 Up to this point we have considered only increase of urine volume as a means of stone prevention. The effect of increased urine volume is to reduce urine supersaturation with respect to stone forming salts and therefore reduce the risk of crystal formation which is the basis for kidney stones.
Up to this point we have considered only increase of urine volume as a means of stone prevention. The effect of increased urine volume is to reduce urine supersaturation with respect to stone forming salts and therefore reduce the risk of crystal formation which is the basis for kidney stones.
WHY CITRATE
Mechanisms
Supersaturation with respect to the calcium stones depends upon urine concentrations of calcium, oxalate, phosphate, and citrate, and, in the case of calcium phosphate stones, or uric acid stones, urine pH. Giving citrate salts can reduce urine calcium excretion and increase urine citrate. Urine citrate binds urine calcium in a soluble citrate complex, which reduced calcium salt supersaturations. Citrate inhibits crystal formation, growth and aggregation. The alkaline citrate salts can raise urine pH.
 Epidemiology
Epidemiology
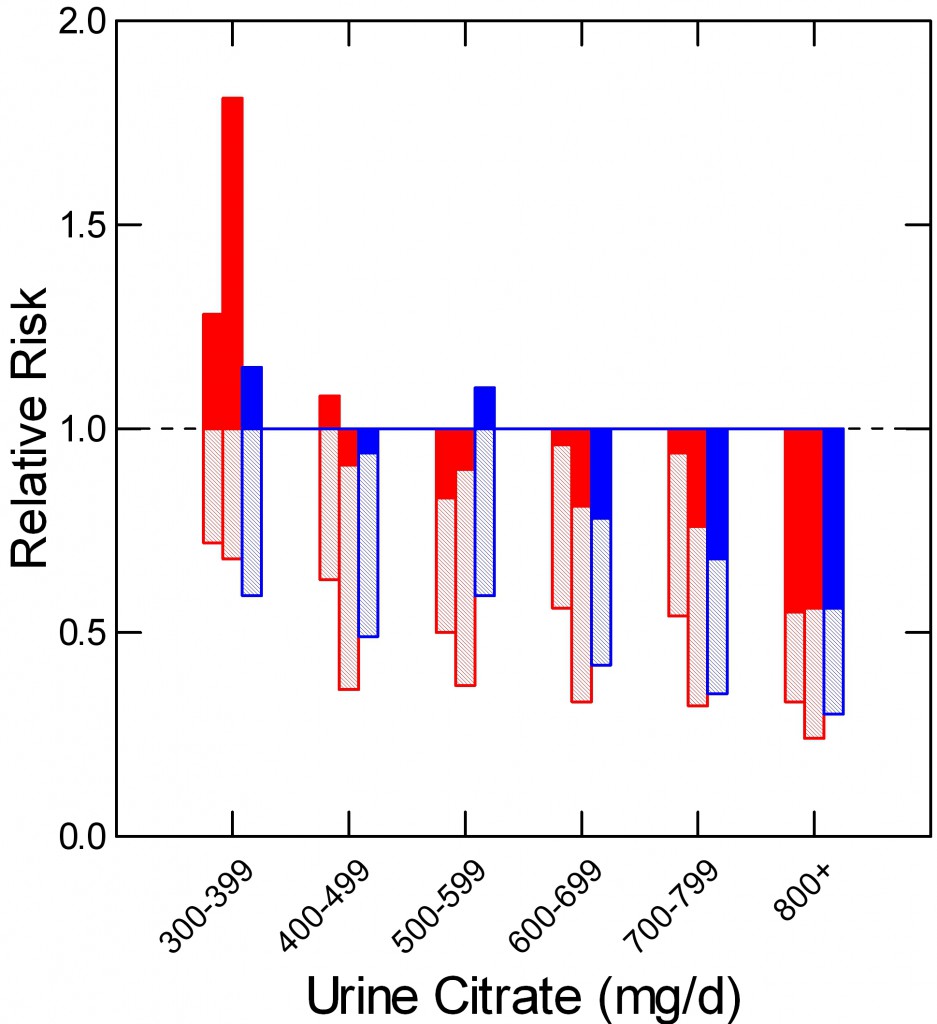
In a prospective study of two nurse (red) and one male physician cohort (blue) Curhan found that relative risk of kidney stone onset (vertical axis) rose as urine citrate excretion (shown in hexiles along the horizontal axis) fell. Below 400 mg/day of urine citrate risk was – compared to above 800 mg/day) increased by nearly 2 fold. Mean relative risk is at the ends of the shaded bars. The upper 95% of risk is at the tops of the filled bars. Even though the average risk (end of crosshatched bars) remained below 1.
CALCIUM STONES
TRIALS
Although I had quibbles with some of the comments it included, I believe the recent American College of Physicians (ACP) review of kidney stone prevention trials was done properly, and therefore have selected for review here those they felt were technically adequate.
Below is a detailed presentation of the five studies. Here is a link to my spreadsheet with all of the numbers. It also contains my references for thiazide treatment.
Ettinger et al (J Urol 158:2069-2073, 1997).
Sixty four patients with at least 2 stones in the past 5 years and at least 1 within the past year before the trial were given placebo (33 cases) or potassium magnesium citrate (63 mEq citrate, 42 mEq as potassium and 21 mEq as the magnesium salt in combination pills) – 31 cases. Each pill contained 21 mEq of citrate; 2 pills were taken 3 times a day. The trial was designed to last for 3 years. There were 5 and 9 women in the placebo and treatment arms. Urine citrate excretions were not different before treatment (549 and 587 mg/day, respectively, nor were urine volume, pH, calcium, oxalate, or any other stone forming risk. After a one month grace period in which new stones were not counted, any passage or radiographic appearance of new stones, or growth of previous stones was considered a treatment failure. During the trial, 15 subjects left the treatment arm, 8 the placebo arm.
New stones or growth of old stones occurred in 63.6% (16 cases) of the 25 placebo cases who finished the trial and in 12.9% (2 cases) of the 16 treated cases who finished the trial. If the 6 subjects who left the treatment arm because of drug adverse effects are added in as treatment failures the drug effect remained significant (8 of 22 or 33%).
Of note, this particular formulation is not available in the US. A version of the supplement is available OTC but the dose per pill is so low that it is impractical for anyone to use it. So the trial is part of a proof of principle, but not actually applicable to clinical practice in this country.
Lojanapiwat et al (International Braz J Urol 37:611-616, 2011)
Unlike the Ettinger study, which concerned spontaneous stone formation, this study concerned new stones or growth of residual fragments after shock wave lithotripsy (SWL) or percutaneous nephrolithotomy (PERC). Their subjects were 80 initial patients, all 8 weeks after either procedure, and either stone free or having no residual stone fragments >4mm diameter (Numbers are in the Table). Hypocitraturia (<325 mg/day) was present in 20/39 who received citrate and 15/37 who did not.
| SWL | PERC | Total | |
| STONE FREE | 24(8) | 15(5) | 39(13) |
| RESIDUAL STONES | 26(17) | 11(9) | 37(26) |
| Total | 50(25) | 26(14) | 76(39) |
They were randomized into 39 treated and 37 placebo treated groups and followed for one year which 76 of the original 80 completed. Numbers receiving citrate in each group are in parentheses. Sodium potassium citrate was given as 81 mEq/day in 3 divided doses).
Of the 13 cases who were stone free and received citrate, 12 remained so vs. 15 of the 26 given placebo. Of the 26 who had retained fragments and were given citrate, 8 were stone free vs. 1 of the 11 controls and 16 others given citrate showed no change (13) or reduction in size (3) vs. 2, no change and 2 decreased size among the 11 placebo. These differences were judged significant at the p<0.05 level by the authors.
Soygur et al (J Endourology 16:149, 2002)
This trial considered 90 patients after SWL for lower pole stones who had residual stones <5 mm or were stone free. They were randomly assigned to potassium citrate (50 mEq/day in 3 divided doses) or placebo (Table). The trial lasted one year. The end
| Citrate | Placebo | Total | |
| STONE FREE | 28(0) | 28(8) | 56(8) |
| RESIDUAL STONES | 18(0) | 16(6) | 34(6) |
| Total | 46(0) | 44(14) | 90(14) |
points were stone free or not and residual stone size increased or not.
New stones occurred (parentheses) in none of the citrate treated stone free patients and in 8 of the placebo treated patients. Among the residual stone group, the fragments disappeared in 8 treated cases and failed to grow or shrank in the others vs. growth or new stones in 6/16 placebo cases. The differences in growth or new appearance were all significant.
Of course, both of these post treatment trials are subject to the biases of a radiography study, but observers appeared to have been suitably blinded to the patient groups.
Hofbauer et al (British J Urol 73:362-365, 1994)
In this trial, an equimolal sodium / potassium citrate was given in doses that maintained urine pH in the range of 7 to 7.2 vs. placebo. Therefore, although patients were allocated randomly to active treatment or placebo, the trial could not be blinded. By the three year endpoint, 22/25 placebo and 16/25 active drug subjects remained. New stones occurred in 16/22 placebo and 10/16 active drug subjects. This difference was not significant. This study is the only one with a negative outcome. It is also the only study that was not double blinded.
Barcello et al (J Urol 150:1761, 1993)
Stone formers with urine citrate excretion rates below 643 mg/day (3.4 mmol/day) were allocated to potassium citrate 60 mEq/day in 3 divided doses. Their mean urine citrate excretion was 359 mg/day. At the end of three years of followup, 20/28 placebo treated and 18/27 citrate treated subjects remained. New stones occurred in 14/20 placebo and 5/18 treated cases, a significant departure from chance.
GRAND SUMMARY
| NEW STONES | |||
| YES | NO | TOTAL | |
| TREATED | 20 | 115 | 135 |
| NOT TREATED | 77 | 71 | 148 |
| TOTAL | 97 | 186 | 283 |
Despite the variability of design, one can, with nerve, simply ask about the beneficial effects of citrate salts across all the trials. In all five trials 283 people completed the desired treatment period. Of these, 97/283 (34%) formed new stones or, in the case of the post procedure trials showed growth of retained fragments. Among all patients who were given citrate salts, 20/135 (14.8%) formed new stones or showed growth of retained fragments vs. 77/148 (52%) of those given placebo.
I have not added back the 6 cases from the Ettinger trial who left because of drug side effects.
From this we can reconstruct a sense of the value of the treatment as applied to the mixed practice of post surgical management and overall medical prevention.
Let us assume these numbers will hold for the future.
For every 1000 cases like the ones in the trials, 520 untreated cases will form new stones or show stone growth after a procedure vs. 148 cases/1000 cases with citrate, a savings of 372/1000 cases overall.
I realize I am not calculating in the most satisfactory manner as a statistician, but I rather like the coarse grained, even vulgar nature of my count me up.
QUALITY OF EVIDENCE
A Personal View
The trial community exhibits the kind of methodological fussiness one expects and applauds in any scientific situation. Among their ilk the citrate effect is viewed as modest at best, the evidence, by their likes, fair.
I am sure they are right according to the mores and social instincts of this discipline, but I do not come from nor inhabit that discipline, and therefore have an altogether different way of counting – for that is all one does after the impatient and often indifferent subjects have played out their roles in the work.
How likely is it, I ask myself, that citrate salts do not prevent new stones or fragment growth?
Not at all likely.
Why assume anything but that blinding was performed when specified, that radiograph readers were competent and blinded to the groups patients were in, that stone events were counted fairly and compared to radiographs to estimate new stones? If we make these assumption of honesty and skill, the marked downward skew from alkali is just too large to be by chance.
My bet will be on the drug, and if I bet that way, I will always win.
Do We Need More Trials For Calcium Stone Formers?
For me, no. It would seem a waste of money.
Some trials treated patients with reduced urine citrate, others did not. Some trials looked at new stones over 3 years, others at residual fragment growth one year after urological procedures. Will another 50 or even 100 cases be likely to change the outcomes? If so, in what way, and why?
It is true that one trial showed no effect and that trial was not blinded. It is actually a drag on the results as I did not remove it.
We Do Need a Trial of Citrate for Calcium Phosphate Stone Formers?
I do not know how often this must be said. Calcium phosphate stone formers must lurk in each of the trials I have reviewed, but I do not know their outcomes. One trial insisted stones be at least >50% calcium oxalate. That means perhaps a few had considerable phosphate is stones.
Calcium phosphate crystal formation is sensitive to urine pH whereas calcium oxalate stone formation will not be. The reason is that calcium phosphate supersaturation requires divalent phosphate be present, and the pKa for the second proton is about 6.8. Citrate salts can raise urine pH, so they can raise supersaturation with respect to calcium phosphate salts. On the other hand, citrate is an inhibitor of crystallization both because it is calcium binding and because it directly affects calcium crystal growth.
ROLE OF TESTING
The very same ACP report from which I derived the studies shown here presented an annoying set of comments that infers we might as well just give a drug like potassium citrate without knowing stone composition, or doing serum or urine testing that concerns stone pathogenesis.
For this reason, I offer some remarks on that subject. This is in the special context of citrate treatment. I have made more general remarks of a negative sort about the APC comments.
Does Stone Analysis Matter?
How can it not? I have already mentioned the problem of phosphate stones. Do we not have to exclude struvite is stones? The odd patient with cystinuria who has slipped by? Drug stones? Conversion from calcium oxalate to calcium phosphate stones?
Do Serum and Urine Testing Matter?
How can they not?
SERUM
Do we want to give potassium loads to people with reduced renal function?
Having prescribed potassium, do we not want to monitor for serious increase in serum potassium; some patients are older, some diabetic, some take ACE or ARB medications, some age or change drugs over the years we treat them.
Do we not want to diagnose primary hyperparathyroidism? You cannot without serum testing and 24 hour urine testing to be sure calcium excretion is not low.
24 HOUR URINE TESTING
If we do not obtain and measure 24 hour urine samples, how can we know anything? Some patients may have very high urine citrate levels. Some may have very high urine pH values.
Here and there urine oxalate is very high, from primary hyperoxaluria, or occult malabsorption syndromes, or very odd food habits.
People change their habits and develop diseases.
Moreover, people do not always take their citrate. Fall in urine ammonia in relation to urine sulfate, and rise in urine potassium assure one they are taking the drug.
URIC ACID STONES
Do We Need a Trial for Uric Acid Stone Formers?
NO
No one really questions that alkali salts will raise urine pH, nor that raising urine pH will reduce uric acid supersaturation and prevent stones. It is common practice. I doubt anyone will pay for or perform an RCT to test this question.
That they will not is very important, because it raises an unexpected question.
WHY NOT?
We Know the Chemistry
Uric acid is a large flat mainly hydrophobic molecule with most of its charge on a single proton receptor site. The protonated from has a very low solubility in urine of around 90 mg/liter whereas 24 hour urine uric acid excretion ranges from 400 to over 1000 mg daily depending upon diet purine loads. The pKa of the proton receptor site is about 5.3 in urine.
Given these facts we can calculate uric acid supersaturation from the urine concentration of total uric acid and the pH, along with minor adjustments for the effects of ionic strength on the pKa. High supersaturation will lead to a snowstorm of uric acid crystals. Raising urine pH to above 6 will generally reduce supersaturation below 1 and end uric acid stone formation.
Everyone Knows Alkali Work
There is a lot of uric acid excreted every day, so uric acid stones can grow rapidly. Uric acid gravel has an orange red color and is often seen. When alkali are given, the gravel goes away only to come back if patients miss doses. The absence of new stones is obvious.
No One Treats Without Stone Analyses
Who can be sure of stone composition without stone analysis? Even during treatment of someone who has produced uric acid stones, calcium oxalate or calcium phosphate stones may begin. So people know the stone type, and proceed by custom.
No One Treats Without Testing Serum and Urine
Uric acid stones are common in diabetics and people with reduced renal function; potassium loads are potentially dangerous. Perhaps this is more obvious among uric acid stone formers than calcium stone formers, although given wide spread use of ACE and ARB drugs and NSAIDS, potential risk is everywhere.
The amounts of alkali needed can be variable, and the only reliable way to ascertain is 24 hour urine testing. Likewise for compliance.
Therefore routine practice monitors before and during potassium citrate treatment of uric acid stones.
TRIALS ARE UNNECESSARY
IN this situation, no one has and probably no one will propose a trial of alkali for uric acid stones. But, there is an almost exact parallel situation for calcium phosphate stones, yet such certainty as pertains to uric acid stones certainly does not exist.
CALCIUM PHOSPHATE (CaP) STONES
Do We Need a Trial for CaP Stone Formers?
YES
WHY?
We Know the Chemistry
Calcium cannot combine with mono-valent phosphate but only with the divalent form. The pKa for dissociation of the second proton of phosphoric acid is about 6.8 in urine, although the precise value varies with ionic strength. Given the molarities of total phosphate, calcium, citrate – which binds calcium – and other ligands that have modest effects, the supersaturation of brushite – the usual initial urine CaP phase – can be calculated as well as we can calculate the supersaturation for uric acid.
Like uric acid, phosphate and calcium are abundant in urine, so the amount of crystal that can be produced in a day is similar to that of uric acid. Therefore stones can, and do, form rapidly and become large.
As in the case of uric acid, high urine CaP supersaturation can produce snows storms of crystallization; though certainly not common, patients can recognize this as white urine.
On physical chemical grounds, to lower CaP supersaturation below one and keep it there is to prevent CaP stones as surely as one prevents uric acid stones by raising urine pH and lowering supersaturation below one. Why, then, is not this treatment as self evident as alkali for uric acid stones?
Everyone Does Not ‘Know’ Treatment Works
We have no drug corresponding to alkali.
We can raise urine pH safely but cannot lower it.
Acid loads raise urine calcium losses and can be detrimental to bone mineral balance. Higher protein intake is a possible way to lower pH, but not all kidneys respond to acid with a prompt fall in pH. In some cases urine ammonium ion excretion will rise. In others, acid retention may occur. Urine calcium will tend to rise.
So treatment is not as transparent as for uric acid.
But Treatment Must Work Exactly the Same Way
We can lower CaP below 1 with fluids and measures – reduced diet sodium and thiazide – that reduce urine calcium, and we can monitor supersaturation as we monitor urine pH and uric acid supersaturation.
Furthermore, patients can tell if white urine has ceased.
Moreover, because stones are often actively forming, effective treatment is reasonably obvious.
However, these measures may be difficult to achieve. Thiazide is not always tolerated, reduced salt diet not always maintained.
Citrate is a powerful inhibitor of crystals, and it would be good to know if it were beneficial for the CaP stone former.


My urologist has me on 40 MEQ Potassium Citrate daily to prevent formation of uric acid stones. This is after the formation and eventual removal of a 6mm uric acid stone last year. My rheumatologist recently told me to start taking 400 – 500 mg of calcium daily to help deal with my osteopenia. Is it possible to replace the potassium citrate with calcium citrate to “kill two birds with one stone” so to speak and if so what would be the appropriate dose of calcium citrate to meet the two dosage objectives?
Hi George, 400 mg of calcium is 10 mmol, or 20 mEq, so it will at best be half of the 40. But I am not sure if this is even right because you will not absorb all the calcium, probably only about 20%, so I am not sure if you will get anywhere enough citrate. You can try but I am not very optimistic. Regards, Fred Coe
After 50 plus calcium oxalate stones in 3 years, my nephrologist put me on 60 mEq of potassium citrate (taken in two doses daily). I had been passing (or not) a stone or two, every three to four weeks. After starting potassium citrate therapy, I have been stone free for 6 months! It is cheap and effective, and as far as I know has no side effects.
The question would be, are there any side effects that I need to look out for?
Hi Richard, you are lucky: Good physician and the drug is effective for your particular situation. No risk. Regards, Fred Coe
Hi, my daughter was subjected to toxic mold at school. She saw a Functional MD who gave her physician strength Glutathione to bring about the mycotoxins for a urine mycotoxin test. My Daughter started having severe stinging pain in bladder area after taking 500 mg a day for a week. Any thoughts on what happened? People are telling me oxylates dumping, mast cell activation caused Interstitial cystitis, ect. I need a cure for this pain, this kid has been bedridden since January 2019. Im thinking she could not detox the mycotoxins properly because she has MTHFR a1298c. Please help, thank you. P.S all lab tests and ultrasounds have been done to rule out UTI, STI, candida, ect all normal. Binders have been used since end of January to help remove the mycotoxins but this pain is still there and debilitating.
Hi Donna, A review on PubMed of glutathione trials shows no evidence of bladder side effects. Oxalate dumping is a myth, such a thing does not occur. Glutathione does improve immune system function, but I found no papers describing mast cell activation. But I must add that as a professor I am broadly speaking here, as neither toxic mold not glutathione supplements fall within my area of specific expertise, and neither is related to kidney stones – which I actually do know about. Regards, Fred Coe
Dr. Coe, I am 52, male, 5’0″, 115lbs, lifelong joint damage from severe juvenile rheumatoid arthritis. Last month I began excreting anywhere from 5 to 15 stones with ‘gravel’ per day every morning for weeks. A urologist later deemed them to be ‘bladder stones’ as there has never been any pain associated. While waiting to see this urologist I lived on the internet trying to understand what was happening. To help my bones and joints I had been taking a daily combination of 5000iu of Vit.D3, 40mg collagen powder, Vit.K, Meriva(curcumin concentrate), magnesium, hyaluronic acid, and in hindsight maybe too little calcium in proportion. I stopped all supplements and nothing changed. I then tried adding some very basic supplements. When I tried a 280mg dose of potassium citrate the stones stopped over night! The PC makes me flush and a mild headache. I have arrived at the lowest effective dose being 210mg day. When I saw the urologist I asked him if I can make stones in 24 hours. He said not possible, it takes a while to form them and that the stones would be sitting in there for a while. I asked him if that’s the case then why does taking PC make me stop excreting them? He didn’t know. I’ve read forums where several people say they can form uric acid stones within hours. After an ultrasound he wants to do a cystoscopy as he said it showed a thickening of the bladder wall and a shadow which could be a stone. I’ve spent a total of 30 minutes with this doctor and I’m headed for a cystoscopy with no hematuria over 5 different samples, no 24 hr urine and no analysis of the 4mm and 5mm stones I brought him. His info says he’s been doing this for 19 years. I’m leaning towards a second opinion. It feels like him “not knowing” is him dismissing me. Is it that odd to be able to stop/start visible stones that quickly with PC?
Also, now that I’ve streamlined to just PC I’ve tried stopping it several times to experiment. If I don’t take PC the stones return the very next morning. I can literally stop/start it that quickly. Urine pH on PC has been 7.0 every time.
Hi Paul, Nice experiment. Surely they are uric acid, and I have already offered my main suggestions. Fred
Hi Paul, I guess the stones are uric acid, and the K citrate raised urine pH enough to stop their forming. You should have the stones analysed to be sure. UA stones tend to be red or orange, but not always. The sudden stopping with alkali is good evidence. Your dose is very low, so you may be at the threshold of forming them, and that is convenient for you. Of course uric acid stones form suddenly and can grow rather fast. I am not your physician so I cannot comment about cystoscopy. That is a decision for your physicians of record and there are considerations beyond stones. Regards, Fred Coe
Dr. Coe,. I have two uric acid kidney stones in my left kidney. I produce kidney stones of uric acid . I’ve had my Stones analyzed several times and they’re always uric acid.. My kidney doctor is trying to dissolve the stones with potassium citrate. My uric acid level in my blood is normal. I am taking 45 meq of potassium citrate daily. My Stones continue to grow. I now have one at 1.57 cm and one at 1.3 CM both in my left kidney. My doctor won’t do surgery on me cuz I’m a very high risk. I have left side heart failure, pulmonary hypertension and I’m 300 lb. Is there anything else we can do to get rid of these stones? I can’t do laser cuz he says I am too fat. If my urine is alkali at 6.25 to 7 pH why is the stones still growing?
Any help at all is greatly appreciated.
Hi Mary, If your urine pH is above 6 and the stones are growing they are not uric acid. They may have been but uric acid is not stable at so high a pH. Since the stones are so large ask him/her to measure the hounsfield units of radiographic density of the stones on your CT images, uric acid is very low compared to calcium stone crystals. Another matter, is your 24 hour urine pH over 6 or are these spot urines? The latter are misleading as long periods may have lower pH. Regards, Fred Coe
Hi Dr. Coe,
I have recently been prescribed potassium citrate 30 meq/ 2x a day for calcium stones and I’ve been trying to find information on how long patients typically stay on the medication. I’ve seen you mention that it may be months, years, or decades. How often do you recommend testing to determine efficacy/safety? And under what circumstances do you continue or discontinue potassium citrate?
Thank you for your time!
Hi Meagan, Great questions. I guess if stones have been a problem and the drug has reduced that problem importantly I would keep it up for years. Repeat 24 hour urine testing yearly, and blood likewise, is a prudent idea. If stones recur despite the drug I always look at repeat studies to figure out why, and change treatment as I need to. After a long while, most patients stop meds, but given how benign this one is, I am slow to do that if the benefit has been obvious. Regards, Fred Coe
hello Doc,
urine retention for 3 years now. detrusor muscle works fine, the lower spincter is the issue. possibly related to lumber L2 to L5 nerve issues the foley in dwelling over the last 3 years plugs up with calcium dust and chunks requiring frequent change outs.
irrigation just pushes it all back in to the bladder.
has the scope run into the bladder a week ago and 9 stones were pulled out . dark grey in color. 3 years of growth . largest one was 8 mm size\
the kidneys were scanned and are fine no stones .
Question : will potassium citrate help keep urine ph lower and slow down calcium dust and new stones from forming at a slower rate. ?
please advise. thank you.
Hi David, You need to get the crystals analysed and figure out if they are calcium phosphate, uric acid, struvite – from infection. Without knowing what it is how can one decide how to prevent it? Potassium citrate will raise urine pH, so that would help if it is uric acid. Regards, Fred Coe
Hi Dr Coe. I have been diagnosed with Cystinuria about 4 years ago now. I’m on many different types of medication to help stop formation of stones and to avoid them growing to big. I’ve had 9 laser surgery a to remove the stones and a kidney removal since diagnosis. I’ve just been put on effercitrate tablets (two, three times a day), instead of Sodium Bicarbonate! Which one do you believe helps alkaline the urine better? Thanks
Hi Cindy, Treatment of cystinuria depends on a lot of changes – high fluids, alkali, reduced protein, and meds. Potassium alkali is preferable to sodium as higher sodium loads can raise urine cystine losses. If stones persist your physician might want to consider having you evaluated at a stone center to be sure treatment is optimal. Regards, Fred Coe
I have found this forum to be extremely informative and useful. My partner has a suprapubic catheter, and we perform citrate-bladed irrigation three times a week (it was originally daily). We continue to experience persistent problems with catheter blockages associated with calculus and biofilm buildup, all linked to multi-resistant organisms acquired in the hospital. At least three times a day, I need to vent the catheter to release gas. If this is not done, it causes pressure, retention, and obstruction.
Additionally, the only way to maintain urine flow is by using a high-flow urometer-type catheter bag, similar to those used in critical care for hourly urine collection. I consistently ensure that his fluid intake is at least 2 liters in addition to his usual minimal oral intake, which is limited due to his aspiration risk.
I would like to know if anyone has encountered similar issues in their practice and if there is a more effective way to manage this situation.
Many thanks
Hi Karl, I am not expert in this very serious problem. I will leave it up in hopes someone will add their experience. I have written about infection stone, and presume part of the crystal build up may be struvite. Best, Fred Coe
My husband has a history of large kidney stones, this February he had surgery to remove large13 mm stone and one from his bladder. In November, he again had a bad stone attack and had to go to the ER they found two stones measuring 7mm and 8mm with a number of small ones. The surgeon told me after surgery that he was concerned he suffered from Cystine stones. They also are afraid his left kidney may have suffered serious damage and may need removed. It has at least two large stones measuring 1.2 cm and is atrophic. We are awaiting test results as well as our follow up appointment 12/10… but the stone analysis came back Calcium Oxalate Dihydrate (Weddellite) 30% Calcium Oxalate Monohydrate (Whewellite) 35% Carbonate Apatite (Dahllite) 35% and the 24 hr urine came back with very low citrate and magnesium. The test results mention Hypocitraturia . To me it seems like he’s an oxalate stone former. Wouldn’t cystine show up in one of those results..? Urologist is recommending lifestyle change of plant based based on cystine stones in order to keep right kidney healthy. Just want to be prepared with questions to ask. My husband has never really delved into why he gets them. This is new for us. So want him to begin to take ownership of his health. He’s 42. Thanks.
Hi Jen, Your husband forms calcium phosphate / calcium oxalate mixed stones and not cystine stones. He needs a full evaluation as to the cause of these stones. Here is a reasonable starting place. Of his physicians are entirely responsible for his care, but I would submit that testing be complete and treatment based on the results. The atrophic kidney may have been damaged by chronic obstruction from a stone or perhaps was never properly formed at birth. Either way he has only one normal kidney so prevention is paramount. I would view his situation as very complex and potentially high risk in the case of new stones on the right – the good side. Perhaps these comments may be of use to his physicians, but of course they know far more about his case than I do being distant and without any more information than is in your note. Regards, Fred Coe
Hi Dr. Coe – I had a 10+mm stone back in July. Unfortunately my urologist at the time never got the stone or its fragments tested for composition. I am now seeing another urologist. In September I passed another small stone which was diagnosed as a uric acid stone. I later did a 24hr urine test, and all results were good except pH was 5.0. I have been taking 4 – 10 meq potassium citrate tablets daily, and my pH is still less than 5.5. My urologist said I should now take 6 – 10 meq potassium citrate tablets daily, but he would not recommend increasing the dosage over that amount. What if this new dosage does not raise my pH? What will be my options then? Thank you for your time.
Hi DClewett, Your urologist is doing what I would do in that 60 mEq of K citrate is a reasonable dose when urine pH stays low. Often, one needs even more alkali, and sometimes that needs to be sodium alkali if potassium becomes limiting. Of course your next 24 hour urine will tell you if more alkali is needed. If it is, then your physician will have to choose more potassium citrate – and follow serum potassium closely for a while – or add sodium alkali. One way or another urine pH will rise and uric acid disappear. Regards, Fred Coe
Hi, I recently had my second round of kidney “gravel”. The first was one year ago. The first stones were not analyzed, but the recent stones came back 80% calcium phosphite and 20% oxalate. Two to three years ago we installed a sodium based water softener. Our water was fairly hard, so the salt in our water greater than the average water softener. I drink a lot of water, around 3 liters a day. Do you think that my sodium consumption change could be significant to the formation of calcium phosphite crystals?
Hi John, If you have genetic hypercalciuria, sodium loading can raise urine calcium and foster stones. I would suggest a proper evaluation for stone prevention, which will show the urine calcium and sodium and all the rest, too. So, the extra sodium may have been crucial but measurement beats guessing every time. Regards, Fred Coe
Thank you for being so kind to answer my questions. I am 300 lb. I have been producing hundreds of uric acid stones for years. I was put on a potassium citrate regimen to try to melt a kidney stone that was 1.3 CM. I have been on the regimen for about 6 months. They have me taking 60 meq use a day. The stone keeps growing. It is now 1.9 cm . My surgeon measured the density to make sure it was a uric acid Stone and it is. I also take a hundred mg of allopurinol a day. Why would it keep growing instead of getting smaller? I am not a candidate for surgery because I suffer from pulmonary hypertension and heart failure. I would hate to die from a kidney stone and leave my children all alone in this world. What else can I do? My blood uric acid is always normal my urine pH level is always above 6. Please help. Thank you
Hi Mary, You are urine the right medication and your urine pH is right for stone dissolution. I gather your 24 hour urine pH is above 6 and occasional spot urines as well. The uric acid crystal cannot grow if urine pH is at 6 or more on average so something else is happening. Perhaps the pH is low more of the time than you think even if the average is above 6. Perhaps the stone is ammonium acid urate – this occurs when urine ammonia is very high. Your 24 hour urine can tell you this. Perhaps your urine has abundant calcium and at the higher pH you are adding calcium phosphate to the uric acid stone. That would not be identified by HU right away. All these are mere suggestions to your physicians. Regards, Fred Coe
Thank you for all the info in these articles.
I’m 29. First had a red/orange gravel stone 2 years ago, then 1.5 years later, and another one today(6 months later). In all 3 occasions over the past 2 years pain onset was rapid and after drinking 80+oz of water over 1.5 hours the stone passes when urinating (I’m able to see it in the toilet). So from start to finish, pain to passing stone, is about 2 hours. Then I feel perfectly fine. No notable symptoms before or after the event.
I’m trying to figure out what is causing them. All I drink is water and plenty of it, 80-100oz per day.
You did say one thing that confused me
“Perhaps this is more obvious among uric acid stone formers than calcium stone formers, although given wide spread use of ACE and ARB drugs and NSAIDS, potential risk is everywhere.”
I take NSAIDs like Aleve a few times a week for cronic foot pain.
In this statement are you saying NSAIDs can cause Uric acid stones?
Any info on my situation would be helpful, should I take some type of supplement to help with this?
I haven’t seen my PCP about this because onset and relief is so rapid.
Thanks
Hi Dillon, I know of only one orange stones, which is uric acid. The phrase you quoted was: “Uric acid stones are common in diabetics and people with reduced renal function; potassium loads are potentially dangerous. Perhaps this is more obvious among uric acid stone formers than calcium stone formers, although given wide spread use of ACE and ARB drugs and NSAIDS, potential risk is everywhere.”. Potassium loads are a worry in the above mentioned situations, which you do not fit into apart from using NSAIDS. You need to collect some of the orange gravel and be sure it is uric acid. Perhaps it is another crystal. Your physician needs to know because perhaps uric acid stones have formed in your kidneys – usually a low dose CT is best to see them. Finally you need serum and 24 hour urine testing to be sure it is low urine pH causing the stones as apart from other causes – like an extreme loss of uric acid into the urine – rare but not unheard of. Please do all this as uric acid stones are very uncommon at 29. Regards, Fred Coe
I apologize for posting this again, but I think I posted it previously on an obscure web page on this site.
Dr. Coe,
They discovered a 1.3 CM L x .8 mm W stone in my left upper ureter on Feb 2nd causing blockage of my ureter with moderate hydophrenosis. I was in pain for a few days and then the pain subsided on its own. On Feb 21st I had ESWL procedure and passed a lot of fragments over the next week and a half. 167.0 mg of 80% CalOX Mono and CalOx Dihy with one 4.0 mg Uric Acid Stone as well.
I had another xray performed on March 6th that showed the stone was still in the same place and appeared just as large? Hard to believe considering how much I had already passed. Regardless, my doctor wanted to wait 3 more weeks to see if the rest would pass? I guess he did not feel the blockage was significant or still there?
After the three weeks I had another xray done and an ultrasound. Pretty much looks the same and in the same place. The ultrasound revealed cracks in the stone, but it also revealed mild hydroprehnosis. The left ureter jet is showing urine is still flowing past the stone and into the bladder, but the left kidney is retaining a lot of urine. My Dr. wants to act now and I had a complete urinalysis done, as well as BMP Serum, and CBC Auto Diff in prep for ESWL on March 27th. Everything came back normal, but I can’t get anything done this upcoming week due to the hospitals and Stones Clinics in New Jersey are shut down this upcoming week due to CoVid19. I do not know how long they will be shut down?
1. What can I do in the meantime to try to protect my kidney? As I said, some urine is still passing through the ureter jet into the bladder, but urine is backed up in the left kidney.
2. Is the left kidney still working under these conditions? Meaning, is it still filtering and producing more urine even though it is backed up, as the ultrasound is showing urine passing into the bladder via left ureter jet.
3. What is your best advice for me considering this scenario and in light of the closure of surgical centers in NJ at this time. My Dr just tells me if I have pain go to the emergency room.
I appreciate any insight as I am really feeling lost and so concerned as to what to do.
Hi Steve, No; it is not an obscure place and I answered you. It is fine to ask again. Good luck, Fred
I’m under the same situation as OP. If already answered, Can you please provide the link/copy-paste answer here once again.
Hi Suresh, I am sorry but the design of the site does not make it easy for me to find ‘OP’ from this page. Can you write back about your issue, and I will be happy to help. Fred
Uh, ‘OP’ means the original poster. He’s talking about STEVE.
Sigh…
Dr. Coe,
What do you think about this protocol? I have found two successful cases on PubMed involving high doses of Boron and antioxidants?
https://www.ncbi.nlm.nih.gov/pubmed/25110210
https://www.ncbi.nlm.nih.gov/pubmed/23641791
Thank you,
Steve
Hi Steve, I am not enthusiastic. If the kidney is compromised by obstruction and in danger of damage, it needs surgery, else things can wait. In the meantime I would not pursue promising but odd interventions. By the way, given uric acid in one stone, there is no loss from beginning potassium citrate in the waiting period – your physician needs to prescribe it. Regards, Fred
Are you aware of any further study on use of hydroxycitrate since a 2016 very-preliminary study at University of Houston
(
Jihae Chung, Ignacio Granja, Michael G. Taylor, Giannis Mpourmpakis, John R. Asplin, Jeffrey D. Rimer. Molecular modifiers reveal a mechanism of pathological crystal growth inhibition. Nature, 2016; 1 DOI: 10.1038/nature19062) on clinical use, long-term safety, efficacy etc for reducing calcium oxalate stones? This article suggests potential superiority of efficacy and tolerability averting high potassium loads as well.
Hi Don, A brief search on Google found this trial that David Goldfarb opened in 2017. Likewise, it found a ridiculous article using it in fruit flies. Given oxalate flies form a calcium oxalate crystal – well known fact – leading scientists to employ the fly as a model for human stones. I also found a review of the molecule. One of the authors, Dr John Asplin, worked with the original group and is a superb scientist. Finally health food retailers outnumbered scientists by orders of magnitude. It is proposed for weight loss in people. What I think is this: It is widely available as a food supplement and cheap. Undoubtedly safe, by this time, as ample experience in the shadow kingdom of supplements would have disclosed real dangers. If I made it a popular item on my site, it would become very widely used by stone formers. I demur because – I suppose – I cannot bring myself to do it. No science, no place here. But, it does work chemically, and if you eat it it can get into the urine. Fred
If dealing with a kidney stone; and an alkaline urine pH (8) (spot check; collected in between bouts of pain):
-might it be reasonable to assume (elevated urinary calcium; normal serum uric acid; and until proven otherwise) it to be a calcium oxalate dihydrate stone?
-although citrate supplements (K; Mg) make sense (to reduce urinary calcium excretion), would it further alkalinize the urine, and if so, would that potentially have an adverse effect on kidney stone formation/excretion?
Hi Richard, I never base treatment on guessing if I can find out. The alkaline urine – if present in a 24 hour sample, for averaging – would suggest calcium phosphate stones. I gather you had such a urine as you mention a high urine calcium. Here is a good start on an organizing template to follow in getting your situation fully analysed. See what you think before trying a remedy. Regards, Fred Coe
Calcium oxalate stones:
Beyond the use of citrate to reduce urinary calcium excretion, is it a good idea to generally recommend eating more foods that acidify an alkaline urine (calcium oxalate dihydrate), e.g., cranberries; or alkalize an acid urine (calcium oxalate monohydrate), e.g., lemon?
Hi Richard, In line with my prior comment, I would do nothing until I knew the stone composition – if possible – and had complete 24 hour urine data and also assurance that no systemic cause of stones was present. The Chapter One reference in the prior note is the safest one to follow in getting to a final answer. Regards, Fred Coe
What is the best source of citrate OTC or prescribed .?
Hello, Doctor, Rx K citrate 10 mEq tabs is the ideal. OTC have too little K citrate per dose. Fred
In my case even the same dose of the OTC K citrate (in unwieldy powder form) resulted in a significantly lower urinary output of citrate versus Rx. Which begs the question, do OTC formulation have a greater chance of not being what they say they are?
Hi David, Potassium citrate is just that, so perhaps you might want to check out how you calculated your dose, that the stuff you bought is indeed pure food grade potassium citrate, and that you have proper equipment to weigh it out. The usual OTC I have read about on this site is just food grade potassium citrate. Fred
Do you do private phone consultations? Please reply to my supplied email address. Thank you.
Hi Franklin, I do consulting via Zoom as part of my employment as a professor of medicine at University of Chicago. My clinical secretary is Banita Williams and her phone is 773 – 702 – 1475. She can make arrangements for you. Regards, Fred Coe
Is Magnesium Citrate a possible therapeutic agent for Ca phosphate stones? As opposed to Potassium citrate, which is more commonly given? And baffled and frustrated by the ridiculous low level research that hyperfocuses on Ca oxalate stones to the detriment and neglect of studying Ca PHOSPHATE stones. They just LUMP all the Ca stone formers into one size fits all analysis. Stop it already. I can’t.
Hi KimO, Magnesium citrate will raise urine pH as will potassium citrate and therefore is untried as a remedy for calcium phosphate stones. Such stones form when urine pH is high. Whereas urine citrate inhibits the initiation of calcium phosphate – and calcium oxalate – stones, added medicinal citrate raise urine pH so the supersaturation with respect to calcium phosphate crystals rises. Absent trials, I work at lowering urine calcium – as noted in the initial linked article. As for research on the phosphate stones, I agree with you, but the NIH has its own ways, and not I have ever made any impression on them. We have done some research on the phosphate stone issue, and NIH paid for it, but the trial we really need seems beyond reach. Best, Fred Coe
Hi Dr. Coe,
You wrote in one of your respnoses to a question here that magnesium citrate will raise urine PH. I have uric acid stones. My urine PH iis almost always between 5.0 and 5.4. I’ve tried potassium citrate, but unfotunaely, couldn’t tolerate it. Would supplementing with magnesium citrate be a good alternative? Thanks..
Hi David, I did not mean to say that magnesium citrate is useful for uric acid stones, but perhaps I wrote in error. Given these stones you need alkali. If K citrate is not acceptable mere sodium bicarbonate tablets – OTC, 10 grain, 2 three – four times a day – is acceptable. There are new OTC mixtures like Moonstone and perhaps the taste etc will work for you. Crystal light lemonade is high in potassium citrate, and a liter daily will help raise urine pH. Since raising urine pH to about 6 cures – prevents – uric acid stones, you really should want to achieve that goal. Regards, Fred Coe
Thanks, Dr. Coe..
With regards to the magnesium citrate, you wrote in your 7/2/21 response to KimO on this page that “Magnesium citrate will raise urine PH as will potassium citrate….”. I’ve taken about 270 mg of the citrate daily for 2 days. According to the dosing instructions on the pill container, that’s about 2/3 of the recommended daily allowance. I know that’s not a huge dose and I know taking it for 2 days isn’t a long time, but after 8 tests with a PH meter over that period of time, my urine PH has risen from a range of 5.0 to 5.4 to a range of 5.7 to 6.2. Could this rise be a result of the magnesium citrate intake or most likely the result of something else? As I mentioned in my original post, I have uric acid stones and am hoping a rise in PH will prevent new stones from forming. I plan to continue testing.
One other question… If I’m diabetic and have stage 3 kidney disease, would magnesium citrate be safe to take on a daily basis? I was reading that it may not be for someione who’s in renal failure. Thanks..
Wow, good reader! I had forgot the comment. Magnesium citrate nonahydrate has a mw of 613, so you take 270/613 or 0.44 mmol but with a valence of 3 giving 1.3 mEq of alkali. That seems way too small to raise urine pH. Trimagnesium bicitrate may be in these OTC materials,, MW is 451 so you are taking 1.9 mmol with a valence of 3 for 5.76 mEq of alkali. I suspect that is the material, and this amount of alkali could raise urine pH a bit. Most magnesium is in cells, and even with mild renal insufficiency I am not overly concerned about 2 mmol/d. But uric acid stones are worrisome, and why use an odd preparation like this when potassium citrate is so much more effective (a lot more alkali)? My concern is that 24 hour urine pH, the real force for crystal formation, will not rise to 6 or more and you are getting just time samples – for example think about overnight. Regards, Fred Coe
The 270 milligrams of magnesium citrate I’ve been taking daily only keeps me in the 5.8 – 6.2 PH range for about 10 hours, so I’m planning to increase the dose to see if I can maintain that range for a full 24. Unfortunately, I wasn’t able to tolerate the potassium citrate or the sodium bicarb for very long.
On Tuesday, I’m scheduled for a utereroscopy to remove a number of kidney stones, the largest, 1.6 mm. This will be my 2nd utereroscopy in the past 2 years. At 57, it seems I’ve become a stone former. This makes me sad. After my last utereroscopy, my urologist had me take a couple 24 hour Litholink tests to determine my stone risk. The first test, about a month post surgery, The second, about 6 months later. Each test result showed a urine PH below 5.5. My urine volumes were also both low, under 1.4 liters. My urologist wanted me to increase my water consumption. Doing that, unfortunately, didn’t increase my urine output, It only raised my blood pressure. Now, I only drink when I’m feeling thirsty.
Hi David, Your story illustrates the real complexity of working out a prevention program. If, for example, increased water intake raised your blood pressure, then there is a need to consider why – this is not a common outcome. Likewise, if you cannot tolerate even sodium bicarbonate, why not and what can be done as an alternative. Given uric acid stones and perpetual low urine pH and volume, of course risk of new stones remains. Rising blood pressure from water increase is not common, but needs to be gotten around. Perhaps, your physicians might with to consider seeking additional consultative input from somewhere convenient to your location. Regards, Fred Coe
Dr Coe,
I’m 60 year old male who just developed his first kidney stone after moving from Chicago to Arizona (the Stone Belt I’m told). Lithotripsy last week seemed to work well as I’m passing small stones (probably calcium oxalate). Besides drinking a lot more water, could you impart one other recommendation to lessen the chances of another stone? Magnesium and B6 are often mentioned. Thank you.
Mike Davitt
Hi Mike, The only reasonable approach is to get fully evaluated. I presume you have long harbored stone risks and the move has brought them into the daylight. Please do not guess, the workup is cheap compared to even one stone surgery. Regards, Fred Coe
Hi Dr Coe. I have mostly uric acid stones with a tiny bit of oxylate. I have tried potassium citrate, sodium bicarbonate and moonstone. I can’t tolerate them. I am dairy free and get very little calcium. My urologist said to try citracal calcium 2 times a day. It has zinc, manganese , copper and D. Will this supplement prevent uric acid stones?
Hi Holly, Uric acid crystals form at low urine pH and dissolve at a higher one so anything you do to raise pH will stop them. Crystal Light lemonade will raise urine pH, a diet rich in veggies and fruits will help – try putting both together. Calcium citrate is also fine and the calcium will be good for bones. If you cannot tolerate potassium citrate or sodium bicarbonate as treatments, perhaps you could tolerate smaller amounts to use on top of the lemonade – one OTC sodium bicarbonate 4 times a day is not much but this would give you about 20 mEq of alkali. Mix and match till urine pH is about 6 in a 24 hour collection. Regards, Fred Coe
Hi Dr Coe.
Many thanks for this article. I am not at all a scientist, much less a chemist, so I hope that you can be patient with me! You talk about Citrate, but – just to be clear – are you saying that taking Calcium Citrate will reduce the instance of Calcium Oxalate crystals in the urine/kidneys etc? Why would the Calcium element not lead to greater instance of crystals?
Many thanks in advance
Hi Mark, I said potassium citrate (or there is a typo I need to fix). The citrate you take is metabolized to bicarbonate and the latter signals the kidneys to release citrate into the urine. Regards, Fred Coe
Hi Dr. Coe
My pshiquiatrist recommended i take magnesium for helping with my burnout. I was wondering which would be best for me, magnesium citrate, magnesium oxide or magnesium glicinate. I tend to make kidney stones, although they are so small i cannot seem to find them. Thanks
Hi Maria, the form I most urine is magnesium oxide. As for the stones, you might collect some and get them analyzed so you know what they are made of, and prevention might be of value. Magnesium oxide is not likely to cause or worsen stones. Regards, Fred Coe
Dr. Coe
Thank you so much.
I have 300 mg magnesium oxide pills to take. Am taking one per day.
I think my stones are more sand and although I use a strainer, I have not been able to catch any. 🙁
Kind regards
Maria
Hi Dr Coe,
Just wanted to let you know that I appreciate your writing. My urologist doesn’t have time to talk in detail, so being able to read your articles is very helpful. Thank you for sharing your knowledge with the wider community – it’s important to have this information from a vetted Urologist resource such as yourself on the internet open and free to all. Thank you, Julie
Thank you, Julie. Fred
Greetings.
This area of science has been a confusing minefield of sometimes-conflicting data, and certainly inscrutable advice at times, even though I’m certain it all comes from a place of care and trying to be helpful.
Quickly, my story, and then my questions(s):
I was diagnosed with Type 1 Diabetes in 2019 and immediately turned to a low-carb diet as a way to best manage my condition. This low-carb diet, in hindsight, also meant a high-oxalate diet (large amounts of almonds, almond flour, peanuts, peanut butter, raspberries, etc. as my primary snacking foods).
Then, in early 2022, I was diagnosed with low blood platelets and low HDL cholesterol. So, turning to the internet to get some natural solutions, I started loading up on spinach, wheatgrass, and chia seeds as well, on an almost-daily basis.
Then, in May 2022, I passed my first stone. And the CT scan in the ER showed another stone in my lower left pole of my let kidney as well. So, suddenly, two stones. Turns out, I passed 2 stones over a 72 hour period, yet the stone in my lower left pole is still there, so I do not know where that other stone came from! In any case, I got one of the stones tested and it was Calcium Oxalate.
I immediately went on a low-oxalate diet, and a few months later did the 24-hour urine analysis and found that my citrate levels were low (189mg), my oxalate levels were high (65mg), Ammonia was high (63mEq), and Uric Acid was high (980mg). The rest of the metrics were within range.
With this, I went to a Nephrologist and he recommended the following treatment: 15mEq potassium citrate 3x/day and a low dose of hydrochlorothiazide (which I am having at least some initial adverse reactions to).
He also said that there’s no convincing evidence to-date that low-oxalate diets impact future stone creation — that it’s far more about getting these “break down” components (like citrate) readily available (along with plenty of fluids) to do the work that needs to be done to ensure no crystal formation happens.
I am surprised by these recommendations (esp the lack of data supporting low-oxalate diets!), and I was curious what your perspective is on this regimen that has been prescribed for me.
Any insights deeply appreciated!
Thank you.
Hi Jon, There are some complexities you mention, and I do not know enough about your particular case to make any strong statements. The low platelets must have a cause, and I do not know what that is. I understand you ate considerable amounts of high oxalate foods, had a high urine oxalate level and that despite a ‘low oxalate diet’. The usual reason for high urine oxalate despite attention to high oxalate foods is too low a diet calcium. Another is a very high protein intake, for which you offer some evidence – high urine ammonia and uric acid; the former is a common response to the acid load from cystine and methionine in meats (or legume species), the latter is from the purines in DNA and RNA, both high in the same sources. The low citrate may be from the acid load or an additional problem for which I would need a lot more data. I can understand the use of alkali and possibly a thiazide, and I understand that there is a miscommunication as well. There is no trial data for low oxalate diet per se, merely a strong epidemiological link between higher urine oxalate levels and new onset of stones. But I am sure that lowering urine oxalate would be reasonable. Yet your whole diet is so biased toward acid load! Another issue is your diabetes. Diabetes alters acid balance, lowers urine pH, but does not generally raise urine ammonia. One could have to relate your urine ammonia total acid excretion to fully understand things, and you do not offer enough information for that. Your nephrologist will know all this, and probably has already considered the diabetes effects, as the research group at Dallas SW medical school has published a lot on the subject. I hope this introduces at least some of the issues, and explains why there seems to be a conflict. Regards, Fred Coe
80 yeas old with an ileostomy and years of kidney stones with several lithotripsy procedures. Recently passed a 5mm kidney stone and multiple weekly smaller stones. Oct. 5, hospitalized with blood infection plus a 6 mm kidney stone blockage, stent was placed. Stone analysis just received.. 80% Uric acid dihydrate; 20% calcium oxalate dihydrate. Currently on daily deptomycin antibiotic infusion until November 25 for blood infection (pacemaker had to be removed and had vegetation on mitro and tricep valve). What would you recommend to reduce the incidence of these stones?
Hi Herbert, Ileostomy usually produces uric acid stones and they can be abolished with alkali. Usually I use simple OTC sodium bicarbonate tablets because GI sodium losses are significant and the pills reliably make the urine alkaline so uric acid cannot form. Do not begin these pills without discussing them with your physician as there may be other issues, Potassium citrate is the usual prevention for uric acid stones. If you have low blood potassium and need more potassium your physician may want to use them. You must have 24 hour urine testing to be sure the dose of alkali is sufficient to raise urine pH above 6. Typically this requires 2 OTC 10 grain sodium bicarbonate tablets 4 times a day. Be sure to discuss this with your physician, as I am not the one responsible for your case and he/she is. Regards, Fred Coe
But how did my citrate get so low (<47) to start with? I eat primarily plant based, 3 servings of fruit, 3-9 servings of veggies a day, 2 servings of fish a week. 10-15g sugar, 1200-1700mg sodium. With k citrate and lemon juice, it's up to 297, but still a long ways from 500. And everything else is now normal. So, is there some systematic problem somewhere else?
Hi Kim,
Do you have any malabsorption issues from illness or past surgery? Have you consulted your doc about why your citrate might be on the low side? Were they able to provide some answers?
Jill
I’ve had red gravel off and on in my urine for several years. Is red gravel exclusively uric acid? Or could it be calcium? I’m going to see a doctor when the new insurance kicks in in the new year, but thought I’d get educated before. Because I jog I’ve been taking potassium and magnesium supplements, worried that I might be sweating out too much. About a year ago I had a bladder stone removed. But never got a clear answer from the doctor about the type of stone.
Hi John, red gravel is the very mark and make of uric acid crystals/stones. But certainly collect some and get it analysed – medicine is based on whatever certainties we can marshall! When UA ia proven – even before – add alkali. It can be potassium citrate 10 mEq tabs 2 twice a day or more depending. But this all requires both crystal confirmation and 24 hour urine testing to determine just how overly acid your urine is, and also your tolerance for potassium (there is blood work, too) and other factors that cause stones. Here is what to get done. The article you wrote on has the treatment options. If it is uric acid, and if your treatment is sufficient, and if uric acid is the only crystal, and if there are no other stone risks in the 24 hour urine, alkali should be a cure – so long as you take it. Regards, Fred Coe
Hi Dr Coe
Since it’s the citrate that ultimately elevates pH, can you explain why calcium citrate is not as effective as potassium citrate for that purpose? I need to increase calcium intake anyway and am dealing with uric acid stones.
Thank you
Hi Brett, Generally it is a matter of amount. Calcium citrate contains 2 citrate molecules and 3 calcium atoms and 4 water molecules to make a crystal, and has a molecular weight of 498 mg The molecular weight of citrate is 192 mg and the atomic weight of calcium is 40 (all in mmol). Each citrate can produce 3 bicarbonate molecules it if is fully metabolized as citric acid. So for every 6 mEq of alkali one gets three mmol (120 mg) of calcium. We need a minimum of 20 – 30 units (mEq) of alkali a day to raise urine pH in a uric acid stone former giving – as an illustration – 30 mEq needed dose /6 mEq alkali per unit calcium citrate or 5 mmol of the crystal. It will contain 5 x 3 = 18 mmol of calcium or 720 mg. This seems reasonable as total calcium intake should be 1000 to 1200 mg/d. So calcium citrate should be alright provided all of the citrate is metabolized to bicarbonate, which is not certain. Put another way I would not mind a patient of mine trying calcium citrate so long as we measure the 24 hour urine outcome and ascertain pH has risen and urine calcium (we are adding supplement calcium, not food calcium ) is not too elevated. Regards, Fred Coe
Hi,
Retired 68 year old male internist here.
Follow up question. You said you would not mind a patient trying calcium citrate as long as urine calcium is not too elevated.
My brief hx; calcium oxalate stone, idiopathic osteoporosis, IBS (I avoid dairy), 24 hr urine studies normal except low citrate. I took K citrate for a while, but can no longer tolerate it due to GI upset. Recently I’ve been taking Citracal calcium citrate 3 per day (with meals) which is 600 mg elemental calcium.
Urine calcium before Citracal was 157-174, after Citracal was 243. Urine citrate was 151-185 before, after Citracal was 565 (was 681 when I was on k citrate 40 meq/d). After Citracal, urine sodium was 153. vol 2100.
So, nice response in the urine citrate, but urine calcium higher. Should I be concerned about the urine calcium? I’ll try to control my sodium intake better and increase my fluids a bit more.
My stone history is really not too bad, first one was as an intern in Milwaukee in 1981 (labs all normal, but this was before urine citrate studies, stone was calcium oxalate), second one in mid 1980s, then none till a renal ultrasound in 2016 showed solitary stone in left kidney that did not change for 4 years.
Thanks, your website is great!
Chris
Hi Doctor, YOu have genetic hypercalciuria and have long used a low calcium diet – for good reasons – and have bone mineral depletion as a consequence. I cannot say much about the low citrate because you do not say what urine ammonia, or sulfate were, nor serum or urine K. It could be genetically low, low because of GI alkali losses or K losses or both. My focus would be on bone, and a plan to maintain better diet calcium intake with low enough diet sodium to prevent excessive urine losses. I would use 24 hour urine panels that include the above measurements – Litholink is the best we have in US (I founded it, sold it to LabCorp in 2006, and have NO interests in it). Best, Fred
I take potassium and magnesium citrate, but had been inconsistent with the potassium. I recently passed a stone and attribute it to a recent, but significant increase in coffee, sugar and salt (Easter candy and ham….). Good incentive to eat only uncured meat and no candy. I had one stone analyzed and it was calcium oxalate. I also need to cut back on coffee and chocolate
Hi Dean, Be sure to get fully evaluated so you know what treatment might aim at the causes of your stones. Potassium citrate is not a general nostrum for stones, and may be a problem of itself. Regards, Fred Coe
Hi! And thank y ou in advance.
I am 57 and just found first stone, .5mm. I immediately cut down my salt, increased my water to 3 liters/day, daily fresh lemon juice and did a 24 hour urine test:
Citric Acid 385
Uric Acid 428.4
Calcium 347*high
Magnesium 94.5
Oxalates 17
Sodium 144
PH 8
I was told Sodium was normal, but i believe its actually high.
I have researching like crazy and your site is the best!
Im wondering about adding dietary calcium (i eat none from dairy sources, so only whatever i get in veggies and fortified stuff, i imagine does not add up to 1200) because I believe high urine calcium is calcium leached from my bones, not from diet excess (my blood calcium is normal). I have read your and Jill’s info about it and i understand.
Also wondering about taking citric acid via lemon or ACV daily or other added (Mag or Potass citrate, as i recently heard NOT to add any citrate because my PH was so high, this I DO NOT UNDERSTAND, can you help, based of my results?
Thanks again
Hi Cara, You have very high urine calcium and indeed have a lot of urine sodium. If your blood calcium is normal, the likely problem is idiopathic hypercalciuria.In that setting the kidney stone diet applies. The key is to lower diet sodium (1500 mg) before adding diet calcium. In your case oxalate is already low, so you would use perhaps 800 mg of diet calcium for bone. The high pH and modest citrate are unclear as to cause – I would need to know more. But in saying this, I must make clear I do not know your medical situation and please do not act on what I say but rather mention to your physician who is in charge of your care. She/he knows your actual condition. Best, Fred Coe
Hi! And thank y ou in advance.
I am 57 and just found first stone, .5mm. I immediately cut down my salt, increased my water to 3 liters/day, daily fresh lemon juice and did a 24 hour urine test:
Citric Acid 385
Uric Acid 428.4
Calcium 347*high
Magnesium 94.5
Oxalates 17
Sodium 144
PH 8
I was told Sodium was normal, but i believe its actually high.
I have researching like crazy and your site is the best!
Im wondering about adding dietary calcium (i eat none from dairy sources, so only whatever i get in veggies and fortified stuff, i imagine does not add up to 1200) because I believe high urine calcium is calcium leached from my bones, not from diet excess (my blood calcium is normal). I have read your and Jill’s info about it and i understand.
Also wondering about taking citric acid via lemon or ACV daily or other added (Mag or Potass citrate, as i recently heard NOT to add any citrate because my PH was so high, this I DO NOT UNDERSTAND, can you help, based of my results?
Thanks again
Hi, I have been a life long Calcium/Oxalate kidney stone former. Allpourinol seems to help. Currently prescribed Potassium Citrate (10meq 3 times a day). I assume from reading the thread above that this will also help greatly. Question. Currently in Mexico and found Potassium Espirulina much cheaper. I assume this is not equivalent since it does not have Citrate. I see from the thread that Citrate is a key ingredient. Can I take a seperate Citrate supplement to make the 2 separate drugs equivalent to Potassium Citrate?
Hi David, it is a preparation of cyanobacteria and will not provide very much alkali. I would hope you have been or will be fully evaluated for cause of stones. Allopurinol as a remedy was first described by me, and has one excellent trial, if it worked perhaps you are best with it pending some other causes come to light. POtassium citrate is reasonable only if your urine citrate is low or you have uric acid stones. Regards, Fred Coe
Hello,
If pH is high at 8, but citrate is 350, is it safe or unsafe to take lemon juice or any other citrate?
Only other high value is Calcium at 350.
Thank you
Dear Caar, possibly pH is high from infection with bacteria that possess urease.Possibly citrate is low because of genetics, or high protein load, or some systemic cause. You do not give me enough to go further. The high urine calcium may be a main cause of stones by itself, and require specific treatment. That is all I can offer based on so little information. Regards, Fred Coe
Thanks here’s more info from last 24H urine in October:
SS CaOx 2.5
Ca 257
Ox 16
Cit 505
SS CaP 1.61
ph 6.991
SS UA .04
UA .536
Na 44
K 57
Mg 99
P .587
Nh 26
Cl 52
Sul 20
UUN 6.41
PCR 1
Ca/Cr 359
Currently doing 11-1200 Calcium, extreme low salt, 3 L water, careful with oxalates, no lemons
Does this seem like IH? What can i do to not make any more stones?
Plus, i just found out i have osteoporosis. Thanks so much
Hi Caar, I cannot be sure as you do not give enough information – no urine creatinine nor urine volume. Given what we have urine calcium remains very high at 359 mg/gm creatinine. From the urine calcium and calcium/creatinine, I can surmise the urine creatinine was 1.396 gm which is high for a women and low for a man and I do not know your sex. But it indicates a sort of complete collection. From these inferences the high urine calcium remains uncorrected. Given bone disease, management becomes complex. We want high diet calcium and low sodium and perhaps bone directed medication or a thiazide, but there is not enough information for me to comment further. I am sure your physicians are properly concerned and will make the right decision here. Present stone risk is low but presumably because of high urine volume, which can be deceptive – peaks and valleys, overnight, etc. Regards, Fred Coe
The Calcium creatinine ratio is the 359 but the urine calcium dropped from 350 to 257 after a month of implementing Jills plan including 3L of water/day, volume tested at 3260ml.
Actual creatinine is 717 and creatinine/kg body weight is 13.7
Female
Hi caar, when this happens, it is usually that the 24 hour urine creatinine changed. As it measures muscle mass, changes usually arise from collection variations. Typically a less complete collection will have lower urine creatinine compared to another one more fully or even over collected (>24 hour of urine etc). It is complicated to sort out variations between Ca/Cr and 24 hour urine calcium and is not possible from this distance. If you are working with Jill, she can sort things out herself. Regards, Fred Coe
Dr. Coe,
Thank you for all your great efforts to discuss stone formation/prevention. Like others here I am grateful for your straightforward and deeply insightful commentary.
I had a 1.8 cm calcium oxalate stone descend to my bladder and enter the urethra. My Urologist pushed it back to the bladder and successfully lasered it.
My research, aimed at preventing future stones, led me to the Ettinger paper which I found interesting in your web review of the overall issue and state of research. Your open discussion with lay people that are motivated to take the best possible actions to mitigate the problem really added depth and breadth. Kudos! The use of citrates seem well accepted as well as well as several OTC products like Litholyte, KSP Tabs, etc … which I had found a report measuring their citrate performance. Numerous wellness options seem reasonable.
My 24 hour urine test came back as follows.
24 Hour Urine Test 1/31/2024
Total Volume = 2750 mL
TEST Results Reference Range
Potassium, 24 hr Urine 25.8 mmol/L 71 mmol/24hr (20-116)
Calcium, 24 hr Urine 5.0 mg/dL 138 mg/24hr (0-320)
Magnesium, 24 hr Urine 2.0 mg/dL 55.0 mg/24hr (12.0-293.0)
Uric Acid, 23 hr Urine 26.6 mg/dL 731 mg/24hr (136.1-771.1)
Oxalate, Quant, 24hr 6 mg/L 17 mg/24hr (7-44)
Citric Acid(Citrate),Random U 50 mg/L (7-1130)*
*Report Note: Results may be questionable-preservation issue
pH Urine 5.2 (4.5-8.0)
Sodium, Urine 86 mmol/L
Creatinine, Urine 79.7 mg/d
I am starting my process to understand this health issue as well as possible as my misunderstandings/lack of information in the past has cost me some poor results. I need to do better. When you have a moment, I would appreciate your opinion of how this appears in your experience and what possible options may be reasonable … realizing that your information is for my learning process and is not direct medical advice.
Your efforts are greatly appreciated.
Bruce
Hi Bruce, The data are not very complete and a mix of 24 hour and casual samples. You do not seem to have high urine calcium or oxalate so the most likely guess as to cause is low urine volume, perhaps in the past as such a large CaOx stone would take a long time to form. As an alternative, perhaps you have residual bladder urine from prostate enlargement and this is a bladder stone. They form because urine is unstable being supersaturated and will crystallize in the bladder if it dwells there too long a time. If it was a bladder stone the correct prevention is better drainage. If it is kidney stones I would suggest proper 24 hour urine collections from a reliable vendor such as Litholink. Regards, Fred Coe
Dr. Coe,
Thank you for your reply!
Since I sent my first note, I went back and pulled a 2020 CT/report that was taken prior to an ulcer cautery. (I also have a 2014 Whipple to add into the mix … eating 5 meals/day … including 3am. My fluid intake is 2L/day.)
I was surprised to find that the report from the CT noted a “large calculus of the left pelvis suspicious for a ureterovesicular junction stone, measuring 6mm in dia and 13mm in length.No significant ureteral dilation. No focal suspicious bladder abnormality.”
So it was of noteable size better than three years ago above the bladder so I will discuss getting the Litholink data with my PCP.
Thank you for your kind help!
Bruce
Hi Bruce, given the whipple procedure malabsorption is common and high urine oxalate as a consequence and caox kidney stones. This is a serious possibility and oxalate is capable of injuring kidneys so proper testing is imperative. Regards, Fred Coe
Hi
This is a question in regards to using calcium citrate instead of potassium citrate. In your answer of April 1, 2023 you said this: “Put another way I would not mind a patient of mine trying calcium citrate so long as we measure the 24 hour urine outcome and ascertain pH has risen and urine calcium (we are adding supplement calcium, not food calcium ) is not too elevated.” This was in reference to a person with uric acid stones.
My question is at what level is the urine calcium considered to be too elevated? My situation is calcium oxalate stone, osteoporosis, and IBS (avoiding diary due to gi symptoms). Labs including 24 hour urines all normal except low urine citrate. I had been taking K citrate, but can no longer tolerate it due to gi symptoms. I am now taking calcium citrate 950mg (200 mg elemental calcium) three times per day with meals,
24 hour urine calcium before calcium citrate; 157-174, on calcium citrate; 243. Urine citrate before calcium citrate; 151-185, on calcium citrate: 565 (urine citrate was 681 on K citrate 40 meq per day). urine sodium on calcium citrate: 153, volume 2100.
Thanks, this website is great.
Chris
Hi Doctor, I answered some of this already but there is more here. Epidemiological risk of stone rises at urine calcium >200 mg/day. You abrogated this with low calcium diet but I think caused bone mineral loss because of the physiology of idiopathic hypercalciuria. I commented on the low urine citrate in my other answer. Food calcium is a lot less risky than supplements – your dairy intolerance has a cause and can be got around – I do not know the reason in your case. Best, Fred
Dr Coe, Since my permanent ileostomy in 2008 I form many kidney stones. I had four operations to remove them. One with percutaneous nephrolithotomy (20 and 15 mm of almost pure uric acid stones) and three with ureteroscopy (of various sizes of 6,5 to 20 mm stones). Initially I was keeping urine pH to 6-6.5 (regularly checking with pH strips) by taking baking soda and at that time kidney stones were almost pure uric acid. Lately, I increased my urine pH range to 7.5-8 by taking potassium citrate and magnesium citrate and my last operation removed stones of 90% calcium oxalate monohydrate and 10% calcium phosphate. I am desperate to find an equilibrium without having to be repeatedly operated. What would be the optimum urine pH range. It seems that some urologists recommend having a urine pH of around 7.2, while some others of 6-6.5. Thank you very much Konstantinos Fytas
Hi Konstantinos, Here is my article on ileostomy.You want urine pH above 6 but no higher. The crucial range is 5.5 or lower. So you overdosed. IN addition, be sure you get 24 hour urine testing. Possibly there is still some colon and urine oxalate is high – unlikely. Urine volume can become very low – do not let that happen. As for pH values above 6.5, they have no sense in them. Regards, Fred Coe
Thank you very much, Dr Coe
Hello Dr Coe, I am a long time Uric Acid kidney stone sufferer, passing multiple stones every week (not fun)! I recently found a Doctor who finally has put me on K Citrate to treat my plight (I learned about K citrate mainly from this article, and am surprised how many doctors don’t know of this treatment. My question is what happens to the stones? Will they break up and pass or dissolve completely? I have been put on 10meq 3X times per day, I know this is an ambiguous question but how long could it take to break up stones, I have been told they are not very large and I have a small cluster of them. Thank you Dr Coe, I really appreciate your vast knowledge on this topic.
Hi John, So sorry the message has not got around better – I try! Your goal is a 24 hour urine pH around 6, no need to go higher. Uric acid stones can dissolve but it is slow. I would wait – no loss to let them shrink. Be sure about the urine pH and adjust the dose as needed. Best, Fred