 In contrast to the almost normal appearing (except for sites of interstitial plaque) kidneys of idiopathic calcium oxalate stone formers (ICSF), our biopsy and mapping studies that now include ten additional kidney stone forming phenotypes (see Table 1), reveals striking changes in the renal medulla noted by both endoscopic and histopathology characterized by crystalline deposits in the lumens of inner medullary collecting ducts (IMCD), and ducts of Bellini (BD) (Figure 1), with less evidence of damage in the cortex.
In contrast to the almost normal appearing (except for sites of interstitial plaque) kidneys of idiopathic calcium oxalate stone formers (ICSF), our biopsy and mapping studies that now include ten additional kidney stone forming phenotypes (see Table 1), reveals striking changes in the renal medulla noted by both endoscopic and histopathology characterized by crystalline deposits in the lumens of inner medullary collecting ducts (IMCD), and ducts of Bellini (BD) (Figure 1), with less evidence of damage in the cortex.
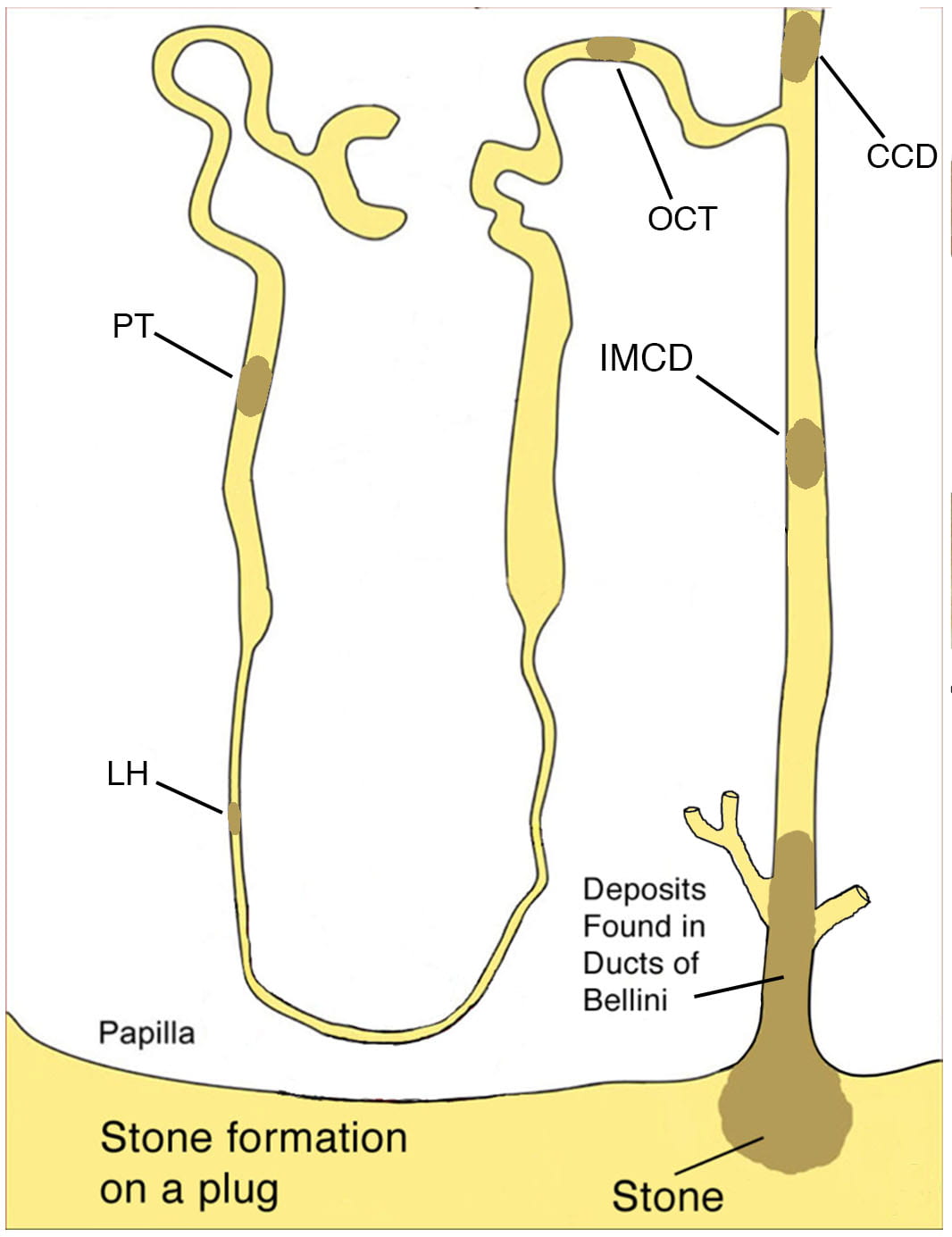
Figure 1.
Illustration showing a BD plug/overgrowth complex and other sites of crystalline deposition alone the nephron in human kidney stone formers. A crystalline deposit is noted plugging a BD and at the urinary end it is covered with an overgrowth or stone. Intraluminal plugs are also common in the IMCD and less frequent in the loop of Henle (LH), distal convoluted tubule (DCT), cortical collecting duct (CCD), and proximal tubule (PT).
Endoscopic and histopathologic characteristics of IMCD and BD plugs
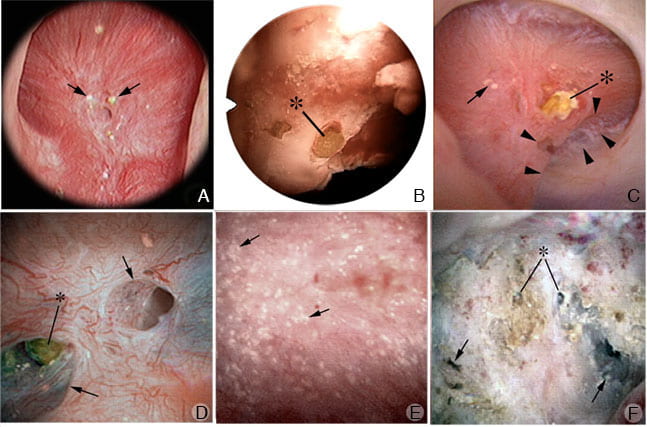
Endoscopic observations: Endoscopic examination of the renal papilla of all ten stone forming phenotypes listed in table 1 show varying degrees of change which include: 1) dilation of the openings of the BD some with or without protruding mineral plugs, 2) suburothelial sites of white (interstitial) and yellow plaque, 3) pitting and/or erosion of the tip of the papilla and 4) retraction of the papilla (Click on phenotype to see PubMed article).
Table 1
- dRTA – Distal renal tubular acidosis
- BP – Bypass surgery for obesity
- CYS – Cystinuria
- HPT – Primary hyperparathyroidism
- SBR – Small bowel resection
- ILEO – Ileostomy
- PHOX – Primary hyperoxaluria
- MSK – Medullary sponge kidney disease
- HASF – Hydroxyapatite stone formers (without systemic disease)
- BR – Brushite stone formers
Dilation of the openings of the ducts of Bellini at the tip of the renal papilla is a prominent feature of these kidneys (Figure 2, panels a-f). While the degree of dilation is generally about 2 or 3 times normal (Figure 2 panels a, b and f), the most extensive dilation (up to 20 times normal) is noted in brushite stone formers (Figure 2, panel c). The number of dilated BD also varies between phenotypes with the bypass for obesity patients showing the fewest (Figure 2a) and the dRTA (Figure 2f) and HPT possessing numerous dilated BD.
Endoscopic view of renal papilla from stone forming phenotypes with BD plugs and yellow plaque. Panel A shows papillary surface of intestinal bypass patient for obesity, revealing small round nodular structures of Randall’s plaque (arrows) near the opening of modestly dilated BD. Panel B shows a modestly dilated BD with protruding overgrowth (asterisk) on a plug from an ileostomy stone former while panel C shows a massively dilated BD with protruding overgrowth (asterisk) on a plug from an brushite stone former. Also note a site of Randall’s plaque (arrow) and pit (arrowheads). Panels D-F show a range of papillary abnormalities observed in stone patients with distal renal tubular acidosis. Panel D shows 2 modesty dilated BD (arrows) one with a visible plug (asterisk), panel F shows a field of diffuse yellow plaque (arrows) while panel F shows extensive papillary damage with retraction, loss of normal architecture, multiple dilated BD that produce a pitted appearance (arrows) some with protruding mineral deposits (asterisk), and a whitest thickened membrane appearance.
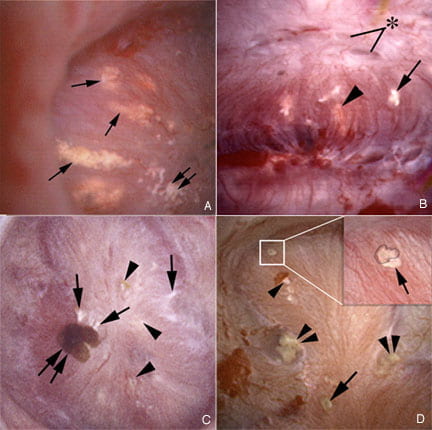
Yellow plaque represents deposits in the lumens of primarily IMCD, and BD (Figure 3). Yellow plaque in the lumens of BD is easily seen filling the openings of these dilated ducts or detected as protrusions from these ducts forming fixed stones. Fixed stones can form from end of those plugs protruding from dilated BD of any of the 10 phenotypes (Figure 3) (Table 1). These plug/stone complexes can be removed at the time of stone removal for further analysis (presented later in this blog). In addition, a few attached stones can be found at sites of interstitial plaque in HPT, ILEO, BR, SBR and HASF. Much fewer stones are seen in these phenotypes compared to ICSF patients.
Papillary pitting and retraction presents a quantitative gauge of architectural distortion that can be extensive in this phenotype. Brushite, dRTA and HASF patients can present extensive distortion of the normal papillary architecture compare to the other stone forming phenotypes.
Figure 3.
Endoscopic view of renal papilla from stone forming phenotypes with BD plugs, yellow plaque and attached stones to Randall’s plaque. Panel A shows extensive regions of yellow plaque in IMCD (arrows) and a single site of Randall’s plaque (double arrow) of a brushite patient. Panel B shows modest changes in a papilla from an ileostomy patient including dilated BD (asterisk), yellow plaque (arrowhead) and white plaque (arrow). Patients with small bowel resection (panel C) show attached stones (double arrows) in a region of white (arrows) and yellow (arrowheads) plaque. Patients with hyperparathyroidism (panel D) also have attached stones (within white box and insert) is magnified in the insert at the upper right; the stone is outlined within the insert by a black dotted overlay and the plaque border is indicated with an arrow. Areas of yellow (double arrows), white (single arrowhead) plaque and BD plug (single arrow) are seen on one papillum.
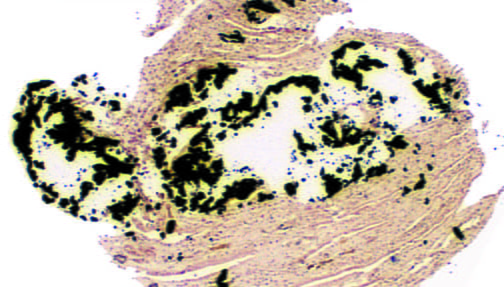
Histopathologic observations: The primary histopathologic changes of these 10 stone forming phenotypes are 1) mineral deposit formation along the distal nephron, 2) a loss of the tubular lining cells adjacent to sites of intraluminal plugs and 3) sites of interstitial fibrosis usually adjacent to the intraluminal deposits (Figure 3). The mineral deposits are seen to partially or completely plug tubular lumens and occasionally protrude out of the openings of the ducts of Bellini. While the primary sites of mineral deposition occurs in the IMCD, BD and outer medulla collecting ducts, mineral deposits are also found occasionally in the thin loops of Henle, distal convoluted tubules, cortical collecting ducts and proximal tubules depending on the stone forming phenotype.
Mineral type, size and number are the other critical variables concerning the characteristics of the intraluminal deposits. All three of these variables change depending on the stone forming phenotype. Hydroxyapatite is by far the most common mineral composing intraluminal deposits and is found in BP, dRTA, SBR, IlEO, HPT, BR, MSK, CYS and HASF. In HPT and HASF apatite in the only mineral found along the nephron. In dRTA, BP, SBR, and MSK apatite is mixed with CaOX, in cystine it is mixed with cystine, in ILEO it is mixed with sodium acid urate, and in brushites it is mixed with CaOx and brushite. In those phenotypes with a mixture of apatite and another mineral, apatite is usually found by itself in the IMCD and the mixture is located in the BD. PHOX is the only phenotype that exclusively has CaOx along the nephron including the proximal tubule.
The second major histopathologic change found in all stone phenotypes except ICSF, is a complete loss of adjacent lining cells at sites of crystalline deposition regardless of the mineral type (Figure 4). This finding probably explains way it is so difficult to remove plugs with their overgrowths, in that the intraluminal portion of the plug/stone complex is tightly fused to the basement membrane of the tubule. The only exceptions are the plug/stone complexes in the BD of cystine patients, whose plugs are easily removed at the time of surgery. In addition, we have not been able study the BD plugs of MSK patients by histology so we are not sure if there is cell loss at sites of BD mineral deposits.
The third histopathologic finding is interstitial fibrosis (Figure 4). The primary location of the interstitial fibrosis is in the medulla (mostly inner medulla) adjacent to sites of intraluminal deposits. Therefore, the extent of fibrosis is correlated with the number of plugged tubules. The exception is PHOX stone patients, where the level of papillary interstitial fibrosis is excessive for the number of plugged tubules and generally involves the entire papilla. The level of fibrosis probably correlates with the degree of papillary retraction. In addition, cortical interstitial fibrosis is prominent only in BR patients.
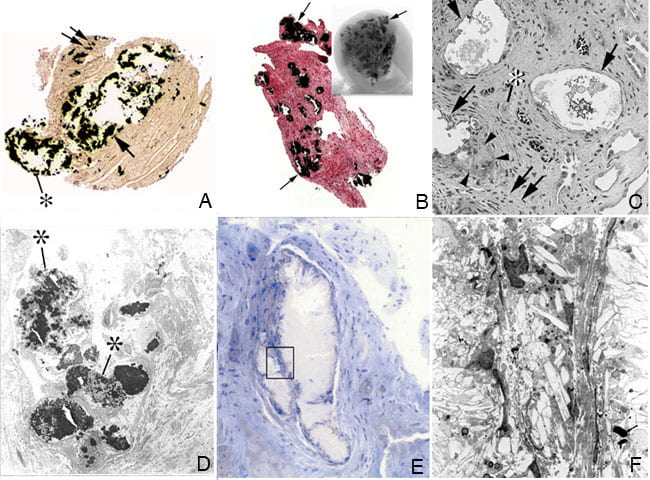
Figure 4.
Histopathology of renal papilla from stone forming phenotypes with BD plugs and yellow plaque. Panel A shows a light microscopic image of a papillary biopsy from a brushite patient revealing sites if calcium deposits (apatite in this patient) in an IMCD and BD stained black by the Yasue method (arrow). The crystalline material is seen protruding from the opening of a dilated BD. A small site of Randall’s plaque (double arrows) is seen. Panel B shows numerous IMCD’s filled with Yasue positive material (arrow, the mineral is CaOx in this patient) from a patient with distal renal tubular acidosis. This same biopsy was also viewed by micro-CT (insert) to show numerous, small crystalline deposits in the papilla of these patients. Panels C and D show the histological changes occurring to the lining cells of those tubules plugged with mineral in brushite patients. Panel C is a light micrograph showing extensive cellular damage is several IMCD (arrows) filled with mineral. There are extensive regions interstitial fibrosis (double arrows) surrounding the plugged IMCD, entrapped loops of Henle (asterisk) and evidence of giant cells (arrowheads). By transmission electron microscopy (panel D) the tubular cells show evidence of injury and are filled with crystalline deposits (asterisks). Panels E and F show a light microscopic and transmission electron microscopic image of a plugged IMCD’s from an intestinal bypass patient for obesity. There is a complete loss of all lining cells. The boxed area in panel E represents the region seen in panel F.
Overgrowths on BD pugs:
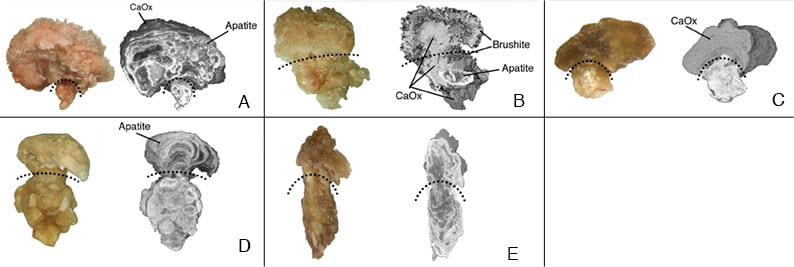
BD plugs present to the surgeon as dilated BD filled with crystals and sometimes crystals grow over these plugs protruding into the urinary space (video 1). The overgrowths on plugs have a variety of shapes (usually round) and are about 1-2 mm. Dr. James Lingeman has successfully pulled the overgrowth with attached intraluminal BD plug free from the BD allowing for detailed micro-CT analysis of the plug/overgrowth complex. Figure 5 shows a set of light microscopic and high-resolution micro-CT images of plug/overgrowth complexes from an HASF, BR, ILEO, PHT and MSK stone patients respectively. The BD plug of the HASF patient is only apatite while the overgrowth is primarily apatite with a crust of CaOx. The BD plug of the BR patient is a mixture of CaOx, BR and apatite, while the overgrowth has a core of CaOx and an outer surface of BR. The BD plug of the ILEO patients is apatite and urates while the overgrowth is entirely CaOx. The BD plug of the PHT patient is all apatite as well as the overgrowth. The BD plug and overgrowth of the MSK patient is primarily CaOx with a small amount of apatite. We have not been able to collect plug/overgrowth complexes from all 10 phenotypes but those we have been able to study show distinct patterns of mineralization of this complex unique to the stone phenotype. Dr. James Williams has been able to study the plug/overgrowth complex using µCT imaging (Video2).
Figure 5. Examples of BD plugs with overgrowths. Panels A-E show examples of BD plugs with overgrowth by both light microscopy (on left) and micro-CT (on right) for an idiopathic HA stone former (panel A), an idiopathic brushite stone former (panel B), an ileostomy (panel C), an primary hyperparathyroidism (panel D) and a medullary sponge kidney (panel E). A curved, dotted line divides the BD plug from overgrowth region.
Clinical consequences of overgrowths on plugs
It is conceivable that overgrowths on BD plugs could detach and grow within a calyx to reach 3 or more mm and present as passage of a clinical stone. The likelihood that an overgrowth would detach seems slim because our present data shows these overgrowths to be an integral component of the plug/overgrowth complex and most plugs are tightly fused to the wall of the BD. For discussion sake lets assume an overgrowth can detach, an obvious question arises: how would one know if a stone originated as the overgrowth over a BD plug and not on a site of Randall’s plaque or grew in free solution? Such a stone must have remnants of the plug at one border – where it was attached. We have not as yet observed removal of such a stone, but in fairness this has not been a specific surgical research aim.
Mechanisms of plug and overgrowth formation
A number of excellent studies have been performed on animal kidneys that have intraluminal plugs. However, only few studies have followed events that initiate human BD plugging. An appealing idea derived from cell culture work is that SS drives crystallizations, and some kind of tubule cell injury exposes hyaluronan rich areas of the membrane to the tubule fluid so that crystals may anchor there. Evidence for this in humans has come from studies of transplant kidney crystals in cortex, but no human studies have shown it in papillum except our own in which hyaluronan expression was found in cortex and papillum in the absence and presence of crystals in patients with PH1, and in the papillum of those with CaOx stones from obesity bypass. Hyaluronan expression was never found in papillae of ICSF even in regions of plaque. Other plug forming stone diseases have not as yet been studied in this detail. While urine SS values are a likely candidate controlling plug formation, SS in itself is not sufficient to explain composition of plugs and overgrowths. Pursuit of more basic understanding of plugging mechanisms in human tissues needs to go far beyond simple SS and crystallization.

Can a stone that’s embedded in the BP cause flank pain? The general theory is that stones don’t hurt unless they’re being passed (though I know too well from personal experience that stones inside the kidney can hurt), but it seems that a calcium growth literally plugging a filter of the kidney would cause pain. Is that incorrect?
Dear Becky, The inner medullary collecting duct plugs are indeed inside the kidney tissue. No one knows if they can cause pain. We know they can cause damage with scaring which means that inflammation has been present. So your excellent question is a research question, one which we hope to continue working on if NIH continues to fund us. It is a long road from discovery to practical outcomes! In the meantime, painful kidneys with many plugs may possibly benefit from surgery, but that is conjecture, simply an idea. Regards, Fred Coe
That’s a very good question Becky! I presume you suffer from chronic pain and have been told by your Drs and in ER when suffering from severe pain, but following CT or US, Drs have informed you that you are not passing a stone, there is no obstruction that “stones don’t cause pain unless passing”!? the same story our MSK group members have been hearing for years even though they have been diagnosed with MSK, nephrocalcinosis, RTA, recurrent stones, frequent UTI’s! Many of our members pass stones if not daily, weekly or monthly but so many others rarely pass stones (or need surgery for removal due to obstruction) all complain of daily chronic pain! I’m still wondering why Drs treating stone disease and MSK can’t just admit to chronic pain in this disease? Instead of putting up such a fuss? If there are so many patients all suffering from the same darned unrelenting daily chronic pain? I think it should be proof enough!! All we need now is for researchers to find out why!
Well add me to the ranks of the “god that hurts” but no obvious presenting cause group. Had a few stone episodes over the last twenty years but nothing that has lasted this long. (Several weeks😡)
My urologist said CT shows no obstruction and urine no infection. I am vetting my own symptoms and found pain is dramatically position sensitive. Sitting -especially in a car – is very painful. I have been able to pinpoint where pain initiates (left side rear flank just below rib cage and then radiates from back to front.)
If I sleep on my stomach with legs fully extended or stand up straight there is no pain. But lying on either side and sitting brings it on.
Will be returning to doctor to rule out tumor and hopefully figure out some course of action. This has been life limiting and really want to resolve it.
I have a problem. Whenever I take any sort of pill, weather it be a multiple vitamin, or even fish oil, or any off the shelf standard multivitamin, even including pain reliever like tylenol or ibuprofen, I get lower back pain, that last for a few days. The pain comes and goes, and moves from one side of lower back, to the other, or I can experience the pain on both sides of my lower back simultaneously. I have seen a nephrologist, and have taken blood and urin tests, including sonogram ( looking for kidney disease ), but all comes back negative. Nobody seems to know why my lower back hurts when I take any kind of pill. I need help, but I am at a loss. Anyone out there, have any suggestions for me?
Hi Chad, Given no stones or other kidney findings, I doubt the pain originates in your kidneys. I have no useful suggestions. Sorry, Fred Coe
Dear Dr. Coe,
Is it possible to have both Msk and BD plugs?
Hi Laura, In our published work, we found only one BD plug among 12 proven MSK cases, but all the MSK patients had dilated inner medullary ducts filled with the tiny micro-crystals I have spoken about. Regards, Fred Coe
I work at the Kidney Hospital in Brazil and i do mostly stones and I believe the BD plugs can cause lumbar pain in some cases despite the lack of scientific support.
I would say that the majority of caliceal stones, attached to the papila or not, do not cause any pain unless they move and obstruct. Nevertheless, in a very few cases, the patients have a lot of pain without any obstructing stone on CT scans, usually there are a lot of small stones ( 2, 3 to 6mm) incrusted in the papila and after they removal in a flexible ureteroscopy the pain magically stops. This is an exception, most people that have a lumbar/flank pain without obstructing stones will have an orthopedic cause for that pain. However, if no one believe in your pain, no osteomuscular pain is possible and you have a kidney full of small non obstructing stones, I do offer flexible ureteroscopy as a chance to get rid of the pain.
It is very gratifying to resolve those unusual pain cases, believe and listen carefully to your patients!!!
Dear Dr Bruna, Thank you very much for sharing your observations. Personally I think the same but evidence is hard to come by. Thank you, Regards, Fred
This nearly made me cry. Since I had a blockage at age 16 in the 70s, I have had bouts of severe flank pain for months on end, visiting ERs, minor emergencies, primary care docs and urologists. All tell me basically the same thing: we see nothing that can cause that kind of pain. Yes, you have tiny stones in your kidneys, but that doesn’t cause the pain. My last round lasted over a week when my PC doc was on vacation. It resulted in a kidney infection. The ER doc sent me home (with the nurse protesting under her breath.) I could not urinate and was wild with pain. Then I did pass a rather large stone. How can they be invisible in a CT scan? Three weeks later, my pain level still frequently goes up to, I’d say, an8. Generally, now, I just stay home with the pain and grit it out (I’ve had natural childbirth) rather than be treated like a narcotics seeker.
Hi Jo M, I do not quite understand what happened. If you passed a stone and had pain, that is the common situation. No one doubts that stone passage causes horrid pain. If you have pain and small non obstructing stones in your kidneys, that is the area of controversy. Infection itself surely causes pain. So I imagine your main problem is being one of the large number of people with small stones, not obstructing, and with considerable pain. This latter is presently a matter of concern everywhere, but no studies have as yet established the role of surgical intervention. In your case, physicians may not be able to recommend any specific surgery. However, I believe that crystal passage may cause some of the pain in some cases, so efforts to prevent crystals – identical to prevention of stones – may be beneficial and I would urge this course. In other words, undertake stone prevention measures, testing and treatments, and perhaps the pain will be better. Regards, Fred Coe
Jo M.
I have been living the same Life, I was finally diagnosed in 2010 after suffering almost 2yrs with the Chronic Pain. Dr. would say it’s All in my head ‘n that I was a “Drama Seeker” by this time in my life I had already had the last #6th of my healthy babies. All born incl. Twins Healthy ‘n Beautiful. So shortly after my MSK kicked in like Wham Ouuch!, Started telling Doc’s that my kidneys hurt. Nope All in Ur Head, 1yr ‘n half later I get Properly Diagnosed ‘n now Almost 12yrz Later I’m still Re-duced to living a Sad, Lonely Very Pain’ful Life that No-One in My Circle can Understand. I have Constant Flank Pain that Only Strong Meds have helped with only a small percent of the Pain. Dr have given me little to No Hope of a Normal Life. I’ve had to make Alot of Changes in my life. Ive Been Ridiculed ‘n Critizied ‘n have Lost Slot, But though through All the Darkness ‘n Sadness I never lost Hope or the Love for Myself or Others. I justed want to Reach out to let U know that U aren’t Alone, ‘n that just because No-One Else can Understand Wut Yr Sufferings R, doesn’t Define U. Meaning that No-One has A Right to Judge, Dictate or Make a Personal Opinion to how the Reality of Yr Life is. U just Live the Best U that U can.
It’s a Sad Reality in Our World that Science Choose’s who Live’s Matter. All We can do as Survivors is Live the Best of “Us” We Can.
Much LoVe. P. Mom
I have been dealing with kidney stones since 2005, passing 50+ over the years, lithotripsy three times and uteroscopy twice. My stones are primarily calcium phosphate. In 2005 I was diagnosed with Renal Tubular Acidosis, prescribed Sodium Citrate. I did not take it seriously and stopped taking the prescription pretty quickly thereafter. About 2 weeks ago I was diagnosed with MSK (via ultrasound) with calcification in the medullary of both kidneys.
I have been dealing with chronic flank discomfort (2-4 level on pain scale) for approximately six years and told that it probably just typical back pain that I attribute to my kidneys, however it worsens when I urinate.
I am getting a CT scan on Friday to see if there are any stones that need attention. I am thinking it may be best to request all stones, no matter location or size to be removed, a fresh start, continuing with prescriptions for RTA.
Is this is MSK or just RTA? Or possibly BD Plugs? What is the best test or methods to get answers to formulate a better plan moving forward? I have blood, 24 urine, ultrasound completed. CT scan next.
Hi Candace, You have plugging not MSK – almost surely – in that your stones are CaP. RTA means an abnormally low serum bicarbonate and an alkaline urine pH together.If your serum bicarbonate is not low, you are a calcium phosphate stone former with the high pH attached to that syndrome. Flank pain in people like you may well be renal in origin, the controversy right now is whether surgical stone removal helps. But with plugging, very possibly many of the ‘stones’ seen on CT will be plugs and they cannot be removed as being imbedded in your kidneys. Most CaP stone formers have high urine calcium, and that can be treated with reduced diet sodium and thiazide, with some hope of reducing stones. These are complex matters, and your physicians are responsible for your care. You might share my comments with them, and they may well dismiss them as I have no real knowledge about you. Regards, Fred Coe
i was told 20 yrs plus ago that i have MSK, i have had over 20 Litho’s, Lazer zapping and have had stone hand pick. now at the beginning i only had pain when passing stones, but now for the past 2 years i have pain daily in both kidneys, the level of pain varies from a 3 to 7 the ct shows many too many to count…i am hypokalemia and my gfr is all over the place between 46 and 56…my drs beleive me on my pain… but why so much cronic pain daily and will msk cause other health issues? cuz i have a ton…. surgeon said im a complex person
Hi Dianna, I wonder if you have MSK or another disease. MSK will not cause hypokalemia nor reduce your GFR. I would ask your physicians what they think have caused both of these. Are you taking a diuretic – a common cause. Pain is not rate in patients with many stones, and we do not know why nor whether surgery will help. Some of us consider OTC NSAIDS, because there may be inflammation, but your physicians need to be consulted if GFR is reduced. Regards, Fred Coe