems folly to me. What if the problem were indeed diet or slight kidney function reduction?
Everyone I write for here has calcium stones, so treatment must be done. That leaves surgery or medical treatment directed at IH. I cannot but favor the latter, and watch carefully along the way.
Treatment of PHPT
My job is to establish the diagnosis. After that, the surgeon does the rest.
That means I do not require the surgery to confirm my diagnosis. I need to know beforehand.
In case the surgery finds not abnormal glands, it means the surgery failed – the disease is present still. If abnormal glands are found and their removal cures the abnormalities, well and good, but the original diagnosis should not require such surgical confirmation.
I mean by this, that if you do as I have said, the diagnosis can be made with surety and surgeons sent on their difficult tasks with confidence. They will do scans, and if the scans find abnormal glands or not should make no difference if I have done my work properly. Likewise for their surgery.
The corollary: Much like carpentry – measure twice, cut once.
Parathyroid surgery is a highly technical procedure, and not all neck surgeons choose to perform it. A valuable resource for university based endocrine surgeons is this site listing surgeons who belong to the American Association of Endocrine Surgeons. This society is noncommercial and I feel free to recommend it as a resource from this university site.
Other Apex Articles Related to this one:
Five Steps to Stone Prevention


I have thyroid disease and kidney stones. This may be the answer I have been looking for my whole life.
Hi Deanne, Do you mean hyperparathyroidism? It is not part of thyroid disease. Stones can occur with hyperthyroidism, either spontaneous or from excessive thyroid hormone. If you have had stones, be sure to follow an orderly approach – as in the article. Here is a broader one to think about. Regards, Fred Coe
Hello Dr. Coe,
I am a 41 yr old female. I have made several calcium kidney stones and have had 3 surgeries to remove, I am waiting on a date for my 4th surgery. After completing a 24 urine collection and blood analysis, ultrasounds and xrays, I have been diagnosed with Medullary Sponge kidney disease.
I also have hypothyroidism since I was 12, but tests for parathyroidism are normal. I have vitamin D deficiency.
I have higher levels of calcium and lower levels of sodium in my urine.
Most days the pain is unbearable.
Is there any further insight that you could give or direct me to for the Medullary Sponge kidney disease? I have reading many of your articles and find them very helpful informative. Any reply would be appreciated…thank you!
Hi Darlene, Medullary sponge kidney cannot be reliably diagnosed except during stone removal surgery or by CT with contrast infusion, so perhaps all you have is multiple renal calcium deposits or stones. Ask your surgeon if he/she actually saw the sponges during surgery to be sure the diagnosis is not simply from a radiologist. Also, MSK patients usually form calcium oxalate stones; are your stones perhaps calcium phosphate? For treatment, you want the same exact as for idiopathic calcium stones but if it is MSK you want the highest possible fluids, and the lowest possible sodium – below 1500 mg daily. Take a look at the treatment approach. Regards, Fred Coe
Hello Dr. Coe,
Very informative, I enjoy reading your work. I’ve been searching for an answer for a long time, would love to hear your opinion. I’ve been forming stones for over 25 years now, started very young, no doctor can tell me why. Sometimes urine calcium is high, sometimes normal. Serum calcium is always normal, PTH has been high just 2 or 3 times, vitamin D is only borderline low or low normal. Stone analysis shows calcium phosphate carbonate, sometimes calcium oxalate. Could I have HPT? I would love an answer after all these years, especially given my long list of symptoms. No one has been able to put the puzzle pieces together for me. Would love to hear your thoughts. Best to you.
Hi Lauren, given a variable high urine calcium and PTH, everything hinges on the blood calcium level. You need to have it measured fasting, off any medications than can affect it – thiazide diuretics, calcium supplements, lithium – and see if values are all normal. If they are then the high urine calcium is probably idiopathic hypercalciuria, a common stone cause easily treated given patience and finesse. The fact of phosphate/oxalate stones does not much help, only the serum calcium – but do it as I said. Regards, Fred Coe
Dr. Coe,
I very much appreciate your reply. I’ve never been on medications so I think it’s safe to assume that my serum calcium is indeed normal and HPT not to blame. Thank you for your time and input. Best to you.
Dear Prof. Coe,
Your articles are a godsend.
I have normal blood calcium levels, normal 24h urine calcium levels.
Low citrate and generally high urine PH. Good flow.
Recently I was tested for PTH and they found it was high. 11.45 pmol/l.
My Vitamin D is on the low side of normal. I am mixed race.
Formed two stones last year both calcium oxalate. So far no others.
All other blood and urine tests are unremarkable.
I do get some symptoms which I know now can be associated with high PTH (and have been for a few years).
What should I push for as far as testing, scans etc…?
Many thanks!
Ray
Hi Ray, High PTH is either with high blood calcium or not. Are your normal serum calcium levels normal or high normal? High normal may be high as labs are not all alike and standards vary a lot. If your actual level is near 10 mg/dl – 2.5 mmol/l – I would be suspicious of primary hyperparathyroidism. If they are safely below this, then you probably just have secondary hyperparathyroidism from low calcium diet, low vitamin D or both. The normal urine calcium is also an issue – what is normal in the lab you frequent? For stones, over 200 mg/d of calcium begins to confer risk. See what you and your physicians make of this. Regards, Fred Coe
Thanks.
My calcium levels are:
2.36mmol and 2.32 adjusted and all historical values for past years have been pretty much identical.
My vitamin D is 77nmol, bit higher than normal as I’ve been out in the sun more recently.
Urine calcium is 1.63mmol but no range given.
Urine calcium 24h is 4.73mmol (lab range 2.5 to 7.5)
Urine phosphate for 24h is 33mmol.
These are based on 2.9L of urine.
Being lactose intolerant I only eat a little bit of cheese daily, vegetables for calcium but get nowhere near the recommended 1g.
I would really wish to avoid the condition to deteriorate as I’m 30 years old and don’t want to form any more stones or feel tired for no reason.
Many thanks for all your help.
If I don’t find any satisfaction can I look into seeing you with all the information I have , I’m sure you’d be able to solve the puzzle?
Best regards
Ray
Hi Ray, The blood calcium seems normal, the urine calcium not remarkable – risk is known to increase at about 5 mmol/d; the urine volume is plenty high. So, why did you form stones? Usually there are reasons not evident only from labs, reasons not always evident at first pass. Regards, Fred Coe
Dear Prof. Coe,
These are the possible reasons:
In all honesty, I was not drinking anywhere near enough, I wouldn’t get thirsty easily.
I also train a lot, so lost a substantial amount through sweat.
My diet was maybe a bit higher in oxalate than it is now.
My citrate is low, I forgot to mention. 0.5mmol/24hr (range 0.6 – 4.8)
I’m now taking potassium and magnesium citrate combination.
Also, my specific gravity is consistently around 1.015 and urine PH is around 6 to 6.5
even before the citrate supplements.
It’s the PTH levels that concern me however, could they be linked to
lower than optimal vit. D levels? (77nmol) I’m mixed race and my dad was found
to have some vit. D related metabolic issues many years ago.
Thanks
Ray
Hi Ray, Certainly low urine volume raises stone formation risk. Likewise, reduced urine citrate. The higher urine pH values can increase calcium phosphate stone risk but not calcium oxalate stone risk. High serum PTH with normal serum calcium is usually low diet calcium, low vitamin D or both. It is never treated surgically. Regards, Fred Coe
Thank you so much for the priceless info.
It’s reassuring.
Best Regards
Ray
My PTH levels have returned to normal by the way 6.6pmol/l and calcium 2.3mmol
Vitamin d dropped to 55nmol, all these values were when fasting . Thanks regards ray
Dear Dr. Coe, I can’t thank you enough for explaining this very complex topic. Thanks to you, I believe I now understand the general mechanics of primary hyperparathyroidism. Would you kindly help me to understand how to apply this when there is variability in the serum CA lab values? I am a 55 year old female with a history of kidney stones, severe osteoporosis and subacute thyroiditis which left me hypothyroid and taking synthroid since 2003. I am very concerned about the osteoporosis because my doctor told me last year due to the rate of my bone loss that my bones would collapse on my organs and I would not be able to breathe by the time I am 64. I am allergic to bisphosphonates but have no fractures.
Here are some lab values:
11/26/2014 – CA 10.2
10/7/2015 – CA 9.8
3/31/2016 – CA 9.3, PTH 47, Vit D 55
4/21/2016 – CA 9.5, Ionized calcium 1.24, Urine calcium 284
5/8/2016 – Started Chlorthalidone Thiazide diuretic
6/23/2016 – CA 10.0, Urine calcium 246
7/8/2016 – CA 10.0
12/16/2016 – CA 9.7, Vit D 44
10/5/2017 – CA 9.9, Ionized calcium 1.23, PTH 38, Urine calcium 211
10/20/2017 – Urine calcium 190
1/7/2018 – Started Raloxifene
4/12/2018 – CA 10.4, Vit D 43, Urine calcium 193
8/9/2018 – CA 9.9, Ionized calcium 1.21, PTH 37, Vit D 47
I drink a ton of water since my first kidney stone in 2003 so my urine volume is always flagged as generous, usually 2500-2900 ml against a reference range of 600-1600 ml. Can you help me to understand if my osteoporosis and stones could be caused by hyperparathyroidism? Many thanks for your help, I am very grateful to you. – Cori
Hi Cori, Here is the problem – what is your serum calcium? Chlorthalidone raises serum calcium so values after taking it are suspect. Food raises it so all values must be fasting. To my eye your serum calcium is not elevated making PHPT not a viable diagnosis and leaving common genetic hypercalciuria as the problem. That can cause bone disease as can simple low calcium diet and menopause. If any doubt, you can stop the chlorthalidone, wait for 3 weeks, then get several fasting bloods with serum PTH – I think they will be normal in calcium and PTH. If your bone disease is so severe, your physicians may want to consider more focused bone drugs – PTH or newer agents – this becomes very technical. If your bones are still intact but mineral loss rate is high, high calcium very low sodium diet is a possibility. Regards, Fred Coe
Dear Dr. Coe, Thank you so much for taking the time to review my information and for the advice. I really appreciate your thoughts on the viability of hyperparathyroidism. I read your article on the high calcium/low sodium diet and it certainly seems to be the only clear path to positive bone mineralization. I checked my 24 H urine test results but didn’t see any values for sodium. I will request this test as none of my doctors have mentioned the connection between bone mineral loss and sodium intake before. I don’t think I use a lot of salt but my blood pressure tends to be low so I never really thought about it much. You are so kind to reach out to others and share your fantastic knowledge, and I love the imagery you use to explain these difficult topics. With my best wishes, Cori
Dear Dr. Coe
I am 68 years old retired male.
From time to time, since the age 22, I had kidney stones.
History of stone episodes
1972 – AGE 22 > Passed 2 stones (Flush out)
1983 – AGE 33 > 1 Stone removed by ESWL
2010 – AGE 60 > 1 Stone removed by Ureteroscope & Passed 1 stone (Flush out)
2016 – AGE 66 > Passed 1 stones (Flush out)
I visited Dr YYY for periodical check last year and he suggested that I should go for Litho Link kidney stone test. 04 September 2018 test result > PTH intact 79 / Calcium 10.3
During my yearly check up blood test on 27 December 2018, Dr XXX asked for PTH/Calcium testing. Result > PTH intact 106 / Calcium 10.1
Previously, I had Calcium as 10 on 18 December 2017 and 8.8 on March 2018.
My PTH/Ca indicates that I have Normocalcemic Hyperparathyroidism.
My Vitamin D in blood is LOW.
What do you suggest?
Hi Teo, Your blood calcium is rather high on several occasions, your PTH quite high. Here is how I would approach things. First, bring your vitamin D up to normal. WHen it is normal, get at least three fasting morning bloods for calcium and PTH – in the same sample, and a 24 hour urine – or even two – to determine urine calcium when your vitamin D level is in the normal range. PHPT is high blood calcium + normal or high PTH + urine calcium not low. You cannot make sense of things when you are vitamin D depleted. Likewise, if the bloods are not fasting and in the morning. Normocalcemic hyperparathyroidism is always secondary to something else; primary hyperparathyroidism is always hypercalcemic – often just a bit so. Regards, Fred Coe
Dear Dr. Coe,
I am writing on the advice of Jill Harris whose KSD class I am taking. She thought you might be interested in and/or have insight into my situation which has so far stymied urologist, nephrologist and, currently, endocrinologist. About 5 years ago I had a UTI out of the blue. Then in May and June of 2017 I was in ER for pyelonephritis, the second time with stones blocking at kidney to bladder on one side, bladder to ureter on the other. Stones were removed and found to be CaOx. Since then I have had at least two more stones, one needing removal by urologist and have UTIs every 2-3 months. 48 hrs of urine test in June 2019 showed extreme hypercalciuria ( 655, 742), mild hyperuricosuria (0.806) one day, mild – high CaP (1.57, 2.64), and borderline high pH one day (6.435). Ox levels were 29 and 26. My PTH tested later in June was 17 with Caat 10.3, ionized Ca of 5.6. Ca levels for past couple of years have been borderline high. Ionized Ca done in Sept was 5.8, Ca was 10.1, PTHrP normal. Vitamin D 25 in August was 14, calcitriol 51.9. My TSH has been normal over three years of testing. Alkaline Phosphatase levels low or near low over several years. I am prediabetic (c. 10 years since discovered) and on metformin (500mg 3x a day) and take fenofibrate for high triglycerides. My highest HbA1C was 6.1, but is usually 5.4-5.7. I am 58 and overweight but not obese. My kidney function when I am not dealing with a stone or UTI is normal. I am scheduled for a thyroid ultrasound next month to check on enlarged thyroid with at least one nodule, discovered incidentally on MRI of shoulder. Other lab work seems to rule out sarcoidosis. Bone scan shows mild osteopenia with signifying numbers in hip rather than wrist. I am aware that thyroid cancer could be present with normal TSH but be making calcium regulation wonky. Neuroendocrine tumor has not been completely ruled out. I have has ultrasound which was normal other than showing fatty liver. Colonoscopy and mammogram were fine other than two tiny polyps. I have been struggling with vocal instability and hoarseness since last May and am now on PPI for LP reflux. I am interested in your thoughts. Have you encountered anything similar in the past? How would I proceed beyond what I am currently pursuing? Thank you.
Hi Debra, All of my attention is on the very high urine calcium and high serum calcium + ample 1,25D. Sarcoidosis is possible, but given the very suppressed serum PTH your physicians might consider a CYP24a1 deficiency – genetic varient as cause. Alternatively, serum PTH is very unstable, so the value measured may have been in error. If you were my patient I would stop any medications that could possibly alter serum calcium or plasma PTH, and draw a blood, fasting, between 7 and 9 am for calcium and PTH on three separate days. This will settle matters as to both measurements and one can get on with treatment. That is of course a distant opinion, and only your own physicians are responsible. Regards, Fred Coe
Dear Dr. Coe,
I had actually thought the CYP24a1 deficiency was not a possibility since my D 25 is very low (only 14). What medications can can alter serum calcium or plasma PTH? I was not on pantoprazole, vitamin D3 or methenamine hippurate when first labs were done but now am. Other meds I am taking are metformin, fenofibrate, Lyrica, magnesium, B6, Boswellia, topical steroids, topical Voltaren, fluticasone nasal spray, albuterol inhaler, and Claritin. Would any of these need to be stopped prior to testing and, if so, for how long?
Thank you,
Debra
Hi Debra, if you mean your routine serum vitamin D, that is not an important consideration. What is high is the active form of vitamin D, 1,25 dihydroxy vitamin D. Your list of meds seems rather benign to me, but your physician should check the appropriate references to be sure that none can alter serum calcium. Regards, Fred Coe
Thank you. I will run these thoughts by my nephrologist and endocrinologist. I am also having thyroid nodule (1 of 6 in multinodular goiter) biopsied soon. Have you any experience of thyroid issues causing calcium issues?
This from one of many studies I have read is why I did not think the gene mutation to be a likely fit for me: “A typical biochemistry profile was found within this phenotype group, with normal/high serum calcium levels, suppressed parathyroid hormone, high levels of active vitamin D metabolites (25-hydroxyvitamin D3 and 1,25-dihydroxyvitamin D3) and low levels of inactivated vitamin D (24,25-dihydroxyvitamin D3)”
My 25-hydroxy is low (14) and 1,25 dihydroxy mid range (51.9 on ref of 19.9-79.3). Do you disagree with this author? I welcome your input and hope your Thanksgiving is/was healthy and happy!
Hi Debra, I do not think I realized you were giving me a 1,25D level. Yours is mid range, but of course your serum PTH is suppressed and PTH stimulates 1,25 D production, and you are 25D deficient. From here I am not in a position to tell, but if your get all of the hormones as noted your physicians may be able to sort things out. Dr Raj Kumar, at Mayo, is perhaps the most expert person on this topic as he was among the first to recognize the problem. He is a good friend of mine. You might want to write to him, or even see him. He has all of the requisite genetic testing available and is very smart. Regards, Fred Coe
Thank you very much. Mayo is out of range for my very limited insurance, if nothing works out here in NY, I may end up at least writing to him.
Dear Dr. Coe,
These are my latest lab results. On your earlier advice I made sure the blood work was fasting and between 7 and 9 am.
Creatinine was 1.05
eGFR 59
Calcium 9.9
Albumin 4.4
Alkaline phosphate 35
AST 66
ALT 118
Calcitriol 48.6
D 25-hydroxy 34.9 (on 1000 IU/day supplement)
No PTH was ordered.
24 hr urine done three days later showed calcium at 725 and creatinine 1559.
I see endocrinologist later this month. I appreciate any further guidance you have based on recent (Dec 20, 23) labs.
Thank you,
Debra
Hi Debra, Your blood calcium is normal, so the very high urine calcium is not from primary hyperparathyroidism. Your calcitriol is not exceptionally high either. I am sorry no PTH was ordered as some past value(s) were reported as low. A CYP24a1 disorder still seems not unlikely to me. In NY Dr David Goldfarb is very expert and perhaps he can be of help. You have an unusual condition and need expert help. Regards, Fred Coe
Dear Dr. Coe,
Thank you again. When I see the endocrinologist this week I will share your replies and see if she will order additional vitamin D with PTH and calcium levels to see if PTH is still suppressed. If she will not I will try my urologist in Feb our local nephrologist in March. Doctors here are limited, so visits are usually every three months at most.
Your response has given me hope about my scheduled June visit with Dr. Goldfarb.
My previous reply was submitted in the wrong place…
Dear Dr. Coe,
I was missing a page of my lab report from Dec. 20.
PTH was tested (fasting between 7 and 9 am) and was 24.
That was with the other labs cited in my earlier post:
Calcitriol 48.6
D 25-hydroxy 34.9 (on 1000 IU/day supplemeant)
Ionized calcium was 5.3
Calcium 9.9
Urine calcium three days later 725
This may now look more like idiopathic hypercalciuria that could be safely treated with diuretic? Perhaps previous hypercalcemia was due to insufficient vitamin D?
Thank you..
Hi Debra, I guess you mean that your PTH is not suppressed and your 1,25D (calcitriol) level is not very high. Your situation is subtle, however. PTH has been lowish, whereas in IH PTH levels are midrange despite high calcitriol levels. So something is altering the poise of PTH calcitriol balance. The most likely cause is a genetic increase in your 1,25D receptor, something accessible only in a research setting. Lowish PTH will reduce absorption in the more distal parts of your nephrons (distal convoluted tubules, for your physicians) so that the fraction of calcium delivered there that is excreted in the urine will be high. The lowest possible diet sodium intake would be expressly valuable for you, perhaps as low as 30 – 40 mEq/day, or 1200 mg of sodium, as that will reduce delivery. Thiazide would be used in a very low dose on top of that diet, but the diet would be first. It may just do it for you. Serum calcium may rise slightly, raising the spectre of primary hyperparathyroidism, as I have seen that happen. You are a very unusual patient. If you were in our area of the country, and were willing, you would be a reasonable candidate for our NIH research study, that unusual. But I would hope that what I have mentioned might help your physicians who are indeed utterly responsible for your care. Regards, Fred Coe
Dear Dr. Coe,
I very much appreciate your responses and am showing them to my local endocrinologist and nephrologist who also appreciate them! Thanks to Jill, I have already lowered my sodium intake to, and at times below, 1200 mg daily. The last 24 urine calcium of 725 was while doing that. Since then I have been better about also eliminating added sugars, esp since my HbA1c edged back up (5.7).
I am wondering if my serum calcium returned to normal because my vitamin D is now in range. I did read one paper suggesting that deficiency can cause hypercalcemia (https://www.mdedge.com/clinicianreviews/article/72368/endocrinology/hypercalcemia-common-yet-challenging), but my endocrinologist is not sure that is likely. I guess the next months/years of labs will tell if it rises again.
I am very interested in medical research and would love to help further things in this area. Are there ways to participate in your study from a distance through doctors more local (possibly Dr. Goldfarb in NYC whom I see in June)?
Again, I appreciate the detailed responses. I am sure they will be helpful in pointing my doctors toward things that may be of help.
Sincerely,
Deb
Hi Debra, Low 25D will lower serum calcium and raise PTH. One possible maneuver would be to begin fosamax or another bisphosphonate, which will reduce bone mineral loss. That might much reduce urine calcium and also give a clue as to the amount of urine calcium arising from bone. Another matter is your diabetes. It can raise urine calcium remarkably, and we also did not mention your menopausal /or not status. Rapidly progressive bone mineral loss can occur during or near menopause and lead to what you have. Regards, Fred Coe
Dear Dr. Coe,
I have never had an HbA1c higher than 6.1 and no diabetic level fasting or daily glucose readings. I hover between normal and pre-diabetic. I did discover the hyperglycemia due to losing feeling in both feet more than 10 years ago. I am postmenopausal as of October 2013. AS far as I know the first UTI was in 2014, first stones in 2017. I did wonder if menopause might be a factor.
Thank you,
Debra
Hi Debra, we know that blood glucose runs high in people with idiopathic hypercalciuria but have not as yet published the fact. I would suspect you are an example, and not diabetic. But that is a complex matter, in that most of the IH have lower HbA1c than 6. Regards, Fred Coe
Dear Dr. Coe,
I neglected to add that nephrologist would not treat the hypercalciuria due to borderline high serum calcium. Endocrinologist started me on 1000 units of vitamin D daily. I do repeat of most labs and a non Litholink 🙁 24 hr urine test for her next to see what may change.
Hi Debra, I noted my suggestions below. Fred
Dear Dr. Coe,
I was missing a page of my lab report from Dec.
PTH was tested (fasting between 7 and 9 am) and was 24.
That was with the other labs cited in my earlier post:
Calcitriol 48.6
D 25-hydroxy 34.9 (on 1000 IU/day supplemeant)
Ionized calcium was 5.3
Calcium 9.9
Urine calcium three days later 725
This may now look more like idiopathic hypercalciuria that could be safely treated with diuretic? Perhaps previous hypercalcemia was due to insufficient vitamin D?
Thank you..
Dr. Coe –
Thank you for this information. I would appreciate your input.
At my last checkup in Oct, 2019, my Calcium was 10.4, Vit D 19.1 (fasting). I was sent back for a PTH and this was normal (can’t remember the reading) so nothing further was done. I’ve always had a low Vit D but this was the first time my Calcium was elevated. At 53 years of age, I am sitting here waiting for my first ever kidney stone to pass. I feel this all must be related. The ER doctor recommended I follow up with the urologist to have the stone content evaluated.
What are your thoughts?
Thank you!
Hi Cheryl, I would suggest your physicians might want to obtain several serums for calcium and PTH fasting, between 7 and 9 am; those are the conditions under which normal serum calcium values were obtained. As well, the low vitamin D needs to be corrected no normal before measurements as low vitamin D levels can mask hyperparathyroidism. If serum calcium values are above normal fasting and PTH is not suppressed and urine calcium is not low, you have the diagnosis – as in the article. You may have it as stones have begun a bit late in life. Regards, Fred Coe
Dr. Coe,
Given that hypercalcemia (or should should I say ionized hypercalcemia as ultimately it’s the unbound, free fraction that binds to the CaSR) should result in a suppressed PTH, isn’t it reasonable to pursue PTH testing in patients on a thiazide who develop hypercalcemia? I’m asking as your writing above would suggest to stop the thiazide and recheck calcium.
My thought is that if the calcium reasborption increases due to the thiazide, the serum calcium should not elevate unless there is disordered activity of PTH or active vitamin D. Now, perhaps the ionized calcium doesn’t elevate and the total serum calcium simply reflects more calcium relative to water (the latter lost through the action of the thiazide). I guess another possibility is that the often-seen metabolic alkalosis associated with the use of a thiazide could reduce the free calcium concentration and this could provide impetus for a PTH release.
I’m interested in your perspective on this…thanks.
Hi Stephen, Thiazide lowers FE Ca and PTH. Serum calcium rises bu 0.03 (0.008, 0.052) mmol in the fed state but only 0.02 (-0.03, 0.08) NS, fasting. Serum calcium comes under several influences – higher tubule calcium reabsorption (FE Calcium fasting -1.2 (-2.1, -0.2) and fed -0.7 (-1.2, -0.3)), which raises it, and lower PTH (presumably from the higher serum calcium) which would reduce it via reduced GI absorption via reduced 1,25D activation, and via reduced PTH mediated bone mineral turnover. Indeed PTH falls fasting -5.4 (-10.6, -0.069) and fed -3.5 (-5.6, -1.3). I have to assume higher calcium reabsorption increases serum calcium which then readjusts via suppression of PTH over time – our experiment was 6 months: control then 6 months of CTD. PTH and serum calcium remained in the normal range. Primary HPT is a primary upregulation of PTH so I would presume the rise in serum calcium would be greater with thiazide, but normal ranges are not well established, and would depend on a lot of factors, like diet sodium etc. I am much happier using normal ranges for serum calcium fasting – given all the problems with it – and PTH just being in the normal region or high. Ionized calcium is ideal but I used to run them, and sample handling is a big deal: quality of the blood draw – these are venous with halted circulation during puncture -, for example. It is easy and cheaper to just measure a lot of fasting AM bloods for calcium and PTH, though I have not run any cost benefit experiments. As for alkalosis from thiazide increased PT reabsorption and from potassium depletion, it will certainly lower ionic calcium as a fraction of total calcium, another problem. For all these reasons I avoid sampling on thiazide. Thanks for such a good question! Fred
Dr Coe; I sent a similar question a week or so ago but it must have not gone thru. Anyway, I am concerned I may have PHPT. A recent serum calcium (not fasting) was 10.0. (was also 10.0 with the same test two years ago). Parathyroid hormone level was 20pg/ml. 24 hour urine calcium was 340. Potassium 46, Phosphorus 663, Citrate 556, Oxylate,U 0.31mmol/24hr, Oxylate, mg/24hr 27.3, Calcium Oxylate crystal 2.42DG. First stone was at age 60, and since then they have formed more frequently. I’ve had three stone removal surgeries in the past 8 years and a recent scan shows four new ones. I had been drinking nearly 2 liters of water but no citrate for the past two years, so of course stones proliferated. A website for The Norman Parathyroid Center in Tampa says if serum calcium is 10 or higher for someone in their 60s, and first onset of kidney stones is in their 60s, with high urine calcium, there is a 90% chance they have Hyperparathyroidism. I realize they are surgeons and surgeons like to do surgery but what is your reaction to this? Is it possible with my numbers that PHPT is a real possibility?
Hi Robert, It is indeed quite plausible, including the hint that your stones began in later life. I would do repeated morning fasting serum calcium measurements and convince myself and physicians the level is actually high – I bet it is, then let the surgeons cure it. This is the message of the article you have posted on. Fasting is crucial, as serum calcium varies with food, and morning, too, as normal values all arise from then. The big problem is to be sure about serum calcium before surgery – surgeons do not do surgery to confirm the diagnosis, but to cure what is surely there. Regards, Fred Coe
Thank you Dr Coe! I’m trying to convince my urologist to do just as you suggested with the fasting blood tests.
Well, I had fasting blood serum tests and they came back 9.6 and 9.5 with pth at 29. HPTH was then ruled out by my nephrologist. However, I insisted on a bone density scan, ans sure enough, today I was diagnosed with osteoporosis, following the scan. Doesn’t that make it even more likely I could have HPTH, even with relatively normal numbers?
Hi Robert, No. You do not have evidence for PHPT. I presume you have some other cause of stones, but not that one. For example, genetic hypercalciuria is associated with loss of bone mineral. Regards, Fred Coe
Dr. Coe, I had my first 12 mm calcium oxalate/phosphate stone removed via ureteroscopy with laser lithotripsy a few months ago at age 48. Initial CT scan without contrast showed 12 mm stone in right kidney and possibly a 5 mm stone or complex cyst in left kidney. I’m postmenopausal and had a hysterectomy at age 44. I had a brief phone consult with Jill Harris and she recommended I read this article. I have done fasting bloodwork in morning twice in past three months:
February 18, 2021
Calcium 10.4 mg/dL
PTH Intake 29 pg/mL
Vitamin D, 25-Hydroxy 50.4 ng/mL
Phosphorus not checked
May 17, 2021
Calcium 10.1 mg/dL
PTH Intake 22 pg/mL
Vitamin D, 25-Hydroxy 64.6 ng/mL
Phosphorus 3.7 mg/dL
I have done two 24 hr Litholink collections on March 29 & 30th, 2021:
Ca24 189, 199
Ox24 35, 36
pH 7.533, 7.334
P24 0.267, 0.386
PCR 0.6, 0.7
Ca24/Cr24 279, 269
I did increase my dietary intake of calcium to ~1000 mg/day about a month prior to May’s blood work and tried to reduce my sodium a bit. I have not had any bone scans done. I would greatly appreciate your thoughts on my situation and whether I need more blood work, urine or other tests to rule out PHPT. Thanks so much!
Hi Jenny, Both serum calcium results are above 10 which is highly suspicious. The PTH levels are low, but still normal. Early primary hyperparathyroidism is a high probability. Given the importance of the diagnosis – surgical cure – I would wait a while and get another pair of morning fasting serums for calcium and PTH. I would ask the PTH sample be in plasma as it is more stable – in serum PTH degrades and perhaps your real values are higher than those reported. Your urine calcium is very high when normalized for your muscle mass – Ca24/cr24 is far about 140. If the next two are like the first two your physicians might want to take the diagnosis seriously indeed and pursue the evaluation accordingly. Regards, Fred Coe
Dr. Coe, thank you so much for reply. I greatly appreciate it. Do you recommend any further and specific testing outside of the calcium and plasma PTH? My primary care physician is referring me to an endocrinologist and a another urologist (different than the one who performed the ureteroscopy so I can get a second opinion). I want to be sure I am asking the right questions and getting a more accurate diagnosis when I see these physicians. My goal is to prevent any further kidney stones from forming if all possible.
Hi Jenny, when primary hyperparathyroidism (so long a name!!!) is at issue, the foundation is serum calcium – is it above normal in the fasting state in the morning (when normals were studied to get the ‘normal range’). If it is not the disease is not present. If it is high then the disease may well be present unless the PTH is LOW (suppressed below the normal range). So, if I have the 100 pennies, I spend the first 99 on serum calcium + PTH, fasting, in the morning, and, as for the 100th penny, I spend it, too, in the same way. Once we know this one thing, the rest is routine, if – surgery – highly technical and for experts to do. Regards, Fred Coe
Dr. Coe, I was diagnosed with hyperparathyroidism with PTH at 216 and calcium levels consistently over 10. I had two parathyroid glands surgically removed at NIH in 2011; one was the largest hyperparathyroid tumor NIH had ever removed (according to the surgeons present), while the other turned out not to be a tumor but had looked suspiciously large at the time of surgery so was removed.
Question 1: Do you view the following symptoms as associated with hypoparathyroidism? In the past year I have had movement disorders in the mouth/chin area with lip puckering and chin spasms. I never had this issue before. So I increased my calcium and vitamins D and B12 intake about three months ago mainly via supplements to see if that was related because my calcium had been at 8.5 and had been low like that for years.
After I increased my intake, the mouth/chin movements quelled substantially (maybe 85%), but not entirely. My calcium reading today is now up to 9.0; ionized calcium serum score is 5.0; Vit D is at 38.5; and PTH at 19. I have recently made appointments with both neurologist and endocrinologist who have ordered CT and MRI and told me to keep my calcium and D up.
Question 2: Do you have an opinion on whether taking calcium via supplements (rather than natural intake such as via dairy) can cause kidney or heart problems down the line? Back in 2012, post surgery NIH warned me not to take calcium supplements and to get 1200 units of calcium naturally. (They may have changed their views since—don’t know.) Being lactose intolerant, getting my calcium levels up naturally is not easy. I did show a 2 mm kidney stone on an x-ray in 2018 but never felt it. What is your view on supplements for calcium and Vit D over the long term? Thank you.
Hi Carol, I am suspicious you are hypoparathyroid in that your PTH is low and serum calcium at 9 with supplements. The concern is urine calcium. With low PTH renal calcium conservation is reduced so supplements will raise urine calcium and stone risk. I would advise your physicians obtain a kidney stone oriented 24 hour urine test for you while taking sufficient calcium to keep your serum calcium at least at 9 mg/dl. The urine may be high and that is the reason for your stone. Regards, Fred Coe
Many thanks for your response, Dr. Coe. Since I wrote my message to you and before I saw your reply just now, I have learned more that is consistent with your suspicion about my condition, and it looks like I have found a way forward. First, I got results from a brain MRI that showed a small brain tumor so I contacted Johns Hopkins/Baltimore/Meningioma Center, where I had an EEG and other testing done. The JH neurosurgeon determined the 5mm meningioma was unrelated to the facial movement disorder I was experiencing (which was the same conclusion as that of a neurologist at Georgetown U. Med Center who also reviewed the brain MRI). Second, I went ahead then and snagged an appointment for the end of this month with NIH/Bethesda to review my facial movement disorder as potentially related to my post-parathyroidectomy low-calcium level issues. I also raised my kidney stone history. My status as a former NIH surgical patient for hyperparathyroidism streamlined my acceptance in another NIH parathyroid-related protocol. I will certainly raise the supplements concern and the kidney stone-oriented 24-hour urine test, as you have advised, at my NIH appointment. Am looking forward to getting the facial movement disorder resolved there before it gets worse, and, in the meantime, JH will watch over the meningioma. What dumb luck I have living near these great research centers. Life is good. Again, thank you for your perceptive response and recommendation!
Hi Carol, It sounds like you have experts enough, and hope things work out well for you. Fred
I am a later in life stone former as well and am getting ready to have stone surgery. I keep seeing people posting bloodwork results in regard to PHPT, but not what these tests are actually called. What do I ask my urologist to order? (or is it something I can order from one of those walk-in labs?) I have to have a sepcific request or my urologist is not going to do it – there is no interest in finding out “why” and preventing. (I just finally got her to agree to do 24 hour urine once I am past surgery). Thank you!
Hi Barbara, Fasting serum calcium is above normal with PHPT, serum PTH is not suppressed below normal, and urine calcium is not abnormally low. In later years PHPT is not at all rare in new onset stones, and you are right to ask it be looked for, It is curable with minimally invasive surgery. Regards, Fred Coe
Dr. Coe
Hello. I am so happy I found you. I am a 40 year old female. I formed/passed my first stone at 13–with increased frequency over the past decade or so. I have formed countless stones, more than 10 lithotripsies, several hospital stays, 3 septic infections, and I can’t tell how many blood draws. In the last year alone, I have been hospitalized 4 times (1 visit in the ICU), had 4 stent placements, 2 lithotripsies, and 1 PCNL. My last CT Scan (09/18/2023) showed multiple bilateral stones–and cysts. My regular urologist finally decided I should see a kidney stone specialist (who performed the PCNL).
The specialist asked if I have had a parathyroid test and/or completed a 24 hour urine. I didn’t know the parathyroid was different from the thyroid–which had always came back normal. I had the PTH intact test done 10/05 and noticed that it came back high at 84 pg/ml.
This lead me down a rabbit hole of “self diagnosis” research. PHPT checks a lot of boxes considering the progression of symptoms. Outside of the kidney stones, I have been seeing a few different specialists for what appear to be unrelated issues. I have experience back pain due to multilevel cervical spondylosis (my last MRI was in 2019)–remember I just turned 40. I also went from being a “perpetual student” to being unable to concentrate/focus. My energy is non existent–I feel extremely exhausted most days. There is also depression, anxiety, “shaky hands”, and headaches. Most recent developments are numbness in my left thigh area and muscle cramping in my legs.
Anyway, I went back through my lab results over the last couple of years. I am still waiting for the results of my 24 hour urine.
10/05: PTH 84 pg/ml
10/05: Uric Acid 4.2 mg/dl
Stone Analysis
09/29: PCNL: stone analysis 100% calcium phosphate (hydroxyl)
08/31/2022: stone analysis 40% Calcium Oxalate Monohydrate 60%Hydroxyapatite
03/04/2016: Stone analysis 10% Ca oxalate dihydrate 55% Ca oxalate monohydr. 35% Calcium phosphate
Calcium/phosphorus levels (all from hospital stays/visits/procedures related to kidney stones/infections)
09/20: Calcium 8.6 mg/dl
09/19: Calcium 8.0 mg/dl
09/17: Calcium 9.3 mg/dl
09/14: Calcium 9.5 mg/dl
09/05: Calcium 8.7 mg/dl
08/31: Phosphorus 2.6 mg/dl
08/31: Calcium 8.6 mg/dl
08/31: Calcium 8.4 mg/dl
08/30: Phosphorus 3.1 mg/dl
08/30: Calcium 6.6 mg/dl
08/30: Calcium 8.2 mg/dl
08/29: Calcium 8.7 mg/dl
08/29: Phosphorus 1.7 mg/dl
08/28: Calcium 9.2 mg/dl
08/23/2022: Calcium 9.9 mg/dl
08/08/2022: Calcium 9.6 mg/dl
05/07/2022: Calcium 9.3 mg/dl
06/02/2021: Calcium 9.3 mg/dl
06/04/2020: Calcium 9.6 mg/dl
12/10/2019: Phosphorus 2.1 mg/dl
12/09/2019: Calcium 8.2 mg/dl
06/27/2019: Calcium 10 mg/dl
12/22/2014: Calcium 9.5 mg/dl
05/20/2013: Calcium 9.2 mg/dl
Do you think I am on the right track with the PHPT? I have a follow up appointment with the kidney stones specialist to go over test results and develop a treatment plan. I just want to be prepared–and am a little impatient.
Thank You in advance-
Misti
Hi Misti, I do not think so. Your serum calcium values are all in the normal range. I suspect you have high urine calcium as a cause of your stones which have gradually converted from calcium oxalate to calcium phosphate and need preventing. Rather than guess from random testing I suggest a more preconcerted effort like this one. From all of the stones your kidney function may have fallen a bit which can raise serum PTH. There are other reasons for high PTH – low calcium diet, low serum 25 vitamin D. Regards, Fred Coe