LISTS – AND LISTS
I know you are all looking for THE list. Here is one from a reliable source I have have downloaded on my site to a separate document so it opens with one click.
The reliable source, as it turns out, needed some updating. Dr Ross Holmes, professor, School of Medicine, University of Alabama, was kind enough to review the work of Dr. Michael Liebman who is a professor of Human Nutrition and Food Option at University of Wyoming and determine which food entries on the Harvard list needed changing. We cannot change the original but we have updated our lists accordingly and annotated updates with *** marks. So the lists here are the most recently edited available at present.Fred Coe and I have updates and annotated the list for those with a tendency to perfectionism: Updated table of oxalate foods. Set it at 50% for easier reading. Get yourself acquainted with the lists. They will tell you much of what you need to know. A lot of it will even surprise you. You are not as restricted as you think you are or as you have been told.
A more dramatic list is the 177 high oxalate foods we distilled out of the big list. Here are culprits! Not on this list? Probably not very high in oxalate so far as we know – with perhaps a few exceptions. Note that quantity is critical. For example black pepper is high in oxalate but the amounts used are small enough that total oxalate intake from it is negligible.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
LET’S DIVIDE AND CONQUER
FOODS TO WORRY ABOUT
A List of Concerning Foods
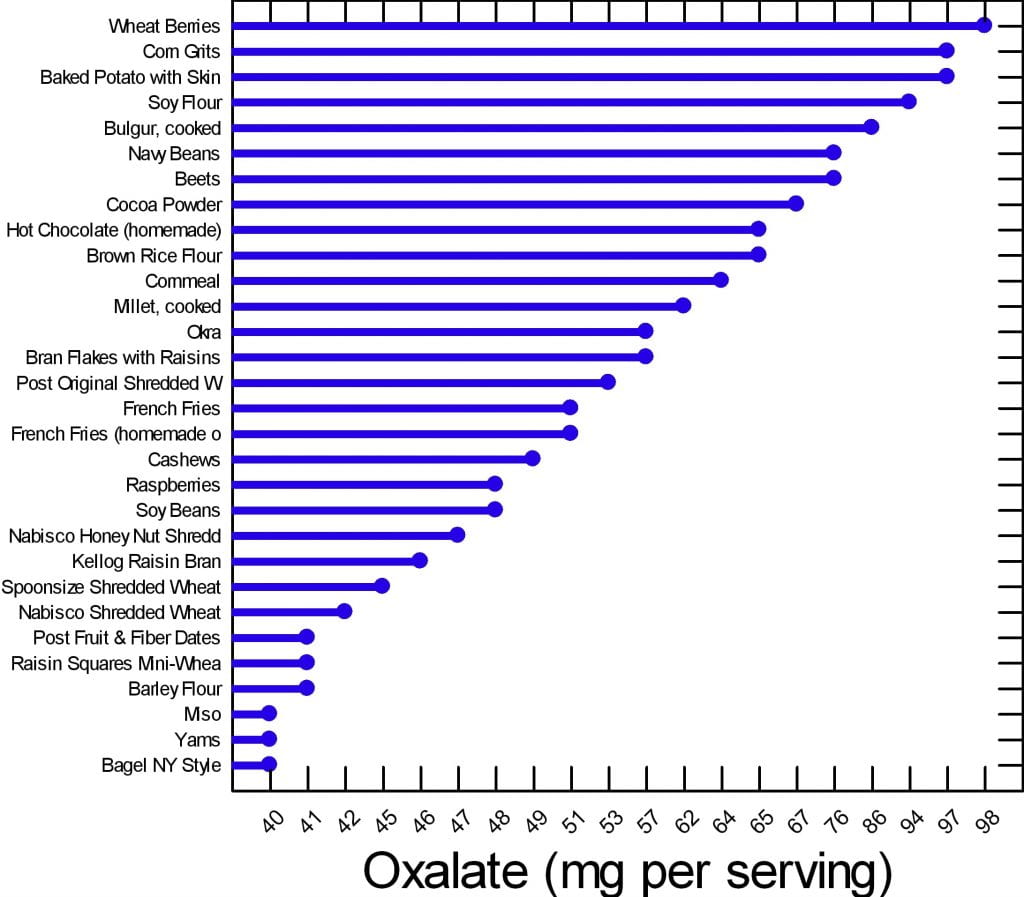
We have created two graphs for this article. Of the 177 foods on our master list, many are of concern but can be used in your diet if you control the portion size and how often you use them. There are 30 of them that are worrisome enough to deserve special attention.
Here are the 30. The graph shows mg of oxalate in a common portion. The details of the portions are in the complete list. The foods have in common that all contain at least 40 mg/serving. All other foods for which we have reliable data have less oxalate per serving.
Your budget is about 100 mg/day.
What does this graph mean? Does it mean you can never have chocolate, or a baked potato?
No.
It means if you want to use your whole budget on a treat, do it, but keep track and make sure you do not overspend in any meal or in any one day. Have your baked potato, but maybe share half with your partner. Or, have some hot chocolate but make it with milk because calcium helps reduce oxalate absorption. Eat your cashew nuts, but pay attention to how many. If one handful leads to ten, you cannot have them.
FOODS TO AVOID
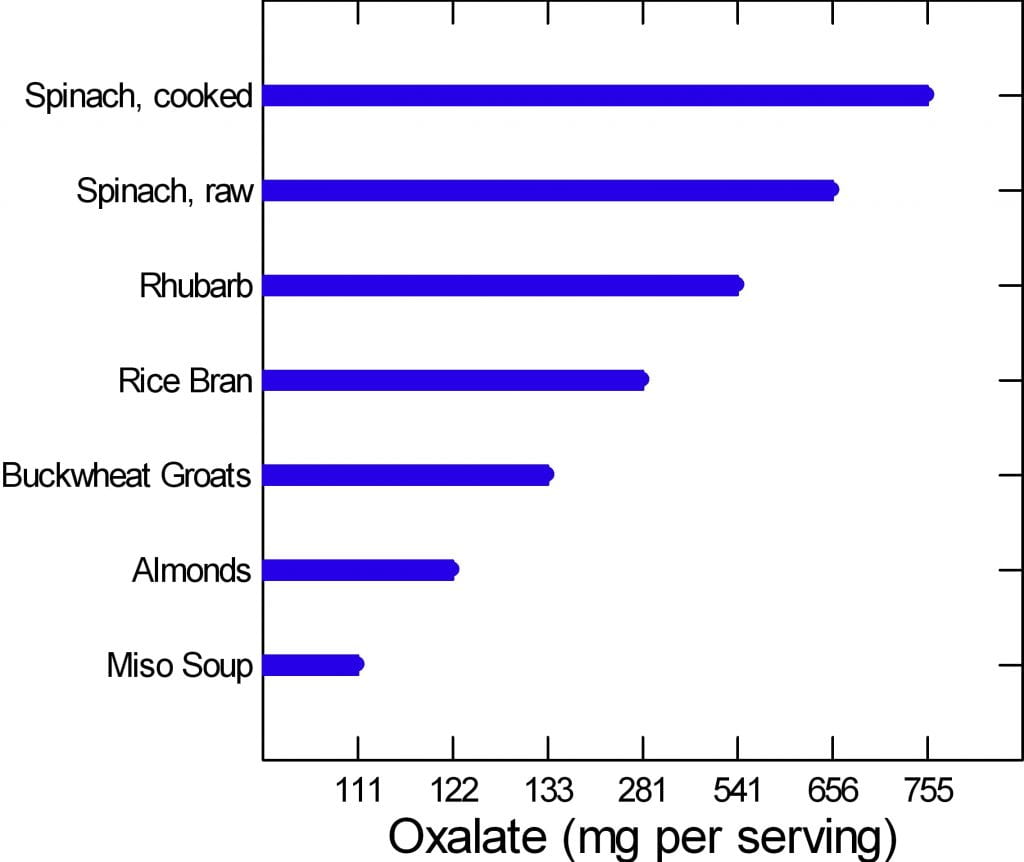 The graph to the left is of the very few dangerously high oxalate foods.
The graph to the left is of the very few dangerously high oxalate foods.
There are only six foods, but spinach, being worst of all, has two entries. Be careful of this plot because of its range. It begins at 100 mg/portion and rises to 755 mg/portion in only 7 steps, so the distance from miso soup to spinach is about a 7 fold increase.
Rhubarb and spinach are so high you just cannot eat them. Rice bran is something few will miss, the same for buckwheat groats.
People like almonds but have a hard time controlling portion size. If you can keep it to 11 almonds a day – the portion size that gives 122 mg of oxalate, alright. Otherwise stay away from them.
If you have to eat any of these foods, caution is hardly a strong enough word.
Are you sure you need to eat them?
Why?
WHAT ARE WE SAYING?
We are saying that oxalate is common in foods, and that you have to be careful, but care is a scarce resource. How much care can you give every bite? The graphs say if you eat moderately high oxalate foods – the first graph – be careful.
Watch portions.
If you are eating one of the six dangerously high oxalate foods, stop eating it.
It is too hard to be careful with those six foods. They have too much oxalate for most of you to handle. So, just say no.
WHY BELIEVE OUR DATA?
These data arose from a major effort at the Harvard School of Public Health. A world class expert has curated it twice. Harvard can be wrong and so can Ross Holmes, but both will tend to be wrong less often than the average persons who attempt to put complex data into the public domain. We have always appreciated comments, and if anyone has a peer reviewed publication with different food oxalate levels than ours, we will read the paper and see if it warrants our making a change.
Medical research is endlessly argumentative, and food oxalate is no exception. A recent paper contrasts findings from 6 websites and 2 applications and finds some wide variations. Of the sites, the Harvard site – used here as our reference, and the Wake Forest site – which is a legacy of an outstanding investigative group have most standing with me. Leaf through the comparisons between them in the 4 charts and in the large table at the very end. On the whole differences are modest. The hyperoxaluria and oxalosis list from the paper has been withdrawn from their site.
DO YOU NEED A LIST?
Sure, a list is nice. But we helping you here. Lists can run on to hundreds of foods. The picture is meant for focus. Here are the ones to focus on.
Many of you leave the doctor’s office thinking you will never be able to eat a fruit or vegetable again. If that wasn’t bad enough chocolate and nuts are gone, too. Some of this sadly is true, most of it is not. I am here to bring you good news: Almost everything, high oxalate or not, can be incorporated into your diet safely.
Do you need a low oxalate diet? You may if your stones contain calcium oxalate crystals and your urine oxalate is high enough to pose risk.
If you do need a low oxalate diet, what is your goal? Less than 100 mg of diet oxalate is good; less than 50 mg is ideal.
If you want to read some of the science about urine oxalate and risk of stones and about how we get to the diet oxalate goals, it is summarized at the end of this article.
Here we assume you do need to lower the oxalate in your diet.
CALCIUM FIRST
Low calcium diets can raise urine oxalate, and the solution may be as simple as a proper calcium intake. There is every reason for stone formers to eat 1000 mg of calcium daily to protect their bones. The common hypercalciuria of calcium stone formers puts bones at special risk when diet calcium is low.
Before changing your whole life around, ask yourself if you are avoiding calcium foods. If so, add them back and ask your doctor to check your urine oxalate again. It may fall enough that a low oxalate diet is not necessary.
If low calcium intake is not your problem, and you need a low oxalate diet, here is my take on how to do it.
WHAT IS THE DIET OXALATE GOAL?
Typical diets contain upward of 200 – 300 mg of oxalate. For stone prevention, a reasonable goal is below 100 mg of oxalate daily. An ideal would be about 50 mg daily if that can be accomplished.
To get there, consider the oxalate contents in common serving portions of all of the foods, and make up a plan for yourself.
FRUITS
FRESH
Everyone who comes to me is very unhappy thinking they can never have a berry again. This is Baloney. The only berry that is very high in oxalate is raspberries (look at the list). On the other hand, people do not realize avocado, oranges, dates, and even grapefruit and kiwi are very high and need caution.
This doesn’t mean you can never have these healthy treats. If you incorporate any of these high oxalate fruits into your morning yogurt you can reduce some of the effects of the oxalate content.
Also look at your portion sizes. You really cannot eat a lot at any one time. Dates are not a good bargain: One date is 24 mg!
CANNED OR DRIED
Canned pineapple is a problem.
Dried fruits have to be a worry because the water is taken out, so a ‘portion’ of dried fruit can be gigantic in oxalate content. Figs, pineapple and prunes are standouts. Just think: 1/2 cup of dried pineapple is 30 mg – not a lot of fruit for a lot of oxalate. If you want dried fruit, think about apples, apricots, and cranberry as lower oxalate options.
VEGETABLES
Spinach and rhubarb are standouts; stay away.
Other vegetables you need to be aware of are tomato sauce, turnips, okra, and yams (sweet potatoes) along with beans of different sorts.
I am not in the business of taking healthy foods away from people. But in the cases above you really must limit; there is just too much oxalate and these foods do not pair well with high calcium foods the way fruits can be mixed right into your yogurt or cereal and milk.
Many of you have been told to stay away from all green leafy vegetables. This is not true. Look at the list. There are plenty of salad options still available for you including kale. Even though tomato sauce is high in oxalate (see below) that is because of concentration. A whole medium tomato is only 7 mg and who eats more than one at a time?
Many of the salad vegetables are so low in oxalate they are freebies. Eat what you want.
POTATOES
These are Trouble! I put them into their own separate group even though they are vegetables.
From french fries to baked potatoes they are very high oxalate items. One ounce of potato chips has 21 mg of oxalate and who eats one ounce? Not I. Baked potatoes are terrible. One comes in at just under 100 mg of oxalate. Mixing sour cream into the potato will not help much; one tablespoon of sour cream contains only 14 mg of calcium. One ounce of cheddar cheese contains 200 mg of calcium, which could help, but it increases calories, salt and fat. But all in all, why struggle so hard? Potatoes are not ideal for stone formers.
DAIRY PRODUCTS
They have no oxalate. They are your main source of calcium. Use them. They can add a lot of salt – cheeses – and can be caloric. But they reduce oxalate absorption and preserve your bones.
For a stone former who has to watch salt intake, increase calcium intake, and lower oxalate intake, here is how to do that. You cannot have as much cheese as you want because of the salt. So portion sizes are very important. Yogurt, milk, even ice cream are good bargains – modest sodium and high calcium. These are a great place to add in a wee bit of chocolate – high oxalate foods – for those of you who cannot live without these high oxalate treats.
BREADS AND GRAINS
Some of the basic ingredients to make these foods are very high. White flour and brown rice flour are high in oxalate so everything you make from them will be high.
BREADS
Even so, as far as kidney stones go, breads are mainly alright because of portion size: not that much flour so one slice is 5-8 mg. French toast and New York style bagels top the list at 13 mg for two slices and 40 mg for one bagel – as much as anyone will eat of either food.
PASTA RICE AND GRAINS
Spaghetti, one cup cooked is 11 mg and most of us eat more than one cup.
Buckwheat groats, one cup cooked is 133 mg – I don’t see many of you saying ‘darn it’ or taking to your bed, but beware. Millet and bulger, wheat berries, rice bran, corn grits, and corn meal, these are widely used and are high. If you are using these, be thoughtful.
Here are some low oxalate options in this category: White rice, hummus, corn flour, corn bran, flax seed, and oat bran are popular and safe.
MEAT PRODUCTS
Since oxalate is only found in plant foods, all the meats are safe. Fish, too.
For our vegetarian friends, tofu and veggie burgers are very high.
NUTS AND SEEDS
These are just dangerous for two reasons.
Obviously they are very high in oxalate.
Secondly, I don’t know anybody who just has a few nuts at a time.
Just like chips no one eats one – the whole jar is more like it.
But, for one cup of pumpkin sunflower or flax seeds the highest is only 17 mg of oxalate and none for flax. For those of you who love foods in this category seeds are the better choice and they can be sprinkled on yogurt and ice cream.
SWEET STUFF
I have good news for my chocolate lovers. I know most of you have been sent home with a list and chocolate is high on it. But if you look at the numbers nuts are a lot worse than chocolate. Chocolate can be mixed in with dairy products, too, so as to reduce oxalate absorption.
Even so I do want to point out that half a brownie is on the high side, and who eats one half?
You can still satisfy your sugar craving but pay attention to your portion size.
Keep in mind, however, that sugar loads increase urine calcium loss which increases stone risk, so there are two reasons why this food group can be a problem.
But even without chocolate, you eat a lot of flour when you eat a piece of cake, so cake can be a problem – about 15 mg per piece, like french toast. Pies are half the risk because of their fillings – unless they are chocolate pies!
CRACKERS AND CHIPS
The big enemy here is potato chips. A one ounce serving contains a whopping 21 mg of oxalate. I repeat: A one ounce serving.
Your best bet in this category if you’re looking for something crunchy is corn chips – one ounce is 7 mg, popcorn – one cup is 5 mg, and pretzels, one ounce is 5 mg.
Crackers are OK mainly because they are small and the amount of flour is not that much.
BEVERAGES
PLANT SOURCES
Hot chocolate is the clear loser at 65 mg per cup; carrot juice is the runner up at 27 mg per one cup. Lemonade, tea, tomato juices, rice dream and the like are better but still high. The are 15 – 18 mg per serving. Lemonade – frozen concentrate – is 16 mg per 8 ounces so be careful about this as a source of citrate.
Soy milk, for those of you who prefer it, is not a good option. It is very high at 20 mg per cup. We have no data from standard sources for rice milk, cashew milk, and coconut milk; almonds are high in oxalate so the almond milk product will certainly be high.
Tea is so commonly used, here are the details. If you brew your own tea it is high in oxalate. The longer you steep your tea, the more oxalate it will have in it. If you use a sweetened instant iced tea one cup has 0 mg of oxalate.
Here are some juices that are low in oxalate and better substitutes: Apple juice, apricot juice, orange juice, grapefruit juice, grape juice. For all the lemonade drinkers, diet lemonade is low in oxalate.
Here is something very important: Coffee is oxalate free – almost, 1 mg for a cup (2 mg/cup for decaf). We already told you that coffee drinkers have a reduced stone risk, so lets debunk the coffee myth here: Drink it as you wish.
DAIRY SOURCES
Everything is good except chocolate milk. Even that is only 7 mg a cup for a sweet treat here and there.
ALCOHOL
What tops the list in this category is a can of beer: 4 mg of oxalate. All the rest are low and, frankly, the oxalate in a can of beer comes with a lot of fluid. This is not the problem area for stone formers.
WATER
If I didn’t say this to you I could not sleep well tonight. Water is the clear winner in this whole category. It is free of calories, sugar, and oxalate. Please use it as your main beverage and supplement with the items above.
SPREADS AND SAUCES
Chocolate, miso, peanut butter, and tahini are all high.
SOUPS
Miso soups is extremely high – 111 mg/cup. Lentil soup is high, and so is clam chowder – the potatoes.
BREAKFAST FOODS
This is a dangerous meal if you are a cereal lover. Many cereals are high in oxalate. I am afraid you need to look them up in the list by brand. Unfortunately the healthier cereals are highest in oxalate because they contain more plant based ingredients. Probably having milk in your cereal is wise, but we have no data to show.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
HOW DO WE MANAGE ALL THIS?
The first thing you need to do is to learn and remember what are the highest oxalate foods and beverages. Without this in mind it is impossible to shop and cook intelligently. Here is a short list of the highest oxalate foods all in one place.
BREAKFAST
For those of you who love cereal because it is quick and easy check out the list and see if the one you love is high in oxalate. If it is, choose the next best one with lower oxalate. Put milk in the cereal.
Alternatives to cereal that are also quick and easy: Yogurt or cottage cheese and fruit. The only fruits to worry about are raspberries because no one puts oranges on their yogurt. Bananas, peaches, blueberries and strawberries are perfect toppings.
More trouble, but no oxalate, eggs any way at all. Boil a batch on Sunday and have them for the week for breakfast, and snacks, too.
Your breakfast coffee is free and so is your water. For juices use orange, apple, pineapple, grapefruit – all great. If you want tea, don’t steep more than a minute and consider adding milk to it. Green tea is better than black.
LUNCH
Typically you are grabbing a salad or a sandwich for lunch, so what now? Many clients tell me they no longer eat salads because their physicians told them to stop all green leafy vegetables.
I’m bringing salads back to you.
Arugula, iceberg, romaine lettuces, and kale, are fine as your base. Stay away from spinach. Here are good toppings. Cauliflower, corn, cucumber, mushrooms, onions, peas, scallions, squash and zucchini are all fine. Tomatoes are fine, too; it is only the sauce that is high. Broccoli and green pepper are moderately high so watch the portion size.
Sandwiches will cost you between 12 and 16 mg of oxalate depending on the bread you are using – 2 slices. This doesn’t mean you can never have a sandwich, it just means you have to keep track of how much. You can have 50 to 100 mg daily. What goes inside between the two slices of bread is usually cheeses and meats which are oxalate free. So sandwiches are not something to be afraid of.
SUPPER
Beef, chicken and fish are all fine, and those the main courses for most of us. You will run into problems if you are a pasta or potato eater. If you are you need to limit the amount of times you have these foods each week and also the quantity each time you use them. Substitutes are a problem: White rice is a nice substitute for potatoes but there are few others. It is more veggies that have to fill in – very healthy but not as much fun.
Here is a recipe for cauliflower – ‘mashed potatoes’ you will like and even think, sometimes, is the real thing. There are many versions on the web, choose the one that makes you happy but be careful about the ingredients.
There is also quinoa which is not on our lists, but may well be high. A recent scientific article on this plant does not give oxalate contents which suggests they are not reliably known.
I have recently put together a private FB page called THE Kidney Stone Diet. It is a group that helps educate you on your physician prescribed treatment plans. As you can imagine, oxalate comes up in many posts. I moderate it to keep it clinically sound. Come on over and join the discussion!
URINE OXALATE AND RISK OF KIDNEY STONES
I promised you some science – here it is for those interested. It concerns only highlights from the food – urine oxalate research recently performed and seemingly germane to the problem of how stone formers should control oxalate intake.
The most useful data about urine oxalate we have so far is from three cohorts studied by Dr. Gary Curhan. Two are cohorts of nurses one a cohort of physicians. These people have kept track of many aspects of diet and health for decades, and among their records are onset of kidney stones.
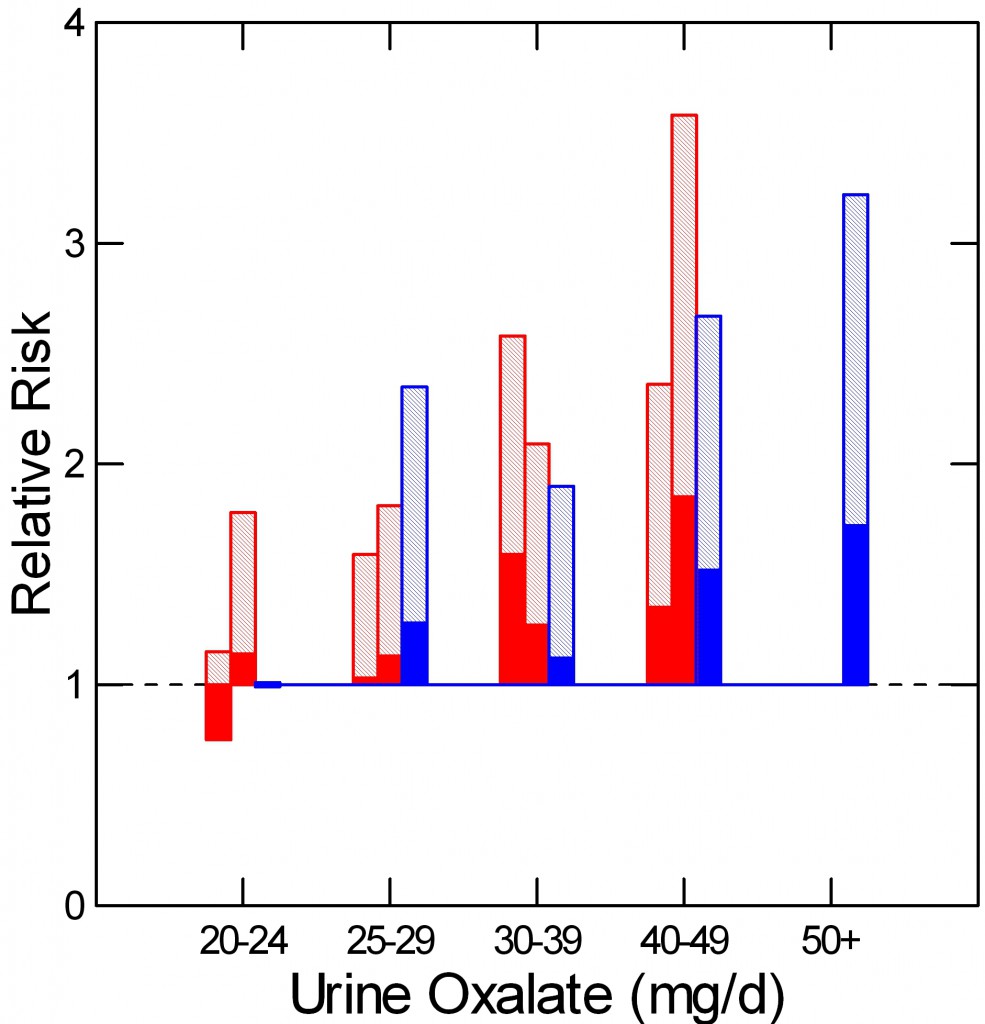 As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
The two nurse cohorts are red, the physicians – all men – are blue. The dotted line at 1 is the risk threshold: Above that line, risk is present.
The top of each crosshatched bar shows the mean relative risk for each of the five urine oxalate ranges. Clearly the mean goes up as urine oxalate goes up.
But the mean relative risk has a range of uncertainty around it. The bottom of the solid portion of each bar is the lower 95th percentile for that range of uncertainty. When that bottom lies above 1, risk is very likely to be present.
For both the women and men groups, that point is reached between 25 and 30 mg of urine oxalate a day. Therefore one wants to try to get urine oxalate below 30 mg daily and even lower, below 25 mg daily if possible. The average urine oxalate excretion among the women in this study was close – 26 and 28 mg/day for those who did not form stones and just a bit higher for those who did – 28 and 30 mg per day. The men are a problem: 39 and 41 mg/day for those who did not and those who did form stones.
This is not diet oxalate, it is urine oxalate. Urine oxalate is how much the body makes and how much is absorbed from foods. Mostly, we can control only the second part – how much is in the food.
HOW MUCH DIET OXALATE DAILY
All dietary advice depends on having a reasonable goal in mind for oxalate intake. My goal of 50 – 100 mg of oxalate from food daily is not unreasonable given the research that has been done in normal people and stone formers.
Holmes and colleagues found a urine excretion of oxalate of about 10 mg/gm urine creatinine in normal 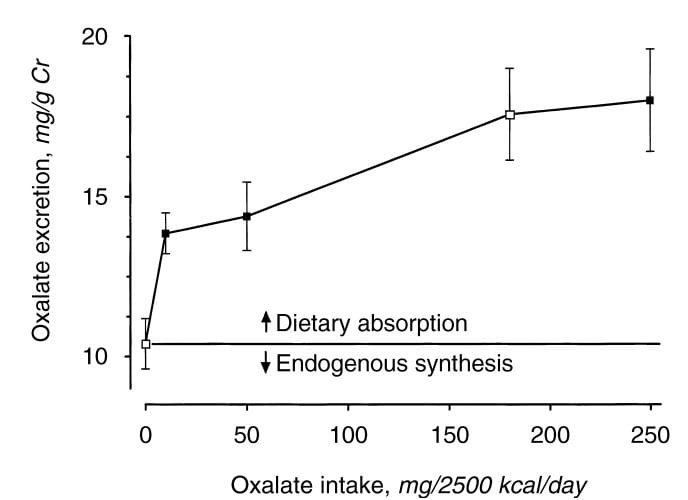 people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
From this work the percent oxalate absorption could be calculated as around 10 – 15% and the contribution of diet oxalate to urine oxalate excretion as around 25 – 40% when intake of oxalate was between 50 and 350 mg/2500 kcal. Therefore one can consider a whole food 1000 mg calcium 50 mg oxalate as a usable low oxalate diet, and a 150 – 250 mg oxalate diet as relatively high.
The balance between diet calcium and diet oxalate does not matter greatly if diet calcium is high. Among normal men and women eating 1000 mg/day of calcium and 750 mg/day of food oxalate, 24 hour urine calcium was about 110 mg/day and oxalate about 44 mg/day.
If the calcium oxalate balance is altered so calcium intake is 400 mg and 20 mg of oxalate at breakfast and lunch, and 200 mg of calcium and 710 mg of oxalate at dinner, as compared with simply 333 mg of calcium and 250 mg of oxalate in all 3 daily meals, urine oxalate is lower after the high calcium low oxalate meals, but only slightly higher after the high oxalate low calcium evening meal than when calcium and oxalate intakes were balanced. This means that when diet calcium is at least 1000 mg daily the balance of calcium to oxalate within any one meal is not likely to affect stone risk.
Seiner and colleagues make clear that stone formers are different from normal people. They divided male and female stone formers into 2 groups of 93 people each, one with urine oxalate above 0.5 mmol (~50 mg) of urine oxalate daily and the other with urine oxalate below 0.4 mmol (~40 mg) daily. They found virtually identical calcium and oxalate intakes: 845 vs. 812 calcium and 101 vs. 130 mg daily of oxalate respectively in the lower and higher urine oxalate groups. But the below 0.4 mmol group excreted only 27 mg of oxalate daily on average, whereas the high oxalate group excreted 64 mg daily. In other words diet was not responsible for the higher urine oxalate excretion, suggesting a difference of oxalate absorption. Those prone to high oxalate excretion seem, therefore, to most need diet modification.
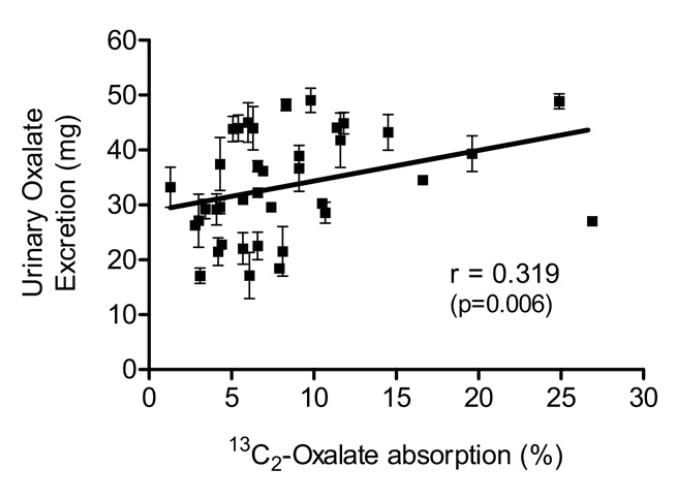 Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
PROTEIN AND GELATIN
Diet protein intake does not affect urine oxalate excretion. In 11 normal people fed a 1000 mg calcium, 51 mg oxalate, 3000 mg sodium fixed diet, varying protein intake from 0.6 to 1.6 gm/kg/day – a very wide range – did not alter urine oxalate appreciably (mean values were 23, 23, and 25 mg daily for the three protein intakes) even though oxalate precursors like glycolate rose markedly (25, 22, and 46, mg daily).
Jello is a source of hydroxyproline which converts to glycolate and oxalate, and oral loading with gelatin can raise urine oxalate. Ten normal people eating a 1000 mg calcium, 150 mg oxalate diet (typical normal level) were fed supplemental gelatin as one quarter of daily protein intake. Urine oxalate was 24 mg daily vs. 17 mg daily when the same diet was supplemented with whey protein – containing little hydroxyproline – as a control. So lots of jello is not an ideal plan for stone formers.
Where does this leave us about how much oxalate is alright for a day. If diet calcium is high, as it should be, at about 1000 mg, then one should try to limit diet oxalate below 100 mg daily. Perhaps this is most important in those patients whose baseline oxalate excretions are higher – in the range of above 40 mg daily.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life.
For those who need special help, I run an online course: The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.



Hi, While the spreadsheet of foodstuffs and their oxalate content is the best I can find on the web, it strikes me that the original Harvard list is now ten years old. Do the figures hold true, or have advances in science led to any revisions? I am particularly confused by the strawberry advice. The list shows them as low (2mg for 1/2 cup) while they are listed as a no-go on the advice provided to me on a recent hospital visit here in the UK. Regards, Doug.
Hi Doug, Dr Ross Holmes curated the list to update where possible, and has added incrementally since. He has not been concerned about strawberries as listed. He is about the best expert I can think of. Regards, Fred Coe
Hi Doug, Dr Ross Holmes curated the list to update where possible, and has added incrementally since. He has not been concerned about strawberries as listed. He is about the best expert I can think of. Regards, Fred Coe
I am wondering what the consensus is with soy milk? The article states that it has a high level of oxalate (20 mg), but the attached spreadsheet Oxalate Content of Foods By Food Type shows that it is of low oxalate content (4 mg) on line 384. Also, a Pubmed article (https://www.ncbi.nlm.nih.gov/pubmed/15998131) published in 2005 showed that 2 brands of soy milk did have lower contents. I was not able to access the article and see which brands. I’m not sure if the entry on line 384 was a mistake, but I would love to hear your thoughts on the matter!
Thank you!
Hi Janet, I think Jill should answer this one. Obviously soy milk oxalate varies or labs vary. She is the expert on these foods. Regards, Fred Coe
Hi Janet,
Even though you may see varying numbers on the same type of food, it is believed soy should be avoided if one is following a low oxalate diet. I would use it sparingly if you must use it at all.
Warmly,
Jill
Tums or similar antacids are high in Calcium (400 mg per tablet). Is that a good source of Calcium to counteract oxalate? Of course real food is usually considered preferable to pills, but I take Tums anyway for another purpose, so was wondering if they help do the job vs kidney stone formation. Many thanks.
Hi Daniel, Great question. I did not propose supplements but use them in real life. They will lower urine oxalate but only if timed WITH the meal, not before not after. The calcium needs to be in the bowel when the oxalate is. You would need 2 of them for two big meals, but 1000 mg of daily calcium is more or less lower level for US people. Did you see the other oxalate article? REgards, Fred Coe
Hi, and thanks for such an informative article! Dr. Gerber just removed a 2.5 cm stone, along with some smaller stones, from my left kidney. I am also a patient of Dr. Pekoe for Crohn’s disease. I have had 2 bowel resections and am currently asymptomatic with no meds. I am now taking regular calcium supplements, but do you know if I would be at higher risk due to the bowel resections? Thanks again!
Hi Michael, Indeed you are and need rather specialized care. I have not written about small bowel resection stones but you should consult with an expert on stone prevention as the condition is complicated. Regards, Fred Coe
If calcium goodies are to help aide against a high oxalate food, then why is chocolate milk considered high?
Hi Britney, Smart question. Chocolate additives have a lot of oxalate. But being milk and loaded with calcium the product is very unlikely to increase urine oxalate so it is safe. Regards, Fred Coe
So I recently removed (surgically) a 9mm stone and the urologist told me it was a calcium stone. I am a bit confused as to whether it’s a calcium oxalate stone or simply a calcium stone, and does this mean that I need to avoid oxalate foods? Also, is it ok to have soymilk/almond milk being that these are loaded with calcium and I would be needing calcium to bind the oxalate before it gets to the kidneys for urine formation? Please shed some light. Thank you.
Hi Marsha,
There is no such thing as a “calcium” stone. They are made of calcium and oxalate or phosphate. Please ask your doc which one he/she removed from you. He then needs to order you a 24 hour urine collection and fasting blood draw to see WHY you are making stones. You can begin your treatment plan at that point and see if you do indeed need to lower your oxalate. You may not have to do that. Check with doc about testing and based upon those results they can get you on treatment specific to those results.
Best,
Jill
im having pain in the left side abdomen down just above urinary tract and it has 6mm stone,but how to whether it is calcium oxalate stone or uric acid stone?
Hi Bala, You can tell when it has passed – get it analysed. On CT the radiographic density of uric acid stones is low – your physician can measure it easily. Regards, Fred Coe
How long does a stone take to form? I have four 4mm+ stones and I’m wondering if they were formed when I was on a diet plan based on soy potein. Thank you!
Hi Steve, if calcium oxalate, certainly many months. If uric acid, as fast as in weeks. From the nature of the diet I suspect the former. Check out the stone type with your physician. Regards, Fred Coe
I came to this site because and organic acid test (am sample) showed 5x hgher than reference for oxalic acid. I do have osteoporosis and years ago had a tiny kidney stone (that has stopped bothering).
MIght there be pdf instead of those excel files?
Other sites don’t list avocado or olives as high. Who are we to believe? Odd that scientist can’t agree on the oxalate content of foods.
This “oxalate content guide” is significantly different in some areas: http://www.urinarystones.info/resources/Docs/Oxalate-content-of-food-2008.pdf
Pretty much all my favorite foods are high in oxalates according to this website info ( avocado, rice crackers, pecans. almond butter, cashews,olives, sweet potatoes). What about coconut milk? It’s a staple of mine so I’m guessing it’s high, right? What about whey protein?
Sorry, this news is making me grumpy!
Hi Sally,
I get that all of this makes you grumpy. We use the list we do from Harvard and trust it because our patients, when they use it and listen to our advice on how to use it, usually lower their urinary oxalate. Different parties have different values bc depending upon where the plant was grown and the soil conditions, values can vary.
It is important to get dietary help so you can safely incorporate your favorite foods. There are so many you can have, even the higher ones. The only two I take away are spinach and rutabaga…otherwise you can learn to eat most others. Remember to look at portion size when you are reading our list. You can have all your favorites, just watch portion size.
Coconut milk is ok, my patients use it and absolutely have lower oxalate values on it.
Hope this helps-
Jill
Thanks for your quick reply Sally.
Since oxalates are high in rice chips (rice flour), potato chips, corn chips AND the table said plantains have almost NONE, I went out and bought plantain chips.
I want to doublecheck so I google “plantain oxalate” and first hit says plantain “Very High”. ??? Maybe they are right — I’m feeling that familiar sting/burn in my flank after eating the plantain chip with brie.
So depending on where the plantain, avocadoes and olives are grown, they’ll have (drastically) different oxalate concentration? There seems to be consensus on spinach, rhubarb, lamb’s quarter, sorrel, chocolate, nuts but not much else.
I guess you see this kind of frustration often? Thanks for the info re coconut milk — that’s defintely helps.
It would be nice if someone would develop an oxalic urine dip stick so we could test food/meals ourselves.
What advice do you have for someone following a vegan diet? Everything seems to be high in oxalate. Help
Hi Eva, Jill Harris needs to answer this one. Regards, Fred Coe
Hi Eva,
I suggest you work with someone who can help guide you. It can be difficult but very doable. I have helped many vegans decrease stone risk. If you look at your list there are still many foods you can eat and many non dairy calcium fortified foods to help you. Perhaps if you decrease the portion size of the high oxalate foods and get enough calcium in your diet you will see that there are many foods you can still safely eat.
Do you know your oxalate value? Have you done 24 hour urine testing?
Let us know-
Jill
Hi
I recently had kidney stone and was diagnosed with anemia due to very low iron and lack of almost all B12. I should add I have been a vegetarian for 42 years.
Can any one help with a diet that would be low in oxalate but high in iron with no meat but I do eat dairy.
thanks in advance
Hi Gaby, This is so complex! I would contact Jill Harris, who wrote the article, and talk to her directly. She runs courses on stone diets. Perhaps you might even consult with her personally. Her site is linked to the article. Likewise, being anemic, you need your personal physician to be sure nothing more is wrong than your diet. That is imperative. Regards, Fred Coe
Is liquid stevia (not the powdered in packets) considered high in oxalates also?
Hi Mary, the plant extracts have oxalate the chemical has none, so the label will tell you. Regards, Fred Coe
Thank you! The label reads Stevia Leaf Extract 50mg. (standardized to 90% steviosides)(Stevia rebaudiana). Not sure how to interpret it? Thanks for your help!!
Hi Mary,
Once the leaf is processed there is no longer any oxalate.
Hope this helps- Jill
I am so glad for the updated version of the Low Oxalate Diet. My Doctor gave me the one that is outdated from UPMC. But here I see that Stevia is high! I use it everyday in my coffee. I have Type II Diabetes so what can I use? Monk Fruit, Coconut Sugar, Erythitol or Xylitol??? Also I do not see a lot of herbs or spices on your list. Can you help?
Thank you.
Hi Jennifer, Stevia plant is high, chemical stevia is free of oxalate. Just use it not the plant. Best, Fred Coe
Hi Jennifer,
We don’t have much info on spices. I do know that turmeric can be high. Just use spices normally and you really should not have too much issue. Worry about the highest oxalate foods and eat foods that contain calcium and get your daily requirements of it- 1,000 mg/day for premenopausal women, and 1,200 mg/day for post menopausal women. Do not go over the limit, just up to.
Best,
Jill
Hello Dr. Coe and Jill,
Thanks for all the great info on this site.
I have a doubt about my kidney stone’s rate of growth.
It is located in my left kidney. In December 2015 it was at 1.2 cm and in May 2017 (17 months later) it was at 1.5 cm.
Will it continue to grow at the same rate? If left to itself, how long before it fills up the entire kidney?
Roger
Hi Roger, the growth of your stone is not ideal and it is large. Be sure you know what caused it, and get treatment. As large as it is I would consider removal – discuss with your urologist. If so, be sure it is analysed. Here is a good plan. Yes, stones will keep growing until you find out what causes it and fix that cause. Surgery is not ideal until that is accomplished. Best, Fred Coe
Hello. Thanks for the great information. I have had kidney stones that show up on an Xray and passed a painful one a few years ago. ER didn’t test stone, so don’t even know what I have, but assume it’s oxalate since I notice my entire body hurts with too many oxalates. I had also quit dairy at the time. They told me not to worry about oxalates after the stones, now I have them showing up in my utterer on both sides. Am lowering oxalates and I feel better in my pain levels all over, and in pelvic region. I have mast cell disease and POTS/dysautonomia. I get dehydrated often and have to go in for hydration IV’s. But not getting enough salt and potassium. I just made a concoction of salt and potassium, and I was able to hold fluid in my body today, but am concerned about stones. If we are low on sodium, is extra going to hurt most kidney stone patients?
Hi Maiysa, If you do not eat adequate calcium, urine oxalate will rise, so your diet change sounds less than optimal. Take a look here. You need 24 hour urine studies to figure out what might be causing stones, and you need analyses of the stones in your ureters. Here is a good beginning article. Figure out the cause – testing and help from your physicians, then pursue what you need Regards, Fred Coe
This is the best, most useful, scientific but easy to follow site I’ve seen on this subject, thank you very much. A couple questions:
Why is canned pineapple high, but not fresh? Because it’s usually “in heavy syrup?” I eat canned in “100% pineapple juice” so is it okay?
Also, why is orange juice okay but not whole oranges? Because of the pulp? Should I get “no pulp” OJ?
Hi Laura,
I am so happy you are finding the site helpful. Canned pineapple can be assumed high because of the syrup and the oranges are higher because of the rind and pith.
Hope this helps! Jill
Hello, thank you for this website! Through your i have found that I was, for maybe a year or more now, consuming a high oxalate diet. I ate, nearly every day, an entire avocado, one raw carrot in my salad, potatoes in moderation, a cup of blueberries, but the kicker is…at least one cup or more of mostly almonds, some walnuts and lots of pistachios and recently added peanuts. I also avoided dairy and blood calcium was low. I passed a 4 mm calcium oxalate stone last month! I am 60 in otherwise good health. If I ditch the nuts, vary my diet, add calcium, and avoid high levels of high oxalate foods…are my chances of avoiding stones pretty good? Or did I damage my kidneys, now making them prone to stone formation?
Hi Anne, Sounds like diet may have done you in. Here is a good summary of the kidney stone diet. It is identical to the present ideal US diet. It should certainly help. Be sure and be evaluated properly, not just run from remedy to remedy. Regards, Fred Coe
Thank you for all this information. However, I am puzzled by the mention of tofu, which is, unless I am mistaken, also very high in calcium. Would it not make it safe?
Hi Francois,
Yes, tofu is high in oxalate and calcium. Sometimes the oxalate is too high even if it has calcium. It is not worth the risk.
Warmly,
Jill
Hi,
I’m confused, you write that hot chocolate has 65mg/cup of oxalte and that chocolate milk has only 7mg/cup.
Does the heat somehow increase the oxalate levels ?
Hi Mike,
I would think that it is the type of cocoa used for each and the concentration. Heating does not matter.
Thank you for writing!
Jill
I am reading ‘Nor More Kidney Stones’ by John S. Rodman, M.D. He has avocados as low oxalate and ‘eat as desired’ and you have them as high oxalate. This is getting very confusing. Other sites have avocados as low oxalate and they are very alkaline. So, what’s the story? I do not know, yet, what type of stone I have and am having surgery in a few days. But, I’m trying to maintain a decent diet.
Hi Karen, You do not know your stone type nor the results of your 24 hour or serum evaluation for stones, so I would not fret about oxalate just yet. Here is perhaps a useful idea – the kidney stone book section, especially chapter three, is a good introduction to how you might want to think about things. An orderly approach works, but it does take some time. As you get the stone analysis and a proper evaluation together things will settle out and you can focus on that will do the best for you. RIght now, random efforts to generally improve matters have a low probability of success. REgards, Fred Coe
Why do some lists have avocados as very low oxalate, and this list has them as very high?
Hi Heather, I am asking Jill Harris to comment on this. Thanks, Fred Coe
Hi Heather.
A very popular question. Every list will say a bit different. That is why we say stick to one list. Avocados can safely be eaten. They are listed as high on the Harvard list but are only 19 for the whole fruit. You can eat up to 100 mg/day of oxalate. So eat them. They are very healthy. And get your calcium requirement too as we talk about on this website. The calcium blocks absorption of oxalate so you do not need to be so stringent. You will be fine!
Jill
So when you say “whole fruit” of the avacado are they measuring the oxalate content of the skin also in this test? Thank you
I just passed a stone, but I don’t know what type. I assume it was oxalate because I had been eating huge amounts of nuts and seeds and high oxalate vegetables I cannot tolerate milk products and have read that calcium supplements can cause heart problems. I take vitamins D and K, but I’m still concerned about taking 1000 mg of calcium. I have a lot of food sensitivites, so it’s difficult to go low oxalate. I have lowered my calcium intake down to 600 mg/day in an osteoporosis supplement because I have that, too.
Hi Janice, Here is a good source article about the kidney stone diet. It matches point for point the diet recommended for all Americans. So none of the recommendations cause harm. But you are jumping to conclusions and I would advise a more measured approach. Try this. Regards, Fred Coe
To clarify earlier discussion, sugar or stevia in my tea? We buy Truvia packets from the store. The Truvia ingredient statement says, “Erythritol, stevia leaf extract, natural flavors.” A recent response said, “Stevia plant is high, chemical stevia is free of oxalate. Just use it not the plant.” So is stevia leaf extract considered the chemical stevia that is free of oxalate? Many thanks.
Dear Daniel,
Having truvia is fine.
Jill
Nice list, but very limited choice for carbohydrates, and the acceptable ones are all white starch. Absolutely floored about pasta.
Hi Francisco,
You can still eat carbs. Remember you have 100 mg/day of oxalate in your bank and you can choose how you want to spend it. Eat normal portion sizes and get enough calcium and you will be fine. Make sure you do indeed have to limit oxalate by doing a 24 hour urine collection.
Thanks for writing-
Jill
Question
I have Gout and concerned about Calcium intake
Can I use flax seed flour to help clean out my system
Making homemade juice with lots of water will with this help me? Very concerned???
Cucumber
Ginger medium amount
Turmeric medium amount
Parsley
Onion
Cayenne
Cinnamon
Garlic
Beets small amount
Flax seed
Potato starch
Lemon
Lime
Apple cider vinegar
Lots of water
Can you comment – very concerned
Hi John,
Concerning gout, lower your animal protein intake to lessen uric acid levels. Use dairy products to get your recommended calcium levels increased to about 1,000 mg/day. As far as your juice- are you using all those ingredients to make it? I am not sure what you are asking.
Let me know-
Jill
If I use a calcium supplement to help achieve the recommended calcium levels, is there an advantage to using an immediate release vs an extended release tablet?
Hi Jim, I have no way to help decide as no trials have compared them. Use either. But be sure to take in the calcium with your main meals. Not between meals and never fasting. Regards, Fred Coe
This list has blueberries as low oxalate and every other list has them as high oxalate. Can you help explain? Thank you
Hi Scott, I will ask Jill Harris to respond to these two questions. Regards, Fred Coe
Hi Scott,
I am assuming they mean whole fruit, not half and skin is not included.
Warmly,
Jill
Hi Scott,
Harvard does list them as low and I do have my patients eating them. My patients that do eat them usually pair them with a dairy product like yoghurt and still remain with lower urinary oxalate. You see many differences from list to list as plants are studied from region to region and have all been grown with different soil conditions. Can be confusing. We use the Harvard list as we have found great success with it. When following it, along with our other dietary advice, patients can and do decrease their risk of new stones.
Hope this helps,
Jill
Thank you for this informative article. I suffer from Fluoroquinolone Toxicity and recently discovered that fluoroquinolone antibiotics can eradicate oxalobacter formigenes in the gut, leading to an inability by the body to process oxalates. The healthy, organic diet I intended to follow for recovery included a lot of oxalate-high vegetables, nuts and supplements (e.g. vit C). Obviously I don’t want to risk ruining my body even further with this. My questions are the following:
1. Would a urine oxalate level test show my body’s (in)ability to process oxalates, much like with kidney patients?
2. How soon after o. formigenes had been wiped out, would the effects start to be felt/noticed/show up in e.g. urine?
3. As far as I understand, there’s currently no way to repopulate o. formigenes through probiotics; would a fecal microbiota transplant work?
Thanks.
Hi Bram, I gather you cannot take fluoroquinolone antibiotics so their effects on gut flora seem less than fully relevant to your health. I presume you once used them and are asking if might have erradicated oxalobacter. They may. But the links between O Formigines and even stones is weak, and the science mediocre so I have little concerns. Eating a high oxalate diet could in theory raise risk of kidney stones, but eating a high calcium diet will act in the opposite direction. I would guess the ideal is to moderate your oxalate and be sure ande follot US guidelines about high calcium intake. As far as repopulating, there is not a shred of evidence that O formigines matters to human health, and scarce data it actually related to stones. Regards, Fred Coe
Hi Bram, You are wasting your valuable time on this problem as it is not a problem for you at all. In theory, with little real data, some have suggested this bacteria or its lack matter for patients with calcium oxalate stones. You do not have such stones. If you wish have your urine oxalate measured, but no medical reason exists to do that, nor would anyone have reason to suggest you should change your diet or life on such a basis. Regards, Fred Coe
Esteemed Dr Coe, I meant to say that I suffer from long-term side-effects (tendon issues, neuropathy etc.) following a fluoroquinolone treatment, that (like you say) may or may not have eradicated my o. formigenes. Some studies do indicate that o. formigenes and stone formation are indeed linked; hence my concern about potential eradication.
Let me rephrase my questions: if for whatever reason (regardless of o.formigenes involvement) at any point my body became less capable of processing oxalates,
1. would this automatically show up in a urine test before any damage is done?
and 2. how long before this hampered ability to process oxalates would start negatively impacting my health?
Hi,
Should we be looking at Oxalate to Calcium ratio rather than purely the oxalate content of a food before deciding whether it is good or bad?
Take for example Soybeans. It has high oxalate 96mg/cup – which is about 1.09 mmol of oxalate. But it also has high calcium – 175 mg/cup for boiled soybeans – which is about 4.375 mmol of Ca. Wouldn’t the high calcium offset the oxalate in the gut? Based on this can we conclude that soybeans are actually safe?
Please let me know if my logic and calculations are correct or if I am completely missing something.
Thanks
Hi Josh, Good thinking and good calculating. The problem: As foods are digested, the various constituents become active. If some of the bean proteins or other molecules begin to bind calcium, oxalate may well slip through. So only feeding trials give real data, and no one wants to pay for them. That is the problem. Put another way, too risky without good data. Best, Fred Coe
Hi. I took a Litholink test recently. My SS CaOx result was 6.00 which is sort of mid range according to their graph. Should I be trying to get this number higher for decreased risk of kidney stones? And do I do that by eating more Calcium (as well as eating a low oxalate diet)?
Also, my Urine Calcium score is 181 mg/day. That score has been going up in test results over time as I deliberately eat more Calcium. Is that good or bad? Thank you so much.
Hi Daniel, You want your supersaturation lower. The higher diet calcium is part of an entire diet structure: High calcium reduces oxalate absorption, low sodium keeps the urine calcium from rising. Both need to be in place. The calcium needs to be with the meals that have oxalate in them. Highest oxalate foods need to be avoided. Fluids high. The goal is to lower supersaturations. Your urine calcium is normal, you do not give your urine oxalate – is it high? Take a look at a full scale plan. Best, Fred Coe
Thanks for the feedback. You asked about my urine oxalate. Over the past 4 years my Litholink results have been 56, 46, 97, and 81 (most recent 8/23/197). So they are generally high. The 97 may have been an anomaly since other scores that day looked a bit off too, especially my urine citrate of 174. Perhaps something I ate just prior to or during the test period skewed the results? Regardless I need to follow the regime you reference.
Hi Daniel, Values that high and that variable are from diet, but almost certainly from low calcium diet. If you were eating the 1200 mg of diet calcium you need, oxalate absorption would rarely get so high as this – I presume you do not have GI diseases or obesity surgery. So I would consider that in planning for the future. With low calcium diet, oxalate loads promptly raise urine oxalate and post a hazard for stones. You need the entire ensemble as you already noted. The diet calcium needs to be in the meals that contain appreciable oxalate. Regards, Fred Coe
Thanks for the feedback. I am lean and otherwise healthy except that I do have GI disease (diverticulitis and bacterial overgrowth of the small intestine) that is being treated. Previously, I have had to get iron infusion treatments because nutrient absorption in my gut has been reduced. I have been under treatment with antibiotics for several years and am improving to feel almost normal. However, the GI issue may explain some of my Litholink scores. I do eat a lot of calcium in my diet. Perhaps only a fraction is being absorbed into my bloodstream, so I need to eat more calcium than normal.
Hi Daniel, I am suspicious you have malabsorption and that is why oxalate is so high on and off. Iron absorption is abnormal, you need antibiotics etc. Ask your physicians if they might consider this possibility and evaluate it. Regards, Fred Coe
Thank you for this site and the updated list. I noticed the updated list now has Soy Milk twice with different values. The updated value is under Beverages>Soy milk and lists 20mg per cup. However, the old Harvard value is still under subcategory Beverages>Dairy Beverages>Soy Milk as 4mg per cup. I mention in case you wish to remove the old value as was done with the other updated values.
Hi Lex, thank you. I have asked Jill Harris if she could correct this. Regards, Fred
I have had gastrci bypass surgury and now get oxilate kidney stones…..any addtional info for those of us that have done this?
Hi Julia, Indeed weight loss surgery does lead to calcium oxalate stones. I have not as yet written about the matter but will do so. It is usually from excess urine oxalate. Treatment with high calcium with meals, or even supplements with meals can help. Your physician may be able to help with this strategy. Best, Fred Coe
I have osteoporosis so am trying to increase my intake of calcium esp. from leafy greens such as kale and other vegetables as well as diary foods. Oxalates interfere with the absorption of calcium so I try not to take them at the same time. Wise or not
Hi Jen,
Not wise. When you are eating foods high in oxalate, you need to eat calcium with the product to lessen the absorption of oxalate. Do your best to eat at the same time otherwise the calcium will not help. You are making the oxalate issue worse (if that is a problem for you).
Hope this helps,
Jill
Most lists place popcorn in the high-oxalate category yet you mention that one cup = 5mg. Since I eat microwave, butter-less, salt-free popcorn daily I’m interested in knowing how safe it is for me to continue eating since I just underwent lithotripsy surgery 2 months ago. Thanks
Hi Jack,
My patients eat popcorn as a snack and still remain on a low oxalate diet. Will be fine!
Jill
I am confused with multiple issues. I am obese, I have high cholesterol, and htn. They recommend low fat, low cholesterol, low animal protein and fat. I kidney doctor says low salt, low oxalate, calcium. For kidney infections low animal protein. How do I do all this at the same time?
Hi Debbie-
You work with someone who can help you figure this all out as it can be complicated as you already know. I certainly can help as I do this for a living. You can go to my website and get private coaching with me to help you sort everything out. Go to: jillharriscoaching.com
Warmly,
Jill
Hi Jill, I noticed there is allot of contradiction among researchers on what foods have high oxalates or not, I read on one site, when looking to find out if avocados were high in oxalate or not, the site I went to said they were low, the list you provided said they are high, I’m curious to how researchers actually come up with the mgs from each of the listed foods, do they actually test each of these foods to see the amounts of oxalate are in them. Why is there so much contradiction among researchers and how do we as kidney stone suffers know which lists are accurate or not, thanks for any help you can provide.
Hi Jimi,
Depending on where the plant was grown, the growing conditions, etc the foods have different amounts. We trust the list by Harvard as we have been helping patients from it for many years and they tend to lower their urinary oxalate. Along with adding calcium from foods back into your diet. Please remember not just to read the words, high, very high, low. Avocados are listed as “high” on the Harvard list but if you look at the actual number 19 for a whole one, you can safely incorporate them into your diet. Sunflower seeds are listed as “high” but 22 mg for one whole cup is not bad and who the heck eats a whole cup. See what I mean?
Jill
Hi Jill, is there a source for oxalate content that actually gives the weight of the food rather than, e.g., “1 fruit”? Milligrams of oxalate per grams of the food would be ideal. Also, any idea about oxalates in extra virgin olive oil? Thanks.
Hi Craig,
Not too worried about olive oil in general. Our list is the one we like, and how it is listed it how it is listed. Most of the time you don’t even have to worry about oxalate, except for the very high items on the list if you get enough calcium.
Jill
The frustration about this “diet” (which I am trying valiantly to follow after two bouts of kidney stones in 3 years) is that it seems as if I have to choose heart healthy (e.g. brown rice, whole wheat bread, etc) and low oxalates. In addition, my ENT doc wants me to cut out all calcium as it causes reflux and closes my throat! Hard to know where to go with all of this!
Hi Mary, Be sure you need the diet – it is much overprescribed. High diet calcium can reduce oxalate absorption and make diet oxalate issues a lot less stringent. Your ENT doctor has his eye on one place but you have a skeleton so a low calcium diet is not safe. As well, I am not so sure about calcium foods per se causing reflux, but if it is you can use calcium supplements with meals. They can work if taken with larger meals and will not cause reflux. They will reduce oxalate very strongly. Here is the correct kidney stone diet, which is identical to the diet recommended for all US people. Regards, Fred Coe
I am lactose intolerant and a vegetarian. What are alternate sources of calcium?
Hi Judy, This is best for Jill Harris to answer. She will do so. Best, Fred Coe
Hi Judy,
You can find some fortified flax milk, coconut milk, and oj as well. You can google non dairy sources of caclium and make sure they adhere with your other diet restrictions as well.
Hope this helps,
Jill
Judy,
Coconut yogurt as well. There is one called So Delicious coconut yogurt that has a nice amount of calcium in it-jill
I did not see anything about gluten free products. I have printed the harvard list and plan to follow it as well as sign up for the course. Today is first shopping trip using the list, just want to be sure. Thank you
Hi Holly, Gluten is in wheat products that contain little oxalate. Be Sure you need this diet. Take a look here before you begin. Regards, Fred Coe
Does taking Calcium supplements help with trying to increase ones calcium intake to help with oxalates?
Hi Mitchel, Yes. If supplements are taken with the larger meals that contain oxalate they reduce oxalate absorption and urine oxalate. High calcium diet is necessary for bone health and is part of how idiopathic calcium stones are best treated. Regards, Fred Coe
I knew I had kidney stones from a CAT scan 7 years ago when my neuroendocrine cancer was discovered. I wish I would have paid attention to that information at that time…now 7 years later, been trying to stay healthy mostly on Ketongenic type diet for cancer (NETS in my liver right now), and thought I was doing well, but had first kidney stone attack Saturday. I have a stent in and will have to have a large 7mm removed next week. I now have to adjust my diet once again from raw, leafy greens, nuts, almond butter (that I love!!!) to low oxalate which I am assuming I would benefit from based on things I am reading. I will hopefully get feedback on the stones. I have many more in my kidney. I also have Osteopenia. Any thoughts for me? I had stopped taking calcium supplements awhile back, was just taking magnesium glycinate and D3. Will I be able to get concrete answer on what is causing my stones from Doc…what should I be asking?? Thank you
Hi Carrie, A low oxalate diet is rarely the right approach per se. Get a full evaluation and treat accordingly. The osteopenia is complex because of the tumor – what is the specific type. I presume it is islet cell. Those tumors have no special relationship to osteopenia. I would read the linked article and get it all done. THe evaluation will point to what to do. By all means do not trash about doing this and that remedy – recipe for failure. Regards, Fred Coe
Once again, it seems a mistake is made on the recommendation. Here are some low oxalate options in this category: White rice, hummus, corn flour, corn bran, flax seed, and oat bran are popular and safe” Hummus is one of the worst possible choices given it is made with tahini and garbanzo beans. This is so frustrating.
Hi Ann,
Thanks for writing. Please remember that this is always about portion size. So you will see hummus as “low” but the amount listed is on 2 tbs. That is not a lot. The more you eat the more oxalate will be in it. But for the serving size it is “low”. Hope that makes sense. The item though, is correct.
Warmly,
Jill
Hello, great site, thank you for the great information. I’ve been eating a small kale salad with tahini dressing, and often for dinner I’ll have a sandwich with hummus instead of mayonnaise. Should I disregard one or either of these spreads considering how they’re used? I was under the impression they were safe at low quantities, but I’ve seen different opinions on both of these. In fact, some places state that kale should not be a part of a low oxalate diet but I’ve seen otherwise stated here. Thanks for your help.
Hi Bill,
I know that all these lists can be confusing. We stick with the Harvard list bc we have used it for many years, and along with our other advice, our patients do indeed lower their urinary oxalate levels. Always remember the amounts you are using and how often. Remember to incorporate calcium into your diet as well. Tahini is on the higher side in regards to oxalate so why not do an oil and vinegar on your salad? Make sure you need a low oxalate diet too!
Best,
Jill
Thank you Jill. I’m puzzled why tahini is on the list but elsewhere it’s recommended to use hummus as a spread, which contains tahini as an ingredient. Is it because of the small amount used that hummus isn’t frowned upon? Also, is kale indeed a good substitute for other greens?
Hi BD,
You can sub out kale for spinach. You can totally eat plenty of other veggies on the list. Tahini is high, but little is used in the portion size of the hummus that is given on the list. Meaning 2 tbs of hummus is low, but who is only eating that much hummus. Watch portion size and mg of oxalate instead of just reading the adjective that is listed. It is more work than that.
Since there is just a little bit of tahini in the 2 tbs of hummus that is the reason.
Thanks for writing,
Jill
Why is corn ok to eat, but cornmeal is considered high in oxalate? Cornmeal is nothing more than ground corn.
Jan,
This is typically because of the concentration of the item.
Jill
This is American based information can you tell if it is also applicable to Australian foods apart from the obvious US brands ?
The foods themselves will be the same. Brands, not so. Regards, Fred Coe
Hi,
I found this information about cocao powder and its oxalate content and that is only cooked oxalic acid combines with calcium to form oxalates that can accumulate in the body. Is this correct – see info below:
‘The many raw cacao benefits are also called into question when people learn about its oxalic acid content. Oxalic acids can accumulate in the body blocking calcium absorption, causing kidney stones and other forms of calcification. It should be noted that many other common foods can contain up to 10x the amount of oxalic acid as chocolate. When you compare how much chocolate people eat at once (a few grams at most) to the amount of spinach (which is high in oxalates) that can be eaten, it becomes absurd to be afraid of this factor that’s present in cacao beans. One of the cool facts about chocolate in it’s unheated state is that the oxalic acid is harmless since only cooked oxalic acid combines with calcium to form oxalates that can accumulate in the body!
http://www.secrets-of-longevity-in-humans.com/raw-cacao-benefits.html
Thanks, Christina Stephenson
Hi Christina, In moderation dark chocolate is fine. If the chocolate has milk I imagine the oxalate absorption will fall – no data I know of. I do not know the paper showing that uncooked food oxalate is somehow different. Could you provide a link. This link has no data in it, only summary. Regards, Fred Coe
Thank you putting these lists on line! The information has been very helpful. I have been preparing oatmeal for my breakfast with apples & dates. The recipe is 1 1/2 cup oats, 1/2 cup chopped apples and 5 chopped dried dates boiled in 3 cups of water for 5 to 10 minutes. I was wondering what happens to the oxalate? Does cooking the dates remove it? Also, I have seen avocados on another list that indicates that they are high in oxalate. Thank you in advance for your reply. K
Hi Kristin, Cooking the oxalate will not alter it. Avocado is not remarkably high in oxalate – it is all about the portion size. But note that your dates have a lot of sugar in them. Even so sounds delicious; I doubt it will cause stones. But – be sure you have evaluated your condition; mere oxalate lists are nothing much. Prevention needs a lot more thought. Here is a good guide. Regards, Fred Coe
I am a type one diabetic and have been drinking a low calorie/low sugar lemonade that is sweetened with a small amount of cane sugar along with stevia leaf extract. I see stevia (1 tsp. serving size) on the list of high oxalate foods and products and am wondering whether this is something I should be concerned about. There is no indication of the amount of stevia leaf extract that is used in the mix. I struggle to drink sufficient quantities of plain water with little to no flavor and have been trying to avoid drinks sweetened with artificial sweeteners such as aspertame.
Your thoughts?
Thanks,
John
Hi John, chemical stevia has no oxalate at all. Avoid the leaf because it does have oxalate. Most products use the chemical. Regards, Fred Coe
My urologist tells me to add Crystal Light lemonade sticks to my water because it adds citric acid . He tells me to make sure every bottled drink that I buy has citric acid in it. How does the citric acid help?
Hi Lynn, Crystal light is a way to get potassium citrate without buying expensive pills. It is the best source of it among commercial drink products thus far. I presume your physician wants to raise your urine citrate. Perhaps the best place for you to start is here, and see if you have been fully evaluated and are being treated for diagnosed disorders. Regards, Fred Coe
Oxalate lists contradict each other. The most obvious are for stevia, kale, green beans, avocado, brown rice flour, grapes, summer squash, broccoli, carrots, parsley, kale, collards, and yams. These are on some lists as high and other lists as low. I have a University of Pittsburgh Medical Center List, (4 pages) & your list, & one from the website http://www.lowoxalate.info. (9 pages) & another list of high oxalate foods only, related to UPMC
I believe the problem of vision decline is from oxalates = autoimmune, therefore the information is crucial to know which foods to completely avoid. How do I know which list is the most accurate? Thanking you in advance for answering this question.
Hello Bea,
Oxalate lists can be very contradictory. We like to use the list from Harvard because it, along with the other advice we give to patients, helps lower their urinary oxalate. We have had great success with this list for years so we stick by it. I tell patients to stop looking at every list. They will vary as plants grown in different places, with different growing conditions, etc may have different levels of oxalate.
Pick one list, stop pulling your hair out and follow all the other advice stone patients should and you should be on your way to prevention. If you need more help you can always find me at jharris1019@gmail.com
Warmly,
Jill
I have a stone of 8.6mm stuck in the VUJ of right kidney. What is the likelihood of it passing out on its own , ofcourse with the help of medication and some home remedies? The first time I was detected a stone was in March of this year which was 3.6 mm in right kidney calyx. Since then I had 6-7 various USG out of which twice it failed to detect any stone; while rest of the tests it showed stone at various places of various size. I am not sure if it is the same stone that has grown from 3.6 to 8.6 or a new one. It is six months now. Should I wait to pass or get it operated?
Hi Wally, that large a stone has a low probability of passage. The big concern is obstruction. I would ask your physician if ureteroscopic removal were not a good idea. Likewise given its location, if there is any obstruction presently. Regards, Fred Coe
The stone size is 7.8 now according to last USG and is sitting at the tip of VUJ without obstruction.
Hi Wally, Given no obstsruction, timing of a procedure is entirely up to your surgeon and you. Regards, Fred Coe
Thanks ! So first things first. I passed the stone last night after I developed burning and pain down the bladder all of a sudden. It was indeed a nightmare for past 8 months when the stone grew from 3.6 to 8.4. Some tips of what I did, may be helpful for others. Although there is nothing new.
1. Lots and lots of water
2. A glass or two of warm water with lemon and honey in the morning
3. A glass or two of horsegram waterin the morning. Horsegram is widely available and used for cooking in India with various names e.g. kulith, mudhira. Soak it overnight and drink it down the next morning. Sometimes I boiled it for about 45 minutes to reduce 1 Ltr to half Ltr.
4. Coconut water
5. 2 bananas every day
6. Half Kg watermelon every day
7. Orange, Sweet lime, Pineapple and sort of fruits
8. Avoided spinach for entire 6 months
9. Of course medication – homeo, allo
10. Exercise, that helped the stone move down the ureter. I was told that a stone of this size i.e. 8.4 are least likely to pass on its own.
Point 2,3,4 were randomly exchanged and haven’t had specific chronology. Finally I am out of it.
Hi Wally, As a principle I publish all reasonable comments. I am glad things are going well for you but I need to make clear that I cannot endorse your approach to others as it lacks evidence of serum and 24 hour urine testing to detect possible underlying diseases, and presents remedies that are not aimed at identified urine abnormalities known to produce stones. I hope you continue to do well. Should you make another stone, here is a plan that might prove valuable. Regards, Fred Coe
macleodkaren5@gmail.com Hello my name is Karen I passed a 6.3mm kidney stone a couple of weekends ago very painful. I went to hospital with ambulance had a CT scan and that was determined. I seen a urologist last week. had an x-ray no stones now in the kidney. I have to bring the stone to the doctor to be checked out.. I have changed my diet completely. I gave up spinach for sure But I am struggling with what not to eat I am also Pre diabetic and have changed my diet for that also I was wondering if you could please send me the list for the stone diet that would help me so much I eat an Avocado every day, Hope this is ok. Half in morning half at dinner. Thank you for all these great comments gives one so much more knowledge. I made a choc diabetic cake with cocoa it is a great new sugar free recipe but was wondering about the cocoa and sugar free choc. Thank you
Hi Karen, Given a first stone analysis is correct and you need to figure out the cause before changing diet around. Here is my best effort at a proper evaluation.When you know the cause you can change things rationally, but not now. Regards, Fred Coe