 Glomerular filtration is the main life sustaining kidney function, and kidney stones can cause enough damage to lower it. Usually the reduction is very modest, but sometimes stones can cause kidney failure. This means, like all diseases, stones are best prevented as early and as completely as possible.
Glomerular filtration is the main life sustaining kidney function, and kidney stones can cause enough damage to lower it. Usually the reduction is very modest, but sometimes stones can cause kidney failure. This means, like all diseases, stones are best prevented as early and as completely as possible.
This ‘just the facts’ version tells about what filtration is, how physicians measure it, how much kidney stones lower it, and how often that occurs.
Two longer articles give the details. One is comprehensive. The other focuses on only kidney disease, but is long.
Much of this text is redacted from the other two articles. I left out pictures, data, and links to PubMed to emphasize the main points.
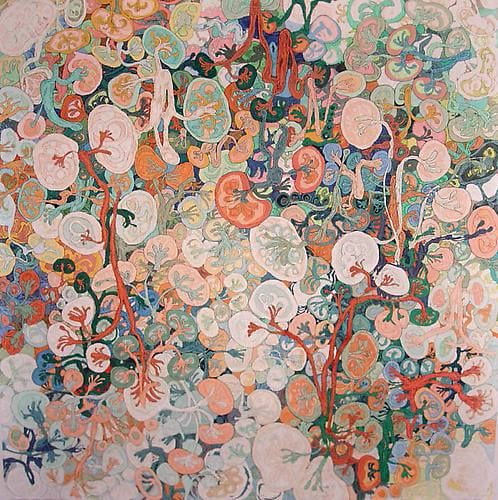
The featured painting is by You Si 游思 (b. 1954), based in Shanghai, China. He is the son of two artists who lived through the cultural revolution and paints in new ways. I think his work is gorgeous but could not find a serious biography or critical study, or any museums that show his work.
What Filtration Is
Our two kidneys are each made up of about one million nephron units. A nephron is a complete and complex structure that begins its function by filtering from blood plasma a clear solution of water and small molecules. That filtrate enters the long loopy tubule of the nephron that reabsorbs a vast fraction of water and salts back into the blood leaving behind only that destined for export out of the body.
The glomerulus, a tuft of capillaries nestled in a tiny cup that drains into its tubule, performs this filtration. So we name it glomerular filtration rate, or GFR.
Blood flow and pressure from the heart drive filtration, but kidneys can regulate its rate. The cells that line the tubules regulate what fractions of innumerable individual salts and small molecules are taken back or let go into the urine.
Filtration Keeps Us Alive
Filtration rids the blood plasma of metabolic wastes, like oxalate, and permits us to excrete the extra water, salt, and all other materials we might eat or drink every day. Without filtration we need dialysis or transplantation to continue living. So this kidney function stands above all the others. When physicians speak of kidney function, they mean, and measure, filtration.
Filtration and Kidney Stones
Kidneys filter copious volumes of water and small molecules – like calcium, oxalate, citrate, phosphate, uric acid, sodium – hundreds of distinct materials. They then return most of this flood – 100 to 200 liters a day of water alone – back into the blood keeping behind only what they destine for export as urine.
Because kidneys filter such vast amounts, very subtle variations in what they take back into blood can load the urine with stone forming salts like calcium and oxalate, and cause stones. In other words, stones arise in significant measure because of subtle imbalances between filtration and reabsorption of key materials like calcium, oxalate, citrate, and water itself.
The filtering system, though powerful, is delicate. Through obstruction, infection, loss of one kidney, or surgical trauma stones can injure it. Such injuries reduce the ability of kidneys to protect the body, and when severe can lead to chronic kidney disease and even need for dialysis or transplantation.
How We Measure Glomerular Filtration
Serum Creatinine
Muscles make creatinine steadily and send it into the blood. Like almost all small molecules, kidneys filter it. Serum creatinine therefore reflects the balance between muscle production and filtration. When filtration falls serum creatinine rises. It is like your golf score – bad day, higher score. Serum creatinine gauges filtration adequately enough for clinical practice. But because kidneys not only filter creatinine but also secrete it from blood into urine, creatinine overestimates true filtration.
eGFR
To get a better estimate, scientists compared serum creatinine to true GFR in reasonably large populations and calculated the best fit between them using regression techniques. The resulting regression equation gives estimated GFR, or eGFR, from serum creatinine, age, sex, and race. This highly derived index dominates medical practice. When physicians speak of reduced kidney function they mean reduced eGFR.
Kidney Function in Stone Formers
Average Function is modestly reduced
Our Own Patients
In our own patients, we found that stone formers have lower kidney function than normal people. The common idiopathic calcium stone formers are just slightly low. Likewise for those with primary hyperparathyroidism. But kidney function is reduced by about 20% in people who make stones because of bowel disease or diseases like renal tubular acidosis or cystinuria. Uric acid and struvite stone formers have even greater reductions.
US Health Surveys
The national NHANES data survey results showed modestly reduced kidney function in overweight people who had a history of stones. Women who formed stones had increased risk for serious chronic kidney disease, and even dialysis.
Olmsted County
This community uses Mayo Clinic for care so records are very complete. A history of kidney stones increased risk of CKD and eventual dialysis.
Large Reviews
Two extensive reviews of all published studies – not just the few I mentioned – concluded that where ever looked for, stone forming raised risk of high blood pressure, serious chronic kidney disease, and even dialysis.
Though Increased, Kidney Disease Rates are Not High
Stones raise the risk of serious kidney disease from the very low levels in the general population to higher though still low levels. The vast majority of stone formers do well and never have problems that require special kidney care. Only rarely do stone formers need dialysis. But they can come to need such care more frequently than people who never formed a stone.
The message is obvious. Stone recurrence should be minimized through prevention efforts. Physicians who practice stone prevention need to measure eGFR appropriately, and if it begins to fall take proper steps to mitigate the causes of that fall.
Obstruction from stones always needs prompt, skilled, urological care that minimizes risk and trauma from surgery. Because silent obstruction can destroy a kidney, any symptoms that suggest new stone passage deserve urological attention.
High Blood Pressure
The NHANES and Olmsted County data show that a history of stones raises risk of elevated blood pressure. Loss of kidney function, even subtle, could raise blood pressure, and increased blood pressure can harm kidneys and reduce GFR. Unlike significant kidney disease, high blood pressure is easily treated to prevent strokes, heart disease, and kidney failure. But high blood pressure commonly escapes diagnosis and adequate treatment.
This means kidney stone prevention clinics are high blood pressure clinics, or at least a common place where high blood pressure can be first detected. All stone formers need to know their blood pressure and seek care if it is elevated.
Bottom Line
Stones are a painful and recurrent chronic disease that kidneys generally tolerate with at most a modest amount of injury and function loss. But compared to people without stones, those who make them have measurably increased risk of high blood pressure and loss of kidney function. Years of study have made clear that this disease demands attentive treatments aimed at prevention, and that surgeons who manage stones do everything possible to preserve kidney tissue.

My daughter has had trouble with filtration since she was young. She’s 24 and has had many stones and stents. Her Dr prolonged her getting one stone removed and I fear this has done damage. Now she has more stones now causing Low kidney functioning and alot of blood in her urine and it’s Friday. They put off helping her. She was told to go to the ER if she sees blood. No call back from urology. Please advise. She’s not feeling well at all
Hi Heidi, It sounds like your daughter has lost some kidney function because of obstruction from stones. That is unfortunate. Protecting her kidneys against obstruction is a main role for her urological surgeons, and if they are having difficulties in doing this they might want to help her find additional help at a kidney stone center – usually in medical school hospitals. It soulds like that may be the case, and that additional consultation is important. Regards, Fred Coe
How common is it for a person’s kidney to completely fail from a large kidney stone? My sister has very severe MS and lost most of her feeling from her waste down, so last year her urologist diagnosed her with a large kidney stone. Since she could not feel it, the Urologist was fine with letting it be. So now we fast forward to this year, and her kidney has lost 100% of its functioning, she’s been in and out of the hospital with infections, near death, and they are just now deciding to take out that kidney completely since all function is gone. She is only 41 and living in a nursing home. Her quality of life is so low anyway. We are just so upset about this. I don’t understand why a urologist would let a person with neurological problems continue on with such a large stone to the point they lose a kidney.
Dear Joni, I am afraid it is not rare. Large stones obstruct the kidney and obstruction can destroy that kidney. I imagine her physicians felt the surgery was excessive given her general state, but a common outcome is sepsis from the obstructed kidney as I imagine happened here. At this stage removal is more or less necessary. Stones in her remaining kidney need care, because it will be her sole renal support. Regards, Fred Coe
I have a question. I have had chronic stones since I was 21, for the past 30 years. I currently have them bilaterally, and am passing one on the left which has a uretal stricture, and a larger stone of 4mm on the right. My GFR dropped from 87 to 51 in early August and has stayed no higher than 58. I am achy, itchy, hurting, and wondering if the GFR drop is part of the reason. Should I be concerned about a further drop? I have systemic lupus as well. Thank you!
Hi Martha, The lower GFR could cause symptoms – and I presume the fall is from obstruction. Your Lupus is another serious cause of GFR reduction and I presume your physicians are carefully monitoring that aspect of your problem. I presume your physicians are also monitoring for obstruction on either side, and it is very important that obstruction not be left for very long. Perhaps that left stone needs to be removed so the kidney can drain better. Regards, Fred Coe
Can kidney stone affect egfr?
Hi Sonny, Indeed, and in many ways. OBstruction is the obvious one.But just being a stone former increases risk of high blood pressure, kidney disease, and – in women – preclampsia. egfr is a crude calculation of glomerular filtration and a fall reflects these effects of stone forming. REgards, Fred Coe
I faced lithotripsy in 1995 PCNL in 2009 and now larg staghorne stone 3cm with multipls GFR 9.5%.
Is it because of stone? Should I go for nephroctomy ? Right kidney is functioning 50%
Hi Anil, I gather the kidney with the staghorn stone has 9.5% of function. The judgment about removal of the stone vs. kidney requires an assessment of the radiographic images – is there functioning kidney but obstruction is impairing function, or is there just little remaining kidney tissue. Your surgeon makes that judgment. Regards, Fred Coe
Hello. I do have kidney stones and had surgery to blast them away several years ago. The stone was fragmented and not fully destroyed. I was not happy about the outcome. 4 years later I got Basic Metabolic panel and eGFR 60. I am 43 and waiting for a follow up at the end of the month. Should I be worried and if I remove any kidney stones will that improve my kidney function?
Hi Kristina, GFR will increase to the extent that it is being lowered by an obstructing stone. That it is so low means that both kidneys are involved, as obstructing only one kidney with the other one normal, gfr would be 80% or more of normal. So obstruction is the big worry and your urologist needs to minimize the length of the obstructed interval. Regards, Fred Coe
After stent installed for kidney stone..gfr is 60. Will it improve. Done after stone stuck at ureter.
Hi Uthamanan, Obstruction reduces kidney function, and the other kidney has to do much of the work for the body. I would hope that stent removal reverses obstruction so kidney function returns. Regards, Fred Coe
Hi, 22 female here. I went to the ER early September from excruciating pain that I found out to be a kidney stone. Was told it was in a good place and 1-2mm and should pass soon. At the time my gfr was ‘normal’ somewhere above 60 the one clinic didn’t report the exact number just an above or below percent. Had another flair of pain the following day and nothing more. Until recently/a month later I had more flares of pain. Another CT showed I still had the kidney stone(or a second one of the same size in the same place) but my blood test showed my gfr was at 46(different hospital). Can the kidney stone alone cause my gfr to drop that much that quickly, and after having it removed will my gfr return to normal?
Hi Avi, I am concerned that a stone has passed into the ureter and is obstructing a kidney. The CT should have shown this, but perhaps it was overlooked. That is the only reasonable cause of falling eGFR given what you have told me. I gather there are two stones in play, one that was passing and another ‘in the same place’ but I cannot tell what place that place is. Anyway, all my suspicions fall on possible obstruction and I would hope if any is present it is remediated with dispatch. Regards, Fred Coe
I am 59 and my kidney function (GFR) has been fluctuating between 48-60 over several years. An ultrasound of my kidneys a few years ago showed small stones, but I have never had any pain. Could these stones be effecting my GFR? My doctor says my results indicate I’m dehydrated, but I drink a lot of fluid and my urine is always very light colored.
Hi Lori, If they are small and not obstructing the outflow of the kidneys they should not themselves reduce kidney function. But stone formers often have reduced kidney function. Sometimes is it damage from prior surgery or shock wave treatments, sometimes from prior stone obstruction that has injured the kidneys, sometimes because blood pressure is too high – stone patients have elevated BP commonly. Uric acid stone formers often have diabetes or vascular disease that affects the kidneys. Fluids will not alter filtration. Your physicians need to figure out what is lowering your kidney function. Regards, Fred Coe
I found this thread as I was looking for whether there is a connection between GFR levels and having had kidney stones some years ago. If someone has had kidney stones, would you expect GFR to remain high? If so, would that indicate the kidneys are stressed? Thanks
Hi Dan, Stone formers are at higher risk for kidney disease with reduced GFR. If the GFR remains high that is fine. Not everyone forms stones, not everyone who forms stones develops kidney disease. Regards, Fred Coe
Recently found out I have a 6mm kidney stone, and today that my BUN and BUN Creatinine is high, is this from the stone, most likely?
Thank you,
Michele
Hi Michele, A stone on one side should not raise BUN or creatinine very much as the other kidney takes up the slack. Lets presume things become normal when the stone has passed. Regards, Fred Coe
I’m a 69 year old male with ulcerative colitis. You mention bowel disease as a possible cause of renal deterioration, and I’m hoping you can expand on that. In addition, I’ve been taking a fairly high dose of mesalamine for over 5 years and am now seeing my BUN level increase, so I don’t know if this increase is connected with my age, my UC or my ASA-5 use (or, possibly with some recent side pain which I guessmight be a stone).
Thanks for your thoughts on this.
Hi Walter, Shrewd guess. Mesalamine can cause progressive kidney disease, and you are wise to discuss this with your physicians so they can decide about the benefits and risks of stopping it. Here is a good reference for them and for you. OF course UC can itself be associated with kidney damage, which is why it is your personal physicians who need to sort things out. Regards, Fred Coe
Hi, my husband is in the hospital for the 4th time in less than 2 years with large kidney stone blockage. This time, it’s in both kidneys. They put 2 stents in and plan to laser the stones in 2 weeks, because currently his BUN is 72.0 mg and Creatinine level is 5.4. His potassium levels are also high, 5.6. They will not do surgery for stone removal while his kidneys are under such stress. They gave him insulin (he is not diabetic) because he does have heart issues. I don’t know why he keeps getting these attacks every 4 to 6 months. I reviewed his medications that he started taking 3 yrs ago, and I’m wondering if prilosec could be causing them? It’s the only drug whose timeline fits when this all began. Thank you for any help!
Hi Helen, I wonder if the stones are uric acid. This would fit with his situation. If so they are easily prevented. Right now he has kidney insufficiency from the obstruction. The Prilosec is not an established cause of kidney stones. I hope his surgeons can restore proper drainage, and be sure about what kind of stones these are. Regards, Fred Coe
I’m 62, lately GFR was 58. I am chronically dehydrated due to IBS watery stools and diarrhea about 80% of my BMs. Recent history of passing stones (last one one week prior to GFR results), with some blood prior to passing. Also, last five weeks training for half marathon and cross training 6 days per week, lots of sweating. Do any, or all, if these factors drop my GFR?
Thanks
Hi Mark, You seem a setup for uric acid or calcium oxalate monohydrate stones. Hydration is so crucial- have you considered sport drinks that contain replacement electrolytes?? The eGFR is an inexact estimate. Perhaps you should have blood drawn away from marathon training – at a time you are less dehydrated – and see if it is higher. Indeed dehydration lowers GFR as part of the physiology to conserve sodium. Altogether, given your history and stones and reduced GFR I would change things, but how to do this depends on the serum and 24 hour urine results, which are very important for you. Regards, Fred Coe
hi.i had multiple stones in my left kidney since 2019 but not treated. last month i had a severe pain and went to hospital. after ultrasound check they found that i had a stone between 1,4-2,0 mm big and because of stone blockage grade 2 hydronephrosis. before the operation gfr was 45. then i had my stone removed with rirs and they planted double j stent. 3 days after surgery i went to the hospital again with severe pain. they said that stent migrated to bladder because of the stone. doctor broke the stone in two piece and one is still in my kidney and pushed the stent down. son i had another surgery. my gfr raised to 60 14 days after surgery. in my 24 hour urine test ptoein level is 850mg/dqy amd microalbuminia is 430mg/day with mic. erythrocyte 296 and leukocyte is +2 mic.leukocyte 20 . they will tqke out the stent next week. do you think does this rirs procedure made any harm to my kidney? and is protinuria because of surgery or lost of kidney function.
Hi resat, The blood in the urine is what causes the high protein and albumin – have it checked when there is not blood. Of course improving drainage of one kidney increased overall kidney function but you have had some real trouble and prevention is urgent. Here is a good starting article. Regards, Fred Coe
I am 42 and found out I have a 6×5 stone obstructing my ureter through an ED visit. My creatinine was 1.34 and my eGFR was 49. I have no prior Hx of kidney issues. They placed me on Flomax, which I am to take for a month and if the stone hasn’t passed I will have a procedure. My concern is with having the obstruction and decreased function for so long. Is this normal practice? Is it likely my function will return to normal?
Hi Steph, I share your concern and have written about the topic on this site. I found that evidence as it is supports 2 – 3 weeks at the outermost for waiting, and frankly I think 2 weeks is more than long enough. AUA guidelines are far more generous, and urologists are absolutely right to follow them until and if they change. I have not published my work in peer reviewed journals as yet because it is only a review of published researches, but they all seem to say the same thing – don’t wait overlong as kidneys might incur damage. I emphasize that AUA guidelines are the US authority and I am not a surgeon. So I am speaking ex cathedra. Warm regards, Fred Coe
Hi! I am 23 years old, I am from Colombia (English not so good), last year I had an eGFR of 88, this year I have it at 62, which is why I went to a nephrologist, and he sent me multiple medical exams, including an ultrasound of the urinary tract where they reported multiple microcalculi in both renal calyx with bilateral ectasia of the renal sinus. I had a normal urinalysis, and reduced kidney function. I do not have high blood pressure, diabetes, or any symptoms. I am an athlete and I am in good health. My concern is whether these stones may be the cause of the kidney damage and whether it may continue to progress. What measures should I take?
Hi Juan Felipe, Stones in general reduce kidney function by obstructing the flow of urine. The US does not seem to suggest that but perhaps your physicians might want to consider a dynamic renal scan to assess the function of each kidney separately and also as a sensitive test for obstruction. Possibly you have a disease in which stones are associated with problems with kidney function. These are uncommon, and I do not have enough information to comment. Regards, Fred Coe
I am a 68 yo woman with no history of hypertension, diabetes, or kidney disease. 2 months ago my doctor got labs because I was suddenly losing my hair, and in addition to finding hypothyroidism my serum creatinine was elevated at 1.31. Because my FBS and lipid profile were a little high, and I didn’t know if there might be an autoimmune component to my hypothyroidism, I embarked on a serious dietary change and increased my fluid intake in case I was dehydrated. Because I’ve had chronic GI issues with severe constipation, leaky gut, reflux, and possible SIBO, I decided to limit grains, lectins, gluten, dairy, carbs and started adding numerous supplements, etc. I had follow-up labs 2 weeks ago and my creatinine was now 1.55 and BUN 30. I have been trying ever since to get an appointment with a nephrologist ASAP, concerned I might have some kind of acute kidney injury, but am not able to see one until 8/8/22. I do have a history of gross hematuria quite a few years ago, and was found to have multiple stones on imagining, but I have never passed a stone. I was never advised about diet or stone prevention and pretty much forgot about it. From my recent research I’m thinking I caused myself to have hyperoxalosis/hyperoxaluria from a leaky gut combined with excessive dietary oxalates (esp. tons of almonds and nuts) aggravated by supplements (such as high dose vitamin C). My main concern is whether there is an acute process going on that might be aggravated by having to wait 2 more weeks for an evaluation. I really have no symptoms, (except bouts of froth in my urine), and my temp and BP is fine. Have you seen acute/chronic oxalate poisoning from diet/supplements, or is something else more likely? Is it OK to wait 2 more weeks? Thanks so much.
Hi Geri, My first concern would be a stone causing painless obstruction. High urine oxalate with kidney problems is possible but a lot more tenuous. I think an ultrasound or CT to rule our obstruction is very important. Perhaps your regular physician might want to consider this. Regards, Fred Coe
Fredric Coe, MD,
Hi, I just found your site, I left a comment for Geri snoke, I am in the middle of trying to move, but i want to start sharing ideas on your site, DR, Fredric I you seem to speak the truth, I am looking forward to getting to share ideas on here.
Thankx Martin
Fredric L Coe, MD, I want to say thankx for taking time out of your life and sharing your knowledge with us, as I said with the other comments I just found your site, I did a quick search about you, (YOU SIR) are a very impressive nephrologist / man@ 86!!
I hope you will keep responding and sharing your knowledge with us? tomorrow I am going to see if you have a YouTube channel, if you do, I am going to subscribe to you.
Thank you so much for your response. I absolutely concur that an US or CT is needed, and hope/assume the nephrologist will order one tomorrow. I guess I thought obstruction from a stone was less likely because it would have to be bilateral in order to cause the noted kidney damage (increase BUN, creatinine), and I didn’t seem to have pain or fever or decreased urine output etc. If it might be obstruction, an acute process, I’m clueless why the wait, when things could go south so quickly at any moment? But I’m just a scared patient. What do I know?! I will never take my kidneys for granted again.
Hi Geri Snoke,
I just found this site and read your comment, WOW, I have just experienced similar test results as you, I feel/believe that eating foods high in oxalates for so many years is the cause too,
I am getting ready to start eating a almost 100% oxalate free life style, and no fruits, no veg’s, fruits and veg’s always hurt my kidneys, and make my urine test strips test for high creatinine and albumin, I believe from the high citric acids/malic acids and other acids in all of them fruits break my kidneys down, basically I guess I’m getting ready to start eating like a carnivore way, my body needs a little carbs though,
I have a lot more to talk about if your interested in sharing each others diets? I ask you reply back or email me? Deathicu@gmail.com Thankx
Hi Martin, I answered her by pointing out that obstruction from one of her stones is far likelier to have reduced kidney function than diet induced increase of urine oxalate. In fact, the latter is almost never a cause of reduced kidney function. In your case I am not clear what may be the reason to avoid oxalate in foods, as you do not mention stones but rather albumin in the urine. The latter is not related to food oxalate per se. Regards, Fred Coe
Hi Dr. Coe. This is in follow-up to my previous post. I am still in process of work-up. There is no significant protein in my urine, and US showed stones bilaterally but none obstructing or causing hydronephrosis. I guess my kidneys were a little small in size (?atrophy). I just sent in 48 hour urine samples (Day 1 – 4.2 L, and Day 2 – 3.7 L, though I’m pushing fluids). My question today is about Miralax or polyethylene glycol which my doctor wanted me to take for severe constipation (no BM in 3 weeks), but I have read it can be metabolized to oxalates and/or hydrolyzed into or contaminated by ethylene glycol (anti-freeze) which is a known serious kidney toxin and even the package label on the bottle of Miralax says it should not be used if kidney disease, but my nephrologist said it would be safe. I have found lots on-line to the contrary. I was hooked on Miralax, taking it daily for many months several years ago, and even wonder if it might have contributed to my CKD stage 3 that was only recently discovered. From my research, oxalate nephropathy still seems the most likely culprit. I am not allowed to take any magnesium, ginger, Fleet’s enema or other supplements which might help with the constipation. Any thoughts about the potential kidney toxicity of Miralax (polyethylene glycol)?
Hi Geri, On PubMed using the search term Miralax AND oxalate I found only one rather trivial result – a large compendium of chemical terms. So I do not have reason to believe this laxative raises urine oxalate. I see where Mayo clinic is organizing a trial to determine if this occurs. . A case report of oxalate kidney damage associates it with high intake of leafy green veggies but did not include urine oxalate levels. I think it most likely this patient had a form of primary hyperoxaluria. However, laxatives can cause ammonium acid urate stones, or calcium oxalate stones because of low urine volume. The 24 hour urine testing is crucial here and one should do it while taking the PEG and afterwards as well to isolate what is from the laxative and what is inherent in you. Regards, Fred Coe
Thanks for your response Dr. Coe. I remain skeptical about Miralax being safe, esp. in patients with CKD and oxalate issues. I would never use PEG to get pre- and post urine testing because the risk wouldn’t be worth it. I used Google for my search and found:
1 – “Unusual presentation of oxalate nephropathy causing acute kidney injury – A case report”, due to Miralax used for constipation – in HSPI – Journal of Clinical Nephrology, publ. Nov. 4, 2020, by Anas Diab et al, from Nephrology Dept. WV Medical School
2 – FDA study showing ALL samples of MIralax (polyethylene glycol) tested to contain trace amounts of ethylene glycol (used in the production process), a well known kidney toxin (antifreeze). Also, polyethylene glycol can be hydrolyzed to ethylene glycol in the body (perhaps by gram neg. bacteria), and patients with leaky gut and dysbiosis or other GI issues may be susceptible to increased absorption of EG and/or PEG.
3 – There are several lawsuits, including class action lawsuit, in connection with doctor prescribed Miralax resulting in acute kidney injury, some permanent.
4 – Numerous articles documenting oxalate nephropathy/AKI from dietary oxalates and vitamin C use.
5 – Under pressure, the FDA authorized an adverse event reporting site for Miralax, with thousands of reports submitted already – many from parents whose children were harmed by Miralax. (It has even been suggested that Miralax may be the new Vioxx, with adverse events initially denied resulting in much health damage prior to finally being recalled.
I do not know why any CKD patient would ever risk using Miralax (PEG). Why does the Miralax package label itself WARN about NOT using it if kidney disease? (It doesn’t just say don’t use “only if low urine volume” – They must know something!) I am still waiting on my 48 hour urine results, but my creatinine levels have been slowly improving, suggesting reversible AKI (superimposed on some level of CKD), and I don’t know what else would be responsible apart from my very high oxalate diet compounded by high dose oral Vitamin C, and other supplements I mistakenly thought were general or thyroid or gut health promoting – (antioxidants like green tea extract, guggal, ginger, turmeric, vitamins D, A, E, K, polyphenols, collagen, glutamine, cinnamon, etc.), that I have ceased using. What else causes reversible AKI without specific treatment, (like stone removal) ? ???
Hi Geri, Thank you for the informative details about Miralax. As for diet oxalate and excessive vitamin C (that does produce oxalate) no one has doubts. About Miralax, I do not know of data showing increased urine oxalate, but perhaps some group should look. I have encountered patients with chronic diarrhea from over use of Miralax and consequent stones as a result of the fluid and alkali loss, but I could not directly implicate the medication. Using the search term “miralax long term” I found 22 articles on PubMed of which this is a serious metanalyses. I found no serious side effects reported, nor did I see them in the other titles, but I did not read the other papers. Regards, Fred Coe
Hi Dr. Coe. Thank you for your most recent response (9/15/22). I read the meta analysis you referenced. There were NO details of ADVERSE EVENTS of PEG, NONE, only comparisons of EFFICACY. What does GI benefit matter if the COST is possible AKI/CKD? Did you have a chance to look up the case report I mentioned in the Journal of Clinical Nephrology? Is there not any validity to it? Is it true that ethylene glycol (antifreeze) is used in the manufacturing of PEG? What about the FDA finding SOME amount of ethylene glycol in ALL Miralax/PEG samples tested? What amount of ethylene glycol is safe? Is there a study somewhere documenting safe limits? Do the pharmaceutical companies or FDA have any ONGOING monitoring, or minimum allowable amounts of ethylene glycol, in these widely sold over-the-counter PEG products? WHY does the package insert/label IN the Miralax product itself say to NOT take it if you have kidney disease? WHAT risk are they referring to? Where is a thorough Miralax/PEG SAFETY study documented? Is there a detailed pharmacology analysis of how PEG is metabolized in the body (i.e Does any of it metabolize to ethylene glycol, or to oxalates? How much?) Where can the consumer find all this information? Thanks again for the dialogue and your expert opinion. I really appreciate it, and just am trying to find out what is safe and what isn’t.
Hi Geri, I admire your excellent reference tracking, and made a note to myself to take on an article about the matter for this site. It will take some time and energy but you have convinced me to do it. Will you privately send me your references? I will do my own but perhaps some areas, like pending lawsuits would not be my common choice. I will acknowledge your contributions in the article, if you so wish. (coe@uchicago.edu). Regards, Fred Coe
So, I had a high urine calcium at 320, high urine oxalic acid at 80.
2 wks later, I had a repeat of JUST the urine calcium, and it was exceptionally normal. They may do a repeat of urine Oxalate. Is this necessary?
Also, my Oxalate serum is normal, and eGFR is 100. Urea is at 7, borderline low / normal. I am unable to see a nephrologist until December. Basically, I just want to know if I should be concerned?
Hi Donna, I would suggest the testing is a problem, and recommend your physician use a national vendor for kidney stone testing. Litholink is the best, by far. I recommend it and say I have no financial involvement with its owner – LabCorp. If you urine LL, you get reliable calcium and oxalate and all the rest and you should not such wildly varying values. Serum oxalate is not available clinically and difficult to measure in a research lab, so I doubt your physicians ordered it. As for measurements, if you are a stone former one wants measurements in at least duplicate and expects the duplicates to match more or less. Regards, Fred Coe
I am 62 years old. I changed my diet when I realized I was turning prediabetic. I started eating raw spinach, honey peanuts and grape juice.
Hi A Woub, You certainly have turned to high oxalate foods. I hope you have not become a stone former. I would suggest your physicians offer you some diet counseling as you can do better for diabetes control with less stone risk. Regards, Fred Coe
My 54 year old partner was diagnosed two days ago with a 3mm stone in one ureter. His GFR was 68. He was discharged overnight and went back yesterday morning for a blood test that showed GFR of 35. He’s on a drip pending a further blood test. How is his GFR so low if only one ureter is obstructed? (He is on high blood pressure meds and has regular blood tests and there has never been an issue with GFR before)
Hi Naomi, there exist multiple reasons – unsure which is true: His opposite kidney is obstructed; his opposite kidney is not functioning well so the obstructed kidney was always contributing more than half of his total kidney function; the stone obstruction event has led to some systemic issues (sepsis, low blood pressure) that damaged his other kidney. His physicians no doubt will sort this out. I cannot do that from here. Best, Fred Coe
Hi Dr Coe, I do work in the science field and recently got into the world of kidney stone. I find very amazing all the time you put to connect with your readers, to help the patient community. I think it is really great! I have learnt so much by going through your website, but I have a question concerning preclinical testing. Do you think we have appropriate preclinical models that mimic some mechanisms found in stone formers?
Hi Evy, Stones seem to me the cross between genetic traits and diet + lifestyle (hydration). The traits that predispose are mostly _ I think – heterozygotic and related to calcium balance, citrate, urine pH and perhaps oxalate. If by preclinical models you mean animals, we have quite a few but these are incomplete – usually one trait, like calcium or urine pH regulation. Regards, Fred