LISTS – AND LISTS
I know you are all looking for THE list. Here is one from a reliable source I have have downloaded on my site to a separate document so it opens with one click.
The reliable source, as it turns out, needed some updating. Dr Ross Holmes, professor, School of Medicine, University of Alabama, was kind enough to review the work of Dr. Michael Liebman who is a professor of Human Nutrition and Food Option at University of Wyoming and determine which food entries on the Harvard list needed changing. We cannot change the original but we have updated our lists accordingly and annotated updates with *** marks. So the lists here are the most recently edited available at present.Fred Coe and I have updates and annotated the list for those with a tendency to perfectionism: Updated table of oxalate foods. Set it at 50% for easier reading. Get yourself acquainted with the lists. They will tell you much of what you need to know. A lot of it will even surprise you. You are not as restricted as you think you are or as you have been told.
A more dramatic list is the 177 high oxalate foods we distilled out of the big list. Here are culprits! Not on this list? Probably not very high in oxalate so far as we know – with perhaps a few exceptions. Note that quantity is critical. For example black pepper is high in oxalate but the amounts used are small enough that total oxalate intake from it is negligible.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
LET’S DIVIDE AND CONQUER
FOODS TO WORRY ABOUT
A List of Concerning Foods
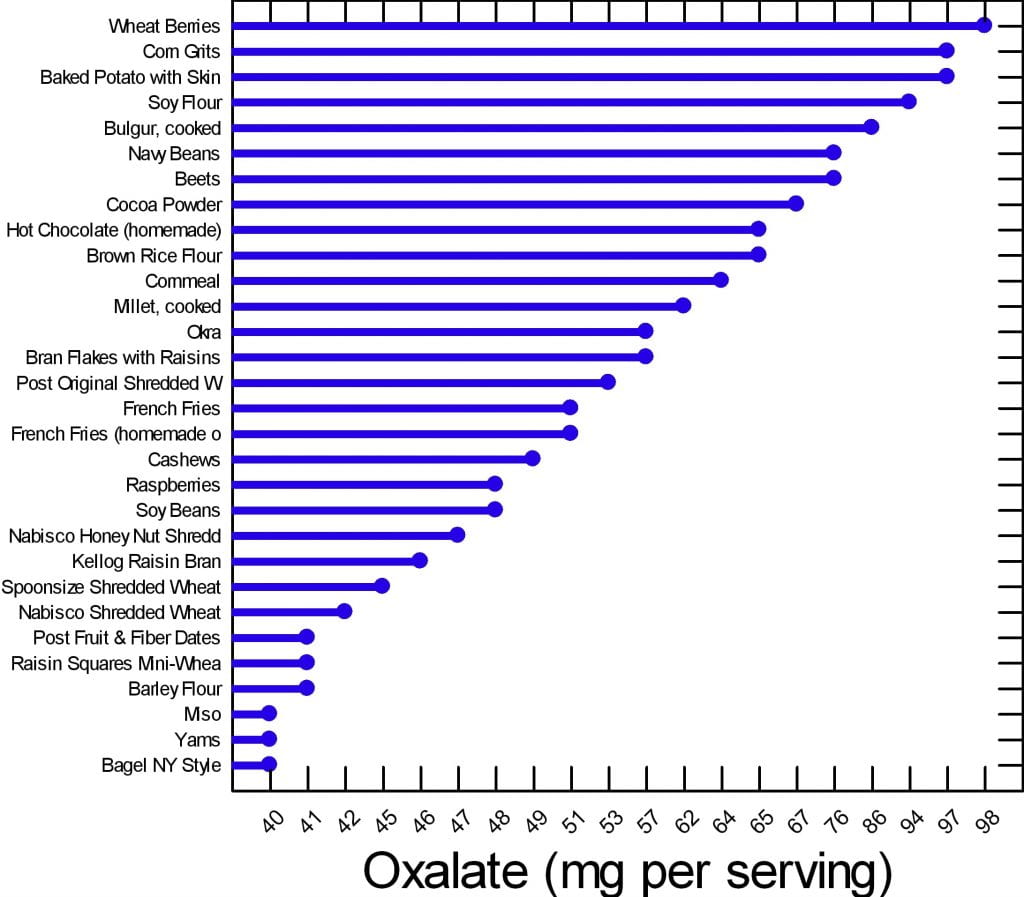
We have created two graphs for this article. Of the 177 foods on our master list, many are of concern but can be used in your diet if you control the portion size and how often you use them. There are 30 of them that are worrisome enough to deserve special attention.
Here are the 30. The graph shows mg of oxalate in a common portion. The details of the portions are in the complete list. The foods have in common that all contain at least 40 mg/serving. All other foods for which we have reliable data have less oxalate per serving.
Your budget is about 100 mg/day.
What does this graph mean? Does it mean you can never have chocolate, or a baked potato?
No.
It means if you want to use your whole budget on a treat, do it, but keep track and make sure you do not overspend in any meal or in any one day. Have your baked potato, but maybe share half with your partner. Or, have some hot chocolate but make it with milk because calcium helps reduce oxalate absorption. Eat your cashew nuts, but pay attention to how many. If one handful leads to ten, you cannot have them.
FOODS TO AVOID
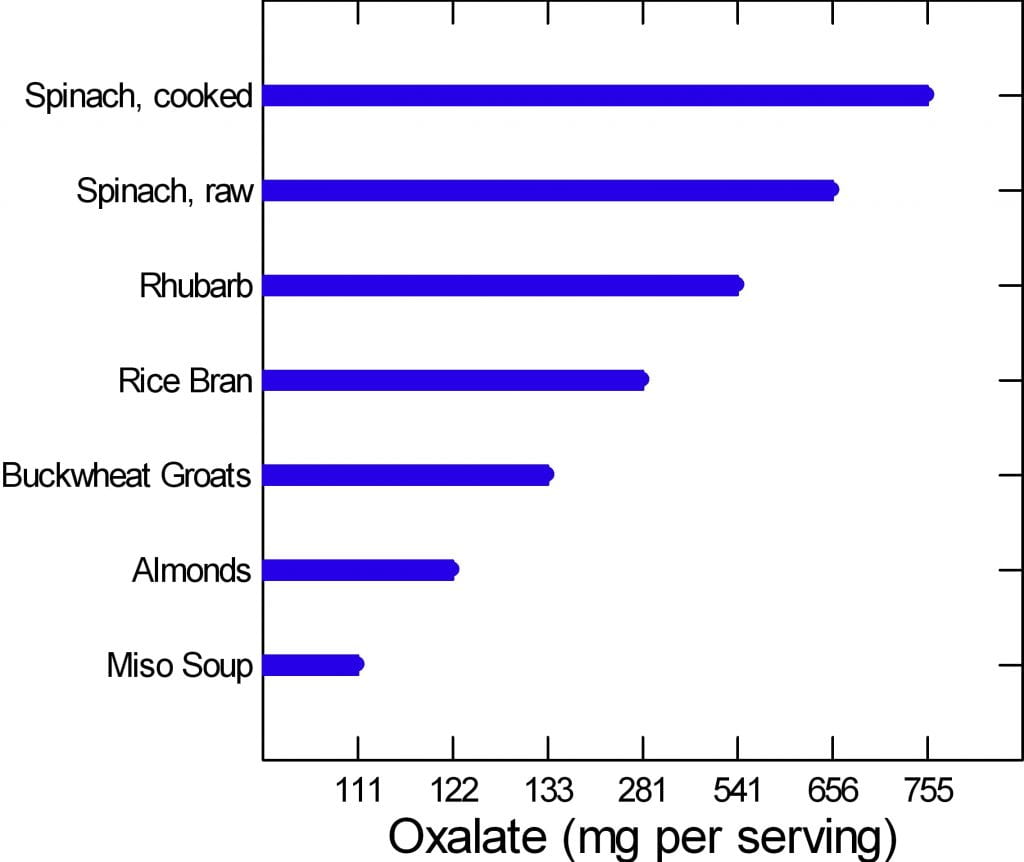 The graph to the left is of the very few dangerously high oxalate foods.
The graph to the left is of the very few dangerously high oxalate foods.
There are only six foods, but spinach, being worst of all, has two entries. Be careful of this plot because of its range. It begins at 100 mg/portion and rises to 755 mg/portion in only 7 steps, so the distance from miso soup to spinach is about a 7 fold increase.
Rhubarb and spinach are so high you just cannot eat them. Rice bran is something few will miss, the same for buckwheat groats.
People like almonds but have a hard time controlling portion size. If you can keep it to 11 almonds a day – the portion size that gives 122 mg of oxalate, alright. Otherwise stay away from them.
If you have to eat any of these foods, caution is hardly a strong enough word.
Are you sure you need to eat them?
Why?
WHAT ARE WE SAYING?
We are saying that oxalate is common in foods, and that you have to be careful, but care is a scarce resource. How much care can you give every bite? The graphs say if you eat moderately high oxalate foods – the first graph – be careful.
Watch portions.
If you are eating one of the six dangerously high oxalate foods, stop eating it.
It is too hard to be careful with those six foods. They have too much oxalate for most of you to handle. So, just say no.
WHY BELIEVE OUR DATA?
These data arose from a major effort at the Harvard School of Public Health. A world class expert has curated it twice. Harvard can be wrong and so can Ross Holmes, but both will tend to be wrong less often than the average persons who attempt to put complex data into the public domain. We have always appreciated comments, and if anyone has a peer reviewed publication with different food oxalate levels than ours, we will read the paper and see if it warrants our making a change.
Medical research is endlessly argumentative, and food oxalate is no exception. A recent paper contrasts findings from 6 websites and 2 applications and finds some wide variations. Of the sites, the Harvard site – used here as our reference, and the Wake Forest site – which is a legacy of an outstanding investigative group have most standing with me. Leaf through the comparisons between them in the 4 charts and in the large table at the very end. On the whole differences are modest. The hyperoxaluria and oxalosis list from the paper has been withdrawn from their site.
DO YOU NEED A LIST?
Sure, a list is nice. But we helping you here. Lists can run on to hundreds of foods. The picture is meant for focus. Here are the ones to focus on.
Many of you leave the doctor’s office thinking you will never be able to eat a fruit or vegetable again. If that wasn’t bad enough chocolate and nuts are gone, too. Some of this sadly is true, most of it is not. I am here to bring you good news: Almost everything, high oxalate or not, can be incorporated into your diet safely.
Do you need a low oxalate diet? You may if your stones contain calcium oxalate crystals and your urine oxalate is high enough to pose risk.
If you do need a low oxalate diet, what is your goal? Less than 100 mg of diet oxalate is good; less than 50 mg is ideal.
If you want to read some of the science about urine oxalate and risk of stones and about how we get to the diet oxalate goals, it is summarized at the end of this article.
Here we assume you do need to lower the oxalate in your diet.
CALCIUM FIRST
Low calcium diets can raise urine oxalate, and the solution may be as simple as a proper calcium intake. There is every reason for stone formers to eat 1000 mg of calcium daily to protect their bones. The common hypercalciuria of calcium stone formers puts bones at special risk when diet calcium is low.
Before changing your whole life around, ask yourself if you are avoiding calcium foods. If so, add them back and ask your doctor to check your urine oxalate again. It may fall enough that a low oxalate diet is not necessary.
If low calcium intake is not your problem, and you need a low oxalate diet, here is my take on how to do it.
WHAT IS THE DIET OXALATE GOAL?
Typical diets contain upward of 200 – 300 mg of oxalate. For stone prevention, a reasonable goal is below 100 mg of oxalate daily. An ideal would be about 50 mg daily if that can be accomplished.
To get there, consider the oxalate contents in common serving portions of all of the foods, and make up a plan for yourself.
FRUITS
FRESH
Everyone who comes to me is very unhappy thinking they can never have a berry again. This is Baloney. The only berry that is very high in oxalate is raspberries (look at the list). On the other hand, people do not realize avocado, oranges, dates, and even grapefruit and kiwi are very high and need caution.
This doesn’t mean you can never have these healthy treats. If you incorporate any of these high oxalate fruits into your morning yogurt you can reduce some of the effects of the oxalate content.
Also look at your portion sizes. You really cannot eat a lot at any one time. Dates are not a good bargain: One date is 24 mg!
CANNED OR DRIED
Canned pineapple is a problem.
Dried fruits have to be a worry because the water is taken out, so a ‘portion’ of dried fruit can be gigantic in oxalate content. Figs, pineapple and prunes are standouts. Just think: 1/2 cup of dried pineapple is 30 mg – not a lot of fruit for a lot of oxalate. If you want dried fruit, think about apples, apricots, and cranberry as lower oxalate options.
VEGETABLES
Spinach and rhubarb are standouts; stay away.
Other vegetables you need to be aware of are tomato sauce, turnips, okra, and yams (sweet potatoes) along with beans of different sorts.
I am not in the business of taking healthy foods away from people. But in the cases above you really must limit; there is just too much oxalate and these foods do not pair well with high calcium foods the way fruits can be mixed right into your yogurt or cereal and milk.
Many of you have been told to stay away from all green leafy vegetables. This is not true. Look at the list. There are plenty of salad options still available for you including kale. Even though tomato sauce is high in oxalate (see below) that is because of concentration. A whole medium tomato is only 7 mg and who eats more than one at a time?
Many of the salad vegetables are so low in oxalate they are freebies. Eat what you want.
POTATOES
These are Trouble! I put them into their own separate group even though they are vegetables.
From french fries to baked potatoes they are very high oxalate items. One ounce of potato chips has 21 mg of oxalate and who eats one ounce? Not I. Baked potatoes are terrible. One comes in at just under 100 mg of oxalate. Mixing sour cream into the potato will not help much; one tablespoon of sour cream contains only 14 mg of calcium. One ounce of cheddar cheese contains 200 mg of calcium, which could help, but it increases calories, salt and fat. But all in all, why struggle so hard? Potatoes are not ideal for stone formers.
DAIRY PRODUCTS
They have no oxalate. They are your main source of calcium. Use them. They can add a lot of salt – cheeses – and can be caloric. But they reduce oxalate absorption and preserve your bones.
For a stone former who has to watch salt intake, increase calcium intake, and lower oxalate intake, here is how to do that. You cannot have as much cheese as you want because of the salt. So portion sizes are very important. Yogurt, milk, even ice cream are good bargains – modest sodium and high calcium. These are a great place to add in a wee bit of chocolate – high oxalate foods – for those of you who cannot live without these high oxalate treats.
BREADS AND GRAINS
Some of the basic ingredients to make these foods are very high. White flour and brown rice flour are high in oxalate so everything you make from them will be high.
BREADS
Even so, as far as kidney stones go, breads are mainly alright because of portion size: not that much flour so one slice is 5-8 mg. French toast and New York style bagels top the list at 13 mg for two slices and 40 mg for one bagel – as much as anyone will eat of either food.
PASTA RICE AND GRAINS
Spaghetti, one cup cooked is 11 mg and most of us eat more than one cup.
Buckwheat groats, one cup cooked is 133 mg – I don’t see many of you saying ‘darn it’ or taking to your bed, but beware. Millet and bulger, wheat berries, rice bran, corn grits, and corn meal, these are widely used and are high. If you are using these, be thoughtful.
Here are some low oxalate options in this category: White rice, hummus, corn flour, corn bran, flax seed, and oat bran are popular and safe.
MEAT PRODUCTS
Since oxalate is only found in plant foods, all the meats are safe. Fish, too.
For our vegetarian friends, tofu and veggie burgers are very high.
NUTS AND SEEDS
These are just dangerous for two reasons.
Obviously they are very high in oxalate.
Secondly, I don’t know anybody who just has a few nuts at a time.
Just like chips no one eats one – the whole jar is more like it.
But, for one cup of pumpkin sunflower or flax seeds the highest is only 17 mg of oxalate and none for flax. For those of you who love foods in this category seeds are the better choice and they can be sprinkled on yogurt and ice cream.
SWEET STUFF
I have good news for my chocolate lovers. I know most of you have been sent home with a list and chocolate is high on it. But if you look at the numbers nuts are a lot worse than chocolate. Chocolate can be mixed in with dairy products, too, so as to reduce oxalate absorption.
Even so I do want to point out that half a brownie is on the high side, and who eats one half?
You can still satisfy your sugar craving but pay attention to your portion size.
Keep in mind, however, that sugar loads increase urine calcium loss which increases stone risk, so there are two reasons why this food group can be a problem.
But even without chocolate, you eat a lot of flour when you eat a piece of cake, so cake can be a problem – about 15 mg per piece, like french toast. Pies are half the risk because of their fillings – unless they are chocolate pies!
CRACKERS AND CHIPS
The big enemy here is potato chips. A one ounce serving contains a whopping 21 mg of oxalate. I repeat: A one ounce serving.
Your best bet in this category if you’re looking for something crunchy is corn chips – one ounce is 7 mg, popcorn – one cup is 5 mg, and pretzels, one ounce is 5 mg.
Crackers are OK mainly because they are small and the amount of flour is not that much.
BEVERAGES
PLANT SOURCES
Hot chocolate is the clear loser at 65 mg per cup; carrot juice is the runner up at 27 mg per one cup. Lemonade, tea, tomato juices, rice dream and the like are better but still high. The are 15 – 18 mg per serving. Lemonade – frozen concentrate – is 16 mg per 8 ounces so be careful about this as a source of citrate.
Soy milk, for those of you who prefer it, is not a good option. It is very high at 20 mg per cup. We have no data from standard sources for rice milk, cashew milk, and coconut milk; almonds are high in oxalate so the almond milk product will certainly be high.
Tea is so commonly used, here are the details. If you brew your own tea it is high in oxalate. The longer you steep your tea, the more oxalate it will have in it. If you use a sweetened instant iced tea one cup has 0 mg of oxalate.
Here are some juices that are low in oxalate and better substitutes: Apple juice, apricot juice, orange juice, grapefruit juice, grape juice. For all the lemonade drinkers, diet lemonade is low in oxalate.
Here is something very important: Coffee is oxalate free – almost, 1 mg for a cup (2 mg/cup for decaf). We already told you that coffee drinkers have a reduced stone risk, so lets debunk the coffee myth here: Drink it as you wish.
DAIRY SOURCES
Everything is good except chocolate milk. Even that is only 7 mg a cup for a sweet treat here and there.
ALCOHOL
What tops the list in this category is a can of beer: 4 mg of oxalate. All the rest are low and, frankly, the oxalate in a can of beer comes with a lot of fluid. This is not the problem area for stone formers.
WATER
If I didn’t say this to you I could not sleep well tonight. Water is the clear winner in this whole category. It is free of calories, sugar, and oxalate. Please use it as your main beverage and supplement with the items above.
SPREADS AND SAUCES
Chocolate, miso, peanut butter, and tahini are all high.
SOUPS
Miso soups is extremely high – 111 mg/cup. Lentil soup is high, and so is clam chowder – the potatoes.
BREAKFAST FOODS
This is a dangerous meal if you are a cereal lover. Many cereals are high in oxalate. I am afraid you need to look them up in the list by brand. Unfortunately the healthier cereals are highest in oxalate because they contain more plant based ingredients. Probably having milk in your cereal is wise, but we have no data to show.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life. I just released a course called The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.
HOW DO WE MANAGE ALL THIS?
The first thing you need to do is to learn and remember what are the highest oxalate foods and beverages. Without this in mind it is impossible to shop and cook intelligently. Here is a short list of the highest oxalate foods all in one place.
BREAKFAST
For those of you who love cereal because it is quick and easy check out the list and see if the one you love is high in oxalate. If it is, choose the next best one with lower oxalate. Put milk in the cereal.
Alternatives to cereal that are also quick and easy: Yogurt or cottage cheese and fruit. The only fruits to worry about are raspberries because no one puts oranges on their yogurt. Bananas, peaches, blueberries and strawberries are perfect toppings.
More trouble, but no oxalate, eggs any way at all. Boil a batch on Sunday and have them for the week for breakfast, and snacks, too.
Your breakfast coffee is free and so is your water. For juices use orange, apple, pineapple, grapefruit – all great. If you want tea, don’t steep more than a minute and consider adding milk to it. Green tea is better than black.
LUNCH
Typically you are grabbing a salad or a sandwich for lunch, so what now? Many clients tell me they no longer eat salads because their physicians told them to stop all green leafy vegetables.
I’m bringing salads back to you.
Arugula, iceberg, romaine lettuces, and kale, are fine as your base. Stay away from spinach. Here are good toppings. Cauliflower, corn, cucumber, mushrooms, onions, peas, scallions, squash and zucchini are all fine. Tomatoes are fine, too; it is only the sauce that is high. Broccoli and green pepper are moderately high so watch the portion size.
Sandwiches will cost you between 12 and 16 mg of oxalate depending on the bread you are using – 2 slices. This doesn’t mean you can never have a sandwich, it just means you have to keep track of how much. You can have 50 to 100 mg daily. What goes inside between the two slices of bread is usually cheeses and meats which are oxalate free. So sandwiches are not something to be afraid of.
SUPPER
Beef, chicken and fish are all fine, and those the main courses for most of us. You will run into problems if you are a pasta or potato eater. If you are you need to limit the amount of times you have these foods each week and also the quantity each time you use them. Substitutes are a problem: White rice is a nice substitute for potatoes but there are few others. It is more veggies that have to fill in – very healthy but not as much fun.
Here is a recipe for cauliflower – ‘mashed potatoes’ you will like and even think, sometimes, is the real thing. There are many versions on the web, choose the one that makes you happy but be careful about the ingredients.
There is also quinoa which is not on our lists, but may well be high. A recent scientific article on this plant does not give oxalate contents which suggests they are not reliably known.
I have recently put together a private FB page called THE Kidney Stone Diet. It is a group that helps educate you on your physician prescribed treatment plans. As you can imagine, oxalate comes up in many posts. I moderate it to keep it clinically sound. Come on over and join the discussion!
URINE OXALATE AND RISK OF KIDNEY STONES
I promised you some science – here it is for those interested. It concerns only highlights from the food – urine oxalate research recently performed and seemingly germane to the problem of how stone formers should control oxalate intake.
The most useful data about urine oxalate we have so far is from three cohorts studied by Dr. Gary Curhan. Two are cohorts of nurses one a cohort of physicians. These people have kept track of many aspects of diet and health for decades, and among their records are onset of kidney stones.
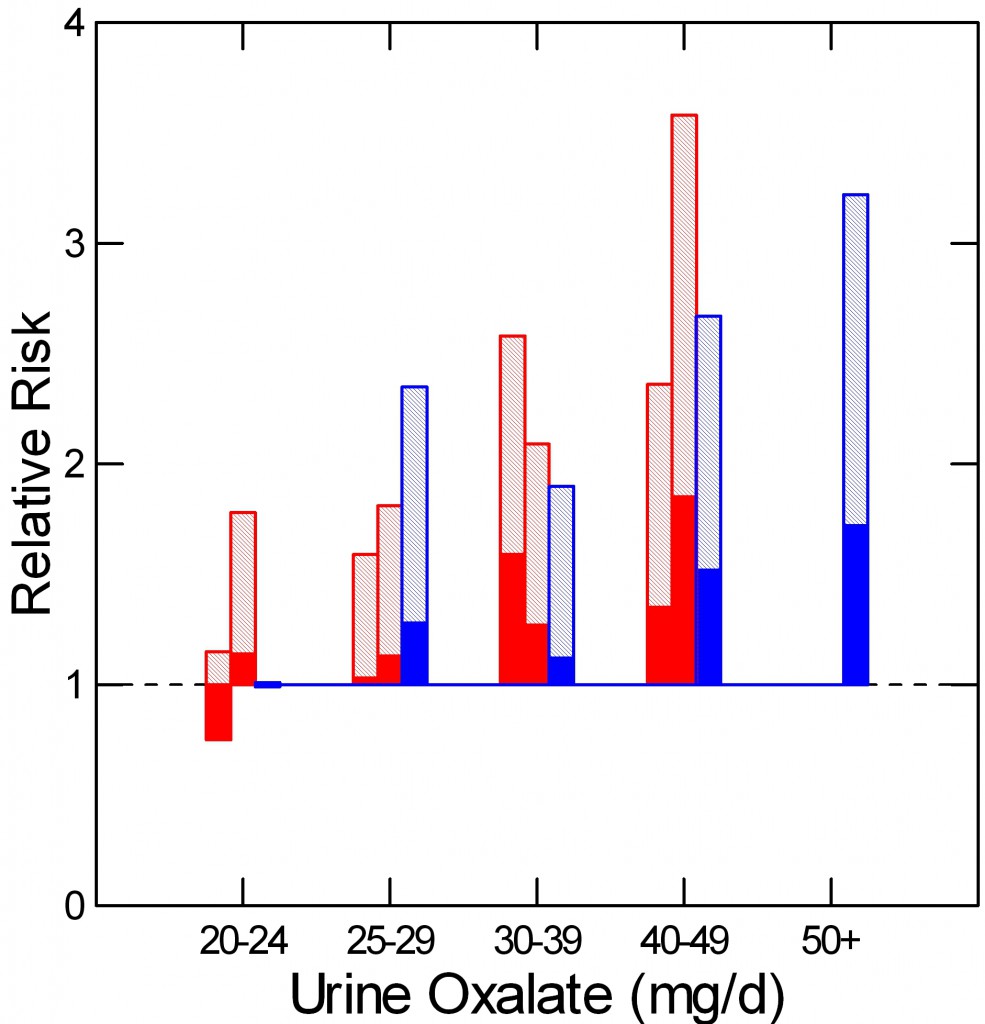 As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
As he did for urine calcium, Curhan measured urine oxalate in properly selected subgroups from each cohort, including people who did and did not begin forming stones. From these samples he could calculate the relative risk of new onset of stones in relation to 24 hour urine oxalate excretion.
The two nurse cohorts are red, the physicians – all men – are blue. The dotted line at 1 is the risk threshold: Above that line, risk is present.
The top of each crosshatched bar shows the mean relative risk for each of the five urine oxalate ranges. Clearly the mean goes up as urine oxalate goes up.
But the mean relative risk has a range of uncertainty around it. The bottom of the solid portion of each bar is the lower 95th percentile for that range of uncertainty. When that bottom lies above 1, risk is very likely to be present.
For both the women and men groups, that point is reached between 25 and 30 mg of urine oxalate a day. Therefore one wants to try to get urine oxalate below 30 mg daily and even lower, below 25 mg daily if possible. The average urine oxalate excretion among the women in this study was close – 26 and 28 mg/day for those who did not form stones and just a bit higher for those who did – 28 and 30 mg per day. The men are a problem: 39 and 41 mg/day for those who did not and those who did form stones.
This is not diet oxalate, it is urine oxalate. Urine oxalate is how much the body makes and how much is absorbed from foods. Mostly, we can control only the second part – how much is in the food.
HOW MUCH DIET OXALATE DAILY
All dietary advice depends on having a reasonable goal in mind for oxalate intake. My goal of 50 – 100 mg of oxalate from food daily is not unreasonable given the research that has been done in normal people and stone formers.
Holmes and colleagues found a urine excretion of oxalate of about 10 mg/gm urine creatinine in normal 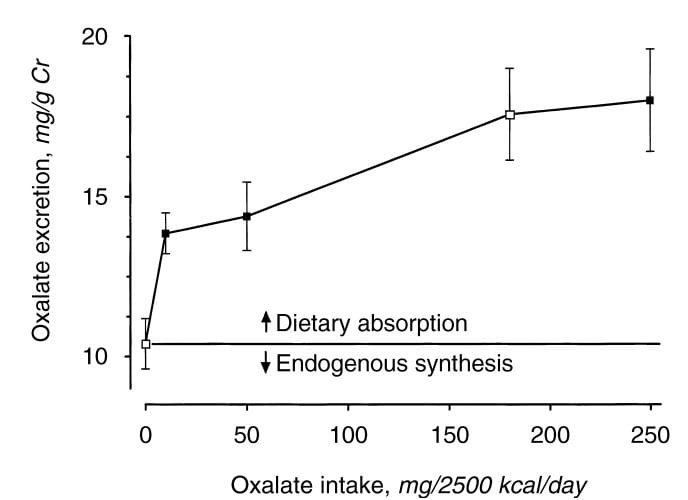 people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
people eating a synthetic oxalate free high calcium diet (graph at left). As diet oxalate increased, urine oxalate rose from 0 to 10 mg/2500 kcal/d, urine oxalate rose steeply from 10 to 14 mg/gm urine creatinine. It rose more slowly, from 14 to barely 15 mg/gm urine creatinine as diet oxalate was increased to 50 mg/2500 kcal/d, and more or less at the same slope thereafter so that an increase from 50 mg/2500 kcal/d up to 250 mg/2500 kcal/d increased urine oxalate only from 14 to 18. The closed symbols are whole food the open symbols synthetic diets.
From this work the percent oxalate absorption could be calculated as around 10 – 15% and the contribution of diet oxalate to urine oxalate excretion as around 25 – 40% when intake of oxalate was between 50 and 350 mg/2500 kcal. Therefore one can consider a whole food 1000 mg calcium 50 mg oxalate as a usable low oxalate diet, and a 150 – 250 mg oxalate diet as relatively high.
The balance between diet calcium and diet oxalate does not matter greatly if diet calcium is high. Among normal men and women eating 1000 mg/day of calcium and 750 mg/day of food oxalate, 24 hour urine calcium was about 110 mg/day and oxalate about 44 mg/day.
If the calcium oxalate balance is altered so calcium intake is 400 mg and 20 mg of oxalate at breakfast and lunch, and 200 mg of calcium and 710 mg of oxalate at dinner, as compared with simply 333 mg of calcium and 250 mg of oxalate in all 3 daily meals, urine oxalate is lower after the high calcium low oxalate meals, but only slightly higher after the high oxalate low calcium evening meal than when calcium and oxalate intakes were balanced. This means that when diet calcium is at least 1000 mg daily the balance of calcium to oxalate within any one meal is not likely to affect stone risk.
Seiner and colleagues make clear that stone formers are different from normal people. They divided male and female stone formers into 2 groups of 93 people each, one with urine oxalate above 0.5 mmol (~50 mg) of urine oxalate daily and the other with urine oxalate below 0.4 mmol (~40 mg) daily. They found virtually identical calcium and oxalate intakes: 845 vs. 812 calcium and 101 vs. 130 mg daily of oxalate respectively in the lower and higher urine oxalate groups. But the below 0.4 mmol group excreted only 27 mg of oxalate daily on average, whereas the high oxalate group excreted 64 mg daily. In other words diet was not responsible for the higher urine oxalate excretion, suggesting a difference of oxalate absorption. Those prone to high oxalate excretion seem, therefore, to most need diet modification.
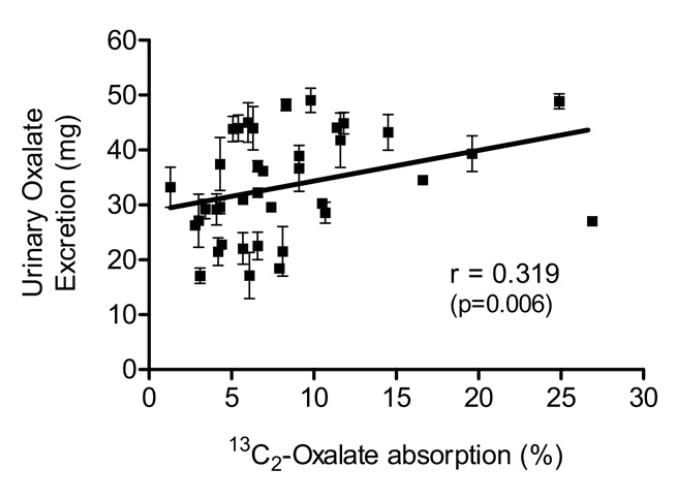 Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
Knight and colleagues found a wide range of oxalate absorption among 38 calcium oxalate stone formers eating a self choice diet. Urine oxalate excretion (vertical axis) varied with percent of diet oxalate absorbed (horizontal axis). The mean absorption centered around 5%; a few outliers absorbed over 15% up to 25%. This supports what Seiner found – some stone formers will have urine oxalate levels very responsive to diet oxalate and sans a research protocol we will not know. This is another good reason to keep diet oxalate low – 50 to 100 mg if possible.
PROTEIN AND GELATIN
Diet protein intake does not affect urine oxalate excretion. In 11 normal people fed a 1000 mg calcium, 51 mg oxalate, 3000 mg sodium fixed diet, varying protein intake from 0.6 to 1.6 gm/kg/day – a very wide range – did not alter urine oxalate appreciably (mean values were 23, 23, and 25 mg daily for the three protein intakes) even though oxalate precursors like glycolate rose markedly (25, 22, and 46, mg daily).
Jello is a source of hydroxyproline which converts to glycolate and oxalate, and oral loading with gelatin can raise urine oxalate. Ten normal people eating a 1000 mg calcium, 150 mg oxalate diet (typical normal level) were fed supplemental gelatin as one quarter of daily protein intake. Urine oxalate was 24 mg daily vs. 17 mg daily when the same diet was supplemented with whey protein – containing little hydroxyproline – as a control. So lots of jello is not an ideal plan for stone formers.
Where does this leave us about how much oxalate is alright for a day. If diet calcium is high, as it should be, at about 1000 mg, then one should try to limit diet oxalate below 100 mg daily. Perhaps this is most important in those patients whose baseline oxalate excretions are higher – in the range of above 40 mg daily.
Eating a low oxalate diet can be overwhelming and difficult to incorporate into your daily life.
For those who need special help, I run an online course: The Kidney Stone Prevention Course to help you understand how to implement your physician’s prescribed treatment plans.



Hi Jill & Dr. Coe,
The Harvard table says strawberries are low in oxalate and raspberries are very high.
But I Googled “oxalate strawberries” and the first hit was an NIH study which concluded “Although oxalate-rich foods enhanced excretion of urinary oxalate in normal volunteers, the increase was not proportional to the oxalate content of the food. Only eight foods–spinach, rhubarb, beets, nuts, chocolate, tea, wheat bran, and strawberries–caused a significant increase in urinary oxalate excretion.”
That points in the opposite direction – they warn of strawberries and don’t even mention raspberries.
How is a berry lover to sort this out? Thanks in advance.
Sam
Hi Sam,
Take this advice and apply it to every food you choose to eat. Have the raspberries-in limited amounts- and with a calcium source to help bind with the added oxalate. Also this- you have 100 mg of oxalate in your bank that you can withdraw from any way you wish. You choose what foods are important to you to make your withdrawals. Try not to be overdrawn on most days and get your RDA of calcium. The problem with our country is we overeat, even the healthy foods, and that is when we run into problems.
Take care,
Jill
Hi Jill and Dr. Coe,
I recently learned at I have to alter my diet and drastically lower my oxalate consumption. I am vegan, and confused after reading some information stating that dairy products should be eaten for the calcium. My doctor said animal products should not be in my diet. I’m also trying to find the oxalate content of coconut meat (fresh, dried, or flour) as it seems all my sources of desserts are removed, but I haven’t been able to find this. Thank you!
Hi Pam,
Not certain why your doc said no animal products. My patients do enjoy coconut products and continue to have low oxalate values. I have worked with many vegans and when they come to me they do indeed have high oxalate values. It is typically because of their lack of calcium and overeating the highest oxalate foods. Get rid of spinach and almonds (sad and I know), and most other foods you can eat within reason and with calcium sources if they are higher in oxalate. Stay away from the highest oxalate foods. If you need more help (many vegans do) please consider getting outside help.
Best, Jill
Thank you for your reply. Do you have any suggestions that would help me optimize my calcium intake on a vegan diet? Thank you.
Hi Pam,
Google non-dairy calcium foods and you will need to also adjust for lower oxalate ones and pick what you like. Fortified flax milk and coconut milk are used frequently by my vegan patients.
Best,
Jill
That was my question too, thanks Pam. I think I might be overdoing the pea protein shakes or the peanut butter!
Hi,
Do you know if coconut meat (fresh, dried, flour) is high in oxalate? Also, I am a long time vegan and new to watching my oxalate intake. Do you gave any suggestions for consuming adequate calcium on a vegan diet?
Thank you.
I read in one of the oxalate articles that cut down salt intake and one said that Himalayan salt is OK to use. True?
Hi Rev Ruth,
No matter what type of sodium you ingest, make sure it is no more than 1,500 mg/day on most days.
Be well, Jill
Also, I take Magnesium about 340 mg/day, does it help, hinder with CaOxalate stones?
Hi I was just recently diagnose with having too much calcium in my urine and I am confuse on what to eat and what not to eat!
Hi Lisa,
We have many articles on the site regarding hypercalciuria. Take a look. It can be genetics, too much sodium, too much sugar and or too much protein. You would need to speak with someone who can help you manage your specific cause(s).
Best, Jill
Hi Jill and Dr. Coe,
Do you have informations about oxalate content in mulberry(white&purple), pomelo, cherimoya, kiwano(horned melon), pitaya(dragon fruit) .
Thank you,
George.
Hi George,
We are unaware of these oxalate values.
Be well, Jill
Same question… wondering about values for cherimoya, soursop, durian, dragon fruits, etc.
Hi Lorraine,
Here is all the info you need to know what to do when a food has not been studied.
kidneystonediet.com/oxalate-list
Jill
This is a great article and has helped me greatly. I have had many kidney stones over the last two years and my urologist has recommended a low ox diet. I have been researching and wondered your thoughts on the DASH diet. The Kidney Foundation recommends this diet but when I look up the recipes they contain high ox foods. What are your thoughts?
Hi Kara, It may take another generation to get rid of the low oxalate diet as a seeming catchall treatment. The proper diet is here, not really the dash at all – too much oxalate, also becoming way too commercial for my taste. The kidney stone diet is ideal. I am not arrogant saying this because it is identical to the diet recommended for all American people. So let’s all eat as we should. As for oxalate, the kidney stone diet recommends some care – below 200 mg of oxalate which is enough because the diet is high in calcium that prevents oxalate absorption. The Kidney Foundation should stop recommending this diet for kidney stones, but I cannot stop them. Regards, Fred Coe
Hello. 🙂 Are you aware of any research regarding butternut squash and if it’s considered high, medium, or low oxalate? I have only seen information about summer squash. Thank you!
Denise
Hi Denise,
We do not have valid research on butternut squash. Wish we did as I am asked this question daily in my practice. I tell patients this: “have this food once or twice a week and in normal portion size and should be fine”. It is in the squash family and squash is low.
Best, Jill
Are chia seeds high in oxalates
Hi Nancy,
Most of the time it comes down to portion size of these foods. I don’t have a reliable source for chia seeds, but don’t overeat them and you will be fine. Also, perhaps more important is to get your RDA of calcium each day, by food is best.
Thanks for writing,
Jill
Hi Momma Jill!
Another great article. I’ve switched from supplemental calcium to food based sources and am even now avoiding the cheese I used to eat (I save it for pizza once a week) because of the sodium. I noticed some hypocalcemic symptoms creeping back and checked with my endo and he said I could increase my calcium intake as our bodies are known to process the two types of calcium (supplements vs. food) differently. I’ve increased my milk (which I drink at every mean unless I’m having yogurt for lunch) from one to two cups. Should that help bring down my urine oxalate levels significantly? And will all that milk change up my urine pH and increase my stone formation risk? THANKS!
Hi Lisa,
It definitely will help lower the oxalate, by how much will be known on your next urine collection! Remember, stay within the 1,200 mg/calcium for non-menstruating women, by food is best, low sodium, even better. Keep up your hard work.
Jill
Please keep me updated. Thank you!
Hi d, the best way to stay updated is to register for my emails – see the front page of the site. Regards, Fred Coe
Hello. I’m a 77 year old woman and had PNL surgery a year ago, followed by a Uteroscopic procedure, although he was unable to get all of it. Still have two small stones. My stone was a 5 cm staghorn calculus which my urologist said was formed by urinary bacteria. I had had many UTI’s in the past 3-4 years. My question is, around that time I began eating vegan, no dairy and lots of vegetables, grains, pasta, etc. Could this dietary change have brought on the UTIs and subsequent formation of this stone? I take calcium supplements and try to get as much as I can in my diet. My urologist doesn’t think diet is especially important with this type of stone. I did a urine capture and he said my oxalate level was a little high and to try not to eat high oxalate foods. Sorry this is so long and thank you.
Hi Sue, If caused by bacteria, your physician means a struvite stone. The bacteria make the crystals by cleaving urea to ammonia in your urinary tract, and they live within the crystals. Prevention requires that all stone material be removed as best as possible. Your diet would play no role given what you were told. Likewise your urine oxalate. It is really about an infected foreign body in the kidneys, so your physician is right. But s/he needs to prevent more. Regards, Fred Coe
Hello Jill
Thank you for a very informative article!
I’m considering joining a diet program after reading this article and maybe you could tell me if it is good or not. https://demandtobehealthy.wordpress.com/2018/01/10/complete-review-of-brian-flatts-2-week-diet/
It seem good but what do I know. Perhaps you could recommend something?
Much appreciated, Gracie
Hi Gracie,
Unfortunately, I am not a fan of this “two-week” diet. I recommend someone experienced in helping people implement the dietary changes they need for their specific medical conditions, likes and dislikes, allergies, etc. We are a nation of overweight people because there is NO quick fix solution. Changing your lifestyle takes first– knowledge, second– commitment, and third– hard work. EVERY SINGLE DAY. If it were easier than that no one would be overweight (in most cases). I recommend The Kidney Stone Prevention Course that I put on based on Dr. Coe’s work. You get all the education and 5 weeks of working with me every single day by phone so you can lose weight, keep stone risk lowered, and feel better overall. You can read about it on this website under The Kidney Stone Prevention Course. We have tons of fun too!
Best, Jill
Where is the complete list with numbers? you bleat on about low, medium & high oxalate foods, yet all you provide is a tiny paltry list. I need a COMPLETE list of the oxalate content of foods BY THE NUMBERS. I don’t need your interpretation. I want FACTS. i’d give this site a D- except that most of the others are just as bad. Look at Wake Forest for a glimmering. I thought you people were scientists. Apparently not. Just another group of bozos flogging your books and egos,
Hi Robert, You seem a bit impolite, but I am not sure why. The second link in the article is to a spreadsheet that goes down 661 rows each one with an amount of oxalate per serving. Surely those are facts enough for most people. The shorter lists you mention are meant as a convenience. The first link in the article is to the origin lists at Harvard from which we curated our list. So if you like numbers, they are plentiful indeed. As for interpretations, please feel free to just peruse the lists. As for your grade of the site, perhaps after you look at the lists you will be happier. As for us being scientists, we are indeed. As for us being ‘bozos flogging (our) books and egos’ I am not so sure. Regards, Fred Coe
Just found this today after avoiding tomatoes and eating quite a lot of
strawberries and cream. The breakfast I really wanted was nearly 2 cups of milk
and a banana. Glad that was acceptable.
Thank you for your work. It is lovely to have some painfree days and it will be
even better to know how to have more. Thank you again.
Hi Patricia, Be sure that oxalate lists are all you need. Here is a good plan document to be sure. Regards, Fred Coe
Do you have any information regarding the oxalate content of sorghum flour, potato starch
and carob powder? I have found conflicting information. I can’t have chocolate, and
I am gluten intolerant so I need to know about the flours I am using for baking. Thank you.
Hi P. Minando,
I don’t have good numbers for any, but assume they are on the higher side due to the fact that the base of these flours is foods all high in oxalate. Can you try oat flour? Also, gluten free.
Best, Jill
Afternoon. I have a history of Calcium-Oxalate kidney stones and read your article with interest as to the oxalate content in various foods.
Quick question. I do not see Eggplant listed on the “High Oxalate” List contained in your article nor in any of the resource lists you have provided via links in your text. However, it invariably appears as a “High Oxalate” Vegetable on virtually every other list I have reviewed.
My wife and I love stir-fried Chinese Eggplant cooked with a little olive oil. Should I avoid it?
Thanks.
James
Hi James,
The Harvard list doesn’t list them. I advise my patients to eat eggplant in smaller quantities and only once a week. Make sure you get your daily allowance of calcium too.
Best, Jill
Good Day. I have a family history of kidney stones, and have them myself. After reading your very helpful article, I’m still somewhat confused. Your list only notes Raspberries as a berry to avoid, but most other lists I have read also include Blueberries and Strawberries as offenders on the High Oxalate List.
I love all three and certainly don’t want to eliminate them all if I don’t have to do so! What do you advise?
Thank you.
Heidi
Hi Heidi,
I advise my patients to drop raspberries and enjoy the others. Helps if you put them in calcium-rich foods like yogurt.
Best, Jill
There is only one sheet. I’ve checked several times and it stops at cereals. Nothing on sheet 2 or 3.
Hi Jennie, If you mean this link useful table of oxalate foods it goes to a spreadsheet with only one sheet but that sheet has 661 rows that cover about all we have of reliable data. It ends at cereals but has covered a long list of other foods by that time. Regards, Fred Coe
Hello. I am a 28 year old female with a strong family history of kidney stones and just one of my own hanging out in my kidney. My urologist just recommended a low oxalate diet, but after reviewing your site and others, I’m a bit concerned. I cut dairy completely out of my diet six months ago because it bothers my stomach significantly. As such, I’m sure I’m low on calcium. In addition, every dairy-substitute that’s available and worth anything as far as taste is almond-based. I use almond milk, almond yogurt, even almond ice cream. (However, I typically only have an 8oz serving of almond milk about twice a week. Plus a serving of almond butter with an apple a few mornings per week, and an almond yogurt on alternating mornings. Almond ice cream occasionally.) Any guidance would be greatly appreciated!
Hi Rebecca,
Try coconut or flax milk products that are fortified with calcium. Orange juice can be used as well. You must get rid of almonds as they are just too high. When you look at the list we suggest to use, note that there are still so many foods you can still eat. The highest foods, that like almonds and spinach are just too high to work into your diet. At 28, you need 1,000 mg/calcium per day so google non-dairy calcium-rich foods and take away the high oxalate ones. Start there.
Best, Jill
Please let me know if collagen is high in oxalates. I take one scoop of collagen in my matcha green tea (should I switch back to coffee) for my joints as I’m running still at 63 yr old and have no joint problems. Collagen is also good for your skin, nails, hair, etc….
Also, I squeeze one lemon in water first thing in the morning with another big glass of water for my liver. Should I cut out the lemon?
Thank you,
Virginia
Hi Virginia, Yes, collagen is high is hydroxyproline that your liver can convert to oxalate, so I would stop the supplement. If you have stones you want to prevent, might I suggest a more balanced program than your lemon – take a look. Regards, Fred Coe
Hello,
I am a parent of a young adult with multiple disabilities who has:
-CKD IV
-Hypothyroidism
-Hypocalcemia
-Hydradenitis Suppurativa
-1st kidney stone 01/18
Diet has consisted of low phosphorus, low potassium (as needed), nightshade free & now need to incorporate low oxalate into the mix…whew.
Need to find a dietician with strong experience to help tuning up the diet. Have consulted with a few but fail to recognize all her needs in recommendations.
Any recommendations would greatly be appreciated!
Barbie
Hi Barbara, Before searching for a dietician about oxalate, be sure your child has been fully evaluated as to the cause of the stone. It is calcium oxalate? Is urine oxalate elevated and therefore a problem. Perhaps other problems are causing the stone and you will exert yourself to no avail. Avoid confusion. Regards, Fred Coe
What is the best way to insure I have enough protein intake while on a low oxalate diet?
Hi John, Since oxalate is mainly in plants, protein is not usually an issue. But more important, be sure you need a low oxalate diet. Usually they are not a major benefit in a proper prevention program. Take a look here. Before using your valuable time and energy be sure you know why stones are forming, and that diet oxalate is really your issue. Regards, Fred Coe
hey, plz suggest me what can i eat if i am suffering from kidney stone
you nearly listed all normal food i take on daily basis and that’s why i am little bit confused, so i need some guidance on this that would be greatly appreciated
thank you
Hi Abhishek, The low oxalate diet is not needed most of the time. Here is a good article on how to prevent stones. You can see where a lot of diet changes are healthy and mainly obviate special oxalate lists. Take a look. Regards, Fred Coe
Fantastic website, and great advice for all of us who suffer with stones. I have a related question about potato chips and pasta sauce.
I understand that both potato chips and pasta sauce are not generally given the seal of approval for consumption by those who have a history of calcium-oxalate stones. I, like I’m sure many others, can purchase brand-name potato chips without any salt added and pasta sauce with no added sodium at my local grocery store. Are such purchases wise or not for someone with a history of stones? Or, is the lack of salt still not sufficient to make either item a smart choice for stone formers?
Thanks very much.
Paul
Hi Paul, As you mention, the ideal kidney stone diet is low in sodium compared to present US consumption but identical to the diet recommended for the US population. Chips and sauce labeled no salt added may be in fact low in sodium or may have a lot of sodium from other ingredients; what matters is the total sodium per serving and the number of servings you actually eat. The actual kidney stone diet is rather liberal, take a look. Chips and sauce sans sodium are not a problem. Regards, Fred Coe
Thanks for making this so much clearer! Any ideas for vegan sources of protein? Tofu and wheat-meat both appear to be high. Same for beans and many grains 🙁
Thank you for making this so much clearer! Any ideas for vegan sources of protein? Looks like white rice and oats for grains. What about legumes? Is Quinoa okay? Steel cut oats? Thanks for your time in responding!
Hi JulieL, This is response to both of your comments. Jill Harris needs to answer your specific food questions. But do you need a low oxalate diet in the first place. Take a look at this article ane be sure. Mostly urine oxalate falls when diet calcium is high enough. Here is my favorite article on stone prevention. If you do all of the things you need, the oxalate part is rather modest. Regards, Fred Coe
I am 40,I have kidney stone on right and left kidney of 4mm. I am drinking pomegranate juice and 1 lemon juice in empty stomach in the morning as well as taking water melon after food.
Will it dissolve kidney stone.Can I continue taking above.
Hi Raja, only uric acid or cystine stones dissolve, calcium stones will not. What you take will do nothing to dissolve calcium stones. You need a proper approach, and here is a reasonable start. Regards, Fred Coe
Please can you confirm that avocados are high in oxalates?
Livestrong ‘s website classifies them as low in oxalate content.
Thank you
Hi, thanks for this article! I recently suffered from an excruciating kidney stone that had developed inverted fish-hooks, and logged itself into my ureter. Surgery was the only option. My “other” problem is that 2 years ago, I nearly died on the operating table after undergoing 3 major surgeries, which resulted in having 17ft of my small intestine removed (I was born with malrotation). So, I certainly have a dietary challenge ahead of me, partly because I now form kidney stones, and also because I suffer from Short Bowel Syndrome. I am having a very difficult time finding a nutritional expert who has enough experience with my unique combination of problems. However, I do have a few questions please. In general, how much oxalate should a person who has to eat 5-6 smaller meals per day consumer at each meal? I do have to supplement potassium and magnesium (due to my SBS). What is the normal amount of magnesium a person should consume each day? You mention chocolate as being “potentially OK” to consume, in small amounts? Which is better, milk, dark, or white chocolate? Regarding milk, my SBS has left me lactose intolerant. So, I “was” drinking almond milk. But, I now see that almonds are high in oxalate. Any suggestions on a different type of milk? Thank you very much!
Hi Steve,
Try flax milk or coconut milk if you enjoy them. Make sure they have been fortified with calcium. You might check out my website to see if I can help with all your issues. It’s what I do for a living. jillharriscoaching.com
Best, Jill
Hi Jill, Ive noticed that many Almond milks only have s small percentage of almond in them (2-12% typically), if only 2% then these would be ok in moderation?
Hi Jo,
We tell our patients to stay away from almond milk as one cannot be sure of the exact amount of almonds in the milk. Go with Flax milk instead!
Best, Jill
Hi Jo,
Almonds are so high why risk it? Have flax milk or fortified coconut milk.
Best, Jill
I read a post by Dr. Coe where he mentioned that pure stevia extract does not contain oxalate but stevia brands that contain the stevia leaf do. Can you tell me which stevia products do not contain the leaf but only the extract? The product labels are confusing to me. Thanks if you can answer this. (I accident.y hit the submit comment button twice. Hope this gets to you…)
Hi William, commercial stevia extract has no oxalate. Stevia – the plant – does. Regards, Fred Coe
Question. When measuring oxalate content of popcorn, is that referring to popped or unpopped.
Hi Mark,
Not sure to be honest. I assume popped and tell my patients to eat it but not have barrels of it. The problem with all food is the portion. We eat too much. Eat within normal portions and watch the magic happen in all health concerns!
Best, Jill
Can you tell me the oxalate content for a serving of cooked quinoa?
I cannot find any information on quinoa.
Hi Cathy,
We do not have good numbers. I tell my patients to eat it once a week within normal portion size. They do fine with that advice.
Best, Jill
On some lists avocados are on the low oxalate list: http://drcherylkasdorf.com/wp-content/uploads/2015/02/OxalateContent092003.pdf. On the lists you have here, avocados are on the very high list. So confusing! How do we know which list is correct?
Hi Andrea,
Please look at the numeric value and not the adjective describing it. On the Harvard list that we use with our patients, avocados are listed as high, but they are only 19mg/fruit. If you are allowed 100 mg/day in oxalate you can see that you can still eat these healthy fruits. Calcium intake is much more important than oxalate.
Best, Jill
Thank you for providing this list. Ive dealt with kidney stones since I was 16. I have both Calcium Oxalate and uric acid stones. I recently decided to try a low oxalate diet again. looking forward to reviewing the list and seeing if this diet will make a difference. Thank you
Hi Kristina, given uric acid and calcium oxalate stones, I doubt the list is really your best bet. For uric acid stones, one needs to alter urine pH. For calcium oxalate stones, there are multiple causes, and treatment depends upon what is found. I would not depend on just this one element of treatment as it will not do what you need. Regards, Fred Coe
Hi just wondering if you have any data on the oxalate content of hemp? Feeling a little overwhelmed with these kidney stone dietary restrictions where I don’t know the composition of my stones. Avoiding animal protein and oxalate at the same time seems almost impossible, if you could make a suggestion about what should I use as a protein source?
Tessa,
You can def have protein, just watch your portions sizes. You can also eat many fruits and veggies that are low in oxalate. Have you done a urine collection? You may not even need to worry about some of this. But this game is about portion size, not total restriction. Also remember, getting your daily calcium is very important too.
Best, JIll
Thank you for a very informative article. In addition to oxalate stones I have been diagnosed with idiopathic hypercalciuria. How would this affect your recommendations for calcium intake? I’m a relatively thin 58 yo male with no family history of osteoporosis.
Thanks!
Hi Paul,
If you have true IHC you will need to go on a pill to lower urine calcium. BUT. Have you followed The Kidney Stone Diet? By doing so you may not need the pill or at the very least go on a lower dose. Lowering sodium and sugar will help, hopefully. Ask your doc if you can change diet and do a follow up urine test to see how low you can get your urine calcium before starting the pill. This is all under the assumption that you have not already done said things.
Best, Jill
My urine test showed really high calcium oxalate levels caused my kidney stone. I started a low oxalate diet cold turkey and have continued for about a month now. Then, I read online about oxalate dumping. Did I do something bad by going cold turkey? Am I harming my kidneys since I have been doing this for 4 weeks?
Hi Elizabeth, I found out what oxalate dumping is thought to be. Here is a sample. It is probably the most ridiculous idea I have ever read about. The idea is that oxalate in the body is holding on to enough minerals to make a difference so that as oxalate leave the body it takes minerals with it causing shortages. The very idea is silly in that the total amount of oxalate lost a day is about 0.5 mmol, whereas urine calcium itself is 2 – 4 mmol, magnesium another 2-3, and there is no evidence that oxalate crystallizes in the tissues of people who do not have kidney failure or rare oxalate diseases. As for the low oxalate diet, it will rarely cure stones, being just part of a proper treatment plan. Take a look here. If your urine oxalate was itself very high, diet is not likely enough so be sure and have it rechecked – I cannot tell from your comment if your urine oxalate was high or the calcium – oxalate supersaturation was high. Regards, Fred Coe
Where is Kelp on the scale?
Hi Kyla,
I don’t have valid numbers on kelp. Don’t make it a regular thing (say once a week) and in normal portion sizes.
Best, Jill
Hi Jill, I’ve looked at so many lists that mention oat bran, flour, etc. What about just plain oatmeal? I usually eat a half cup of Quaker quick oats with milk for breakfast. How high are the oxalates in this portion? Thanks for your help!
Hi Becky,
My patients enjoy products made with oats. Look at the list we provide, you can see that oats are on the lower side. Making sure you get your calcium intake is most important of all to lower your oxalate.
Take care, Jill
Thank you, Jill. Adding more dietary calcium is something I will focus on.
I suffer from Lichen sclerosus and was led to this website saying a low oxialate diet would help. Can you tell the acceptable percentage per meal for me ? Or per day ?
Hi Michele, Lichen sclerosis is an immune disorder with complex treatments. It is not caused by oxalate nor treated with low oxalate diet. I did find spurious websites proposing low oxalate diet for it, but reliable sites – like Mayo linked here – do not include it. I have no reason to believe the oxalate molecule could indeed cause it. Regards, Fred Coe
I am trying to be low fodmap low carb and oxalate i can’t eat anything??!! don’t know what to do…
Hi Barbara, Given all this I have asked Jill Harris if she would answer you about diet. Fred Coe
Hi Barb,
You need someone who is experienced to help you sort out your different food restrictions. It can be overwhelming to say the least. Unfortunately it takes time and the work that is required is more than this email response can give. You can ask your doc for a referral to a nutritionist but finding one that is well versed in stone prevention might prove to be difficult. If you are interested I do this for a living and can help. Jillharriscoaching.com
Best. Jill
Morning. Wonderfully informative website. Thank you.
Question. As someone attempting to limit the amount of high oxalate foods I consume, I find myself totally confused about berries. I realize you state that the only berry that is high in oxalates is raspberries. However, many other sites (University of Pittsburgh Medical Center; University of Michigan Health Center; Kaiser Permanente, etc.) list all berries as either High or High-Moderate in oxalate level (including two of my favorites to have with morning oatmeal – blueberries and strawberries!).
How should I interpret this disparity among various healthcare websites? Especially, as relates to berries.
Thanks very much.
Hi Suzie!
Please don’t look at multiple websites. They will only confuse you. We use the Harvard list bc it works for our patients for the last 20 years. BUT. It is bc they follow all our advice from The Kidney Stone Diet. Must get your calcium intake up too. My patients eat blueberries and strawberries. Please use these fruits within a normal portion size. Most people got stones because they just ate too much period. Eat within portion size of things and this will help greatly. Also, items not on the list follow this advice. Eat within a normal portion size and once a week. With a calcium containing product when possible.
Have a good day,
Jill
Hi,
I had my first small stone in 2012 and then just last week I had a 2nd one. The doctor is getting the stone tested. I am certain that one problem I have is that I don’t drink enough water and I plan to increase my fluid consumption. However I also do eat peanut butter pretty much on a daily basis for breakfast because it is easy protein and it will be hard for me to give that up. I do also eat other high oxalate foods which I will have to work on. My question is – how much benefit will I get from drinking the proper volume of fluids? So if over the past 6 years I drank the proper amount of fluids, is it likely that I would have avoided this current stone? I know that is not easy to answer but I am trying to gauge the impact of fluid intake. It seems logical that more fluids will help flush small particles through the kidneys. Many Thanks!
Hi Patrick, Fluids alone are a weak approach. Peanut butter is a risk, but without 24 hour and blood testing you cannot know what is really your problem. Given two stones already I would have my physicians do it right and treat what seems to be the causes. Regards, Fred Coe
Have there been any trials to see if dietary modification (in people who have had a renal tract stone), has any measurable effect on the real world recurrence rate?
Hi Dr Bugden, There is one prospective trial of consequence, and it was positive. There was also one trial of high fluids – in the same article. My view is simple; the diet in the trial is more or less the same as the present US recommended diet for everyone, so I always recommend it – even for people with no stones! Fluids relate to new stone onset such that risk begins at volumes <2.25 l/d on average (same article – I put all the data in it) so I always aim for more. My goal is to lower supersaturations to 1/2 of where they were when I started, and if new stones appear or I cannot get that lowering with fluids and diet, I begin thiazide. I prefer to use it against a background of the lowest possible sodium intake so I can use very low doses and yet get good lowering of urine calcium sans much problem with potassium wasting. The thiazide trials seem to me, more or less, overwhelming in the aggregate: I would not bet against them even though trialists correctly say no one of them is completely rigorous. Regards, Fred
Hello,
I have chronic lyme disease and have been told to follow a Paleo diet. Many of the foods consumed in this diet include leafy greens. What are the portion sizes that I should be following? I have been including about 1-2 cups of blueberries and blackberries in my smoothies with kale and other veggies. I was told to have lemon water in the morning before my meals. Is this supposed to cleanse my system including my kidneys to help with possible kidney stones?
Thank you,
Jessi
Hi Jessi,
I assume you are a stone former? If you are, please get a 24-hour urine collection done so you can see if you need to lower oxalates. Too big a portion for foods, even healthy foods, can lead to a problem for stone formers. Many people do not need lemon water. It is fine to use, but it will not “cleanse” your kidneys or system. It can provide a bit of citrate and help if yours is low, but again, you need to do a 24-hour urine collection if you make stones to find out the best plan for your specific needs.
Best, Jill
Does anyone know the oxalate content of olive leaf extract?
Hi Brenda,
No oxalate in extracts.
Jill
Great information.
Question:
Do you have a list of high calcium foods and their calcium content? If so, can you provide a link? It seems that it is just as important to have that info for when pairing calcium with oxalates to lower oxalates excretion. Thanks.
Hi Terry,
Just google foods high in calcium and limit the ones that are high in oxalate.
Best, Jill
Great information.
Do you have a list of high calcium foods and their calcium content? If so, can you provide a link? It seems that it is just as important to have that info for when pairing calcium with oxalates to lower oxalates excretion. Thanks.
Hi Terry,
Just google high calcium foods and you will see. Remember to notice which might be high in oxalate, like spinach. If you tolerate milk, you can use it, if not you can also use flax milk. I personally think it is the quickest way to get your calcium needs met.
Best, Jill
I have long struggled with conflicting info. As just one example, your article above says Orange Juice is “great” – but I see it on other “high oxalate” lists. Can you help me understand? Otherwise this research seems like a total waste of time for me…
But I’m doing it because I’d really like to get it right.
Hi Tony,
There are many different lists out there. We tell our patients to use one and stick with it. The Harvard list we use has helped many of our patients lower their oxalate so we do trust it. Orange juice, when drunk in small quantities is fine and will also add to your total daily fluid output. Please remember our other advice, esp concerning calcium when choosing higher oxalate foods. Plus we need it for our bones as well.
Best, Jill