Middle age 45 – 65, not the usual time to form your first kidney stone. The average for new stone onset is 35, with a spread of about 12 years, so by 45 you might think the odds are in your favor. But not always. Sometimes they start late, even into your fifties or sixties. It doesn’t matter some of the time. A stone is a stone. But older people get stones for a different spectrum of reasons than when young, so you have to think a bit about why.
The image, a self portrait by Jan van Eyck (1390-1441), was painted in 1433 in oil on panel. It hangs in the National Gallery, London.
This article is co-authored by me with Jill, but was her choice of topic. She is sure her patients will love it. I hope so.
Primary Hyperparathyroidism
This is not rare as a cause of stones, and very important. On the one hand, it is a systemic disease. High serum calcium can cause kidney injury, and raise blood pressure. Bone mineral can be lost. On the other hand, it is curable. Although PHPT can occur in youth, the average age of diagnosis in a recent and large VA hospital record review was 67-68. A large Canadian survey of published papers estimates that diagnosis is usually after 50 years old and that, as is well known, women have it more frequently than men. In a large single center report of a university cohort the mean age at diagnosis was 61 years with stones, 69 without stones.
We have already written two articles on how PHPT works, and how it is diagnosed and treated. This one is very clinical. This one is very detailed, all about mechanisms and for the curious. What matters here is that if your stones begin later in life – after 50, for example, this disease needs to be higher on your list than if they begin at 25 or 30. You need to be sure about your serum calcium. You need to be sure it is measured when fasting, and looked at carefully. Even a little elevation should raise an eyebrow and lead to more measurements to be sure.
Uric Acid Stones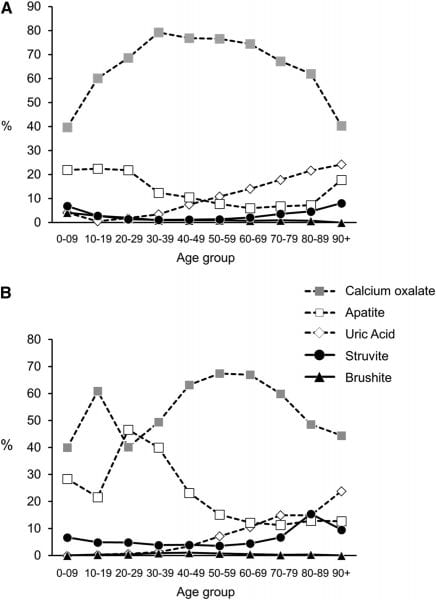
When Do They Occur
This nifty figure from a paper by the Mayo Clinic group shows how age changes stone type. Men are on top. Calcium oxalate stones are always the most common, in both sexes, but under age 30 or so calcium phosphate stones (the open squares) are reasonably common, especially in women.
Uric acid stones, the open diamond, creep up on both sexes, after age 40 in men, and 50 in women, and by the sixties are more common than calcium phosphate stones in either sex.
Uric acid stones occur because the urine pH falls, we know that with perfect certainty. The low pH protonates the uric acid molecule, so it loses its only charged site. Water no longer has a good way to connect with it, so it just leaves the solution as crystals.
Why Does the pH Fall?
We asked ourselves that very question and tried to find out.
Lots of things happen as we get older. We get fat. Our kidneys gradually lose their youthful glow. Both of these can lower the urine pH. We get diabetic, and that surely lowers urine pH. Do any of these account for what this figure shows us?
Urine pH Does Indeed Fall
We were fortunate to come into possession of a large set of laboratory data collected by a national kidney stone testing laboratory. It has no names, but did have age and sex, and urine stone risk factors. So we could reconstruct what happened to urine pH with age in men and women.
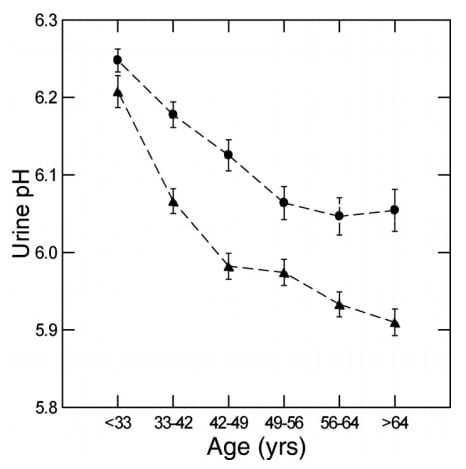
In both, men are triangles, urine pH fell very rapidly beginning below age 30, and at all times women had a higher pH than men. We have already written about this feature of women. Eating exactly the same food as men, women extract more alkali from it, so their urine is more alkaline. That is why they form more calcium phosphate stones, as the picture from Mayo Clinic shows.
But something happens to women as they age, and men, too. Whatever it is that makes their urine rather alkaline at the beginning gives way with age, and not so old an age, either. After all, much of the fall is before 50, the early part of so called middle age.
It Is Not The Getting Fatter
We get fatter with age. Everyone knows that. Not everyone does it, but on average we all do. I suppose it is less exercise and too much food, but we are not studying this matter here, now.
Below, you can see body mass index (BMI) rising with age in this very large set of data (nearly 9,000) patient lab
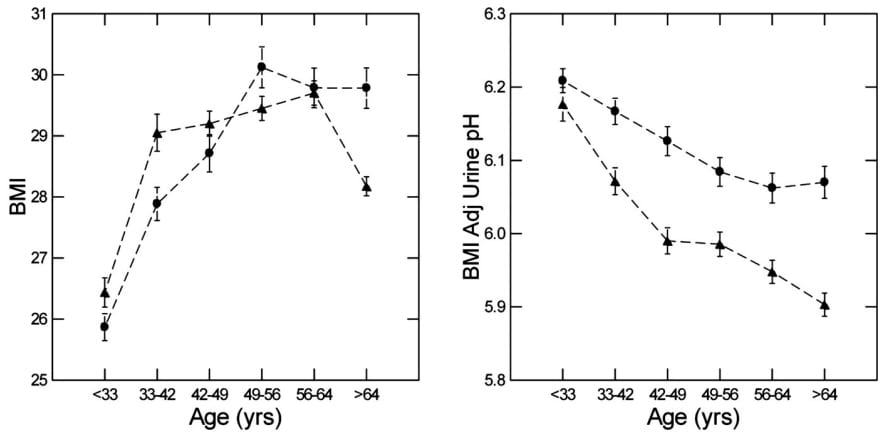
studies. It goes up in men (triangles) and women, and it goes up very rapidly between 33 or younger and 50.
But, if you adjust for the BMI, the urine pH fall is not affected.
The urine pH falls about the same in both sexes. Compare the graph just to your left with the one just above.
By adjusted, we mean we used complex multi-variable models to account for the rise in BMI and the linkage between BMI and urine pH. They are linked, and BMI rises, but the rise is not enough, given the linkage, to explain almost any part of the falling pH. So it is not obesity.
It is Not Loss of Kidney Function
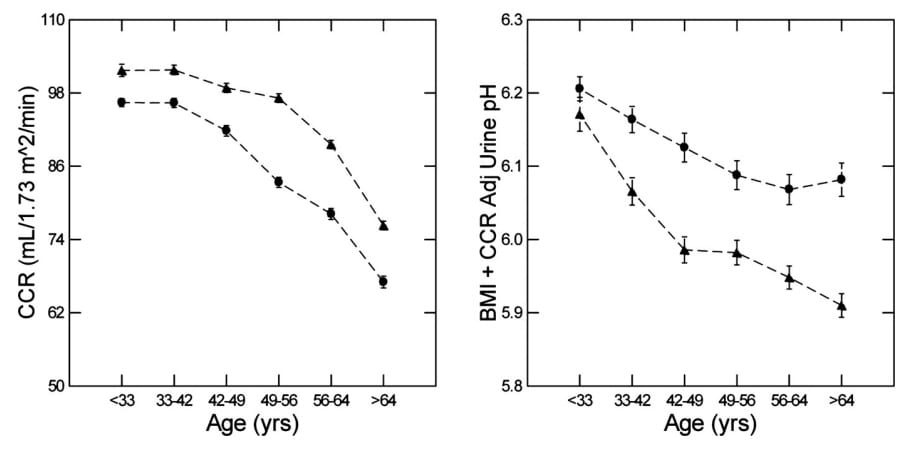 Here is another graph. Kidney function was measured using creatinine clearance, a common measure.
Here is another graph. Kidney function was measured using creatinine clearance, a common measure.
It went down with age.
But, it began to fall after urine pH had already fallen quite a bit. In other words, the one was not correlated with the other very well. Correlation is not causation, but the other way around is true. Things that are not correlated are not often related causally.
A more elegant approach is to do another of the multi-variable analyses, which we did. The graph on the right, just above, shows that urine pH fell more or less the same if you did (as here) or did not (the original graph above) adjust for kidney function. So, it is not BMI and not kidney function.
pH Falls Even Though Alkali Absorption Rises
 The reason for the higher urine pH in women is their greater ability to absorb alkali from their diet. So, was it possible that with age people lost some of that ability? Their bodies would have less alkali from food, and their kidneys would have to work harder excreting acid, and make the urine more acid in the process.
The reason for the higher urine pH in women is their greater ability to absorb alkali from their diet. So, was it possible that with age people lost some of that ability? Their bodies would have less alkali from food, and their kidneys would have to work harder excreting acid, and make the urine more acid in the process.
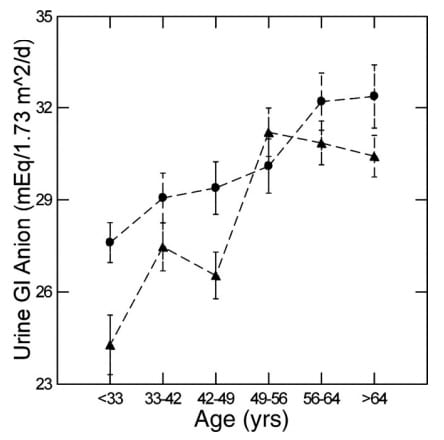
What we found was the exact opposite. The absorption of alkali, which is called GI anion for historical reasons, rises with age. It does so in women and in men. When women are younger, they absorb more than men. See how the circles, women, are higher than the triangles. But around 50 or so women and men converge because women are rising slowly, men rapidly.
But all the while, urine pH is falling. That is backward. When we showed you how women act, you could see that with each meal their GI anion rose and their urine pH rose with it. Here, the urine pH is falling despite more alkali.
You might ask what would happen if we used our multi-variable mathematics to remove the effects of the increased GI Anion. How much does it help keep the urine pH from falling even more?
Without The Extra Alkali Urine pH Would Fave Fallen Far More
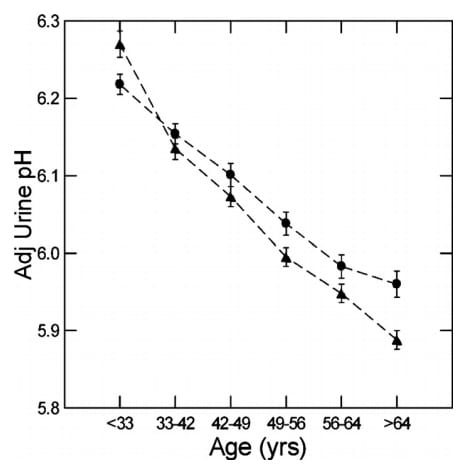 Here is the calculated effect. Urine pH falls far more and far more steadily, and the sexes are now more or less the same.
Here is the calculated effect. Urine pH falls far more and far more steadily, and the sexes are now more or less the same.
We think that the actual losses of kidney function and the rising BMI were always important. But, as these would have tended to make the urine acid, rising GI Anion offset their effects.
If you take it away, admittedly by mere mathematics, you see what would happen if there were no compensation.
Do we really think that somehow the intestines know to raise their absorption of alkali?
Why not?
They have about 10% of all of our neurons, and the brain communicates with the GI tract.
This is all for some future research. But what it tells us is that age itself, for reasons we do not as yet know, lowers urine pH. As a result uric acid stones become far more common, and the phosphate type of stone far less common.
Diabetes and Insulin Resistance
All of the forgoing was a large scale population effect. Within that population were certainly people with diabetes or insulin resistance. They cannot account for what we found because most of the fall in urine pH occurred rather young, at a time when the sheer prevalence of diabetes has not as yet risen so much.
But for many people, particularly those with serious obesity, or simply those over age 50, diabetes and insulin resistance are increasingly common. Both states lower urine pH, a lot, and cause uric acid stones. We have reviewed the main research work on this topic, that was done mainly by our colleagues in Dallas, Texas.
New onset uric acid stones can simply reflect the general age effect. But it may not be that. In the earlier stages of insulin resistance, insulin levels run high and common fasting blood glucose levels remain ‘in the normal range’. Usually they are at the top of the range, and the hemoglobin A1C is too high – 5.9 or more. It is then that one is best off taking steps, like weight loss and major life changes.
You Are Just Late To The Party
Life Has Changed
The onset age for stones may center around 30, but there are those who are slow and wait until later. Perhaps they formed their stones in their 30’s but no one knew. Perhaps they changed something and brought the stone on. Some people begin a busy travel schedule because retired, some take up extreme sports or marathon running to stay young. Some progress at their work and are promoted to a job that requires lots of long distance travel. Lots of people make eating out a time to meet friends and family, because the children are all gone.
You might think this has no special significance, but it may.
More than eating out, people change their diets in mid-life, to be healthier. But the changes may not always be healthy. Fad diet are always like the butler in a murder mystery: present at the scene, and capable of almost anything.
Your Genetic Hypercalciuria Was Unnoticed
If you had genetic hypercalciuria, you would not have known about it. So new stones mean that you need to check for that problem, and also for bone disease.
For men, the association between stones and bone disease is very well documented. For women, at least in a large epidemiological study, a history of stones and finding of reduced bone mineral were not linked. But whether they might be through genetic hypercalciuria could not be ascertained because no urine testing was available.
In studies that specifically focus on stone formers, a link to bone fracture appears far more obvious than in studies that focus on bone mineral loss as a primary aim.
Urine calcium is known to rise with insulin resistance and diabetes. Although we are not convinced about new calcium stone onset, it is enough to mention here that new calcium stones should always lead to at least a brief look at fasting blood glucose.
Drugs
If anyone asked me, I would say Topamax and its many relatives are a common reason for new stones anytime in life. Especially in people with genetic hypercalciuria, new use of calcium supplements can cause stones. There are so many more possibilities we can just say that with new stones you need to review all of your meds and supplements, perhaps especially the latter. Maybe change your diet and stop the Tums for esophageal reflux.
Retention and Incontinence
Prostate enlargement increases resistance to urine flow during micturition. Bladder wall muscles compensate by thickening and increasing their innervation. As a result urgency begins at lower than normal bladder filling volumes – frequent urination, by day and at night. Strong contractions can cause incontinence. I have had many patients who reduced fluid intake to limit frequency and nocturia and unknowingly increased stone risk.
In women, pelvic muscle weakness with age and lack of estrogen, coupled with residual problems from deliveries lead to incontinence. As for men, they respond by limiting fluid intake. I have seen this lead to low urine volumes and consequent increase of stone risk.
I have not published my cases, but an epidemiological study links incontinence to increased stone risk. Incomplete bladder emptying can cause bladder stones ascribed to stasis, too common to require a reference. But I have not seen a publication linking it, via reduced fluids, to kidney stones.
What Does This Mean For You?
New stones in midlife or later mean they must be analyzed. This is absolute. Otherwise how can you be sure about uric acid? Primary hyperparathyroidism produces calcium phosphate and calcium oxalate stones. We have always advocated for analysis of every stone, and in later years that maxim is more important than ever. New ones are a worry. But established stone formers can change from calcium to uric acid.
Apart from stone analysis, be sure your fasting blood calcium is truly normal. We mean by this not only within limits but a bit below the very top, because PHPT can raise blood calcium very slightly yet be there and a serious disease. If it is even suspicious, we have already written out what we do, which is to get many more fasting morning bloods for calcium, and with time things will become clear.
Think about your bones and your drugs, and how your life has changed. Think about blood glucose and be sure it is normal.
At the end, you may simply be a late comer. If so, treatment is as it is for everyone. But if not, a serious inquiry may give you real benefits.




Thanks for the eye opener.
Questions please :
Which is more culpable for stones, alkaline or acid urine? How can I modify my pH?
Hi Titi, Both can be a problem. Too low a pH – below 5.3 can foster uric acid stones. Too high a pH – above 6.5 or so calcium phosphate stones. It is kind of like the Three Bears. The safe approach if you have stones is to get 24 hour urine testing and find out what causes the stones. Here is my best on that. Regards, Fred Coe
Thanks for writing this up! As a 60 y/o new stone former, I have asked Jill repeatedly “why now?” The more I learn, the less anxious I am and continue to do all the things I can to control future stone forming.
Hi Barb, I am glad it was helpful! Fred
This instructive data and analysis that you provide can prevent the horrible pain of kidney stones. May you both live forever.
Dr. Coe,
I am so thankful for your service to all of us who suffer kidney stones, Thank you! I am a 62 year old female. I had my 1st stone in 2016 which sent me to the ER in horrible pain. After PCNL surgery my stone analysis was: 60% CA OX dihydrate as a 1st constituent and 40% CA PHOS apatite. I had currently been on a ketogenic diet and then switched to a vegan diet which I now know were both detrimental to my health! My Urologist doesn’t recommend any dietary plan and has not ordered a metabolic blood panel or a 24 hour urine collection either. Should I make an appointment with a Nephrologist? I am afraid to take any CA supplements & am trying to eat dairy rich CA such as Keifer & whole milk yogurt; is whole milk better or low-fat? After PCNL, a fragment of stone was left behind I was told it was small but the lab came back as a 7.5 mm! I asked if he could remove it using uteroscopy and he said no because it was in the Inferior Pole calyx (Right side) and he couldn’t get the basket in that area. He advised ESWL 6 weeks after PCNL but I asked for more time for my kidney to heal completely so he scheduled my x-ray in February 2020. I have concerns about the apatite in my stone. Isn’t this an infectious stone? If so, isn’t it risky to break it up, causing more infectious particles to invade my kidney and create more stones? I am drinking fresh organic lemon juice in distilled water 1/2 C twice daily along with a natural B-Complex and 2-3t. daily (spread out) of Calm brand powdered Ionic Magnesium Citrate. I quit taking all other supplements. Please advise me on your advice to move forward; I am very confused as to what to eat at all…very stressful! I am eating very few oxalates! My current urine Ph is 6.5-7.5 using Ph urine strips and my Parathyroid was in “normal” range. God Bless You! Jolie
Hi Jolie, You have significant calcium phosphate in your stone and that is due to the high urine pH, not infection. I am sorry that so large a fragment was left behind. I am not a surgeon and second guessing a surgeon has no good in it. But you might want a second opinion before getting a SWL treatment. Lower pole stones do not clear so well. As for prevention, serum and 24 hour urine studies are essential. Here is a good article on the subject. Home remedies are futile, you need to know what is wrong and aim treatment there. Since the calcium oxalate in the stone was the dihydrate, I assume your problem will be high urine calcium from genetic hypercalciuria. A nephrologist is important as your surgeon is not willing to provide for you. Regards, Fred Coe
Thank you so much Dr. Coe! I will get an appointment with a nephrologist out here. One important question: My urologist has me taking lemon juice 1/2 C. daily with water to keep my urine alkaline, is this a good protocol for my case? I also need to know if taking 320 mg. of Magnesium Citrate is helpful due to the fact that most foods high in Magnesium contain significant oxalate? Ideally what is a good urine pH for my case?
Kindest Regards, Jolie
Hi Jolie, Stone prevention is reasonably well structured, and does not feature lemon juice. Here is a good introduction to a proper evaluation from which you and your physician can plan long term prevention. Regards, Fred Coe
I think you all need new Dr’s and get a second option
I’ve never heard such craziness from people, I have kidney stones, I have no problems like anyone of you, I’m 65 female
This is an extraordinary website. I am sure it has helps thousands of people.
I am a 70-year-old male with a history of calcium oxalate stones since age 55. I have finally made a major change in my diet over the past 3-4 months. I am following the guidelines put out by you and Jill Harris, especially in regard to drinking much more liquid and drastically lowering my sodium intake. My question relates to liquid intake. I am putting out about 4,300 mls. of urine every 24-hours because I am making it a point to drinking a lot of water, even when I am not
thirsty. I am extremely healthy for my age with no ailments whatsoever. I am 5’11” tall and weigh 175 lbs. Is an output
of 4,300 mls. of urine too much for a man of my age, size and health? Would such a high output, eventually, cause my
kidney’s or heart to have to work too hard. Thank you.
Hi Kurt, No, a high water intake is perfectly safe unless you are taking some medication that affects kidney water excretion. Typical agents are anti anxiety meds. Likewise, diuretics impair water excretion and you need to be careful to avoid falling blood sodium. But absent these issues and rare diseases, water at this level is fine. Be sure your physician knows, has checked off the boxes about meds, and checks a blood once in a while for sodium. During part of our evolution we lived in the lakes and rivers of the world and adapted our kidneys to remove water without sodium with miraculous efficiency. Regards, Fred Coe
Dr. Coe,
I am a 45-year-old woman. I had my first bout of kidney stones about two weeks ago. I had been feeling “off” for several months and all kinds of tests were run because I kept having a trace of blood in my urine and a low-grade fever. including a CT a week before my stone attack and nothing was there–“demonstrated normal kidneys without HDN”. And even at the ER, they didn’t find it but saw that “mild right HDN and stranding around the kidney with dilation to the bladder. No stone or obstructing lesion was noted.”
I went to the urologist after and did a urine test. My pH is 6.5 and still a trace of blood. Still having some pain on right side and she now wants to do a ” Lasix renogram. If normal, she will FU for cystoscopy in the office. If not, she will require an RGP and cystoscopy in the OR.”
I am so beside myself that this happened. My sister had Bartters Syndrome and has it it over 20 years. She lives he r life but this one episode has gotten the best of me, especially now that I know I will need more tests.
My questions are why now? Why at 45? And will I have to do this diet to make sure it doesn’t happen again? I’m guessing yes but it had totally disrupted my life. My anxiety is off the charts and I can barely think, work or eat. I am looking for some guidance.
Thank you,
-Natalie
Hi Natalie, Your physician is acting as well as anyone would want. Perhaps you are passing some tiny stones, and they are not visible. If there is no sign of any stone a diagnostic cystoscopy is a good idea because of the blood. Though all a big bother, risk is very low, and whatever is found treatment excellent. As for Bartters, there are cases of late onset crystals or stones, but that can wait until your urologist is finished. I would not so much worry as be aggravated at all the bother and time wasting. You have mostly all good alternatives. Regards, Fred Coe
Thank-you for all the education and help your site provides!
My husband was found to have 5 large stones in 2016 and was also diagnosed with CKD Stage III. Initially we saw a nephrologist for the CKD and our urologist for treatment/prevention of stones, (he removed 2 via sub cutaneous nephrostomy which we had analysed and the others via lithotripsy, we were unable to capture any fragments for analysis.) 6-weeks after removal our urologist started a monitoring and prevention program with us using Litholink testing. After a few months the 2 doctors decided between themselves that the nephrologist would take over and only refer us back if she suspected new stones. As we were newly arrived in the area and somewhat overwhelmed by recent events we just went along with it.
So far so good – no more stones. But as I have learned more via your site I feel we need a urologist to be monitoring stones and reviewing the supersaturation results with us. The nephrologist has had my husband on Allopurinol since 2016 and gave the reason as the 50% uric acid content of one of the stones. This is contradicted by your articles (only recently read by me) on uric acid stones where you advise that increasing PH above 6 is the way to go and that Allopurinol does nothing. Hubby’s PH was immediately corrected back in 2016 with Potassium Citrate and remains good –
We live in the North Dallas area. Are you be able to recommend any urologists ? Would greatly appreciate it –
Kind Regards-Colleen
Hi Coleen, Indeed the uric acid portion of his stones require potassium citrate as you note, and the other half, no doubt calcium oxalate monohydrate may require more. You are fortunate in that superb stone experts work in Dallas. I would recommend Dr Peggy Pearle at UT SW in Dallas. She is a brilliant stone surgeon and can take care of everything including prevention. Feel free to use my name, as she is a close friend. Regards, Fred Coe
Hi Dr Coe,
Many thanks – we see Dr Pearle next week.
Re stone analysis – you are correct – the uric acid stone(50%) was 50% calcium oxalate monohydrate. The other stone was 70% calcium oxalate monohydrate, 15% calcium oxalate dihydrate and 15% carbonate apatite.
We will be discussing all this with Dr Pearle but I have a question:
– What does it mean if urine pH gradually corrects requiring a steady reduction in Pot Cit dosage?
Initially (2016 2 LItholink tests)
urine ph = 5.096 , 4.994
24Cit = very low at 212 and 145. Potassium Citrate prescribed at 15MEQ 2tabs twice daily.
2 months later Litholink test
urine pH = 6.104.
24Cit = 621
The nephrologist took over. No Litholink test ordered for 2017 but another 24hr urine showed urine pH 7.1 so Pot Cit reduced to 3 15MEQ/day.
2018 Litholink
urine pH = 6.729
Cit24=738 so Pot Citrate reduced to 2 15MEQ /day.
2019 Litholink
urine pH =6.782
Cit24 =724 so Pot Citrate reduced to 1 15MEQ/day.
1 month later urinalysis showed urine pH at <= 5.0 so this dosage insufficient. If the Nephrologist noticed she did not comment or increase dosage and I completely missed this. So unfortunately my husband has been at this urine pH for 6 months before I noticed a few weeks ago and panicked. I understand correct dosage (TBD) should raise urinary pH to above 6. But is it clinically significant that Potassium Citrate dosage has required steady reduction like this?
Many thanks
Colleen
Hi Colleen, You saw what one does not want to do: If the pH is above 6 is there a reason to make all these changes? Dr Pearle will solve the problem for him, and after that the uric acid will be gone. She will figure out whatever else is wrong, too, as she is a wonderful expert. Send her my warmest regards and let her fix things. Regards to you as well, Fred
Hi Dr. Coe,
I am a 31 year old, otherwise healthy, male with a Y shaped ureter on my left side, the only side producing stones. I had two stone analysis done on the pile of fragments I collected after my only lithotripsy done 11 years ago, and they were 60% and 65% calcium phosphate, respectively, with the remainder a mix between calcium oxalate mono and dihydrate. Before this procedure in 2008, there was one stone in each of the lower, mid and upper poles. Fast forward to today and I now have 3 very large ones in the upper pole, 2.4cm, 1.3cm and 1.1cm.
My urologist suggested to do a lithotripsy and put a uretal stent in so he could do a uteroscopy a few weeks later. I’m curious if you would suggest this approach, or if not, what you might do instead?
I’m also interested in finding out if there is some type of systemic issue going on that is causing me to form stones. Since I have the duplicated collecting system on the left, and that is the only side with stones, my doctors have always just said that the anatomy is the cause. I have had a bunch of normal serum calciums over the years, some low vitamin D levels, some higher 24hr urine calciums, and for some reason my 24hr urine creatine/kg has always been high, even though I am not overweight.I am already on a low oxalate diet, trying to up my calcium with meals, increasing water intake, and decreasing sodium and sugar. I have been on and off citrate supplements over the years, and am going to begin testing my urine pH while taking them to make sure it doesn’t increase too much. Since the stones are mostly phosphate, do you recommend any adjustments in regards to dietary phosphorous/phosphate? Does dietary phosphorus intake have a significant effect on phosphate supersaturation?
Thank you in advance for any thoughts you might have, and thank you for all the information on this site, it is incredibly helpful.
Hi Vincent, The high urine calcium is the main culprit, and the abnormal urology on the left adds risk by increasing likelihood that crystals will be retained in the kidneys – a two hit model. That the stones had abundant calcium phosphate suggests that possibly the upper pole drains less well than normal and the renal elements thus drained may have lost normal acidification so urine from that segment is more alkaline than the bulk phase urine. Firstly, I would hope that your surgeons have secured the best possible drainage of the upper pole. Then, I would use reduced diet sodium and perhaps thiazide to lower urine calcium as much as possible. I have no idea why potassium citrate would be an ideal choice as we lack trial data for those with abundant stone phosphate content and the agent does raise urine pH. This article parses out the interactions of diet and meds. Of course, your physicians are in charge here, and the only use for my remarks is that they might find them helpful – or not. Regards, Fred Cpe
Hi Dr. Coe,
Thank you so much for your reply. I have a few follow up questions. I know there many, so short/no answers are completely understandable 🙂
1. “The upper pole drains less well than normal and the renal elements thus drained may have lost normal acidification so urine from that segment is more alkaline than the bulk phase urine” – It seems like their would not be, but is there any way to test any part of this statement?
2. On securing the best possible drainage of the upper pole – do you mean clearing the stones? If so, do you see any potential issues with the combination of lithotripsy and uteroscopy – or when is nephrolithotomy a better approach? My urologist mentioned a few uteroscopies because of the overall stone burden, and I would like to have as few procedures as possible.
3. I don’t see anything in your or other articles regarding dietary phosphate – do you think it has a significant enough affect on stone formation to consider dietary change as with oxalate and oxalate stone formers?
4. Is there any concern here for any endocrine issues? Is supplementing with vitamin D contraindicated for any reason?
Hi Vincent, only that stones from the upper pole will have high calcium phosphate content. Ureteroscopy is the best procedure overall, in that PERC, though very definitive, is a more invasive surgery. During URS laser light is used to disrupt the stones. As for diet phosphate, I have no basis for commenting in that it has not per se been linked to stones. Cola drinks have a lot of phosphate and are linked to stone disease, so perhaps by inference one can indict it. The very article you post on concerns primary hyperparathyroidism, the main endocrine issue. Regards, Fred Coe
I am a 55 year old female. I had kidney stones issues that first became apparent at age 54 (Spring of 2018). I’ve had lithotripsy on two stones since then. I’m told one remains. I have had a Litholink analysis done, but I don’t have the results yet.
In 2002, I had radioactive iodine ablation of my thyroid. In 2017 and up until the first stone symptoms in 2018, I had mild depression and severe panic attacks and anxiety that I had never experienced before. I attributed it to perimenopause, but have since read that anxiety can be a symptom of hyperparathyroid. The last time I had calcium checked was in 2017 and was in the middle of the normal range at that time. As far as I know, I’ve never had parathyroid levels checked. Do you feel that’s something that I should have done? The one time I mentioned it, at the onset of he kidney stone problems, my concern was dismissed because my calcium level was normal.
Hi tastowell, a normal serum calcium level makes PHPT a very low likelihood diagnosis. The only caveat is some patients have borderline normal calcium levels in their blood and are called normal. You seem to be mid normal. Your LL tests will help determine the stone cause, I am sure, and be sure and do what is needed to reverse what is abnormal. Regards, Fred Coe
Hi Hi Dr. Coe,
I have 4 stones in both kidneys. The biggest one is about 3 mm. Those might hopefully not be a big issue since they may pass by their own. The issue is that I have another stone between the upper and middle course of the right ureter. It was about 9mm before I had my first ESWL session. After that session, two small fragments of the stone came out within a week. I did a stone analysis test and found out they were composed of CAOX and CAP. The CT scan showed that the stone was still there. So, I had my second ESWL session 3 weeks after the first one. Nothing came out, but 3 tiny sands. I had another recent CT scan, and found the stone measuring 5.6×7.4 mm, with 1120 HU and causing mild back pressures.
However, I don’t feel any pain at all because of it.
My urologist now suggests to do a Uteroscopy. I’m curious if you would suggest this approach, or if not, what you might do instead?
Can this stone pass by its own? Especially since its 5.6 mm width is inside the ureter diameter.
Thank you in advance for any recommendations you might give, and many thanks for all the information on this site, it is greatly helpful.
Hi Islam, Given a retained ureteral stone with obstruction – even slight – your urologist is certainly right to suggest removal via ureteroscopy. It has been there long enough and is not so small. Regards, Fred Coe
Dr. Coe, I am 66, just had my first stone. I don’t know how to find a doctor in my area that is concerned with stone formation, analysis of my situation, and correction/prevention. Those I have spoken with don’t advocate for dietary changes and are more interested in the surgical procedures to remove stones. In an earlier article you recommended a wonderful kidney stone expert in Dallas, but that’s not feasible as I am in New Jersey. I want to find out why this happened, and what may underlie this situation. No pain now after passing the stone, but not feeling 100% either. This was a one time occurrence, but the other night i showered, dried my hair, then sat down to relax. All of a sudden i became flushed, face reddened and felt like sunburn, eyes dry. It subsided in a few hours, but I’m curious to know if this can be linked to an underlying disease. Can you recommend a doctor/practice in NJ or Philadelphia area that would delve into my stone situation with proper testing and analyses? Should I be talking with a urologist, a nephrologist, or other discipline? Thank you!
Hi Susan, Dr David Goldfarb at NYU is not so far away, and is excellent. See if he will be what you can use. Regards, Fred Coe
I am a 57 year old woman with no prior history of kidney stones. I was diagnosed with SLE 3 years ago and I currently take plaquenil & Rasuvo (soon to switch to Benlysta). For the past year I have had blood in my urine along with occasional UTIs. Neither my rheumatologist nor PCP was overly concerned until recently. I was finally referred to a urologist 3 weeks ago. I had a CT urogram and cystoscopy. The CT urogram indicated the presence of several small (<5 mm) stones in my right kidney, of which only one was visible in comparison with a CT scan that was done 3 years ago (for a different reason). It was noted that my right kidney has a duplicated ureter. My left kidney has a stone of 13 mm, along with several smaller ones.
My urologist suggested ESWL, and a document regarding diet was placed in my patient portal. No in office discussion of diet took place. A 24-hr urine collection was not suggested. My urine pH is typically 7-7.5. Would you suggest that a 24-hr urine collection be done? Are there any other tests you would recommend?
Hi Linda, SLE can cause forms of renal tubular acidosis and calcium phosphate stones. Rasuvo – methotrexate – does not cause stones. Perhaps your physicians might want to consider this possibility. In any event you should indeed be tested for all causes of stones, so prevention can begin. Regards, Fred Coe
Thank you for responding so quickly.
Would you happen to have any suggestions for a kidney stone expert near central PA?
Hi Linda, Dr Wasserstein is excellent, at U Penn, Philadelphia. I looked at Pittsburgh and recognized no one in particular. I cannot tell which city is closer to you. In the middle of the state I have no suggestions. Regards, Fred Coe
Just diagnosed with multiple kidney stones at age 75 had ureterscopy to break them down . What could be the causes at this late age?
Hi Robert, The most common would be uric acid stones, a simple matter to confirm via stone analysis. They are completely prevented by treatment. Another is primary hyperparathyroidism, also curable. Regards, Fred Coe
I’M VERY WORRIED ABOUT KIDNEY STONES AS THEY CAUSE TOO MUCH PAIN , MY AGE IS 22 IS THIS AGE PRONE TO GETTING STONES. PLEASE IF POSSIBLE TELL IN PERCENTAGE. THANK YOU!
Hi aamir, If you do not have stones, I am unclear as to why you would be concerned. It is true that peak onset rates are 20-35, but most people are not stone formers. Regards, Fred Coe
Hi,
I’ve had multiple stones, mostly calcium oxalate, but the latest 2 stone were:
Carbonate Apatite (Dahllite) 90%
Calcium Oxalate Dihydrate (Weddellite) 10%
Would you recommend anyone in the Chicagoland area to help me conquer this problem? I desperately need someone who can help me figure this out. Thanks for any help.
Hi Beth,
Dr. Robert Nadler at Northwestern is a highly skilled surgeon and does believe in prevention.
Best, Jill
Hello from New Brunswick, Canada. My husband is 70. No prior history of kidney stones at all. Suddenly, last week, he began vomiting and found out he had one stone in each of his kidneys. Left one was larger (around 4 mm or so x 3.6 mm), the right one was smaller. After a failed attempt at removing the stone, and subsequent damage causing bleeding, the stone passed on its own. Now, he is told he has two more in each kidney, plus he has a large prostate, (apparently the size of a grapefruit) which causes difficulty in reaching them to remove them. The doctor says he won’t attempt to retrieve the new stones. Why now? His diet hasn’t changed much, maybe healthier. They couldn’t analyze the first stone because it was passed. With the urologist not wanting to touch these other stones, how can we find out what causes them?
Hi Darla, You are a very good reader and have commented on my ‘why now’ article. In it, I gave my best on why and what to do, and suggest his physicians consider looking for what is most likely – uric acid stone can be tested using the stone that passed. Being completely preventable, it is crucial to identify them when present. Other later in life causes likewise. Of course your physicians do not need to read the article, as they already know anything I would have written – they should look. Regards, Fred Coe
My physically fit 53 year old mother had her first stone in 2019. She went to the ED and was referred to a urologist, who found dozens of calcium phosphate and calcium oxalate stones in each kidney, some up to 9mm. She had stents placed and was bedridden for months. The Dr. was unable to remove the stones surgically, as he was worried about damaging her ureters. He broke up the stones, and she eventually passed all of the fragments. Since then, she has adopted a low oxalate diet. However, yesterday, she started passing more stones. The doctor gave her anti-inflammatory medication and told her to drink lemon water. I am concerned about her health and wondering if she should pursue further evaluation. Would appreciate hearing your thoughts. Thank you.
Hi Ellie, Calcium phosphate stones have nothing to do with oxalate, and making the urine more alkaline with lemons could worsen matters. Your mother needs proper evaluation with 24 hour urines and bloods to find out why she forms these stones, and treatment that is rational and effective. This is a good introduction, and so is the article you wrote on. My main concern is primary hyperparathyroidism because of the recent onset and abundance of phosphate. I think her personal physicians might be willing to look into this and should be able to figure things out. If not, perhaps they can suggest a stone center at a nearby university. Regards, Fred Coe
Hi Dr. Coe
Was reading this article. Have been attending Jill´s calls and did the course. So far my 24 hour urine test was considered normal. I will be doing a blood test for the parathiroid and checking it out. Regarding the pH, I also have a equipment for measuring and in my urine tests I can go from 7 to 5 (curiously with drinking lemon water – real lemons) and that time i have a urine infection (pH 5). Cannot seem to catch my small stones, as i assume they are like gravel or something. I sense some blood clots passing when I have crisis. Last year I had 3. This year I have had 1. I have been reducing my protein intake (only meat and fish), i increased animal protein via increasing the yoghurt and fresh cheese intake. My mum has kidney stones but has never paid a lot of attention to it. She eats very little amount of vegetables and little fruit. she only has one large cup of milk in the morning. She is 77. She is, at the moment taking calcium supplements and eating spinach soup (yes…. very high in oxalates). She was a former pediatrician… I get lost, although I do want to keep paying attention to my diet and drink. Any suggestions? Thanks
Hi Maria, If you are seeing Jill, she is a very good resource. I do not know your 24 hour urine or serum values, stone analyses, etc and so cannot say much. Are your stones by any chance orange or red? They seem to behave like uric acid. Regards, Fred Coe
Hi Dr. Coe
I think they are so small i havent been able to collect them. Jill has seen my 24 hour urine test and says its in the normal range. I increased lemon juice to increase the citrate. Am just trying to prevent them from happening… its a bit frustrating, but… at least I eat healthy. My pH value vary a bit during the day, from 5.15(afternoon) to 6.48 (morning before breackfast). I have a pH meter.
Hi Maria, I do not have enough here to help. Your urine pH is so low sometimes the stones could be uric acid. Be sure about the color, if they are orange or red that means uric acid. If you can catch even the tiniest fragments they can be analyzed. Regards, Fred Coe
very interesting article, I live in Marlborough Massachusetts and am having issues at 68 for the first time with kidney stones and high blood pressure. My father and some of my siblings are having the same experience. I have gained a lot of weight in the last 4 years also. Is there a doctor in or around Worcester Massachusetts that specializes in this that i could see?
Hi Joan, There is an excellent kidney stone center at MGH. I think it would be worthwhile to make the trip – it looks reasonable on my map. As for your town, I know of nothing special. Regards, Fred Coe
Dear Dr. Coe,
I am 61 and just has my first kidney stone, at least that’s what’s probable. (I went to the ER for pain in my lower right abdomen and back and a cat scan showed moderate right hydronephrosis with asymmetric with perinephric stranding without identifiable obstructive etiology. They didn’t see any stones and thought that I had passed a stone. I also had hyponatremia.)
I was referred to a nephrologist who has not been as helpful as I would like. I want to find someone to help prevent more stones, who uses diet and the 24-hour urine analysis. Are there any doctors in the Knoxville, Nashville, Johnson City, or Chattanooga area of Tennessee who you would reccommend?
Thank you for your generosity in sharing so much information with us. It means a lot to have someone who wants to help.
Lilly
Hi Lilly, I suspect either primary hyperparathyroidism or uric acid stones, given the very article you have written in on. As for Nashville, Dr Nicole Miller is at the university and a terrific stone surgeon and expert in prevention. I would use her as an ideal physician for your situation. Regards, Fred Coe
Hello,
I am white men of 46 years old. What is wrong with my body if my creatinine is in normal range and my Glomerular filtration rate (GFR) is going down. Creatinine result: 88,82 ml/min/1.73m2. GFR: 85,03 μmol/l.
How can recover my GFR?
Thank you
Hi Evaldas, Creatinine clearance is a measure of GFR and is apparently measured at 88.82 ml/min/1.73 meter square of body surface. 85.03 umol/l is a concentration, presumably serum creatinine; in the US we use mg/100 ml, so your value would be 1.04, a normal value. Regards, Fred Coe
Why now, indeed. This past April, at age 77, I had my first and only episode of passing kidney stones (as far as I know). I am in generally good health and physically active (tennis, gym, ballroom dancing) and manage to stay skinny despite a prodigious appetite and way too many sedentary hours as a writer. About five microscopic stones were detected by a CT scan my doctor ordered after I complained about what I thought was a urinary tract infection. After about three weeks, just before a telehealth consult with the urologist I was referred to, the symptoms ceased. I had already started making dietary changes based on my own research into kidney stones, The discomfort has not recurred and I never saw (and thus didn’t collect) a single stone.
The urologist I spoke to in May never said anything about diagnosing the cause of the kidney stones or preventing them in the future. All he wanted to do was give me a cystoscopy ASAP. Why? Because “It’s in the AUA guidelines for a history of microhematuria.” Does the single incidence mentioned in my doctor’s kidney stone report constitute a history? I told him none of my annual urinalyses had ever detected blood, including the one I’d had just before the pain started. (Nor did a follow-up urinalysis I requested in late August.) I decided to decline the cystoscopy – in no small part because of a painful experience after a prostatectomy in 2007 – until I heard a more compelling reason to have it.
Meanwhile, my kidney stone research using sources such as yours led me to believe that my usual diet – which for the past two years had included frequent helpings of spinach salad and almond milk, and had for decades included 16 oz. of black tea and wheat bran cereal every morning, plus plenty of dark chocolate, raspberries, and skin-on baked potatoes – might have caused the formation of calcium-oxalate stones. I immediately stopped all spinach and chocolate, started drinking much more water, replaced the almond milk with oat milk, sharply reduced the other high-oxalate stuff, and tried to pair any remaining oxalate consumption with a good dose of calcium.
Then, at the end of August, I found out about the Litholink test. I sent a request to the urologist, and got an assistant’s response saying I’d been handed off to a nephrologist in the practice who would order the test. I asked whether I should revert to my previous diet for the purposes of the test, or continue my new-normal diet, which by then I’d been following for nearly five months. I was told to stay with the new diet.
My telehealth appointment to discuss the results was scheduled for November 17. On September 21, I submitted two 24-hour samples and have just retrieved the results from the Labcorp website. The only significantly out-of-range item is urine pH (at 6.438 and 6.626 in the two tests). Urine calcium is “borderline elevated.” Urine oxalate was only 20mg and 22mg per day. Apparently, I now have a “mild CaP stone risk.”
Now, I am not qualified to interpret any of the findings. But I am having trouble imagining how this test will pinpoint what caused my stones in the first place and help me prevent them in the future. What do you imagine the nephrologist will tell me on November 17? Will he have to draw some reasonable conclusions based on probabilities? Could I keep eliminating the spinach (not an unbearable loss) but allow myself enough dark chocolate and tea to regain the boost to body and brain I need to get through many a hard day? And what can offset the frequent impossibility of downing a gallon of water on days when long meetings and/or travel combine with a certain post-prostatectomy malady? Do you have any thoughts about what I should do next? Any advice would be greatly appreciated. I’m in Columbus, Ohio.
Hi Colin, Your story says you ate a lot of oxalate in foods and then became a true believer, which is probably why your urine oxalate is minimal (20,22). There is no sense in lowering it more! The borderline urine calcium could be hereditary, and could contribute to stones and even bone mineral loss. Perhaps your diet is low in calcium, as you were using milk substitutes, and perhaps it was so when you collected. Possibly your serum calcium, fasting, in the morning, is a bit high, pointing to primary hyperparathyroidism. I would hope your nephrologist will answer all of your questions. Given telehealth, you can seek consultation and many medical schools, too. Regards, Fred Coe
Why now, indeed. I am a healthy, active 78-year-old who, last April, had what I thought was a urinary tract infection. A CAT scan showed about five microscopic kidney stones. While waiting for a referral to a urologist, I consulted websites such as yours and changed my diet based on what seemed to be good odds that I’d formed calcium-oxalate stones. Two years earlier I had started what I thought was a healthy habit: frequent spinach salads. I eliminated those, along with my regular doses of dark chocolate, almond milk and skin-on baked potatoes. I also cut back on several other high-oxalate foods (including my once-daily habit of downing 16 oz. of strong black tea) and started drinking lots more water.
My symptoms ceased within three weeks and haven’t recurred. I never saw a stone, so there’s nothing to analyze. Long story short, I went four months with my new-normal diet before anyone suggested a Litholink test. The urologist told me to stay with the new diet for the test, which I took on Sept. 21. Last week, I got the results from the Labcorp website: The only significantly out-of-range item is urine pH (at 6.438 and 6.626 in the two 24-hour samples). Urine calcium is “borderline elevated.” Urine oxalate was only 20mg and 22mg per day. Apparently, I now have a “mild CaP stone risk.”
Now, as I await my follow-up consult with the urologist next week, am having trouble imagining how this test will pinpoint what caused my stones in the first place and help me prevent them in the future. Should I be concerned?
Hi Colin, I believe I have already answered this. Fred
You did indeed answer it, and I thank you twice: First, for taking the time to read the too-long version of my question and providing a kind and informative response. Second, for all the brilliant work you’ve done (and continue to do) in this field. I found out about the Litholink test, and your development of it, from a friend who happens to be a retired nephrologist. I’ve searched the Internet for lots of answers to lots of questions, and I’ve never come across a source as thorough and enlightening as your Guide Book-in-the-making. (I appreciate your artistic and historical perspectives as well!) Best regards!
Thank you, Colin. Fred
Hello Dr. Cole, I’m a 73 year old woman. I had my first calcium oxide stone of 9mm at 70, and needed surgery & a stent for a ruptured urethra. After a recent 24 hour urine test it shows my citrate level is 50 mg. The doctor’s only recommendation is to drink 4oz lemon juice in 3 quarts water. Ultrasound shows three small stones 2,3,5mm. What is your suggestion on raising the citrate level? I have changed my diet because of information from Jill. Thank you for your time
Kandy
Hi Kandy, Given a first calcium oxalate stone so late in life, primary hyperparathyroidism is my first worry. Is your serum calcium really normal? Your citrate is very low. Is there bowel disease? Are you taking drugs that might lower urine citrate? Sometimes eyedrops for glaucoma can do this. Have there been events like a period of calcium supplement use? I am not satisfied on your behalf and suggest you inquire of your physician if he/she might have some ideas about why the citrate is so low and why such a late onset of stones. Regards, Fred Coe
I’ve read most of your blog posts, especially on calcium oxalate stones. And you’ve responded to my questions. I’m currently exploring HPTH as a possible cause. (Lost contact with my endocrinologist in the middle of this, due to her changing positions.)
New question. I’ve been aware if osteopenia for 2+ years. Couldn’t do weight bearing exercise due to sciatica, but took Ca supplements until the stone a year ago, when I switched to dairy thanks to Melanie. Had lumbar fusion 2 months ago and the doc described my spine as “melting under the drill”. However, am now able to walk without pain, which I now do daily. I recently encountered recommendations to take K2 to increase Ca uptake in bone, which I presume would also reduce urine Ca. Is there any substance to this? Any current research? What I’ve been able to find has older, and somewhat equivocable.
Hi Kim, if there is any possibility of primary hyperparathyroidism, and you have bone disease, that diagnosis needs to be pursued to the limit. The key is morning fasting serum calcium and PTH together on multiple occasions, and a 25 D in at least one. High serum calcium with normal or high PTH is primary hyperparathyroidism unless vitamin D is very low, and surgical cure is appropriate. No drugs or supplements for several weeks before beginning the serum measurements. Regards, Fred Coe
Dr Coe,
I had my first bout of calcium oxalate kidney stones at age 50 (about 5 years ago) and had lithotripsy to remove them. Every year since then (almost exactly 12 months apart), I’ve had recurring kidney stones and lithotripsy to remove them.
Just curious as to what could cause stones to suddenly start at age 50 and then re-occur on such a regular basis.
I’ve had multiple LL tests and my urologist tells me i need eat healthier (too much sodium, sugar, and animal protein). He believes my diet is the cause. However, I’ve been eating the same diet for almost 3 decades so not sure why i didn’t have stones back previously.
I’m not a doctor but I believe something else is causing my kidney stones other than diet. And the only thing that changed for me around age 50 is that I was diagnosed with Lymes disease and was treated with Rocephin. About 6 months after that is when my I had my first lithotripsy.
I’m scheduled to see an endocrinologist in a few weeks to get tested for hyperparathyroidism. I hope I test positive because at least I’ll know what’s causing my stones.
Hi Tommy, I would guess primary hyperparathyroidism is one common reason. Another is uric acid stones. Both increase with age. Both are diagnosed with ease and curable. Do you know your stone analysis? Your fasting serum calcium level? Regards, Fred Coe
Topamax????!!! I’m 56 and took Topamax in my mid thirties. I never had stones and now I’ve had them twice. The first time was last year 2023, and again this year, 2024. I’ve had to have laser lithotripsy both times. I’m terrified and traumatized. I can’t explain what’s causing this but could the Topamax be the culprit so many years later? Surely not! Right?!
Hi Sara, Indeed it could be the culprit. I would recommend a full evaluation to be sure you do not harbor ongoing stone forming risks. Regards, Fred Coe