 Agonizing, intolerable, miserable, excruciating, stabbed with a knife, worse than childbirth.
Agonizing, intolerable, miserable, excruciating, stabbed with a knife, worse than childbirth.
As a urologist specializing in the treatment of patients with kidney stones I have learned a new lexicon exclusive to stone formers describing bouts of renal colic.
Pain, the hallmark symptom of stone disease, accounts for over one million emergency room visits by such patients in the United States each year.
Over the past several decades considerable progress has been made gaining insight into the physiology of renal colic and optimizing methods to treat it. However, despite improved scientific explanations we as clinicians still lack a perfect understanding of why it occurs.
PAIN FROM STONE PASSAGE
Patients have been suffering from renal colic secondary to stone disease for over two thousand years. As a matter of fact, it is remarkable how little has changed in its clinical presentation over this time period. In 400 B.C. Hippocrates referred to it as first disease of the kidneys. He was one of the initial observers to comprehend the association between urinary obstruction and pain, writing:
An acute pain is felt in the kidney, the loins, the flank and the testis of the affected side; the patient passes urine frequently; gradually the urine is suppressed. With the urine, sand is passed; as the sand passes along the urethra, it causes severe pain which is relieved when it is expelled; then the same sufferings begin again.
We have since come to appreciate the complex physiologic basis for this relationship at a much deeper level.
How Pain Begins
 The first step in this process is acute obstruction, most commonly from a stone. But in stone formers masses of crystals can create obstruction, as can blood clots if bleeding is particularly brisk.
The first step in this process is acute obstruction, most commonly from a stone. But in stone formers masses of crystals can create obstruction, as can blood clots if bleeding is particularly brisk.
Urine from the kidney can no longer pass to the bladder and as a result builds up and stretches the proximal – closest to the kidney – ureter and renal collecting system. This stretch activates nociceptive nerve fibers – fibers which sense injury – within an entire neuronal network located submucosally in the renal pelvis, calyces, capsule and ureter.
Figure 1 (left) – Example of obstructing proximal ureteral stone with dilation and stretch of the collecting system above the level of obstruction.
These fibers then transmit afferent signals to the T11 – L1 spinal cord which the body interprets as pain at the corresponding level of neuronal activation. As the stone migrates from the kidney down the ureter and towards the bladder, pain usually shifts downward as well. It is commonly sensed as high as the upper flank when the stone is lodged in the proximal ureter and as low as the labia/testicle when down near the uretero-vesical junction at the entry to the bladder.
Patients passing stones may experience other symptoms in addition to pain. Many of the nerves involved in the process of obstruction are intimately linked to innervation of adjacent organs, for example the gastrointestinal tract. Cross activation of these associated nerve fibers has been proposed as an explanation for the nausea and vomiting which so often occurs in the setting of an acute episode of renal colic.
In rare instances patients may even have alternative symptoms without any pain at all. In some cases, particularly when the stone is at the uretero-vesical junction, urinary symptoms predominate and the only appreciable symptoms are urinary frequency, urgency and discomfort while voiding. These symptoms mimic urinary infection and often result in temporary mis-treatment with antibiotics until the correct diagnosis is made.
What Happens Later
Increasing renal pelvis pressure from persistent obstruction causes a release of prostaglandin E2. This chemical mediator of injury response produces a perfect storm.
It causes ureteral hyperperistalsis (increased intensity of the waves of coordinated ureteral contractions which normally drive urine down to the bladder) and eventually even ureteral spasm. It also leads to dilation of the afferent arterioles – those tiny resistance vessels which control the flow of blood into the capillaries of the kidneys.
The arteriolar dilation increases blood flow to the kidney and promotes a temporary diuresis just as ureteral smooth muscle hyperperistalsis and ultimately spasm tighten the ureter around the stone and worsen obstruction. Spasm leads to lactic acid build up, as occurs when any muscle is over-exercised, and sets off an inflammatory cascade that itself can worsen pain.
With time, blood flow to the affected kidney falls, even though the arterioles which let blood into the renal capillaries remain dilated. It falls because the efferent arterioles, which let blood out of the capillaries where filtration occurs, begin to constrict and raise filtration by the renal glomerulae. The increased filtration maintains and can even raise pressures.
Figure 2 – Diagram of blood flow to the nephron. Blood enters through the afferent arteriole and is then filtered within the glomerulus, producing urine in the process. Blood exits through the efferent arteriole. Both the afferent and efferent arteriole are able to dilate and constrict in order to regulate pressure and ultimately filtration via urine production.
In many ways, this complex system is analogous to the soaker hoses many people use to water their lawns. The afferent arterioles are the faucet the hose is connected to and the efferent arterioles are the opening at the end of the hose which can be closed or left open into a sprinkler.
Filtration is the many tiny flows of water all along the hose which keep the grass growing.
When working appropriately, the faucet and the end are both open and water (urine) is produced at a slow, constant rate (Figure 4 – left). With an obstructing stone the faucet – so to speak – is opened more and the end clamped more so more fluid – water – is filtered out along the length of the hose at high pressure (Figure 4 – right). In the kidney this filtration is into the nephrons and raises pressure. When the clamp is tightened, the total amount of flow through the hose can fall just as the amount of water filtered out along the hose rises.
Figure 4 – Soaker Hose Analogy to Renal Blood Flow and Filtration. On the left, there is little pressure in the system and water (urine) seeps out slowly from along its length. On the right, the inflow is much higher than the outflow and water (urine) shoots out from along the hose at exceedingly high pressure.
Three Phases of Pain in more Detail
The Physiology
No discussion regarding ureteral obstruction would be complete without the work of E. Darracott Vaughan, who characterized the physiology of urinary obstruction in the 1970’s.
Assuming two functional kidneys, the physiologic effects of acute unilat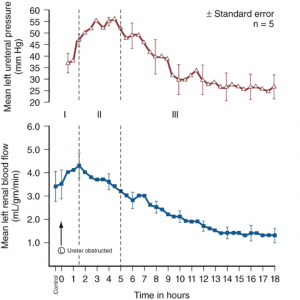 eral ureteral obstruction can be marked by three distinct phases.
eral ureteral obstruction can be marked by three distinct phases.
In phase one, the effects of the inflammatory cascade described above cause a progressive rise in renal blood flow and renal pelvis and ureteral pressure. This phase lasts for approximately one to one and a half hours. This is the portion where the afferent arteriole – the faucet – is maximally opened.
Phase two is marked by efferent arteriolar vasoconstriction which causes a decrease in overall renal blood flow but an increase in ureteral pressure for up to five hours. The faucet is opened and the end clamp is tightened.
Phase three is marked by a further decrease in renal blood flow to the affected kidney and ultimately decreased ureteral pressure. The end clamp is progressively tightened so blood flow to the kidney is reduced enough that filtration and urine production begin to fall, and pressure with it.
Measurements of ureteral pressure (red) and renal blood flow (blue) after onset of acute unilateral ureteral obstruction. (Courtesy Campbell-Walsh Urology, Tenth Edition, Elsevier Inc.)
The fall in blood flow is not injurious during an acute attack, but over time it can be. This means that relief of an obstructing stone is an important matter. Commonly stones pass of themselves. But stone attacks need medical attention because if the stone continues to obstruct it must be removed.
The Symptoms
It is easy to conjecture how these three distinct phases correlate clinically to the symptoms experienced during an acute episode of colic.
The onset of pain classically correlates to phase one and the inciting obstructive event. It is at this point that the patient commonly seeks care in the emergency room or physician’s office.
The pain classically persists at a severe level for several hours (phase two) but ultimately subsides, at least partially (phase three).
In many instances pain comes in waves, potentially a sign of intermittent obstruction activating the above pathway each time urinary flow is obstructed. This occurs through a combination of the stone moving and the tensions of the ureter with increases or decreases of muscle spasm.
THE CONUNDRUM – Pain Without Obstruction
Opinions of Urologists in General
Though the physiologic basis of pain in the setting of obstruction is clear, it does not provide an explanation for one of the most commonly encountered conundrums in stone disease – the symptomatic non-obstructing stone. These can be actual free stones that have not passed, stones attached to plaque, or actual plugs in the kidney tubules that are massed together enough to show up on a CT scan as ‘stones’ though actually tissue calcifications.
There is perhaps as much variation in clinical opinion in such instances as any other clinical scenario in the field.
If one were to ask a group of urologists whether they believed that small nonobstructing stones could cause renal colic, opinions would range from absolute certainty to complete dismissal of the concept altogether.
What Happens to Patients
As a result, there is no standard of care regarding how to optimally manage such patients. In all cases it is first imperative to rule out other potential sources of pain; however, such workups often end with the same result – a patient with bothersome flank pain and evidence of one or more nonobstructing stones on imaging.
Lacking a physiologic explanation to explain their symptoms, patients with pain and non obstructing stones are often sent for detailed workups, secondary and tertiary consultations and referral to pain specialists and even psychiatrists. However, in an age where flexible ureteroscopy can be performed quite safely and on an outpatient basis one must wonder whether such patients are being treated appropriately.
A Specific Example
As an example, I recently met a patient who had been referred from several hours away seeking a fourth opinion regarding her chronic flank pain. For months she had suffered from a severe ache in her left flank that had limited her ability to work and live her normal life.
She had attributed the pain to a 7 mm lower pole nonobstructing renal stone on that side which was discovered on a CT scan during her initial presentation to an outside emergency room (Figure 3). However, none of the physicians she had seen agreed with her self diagnosis.
scan during her initial presentation to an outside emergency room (Figure 3). However, none of the physicians she had seen agreed with her self diagnosis.
Figure 3 – CT image of left lower pole nonobstructing stone (red arrow). There is no evidence of obstruction or inflammation around the kidney.
In the ER she was given narcotic pain medication and sent home to follow-up with a urologist.
The first urologist she saw told her that while the stone was visible, its location within the kidney meant that it could not possibly be causing her pain. He refilled her prescription for pain medication and sent her to see a pain specialist.
The pain specialist tried physical therapy for what he thought may be a musculoskeletal source but ultimately this did not prove effective and she was given more pain medication.
She later sought care from a second urologist who also told her that the stone could not possibly be causing her pain in the absence of obstruction. This time however she was accused of having an agenda and seeking care specifically to get pain medication. Similar visits to a variety of emergency rooms elicited more CT scans as well as accusations of seeking pain medications. Each CT result was the same though, all demonstrating a 7 mm non obstructing left lower pole stone.
On one instance a treating practitioner even admonished her, saying that nonobstructing stones don’t cause pain and he should know since he too had been diagnosed with such stones incidentally on a CT scan.
Ultimately she made her way to the clinic for consultation at which point she was offered a ureteroscopy and stone removal. The procedure went well and she was discharged with a stent for one week. She was last seen back 5 weeks after the procedure and reported complete resolution of her pain. She was no longer taking any pain medication whatsoever and there was no evidence of any stone or hydronephrosis on follow-up imaging.
What is Known to Date
Such patients are frequently encountered. Despite a lack of physiologic explanation as to why these non-obstructing stones may cause pain, there is emerging evidence that they do and therefore that removal can cure it.
In 2006 Taub et al. described outcomes of twenty such patients who had chronic flank pain as well as radiographically evident calcifications within their papillae without obvious collecting system stones. Ureteroscopy with laser papillotomy to unroof and remove all evident stone was performed on twenty seven kidneys. Pain improvement was seen in 85% of cases with a durable improvement for greater than one year in nearly 60% of cases.
This study was then repeated on a multi-institutional level with 65 patients undergoing similar procedures over a ten year period. Overall there were 176 procedures performed in this cohort with patients reporting less pain after the procedure 85% of the time. The mean duration of response was 26 months with 60% of patients having sustainable improvements in their pain levels for over one year.
Finally, this clinical scenario is seen commonly enough that it garnered its own nickname at Massachusetts General Hospital where it has been described as “small stone syndrome”. In a retrospective review of patients treated there with ureteroscopic removal of small nonobstructing stones (<4mm) for reasons related to chronic pain, 11/13 patients reported being pain free after the procedure with the other two noting a partial response.
What I think
We still do not completely understand the physiologic explanation for pain in these patients. However, much like Hippocrates over two thousand years ago, clinical observation often precedes scientific understanding. In this regard it is unfair to dismiss the notion that small non obstructing stones can elicit legitimate renal colic.
Physiologic breakthroughs in the understanding of pain signaling and inflammation are currently happening at a rapid rate and it is likely that in time we may be able to better decipher which non-obstructing stones are truly responsible for symptoms. However, until then, such scenarios will continue to be a commonly encountered clinical complexity for urologists.
For the time being I would still advocate consideration of alternative causes of pain in such situations including urinary infection, obstruction and malignancy. A careful history is critical to rule out non-urologic sources such as pathology within the musculoskeletal, pulmonary, gynecologic and gastrointestinal systems. Another important element of the history is whether the patient has previously passed a stone and if the current symptoms are similar to that experience.
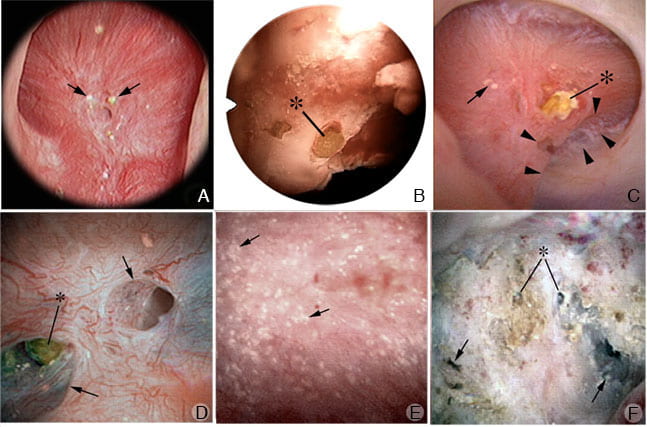
Once other explanations have been ruled out, offering stone removal is entirely reasonable. This not only has the potential to improve pain but may also decrease the risk of future stone growth or spontaneous passage at a later date. In such instances, I prefer flexible ureteroscopy with stone removal to shock wave lithotripsy. First, ureteroscopy maximizes the likelihood that all stones can be identified and removed which is especially important in the event that pain persists after the procedure. Second, with ureteroscopy one can inspect the inside of the kidney in high definition which has the potential to offer information not readily available on x-rays and CT scans such as embedded stones, tissue calcifications, and other pathology (Figure 4).
Figure 4 – High definition images obtained during renal endoscopy demonstrating tubular plugging (stones embedded in the kidney) (Courtesy: AE Evan, IMCD and BD plugs: Do they have a role in stone formation).
Finally, it is critical to establish realistic expectations before surgery in regards to pain control. Our understanding of this concept is in evolution and the published literature suggesting a treatment response is limited to relatively few patients. However, as science and history have shown us, just because we don’t fully understand the connection doesn’t mean it doesn’t exist.
More You Might Like
What Kidney Stones Are
Types of Kidney Stones
Do We Need to Analyse All Those Stones?
How Kidney Stones Form
When Crystals Plug The Kidneys
Medullary Sponge Kidneys


Hi,
I have just been diagnosed with non blocking calculus of 7 mm at the lower pole in left kidney with no suspicious focal renal lesion. No hydronephrosis. I’m in no pain or discomfort.
Previously i had 1cm calculus in same area which was removed last year.
My doctor ( GP ) has said nothing to worry about at the moment as there’s no pain but i’m concerned this could get bigger and cause me problems like before, should i go to see specialist now or wait for symptoms?
Rgds
Ian
Hi Ian, It sounds like you had a stone removed and another one grew back in the same place. Absent significant pain, obstruction, bleeding, or infection, I see to benefit in surgical removal. I wonder if all of the original stone was removed. Either way, new or just growth, the same for intervention. But your physicians are the ones responsible and they know you a lot better than I, so do what they say. Regards, Fred Coe
I have a 7mm stone non obstructive stone and have had chronic flank pain, back pain, bouts of frequent urination for a year or so now. I can feel the build up in my kidneys and then a release and then I often have dark tea coloured bloody urine For the next couple of voids. My kidneys hurt the most when my bladder is full and I can feel spasms upon voiding. It feels like it’s all in my head when the specialists all shrug it off like it can’t be hurting me. I have doubted myself and put it down to back pain a lot. This article explained so much and describes so much of what I feel and it’s great to know that I’m not alone. I’ll be speaking with my specialist in a few weeks so hopefully I can address this issues properly.
I also have congenital medullary sponge kidney.
Hi Tiffany, Your symptoms seem like crystal attacks, and if so there are always reasons. I would get a low dose CT and see if any new stones have formed. Your physician can look for crystals when your urine turns tea colored – a sign of bleeding. You need 24 hour urine testing to find out why you form crystals, and how to stop them. Regards, Fred Coe
THANKYOU for your knowledge! And you are easy on the eyes too!
I had to go back to this article again to share again for our Cystinuric community. I originally found it in July 2019 as I sat ONCE AGAIN trying to advocate for my daughter to validate her kidney stone pain. YES IT IS REAL! It becomes even chronic with cystinuric patients, especially the ones who form severe like my eldest. Geeze! After all these years in a Childrens Hospital setting and with 3 kids with cystinuria and my mother as well who went into renal failure from multiple cystine stones….you’d think there would be some respect just automatically after shes passed 1000s of stones on her own, in ER settings and with surgical intervention. They didn’t just move her kidneys around for nothing….to help the pain and to preserve her kidney function. Anyway, I would like to thank the author, Dr Mike Borofsky for his thorough investigations and understandings of even microscopic crystals that may form (no matter what chemical make up)….they HURT and cause pain.
My hopes are that more investigations or even more discussions like this one reaches the Urolological professionals that are in front of stone patients….ESPECIALLY OUR CYSTINURIC community. Cystinuria is unlike no other stone disease and despite all preventative measures, stones just keep on forming for some (like my eldest) My son produces his fair share and surprisingly my middle daughter ( who has the higher cystine concentrations on her Litholink) never produced one. Wish someone would take interest in studying that genetic component here. I read these posts and feel people’s pain as I am a caring empath (it is my nature as a Registered Nurse) so I just wanted to put out there that if you don’t know the composition of your stones and they seem very frequent, please find out if they are Cystine. We have an International Cystinuria Foundation that you can find even a private Support connection. Sorry I didnt want to hijack this in comments but just very grateful to see Urologist so dedicated to stone disease and understanding a patients pain associated with them. Bravo!
Hi Dawn, I am happy to have your comments on the site. Treatment of cystine stones is imperfect, though often successful, and indeed pain is very common and serious. The genetic basis for cystinuria is well known. Several transporter molecules are abnormal. But knowing all that has not led to new treatments. Best to you and your family, Fred
Great tips! This blog very helpful who suffering from Kidney stone pain. Thanks for sharing your great tips.
Hi
I have been diagnosed with a 7.8mm stone in right lower ureter with upstream mild hydronephrosis.
It had been hardly an hour since I got to know this.
Please suggest something
How can I get rid of it naturally.
Please help😒
Hi Deepankar, You must have the care of a urological surgeon to supervise matters. Even if the pain goes away the stone can still be obstructing. If may pass on its own. But a urologist is a necessity until it does pass or is removed. Regards, Fred Coe
I had two 3mm stones. One in the lower pole, one stuck in the uvj. Tried and tried to pass the uvj stone without luck so I had it removed. Wish they would have removed the other while in there. They’re not visible on X-ray, and it’s not reasonable to keep having CT scans. After removing the one, I continued to have pain and small blood in urine (not visible). They told me the lower pole stone absolutely could not be causing pain and I was probably just constipated. 8 months later I still have attacks of pain in this area. I’ve had many kidney stones all in the left side. I know what they feel like. The UVJ one was a mystery to me because the pain radiated to my labia. But after some research I found out that in men it can radiate to testicles and women to the labia. Otherwise, the lower pole stone feels exactly like renal colic. No one wants to consider it could be the stone, and no one wants to investigate the blood in urine cause. It’s so frustrating. It’s not 10/10 pain as an obstructing stone…but it’s not enjoyable either. I’m an RN and I cannot understand a practitioner who can claim something is just “not possible”. In the world of medicine, we all know strange things are possible. I don’t take narcotics, can’t be doing that. So it’s obvious I’m not drug seeking. Wish I could find someone who would think outside the box. I have had a gyn ultrasound, all clear. I don’t have bowel problems. Just over it.
Hi Ashley, Do you know what the stones are made of? Not visible on routine x ray but on CT could be uric acid, and these can dissolve. As for having CT scans, ultra low dose CT is now below routine FP. If the stones are calcium based and you are having distinctive stone pain = labial radiation – removal is a reasonable idea. Regards, Fred Coe
I have a history of kidney stones but the most recent ct scan was clear with no stones visible. However, I am having twinges of stabbing pain in my left kidney that last a few moments and then go away. The pain is followed by waves of nausea and groin pain that lasts a few hours but without the persistent flank pain that is indicative of a moving stone. Have you ever seen this before? What would you recommend?
Hi Erin, Crystal attacks can do this and the crystals be not found – one has to look just at the right time. I would try to have your urine looked at during an attack. As well, you need 24 hour urine testing to determine the cause of stones – usually the cause of crystals, too.
My 24 year old son has unilateral hydronephrosis of the right kidney identified by ultrasound nearly 2 years ago, which is intermittently painful during the day. 2 renograms, an mri scan, and an x ray have all failed to identify the cause. It doesn’t appear as obstructive on the graphs and the pain doesn’t always follow drinking large amounts of fluid. Could this be due to crystals that come and go? We are very concerned about the potential ongoing damage and no answer to the possible cause.
Hi Louise, This is potentially serious and if his physicians have reached the end of their search you or he might want to ask them to arrange for an opinion from an outside specialist who might contribute additional knowledge and experience. That is a common action when diagnosis and treatment remain in doubt despite vigorous and focused efforts. I would advise this. Regards, Fred Coe
Thank you so much for this thoughtful advice. We will follow it as soon as the health service here reopens for non Covid 19 cases. Thank you again.
Hi. I’ve had about 4 years of chronic mild to moderate right flank pain. Gall bladder with ejection fraction of less than 5% but no stones was removed about 3 years ago with no resolution of ongoing pain. Liver is normal – few small cysts. Ct 2 months ago was normal – no kidney stones. Over the weekend I had what would be considered a classic kidney stone episode. Severe colicky right back/flank pain radiating to groin associated with nausea/lack of appetite and frequent urination – no frank blood. I was in a remote area on a long weekend so I treated with heat, fluids, and ibuprofen/acetaminophen. Didn’t sleep at all but I got through it. It lasted almost 40 hours and then stopped and has returned to normal chronic pain levels. Question is – should I be pushing for a referral to a urologist. I’ve been dealing with internal medicine doctors who can’t find anything and ct scans of abdomen have all come back normal. I’m tired of being in pain but I’m also tired of being told there is nothing wrong.
Hi Susan, I may be wrong, but crystal attacks are not an unreasonable alternative. One clue is a remote region – often dehydration occurs and is not obvious. If attacks like this have been recurrent, 24 hour urine testing for kidney stones can be revealing – of factors that promote crystallization – and point to prevention. Regards, Fred Coe
I have an 8mm stone in my left kidney and a 6mm stone in my right kidney. Both are in the lower poles and are non-obstructive. However, the stone in my right kidney (surprisingly) is the one giving me very mild, intermittent pain, which I have had for at least 4 months now. It’s like a throbbing which I feel in the right side of my back and an occasional stab in the groin. I never have to take a pain killer for it but I tend to feel the throbbing most in the mornings while still in bed. I am aware of a slight niggle almost all the time, even whilst simply sitting but it doesn’t stop me doing anything. Both stones have increased by 2mm in the past 19 months. There are no other abnormalities, but my PTH level remains high at 7.2. My urologist is willing to do a ureteroscopy to remove both stones in separate procedures one week apart but it’s my decision whether to proceed. I’m certain the discomfort isn’t muskeloskeletal – I get no pain or any extra pain with any type of movement. I feel it would be safer to be rid of the stones, especially if they keep getting bigger (I have had kidney stones before – one that caused a blockage but passed 20 years ago, another two that were broken up with lithotripsy more than ten years ago. I am a 62 year old female in very good health otherwise. I am fit and exercise regularly and do not take any medication but I’m starting to get cold feet about having the stones removed. I would really appreciate a second opinion.
Hi Mirella, If your symptoms on the right are sufficiently disturbing to warrant surgery it is probably worthwhile. The left stone seems without symptoms but is enlarging, but does not need surgery medically at present. What you need is proper testing to figure out how the stones are forming and take steps to slow growth and prevent more. Here is my best on that. As for the serum PTH, it is not a way to diagnose primary hyperparathyroidism. The latter depends on serum calcium – which must be high for that diagnosis. Here is an article on it. Regards, Fred Coe
Sir I have 4mm stone in upper pole of left kidney is it treatable? ….suffering with lower back pain how can I reduce my pain without using pain killers?…please give me your valuable suggestions..thank you..
Hi Gowri, Your back pain may not be from the stone but from other causes. Your physicians need to help you distinguish if the stone is the cause or perhaps muscles or spine. If the stone seems a cause of the pain – which seems not too likely – it can be removed by your urologist. Regards, Fred Coe
Ihave before13mm stone I do surgery right side kidney feb 2018 and one more 6.5mm left side kidney I passed by urine tie now again getting pain for right side kidney I do ct scan again1.6mm how to solve this issu
HI Senthilkumar, Prevention is step wise. Here is my best on how to proceed. As for present stones, I am afraid they are the responsibility of your surgeon. Regards, Fred Coe
Thank you for this. I feel like I’m going crazy, 6 stones in left kidney with one at 7mm and another 9mm, and 4 in the right, two of those at 6mm and two at 4mm.
I’ve been to the ER several times with pain, been CT scanned, ultrasound, family dr follow up, ultrasound, ER, specialist, ER. Keep saying I’m full of stones but none passing, so no reason for my pain. First few ER trips got me decent pain meds, now not so much like I’m crying wolf.
I do currently have an untreated hernia I’m waiting for surgery on, and understand that can explain the abdominal pain, but not the flank, the back, the urge to pee, etc. It’s either im passing stones and growing new ones, or my body is acting like im passing one from the ones in the kidney. If this keeps up, I will ask to see a specialist again and see if they can be removed as I can’t keep going to the ER each week, living in pain, hoarding my pain meds to the last possible second as I don’t know if I’ll get more, it’s all at the whim of what ER is there.
Hi Jay, I suspect from your brief precis that you may be passing tiny stones or even crystals. Possibly surgical stone removal might help but that is a complex surgical issue – if so, ureteroscopy would be ideal if the mass of stones is not too large. More immediately you should pursue stone prevention as aggressively as possible in case it is crystal attacks. Here is a good plan. Regards, Fred Coe
Have a 8.5mm right now. ER visit Thursday, kept overnight. Stint placed. Burning sensation is unbearable. Last year a 24mm multiple ops. Looking for info on prevention! My dr. Says drink water. I’ve been doin low oxalate diet, tons of water. Is there a way to tweak my urine stones don’t form?
Thanks
Hi Ian, Surely it can be a lot better. Here is my best overview of how to go about it. Regards, Fred Coe
I went to the ER last week after a night of 105.1 fever and severe left flank pain. History of numerous stones, though no problematic ones in a few years. CT showed a very small, 1-2mm, stone in the RIGHT kidney. I believe I’ve only had this happen once before. Can you explain the pain on the opposite side? Also with usual stone symptoms: n&v, urinary urgency, fatigue.
Hi Anita, I am guessing – far away – but perhaps you had an infection in your left kidney. Regards, Fred Coe
I had kidney stone 7 mm in my left kidney, which was obstructed or blocked in urine tube . Further , the doctor had used followed ureteroscopy procedure (April 2019) and removed stone and placed JJ stent in the duration of one month. Further removed end of one month(June 2019). After wards, I am drinking plenty of water and But I feel frequent moderate pain in left side. Last February 2020, through MRI scan, It was found very small <1 mm kidney stones and doctor told that these are common and suggested to drink plenty of water and stones may pass..However, I feel again unfrequent mild pain and If I carry any weight on left side abdomen, I feel some moderate pain on left side .. What is the reason? Tell me some suggestions…
Hi A., MRI does not visualize stones so it must have been a CT. Was that small stone present after your 2019 surgery? The tiny stone does not cause pain unless it is blocking a ureter. The fact that the pain is worsened by carrying things suggests it is not from the kidney but from the muscles and back. Regards, Fred Coe
Dear Doctor…
Many Thanks for reply Doctor..However I feel the moderate pain continuously ..But, I am drinking the plenty of water and passing urine with in half hour..During the removal of JJ stent in the year May 2019, the doctor forcely removed. Therefore, my main question is that ‘Is the pain mainly due that hardly removed stent and is it continuous for the long duration?.. Or Can I go for again scanning based on your Answer (The tiny stone does not cause pain unless it is blocking a ureter)
Thank you Doctor..
Hi, You are asking very good questions but I am afraid I cannot answer them. To do so would require I review all the images that have been made. I would be remiss otherwise. Best, Fred Coe
dear sir
I suffer with kidney stone last 2years when first time occured .i cured with urologist and dessolved it .and after 9monts later again occured in bothe kidney then it did nat dessolv it with medicine. so i attended lethotripsy. after 6month again occured in bothe kidney please advise what should i do to prevent kidney stone in life and what should examine in blood
Hi Ramayan,
Follow our diet:https://kidneystones.uchicago.edu/two-gates-into-the-city/
Best, Jill
Hi..I had 4’5mm kidney stone removed 2 months back and then DJ stent removal. My only question is can I sometimes have mild pain on the right abdomenal region. Is it normal to feel mild pain after 2 months? Or do I have to see a doc?
Hi Kizzy, It is indeed. Your urologist might want to do an ultrasound to be sure there is no obstruction. Regards, Fred Coe
Beginning in 2001 Had frequent UTI’s and severe pain that were caused by stones that I hadnt been aware of. All Doctors seen said they were just UTI’s, conducted no tests, no blood work, prescribed no pain meds only antibiotics, eventually antibiotics no longer helped. After I had almost given up my uncle, a doctor recognize the symptoms of UTI’s but also kidney stones and he was right without even doing any tests, prescribed me a year of doxycycline which stopped the infections and seemed to stop the pain only very rarely having brief UTI’s while still passing stones without knowing. 2007 diagnosed with obstructive 8mm calcium stone, Doctor advised I would have lost my kidney if I had waited much longer, had already been experiencing daily horrific pain for close to 3 weeks, discovered I had massive infection as well, had developed sepsis, collapsed at work, had to be helped to the car and went home, hospitalized the next day. After discovery of 8mm stone in 2007 I was hospitalized and I was given pain meds and lights out. Woke up and was coherent enough to over hear the Doctors threatening my family, demanding upfront payment of every cent of the $14,000 he planned to charge me (against the medical “contract” I agreed to)or he would not perform the procedure although he was a resident Urologist of the hospital and was required to do the procedure. Family threatened to sue him, what he attempted to do was illegal and he would be and was reported to the hospital director, turned out according to other patients he had done this frequently and worse, intentionally injuring them during surgery. I knew several of his past patients and a former nurse who had witnessed his actions, he was later replaced for unknown reason and closed his personal practice but only relocated. Because we refused to pay upfront, he refused to do the operation and since there was no other Urologist on site I was transferred to another hospital where I was placed under another Doctors care but that doctor was unable to attend and to my dismay my original doctor who also had residency at the second hospital had to do my procedure after all. Surgery was no longer considered, new place, new diagnosis and intervention. To my relief they used Ultrasound lithotripsy to break it up, it was my original choice despite the doctor essentially initially demanding, yes, demanding actual surgery where he stated he planned to remove my affected kidney and manually remove the problematic stone, yes organ removal for one stone(albeit there were many others). After the Lithotripsy the Doctor proceeded to implant a stent against my consent, later confirming while my family was present that the stent was never necessary, sadly no lawyer would help with a malpractice case because I hadnt paid, those included Fieger and Burnstein, I was still implanted with a medical device against my consent and without reasonable cause, “F” those lawyers. Further CT revealed a minimum of 30 various sized stones in left kidney and a minimum of 15 in the right kidney that they had some how missed in the multiple previous scans. Stent was removed 3 months later due to medical complications that persist to this day. Doctor diagnose me with Chronic stone formation and Advanced calcium stone formation. To this day I pass a minimum of 1 stone a week, frequently more and regularly pass sandy sediment effectively etching my toilets. I’ll admit im glad I got treated, I would have lost my kidney, potentially both, Dialysis had been discussed because the possibility of irreversible damage after the procedure and the stent. Although I pass and have passed hundreds of stones my kidneys are reportedly in good working order just filled with very painful spikey calcium crystals. I live with near constant pain in both sides but thankfully i’ve developed enough tolerance to the pain so the smaller stones dont bother me much unless they get stuck especially when I somehow pass them while im not peeing. Just collected my newest 4mm a few hours ago, took 2 days. I know im not alone, im sure other have been mistreated, had their well being endangered by a doctor due to their ego or greed, or both but its been 13 years and I still fear the thought of going to any urologist, I have irreparable damage to the nerves in my genitals due to the stent, damage not present before its implant. My terrible urologist is now practicing in Florida, originally Oakland County Michigan, He’s a monster and should be feared.
Hi,
Thank you so much for providing this forum. I’ve had gross hematuria on and off for about 8 months. When it first presented, I was given a full urological workup (cystoscopy, cytology, and CT scan). The findings from that were a mildly enlarged prostate and a 4mm stone in my lower pole of my left kidney. The urologist at that time suggested that the hematuria was a result of the enlarged prostate pushing against my bladder, and suggested it could go away on it’s own. It sort of did, but then came back again in the last three months, and is occurring regularly.
This time around, it is accompanied by episodes of moderate discomfort on my left side. What usually happens is I feel the left side discomfort come on, it lasts for an hour or two, and then subsides. Shortly after, I will experience the gross hematuria. It seems that sometimes this happens after moderate exercise (riding my bike for example), but not always.
Once again I suspect the stone, however my doctor is still focused on the enlarged prostate. I just today received results from a CT scan that shows the stone as 5mm now and that is has moved into the left renal pelvis (without evidence of hydronephrosis). My doctor has commented that given the location of the stone, it should not cause any problems (pain or blood). Sorry for the long winded explanation, but my question is, do you agree with this assessment?
Thanks very much!
Hi Adam, I have several suggestions, of course from a distance as your physicians are the ones in charge. Perhaps you are forming crystals which cause bleeding without necessary pain. The 24 hour urine studies you should have given your stone may show a high urine calcium that can cause crystals and bleeding, and stones. Finally, if it is just the stone – seemingly unlikely, your surgeon and you can decide if it is worth removing it. Regards, Fred Coe
I am so grateful for this article. As a frequent kidney stone patient I am seeking input from a phycicians outlook on pain management. I passed my first kidney stone at age 18. I am now 37. On average I would say I pass 3-6 stones per year. In my younger years it seemed even relatively large stones would pass without the need for surgical intervention. Around age 28 I had my first uriteroscopy w/stent to remove an obstructed stone. Followed by 2 occasions of lithotripsy to free both kidneys of all stones. I have now had 8 uriteroscopy w/stents to remove obstructing stones whilst still passing the occational stone naturally. The majority of those years I lacked health insurance so never had the means to have them analyzed (now having it done in sep 2020). It seems to follow a pattern. Excruciating pain, a couple trips to the E.R., then I either pass it or have to see the urologist who suggests surgery. Plan removal, urologists attempts but is unable due to large infection behind the stone. Stent is introduced to drain infection for 1-2 weeks. I am completely miserable, in pain with a constant feeling of urgency and very little urine output until I eventually start running a fever, go to the E.R. where they discover a bacterial infection in blood and urine accompanied with sepsis, extremely low BP, and Large amount of blood in urine. This has been the routine for my last 3 surgical interventions. I blame it mostly on poor pain management. What they prescribe for pain doesn’t work I don’t know why but it doesn’t. I don’t feel like I can make a case for something stronger for fear of looking like a drug seeker. But the frequent trips to E.R. probably make me look like one anyway. I have never continued or felt the need to continue seeking pain medication when I am no longer in pain and have never requested pain management without them finding a stone in my ureter. My theory, and please correct me if I am wrong is I deal with the pain but worsening spasms and swelling leads to more retention and elevated lactic acid, which leads to infection/sepsis, then low blood pressure, and excessive blood in urine, and decline in kidney function and ultimately a delay in removal of the stone which I fear is doing permanent damage. How do I have a successful discussion of pain management with my doctor without seeming like I am just after pain meds. I have tried and they don’t budge. Does something work better than narcotics or some combination? I don’t necessarily want to have to go to the E.R. for the extremely strong narcotics. But the ones they prescribe arent strong enough. I want to be able to be honest about my pain and find something that works instead of just dealing with it or being accused of drug seeking. Any suggestions?
Dear Emily, It would seem to me you need better stone prevention and as well as perhaps more helpful pain and surgical management. I have seen many times where stone disease becomes so difficult it goes beyond the capacities of the finest practitioners and it is time for another opinion. If you say where you live I can try to suggest an alternative for secondary consultation. Regards, Fred Coe
I had a 0.5 cm non obstructive kidney stone in the lower calyx . I had continuous pain.Doctors told me to ignore it as it is not the cause of pain and cannot cause renal damage. The stone continued to grow. But Some ultrasound showed it and others didn’t. Until i had an ultrasound which showed it became 2 cm but also skowed a kidney shrinkage ( atrophy ).
That means that non obstructive kidney stones can cause kidney damage and renal atrophy.
Hi Cherine, I suspect the 2 cm stone was obstructing, not of the ureter but of part of the internal drainage system within the renal pelvis. Loss of kidney mass would otherwise not have occurred as you do not mention obvious infection. Regards, Fred Coe
I am in my 30s and had an ultrasound that notes 5 stones, 2 on right (4mm and 2mm) and 1on the left upper pole (3mm) and 2 on left (3mm and 2mm). Also have mild dilation of left kidney. Have had pain on left side on and off for almost a year, not sure if related. Based on the size, will I likely just have to wait or will they have the option for medical intervention? Also curious if any correlation with tonsil stones, as they started for the first time this year as well. Both of these after starting singular, not sure if that medicine is related to stones? If you have any doctor recommendations in northern VA, that would be greatly appreciated.
Hi Beka, I think the University of Virginia is your best bet. There are many private renal groups but unfortunately I cannot help distinguish among them. As for the present stone, your physician is responsible for guarding the left kidney against damage from what appears to be mild obstruction. Be sure to follow up with her/him and do exactly as told. Regards, Fred Coe
I had chronic shoulder pain for YEARS and intensified side flank pain when dehydrated. UTI’s at least twice a year for years. Shoulder physical therapy with no results. Urologist diagnosed a non-obstructive 12mm stone and she flat out told me “this isn’t causing your pain”. I had subsequent bladder biopsy, more uti’s and continued referrals to PT for my shoulder pain (no one could see a correlation between the two). I had chronic inflammation, tiny bladder syndrome (i’d have to urinate all the time to relieve bladder anxiety). I left jobs due to pain, I left relationships due to pain. I was told I was depressed, I was told ‘its in your head’.
Finally, a new urologist agreed to simply remove my non-obstructive 12mm kidney stone.
I feel amazing. Each week post surgery my shoulder is loosening up and my entire core has regained flexibility and mobility that I hadn’t realized I had lost. I used to slump forward while seated or lay on my side as much as i could to relieve pain. Now I can remain upright all day!! Absolutely amazing change from the chronic pain I had suffered for years. I am able to exercise, stay active. This simple removal of a stone was life changing.
I had 7mm right ureteric kidney stone with mild hydrouretornephrosis. My urologist did CT scan and prescribed me pain killer along with alpha blocker and magnesium citrate for 30 days. Fortunately I passed my stone on 17th day with supportive medication only. So my question is how soon the hydronephrosis will resolves after passing the kidney stones.
It should resolve in a week or so. I presume your urologist will do whatever is needed to be sure you have no more obstruction. Regards, Fred Coe
I am diagnosed 12 mm stone. How can i pass it with medication and food habits? I dont want to go under a surgery or any procedures. I get pain once a month But it lasts more than 2 hours or so.
Hi Dashy, That is a large stone, and only your surgeon can help decide about surgery and its timing. I would advise you do exactly as your surgeon suggests as obstruction from stones can damage kidneys. Regards, Fred Coe
Experienced kidney stone passer here. I have passed countless stones (probably 50 +) and have encountered 5 I’ve had to have procedures to remove. My urologist says 5mm and below are passable, anything larger is more of a danger. I just had a 10 mm stone removed that caused a world of hurt once it blocked ureter. And Yes they hurt in the kidney too!!!!
Hi Kevin, so long as your urologist is in charge and watching, larger stones – >5 mm – are not a danger. If too long an obstruction, surgeons always act to save kidney damage. Have you considered better prevention? Here is something you might fine interesting. Regards, Fred Coe
I can’t believe I stumbled upon this article! I am experiencing EXACTLY the pain described and have had similar experiences to what was described in the patient example. I’m desperate, I’m in frequent pain and have been for close to five years. External ultrasound, internal ultrasound, $3000 CT scan! All showing stones, but non obstructing so I’m told to “just leave them in there, it hurts worse to pass them” by my pcp. I’m told to take Advil for the pain. So I switched family doctors who sent me for several expensive thyroid tests and bloodwork and then literally gave me the exact same response. I started seeing a kidney specialist who had me perform a 24 hour urine collection then put me on a water pill which made me dizzy so I stopped taking it. She then sent me to a urologist who told me that the stones aren’t causing my pain. I have an appointment with a different urologist next week but I’m running low on hope and good credit! I’m so frustrated, I’m so sore, I’m so tired. I just want to enjoy life again without wincing in pain every 70 seconds or so. Some days I actually have no pain, but most days I do (especially in the evening). Lately it’s been even more severe and lasting longer throughout the day. I feel like people think I’m exaggerating or lying but I’m really not! I even have been known to have quite a high pain threshold but I can’t seem to get anyone to hear me! I only really drink water (no coffee or tea in my daily routine)! I limit my soda intake to maybe twice per month and similar for alcohol intake. I’ve been working hard at reducing my sugar intake overall but I’ve yet to see relief from the pain. I’m willing to make necessary lifestyle changes to reduce the reoccurrence of stones but this article just confirmed for me that I need these ones out!! I’m in PA, please if you have any recommendations in my area I would be so grateful! Thank you in advance, I so greatly appreciate your time in reading this!!
Hi Krystal, In PA your safest bet is the university. The link is to their urology program which would deal with present stones and questions about pain or removal. They have a medical program for prevention, too. Regards, Fred Coe
I have a non-blocking 12mm stone. Ultrasound confirmed. Went to ER because of pain in testicals, groin and lower back same side as kidney with stone. CT scan was done and nothing found. All tests came back negative. CBC, urine and a bunch of others. They said that non-blocking stones don’t cause pain. I was sent home and still continue to have pain. I see a urologist next week. So can this stone be causing my testical and back pain? Nothing seems to help. Heating pad, Tylenol, Advil, muscle relaxers.
Hi Derik, back and testicle pain are famous as from a stone, and I suspect either that your stone moves and occasionally obstructs the kidney or that you form crystals that can cause the exact same symptoms. Regards, Fred Coe
Hello,
So glad for finding this website. I’ve read all the comments and can rely to a lot of it. So thank you for that.
Now, I got some concerns and I am hoping you may be able to help me.
3 days ago I got an RIRS. I have had an 8 mm kidney stone in my lower calyx for the last 4 years and it has been giving me a hard time. Flank pains have been the worst for me and sometimes the pain was so bad that I needed strong meds to get calm.
During my RIRS they lasered my 8 mm kidney stone to 4 pieces. They then removed 1 of the tiny fragments for stone analyse and left the other 3 fragments in my kidney, sizes between 2-3 mm each. According to the person who did my RIRS they were not able to catch the last 3 fragments with the basket and suddenly they disappeared and they couldn’t find them. They then gave me a kidney stent and told me that the fragments will pass.
So here I am 3 days later with a stent that are giving me chronic flank pains (even worse than the 8 mm kidney stone gave me) while knowing that I now got 3 kidney fragments between 2-3 mm each inside my right kidney.
This is leaving me with some concerns. Because from what I understand there is no guarantee that these fragments will pass are there? also, this now means that there is a risk of stone infections, stone recurrence and growth as well as new flank pains if the fragments decide to locate themselves in my lower calyx?
Also, is it even possible for the fragments to pass through a kidney stent? isn’t the stent too small for 2-3 mm fragments?
Last, is it really possible for them not to catch the fragments and can the fragments really just disappear like they told me?
Right now I am just so sad about the whole situation and the stent is giving me so much pain. I can’t keep my mind positive because of the pain and right now all I can think of is that these new fragments probably won’t pass and if they do they will probably get stuck in my ureter once the stent is removed in 2 weeks. 🙁
I wish you all the best!
Hi Louisa, Your surgeons actually did well in cutting up the stone rather than dusting it. The small fragments are well within the range of passable, so I have every reason to hope things will go well. Though the fragments sound large, they are easily ‘lost’ inside the kidney – and spending lots of time looking for them imposes risk from anesthesia time and instrument use. So as best as I can tell, your surgeons did as much as they could. Of course it is they who should be answering, as they were there and are responsible for you. Though I am often critical, this time I feel you probably got high quality care marred by a common mishap. When the stent is out you will feel a lot better, and I hope the fragments pass easily. Regards, Fred Coe
I was diagnosed with Kidney stones since 2015. I was 16y/o then. My first lithiotripsy was in December 2017. The SWL procedure was done after two stones 9mm and 10mm decided to come down in the right side.
Currently I have a 7.3mm stuck in my left PUJ. And multiple other calculi formations all over the kidneys- (both).
I don’t know whether the stone passing meds will work or I will need to go for SWL procedure again yet.
But what I wanted to know is lots of people here who are experienced stone passers seem to be doing so for years. Can you suggest what it takes for stones to never form again? I don’t want to enter the prime of my life with a crippling disease that takes away too many working days of a month. So how can one overcome this tendency of forming stones?
Hi Prateekee, Here is a good place to start. Prevention of stones is what this site is about, and this article is the introduction. Regards, Fred Coe
I have a 5mm ureteral stone proximal left ureter, spotted on a CT scan about 30 days ago. Urologist prescribed Flomax and asked me to come back in 6 weeks for another CT scan. I have no pain whatsoever, am drinking lots of water but no sign of a stone. Since I have no pain does that mean the stone is stuck in the ureter and not moving?
Hi Eric, At issue is safety of the kidney. Six weeks is the guideline time to allow an obstructing stone to remain in place, but as my article points out it is rather long and maybe too long. I would be sure to keep that appointment and if the stone is still there and obstructing have it treated -of course your surgeon is in charge and perhaps the stone is not obstructing, etc, and there are reasons to wait longer. Regards, Fred Coe
First, thanks for putting this together. Secondly, I am a urologists best friend, it seems that I don’t have the ability to pass stones naturally. Every single time I have gotten one, it has required surgical removal. Now, I find myself with another 5mm stone and a potential surgery on the way.
My question is – Are the stents absolutely required? What are the risks if I decline having one put in after the surgery? Sometimes, I believe those hurt a lot worse than the actual kidney stone.
Hi Joshua, Surgeons almost always use them as a precaution. I would not decline if your surgeon wants them in. But I would pursue stone prevention so you do not need the surgeries. Take a look at a way to begin. Regards, Fred Coe
I’m pregnant with two non obstructing stones and significant renal colic. I’ve had stones in the past, and have only successfully passed 1/4. Because I’m pregnant they are engaging in a wait and see approach. I’m frustrated bc I can’t sleep, I’m in pain, and scared to take the pain meds prescribed.
Hi Kallie, URS during pregnancy would be a difficult choice. Non obstructing stones are at least not damaging kidneys. The pain makes me wonder if the stones really are not obstructing – I am sure your physicians are quite certain about that. Is there infection as a cause of so much pain. Perhaps your physicians might want to figure out why so much pain in the absence of any obstruction. Regards, Fred Coe
Hi. I have had pain in the left testicle for a week. I then experienced pain in the abdomen. Then my penis began to feel a constant burning sensation. Then I randomly passed a stone. It was a URIC ACID Stone. I felt amazing like it had never happened. Then 5 Days later same symptoms of my penis is constantly burning again. Is it likely to be a second stone and how can I try to pass It. It’s constant burning of my Penis
Hi Dean, Stones not rarely refer pain to one testicle or to the penis. Uric acid stones are very easy to cure, so read this and get rid of them. Regards, Fred Coe
This is very interesting, for the last 2 weeks I’ve had severe diarrhea and pain in my stomach and side/back and low grade fever on and off. If I eat anything I’ve thrown it up. After 3 Er visits finally had a CT scan today and they found a kidney stone 4x5mm and they said that explains all the symptoms?
I have had 2 cat scans W/ contrast, the ER sent me home saying stones don’t cause pain unless in ureter, my is in kidney 4 mm, terrible pain in lt flank area to front under rib, takes my breath away, I can’t sleep, I feel my insides are swelling, I can pass Urine. Help!
Hi Sharon, Pain from small and non obstructing stones is very common place, but we lack trials concerning the benefits of removal. Perhaps the stone is obstructing within the kidney – I suspect your urologist would have noticed this – or you are infected. Both are treatable causes of pain. Perhaps the pain is not from the kidney but from the spine and muscles – a physical medicine consultant can help. Regards, Fred Coe
I’ve been in pain for two or 3 weeks now every time I go for a wee it burns the doctor said I don’t have a bladder infection or nothing she said I need to tighten up Abit but I’ve none everything plus I suffer with bad stomach acid I just fed up of running to the towlet because as soon as I feel it there I need to go other wise I will wee myself an it burns all day just gets worse when go for a wee
Hi Latoyah, if you do not have a urine infection and have a need to urinate frequently you may have a tiny kidney stone at the junction of your ureter and bladder. Perhaps your physicians have already looked for this, but if not they might consider it as a cause. Regards, Fred Coe
Wow crazy, i am in the same boat of the second half of this article about kidney stones in the kidney causing pain. I was looking to get a second opinion as the first urologist I saw said there is no way my left side flank and low back and groin pain is caused by kidney stones that were only in my Kidney and not in the Ureter. CT scan shows four kidney stones in the left kidney, the largest is 6mm. No infection, no blood in urine. I had a 3mm stone removed about 15 years ago by Lithotripsy because it got stuck in my ureter. Good luck passing a 6mm i say. Coincidentally, Dr. Borofsky actually works 10 miles away from me and I was trying make an appointment with him, but man it’s a six week wait even for a video visit. It’s crazy i had found him and then I see this article speaking of my exact situation that I wanted his second opinion on. Cheers!
Hi Kristian, Mike is great and probably that is why he is so busy. Call back and ask if he has a younger partner – go ahead and say I suggested it. Regards, Fred Coe
I have a 0.3cm kidney stone but am waiting to pass i dont have any pain maybe a little bloated but am bleeding quite a bit for the last 20hours when I pee but also it is coming out without peeing…is this normal
Hi Jo, Your urologist needs to oversee things to be sure the stone is not obstructing a kidney. Be sure he knows what is happening. I am sorry this is so late – Holidays. Fred
Seems I’m not crazy then. I have three “non obstructed” stones in my right side Which I also feel some discomfort and pain.
Luckily they are doing the “laser thing” in two weeks to get them out. But it’s good to know that they can cause some pain/discomfort just being there.
Hi Paul, you are NOT crazy. Fred
Paul have you felt relief?
I was so happy to find this article. I have had stones on and off for 28 years. With the exception of the first two (1 month apart) the early ones were separated by long periods of time, years. In October 2006, i was 5 mos pregnant and i began having them one after another. By the time they could do a CT scan after i gave birth, my kidneys looked like snow had fallen in them. I began seeing an amazing nephrologist, got on some meds, changed diet and not much changed. We tried Allopurinol twice, and definitively found out I’m allergic to it.
I have seen so many urologists that have told me there is NO way a stone could be hurting if they were not obstructing or actively moving. I got snippy with the last PA that very smuggly relayed this info to me and asked her if SHE had ever had 2 or 3 dozen rocks anywhere in her body that they don’t belong?! I even got to meet Dr. Coe several years ago! Idk if he will remember me, but the thing he said that made an indelible impression on me was that of his 6-7,000 patients he had, i was odd amongst the odd. I had both calcium oxalate and phosphate stones 🤦🏽♀️. I’ve always been an ‘overachiever’, but never when i really want to be.
After so many years of struggling, i finally ended up leaving my job which was highly active and required tons of constant movement. The most comfortable thing when my renal pain comes is sitting or lying down with an ice pack. This past Oct is was lucky enough to get into the Mayo Clinic and they diagnosed me with dRTA. I have about 14 stones left and I’m not sure if i am making more. I wish there was a way to just go in and irrigate my kidneys, but there is no guarantee i will or have stopped making them. My stones are small, so lithotripsy is not an option. I take potassium citrate and methotrexate (also for autoimmune issues) to help with stone formation, plus a plethora of other supplements and meds for RA.
I wanted to thank you so very much for writing this article because at times, my doctors have made me feel like i am crazy and just imagining my pain. It’s depressing! Thank you for shedding light on a subject very few people understand. If you have any additional info on Pain without Obstruction, please send it my way! Thank you for all you do 🙏
Ruth B
Hi Ruth, Indeed small stone pain is very prevalent and some research is being done concerning the possible benefits of surgery. I have asked my secretary to look up your record, as I cannot quite remember our time together. I hope the treatment reduces pain for you. Our present thinking is that possibly stones can cause inflammation in kidneys, thence pain. Regards, Fred Coe
I am so glad I found this article. It gives me hope that there are doctors out there starting to realize it is not in our head, but we actually are experiencing pain from non obstructing kidney stones! I am considering going to U of Chicago to be seen. I live in southwest Michigan and having an extremely difficult time getting in to be seen by my Urologist in Kalamazoo. I was diagnosed 3 weeks ago with a 6mm stone in my right kidney and 2mm stone in my left. Last night I made a second trip to the ER for the pain, with reduced urine output. I was concerned it was obstructing. My kidney function came back good. Trace of bacteria and some WBC in my urine, as well as oxilates present. I was sent home with some pain medication, flomax, and torridol. I have been trying unsuccessfully to get an appointment with my Uro. They are not returning my phone calls or MyChart messages. I am an EMT that can’t be out of work for too long. I need to be out taking care of other patients, not being one myself. Is it possible for me to travel to Chicago to be seen? Would I need a referral from my PCP or is the CT confirmation done at the ER enough? I am really struggling with the pain.
Hi Linda, Given your work the ideal is probably that I see you via telehealth concerning the medical issues related to your stones, and you then come into Chicago to see my partner Dr Luke Reynolds who is a brilliant stone surgeon. That way, Luke can have whatever I can add at the beginning, and he can consider what might be worthwhile from a surgical standpoint. If that works, Banita Williams can arrange the former – 773 702 1475. Regards, Fred Coe
Thank you Dr Coe, I wish I had come back and checked the page sooner. I am having lithotripsy for the 6mm x 4mm x 3mm stone on Tuesday (Jan 10th). They are doing nothing for the 2mm in the left kidney. So I would love to see you concerning the 2mm and work on a plan of action. My husband and I both feel it is worth the out of network costs to be treated by you and your colleagues. My in network provider doesn’t believe at all that stones in the kidneys cause pain. I will definitely be in touch to schedule a video consult and possible arrangement to come to Chicago.
Hi Linda, My secretary is at 773 702 1475. It might be most practical to do a telehealth visit first to get things in order and then plan a personal visit if it appears that surgery is really your best approach. Regards, Fred Coe
Thank you for your article. It was very informative. I’m a 40 year old male looking for answers. I have been dealing with burning only after urination for months and some pains in the testicles, pelvic area and back. CT Scan shows a 4x6mm stone in one kidney and two smaller stones in the other. Urine culture is clean. I’ve been on two antibiotics with no help. My urologist doesn’t feel the stones could be causing this issue. Have you experienced any patients that have had urethra burning symptoms with non obstructing stones? I’m wondering if I should have the stones removed or have a cystoscopy first to look at a possible bladder issue. If you are available for a telehealth appointment that would be wonderful.
Hi Eric, Pain in the testicle famously arises from radiation from stones passing in the kidneys. Crystal formation and passage can cause burning and perhaps is causing it for you. Your physicians may find crystals in the urine. Of great import is the cause of all this. I do telehealth as part of my work as a university physician. My secretary is at 773 702 1475. Regards, Fred Coe
Thank you so much for writing about your own experience with this. I feel like I’ve finally looked through a window into something that can actually help me, if I can find a doctor near me that will do this for me! I was told my nonobstructing stone on the right (6mm) was too small to have them break apart because, while it was clear as day on the CT scan it was not visible on the X-ray they did at that appointment. They never mentioned a ureteroscopy was even an option. This gives me hope and tells me I should definitely get a second opinion as I constantly experience pain on my right side between my hip and my ribs, and nothing else has been diagnosed or identified and little helps.
Hi Mon, If you tell me where you live I can try to identify a nearby center. Regards, Fred Coe
This article described exactly what i am starting to go through. My ultrasound showed I have a 1.7 cm kidney stone at the UP Junction and also a 0.6 cm in my right kidney. Instead of removing these stones which already caused my first excruciating wave of pain, my urologist wants to do a cystoscopy to check my bladder. Well, I also had an ultrasound of my bladder and they didnt find anything wrong. So I feel its a waist of time and would prefer my stones be removed immediately.
Hi Richard, I hesitate to comment in that perhaps there are surgical issues here and I am not a surgeon. But given the stone is 1.7 cm I would imagine removal would be important. I apologize for the lateness. Some how your comment was buried. Fred
Have a 19×7 non obstructing stone in left lower pole collecting system. Uro is suggesting litho is this best option? Have had aching left flank for over 12 months and the occasional bout of pain that last a few hours .
Hi Warwick, Let me preface that I am not a surgeon and your question is surgical. Even so, I am aware that large lower pole stones are not ideally treated with shock wave lithotripsy. Perhaps your surgeon is offering ureteroscopy with laser lithotripsy, a better option. As I am not a surgeon, my comment is just that. Regards, Fred Coe
Dr. Borofsky, thanks so much for this article. I obviously don’t know for certain if this is the case, I’m a 45 y/o male with a history of IBS, psoriasis/psoriatic arthritis, and I’ve passed 2 kidney stones previously I have recently had recurring lower abdomen that radiates to my flanks and lower outer back and ended up in the ER recently. For days it won’t hurt at all, but then it comes in waves and it makes me nauseous and feel terrible all over. Best description I could give my wife was, “I would imagine this is what it feels like if a Dementor from Harry Potter touched you.” I didn’t make any connection to potential kidney issues until I read this article…my CT showed “multiple bilateral nonobstructive renal stones measuring up to 4 mm in the inferior pole of the right kidney and 4 mm in the superior pole of the left kidney.” I also showed mild ascites (recovering alcoholic, sober since 2009 but very heavy drinker for years before that) and enteritis, but I’m not sure if that adds any context. At times I feel like the pain radiates TO my kidneys. but then at others I think it’s radiating FROM my kidneys. It is very hard to pinpoint the pain sometimes because of the radiating nature of it. .Either way. my PCP told me that I should follow up with mental to “manage my stress” about this when I talked to her yesterday. Like others have said, this gives me hope that 1) something can help I think I’ll bring this up when I follow up. I’m tired of feeling crazy and looking like a huge hypochondriac. Thank you again!
Hi Brian, Kidney stones can cause pain even when not passing, so the ER physicians can look for blood or crystals. Given your past history there is the possibility of pancreatic pain – pancreatitis from cysts as a possibility. Regards, Fred Coe
I have a small stone 2 .5mm x2 5mm in the right kidney. Un obstructive. Confirmed by ultrasound and CT abdomen .Urine and blood reports are normal.
I am having pain at times and discomfort under the ribs.
Have met 5 urologist as per them stone is not the cause of it…I am taking citrate and flomax as prescribed.
Hi Kumar, I suspect the character of your pain is not like that of kidney stones and your surgeons disdain to operate. I would follow their advice. Regards, Fred Coe
Dr. Coe, My daughter (23) has spent the last 3 years suffering with kidney pain from a series of non-obstructing stones. We have seen every specialist and have a long list of what she ‘doesn’t’ have – she is being turned away from pain specialists because “nothing is wrong”, and was turned away from our local emergency room yesterday with the pain of passing a kidney stone because CTs are clear and blood/urine tests are almost normal (even though her medical history shows three years of tests/doctors visits trying to figure out her condition). Mayo Clinic denied her application for case review, every specialist sends her along to the next, and she is literally in a pain episode as I write this. This article gave me hope that there may be help for her, do you still see patients (we are in Plainfield, IL)? Thanks for the exceptional collection of information. Laura
Hi Laura, I do only telehealth consultation but perhaps can try to find some help for her. I am not a pain specialize not surgeon, although I have an excellent surgical colleague. Regards, Fred Coe 773 702 1475
Are you still seeing patients with televisits?
Hi Laura, I am but I believe things will stop around May 15 for everyone in the US. Regards, Fred
Good Morning Dr.
I was in the ER a month ago now from severe pain in my right side that put me on the floor and nauseous. I got a CT scan w/o dye. Determined it was a stone. Gave me a referral to urologist, and antibiotics Finally got an appointment with him. He dismissed my pain symptoms, ordered a cystoscopy and gave me flomax and an antibiotic I have been in pain since the first day I went to er. I have had constant bladder infections and uti’s that Havnt gone away with the antibiotics. Any activity I do from simple things cause excruciating pain followed by nausea and vomiting. I haven’t been able to work either because of this.
At cysto appointment I was treated very bad. He came into room very dismissive and argumentative. The cystoscopy went bad. I told him it hurt and to stop which he didn’t. The camera was covered in iodine so you couldn’t see anything. From there he left without any comment or explanation. I asked and asked what to do next and he left the room. Next I know the nurse walks me to check out.
I was wondering if I can connect with you to get assistance with information or help.
Thank you
Hi Heather, I am sorry you have had a bad experience, and also sorry this reply is so late – we have had some technical problems on the site. I hope by now things have been better for you and you are well. I do see patients – telehealth – and if that would help please let me know. Regards, Fred Coe