
Uric acid stones, to me, means not just pure uric acid stones but any uric acid in stones. If this seems fey, let me explain. Uric acid is a peculiar kind of crystal. Low urine pH causes them and treatment that raise urine pH prevent them altogether. Whether they form combined with calcium stones or pure, treatment is the same.
Why then scruple over percentages? If I find uric acid in any stone, I look at urine pH with a yellow eye. Should it be low I treat it surely and on the moment so at least that crystal be banished forever.
The Profligate Punished by Neglect, Edward Penny 1774 catches the common motif of diet excess, obesity, diabetes, and gout – the joint manifestations of uric acid crystals. Note the abdominal fat denoted by his overly tight vest. All of these states can lower urine pH and lead to uric acid stones.
This article has a pragmatic leaning and eschews excessive scientific details. I have written a more mechanistic article that explores how the low urine pH might arise and cause uric acid stones. Read this one first unless you are already reasonably expert.
Who Are Uric Acid Stone Formers
Stone Analysis
Given my prior reasoning, I call patients who have any uric acid in their stones uric acid stone formers but reserve the right to use compound names when needed. If all stones are only uric acid, I call such patients pure uric acid stone formers. Those whose stones contain uric acid and other crystals I call mixed uric acid /x stone formers: mixed uric acid calcium oxalate, mixed uric acid calcium phosphate stone formers, as examples.
These niceties of naming have the practical value of calling to mind the perpetual need for dual or multiple treatments – for uric acid but also for whatever crystals might be present.
Radiographic Evaluation
Commonly uric acid stones show poorly on routine flat plate x rays having only carbon, nitrogen, oxygen and no heavier atoms such as calcium. On CT scans they do not look different from calcium stones but radiographic density can be measured and tends to be lower. As this article points out, machines differ in their results and evaluation may therefore be less than perfect. Dual energy scanners are more precise, but also prone to many potential artefacts. Multiple reports, by contrast, indicate that CT measurements of radiographic density can reliably distinguish uric acid stones from calcium stones.
A reasonable present view is that lower radiographic density is an excellent clue to uric acid in stones, but far from definitive as stone analysis is. I hesitate to classify a patient on scanning evidence alone.
Signs and Symptoms of Uric Acid Stones
Pigmented Stones and Crystals
Being stones, uric acid stones cause the usual problems of pain, obstruction, bleeding and infection. But they have some special features. The most obvious is stone color – red to orange because the crystals take up a variety of pigments mostly derived from hemoglobin breakdown. Recently scientists have determined the structure of one of these – urorosein. Sometimes, coarse or fine orange or red gravel passes, made up of uric acid crystals.
Rapid Crystallization, and Stone Growth
Because the crystals form not as a complex lattice like calcium with oxalate or with phosphate but simply as uric acid crystallizing with itself, the process can be swift to begin and require very little supersaturation. Said more technically the energy required to create the crystal is relatively low. This means the upper limit of metastability – the supersaturation needed to initiate crystal formation is not far from solubility, so values above 1 even if below 2, could suffice. Practically it means that bursts of supersaturation during the day can bring on showers of gravel and growth of stones.
Also, urine contains a lot of uric acid. Common daily losses of oxalate approximate perhaps 25 – 50 mg, compared to 600 – 1,000 mg of uric acid. The sheer amounts available when coupled to the rapid and facile crystal formation and growth allow stones to enlarge rapidly and achieve very large sizes, enough to fill the renal pelvis and calyces – so called staghorn stones.
Acute Uric Acid Nephropathy
Very uncommonly, sudden lowering of urine pH coupled with low urine volume can cause crystallizations in the terminal collecting ducts with acute kidney failure. This was once not uncommon during treatment of malignancies, but modern attention to uric acid surges from tumor killing has made it rare indeed. Today, one does not expect to see it apart from unusual situations.
Uric Acid Supersaturation
I made the figures for this section anew but from a lovely data file constructed some years ago by Joan Parks, who was my scientific colleague from 1976 until her retirement about 8 years ago. Her legacy of curated data files sustains a lot of my public writing, now, and she deserves a place in it. 
Effects of Urine pH
Uric acid crystals form like all crystals because of supersaturation. In this instance, that supersaturation varies remarkably with urine pH.
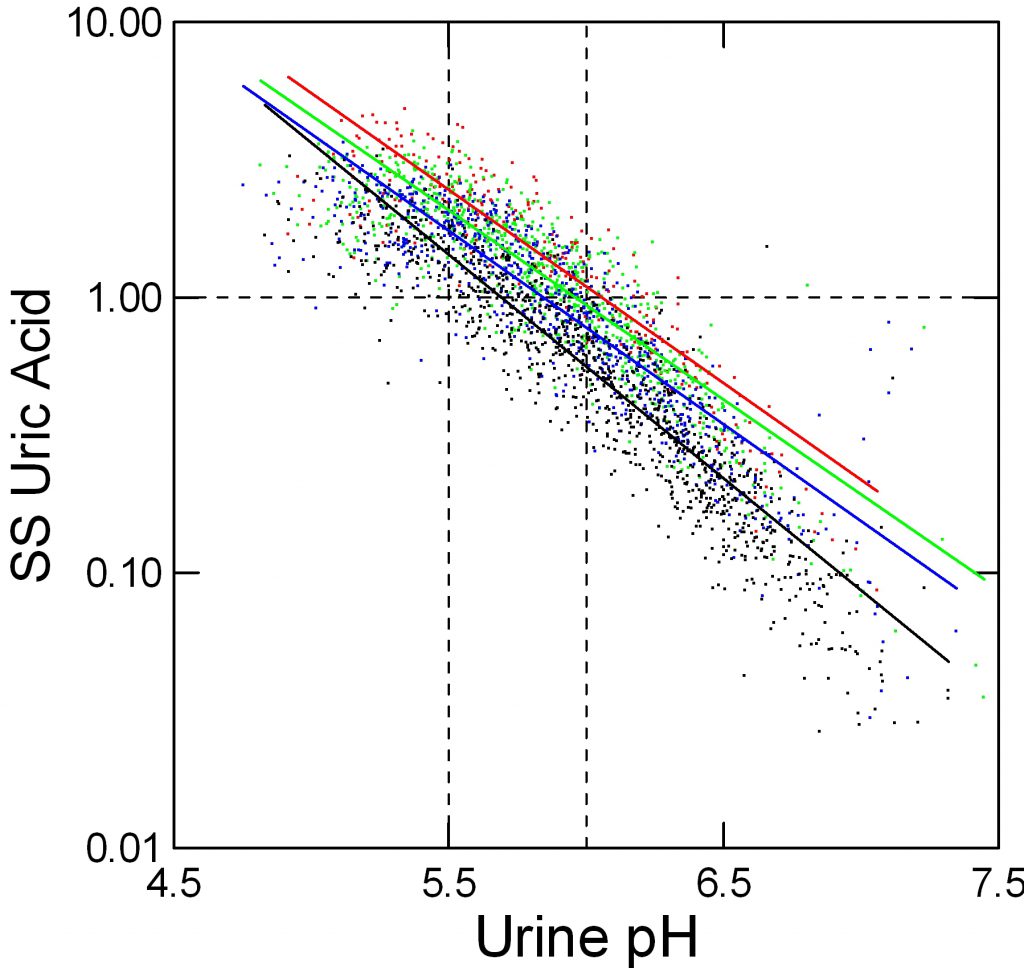
In the figure, supersaturation ranges from 0.01 to 10 fold. The dashed line at 1 represents equilibrium, or saturation, the level where crystals neither form nor dissolve. The horizontal axis shows urine pH. The dashed lines at 5.5 – acid urine and 6 neither acid nor alkaline urine are for visual reference.
The tiny points each are one 24 hour urine from patients and normal people. Like an ancient Persian scimitar, points curve downward from 8 to 0.03 as pH rises from 4.5 to 7.5.
Effects of Urine Volume
Urine volume matters. Low volumes (red) 0.5 to 1 liter/day give higher supersaturation than 1 to 1.5 liters/day (green), and 1.5 to 2 and above 2 liters/day (blue and black) lower supersaturation progressively.
But pH trumps volume. At pH 5.5, the whose distance from red to black varies supersaturation between about 2 and 5 fold (use the lines for averages) whereas raising pH from 5.5 to 6 brings almost all the points down below 1. Below 5.5 virtually no points are below 1 at even above 2 liters of urine volume daily.
Effects of Uric Acid Excretion
In speaking about excretion of uric acid we need to insert a note about the molecular species involved.
Form of Uric Acid in Urine
Uric acid is a weak acid, which means it can take up or donate a proton to water. When it has its proton, that proton neutralizes much of its charge, so water molecules cannot themselves form charge bonds with it to keep it in solution. This means that the molecule becomes very poorly soluble and tends to crystallize.
When it loses its proton into solution, it has a charged site for water to relate to and also requires a counterion, which in urine will be sodium, potassium, and ammonium ion. These ‘salts’ of urate – the name for uric acid when it has given up its proton and is a charged ion – can themselves form crystals just like calcium and oxalate form a salt – calcium oxalate – that can crystallize. But all three salts have much higher solubility than uric acid itself.
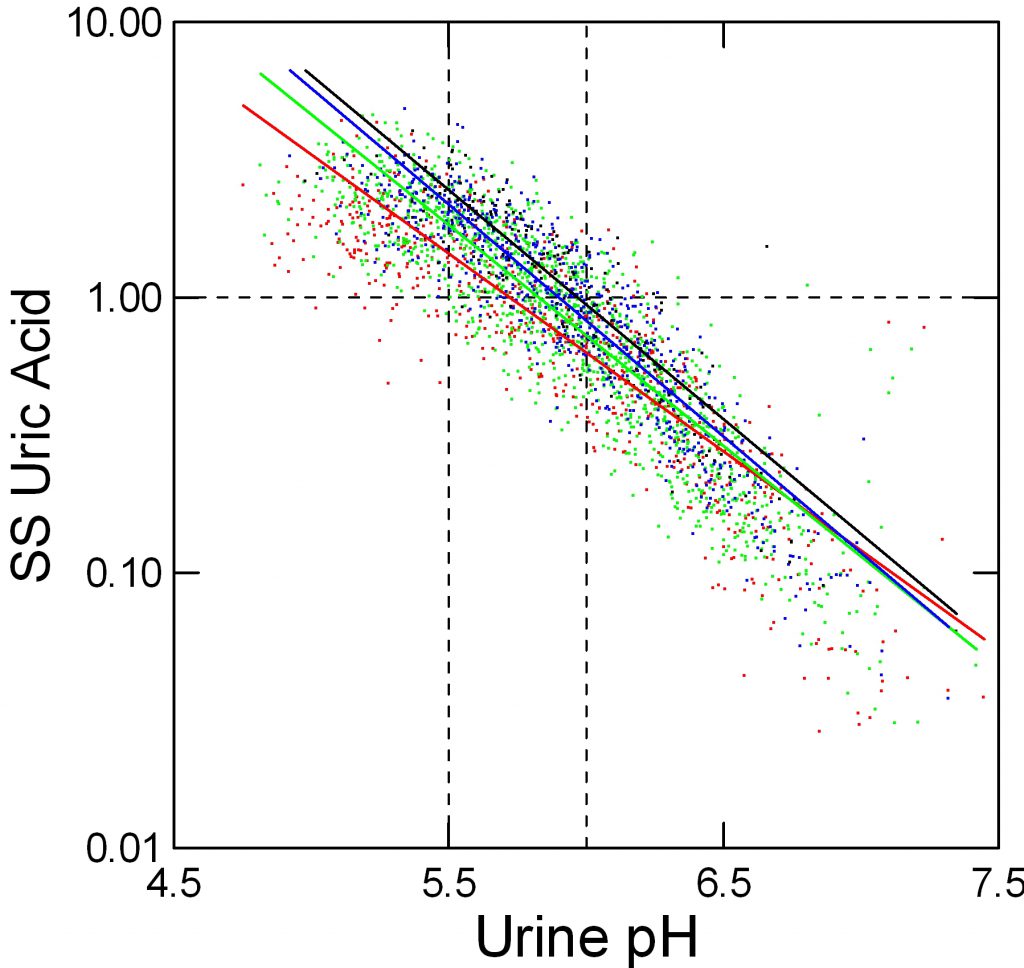
Effect of Uric Acid Excretion on Supersaturation
When we measure and report urine uric acid excretion we show the sum of all salts and the acid in one number. Obviously this total should affect supersaturation, but the effect is relatively small because so much depends on pH that sets the percentage of uric acid per se – the fraction that has its proton and is therefore poorly soluble.
Here, red, green, blue and black stand for below 500, 500 to 750, 750 to 1,000, and over 1,000 mg/d of urine uric acid excretion respectively. As for urine volume, the total amount of uric acid matters; a fivefold increase from below 500 mg to over 1,000 mg/day raises supersaturation at pH 5.5 from about 1.2 to about 3 fold.
Urine pH of Stone Formers
One presumes that urine pH of uric acid stone formers must lie below that of other kinds of stone formers, and numerous reviews and case descriptions have proven this true.
My own collected data make the point as well as any.
The dot distribution just below shows individual 24 hour urine pH measurements for calcium oxalate (blue), calcium phosphate (green) and uric acid (red) stone formers. Here I include among uric acid stone formers those with both pure and mixed stones.
Calcium oxalate stone former pH ranges widely with an average at about 5.8 pH units. Calcium phosphate stone formers average a lot higher – around 6.4.
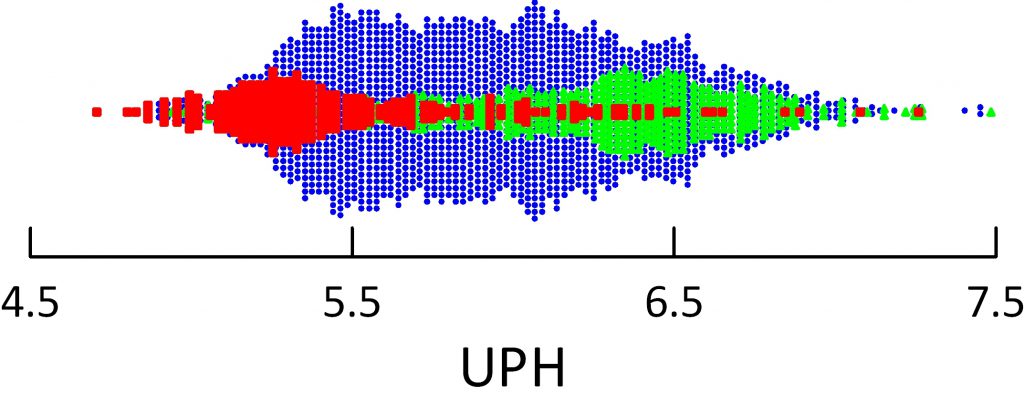 Uric acid stone formers lie in an acid range. Their average is about 5.3 – 5.4 and only a tiny scattering of points range above 6. So uric acid stone formers produce a very acid urine compared to other stone formers, and the pH is exactly in the range to produce supersaturation that can drive formation of uric acid stones and hold them steady or cause them to grow.
Uric acid stone formers lie in an acid range. Their average is about 5.3 – 5.4 and only a tiny scattering of points range above 6. So uric acid stone formers produce a very acid urine compared to other stone formers, and the pH is exactly in the range to produce supersaturation that can drive formation of uric acid stones and hold them steady or cause them to grow.
To see this, just look back on the graphs showing supersaturation vs. urine pH. Below 5.5 values almost all lie above 1 – solubility – meaning that crystals can form and grow.
UA Fraction in Stones
The General Pattern
I have said that any uric acid in stones means pH should be raised because at least that portion of the stone burden might dissolve or at leasts not grow.
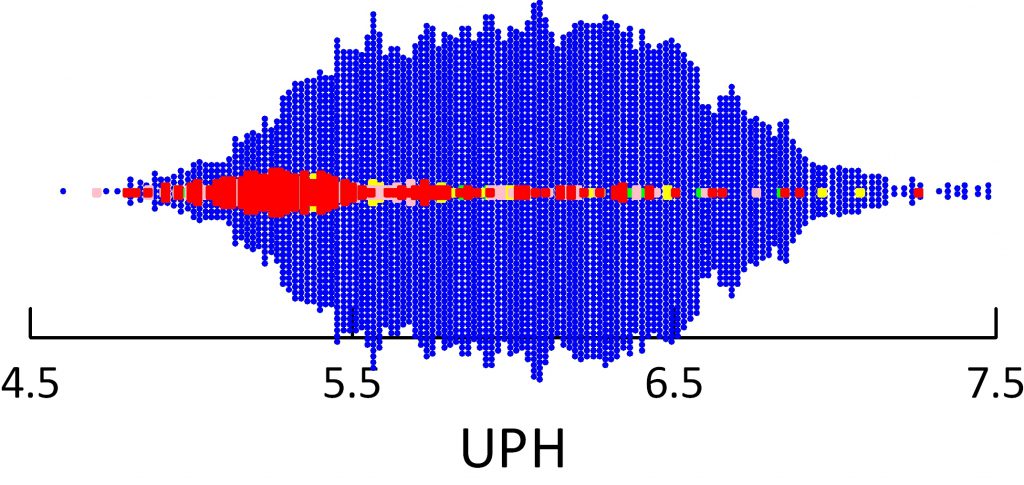 The figure below shows urine pH associated not with the kind of patient – calcium oxalate, calcium phosphate or uric acid stone former, but by the fraction of a given stone made up of uric acid.
The figure below shows urine pH associated not with the kind of patient – calcium oxalate, calcium phosphate or uric acid stone former, but by the fraction of a given stone made up of uric acid.
Blue means no uric acid at all. Red means 100% of the stone is uric acid, and pink and green lesser amounts. With a scattered few points as exceptions, stones made of mainly uric acid go with urine pH values mostly below 5.5.
The graph makes a point we often speak of but rarely show. Oxalic acid has a very low pKa – is a strong weak acid. So it has charges available for binding to calcium that very hardly at all with urine pH all the way down to 4.5, about the lowest value human kidneys attain. So these stone crystals are indifferent to pH.
Paucity of Mixed Stones
I makes another point, too, one that a patient emphasized in a comment to this article and that I failed to mention in the original version. Of all stones that contain any uric acid, at least in my collection of data, most are mainly composed of uric acid. See where the red – pure uric acid – stones make up the largest mass in the figure just above?
This is not to say that patients are uncommon who make both calcium and uric acid stones – mixed stone formers. The graph shows the stones themselves. People who make both kinds of stones need treatment with alkali so they will stop making uric acid crystals. They also may need treatment against their calcium stones. Stones that contain both uric acid and calcium – usually calcium oxalate – mean the patients may need treatment against both their uric acid stone formation – that would be alkali, and for their calcium stone forming.
So in the final analysis, whether the stones are mixed, or patients form both uric acid and calcium stones the answer is the same: Treat against both crystals.
Who Produce Uric Acid Stones?
Low pH Without Intestinal Disease
Genetic Factors
In identical twin studies, urine pH had only a 60% concordance compared to over 90% for calcium excretion. In a larger study urine pH seems as heritable as urine calcium excretion. Of interest, such dietary traits as sugar, calcium, and protein consumption that could influence stone formation also had significant heritability.
Systemic Disorders
Historically, uric acid stones have been linked to gout. A recent but brief review repeats that fact. Likewise, another review.
Given low urine pH drives uric acid crystallization, one has to ask whether some kinds of patients might be expected to produce acid urines. In answer, those most common are obese, older, diabetic, hypertensive, and prone to modest reduction of kidney function. Obesity itself, without necessarily overt diabetes correlates with lower urine pH in a progressive manner – as obesity increases urine pH falls.
Resistance to the actions of insulin – so called insulin resistance – is often invoked as a general paradigm to encompass the general class of abnormalities that lower urine pH. Metabolic syndrome, a mix of insulin resistance with lipid and vascular abnormalities is linked to kidney stones. But not to uric acid stones per se. Attempts to link uric acid stones to gut bacteria – use of the genetically defined biome -failed in a tiny study to disclose any species unique to uric acid stones.
Kidney Physiology
At least one specific abnormality that produces the low pH is an inadequate production of ammonia with which kidneys can remove acid. I plan another article on uric acid stone formation that will review the underlying disease mechanisms, and do not wish to burden this text with more detail. The linked articles from the group at UT Southwestern Medical School give access to the best current work on the subject. Essentially uric acid stone formers respond to acid load with less ammonia than normal people. Insulin resistance probably produces the renal tubule abnormality.
The issue is complex, as illustrated by a recent publication that found no evidence for low urine ammonia in uric acid stone formers. But the conditions of that study – mere measurements made in uric acid stone formers with comparisons to normal ranges hardly have any power to test the ammonia hypothesis.
In an elegant analysis of a single patient, Kamel and his colleagues point out two matters I use in my own work. Urine ammonia needs to be viewed in relation to urine sulfate – the net acid load. Likewise, the low urine ammonia of their case was accompanied by a high urine citrate – this occurs when proximal tubule cells consider themselves in an alkaline state that would cause a fall in ammonia production.
I have allowed myself a bit more about the urine pH than perhaps is ideal, and will end here. Either I will write another article on this subject or expand this one with my own data on ammonia and citrate.
Intestinal Causes
Intestinal Diseases
Any organic cause of diarrhea can lower urine pH because the fluids contain appreciable bicarbonate, the main blood buffer. In turn kidneys increase acid excretion in compensation. This requires both an increase of ammonia excretion and lowering of urine pH. Common situations include small bowel resection for such conditions as Crohn disease and partial or complete loss of colon. The latter, ileostomy, can cause marked alkali loss with acid urine and uric acid stones.
Chronic intestinal fluid losses also deplete body sodium and potassium. The 24 hour urine is very valuable for assessing both as excretion rates fall with such losses. Repletion with a mixture of sodium and potassium alkali is often valuable.
Bariatric Surgery
Howsoever valuable, these can result in both enteric hyperoxaluria and chronic alkali loss so calcium oxalate and uric acid stones do occur. The former are more common. This recent and excellent review details new stone frequencies but stone analyses are not widely reported so I cannot state the balance between calcium oxalate and uric acid crystals. Treatment with potassium alkali is recommended to increase citrate and pH.
Overuse of Laxatives
By increasing Gi fluid and alkali losses one might think these drugs would cause uric acid stones. In fact, a recent review of reported cases – not many! – suggests that mainly low urine volumes from fluid loss causes calcium stones. Not uric acid, in fact, but ammonium urate stones have been documented. I presume they represent induction of ammonia production by the potassium depletion from the diarrhea. As ammonia increases urine pH can rise despite loss of alkali and the higher pH would favor the ammonium acid urate salt.
What Happens With Treatment
Changes in Urine pH
In principle, potassium alkali in the proper dose will raise urine pH and abolish uric acid formation. The reality of practice has a bit less perfection.
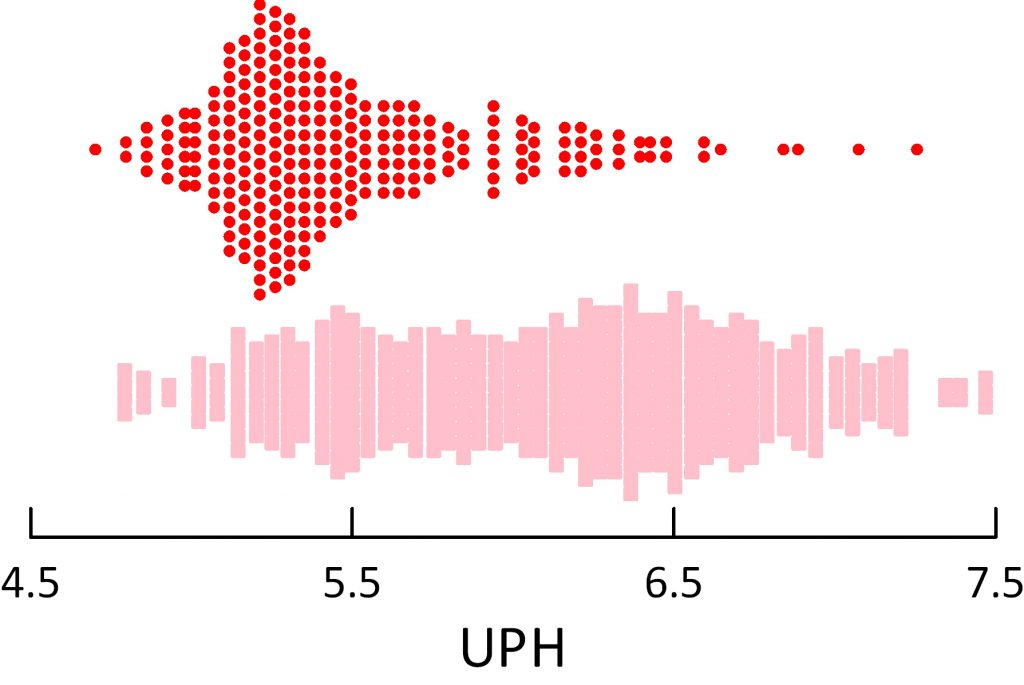
These are data from my own work.
The original pretreatment urine pH values are at the top of the figure, for reference, in red. Below them, in pink squares the treatment data show a large shift toward high urine pH so that a majority of values lie above the pretreatment ones. But some patients did not take their medications, and in some I miscalculated the dose needed.
Even with this natural variation in physician intent and patient willingness, the shift of pH with treatment was drastic in my own practice.
Given the powerful dominance of pH over supersaturation, I decided to not add a figure showing that supersaturation fell – it would be redundant.
Treatment Complexities
Potassium
Although potassium alkali – potassium citrate or potassium bicarbonate preparations are an obvious and widely used treatment, the kind of patients involved – often older, diabetic – may not tolerate large amounts of extra potassium without increasing serum potassium. Especially, common and effective blood pressure medications such as angiotensin converting enzyme inhibitors or receptor blockers can worsen the risk. Typically most clinicians are aware of the problem and proceed based on serum potassium level and whether kidney function is normal or not. Sometimes I use a low dose of thiazide diuretic along with potassium citrate – the diuretic to foster renal potassium loss. This can enable patients to get more alkali without risk of raising serum potassium.
Sodium
In the intestinal diseases, sodium depletion may be great enough one wants to use sodium alkali. I prefer inexpensive sodium bicarbonate tablets bought over the counter, being cheap and easy to use. Two provide about 13 mEq of base.
Dosing
I almost always begin with 40 mEq daily and repeat the 24 hour urine measurements. Spot urine pH testing with pH paper never impresses me as very useful because results scatter and, after all, what most matters is average supersaturation over the day. These crystals can form and dissolve rather rapidly, and one hopes to achieve 24 hour average SS below 1. Overnight is clearly a high risk because of lower urine volumes so a nighttime dose of alkali before bed seems reasonable. If I need to I increase dosing in 20 mEq/day increments.
Effect on Uric Acid Stones
Uric acid in stones has a different meaning than we attach to calcium oxalate or calcium phosphate, or even cystine. This crystal can be prevented by raising urine pH within the common physiological range between 4.5 and 6. This means that simple alkali treatment should and will prevent such crystals in stones. Likewise, lowering supersaturation below 1 must eventually reduce kidney stone mass. Put another way, not guile or special knowledge but simply persistence with alkali use must inevitably stop uric acid crystallization.
Even so, data are hard to come by. This small report says that 91% of 24 uric acid stone formers treated with potassium citrate had no recurrence after a mean of 31 months.
No Formal Trials
A look on PubMed found no prospective uric acid stone prevention trials.
(For the purists, this was my search: ((“prevention and control”[Subheading] OR (“prevention”[All Fields] AND “control”[All Fields]) OR “prevention and control”[All Fields] OR “prevention”[All Fields]) AND (“uric acid”[MeSH Terms] OR (“uric”[All Fields] AND “acid”[All Fields]) OR “uric acid”[All Fields]) AND (“calculi”[MeSH Terms] OR “calculi”[All Fields] OR “stones”[All Fields])) AND Clinical Trial[ptyp])
I am not surprised. Given all we know can we assign such patients to a control group that does not receive alkali? Given the ease of use should one even try to do so?
I say not.


Dr. Coe – I am a 47-year old female with muscular dystrophy. The lack of ability for much movement/exercise has lead to the onset of Type 2 diabetes. After 2 stone episodes (none of which were collected) and a 24-hour urine test, it appears as though I am a uric acid stone former. My ph level was 5.217. My SS Uric Acid was 1.68 and my Urine Uric Acid was .750. My urine citrate is high – 1455. My nephrologist wanted to put me on a 30 mEq prescription for potassium citrate. (3 pills a day.) I’ve read about the potential side effects of potassium citrate i.e. the potential for muscle weakness and the gastrointestinal upset. I am very hesitant to take these pills primarily because of the risk for muscle weakness with my muscular dystrophy but also because I have a very sensitive stomach.
I read your article about the cost of potassium citrate (another strike in my mind) and about the citrate levels in Crystal Light. Was wondering if your patients have seen much success going the beverage route for remedying urine ph vs just going on the pills? Is drinking a liter+ of Crystal Light spaced throughout the day, along with lowering my sodium intake and animal protein likely to help and circumvent the need for me to be on the pills? I also read where you said uric acid crystals can form very quickly. What are we talking about here – for example, if you don’t have enough citrate (through the beverage route) in one day because of travel, will you form crystals/stones that quickly?
Sorry for the multiple questions. I am taking the class with Jill Harris (it is EXCELLENT) but I have such a unique situation with the muscular dystrophy/diabetes combo that I wanted to ask these questions specifically to you. Thanks in advance for your reply.
Hi Kim, Your low urine pH is indeed a cause of uric acid stones although you do not know you form them. Diabetes indeed can lower urine pH and also raise urine citrate. Beverages like Crystal light can raise urine pH and I suggest you try some – a liter is said to have 20 mEq of potassium alkali. If it works, use it. Indeed uric acid crystallizes rapidly, often forming obvious red or pink crystals in the urine. So raising the pH is a good idea. More, try to collect some crystals and be sure. Regards, Fred Coe
Thanks so much, Dr. Coe. I’m trying to get a sense of what you mean by “rapidly.” Could uric acid crystals form in only one missed day of citrate treatment? During my first stone episode 9 months ago, I did see small red crystals in my urine but have not seen anything since.
Hi Kim, Yes they can. Uric acid crystallized when urine becomes acid, and in a day red crystals mean uric acid. Take your med. Regards, Fred Coe
I am trying to understand the “UA fraction in stones” graph. Majority of the graph is either blue or red (mostly blue). Very few pink or green points. Does this mean that mixed uric acid stones are very rare?
When one does have a mixed uric acid stone, is the fraction of uric acid pretty low compared to CaOx in general? Or could this fraction span the gamut..i.e… 1%-99%
Thanks
Jason
Hi Jason, You are a good reader of graphs. Most stones have little uric acid. When one does have a mixed stone the fraction of UA can be very low or very high with a scattering of points in the middle – just like the graph. I am going to edit the article to make this point more obvious and Thank you for being such a help. Fred
Thanks Dr. Coe.
Is it harder to dissolve the uric acid portion of a partial uric acid stone , as compared to a pure uric acid stone with K citrate?
I guess if the uric acid stone is covered all the way round with Ca oxalate this could be the case.
On that vein, do Calcium oxlalate crystals get attracted to uric acid stones and form over them?
Thanks
Jason
Hi Jason, yes it can be because calcium oxalate will not dissolve. I believe calcium oxalate will nucleate over uric acid. Even so, alkali is the right thing, and over time the stone will either dissolve or at leasts stop growing, and no new ones form. REgards, Fred Coe
I had an illeo-anal-anastamosis more then 25 years ago. For many years I had many bouts of uric acid kidney stones and small bowel blockages. Sometimes at the same time. I have been on Potassium Citrate for many year. First at 60 units a day then a 30 unit maintenance dosage for the last few years. After surgery to remove scar tissue three years ago I have not had any kidney stones or blockages but have had one in stuck in one kidney for more then three years. I just went though a bout of uric acid bowel stones. My urologist suggested increasing the potassium citrate to raise the PH of my urine.
If the solution to the uric acid bowel stones and the dissolving of the old kidney stone is an increase in potassium, will I be able to absorb sufficient potassium through mu digestive system without a colon?
Hi Alan, Certainly ileostomy causes low pH and uric acid stones – have not written an article on this but need to. You can use sodium or potassium alkali as all ileostomy patients have low urine sodium – their bicarbonate losses are sodium bicarbonate more than potassium. I do not understand uric acid bowel stones – bowel fluids lost are all alkaline, so perhaps you mean bladder stones. I often use simply sodium bicarbonate OTC tabs two are 12.5 mEq of alkali and so two tabs 4 times a day gives quite a bit. Your 24 hour urine tests give urine sodium and if it is low, as usual, perhaps your physician might want to use sodium and potassium together so neither has to be pushed. Do not make any changes without discussing them with your physician. Absorption of the sodium bicarbonate is high up in the intestine. Regards, Fred Coe
Dr. Coe,
Would most people who form pure uric acid stones or mixed uric acid stones with high uric acid content, tend to pass red or orange gravel in their urine?
Thanks
Tom
Hi Tom, Yes. And, treatment makes the gravel go away on the day it begins. Regards, Fred Coe
Dr. Coe,
Your chart shows that after pot citrate treatment, the pH shifts from below 5.5 to 6.5 or above. Especially for a mixed stone former (CaOX and Uric mix) , doesn’t this dramatically increase the risk of forming CaP stones?
Especially for a mixed stone former, wouldn’t a less risky proposition be to reduce uric acid in urine via meds to see if one can get Uric Acid SS below 1, and if that is not enough, add a little bit of alkali to get you over the hump?
Can you also explain the downside of using meds to lower high levels of uric acid in urine, when serum uric acid is normal?
Thanks
Tom
Hi Tom, Good thinking but not quite. The pH effect is too strong vs. urine total urate. From 5 to 6 the fraction of total urates in the form of dihydrogen urate – the one that crystallizes – falls to nearly nothing. However you raise an important point – no one needs to raise urine pH too high. Typical pure uric acid stone formers tend to have unremarkable calcium kidney stone risk factors, and alkali lowers urine calcium. So alkali is pretty safe. But mixed stone formers are an issue and one needs to treat against both kinds of crystals – almost always uric acid and calcium oxalate; phosphates and uric acid rarely cohabit. As for meds, allopurinol will drop urine uric acid from about 750 to 450 ot 500 when used in a typical 200 mg dose, but the benefit in sparing alkali is trivial and there are side effects – allergic reactions – that are not always benign. Higher doses asociate with more such reactions. Regards, Fred Coe
Dr. Coe,
Thank you for that explanation. But I am a little confused about your statement “From 5 to 6 the fraction of total urates in the form of dihydrogen urate – the one that crystallizes – falls to nearly nothing”. How is that possible when there is a big cluster of red dots between UPH 5 to 5.5? Maybe you meant to say “from 5.5 to 6”? Please correct me if I am wrong.
Also, how do you explain the red dots above UPH 5.5, and especially above UPH 6, even though they are not as abundant?
Thanks
Tom
Hi Tom, The two supersaturation graphs are the first two in the article – SS vs. urine pH. Above pH 6 no more than about 10 tiny dots are above the line at 1 meaning all the rest – about 2000 – are undersaturated. The big color dot graph – the third in the article – shows patients, and their urine pH is as a function of stone uric acid content. Stones are geological consequences of supersaturation, and no doubt some patients had partly treated themselves by the time I got these urines. They are from before my treatment, but need not reflect their state when they formed the stones. Regards, Fred Coe
Dr Coe: It is necessary any preservative in the 24 hour urine collection to size the urine pH?; and more, It is necessary any preservative in the 24 hour urine collection to size the urine concentration of calcium, oxalate, uric acid, etc?
Hi Victor; Preservative is crucial against bacterial overgrowth. Thymol has been in common use and will hold a urine for a few days. Best, Fred
Thanks Dr Coe
I’m currently using A Vogel alkaline powder to increase my PH – was also instructed to limited animal products e.g. Sausages and red meat and processed foods to the bate minimum to combat Uric acid stones – I’m also drinking 4 liters of water per day and and night the juice of one lemon – I was told to get my urine PH level up to 6.5 at least – what is your comment
Hi Richard, if you have uric acid stones as your sole stone problem, potassium alkali enough to raise 24 hour average urine pH above 6 will prevent recurrence. But be sure about other issues and also that your stones are pure uric acid. As for purine sources, they affect urine total urate species but have little benefit on uric acid stone formation given a urine pH above 6. Likewise, with that pH urine volume of 2.5 liters is plenty. As for lemons, do it if you want but I prefer the constancy and reliability of potassium citrate. Regards, Fred Coe
Dear Dr. Coe,
My doctor is adhering to your plan… I am 65 years old and recently had surgery for a 100% uric acid stone 9mm. He has prescribed 10MEQ tabs, take 2 tablets morning and night of potassium citrate as a preventative measure., he read your column about 40 to be taken. Is this sufficient to prevent or is this an overload?, I never had stones before. Thank you so much, I never did ever see red or orange crystals in my urine? Thank you for your help Dr. Coe!
Hi Gail, The potassium citrate is ideal for preventing uric acid stones. One does 24 hour urine studies to see what the results of the drug have been and makes adjustments as needed. Your physician will no doubt do that without difficulties. Usual causes of the low urine pH that causes uric acid stones are diabetes, insulin resistance, or obesity. These can be improved when possible and the dose of alkali may fall. You need not have seen the crystals – some do some do not. Regards, Fred Coe
Hi Dr. Coe,
I passed calcium stones in the past. In March 2017 I took a trip and did not take enough fluids during 14 days. I started with urinary symptoms and my FD treated me for infection with 5 days of Cipro. After that, the symptoms increased and I released 2 stones, one is 3 mm and it looks like uric acid stone. Since then I have been releasing crystals in my urine, my pH is around 6 and I am on allopurinol right now, then my blood uric acid went back to normal. The urologist sent me for a dynamic test of the bladder and CT, all came back normal. Anyway, he does not think I have uric acid crystals although he never sent the stones for testing nor checked the uric acid concentration/pH in 24-hour urine sample. He says that increasing the pH will not help, but the symptoms persist. Any thoughts on how to proceed?
FYI, I am a scientist so I have access to a microscope, then I have pics of the crystals and the stones. I also got urine strips for UTI control, they show nothing else but leukocytes. How could it be possible that my urine analysis comes back always normal from the lab?
I do appreciate your input. Thank you in advance,
Adriana
Hi Adriana, I cannot be sure at this stage, but surely the first step is to take that 3 mm stone and have it analysed. The usual method is FTIR and it costs very little. I would work from there. Given your urine pH uric acid would not be my prime guess as to your stone type. Likewise, allopurinol may have no basis for use. Regards, Fred Coe
Thank you, Dr. Coe, for your prompt reply.
Since I am living in Winnipeg, Canada, could I send my stone to your lab for FTIR? if so, who should I contact to make arrangements for shipping and payment? I have them taped to a microscope slide for now.
Your advice will be much appreciated
Regards,
Adriana
Hi Adriana, You can send them. We outsource to Beck labs in Indianapolis, but can get the testing done and send you the results. The university pays for it, but we can pull out your sample and you can send the payment. It is not very expensive. Get rid of the tape and put them into some tissue in an envelope – chemicals on tape can show up or blur tacings. I would fed ex the materials. Call Kathleen Dineen at 773 702 1475 monday and she will get you the right address. Let her know we arranged this on my site as she will never find this among all of the other messages. Regards, Fred Coe
Thank you so much!
I just released a new one, 1 mm probably bigger which correlates with the worsening symptoms that I have been having this week.
Your help is very much appreciated. I will contact Kathleen on Monday.
Adriana
Dr. Coe,
I just received the report back from the lab and it says that the material is all blood and tissue. Any thoughts on that? My symptoms are not going away, I am now on 10 days of Cipro but if the stones cannot be detected it means that I do not have them and no one will put me on treatment for that. Anyway, thank you very much for your help with ruling this out.
Adriana
Hi Adriana, If there are no crystals, it is hard to figure out what to do. But I would keep sending solid things in urine as there may be crystals and the test is not very expensive. Urine should not have anything in it but fluids. Regards, Fred Coe
Thank you, Dr. Coe. I will follow your advice.
Adriana
Hello Dr. Coe,
I am no stranger to kidney stones, as I was blessed with my first one in July 2014, and have had lithotripsy once for a 6mm and had “bladder crystals” removed as well in September 2016. I have passed several stones without going to the doctor, as I have almost gotten used to it. About 2 months ago, I passed a very unusual stone, as it was soft, “squishy”, and at first very sticky to touch. I since have passed 3 more (total of 4 of these squishy stones in the past 2 months), and my 3rd one was sent to the lab by urologist for analysis. The stone was unable to be identified after 8 attempts per my doctor’s office. My first stone in 2014 was a oxalate stone, and was hard and looked like gravel. I passed my 4th squishy stone yesterday, and upon calling the urologist, they are performing a cystoscopy in the morning. These stones average approximately 6 mm and present more like sciatica pain and/or back pain. I am in NP school, and study a lot, and I thought I had developed a DVT is the only reason I went to ER with 3rd stone. On CT scan a couple of months ago I had two 6 mm stones on right and one stone on left (which size was not mentioned on report). I have passed a total of 4 stones since that I am aware of. The pain is not terribly unbearable, but my urethra hurts temporarily after passing stones. Have you ever encountered a stone that could not be identified? If so, what is your guess on this? The only other significant hx is I had a lap cholecystectomy for sludge in 2000, +ANA, antiphospholipid syndrome, and currently have a rash for 2-3 months (on my neck, upper arm, chin, and cheeks) and have seen two different dermatologists, and the culture was negative for anything. The derm cannot figure it out, and is leaning towards autoimmune in nature. I also see a rheumatologist, and the labs I had drawn last week shows a TSH 5.17, but I continue to lose weight, despite eating a lot. I currently weigh 101 pounds and I am 5’1″.
Thank you!
Brooke
Hi Brookel, In some people urine proteins can congeal to produce so called matrix stones. If studied carefully one often finds tiny amounts of crystals. My suggestion is to have a full evaluation to determine why you made stones and fix what is wrong. When that is done, crystal formation may fall and with it formation of these matrix stones. Regards, Fred Coe
Thank you, Dr. Coe. I am learning a lot from your articles. I have a VUR reflux which was very bad when I was born. After surgery it got better but still have and cause problems. I started with calcium oxalte stones when I turned 29. I also have sponge kidneys. I just had a new 24 hour urine and it now shows high calcium excretion 1,856, high excretion of uric acid 1,856 and high CIT acid excretion 1,856 and my oxalate was still high 1,775 after 2 weeks on a low oxalte diet. The high acid is new. I am overweight and have hypertension controlled on meds, and I am now 50 years old. I have not passed any acid stones. What should I start doing now to keep from making acid stones? Is there anything I can do with my diet to better my urine ph and acid levels? I already eat low protein, working to get it up with non-meat due to low protein and low albumin. I try to meet my calcium numbers to protect against the calcium oxalate stones.
Hi Debi, I am confused. Did you have uric acid stones, too? Your numbers are not correct – urine calcium, citrate, and uric acid are the same and that is just a misreading. Check again and feel free to post the correct numbers. Is your urine pH low? Before doing anything, try to get the numbers in order. Regards, Fred Coe
HI Dr. Coe. I’m a 43 year old male. My Urologist removed an 8mm stone in my ureter and said I was done and not to worry about the 3mm in my other kidney. I later emailed him after doing my own research and asked what kind. He said “8 mm was Uric acid. Lower meat, lower salt, and lemon.”
Well after reading your article I am inclined to think he should have mention Potassium Citrate. Can I just begin taking this or is there anything else I should do…or change doctors?
Also , could 5 alcoholic drinks on many Saturdays and not urinating or drinking much water till Sunday afternoon change my PH enough to cause rapid uric stone formation? Thanks!
Hi WIlliam, if the stone is uric acid the cause is low urine pH. You should have proper testing, and no doubt alkali to raise urine pH. The drinks are not relevant. Potassium citrate is prescribed; you can purchase bulk forms of it, but because some people with uric acid stones have other diseases their blood potassium can rise with use of the supplement. SO you need a supervising physician. Diet alone is not a treatment for uric acid stones. Regards, Fred Coe
Thank you for the quick reply and detailed answer! I am sorry for my late follow up, I didn’t think I would get a quick response.
I have another problem now though, its been a month since the procedure and starting 5 days after the procedure and still now I have flank pain under my rips and stomach.
I had a ultra that showed mild blockage a few days ago, but no stones. I just had a CT scan and am waiting results. What could be wrong? Could this result of the Ureterscopy and lithography? I’m so frustrated.
Hi William, any blockage is cause for concern. The CT is a good approach. Possibly it is a small stone, or perhaps some ureteral damage. In any case, your urologist will need to establish normal drainage to protect your kidney and I am sure she/he will do so. Regards, Fred Coe
Hi Dr. Coe, Thanks again for the reply.
So CT showed nothing. Urologist says I am fine. However I still have the same pain, now going on 7 weeks post procedure. I guess it would be urethral damage from surgery? I am going to get a second opinion now, I’m at a loss at what to do and my urologist is not very helpful. Is it common to have this type of thing post Ureterscopy and lithography?
Hi William, pain is always possible. I would ask about a convenient second opinion. Continued pain can always mean something has gone wrong and needs fixing. You cannot do much yourself. When you get your second opinion be sure and bring the images with you on a CD – not just reports. Regards, Fred Coe
Hi Dr Coe,
I have uric acid stones lodged in my left and right kidneys measuring up to 6mm and 4mm diagnosed with a recent renal ultrasound. I am non symptomatic (no pain). I had a stone passing episode 10 years ago but nothing since. I was prescribed potassium citrate 10 years ago but have become lax in adhering to the prescribed dosage in recent years. I have re-started the proper dosage but my question is, for stones of this size, do you think it is still possible to dissolve them though potassium citrate? Or is potassium citrate largely a preventive measure? Also do you have any opinion on Chanca Piedra for uric kidney stones? Thank you
Hi Ken, Possibly the stones may shrink, if they are pure uric acid, especially. Try to keep up the med, as uric acid stones can grow rapidly. Chanca Piedra is a folk medicine now being hyped for profit. I have not done much research yet, but there are only 13 reputable publications, I read them, and not much. One day I will try to do a real article. For you, potassium alkali is nearly perfect, so why fool around. Regards, Fred Coe
Hi Dr Coe,
My husband had his large bowel removed when 32, due to Ulcerative Colitis. They did the j pouch procedure. So no bag. He dehydrates quickly. He had kidney stone this year and passed but no pathology. Also he now has gout on big toe and heal. Thought might be due to high levels of uric acid caused by removal of large bowel? Do you think gout and renal stone are caused by the same thing?
He is now 57.
Hi Ann, I think it could be. He needs proper evaluation, stone analysis and 24 hour urines etc. Here is a good review. Don’t guess, measure and treat accordingly. Regards, Fred Coe
I’m a uric acid stone former and have struggled to find good information on the subject online. This is absolutely the most informative site I’ve found on uric acid kidney stones. In July of 2017, I had my first stone adventure. I had a 1cm stone in my left kidney that decided to head for the exit. It was a total surprise and excruciatingly painful. I oscillated between thinking I was going to die and wishing it. My urologist was great though and after enduring the surgery (Uretroscopy) and the subsequent stent, life went back to normal for a couple of weeks until I passed a 4mm stone on my right kidney.
I’ve since changed my diet extensively and started exercising. I’ve lost about 15lbs and have dramatically increased my water intake, started eating a LOT more salad, almost eliminated alcohol and red meat and am generally trying to reduce sugary things and meat proteins. Additionally, my family doctor put me on Allopurinol (300mg) daily.
I get a fairly comprehensive annual physical that involves lab work and ultrasound. Based on your article, the relevant results are below.
2015 – Uric Acid (Urate) 344; pH 5.0
2016 – Uric Acid 399; pH 5.0
2017 – Uric Acid 291; pH 5.0 (in December – after dietary changes and daily Allopurinol)
Unfortunately, the recent ultrasound also revealed stones in each kidney measuring 7mm along with some smaller ones. It’s pretty frustrating given the changes I’ve made to my lifestyle in an attempt to avoid recurring stone formation.
Your article makes me question the Allopurinol versus (or in addition to?) potassium citrate or potassium bicarbonate. The drop in my 2017 uric acid results seems to indicate the Allopurinol is doing what is intended (if I understand that correctly), however, my urine pH is still at 5.0. Based on your article, it seems critical for me to adjust my pH.
I’m otherwise healthy (47, male) with no pre-diabetic conditions or other ailments. I have CAT scan scheduled next week to get a better look at the stones and a follow-up with my urologist to discuss the ultrasound and CAT scan results. Would you recommend I take potassium to increase my pH? If so, is there a standard starting dosage and an effective way to monitor it? Note that whatever you recommend I’ll discuss with both my urologist and family physician just to be sure.
Thank you very much for your time.
Hi Scott, You have it right. Allopurinol has almost no role in uric acid stones. The pH of 5 is the whole answer. You need to raise it to 6 using potassium alkali, presuming you have normal kidney function and can therefore take the potassium. A common starting dosage is 40 – 60 mEq daily, and 24 hour retesting is mandatory as the dose may have to go higher still. Once the pH rises above 6 UA stones cease to be possible, and those present may dissolve. But you need comprehensive 24 hour urines to be sure the higher pH does not engender calcium phosphate stones. Regards, Fred Coe
I have been dealing with kidney stones for about 4 years. I was told they were uric acid stones and was prescribes Potassium Citrate (10) but continued to have small stones about once a month. Then I had bladder stones but no changes in mediation was suggested and no information about diet at all. My Ph level went up to 6. Then I changed my diet and within a week I was up to 6.5. BUT my doctor told me today that the Buckwheat, beets and Almonds I have added to my diet are high in oxalates and should be totally avoided. Now I am even more confused. So which is more important, eating a Alkaline diet or a low Oxalate diet or are both important?
Hi Lee, this is in answer to both comments. Uric acid stones are treated with potassium alkali, period. Diet has no relevance. If you formed more uric acid stones then you need more alkali. If you now have calcium oxalate stones, from the high oxalate foods, just stop them and use the alkali supplement. So low oxalate diet and alkaline diet are alike irrelevant for uric acid stones. Regards, Fred Coe
Hi. I enjoy this website. I am wondering if u can tell me how fast does stone dissolve with potassium citrate and allopurinol use. Do u see anything in urine or have symptoms when this is dissolving?
Hi Pat, Slowly, because stones have a low surface to volume ratio. Weeks or months can go by with only modest changes. Larger stones are aggregates of small ones, so as they dissolve you might pass fragments. Note -I never have recommended allopurinol for uric acid stones – ineffective. It is not useful for the stones. Regards, Fred Coe
hi. I’m not sure the email I sent yesterday went through. I am wondering how long it takes or if there is a general measurement of how quickly uric acid stones dissolve with Potassium Citrate and Allopurinol.
I was also wondering if there are symptoms while this dissolving occurs, like different colored urine or blood in urine, cramping, etc?? Thanks for any help.
Hi Pat, It did and I answered you. Regards, Fred Coe
Hi. At what rate do uric acid stones dissolve? Do u have symptoms while they are dissolving?
Hi Pat, I think I did answer already. Regards, Fred Coe
Dear Dr. Coe
I am a 75 yo male MD with a history of having had 3 urinary calculi. My father also had kidney stones. Other than orthopedic problems and osteoarthritis, I have no h/o gout or D.M.
The latest stone measured 1.5 cm and was located in my left kidney’s collecting system. It was lasered earlier this month and found to be composed of 88% uric acid and 10% Ca oxalate monohydrate. Thus, I am a “mixed uric acid /x stone former”, as per your definition.
My previous episode was 12 years ago. The stone at that time measured 1.6 cm and was also located in the collecting system of the left kidney (described as “staghorn”). The stone was composed of 95% Ca oxalate and treated with lithotripsy.
Aside from hydration with H2O, taking potassium citrate 10meq tid, and food rich in potassium, I am totally confused about what other dietary measures, if any, I should take. High calcium vs low calcium, meat protein, yes or no? Check urine pH daily? I gather from your posts that diet has little, if any, impact on uric acid stones.
I am scheduled for an ultrasound in 3 months.
Any advice would be greatly appreciated.
Thank you
Herb Goodheart
hgoodheart@gmail.com
Hi Dr Goodheart, for uric acid stones you are certainly correct; all that matters is urine pH. Frankly, I use 24 hour pH and want a value above 6. I like bid dosing, and usually start at 20 mEq/dose unless there is a problem with renal potassium excretion – unlikely in your situation. I re-measure 24 hour urine after a few weeks of treatment and adjust the dose as I need to. As for the calcium oxalate component, I would look at urine oxalate, calcium, and citrate in the same urine. Perhaps you were hypercalciuric when younger and that has waned – as things do – with age, and urine pH has fallen at the same time. Perhaps you still have high urine calcium or oxalate and if so I would treat those as well. The link is to my favorite article on the urine calcium and oxalate treatment. Warm regards, Fred
Thanks Fred
You’ve given me a plan and I like the bid dosing of K citrate, rather than tid
My very best
Herb
Hello Dr Coe
I have been treated for uric acid stones by means of two operations: URS and PNL
This after a double-sided obstruction and hydronefrosis caused by the stones.
The diet that is recommended to me in the context of metaphylaxis is extremely heavy.
No meat, no fish, no crustaceans, no orange juice
and numerous vegetables.
I understand that your opinion on this is different.
Would it suffice to keep the urine alkaline a using potassium citrate and/or sodium bicarbonate?
And of course drinking lots of water.
Would like your opinion
cordial greeting
Arnold de Brie
Netherlands
Translated with http://www.DeepL.com/Translator
Hi, Diet is almost completely ineffective for uric acid stones compared to alkali. Whereas in theory diet change away from meats to vegetables could raise urine pH, those with uric acid stones have some underlying disorders of pH regulation that make such changes difficult. Potassium alkali works; typically one begins with 10 mEq 3 times a day and increases as judged by 24 hour average urine pH. The goal is above 6. Sodium alkali have the disadvantage of sodium loading with increased blood pressure and increased urine calcium in some people and of course the unlikely event of sodium acid urate crystallization. Because of the power of urine pH to alter uric acid solubility I can see no reason for any other measure. Please discuss this with your physicians as they are in fact responsible for your care. Regards, Fred Coe
Great article ,Thank You for your valuable insights ,,I have been passing uric acid stones for 3 years off an on with the usual symptoms,,,,,my scan indicates flank surgury from the back in,,,,,is this absolutely necessary?I have more bowel surgury coming up and I am abit tense about both…Im going to start to take the Potassium citrate you recommend.Thank You
Hi Barry, I take it you have bowel disease as a cause of uric acid stones, and some stones are large. In some bowel disorders, sodium alkali may be preferable – I do not have enough detail to help here. Regards, Fred Coe
Hello Dr. Coe,
I have suffered from chronic kidney stones for the past 4 years (passing stones on an almost weekly basis). After performing several tests and having several stones analyzed I have just found out that my stones are Ammonium Urate stones. Do you know what the treatment is for prevention?
Thank you!
Christie
Hi Christie, These stones require high urine ammonia, not too low a urine pH and the usual cause is potassium depletion. Bowel disease, high laxative use, vomiting – all these are known causes. The reversal is not hard if the cause can be fixed. Regards, Fred Coe
My urologist thinks allopurinol is even more important than potassium citrate, though he has prescribed both for my uric kidney stones. I’d be interested in your opinion.
Hi Don, Perhaps your physician might want to read this other article – more technical. Total urine uric acid is a very weak determinant of uric acid crystallization as against urine pH, but that may be more apparent in this latter article. Regards, Fred Coe
Hi, your link from the the menu to Struvite Stones does not appear to work or lead anywhere. It should probably be fixed if there is a page it should go to, or perhaps removed if there isn’t one.
Thanks, Alastair, I have not written it and thought I would. I will remove the link. Fred
Hi Dr. Coe,
I previously consulted with your group by sending little stones. The report came back negative for stones, just tissue and blood debris. However, I did have some urine cultures back positive for Streptococcus feacalis and E. coli. I had a few treatments with Nitrofurantoin, Ampiciline, Amoxicillin and finally with Vancomycin (IV). An indium 111 scan just came back negative but my symptoms persist. Since I am a microbiologist and have access to a microscope, I can see the cocci under the microscope mostly invading epithelial cells or some kind of mucoid structures instead of showing in a planktonic form. I would appreciate if you could refer me to an ID specialist or any group working in biofilm treatment who could help me clear the infection. The last one I saw here in Winnipeg, Canada, sent me back to see my family doctor.
Regards,
Adriana Trajtman
Hi Adriana, Very interesting observations. I know of no one in the field you mention. Sorry. Regards, Fred Coe
Hello Dr.,
Great article. I have just had my second kidney stone removal operation in as many months, one from each side. Each stone was 5mm; one obstructive one not – neither of which wanted to leave the kidney on its own! Apparently I have many more lying in wait in my kidneys but at this time they are much smaller and may hopefully pass without notice. I also have been diagnosed with gout. I have dropped the uric acid level in my blood by a complete diet change for the past 6 months. During my most recent stone episode I learned that this diet, as mentioned in your article does not have much if any impact on the urine ph. My urologist is convinced that my stones are uric acid. I see that you mention potassium alkali as an effective ph modifier that might reduce the existing or new formation of stones; what are the sources of this, is there natural vs. pharmaceutical, is daily ingestion required ?
Thank you
Hi Gregg, If the stones are uric acid treatment as outlined in this article is nearly perfect and you should do it. Since stones were removed your physician knows their composition as he/she had them analysed. Potassium citrate is a simple salt of citric acid and the ideal treatment. There is no ‘natural’ vs unnatural source of this material as it is all produced as a pharmaceutical and food additive. It is needed every day – forever, benign, and effective. But, how sure are you of stone composition? Make sure, check records and reports. If not sure, there is confusion, and here is a way to proceed. Regards, Fred Coe
Hi Doctor Coe,
I just had my second PCNL. My stones are 80 percent uric avid and 20 percent calcium oxalate. My urologist wants me to take 2 potassium citrate pills 2 times a day. I also take vasotec and have a tendency toward heartburn. When I take these pills do I have to limit potassium Rich foods? I am worried about the pills with ths vasotec. Can 2 pills a day instead of 4 also be therapeutic? Very anxious about the pills.
Hi Holly, Your physician can check your serum potassium a week after a given dosage regimen. In general your drug will make no difference provided you have normal kidney function. You will need enough to raise your urine pH above 6 and usually that takes 1 – 2 tabs 2 – 3 times a day. As for gastric irritation, take them with food. Potassium rich foods are not a problem even with the pills. But – that word! – your physician knows your kidney function and can retest you so let s/he protect you as you take enough to prevent the stones. Regards, Fred Coe
Hello Dr. Coe,
I found your article very informative and myself have been struggling with recurring Gout and Kidney Stones for several years now that still isnt under control. I am a 40 year old male on daily allopurinol and do not drink alcohol or eat a bad diet, avoid obvious triggers for my Gout yet continue to have regular flare ups typically when I over exert myself working or something to that effect. I also get heartburn daily and have passed atleast 20 stones over the last 2 years. I was convinced it was all related, however my Dr stated my stones are “calcium based” as he put it and completely unrelated and and since all have been 3 to 6mm and passed on their own, not esspecially concerned. I was wondering during if you had any opinions on the above or could point me towards any other articles where I can better educate myself since the multitude of symptoms and attacks is impacting my day to day life. I push through but have a demanding job as many do, and 3 little ones at home with a 4th o. The way. I can’t imagine not being able to keep up with them because of continued pain from gout and stones but my Dr is very dismissive and feels allopurinol is the answer and colchicine when I do get a flare up.
Hi Mark, It appears we have too little information. Are there actual kidney stone analyses or not? Are they recent? Do your 24 hour urine studies show the low pH needed for uric acid stones? What do they show in terms of stone risk? Allopurinol is a treatment for gout but usually not for kidney stones. A good read for you would begin at Chapter One of the kidney stone book, and up through the first few after that. The stones are so numerous, treatment should be easy but you need the data. Regards, Fred Coe
Hi Dr. Coe, I am 63 year old diabetic II, I have had tested and confirmed Uric Acid stones for 5 years. Many lithoscopy procedures. Anyway the 10mEg. x 4 daily is not digesting – coming out of almost entirely undigested. Is there a liquid or easier to digest Potassium Citrate solution. In the meantime, my Urologist is prescribing Sodium Bicarbonate pills 650mg (don’t know dosage yet) – besides my question of easier to digest or liquid alternatives – will Sodium Bicarbonate be helpful in preventing more stones? What dosage might you have seen work before? Thank you Joe
Hi Joe, The wax matrix is what you see, the drug is surely being absorbed. Check the 24 hour urine pH while taking the 4 k citrate, and see if the pH is not 6; if not, go up in dose until it is. Sodium bicarbonate is a sodium load and not as good for your overall health. Regards, Fred Coe
Hello, I used to be from the Chicago area and enjoy your articles. I get flare ups akin to kidney stone pain. I then go though work ups like kub and ct scans. All have shown as Normal. The. I get an ultrasound. One time it showed a 6 mm kidney stone, another time a 3 mm kidney stone. My urologist insists if it is a kidney stone it must show up on a CT scan. I went to a nephrologist and I had high uric and low urine ph and was put on allopurional and potassium citrate. My question is do uric acid stones show up better on ultrasound than ct scans? I keep passing these black spots when I pee, some tiny and others bigger. But it just seems to be chips of a stone and not the whole thing.
Hi Mark, CT scans show uric acid stones very well, and a negative CT is almost certain evidence against stones. So I agree with your urologist. Your nephrologist does no harm raising urine pH just in case you might form a uric acid stone. Black is not likely uric acid, as the crystal adsorbs a red – orange pigment from urine. But I would collect some of the tiny black items and have them analysed at a kidney stone lab. The analysis is fine with even a tiny fragment. Regards, Fred Coe
Hi,
I was wondering if high molybdenum supplements (150-250 mg/day) could cause kidney stones? This is in someone who has had kidney problems before due to her myeloma?
Do you know of any studies I could read up on?
Thank you!!!!
Karen
Hi Karen, I could find no articles on molybdenum and kidney damage, so I presume the kidney injury is from myeloma. Regards, Fred Coe
Dr Coe
I have been reading your newsletters for a year as I had a 4+cm stag horn calculus with multiple points.
I had a friend whom had surgery at your hospital with great success removing the stone through a tube in her back – alas you were not in my network – however I met with a urologist in my network and had the surgery on 10/4
The nephrostomy tube from my back yesterday and I am leaking urine through my back soaking the dressings every two hours- is there a better way to dress this? What is the average leakage time – I know hard to say without performing- just looking for your experience and averages?
And a way to keep the skin on my back
Also I just started on the potassium citrate – I have a Nother large stone in my right kidney hopefully this works I had three standard lithotripsy‘s with no success on the left kidney that this latest surgery thank you for your information just looking for guidance wish I could come see you.
Brian
Hi Brian, I believe I answered this, but my advice was to contact the surgical nurse concerning the leakage. These large stones are worrisome – do you know their composition?? Prevention is a big deal; if they are uric acid, the potassium citrate is fine, if not it may be no good at all. Very large stones are not common, and prevention is crucial for you. Regards, Fred Coe
Hello Dr Coe,
Excellent article, but I have a hard time understanding the information, so please forgive my simple questions.
Can Uric acid stones be dissolved by potassium citrate?or by any other means?
Is low acidic foods one way to prevent these types of stones?
I currently have three, but they have been decreasing in size.
Thanks,
Kevin
Hi Kevin, I guess the article is not so good in that I did not make things properly clear. Yes, uric acid stones can dissolve if urine pH is raised to 6 or higher with potassium citrate. Diet plays no role; too small an effect vs K citrate. Nothing but alkali matters in most cases. Perhaps the only except would be remarkably low urine volume below 1 liter a day should be raised to at least 2 liters per day. Regards, Fred Coe
Dr Coe,
Your article is amazing, but some of the language is above my level of comprehension is all. One more question if that is okay.
Would one have to take potassium citrate in supplement form, or through foods high in potassium?
I know you mentioned that several drinks contain potassium citrate, but those drinks often upset my stomach.
Thanks again Dr Coe!
Kevin
Hi Kevin, Indeed you would need potassium alkali, and food itself is not likely to help. Some drinks contain potassium citrate as you note, but for uric acid stones – can become large and troublesome – potassium citrate is the only correct plan. Regards, Fred Coe
So drinking more water will help increase urine pH and dissolve Uris acid stones?
Hi Suma, No, it will not. All I meant is that extremely low urine volume could perpetuate uric acid stones despite alkali, so urine volume should be in the normal range of about 1.5 liter/day or more. Alkali are needed to raise urine pH in uric acid stone formers. Regards, Fred Coe
Hi Dr Coe,
I posted a reply to your reply too me, but for some reason it did not upload. If you see it please disregard.
I just wanted to know what you meant when you said “Diet plays no role; too small an effect vs K citrate” in your response to me.
And you did a great job in your article, I just have a hard time understanding the language. That is my fault.
Kind Regards,
Kevin
I meant that given alkali to raise urine pH, diet need not change to prevent uric acid stones. Regards, Fred Coe
Dr Coe,
Also, “alkali”and “alkaline” the same thing? If I ate foods that have a high ph (alkaline), would that be enough? or do I have to go and but a alkali supplement?
Sorry for all the questions.
Kind Regards,
Kevin
Hi Kevin, You need to get an alkali supplement. Diet will not suffice. Regards, Fred Coe
Hi Dr Coe,
Thank you for your replies. Very much appreciated. I guess supplements is the only way.
Hi doctor,
Great article. I have been diagnosed with two 7mm stones in right and left bladder. My uric acid levels are 8.7-9.3 (uricase).
The doctors prescribe Febustat 80mg tablets. I did not see and discussion with regards to this form of medication.
Also, do you suggest I start with potassium citrate medicene?
Hi Apoorv, For the uric acid stones, neither allopurinol or Febustat matter; prevention relies on raising urine pH. Febustat would be to prevent gout by lowering serum uric acid. I should add that medication to the article, if only to say there what I have just said here. Thanks for pointing out the missing material. Regards, Fred Coe
Hello Dr,
Is there a way to know what kind of stones I may have? My family doctor said the only way is to wait until it passes and obtain it for analysis. There must be another way!?
Thanks
Kevin
Hi Kevin, The only way is stone analysis – of the stone. Using CT radiographic density one can tell uric acid from calcium stones, but that is indirect. For calcium stones, the common ones, calcium oxalate and calcium phosphate cannot be distinguished. Regards, Fred Coe
A wonderful and considered overview! I am presently eating a ketogenic diet and have high uric acid. I do not have symptoms of gout, but I do have orange sediment in my urine. My only concern with potassium bicarbonate is the alkalizing effect on stomach acid. I value my ability to diet fat and meat well, and am concerned taking bicarbonates will negatively impact digestion, even if spaced hours from a meal. What is your experience in your practice with this? Thanks so much for providing this article to users of the Internet, it is a tremendous resource! You are a good man.
Should read “digest fat and meat” not diet.
Hi Benjamin, The orange gravel is certainly uric acid. If you take potassium citrate tablets, they will have no effects on the stomach. Likewise for sodium citrate – assuming you can tolerate the extra sodium. Regards, Fred Coe
Thanks Dr. Coe. I should have clarified that I had a bias towards potassium bicarbonate over citrate as there seem to be innumerable general health and performance benefits to bicarbonate itself independent of potassium. Have any of your px had stomach issues from potassium bicarb?
Hi Benjamin, I do not use it myself for my patients. But sodium bicarbonate surely has its problems. Perhaps a liquid formulation might help – I cannot tell if you tried it. Regards, Fred Coe
Thank you Doc!
Hi Dr. Coe,
Having read your entire Guide Book book and all of the comments, the information you provide is by far the best I have found anywhere, and very much appreciated. I am a 62 year old male with no known issues other than what is stated below. Last week I finally had a 12mm stone removed via laser hopefully ending this 19 day nightmare involving 2 separate procedures.
The first procedure during my second ER visit placed the first stent and the second one which dusted the stone and placed the second stent 10 days later. This current stone was initially discovered 12 years ago during an unrelated MRI. I was told at the time it was not an issue and that I would know when it was time to deal with it. That time has apparently come with prevention now being my top priority.
My follow up is scheduled in two days which will be one week from the dusting procedure and 4 days after removing the “string” stent at home. My Dr told me upon release from the hospital that at the first follow up he will start a 24 hour urine test and I assume inform me about the stone’s makeup to device a prevention plan.
I would like provide you with a brief history as we await my test results.
20 years ago – Hospitalized while working out of town eventually passing a stone within 2 days of admission. This was my first time experiencing a stone. I do not recall the size but do remember being told it was uric and obviously passable.
16 years ago – Emergency surgery for a perforated colon which resulted in a 2 foot section being removed with a colostomy bag placed. Fortunately the bag was removed and the colon was reattached in a second surgery with no complications since.
5 years ago – Heart attack (MI) where 2 stents were placed, so far so good.
3 years ago – blood tests showed very high levels of potassium but no action by my Dr.
Over the past 10 years knowing the stone was there, I have had numerous bouts of moderate pain with lots of blood in my urine when it flared up but nothing severe or unbearable, so no action was taken.
Having regular blood work done for years, I’ve been taking Atorvastatin for elevated cholesterol, Flomax for enlarged prostate and a baby aspirin daily.
Without know any numbers or test results yet, do you see any correlation or potential correlations from any of this history?
Kindest Regards,
James
Hi James, You have had stone production years ago and a present stone found 10 – 12 years ago, so you do not seem to be actively forming new stones. The stone itself could have caused the pain and bleeding attacks, unless there is reason to suspect otherwise. Of most importance, gather some of the dust – or be sure your surgeon did – to get an analysis of what the stone was made of. The 24 hour testing will be far more useful with that knowledge. The very high potassium seems a fleeting thing as if constant you would long ago have had extensive testing for it. THe usual reason for a sporadic very high value is hemolysis of the sample during the blood draw. If you have generally high serum potassium that is a special kind of problem your physicians need to correct. The cardiovascular disease has no obvious link to stone production, but stone formers are at higher than average risk for such disease. Regards, Fred Coe
Thank you for the speedy reply,
I’m looking forward to the results of the stone analysis tomorrow at my first follow up visit as he did collect samples during the procedure. I will reply with my stone analysis and 24 hour urine test results when available. It’s good to know that you suspect no new active stone formation has occurred based on the limited information I’ve provided.
James
I feel very fortunate to have drawn by chance Dr Geoffrey Habermacher of UAB locally as my urologist on my second ER visit. He is not only an MD but also has a Ph.D in Cell and Molecular Biology and is an amazing young man that spent 17 years in college perfecting his craft. At my follow up he informed me my stone was 70% Calcium Oxalate Monohydrate, but I failed to ask about the remaining 30% which I will do in the near future. Now we wait for the results of the 24 hour urine test.
Hi Dr Coe, firstly thank you for your expertise and research on Kidney Stones, I appreciate it. Just recently had a kidney stone episode and after analysis, it was determined it was a Uric Acid Stone. I have had chronic nausea for about two years now, and after passing this stone, I’m feeling better. Two questions: Could the stone have caused nausea in that time and any advice on not forming other ones in the future? Thanks
Hi Jim, Stones can cause nausea when they obstruct. As for the uric acid stone the article you have written on has the main message: caused by acid urine pH prevented absolutely by potassium citrate to raise urine pH above 6. No one with uric acid stones should be without alkali, and no one taking alkali should form another uric acid stone if the dose is right and the urine volume in a reasonable 2 liter range. Regards, Fred Coe
Dr come, I formed a Uric acid stone and have been trying to lower Oxalates also, but should I be more concerned with increasing my ph? My primary care doctor recommended that I start an alkaline diet to heal my esophagus bc of acid reflux and it seems that I will also be helping prevent Uric acid stones, is this correct? So should I not be as concerned about Oxalates? Anxiously waiting your reply , Sandy
So Sorry about the auto correct on your name.
Hi Sandy, As you can see from the article, oxalate would have no place in uric acid stones. Alkaline diet is not a bad idea but not likely to be sufficient for prevention unless your 24 hour urine pH rises above 6. Low pH is all there is to uric acid stones, and raising urine pH all you need to do. There is no reason to bother yourself about oxalate at all unless your stones contain oxalate. Some uric acid stones contain calcium oxalate, and if so that part of the problem needs its own treatment, so be sure about the analysis. Regards, Fred Coe
Yes, Dr Coe, my stone was 80% Uric acid and 20% calcium Oxalate. I have a stone in the left kidney but don’t know what kind it is. After the 24 hr. Urine test , my ph was low, urine calcium was high, low citrate, high sodium and blood test showed low D. So I’ve been trying address each issue. But should I be more concerned with increasing the ph than lowering oxalates? I m a bit nervous about how to manage this, and the reflux too. Stress is not helping me.
Hi Sandy, The urine pH is highest priority as the bulk of the stone is uric acid, so you need potassium citrate 10 mEq maybe 2 twice a day or more, use 24 hour urines to check if you are high enough. Citrate may rise with this medication. Your physician is in charge of this. The high urine calcium accounts for the calcium part of the stone, and the high urine sodium reflects high diet sodium. If you reduce your diet sodium to 2000 mg before your next 24 hour urine the urine calcium may be lower. Urine calcium parallels diet sodium. Oxalate has no priority – your urine level is not high. Your physician may want you to use OTC vitamin D, a good idea and not a stone risk. Regards, Fred Coe
Thank you so much Dr. Coe. I want to get started on this. I’m new to mEq’s…does the 10 mEq equate to 750 mg? I want to purchase the potassium citrate but only find it in mg. I appreciate your help, greatly.
Hi Sandy, 10 mEq is 1080 mg of potassium citrate. Regards, Fred
Hi Dr Coe,
2 days back I was diagnosed with a 8mm uric acid stone in my right kidney. My urologist has asked me to take a medication called ‘Cystone Himalaya’. I would like to know, is an 8mm stone passable naturally. Are there any medication that can dissolve the stone of this size to make it smaller? I am very worried. My next appointment is in 6 months time.
Hi Santhni, A one year trial of the stuff showed no changes in urine chemistry that would tend to reduce stone formation, and no change in the numbers and size of stones in the kidneys. So, no. If your stone really is uric acid, and your physician can tell from the CT density, potassium citrate will dissolve it. I would suggest you pursue this less glamorous but scientifically validated approach to preventing more stones and dissolving this one. Regards, Fred Coe
What does this mean:
“Sometimes I have urine potassium citrate with a low dose of thiazide diuretic – the latter to foster renal potassium loss.”
Does it mean it’s good to give thiazide diuretic with potassium citrate to raise pH levels in urine? I asked this cuz we are having trouble raising my pH level in urine. I’m on 20 meq of potassium citrate a day. my potassium blood serum level is at the very top of normal so I cannot take any more potassium citrate higher than that of 20 meq. My doctor has not offered any other way to raise pH in my urine. I am following a low purine diet. Still my urine pH remains at 5.3 or lower. Do you have any suggestions?
Dear Mary, How lovely of you to read so carefully. Of course I left a silliness in my prose. I should have said sometimes I use potassium citrate with a low dose of a thiazide diuretic… The purpose is to provide a way to foster potassium excretion by the kidneys so the dose of potassium citrate can be increased. I have just edited the remark: “Sometimes I use a low dose of thiazide diuretic along with potassium citrate – the diuretic to foster renal potassium loss. This can enable patients to get more alkali without risk of raising serum potassium.” Speak with your physician about more potassium citrate, and if serum potassium rises, use the thiazide (I like chlorthalidone 12.5 mg) to keep it lower. Regards, and thanks, Fred
Dr. KO, thank you for being such a generous doctor answering questions. You answer more questions than my regular doctor. My question is on diet for uric acid Stone formers. We are told to follow an alkaline diet and a low purine diet. The problem is that many of the alkaline foods are very high in purines. So these two diets seem to cancel each other out. For someone like me who has normal uric acid in their blood, high uric acid in their 24-hour urine, and a pH in my urine of 5.3, if I had to choose which diet to follow that would be most beneficial would I choose the alkaline diet or the low purine diet? I am on allopurinol and potassium citrate at 20 meq a day. My blood serum potassium is high end of normal so I cannot increase my potassium citrate. So which diet do you think would be better for me to follow? Again thank you so much for how much you care about everyone.
Hi Mary, Diet will not prevent uric acid stones very well, so you will need alkali. Low purine diet has very limited effect in that with your low urine pH even modest amounts of total UA will lead to crystals. Your blood potassium should not be high with your dose of K citrate unless you have kidney disease, are diabetic, or are getting blood drawn soon after taking the medication. If you have a reason for the elevated blood potassium you might mention to your physician adding a low dose of chlorthalidone or indapamide, these diuretics foster potassium loss and permit full dosing which is the only thing that will prevent your stones reliably. Regards, Fred Coe
I recently got results of an ultrasound showing 2 bladder stones, one of which is 27 mm, and one kidney stone 4mm. Does what you say in your articles on kidney stones apply to bladder stones? I’ve had sometimes severe pain on urination for several months and thought it was due possibly to prostate enlargement and tried to make dietary changes to address that, but the pain got too much and hence my trip to a urologist. I do not know what the compostion of the stones are. I have been drinking a lot of lemon juice, watermelon for citrate which sometimes seems to help; and using potassium chloride (NuSalt) for potassium. Is that form of potassium going to make a difference? I had been eating a lot of meat for years (Paleo diet… uric acid overload???) and never noticed how much I peed volume wise, so maybe I wasn’t drinking enough water. Is 27 mm something that can be broken up with laser or ultrasound or lithotripsy? Also, they scanned the bladder and said I was not retaining unusual amounts of urine. The ultrasound showed my bladder wall was 11 mm of the posterior bladder wall (what is normal?) and “no evidence of hydronephrosis bilaterally” I would like to avoid any kind of intrusive procedures if possible. Any comments would be greatly appreciated. I don’thave results of urinalysis yet, my next appointment is not for a couple weeks. Your work on this subject is amazing and has been very helpful in me understanding all this better. Thanks so much!
Hi Robert, bladder stones almost always arise because of outflow obstruction, so I would ask your urologist to be sure. Simple crystallizations simply pass by without retention in the bladder. The kidney stone is another matter. I would be fully evaluated as to cause of the stones, including appropriate 24 hour urine testing and serums. Uric acid is indeed a plausible possibility as you note by your choice of article. Prevention without known cause rarely works, so get testing. If there is any stone removed have it analysed. Regards, Fred Coe
Thanks for all you are doing with this site. Regarding bladder stones, it seems that most internet sites say they cannot be dissolved with a few saying they can be dissolved but it will take too long. At least one site says that bladder stones are most commonly uric acid stones. If this is true, why wouldn’t urine ph of 6.5 dissolve them? Thank you.
Hi Vincent, if they are uric acid, they can dissolve and it can take a long time. But most important, new ones can be prevented by raising usine pH. If urine pH is low enough for bladder uric acid stones, it is low enough for kidney stones of the same crystal, so raising pH is necessary anyway. Regards, Fred Coe
Hello Doctor, recently released a kidney atone the pathology test resulted Uric Acid + Whewellita (Calcium Oxalate) what is the best advise to prevent these kind of mixed stones? I appreciate your help!
Hi Jose, Uric acid stones are prevented as in the article, using alkali to raise urine pH. The calcium part may reflect a second problem and the 24 hour urines you need for the uric acid stone – to be sure of the treatment effect – will help find that second problem. Regards, Fred Coe
Hello good doctor. Would you agree or disagree that potassium taken as citrate is better had with a meal, to simulate how it would be found in nature in a complex food matrix? Conversely, would you comment please on potassium as bicarbonate being taken preferably away from food, with water, to ensure stomach acidity is not diminished from the effect of the bicarbonate? Any concern that chronic use of supplemental alkali in the form of bicarbonate impairs stomach acidity in the long run?
Hi Ben, Potassium citrate would indeed be in fruits and veggies, and taking it with foods is not at all a bad idea. No data I know of concerning better or worse outcomes. Potassium bicarbonate is an alkali – bicarbonate – and will be absorbed fasting or with food. But it may indeed raise gastric fluid pH, so I would take it fasting. Long term bicarbonate is not known to affect the stomach. Regards, Fred Coe
Dr Coe, I’m your typical uric acid stone former — 79, overweight, low fluid intake, recent 24-hour pH just under 5.5, 17-year history of stones, 4 mm fragment tested last week as 100% uric acid. I have two large non-obstructive stones (lower and upper) in left kidney based on CT exam 5 months ago. Specific size was shown only for the lower stone — 12mm X 8 mm. Have started taking baking soda and find that small amounts are keeping my pH between 6.5 – 8.0. My doctor suggests stay away from pH over 7.0 because it could create calcium stones. Maybe so but wouldn’t that take quite some time ? Meanwhile I have the more pressing problem of trying to treat the large uric acid stones. I would like to be as aggressive as possible in increasing pH. I have not taken any magnesium citrate yet. The sodium bicarbonate seems to be handling it nicely at well under 1 tsp daily (surprising to me based on things I’ve read). A question I have is how fast can these stones dissolve (weeks, months?) if I keep the pH higher at whatever level is reasonable. A hope I have is that the stones will gradually erode on their outer circumference. My fear, of course, is that they might shatter into smaller stones that are still large enough to cause a kidney stone attack. Perhaps unrelated, I had gross hematuria and clotting for four months.Cystoscopy, cytology study, etc did not identify source. There has been no pain in left kidney but doctor says that nonetheless the bleeding may have originated there or from my 99 gram BPH. I would really appreciate hearing your thoughts, particularly on aggressively people raising urine pH for a short time and if there’s some compelling reason to switch to potassium citrate when baking soda is working. Thanks very much.
Hi Ted, Raising urine pH is how to stop uric acid stones. Your physician is right in that too high a urine pH can promote calcium phosphate overgrowth on uric acid. Aim for 6.5 or so on a 24 hour average. I do not like all sodium bicarbonate. How about some potassium citrate, some lemonades that have potassium citrate in them, more fruits and veggies, and use the bicarbonate as an add in? As for the bleeding, we have to take your physicians opinion – I am far away and she/he is right there. Regards, Fred Coe
Thank you Dr Coe. I don’t want to just stop uric acid stones, a most worthy goal. I want to make my big >1 cm uric acid stones vanish. Are we talking about the same thing? Will an average 6,5 pH do the trick? Realistic time frame for this to take place and, importantly, are they likely to wear down gradually or just break into pieces one day?
Hi Ted, Yes – a pH of 6.5 or so is fine. The stones are often aggregates of smaller stones, so as they dissolve you may be passing some small stones. Dissolution is not very fast because the surface to volume ratio of stones is low. You are doing the right thing. Regards, Fred Coe
Dr Coe:
Correction…in my post a few minutes ago the “magnesium citrate” reference was supposed to read “potassium citrate.” Thank you.