 Nephrocalcinosis means kidneys contain many calcium deposits. You can see them on CT scans or during surgery to remove stones. This article tells about where in kidneys the deposits reside, what they mean, and what significance we need to attach to the word.
Nephrocalcinosis means kidneys contain many calcium deposits. You can see them on CT scans or during surgery to remove stones. This article tells about where in kidneys the deposits reside, what they mean, and what significance we need to attach to the word.
Fuller Albright Made Up the Word Nephrocalcinosis
The boyish face of perhaps the greatest 20th century scientist concerned with kidney stones, Fuller Albright, fills the featured picture. In 1934, Albright, then an Assistant Physician at the MGH and an instructor in medicine at Harvard Medical School, used his newly coined word, nephrocalcinosis in a remarkable paper. That paper described calcium deposits in kidneys of patients with hyperparathyroidism – a mineral disorder caused by enlargement of one or more parathyroid glands.
Who Were His Patients?
He described three types of kidney involvement in primary hyperparathyroidism. Whereas type 1 patients simply formed kidney stones, type 3 patients suffered from acute ‘parathyroid poisoning’, with kidney failure and death. Midway between these two, type 2 patients had stones and kidney tissue calcium deposits but adequate kidney function.
About these Type 2 patients he wrote this passage in which the word first appears (In text box below).
 What Limitations Did His Patients Impose on His Understanding?
What Limitations Did His Patients Impose on His Understanding?
All of his patients suffered from primary hyperparathyroidism, a disease found in only 5% or so of calcium stone formers we see today in our clinics.
Moreover, the tissues he observed came from autopsies, meaning from only his type 2 and 3 patients. His Type 1 patients, who simply formed kidney stones, rarely came to autopsy, so he did not have tissues from them.
As a result Albright coined the word nephrocalcinosis to describe the scarred, contracted kidneys of patients whose primary hyperparathyroidism had caused kidney disease. Their kidney calcifications were a mixture of those from stone formation and those that occur with kidney failure.
Who Are Our Patients?
Like Albright, some have primary hyperparathyroidism. But none have significant kidney failure. They resemble his Type l patients.
Unlike the patients for whom Albright coined nephrocalcinosis, we mainly study patients whose stones arise from no systemic disease at all. They just form stones we ascribe to excessive amounts of daily calcium or oxalate excretion, or low urine volume or citrate, or to combinations of these – so called idiopathic calcium stone formers.
So physicians today use the word nephrocalcinosis to describe very different patients than those Albright studied when he made the word up.
Who Uses the Word Nephrocalcinosis?
Radiologists
They mean many calcified – radio dense – regions overlay the outlines of the kidneys on various kinds of imaging studies: Simple flat plates, ultrasound studies, and CT scans.
But, as in the Cave of Shadows, radiographs are to the reality of tissue as shadows to real objects.
Many Others
When I looked up nephrocalcinosis in PubMed, I found 2686 entries.
Of these, most concerned diseases that calcify kidney tissues: Medullary sponge kidney, kidney transplant, distal renal tubular acidosis, primary hyperparathyroidism, inherited disorders of the kidney, hyperoxaluria, loop diuretics in neonates, vitamin D and A toxicity, FAM20A mutations – enamel renal syndrome -, claudins, hypomagnesemic states, and hypophosphatasia.
As well, I found an excellent review from which this this article takes its starting point: ‘What is Nephrocalcinosis?’ by professors Shavit, Jaeger, and Unwin.
That review begins with a definition: ‘Strictly, the term ‘nephrocalcinosis’ refers to the generalized deposition of calcium oxalate (CaOx) or calcium phosphate (CaPi) in the kidney.’
But where do they form in kidneys, and what do they signify?
Where Kidney Crystals Form
Cortex, Medulla, and Papilla
This stock web drawing depicts a slice through a kidney. The outer capsule runs along the top.
The cortex occupies the upper 1/3 of the kidney slice, above the crescent of red and blue vessels. In it are the filtering units that begin the nephron, the glomerulae, shown as round balls.
Below that crescent of vessels lies the medulla.
At the very bottom of the medulla lies the rounded papillum where urine drains into the renal pelvis and thence down the ureter. Urine exits through the terminal collecting ducts of Bellini – the opening of the thick long tube that runs vertically from cortex to the bottom.
Glomerulae
Each contains a tuft of capillary held within a complex web of cells. The force of the heart filters water and salts out of the capillaries into the tubule of the nephrons. Normal human kidneys contain about one million nephron units. Common measurements of ‘kidney function’ such as serum creatinine reflect the sum total of filtration through all two million glomerulae. Obstruction from stones can reduce filtration.
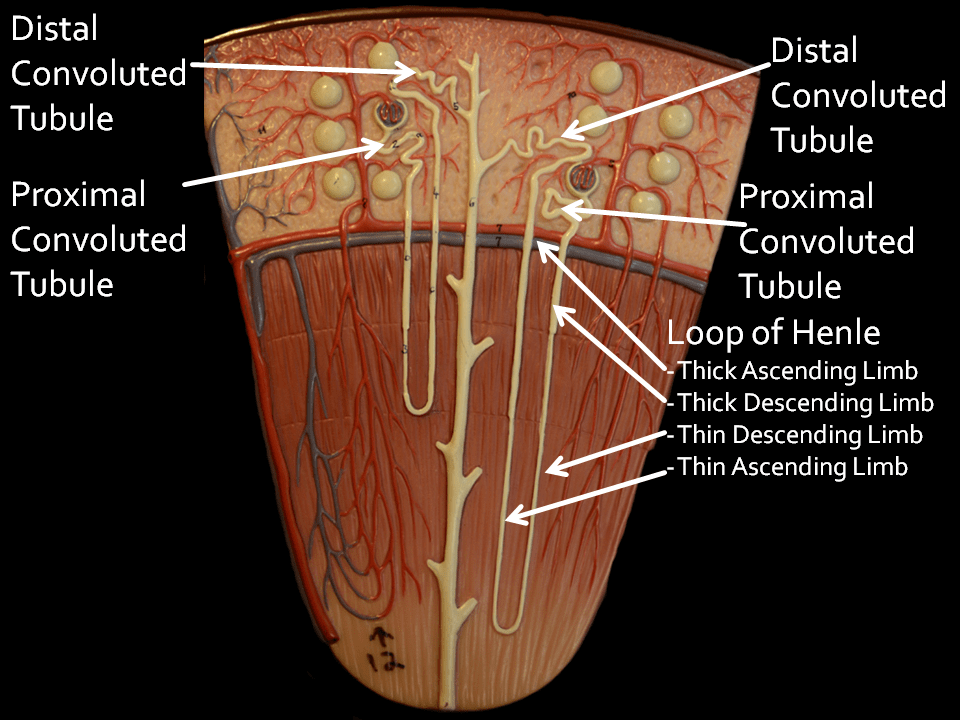
Nephron Segments
Proximal Convoluted tubules
Each glomerulus drains its filtrate into a squiggly – convoluted – ‘proximal’ tubule which gives way into the remaining nephron. These tubules reabsorb much of the filtered water and salt back into the blood. They leave behind materials destined for export into the final urine.
Proximal Straight Tubules
Mislabeled thick descending limbs on the drawing, a part of the proximal tubule extends below the arc of vessels into the medulla and is called the S3 segment. I mention it only because crystals form there sometimes.
Loops of Henle
As they travels downward below the proximal convoluted tubule each nephron thins into a hairpin shaped loop. Those hairpin loops of glomerulae that lie near the outside of the kidney (look at the nephron to the left) reach down only part ways into the medulla – the portion of the kidney below the red crescent of vessels. By contrast, loops from glomerulae near the medulla – just above the crescent of vessels – reach down into the deepest parts of the medulla.
These hairpin loops permit kidneys to concentrate the urine, which means extracting water from the filtrate and putting that water back into the blood. Unlike the proximal convoluted tubules that reabsorb water and salts back into the blood the loops permit reabsorption of water without the salts, so the salts destined for export are concentrated.
Names for the Segments of the Loops
As already mentioned, the ‘Thick Descending Limb’ is actually the S3 segment of the proximal tubule.
It gives way to the descending and ascending thin limbs of the hairpin. The top of the thin ascending limb widens into the ascending thick limb. This segment reabsorbs sodium chloride back into the blood without water, leaving the ‘extra’ water – without its sodium – as a diluted fluid in its lumen. The sodium chloride collects in the medulla around these thick limbs which becomes saltier than blood.
So called Randall’s plaque, over which calcium oxalate stones may form, originates in the outer parts of the thin limbs,
Distal Convoluted Tubule
The dilute fluid drains into the ‘Distal’ convoluted tubule’. Here, the ‘extra’ water leaves, back into the blood. This segment can make the fluid more acidic, and remove calcium back into the blood.
Collecting Ducts
From there, fluid drains through the unmarked straight connecting segment and thence into the collecting ducts. Like any plumbing drains, these run from the cortex down the medulla all the way to the papilla where the final urine flows out. Along the collecting duct the ‘salty’ interstitium around the thick ascending limbs draws water – but not calcium or phosphate or oxalate back into the blood, supersaturating the fluid that remains in the tubule. Collecting duct cells make the fluid more acid, a protection against calcium phosphate crystals.
We name the portion of the collecting ducts that run alongside the medullary thick ascending limbs the outer, and the remainder the inner medullary collecting ducts.
Ducts of Bellini
These terminate the nephron and empty the final urine into the urinary collecting system through tiny holes in the lining of the papillary tip. Because they hold the final, most supersaturated urine, crystals often form in them, creating plugs over which stones form.
Where is the Interstitium?
Envision a tall building. Pipes run from the basement to the roof – water, steam, drains, electrical conduits, elevator shafts, stairwells. Now, think about the space between the elevator shafts, stairwells, and all the pipes and conduits: That is the interstitium, what stands between.
In the kidney the long structures are the tubules and vessels; the interstitium is the space between them. That is where plaque is. There are cells in the interstitium – it is as though, as an example, insulation blocks were stuffed into the spaces between pipes.
Mice can live in the spaces between things, but not in the pipes. Rust can plug pipes but not the spaces between them.
The Reward for Brave Hearts
To those who have read the foregoing: My regards and admiration. Like tourists who climb the ancient, winding, broken stairs up into the towers of medieval cathedrals or the battlements of long abandoned castles, panting and worried about getting back down, you now come into the reward of so much virtue and endurance. Before you lies the architecture of the nephron.
Where the Crystals Form
From what I have told you, where would you surmise crystals might form?
Surely not, you might say, in the glomerulae or proximal tubules, or in the thick ascending limbs with their excess of water. The distal tubules, perhaps, as they extract water, but – you might think – it is only the extra water.
Ah! That vast long drain, where water extraction supersaturates urine – there would crystals form.
And, those uncanny thin limbs, so deep into the medulla.
You are right.
Who Sees Them?
When radiologists spy calcium deposits in kidneys so numerous they name them nephrocalcinosis, the deposits lie – with rare exceptions – in the medulla, the papillum. Surgeons can see them in the collecting ducts and interstitium. For pathologists they lie in the thin limbs, the collecting ducts, and the interstitium – the space between the ducts.
Crystal Deposits in the Cortex
These occur in rare stone diseases. I list them for completeness only.
Glomeruli
In humans, high blood calcium can produce glomerular crystals. Hyperparathyroidism for example, when severe.
Shall I mention intravenous dibasic phosphate in rats, Vitamin D intoxication in suckling rats, calcifications of large immune deposits? No; I demur. Not relevant to humans.
Proximal tubules
We have found calcium oxalate crystals in the proximal tubule S3 segment in primary hyperoxaluria. 2,8 dihydroxyadanine crystals due to APRT deficiency can plug proximal tubules. In transplanted kidneys we have seen scattered birefringent crystals presumably calcium oxalate.
In other words, common stone formers have no proximal tubule calcifications, only patients with rare diseases.
Distal Convoluted Tubules and Cortical Collecting ducts.
Acute phosphate nephropathy from bowel preparation is well known. Distal convoluted tubules contain calcium phosphate deposits in cystine and primary hyperparathyroid patients,and calcium oxalate in primary hyperoxaluria stone formers. In transplanted kidneys tubule and interstitial deposits are found not rarely and are said to be calcium phosphate. In primary hyperparathyroidism with stones, and ileostomy patients, deposits were found in the cortical collecting ducts.
This means, here and there, uncommonly, scattered deposits can lie in the cortex.
Cortical Interstitium
When kidneys fail and blood accumulates excesses of salts and molecules kidneys normally eliminate, crystals form in the space between tubules, the interstitium because blood itself supersaturates. The same for primary hyperoxaluria: so much oxalate is produced it can accumulate in blood and crystallize in the interstitium.
Cortical Blood Vessels?
We believe it is potentially confusing to lump vascular disease and its associated calcifications together with calcifications within the renal tubules and interstitium.
Crystal Deposits in the Medulla and Papilla – Work by Us
Our reports comprises the bulk of human kidney tissue work to date.
Thick ascending limbs
No deposits have been found in any stone formers to date.
Thin Loops of Henle
We have found rare hydroxyapatite deposits plugging thin limbs in ileostomy, cystinuria and primary hyperoxaluria patients with reduced renal function. These are best illustrated in Figure 4 of the ileostomy reference. As I have mentioned, plaque begins in the outer shells of the thin limbs.
Outer Medullary Collecting Ducts
Patients with primary hyperparathyroidism are the only stone formers who show deposits (calcium phosphate) plugging this tubular segment.
Inner Medullary Collecting Ducts
Here is the main place for crystal formation. Are you surprised? The tubule contains supersaturated fluid progressively approximating urine itself. No wonder of it: crystals from where supersaturation is.
Hydroxyapatite crystal plugs
Crystal intraluminal plugs have been found in all eleven stone forming phenotypes examined. The majority of these plugs are composed of hydroxyapatite. Note the link goes to an article on this site which lists 10 phenotypes; ICSF, the 11th phenotype, did not reveal collecting duct deposits in our work but deposits of HA were found in cases of ICSF reported by Wang et al.
Calcium oxalate crystal plugs
Obesity bypass surgery, distal renal tubular acidosis, small bowel resection, and medullary sponge kidney stone patients form calcium oxalate deposits.
Mixture of sodium acid urate and ammonium acid urate was admixed with biological apatite in ileostomy stone formers.
The Odd Microliths of MSK
Microliths, myriads of extremely small, round, non-adherent stones have been found only in the dilated IMCD of MSK patients. These differ from plugs in virtually all respects. Plugs adhere to IMCD lining cells and cause cell damage, and death, MSK microliths do not adhere nor cause any perceptible damage. Microliths are round, not cylindrical, and made up of concentric layers of crystal; plugs also have layers but much less regular.
Cystine Plugs
Cystine plugs also differ from all other plugs in not adhering to tubule cells. They move freely and do not appear to damage the cells.
Ducts of Bellini
We have found Bellini duct crystal plugs in all stone forming phenotypes.
This is expected as these ducts contain the final urine.
Bellini duct plugs may attract overgrowths at their distal ends that protrude through a dilated opening of the duct into the flowing final urine. These proto stones may well grow to clinically significant size. Growth on plugs is one pathway for stone production.
Interstitium
To date, all interstitial deposits found in human kidneys have been hydroxyapatite ‘Randall’s’ plaque. Growth of stones over plaque is another pathway for stone production.
What About Blood Vessels?
No evidence exists showing calcium deposits within the vasa recta within the medulla or papilla. Deposits of hydroxyapatite can be found within and involving capillaries, but this is not evidence of a primary calcification. Theoretical papers proposing vascular injury and calcification as causes of plaque have failed to advance direct evidence in support of the theory.
Crystal Deposits in the Medulla and Papilla – Work by Others
Idiopathic calcium oxalate stone formers
Idiopathic calcium oxalate stone formers display variable amounts of interstitial plaque. Those with hypercalciuria had the heavier plaque deposits, much as we have found. Unlike our work, many patients had crystal plugs in Bellini ducts. Wang et al described much the same.
In biopsy tissue from 15 patients with ‘idiopathic calcium stones’ not otherwise characterized, Khan et al found Large areas of interstitial plaque. Crystals were HA. No plugging was found. Stones were calcium oxalate. The main finding was intimate association of plaque with collagen, as we have also described.
Mixtures of stone formers
Linnes et al studied ICSF, ICSF with malabsorption, phosphate stone formers which included struvite stones, and, also, uric acid stone formers. In 99% of patients they found interstitial plaque with an average low abundance. It was only when they separated out hypercalciuric ICSF that they found high plaque abundances as we have. They found plugging in all stone phenotypes. The patients were mostly female, and hypercalciuria was not impressive. They did not analyse the crystals in the plugs.
Single case report
Report of a single case describes interstitial plaque deposits identical to those we have described. The patient had large calcium oxalate staghorn stones. By EDX analysis the interstitial deposits were calcium phosphate. Tubule plugs were found in the medullary collecting ducts and these were calcium oxalate. We suspect this patient had primary hyperoxaluria.
Putting it All Together
Overall, these and our papers more or less agree. Stone former kidneys contain interstitial calcium phosphate deposits and plugs in Bellini duct and inner medullary collecting ducts. Only we and Khan have described the crystals in plugs to date. So, when we speak of multiple crystal deposits in the kidneys of stone formers, or nephrocalcinosis, we all seem to mean plaque and plugs. MSK differs altogether, because dilated ducts contain myriads of calcium oxalate microliths.
Virtually all Stone Formers Manifest Nephrocalcinosis
Virtually all Stone Formers Form Kidney Crystal Deposits
Shavit, Jaeger, and Unwin concur with Albright: ‘Strictly, the term ‘nephrocalcinosis’ refers to the generalized deposition of calcium oxalate (CaOx) or calcium phosphate (CaPi) in the kidney.’ Since virtually all stone formers deposit crystals in their kidney tissues, virtually all have nephrocalcinosis.
The Kinds of Deposits Number Three
One kind is plaque – calcium phosphate as hydroxyapatite – in the interstitium.
The second kind is plugging of the lumens of the various tubule segments, mainly the medullary and papillary collecting ducts. These plugs are usually calcium phosphate but can be calcium oxalate, cystine, or uric acid salts.
Of the three, the microliths of MSK, unique to this one disease, make up the third.
The Word Means Plaque and Plugs, or MSK
In any one patient nephrocalcinosis means interstitial calcium phosphate crystals, tubule crystal plugs of diverse kinds, or both, and microliths in the dilated tubules of MSK.
Because of this specificity, I propose we restrict the word to this exact meaning: Calcifications within kidney tissues as demonstrated directly in the tissues themselves.
Radiographic Nephrocalcinosis
Because tissue calcifications and stones both brighten the confining shadows of the radiologist with similar points of light but stones do, also. Therefore, we propose the term ‘radiographic nephrocalcinosis’ define what radiologists report. I say this because radiological means cannot always distinguish masses of tissue plugs or of microliths in MSK from stones.
Surgery
Because they visualize stones, plaque, and plugging, and also the odd contours of MSK, surgeons can not only specify nephrocalcinosis but the type of calcium deposit. Therefore, they mean by nephrocalcinosis what pathologists mean. The only difference between them is in resolution. One has a microscope, the other simply an external view of the kidneys at modest magnification.
Meaning of Nephrocalcinosis
Since all stone forming patients deposit calcium in their kidney tissues, it signifies a quantitative vs. a qualitative distinction. Unlike other patients, those with nephrocalcinosis have more tissue calcium deposits and therefore, perhaps, what one might call more disease burden.
By disease burden I mean the tissues carry more crystals in them, and therefore a greater hazard from whatever evil it is that crystals might do.
One such evil: lodgment for new stones to form on. Because stones form on plaque and the ends of plugs, more plaque and more plugs implies a greater stone production potential. Although evidence for such potential must come, eventually, from prospective observations greater tissue mineral burden seems a proper spur to greater treatment effort even now. Such greater treatment efforts mean perhaps more emphasis to patients about diet and fluid change, and earlier use of medications.
Another is tissue damage. For example, crystal plugs cause obvious tubule cell loss and inflammation in the surrounding interstitium. Although papillary, plugging may affect the cortex. Compared to patients without plugging, those with plugging have more cortical interstitial scarring that treatment might benefit. Such treatment, as opposed to stone prevention alone, would specially emphasize reduction of calcium phosphate supersaturation.
Like many stones, nephrocalcinosis quantifies stone diseases. But in a new dimension, one that complements those already in use. Because complementary, the word adds specific value, provided we use it carefully.

I like your definition of “Interstitium” 🙂 I finally understand what it means! In not one of the articles or studies I’ve read to date that mention interstitium, do they explain where it’s found! Thanks.
I think many people are unsure where it is. Fred
I have a question Fredric. You say that blood vessels and vascular disease have nothing to do with cortical calcifications and again quote “No evidence exists showing calcium deposits within the vasa recta within the medulla or papilla. Deposits of hydroxyapatite can be found within and involving capillaries, but this is not evidence of a primary calcification” however you also refer to a study in Pubmed “What is Nephrocalcinosis?’ by professors Shavit, Jaeger, and Unwin; where they state ” . We have concluded, and hypothesized, that nephrocalcinosis is primarily a renal interstitial process, resembling metastatic calcification, and that it may have some features in common with, and pathogenic links to, vascular calcification”. Since my sister was also diagnosed in 2012 with atherosclerosis, besides MSK and nephrocalcinosis,
I’ve read many similar studies that compare atherosclerosis or soft tissue calcifications to nephrocalcinosis, that renal arteries may also be affected, that heart disease due to atherosclerosis is associated to CKD. I’ve read that some of the systemic autoimmune disorders like lupus sjorgren’s scleroderma Wegener’s vasculitis can cause glomerularnephritis, renal vasculopathy involving renal arteries, arterioles and small blood vessels. Some of our members have been diagnosed with one of those autoimmune disorders, one or more with EDS. One of our MSK members was recently admitted to hospital following a heart attack and was diagnosed with atherosclerosis.
Do you think in these cases, their MSK and nephrocalcinosis could have something to do with vascular disease? If not, how exactly do these systemic autoimmune diseases affect kidneys and what do they have to do with MSK and nephrocalcinosis in our members? Thank you.
Hi Celia. Thanks for the detailed and interesting question. Clearly I admire the review, which I chose as an introduction to my article yet do not agree with everything in it. In particular the vascular theory of plaque seems, to me at least, to lack adequate supporting data and therefore remains a theory and no more. Many confusions arise in the area of renal crystallizations because kidney disease itself appears to lead to deposits and certain kinds of renal diseases arise from vasculitis. Thus far no evidence supports the idea that interstitial plaque is part of an atherosclerosis process. Chronic kidney disease is associated with heart disease, and kidney stones are epidemiologically associated with vascular disease, but plaque and vascular disease are not associated. Sjogren syndrome causes a form of renal tubular acidosis readily identified in most cases by reduced blood bicarbonate and unduly alkaline urine. SLE renal involvement can produce a form of renal tubular acidosis. These are easily distinguished from the idiopathic stone formers, and readily diagnosed on their own terms. The vasculitides – scleroderma and Wegener’s renal involvement are very serious and usually reduce kidney function and produce multiple other abnormalities that permits their diagnosis. MSK itself is a renal developmental disease and I know of no associations with the aforementioned conditions. All of this negative commentary is not meant as a final word, but as my best immediate summary of what has supportive data and what does not. Moreover, although I am a nephrologist, I do not pretend to definitive expertise across the vast range of diseases in this paragraph. So, take this as an initial note, and over time our site will – in the course of things – try to clarify these inter-disease relationships. The site is very new, only one year old, and meant to evolve over some years. I hope this initial answer offers some ideas to consider. Regards, Fred Coe
Thank you Fredric for your expert feedback, I appreciate that. You’re right about the different systemic autoimmune diseases that affect kidneys do cause RTA besides nephrocalcinosis, I forgot about that! I don’t have a nephrologist so have no one I can ask these questions, thanks for your help and patience!
I am delighted, Celia; I put up this site so people could get reliable information, from me or from other people who are experts in this field. Thanks for affording an opportunity to bring these issues into a public forum. Regards, Fred
Very interesting article.
Thank you, Linda. I appreciate your compliment. Best, Fred
I was diagnosed with dRTA, nephrocalcinosis, and medullary sponge kidney. Is it safe for me to assume that one or more of these diagnostic outcomes could better be diagnosed by endoscopy during surgery? I have had approx. 6 laser ureterscopies and never , what would be the advantage of one over another? Also, on this topic which procedure would be best to access the bellini? Last time my urologist accessed the caylx! Could he go further? He has been my surgeon since the start and I fully trust him, I pestered him to get to the calyx (often in the past he would do mine for a stuck stone, which happens often. I am also wondering is it the bellini that needs to be unroofed? Thank you for this article I am really liking this dialogue with you, saves us all from confusion, and I love the analogies and gives us a chance to ask instead of waiting until the next appointment with our doctors.
Hi Laura, During ureteroscopy your surgeon could surely determine if you do or do not have MSK. Renal tubular acidosis is diagnosed by functional testing, not surgery. The Bellini Ducts are very tiny and are not entered. Unroofing ducts to remove crystal deposits is presently an untested surgery. Some surgeons favor it when deposits are large and there is pain without obstructing stones. Surgeons remove stones from calyces so I assume your surgeon easily enters them when needed. I am glad this site and some answers are helpful. Most of all, it is your physicians who care for you, and I am sure their intention is always to prevent stones – that is the main purpose of everyone. Regards, Fred Coe
I understand that my physicians are my primary source of information and care and I have good doctors. What I meant to ask and realize now that I left it out somehow, is what is the main difference between ureterscopies and percutaneous procedures? For instance why would one be benefical
Over the other. When would one be used over the other.
Hi Laura, I believe I answered this below. The decision is specific to a particular patient and stone problem, and to the surgeon, also. Both modalities can achieve outstanding results when used properly. Being to particular it would be foolish of me to try to offer any useful generalizations. Regards, Fred Coe
Laura,
I also have dRTA. I can only tell you what I have learned about my specific issues and this may or may not apply to you. Often, PCNL percutaneous nephrolithotomy is done to remove large stones… usually your urologist has already tried URS and/ or ESWL, often more than one time and nothing worked. PCNL is usually the most invasive procedure urologists do to remove kidney stones, so it can be the procedure of last resort. Since, an incision is made there can be a greater risk of infection and greater chance of some other complications. Also I believe a nephrostomy tube usually may be left in… it drains urine from your kidneys but bypasses the ureters and bladder… I think this is the tube that your urologist uses to get the instruments to your kidney… the instruments used to remove the offending stones. However, when there is a need for a PCNL your situation is carefully evaluated by urologists and radiologists.. before they do anything.
Also it is beneficial to have a nephrologist be involved… in 1983 I had emergency open surgery… after my urologist and nephrologist had an argument about releasing me from the hospital. Additional tests were performed.., an IVP which was used before CT scans were invented and a group of stones was about to move around and form a new blockage. I would have had to make another trip back to the ER room, if my nephrologist had not been there. I did not feel extremely sick but, I was in the OR within 20 minutes after the anesthesiologist came into my hospital room..( when you had an IVP, you could not eat or drink anything for a while… and or urinate.) I did make a full recovery but the normal recovery time from open surgery was about 3 months… that is why the new procedures are so important. Hospitalization time has become very short and often people can go back to work within a few days after a procedure. Many procedures are done out patient or in day surgery situations..
Dr. Coe may tell you some of this is erroneous, which it may be. I am not claiming to be an expert … I am only trying to explain some things I experienced.
Trish
Before, lasers and modern techniques : cystoscopies with a stone catcher basket could be done and open surgery. Many urologists have never done open surgery… because they are young enough that URS, ESWL and PCNL existed.. these started to be used in the US around the mid 1980ies, I believe. Towards the end of the 1980ies these methods were taught in urology residency programs.
This is my general understanding of the development of modern surgical methods… and some hospitals, medical groups etc. got the lasers and instruments for the new methods, years before smaller hospitals did. Even today, there are companies that have ESWL machines in the back of a semi truck and they travel around to various hospitals…
I was also told that either ESWL or URS can be used in a given situation.. it is up to the your urologist to determine this, based on his skill set and experience… Some are better at one than the other… and sometimes your doctor may refer you to his partner or another urologist he believes is more skilled then he is
Dear Laura and Trish, No, I will not say any of what you have said is erroneous; you are valiant and capable people fathoming the complexities of a very complex branch of surgery. I will say that there are three prime modalities for surgical stone management, ESWL, PERC, and URS, and their use in a given case is a subtle choice for even the most skilled urologists. I believe all three modalities should be available for a patient, and patients should have their pros and cons explained so they can participate in the final choice. All of the urologists I know well more or less will agree with this statement. Ideally it is not so much the skill set of the surgeon as it is the best modality for a given stone situation that drives the eventual decision. If I may I would add that prevention is better than treatment, and every effort should be made to stop stones from forming. Warm Regards, Fred Coe
Hi Laura, ureteroscopy is via the urinary tract; an instrument is passed up the urethra into the ureter and thence the kidney. Percutaneous nephrolithotomy requires a hole be made in the back and an instrument passed into the body and through the outer cortex of the kidney into the renal pelvis. This permits use of larger instruments but is invasive. The choice of URS vs. Perc is very complex and individual to the specific patient and surgeon. Regards, Fred Coe
Thank you for letting me post Dr. Coe. I do appreciate what you are doing and how you are trying to educate all of us kidney stoners. I had several urologists who explained things to me over time… for about 4 months in 2008. I also had lots of problems as the last time I had procedures, I was forced to go the university in my state. My urologist of over 20 years retired. There is one medical school here and indigent people can come from 300 miles away… besides the more local ones.
I had many problems getting my urologist/attending to communicate with me… as the residents were in the middle of it. So I became friends with an administrative assistant for the urology department. Also the man who became my doctor, was forced to work on kidney stone patients.. for a few years. His sub specialty is not kidney stones. There is a shortage of doctors in my state and the university has a hard time recruiting new doctors… and many come and stay a couple of yeasr. I also had/have a better rapport with the urology nurse practioner… Since my urologist was so busy with other patients… who are sicker than I was/am I elected to see the nurse practioner.., I did not need the expertise of my urologist.
Due to the fact there are really no urologists in a metro area of over 500,000 people who I feel are qualified to treat me.. I have elected to go to another state. My new doctor’s sub specialty is kidney stones and he/she is one of the best doctors in the US.
Trish
Dear Trish, I hope your move gets you better care. With your new doctor I hope the emphasis is on prevention of more stones. The whole secret for stone formers in getting life back together medically is prevention of new stones. That is what this site aims at, and your new doctor, too. Best, Fred Coe
Dr. Coe,
Can you explain about the GFR and what it means? Is it possible to estimate the course of dRTA from all the lab work and 24 hour urine tests? I know my kidneys are irreversibly damaged by nephrocalcinois. Is it possible for me to make a bucket list prior to dialysis? I am going to call my nephrologist and ask him these questions… and if he could give me that information, why hasn’t he? I am only asking for general guidelines and a broad time frame. According to what I have learned, better technology might be able to offer some hope.. as you described the need for more accurate and better CT scans… and that there are doctors, and other scientists working on that right now. My other thought, may be too disturbing for this: but it is possible I could die from something else, before dialysis is necessary.
I am not trying to scare all these other folks and say everyone with dRTA will need dialysis.. I can’t generalize my situation to all of the other kidney stoners. I know most of my stones are calcium phosphate and calcium oxalate. I also understand there are degrees of neprocalcinosis and mine is worst than most people have. I want to understand what is really going on with my disease and be told the truth, as much as possible. No doctor ever told me I would be dialysis material if I lived long enough; I went to the medical library and looked it up myself after my emergency open surgery I mentioned.
So all that is left is to take my Urocit K, drink lots of water and moderate my salt intake.. It is very frustrating to feel like there is so little I can do.. but I want to enjoy what time I have left. I can’t begin to describe how I feel… only that I have had dRTA for almost 50 years, and I am 63 now. I don’t need sympathy and I am not trying to get attention by having other people feel sorry for me. I guess what I want is an action plan. I don’t want the other kidney stoners to think I am an expert or that there is no hope for anyone with kidney stones. I know most folks can have a better treatment plan and prognosis than I do.
Trish
Hi Trish,I am not so sure you are right about dialysis. The routine serum measurements you got especially if used along with 24 hour urine measurements give pretty good values for kidney function and I will bet – on sheer likelihood that your kidney function is normal or near normal. I have had a very long career experience with kidney stones including renal tubular acidosis and almost no one has even gone on to dialysis. Those few have included patients from an earlier time who lost kidneys from obstruction or from the very invasive surgical procedures that once were needed. By all means ask your nephrologist about your kidney function, however, and if it is reduced about the rate of progression. Hopefully I am right – and you are not in such danger of dialysis. Regards, Fred Coe
Thank you Dr. Coe. Maybe I have misunderstood what my new urologist inferred. Also I still live in the same place with a shortage of good doctors… I got sick of how I was treated at the university and discovered that at this point in time, they offered the best doctors. It is not the doctors fault.. things are bad, due to a shortage of funding and too many patients, mainly. It is the fault of the state legislature and board of regents who mainly determine funding for the medical school/university hospital and clinics. It is a problem with the state I am in because it is largely a poor state with a population spread out in remote areas. The whole situation is a very complex political problem… how to treat all these indigent people. I saw people who appeared to be disadvantaged in ways I could never have even dreamed of. Each time I went there, I felt very fortunate.
It is around 1500 miles to see my new urologist, round trip. The way I look at it is you only have 2 kidneys, but only one life. It is worth it to make the best of the time I have left.
I am getting a lot out of this and trying to understand all this anatomy, physiology and chemistry. If I had known when I was younger that I would need an understanding of that so I can advocate for myself, I would have taken biology, chemistry etc. in college and not botany, geology and astronomy.
Trish
Thanks, Trish, for your comments as I am sure many will find them of interest and value. University hospitals do often have excellent doctors who are urged to see too many patients or have competing activities like patients and grants and research publication, or both with the result that nothing is done as well as it could be done. As for botany, geology, and astronomy, these may be better for a life lived – the small and the large plants, the world of earth, and the cosmos. All the best Fred Coe
Dr. Coe,
Does nephrocalcinosis caused by previous kidney infection will eventually lead to end stage kidney failure/dialysis?my nephrologist and urologist say i have a normal kidney function according to previous tests i had. My calcium, potassium, hemoglobin,uric acid are in normal range, and no protein in my urine.my right kidney is scarred and reduced in size but is working 24%, my left kidney is normal in size and shape but with nephrocalcinosis..what is the prognosis?im too scared and have pain on my kidney but my doctors tell me not to worry.im 36 y/o, female..thanks
Dear Antonette, nephrocalcinosis does not usually result in kidney failure. It appears that your right kidney has been damaged, but it is not clear why. Do you know why? Have you produced stones? Do others in your family have kidney disease of this kind? Is your kidney pain from infection, stones? Is your blood pressure high? I would be happy to help more but the amount of information is too slight. Regards, Fred Coe
Dr. Coe,
I was told by my doctors that maybe i was born with my small right kidney, but i was thinking my recurrent kidney infections in the past have caused it. I have no diabetes, normal blood pressure, no kidney disease runs in my family, i never had produced a single stone and never passed one. My urologist tells me every time that my pain is not kidney related as my urine test always comes back normal but im still sick worried because it is constant though its the dull type. He tells me as well that i should not worry about having dialysis in the future as the possibility is very low.I am worried because i have only one functioning kidney but it has nephrocalcinosis and i have pain.my last creatinine reading was 68 mmol/l, i am a 36 y/o, female, small built (95 lbs, 5’0″ tall), asian descent..hope you could give me some more insights about my condition..im starting to feel so hopeless because of my pain and the endless worry i seem to have every single day..thanks
Antonette
Hi Antonette, It sounds like the right kidney has somehow been mostly lost and your good kidney has stones in it. Your doctor is right that you should be able to live a full life without fear of dialysis. It is very important to know why you made the stones and to undertake prevention against more of them. If you have stone passage get care immediately as one obstructed kidney means transient but possibly severe loss of kidney function until it passes. I would avoid shock wave lithotripsy if possible in favor of flexible ureteroscopy if you need stone surgery. Regards, Fred Coe
Hello and thank you for the informative site! I was just diagnosed with MSK following a renal ultrasound and CT w/o contrast showed that my pyramids were “full” of stones, mostly tiny but a few large, 4-10mm. I have no pain and haven’t passed a stone in 20 years, that I know of. The purpose of the ultrasound was to check my renal arteries (which were fine) bc of sudden hypertension. After reading this, I am unconvinced that what they saw are actually stones, but it seems as though the only way to know for sure is uteroscopy? Am I understanding that right? But if mine are in the medulla, uteroscopy can’t reach them, correct? Any insight or guidance as to how to proceed or what to ask my neph for would be greatly appreciated!
Hi Melissa, You ask a very important question. If you have no pain, and are not passing stones it is not clear to me why you would benefit from any urological procedure at all. I would guess many of the crystallizations are in the most distal parts of the collecting ducts and this would be seen during ureteroscopy but why see them if nothing needs to be done. The big question is why the sudden increase in blood pressure and if there is a relationship between the calcifications and the blood pressure. The obvious link is the blood calcium; primary hyperparathyroidism can produce the calcifications and raise blood pressure so it is crucial that your blood calcium be normal. Also crucial is your level of kidney function. There are conditions in which calcifications occur because of kidney problems which in turn can raise blood pressure. So there is a lot for your nephrologist to do, and little your urologist needs to do. If you have further questions please feel free to post them. All the best, Fred Coe
Thank you!
Thank you so much, My daughter has nephrocalcinosis. She is 12. She was diagnosed about 7 years ago. It is so hard to find good information on the net. They tell me that there is no reason she would have nephrocalcinosis, so they say it is hereditary. She leaks protein and calcium. Currently she is on a low sodium diet and take 2.5 mg lisinopril, Diuril and Cytra K. I am told this is managing the condition. I am also told Transplant is inevitable at some point but we are not sure when. Its frustrating that I am unsure a clear cut prognosis. At some point they thought she had Dent’s Disease, but this was not the case. Are there any more sites or helpful information? Thank you so much for your time and consideration.
Hi Chris, I gather your daughter that the combination of high urine calcium, nephrocalcinosis, and high urine protein. There are many genetic causes of which DENT is one – and it is a catchall name for a variety of genetic abnormalities. Here is a link to OMIM – the main national database for gene disorders involving the three problems your daughter has. She needs a full evaluation to figure out exactly what is wrong and then help evaluate possible treatment and prognosis. I would urine her physicians to consider the wide range of possibilities and identify her problem more exactly. Regards, Fred Coe
Dear Dr Coe, I just had my health screening down. Report came back with hypertension for CASP of 148mmhg with arterial stiffness severe. Radiology report stated ‘echogenic renal pyramids seen bilaterally secondary to nephrocalcinosis and right renal septated cyst 0.8×0.5cm in mid pole of right kidney’. Blood calcium is 2.53mmol/L (within normal range). Free T4 is 14.39pmol/L and TSH 0.8157mIU/L. All other test including cholesterol & renal function screen were in the normal range. I am active in sports and has a BMI of 8.4 (just hitting the normal low range). As my BP is high, the doctor wants to put me on Norvasc 10mg. I am a little hesitant to start as I was wondering if the high BP could be due to nephrocalcinosis or any kidney conditions such as pheochromocytoma? I am reading up more on nephrocalcinosis & your posts have provided me with more insights about the condition. I am just perplexed about my hypertension & was wondering if there’s even a slight chance of nephrocalcinosis linking to hypertension, in my case, since my hypertension is idiopathic & now I know I have bilateral nephrocalcinosis & cyst. Would appreciate your advise on this. Thank you. Rdgs, Jen
Dear Jennifer, nephrocalcinosis itself is not known to be a direct cause of hypertension, although I would assume that in some cases it might play a role. Pheochromocytoma is an uncommon adrenal tumor and has no relationship to nephrocalcinosis, nor is there any specific evidence for it in your case that you have presented in your note. Renal cysts are their own world in that they require appropriate surveillance and interpretation by experts in reading those kinds of ultrasound and CT images. SOmetimes renal cysts can raise blood pressure if one compresses an important renal arterial branch but it is an uncommon situation. So although I like to find unitary diagnoses, you may indeed have separate ones. As for treatment of your increased blood pressure, you should certainly take whatever means your physicians suggest to lower it. Regards, Fred Coe
Dear Dr Coe,
Thank you for taking the time to explain to me. I now understand that there may be other specific areas which I need to address wrt to hypertension. I am at least now comforted to know that nephrocalcinosis isn’t a condition which has drastic end result as I have ‘feared’. Thank you very much. Rdgs, Jen
Following Microscopic Haematuria, My daughter is diagnosed with Medullary Nephrocalcinosis in correlation with calcium metabolism. Also in her ultra sound scan it states ‘no Hydronephrosis of obvious calculi seen’.
Her renal function tests state Sodium 141 mmol/L 133-146 Potassium 3.9 mmol/L 3.5-5.0 Creatinine 46 umol/L 46-70
Can her condition be reversed or fully cured with treatment and relevant diet?
Hi Nicky, The serum values you sent are normal. Of greater import are her 24 hour urine results. SHe needs such studies and they will be the key to prevention of more calcifications and stones. One cannot reverse the calcifications in place, in most instances, but preventioin of more is reasonable. Diet is important as is fluids and perhaps medication depending on the results. Regards, Fred Coe
Thank you Dr Coe for taking time out to help very distressed people, understand and manage a life changing and often very debilitating condition.
Hi Doc,
I am 25yr/old and diagnosed with BILATERAL RENAL MEDULARY NEPHROCALCINOSIS.
Both of my kidneys has it. On the right it measures 10.0×5.2×3.6 cm. left kidney 10.8×3.8×4.2 cm cortical thickness of 1.2cm. both have hypoechoicparenchymal echo. there are innumerable small medullary calcificatin in both kidney. No hydronephrosis.
creatinine= .7 mg/dL
uric acid= 4.6
calcium= 2.39
My treatment as per the doctor i seen is diet modification, I have to take potassium citrate (acalka) 1tab 3x/day and drink plenty of water. I wanted to ask if this condition is reversable, or can easily be treated. What things shoul I have to do so it will not lead to some serious kidney disease (renal failure) ? will it be illiminated, its really been bothering me if my kidneys are in serius problem already. Please help me be enlightened on my condition.
Hi Mariel, You have formed a large number of small stones, usually these are calcium phosphate. Prevention of more is important – take a look at this summary article that links to others you may find valuable for details. Kidney failure is rare, and prevention of more stones certainly a reasonable goal. Regards, Fred Coe
Dear Doctor Coe, thank you so for the informative articles. I am so greatful to have an idea on what to do, and I now have certain relief on my anxieties on it having to turn into serious kidney disease.
I have Medullary Nephrocalnosis. The last few months I been passing many stones together 15 at once .The biggest was 6mm with spikes rest were 1 mm so 22 mm at once . This is crazy .It like I shedding stones is this a normal thing ? I use to just pass sand and 1 big one a month .what is going on with me.I feel like I have Aliens living inside me.I have pain all the time with pain control.
Hi Lori, I suspect these stones are calcium phosphate; is that the case? If not, let me know. Usually there are obvious abnormalities in the 24 hour urine tests; do you have such tests and so they show abnormalities?? Regards, Fred Coe
Hi Dr. Coe, I had a recent kidney ultrasound and it says that medullary calcification left kidney. Normal sonogram on the right kidney and urinary bladder. What does that mean? Can you please explain to me? Thank you!
Hi Babee, It means you have stones or calcium deposits in your left kidney which is most likely stones and you need to find out why you are doing this. Here is a reasonable approach. Since you do not pass stones, you cannot know what the crystals are, but you can get 24 hour urine testing and find out what about you might predispose to forming crystals and treat that, Regards, Fred Coe
I had my first kidney Stone diagnosed in 2007. It was almost an inch long and lying in the bottom pole of the left kidney. The urologist I saw said we didn’t need to do anything because that stone was not blocking any ducts and could not be causing me any pain. I went back to him a year later and told him the pain was unbearable and he finally did a lithotripsy. He did not get all the fragments out because the stone was extremely hard and he had to stop the shockwaves before he damaged my kidney. After that, though, the pain went away as well as my IBS symptoms. This lasted almost two years, but I started to have mild pain in BOTH kidneys. When it started getting really bad, I went back to that urologist. Again, I had a stone that was a little over half an inch long lying in the bottom pole of the left kidney. Again, he told me it could not be hurting me and refused to do anything. I asked him why both of my kidneys were hurting and he told me that the right kidney had no stone on x-ray. A few months later I went to a new urologist and she told me the same thing and refused to do any procedure to remove the stone. I finally went to a new urologist in 2015 (I was caring for my mother with terminal cancer in the interim). After my mother passed away I was able to go and see this new urologist who told me that of course the stone would cause pain because of the size of it and because it’s a big rock in my kidney that doesn’t belong there. He agreed to do a stone basket retrieval, which was successful, but my pain didn’t go away. He also told me that on CT without contrast he diagnosed bilateral medullary nephro calcinosis. He referred me to a nephrologist but the nephrologist told me that nephrocalcinosis doesn’t hurt. He refused to do anything about it such as further testing, such as a 24 hour urine test or another scan, to find out what was causing it and see if we could stop it’s progression and do something about the horrible pain I was experiencing along with the return of my IBS symptoms which were severely acute. Together, the pain in my kidneys and the every single day almost non-stop IBS episodes have caused me not to be able to work for the last 10 months.i cannot qualify for temp disability. I went back to the urologist and they did an ultrasound of my kidneys and of my neck to look at my parathyroid glands thinking perhaps I had hyperparathyroidism. This was at my request because my blood work for hyperparathyroidism has been borderline. The ultrasound came back showing no new stones, but also did not show the nephrocalcinosis. When I asked the doctor about that he told me that the type of nephrocalcinosis I have is not visible on ultrasound. Also the ultrasound of my neck did not show the parathyroid glands at all, they were not visible on sonogram. Could you review this and just give me your opinion on everything? I’m not really sure what to do next. Thanks so much!
Hi Tracy, You obviously have multiple stones in your kidneys or calcifications in kidney tissue – it is hard to tell from here – and a need to prevent more crystal build up and more stones. You do not mention stone analysis but the hardness suggests it is brushite. You need to know the stone composition. You also have pain in association with multiple small kidney calcium deposits – stones or tissue – and that is a fairly common complaint. The best treatment – surgical, for example, is still uncertain. What is certain is prevention of more crystals and stones. Take a look at this and try to see if these steps have really been followed. If so the answer to how to prevent should be reasonably clear. Let me know, Regards, Fred Coe
Thank you for your response. The stones were half calcium oxalate and half calcium phosphate. My urologist said that the tissue was calcifying. I drink at least three 32 oz glasses of water per day, sometimes fruit juice and I let myself have 2 cups of coffee per day, but always drink water afterwards. I have polyuria, urinating 20 or more times per day. I also have nocturia. I get up 4 to 5 times per night to urinate. I have to be careful with my electrolytes because I also have SVT which is currently controlled by 240mg of cardizem daily. My urologist thought about hyperparathyroidism because of all my symptoms. My serum calcium hovers around 9.9 to 10, but my vitamin D is always in the teens or lower, despite taking a supplement. I’m at a loss as to the next step.
I forgot to mention that the ultrasound showed thinning of the cortical walls bilaterally. My IBS is directly related to my kidney pain. In the ER they gave me pain meds and the IBS (obviously not constipation) stopped immediately as soon as my kidneys stopped hurting. The kidney pain is like back labor sometimes and hurts down both legs. It can be excruciating or just annoying. The constant IBS keeps me homebound, but three GI doctors have said there’s nothing they can do and insist the IBS is not related to the kidney issues.
Hi Tracy, Thinning of the renal cortices is important and raises the need for a diagnosis and treatment. Once again I urge an organized approach such as I offered in my link. IN the course of pursuing the needed information you and your physicians should find the right answer. Let me know. Regards, Fred Coe
Hi Tracy, half phosphate fits with what I would have expected – is any of the phosphate calcium monohydrogen phosphate – brushite?? I am suspicious of idiopathic hypercalciuria and I urge you follow the five steps in the article I linked to yesterday. Regards, Fred Coe
Thank you, Dr. Coe
Dr. Coe,
i just wanna know the meaning of differential function of right and left kidney, whats the meaning if right kidney functions at 12% and left kidney at 88% does this mean total kidney function is good/ normal?
thank you and will be waiting for your response.
Hi Antonette, It means that the function of your two kidneys was measured and each expressed as a percent of the total of the two. Your left kidney is contributing 88% of your total kidney function and the right kidney is contributing 12%. The total function is not stated in your question. Sometime or other the right kidney lost a majority of its function. In stone formers this is usually from obstruction with damage to the organ. Since one can live a full life with only one kidney you are quite safe but it means if your left kidney is ever obstructed you will be without much total kidney function until that obstruction is relieved. It also means that prevention of more stones is more important for you than for most other people. I am sure your physicians will want to pursue that with great vigor. Regards, Fred Coe
Hi Dr. Coe,
This is an immeasurable service that you and your team are offering to “stoners” and interested others. Thank you.
In 2014, at 60yrs, a known idiopathic hypertensive, I was diagnosed with bilateral medullary nephrocalcinosis following primary hyperparathyroidism (2 parathyroid adenomas). 24hr stone panel showed low phosphate, sodium, magnesium, calcium and citrate rates. I was not advised as to which type of stones I was liable to form, but now there are 0.5cm calculi in both renal sinuses. Serum creatinine progressively went from 0.8 in 2013 to 1.1, 1.45 in 2014. Now 2 years post parathyroidectomy (and concomitant total thyroidectomy for hyperplasia), creatinine seems stable at 1.0-1.1. No microalbuminuria. I developed severe osteoporosis secondary to the parathyroid adenomas and now have to take risendronate and calcium/Vit D supplements.
LDL rose from <100 to uncontrollable 140+ and I gained an intractable 20lbs in 6 months. BP is no longer well controlled on losartan/verapamil +maxide.
I wonder if I still have a propensity to nephrocalcinosis with hyperparathyroidism over.
And does taking calcium for osteoporosis increase my risk for particular calcium stones (female)?
Is there anything I can do to "dissolve" the calcinosis?
Thank you.
Hi Titi, I gather that you have had high blood pressure and also primary hyperparathyroidism which caused bilateral medullary calcifications. Your 24 hour urine results are confusing as urine phosphate and calcium will be high in that condition. I alsos gather that after surgical removal of two large glands you formed 0.5 cm calcifications in both kidneys in addition to the prior medullary nephrocalcinosis. This latter is not clear. How can the CT scan differentiate these stones from the prior calcifications? If you have formed more stones it is likely from residual hypercalciuria – very common after cure of PHPT; but urine studies would have shown the high urine calcium along with normal blood calcium. The bone disease of PHPT is known to heal spontaneously and bisphosphonates are not usually needed nor ideal, so perhaps your physicians are concerned about another disease. That your weight and blood pressure both went up is expected; more weight usually does that to blood pressure. The rising serum creatinine with PHPT suggests serum calcium was quite high – you do not mention it. So I am a bit uninformed about critical facts here and cannot do proper justice to your questions. Can you clarify things? Regards, Fred Coe
The message ran away before I could complete the story.
Sir, nephrocalcinosis was diagnosed by USS only following the PHPT. No CT scan was done.
I am just worried about the increasing abnormality in the kidneys. Is there something I need to do to reduce the negative progress and improve my GFR?
Will drinking alkaline water help to reduce the acidity of urine? In my case, with prior osteoporosis, how important is taking Ca supplements even though there is no longer the “hungry bone syndrome?
Thank you so much for your patience and for sharing from your wealth of knowledge.
Hi Titi, I understood the NC was diagnosed after PHPT but shortly after and no doubt formed from that disease. The rise in your serum creatinine appears to have occurred when you had PHPT and could well have been from the very high serum calcium at that time. As for alkaline water, I have no reason to think it helpful. As for bone renewal, it is likely and is slow. Calcium supplements – with meals! – or just a high calcium diet is important; your urine calcium seems so low – if I understand the units – there is no stone risk. The bone disease of PHPT is not osteoporosis as bone trabeculae are usually preserved and will regain mineral. Regards, Fred Coe
Thank you Dr. I am sorry for the confusing layout of information.
07/09/14 — Initial diagnosis of PHPT followed the finding of 12.6 Ca and intact PTH 348.
09/09/14 — Post op PTH was 20, and Ca 9.2mg/dl (ionized 1.26mmol)
09/25/2014 — Medullary nephrocalcinosis was diagnosed on USS. No stones.
Dexa score was -3.5 (severe osteoporosis).
10/01/14— BUN and Creatinine were 9 and 1.1 respectively
Postop 24hr urine panel (10/22/2014) showed low phos (0.2), magnesium (3.9) and citrate (240). Ca was just 54
Repeat stone formation panel (01/09/15) Ca 32.4, phos 0.2, mag 3.0, citrate 324, Na <30, oxalate 17.1
USS 07/10/15 medullary calcinosis plus 1.3×1.5cm left cyst, no stones
USS 11/03/16 medullary calcinosis plus 2.2×2.1 & 1.6×1.1 left cysts with 0.5cm intracystic and 0.6cm sinus calculi,
[Ca and PTH have remained normal postop. It has been difficult titrating my levothyroxine.]
Hi Titi, You did indeed have very marked PHPT and it was cured by surgery, although with 2 glands enlarged the possibility exists of recurrence. The medullary NC clearly occurred while you have PHPT. The urine panel after surgery looks odd; are these 4 hour excretions, and what are the units? The urine panel in 2015 also is not interpretable because the units may be millimole or mg; citrate is in mg/day, I think, magnesium in mg/day is not possibly 3. Can you clarify what these numbers are? The ultrasound studies are not very helpful in that stones are detected at about 65% efficiency vs. CT scan, so the changes may be real or technical. Regards, Fred Coe
Thank you for your calming review. I am glad to know that the bone disease of PHPT is not really osteoporosis and sort of reversible.
The 2014/2015 24hr urine results were as follows:
10/22/14 01/09/15 Range
Ca 54 32.4 50-250mg/day
Phos 0.2 0.2 0.4-1.3g/day
Uric 270 266 250-750mg/day
Na 72 <30 40-220mEq/day
Oxalate 18.9 17.1 8.0-48.0mg/day
Mg 3.9 3.0 6.0-10.0/day
Citrate 240 324 280-1240mg/spe
Crea 0.9 0.7 0.8-1.8g/day
K 57 64.9 25.0-125.0mEq/day
Should request a CT scan of the kidneys if possible? And a new 24hr urine panel?
Best regards
Titi
I tried to paste a table to show results from 2014/2015/Lab Range. I’m sorry it is messed up.
These are the 2015 figures alone with the range
Ca 32.4 50-250mg/day
Phos 0.2 0.4-1.3g/day
Uric 266 250-750mg/day
Na <30 40-220mEq/day
Oxal 17.1 8.0-48.0mg/day
Mg 3.0 6.0-10.0/day
Citrate 324 280-1240mg/spe
Crea 0.7 0.8-1.8g/day
K 64.9 25.0-125.0mEq/day
Hi Titi, Having the units, you indeed have very low calcium and phosphate in urine, low sodium, and are small – very little creatinine. Magnesium is in mmol/day, which is 24 mg/mmol giving 72 mg a normal to high value. I think you must eat only modest amounts of animal protein given the low uric acid, and lots of veggies. The low phosphate could be part of bone remineralization and poor absorption because of calcium supplements. The low urine calcium is almost certainly bone uptake. I would just let things go, eating high amounts of high calcium foods, and retest in 6 months or so. Stone risk – supersaturations – will be very low unless you forget about the needed 2.5 liters of urine flow/day. Regards, Fred Coe
Hi Titi, I responded in your other note. I would ask my physician about a CT to get a reliable baseline for stone counting. Regards, Fred Coe
Thank you Dr Coe. Iwill request a CT scan and a repeat urine panel since the last one was a year ago.
I wish you a most blessed 2017.
Titi
Dear Dr Coe
I would like to know if there is any way of getting rid of a Calcium mass in my right kidney? I also have a lot of small stones caught in the meat of the kidney. The kidney measures 13cms. My other kidney is not affected and measures 9 cams. After having my first child I was in Intensive care after passing blood an vomiting. I was diagnosed with a Medallary Sponge Kidney at the age of 22 in 1972.
I do felel intermittent pain in my kidney that passes.
I would like to know if there is anyway to dissolve the Calcium in my kidney?
I have recently been diagnosed with Osteoporosis and I am now taking a natural supplement from BoCeuricals called AdvaCal Forte with K2 and D3 it does contain Calcium etc
I have always led a healthy outdoor life and have a mainly organic vegetarian diet.
I look forward to hearing from you
Hi Kristin, Without seeing the actual images I cannot say anything useful about the calcifications. You may indeed have MSK involving one kidney. If you do not have pain, bleeding, infection or obstruction, surgery would be a poor option. Your bone disease with kidney stones maybe part of idiopathic hypercalciuria, and that would require careful management. But most of all, I sense a lack of purposful evaluation and prevention. Take a look at this article and see if it applies to you. Be sure you have been tested properly and know what is wrong, then get it treated. Remedies like advacal are essentially useless without clear reason to take them. They can cause disease if not used in the proper setting. Regards, Fred Coe
Hi I was diagnosed at 19 with msk, dRta, medullary nephrocalcinosis, metabolic acidosis and hypokalemia. I form stones due to extreme hypocitraturia and recently have been put on sodium bicarbonate due to excess carbon dioxide. I take massive amounts of potassium citrate daily as well because I become very hypokalemic if not. I pass sandy stones very frequently and only recently had an emergent blockage that required stent placement and lithotripsy. I suffer with chronic utis as well and my latest gfr was 39 and the highest I’ve seen it get was 42. Everything I read says msk is usually a mild disease with a good prognosis so why am I at 26, living with less than half of my kidney function? On top of all this, I am suspected to have systemic sclerosis aka scleroderma, or possibly mixed connective tissue disease. Do you know if there is an association? And what do you think my prognosis might be? Also does it matter that my mom and her dad were born with unilateral renal agenesis? There has to be a connection with the kidney diseases right?
Hi Elizabeth, I believe you were put on sodium bicarbonate because of low serum bicarbonate, but why the sodium I am not yet sure. Perhaps it is that you lose sodium in your urine and your blood pressure falls. The sandy stones are, I presume, calcium phosphate or carbonate because of high urine pH. I do not at all believe this is MSK, it is renal tubular acidosis and rather severe sounding. There are deep associations between some collagen vascular diseases and RTA, and you may well have one. As for the unilateral agenesis I am more sceptical. Your overall concern about the stones and reduced kidney function is justified and I would ask my physicians if they can provide a referral to a specialized center that is geographically reasonable for you. If that is too difficult, I would offer to review your records as a free service to them and you because this is a very complex problem and perhaps I could be helpful. Regards, Fred Coe
For Elizabeth I would like to investigate possibility of Sjögrens Syndrome which may need specific treatment besides stone prevention and other metabolic interventions. I agree that sodium in the regimen may be replaced, possibly with potassium bicarbonate. Best regards. Aydin Olgun
Hi Aydin, Thank you for adding your thoughtful comment – I presume you are a physician. I think she has renal tubular acidosis and Sjogren syndrome is certainly a well known cause. Warm regards, Fred
I wish i had a doctor, like yourself, that could explain to me my diagnoses of MSK and Nephrocalcinosis. I was told 4 years ago that i had these but no real exsplaination of what it is or what will be my future. All i really know is from articals and sites like yours and that i live in almost some level of constant flank pain and nausea. I get recurring kidney infections that last months due to wrong antibiotics and/or not a long enough course to remove entire infection. 8 times out of 10, when pain and nausea are at their worst and i do go to the ER, im told that because they cannot see an obstruction thru ct w/o contrast that the pain im feeling and following nausea is in my head. That without obstructions there should be no pain. Since im normally, upto the last few years at least, was active person, involed with my childrens school and a boy scout leader and now have to struggle to get out of bed most days, id like to hear your opinion before i book myself a rubber room.
Tired of being branded a drug seeker without history of drug use.
Lost in southern indiana, kim
Hi Kim, I am very sorry to hear about all this. Perhaps you might benefit from evaluation and treatment in a center devoted to stone management, Given you live in Indiana, you might want to consult with Dr James Lingeman at Indiana University, Indianapolis. Small stones with pain are well known to him, and he may well be able to help. Regards, Fred Coe
I am a 66 year old woman who was put on Telmisartan (80 MG) and Hydrochlorothiazide (12.5 MG) for high blood pressure in February 2016. Since I have been placed on these drugs, I have had kidney stones 3 times and never before taking these drugs. I had to have surgery to blast very large kidney stones in July 2016, had kidney stone again in December 2016 and now in March 2017. What do you recommend I take for high blood pressure that would not cause kidney stones. I now believe it is the Telmisartan causing this problem. I have no other side effects from this drug and it has stabilized my blood pressure but having kidney stones 3 times since starting this drug a little over a year is not good. Can you explain why this is happening and what I can do about it? Thank you!
Greetings Dr. Coe
I am a female, 37 y.o. 5 ft.tall, 92 lbs. Asian. With solitary kidney with medullary nephrocalcinos (not passing stones)
I just wanna clarify my recent blood works and ask for my prognosis
Normal urinalysis, no protein no uti, no rbcs/wbcs
Serum Creatinine june 2016: 67
Serum creatinine sept 2016: 75
Serum creatinine december 2016: 84
Serum creatinine march 2017: 66
My creatinine as well as egfr for the last 2 yrs are fine according to my nephrologist. Sept 2014: 62 as the lowest creatinine and dec 2016: 85 which is the highest.
Pls let me know about my chances of avoiding dialysis, i mean with these level can i have a normal full life at least until age 80?
Thanks
Hi Antonette, I assume the creatinine is in units of micromoles/liter, and therefore the range translates into 0.7 to 0.96 mg% which is common in the US. These values are not at all alarming. MSK has little known tendency to progress to kidney failure absent surgical accidents. My only suggestion is to be very careful about any surgery and if you do ever need stone surgery try to have it done by physicians who are very adept and experienced. Likewise, if you do pass a stone be vigilant about obstruction – always follow up with your physician who can be certain about such matters. Regards, Fred Coe
Dear Dr Coe, I have a question for myself. I would be very interested in your advice.
I am 58 Years old, fit healthy,male, non smoker, non drinker, good blood pressure, BMI 23.6. Originally from the Netherlands, now working in New Zealand as a GP. I had 2x a kidney stone attack 20+ years ago. I went to the Urologist recently for review prostate and had a CT kidneys done:
My CT kidneys. Technique helically acquired axial images of the abdomen and the pelvis with sagittal and coronal reformats. IV contrast (100 ml Omnipaque 350 IV)
Findings: There are multiple calculi in both kidneys. In the inter polar region of the L kidney there is a large calculus measuring 15×11 mm as well as several smaller calculi in the region and one in the lower pole.
In the Right kidney there are also at least 5 renal calculi, the largest in the upper pole measuring 4×2 mm.
Both kidneys demonstrate multiple cortical and parapelvic cysts, some demonstrating faint wall calcification.
There is a pre contrast hyper dense cyst arising from the upper pole of the left kidney. No enhancing solid renal lesion. No hydronephrosis. no ureteric or bladder calculi. Rest all N
General lab: Lab: blood results Sodium 141 mmol/l (135-145), Potassium 4.0 mmol/l (3.5-5.2), Chloride 101 Mmol/l (95-110)
Urea 4.5 mmol/l (3.2-7.7), Creatinine 79 umol/l (60-105), eGFR>90 mL/min, Urate 0.35 mmol/l (0.23-0.45) Ca 2.4 mmol/l (2.2-2.6) Phosphate 1.0 mmol/l (0.8-1.5) albumin 43 g/l (32-48)
I had my urine tested before and after starting a Low Oxalate diet:
Normal Oxalate full diet
Volume 4110 ml /24 hrs secretion this period normal /24 hrs
Oxalate 99/umol/l 407 umol H 0-310 ELEVATED
oxalate/crea ratio 35 N 0.15
Concentration secretion this period Normal/24 hrs
Ca 2.0 mmol/l 8.3H 2.5-7.5 ELEVATED
creatinine 3.0 mmol/l 12.0 mmol/d 9.0-18.0
Na 16 64 N 100-250
K 22 89 N 35-100
Urate 0.9 3.6 N 1.5-4.5
After a low oxalate, low sodium and Ca “max 1000mg through the day diet”
24 hrs Volume 3.51 ltr
Oxalates 0.28mmol/d (0.06-0.49) NORMAL
Citrate 2.5
citrate/creatinine ratio 0.4 mmol/l
creatinine 4.2
24 hrs creatinine 14.7/d (7.0-24)
24 hrs Volume 3.82ltr
Ca 9.9H STILL ELEVATED
Urine Ca/Creat ratio 0.83 (H) (0.00-0.60)
Na 54 N
K 99 N
creatinine 3.1 11.8 N (7.0-24)
Urate 3.4 N
So following a low oxalate diet lowered the oxalate levels in my urine but my Ca is still to high.
What would you advise? Stay on the low Oxalate diet even though my last kidney stone attack was more than 20 years ago.
But I have been making stones during my last 20 years (even when not experiencing attacks) and I have partly medullary sponge kidneys.
Start on a thiazide to reduce my calcium in the urine? what dose?
Kind Regards Nga Mihi (with respect as the Maori say)
Dr van Rens
Hi Doctor, Your urine oxalate was a bit high, urine calcium more so. Diet – less oxalate and I gather 1000 mg calcium lowered the oxalate but the calcium remains high. I suspect you have idiopathic hypercalciuria, and even so low a sodium intake of 54 mEq/day does not lower it fully. I think this article is my best on the low sodium high diet calcium as a treatment. It has links to a deeper article on the science supporting this kind of diet. You obviously formed stones but with your new data, are your supersaturations now lower than they were? They are key as guides to overall stone risk. If not available, and given the numbers of stones that appear to have formed, you might add a low dose of chlorthalidone – 12.5 mg/day or the equivalent of Indapamide 1.25 mg/day to the low sodium high calcium diet. Regards, Fred
Hi, my name is Kayla. I’m 23 and was told I have nephrocalcinosis when I was 16. They ruled out everything that would cause nephrocalcinosis so they never found an underlying cause. Although a year ago I found out I have PCOS and insulin resistance so I take metformin for it. I see a nephrologist every year and he doesn’t really give me answers to my pain. He just assumes I’ve passed many stones which I don’t believe I have. I almost go daily with waves of pain in my back and constant flank pain. Is there any suggestion of treatment I could do?
Hi Kayla, Given multiple calcifications I would be sure about the immediate cause – this means proper blood and 24 hour urine testing. You may have hypercalciuria. Possibly you have medullary sponge kidney. Early insulin resistance could point to possible genetic issues. Do the above testing first and be sure what is causing your crystallizations. Regards, Fred Coe
Hi Dr. Coe;
About 3 weeks ago I went to urgent care with pain in my left side and abdomen. After a CT scan of my abdomen and pelvic area, urine with blood (moderate), the doctor said, I had a small stone in my Uterer. He sent me home with pain meds and said, it would probably pass in 4-5 days. No such luck. I just recently visited a urologist who confused me even more. She said, it may be a calcification and not a stone and I need to re-do the CT scan. What is the difference? And my pain and frequent urination is a symptom of a stone right? Very confused and worried. Linda.
Hi Linda, I am afraid this is so bound up with the images themselves I have little to offer. But, frequent urination suggests the stone is at the junction of the ureter and bladder. Your urologist is right to take another look. If it is there it will pass or she can get rid of it for you. In all this, be sure about prevention. I like this article as a starter for people. Regards, Fred Coe
Thank you for getting back to me so quickly! I have been worried all weekend that is was something more serious, when she said, calcification. I have more pain then usual today and im just a worry wart. I’ll read the suggested article, thanks again. Linda
One last question. If it’s a calcification and not a stone what is treatment for it? Thank you
It would be outside the urinary tract and of no interest. Regards, Fred Coe
Dr. Coe,
I have been dealing with calcium oxalate stones in my right kidney since I was 12 years old. I have also had 4 lithotrypsies to break up the stones. Even on potassium citrate and Hydrochlorothyazide and drinking lots of water I seem to keep making new stones. The kidney that I am having trouble with actually has two ureters coming off of it that merge into one. It’s a hereditary thing as my father’s ureters merged into one half-way from the kidneys to the bladder. I have had a theory that because my kidney has the two ureters not enough pressure is being built up inside the kidney to help push out crystals that have formed which eventually turn into stones sitting at the bottom of the kidney. Does that make any sense at all?
Hi Mark, You do not mention your 24 hour urine tests, but I imagine they are abnormal and prevention has not been complete. It is true that urinary abnormalities can promote stones but calcium phosphate would be the more common type of crystal. If you wish to put up the 24 hour labs I could take a look. Regards, Fred Coe
I just had found out I had kidney stones (which I had removed) but still have the calcium on my kidneys. did the study after & they drew blood. found that they were Oxilatine type stones. still not feeling well nasau & pain in back, joints. not sure why they cant help do anything. is there anyone I can take the results too & get another opinion. my current Urologist said we will try diet which I have no idea what not to eat. then if we get another stone we will go from there. I don’t agree with this at all. I say get this off my kidneys before further damage is done & help me feel better. Anyone have ideas or help? thanks
Hi Dee, I gather you have had calcium oxalate stones and still have either more stones in the kidneys or calcium deposits in the kidneys. Here is perhaps an article to help you sort things out. As for suggested additional physicians, I do not know where you live, so I cannot be helpful. Regards, Fred Coe
Please help me understand why my eGFR is going down and what can I do to fix it. I am a 72 year old female, very active, no pain, non smoker, non Alcohol drinker, non drug user. In August 2009 eGFR 45ml, BUN 20mg, Serum Creatinine 1.4, Glucose 110, Calcium 9.8mg.
July 2011 eGFR 34ml, BUN 30.4mg, Ser Creatinine 1.7mg, Glucose 96mg, Serum Calcium 10.6mg, PTH Intact 85pg, Alk Phos 19.9ug, Vit D 38ng. 24 hour URINE Calcium 36.6, urine volume 3325 ml, urine sodium 103 mmol/vol, urine creatinine 1.9 gm. Beta cross laps 583.
Random urine creatinine 56mg, random urine calcium 1.1 mg, random urine sodium 31mmol/L, urine microalbumin 4.30, Albumin/Creatinine ratio 58.9. I’m taking Aspirin 81 mg and Telmisartan 80 mg tab. DEXA shows mild bone loss left hip T-1.5, US Kidney Impression – Increased cortical echogenicity likely related to medical renal disease. No hydronephrosis, contour deforming mass or renal calculi. The bladder appears unremarkable. I have seen an Endocrinologist who suggested consuming 1200 mg calcium not supplements, 2000mg vitamin D and recommended Alendronate to limit bone loss. I have also seen a Nephrologist who recommended Atorstatin 20mg daily for chronic kidney disease. He stated my calcium/creatinine clearance ratio 0.0046 may indicate a benign inherited variant, (FHH). I have not started taking these two new meds yet. I am more concerned about why my kidney function is going down. All other tests results (CBC, Lipid Panel and Comprehensive Metabolic Panel) are normal. Please help. Thank you and know that your opinion is greatly appreciated. Vee
Hi Vee, This is a very complicated problem. You have a significant and progressive kidney disease with scant urine protein and a high blood calcium and PTH level. The low urine calcium is hard to assess in the presence of so much kidney function loss. I would be remiss to say anything from this distance. If your physicians and you would like a serious opinion from me and my colleagues we would need to see all of your relevant medical information and try to offer something useful. I certainly recognize this is a serious matter in an otherwise well person, and a bit unclear as to cause and possible amelioration. Regards, Fred Coe
Hi, my name is Chelsea . I am 28 , I was diagnosed with medullary sponge kidney with major nephrocalcinosis about a year ago. I have had kidney/ flank pain on both sides for over 5years with out finding a cause. I have never had passed a kidney stone. After all testing (X-rays , ct , blood , 24 hr urine) I was informed I had two major contributors- very low citrate and very high calcium in the urine. I have been able to correct the citrate by adding lemon juice to water but can not find a natural way to fix the high calcium. I am very sensitive to all of the medications they have tried (old school blood pressure meds) and become quite ill when on them. My urine output is also kept quite high. Do you have any suggestions to help lower my urine calcium ? Thanks
Hi Chelsea, As the article points out MSK cannot be reliably diagnosed except during stone surgery or by special CT scanning with contrast injection. SO you may just have multiple calcifications from stones. The high urine calcium is part of idiopathic hypercalciuria, I suspect, the low citrate is not obvious from what you have told me. Here is my best article on control of urine calcium. It is all about salt. Here is the ideal kidney stone diet – based on what trial data we have. You have kidney stones, even though none have passed, and they may well be calcium phosphate. Given the stone mass and pain, surgical approaches are a matter of present debate. Please understand that all of these remarks are in ignorance of your complete medical situation, so the best approach is to share them with your physicians who may agree or have reasons to not agree with me. Regards, Fred Coe
Thank you for your timely reply. I will look into the articles! I have had a ct with contrast to confirm the msk. I don’t know if this makes the mentioned articles contradictory? It’s very hard to find legitimate kidney stone / msk information and most seems under/ untested , especially for msk. I really appreciate the work you’re doing and the informative article
Hi Chelsea, If you have had contrast CT and is showed MSK you have msk. take a look at the article on it. We were the only group to actually do the surgical anatomy. Treatment is complicated in that stones may form because of simple stasis of urine in the cysts. Minimal supersaturations are the best I can think of. With a lot of pain some surgeons are trying to empty out the cysts. SWL is not a good idea. Take a look. Regards, Fred Coe
Hi I am a very scared mother of five. I was told I have nephrocalinosis Msk. I have surgery to remove my stones every two months and was just told I’m a very rare case and basically there is nothing to stop my kidneys from turning into stones. Is there any truth to that?
Hi Amber, most nephrocalcinosis is not MSK, but if it is or not prevention of more deposits is your goal. Surgery for stones that reform every two months suggests an active ongoing cause that needs to be stopped. Here is a good starting place. See if it helps orient you. Ask your physician/. Regards, Fred Coe
Hi my boyfriend is 53 yrs old and has suffered since he was a small child with his kiddneys and to much calcium in his blood. Hes not supposed to have milk, chocolate and if he eats a few gallons of ice-cream in a week he says it puts him in the hospital. so on and so I’v started him on magnesium wich turns out his mother did when he was younger and it helped him then. Hes says the stones shred his kidneys badly he had a stent in one for a while and he has kidney pain when he consumes too much calcium and his kidney is tender to the touch. Im giving him bee pollen, magnesium oxide, multivitamin and mineral with low calcium 10% daily value and b-complex. he works “HARD MANUAL LABOR” none stop from dusk till dawn in the sun Im pretty sure the magnesium is stopping his migraines and sever muscle cramps But am I POISONING HIM WITH THE BEE POLLEN! Bee Pollen is the top super food and nutritional supplement anyone could eat helps to flush all toxins out of your body but the toxins flood the blood and if your blood doesn’t flush the toxins out you can get very sick. help I read your whole article and understand it quit well. all he remembers is the doc He had had as a child said his body doesn’t flush calcium. So i wanna do the magnesium for him it seems to help and the bee pollen. whats your thoughts on that. pretty sure he has no hypothyroidism he is a very hyper active person though.
Hi Breezy, If you really mean his blood calcium is above normal, low calcium diet is not at all right. Perhaps you mean too much calcium in his urine, and then low calcium diet is not at all right. It is never right. I think his care is confused, and here is an article to help. As for bee pollen, I have no opinion, but it will not be sufficient if his blood calcium is high. He needs his physicians to determine what to do. Regards, Fred Coe
My name is Annette, I am 60 years young. I have had a history of Hyperparathyroid, and had one parrathyroid removed. Today I went to the doctor where he found 40 stones, most in the lining, have had 4 stone removals since 2006, it appears to be Nephrocalcinasis and Neprolithisis. before the parathyroid my urine calicum was 528, Vitamin D is 26, doctors kept trying to push the D, it doesn’t help. I have hypercalcemia and last urine count was 150, do your believe this has something to do with not taking out enough parathyroids that so many stones are happening?
Hi Annette, I gather you had surgery for primary hyperparathyroidism and still have a high blood calcium level. This would suggest that multiple glands were involved and they are maintaining hyperparathyroidism. If so, you will need another surgery. Alternatively, perhaps the gland removed was not the one causing your problem. I would expect your physicians would want to check several fasting serums for calcium and PTH in the absence of any medications that might influence either measurements. If your blood calcium is high and your PTH is not suppressed, you likely have PHPT still. Your physicians need to do this for you, if they believe it is worthwhile. Regards, Fred Coe
Hi Mr. Coe
Thank you for your feedback, I will take care of that with the doctor, its hard for doctors
to understand as Normal is what I hear alot of. I have heard from 4 kidney doctors its my
parathyroid issue and now yourself. I am grateful for your help. Dr. Norm in Florida does
this Primary Parathyroid teaching and operations will contact him in the morning, as N.C.
doesn’t get it . Here is a site I researched last night and it makes sense, your articles and
site has helped me so much to have hope. Blessing to you and yours. Will check in when
this operation is done. http://www.parathyroid.com/secondary-hyperparathyroidism.htm
Hi Annette, No; secondary HPT does not produce high serum calcium and does not ever require surgery except in end stage kidney disease. It is high PTH levels with normal or low serum calcium, and is a response to low calcium diet, vitamin D deficiency, or reduced kidney function. Nothing to do with you. Regards, Fred Coe
Hi Annette, No; secondary HPT does not produce high serum calcium and does not ever require surgery except in end stage kidney disease. It is high PTH levels with normal or low serum calcium, and is a response to low calcium diet, vitamin D deficiency, or reduced kidney function. Nothing to do with you. Regards, Fred Coe
Dr. Michael Stang, Raleigh; Dr. Julie Sosa, Durham; Dr. Kristen Wagner, to name only a few from NC, are all experienced parathyroid surgeons.
I would mention also that on the AAES Patient Education website is a downloadable interactive surgical consultation worksheet, in either Word format or a pdf, that is of tremendous help to many PHPTer’s in knowing what questions to ask, and certainly also in the context of the re-operative environment.
UCLA’s website also has a helpful chart listing the decreased incidence of stone formation, post-op PTx, over the course of several years.
Good health to you on your journey.
Hi Dr. Coe, and thank you for your information.
As a patient, formerly with pHPT, I’ve volunteered for a number of years in the capacity of parathyroid patient advocate and navigator.
Thanks are offered for physicians such as yourself who continue to educate, and certainly those surgeons who are members of the American Association of Endocrine Surgeons who are making great inroads to educating the public worldwide regarding the 3rd most common endocrine disorder, Primary Hyperparathyroidism.
It would be greatly appreciated if you will assist in a navigational role on behalf of those on a journey who seek unbiased information regarding PHPT, while web surfing, to offer a directional compass pointing toward the AAES Patient Education website with it’s accompanying experienced-endocrine-surgeon locator. Much appreciated and thank you for the forum you have offered here.
Regards
@#CheckYourCalcium & PTH
http://endocrinesurgery.org/
Hi Angelia, Thank you for mentioning the society. I will indeed put a link to the endocrine surgery site on both my primary hyperparathyroidism articles. I should have done so before, as it is a reputable professional society of experienced and expert surgeons. I have added this to my clinical article on PHPT: “Parathyroid surgery is a highly technical procedure, and not all neck surgeons choose to perform it. A valuable resource for university based endocrine surgeons is this site listing surgeons who belong to the American Association of Endocrine Surgeons. This society is noncommercial and I feel free to recommend it as a resource from this university site.” Warm regards, Fred
Dr. Coe,
How common is it for someone with nephrocalcinosis (and no prior RTA) to develop an RTA secondary to the nephrocalcinosis?
Hi Joyce, I have no evidence of anyone developing true RTA because of papillary calcium deposits. I believe it could happen. There is ‘incomplete’ RTA wherein urine is too alkaline and when challenged with an acid load kidneys cannot lower urine pH to the usual normal nadir. The distinction is about true RTA – blood is acid, urine alkaline. If you have acid blood I suspect you had RTA or developed it from some cause – there are many. Regards, Fred Coe
Thank you, Dr. Coe. I do not have any blood abnormalities, only the alkaline urine, low citrate, and nephrocalcinosis. The doctor at the U of Michigan I saw did mention that I could have some sort of incomplete acidifying abnormality.
I have noticed this last month that my blood pressure is running high (for me), at about 127/80. My blood pressure has always been very low, and was almost never above 110/70 tops. Could this be related to the nephrocalcinosis? Thank you.
Hi Joyce, higher blood pressure is well established as a problem of stone formers. Of course 127 is pretty benign, but home BP measurements are not unreasonable. If pressure does increase, remember the kidney stone diet is an ideal first line treatment – low sodium, high potassium, moderate protein, low refined sugar etc. Regards, Fred Coe
Dr. Coe,
You’re truly the only reason I’m still sane thru all of this. I’ve written before, but had another question. Most all websites I read act as if nephrocalcinosis is a sure predictor of renal failure. I’m only 30, healthy, and that freaks me out!
I developed nephrocalcinosis quote quickly (over 6 months) of a very high protein diet. I have very low vitamin d and wasn’t taking any supplements during this time, which seems to have contributed to the vast amount of stones formed during that time.
The docs started me on Potassium Citrate ( I was shown to have made a calcium phosphate stone after litho). I had been urinating brown flakes and that brought me to see the doctor and discover the calcinosis. I’m also an ultrasound tech and had seen it developing, not knowing my high protein diet was contributing.
I since have had a successful pregnancy whilst taking Potassium Citrate, and didn’t have any brown urine sediment during the pregnancy, but now 7 weeks later, I have it again.
When I saw the doc, he didn’t seem concerned with sediment and said probably related to the stones in some way.
Is this something I may have my whole life? I also sometimes have aching in my kidneys. I do have a few measurable calculi the kidneys themselves as well.
Should I be worried these flakes in my urine (sometimes white, sometimes brown) are tissues being damaged?
Is all that I can do to help just the increased water, reduced sodium, and potassium Citrate?
I just want to be done with this and am concerned this could be a lifelong ailment, which at my young age is overwhelming.
Thank you so much for your help!
Joyce
I should add – I had a 24 h urine that showed low Citrate (334), high ph (6.8), and the rest was normal (no high enough supersaturations for concern, no hypercalciuria). My blood was normal.
The Potassium Citrate brought my Citrate up to 436, but my ph is now 7.3, but the supersaturations are well below even close to a concern.
I’m your opinion, is this Citrate increase enough to help my situation?
I have a feeling (since my nephrocalcinosis all developed during a period of EXTREME high protein – mostly from dairy) that my problem may resolve with just adequate water intake alone and don’t want to make things worse by raising my ph.
What is your opinion?
Hi Joyce, sorry I missed this for my first note. Yes, protein loading can raise urine calcium a lot and promote stones – I believe. Possibly you became hypercalciuric as well from the calcium load in the dairy products, and possibly you are not hypercalciuric now because you are eating a low calcium diet – not a reasonable long term approach. So a lot depends upon exactly what happened and what is happening now. As for just water, I am very skeptical, and given NC I would be more likely to push for as definitive a prevention plan as you would accept. Regards, Fred Coe
Hi Joyce, Of course NC does not invariably result in kidney failure – quite the opposite. But your treatment is surely not complete. The flakes need to be analysed – perhaps they are crystal aggregates. You need the usual complete evaluation and prevention measures, and should do well. Here is a good plan. Regards, Fred Coe
Thank you!
I’m so very upset with myself for hiring an expensive trainer, who had me eating strict protein intake of between 125-150 g a day. At the time I was 128 lbs. I did this for 8 months, during which the nephrocalcinosis developed.
I hope I can fix the problem and wish I could go back, but am thankful for your help nonetheless.
Dr Coe,
What do you say for nephrocalcinosis worsening (on ultrasound) while blood work, and 24 hour urine are normal?
I have seen docs in Lansing, MI as well as at University of Michigan. They seem puzzled.
I would come see you if you think you could help!
To further clarify, I guess I’m wondering if there is any condition that does not involve hypercalciuria or high supersaturations, that also leads to nephrocalcinosis.
Hi Joyce, there exist some conditions, and sometimes there are clues buried here and there as to what might have happened yet not obvious, as in the purloined letter. Over time, I never cease to wonder at them. Regards, Fred Coe
Hi Joyce, if the physicians at U Michigan seem puzzled you might possibly benefit from coming to U Chicago in that I have done some complex cases. Ask your physicians if they think I could be useful. Regards, Fred Coe
Hi Dr Coe,
I am a 24years old male who recently developed abdominal pain in the left lumbar area and loin. I had an abdominal scan done which showed widespread, bright, echogenic deposits on the wall of the left renal pelvis. I also had urinalysis done with trace amounts of protein seen.
A diagnosis of left nephrocalcinosis was made.
I was asked to be on dietary salt restriction and fluid hydration. I wanted to get your opinion on this and if it will give a complete resolution of the calcium deposits.
Thanks.
Hi Molokwu, The cause of the calcifications needs to be found. Here is a good starting place. Being in one kidney this could be medullary sponge kidney or any other kind of stone disease. Treatment without understanding of cause is usually futile. Regards, Fred Coe
Hi again, Dr. Coe!
I have written before regarding my nephrocalcinosis, after a high protein diet. They had me on Potassium Citrate for a year (and I also had a pregnancy during that time), but recently the doctor I saw at U of Michigan, Dr Adil Jadoon, took me off of the Potassium Citrate, as based on my urine results (very high pH, but extremely low supersaturations across the board), he didn’t think I needed it.
I recently had my first blood work since stopping it 3 months ago. A few things are concerning to me. First of all, my blood Potassium is 4.9, which is higher than it’s ever been. Secondly, my BUN , while still within the reference range, is 19, also the highest it has ever been (previous numbers from 2010 until now are 7, 11, 8, 14, 12, 7, 12, 19). My creatinine is normal at 0.74. The only other thing of concern is maybe Alkaline Phosphatase, at 102, mildly high.
Things to note: I am breastfeeding. I typically take in about a gallon of water a day, but the blood work was done when I had not yet drank water for the day and it was done around 11 am. I am on a low salt diet.
Also to note- after my most recent urine test showed very low supersaturations if anything stone-forming, and a high pH, my original urologist suggested increasing potassium citrate because the oxalate was slightly high at 49. For a second opinion, I went back to u of M neprhology, where Dr. Jadoon completely disagreed and thought I should not be on it at all, as my supersaturations were low and urine pH was 7.3.
My concerns are as follows:
I am only 31 years old, and in good health. I’ve always exercised, eaten quite healthy, and maintained a normal weight, etc. I am worried that the doctors are not putting much effort into my care, as my situation doesn’t seem “that bad”. I want to be confident in my health care plan and know that I am preventing further kidney damage from developing.
As a recap, my history is that of a few isolated kidney stones during pregnancies. I drank very little water. Then an extreme high protein diet for 9 months or so led to rapid nephrocalcinosis bilaterally, which they assume was a result of the protein. I have no fam history of stones.
Let me know if you need any more info. I highly respect you and your knowledge on this disease, and appreciate your help so much!
Hi Joyce, while breast feeding, 24 your testing can be misleading and therefore futile. Urine calcium falls because of the demands for milk calcium, so there is no sense in doing the test. High fluids are a good thing, and right now you seem to have little risk. Just high protein to convert a few scattered stones into nephrocalcinosis – how unusual! Perhaps. I would finish breast feeding, and then do another 24 hour urine; obviously with a high urine pH and lots of fluid the potassium citrate cannot do much for you and could be stopped – of course I am saying this based only a few fragments of your total situation. Regards, Fred Coe
Thank you so much. No one mentioned to me the effect of breastfeeding on 24 h tribe calcium. That is good to know. I will see my doctor after I finish breastfeeding. Thanks so much for your input and knowledge.
Hi Dr. Coe,
I am 42 years old and have recently been diagnosed with nephrocalcinosis on both kidneys using a CT scan with contrast. I had a surgery for a kidney stone when I was 22 but never had any stone attacks since until recently. A 24 hour urine test by Lithiolink showed the following:
Low urine volume, Hypercalciuria, borderline hypocytraturia, moderate CaOx stone risk, moderate CaP stone risk.
In addition, my blood pressure has increased slightly and I am having a pain on my left side. I recently had a hysterectomy and my physician did not “see” anything unusual causing the pain on my left side . I have since had two more scans without contrast, finding nothing but diverticulosis. I am assuming the pain might be the kidney condition??? Also, my vision was changed since my surgery, but no doctor seems to think it was related to the surgery. Could it be kidney related? My doctor wants me to start hydrochlorothiazide but I have no idea what to eat and how to manage so many different things. I am also sensitive to dairy and gluten and try to avoid it. What should I eat and should I take this medication?
Hi Betsy, Prevention of more stones and kidney calcifications is a complete program. Take a look at my favorite article on how to proceed. The kidney stone diet is critical. Meds are uses when the diet proves inadequate. Dairy products are various and you will not be sensitive to them all – supplements are a last resort, I rarely need to use them. As for your blood pressure, here is what I have to say about it. The kidney stone diet is ideal for lowering blood pressure. Regards, Fred Coe
Four years ago I had an eGFR of 12 and a biopsy showing calcium oxalate nephrocalcinosis with focal acute tubular injury (consistent with an oxalate cast nephropathy); arterioschlerosis, focal & moderate. My diagnosis was hyperoxaluria. Since then, I have progressed to Stage III. I avoid all high oxalate foods and most moderate ones as well. I eat about 4 oz. of fish or fowl per day, have a diary product with every meal, drink 2.5L of water daily, avoid processed foods, sugar, caffeine, and salt (other than what naturally occurs in the meat and dairy that I eat). I take 10 meq of potassium citrate, 100 mg B6, and 2000 IU D3 (for osteopenia). I’ve been tested for the hereditary forms of hyperoxaluria, and do not have these. I would love to know more about why I became ill and how to prevent its recurrence. I continue to have small stones and periodic flank pain, but I’ve never knowingly passed a stone. My 24 hr. citrate is 223 mg/24 hour for a volume of 3650 ML. Potassium is 95 mmol (17-77). PH is 6.4 (4.5-8.0). Creatinine is very good at 1095 mg/24 h. I am undersaturated for all crystals except hydroxyapatite, and I’m below the mean for that. So, I think I should feel really good about this. Right? Do I need to be concerned with the hypocitraturia? What about low blood sodium, 127 meq/L, and chloride, 95 meq/L? Low RBC, 3.62 million/uL; hematocrit, 32.8%; and hemoglobin, 11.2 G/DL (even though I take an iron daily); a recent unexplained loss of consciousness accompanied by dehydration (despite drinking 2.5L daily); pre diabetes; elevated PTH 81 PG/ML, and hypothyroidism. I am willing to do the work of leading a healthy life. I’m just confused as to what I should do next, or if I need to do anything. I don’t have loose bowels leading to the hypocitraturia. I don’t have a high protein diet (unless I need to further reduce my protein to account for the milk products I consume). My serum CO2 is normal and my doctor says I have secondary, not primary, hyperparathyroidism, and he has not suggested I do anything about that. I’m not taking any of the listed medications that can cause hypocitraturia. Finally, thank you for the incredible gift of your mind on these pages. I cannot imagine all the people–patients and professionalx–you have helped. What a wonderful gift to the world!
Hi Christine, You do not mention your urine oxalate. Was it ever high?? Oxalate crystals in a renal biopsy arise in hyperoxaluric people, so you must have had a high urine oxalate excretion. What was the level, what is it now. The other findings are of no interest by comparison. The low serum sodium may be from high water intake with advanced kidney disease, the other findings seem commonplace for kidney disease as well. Please let me know. Regards, Fred Coe
I have had no less than 26 stones and all unpassable. I’ve had lithotripsy half a dozen times and my urethra is wore out from stents. I recently started urinating blood and went to the ER and they told me my kidneys are turning to stone. That’s all. I have a cup of stones I’ve passed and most look like elbow macaroni. I just want to know if im going to die.
Hi Jonie, You have a lot of stones, and I hear nothing about prevention. Here is a good place to start – it is all about the steps you need to take to reduce risk of new stones. Regards, Fred Coe
Hi I’m 41 I’ve had 2 surgeries to remove kidney stones but they still are there.i need a second option.I’m very health. I would like You to review my medical records online. The hospital is Osnher Hospital in Louisiana. If possible can you email me Personnal so I can give you my access password & etc. please help me. I can also give you my cell number when you email me
Hi Samantha, Firstly, I am sorry to be so late – I missed this question in September. As for your request, I would be practicing medicine improperly if I did what you ask. Telemedicine is a new and emerging modality and right now my institution does not allow it within the US. The reason is each state licenses separately and I cannot practice in your state. If your physicians want me to review your records and advise them, I could do it as a technical issue about numbers but not as a paid medical consultant – same reasons. On the site, I review data publically with the understanding that I have no medical relationships and am simply making general comments. But personal care, right now, is not permitted. Sorry, Regards Fred Coe
Can you develop a nephrocalcinosis by spending a month drinking 4 liters of milk a day during the month of October? in March I had an ultrasound that the kidneys were perfectly fine, but I read that micronephrocalcinosis can not be visualized on ultrasound and I am worried if chronic kidney failure develops.
402/5000
Interesting facts: I am a 22-year-old man, in September my filtrate dropped to 100 with a creatinine of 1.05 mg / dl and after one month to 118 with a creatinine of 0.91 mg / dl. The creatinine / albumin ratio came out 11 out of 30 maximum value, in April I had a filtrate of 125, dehydration or muscle pain can increase creatinine for a few months and go back to normal?
Hi Sergio, These changes in serum creatinine are very tiny and could reflect simple random variation. All of your eGFR values are normal, and the actual equations in use have a wide variance in the normal range. I would be unconcerned unless your physicians have found something they deem worrisome. Regards, Fred Coe
I also commented, when I came on vacation last September my creatinine was 1.05 then after a week I went to 0.96 in a few weeks more to 0.92 and after a month to 0.91, I have always had the creatinine at 0.85 and this scares me something, with 17 years I had once a creatinine of 0.94 so I can assume that these creatinine increases can be somewhat transient, when I came out 1.05 I drank a lot of liquid and my question It is even if I drink a lot of liquid if I had a kidney disease that would cause me to lose the capacity of the kidney, creatinine would not go down by the liquid, right? or maybe? because if my kidney can not expel creatinine in the urine, it would accumulate in the blood and the liquid I ingest if it makes me expel it, right? Sorry to be so heavy but I’m very worried about this issue, it takes away the desire to live ..
Hi Sergio, Once again, these are meaningless changes, and you have no evidence of kidney disease. You have no basis for worrying about this disease. Regards, Fred Coe
Hi Sergio, I do not know if so much milk can cause nephrocalcinosis but doubt it can. I gather you had an ultrasound done out of concern. It is negative. I see no reason to do more, as more is a CT scan, and radiation for no valid reason seems less than ideal. Regards, Fred Coe
397/5000
So without being diabetic or hypertensive and having an ultrasound well I have no risk of chronic kidney failure? The doctors told me that the ratio of albumin / creatinine to being 11 and normal ultrasound I have no kidney problem, I ask this because it really scares me to have to rely on dialysis or a transplant with 22 years and this gives me a lot fear.
Hi Sergio, I see no reason why you should be concerned at all. Your physicians are correct, you have no evidence of kidney disease. Regards, Fred Coe
And one last question and it does not bother him anymore, a urine pH of 9 after eating is a sign of kidney failure or it can be due to the diet? fasting take out a Ph of 6 in the urine, thank you for taking your time with all the questions I have asked your words have helped me a lot mentally.
Hi Sergio, You need not trouble yourself about your kidneys or urine pH so far as I can tell. With food urine pH can indeed increase, although I suspect the value of 9 is not correct. Regards, Fred Coe
What do you mean it is not correct? something wrong?
Dear Sergio, there is no evidence of kidney disease. A urine pH of 9 is above what kidneys can produce (7.9) and is a common artefact. Regards, Fred Coe
Could you please comment on high blood pressure and, kidney disease in a 9 yr. male. He appears to be totally healthy, but this was noted in a regular checkup. I am speaking of my grandson, and my heart is broken. I am afraid for him. Any light you could shine on the subject, would be most appreciated. Thank you.
Hi Marie, Reduced kidney function and increased blood pressure in a child is indeed serious. Of course I have no information and cannot help directly. These problems are generally managed by pediatric nephrologists, and most ideally in a major university medical center. I would suggest strongly that he be seen in such a setting by a team that is set up to handle a matter of such complexity. Regards, Fred Coe
My 4 year old son has been diagnosed with extensive nephrocalcinosis in both kidneys through ultrasound. We just received the results of his 24 hour urine test. The results showed that his oxalate level is 62.5, which is very high based on research on the internet. Can you recommend a pediatric neprhologist? We live in Connecticut, so we can access facilities in NYC and Yale. Thanks!
Hi Brenda, As we have communicated directly, I will only answer this as a general interest question. High urine oxalate in a child is always suspicious for primary hyperoxaluria, but low calcium diet or massive food oxalate excess can do it as well. I would retest after changing the diet to high calcium low oxalate and see if the problem remains. Regards, Fred
Our daughter who is 38 has MSK with nephrpcalcinosis. She has severe pain along with constant dehydration requiring trips to the ER. Do you think in home IF therapy would help her?
Hi Sue, Usually nephrocalcinosis is not MSK but calcium phosphate stones with mineral plugging kidney tubules. But in either case, episodic dehydration will foment more stones, as it occurs with pain attacks. I have used home IV to maintain hydration during attacks so more crystals will not form, and of course find out the cause of stones and do active prevention. Here is a good introduction to the latter. Regards, Fred Coe
Hi Sue, Usually nephrocalcinosis is not MSK but calcium phosphate stones with mineral plugging kidney tubules. But in either case, episodic dehydration will foment more stones, as it occurs with pain attacks. I have used home IV to maintain hydration during attacks so more crystals will not form, and of course find out the cause of stones and do active prevention. Here is a good introduction to the latter. Regards, Fred Coe
Good morning! Recently i had an ultrasound of the whole abdomen. All my lab results are ok except a little high in uric acid. Also have fatty liver, gall bladder polyps and recently right kidney calcification. Didn’t see a doctor yet. What foods are allowed for me to take? Are my results too alarming? Many thanks.
Sheryl
Hi Sherly, The main issue here is what may be a kidney stone. Before doing anything more I would advise your physicians consider an ultra low dose CT scan to be sure it is a stone – ultrasound is not very discriminating – and if so if it is calcium based or uric acid – one can tell from the CT to a large extent. Foods and all are after you are sure what is there. If a stone or stones, here is a good beginning place to read in. Regards, Fred Coe
Hello Dr
I had a kidney stone(oxalat) lodged in my ureter in 2003, something I will never forget. In the years to follow I believe I have passed either a tiny stone or crystals all during emergency room visits. I also had and have at present high calcium 305 in my 24 hour urine test. My dr gave me thiazides diuretic ( moduretic ) but that eventually caused such a bad skin reaction from the sun I stopped it.
I am currently getting some stabbing sensations not to bad and I think I need to do a follow up, I am so afraid of any future kidney damage.
I am 58 female and otherwise in good heath. I do however have very high colesterol and sludge in my gallbladder ( diagnosed through Ct scan last year)
Any suggestions regarding the diuretics???? My calcium in blood is fine as is creatine
Thanks
I was given
Hi Sandy, You seem to have idiopathic hypercalciuria – I assume your serum calcium is totally normal – and a photosensitivity reaction to moduretic, a combination of hydrochlorothiazide and amiloride. The ideal alternative is to lower diet sodium to below 100 mEq/d (2300 mg) or even lower, which can greatly lower urine calcium. As well, refined sugar will raise urine calcium as will a protein intake above 1 gm/kg/d (PCR in the 24 hour urine panel gives this number). You would be best with the kidney stone diet that puts all this together. Take a look. Regards, Fred Coe
Hello, Dr. Coe,
I had onset of many calcium phosphate stones brought on by a high protein diet and low citrate.
I’m an Ultrasound Tech and saw this rapidly occur in one kidney over just 5 months.
After stopping the diet, I continued to have phosphate crystals in my urine for several months.
I was prescribed Potassium Citrate and everything looked good. Dr advised that I could probably stop it because my water intake was so good, I was doing low sodium diet, and my pH was 7.3 with the potassium citrate.
With potassium citrate treatment, my SS Ca P was only 0.46. My citrate was 482.
Now it’s been over a year since ceasing treatment and my other kidney is now full of visible nephrocalcinisos as well.
I’m worried about kidney damage. I’m 32, normal weight, active, and otherwise healthy except for Hashimotos (which has been treated with levothhroxine since age 15).
The doctor can’t see me for two more months. In the meantime, what can I do?
How would you treat a patient for this?
Hi Joyce, I would want serum and 24 hour urine testing to find out how you form your crystals. I would not want to wait very long, either. If you are forming lots of stones, supersaturations for those crystals are above 1, for sure, and you need to know why. Regards, Fred Coe
Thank you very much, Dr. Coe. I was able to get this 24 h urine ordered, even though I cannot be seen until July. I have not been on Potassium Citrate for over a year. As you said, likely one of my SS will be over 1. As you can see, my SS Calcium Oxalate is over 1. However, my pH is very high. My Citrate is lower than it’s ever been. Would you still recommend Potassium Citrate?
Also to note, I notice that my pH is very high, my Ammonium very low (lowest of the range, and the lowest it’s ever been, even though I am not on Potassium Citrate- which I know decreases it) , and my Potassium is 87. I have noticed comparatively to my other previous 24 h urines, that my Urine Ammonium is lower and Urine Potassium higher. Do you think I have some sort of RTA? Or is Citrate usually much lower with RTA? My Comprehensive Metabolic Panels have been normal to date, but I’m wondering if I need to have another done.
I am 32 years old, my GFR is 78 (lower than it’s ever been) and I’m motivated to get this ironed out, and really trust your advice.
Do you know of any connection between low stomach acid and low urine citrate? I have Hashimotos and I know low stomach acid goes along with this. I’m wondering if taking Betaine with Pepsin would be helpful for me, or if it could potentially be harmful.
THANK YOU!!
My Recent 24 h Urine Results:
Urine Volume l/d: l/d: 0.5 – 4 L———————————————————–My level: 4.47 L
Supersaturation CaOx 6 – 10————————————————————–My level: 1.52
Urine Calcium mg/d; male <250, female 450, female >550—————————————My level: 270
Supersaturation CaP 0.5 – 2—————————————————————My level: 0.49
24 Hour Urine pH 5.8 – 6.2—————————————————————–My level: 7.176
Supersaturation Uric Acid 0 – 1————————————————————My level: 0.02
Urine Uric Acid g/day: male <0.800, female < 0.750—————————–My level: 0.521
Stone Risk Factors / Cystine Screening:
Ammonium (normal 15-60)——————————————–My level: 15
Sodium (normal 50-150) ———————————————–My level: 150
Potassium (normal 20-100)——————————————–My level: 87
Hi Joyce, I know your stones are calcium phosphate and see that despite a very high urine pH and high urine calcium your CaP SS is below 1, and your CaOx SS trivial at 1.5. What saves you from the hypercalciuria is the very high urine volume, but given so many stones I would not trust it for prevention. Your urine sodium is 150 mEq/d and if you lowered it to 65 mEq/d (1500 mg Na) you might lower urine urine calcium quite a way. The low ammonia probably reflects your diet which may be low in diet acids – not your main problem. The high urine potassium also reflects diet, perhaps lots of veggies and fruits. I would suggest to your physician a repeat 24 hour urine on a much lower sodium diet, and if that is not enough a low dose of chlorthalidone 12.5 mg/d added to the diet all aimed to lower the urine calcium. Diet calcium needs to be high – you have a skeleton. This article details the diet and use of thiazide. Of course your physicians are the ones responsible for your care, and I am far away and certainly ignorant of details, so we have to rely on them. Regards, Fred Coe
Thanks, Dr. Coe. Your info is so helpful, in addition to my doctor of course. I really respect and appreciate your compilation of information & research. I definitely need to increase my diet calcium.
We are re-checking my 24 h urine in 3 months. In your opinion, what would the goal be for my urine calcium?
I would like to have your opinion so I can ask about the thiazide if I can’t meet the goal with diet alone.
I am a 30 year old woman and ha e had many UTIs and have suffered kidney infections after my pregnancies. I have been suffering from pain in my stomach on my right side. I had an xray the showed kidney stones and a ct without dye that showed excessive stones. On ultrasound I was told it was worrisome nephrocalcinosis. My calcium on my blood test was normal. Is it possible this could just be from the stones and easy to get rid of?
Hi Kimberly, you have stones and as a young woman specially need proper evaluation as to cause and proper treatment. The CT is the only really good way to evaluate stones, and ultra low dose CT is very safe. Full blood and 24 hour urine testing is important for you, so try to get that done, and consider treatments based on CT findings and the blood and urine tests. Do not just let it go. Regards, Fred Coe
Is it possible to have nephrocalcinosis without calcium or raised PTH levels in the blood? if so, what causes this? I am just waiting for my blood work to come back but my ultrasound showed nephrocalcinosis in both kidneys and my symptoms appear to be similar to those for hyperparathyroid disease (fatigue, bone pain, blood in urine, back pain and frequent urination). Thank you so much for your response.
Hi Connie, It is most common to have stones because of urine abnormalities, and less common to have them from primary hyperparathyroidism. Here is a good article on the usual evaluation of patients. If your fasting blood calcium is normal – best is below 10.1 fasting – PHPT is not present. 24 hour urine testing is far more likely to show the cause of stones, so be sure to get it. Regards, Fred Coe
Hi Dr Coe,
I was diagnosed with MSK about 20 years ago. I am now 49. For the first 10 years, I suffered from UTIs and blood in urine, and an occasional small stone ever couple years. Over the last 4 years, I have had two hospitalizations to remove stones, passed a couple stones, and nephrocalcinosis revealed through CT. I take Potassium Citrate and stay hydrated. I have a great doctor. But I am interested in what I have to look forward to. Does MSK generally start accelerating-should I expect more frequent episodes? Should I be concerned about filtration rates? It’s frustrating, it seems not much has changed and there has been so little research about MSK prognosis and treatment in 20 years. It’s hard to get a sense of what other patients deal with over the long term, and what I have to look forward to.
Hi Jen, The most important matter is if you have MSK. Calcium phosphate stones can lead to tubule plugging that produce nephrocalcinosis often falsley labeled MSK. In MSK stones are calcium oxalate. Take a look at the analysis of stones you have made. Calcium phosphate stones can be very frequent, and may require special kinds of treatment. This may involve stopping K citrate. Regards, Fred Coe
hello,dr.
1 have had kidney stones now for over 38 years, been to the emergency room well over 20 times for stubborn stones,and had to pass them with very little help of pain killers, finally at age 52 i had surgery through my back to have multiple stones from my right kidney removed ,after about 2 weeks i had no more blood or sand from my kidney,,O K, 3 years later pow it hit me in my right kidney again , for the next 2 years i have several eppisodes of emergency room visits and passing stones,,57 year old now,bam emergency room again,this time i have a 9 mm stone blocking my urine so i get a stent and a surgery date 3 months away during this time BAM!!! my left side is so bad hurting i forgot about my right kidney to the emergency room i go,,diagnosis, multiple stones in my right and left kidney,on top of the stent and 9mm stone,the perticular stone in my left kidney is to big to pass 5mm so i get another stent,i now have 2 stents and thank God for them because the ferocious pain has eased, now 58 i have surgery or proceedure through the lower you know? during surgery i go septic and almost die from the infection,however the stones were removed and i recover stents, remain for a while 12 days i believe,time to remove them,this time i was awake and was able to see the removal procedure ,one stent removed,i can not recall which one,into the second kidney,guess what?,yes another or a missed stone was there,i got to see them remove it with a little basket or looked like an egg beater,any ways they trapped the small stone in it and removed it and then removed the stone,after recovery and a few months later i go and have a 24 hour urine test,several months later i get the results and they sy i have Hypocitraturia, and Nephrocalcinosis,and are put back on calcium citrate as i forgot to say i had taken it a couple years before the 9 mm stone was found,,i am wondering and hoping maybe you can shed a little light on this almost life long kidney stone adventure,I am 59 in december,and so far have had no more stones,i feel like i am gonna get another Bam! again,, and really dont have much faith in the potassium citrite as i had taken it like i said a couple years before my last surgery,and now this Hypocitraturia,Nephrocalcinosis,,really has me worried,thank you dr.coe,,dennis bouwell
Hi Dennis, It appears that your prevention program has failed indeed. You have had repeated surgeries. Better prevention is essential. I suggest you speak with your physicians about referral to a specialized kidney stone center in hopes of a more perfect prevention program. If you wish to tell me where you live perhaps I can suggest a specific place for you. Regards, Fred Coe
hello I have just passed a 3mm stone from left kidney but during ct scan for this doctor noticed a 28mm x 16mm calcification on my right kidney I am worried
Hi Graham, that is a large stone. I am sure your physician will want to consider its removal. Be sure it is analysed, and that you are evaluated as to cause so as to prevent more. Regards, Fred Coe
A recent US mentions numerous tiny calcifications in left kidney, the right kidney being removed in nephrectomy . An MRI 4 months earlier mentioned numerous tiny renal cysts. Could they be referring to the same thing?
A CT scan and US performed 4 months before MRI reported a 7mm stone in left kidney that seems to have disappeared in subsequent scans. During this period eGFR has went from 41 to 31, and I do have confirmed glomurosclerosis based on pathology report on right kidney. Obviously progressive CKD may contribute to these findings.
Any ideas would be appreciated. Thanks .
Hi Pft, The CT scans are very reliable, so the stone was probably a stone. Cysts are not uncommon in CKD. I am not sure why your eGFR should fall so much and I hope your physicians are attending to possible causes. Given a stone and CKD, perhaps they might want to get a single kidney stone 24 hour urine to be sure about urine oxalate. Best, Fred Coe
Hello, Dr. Coe. First and foremost, thank you so much for your work. You strive to make this complicated subject more understandable for people like me, and I couldn’t be more grateful. I was diagnosed in 2017 with bilateral medullary sponge kidney with bilateral nephrocalcinosis, although I am unsure what the nephrocalcinosis part means for me after reading your article. I’m seriously considering talking with my urologist about the possibility of having my kidneys “cleaned out” after my baby is born this summer. I know the benefits will likely only last for maybe a few years, but I’m desperate to give my family (and myself) some sort of respite from these monsters that are taking over my kidneys. According to my nephrologist, my kidney function is good, which is my primary concern with the possibility of a clean-out. I don’t want to do anything that could cause damage and/or decreased function. What are some things I need to consider and research while deciding if this is the best course of action for me? Do you have any other advice that could help?
Hi Chrissie, I do have some thoughts for you. Given lots of stones, you need to know why. If they are all calcium oxalate it might be MSK, if they are mostly calcium phosphate is probably not MSK. What about your serum and 24 hour urine testing. I would start with this article. It gives a lot of ideas for how to proceed. As for surgery, not a good idea until you know why you make stones and are doing something to prevent them. Otherwise, more may well form. Regards, Fred Coe
Thank you. Also, is there a particular article that should be linked in your above comment, or were you referring back to this article again? I want to be sure I’m understanding you.
I see your other question and will try to be helpful there. Fred
I was diagnosed with Nephrocalconosis a few years back and have never had any stones. My last 24 hour urine showed I had very high urine calcium and phosphorus and high oxalates in my urine. My blood work was normal. My nephrologist said to lower my calcium intake which didn’t seem right to me, so I started following the kidney stone prevention diet with Jill and will repeat my labs next week. My question for you is do you know any ways to lower urine phosphorus? Also is there a test i can ask my nephrologist to order in order to figure out what caused my nephrocalcinosis so I can make sure it doesn’t get worse? My last sonogram said possible MSK. I was in the process of looking for a new nephrologist when everything was shut down so I can get some answers and make sure I’m doing the right things to stop the progression of my CKD. I’m currently stage 2. Do you have any recommendations for a nephrologist on Long Island, NY? I live in Suffolk County.
Thank you for your time,
Gina
Hi Gina, Dr David Goldfarb, NYU, is outstanding at stone prevention. I would use him when the virus is lessened. Urine phosphate is entirely dietary, so it it is high you are eating a lot of it. Common sources are beverages like diet drinks. The NC can have so many causes! I always look to the blood and 24 hour testing for answers, as you have been doing with Jill. Regards, Fred Coe
Is there a more specific article regarding medullary nephrocalinosis in a transplanted kidney?
Hi Christine, I have not written such an article, because I have not seen this phenomenon. I will bring your question to Dr Michelle Josephson, who directs our medical transplantation group and ask her if she has information. Thanks for the question, and I hope to get you an better answer. I have sent her an email and asked her to write to you directly. Regards, Fred Coe