 Of all the knowledge on this site, a tiny nugget of three well established facts has explosive power for patients and physicians. Put to actual use they let you prevent idiopathic calcium stones and preserve bone mineral.
Of all the knowledge on this site, a tiny nugget of three well established facts has explosive power for patients and physicians. Put to actual use they let you prevent idiopathic calcium stones and preserve bone mineral.
If you do not want to read the article, I have made a VIDEO to tell you the story in about 13 minutes (available below). On my iphone the video opens well and looks better horizontal. Please let me know if it does not work well for you.
I have not been shy nor secretive. Article after article speak about the three, but always in context so other facts can distract one, as can superb but unmagical paintings from a few masterpieces hung on the same wall. I know some patients, some physicians, have fully grasped the crucial importance of the three, and put them to use. From the many comments I read weekly, I know many have not. So I am taken with a passion to redress matters.
Les Demoiselles d’Avignon, Picasso, 1907, Hangs in MOMA, NY. It is my choice of masterpiece. I deliberately cropped into the center as I love the abstraction and also want metaphor for limiting attention to a few essentials in the midst of a richness of details.
Because Spring has come to cold Chicago, I used my picture from some Springs ago. Partly it is the green ivy, partly reminiscence.
This is About Idiopathic Calcium Stone Formers
Cystinuria, uric acid stones, struvite stones – all these are to one side. Calcium stones from systemic diseases likewise. Physicians detect these and manage them. My focus is on the vast mainline of patients who form calcium stones without systemic disease.
The Three Essential Facts
Diet Sodium Controls Urine Calcium
If I could I would paint this on the sky, draw it on sidewalks across the world. It has been demonstrated by scientists for at least 70 years,
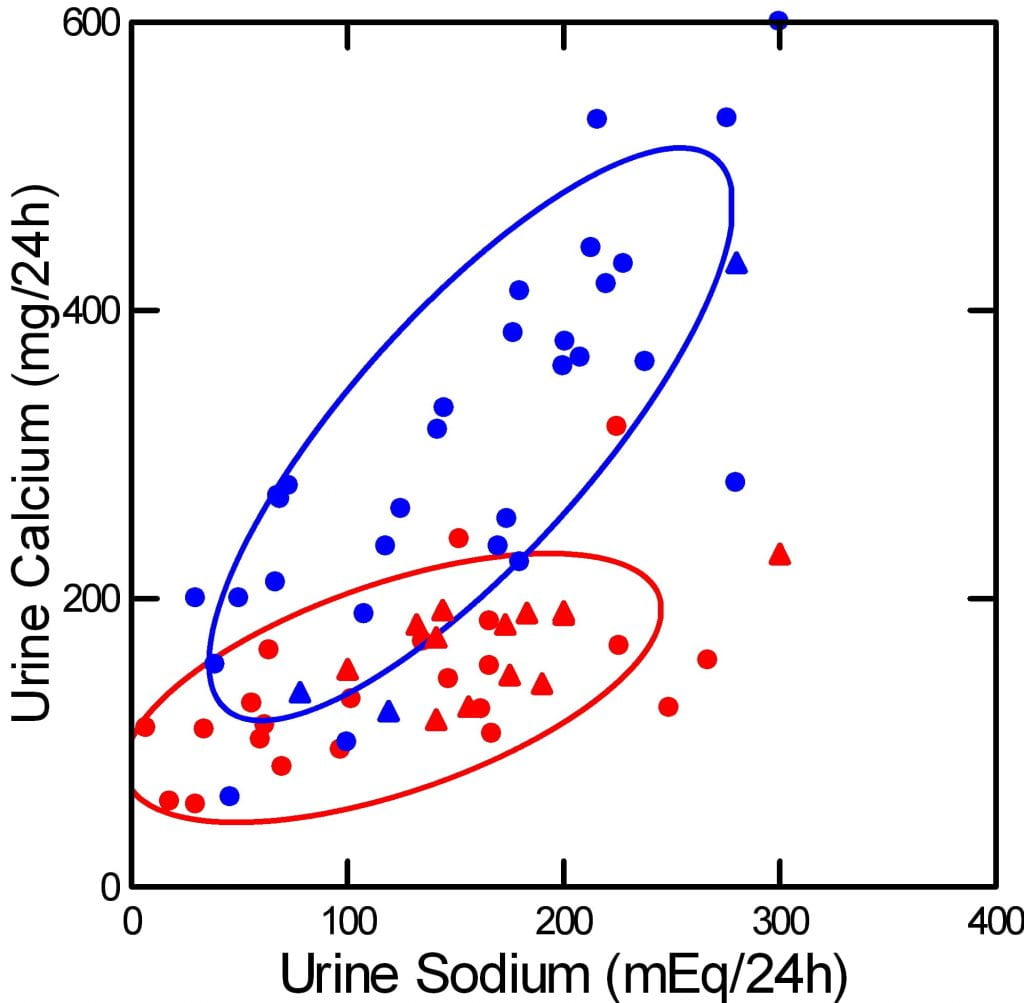
and how it happens is reasonably well known. I made this picture using published data from many sources, and I placed the original data and references within this site. The blue points are from calcium stone formers, the red from normal people.
Urine sodium is diet sodium, because we absorb almost all the sodium we eat, and excrete it in the urine. Urine calcium is not diet calcium. We absorb only 18 – 35% of the calcium we eat, and that absorption is regulated by the intestines, and by hormones like vitamin D.
Stone formers absorb a higher percentage than normals, but that is not why their urine calcium is higher. It is higher because they have idiopathic hypercalciuria and their kidneys do not retain calcium as well. At the heart of idiopathic hypercalciuria is what this graph shows – urine calcium is abnormally sensitive to diet sodium. As you lower diet sodium from the average US value of 150 – 200 mEq ( 3500 – 4600 mg) to the present ideal diet sodium of 65 mEq (1500 mg), their urine calcium (blue) falls into the normal range.
Not rarely my own patients seem disappointed when I begin their treatment with lower diet sodium. It seems so mundane, so like the common nostrum that we all eat too much salt. Many have had multiple 24 hour urine tests, and I make a crude pencil graph of urine calcium vs. urine sodium and show them their own behavior. That works, sometimes. Otherwise, they agree to so alter their food lives, but – I sense this – wonder at coming all the way to a professor for a dull seeming advice. They do not sense the power sodium has, even if I show them this graph – or their own.
Diet Calcium Controls Urine Oxalate

I made this messy but remarkable graph from work other people have done and put the name of the main author below their dots. These were experiments with variations of diet calcium, on the horizontal axis, measurements of urine oxalate on the vertical axis and diet oxalate as the size of the symbols. The smallest symbol means 50 mg/day of oxalate, the largest means 200 mg/d, the middle size is 100. In the main article using this I placed links to the original data.
The data scatter but above 1,000 mg of diet calcium all four authors found only modest urine oxalate, 35 mg/d or less as mean values. Average US calcium intake is about 500 mg/d or less, which permits a much higher swing in urine oxalate.
People with idiopathic hypercalciuria, the reason for high urine calcium in idiopathic calcium stone formers, absorb diet calcium more efficiently than normal, so a higher diet calcium supply will raise urine calcium and stone risk.
But, low diet sodium will offset this, improve kidney calcium conservation, so urine calcium can stay low even though diet calcium is high enough to lower urine oxalate.
This is part of the magic and the peril. You must lower diet sodium first and show it is low by another 24 hour urine. Then you can raise diet calcium to block diet oxalate. If you do it right, and keep the diet sodium low, urine calcium will rise little if at all with a higher diet calcium.
Diet Sodium and Calcium Control Bone Mineral
Only one trial proves this, and only in one kind of person – perimenopausal women. We could use more trials. But this one was so perfectly done, and so dramatic, we can for the moment use it as out guide.
Each woman ate each of four diets, high and low 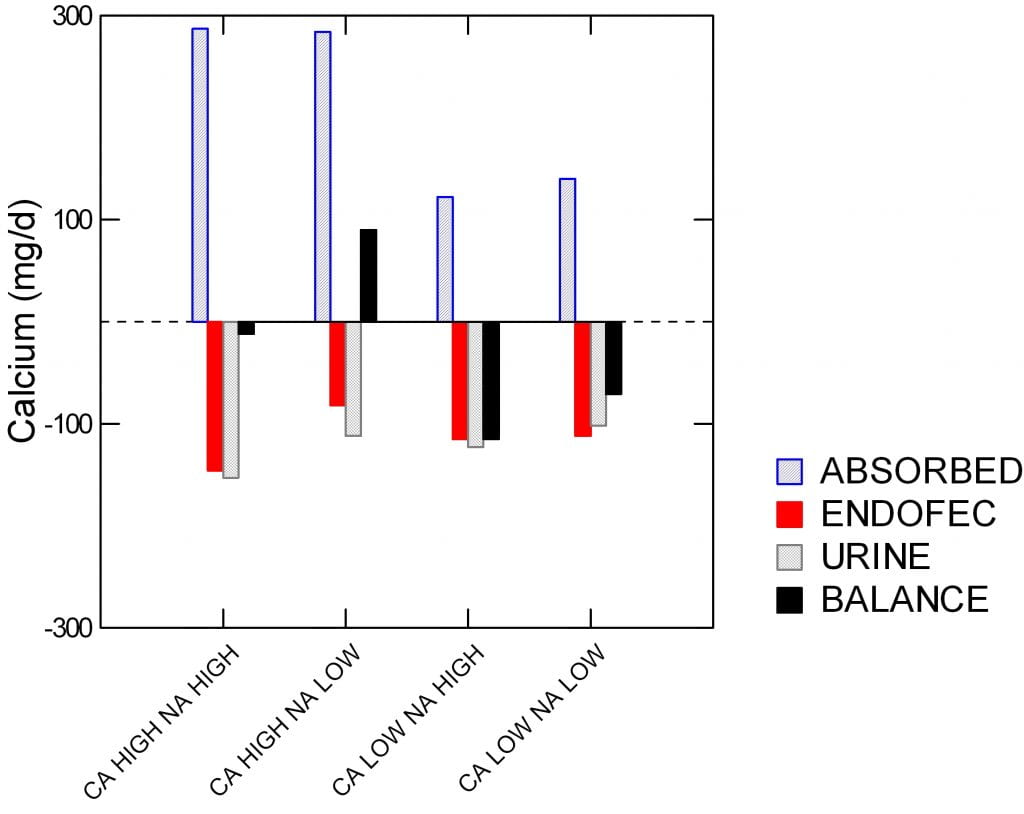 sodium, high and low calcium, and in a random round robin fashion. Specifically, the sodium levels were 1600 and 4400 mg/day, and low and high calcium (518 and 1284 mg/day. On each diet, each woman participated in a full balance study so bone mineral uptake or loss could be quantitated.
sodium, high and low calcium, and in a random round robin fashion. Specifically, the sodium levels were 1600 and 4400 mg/day, and low and high calcium (518 and 1284 mg/day. On each diet, each woman participated in a full balance study so bone mineral uptake or loss could be quantitated.
The four diets are on the horizontal axis. Calcium balance of bone is the black bars scaled on the vertical axis in mg/day, and it can be negative – bones are losing – or positive – bones are gaining calcium.
Absorption is plotted upward, meaning more for bone. Urine and intestinal secretory (‘endofac’) losses downward meaning potential losses for bone,
Balance was positive only with the high calcium + low sodium diet.
The amount of calcium absorbed was higher on the two high calcium diets, of course, and the urine calcium was lower on the low than on the high sodium diets.
As I have already said, the odd term ‘endofec’ means the amount of calcium secreted from blood into the stool by the duodenum, pancreas, and small intestines. This was measured using stable isotopes. If you look close, it was a fall in urine calcium and calcium secretion, both, that created the bone mineral gain from high calcium low sodium diet vs. the high calcium high sodium diet.
Also look close at the urine calcium. The high calcium low sodium diet gave the very same urine calcium as the low calcium high sodium diet. In other words, the women could raise their diet calcium from 500 to nearly 1300 mg/day and yet by lowering diet sodium to 1600 mg/day keep urine calcium unchanged.
The Magic Works for Stones
This is the one trial of the magic formula. Low diet sodium to keep the calcium in the body and thence the bones, high diet calcium to keep oxalate out of the body and thence the urine. It works for bones. Does it work for stones?
Of course, why else would I put it here, and many other places on this site.
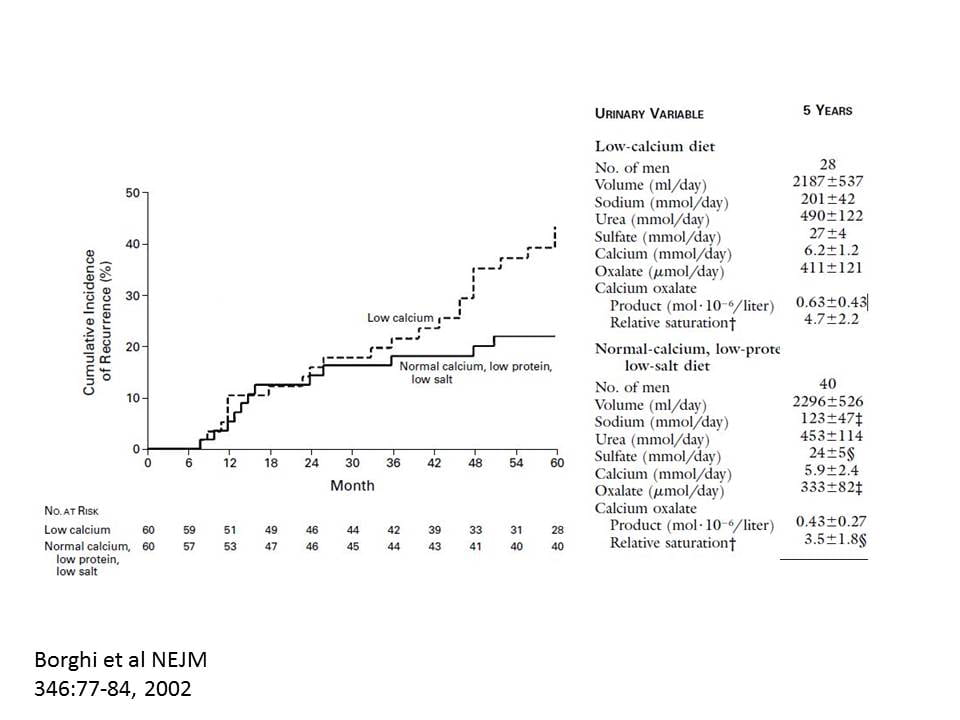
I made the graph very large so your could see the printing in the overlay. The patients were men forming calcium oxalate stones whose urine calcium exceeded 300 mg/d. Low calcium diet was 400 the high calcium 1200 mg/day. The low sodium diet was aimed at 1150 mg, the high at the usual level of about 4000 mg/day.
After five years, stones were fewer in the high calcium reduced sodium group – highly significant statistically.
The why of less stones is exactly what my prior graphs predict.
Of course urine sodium was lower in the low sodium diet group (2,800 vs. 4,600 mg/d, low vs. high sodium, respectively).
Urine calcium of the low and high calcium groups was virtually identical (248 vs. 236 mg/d, low vs. high diet calcium, respectively). Just like for the women in the bone study, one could triple diet calcium yet keep urine calcium the same by lowering diet sodium.
Are you not amazed by this? In two studies one can raise diet calcium three fold and urine calcium does not increase if you also lower diet sodium. Look at the power diet sodium has.
How about oxalate?
Both groups were told to avoid high oxalate foods – walnuts, spinach, rhubarb, parsley and chocolate. The high calcium diet lowered urine oxalate (333 vs. 411 umol of oxalate/d, high vs. low diet calcium, respectively). Supersaturation for calcium oxalate, the proven driver of stone risk, was 3.5 in the high calcium and 4.5 in the low calcium group.
Think about how the threefold magic formula worked. Low sodium diet permitted high diet calcium. The high calcium lowered the oxalate but could not raise urine calcium because sodium was so low.
How to Use the Three Facts
These are magical facts, but they must be used in the right order. It is exactly like casting a magic spell.
Lower Diet Sodium First
Make the change and then be sure you did it by getting a new 24 hour urine. Without the urine test you will never know if you succeeded. Ask yourself if what you did during the collection was like the usual for you and also ask if you really mean to keep the diet sodium as low as during the test. If you get tired of the low diet sodium, and urine sodium rises, all is lost.
Raise Diet Calcium Next
Once you know your diet sodium is low, raise the diet calcium and test again. Is diet sodium (urine sodium) still low? If so, is urine calcium low enough? Low enough is about 200 mg/d of calcium or less.
If so, you are done. If not, you need to keep changing diet sodium and calcium until you get there – high diet calcium, below 200 mg urine calcium.
Some people cannot make do with only diet. Their urine calcium remains too high. For them, we add thiazide to the diet, usually in a very low dose. But for most, this will do. You must keep the low diet sodium, so the thiazide works well at a low dose, and to avoid potassium loss.
Now, Consider Diet Oxalate
With high diet calcium in place, is urine oxalate high enough to raise risk of stones – above 25 – 30 mg/d. If so, it is time to get rid of the highest food oxalate sources. Not all food oxalate, but foods on the high end. I listed some just above. My site has the main ones on a graph. Work from the top down.
Diet oxalate is the last thing to worry about, never the first. One wants to remove what high diet calcium has not removed.
Of course, repeat 24 hour urines are the only way to know if success or failure has attended your efforts.
If You Have Bone Disease
If your bone mineral is deficient, these diet changes are good but you need a physician to be sure they are enough. You may also need medication. Do not rely on just diet. Repeat bone mineral measurements are essential. Be sure your physician is satisfied with your bone health.
If you do Not Have Bone Disease
You may not have looked. Get a bone mineral density. If it is normal, get another some years later. The diet is fine for you unless bone mineral declines. If it does decline your physician needs to manage things. The diet is still advisable, but may not be enough.
There is More but Focus Here, on the Big Three
Diet potassium and protein matter, the former from from fruits and veggies. Diet refined sugars matter, they raise urine calcium. Diet protein matters, too much raises urine calcium. The kidney stone diet accounts for all of these.
Fluids matter. Urine volume should be above 2 liters/d, the point at which stone risk has been reduced. But fluids are never enough.
But the three way magic spell predominates over all else: – lower diet sodium, then raise diet calcium, then consider diet oxalate.
Keep your mind on diet sodium and calcium first, and be sure they are set properly. Then go on, if you must, into the thicket and brambles of oxalate lists. Then control unhealthy sugars, excess protein, and get adequate diet potassium. They matter, I always attend to everything I can.
But always, I urge, stay on the main road. Perform the magic spell and see how far you can get.


Another great article…thanks! No need to post this on your site…and my apologies for pointing out an error, but given the importance of the message regarding diet, I feel it important to let you know that in paragraph 3/sentence 4 of Diet Sodium Controls Urine Calcium, I believe you meant to write “As you lower diet sodium…”. Thanks.
Hi Steve, I so much appreciate your help in this. Changes are made! Fred
Thanks so much for this illuminating piece. You asked about video vs written word: I am partially deaf (esp in speech frequencies) so have a problem understanding spoken words. For me the written word is essential. It also enables going back and rereading a sentence to make sure you got the meaning. Videos would not work well for me. Thanks again for the time and effort you put into helping stone formers find their way!
Thanks for the video – makes this information easy to understand!
Thank you for the article and video – really helps to explain the link between sodium/calcium and kidney stones.
Loved the video. It helped so much. My urine calcium increased to 212 on my last 24 hour test. I see my doctor in 2 weeks but I feel more knowledgeable about talking to her about about it and what I can do to bring it down with diet before medication. Thank you so much for the video.
Thank you SO MUCH, Dr. Coe! You and Jill have enabled me to make so many positive changes to my diet, and feel like I have more control over these stones. Thank you again!
Amy
Your video was so helpful! Thank you very much!
This was a very helpful article and the video is definitely a bonus. I’ve definitely been underestimating the impact of sodium!
Interesting article. I don’t think I realized (after a year on the diet) that the goal is first to lower your sodium, then to raise your calcium if needed, then to worry about oxalates. I went overboard on oxalate tracking right away, because those seemed like the “bad guys” I had to get rid of. Thanks for continuing to educate yourself and us!
This was incredibly helpful. I read the article first but couldn’t grasp what the graphs were saying. When you explained it on the video with the cursor showing where to look, it made much more sense.
The 3 step magic is very easy to understand and has caused me to feel less panicked than I was when I started researching diet for stone formers just yesterday!
Dr Coe, thank you so much for this! Light bulbs went off as you explained the slides. We need more of this from you in all your spare time hahahaha. I think women with osteoporosis should be eating low salt diets as well lucky me, I have both 😀
Hi Barb, Indeed. Low sodium does improve bone mineral balance but only if diet calcium is high enough – over 1000 mg/d. Fred
Can you get too much diet potassium if you are also taking potassium citrate?
Hi Paul, no unless your physician has found some problem with potassium handling – common reasons are diabetes, kidney disease, and specific drug categories. Be sure what she/he says, but in general no. Fred
Thank you so very much for this article and the video! It makes so much more sense now!
You are amazing Dr. Coe!
Thank you so much. I really enjoyed the video.
It made the article more understandable for me.
Thank you so much, Dr. Coe!!! This article finally makes it really clear to me why I need to keep my sodium levels under control!! I have to confess that I was getting a little sloppy with this lately, but your article was like a kind teacher rapping my knuckles with a ruler to get my attention!! Please keep the articles coming!! They help many of us “stoners”!!
Hi Mary Ann, I am glad it got you on board! Best, Fred
Thank you so much Dr. Coe. I’m only 50 and have stones and OP. Both are “silent” I haven’t passed a stone yet or had a fracture. I’m trying to educate myself, make diet changes and work with my doctors. You and Jill Harris provide THE BEST information for me. I can not thank you enough. Thank you too for doing the video- so easy to understand.
Thank you for the material and especially the video Dr.Coe It helps to have visual and auditory information so I learn and retain what to do to help treat my kidney stone issues but also why each piece is important. I appreciate you taking the additional time to create the video to support the article. I will refer back to this presentation myself and share it with my local doctor.
Thank you, Dr. Coe for your wonderful video explaining your article and research. I am very grateful for your hard work, research and dedication to educating others. You are a blessing.
Thanks so much for your work and dedication to helping us stone makers. I have had 10 operations over 4 years and they looked into and couldn’t provide me with a reason for it. I have studied your pages and will adapt my life to stop the recurrence of stones. too much pain and money wasted. thank you thank you thank you. I also follow Jill Harris’ program and thank the stars both yo and her have come into my life.
I both read and watched your video and I must say Dr. Coe, the video enabled me to understand SO much more! Thank you for taking the time to make it!!
Ann P
Great article Dr. Coe, nice to virtually meet you. I find the best part was you telling us exactly what order to do things in. This is extremely helpful to me. The graphs are also quite handy in making the information easy to understand. I’ve enjoyed previous articles of yours, but I feel this one was the most east to understand and at the end I had the most clear direction. Thank you for all of your help.
Hello Dr Coe, thank you for putting this into perspective. The prioritization of lowering sodium, increasing calcium before other aspects of the diet is so helpful. Sometimes it’s hard to make a decision with competing diet elements. Thank you, Anne
Hello Dr. Coe, thank you for this clarification about this magic formula! My question is: Can CA-OX/CA-PHOS stone- formers take supplemental Calcium Citrate to “up” their intake of Calcium from foods? Most high Calcium foods are also higher in Sodium, making it difficult to reach the needed 1,000-1,200 mg. of Calcium daily. I am concerned about supplemental CA due to the problem of it contributing to heart disease per many published scientific articles. Is it safe to take the supplement?
Kindest Regards, Jolie
Hi Jolie, Supplements must be taken with meals, but are reasonable. Because of timing needs they are trickier than calcium containing foods. As for heart disease, I do not know if supplements are a risk. If taken with meals they should be much like food calcium in being absorbed slowly. After all calcium is an atom, the same in food as the supplement except for absorption and the extra alkali. Milk and yogurt are very high in calcium per unit of sodium, so are the best choice. Regards, Fred Coe
Dear Dr. Coe,
Thank you so very much for answering this vital question for me; medical doctors are so evasive concerning this topic and I really look up to you as a mentor and medical professional who answers the hard questions others seem reluctant to! God bless you for your caring heart to help others!
With a grateful heart, Jolie
This was the best article you’ve written yet for those of us not in the medical field. Much easier to read. Thank you!
Thank you, Terri, I am learning – slowly! Fred
Is there any information out there for a Spinal Cord injured person who has to be tube fed so cannot vary their diet? Has a suprapubic catheter.
His stones are formed due to reoccurring UTI’s, (struvite) frequent among paralyzed individuals. His PH is always 8 or over. Read that to avoid infectious stones that his urine must be more acidic – how? Has 4 ozs of lemon juice in his coconut water – has more than 2 ltrs of fluid daily. Read that the lemon juice actually makes the urine more alkaline – true?
Just in Emergency with fever and UTI because he has a 9 mm stone stuck in his utterer plus other stones in his kidneys, he is awaiting surgery – AGAIN ( 6 in 3 and a half years) but delayed due to the COVID 19 virus.
His stones only began to form a year and a half after he fell and became paralyzed C3/C4 due to cervical spinal stenosis – no problems before.
Tried – low dose of antibiotics, Cranberries, D. Mannose, Mandelamine (found out PH had to be 5.5 , Is now irrigating his bladder with Renacidin 3 times a day which has actually reduced the catheter being blocked and was able to go over a year since his last surgery.
Any suggestions – any research into tube feeding and SCI patients with reoccurring UTI’s and infectious stones?
Hi Janice, The struvite stones are being produced by the action of bacteria that hydrolyse urea – a normal urine constituent – into ammonia and CO2. The ammonia raises the alkalinity of the urine to very high levels, even 9 or more, and the CO2 becomes carbonate. Magnesium and ammonium and phosphate, all normal in urine, precipitate into struvite. Renacidin is a magnesium containing solution that can help dissolve struvite and is an excellent idea. The bacteria that make the crystal normally live in the soil and are part of a planet wide nitrogen cycle. Having evolved in soil they rapidly become resistant to antibiotics. His diet is not the cause and change in diet has limited ability to improve things, given the bacteria are so powerful. Acetohydroxamic acid is an oral medication that can block the enzyme in bacteria that hydrolyses urea, and the drug can stop struvite, but it has a lot of side effects. You might want to mention it to his physicians. Regards, Fred Coe
Thank you Dr. Coe. Your articles are very informative! I recently had a 8 mm oxalate stone surgically removed that was stuck, although thankfully not completely blocking the ureter. I have another 3 mm stone sitting in the kidney calyx that is still there. I typically don’t eat dairy products, and am vegan. I don’t eat a lot of sodium but I will keep an eye on sodium content and don’t salt my food. I am taking calcium citrate supplements, as well as magnesium supplements. I also make my daily morning smoothies with almond milk, but maybe there is a better option? My question is will the calcium citrate supplements give me the calcium that I need in order to reach my daily calcium goal? From your articles, it seems that I definitely need to be sure my calcium intake is adequate, and it may not be. Thanks for any suggestions you may have for one who doesn’t eat dairy but needs more dietary calcium.
Hi Pamela, calcium citrate is certainly a way to get the extra calcium, and be sure to use it with your main meals to block oxalate absorption. But also be sure you have been fully evaluated. Don’t just alter your diet without evaluation. You never know what causes stones until you look. Regards, Fred Coe
Hi Dr. Coe,
This presentation was awesome and clear! Thank you. My urine calcium has always been fine. I just turned 70 and was told I have borderline osteoporosis. My doctor has left it up to me as to whether or not to take the med he has prescribed: Alendronate Sodium Tablets 70 mg. This seems to go against everything I’ve been working toward to keep my oxalate stone from growing. In four years (since Jill’s course), I’ve had no change in my stone. Is I opt to take this med, one of the side effects if hypocalcemia. My urologist says my bones are important, so maybe I should take it but I might have to take a calcium supplement. Do you have any thoughts on this? Id love your opinion.
Hi Jeannette, Given borderline osteoporosis the drug is optional, as your physician says. OF high importance is a high calcium low sodium diet, however, as there is one major study in women showing that combination helps prevent bone mineral loss. The study is summarized in this article you have written on. I would strongly hope you might follow such a diet and get a new BMD in a year to see progress. The 24 hour urine is crucial if you would know your success in the diet – it gives you the urine sodium which is the diet sodium absorbed, and a good sense of stone risk from a high diet calcium. Regards, Fred Coe
Very good information. In layman’s terms if I’m correct. 1# Low sodium 2# higher calcium 3# watch the higher Oxalate foods. Is this over simplified? Or good. Just had a 9 mm stone removed( nightmare pain!) I must change my diet! I’m 60. Male. The urologist said the hardness of the stone was 1300, he told me ONLY Oxalate stones are this hard. I’m sending it in to be analyzed. Have another 1 and 2 mm but hardness is 186 only the urologist said these are uric acid stones most likely. Thank you!
Hi Ron, By all means analyze the stones. It can be hard to estimate mineral density in small stones, but if you are forming uric acid stones urine pH will be low and need special treatment. Here is a good introduction to stone prevention that covers the basics and points to the special problems. Regards, Fred Coe
Dr. Coe,
Thank you for such a thorough read. I am a relatively healthy eater, 44 years old, and living in the “kidney stone belt” (NYC). After creating and passing a 4mm Ca-Ox stone last summer, which caught me utterly by surprise the night I returned from a long airplane ride (apparently a trigger, sometimes), I have been working on my health in this area. I had a 24-hr urinalysis last Aug, and by Feb all my numbers improved except the sodium.
pH 5.5 to 5.9
SS CaOx 7 to 3
Ca24 178 to 155
Ox24 45 to 32
Cit24 646 to 748
SS CaP .29 to .32
SS UA 2.5 to .84
UA 24 1.0 to .9
I started with Potassium-Citrate, but didn’t take well to the side effects. So I began a religious course of fresh lemon water every morning, refilling the glass with the lemon rind throughout the day. I have now begun ionizing water with a pH stick (EHM is the company) to raise the alkalinity of the water I drink. Now that I’ve read your article, I’m paying closer attention to the Na24, which actually moved the wrong direction from 151 to 163.
1) Can you explain the lemon process, turning more basic upon ingestion? Does it compete with the ionization of the water (counterproductive)? Should I not ionize the water? What about Apple Cider vinegar as well? Will this help? Does it too turn more basic upon digestion?
2) If I understand correctly, by lowering my digestive sodium (Na24), my calcium absorption should actually increase but my Ca24 should go down a bit more?
3) Is there more I can do to prevent idiopathic hypercalciuria?
Thank you!
PS: I stopped eating spinach. 🙁 But I can’t give up my unsalted mixed nuts in my morning yogurt.
Hi Sam, Given your present low SS values, perhaps you do not need to do more. Lowering diet sodium will reduce your urine calcium further but it is already below the level known to confer risk of new stones. Reduced diet sodium lowers urine sodium by raising kidney calcium conservation. Citrus fruits contain citrate and citric acid, the former is metabolized to alkali, the latter is not. So the more ripe the lemon the more citrate, and the better the effect. As a person in the US, better health is served by lowering diet sodium below 100 mEq/d so if you could you should. Regards, Fred Coe
Dr. Coe,
I’m sure you’re somewhat familiar with HCA, which is widely available for appetite suppression but is also being studies for potential dissolution of kidney stones. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6540651/
Are you aware of anyone who has experimented with it for stones, and if so, what the results were?
Thanks much!
Hi Russell, I am familiar with the compound and such work as has been done. The citrates in general bind calcium and can act to reduce formation growth and even the integrity of calcium centered crystals. Since it is widely available as a health supplement, and perhaps for other reasons, I know of no trials. It seems without obvious harms. I cannot endorse it nor advise against it, but should say that if you have stones proper testing for cause and treatments such as we have data for would have precedent in my thinking and what I do. Regards, Fred Coe
Hello Dr. Coe and thanks for your clear writing.
I had one Ca-Ox stone 30 years ago – I was taking a lot of Vit C (don’t ask why!) and riding my bike in hot weather, probably dehydrated. No stones since. Now I am 61 yo healthy man. I am considering taking tumeric/curcumin supplements for knee pain. I also have osteoporosis. I eat carefully (near vegetarian, fresh food diet, about 80-120 mg oxalates/d) have a high Ca diet and am working to lower Na intake.I don’t think I’m a stone former, don’t know if I have hypercalcuria. Would adding tumeric/curcumin put me at risk? How much should I take? Thanks, Ben
Hi Ben, Tumeric has lots of oxalate. Curcumin is not high in oxalate. Animal work – mice – suggests Curcumin might reduce stones, but animal stone models have so miserably failed and misled the field of stone disease I would not trust any of it to guide physician practice. As for your high calcium diet, remember that vegetable calcium might not be well absorbed – check it on the web by food. Regards, Fred Coe
Hi, i recently stopped taking curcumin as I thought seeing as turmeric was high in oxalate that this would be also. Would i be safe to take again as I have a kidney stone?…also, what are your thoughts on nettle powder?
Thank you
Andrea Lloyd
Hi Andrea, Curcumin is part of turmeric, and as the article says, is dangerous but made safe because not absorbed by the intestines. It has no role in medicine and will not raise oxalate. Turmeric can. Regards, Fred Coe
Hi Dr. Coe,
Thank you for these thorough and clear articles. Can you please comment on the intake of sodium in the context of a very low carbohydrate diet (less than 40g/day net). I am assuming that the studies above and elsewhere on your site were done in the context of a normal American carbohydrate load of between 100-300g/day. I have heard in the context of a ketogenic diet that sodium needs actually increase some. I am curious what you may know or studies you may know of that deal with urinary calcium excretion and net acid loads in the context of low fasting blood glucose levels. My husband (57) forms calcium oxalate stones ( 3 times since 45). He has a history of high fasting blood sugars but has now turned this around with a extremely low oxalate, very low carb (40g or less), higher protein (1.2-1.5g/kg day) diet. His fasting blood sugars are down from over 109 to 88 mg/dl. We are curious what effect on his kidney stone formation his lowered blood glucose might have and how that may or may not change the sodium recommendations included above. Thank you,
Hi Amy, If the diet produces high ketone loads for excretion, the ketones can promote sodium and potassium losses being negatively charged ions. I do know know the data concerning urine calcium response to reduced diet sodium during high urine ketone losses, but suspect urine calcium will be higher from the ketones. This kind of complexity is why he needs attentive physicians, and they need 24 hour urine testing to determine what is happening. I would suggest that 24 hour stone urines be done for monitoring and that urine ketones also be measured. Day to day management has to be from his physicians because this is complex physiology, but I suspect reduced diet sodium will always be helpful. Regards, Fred Coe
Thank you Dr. Coe,
He is about to do another litholink test to see where he is in terms of urinary output of calcium, sodium, potasium, etc. I do not suspect he is actually particularly ketogenic with high urinary ketones despite the low carb intake because his protein intake is higher as opposed to his fat intake being higher as in a typical ketogenic diet. His diet is high meat(1.5kg/kg), very low carb( 40g) , high but not crazy high fat intake.
I guess I am wondering if carb intake being exceptionally low influences sodium requirements or recomendations in the absence of ketones. He has been following a 90% carnivore diet. Mostly animal meat, a bit of onion, mushroom,etc, sometimes a few teaspoons of honey and a little fruit ( one serving or less per day). So his diet is not specifically ketogenic due to high protein intake but again blood sugars have been brought into healthy fasting ranges in the 80’s. The meat offsets the typical ketone production in such a diet.
People who go on low carb diets typically feel better with additional salt intake ( especially during initial transitions).
I guess I am just curious if you have heard of carb intake and higher blood sugar being a lever that affects calcium/sodium output. It is an unusual situation as so few people follow such a low oxalate ( near none), high protein diet. It is not well studied. The best resource I could think of for further info on such low oxalate, low blood sugar situations might be you and your team since you have done so very much with regard to treating stone disease through diet. I am very grateful for this by the way as there are so few doctors who focus on the effects of and are knowledgeable about the intricacies of diet in the diseases they treat. So thank you for any additional insight you might have.
Hi Amy, the only link I know of between CHO restricted diets and sodium is via ketones – they are anions and obligate sodium and potassium loss. High protein without high fat or carbohydrate is a special case. It causes depletion of body fat stores and weight loss if CHO intake is very restricted, so ketones form from one’s own fat. Later on, it is not healthy – good reading here is what happened with Lewis and Clark, 5 pounds a day per person of Elk meat and they lost body fat and were starving. Regards, Fred Coe
Thanks Fred! Great reference. Yes absolutely high protein low fat diets would cause starvation. Completely get that. Rabbit starvation situation. Elk can be extremely lean. Good to remember the importance of fat especially once body fat percentages get really low. I would assume lewis and Clark were in single digits by the time they did all that outdoor living and traveling. Thanks for reminding me. Well if the ketones create greater excretion of salt and potassium it must be why it is suggested to supplement salt while ketogenic. Again specific case here though while trying to fix stone formation. I guess litholink should be best guide here based on mineral excretion data. He has the test on order and will be very interesting to see where he is at. Thank you again for your response.
Could you please post link to article you mentioned re: Lewis & Clark eating lots of meat but starving? I searched online, but couldn’t find it. Thank you, and thanks for creating this article and video. It was very helpful.
Hi Chantal, It was in a book on the expedition and I cannot find it on the web – with a brief attempt. I suspect it was the well described problem of eating animals with no fat and also having no available carbohydrates. This latter – usually arising from eating mainly rabbits that have very little body fat – is well known as ‘rabbit starvation‘. Of course none of this happens in cities unless one pursues a drastic kind of diet. Regards, Fred
I really appreciated how the video explained the article and would love to see a similar video that goes with this article “DIET PROTEIN AND POTASSIUM AND KIDNEY STONE RISK”. Thanks
Hi Terry, thanks for the comment. Others have expressed a liking for the videos, and I will do one on the protein article – for you. Fred
Dr Coe; I don’t know how I missed this article but I did. It seems I already was doing part of the magic potion (based on my 24hr collection a couple months ago). My sodium was 87 mmol, and my oxylate was 27.3 mg. However, at the time of the test, I was not getting much diet calcium (only a little from cheese, berries, brocoli, tomatoes etc) and output only 1.7 liters. I was also making no attempt to add citrate. Consequently, from the 24hr collectiion, my citrate was 556. PH was 5.5. Calcium was at 340, Potassium was 46mmol, and magnesium was 187 mg. This was a two year follow up from previous stone and surgery. Recent CT scan shows a previous 2mm stone has grown to 3mm and I have two new 1mm stones. I have now made the following changes: increased fluids to 2.5 liters a day, and I add two grams of potassium citrate powder (weighed with a scale) to my 2 liters of water each day. I also take 3 capsules a day of a potassium-magnesium bound form of HCA. Finally, I have significantly increased my dietary intake of calcium with mainly swiss cheese (less sodium) and milk to get around 1,200 to 1,400 mg a day. Whether or not it’s enough for my recently diagnosed osteoporosis, do you think it may be enough for stone prevention? I have another 24hr collection coming up in about two weeks. What numbers should I expect to see changed if I’m indeed now on the right path?
Hi Robert, I suspect you have genetic hypercalciuria and your stones are calcium oxalate. Adding citrate seems wrong as there is risk of converting to calcium phosphate stones, and your urine citrate is already far above the risk limit – high enough citrate is not posing any stone risk. Your only stone risks seem low urine volume and high urine calcium, the latter is being treated with low sodium diet is remains very high. Your bone disease may well be from the genetic hypercalciuria. Whereas you may well need more diet calcium for your bones, urine calcium will rise, and I think you are an ideal candidate for thiazide which will help protect bones and also lower urine calcium. There may be other reasons for bone disease that need evaluation – beyond the scope of this site at present. Regards, Fred Coe
Thanks Dr Coe. It’s all so confusing and complicated. I think I understand something, only to discover later that I don’t. My nephrologist doesn’t want me to eliminate all additional citrate intake so I’m stopping the potassium citrate mixed in my water (with a small amount of lime juice for flavor) and just using the potassium-magnesium hydroxycitrate (1 capsule every 8 hrs, total 1.5 grams a day). I have read a couple of studies that show hydroxycitrate (HCA) does not raise PH nearly as much as potassium citrate. She also finally talked me into a trial of thiazide at the lowest dose. I have always resisted because of it’s diuretic properties and my BPH issues and already lowish BP (typically around 115 over 60). She explained it’s a pretty weak diuretic and at the lowest dose, I might be able to tolerate it.
Hi Robert, Thiazides have multiple positive trials in calcium stone prevention, and a massive patient use over the past 5 decades. As for hydroxy citrate, it is a food additive and in health stores, and I have no evidence it does any harm. There are theoretical reasons why it might reduce stones but I have no real evidence that it does. Regards, Fred Coe
Well, it turns out I have no trouble tolerating 12.5 mg of Thiazide and I feel foolish for avoiding it all these years. No bad side effects at all. No dizziness, no effect on blood pressure, and strangely enough it seems to alleviate my most troublesome BPH symptoms. Urgency has gone way down as well as frequency. I have read studies that Thiazide can cause a decrease in PSA levels in middle aged men, they don’t apparently know why. Maybe it’s just psychological but the Thiazide seems to make me feel better overall somehow. I’m writing this for anyone else out there that has been avoiding Thiazide like I was. Just try it. You might be surprised. Added plus…$10 for a 90 day supply even without proscription drug coverage!
Fred, have you read the article, “damaging effects of oxalates on the human body” on the Urology of Virginia website? I found it pretty alarming. They are arguing that, oxalates are a lot more pernicious than just playing a role in kidney stone formation and can cause all types of problems They are also suggesting some radical ways of dealing with it, such as the Carnivore Diet. Is it a reputable institution, this Urology of Virginia? I have no idea as I live in the UK. Best wishes, John
Hi John, I answered you in detail in your private email. The only way oxalate can cause injury – that I know of – is by forming crystals, as the molecule itself is a metabolic end product. Regards, Fred
Hi Dr. Coe. I am an intermittent faster (IF), in which I only ingest calories in a 5 hour window, 24/7/365. Upon discovering your site in May, I modified my diet to ensure I get ~500mg of calcium in my first meal and then ~500 more in my final meal ~4.5 hour later.
1. Is it necessary for me to separate my calcium intake? Everything I’ve found on the web states, “the human body can only process around 500mg of calcium / meal.”
2. What is the minimum time gap between ingesting the 500mg of calcium that would still constitute a separate meal? Is my 4 to 4.5 hour gap enough? I can try modifying my eating window a bit, but would prefer not to.
TIA!
The calcium is meant to bind oxalate, so absorption or not is irrelevant for stone prevention. Fred
Can you expand on your answer, Dr. Coe? For instance, I don’t think you’re suggesting that it’s fine to ingest 1,500+mg of calcium in one meal, in relation to stone formation, are you?
In fact, do you have an upper limit on total calcium for a day, spread out? I try to keep between 950 and 1,100 / day (separated in 2 meals), but in your above article, you indicated that, as long as we are on a low sodium diet, we can go up to 1,300. Are there any data on going higher / day?
And back to how much in a single meal, is it “safe” to have 700-800 in one meal, especially if there is oxalate intake? Or is more research needed to answer these questions? Thanks again!
Hi Brett, US recommendations are for about 1000 – 1200 mg of calcium from food daily and that is about right for stone formers. I think it ideal to put the calcium mainly in meals that contain oxalate in most abundance, as calcium will reduce oxalate absorption. I do not think it much matters for any one meal if food calcium is 1/2 of the day’s intake – absorption of calcium is at best 18-22% and as high as perhaps 30% in idiopathic hypercalciuria, and spread out over hours in food, so stone risk is mainly reduced by lowering oxalate. Refined timing studies are not available. Regards, Fred Coe
Thank you for all of your wonderful articles, Dr. Coe. They are a treasure of knowledge. I do have a question about one sentence in this article. The sentence reads: “At the heart of idiopathic hypercalciuria is what this graph shows – urine calcium is abnormally sensitive to diet calcium.” Shouldn’t the last word of the sentence be “sodium” rather than “calcium”?
Hi Michael, How good a reader! Of course, and I just changed it. Best, Fred
I’m a 54 year old female who has been making kidney stones for 35 years. Most recent (2018) CT scan revealed at least eight stones in my left kidney 5mm or less. Recent stone analysis indicated calcium oxalate. Results from recent 24-hour urine collection tests (2.5/2.8 urine volume) and blood serum test were normal except for urine calcium was borderline elevated (214/198) and urine pH was high (7.4/7.6). Preventing new stone formation by increasing fluids and decreasing sodium is reasonable, but increasing dietary calcium is more difficult since I eat mostly vegetarian and have wheat/dairy sensitivities. To make things more complicated, I have Hashimoto’s thyroiditis (partial thyroidectomy 2012) and a recent osteoporosis diagnosis. Trying to navigate through dietary guidelines for kidney stones, osteoporosis, and thyroid disease is very challenging. Due to my recent osteoporosis diagnosis I’m very concerned about my bone health. I’m hesitant to start taking osteoporosis meds due to side effects. I prefer to try a more natural approach (diet and exercise), Since getting enough calcium from plant-based non-dairy foods is more difficult, I have been researching calcium supplements. I’ve learned traditional supplements are likely to increase new stone formation. Are plant-based calcium supplements from algae also going to increase new stone formation? Do you have any other recommendations for increasing calcium without the risk of forming new stones. Many many thanks!
Hi Lisa, with so many stones, and an alkaline urine pH you really should consider using thiazide diuretics to lower urine calcium and reduce stone production. Ask your physician about the matter. Thiazides have been tested for calcium oxalate stone prevention in three excellent trials and work. I also am suspicious that your stones may contain a high proportion of calcium phosphate crystals – high urine pH does that – and thiazide would be even more specifically valuable for prevention. As for sources of calcium, dairy products are ideal, but given thiazide and a marked reduction of diet sodium you could use calcium supplements especially taken with meals. Regards, Fred Coe
Dr. Coe, Thank you for the wealth of information you provide. If it hadn’t been for your site, I would not have known to ask for a 24 hour urine after my ostoperosis diagnosis at age 54. I thought I was controlling things with diet, but my most recent test showed a level of 400 (I admit I had fallen off the sodium wagon). 12.5mg of Thiazide gives me constant headaches and stomach upset. I started cutting the pills in half and the side effects have vanished. Do you think a half dose could be effective? By the way, I do not have kidney stones and my osteoperosis has stayed stable for the last few years focusing on diet and exercise and high diet calcium. I wish you offered telehealth. I would sign up in a moment! Thank you again!
Hi Shelley, Idiopathic hypercalciuria (and stones, too) associate with bone mineral loss, as does menopause, so things are complex with you. Thiazide is bone sparing, and dose effects not at all clear so very little may help. It may be time to consider bone directed meds, as well. I do telehealth (though I do not advertise the fact) and my secretary can arrange things, if you like (Banita Williams – 773 702 1475; bwilliams15@bsd.uchicago.edu). Regards, Fred Coe
I am a 72-year-old male, treated for prostate cancer in 2016 with TURP and brachytherapy. Cystoscopy in May 2020 reveled stone accumulation in the urethra just below the bladder neck, removed with lithotripsy. Recheck in June 2021 reveled even greater stone regrowth; scope could not be passed into the bladder. CT scan showed large stone accumulation in same area and all else in the area normal, again removed with lithotripsy September 2021.
September Stone analysis: 40% calcium phosphate, 30% calcium oxalate monohydrate and 30% calcium oxalate dihydrate. I have never had a kidney stone.
I’m interested in your thoughts on prevention and possible future treatments.
Hi James, a common cause of crystal formation in the bladder is incomplete drainage, perhaps present despite the TURP. A secondary cause would be 24 hour urine abnormalities that predispose to crystallization via increased supersaturation. A common other contributor is low fluid intake because of bladder drainage problems that is in fact supersaturating the urine via low volume. Perhaps your physicians might want to pursue these possibilities in hope of stopping the problem. Regards, Fred Coe
Thanks for your reply. Please allow me to add a couple of points: I have never had a kidney nor bladder stone, the stone accumulation is in the urethra just below the bladder neck. The latest was 2.7 cm craniocaudal by 2.0 cm AP by 2.8 cm transverse and took about 14 months to accumulate. This caused pain, often severe, for several months.
I’ve has numerous ultrasounds to check bladder emptying and bladder was always fully empty. These stones did not start appearing until had I had the procedure to remove the bladder neck restriction. Could they possibly be growing on scar tissue?
Thanks again.
Hi James, Thanks for the additional information. Quite possibly. Crystals can form on tissues that lack the normal epithelial mucous layer, and become a stubborn nidus. Even so, one wants to make urine chemistries as minimal as possible with respect to the crystals in hopes of reducing growth. Regards, Fred Coe
I’ve gone on a low oxalate diet with particular elimination of spinach which was a big part of my diet previously. And a large glass of water with lemon juice in the AM. I’ll have a recheck for stone buildup in January hoping for none or, at the worst, to not let the stone get as large as before. I’ve had no pain at all since the stone removal in September.
Thanks again
Hi James, This article offers a lot more than you mention, and I hope you consider more than diet oxalate. As for lemons, it is merely a way to get a food version of potassium citrate. You have to ask if that is what you need – low urine citrate, too acid a urine pH, as merely adding lemons has no real basis in fact as a treatment. I do not see mention of diet sodium or calcium, so please consider if they are ideal. Regards, Fred Coe
Another update. I have had urethrla crystals (hesitant to call them stones) removed 3 times in the past year: September ’21. January ‘22 and August ’22. A recent 24-hour urine test revealed the following that were out of range: Ca24 – 433; SS CaP — 3.49; Mg24 – 147; CL 24 – 141 and Ca24/Cr24 – 268.
I’ve been on a low-oxalate diet since November and it, apparently, had no effect on the crystal growth.
I would travel the 750 miles to your clinic but my Medicare insurance does not list U of C Hospital as in-network.
Do you see any reason for this rapid crystal growth or, more importantly, are able to suggest what I may do to solve or slow this issue?
Thanks.
Hi James, You have very high urine calcium that is the likely cause of the crystals; the high SS CaP suggests that urine pH is also high – over 6.3, and that diet oxalate is of little consequence. So I see good reasons for the crystal formation. I imagine it is calcium phosphate crystals and they can form very rapidly. You should have the crystals analyzed. Will your insurance cover telehealth?? If you say where you live I can try to find someone for you. Regards, Fred Coe
Hi Dr. Coe. Have you heard anything about abnormal gut microbiomes with stone formers? Specifically the lacking of Oxalobacter formigenes?
Thanks.
Hi Margaret, Many papers have presented data on OF. It correlates with stones or not but attempts to give it as a treatment have proven futile. Some new treatments have emerged using an oxalate degrading enzyme – I have not as yet worked with it. So in all, an active area of interest, not any major patient benefits thus far. Regards, Fred
Thank you for responding to my first question. I have another question: I read that calcium oxalate stone-formers should avoid soy products. Then I came across this abstract (https://pubmed.ncbi.nlm.nih.gov/15998131/) that said, while soy tends to contain a lot of oxalate that can lead to stones, it also contains phytates that inhibit stone formation. Are soy products still to be avoided by stone-formers?
Thank you for your time.
Hi Margaret, Inhibitors are a dodgy matter. Urine contains innumerable calcium crystal inhibitors but crystals still form. Adding a food with oxalate in hope another molecule will offset the increased supersaturation is just that – a benign hope. I would not desire to trust in it. Fred
I want to make sure I’m understanding the levels of dietary sodium and calcium. I want to aim for 1500 mg sodium (or less, I assume) and 1000 mg calcium? Along with 2 liters of water per day. Is this correct?
Yes. Regards, Fred Coe
Hello Dr Coe,
I have recently passed three calcium oxylate stones in six months. My kidney ultrasound shows bilateral hilar vascular calcifications. Can you recommend a specialist in the Norfolk or Virginia Beach Virginia area for me to see? Also do you have an opinion on Vit K possibly helping to actually reduce this calcification? If no, will it help stop further calcification? Thank you.
Hi Joan, I think the medical school in Richmond is your best bet. They might also have some expertise concerning your vascular calcifications. Regards, Fred Coe
Dr. Coe,
You treated me successfully for kidney stones when I lived in Chicago in 1981. You prescribed a maintenance drug that I took for maybe 20 years, before it was discontinued, and I did not have a stone during that period. I am now 67 years old, and I have had three calcium oxalate stones in the last 3 1/2 years after not having stones for a long time. I moved to CT in 1987 and went up to Yale for a few years, while I was still on your medication. Is it time to go back to Yale, or someone else whom you might recommend? Thank you for providing me with so many stone-free years. Regards,
Peter Seldin
Hi Peter, I do remember. I presume you stopped the drug and had more stones. Indeed you should be under treatment and there is nothing wrong with Yale. Fred
Dr Coe
Retired nurse with pots syndrome, told to always add salt so now I have stone in kidney…Noone saying to address it, but I think I should.. I’m trying reduce salt, I also have osteoporosis dx…not done anything yet, Noone suggesting 24 hr urine or anything, let’s watch and see. I’d like to be proactive. Cut out spinach, high oxalate foods, reducing sugar, adding glass fairlife skim milk daily….I’m guessing bcs no 24 hr urine. Suggestions for potsie with dysautonomia ?
Hi Loree, Given a stone, and bone disease I do not think it is ideal to do nothing. At least ask your physician to measure the density of the stone on CT as people over 50 (I am guessing here) may form uric acid stones. Likewise 24 hour urine testing, because there may be abnormalities one can reverse. Here is my article on stones in midlife. I would not change diet randomly – pointless. There is no obvious link between your autonomic nervous system disorder and stones. Regards, Fred Coe
I had my first stone at age 20, have had lithotripsy twice, have been stented twice, both my aunt and my sister are down to one kidney due to stones. The doctors I have had simply tell me to drink more water….can you recommend someone in the Milwaukee area or would I be best off to come down to your clinic?
Hi Denise, Given the strong family history and stone surgeries I would advise decisive prevention beyond water alone. In Milwaukee the university is your best bet. Given telemedicine, I can ‘see’ you and offer consulting help (secretary 773 702 1475) to your physicians. Regards, Fred Coe
Hi Denise, Given the marked family history I would recommend a full evaluation and a prevention plan based on what is found. In Milwaukee I would think the medical school is a safe choice. Given Telemedicine, I can ‘see’ you (secretary 773 702 1475). Regards, Fred Coe
Dear Dr Fred,
I am a first time stone former and haven’t passed any yet – so cant be sure which ones but they are visible on both CT scan & Xray, so I am told these are Calcium Oxalate ones. I am in Dallas area and I can’t seem to find a urologist who specializes in Kidney stones removal and prevention. Do you know anyone like yourself in the Dallas area ? or do I need to travel to Chicago ?
Many thanks
Rajan
Hi Rajan, In Dallas at UT Southwestern Dr Orson Moe is expert at medical stone prevention. Dr Peggy Pearle is a famous stone surgeon at the same institution. There is no need to come here when you have such talent right there at home. Regards, Fred Coe
Dear Dr. Coe,
Since 2013, I have developed six kidney stones. I currently have three kidney stones, two in the right kidney, and one in the right proximal ureter. I am needing am more help with prevention than I am currently receiving. Please let me know of any qualified urologists in the Denver/Boulder Colorado area that you suggest to be of best benefit for me. Thank you.
Hi Warren, The university medical school is by far your best bet. I would use their kidney stone program. I could not find it within renal medicine but you will do better with a phone call. Regards, Fred Coe
Hi,
This is a bit long….
My family member has complicated and competing medical issues regarding nutrition. In early 2020, he had kidney stones removed by surgery. In May 2022 he had a complete abdominal ultrasound which showed NO stones. He takes a medication nightly that is sedating and can cause constipation (fortunately it doesn’t for him) and will cause high blood cholesterol and blood fats and may also cause diabetes, so he needs to watch his intake of fats, cholesterol and carbs/sugar. He is not very compliant, and his diet is high sodium as well. If he drinks 48 oz of water a day, that would be a lot for him. He hates fruits, the only fruit he’ll eat is canned pineapple, which is extremely high in oxalates.
He had his gall bladder removed on June 17, 2022. He had diarrhea, once after surgery, then was fine for a week with normal bowel movements, now as of this note he has diarrhea (liquid) once daily. I have insisted that he contact the gall bladder surgeon ASAP regarding the diarrhea. For the week after surgery, he stopped taking a magnesium supplement (which he had taken for years) because he was concerned that it would exacerbate the diarrhea. It was immediately thereafter that he passed another stone, in urine, on June 28, 2022, in my opinion suspiciously while he was off the magnesium, which I was under the impression was helpful in preventing stones. His urologist disagrees.
He restarted the magnesium at half dose and was fine, then went to his regular dose and got diarrhea the next day and has had diarrhea once daily since stopping the magnesium again. So currently the most pressing issue for him is what he can eat to calm down the diarrhea, which may be a result of the gall bladder removal because of bile dumping.
His urologist gave him the following Kidney stone prevention advice.
1. Drink at least 10, 10 oz glasses a day of liquid except for dark colas and tea.
2. Limit sodium intake to <1,500 mg a day.
3. Two fresh lemons or "real lemon" lemon juice/lemonade a day may elevate your citrate level and help prevent kidney stones.
4. Most stones are PREVENTED with HIGHER calcium intake, so do NOT avoid calcium. We recommend at least 1 gm of calcium intake a day, (My family member's solution is to eat cheese. but cheese is high in salt, which I have told him many times. I have suggested drinking low fat milk instead of cheese). 5. No more than 8 oz of animal protein a day. (His nightly med makes him very hungry, and he eats large portions.) 6. Obesity is a big risk factor for stones. 7. Limiting some high oxalate foods, like spinach, nuts, berries, avocados and teas within reason- because in general these are very healthy foods and the benefits of consuming these foods usually outweigh the risks. Search foods that you consume daily or in high quantities to check oxalate content and try to reduce intake. (Only raspberries are very high in oxalates, as far as I know.)
If we can’t get him to comply with diet, especially reducing sodium, and drinking copious amounts of water, what meds are available to help prevent stones and what are their side effects? How would a dietician/ nutritionist meet the competing needs of his dietary requirements? So many of the foods he should eat, he refuses to eat or are not compatible with a kidney stone prevention diet.
Hi EmRo, I am afraid that you are flying blind in a cloud of competing GI and diet issues – or at least I am. What are the stones made of? What to the 24 hour urine collections reveal as to the cause of the stones? Diet prevention rests on principles but varies with the details of any one person. For example, is urine oxalate high? Do stones contain oxalate? Is urine volume or pH low from the diarrhea?? Your urologist is not out of line in recommendations but are they appropriate for this person. Like in carpentry – measure twice, cut once. Regards, Fred Coe
I just received by 5mm stone analysis. 60% Calcium Oxalate Monochydrate, 30% Oxalate Dihydrate, 10% Phosphate apatite. I have been diagnosed with hypercalcuria and osteoporosis earlier this year. I was a few days away from starting on forteo when I had a stone attack (June 1,22). I had a Cystoscopy, Left retrograde pyelogram, Left ureteroscopy with laser and Left stent placement on string which was removed after one week. I have not had a follow up with surgeon. From his post-op notes he thinks I may have UPJ obstruction and I go for a renogram next week. May I deduce from the stone analysis that I have to watch my oxalate intake? What does one do for fiber? One can’t possibly their 25-30 grams without bran can they? What other tests might you suggest that will help me with my kidney health and decide on the best bone medication. I love your the quote “A stone clinic should also be a bone clinic” but it doesn’t seem that how it works around here. Thank you for all the wonderful, helpful information.
Never mind about the fiber question, I just read Jill’s Your High-Fiber, Low-Oxalate Grocery List if I really do need to watch my oxalates. If you would be so kind to help me with my other concerns, it would be so appreciated.
Hi
Jill is easily reached on line – https://kidneystonediet.com/. Regards, Fred Coe
Hi Antoinette, No, oxalate is not your main issue, it is the hypercalciuria and perhaps oxalate if your 24 hour urine oxalate is elevated. Be sure you have been fully evaluated. Treat what is abnormal. For the hypercalciuria, as the article notes, reduced diet sodium is a first step. This permits high calcium diet without risk of raising urine calcium and stone risk, and also lowers urine oxalate. Lower diet oxalate comes last, if urine oxalate is high despite the high diet calcium. The article you wrote in on, in other words, is a very good choice. Regards, Fred Coe
Hello and Happy Holidays Dr. Coe!
Had all the testing and I am now on a low dose hydrochlorathiazide 12.5mg once daily for calcium in urine(322mg/24hr). So now to decide what bone med to be on. I have an endocrinologist suggesting fosamax and a rheumatologist suggesting forteo. No fractures. T-score of hip -3.0 and -2.9. Concerned about Forteo and the calcium issue. Do you have any thoughts? Thank you in advance. Antoinette
Hi Antoinette, Thank you. If your two bone physicians can agree, the bisphosphonate (fosamax) does not, and the Forteo does raise urine calcium and stone risk. So on balance perhaps the former might win out. But I am far away and they are not, so it is up to them to argue it out. Regards, Fred Coe
Thank you.
Hi Coe,
how can i get rid from reoccurring kidney stones, I’m having since 2017 every years, and sometimes in a month’s.. there’s is no single doctor is helping me. All just say keep hydrated this is the only solution. i tried everything. i drink daily 4+ litre water + lemon juice, low sodium nothing difference… please help me.
My all tests are normal except 24hrs CA that was 360 but PTH was normal.
Hi Sami, Here is my best effort at what to do and how to get it done. See if it helps you. Regards, Fred Coe
Back on August 20 you asked me to respond with my location but there was (is) no “Reply” button alongside your comment. I sent emails to bwillaims15@bsd.uchicago.edu but received no response. On August 15 I had the stones removed for the 4th time. A followup cystoscopy on October 13th showed very little regrowth so I’m somewhat encouraged. For the record I live in Charlotte, NC and my Medicare coverage does not include your university. I’m currently trying to get into the Urology department at Atrium Health. Is there additional assistance you can provide. Thanks.
Hi James, Sorry for the communication problem. Atrium is the only university provider in your area so far as I know and should be what you need. Regards, Fred