Perhaps the most common abnormality among calcium stone formers, idiopathic hypercalciuria (IH) causes calcium kidney stones and can lead to bone mineral loss and fracturing bone disease. Proper treatment requires a high calcium intake, a low sodium intake, moderation of very high protein intakes, avoidance of refined sugar loads, and – not rarely – use of diuretic drugs which can lower urine calcium losses, prevent stones, and protect bones.
Why The Bathers?
Bone seems, to me, a bather in a bathtub. Calcium flows in from faucets – the GI tract – and out down the drain – the kidneys – as they regulate serum calcium – the height of the water in the tub. I realize the bather does not take up or lose water, but if you ponder the image awhile you may see in it what I
see.
The Large Bathers (1884-87) of Renoir and The Large Bathers (1900-1906) of
What is Idiopathic Hypercalciuria?
What is Hypercalciuria?
As hypertension is defined by blood pressures that associate with stroke, heart failure, and heart attack, hypercalciuria is defined by urine calcium excretions that associate with stones.

Increasing urine calcium losses associate with increasing risk of stones in two cohorts of women – red – and one of men – blue. Urine calcium is along the horizontal axis in six bins. The average relative risk of forming stones is marked by the tops of the bars. A value of 1 means no higher than among people with urine calcium below 100 mg/day – the reference population.
The lower 95th percentile of risk is at the bottoms of the bars. When the bottom of a solid bar lies above one, which is the case for all bars from 200-249 mg/d on, increased risk is very likely present. So the threshold of hypercalciuria is 200 mg/d both sexes.
Diet was not controlled, so we do not need special diets to diagnose hypercalciuria using this criterion.
As the urine calcium rises, risk – top of the bar – rises in smooth progression.
What Does ‘Idiopathic’ Mean?
The overwhelming majority of hypercalciuric stone formers have none of the many diseases that can raise urine calcium excretion. Their urine calcium exceeds 200 mg/d for no obvious reason – idiopathic, arising of itself, without overt cause.
Normal Calcium Excretion
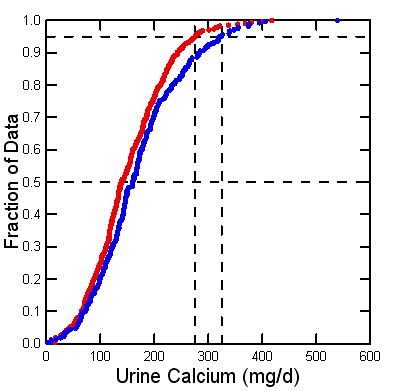
Since 1900 scientists have collected 24 hour urine samples from people in clinical research units, perfect collections, and measured urine calcium. I collected all such values I could from published papers – a tiring exercise. Here is my yield of values from normal adult men (blue) and women (red).
The threshold of clinical hypercalciuria, 200 mg/day, resides at about the 75th percentile: 25% of normal people are above it. But stone formers are perhaps 7-10% or less of the human population. So hypercalciuria raises stone risk, but not everyone gets the stones.
Likewise, stone disease is familial, but IH alone does not fully explain why. Presumably other inherited factors matter.
Decades ago we used the 95th percentiles of these two distributions, at about 275 and 325 mg/d of calcium for women and men, to define ‘hypercalciuria‘. No doubt such high values confer risk of stone, but they are too high for clinical use. They remain useful in research to define people with extremely high urine calcium values.
Hypercalciuria Raises Supersaturation and May Promote Plaque
Supersaturation produces and enlarges crystals and therefore stones. We now have superb evidence that rising supersaturation associates with rising stone risk. Calcium oxalate and calcium phosphate supersaturations rise smoothly with urine calcium, leaving no doubt that urine calcium raises risk of calcium stones via increasing supersaturation.
Many calcium stones form on plaque, tissue deposits of calcium phosphate crystals in human renal papillae. Plaque abundance rises with urine calcium excretion, and a plausible theory, vas washdown, links them.
Idiopathic hypercalciuria is Hereditary
 Family Studies
Family Studies
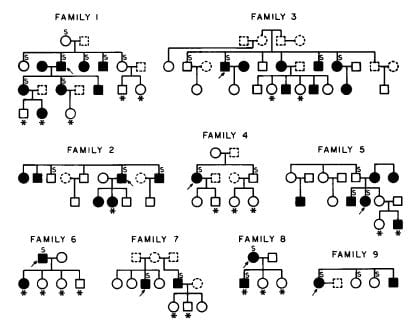
I am not sure if we were the first, but here is our evidence from 1979.
The arrows point to the stone formers whose families we studied. Filled symbols are men (square) and women (circles) with IH, asterisks mark children, open symbols did not have IH, and dashed people are deceased. About 50% of immediate blood relatives had IH, in successive generations. Others have also found IH heritable.
IH might look like a simple dominant trait from one abnormal gene, but it results from a number of genes. Incidentally, urine calcium is not the only stone forming trait that appears genetic. Urine citrate appears to be, as well.
Animals
Dr. David Bushinsky bred rats with the highest calcium excretions. Urine calcium rose for the first 40 generations, and thereafter seems at a near plateau. So the trait is breedable.

These animals form calcium stones and develop a more severe bone disease than normal rats if diet calcium is not ample. So they well mimic human IH.
We humans did not breed ourselves for IH. Something about the trait must have conferred a benefit during evolutionary time.
Children
We had the opportunity to collect 24 hour urine samples from large numbers of boys and girls who were brothers and sisters of children with kidney stones, and also from children in families where none of the children, their parents, or other relatives were known to form stones.
Urine calcium excretions of siblings with more than two stones (left panel of the figure) are highest – farthest to the right. Next highest – second from the right – were siblings with 1 – 2 stones. Siblings with no stones were even  lower, third from the far right.
lower, third from the far right.
Children from families with no kidney stone history were lowest – most leftward – and almost none had above 200 mg/day of urine calcium loss.
The four bars in the right hand graph say the very same thing. Mean values of urine calcium, shown by the top of each bar, rose progressively with stones.
This is expected if IH is genetic and causes calcium stones.
Hypercalciuria with Hematuria
Hypercalciuria in children not rarely causes hematuria found on routine screening. Loin pain with hematuria is a common syndrome ascribed to crystal passage. IH can raise urine supersaturation and higher supersaturations promote crystals. Hematuria can be familial because it is due to IH and crystals or stones. In adults, unlike children, hematuria can be from malignancy so proper evaluation, even in stone formers, requires imaging and considerable care.
Bone Disease
There Is Bone Disease in Stone Formers
Epidemiology of Fractures
This figure, from people living in Rochester, Minnesota, shows the cumulative incidence of vertebral fractures among those who had a symptomatic stone (irregular line) and the expected fracture rate 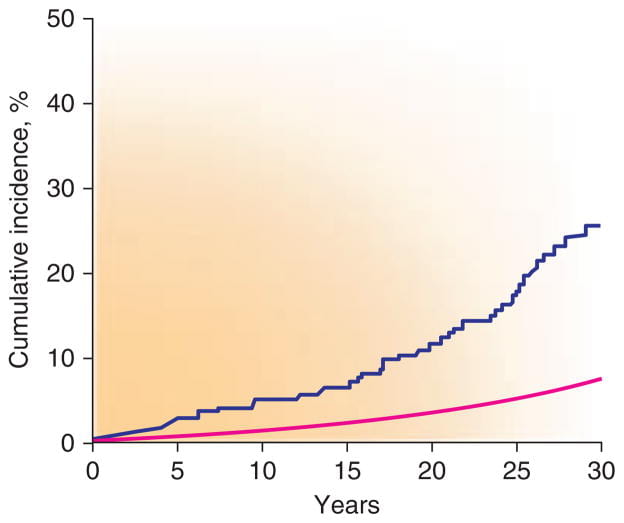 based on the entire population (the smooth line) between 1950 and 1974. The excess of fractures was not observed for hip or forearm.
based on the entire population (the smooth line) between 1950 and 1974. The excess of fractures was not observed for hip or forearm.
Bone Mineral Density
Reduced bone mineral density is a general finding in stone formers. 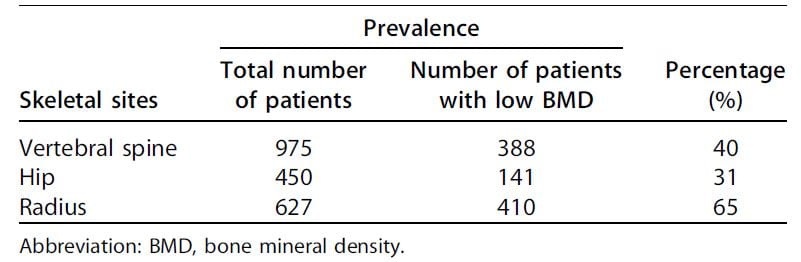
Among 2,052 patients assembled from 20 separate studies, between 31% and 65% had some reduction of bone mineral density (Table). Although not remarkable for fractures in the Rochester study, the radius was most affected.
The authors of this review did not conclude that IH caused the low bone density of stone formers. I infer it played an important role, however, because IH can promote bone mineral loss (detailed in the next section) and thiazide diuretics – well known to lower urine calcium in IH – appear to reduce bone disease.
Prospective Bone Mineral Observations
Another reason I make this inference is that the magnitude of urine calcium loss predicts future loss of bone mineral.
We measured bone mineral density in a number of stone formers with IH, collected 24 hour urine samples, and then re-measured bone mineral density three years later.
When change in bone mineral by three years (vertical axis) is plotted against the urine calcium loss at time 0, (horizontal axis), the trend – highlighted by 68% containment ellipses – points downward: More urine calcium loss at the beginning, more bone loss by three years. A majority of people with urine calcium above 200 mg/d lost bone mineral over three years, whereas those with values below 200 mg/d tended to gain bone mineral.
How Does IH Raise Urine Calcium?
The Extra Calcium Can Come From Diet

In the balance studies from which I derived normal calcium excretions, scientists fed subjects a fixed diet and measured all food calcium eaten and all calcium lost in the stool. The difference between calcium eaten and calcium lost in the stool is net calcium absorbed into the blood.
Typically measurements are made in 6 day blocks after a few days to equilibrate with the diet, so subjects participate for perhaps 8 – 10 days. I have aggregated the calcium absorption measurements that match the urine calcium excretions I already showed you.
Normal men and women (orange) absorb about 18% of diet calcium. I combined the sexes because they have almost identical values. Women and men with IH – the blue curve – absorb much more calcium, about 30%.
You might ask how calcium absorption can be negative – points to the left of the vertical 0 absorption line. It is because salivary glands, pancreas, liver via the bile, and perhaps the ileum secrete calcium from blood back into the bowel lumen. When diet calcium is less than this ‘endogenous secretion’, stool calcium loss exceeds what is eaten.
An early theory held that IH arose from over absorption of diet calcium: High absorption, more calcium comes into the blood, the kidneys lose it – done. This theory led to decades of low calcium diet as a treatment for stones. No one knew such diets might cause fractures.
The Extra Calcium Can Come From Bone
A Glucose Load Causes Bone Mineral Loss
Years ago Dr Jack Lemann did this informative study. He measured urine calcium excretion (vertical axis) then gave glucose or sucrose (table sugar) to normal people, calcium stone formers, and relatives of calcium stone formers.
 Compare the control (left of the big arrows) calcium excretions of the normal subjects to the stone formers: 5 of the stone formers have control values above all but the highest normals. The relatives of stone formers are even higher – and this is fasting, before the sugar load!
Compare the control (left of the big arrows) calcium excretions of the normal subjects to the stone formers: 5 of the stone formers have control values above all but the highest normals. The relatives of stone formers are even higher – and this is fasting, before the sugar load!
Each period was 20 minutes, so this experiment went on for 2 hours. The higher urine calcium with sugar must come from bone – there was no calcium in the sugar drink. It came from bone in normal people and in those with IH but the latter lost far more calcium than the former. Though fasting they had higher urine calcium losses.
In a separate experiment, Lemann proved that the kidneys themselves caused calcium loss from sugar by reducing their conservation of the calcium they had filtered out of blood.
Low Calcium Diet Causes Bone Mineral Loss
We persuaded nine normal people and 27 stone formers with IH to eat a very low calcium diet – 2 mg/kg body weight – for 9 days, and on days 7-9 we collected 24 hour urine samples and measured  calcium losses.
calcium losses.
The diet went well; most people ate what we asked (middle panel). The normals (the 9 people to the left on the plot) lost in their urine less than 2 mg/kg of calcium daily – lower panel, to the left, so the difference each day between what they ate and lost was positive (upper panel, all normal points were above 0).
The patients were different. Many lost more calcium in their urine than they ate, and did so most of the time. This was bone mineral lost in the urine.
On such a low intake surely everyone was losing bone mineral because the fraction of diet calcium that is absorbed into the blood is far below 100%. I just showed you that it is about 18% in normal people and 30% for people with IH.
But those with IH were more flagrant than the normals. Because their urine contained more calcium than they ate we could prove bone mineral was lost.
In IH Urine Calcium Usually Exceeds Net Calcium Absorbed
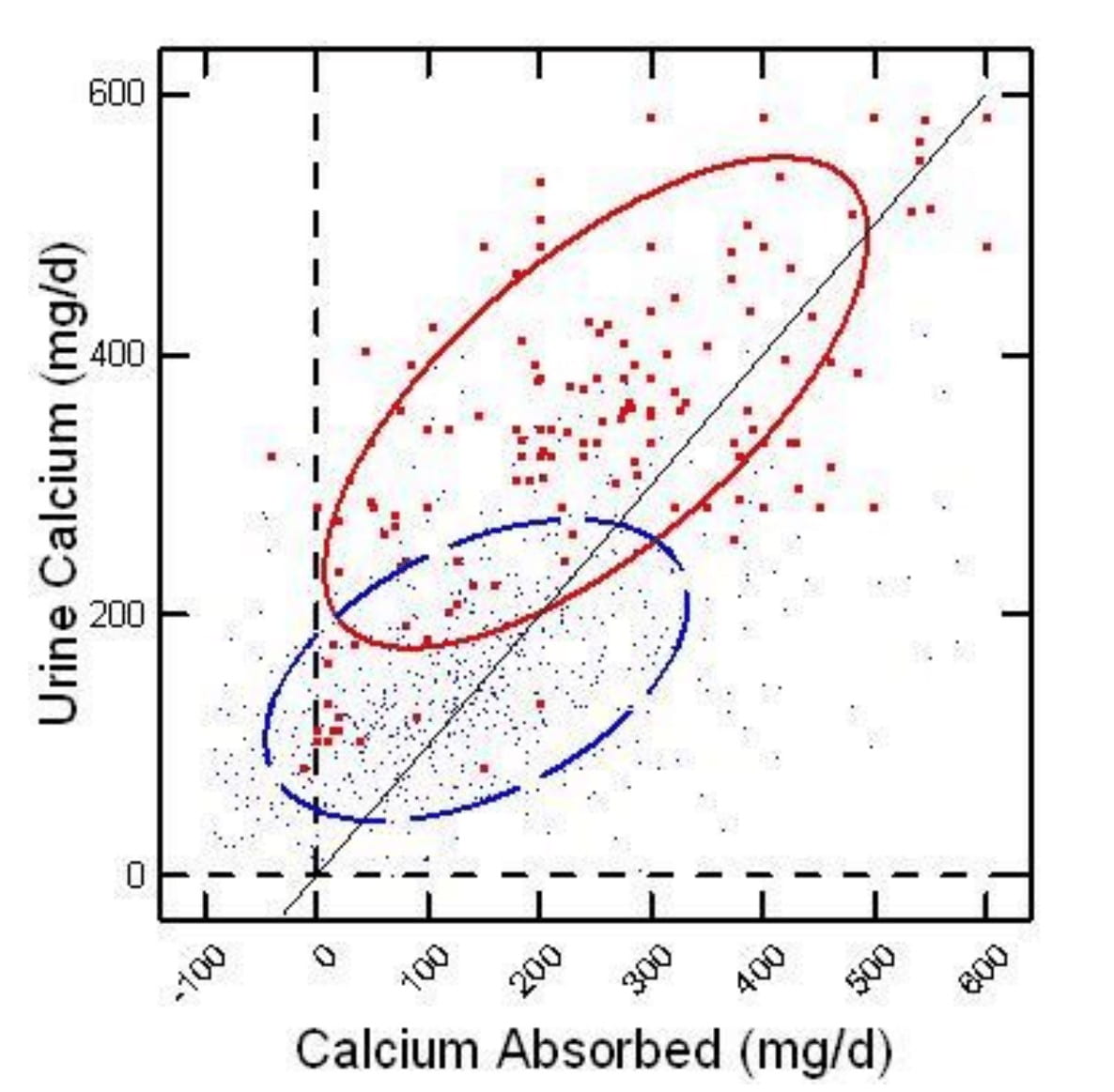
On the horizontal axis of this figure, calcium absorption is the difference between calcium eaten and lost in the stool. Urine calcium is on the vertical axis. People with IH are red large dots, and normal people are blue microdots.
Each point compares calcium absorbed in a day to calcium lost in the urine. If urine calcium is higher than calcium absorbed (points to the left of the diagonal line of identity), bone mineral is being lost in the urine. Those to the right the opposite – bone is gaining mineral.
At a net calcium absorption of 150 mg/d or more, a majority of the normal points lie to the right of the diagonal line – urine calcium is less than calcium absorbed. Bone mineral is stable or increasing.
Idiopathic hypercalciuria points all lie left of the diagonal line, negative bone mineral balance, until net absorption rises over 300 mg/d. It takes a huge amount of calcium absorption to overcome the tendency of IH people to lose bone mineral.
Bone Calcium Retention vs. Diet Calcium
Perhaps a more practical way to envision these balance data is to plot calcium retention – net calcium absorbed minus urine calcium excreted – against diet calcium intake.
At diet calcium intakes above 500 mg/day, the average retention (the jiggly blue line) for normals passes through 0, meaning that their bone mineral stores will, an average, be stable. Higher calcium intakes make the normal average rise so that by 1,000 mg/day  a majority of normal points are above 0.
a majority of normal points are above 0.
Among the IH subjects (red), retention rises with diet calcium intake, but the average – red line – never passes through 0. Some points do lie above 0, meaning that not all IH subjects will share the general high risk of bone mineral loss, just as some normal points lie below 0 even at high calcium intakes. But on average, at all reasonable calcium intakes, IH appears to hamper bone mineral retention.
What Have We Learned?
Low calcium diet is not ideal for normal people and a disaster for those with IH. Given IH, even a liberal calcium intake will not achieve stable bone mineral balance for the average person.
These balance data lay latent in papers published from 1900 through until even recent times. Using a different and sophisticated way to assess bone mineral balance, Lieberman and his colleagues showed as early as 1965 that IH reduced bone mineral stability. Yet low calcium diets remained a common treatment for stone disease for more than a decade thereafter.
IH Kidneys Release Excess Calcium
Filtered Calcium
Calcium gets into the nephrons of the kidneys by filtration from blood. If you do not know about filtration, use this link to learn about it.
Each of the 2 million nephron units we possess in our two kidneys has a glomerular filter that filters water, sodium, calcium, phosphate, oxalate, and thousands of other small molecules and ions out of blood into the long tubules that process the filtrate into urine.
Reclaimed Calcium
The process we care about here is reclaiming filtered calcium back into the blood. Normal people excrete about 2% or less of filtered calcium, those with IH excrete 4% to 5% or more.
Here are a few numbers. We filter about 150 liters/d. The filtrate contains about 40 mg/l of calcium: 40×150 = 6,000 mg/d of calcium. Of that 2% is 120 mg/d, 4% is 240 mg/d, 5% is 300 mg/d. So the differences in percent excreted account for the range of calcium between normals and stone formers.
Where Along the Tubule?
Review the Proximal and Distal Tubules
Each kidney tubule resembles a woman’s hair – long as a long hair, and that thin. Down the center of the hair is its lumen through which the filtrate passes to become urine, and where calcium is reclaimed.
Go back to the filtration article and check out the tubule picture. Pay special attention to the proximal tubule. In the proximal tubule calcium is reclaimed in parallel with sodium. In the distal tubule – on the picture in the link – calcium can be reclaimed independent of sodium.
Urine Calcium Follows Urine Sodium
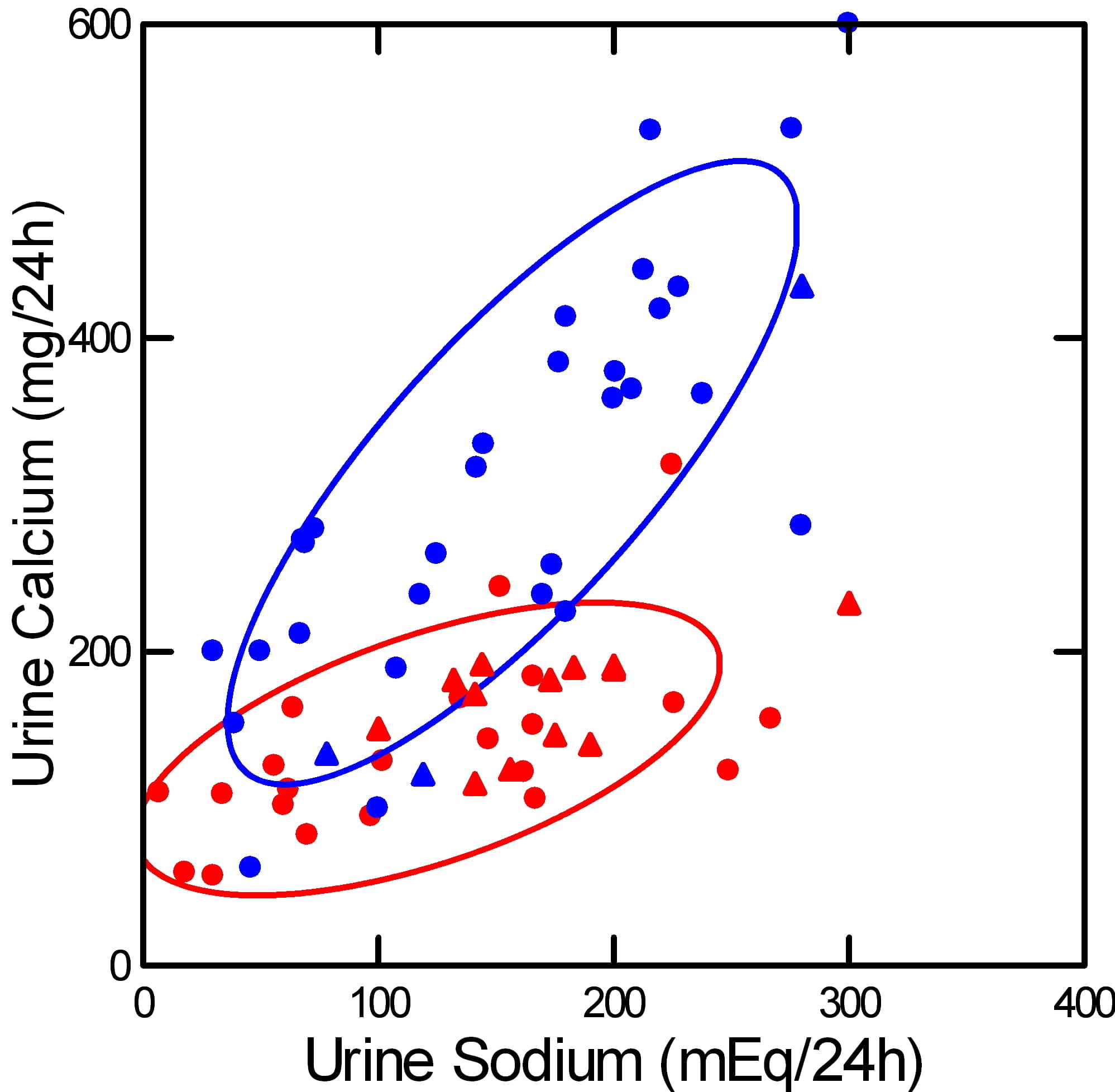
This picture illustrates the basis for recommending a low sodium diet to lower urine calcium in IH.
It shows how urine calcium (vertical axis) rises as urine sodium (horizontal axis) rises. The rise is far steeper among stone formers with IH (blue) than in normal people (red). Circles show experiments – diet sodium was deliberately altered. Triangles show observations – diet sodium and urine calcium varied on their own.
Urine Calcium and Sodium are Linked in the Proximal Tubule
As you eat more sodium, urine sodium goes up so output balances intake. One way the kidney accomplishes this balance is that filtration rises with higher sodium intake. Another is that reclamation of water and sodium in the proximal tubule (the part nearest the glomerular filter) goes down – more sodium and water flow downstream in the nephron. Calcium goes with it, the two are linked by the way that part of the nephron works.
For this reason, the steeper slope of urine calcium vs. urine sodium in IH must arise from abnormalities further downstream from the proximal tubule. We cannot presently identify where or how this happens.
What Can We Do With What we Know?
We can shut down filtration and increase reclamation of sodium in the proximal tubule. Both will reduce urine calcium by reducing delivery of calcium downstream. Lowering diet sodium does both, reduces filtration and increases proximal tubule sodium reclamation. The latter is usually more prominent than the former.
Thiazide diuretics do the same. They increase reclamation in the proximal tubule.
Once you understand this, you understand why reducing diet sodium and taking thiazide are two ways to do one thing. So the more you limit diet sodium the less you need thiazide, or at least the less dosage you need. On the other hand, if you take thiazide and eat a lot of sodium, the sodium will undo the effect of the drug.
What Happens to Bone?
Diet Calcium Must Be High
All this gives some insight into why IH appears to reduce bone mineral.
When we eat, the kidneys release calcium into the urine, normals and IH alike. But IH patients release a lot more calcium, depending on their sodium intake. If the diet has adequate calcium in it, bone can get its share even if more than normal is lost in the urine. If the diet is not so adequate, less than 1,000 mg/d, bone may not get its share even in normal people. Given IH, diet calcium must be quite high, at least 1,000 to 1,200 mg. But that cannot be sufficient as I have shown you. Even at such high calcium intakes, bone balance in IH is usually negative.
Diet Sodium Must be Low
The only present remedy for renal calcium wasting in IH is to lower delivery out of the proximal tubule. Low diet sodium, thiazide, ot both can do it. We presently have no other means that have proven effective.
The Combination of High Diet Calcium and Low Diet Sodium Can Preserve Bone Mineral
 The best proof of this is one study showing that in perimenopausal women the combination of low diet sodium and high diet calcium can promote bone mineral gain.
The best proof of this is one study showing that in perimenopausal women the combination of low diet sodium and high diet calcium can promote bone mineral gain.
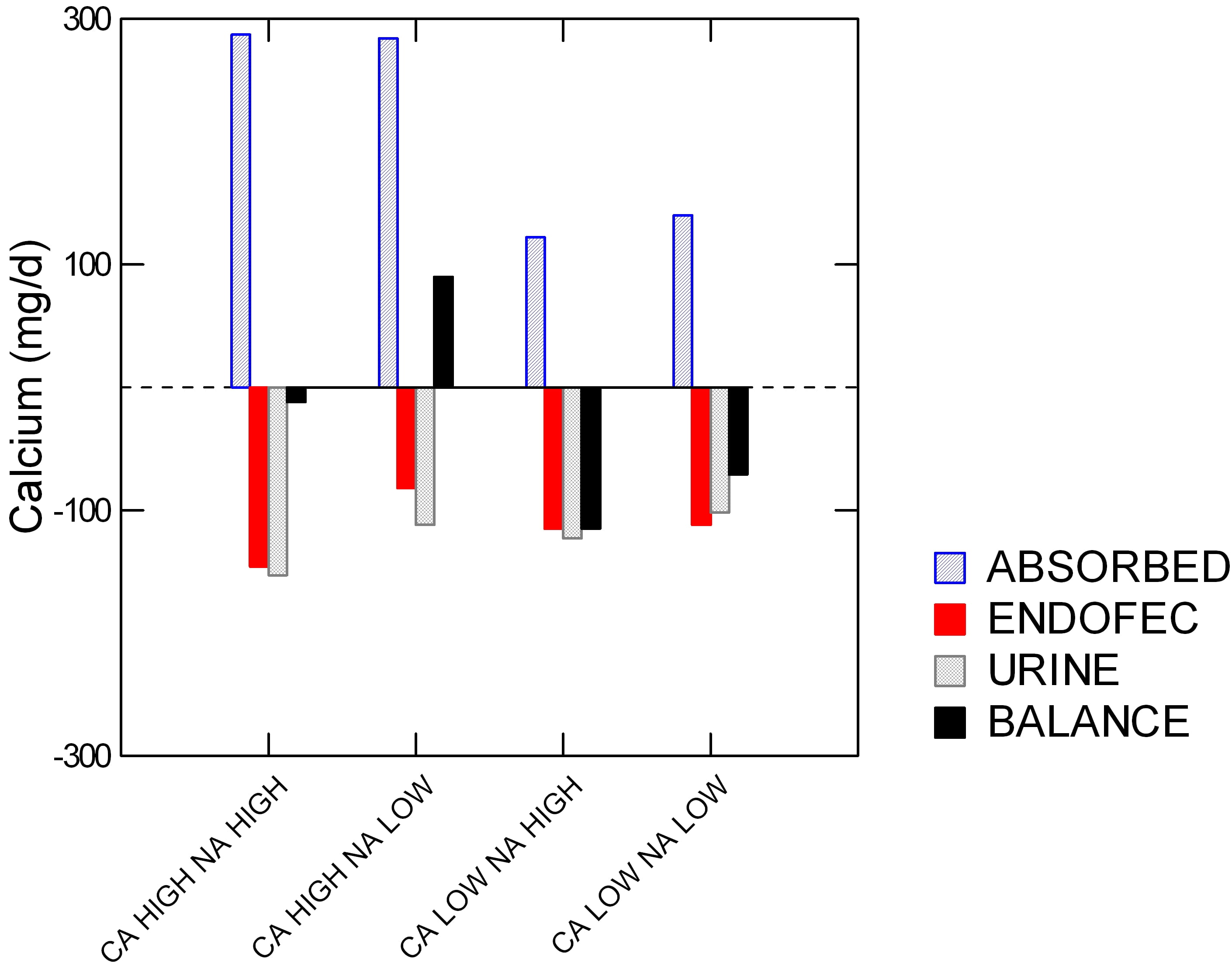
The women each ate all four of the diets shown along the horizontal axis: high and low calcium (Ca) and sodium (Na). Specifically, the sodium levels were 1600 and 4400 mg/day, and low and high calcium (518 and 1284 mg/day.
On the vertical axis is calcium in mg/d. The colors say if ‘calcium’ on the vertical axis is calcium absorbed (blue), secreted by the GI tract (red), lost in urine (gray), and bone balance (black).
Low calcium diets were hopeless. High calcium diets with high sodium led to high absorbed calcium (blue) but also high urine and GI endogenous secretion losses (‘ENDOFEC’): red and gray bars point downward. Reducing diet sodium lowered the urine loss (gray bar was less down) and also – surprise – less GI calcium secretion (red bar is less down).
The net result is good for bone. This one combination drove bone mineral balance positive (Black bar above 0).
Before we leave this powerful demonstration, look back on urine calcium (gray bars). The high calcium low sodium diet gave the very same urine calcium as the low calcium high sodium diet. In other words, the women could raise their diet calcium from 500 to nearly 1300 mg/day and yet by lowering diet sodium to 1600 mg/day keep urine calcium unchanged.
What Makes Calcium Go In or Out of Bone?
Blood is saturated with respect to the initial phases of bone mineral, so called early hydroxyapatite forms. Likewise bone has considerable circulation, so that the outer layers of bone can be in physicochemical equilibrium with the blood. In isolated bone reduction of calcium phosphate supersaturation leads to physical dissolution of bone mineral.
It seems not unreasonable that tiny reductions in blood calcium phosphate saturation can occur when kidneys release calcium into the urine at a rate that exceeds diet calcium absorption. The loss of bone mineral from simple sugar ingestion may well be an example of this effect. Of course bone is regulated by myriads of hormone signallers, but short term mineral balance could be affected by physical forces. This is an area that deserves research.
I should say that in presenting this conjecture about bone it is just that. Furthermore I doubt it is sufficient as an explanation. But it shows at least one plausible connection that can be demonstrated in isolated bone, and perhaps in humans.
In another article, as yet unwritten, I will take up the larger issues of bone and kidney in IH, and show the deeper science that is now available.
What Should We Do?
Kidney Stone Prevention
Without doubt, reduced diet sodium and refined sugar are valuable in all people with IH. Although I did not demonstrate it here, a high diet protein load raises urine calcium and is best brought into the normal range of 0.8 – 1 gm protein/kg body weight/d. Protein intake is calculated from urine urea excretion as the protein catabolic rate (PCR) and best quality kidney stone testing vendors present it on reports.
Bone Disease
Provide Adequate Diet Calcium
Diet calcium must be adequate, 1,000 to 1,200 mg/d. Without concomitant control of diet sodium this alone would raise urine calcium and kidney stone risk. But when combined with low sodium it will not. Multiple proofs of this statement exist. I just showed you one in the lovely four way bone experiment.
Measure Bone Mineral Density
US insurance practices exclude bone evaluation in large swathes of stone forming populations. But bone mineral scans are not very expensive compared to the eventual costs of fractures. A useful medical buying guide places the bone mineral density scan cost to uninsured people at about $200.00, and mentions that in May prices can be lower because it is national osteoporosis month. The price usually includes a simple medical interpretation.
The Kidney Stone Diet
The proper diet for prevention of the common calcium stone arises almost totally from the requirements to treat IH: reduced diet sodium, refined sugar, and protein, and adequate calcium for bone. The last of these, high diet calcium plays another role in stone prevention by lowering urine oxalate. That is fully described in other articles.
As well as stone prevention and the protection of bone, this diet is thought beneficial for reduced risk of hypertension and vascular disease, to which stone formers seem unduly prone.
Because it accords with general diet recommendations for the entire US population, I can recommend its use without hesitancy for stone formers and, incidentally, all the rest of us, too.

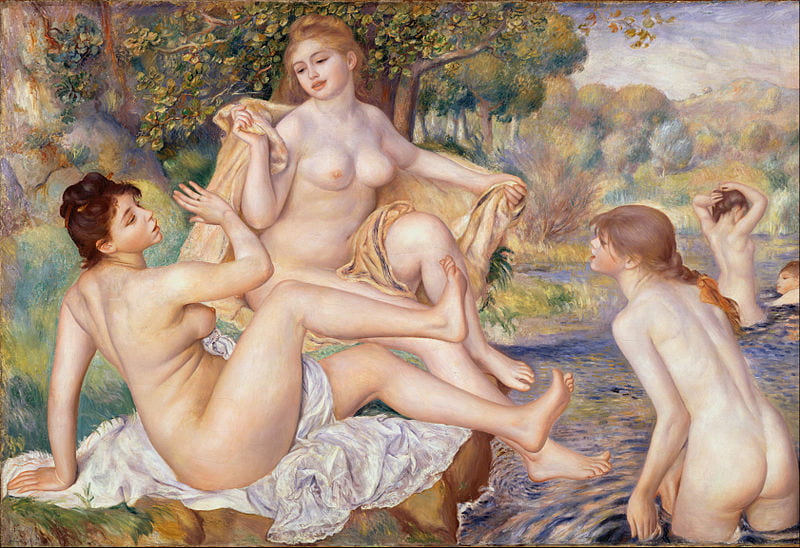
A very good choice these women Bathers by Renoir, not only beautiful but joyous, carefree. A much better choice than Cezanne’s version, colder, darker, almost primitive! I can’t help but think of our MSK members who can only dream of enjoying a bath in this way, most of whom also suffer from hypercalciuria, if only their Drs could figure out what is causing their hypercalciuria, stones, calcifications, chronic pain, hematuria and so many other symptoms and suffering. I find the Bathtub example very helpful to understand how the kidneys work and the fact that high urine calcium can only come from the calcium we eat and our bones, that even a daily urine loss of 200 mg/day is a high risk for bone disease, even though I’ve read many times that MSK can cause bone demineralization, I didn’t know to what extent . And that there are other mechanisms in our kidneys that control absorption, excretion and reabsorption that could go wrong, that there is a combination of causes of high urine calcium but the bottom line is, all urine calcium comes from our food and our bones! If only MSK patients’ Drs could figure out what makes their hypercalciuria tick!
Unfortunately I am still having a hard time with the graphs, as I’m sure our members will too but I’m hoping and will encourage our members to share your article with their Drs who will hopefully understand more than we do.
As always, thank you for listening and sharing.
Dear Celia, Physicians can certainly and happily provide reduced sodium intake, high fluids, thiazide diuretics and potassium citrate, perhaps in combinations to lower supersaturation drastically; this will prevent new stones and crystal attacks. We have treated thousands of patients with IH at the university of chicago and have often published at least our experience. There are formal trials which I plan to review and which support the benefits of treatment. We know enough right now to prevent new stones in a majority of patients. Regards, Fred
Hello Dr. Coe,
Thank you very much for your many detailed and helpful articles. The stone and bone connection was especially relevant to me.
If you are up for the question, would you please share your experience regarding the progression of IH in a given person over time? Specifically, I’m wondering whether I have most likely been excreting huge amounts of calcium since childhood. And, more importantly, as I age, is IH likely to improve, get worse, or remain about the same?
Here’s a brief history for context: My father formed over 100 CaOx stones throughout his life. They started in his late teens. He also broke many bones, including a vertebra. I passed my first CaOx stone at 35. Increased fluids and supplemented Mg. Then I was fine for 15 years except for a single, small instance of hematuria in the middle. (No imaging was done.) Then hematuria occurred again one day, and imaging found smallish stones in both kidneys, 4 attached, one free. Two supersaturation tests reported UCa ~400 mg/day. A DEXA scan showed low BMD, particularly in a vertebra. I was referred to a good nephrologist and was diagnosed with IH – I’m assuming inherited. We replaced Ca supplements with more dairy, and are testing Chlorthalidone.
Hi Al, I suspect you have familial – idiopathic – hypercalciuria yourself and in your family, and it does produce stones and a bone disease of complex nature. Chlorthalidone with very low sodium diet, 1000 mg calcium intake, and a potassium blocking diuretic if serum potassium falls too much sounds just right. IH begins at birth, is a main cause of stones in children, and is highly treatable. It will be in about 1/2 of your first degree relatives. Regards, Fred Coe
Hi Dr. Coe,
Thank you very much for your personal reply. Unfortunately Chlorthalidone & diet haven’t been enough so far. My Ca excretion remained high and I had another stone (thankfully very small) despite clearing 3.5 liters on an average day. So I’d really like to learn more about the specific kind of IH I have, also and how my Ca excretion varies through the day after consuming meals with various amounts of Ca to help me optimize. (I am working with a nephrologist, but also doing a lot of my own research.)
Question – If possible, please suggest ways we may test these two things.
So far, I’ve read about a Ca loading test, but checked with a local lab and they didn’t know about that test, and I am concerned that 1g of Ca at once would pose a very high stone risk.
One other idea I had was to collect measurements similar to those in Table 2 from Dr. Lemann’s study (but for Ca not sugar) which seems to show periodic samples of urine calcium excretion per minute. If creatinine excretion is constant enough, a series of Ca/Creatinine ratio urine tests might work. That’s a standard lab test. There are also “Hypercalciuria test strips” which if their range is appropriate, and if I can actually buy them, might be good enough to be useful.
Best regards,
Al
Hi Al, I re-read your prior note and my reply. There is no extra value from the calcium loading tests in your specific case – marked hypercalciuria and bone disease – and what you would like to do amounts to a research experiment. If you can come to Chicago and are a calcium oxalate stone former we have an active NIH research study ongoing in which we in fact do fasting and meal related mineral physiology and can determine a lot about your physiology. I cannot say this will improve your clinical outcome but can say it would add to your personal understanding of what seems to be a multiple generation bone – stone IH disorder. If you can join us email me directly. Clinically you did not give your urine sodium or calcium excretion on medication, so I cannot say much. Likewise you did not say what happened to your urine supersaturations – did they fall at least by half?? Perhaps you have reduced your stone risk enough. Given the interest in your kind of situation, I would like to know more. Regards, Fred Coe
Dear Dr. Coe,
Thank you for your reply and invitation. I will reply via e-mail regarding studies. However the following follow-up seems to be of general interest. Please allow me to refocus on a very practical question here:
I recently flew down the East coast and passed a small (~1mm) stone a few days later despite a concerted effort to remain hydrated and to find low salt airport food. That was just a short trip. So I am highly motivated to find practical ways to reduce stone risk while traveling (to supplement the customary medication, hydration, and diet which are all of course extremely important), and would be grateful for suggestions.
For starters, do you have thoughts about shifting to a low calcium diet for the evening before and day of a flight? In other words, would a low calcium diet on occasional particularly risky days be protective – even though it is completely the wrong strategy long term? Or could that backfire and actually increase risk even in the short term?
And, would doing an extra 24-hour supersaturation test with a low calcium day as described above, and comparing to a normal test, be a reasonable way of confirming to what degree this would help a given individual with IH?
Best regards,
Al
Hi Al, I doubt the stone you passed after your flight formed during that flight – even small stones take longer to form than a few days. The low calcium diet idea will not work. Any food will increase urine calcium even when that food contains no calcium at all. The best protection from diet is low sodium, with measured urine 24 hour urine sodium values of about 65 mEq/day ideal. This will reduce food induced hypercalciuria and potentiate the thiazide drugs if you are taking them. Regards, Fred Coe
Hello my name is Bryon and am 41 , I start ed having kidney stones about 15 years ago that lasted for about 1.5 year about 4 years ago it started again lithrotripsy every 3to 6 months so 8 times in 4 years on both kidneys. I have developed cancerous tumor on left. We have tried all diets and tested urine with little change. Urinalysis shows high potassium, sodium, uric acid, calcium oxalate,although my blood shows perfect. I have irritable bowl. I have recently been put on potassium citrate, magnesium glyconate, k2, vitamin D because was a little deficient,and a 1000mg. Sodium daily restriction. I have not checked urinalysis since. This has been devastating to my family . I am hoping this diet will work. If someone wants to follow me please let me know
Hi Bryon, From a stone point of view it sounds like you have hypercalciuria and dietary high urine oxalate complicated by high sodium intake and way too many shock wave procedures. Blood tests being normal is what we usually find. I would think the reduced sodium diet should be complemented by thiazide to lower urine calcium further – chlorthalidone 25 mg or indapamide 1.25 mg are common treatments. Potassium citrate is fine unless the stones are calcium phosphate. You have not had follow up measurements so you do not know if the treatment has been effective. Get measured. Prevention requires an orderly approach and here are some tips for managing medical appointments. The tumor is what worries me. Stones do not cause cancer, so it is something separate; it needs its own diagnostic evaluation and treatment. Regards, Fred Coe
How can I be sure I am getting – and absorbing – enough calcium on a daily basis if I do not take a suppIement? Cheese is the only dairy product I eat, and I’d prefer not to eat it daily. I get bleary-eyed looking at non-dairy high calcium food lists that include high-oxalate foods or foods that would require large quantities to reach 1,000-1,200 mg. And then there is the added factor of varying percentages of absorbsion. And getting sufficient Vit D. Thank you in advance for your advice.
(Background: I am 60 and have had two very difficult stone events (2008 and 2011). On my own, I discovered your research, Dr. Coe and even had the pleasure of meeting with you. I was diagnosed with IH – 426 (after some dietary changes but before beginning indapamide). I was also diagnosed with osteopenia and Vit D deficiency (9) in 2011. Since then I have been taking a Vit D supplement and/or Citracal petites off and on and 2.5mg indapamide daily. My diet – most days – is low sodium, low protein, and low oxalate. It is the calcium that has me most concerned and most confused. Annual Litholink labs results for urinary Ca 24 have been 222, 329, 191, and most recently, 248. )
Hi Bonita, From your labs you do indeed have hypercalciuria. I presume there are no systemic diseases causing it so it is idiopathic hypercalciuria. Vitamin D OTC 1000 units a day should maintain your vitamin D stores. It is probably reasonable, all else failing, to take a calcium supplement with meals, perhaps 500 mg of calcium as the carbonate or citrate salt; the trick is to time it so it is taken with the food, and with the larger of your two meals daily – that is 1000 mg. If you can get more in from foods, then just add the 500 mg supplement with your largest meal. You did not say how much sodium is in your urine, be sure it is below 100 mEq/day and even better at 65 mEq/day. Since you have been my patient, as you said, you are free to come back once in a while and let us check things out more directly – Warm Regards, Fred Coe
Dr. Coe,
Is it possible to have enhanced bone resorption (say from PTH-mediated processes) or enhanced GI absorption (say from 1,25vitD-mediated processes) as the primary process leading to hypercalciuria without hypercalcemia? I ask because of the hypercalciuria seen in entity known as normocalcemic hyperparathyroidism (which admittedly could be the result of a primary renal leak, but for argument’s sake let’s assume it is not) or the hypercalciuria of sarcoidosis (that is often seen without hypercalcemia…ionized or total). Assuming that no renal leak exists, I can only surmise that the increased load from turning the faucets (from your bathing analogy) can lead to hypercalciuria from either an increase in ultrafilterable calcium or an increase in the GFR. If GFR doesn’t climb and there is no increase in ultrafilterable calcium, then I’d say to my question is “no”…am I wrong?
Hi Steve, An outstanding question and I hope I can do it justice. PTH increases renal calcium reabsorption so, in primary HPT as an example, filtered load increase has to overcome increased reabsorption. In sarcoidosis, serum PTH is profoundly reduced, and distal tubule calcium reabsorption depressed. This permits marked hypercalciuria without hypercalcemia. Hyperparathyroidism with normal serum calcium and hypercalciuria is indistinguishable from IH except for the elevated PTH and such cases are odd. We have studied a few patients whose fasting PTH values were high, serum calcium normal, and hypercalciuria was present. What we found was a more marked fall in PTH with food so that increased distal reabsorption from high PTH was no longer present. I do not know for sure but these few cases seemed to me an early stage of primary hyperparathyroidism. We have not noted them in our publications. I think reduced proximal tubule and thick ascending limb reabsorptions are critical for understanding these cases, and it is unfortunate that endogenous lithium clearances are so cumbersome that only our group has made substantial observations in IH. If I had to guess there has always been an association of IH and primary hyperparathyroidism as shown by the common residual and long lasting normocalcemic hypercalciuria we and others have published after curative primary hyperparathyroidism. After surgery such patients look exactly like IH and remain that way. So I think they always were that way and have the tubule abnormalities of IH. As for bone mobilization, we have not studied experimental cases – where bone mobilization is promoted by space flight or bed rest so I cannot tell what happens. Warm Regards, Fred
Thanks for explanation. Regarding sarcoidosis, theoretically, there must be a transient increase in blood calcium to drop the PTH or is it the hypervitaminosis D that drops the PTH?
Thanks again.
Hi Steve, Probably the high 1,25 D down regulated PTH gene expression; likewise it will up regulate the PT cell calcium receptor abundance so serum calcium signalling will increase for any serum calcium level resetting the calcium PTH control curve. The opposite – loss of CaSR sensitivity is what I suspect happened in my few cases, and is known to be the beginning stages of PHPT in some patients. Great issues and thank you for bringing them up. Warm Regards, Fred
Dear Dr Coe
Thank you for a very informative article. My children – twins aged 4 – were only recently diagnosed with Hypercalciuria. I deliberately didn’t call it IH because I don’t know what the origins of their conditions are. Their most recent urinary calcium levels as of 14 Feb 16 are 6.66 mmol/L and 5.7mmol/L respectively. This was a one off sample not 24 hr. I was given no dietary advice and while they were initially prescribed Potassium Citrate this was subsequently stopped as one of the boys was having increased abdo pain. He had the abdo pain prior to commencement of PC but this was not addressed or investigated. The dietary advice in your article is wonderful. Both boys but more especially the boy with the higher urinary calcium level & abdo pain was craving salt, sugar meat, and to a lesser extent food items with bicarb(at least that’s why I think he sought out these foodstuffs). Recently cheese was being demanded more frequently. The salt & sugar cravings were alternating every 2 days or so but on occasions every few hours. He also complains of joint pain as well as head neck, back, eyes and thigh The other boy suffers badly with headaches and eye pain and to a much lesser extent knee pain. Can you throw any light on these extra symptoms? Also should they have a bone density scan? Serum calcium was checked and normal and I did point out that my understanding was that this was not adequate in confirming bone health which you have confirmed in your article.
Thank you
Sheila
Dear Sheila, I think it is very hard to diagnose hypercalciuria from just concentrations. A more common approach is to express the urine calcium concentration as a ratio to the urine creatinine concentration, the latter to allow for water conservation. Do they have crystals in their urine, or blood? A common cutpoint for hypercalciuria is a urine calcium /creatinine concentration ratio of above 140 mg calcium/gm creatinine. Try to determine if a creatinine level was measured and factor the urine calcium by that. Regards, Fred Coe
Dr Coe
Thank you for your prompt reply. One of them has microscopic amounts of blood regularly and what I describe as sediment. It looks like very fine salt. If the urine was in a sample bottle then the sediment would make up a quarter of the contents. I am not aware of any blood in the urine of the 2nd boy but his sediment appears to be finer, almost fluffy. One passes sediment most days while the other less frequently. I have noticed that 95%+ times the sediment settles but on some occasions it stays suspended. The Urine looks oily at times.
Sheila
Hi Sheila, what about the urine calcium/urine creatinine? The dense sediment may be crystals – your physician can look under the microscope and determine what they are. I would want to know. Regards, Fred
Are you thinking of casts Dr Coe?
No; the actual crystals should be easily visible under the microscope if it is crystals you are seeing in the urine. If they are crystals, it is important to collect some and have them analysed to determine their structure. A lot is unclear here: Do these children really have hypercalciuria; are these cloudy deposits crystals? What are the crystals? Since you have only spot urines not 24 hour urines, what are the supersaturations in those spot urines? Do they match the crystals? If so, if there are crystals and the urine supersaturations match them, then lowering the supersaturations that match the crystals will stop the crystals from forming and stave off stones. Regards, Fred Coe
I’ll get both tests done for both children as you suggested Dr Coe. Is it possible to misdiagnose IH? There was one 24 hr test done for one boy but I have no idea of the result. It was carried out during a hospital stay. Do you mind if I seek your opinion when I get the result
Dear Sheila, Please feel free to do so. Regards, Fred Coe
Hello Dr. Coe,
I have recently read that the mineral boron can help to facilitate the absorption of calcium and that it may be a good supplement for those who suffer from kidney stones. I was wondering if there has been any research on the effects of boron supplementation for kidney stone patients, especially those with IH. The information I read said that supplementation of 2 mg/day would be sufficient. I would appreciate your thoughts and insight on this topic.
Thank you,
Carla
Hi Carla, Boron has some possibilities but no trials. Here is a recent paper on it. So far the best source is food: From the article: ‘Many of
the foods that contain boron are likely to have beneficial
effects on bone, therefore it is suggested that foods such as
fruits, vegetables, and legumes be the source of boron.” Regards, Fred Coe
Dear Dr.Coe, Would eating less calcium in foods decrease the calcium in the urine??
Hi Sharon, If you have idiopathic hypercalciuria it might but at the expense of risk of bone mineral loss and possible fractures later in life. It is not a very good idea and should be avoided. Regards, Fred Coe
Is it possible that not eating enough calcium in foods could cause an increase in calcium in the urine. i was counting some greens as 135 mg of calcium when in actuality it was only 50mg. of calcium. Therefore I did not get my 1200 mg/day but only 1115mg. for several months.
Hi Sharon, No it is not that way. You have high urine calcium despite low calcium diet and just imagine where that calcium is coming from – bone. Please correct this and treat your hypercalciuria properly: High diet calcium, low diet sodium, moderate diet protein (PCR on your lab report about 1) and if needed thiazide. Regards, Fred Coe
What a wonderful discussion of IH. My wife is 67, has osteopenia, and apparently IH with U Ca at 561.6. U-Ca/U-Cr has been increasing from Feb 2014 at 0.281 to June 2016 at 0.432 – is this cause for alarm? She does not yet seem to have any kidney stone symptoms.
Hi Mac, you are very astute. She may have IH and bone disease is a very common outcome especially if diet calcium has not been optimal. She may be losing bone at a rapid rate because of menopause but it is a bit late in that process for such very high urine calcium levels. The rising rate of urine calcium could reflect new use of calcium supplements or high calcium diet, or rising diet sodium or some combination. Of crucial importance is control of diet sodium, which should be as low as possible; the ideal is 65 mEq or 1500 mg daily along with 1000 mg of calcium. Of course she may want to be on a primary bone directed medication, which is outside the scope of the site as presently constructed. Her physician should want to be sure her serum PTH is in the normal range – not suppressed – and her serum calcium is definitely normal. She might want a kidney stone protocol CT to be sure there are no stones. Regards, Fred Coe
Thank you very much! Her endocrinologist has ruled out common causes of hypercalcemia. She is currently on a regimen that I think is questionable – no calcium supplements, no yogurt, no multi-vitamins, no vitamin D supplement (Calciferol is down to 24.6). A few years ago, she was taking Fosamax but her dentist recommended against it due to bone loss in her jaw. Serum calcium is holding steady at 10.1-10.5. My impression is that her condition is probably deteriorating and that her current treatment is not working well.
Hi Mac, I do not think her serum calcium levels are normal; the values quoted are elevated. A hypercalcemic state would better account for her very high urine calcium levels than would idiopathic hypercalciuria. Her serum PTH values are very critical here. If they are suppressed below the normal range it is one class of disease, if they are normal or high primary hyperparathyroidism is the likely cause and can be cured by surgery. The key is definite high serum calcium with normal or high serum PTH values and – of course – the very high urine calcium levels, and exclusion of systemic diseases apart from primary hyperparathyroidism that might create this combination. The very low calcium intake is not ideal in any event. Perhaps you might want to mention these possibilities to your physicians for their opinions. To me the key is several fasting bloods for serum calcium, ionized calcium and PTH – all in the same samples – on at least several different days over a few weeks – I think I would personally do at least 3 in my own practice. If indeed primary hyperparathyroidism is present it is best treated by a surgeon with a lot of experience in parathyroid surgery – these people usually reside in medical school hospitals. Of course, all this is merely commenting from a distance, and is simply what your physicians might want to consider – they probably have already done so and have decided otherwise. Regards, Fred Coe
Thank you again Her “Intact Parathyroid Hormone” is 17 and has been as low as 10 and as high as 25 since 2013 – so, on the low side of the 12-88 range. Her “PTH Related Protein” is 14-16, on the low side of the 14-17 range. Her thyroid was damaged by radiation treatments as a child, and she takes Levothyroxin 112 mg – so perhaps her parathyroid was also damaged? I agree that “The very low calcium intake is not ideal in any event” – it seems like a particularly bad idea with osteoporosis. Her endocrinologist wants to solve the mystery of the hypercalemia before addressing bone density, but I fear that additional damage is being done meanwhile.
Mac, I understand. High serum calcium with suppressed serum PTH is a very serious problem and needs resolution. Your physician is obviously thoughtful. If an answer is not forthcoming I am sure he would want referral to a university center that specializes in mineral disorders and is geographically convenient to your family. Regards Fred Coe
Dr. Choe,
My Citric Acid is 26, I’ve taken Urocit-K 15 twice a day for three months but my Citric Acid level is still low at 57. That’s from last week’s 24 hour urine test.
The Aston Center in Dallas, Texas doesn’t accept HMO BlueCross right now. I have been accepted as a patient. When they enroll I will see them. I living in a small town in North Texas, I’m 38 years old, local Urology/Nephrology is managing my kidney stones but prevention is not going anywhere.
Is there anything I can do? Am I loosing citric acid somewhere? I’ve read online articles about bowel disorders/renal tubular acidosis.
Thank You,
Bryan
Hi Bryan, You do indeed have a low urine citrate, but what is the context. Take a look at a way to think about your stone prevention and see where you might fit in. The low urine citrate could be from renal tubular acidosis, bowel disease, potassium deficiency, a host of causes. Regards, Fred Coe
Dr. Coe, sorry for misspelling your name in my previous post.
Does potassium citrate lower urine PH?
My Uric Acid was high in my last 24 hour urine.
Protein was high, that seems to change from time to time.
Thank You
I found the answer in your links. Pot Cit raises Urine PH.
Only thing I’m stuck on….if citrate is absorbed by the bowel will taking potassium citrate increase citrate level? Sounds like putting motor oil into a vehicle with a hole in the pan.
Hi Bryan, This is in reply to both comments. Citrate is metabolized as citric acid, so a proton is taken up from blood with every molecule used metabolically. For this reason, potassium citrate will produce bicarbonate in the blood as the liver metabolizes it and that bicarbonate will cause the kidneys to raise urine pH and – through the citrate transporter – reduce reabsorption of filtered citrate so urine citrate rises. Regards, Fred Coe
Hello Dr. Coe,
I’ve been reading your articles since May when I had a 2.6 cm calcium phosphate stone removed (PCNL surgery). Diagnosis is IH. Recommended preventive treatment would have been chlorthalidone, but I have a sulfa allergy. I am 48 yr. old female, 5′ 5″, 120 lbs. and had a hysterectomy last September. No prior stone history, no family history of stones. I think there is a connection with hypercalciuria and low bone density or risk for osteoporosis. What about acidic diet or conditions in the body that would cause calcium to be pulled from the bones to correct and balance the blood calcium level and PH levels? Could this action be one cause of excess calcium in the urine? I am still searching for a plan to prevent future stones and have read several studies about Vitamin K, K2 (mk4 and mk7), potassium (citrate and bicarbonate), and magnesium along with low sodium, low protein diets. What has been your experience if you had an IH patient with a sulfa allergy – can prevention be achieved without thiazide diurectics?
Thank you.
Hi Kris, Your questions are very sophisticated, and the right ones. If you cannot use a thiazide, low sodium diet at about 1500 mg/day is a perfect start. Achieve that, retest to be sure you did it, and see what happened to urine calcium. Diet protein does raise urine calcium – I never finished that article! – but is protective of bone whereas diet sodium raises urine calcium and can deplete bone of mineral. If high fluids and low sodium do not lower SS CaP below 1 and lower urine calcium to below 200 mg or lower then the next step might be a modest intake of potassium citrate – perhaps 10 mEq one daily. Obviously this could raise urine pH and CaP SS if it does not lower urine calcium further, so one needs to check again. But I would do the sodium first with 3 liters of water intake or so to achieve a urine volume around 2.5 liters daily – steady throughout the day. I think you have already read all this- from your questions, but if you have not this is a good summary with links. Regards, Fred Coe
Thank you!
Hello Dr. Coe, now a blood test from last week shows serum calcium has increased to 10.4. PTH is 32. My doctor wants to schedule a scan for parathyroid. Is there anything else I should consider?
Thank you.
Hi Kris, The diagnosis of primary hyperparathyroidism relies on this: high fasting serum calcium values and PTH values not suppressed and high – or rarely – normal but not low urine calcium levels. Be sure all are present. A parathyroid scan is useful in planning surgery but is not a real test for the disease having too wide a false positive and false negative range. Be cause multiple fasting serum calcium levels are indeed high and that the PTH measurements are in the same serum as those fasting calciums. Regards, Fred Coe
Hi Dr. Coe,
My latest fasting blood test has ionized calcium 5.4, PTH 22, and serum calcium 9.8. I don’t know if this is still trending towards parathyroid concerns or too soon to tell. Thank you.
The serum calcium and PTH do not point to primary hyperparathyroidism. Regards, Fred Coe
For 15 years I have been walking around with 6 small passable stones. Now for the last 4 years I am making them so big so quick that by the time my Dr and I realize I have a stone too big it is too late. Every year for 4 years once every summer (always) I need surgery. The basket seems to work best with me.
The last two times I have become spetic. I stayed in hospital for 4 days 2 in intensive care.
The first year I tried just not eating high oxalates. Next year I added low protein low fat. Next year I went vegan (I made 3 stone two In one kidney two in the other Dr went and got them all at one time. After that I was upset and ate like I wanted to. Big mistake I had a 2cm in Feb by may it was 7. That is the one that almost killed me.
So my Dr has me on a low sodium, fat, protein, and oxalates. He wants me to eat a yogurt a day, taking a probontic pill, 3 cranberry pills, drink a gal water.
So I have a read so much on the internet and like what UC drs. Can you tell me how much protein, and sugar I need. I am doing 1000g of calcium, 3000g of salt and under 30g of fat. I have completely taken sugar out. I am drinking a cup of 1percent milk with every meal.
It scares me now that I have been sepis now. They say the next time will be 50percent chance of doing it again. Is that right?
Doing the above for a month when I went to my Dr this week I had a bladder infection. Ugh!!!
My calcium level is 9.2. The blood work shows cal. in urine was OK.
I am breaking bones too now.
Two times last year. Elbow three breaks and my upper arm three breaks. My husband has almost house arrested me.
Any thing you can tell me will be very appreciated. I am at my last straws.
Jeannie Big Stone Maker
Hi Jeannie, I guess so much is missing I need to ask. What are your stones made of? What are your 24 hour urine chemistries? From the course of things I would guess the stones are calcium phosphate and your urine calcium is high and that is why you have bone trouble, but that is really guessing. Let me know more and I will try to be more useful. Here is a good pattern to work off of. Regards, Fred Coe
Hi Dr. Coe,
I am really enjoying your articles on IH as I am a mathematics professor and like to know how things work. You use very helpful analogies and do an excellent job of explaining complicated concepts. I have extreme IH with an initial 24 hr urine calcium excretion level of 597mg in 2011. With dietary modification, chlorthalidone, and potassium citrate I was able to lower my levels to about 250-300mg on subsequent collections. No new stones after initially having 6 just before the first urine test. You are absolutely correct in saying that a stone patient is a bone patient. A bone density scan in 2011 showed I had osteoporosis in the lumbar spine at the age of 47. Fortunately the current interventions appear to have produced a positive calcium balance as my follow up scan in 2014 showed about a 6% increase in bone density. I had earlier stones in my 30’s and a family history of stones but the urologist I saw then never requested a 24 hr urine collection. A more proactive stance then could have avoided this bone loss completely. You discussed that calcium excretion increases with increased filtration. GFR decreases as we age. Does this mean that IH individuals could excrete less calcium as they age possibly improving calcium balance? I see myself as being very fortunate that my current treatment has worked so well, considering how extreme my initial calcium loss was, and wonder if the current interventions will continue to work. If not, are there still additional tools left? I have read that neutral phosphates can also reduce urine calcium even further in conjunction with thiazide type diuretics, but I am under the impression that they are not used very much. Bisphosphonates are not an attractive potential option to me.
Thank you again for your article!
Hi Dan, I am honored that a mathematician would approve. My early career dreams were in mathematical biology but alas I lacked the holy fire for such adventure. Urine calcium does fall with falling filtration and I think that is because calcium reabsorption along the tubule can only fall so much on a percentage basis. In the proximal tubule it is reabsorbed mostly in a passive manner along with sodium and water, and as the kidneys lose filtration fractional reabsorption falls from about 20% to perhaps 40%. But that fall is just enough to balance the loss of filtration. The next segment reabsorbs calcium electrogenically and that cannot be regulated down very much. Phosphate is just the other way. Tubule reabsorption can fall enough that urine phosphate remains constant as filtration falls. As for neutral phosphate, its effects on bone are not well explored in humans. Bisphosphonates do prevent fractures in female osteoporosis but have not much trial data in IH. Warm Regards, Fred Coe
Thank you very much for this nice information about IH, I have question about children with IH, is there any other treatment or not?
Dear Dr Ali, IH in children is like in adults. If stones are forming low sodium high calcium diet is ideal and a low dose of a thiazide like drug if more than diet is required. It is inherited so screening of siblings for hematuria or crystals is wise. Children have low urine volumes so control of diet sodium is very valuable. Regards, Fred Coe
Hello Dr. Coe –
I appreciate all of the data you share. I do have 2 quick questions.
2011 had surgery to remove parathyroid tumor found after 1st kidney stone.
5 years have passed and symptoms have come back, multiple kidney stones, large weight gain and generally feeling terrible.
Recent Parathyroid Hormone Intact test result normal at 41 and blood calcium 9.3.
Dr ordered 24 hour stone formation test, results are as follows:
Calcium Urine: 339 mg/day
Oxalate Urine: 46 mg/day
Uric Acid Urine: 617 mg/day
Citrate Urine: 544 mg/day
pH Urine: 6.8
Total Urine Volume: 1.62 L/day
Sodium Urine: 131 mEq/day
Sulfate Urine: 19 mmol/day
Phosphorus Urine: 744 mg/day
Magnesium Urine: 148 mg/day
Ammonium Urine: 26 mEq/day
Potassium Urine: 69 mEq/day
Creatinine Urine: 1311 mg/day
Calcium Oxalate: 3.71
Brushite: 5.85
Sodium Urate: 2.54
Struvite: 9.36
Uric Acid: 0.30
Do I need to be concerned about Brushite level
and
Can I assume that I am IH?
Thanks for your time!
Hi Suzanne, You have a normal serum calcium and a high urine calcium so it is IH but we have described – so have other groups – hypercalciuria after cure of primary hyperparathyroidism and are not sure if it is IH or something like IH. In either case treatment is the same, and I would advise it – low sodium diet, avoidance of high sugar loads, a normal protein intake, high fluids, and if all else fails, some medication. Here is a recent article that outlines all treatments. You may indeed be forming calcium phosphate stones, but even so treatment is much the same. Regards, Fred Coe
I am 54 years old with severe osteoporosis ( – 3.9 hips and – 2.9 spine) and long history of kidney stones (since I was 15), mainly calcium oxalate.
All my tests, including 24 hour urine calcium tests shows normal results. Should I repeat the urine 24 hour test?
Hi Elaine, Normal is a metaphor in urine studies. I would suspect you have a higher than not urine calcium and perhaps a low calcium diet, but without information I cannot be sure. Genetic hypercalciuria masked by low calcium diet is a pathway to bone disease like yours. Alternatives abound, so it this is not correct you need more detailed evaluation. It is important to figure out what is wrong and fix it. Regards, Fred Coe
Hi Dr. Coe,
New copy without all the autocorrect errors!
This is a great site and it has been very helpful in trying to figure out my issues. I am curious if idiopathic hypercalcuria causes any symptoms such as polyuria, polydipsia and nocturia? I can’t find these associated with IH in any articles.
My initial concerns which got me into my endocrinologist was a worsening of nocturia, polyuria and polydipsia. 4.5-6.5 liters per day. I am a 48 yo female and these symptoms have gone on for 10 years but have been increasing the last 2- years, interfering with sleep and daytime routines. And extreme fatigue (I am not overweight and very active, run 3-5 mi, but has become very hard to keep up) I have no history of kidney stones.
My initial labs:
Spot urine osmol 158mos/kg (300-900)
Spot serum osmolality 289mos/kg (280-300)
Ferritin 16 ng/ml (6-264)
Vitamin D 32ng/ml (30-80)
PTH intact 68 pg/ml (8-54)
Calcium, PTH 9.1 mg/dl (8.4-10.6)
Arginine vasopressin <1 pg/ml (1-13.3)
Overnight water fast 14 hrs: Urine osmolality 750 mos/kg (300-900)
24 hour Urine volume 4600ml
24 hour Urine calcium 432.3 mg/24hr (100-300)
Serum calcium 9.4 mg/dl (8.4-10.6)
24 hour creatinine 1584 mg/24hr (800-1800)
Serum creatinine .77 mg/dl (.52-1.04)
I was placed on 2.5mg of indapimide for four weeks and repeat labs:
Urine calcium, random 7.7 mg/dl (?)
Serum calcium increased to 10.1 mg/dl (8.4-10.6)
Urine creatinine, random 29.93 mg/dl (?)
Serum creatinine, random .7 mg/dl (.52-1.04)
I have other labs too but thought these most pertinent. It seems like my calcium/creatinine ratio .22 and .18 indicate PHPT and my serum calcium is increasing on the indapamide which does occasionally unmask PHPT from my reading. I am still not convinced I don't have an ADH problem or partial diabetes insipidus, nephrogenic or central, due to the nocturia (2-3 per night with up to 800ml). I also thought it could be hyperaldosteronism. My endocrinologist initial thoughts were IH and I have yet to see him after I started on indapimide and my calcium went up. But perhaps just IH?
Family hx: dad had kidney stones and parathyroids removed. Also an adrenal tumor.
Grandma with thyroid issues, HTN- unable to lower with meds and ultimately dialysis.
Thank for any insight or information especially on the symptoms you have seen in your patients with IH if this could be likely for me.
You have provided a wealth of knowledge here. Thank you again.
Hi Robin, You do seem to have idiopathic hypercalciuria given the high urine calcium, normal serum calcium, and lack of obvious systemic diseases. There are indeed some cases of IH with nocturia, noted especially in children, and ascribed [ without complete data – to activation of the calcium receptor in the renal collecting ducts with reduction of aquaporin insertion. The proper way to treat IH is with marked diet sodium reduction to 1500 mg – the present healthy people ideal – and see how far down the urine calcium comes with just that one measure. It may fall a lot. Indapamide is fine on top of this low sodium intake. Nocturia is a special problem because urine calcium overnight stays up in IH – we published that – and thiazide does not reliably lower it. The low sodium may well do so. Potassium citrate may do better with it. So, first achieve the low sodium diet and see what happens. Use the 24 hour urine sodium as a measure of diet intake – it is very close. Regards, Fred Coe
Thank you I am going to lower my salt and see what happens. The polyuria/nocturia drives me nuts but has maybe kept me from getting stones. My brother and dad have them.
Regards,
Robin
Dr. Coe, I’ve done 24 hr urine test 7 times, my average Ca 24 is 402. Leading up to the most recent test I was on 12.5mg of thiazide once a day along with an effort to reduce sodium and protein. Results from the recent test was 380 vs 480 on the prior test. Urine sodium levels showed improvement. I have a renewed desire to solve this because I’m more concerned about bone disease than I am stones. My first DXA 4 years ago showed osteopenia in one forearm. I have my 2nd scan on Monday. I’ve recently been on 25mg of chlorthalidone along with a renewed effort to lower dietary sodium and protein but a side effect I’m having is ED. I tried to go 12.5mg once a day but same side effect. So my main question: Is it likely that I can get the urine calcium down to reasonable levels with ONLY a very strict low sodium and low protein diet or from your experience will that be very difficult to obtain without a thiazide type drug? I see two options right now — go without medication and go very strict on diet OR go with the chlorthalidone, along with stricter diet, AND adding one more medication for the ED, something I REALLY don’t want to do if I don’t have to. I guess I’m just looking for a reality check in this regard. Could I get your thoughts? Also, is 400+ average Ca 24 typical for idiopathic hypercalcuria or is that off the charts? Seems to me to be very high to me. I’ve had the thyroid checked, etc. and a cause has not been identified. Thank you again. Best to you, Robert
Hi Robert, You do indeed have a high urine calcium and unless there is a systemic disease as cause – this is something your physician must determine – it is idiopathic hypercalciuria. As you note, IH can cause bone disease. If you want to avoid thiazide sodium intake needs to be low indeed – there are no trials, so I am just guessing in what I hope is an informed way. About 1000 to 1500 mg would be needed along with high diet calcium. In the one decent study it took this kind of sodium and calcium to bring bone mineral balance to neutral in postmenopausal women with bone disease. Diet protein raises urine calcium but whether it lowers bone mineral is a vexed question; low protein below 0.8 gm/kg/day is not advisable. If bone does not stabilize you may have to consider a bone directed medication. Regards, Fred Coe
Dear Dr. Coe,
Greetings from Macedonia!
During my research on the internet about my daughters condition, I came across your name and your article about IH and decided to contact you.
My 9 years old daughter has been struggling with urinary tract infections with E. Coli since she was 2 years old.
Not long ago, after a really bad infection during a routine screening, the doctors discovered that she has hypercalciuria (calcium deposits around her kidneys) and very high level of calcium in her 24h urine – 4.65 mgr, but could not discover any underlying cause of the condition. Her parathyroid hormone was in a normal level (28.2) as well as the vitamin D.
Around her kidneys there are calcifications. Besides taking pottasium citrate of 90 mmol per day and reduction of natrium and protein, the doctors here in Macedonia did not give her any other therapy.
As im very concerned about her health, I would like to consult with you about her condition.
I would be very thankful if you give me your thoughts on how to prevent stone formations, any diet plans or maybe recommendations for medications.
Thank you very much in advance.
Hi Anika, Her high urine calcium is probably hereditary – that is the usual reason, and I gather there are calcium deposits in her kidneys. Protein intake does not need to be below normal just in the range of 0.8-1 gm/kg/day. Very low diet sodium, 50 – 60 mEq (around 1400 mg) will lower urine calcium. High fluids are crucial. Given many stones, perhaps after low sodium diet is in place a very low dose of thiazide drug would be helpful – chlorthalidone 12.5 mg or indapamide 1.25 mg. The dose of potassium citrate seems too high, 40 mEq/day should be enough. You do not mention the stone analysis – that should be done. Regards, Fred Coe
Hi Al, If sodium in the urine is about 1500 mg or less and urine calcium remains high then the hypercalciuria needs additional treatment. Protein intakes about 1 gm/kg/day could raise it. There might be other reasons, too. Idiopathic hypercalciuria is genetic but not one thing – there are various versions, some seem less sodium responsive although we have yet to study this matter properly. Regards, Fred Coe
Hello,
Since this infection is known to cause kidney stones and is often undiagnosed/misdiagnosed in immunocompetent people, how often do you think it can be the cause of kidney stones?
This infection would explain a case of Progressive encephalitis with rigidity and myoclonus after a “cold,” as well as why Takayasu Arteritis, Takotsubo Cardiomyopathy, and some “autoimmune” diseases usually follow other minor infection, like respiratory tract infections and gastroenteritis, which this infection also causes, mimicking colds, flus, pneumonia, and causing GI problems, etc. Do you think Postural orthostatic tachycardia syndrome, which often occurs after a viral infection, could be caused by it?
My coworkers and I, all immunocompetent, got Disseminated Histoplasmosis in Dallas-Fort Worth from roosting bats, that shed the fungus in their feces. The doctors said we couldn’t possibly have it, since we all had intact immune systems. The doctors were wrong.
More than 100 outbreaks have occurred in the U.S. since 1938, and those are just the ones that were figured out, since people go to different doctors. One outbreak was over 100,000 victims in Indianapolis.
This pathogen causes many idiopathic diseases and conditions, including hematological malignancies, autoimmune symptoms, myelitis, myositis, vasculitis. etc. It causes hypervascularization, calcifications, sclerosis, fibrosis, necrosis, leukopenia, anemia, neutrophilia, pancytopenia, thrombocytopenia, hypoglycemia, polyps, stenosis, and perforations, inflammation of various organs, GI problems, hepatitis, etc.
It at least “mimics” autoimmune diseases, cancer, mental illness, migraines, seizures, etc. It’s known to cause rheumatological conditions, inflammation, and precancerous conditions. It causes hematological malignancies, and some doctors claim their leukemia patients go into remission when given antifungal. My friend in another state who died from lupus lived across the street from a bat colony. An acquaintance with alopecia universalis and whose mother had degenerative brain disorder has bat houses on their property. It’s known to cause delusions, wild mood swings, and hallucinations.
Just one disease of unknown cause that could be caused by Disseminated Histoplasmposis: I suspect, based on my and my coworker’s symptoms (during our “rare” infectious disease outbreak) and my research, that interstitial cystitis and its comorbid conditions can be caused by disseminated histoplasmosis, which causes inflammation throughout the body, causes “autoimmune” symptoms, and is not as rare as believed. I read that “interstitial cystitis (IC) is a chronic inflammatory condition of the submucosal and muscular layers of the bladder, and the cause is currently unknown. Some people with IC have been diagnosed with other conditions such as irritable bowel syndrome (IBS), fibromyalgia, chronic fatigue syndrome, allergies, Sjogren’s syndrome, which raises the possibility that interstitial cystitis may be caused by mechanisms that cause these other conditions. In addition, men with IC are frequently diagnosed as having chronic nonbacterial prostatitis, and there is an extensive overlap of symptoms and treatment between the two conditions, leading researchers to posit that the conditions may share the same etiology and pathology.”
I believe the “side effects” of Haldol (leukopenia and MS symptoms) are not side effects but just more symptoms of Disseminated Histoplasmosis, since it causes leukopenia and MS symptoms. What about the unknown reason why beta blockers cause tardive dyskinesia? The tinnitus, photophobia, psychosis “caused” by Cipro? The hypersexuality and leukemia “caused” by Abilify? The fungus is an Oxygenale and therefore consumes collagen. Fungal hyphae carry an electrical charge and align under a current. It’s most potent in female lactating bats, because the fungus likes sugar (lactose) and nitrogen (amino acids, protein). What about female lactating humans…postpartum psychosis? The bats give birth late spring/summer, and I noticed suicide rates spike in late spring/early summer. A map of mental distress and some diseases appear to almost perfectly overlay a map of Histoplasmosis. The bats eat moths, which are attracted to blue and white city lights.
Apparently, even the CDC didn’t know bats CARRY it and shed it in their feces, although they knew it could grow in bird and bat feces. Researchers claim the subacute type is more common than believed. It is known to at least mimic autoimmune diseases and cancer, and known to give false-positives in PET scans. But no one diagnosed with an autoimmune disease or cancer is screened for it. In fact, at least one NIH paper states explicitly that all patients diagnosed with sarcoidosis be tested for it, but most, if not all, are not. 80-90+% of people in some areas have been infected. It can lay dormant for up to 40 years in the lungs and/or adrenals. It causes RNA/DNA damage. Other doctors are claiming things like sarcoidosis IS disseminated histoplasmosis.
My coworkers and I had GI problems, liver problems, weird rashes, plantar fasciitis, etc., and I had swollen lymph nodes, hives, lesions, and started getting migraines and plantar fasciitis in the building, and haven’t had them since I left. It gave me temporary fecal incontinence, seizures, dark blood from my intestines, and benign paroxysmal positional vertigo. I had symptoms of several autoimmune diseases, including Fibromyalgia, Sarcoidosis, ALS, MS, etc. that have disappeared since leaving the area and taking Itraconazole antifungal.
No one, including doctors, could figure out what was wrong with us, and I was being killed by my doctor, who mistakenly refused to believe I had it and gave me Prednisone (at least 2 years after I already had Disseminated Histoplasmosis) after a positive ANA titer, until I miraculously remembered that a visiting man once told my elementary school class that bats CARRY histoplasmosis….so much of it that they evolved to deal with the photophobia and tinnitus it causes by hunting at night by echolocation. There’s a lot more. I wrote a book about my experience with Disseminated Histoplasmosis called “Batsh#t Crazy,” because bats shed the fungus in their feces and it causes delusions and hallucinations, I suspect by the sclerotia it can form emitting hallucinogens, along with inflammation in the CNS.
Hi SUsan, I have no knowledge about this fungus as a cause of stones. But I have left your detailed comment on the site in case others know more than I do about the matter. I do want to make clear to others who read your work that your comments are meant to promote debate and do not represent established medical science to date. I am not trained in or expert concerning fungal diseases. Fred Coe
Dear Dr. Coe,
I am a 63 year old male with Parkinson’s Disease and MCI. My first stone was discovered back in the mid 1990’s and required Lipotripsy and about 9 months to pass. No problems or other evidence of stones until an CT scan discovered three stones in the same kidney on August of 2014. Less than 2 weeks later I received the Parkinson’s Disease diagnosis. In March of 2017, after three visits to ER in less than a week for pain, I had a Cystoscopy with Laser Lithotrypsy performed with Ureter stent installation to remove “a train of stones” that had passed into the ureter. Stones were made of Calcium Oxalate. Two stones still remain in the kidney.
The PD diagnosis (with mild cognitive impairment) prompted some major lifestyle changes: I retired and began a daily, vigorous, cardio regimen for 30-40 minutes a day on a stationary bicycle as well as hiking local mountains several times per week. I became Keto adapted to control a (pre) diabetic condition and because there was empirical evidence which suggested that a high fat, extremely low carbohydrate diet could be effective in delaying or minimizing the onset of worsening PD symptoms. As a result of this diet I have lost 30 pounds and am still not medicated for the PD or type 2 diabetes. I firmly believe that the diet is, at the very least, partially responsible for these results and recent evidence suggests (although this still needs to be studied in trials) that an increase in Uric Acid levels appears to be Neuroprotective and at least partially responsible for delaying the onset and worsening of symptoms in PD. The primary way I get my calories and necessary fats, while severely restricting carb intake, is by eating a daily diet of mostly green, raw, leafy, veggies with a serving of either chicken, beef or fish…a great combination for producing stones while promoting high Uric acid levels!
I have had three 24 hour urine tests performed since the surgery and have been forced to make some changes to the diet as a result of these tests including: drinking more water (2 litres) daily, eliminating certain super high Oxalate veggies, and reducing the servings of red meat in favor of chicken and fish. Unfortunately, the changes to diet have not been adequate and my doctor has prescribed Hydrochlorothiazide 25mg daily to help prevent stone formation.
Although I have no doubt that this med will help reduce the formation of stones by reducing calcium super saturation, I have serious concerns that there may be a backlash from the loss of the salt and other electrolytes that could impact my cardio workouts and promote an increase in muscle cramping, spasms and rigidity. Additionally, I have Orthostatic Hypotension (common with PD) and exercised induced HBP which requires 25mg Atenolol daily for control. Adding another drug (the thiazide) that also lowers BP seems dangerous to me given my circumstances.
How at risk for further formation of stones am I without adding the Thiazide to my regimen? The most recent 24 hour Calcium Filtration Rate was at 277mg/day (standard range for lab is <250 mg/day). No other values were out of range!
Last question: What exactly does splitting the Thiazide dosage in 1/2 and taking it twice daily (as opposed to full strength 1xd) accomplish?
My Urologist seems to be bent on Thiazide to fix this and I have my doubts and concerns which I have expressed to him but I have not been given any alternatives.
Thanks for your great articles on the interweb!
Charles Leblow
Hi Charles, Your urine calcium is high, and to me the safer plan might be low sodium diet. It will do a lot of what thiazide does with less risk given your complex medical setting. Low sodium intake works differently from thiazide in that kidney sodium regulation remains normal whereas thiazide disrupts sodium handling and makes for a more brittle blood pressure physiology. Ask your physician. Here is a plan based on diet but with thiazide as a kind of add on when there is residual supersaturation. See what he/she thinks. Regards, Fred Coe
Hi Dr Coe, I have hypercalciuria, along with osteoporosis and NAFLD. A couple years ago I was diagnosed with low T, low vitamin D and low iron. The deficiencies have been corrected and my osteoporosis score has improved tremendously. As for my urine calcium, it has barely budged despite being treated with both HCTZ and amiloride. What do you think? Recently, I read that a vitamin K deficiency can cause hypercalciuria. Have you heard of that possibility? Thank you.
Hi Ken, I gather your serum calcium is normal and PTH not suppressed – so it is indeed IH. When thiazides fail, urine sodium is my target; have you brought it down to below 65 mEq (1500 mg) daily? Likewise I prefer chlorthalidone 12.5 or 25 mg daily or indapamide to OHCTZ as being long acting. Finally, keep protein to 0.8-1 gm/kg/day and get away from sugar loads. Your fatty liver makes me think of sugar excess as fructose in refined sugar is notorious. Vitamin K seems far off vs. these alternatives. Regards, Fred Coe
Hi Dr. Coe,
Could you possibly help me better understand two particular subtypes of IH: AH type I and AH type II specifically with bone hyperresorption, *not* renal leak? (Possibly rare, but I strongly suspect my Dad, e.g., had the first.)
I have observed that these two related subtypes seem to be particularly problematic to treat because Chlorthalidone and reduced sodium may only have the effect they would on a normal. And even 1000 mg of Ca from food may not stop bone loss, but due to hyperabsorption, drive stone production more than normal.
I see Heller H.J., et al. (2007) “Reduced bone formation and relatively increased bone resorption in absorptive hypercalciuria” followed Bushinski’s rat studies featuring Alendronate with a (very) small, short-term human trial for AH-1, with results that seem to invite further study.
Can you please tell me, have you or your colleagues tried bisphosonates? And what kinds of dietary and other recommendations in general might you have for anyone with these two subtypes when the tried and true measures are insufficient? Thank you and best regards, Al
Hi Al, the subtypes do not exist. They were a useful strategy decades ago and no one uses them now. Dr Heller was part of the Dallas group that proposed the AH RH ideas. Dr Bushinsky’s rat studies are known to me as I have been his friend for decades and played a role in his founding of the colony and many of the early papers. Not relevant to AH of RH. You are a thoughtful person, but these are deep waters and you will not be able to fathom them details – not being fancy, just realistic. Many physicians have trouble here. The correct approach to all idiopathic hypercalciuria is low sodium high calcium diet, low refined sugar, and moderate protein. Diuretics are to be used on top of the diet. Regards, Fred
Hello Dr. Coe,
I was told that other things can cause kidney stone history beside parathyroid disease, is this true? Could you please give me any feedback on this doctor in wis. on kidney and vitamin D? Thank you. https://www.youtube.com/watch?v=yaEYwfzpbA4
Sincerely Annette McNamara
Hi Annette, Most stones are caused by other than hyperparathyroidism. Here is my best efforts at a go around about all stones. The doctor is talking about the narrow few with that disease. Here is an article on it from here. If you have stones, there is a pretty good pathway to cause and prevention. See if the article on confusion does it for you. If not, come back and I will select another. PHPT is sort of the end of the game for about 5% of calcium stone formers; that leaves 95% of calcium stone formers with something else, and there are other kinds of stones. Regards, Fred Coe
Dear Dr Coe,
I am a 53 year old male who was diagnosed with severe osteoporosis after suffering a lumbar compression fracture in the absence of significant trauma. Follow up blood work could find none of the typical causes associated with male osteoporosis. Twenty four hour urine collection showed somewhat elevated calcium urine levels.
My serum calcium levels have always been normal. My Vitamin D levels were borderline low normal but have since increased to a more ideal level. Im currently on Prolia for the osteoporosis which so far hasn’t significantly increased my lumber spine bone density. Im concerned about the severity of my bone disease at such a young age. The doctors have concluded that my osteoporosis is likely caused by IH. I did a follow up 24 hour urine collection after a course of Thiazide medication with no improvement in the urine calcium levels. The levels actually went up slightly. I have had no kidney stone formations as of this point in time.
Im hoping you could shed some light on whether you think my case seems like IH. I was told by one of the physicians that the prolia therapy may fail for me without improvement of the IH. Im a Canadian dentist who wouldn’t be opposed to travelling to the US for a more in-depth assessment of my situation. If you could recommend a specialist or clinic that specializes in male osteoporosis it would be much appreciated. I wonder if there is genetic testing that could definitively give me a diagnosis of IH. I appreciate any insight you may have regarding my case and any suggestions you may have.
Thanks , Scott
Hi Dr Macpherson, Idiopathic hypercalciuria is indeed a cause – in some patients – of early onset and marked bone mineral loss. Genetic testing is not as yet available except for rather rare versions of it – hypophosphatemic and hypomagnesemic forms. I presume you have normal serum PTH and elevated serum 1,25D, typical findings in IH. The bone disease of IH has sometimes been of the low turnover variety, so blocking osteoclasts may not give vibrant outcomes. You do not mention your family – presumably some other members have bone disease or stones, and no doubt about 1/2 of your immediate relatives are hypercalciuria. I can offer to see you myself clinically. As a courtesy I would be willing to just look at your records. Without a lot more detail, I cannot say much more. Regards, Fred Coe
Hi Dr Coe,
My diagnosis of IH is by exclusion of any other definitive measurable cause. Im trying to determine the cause of my bone disease in the hope that can improve my outcome. My PTH has always been normal . My vitamin D levels were slightly low at initial diagnosis but have since come up to normal levels with supplementation. None of my siblings or parents have been diagnosed with bone disease or stones.
I’m curious is there any unusual dietary causes that could explain or have been linked to high calcium urine excretion? Diet colas, aspartame etc ?
I was taking the medication Nexium for acid reflux for a few years prior to diagnosis. Ive discontinued this medication. Ive read that Nexium has been found to affect absorption of minerals and has been linked to bone density issues.
I may take you up on your offer of assistance. A phone conversation seems like an appropriate first step.
Im just trying to determine if I fit the typical description of IH since that has been surmised to be the likely cause of my bone disease. Im also concerned about my two daughters if there is a possible genetic connection.
I believe you have my email so feel free to message me directly that way.
Thanks Again,
Scott Macpherson
Hi Scott, I understand you have a lot of detailed issues, and they are indeed correct. My institution – U Chicago – does not as yet support formal telemedicine, so I cannot practice via that obvious and important channel. All I can do is offer to read your records and offer comments to your physicians – and you – but not by way of practicing medicine. That latter has special elements that my university needs to supervise. In general idiopathic hypercalciuria bone disease has been strongly familial, and it is often odd as in your case. Nexium is well known as an extra problem. Often we need to moderate the hypercalciuria and also use bone active medications as well. I am sorry I cannot do more at a distance, Regards, Fred Coe
I am a stone former. My kidneys are loaded with tiny stones. I have known about this for two years. I am a women and 69 and had three other larger stones, which I passed in 2015. I have been round and round with nephrology and endocrinologist to get a final diagnosis, to no avail. I have had four PTH tests which were 77, 66, 38,and 83 over the last six months. I have had two 24 hr urine tests. One in August of 2017 and one in November. Urine calcium was 247, and 171. Urine citrate was 645 then 300. SSCaP 1.60 and .52. Ph 6.963 and 6.398. I read your articles on IH and went on a low salt and increased my water diet in the second 24 hr test. Water vol was 2.50 and 3.80 perspectivly. My serium calcium is 9.3 always. I had my iodized cal and vit d done. 4.9 and 43.. my nephrologist and endo believe I have normocalcemic hyperparathyroidism. I visited Dr Norman at the parathyroid center in Tampa, in Sept of 2017 and they said no that my Pth wasn’t high enough. My nephrologist still insists that I have it. Don’t know what to do and am still not being treated in any way except for diet I initiated. This keeps me free from stone pain. I don’t know what kind of stone I make. I just had a bladder and kidney ultrasound but don’t have the results. Appreciate any insight.
Thank you,
Carol
Forgot to tell you that I also have osteoporosis.
Thanks
Hi Carol, your diet calcium may indeed be low, as with idiopathic hypercalciuria such a diet will cause a lot of bone disease. More and more it looks like you need much more diet calcium and perhaps more vitamin D – at least checked. Regards, Fred Coe
Hi Carol, I gather your blood calcium is always normal, your serum PTH values are high, and urine calcium variable. This is indeed secondary hyperparathyroidism. That urine calcium went down with reduced sodium is good – a part of stone prevention. Causes of high PTH with normal serum calcium include a low calcium diet, and the modest reduction of kidney function found in older ages. Perhaps your eGFR is a bit reduced. You do not mention your serum 25 vitamin D, perhaps it is not optimal. By no means even consider surgery. If you have reduced your salt intake and your urine calcium fell, and you continue to produce stones, a low dose of chlorthalidone is not inappropriate provided your physicians concur. It will lower your PTH, too. So, I think you have already begun some treatment, and if stone pain returns the CTD would be a next step. Regards, Fred Coe
Yes, my blood calcium is always normal. My serum 25 vit D is 43. Should I be concerned about the urine citrate being low (went from 645 to 300) in the second 24 hr test and my sscap is not high. The endocrinologist wants me to take Actinel for the osteoporosis…is that a good idea? How much calcium and Vitamin D?
Thank you so much for taking the time to clarify my confusion. It has been a year of ups and downs. I appreciate this sight and your time.
Carol
You seem pretty sure that I gave secondary hyperparathyroidism. Is this because my urine calcium is always normal, PTH is high, but why was it 38 in one testing? And my 24 hr urine is variable and affected by low salt and high fluid. Does this mean my prarthyroid glands are most likely enlarged? Will I eventually have kidney failure.
Hi Carol, My main point is that you do not have surgically amenable hyperparathyroidism. Any increase in serum PTH will be secondary to: low calcium diet, reduced kidney function with age; low vitamin D; or some combine of these. Low sodium diet regularly reduces urine calcium, and we know how that occurs via the kidneys. High diet calcium and low diet sodium are an ideal way to gradually reduce serum PTH. Likewise they are good steps for stone prevention – not your issue – and for bone mineral preservation – everyone’s concern. Regards, Fred Coe
Hi Carol, A bisphosphonate for bone disease is common practice. He/she needs to prescribe the calcium and D needed. Regards, Fred Coe
Thank you, Fred. Appreciate the time you took to help me get a correct diagnosis. I will pass this on to my Endocrinologist.
Dear Dr. Coe,
First of all, this is an excellent site and has helped me tremendously! I am 28 years old male with 3 small calcium stones (first diagnosed at the age of 20), hypercalciuria (found out 2 years ago which I treat with thiazides and low sodium intake), low25OHd3( 7ng/dl which must be for many years as I rarely was under the sun ,found out 2 years ago which I treated) and in the process of investigation I found out a shocking result which still bothers me: a LS t-score of -2.9, Fem.Neck of -2.6 and full body of -2.5, without any fractures or bone pain. Other than that I am healthy and active.
All of secondary causes of osteoporosis seem to be excluded. However, I would like you to evaluate some serum values:
Ca++: 9.9 PTH: 40, Phos: 3.8
Ca++:10.1 PTH: 21 Phos: 3.4
Ca++: 9.8 PTH: 34 Phos: 3.2 (under thiazide)
Ca++:9.6 PTH: 40 Phos: 4.2 (under thiazide)
Ca++:10.3 PTH: 38 Phos: 3 (under thiazide)
Ca++: 10 PTH: 28 Phos: 2.9 (under thiazide)
Ca++ 9.9 PTH: 31 (under thiazide)
Ca++: 10.3 (pth, p, not drawn) (under thiazide)
Serum calcium from 2015: 10.5
4 ionised calcium values I’ve got all are normal except one (over the upper limit)
1.25OHd3: 62
Alkaline Phosphate: 72 (normal)
As far as the urinary calcium: I’ve got many values. The mean value of untreated is around: 360mg/day
With HCTZ/amiloried (25/2.5) I didn’t see any difference, I jumped to bendrofluazide 2.5 which got me around 260mg/day (with 800mg dietary calcium) and for the last 3 months I am with indapamide at around 200mg/day (with 1200mg dietary calcium).
I think with high urine volume and thiazides I won’t get any more stones (considering I had very slow disease progression anyway) but bone disease at such age and finding a diagnosis is what worries me. To investigate further I asked my parents to test their urinary calcium. Father’s was 160mg/day (with approximately 500mg/day dietary calcium), my Mothers was 318mg/day (with calcium diet probably more than 1000mg) and 150mg/day (with 2 dairy servings -about 600mg dietary calcium). Their BMD’s are expected for their age. My mother had a small stone years ago which is no longer detectable with u/s and reported having an uncle with calcium stones). My father at my age had a renal colic ( he reports it was “crystals”, but no further colics after that). Brother hasn’t been tested.
My fist LS t-score was -2.6. I repeated a year later (under bendrofluazide and average urinary calcium 260mg/day and dietary calcium intake 800-900mg/day) and it went down to -2.9 ( it is interesting that BMC didn’t change that much but bone area showed increment which resulted in lower BMD – which makes me question the validity of this loss). Unfortunately I didn’t have Femoral neck the first year to see how if there was loss of mass in neck too.
All my years I lead a sedentary lifestyle was skinny and small body frame which makes me wonder if I started life adulthood with a low t-score anyway.
My questions are as followed:
1) Does this look like a idiopathic hypercalciuria or some other metabolic syndrome (PHPT?) which involves bone resorption? I want to notice that I get high urinary fluctuations according to dietary calcium. For every 300mg dietary calcium change there is about 80mg urinary calcium change too and generally big fluctuations which made me question the lab for very long.
2) The graph in your article shows that most non-IH people have less than 250mg/day ca losses. But for how much dietary calcium is that? Does that mean that these lose almost the same urinary calcium with 800 and 1200 mg/day diets?
3) Does the two discordant urinary values of my Mother (318, 150) guarantee more urinary tests to exclude IH? If we accept that none of my parents have IH, is it rare in clinical practice for an offspring to suffer from IH (probably new mutation?)?
4) From your experience, do you do holiday drug for thiazides when they are taken for too long? (Maybe to refill intracellular potassium storages?) or it is not necessary.
5) My serum 25ohd3 hovers around 40ng/dl (with 1.25OH at 62). Is it wise to increase serum 25ohd3 in order to increase the serum CaxP and hopefully help bone calcification?
6) Any other remarks or suggestions on how to help bone metabolism?
I tried my best to make it clean and short. I know it is not an easy case and I know my doctors should have the last word, however I highly value your words and your dedication. Thank you.
Hi Steve, I do believe you have IH. The high urine calcium, high 1,25D and seemingly normal serum calcium levels. Bone disease is certainly well known as is a reason why it should be there. Your treatment seems to lack definitive reduction of diet sodium to 65 mEq (1500 mg/d), which is very valuable for bone mineral retention. Your serum calcium, being crucial seems a bit patchy. I would be certain via three fasting and off medication measurements, although frankly PHPT seems unlikely. What you need is finesse from your physicians – IH is genetic, life long, and the bone disease not of a common sort. There are limits to how much I can be helpful from a distance except to say judgment about when to consider bone active drugs needs some attention. Of course 1/2 of your immediate blood relatives have risk for IH and should be studied. Regards, Fred Coe
Hi Dr. Coe. This is Dr. Velasco from Central Vermont.
I wanted to ask your opinion. I have this 42 y/o woman who has been diagnosed with idiopathic hypercalciuria since 2012 at YNHH. She is on chlortalidone 25 mg a day and k supplements. Her 24 u calcium is 151, electrolytes are WNL.
She is very frustrated about the disease and her BMD even those she is pre-menopause continues to decline. She is on low dose OCP. I have advised to eat about 0.8-0.9 g of protein a day and to be on a low salt diet. I reviewed some papers and it seems there is not much evidence about using bisphosphonates in pre-menopause woman to improve BMD or worst there is not evidence that that will improve fracture risk. Am I correct? Will you do something differently? Thank you so much.
Dear Dr Velasco, The bone disease of idiopathic hypercalciuria is indeed evolving and we do not know enough. However we do know this much: Bone mineral balance will rise with low sodium/high calcium diet, and with low dose chlorthalidone. That she is on chlorthalidone and got no response suggests a problem with diet sodium, or calcium, or both. Unfortunately the data here are incomplete. My own balance study used only chlorthalidone and showed positive bone balance, but I was fortunate that calcium intake was ample. To achieve positive bone balance in IH takes a lot of diet calcium, but none of the studies also added low sodium (65 mEq/d or better). In one trial – the only one remotely related to your case – high calcium + low sodium increased bone mineral in peri-menopausal subjects. So, I would use the combine of low sodium and high calcium and CTD and also consider if she can safely continue estrogen after menopause. As for bisphosphonates, I share your concerns because IH bone disease has some low turnover features. If needed she may benefit from some of the newer MC antibody treatments if needed to ward off fractures. Regards, Fred
Hello, folks. I’m the patient in question. I was dx’d at U-C in ’06, actually, by Dr. Favus, while doing my residency. I have never formed a stone, and an U/S at U-C found no stones at that time, either. (Isn’t that strange?!) I generally keep Na<1000 mg/day, and Ca intake I obtain from 3 servings of yogurt daily, plus or minus a pile of kale or other high-Ca greens, or a couple of sardines. I experienced bone density improvement one year only, and that was a year when I was living in Indonesia, using Tums for most of my Ca, and eating an extremely low-Na diet with nearly all protein from tempeh, a fermented soy cake. After that, my spinal bone density improved. It worsened after I returned to the States, and I've wondered why ever since.
Here's my question, Dr. Coe: would it be helpful to add Ca supplements atop my yogurt intake? Perhaps Ca citrate, recheck bone density in a year? From past experience, I know my urinary Ca rises when I use supplements, but I'm unsure whether that would negatively affect bone density. I'm not worried about stones. I'm extremely worried about my spine.
IN other words, might my poor spine vacuum up extra Ca if I provide it, given that I don’t seem to form stones (knock on wood)? Could I safely bump Ca to, say, 1500 mg/day and see what happens?
I would also welcome insights as to why my hip bone density improved, 2018 vs 2012, but spine worsened. Why would these two types of bone be going in different directions?
Hi Again, The bone disease of IH can be focal, and I do not know why. Sorry, Fred
Hi there, I’m 19 and have had kidney stones since the age of 11. Currently I have one 9 mm stone in the lower pole of my left kidney as well as a 4 mm stone in the middle. Although both are non obstructing I’ve been getting a lot of pain in my left kidney..what can I do to alleviate this? Also, my nephrologist put me on potassium citrate and said my diet was fine. My blood calcium levels fluctuate from 9-10.1. Is there a chance this could be due to my parathyroid? My 9 mm stone grew from 2 mms in January to 9 mm in late April. The 4 mm stone was not there on the last scan I had in March. Why am I producing stones so fast?
Hi Lily, your variable blood calcium does suggest primary hyperparathyroidism, and you should be sure and get proper testing for it. Pain from non obstructing stones is not uncommon, and we do not as yet know if more surgery will improve it. Regards, Fred Coe
Hi, I suspect you might settle at about 1200 – that was the trial. Those women were peri-menopausal, so not like your condition, but it is all we have. If you keep the sodium low enough, try 1500 mg calcium but check the urines. Consider a very low dose of chlorthalidone 12.5 mg daily as an extra – it can raise bone mineral balance. Regards, Fred
Hi Patient in Question, I gather you have idiopathic hypercalciuria and its associated reduced bone mineral density. Your experiment in Indonesia with very low sodium diet and extra calcium resembles the one – yes only one – actual trial concerning effects of sodium and calcium intake on bone balance – in this article. I believe the very low sodium was important and perhaps the Tums. Here, with some bone loss, I would consider using supplements – the best way is with larger meals – that was how the trial went – along with the lowest possible diet sodium. I would use 24 hour urine testing to be sure of the sodium, hard to gauge. Your urine calcium rise with diet calcium is entirely a function of the corresponding sodium intake and consequent fractional excretion of sodium, so the lower the better. Regards, Fred
Thank you for your reply , Dr. Coe. I will try these ideas. I’ve been on chlorthalidone for 12 years now, and it has not really helped–hence my and Dr. V’s frustration and search for new approaches. (Would you mind removing my name from your reply?)
Hi Patient in Question, perhaps your diet sodium is high enough to offset the effects of the medication. If bone mineral retention cannot be otherwise maintained bone directed meds may ultimately become your best alternative – I think you know that. Fred
Please remove my name from your previous reply. My diagnosis is now linked to my real name on search engines.
OK, I think I did that. Fred
Hi Dr. Coe. I am 59 year old post menopause woman. I had my first stone 2/18 with laser lithotripsy. Took Jills wonderful course and follow the diet vigilantly. My last 24 hr urine in May had all good parameters EXCEPT urine calcium was 351. My first 48 hr collection had calcium of 221 and 295–we figured out that my sodium intake was a little too high–and have resolved that issue. 1) Why would my urine calcium jump so much this time?
Today is my first day of hydroclorothiazinde — 25mg– and I will repeat urine in 2 weeks. Do you recommend increasing potassium intake or should I just wait to see what my urine and blood work looks like. How much of a decrease in urine calcium should I expect? How will I know if it is the medication effect when my urine calcium has been variable (221, 295, 351). My PCP did not believe I needed a bone scan. 3) Do you think I need a bone scan?
Many thanks !!!
Hi Barb Blue, Take a look at the sodium – did it increase. Likewise at the PCR – did your protein increase. Is your urine sodium low enough – below 100 and preferably about 65. Potassium citrate can wait; lower the sodium fully, keep the PCR below 1, and see what the med can do. I suspect part of the increase is you raised diet calcium. Be sure to use foods not supplements if possible. Supplements need to be with meals. A bone scan is a good idea – hypercalciuria causes bone disease. Regards, Fred Coe
Dr. Coe, I was diagnosed with primary hyperparathyroid disease in August of 2017 and had a parathyroidectomy on 3.5 of my 4 parathyroid glands at Yale New Haven hospital. I have also had very high CA reading in my 24 hour urine tests and am diagnosed with osteoporosis. My 24 hour urine tests have consistently been high and in the neighborhood of 387 or so. While my PTH reading fell to normal after my surgery, it is now a high reading again of 86. My bone density test has deteriorated to the following: The L1-L4 BMD has a T-score of -2.8, the L2-4 BMD has a T-score of -2.8 and the L1 BMD has a T-score of -3.0. The femur BMD T-score is -1.5, the femur neck BMD T-score is -1.9. My doctor has tried decreasing my urine CA through drugs such as chlorthalidone or hydrocholorthiazide but I do not tolerate them. One raised my potassium level and I did not feel well with the other. He is now trying me on a low level of potassium citrate (10MEQ, 3 times daily) to see if I can tolerate it and improve the urine CA level. In addition but unrelated, I have Hashimoto disease of my thyroid. He is asking that I get tested for kidney stones due to the high urine CA level. If the potassium citrate does not work, do you have any other suggestions for approaches to address the high urine CA and osteoporosis issue as my osteoporosis continues to progress even though I am very careful with my diet and do strenuous weight lifting twice a week.
Hi Janet, Given that you are at Yale, I hesitate to mention the possibility, but perhaps you have recurrent primary hyperparathyroidism; you seem to have had multi gland disease, and the high PTH and stubborn high urine calcium + failure of bone mineral to increase are most compatible with that possibility. Is your serum calcium perhaps even trivially above normal?? Have they done ionized calcium to check? Hypercalciuria is common after cure of PHPT as we and others have reported, but rising PTH and worsening bone disease are not expected. Perhaps your physicians might consider this idea, if they have not already done so and abandoned it as being unlikely. Regards, Fred Coe
Hi I am a 50-year-old post menopausal woman postmenopausal since 45 years old I have a high urine calcium read out I’ve had multiple lithotripsy and multiple incidences of kidney stones and my renal doctor wanted me to start thiazides. I however do not want to start any type of water pills because I’ve been reading about the adverse affects of them especially on the heart . I started taking Rice bran in food in the morning and at night but I don’t take any calcium supplements. My calcium level was low but my vitamin D level was extremely low and I don’t know what the differences between those two and I am currently having severe pain in my hips and my shoulders. I don’t know what else to do
Hi Lulu, Rice bran and low calcium diet may lead to bone mineral loss. Your best treatment is very low sodium diet to keep your urine calcium down, and a high diet calcium for your bones. Low vitamin D is very bad for bones and I am sure your physician will want to raise it. If your serum calcium is low – as you suggest – the vitamin D deficiency and low diet calcium absorption may be causing serious problems your physician will want to remedy promptly. Regards, Fred Coe
Dr Coe…I emailed you in January and based on my lab results you believed I had secondary hyperparathyroidism. My endochronologist came up with the same due to Vit D deficiency. She raised my Vit D to 4000 in and calcium to 800 mg/day. I am on low salt diet and about 90 oz water/ day. Since implementing these changes, here is my recent blood work.
D25 OH. CAL. PTH
2/23/18 49. 9.8. 31
3/27/18. 61. 9.7. 36
10/1/18. 84. 9.2. 64
I am concerned because my kidneys are still loaded with tiny stones. There has been no change in stones for two years. I have never been able to collect a stone. I also don’t know why the PTH has gone up to 64. Should I be seeing a nephrologist for stones?.
Thank you,
Carol
Hi Carol, I notice the serum calcium is lower. Have you reduced your calcium intake or changed the kind of calcium foods?? Given multiple stones you should want a full evaluation. Here is my favorite article about the subject. Regards, Fred Coe
Coe,
I would appreciate if you could look at my current testing. I’m still in limbo as to my diagnosis. Finally passed two kidney stones and they were both calcium oxalate. I took Jill’s course and have been on the low salt, low sugar diet, high water intake since last summer. I am now on the low oxalate diet for the past month. Nephrologist said that he still thinks I have primary HPT. He said a urine calcium over 400 is most definitely PHPT. I can’t figure out why my urine calcium went so high. I’m taking a cal supplement 800 mg/day. I do eat a lot of calcium in my diet. Am I getting too much? Vitamin d is i2000iu/day. My blood tests were non fasting.
My nephrologist wants to put me on hydrochlorothiazide and do another 24 hr urine in three months. I don’t know if I sent this so you can see my recent test results. If I didn’t send them correctly please tell me how to get them to you.
Sent from my iPaimage1.JPG
image2.JPGimage3.JPG
Forgot to tell you that I still have many stones. My nephrologist requested that I contact you about my test results before going on thiazide. Thanks so much.
Hi Carol, I am always happy to help but this is a slightly unusual issue – to intervene in a real clinical decision as opposed to simply offering routine technical information about 24 hour urine findings. If your nephrologist would actually want my advice concerning your medical management, S/He would need to contact me and send me the materials deemed pertinent. I would then respond to him/her as well as to you. It is the better way to do this, with a proper relationship. Warm Regards, Fred Coe
Thank you Dr. Coe. I will do that.
Here are my last three test results from litholink.
Vol 24 sscaox. Ca24. Ox24. Cit24. SSCaP. Ph. So UAE. Ua24. Date
3.38. 3.99. 373. 27. 684. 1.74. 6.944. 0.05. 0.561. 1/7/19
3.80. 2.37. 171. 26. 300. 0.52. 6.398. 0.17. 0.651. 11/26/17
250. 3.09. 247. 18. 645. 1.60. 6.963. 0.05. 0.478. 7/27/17
Here are my last three PTH, calcium and Vit. D,25-OH
1/15/19. 46. 9.9. 68
12/31/18. 33. 9.7. 61
10/1/18. 64. 9.2. 84. Lowered vit d to 2000iu from 4000 after this test.
Sorry I sent this in three different emails. My nephrologist values your opinion. Thank you.
Carol
Hi Carol, just looking at numbers, serum calcium levels seem normal so primary hyperparathyroidism is not a realistic idea. It all looks like idiopathic hypercalciuria. Regards, Fred Coe
A few more results…sodium is 56, mg24 is 167, cr24 is 1005 on current 24 hour urine. Sorry I sent this in a few emails. Thank you, De Coe
Hi Carol, the low sodium should have lowered urine calcium; I do not know what 167 is. Regards, Fred Coe
167 is urine magnesium. All other numbers were good. Ca24/cr24 was 371. Can”t understand why my calcium is so high. I stopped taking calcium pills and get my 1200 mg in food. Appreciate you so much.
Hi Carol, Idiopathic hypercalciuria, if that is what you have, raises the urine calcium. If low sodium diet does not bring it down, and your blood calcium is really normal, then meds are in order. Regards, Fred Coe
Dr Coe,
I sent you all my test results back in January and you said I had secondary hyperparathyroidism due to vit d deficiency. Saw my endochronologist and she agreed. Since taking 4000 in of vit d and 800 mg calcium my PTH was 31 and calcium was 9.8. Was tested a month later in March 2018 and PTH was 36 and calcium was 9.7. Just saw my endochronologist today after blood work and my PTH was 64 and calcium 9.2. I am on a low salt diet and high water intake. My vit d25 OH was 49 then 61 and now 84. I was told to back off on vit d to 2000 iu and stop taking calcium. My kidneys are full of tiny stones and this situation concerns me the most because things haven’t gotten better for two years. Would appreciate advice on what to do about stones.
Hi Carol, I already responded to your labs. I am confused about the sequence = I presume the many tiny stones were there before. If they are new, that is a real worry. I suggested a full evaluation for the cause of stones and think that is essential. What interests me is why your serum calcium fell – had you lowered your calcium intake before the blood draw? Are the bloods all fasting? If not, they can be very misleading as PTH falls with meals and serum calcium rises. Regards, Fred Coe
Dr Coe, Are my stones caused by the secondary hyperparathyroidism or are they a completely separate issue and not related to SHPT.
Hi Carol, Secondary hyperparathyroidism does not cause stones. It is a response to some drive for more PTH: vitamin D deficiency, low calcium diet, reduced kidney function, intestinal calcium malabsorption. Often stones ’cause’ it because people avoid diet calcium – always a mistake as it will not prevent stones. Regards, Fred Coe
From recent tests my 24 h urine calcium is 338 mg/d and bone density T-score of -1.7 at right total femur(low bone mass). I am allergic to sulfamethoxizole(hives on forearms). Is there an option for my apparent I.H. other than thiazide diuretics ?
Hi John, There is. Reduced sodium intake will reduce urine calcium, and a combination of high calcium low sodium diet is your best chance. The only good trial was in the premenopausal, so none for men. Even so, it is your best bet. Regards, Fred Coe
Dear Dr Coe,
I came across your website because you diagnosed my maternal grandmother with hypercalciuria many years ago when she was having kidney stones, and she has described what a difference your work made for her. I have recently passed a calcium oxalate stone myself, and I am currently having further investigations into the cause, which is what led to my recent interest. My mother and other family members have also had kidney stones, and several family members suffer from low bone mineral density/osteoporosis. Therefore, it was really interesting to read about the stone and bone links and the relevance of family history. I am currently feeling quite unwell even though there are no more stones present on ultrasound, and my serum calcium concentrations have been normal on the three occasions they have been checked over the past few months. However, I did have a raised parathyroid hormone level with normal serum calcium, and I have other symptoms of hyperparathyroidism (fatigue, excessive thirst, finding it difficult to concentrate, feeling slightly dizzy). My calcium levels were not checked after fasting, although in one occasion I had had very little to eat beforehand. I am currently waiting for a bone density scan. Can you suggest any other investigations that might be useful for exploring the cause of my stones and other symptoms? I would be happy to send more detailed results if you are willing to look at them. If so, it might be easier to send them via email if there is an email address I can contact you on.
Many thanks in advance for any advice.
Best wishes,
Emily
Hi Emily, Idiopathic hypercalciuria is genetic and causes stones and a form of bone disease. Obviously I would suggest 24 hour urine testing along with fasting am bloods to be sure about serum calcium. I suspect you have IH, and also perhaps low calcium diet or low vitamin D as a cause of high PTH with normal serum calcium. This kind of normal calcium increased PTH is secondary and without known symptoms of its own. If you wish to write to me personally I can look up my records of your grandmother. If she is still alive ask her permission and also send my regards. Regards to you, as well, Fred Coe
Dear Dr. Coe,
Thank you so much for your quick reply and your offer to look into this for me. I will send your regards to me grandma. She speaks very highly of you and I’m sure she’ll be pleased to hear from you. I will also ask for her permission regarding accessing information from her records. Is there an email address that would be okay for me to contact you on? If you would prefer not to share it on here, I could contact your department and ask them if that’s okay?
Thank you again,
Emily
Hi Emily, Write me directly: coe@uchicago.edu. Fred
Hi Dr. Coe,
I was just diagnosed with IH based on two 24 hour urine tests and the blood test. My level of calcium in urine is 390 and calcium/creatine ratio is 365.
I am 62 and have never had any stones. Moreover, there is absolutely zero history of stone-forming anywhere in my family. I was tested because my bone scan showed osteoporosis in my hip femurs: 2.5 & 2.7 Z scores.
The endocrinologist of course prescribed Hydrochlorothiazide 12.5 Mg daily, but I am interested in avoiding this medication if at all possible. For one thing, I have quite low blood pressure to begin with, and also I would be much more inclined to treat the root cause rather than the symptom. So I am wondering about your advice on diet and any other things I can do. (I have always exercised with weights and am very active so I don’t think I can do much more with that). My diet is very healthy, but I may be eating quite a bit of protein.
I really appreciate any guidance you can provide.
Thank you so much.
Hi Vasiliki, IH produced bone disease and you can do well with reduced diet sodium and high calcium diet. THe ideal diet sodium would be about 50 – 60 mEq (about 1500 mg/day or less), and diet calcium about 800 to 1000 mg. If the low sodium diet is not enough one can add a very low dose of thiazide to it, low enough to prevent too much side effects. If the disease progresses, standard bone treatments are not unreasonable, including bisphosphonates and newer agents. Regards, Fred Coe
Thank you for the speedy and helpful reply! Since you didn’t suggest low protien intake, can I assume that is because I am not at risk for kidney stones, just bone mineral absorption? Thank you!
Your generosity of time is a true gift to people like me seeking to understand this disease better.
Hi Vasiliki, No; low protein diet is not a good idea. You want about 1 gm/kg/day, a normal intake. Fred
Wow, you are the best! Thank you.
Hi Dr. Coe,
I had surgery in May for a calcium oxalate stone (my 3rd kidney stone incident but first analyzed). I finally had a 24 hour urine ordered here in Toronto. My results are:
Calcium per day 12.2 mmol/d
Citrate per day 7.5 mmol/d
Creatinine per day 13.3 mmol/d
Magnesium per day 9.3 mmol/d
pH 5.5
Phosphorus per day 29 mmol/d
Potassium per day 35 mmol/d
Sodium per day 75 mmol/d
Urea per day 359 mmol/d
Uric acid per day 3.5 mmol/d
volume 5.792 l
Bloodwork
calcium 2.4 mmol/L
Chloride 104 mmol/L
Creatinine 49 umol/L
Ionized Calcium 1.24 mmol/L
Magnesium 0.79 mmol/L
Phosphorus 1.19 mmol/L
K+ 4.0 mmol/L
PTH intact litho – cancelled
Sodium 139 mmol/L
Total CO2 26 mmol/L
Urea 2.8 mmol/L
Uric Acid 154 umol/L
They have not shown any oxalate amount even though I saw it on the requisition and I don’t know why the PTH was cancelled. I am hoping to see a nephrologist after I have completed my 2nd 24 hour urine. I am just wondering what I should be asking him/her once I do get in to see them. It looks to my like I have hypercalciuria but I don’t yet know why. Thanks for any help/suggestions you can give me.
Sincerely,
Lisa
Hi Lisa, You do have a high urine calcium and normal serum calcium, suggesting precisely the condition in the article you post on. The PTH would be unneeded given the normal serum calcium. Omission of oxalate is a mistake as it can be high in any stone former, and should be measured at least once for safety. I know that Canadian health systems function on statistical assessments of cost/benefit, and also prides itself on evidence based decisions. But here the system is wrong. Rare people have very high urine oxalate levels AND incidentally high urine calcium, and the former can cause kidney disease. Given it is rare but dangerous one should always look at least once at 24 hour urine oxalate excretion. Overwhelmingly, it will be unremarkable, but even so. insist on at least one measurement. Idiopathic hypercalciuria is familial, certainly genetic, and strongly improved by low diet sodium and if needed thiazide diuretics. Here is my very favorite article on treatment. Regards, Fred Coe
Thank you so much for replying. I re-checked my online results a few days later and the oxalate amount showed up at 556 umol/d which shocked me because I’ve been following your and Jill Harris’ Kidney stone prevention diet for almost 6 months. I will be doing another 24 hour urine next month and then hopefully seeing a nephrologist so I will discuss this with them. Much appreciated.
Hi Lisa, So high a urine oxalate usually means diet calcium is not high enough, or calcium is not timed well to meals that contain high oxalate foods, or some very high oxalate foods are being eaten, or there is an underlying issue raising oxalate absorption or even production. Consider these alternatives with your physicians and perhaps you and they can sort out the cause – everything has a cause. Regards, Fred Coe
Thank you so much. I will definitely discuss with them. Happy New Year.
Hi Dr. Coe,
Thank you for providing such valuable information and for offering this opportunity to ask for your advice! I hope this isn’t too much information, but I would greatly appreciate your in-put
My husband (54 yrs old) had his first (and hopefully last) kidney stone October 31, 2019. After reading extensively on your website, I assume that he has idiopathic hypercalciurea. He has been eating a lot of sodium. It makes sense.
I understand your dietary advice: sodium 1500-2300mg/day, Calcium 1000-1200mg/day, protein .8-1.2g/kg body wt /day, water 3 L.
My question is to ask for clarification of your oxalate recommendation of 100mg/day for stone formers. How do I put that into perspective with the fact that his urine oxalate levels were normal (but he had been eating high oxalate prior to the stone, and then very low oxalate after the stone bc/ it was an oxalate stone) and his calcium intake meets your recommendation? Should he still try to keep dietary oxalate to 2300mg Na/day. He eats 1.1-1.5g protein/kg body weight /day.
Hi Rose Marie, You are wise and shrewd. If his urine oxalate is normal then he is done with the oxalate diet apart from the worst foods – spinach and rhubarb, and lots of nuts, pepper, and dark chocolate. With high diet calcium from food distributed to the main meals oxalate is a minor player in people with low values of urine oxalate as you describe. The big problem is to keep the sodium low enough that his urine calcium is not too high- -so measurements are needed. Be sure everything has been measured and attended to – here is a good overview. Regards, Fred Coe
Thank you so very much for your response and advice. We’ll focus on lower sodium, higher calcium per your recommendations and then re-do the 24 hr urine in a couple of months.
Best, Rose Marie
Correction: I miscalculated my husband’s daily calcium intake. Instead of approximately 1000mg/day, it is closer to 550mg/day. My apologies. Rose Marie
Hi Rose Marie, That is a bit low, as you know. Regards, Fred Coe
Hello Dr. Coe,
I have a question regarding management of a patient with presumed idiopathic hypercalciuria. Urine calciums ~400 mg/24 hours on multiple collections with urine Na ~100 meq. She is 62 with severe osteoporosis and calcium oxalate nephrolithiasis. Her stone disease has been stable for years but I am very concerned about her bone disease. Interestingly, she also has a diagnosis of sarcoidosis. This was based on very mildly elevated 1,25 OHvitamin D levels, hypercalciuria and chest CT findings of nodules/adenopathy over 10 years ago. Serum calcium always wnl. She was never treated for sarcoid, just monitored.
She recently established care with me and we did not see any improvement in her calciuria on chlorthalidone 25 mg. She had significant hypokalemia and hypomagnesemia so I know she was taking it. I believe her diagnosis is most likely IH and not sarcoid. She has a strong family history of stone disease and hypercalciuria with 2 siblings on thiazides. Before starting chlorthalidone, her serum Ca, 25 OH and 1,25 OH vitamin D levels were all in normal range.
My questions are: Why did we not see any reduction in urine calcium on chlorthalidone 25 mg daily and what would you do next? I am inclined to increase chlorthalidone to 50 mg daily and add amiloride but want to make sure I am not missing something here. I would really appreciate your insights on this case. Best, FC
Hello Dr Cormack, You do not mention it, but I assume her PTH was not suppressed – the remaining clue to D mediated hypercalciuria. Failure to lower urine calcium despite a reasonable urine Na of 100 leaves us with only three alternatives: lower the diet sodium more, raise the dose of CTD, or begin a bone active drug to reduce bone mineral loss. Of these, I like the third best, as she may have rapidly progressive bone disease. I like the lower sodium second. I have seen rapid bone mineral loss appear this way, and the urine calcium wane over a few years as bones stabilize. A trial of a bisphosphonate is not unreasonable, or perhaps an other bone active agent. As for amiloride, I agree totally. I find 5 to 10 mg daily a big help. Regards, Fred
Thank you so much for your prompt response and advice on this case.
Her PTH has been high 30s-low 40s. Most recently 39 (12-88 pg/mL) with serum Ca 9.7, 25OH vit D 24.6 (20-50 mg/mL), 1, 25 OH vit D 72 (17-72 pg/mL).
Because of quite severe osteoporosis, her rheumatologist recommended anabolic therapy (abaloparatide) to start but was hopeful we could lower urine calcium first. Historically she resisted bisphosphonates because her mother had jaw osteonecrosis. I agree that best to reconsider antiresorptive treatment at this point.
Kind regards, Fionnuala
Hi Dr Cormack, The anabolic meds may also partition calcium into bone. If it is more desired, I would personally give a try. Fred
Thank you, I really appreciate your input. Best, Fionnuala
I’m sure your preference would be getting your calcium from food but is calcium supplements (citracal for example) another viable option ?
Also how much daily protein do you recommend for a 125lb woman?
Hi Kim, calcium supplements are usable but best taken with the main meals so the calcium will be absorbed along with your food. As for protein about 0.8-1 gm/kg body weight /day is ideal. Warm regards, Fred
Thank you Dr. Coe for your research. I do appreciate it very much. I was a patient of yours when I lived in Chicago. I moved 4 years ago to retire. I followed the low sodium high food calcium diet that you prescribed for me. I make sure I drink a large amount of liquid as I live in a dry climate. I have been kidney stone free for 5 years. This year the urologist noticed a stone in my left kidney. It’s too large to pass. They offered to do a lithotripsy, but after having done two of those in Chicago with no success I refused. I’m waiting for my next appt. to see if they have to do surgery. I also need to tell you that I did have bone loss and now get bone density injections twice a year. Should I allow them to remove the stone via surgery or wait? Thanks for your time.
Hi MIdge, I remember you well. I am sorry about the new stone – that is a failure of treatment. If it is causing no pain, bleeding, obstruction or pain removal is elective. But why a new stone? Have you been able to get yearly 24 hour urine studies to be sure your diet is controlling stone risk? If not, please do that. Things change over time, and diet treatment is hazardous in a way as habits and life style are to complex. Let me know, and warmest regards to you, Fred
Fred, great information, as always. I have one observation, and two questions.
The observation pertains to the need (hypothesized, not proven, but common sense), for patients with IH to take in some calcium at a minimum (probably at least 300 mg/d if not more, EVERY day. It is very easy to take in zero calcium from the diet unless one eats dairy or green vegetables. A typical U.S. breakfast without cheese, say ham, eggs, a croissant, coffee, and orange juice, will have zero calcium. Same for lunch – say a tuna salad sandwich, and dinner (steak and potatoes with a garden salad). Lettuce has a trivial amount of calcium. A good site to look this up is https://nutritiondata.self.com/
I have found calcium supplements to not uncommonly cause constipation, so taking in even as much as 500 mg/d of calcium from food is not easy without dairy. As urinary calcium excretion responds only partially and poorly to reductions in dietary calcium intake, I believe that it’s important to assure that there are very few or no days when dietary intake of calcium is low or absent in patients with IH. The minimum calcium intake (and days of trivial calcium intake) may be as important, or more so, than the average calcium intake.
The second is a question: what is the role of bisphosphonates in protecting the bone against calcium reaborption ?
And a third question/issue. Thiazide type diuretics are known to cause not only potassium depletion, but also magnesium depletion. The potassium issue can be dealt with by combining with a sodium channel blocker like amiloride, but what about magnesium? Re magnesium: and esp. in this day and age when many patients are taking PPIs such as omeprazole: Do you supplement your patients to whom you prescribe chlorthalidone with magnesium or monitor their magnesium levels?
Hi John, As always, perceptive and useful. I favor a full calcium intake of 1000 to 1200 mg/d and that means dairy products more or less. The trick is getting diet sodium down below 100 mEq/d or even lower, and I can manage that in some cases, and recommend we try in all cases. So I agree with you and even add. As for bisphosphonates, I have seen them stabilize BMD in IH patients, and they are a useful first line. But when not enough I am bold about newer agents. These patients can fracture, and fractures can be multiple. The magnesium issue is vexing and I always try to add MgO early rather than waiting for a big deficit. Unlike potassium wasting for which we have amiloride and low sodium diet, the Mg loss is hard to stop in some patients. So I monitor, and have them use OTC stuff. In manotor with 24 hour urines so I can see what is absorbed. Warmest regards, Fred
My doctor has recently diagnosed me with Grover’s Disease, a non-contagious skin rash that causes terrible itching and it can last for 6-12 months. On the Mayo Clinic forum site, a number of patients (with this disease) have said that eliminating dairy products has helped them significantly. Since I’ve had kidney stones 4 times, I have been on chlorthalidone (25 mg) for the past 3 years and my urologist has urged me to drink milk (I do – about a gallon a week). If I was to try and go off dairy for a month or so to see if it helped my Grover’s Disease, how would you recommend me getting sufficient calcium? Many thanks for your help.
Hi Carl, Of course you can use supplements in the mean time. Use a TUM with each main meal. But also mention the chlorthalidone to your dermatologist. I have seen a lot of skin reactions to it. Regards, Fred Coe
Dr. Coe,
Perhaps overly simplistic, but I always teach students/housestaff/fellows that any “hyperelectrolytemia” must be the result of either or a combination of impaired kidney function vs a rate of entrance into the blood that exceeds the rate of the kidney’s excretory capacity. As it relates to hypercalciuria, would it be fair to say that every cause of (ionized) hypercalcemic hypercalciuria is due to either excess GI absorption/bone resorption and the kidney is attempting to excrete the increased filtered load (i.e. “appropriate hypercalciuria”? If so, what level of ionized calcium would qualify as hypercalcemia leading to hypercalciuria (i.e. where enhanced GI absorption/bone resorption is the explanation rather than inappropriate renal loss of calcium)? Do we know this?
Thanks.
Hi Stephen, Because your mind is clear you ask wonderful questions. Of course tubule reabsorption sets the UF level for any given combination of filtration rate and urine excretion rate. That is conservation and no way around it. So all hypercalciuric states – higher excretion – have some element of supply to keep UF calcium appropriate to GFR and tubule reabsorption. In IH we found – as you well know – reduced tubule reabsorption from about 98% in normals to as low as 95% in IH subjects, and equivalent levels of UF calcium and more or less of GFR. The fall in reabsorption is driven by nutrient, including just glucose, so bone mineral can and will make up the difference when diet calcium is lacking. I think that is a reason bone mineral can be lost. If reabsorption does not fall enough to balance a supply rise, from bone mineral dissolution or increased GI absorption, UF calcium must rise. Vitamin D excess is a good model as Jack Lemman studied it decades ago. Give an excess of 25 D to young men and urine calcium rises – a lot. PTH falls, tubule calcium falls, UF calcium is unchanged. But in real life, if GFR fell, for example, or even if sodium depletion reduced PT delivery, UF calcium could rise a lot, and itself reduce SNGFR with the infamous and dangerous and sudden hypercalcemia we all dread. Im IH, urine calcium is not high because of increased FL, we have proven that. But, tubule reabsorption is sensitive to UF calcium (no doubt calcium ion) and no doubt because of enhanced CaSR somewhere in the nephron – I vote for cortical TAHL. We have some new data on this, but have published the effect before. So things seem rather integrated: GI absorption is above normal, renal tubule calcium reabsorption is abnormally responsive to at least UF calcium – and serum calcium, too, so both balance out. We never write about this as no one asks us to do so in the reviews they invite. It is always a level below this conversation – you know, such things as ‘…when should the physician use thiazide?’ Warmest regards, Fred
Yep, it all makes sense while, at least for me for certain conditions, remaining a conundrum…such as the hypercalciuria seen in normocalcemic hyperparathyroidism. It would seem to me that this would simply be another designation or subtype of idiopathic hypercalciuria. It would have to be reduced TmP/GFR with secondary increases in bone resorption and/or GI absorption to maintain the UF of ionized calcium, correct?
Hi Steve, NC PHPT has always seemed a function of how well we can measure serum calcium and how many times we are willing to do it. As to phosphate, I found and published years ago that serum phosphate does indeed run low in stone formers, and it is linked to other PT functions suggesting disordered transporter regulation. Bone will one way or another maintain serum calcium if renal tubule reabsorption falls and diet is insufficient and secondary rise in PTH is inevitable. All the best and thanks for the comment, Fred
Hello Fred,
I am grateful to receive your very useful mailings — thank you. You diagnosed my condition as idiopathic hypercalciuria, and your recent article reminded me of your advice over the years to consume an adequate amount of calcium and to be mindful your other dietary recommendations. Calcium consumption for me means plain yogurt and non-fat milk. You recommend consumption of at least 1,000 to 1,2000 mg calcium daily: I’m writing you because I’d like for you to coach me about what I’m reading on the products’ labels (I’m still overseas).
My habit is to buy containers of yogurt; quantity is 500g. The Iabel says 100g of yogurt contains 143mg of calcium. Am l right in thinking that 500g of yogurt yield 715mg of calcium and that therefore my consumption of this yogurt should be 2 containers daily? I believe you have also recommended cheese, but I usually avoid it because of fat. Fruit juice with calcium added is almost never marketed here.
I’ll close by repeating my thanks for directing me to Dr. Giovanni Gambaro — really outstanding physician and great guy who, by the way, thinks the world of you.
Thanks,
Charles Ellis
Hi Charles, You are right, the yogurt will do it. I hope Italy has remained an idyll for you, and wish you well. Please send my regards to Giovanni. Fred
Hello Dr. Coe, Thank you for sharing your valuable knowledge online on Hypercalciuria. I had 2 kidney stones in 2018. One passed and 1 was removed from my right kidney. So far been lucky not to have another one. My urologist ordered a 24 hour urine test recently and found my calcium level elevated. All results were in normal range, including volume, except the following:
Calcium 243 mg (550 mg)
Sodium 161 mmol (50-150 mmol)
I take Levothyroxine 100 mcg and my TSH level is 0.821 which is within range but the lower side of normal limits. I have been checked for Parathyroid and the PTH level was 26 pg. My Vit D level is slightly low so I take 1600 IU in a multi vitamin that does not contain calcium. My question is could lowering my levothyroxine to 88 mcg as long as I stay under 4.0 ulU/ML help lower my urine calcium? I read that hyperthyroidism can increase calcium so my thought was I might be benefited with a lower dose of Levothyroxine.
Other noted information/thoughts: Last 5 months have had several cortisone injections (spine/hip) trying to figure out groin pain, which ended up being a torn hip labrum. Cortisone causing elevated calcium? I’ve been under high stress from the pain for over a year until recently, maybe elevated cortisol might be contributing to calcium? Also, up until recently have been taking Hydrocodone 5-325. Codeine or acetaminophen effecting calcium?
Just trying to see if an outside factor could be causing the elevated calcium so I don’t have to take medication to lower my calcium. Any thoughts would be greatly appreciated. Thank you so much!
Hi Sandra, Possibly the steroids raise your urine calcium. But surely the high diet sodium plays a role. If you lowered it to 2000 mg or better 1500 mg/d urine calcium will fall to normal – in all likelihood. No meds. The role of sodium is in the article if you want the details Regards, Fred Coe