Thiazide Type Diuretics Reduce Stone Formation
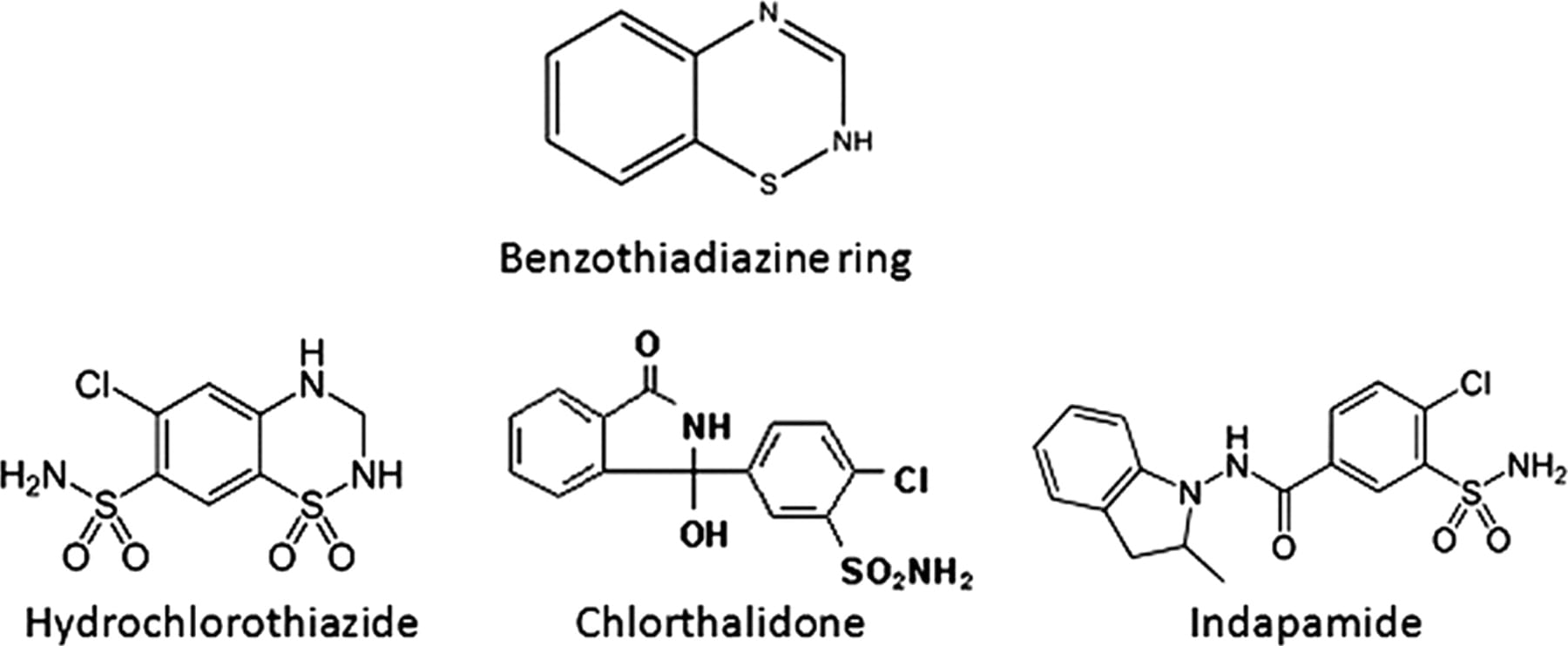
The common thiazide type drugs in use today are hydrochlorothiazide, chlorthalidone, and indapamide. All three have been used in stone prevention trials and shown to have beneficial effects. A nice recent review is also the source for the drug structures pictured above.
I have obtained and studied nine trials. In all nine trials, there was a comparison – untreated – group. This spreadsheet contains links to the trial documents, but you will find it not easy to obtain the original publications unless you have access to a university library system. For this reason I have copied out the key data. Briefly, there were 330 controls, of which 149 relapsed (45%), and 314 treated subjects of whom 72 relapsed (23%), a savings of about half (23%/45%). That is the bottom line for this class of drugs.
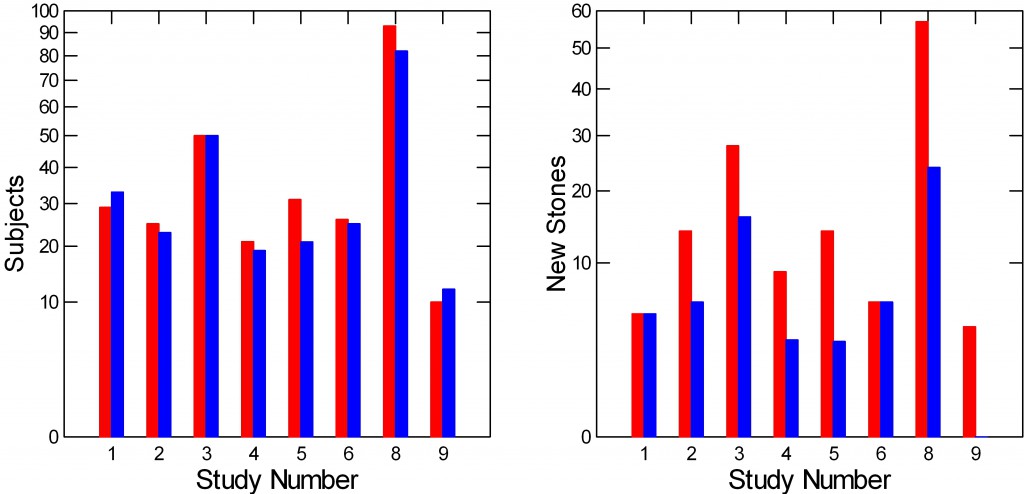
Here is a picture of the 9 studies. For each study the left panel has a bar whose height is how many control – red, and treated – blue subjects it had. The right panel shows how many of the red and blue people made new stones.
It is obvious that there were no differences in new stones between control and treated people (right panel) in studies 1 and 6. These were both brief (see the spreadsheet). In the others, the treated – blue bars – were lower than the red controls. Trial 9 had no relapses in the treated group. (Trial 5 has two drug doses and one control group so the height of the blue bar for 5 on the left panel is the average of the number of subjects in the two dose groups).
By now many of you will want some statistics. The spreadsheet depicts 9 studies each with numbers of treated and untreated people who did and did not relapse. Using ANOVA in which the numbers who relapsed is dependent, treatment or not is a categorical variable, and numbers of total subjects is a covariate, the mean number of relapse subjects adjusted for number of subjects was 16.1 in the control group and 8.3 in the treated group (p=0.008).
A simple X2 test using the four numbers from the bottom line of the spreadsheet: Treated, 72 relapse 242 no relapse; untreated 149 relapse, 181 no relapse gives a X2 of 35.2, p<0.001 (Yates’ correction is virtually identical for those who care).
I have deliberately included all studies that had a control and treatment group without fussing about the ‘quality’ of the trials. Several expert groups have reviewed these trials and a few more I omitted. Fink and colleagues in 2012 reviewed all available stone treatment trials. The same group did a similar review for the American College of Physicians which I did not think much of because of its codicils that seemed inclined to mediocrity – if not folly in practice. Escribano and colleagues authored an outstanding Cochrane review focused on thiazide.
The experts properly quibble about the intricacies of trial conduct and call for more trials. Personally I think more thiazide trials are of marginal importance and little interest. Mine is the untutored opinion of a bystander who does not perform trials as a profession. But I can count, and no one can tell me that the main fact – the pills reduce stone recurrence – will be overturned by trials of increasing ‘quality’. That is very unlikely. So, why do them?
Thiazide is Not Used Alone
Because they can reduce formation of new calcium stones, thiazide type diuretics are co-equal with potassium citrate as a medication physicians can use for stone prevention. Thiazide works differently from potassium citrate, so the two drugs can be used together with additive effects.
But more to the point, diet and lifestyle changes are crucial for stone prevention and need always put in place before writing a prescription.
The goal is to lower supersaturation. Fluids will do this. So will reduced diet oxalate, or raising urine citrate and, in uric acid stone disease, urine pH. Reduced sodium diet will lower urine calcium, and that will lower calcium salt supersaturations. So fluids and diet come first. Aspects of living that promote dehydration are serious obstacles to prevention, and to learn what they are in a given person and some to ways around them is an art of considerable passion and value.
Trials are all about the effect of a pill, and that is a virtue. But no doctor who practices stone prevention with a mere pill can achieves the joyous satisfaction of an accomplished clinician. So all I want or need from trials is to know the pill can reduce stones – presumably by reducing urine calcium, and thereby feel justified to add it into my instruments of practice, which I had done decades ago.
Why Use Diuretics?
It is Not to Raise Urine Volume
Because of the name one might think the drugs work by increasing urine volume, and therefore prevent stones the way water or other fluids might. That is not the case. Diuretics raise urine volume only transiently. Urine volume is set by how much extra water is available for urine loss. After a short while on any diuretic, the average day’s urine volume will be no different taking a thiazide than it would be not taking it.
They Lower Urine Calcium and Urine pH
How they do this is a matter for some detailed commentary, but let us begin by saying they do indeed. When physiologists comment on how this occurs the correct answer is that they lower the urine calcium by stimulating the kidney tubule cells to reclaim back into the blood a higher than usual fraction of the calcium that the kidneys filter out of the blood in the usual course of their functioning. How they lower urine pH is not well known.
But higher calcium reabsorption, though true, could not lower urine calcium for very long any more than reducing the radius of a bathtub drain can lower the flow of water out of the tub whose faucets are open. If you did that, narrow the drain of such a tub, the water would rise until the greater weight of the water column raised outflow back to match the inflow from the faucets or the tub simply overflowed onto the bathroom floor. The amount of calcium in the urine every day is exactly the amount entering the blood from diet and bone. So thiazides have to somehow alter that inflow – either reduce diet calcium absorption or promote calcium entry into bone. It is mainly the latter they do, so they are not without some potential to maintain bone health.
They Must Lower Calcium Salt Supersaturations on Average
This is an old theme on the site. Reduction of supersaturation will lower formation of stone crystals and eventually stones. Given a random variability of urine volumes, and of other key factors that control supersaturations for calcium oxalate and calcium phosphate – eg. excretions of oxalate, phosphate, citrate, and urine pH, a fall in urine calcium from a drug will inevitably lower supersaturations on average unless that drug systematically raises urine oxalate or phosphate excretions, lowers citrate excretion, or alters pH upwards – calcium phosphate. In fact, thiazides can lower urine citrate, probably in part because they deplete body potassium stores and lower the pH inside kidney cells, but that can be corrected by potassium repletion. Lower pH from thiazide will specifically reduce calcium phosphate supersaturation.
How do Thiazides Affect the Kidneys?
Calcium and Sodium
With a brief blush and downward gaze, I choose our own publication as perhaps not unreasonable as a source. Partly I am guilty of favoritism, partly we are the only group to have studied individual stone formers before and during thiazide treatment in a clinical research setting on a constant diet. We did do this, and the results, if perhaps not exactly arising from a multitude, are secure in their precision and in their depth of insights.
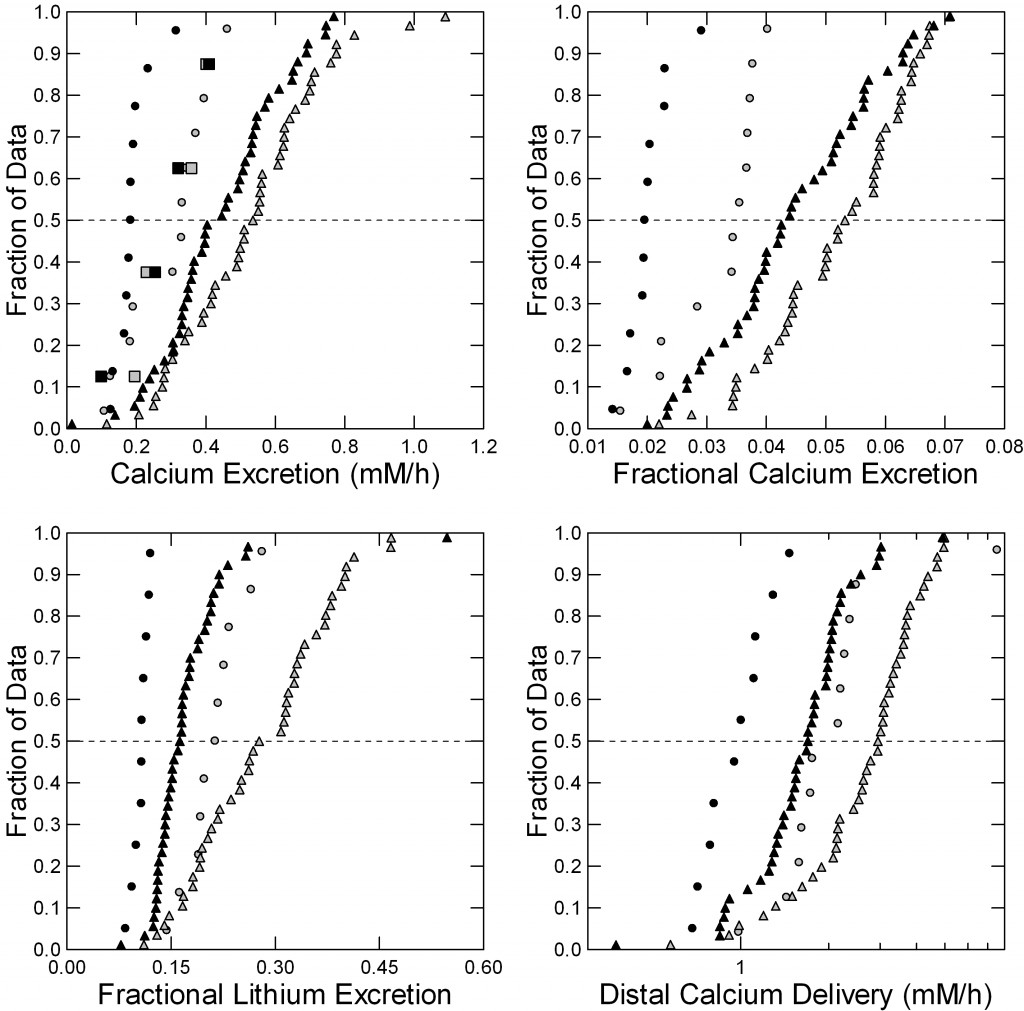 Four men with calcium stones and idiopathic hypercalciuria were studied in our CRC before (gray symbols) and after 6 months (black symbols) of chlorthalidone, 25 mg daily used in treatment for stone prevention.
Four men with calcium stones and idiopathic hypercalciuria were studied in our CRC before (gray symbols) and after 6 months (black symbols) of chlorthalidone, 25 mg daily used in treatment for stone prevention.
We have spoken of filtration and reabsorption elsewhere on this site. The drug had no effects on glomerular filtration, and therefore on the filtration of sodium and calcium. It lowered urine calcium – as expected – but did not change urine sodium excretion.
Fasting (circles) and fed (triangles) but not overnight (squares) the drug lowered urine calcium excretion (Figure to the left, upper left panel) shown here as millimoles/hour. The effect was statistically significant fed because of the large number of observations; fasting it was more marked but we had fewer measurements so formally speaking it was not significant. Overnight there was no change at all.
The fraction of the filtered calcium excreted (upper right panel) represents how the kidney tubule cells alter their reabsorption of filtered calcium – a highly regulated process. Both fasting and fed, that fraction fell markedly with chlorthalidone and both effects were statistically significant. Note that you can make these fractional excretions into percents – multiply by 100 (0.04 = 4%).
Lithium is everywhere, in our water and our food in minute concentrations. It has an odd property. Part of the kidney unit – the nephron -, that part closest to the glomeruli and therefore called the proximal tubule, handles lithium and sodium more or less equally, whereas the latter parts of the nephron do not handle them equally but let most lithium go by into the urine.
This tiny fact lets us sort out where along the nephron thiazides might have their main effects. Fasting and fed, chlorthalidone raised the fraction of filtered lithium reabsorbed in the proximal parts of the nephron so that less went forward into the later parts of the nephron (Lower left panel of the figure).
Here is a fact. Calcium and sodium and reabsorbed along the proximal nephron more or less in parallel. So by knowing the fraction of filtered lithium and therefore the fraction of filtered sodium sent forward, we also know the fraction of filtered calcium (lower right panel), That fraction falls with chlorthalidone. As a result, the early portions of the nephron conserve more calcium with the drug than without, and that is one part of why the urine calcium falls.
My article on idiopathic hypercalciuria is an excellent primer and overview of lithium clearances and proximal vs. distal nephron calcium handling.
Acidity of the Urine
Chlorthalidone, and presumably other thiazide type drugs make urine more acidic. Fasting (upper left panel of figure, circles) the effect is small: Chlorthalidone points (black circles) are just a little to the left – lower pH more acid – than without the drug. But overnight, the four black squares are far to the left meaning the urine is a lot more acidic with the drug. Fed (Upper middle panel) the same.
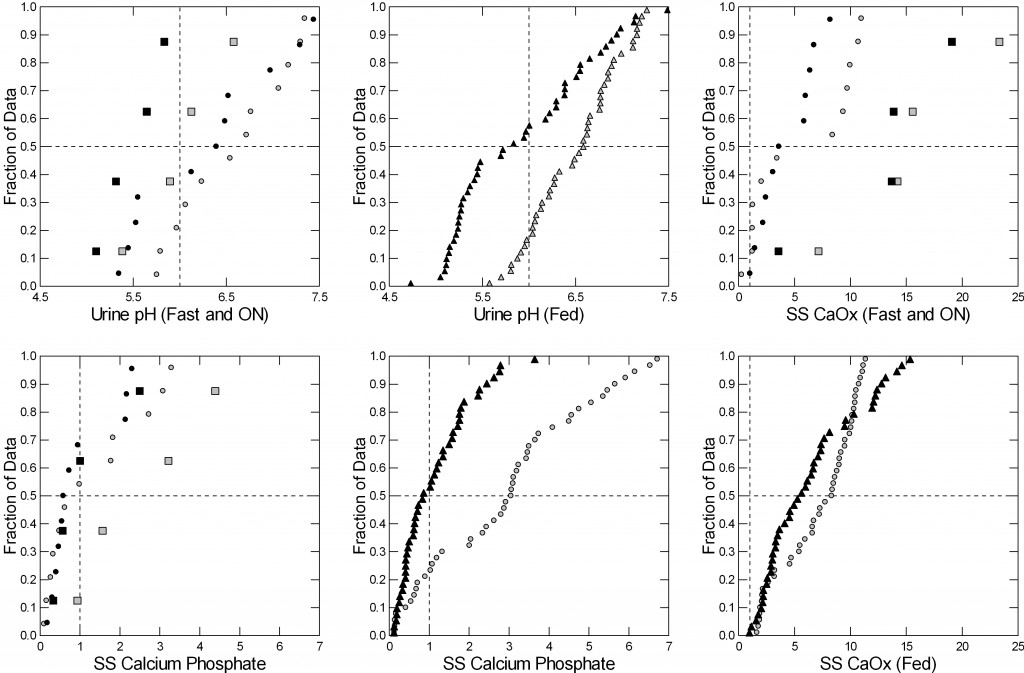 This matters a lot for supersaturation with respect to calcium phosphate, not so much for calcium oxalate. Therefore, although the calcium oxalate supersaturations with and without the drug are barely different (right upper and lower panels) those for calcium phosphate are much lower with the drug (lower left – fasting and overnight and lower middle panel – fed).
This matters a lot for supersaturation with respect to calcium phosphate, not so much for calcium oxalate. Therefore, although the calcium oxalate supersaturations with and without the drug are barely different (right upper and lower panels) those for calcium phosphate are much lower with the drug (lower left – fasting and overnight and lower middle panel – fed).
This makes thiazide type drugs ideal for preventing calcium phosphate type stones and calcium oxalate stones. They can prevent the former because they lower calcium phosphate supersaturation via both reduction of urine calcium excretion and urine pH. Calcium phosphate stones form on plugs of calcium phosphate in kidney tubules or perhaps just in the urine itself, driven by supersaturation.
Calcium oxalate stones are more complex. They form on the surfaces of the renal papillae over deposits of calcium phosphate in the kidney tissue (plaque). A crucial initial step in this process involves the laying down a film of calcium phosphate over plaque. Calcium oxalate then deposits from urine on top of this initial film to make the stone. So thiazide acts in two ways to reduce calcium oxalate stones: by lowering calcium phosphate supersaturation and therefore hampering formation of the calcium phosphate film needed for overgrowth of calcium oxalate on plaque, and by reducing calcium oxalate supersaturation itself.
Note that the nine trials concerned calcium stones, and did not always distinguish between those that did and those that did not contain appreciable percentages of calcium phosphate.
I have not discussed here how thiazide lowers urine pH. That would take us too far afield. The original article points to changes in intestinal uptake of alkali, which seems to be reduced by the drug.
Urine Oxalate
In our paper reviewed above we found no changes in urine oxalate with chlorthalidone, and did not therefore include oxalate data in the tables. In the past we have published a rather large group of patients who were put on thiazide and exhibited no increase whatever in urine oxalate. I do not believe it is likely that thiazide treatment raises urine oxalate.
How Do Thiazides Lower Urine Calcium?
I have said it is not just by acting on the kidneys, for that is to close down the drain – the bathtub will overflow perhaps but you cannot reduce the flow out of the drain for long that way. This is a sometimes overlooked point when people speak about urine calcium losses.
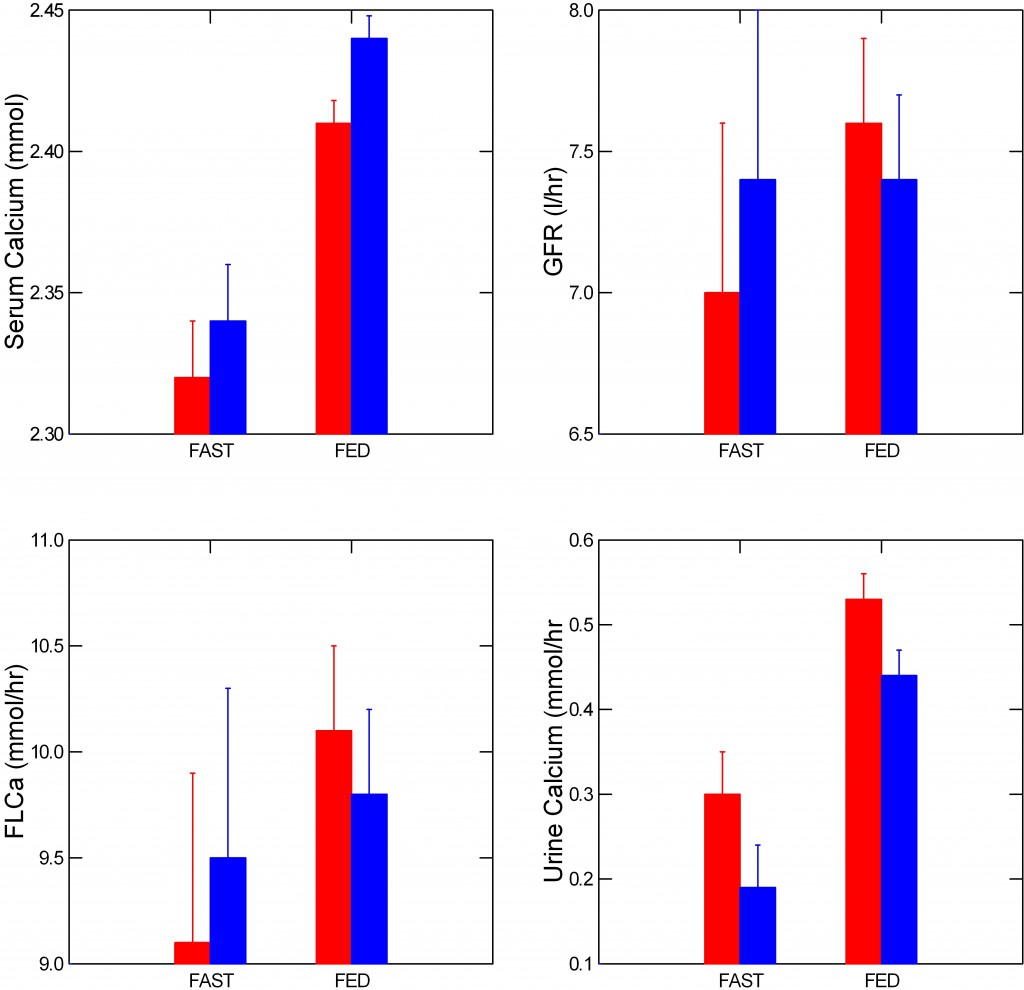 What happened in our patients must have been a fall in absorption of calcium from food, or an increased uptake of calcium into bone, because multiple measurements of serum calcium – the water in the bathtub – were almost unchanged despite a fall in urine calcium.
What happened in our patients must have been a fall in absorption of calcium from food, or an increased uptake of calcium into bone, because multiple measurements of serum calcium – the water in the bathtub – were almost unchanged despite a fall in urine calcium.
But almost is not quite unchanged.
Serum calcium – the upper left panel of the figure, rose significantly with thiazide. The amount of calcium filtered from blood into the kidney tubules (lower left panel) did not change significantly – the error bars overlap -, because filtration itself – (upper right panel) also varied. As I already showed you, urine calcium fell (lower right panel).
So the picture does have in it a bit of the bathtub with a somewhat closed drain – the water level, serum calcium, rose.
Now, I am about to leap into conjecture: Possibly, this increase in serum calcium could promote near instantaneous movement of calcium into bone by sheer physical chemistry.
A body of work that is perhaps more obscure than it should be, edges toward the idea that a portion of bone mineral, brushite in fact, may be in physical chemical equilibrium with blood so that large amounts of calcium can move in and out of bone mineral without any necessary cellular control.
This latter is critical, because bone cell process hours to change in response to hormones whereas urine calcium, as an example, can rise within a few minutes and yet serum calcium remain unchanged or even rise slightly as seen here.
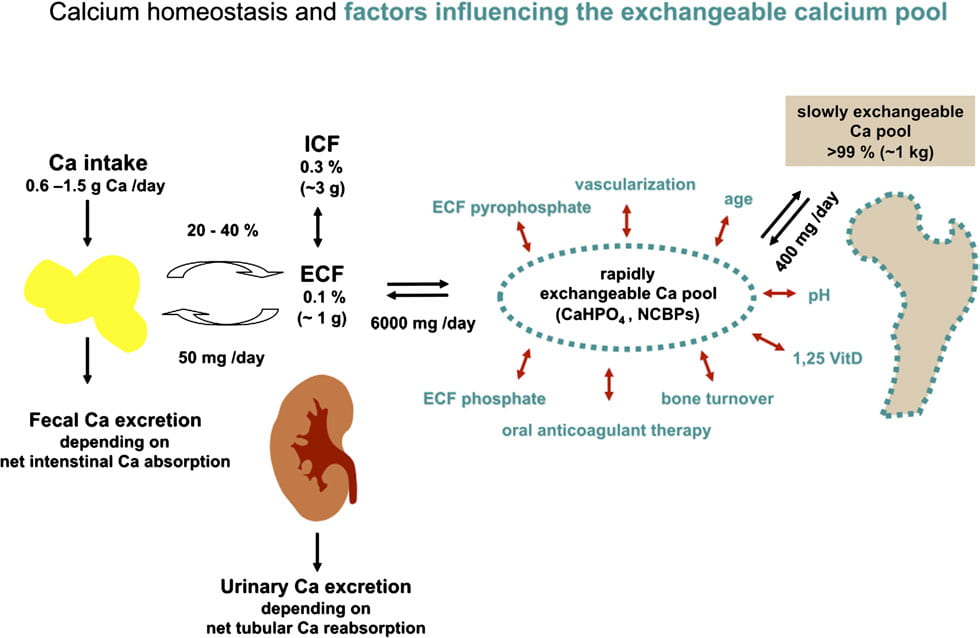
This colorful picture (shown below) is similar to much of what we have often discussed on this site. To the left is diet calcium coming in and leaving, the absorbed calcium entering the ECF or extracellular fluid – we have approximated this as blood. Kidneys can release calcium, as noted.
The big addition is that a large amount of calcium may well be circulating between blood and bone – the 6,000 mg in the middle of the picture. This exchange is affected by serum phosphate, drugs like anticoagulants that alter bone mineral modifiers, and other factors. Of the 6,000 mg of calcium that enter and leave bone every day, only 400 mg go into the slowly exchangeable bone pool which is our familiar hydroxyapatite – the majority of calcium phosphate stones and the principle stiffener of bone.
 What if, when kidney conservation falls – the drain opens – calcium leaves the exchangeable pool so the ‘faucet’ opens. What if, when thiazides raise conservation, the slight rise of serum calcium – from diet inflow perhaps – is just enough to nudge calcium flow into bone?
What if, when kidney conservation falls – the drain opens – calcium leaves the exchangeable pool so the ‘faucet’ opens. What if, when thiazides raise conservation, the slight rise of serum calcium – from diet inflow perhaps – is just enough to nudge calcium flow into bone?
In other words, envision that bathtub. As we eat, the drain opens, the diet ‘tap’ opens, and bone comes into a kind of balancing act: If diet inflow is large enough calcium flows into the exchangeable bone mineral – brushite – pool. If not, calcium flows out. Thiazide clearly tightens the drain, the diet is the same with and without the drug, so possibly diet calcium inflow is raising blood calcium a bit and calcium is moving into bone.
If I were young I would test this idea in humans.
Effect of Thiazide on Bone Mineral Balance
All this raises an obvious question: Do thiazides improve bone health, reduce fractures, increase bone mineral content?
A recent review summarizes a large amount of evidence that they do indeed reduce fractures. The data, from the Danish population, suggest that duration of continuous treatment is more important than dosage in fracture prevention. In particular, fracture risk appeared to increase during the first year of use but then fall progressively. A Cochrane analysis concludes that all evidence to date – 2011 – supported this idea of reduced fractures, albeit there were no prospective controlled trials. Several such trials subsequently confirmed that thiazides maintain or increase bone mineral. Dalbeth and colleagues describe a link between rise of uric acid and bone mineral with thiazide implying a possible causal linkage not otherwise tested.
The overall impression is that one would not win by betting against thiazide as helpful to bone.
By now you might be asking if stone formers are at risk for bone disease. A recent long term followup of nurse and physician cohorts showed an increased risk of wrist but not hip fractures. Our article on idiopathic hypercalciuria summarizes additional information linking it and stone disease to fractures.
How About Salt?
As their prime purpose diuretics cause renal sodium wasting so that for any given intake of sodium the total body sodium stores will be less than without the drug. This is perhaps a main reason why they can reduce urine calcium via increase of proximal tubule calcium retention and also reduce blood pressure.
From this, one might think that low sodium diet might be like thiazide and help with bone mineral balance. In the one really ideal study testing this idea it was correct, and I have summarized that work in another article on this site.
Clinically, reduced salt intake is critical for successful thiazide use. From its basic physiology, high sodium intake will essentially undo the effect of the drug, and raise urine calcium. More, thiazides cause losses of potassium and lower serum potassium, and this is worsened by high salt intakes.
A caution. Thiazides can lower serum sodium levels, especially in older people, and this site advises reduced sodium intake which could increase that risk. In general diagnosis of low serum sodium was made 19 days after initiation of treatment (95% CI 8, 31 days). For this reason physicians invariably monitor serum electrolytes after a few weeks of treatment, and should do so after a few months, and at reasonable intervals, as well.
Is One Drug Better Than Another?
I think so. For example, hydrochlorothiazide has been used 2 times a day in the stone trials, whereas indapamide and chlorthalidone are long acting and needed once a day. People can forget the second dose. It is said that hydrochlorothiazide causes less of a fall in serum potassium but at least in hypertension trials it is less potent so you need more and when more is used it is the same as the other two drugs with respect to potassium, and dosed twice daily.
Dosage
I like to start with lower doses than used in the trials. For chlorthalidone, 12.5 mg (1/2 of a standard 25 mg pill) is enough for most people. For hydrochlorothiazide I like the 12.5 mg pill twice a day – short acting. For indapamide I like 1.25 mg pills. Chlorthalidone and indapamide are long acting so the pill is once a day.
What Have We Learned?
Thiazide drugs can reduce stone recurrence at least in part by reducing urine calcium loss and supersaturation. They act on the kidney but also seem to improve bone mineral balance and reduce fractures. While stone prevention is certainly not accomplished by one pill, thiazide is an important part of what physicians can offer for prevention of stones.


If someone has low blood pressure, is this regimen still recommended? Would one drug be better than another? Should the potassium citrate be started first to help offset its possible side effects?
Hi Linda, People with low blood pressure may not do well with thiazide, and for them I believe – no trials here – a low sodium diet will be best. Thiazides work by depleting the body of sodium, but low sodium diet does this differently from thiazide. I have observed that although low sodium diet will lower blood pressure in people with high blood pressure, it has little or no effect on otherwise normal people with low blood pressure. So I would use low sodium diet to control urine calcium, in your situation. Here is a good approach. Regards, Fred Coe
I will do that. Should the potassium citrate be added to my diet if it’s not “balanced” with the thiazide?
Hi Linda, Potassium citrate is best used when urine citrate is low or when uric acid stones are forming. Otherwise, it is a reasonable but untried remedy. Check your 24 hour urine results and see if your urine citrate is indeed low. Regards, Fred Coe
Thank you. It is not low (991) so I’ll stick to the low-sodium diet and drink gallons of water. Someone suggested drinking water that is higher in alkalinity. Has there been any scientific evidence that it can improve body chemistry?
Thank you. It is not low (991) so I’ll stick to the low-sodium diet and drink gallons of water. Someone suggested drinking water that is higher in alkalinity. Has there been any scientific evidence that it can improve body chemistry?
The PTH value you give is not in familiar units which are typically in the range of 20 – 70; please check again. The water is unlikely to matter because alkaline or not it will have little effects on your body. Regards, Fred Coe
Dr. Coe, if it is the K 24, my last three samples were 44, 80 and 70. I’ve been looking at my diet and have had a rude awakening regarding sodium. It appears to be an area where I can make quick improvements.
Is magnesium citrate (vs. potassium citrate) useful for calcium stones? An M.D. recommended magnesium citrate to me.
Hi David, Potassium citrate is a valid treatment for calcium oxalate stones – it is part of a prevention program. Thiazide – which is the article you read is another valid treatment. But one does not use just a pill. Regards, Fred Coe
Wow, Dr Coe,
I’ve just stumbled upon your site and am blown away by your generosity with your knowledge and experience. I’m a new NP in charge of a tiny rural clinic out west. Minimal mentoring or support from my busy medical supervisor (500 miles away). I plan to read all your site articles, as I imagine most of my many questions are answered there. In the meantime, one question: Have you seen any problems with chlorthalidone causing erectile dysfunction? I have a new patient, robust middle-aged man, treated for years for HTN with 100 mgToprol XL and 25 mg chlorthalidone daily. Has ED and not happy about it. Clueless as to why his previous MD gave those particular meds; no hx of MI. Over the past month I stepped him down on the Toprol and added 20 mg Lisinopril. He showed up happy last week, reporting a decrease in his chronic fatigue, and his BP is down 10 points. I was delighted–and told him to decrease his chlorthalidone to 12.5 mg and we’d check his BP in another month. (plan was to gradually transition him off the Toprol and chlorthalidone and see if he could maintain on just Lisinopril. My research showed that both metoprolol and chlorthalidone were associated with ED). He agrees happily, starts to leave, then with hand on the doorknob mentions that, BTW, he has a hx of kidney stones and he thinks he just passed one last weekend! (Clueless as to what kind of stones, and no one ever told him to collect the stones before.)
From what I’ve read on your site so far, looks like I’d better keep him on 12.5 chlorthalidone, at least for now, reduce his salt intake, and start to sort out his stone history at next visit. But as to ED? Any thoughts on this in terms of chlorthalidone? Any alternatives that work for both ED and stones?
Thanks and Regards,
Peg Nicholson
Hi Peg, Firstly I am just delighted that I can be helpful. For blood pressure an ACE may well be enough; CTD at 12.5 mg will permit control of BP with very low doses of ACE because CTD causes volume contraction which makes BP highly dependent on A2 – which you are blocking with the ACE – so there is synergy. Reduced sodium intake to the current FDA recommendation of 65 mEq (1500 mg) daily will often lower BP so much drugs are not needed, and I always try that first. Home BP are very useful here. My own approach is low sodium diet for 6 weeks with home BP and then perhaps an ACE or ARB (I love Losartan) if needed. The CTD is when low sodium cannot be obtained – but I try hard. Here is where his stones help you because 24 hour urine stone testing gives you 24 hour sodium excretion which reflects the 4 day running average of sodium intake. For me reduced sodium diet is the foundation for everything: Stones, hypertension, and happiness in life. Warm regards, Fred
A very interesting and informative article, thank you.
I have a several year history of primary hyperparathyroidism discovered randomly during a health check. I don’t take any medication and we have decided on a watch and wait regime. Twice in the past 5 years I have had severe back pain, rigors and vomiting which have been diagnosed as renal infections and responded (too?) quickly to trimethoprim. I live in fear of another attack. My GP wondered if it might be a renal calculus and having painlessly passed what felt like a tiny pea two days ago, I suspect she might be right! My question is, is there a link between the PHPT and renal stones? My urine often has leucocytes and a trace of blood and occasionally grows an asymptomatic e coli pathogen.
Sorry for the length of this question but I would so value your opinion.
Hi Gill, primary hyperparathyroidism is a major cause of calcium stones, and if you have stones surgical treatment is certainly indicated. Perhaps a renal CT stone protocol might clarify if stones are present. The surgery when done by university level parathyroid surgeons is almost always benign and effective. Regards, Fred Coe
Very many thanks for your comments and advice – much appreciated.
I am a long time stone producer with dozens of litholink studies.
A few years ago I had a sigmoid colectomy for recurrent diverticultis
I stopped taking my 25mg CTD beacause it also eequired 600 mg of Potassium chloride which I assumed would cause GI issues.
I am now wondering weather I made the right choice. Especially, after reading your article pn Thiazides? Perhaps , I could have supplemented the potassium loss dietetically? What a great site
I found. Thank You, John
Hi John, A lot depends on whether you still make stones. Without a sigmoid but with the rest of the colon you should be pretty normal, and whatever was your stone forming state – I gather it was idiopathic hypercalciuria – will be there, still. So maybe it was a bad choice. Is your urine calcium still high? Are you controlling sodium intake to control it? The lower the diet sodium the less drug you need and the less potassium wasting. I am glad the site works for you. Regards, Fred Coe
Yes, I try to stay at 1500 mg sodium daily. my ss caox is 5.66 ca is 218 urine ph is always in the 6.3 area. Does the potassium chloride have any serious GI side effects?
Hi John, Potassium chloride is irritating to the GI tract and occasionally can cause erosion of the tract lining. But the supplement is used in vast quantities and serious side effects are not common. Is your urine sodium really 65 mEq/day (1500 mg diet)? It is best to be sure as diet sodium is hard to estimate. Amiloride could reduce potassium loss, and reduce the need for supplements. Perhaps your physician might want to consider adding it. Regards, Fred Coe
Hi Yasin, Thiazides do not damage kidneys except for rare allergic reactions or neglected and severe potassium depletion. They are used by physicians, and people should not take them without physician supervision. Most stone formers will not need them. Regards, Fred Coe
I really appreciate this website and your dedication. The endocrinologist who is treating my hypercalciuria and osteoporosis has prescribed 12.5 mg of hydrochlorothiazide once daily. I have read here that this drug is short acting. Should I split the tablet and take half every 12 hours or would that dosage be ineffective? Also, when do you have to start worrying about hyponaremia? I am following the recommended hypercalciuria diet – under 1500 mg sodium and 2+ liters of water daily; my serum sodium has fallen to 135 mmol/L.
Hi Paula, with low sodium diet, serum sodium can indeed fall – when fluids are high. I would not recommend a thiazide along with low sodium and high water but just rely on the diet. Thiazide reduced renal free water excretion as part of its action to inhibit the distal tubule sodium chloride cotransporter. Of course you also need high calcium intake 1,200 mg is ideal. Let your physician know what I said and see if she/he agrees. Of course, being at a distance I am in no position to make any direct medical recommendations but only comments that might be of use. Regards, Fred Coe
This website has been invaluable to me since my kidney stone experience last October. I’m 68 and this was my first stone. My first urine collection revealed high calcium levels in spite of the fact I drink 96 oz. a day. After my MD added a daily dose of 12.5 mg chlorothiazide the calcium levels returned to normal. He did not suggest any dietary changes in conjunction with the diuretic. I have gained 10 lbs. in the 7 months that I have been taking the medication in spite of the fact that my daily calories have not increased. Is it possible that this medication can cause weight gain? In addition, after I started taking the drug I had what appeared to be a chronic vaginal yeast for 4 months. Those symptoms persist in spite of the fact my MD ruled out yeast and every other possible type of infection. This has made me wonder if changes in the urine might be causing the discomfort? I am now seriously considering returning to my MD to explore other options than the diuretic. Thank you so much for all the time you spend on your research and publications Dr. Coe!
Hi Marilyn, Thiazide can worsen glucose tolerance and raise blood glucose so yeast flourish. Your physician can check for this. Likewise falling potassium from the drug does this, too. The drug causes no weight gain if it is taken regularly. But some people raise sodium intake drastically which complicates matters. Compare your urine sodium before and after the drug, and your serum glucose and potassium. Low sodium diet always helps. Regards, Fred Coe
Dr. Coe Thank you so much for writing these articles. You have decrease my anxiety SIGNIFICANTLY. I’ve been researching calcium stone formation. ‘m an idiopathic calcium oxalate former. I take essential oils internally, lemongrass and lemon. Tumeric has a high oxalate content so I’m weighing risk vs benefit. Would lemongrass, lemon and apple cider vinegar be appropriate to adjust urine pH. What’s the target number for urine pH. Can renal plaque be eliminated. Thanks
Hi Jackie,
I am so happy that the site has helped you so far. Given what you say, why run from one unproven remedy to another. Here is an article about confusion. Here is a good plan for you to get prevention. Here is how I treat your condition. Best, Fred Coe
Dr. Coe,
Thank you for your dedication. When I was 16 I had my first stone. I kept producing stones even after several attempts at diet change, supplements and specialist recommendations. After I finished my analysis at UIC I go to meet you. You put me on 25mg of Chlorthalidone daily and it changed the entire trajectory of my life. Only episodes I have ever had were when I irresponsibly took myself of the medicine as I suspected it was the cause of my unexplained heart palpitations. I was never able to get the dots connected between the palpitations and the medicine after routine blood work, check ups etc. I am certain at this point that it is completely unrelated. However, is this something that you have dealt with? Regardless, thank you for everything. I have family members that are currently dealing with repeat stone episodes that are not getting resolved after diet, medication etc. I talk about you…but to them you are like an urban legend since you are retired. It has been 20 years and I have a great family that I am able to thoroughly enjoy because of your hard work and dedication. Thank you sincerely.
Hi Matt. I cannot imagine anything more exciting! Urban legend, indeed. As for your treatment, I am thrilled and hope you stay with it. These days I do a lot more with diet and use drugs as backup. Take a look. Palpitations from chlorthalidone usually mean not enough potassium, so be sure about that – your PCP measures blood potassium. You can tell your family members I certainly did not retire and see patients every week as I always did. I have two younger partners who know what I know, so if they want they can come. But urban legend! Wow. I will tell my friends. Best, Fred
I am regular reader, how are you everybody? This piece of writing
posted at this web site is truly good.
Dr. Coe, I am a former patient on chlorthalidone 1X day with 2X day potassium and prescribed past 7 years and no more stones. I get blood tests annually to be sure my potassium levels are normal, which they are. Question: my general doctor continues to prescribes these meds to prevent stones , but is there a danger or concern to the kidneys with prolonged use ?
Is it safe to stay on these meds long term… I’ve been on past 6-7 years.
Hi Denise, I am happy for you that no more stones have formed. Thiazide has long been used in patients for prolonged periods for control of blood pressure, and I have long experience with them for stones. I know of no kidney disease from the pills if potassium and magnesium levels are normal unless one becomes allergic and develops kidney reactions to them. This latter is very uncommon. You could in principle switch to diet management, but if so you might want to see me again to understand what is involved. Here is the ideal kidney stone diet. There is only one diet trial, vs. three with thiazide. Let me know. Regards, Fred Coe
Hi,
I read somewhere that thiazides increase blood sugar. Is that true, and if that is the case, is it not recommended for diabetics who form CaOx stones? Is the impact of thiazides on blood sugar small or large?
If thiazides do have an big adverse effect on blood sugar, are there other medications that lower urine Ca without impacting blood sugar significantly?
Thanks
Josh
Hi Josh, Good issue. The glucose effects are dose related, and also from potassium depletion. That is why I propose the kidney stone diet be in place first. Low diet sodium allows very low doses of thiazide to work well, and also reduces potassium wasting. No other meds exist right now. Regards, Fred Coe
Dear Dr. Coe,
Please accept my sincerest apology, for contacting you, on Christmas day. If you celebrate, I wish you a very Merry Christmas; should you not, celebrate…I wish you a peaceful day. To the point, my body has the propensity for creating kidney stones. Both kidneys have #8, 4-6 mm stones, while the left kidney appears to contain 3 stones which have united, creating a diameter, over 2 cms., said stone, is blocking the left ureter. I find it hard to understand, and am unable to extract the answer, via my treating physicians; why may I not take HCTZ if it helps with the severe pain? I have been prescribed Oxycodone and was told to take it for severe pain, instead of 12.5 mg HCTZ, which works, like a miracle. I am due to have a percutanous nephrolithotomy, within the next week. I am trying to exclude the need of a percutaneous nephrostomy catheter; until, I reach the surgery date. I would appreciate your advice. My sincere thanks, in advance, for your time.
Sincerely,
Debra Connelly
Hi Debra, The stone blocking the ureter is a risk to your kidney and needs to be removed. I gather that ureteroscopy will not suffice? The hydrochlorothiazide will lower urine calcium and prevent new crystal formation, but should not affect an obstructing stone, so I am unsure why you are experiencing a benefit. I do not think the drug can do anything about the stone, either, unless it should happen to pass. But if you have enough potassium to prevent a falling blood level the diuretic is also harmless. Good luck, and I am very sorry your Christmas is so marred. Best wishes, Fred Coe
Hello Dr. Coe,
Had a question on the short acting hydrochlorothiazide 12.5 mg drug. From the time you take the tablet, how many hours before it starts working and from that point how many hours does its effect last?
Thanks
Tom
Hi Tom, the drug acts within the first hour or two and has a 6 hour 1/2 life. I prefer more long acting drugs like chlorthalidone that have less peaks and valleys. Regards, Fred Coe
Dr. Coe, I have been taking 12.5mg of chlorthalidone every other day for 6 months. My 24 hour urine results revealed a reduction in calcium from 427.5 to 217.8. However, my uric acid saturation went up from .9 to 3.13 even though my uric acid itself went down from 589 to 425. My citrate acid went down from 728 to 252. I’ve now been asked to start taking 2x 1620mg in addition to continuing the 12.5 chlorthalidone every other day. Is this standard protocol?
Hi Michele, I presume the chlorthalidone reduced your urine pH, a well known effect. The lower pH would have raised SS uric acid. Uric acid went down because some crystallized in the collection container – or possibly in you. Citrate fell because serum or tissue potassium fell from the thiazide. Supplemental potassium citrate is a good and proper response by your physician. Regards, Fred Coe
Dr. Coe,
I have a question about the longer acting effect of chlorthalidone vs. HCTZ. I’m a 55 year old post-menopausal very active woman who has never had a stone. Ever. Quite unexpectedly, upon my “baseline” dxa scan two years ago it was discovered I have severe osteoporosis in my spine (hips are ok, spine was -3.8 t-score). I’ve also never had a fracture.
Many tests later with many possible causes for osteoporosis ruled out, the only item found was that I have hypercalciuria: my 24 hr tests routinely come back at 300. Again, I’ve never had a stone. I tried 12.5mg of HCTZ (along with 15MeQ postassium citrate twice a day) and that didn’t change the outcome of the 24 hr test. We increased the HCTZ to 25mg once a day (in the morning) and the next 24hr test came back at 200, so we assumed it was “working.” I’ve just had the labs for my 6 month re-check next week and to my disappointment, the 24 hr test is once again registering 303. FYI, I am also taking alendronate 70mg once a week with no side effects or problems.
I’m now being seen at the bone clinic at Johns Hopkins so I’m sure I’m in good hands, but I’m doing my homework before my appointment next week. One of the first endrocinologists I saw (before I got in at Hopkins) had prescribed chlorthalidone rather than HCTZ and I’m curious if the long-lasting difference you refer to above could make a difference. I admit that frequently I don’t drink as much water during the early and mid portions of the day as I do in the afternoon and evening, especially on the days of the 24 hr test. Human nature is that if I see my collection is hovering between 1.5 and 2 liters as I head to bed I think that’s not enough and tend to drink enough to produce my 3 liters by the morning. Of course, this is the time *furthest* away from my dose of HCTZ. I wonder if that could be making a difference.
I also wonder if there is a circadian rhythm to calcium excretion. I thought I had seen something about that in one of your articles, or at least that I’d seen it somewhere. If I’m drinking too much water late in the day, that’s something I need to alter.
Do you think it would be most effective to increase my dose of HCTZ, split it up over the day, or would it be prudent to try chlorthalidone instead? I am very compliant with dosing, and take vitamin K2 (MK4) three times a day, so taking two pills a day isn’t a problem. Any other suggestions? What does one do when hypercalciuria persists?
Hi Trijntje, Bone disease is quite common in IH. The secret is low diet sodium – 1500 mg or so and a low dose 12.5 mg of chlorthalidone. The drug acts to increase renal calcium retention but only when diet sodium is low. It has nothing to do with urine flow. Food increases urine calcium loss and also provides diet calcium supply so you need a high calcium diet from foods 800 – 1000 mg; supplements are tricky to use, food is better. OHCTZ is a miserable drug – short acting, bursts of increased urine flow and sodium loss. I never use it. Low sodium + high diet calcium + CTD + alendronate = good initial recipe. We have only one diet bone trial worth reading. It is in this link. Regards, Fred Coe
Thank you for the reply. Perhaps it is as simple as my salt intake creeping up: your salt atricle shows that there’s clearly a correlation between salt intake and calcium output for those of us with IH – really drives the point home! I last evaluated my salt intake a year ago and it was fine (it has always been low), but I’ll get on that to make sure. I have always had NO problem getting enough calcium in my diet – I love milk and cheese (but realize that cheese can pack a salt wallop) – sometimes I have to cut back to keep it from going above 1200mg a day.
I appreciate your information about HCTZ; I’ll have a talk with the doctor next week about that, and ask proactively to either split the current dose or any increased dose of HCTZ or to switch to CTD.
My last two metabolic panels have shown low serum sodium and chloride, so I’ll talk to her about that, too. It’s certainly all a jigsaw puzzle!
Hi Trijntje, low serum sodium probably comes from the diuretic. Your personal physician really needs to sort that out. I am too far away. Regards, Fred Coe
Dr. Coe,
I am 45 years old and I was diagnosed with kidney stones in 2015 after having a stone lodged in my ureter. This was the first time I ever had a stone and the ER doctor said my “kidneys are full of them”. I didn’t get an exact number. Upon getting an MRI they also revealed that I have a cyst in my right kidney. I have been doing 24 hour urine samples ever since then. The only suggestions I was given for diet was “low sodium, low protein” (which I had to figure out on my own through trial and error). I didn’t even receive information on foods to avoid that are high in oxalates until one of my 24 hour urines came back with high oxalates. My numbers on my 24 hour urine have improved except for the urine calcium which is high (451mg/d) and my pH is 6.661. My sodium is fine at 127mmol/d and PCR is 1.2g/kg/d. My urine calcium prior to this time was in the 200’s each time. I drink plenty of water with a 2500-3000ml output. My doctor had me taking HCTZ 25mg at the onset in 2015, but after 2 weeks of taking it I was on the verge of passing out by 3pm and was lethargic. I am a nurse and I took my BP when the episodes were happening and my BP dropped every time. I then started taking it at night and when I needed to get up to the bathroom in the middle of the night I had the same symptom of feeling like I was going to pass out as well as in the morning when I woke up and tried to function. So he cut the dose in half and I still had the same symptoms. Have you ever heard of this? My urologist has not and doesn’t want me to stop taking it, but I can’t live my life like this. I also feel as though I wasn’t getting enough calcium through my diet possibly and I don’t take calcium supplements. My doctor has not given me any information regarding the calcium issue except to take HCTZ. I would certainly take it if I knew it would help but the little bit I was taking didn’t seem to help my calcium level. It seems as though I would probably need more HCTZ that I don’t think I can handle. Also, I have not had any follow up blood testing or any further interventions since 2015 besides the 24 hour urine tests and 2 KUB’s where the kidneys were unable to be seen due to stool in the colon despite taking MagCitrate prior. I am just curious if there is something else I can do to get my calcium down? I am NOW working on pushing calcium to 1000mg/day through my diet, but is there something else I should be aware of?
Thank you so much!
Hi Angie, You do indeed have a very high urine calcium loss rate, and an alkaline urine, so I imagine your stones are calcium phosphate. Your diet protein is high and can raise urine calcium. If your serum calcium is normal and you have no known systemic diseases I presume you have idiopathic hypercalciuria. Treatment is as low a diet sodium as possible, high diet calcium from foods if possible, and thiazide – if at all – at very low dose. You cannot just raise diet calcium without really lowering diet sodium because urine calcium is increase and stone risk with it. This article seems to relate to you. Basically you need someone with some skill and finesse to fashion you a treatment you can use. For diet, Jill Harris could be helpful. Regards, Fred Coe
I cannot thank you enough! Especially for the recommendation. I use a lot of my time trying to figure this out and it is frustrating. This is very helpful. Thank you again!
I forgot! Two things, I do have Hashimoto’s Thyroiditis if that effects anything at all. Also, I live in the Chicago area. Who do you recommend that would have the skill and finesse that would help create a treatment for me?
Hi Angie, If you live in Chicago, I can see you personally, or one of my partners. Our secretary is Kathleen Dineen, 773 702 1475. Regards, Fred Coe
Have you ever had anyone on Indapamide incrreae in their uric acid levels and develop gout? I havent been to Dr yet but will be, all of a sudden since a few months after starting this drug started with right hand index finger knuckle joint pain and now few months later both great toes joint pain and left knee which I am not sure is with that or a different problem. I made an appt but just curious if you have had anyone who has had similar complaints.
Hi Martha, Indeed indapamide like all of its ilk can raise serum uric acid and provoke gout. Your physician needs to find a remedy for you. Usually it is a drug to lower serum uric acid. You have thought well. Regards, Fred Coe
Dr Coe
This is a beautiful written article. As an academic nephrologist, I keep visiting your webage ever so often to ‘re-learn’ all I have forgotten about stone disease to help manage my patients better. Thank you for the constant education.
Regards
Pranav Garimella
Hi Dr. Garimella, Thank you very much for saying this. I much appreciate the feedback. Warmest regards, Fred
Great article. I have calcium oxalate stones, have just been started on hydrochlorothiazide 25 mg. I would still like to get enough calcium but have issues with dairy. Is there a good calcium supplement I cant take that will not cause a problem? Should I also be taking potassium and/or magnesium? Thank You!!
Hi Laura, Thiazide is good; but be sure and do the whole kidney stone diet, not just a part. Begin with the low sodium as it will greatly enhance the efficiency of the thiazide. Then add the calcium – for your bones and oxalate control; lots of dairy products lack lactose, many differ a lot from cow’s milk so most people can find something better than calcium supplements. You will need potassium and /or magnesium if either blood level falls. Regards, Fred Coe
Hello Dr. Coe,
I’m wondering how much reduction in calcium excretion you expect with thiazides (in ideal setting of low Na intake, appropriate dosing). Looks like RCT on indapamide reported ~50%. I am also curious about spironolactone’s effects on calcium excretion. Is there a role for it for K sparing effects, further reduction in urine Ca? Thanks so much.
Hi FC, I have some data on this. The article you are posting on shows our excretion rates in the CRC giving about 0.1 mmol/hr (4 mg/hr) reduction at about 100 mEq sodium/day diet; this gives about 100 mg/day of overall reduction. I found in other experiments that at any given sodium intake thiazide created about that large an effect on the intercept of the urine calcium/sodium regression. As for potassium sparing drugs, I like amiloride and use it a lot; spironolactone has too many side effects for my taste. But I always lower diet sodium aggressively before using thiazide as without that life is nothing but potassium issues. Regards, Fred
Several previous cross-sectional studies have demonstrated the association between gout and kidney stone formation. Allopurinol has been shown to decrease the risk of calcium oxalate stone formation by reducing urinary uric acid excretion. What are your thoughts regarding using both allopurinol and a thiazide in this presentation? With regards to a combined history of gout and calcium oxalate/uric acid stone formation, is the goal to eat a diet low in oxalate, increase fluids and reduce salt and sugar? I am toiling between the kidney stone diet and the low oxalate diet?
Hi Deborah, I gather you have gout and form stones composed of both uric acid and calcium oxalate. This is what I take from your comment and what I am replying to. For the uric acid component of stones, allopurinol is ineffective; you need to raise urine pH above 6. For the calcium oxalate component, this article is my best. I originated the allopurinol calcium oxalate story and you will find it in the second article. It is a last step, rarely employed. The ideal diet is always the kidney stone diet. Low oxalate diet is a minor – if radically over done contributor. Regards, Fred Coe
I’m going to do another 24 hr urine test, this will be the 3rd one. My urine calcium was still too high on the last test. I have drastically reduced sodium, reduced protein, and oxalates. If I get results back again that calcium urine is still high, my urologist suggest putting me on medication. If so , does this mean I would have to be on it for the rest of my life? Or is there a chance I can get off of it? I just hate the idea of taking medication for this. I’m 65 , had 2 lithotripisy , still have a 3 mm stone left. I do already have osteoperosis. Never a fracture or broken bone yet.
Hi Vickie, It is hard for me to help as you provide no numbers. Did your urine sodium actually fall to below 100 mEq (2300 mg) per day? Is your supersaturation no lower than at the start of treatment? Here is a strategy for treatment, so you can see how it is done. Regards, Fred Coe
Dear Dr Coe,
Can the effect of thiazide diuretics on urine calcium wear off after a number of years? I read with interest your bathtub analogy, and was wondering if eventually no further calcium can enter the bone?
Warm regards
Hi Jon, In our long term observation studies we found no evidence of a waning effect. Of course we were looking at 24 hour urine calcium, not bone. Regards, Fred Coe
I took this medication for several months for blood pressure and felt the worst I had ever felt in my life. Blood tests showed my cholesterol was 302. My sodium count had dropped well below the recommended level. I do have kidney stones and my kidneys ached continuously even though I was drinking plenty of water. I was tired, had no energy, had diarrhea and nausea. EKG registered an extra heartbeat, blurred vision and somewhat disoriented. I stopped taking the medication and had blood work done 5 days later…two weeks after my previous blood work. Cholesterol dropped to 185 and I actually started feeling human again. It’s been almost five months since I stopped this and I feel a heck of a lot better. There’s a reason some people say doctors love this medication and patients hate it. No doubt it does work with some patients but I recommend anyone taking it to tread carefully. It can play havoc on the body.
Hi Fran, I presume you took the medication for high urine calcium as a cause of kidney stones. An excellent alternative is low sodium diet, that will do as well – almost – if you can manage it. The entire diet is ideal for stone prevention – see the link. Regards, Fred Coe
Dr Coe,
Two questions:
1) Several years ago Dr Prien from MGH put me on Moduretic 5-50 once a day for IH. I notice your article does not have Moduretic as an option. Should I request a different medication to be considered at my next appointment?
I make Calcium oxalate stones stones but have a small amount of calcium phosphate in the stone as well. My latest 24 hr urine has my urine calcium borderline at 213. My urine volume is great at 3.8. My ssCaOx is low 2.36. My oxalate was 27. My citrate is high at 681. My ssCaP is borderline at 1.20. My pH is high at 7.180. I do a low sodium diet – Na24 is 72. And low protein. And low added sugar. (I took Jill’s prevention course- money well spent!)
2). I am osteopenia (age 57) so I began my 1200mg of calcium a day between skim milk, yogurt and Swiss cheese. My 24 hr urine without dietary calcium a year ago was 185 and my recent one is 213 with the calcium. Went up! ) Should I aim for 1000mg dietary calcium a day instead of 1200?
Thanks
Julie
HI Julie, Your urine chemistries and supersaturations seem low risk for more stones except for the remarkably high pH. Are you using alkaline calcium supplements – Tums, calcium citrate?? I suspect that is the problem. Can you not get more calcium from food and less from supplements?? Otherwise things look rather good to me. Regards, Fred Coe
No supplements. No tums.
Just milk, yogurt and Swiss cheese.
Would too much fruit give a high ph?
Hi Julie, but it would take quite a lot. Juices and smoothies would be very likely to do this. Regards, Fred Coe
Dr Coe, I have been taking Lasix (a loop-diuretic)for 10 years or more. I am a heart patient and have filled up with fluid twice resulting being put on ventilators. I now (2014) have a pacemaker and am dependent. I was taking 40 mg of Lasix twice per day but now am down to 40 mg of Lasix once per day. I am also a kidney stone former and have been wondering if a Thiazide diuretic would be better for me as my 24 hr urine calcium is high. I am on a LOD and try to keep sodium below 1,500 per day. I want the best way to treat my heart and kidneys. Maybe time for a change or maybe I am just fine the way things are. I will ask my nephrologist and cardiologist but wanted to get a heads up from you and if you have any suggestions. Thank you for helping so many with kidney stone prevention.
Hi Hanene, you seem to have serious heart failure that requires lasix to prevent pulmonary edema. Thiazide might not be enough for you. Your physicians need to determine this. Usually lasix raises urine calcium, and possibly might cause stones and bone mineral loss, so if you could make do with thiazide it might be of benefit. Your situation is so complex, however, I cannot say much in any detail. Regards, Fred Coe
Hi Dr Coe, saw my Nephrologist today and after reviewing my latest 24 Hr test results. He switched me from Lasix 40 mg to Indapamide 2.5 in hopes to lower my urine calcium which was 255. The highest was 284 just over a year ago. I see the cardiologist the end of October. Hopefully this will be a good move in the direction of reducing kidney stones. I have punctate calculi which will not come out no matter how much water I drink, complicated with duplex kidneys and duplex ureters. You are right…I have a complex situation, just trying to balance many co-morbidities. I have a good team and with your help I am making progress in the right direction. Trying not to have infections or stones. Thank you so much!
Dear Janene, Indeed complex, but I hope for a good long term outcome. Regards, Fred Coe
Hi Dr. Coe,
I have been a chronic kidney stone former for approximately 20 years now and have been taking 25 mg hydrochlorothiazide daily and 1620MG potassium citrate (3x/day) and still manage to form stones. This month my nephrologist had me complete another 24 hour urine collection and it shows that my calcium levels remain elevated at 312 mg/day and my sodium levels are also elevated at 220 Meq/day. It is now being suggested that I increase my hydrochlorothiazide to 25 mg (2x/daily) to help reduce the calcium content but I am concerned about long term consequences of taking this medication. I have read that taking hydrochlorothiazide can cause kidney disease after long term usage. Are my concerns valid? I really would like to eliminate the creation of kidney stones but I don’t want other negative issues either. I have been trying to implement your diet plan as of late as well to try to minimize stone formation and I just feel frustrated at this point after having suffered with this issue for so long. What are your thoughts?
Thanks,
Matt Nelson
Dr. Come,
Thank you for all the info. and research work.
Please talk more about saturation prevention, low salt, and no medication treatment…….to prevent stone formation. Thank u
Ps. Do u know Dr. Rita McGill?
Hi Suzanne, Here is my best on treatment using diet and showing meds as an addon when diet is not enough. I do indeed know Rita, we work together. Warm regards, Fred Coe
Thank you for this article.
I am a Kidney Stone sufferer for over 6 years.
Even though I am not a doctor and didn’t understand all the references and points it did give me a lot clearer reason for my doctor prescribing chlorpheniramine.
I do have 2 questions.
1. I saw Uric Acid mentioned in this article and wonder how does this drug effect someone with Gout that is also taking Allopurinol?
2. I was told by my Urologist that salt counter acts this drug. I have seen a wide range of “suggested” levels of salt intake for a low sodium diet. Any option on what one is somewhat average.
(Of course I want it to be the highest sodium intake but after the problems with this lost round, I want this medication to be effective).
Again thank you very mush for this information.
Hi Gary, I think you mean chlorthalidone. The drug can raise serum uric acid and your physician will re-measure to be sure your level is controlled. Of course chlorthalidone is for calcium stones; if your stones are uric acid – as is common in gout patients – it is not the right treatment, so be sure of stone type. I imagine your physician is indeed already clear about this matter. Try to lower diet sodium below 100 mEq (2300 mg of sodium)/day or lower; 1500 mg of sodium would be ideal. Regards, Fred Coe
It is to my understanding that in some cases, an abrupt decrease in dietary calcium intake can actually cause a paradoxical calcium oxalate stone. So in your many years of experience have you ever come across a case where thiazides actually caused calcium oxalate stones?
Hi Abd-Arahhman, No; I do not believe the phenomenon exists. Thiazides lower urine calcium, and supersaturation. A fall in diet calcium, on the other hand, can raise urine oxalate by increasing oxalate absorption, so low calcium diet could in principle promote stones. It is an unhealthy diet, as you know, and one to avoid. Regards, Fred Coe
I had 5 lithotripsy procedures in 2017 and have been prescribed 25 mg of hydrochlorathiozide and 1080 mg of Potassium Citrate. At the time, I was not as active as I am now. I am currently very active and exercise moderately to intensely approximately 5-6 days per week. In the summer I cycle for 1-2 hours and sweat a lot. I also take 50 mg of Atenolol for the control of a rapid heart rate. I was wondering if the combinations of any of these drugs, or the drugs/exercises is contraindicated?
Thank you for your articles!
Hi Stefanie, I take it your stones have not recurred, which is fortunate. Taking a diuretic and exercising is fine but you have to be sure to maintain hydration – water, but also (I know this will sound contrary to everything I usually say) enough sodium to replace losses. You need to work with your physician on this, to avoid salt deficiency and falling blood sodium, and also avoid salt excess that will vitiate the value of the diuretic. Only your physicians can counsel you on this and it is very important that they do so and maintain some surveillance over the results. Regards, Fred Coe
Hi Dr. Coe,
First, thank you so much for providing such valuable information to the public. I am a kidney stone producer (hypercalciuria) and try to be very meticulous now about what I consume, with guidance of my nephrologist. I have been on hydrochlorothiazide for some time now and my nephrologist recently increased the dosage from 25mg to 50mg, without much improvement in my calcium levels as of recent urine analysis. I have recently started to pay close attention to what inactive ingredients are in some of my supplements, as they can be quite hidden. I recently reviewed my prescriptions and found that an inactive ingredient in hydrochlorothiazide is dibasic calcium phosphate dihydrate. That’s a mouthful, but it is concerning to me that it has calcium phosphate in it. Should I be concerned?
https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=01f1f478-5493-439f-9b99-f4f82023781c
Thanks!
Hi Tad, No; it is a minor amount. But if the drug is not lowering your urine calcium, suspect your sodium intake first. Is your urine sodium low enough?? I imagine your physician will want is below 2000 mg (about 100 mEq). I try for even lower. The drug works best that way. Another issue is too high a diet protein intake. Finally, there is refined sugar – that raises urine calcium in a spiky way. Here is my favorite article on the treatment issues. The article you are writing on has some of the sodium – drug interaction issues in it as well. Regards, Fred Coe
Is 12.5 of hctz just as effective as 25 mg in preventing stone formation?
Hi Don, No trial data on that range. But I use 12.5 mg of chlorthalidone and at least in terms of lowering urine calcium it works very well so long as urine sodium is near 100 mEq/d or so. A lot more sodium and even 25 mg/d gives me more potassium wasting and less calcium lowering. Fred
Is there a significant difference in urine ca and stone incidence between hctz 12.5 vs 25? Have the doses been compared?
Thanks
Hi Don, No, these two doses have not been compared. Fred
Hi. i just found your site and is so happy to read about how diuretics can prevent kidney stones’ I am 62 years old and had my first attac when I was 22. Over the years I have had many. Especially during my pregnancies. I recently had a new ct scan and it showed four small stones In my left kidney and 3 in my right. One of them is O’8 mm and the rest of them are smaller. I have had them for many years now. They don t bother me or at least the did not bother me. This last year I have had severAl attack’s lasting only a short day. I cannot see any stones coming out so I suspect they are caused by sand. Now the doctors want to remove the stones. But I am not sure what good that will do me since it is not the stones but the sand that cause me all this trouble. I eat very healthy. Is just a little overweight, I walk and trim almost every day. But I know I should drink more water….I try to remember but often forget. All my blood tests are normal according to the hospital. Should I try diuretics? nobody has suggested that to me. And can the stones in my kidneys cause the kidney sand that often bothers me? I will be so grateful for advice and answers because this hurts, I promise you. Best wishes from Rikke
Hi Rikke, These drugs do work. But you should have 24 hour urine testing to know what is really causing stones, likewise what the stone crystals are. The linked article shows a reasonable strategy for evaluation and treatment. Regards, Fred Coe
Dr Coe,
I really enjoy reading your all your wonderful Kidney stone articles. I have learned so much. I’m a kidney stone patient as well as a Medical Laboratory Scientist aka Medical Technologist who works in a clinical laboratory for over 40 years.
I’m also a member of Jill Harris wonderful Facebook group.
I have some questions that hopefully you will answer for me.
I have a history of kidney stones, large calcium oxalate stones (1.5 cm 1.9 cm and numerous others) I recently had my second Ureterscopy Bilateral Laser lithotripsy in March and previous I had the same procedure in December 2015. I presented both time in the ER septic with kidney infections and large stones at the apex of my kidney blocking my ureter.
I’m now going to a nephrologist who a little over 2 weeks ago started me on Chlorthalidone 25mg. This is the first time I have taken any thiazide diuretic.
I’m eating a low sodium diet 1500 mg or less
Low calcium oxalate 100 mg or less, no added sugars low card and a low protein diet (calculated with Jill’s formula) I drink lots of water (no sodas or coke) and I’m a ‘high volume’ 24 hour urine patient volume= 4+to 5 liters. Here are my questions:
I had my first blood work on Tuesday after starting Chlorthaladine 25mg. My Electrolytes were in the normal reference range just prior to this, as was my uric acid and my serum phosphorus.
No surprise that now my K, Cl, Na are very low. Yesterday she prescribed KCL 20MEQ ER twice a day. She lowered my dose of chlorthaldine to 12.5 mg. But my serum phosphorus is now also very low too . My doctor told me today this is caused by the calcium citrate 600 mg tablet I have been taking daily with food. She just told me to stop taking it. But to continue taking liquid MG citrate.
Question Why would my calcium citrate supplement now cause my serum phosphorus to be low? This just does not make sense to me.
I’m getting most of my calcium requirement from my food.
Plus my previous normal uric acid is high too.
I have idiopathic hypercalciuria diagnosed from my multiple litholink 24 hour urine studies and osteopenia diagnosed with my DEXA scan. My PTH is normal as is my ionized calcium and my vitamin D.
Thanks for your help! I find this all very frustrating as I now just don’t feel well since I started Chlorthaladine.
Hi Ruth Ann, The low potassium is from the thiazide and the KCl will help raise it. CTD will raise serum uric acid because of reduced ECF volume and increased kidney tubule reabsorption. The low phosphate is not expected. I agree with less CTD and with Mg supplements, but would just re-measure to be sure the serum phosphate is really low; stop the calcium supplements for a few weeks, which is a good test of your physician’s hypothesis – before doing the serum. If the phosphate is low, a 24 hour urine will tell you how much is being absorbed. Regards, Fred Coe
Hi Dr. Coe,
I’ve followed your blogs for several years and have found them really helpful in trying to minimize the risk for kidney stones, having had 5 episodes over the years (I’m 64 years old). I’ve had the 24 hour urine test for 3 years and my urologist has me on chlorthalidone for over 1-1/2 years (12.5 mg the first year and now 25 mg. daily). I’ve had benign positional vertigo in the past and over the past 3-4 months, have had some pretty drastic dizzy / lightheaded spells. I went to an ENT and they told me that these latest episodes are not benign positional vertigo. They also want me to go on a low sodium diet and they seemed to be questioning why my urologist has me on the chlorthalidone. My sodium level was 139. I’m beginning to wonder if the chlorthalidone is causing these dizzy spells. Do you know if this is a common occurrence and if so, are there any substitution medicines that could help me prevent kidney stones? A million thanks!
Hi Carl, chlorthalidone can indeed cause postural fall in blood pressure and therefore dizziness. The sodium level you mention is of course in blood which will generally be normal and unhelpful in understanding things. Given these attacks, perhaps your physicians might want to stop the drug in favor of low sodium diet with 24 hour urines to document it is indeed low and also to determine if that diet might not be enough to lower urine calcium and stone risk. That is not an unreasonable idea, and this article details how it is implemented. Take a look and speak with your physicians. Regards, Fred Coe
I am being prescribed hydrochlorothiazide 12.5 bc of calcium leakage in my urine. My bone density readings this year decreased significantly and the Dr. wants to try this. With the bathtub analogy above I am concerned that it might be futile. I have never had a kidney stone and am otherwise quite healthy (weight 100 lbs.) and exercise daily. Should I also reduce my sodium intake?
Hi ELizabeth, I presume you have idiopathic hypercalciuria and bone disease with it. Indeed lower diet sodium is valuable for maintaining bone balance, and allows the thiazides to work better at lower doses. The combination of low diet sodium with high diet calcium has been proven to cause positive bone mineral balance, as well. If bone mineral keeps falling your physicians should consider bone active drugs in addition to these measures. Regards, Fred Coe
I have osteopeonia, and am trying to do my best not to get into full osteoporosis. I met with a dietician to increase my calcium intake without taking calcium pills and she was able to provide some ideas for higher D and calcium foods. Is it inevitable that I will develop osteoporosis?
Hi Elizabeth, High calcium with low diet sodium (1500 mg) was shown to produce positive bone mineral balance in one very well done trial, so I can recommend that combination without reservation. So it is not inevitable. The real problem is to intervene early so as to minimize need later on for more bone active drugs that all have their problems. Regards, Fred Coe
Hello, I had calcium oxalate kidney stones that required surgery to remove. Follow up ultrasound showed calcifications of the renal papilla. I am on a low oxalate diet and drink 1.5L water daily. I have just been prescribed hydrochlorothiazide 12.5mg once daily. I don’t consume any dairy products and am confused about how much calcium to supplement my diet. Also, would the addition of potassium citrate be helpful? Thank you, Deborah
Hi Deborah, Here is the problem. Low calcium diet is a bad idea for anyone who has a skeleton, and also makes oxalate into a big issue. This latter is because without diet calcium food oxalate is readily absorbed, with a lot of food calcium it is not well absorbed. Potassium citrate is worthwhile for those who need it. Here is a good diet for a calcium oxalate stone former. Here is a good evaluation outline and also about how diet and drugs work together. Regards, Fred Coe
I take Topamax for Epilepsy and have calcium oxalate stones. I’ve had stones for about 17 years and have passed several and currently have 6. They are relatively small-no surgeries or stents. I take potassium citrate 15 meq at least once a day, twice if I can remember. Years ago Hydrochlorothiazide may have been mentioned, but I’m not sure why it wasn’t pursued. Possibly because my blood pressure runs on the low side? Stopping the Topamax is a thought and I do take other anticonvulsant meds, but it’s a difficult decision to make. What is your opinion on Hydrochlorothiazide and patients with low blood pressure? If I follow a lower sodium diet, drink enough fluids, eat fruit and vegetables, cut down on refined sugars, is it necessary to decrease protein intake? I try to use a 30-40-30 calorie ratio- 30% protein, 40% carbs, 30% fats.
Hi Lesley, Topamax causes a form of renal tubular acidosis and stones are usually calcium phosphate. No drug really can offset stones from Topamax. Ideally you would be on another drug if possible. Potassium citrate and hydrochlorothiazide are not likely to help prevent more stones. But in the final decision, your personal physicians need to help you weight the balance between more stones and problems of changing drugs. Regards, Fred Coe
I recently had my first kidney stone at the age of 25, which required an unpleasant procedure to break up. I had begun taking Edarbyclor 6 months ago for high blood pressure. Do you think this drug could have caused or contributed to the formation of the stone? The drug includes a diuretic (12.5 mg chlorthalidone), but not the one you recommend, should I use a different BP drug to reduce chance of more kidney stones? Thank you, Eva.
Hi Eva, Your drug is a combination of chlorthalidone diuretic and Azilsartan medoxomil a angiotensin receptor blocker. Clorthalidone has been used to lower urine calcium for stone prevention. The ARB is well known for blood pressure, but at your age one might think the chlorthalidone itself might be enough. The drug will not cause stones so far as I can tell. But you need to know what is causing the stones, and here is an article about how to get properly evaluated so treatment is targeted. As for your high blood pressure, the need for 2 drugs at your age is unusual, and I wonder if there is a reason. You might ask your physician. Regards, Fred Coe
In patients with a history of calcium-containing kidney stones who also have gout, or in patients with a mixture of calcium and uric acid containing stones, would thiazides still be beneficial? Or would you expect the benefits of reduced urinary calcium excretion to be offset by the increased uric acid?
Hi Anna B, Indeed thiazide can raise serum uric acid and even provoke gout attacks, so when needed in someone with an elevated serum uric acid physicians usually prescribe a second med to lower the serum uric acid. For uric acid stones, the treatment is to raise urine pH with potassium citrate or a sodium alkali if needed. For the calcium part of mixed stones, one treats as for calcium stones without uric acid, and here is a good article on just that part. Regards, Fred Coe
I had Total Thyroidectomy August 2019 for Thyroid Cancer. My parathyroids were not functioning after surgery. I was given a calcium infusion while in the hospital and re-hospitized the day after requiring another calcium infusion. For 6 months after surgery I was taking up to 8000mg orally of calcium daily and my numbers were barely if in range. I now take 3600mg daily and I still have days of symptoms ie, tingling in my lips,face,feet and fingers. I did a 24 hour urine and my numbers were 468mg (100-300) range. Endocrinologist has prescribed 12.5 mg of hydrochlorothiazide once daily. I take Calcitriol 2 x daily along with potassium & magnesium. Does this sound right? I’m worried about getting stones.
Hi Andrea, You do indeed have a problem, and a famous one at that. Your bones are a taking up calcium and your kidneys are not conserving it, and stone risk is real. After a while things will get less extreme. IN the meantime high fluids – a gallon of fluid a day – is your best protection. Your physicians can consider replacement PTH but it is injected, complex, and fraught with possible risk, so that is a very complex decision. Regards, Fred Coe
Hello Doctor,
I have recurring kidney stones which started apparently from bad parathyroids (my mother also had this). I had 8 stones and 3 1/2 parathyroids removed in 2016. My doctor has had me on hydrochlorothiazide 12.5 mg ever since. Two new small stone have formed since then. I’m told to take this medication in the morning, 1 per day, but I have read some literature that says it is better to take it at bedtime. Does it matter? Is it OK to be on this medication long-term at this low dose? Thank you
Hi Lois, We have published that hypercalciuria is common after cure of hyperparathyroidism. Assuming your serum calcium is normal – meaning surgical cure – the drug is reasonable, but you have had recurrence. One possibility is that the drug and/or dose is/are less than optimal. I have always favored chlorthalidone, 12.5 mg over OHCTZ as being very long acting. But for either drug you need to control diet sodium for it to work and be sure via 24 hour urine testing that what you are taking has indeed reduced urine calcium below the risk limit of about 200 mg/d. Regards, Fred Coe
How long one should use this hydrochlorthalidone or diuretics after an incidence with calcium oxalate stone
Hi GMP, if you have an indication for the drug, one may need it life long. But the drug is best used in the context of diet management, and often the latter will suffice. Take a look here at how diet comes first, thiazide as an addition. Regards, Fred Coe
Hi Dr Coe! What a fabulous site you have created. Thanks for your generosity! I am a 120lb female with 300 urine calcium and urine sodium at 115 and I make calcium stones. I am trying to find a general rule of thumb for how much to expect urine calcium to decrease using
1. HCTZ 12.5 once a day
2. HCTZ 12.5 twice a day
3. Chlorthalidone 12.5 once a day
4. Chlorthalidone 12.5 every other day.
I thought I read you generally expect #3 to reduce calcium by 100 but I am wondering how these other meds/dosages might compare in your mind. I know there are no guarantees but your vast experience is appreciated. Thanks!
Hi Denise, You ask a very good question. My only data – much of it not published, some extracted from trial data – shows the 100 mg fall in urine calcium from what is expected given the urine sodium. For you, as a general rule, lowering your diet sodium from 115 to perhaps 60 or 65 will get urine calcium down by 75 to 100 mg, and chlorthalidone 12.5 mg daily will get you another 100 or so mg/day – as a rule. No two people are alike, the data spread a lot, so you will have to get 24 hour urine testing to find out. The sodium step is very powerful, and if you can do it you may not even need the drug. Regards, Fred Coe
Dr Coe,
You are a gem!! After reading your response a lightbulb went off! I finally understand the power of sodium reduction. You see, I was deluded into thinking my sodium level of 100 was good based on comments from 2 different urologists saying it was low and both explaining there would be no benefit to reducing it further. As such, I believed the 100 sodium level signified I was successfully implementing the 1500mg diet. Boy, I was fooling myself. I understand now my diet sodium was actually 100/.044 – 2300mg not 1500mg. I clearly have more work to do. Your quick analysis illustrating possible results of a low sodium 1500mg diet applied to my situation was impactful and gave me the strong motivation I needed to put in the extra work to successfully implement my low sodium diet. I have received 3 different scripts for medication and have been so close to just medicating for the rest of my life. I emphatically wish to avoid medication. I am so happy I held out and continued to educate myself on your site. I feel empowered to control my health. I am thankful you are in a position where you can not only educate other doctors at U of Chicago but also millions of people like myself who read your site. Please know, Dr Coe, you are extremely valued and the generosity of your time and talents is both admirable and remarkable. Thank you!
Correction – meant to write current sodium of 115 = 2613 mg rather than the 1500mg.
Hi Denise, Thank you for your supportive remarks about the site, and also for being so preceptive about your own care. If you do achieve a lower urine – diet – sodium, urine calcium will be at that level one can reasonably attain with diet sodium management, and I presume with adequate diet calcium of 1000 mg or 1200 mg daily. At that point one can use the meds if needed. One can expect a fall of 100 mg of calcium below what diet sodium yields using either K citrate or a low dose of chlorthalidone of 12.5 mg. I said this before but here is the article showing the data. You are right about numners. About 3 million people have come to this site since I opened it in 2015, so it is hopefully helping a lot of people. If you like irony, these numbers exceed by orders of magnitude those who have read my scientific papers (300 or so published) and books, reviews, chapters etc (another 300 or so) in aggregate – probably no more than 10 thousand albeit mostly physicians and scientists – over the 50 years of my career. Regards, Fred
I was wondering what is stronger – 1.25 indapamide or 12.5 chlorthalidone? I hesitate to be on chlortalidone based on a negative experience I had so was wondering if the indapamide would also be just as good.
Hi John, I use both drugs and consider them interchangeable. Both reduce urine calcium the same, and both have the same very long duration of action. Choose for price – both cheap – and tolerance. Regards, Fred Coe