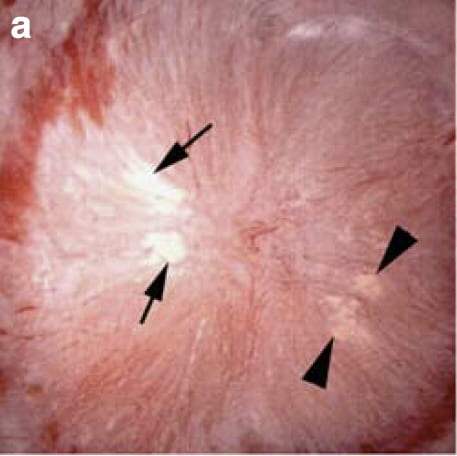
The large picture shows a papillum of a patient with ileostomy as seen at surgery for stone removal. The large white patch between the arrows is plaque, the stuff calcium oxalate stones can anchor to and grow on. The yellow material between arrowheads is terminal ducts of Bellini (BD) plugged with crystals. Both are abundant in patients with ileostomy and part of how they form stones.
This article relies on only three research publications, and in all modesty I must admit they arose from our research group. But in defense, one is remarkably comprehensive and one the only one with detailed study of kidney tissue obtained during stone surgery. Also in defense, their reference lists are good enough to give anyone access to other related papers. Finally, apart from the kidney tissue, our work is in line with what everyone else has found, so in using it I am presenting a main consensus.
How Ileostomy Promotes Stones
Water and Electrolyte Loss
The colon reabsorbs large amounts of water, sodium, bicarbonate, calcium, and potassium. When colon is lost from surgery for cancer or inflammatory bowel disease, what it once reabsorbed is also lost into ileostomy drainage. Kidneys compensate as expected, by producing a scanty and acidic urine low in sodium, calcium and potassium. Kidney cells conserve filtered citrate and metabolize it to bicarbonate to help make up for ileostomy losses. Likewise, they produce copious ammonia, a way of removing acid from the body.
All these compensations supersaturate the urine with respect to calcium oxalate – low volume, and uric acid – low volume and pH. As a result, calcium oxalate and uric acid stones occur.
Does Not Increase Urine Oxalate Excretion
Much the same pattern of water and electrolyte loss occur after loss of small bowel from surgery or other cause. Losses are less severe when the colon remains in place because it can reabsorb some of what escapes from the small bowel. But the colon is affected in such a way that it permits abnormal amounts of oxalate to pass through its linings into the blood. As a result urine is high in oxalate as well as scanty and acidic – so called enteric hyperoxaluria.
Dehydration vs. Oxalate
This is a key point of distinction. Ileostomy causes stones and poses serious risk of kidney injury from dehydration. Small bowel resection poses less risk from dehydration but more from excess oxalate excretion that can cause both stones and severe kidney injury. Ileostomy plus small bowel resection, therefore, causes extreme risk of dehydration, but loss of colon removes the source of extra oxalate. In other words, with or without associated small bowel disease, patients with ileostomy form stones because of electrolyte and water loss, not excess oxalate.
Supersaturations
In our past and recent publications we have found people with ileostomy mainly form uric acid and calcium oxalate stones. The papers referenced in the bibliographies of these two papers describe about the same proportions of stone types. One should expect that urine supersaturations will be high for both crystals. Moreover, given that ileostomy leads to scanty acidic urine we should find that supersaturations arise from low urine volume and pH.
Urine Volume

The importance of urine volume is easy to demonstrate using our own data from 7 patients with ileostomy whom we studied in considerable detail.
In the figure, SS for uric acid is in red circles, that for CaOx in blue. Both rise as urine volume falls. The vertical line at the right marks the volume at which Curhan found overall population stone risk was reduced to baseline. Four points lie on or to the right of this line.
In our cases that volume of 2.3 l/d seemed to confer only marginal safety. I say this because risk of uric acid crystallization begins as soon as supersaturation rises above 1 (lower horizontal dashed line) and one of two uric acid points lie above 1. Similarly, one CaOx SS lies below the point at which these crystals usually form but the other is much higher.
So, one should raise urine volume as much as possible and try to reach above 2 liters/d. But that may not be enough in all patients, so 24 hour urine testing is always required.
Uric Acid SS
Urine pH
An obvious reason one needs such urine testing is to ascertain 24 hour average urine pH. In the main article on this site concerning uric acid stones, I offered evidence that urine pH is the main factor controlling uric acid supersaturation, and that is the same for ileostomy patients.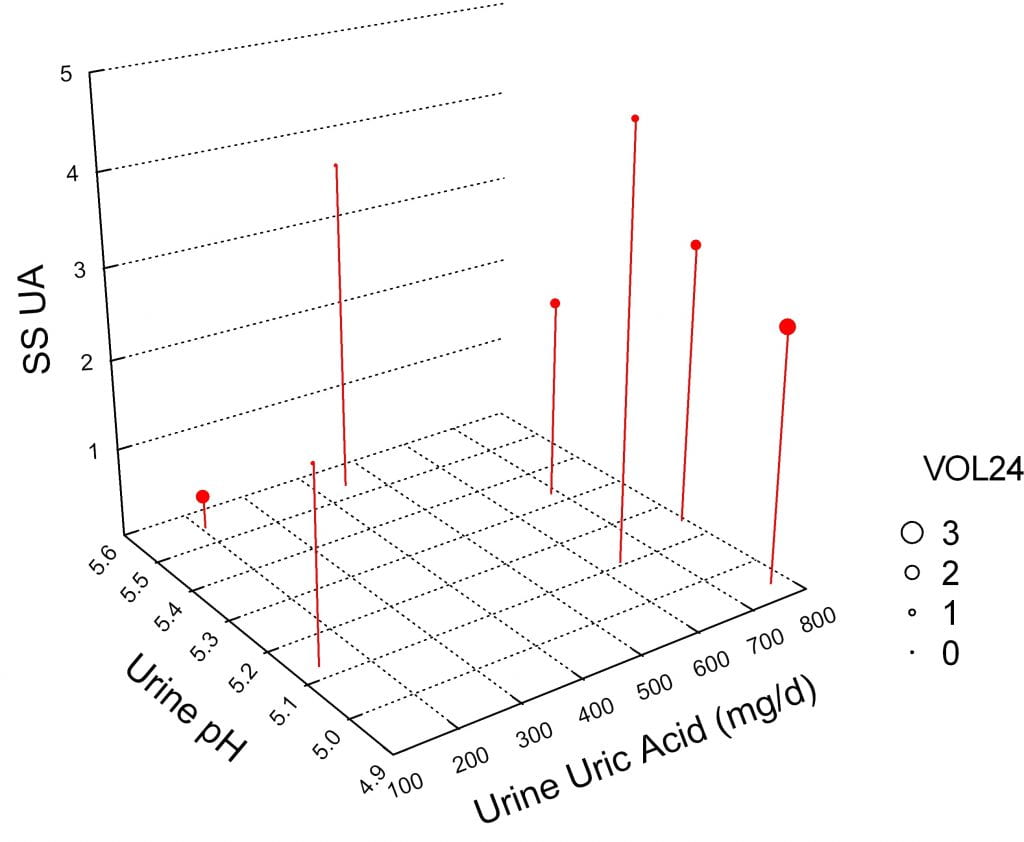
In the 3D figure to the right, uric acid SS is on the vertical axis. SIx of the SS points lie above 1, as on the graph just above, and one is below 1. This last had the largest urine volume (size of the symbol), among the highest urine pH, and lowest 24 hour urine uric acid excretion rate.
Uric Acid Excretion
The graph shows little correlation between the 24 hour urine uric acid excretion rate and uric acid SS, That is because urine pH is so powerful a determinant of SS. The two patients with very low 24 hour urine uric acid excretion (values at or below 200 mg/d) undoubtably crystallized uric acid either in the collection container or in themselves, as these values are below any expected from an adult.
Calcium Oxalate SS
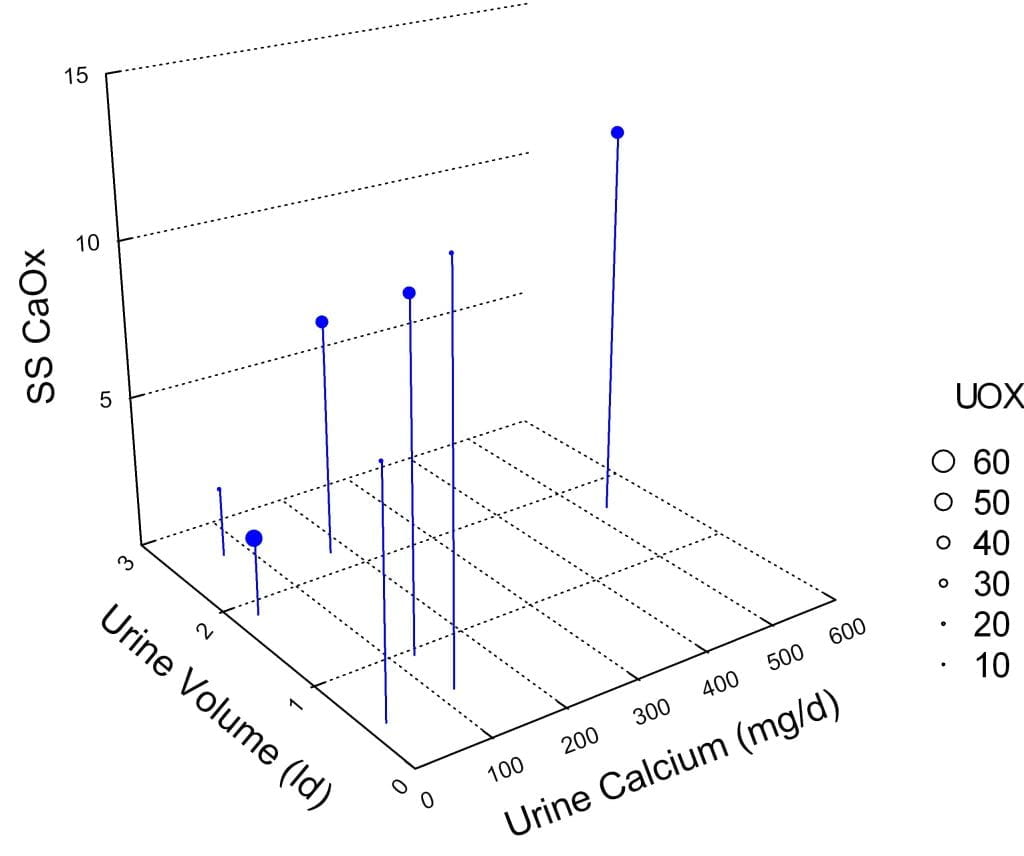
Urine Calcium
In general the lowest SS CaOx was in the patients with very low urine calcium (below 100 mg), but in fact all but one patient had a urine calcium excretion below 200 mg, the level at which Curhan first documents elevated stone risk in a general population. The one patient with very high urine calcium had very high supersaturation despite high urine volume
Urine Oxalate
As others have found, and we in a larger patient series, urine oxalate was not remarkably high in our patients – size of symbols. Moreover, urine oxalate had little correlation with supersaturation.
Urine Volume
As I have already shown, but in isolation, supersaturation was generally higher in the patients with low urine volume, with the exception of the one person with exceedingly high urine calcium.
Confirmation in a Larger Series
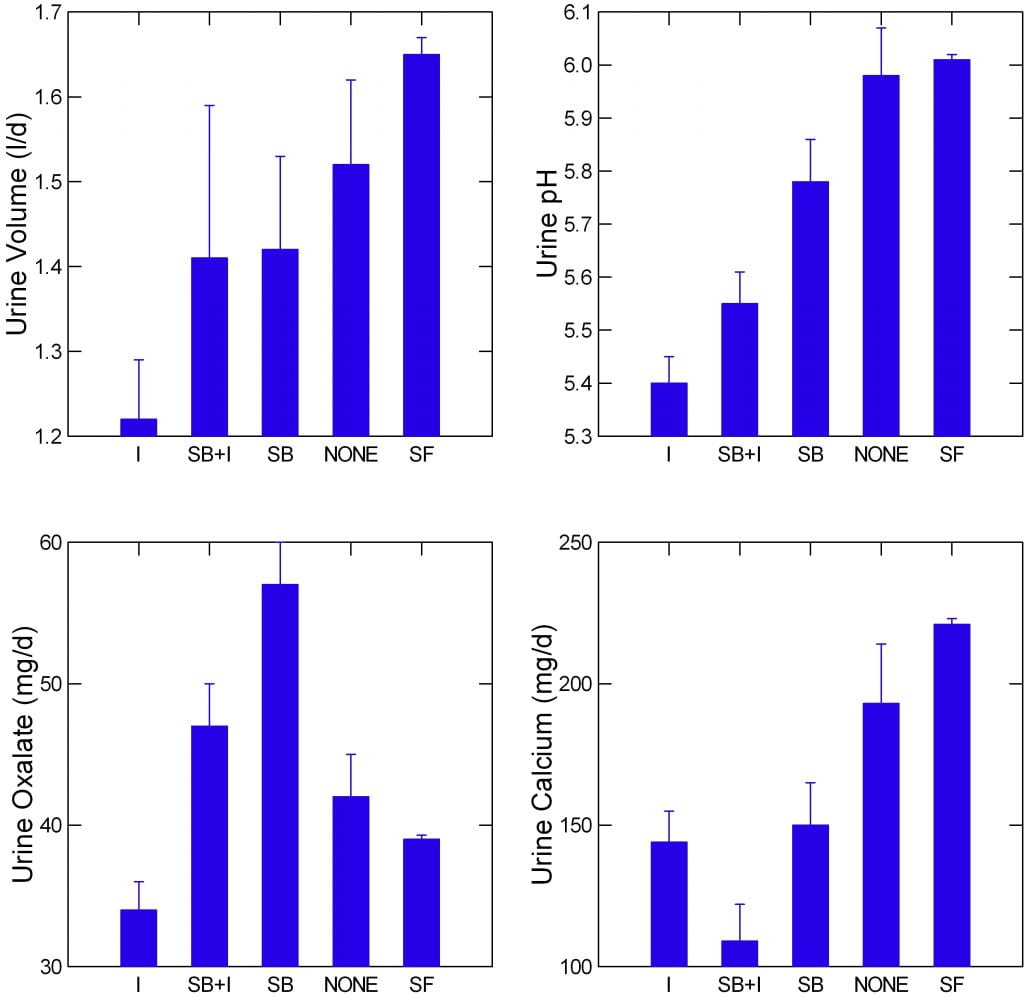 I have illustrated only the 7 cases we biopsied in order to demonstrate the tissue changes in ileostomy, but in all fairness I should show that the pattern among the seven is the same as that in our larger series of more routine cases that never were biopsied.
I have illustrated only the 7 cases we biopsied in order to demonstrate the tissue changes in ileostomy, but in all fairness I should show that the pattern among the seven is the same as that in our larger series of more routine cases that never were biopsied.
In this much larger series, ileostomy cases (I) are compared to those with small bowel resection and ileostomy (SB+I), with small bowel resection but retained colon (SB), with no surgery but bowel disease (NONE) and stone formers with no bowel disease at all (SF).
Urine volume and pH (upper two panels) of ileostomy patients are lower than any of the other groups. Of interest, urine oxalate (lower left panel) is also lower – presumably as colon is absent. Urine calcium (lower right panel) is not as remarkably divergent except as against stone formers without bowel disease. It is the ileostomy patients who also have small bowel resection who display remarkably low urine calcium having lost main areas for calcium absorption.
How Stones Form
Growth on Plaque and Plugs
 Stones form in the common ways we have found across a spectrum of stone diseases, as overgrowths on plaque or on tubule plugs.
Stones form in the common ways we have found across a spectrum of stone diseases, as overgrowths on plaque or on tubule plugs.
The upper left panel shows a papillum from a patient during stone surgery. The dark blob is a large crystal plug. The little inset shows a biopsy of this area scanned in a research high resolution CT instrument. The arrow points to the crystal deposit in the biopsied tissue.
All seven of our biopsy cases had plugs, between 1 and 26 plugs/mm3 of biopsy tissue. At the highest level, tissue is significantly replaced by plugs. The upper right panel shows a plug protruding from the opening of a tubule (at the arrowhead).
Panel C at the lower left shows a stone (double white arrows) growing over white plaque. The attachment site on the removed stone is the white region in panel d marked out by arrowheads. All stones that grow on plaque have these attachment sites that are always calcium phosphate (hydroxyapatite) even when the stone itself is calcium oxalate.
This stone was no exception. A micro – CT analysis of the stone shows mainly calcium oxalate – the iron grey mass. The attachment site (arrowheads) was hydroxyapatite, as expected.
So in a way ileostomy offers no surprises. Dehydration raises supersaturation, plaque forms, tubules plug, and calcium oxalate stones grow in the common way. Alkali loss lowers urine pH, and uric acid crystallizes forming stones.
Uric Acid Stones were Not attached
Growth on plaque or plugs applies to calcium stones. Uric acid stones were never found attached to plugs or to plaque. They were free in the urinary system. We presume that because urine contains a lot of uric acid compared to oxalate, and because uric acid can crystallize rapidly when urine pH is low, crystals form and somehow manage to stay in the kidneys long enough to form stones rather than be washed away in the urine.
Tissue Damage
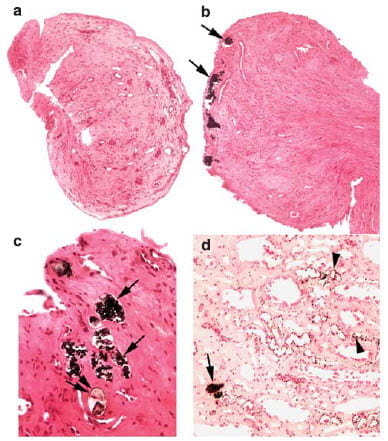
One might expect that tubule plugs damage the papillae and in fact they do.
The upper left panel labeled a shows minimal damage in one of the seven patients we biopsied. Panel b just next to it, shows a ring of plugs. A higher power view in c shows how the lining cells of the tubules are gone – damaged and lost, and around the tubules with plugs the tissue looks condensed because scarred. In panel D the arrowheads point to plaque growing as tiny beads in thin limbs of the loops of Henle, and a plug at the tip of the arrow.
Not shown here, a few collecting ducts were plugged in the renal cortex – the region that contains the glomerulae and is very sensitive to crystal injury. Cortex crystals are rare in common stone formers.
What Plugs Were Made Of
I have shown you how acid the urine is in ileostomy and for the obvious and well known reason that ileostomy fluid is alkaline because enriched with bicarbonate the colon would have absorbed back into the blood. The urine pH is low enough to produce uric acid stones, geological proof that low pH is common and enduring.
What, then, would you predict the plugs were made of?
I would have said uric acid, of course. But in fact that was wrong.
Plugs Were Calcium Phosphate
Many plugs stained with the Yasue stain meaning they contained calcium. Using high resolution IR scanning we found the crystal was hydroxyapatite – as in almost all other plugs studied to date.
But why?
The urine produced in these tubules is very acid, acid enough to produce uric acid stones, and stones themselves are calcium oxalate – indifferent to urine acidity or alkalinity, and uric acid. None have appreciable apatite.
All of the urine in a 24 hour urine collection comes out of the terminal collecting ducts of Bellini (BD). There is no other pathway out of the kidneys. That urine is acid and only one of our patients had any supersaturation for calcium phosphate – the other 6 produced a urine undersaturated for that crystal so it would dissolve. How, then, did apatite forms of calcium phosphate come to predominate in those very same tubules?
We guessed that somehow plugging began with uric acid, or even possibly calcium oxalate, cells were damaged, and local pH in the damaged tubules rose way above that of the bulk urine so whatever crystal began the deposit would dissolve in favor of calcium phosphate. Given that calcium oxalate will not dissolve if pH rises, this leaves uric acid as the main possibility.
Some Plugs Were Urate
Urate sounds like uric acid but is not. It is the salt of the urate ion with sodium or ammonium, in these cases, whereas uric acid is not a salt but the pure molecule essentially crystallizing with itself. These two urate salts were found in some plugs, as regions that did not stain with Yasue stain nor contain apatite when scanned by IR.
How Could Urates Form?
These two urate salts can exists at higher pH levels than uric acid, so they could coexist with apatite. But how either formed, urate salts or apatite, remains a mystery. Before crystals forms, these ducts produced a fluid too acid for urate or apatite. After crystals formed, damage from crystals could have raised fluid pH and permitted urate and apatite to form. The only crystals that could form at the low urine pH of ileostomy patients are calcium oxalate and uric acid.
The Uric Acid Theory
Obviously that leaves uric acid, and one asks if any uric acid was in plugs.
Unfortunately, the IR technique we used to identify the urate crystals and apatite crystals cannot identify uric acid itself. Uric acid produces no unique infrared bands as a signature. This leaves untested the theory that plugs begin as uric acid, damage tubules so pH rises, and uric acid converts to the two urate salts. It is a powerful theory because if true it means that consistent alkali treatment to prevent uric acid could prevent plugs and tissue injury but after tubules lose acidification because of injury alkali cannot undo the injury process.
The Calcium Oxalate Theory
Urine and therefore tubule fluid was supersaturated with respect to calcium oxalate, and surely this crystal was abundant in stones. Why not imagine it formed first, damaged tubule cells, and dissolved in favor of urates and apatites?
It is less likely than the uric acid theory.
To date calcium oxalate has been rare in human plugs, seen only in obesity bypass patients and primary hyperoxaluria, states of marked oxalate over excretion. Urine oxalate tends to be low in ileostomy patients and CaOx SS was not remarkably high compared to common stone formers whose plugs never contain calcium oxalate.
Dissolution of calcium oxalate is not very likely. It is a very insoluble phase, and conversion of calcium oxalate to apatite or uric acid has not been demonstrated very often even in vitro. More, the IR technique we used easily detects calcium oxalate, so even traces were absent in these patients.
So while possible, the calcium oxalate theory takes second place to the uric acid theory. Wanting is a method for micro-analysis of tissue plugs that can detect uric acid in the presence of urates.
Apatite and Urate Deposit Locations
Sometimes the apatite and urate deposits were together in one tubule, but more commonly they were separate. Those that did not stain with Yasue – no calcium – tended to locate in terminal collecting – Bellini ducts, whereas those with calcium were higher up, in the inner medullary collecting ducts. Moreover, tissue around ducts plugged with urates showed more inflammation, and tubules more signs of injury as compared with tubules plugged with calcium – apatite – crystals.
What Do We Say to Patients and their Physicians?
The problem of ileostomy stones is loss of alkaline fluid from the intestines. Kidneys adapt properly and form an acidic scanty urine.
Treatment Priorities
The low pH may well be of most primary concern because of plugging as an irreversible outcome from an initial uric acid deposit, so alkali treatment should be early and consistent with a goal of urine pH about 6. Because ileostomy causes sodium losses, sodium alkali may be useful; here 24 hour urines will be very valuable as a guide.
Urine volume is the other critical factor. WIthout any trial justification, I have come to favor glucose containing beverages. Sodium coupled glucose transport in the jejunum may improve absorption so fluid intake does more than increase ileostomy output. Usually, I have been able to achieve increases in 24 hour urine volume, often to 2 liters or more. But doing this is highly individual to each patient and physician.
High urine oxalate, often thought of in bowel disease related stones, is rarely an important factor given ileostomy. Likewise, urine calcium usually is not high. Nevertheless both need to be looked for and treated if present.
Testing as a Priority
Serum and 24 Hour Urines
This entire set of comments points out the critical role of 24 hour urine testing for sodium, calcium, oxalate, pH, volume – all of the factors used in evaluating stone formation. They are needed to plan treatment and monitor its course.
Ileostomy can cause acute and chronic kidney damage, and also cause metabolic acidosis or alkalosis, so serum measurements need to be perhaps more frequent than 24 hour urine collections. Kidney failure risk is particularly well documented in the period immediately and one year after ileostomy.
Kidney Stone Analysis
Likewise all kidney stones need be analysed to help assess the relative concern over calcium vs. uric acid stones. Even though 24 hour urine testing gives insight into stone cause, stones give insights into the actual urine supersaturations over a longer term average.
Timing of Treatment
Although I am perhaps speaking a bit out of line in terms of clinical practice, I certainly do begin alkali treatment after even one stone in a patient with ileostomy and not wait for another. This is because plugging is damaging and may progress without evident new stones for a time.
One might even question if prophylactic alkali were not unreasonable in anyone with an ileostomy. Lacking any trial data, I am of two minds. Sodium depletion is so common, and sodium alkali so relatively inexpensive – some sodium bicarbonate tablets might do – the benefits could easily outweigh any risk and cost. I do not indeed see non stone forming ileostomy patients, however, and therefore have no experience in this matter. Individual physicians can determine the issue on a case by case basis.
But immediately after ileostomy, acute kidney injury is specially frequent, and given low urine volume and pH are very likely uric acid crystallization is as well. One might want to use sodium alkali especially during this period. A trial might be of high importance for this matter.

Is it too much.or too little acid causing heartburn and burning in stomach for ileostomy
Hi Michaele, Ileostomy does not affect the stomach per se. Urine is too acid. But here, physicians need to be in charge of treatment. It is beyond what a patient can manage. Regards, Fred Coe
I have pass 3 stones since 10/26/18. this is not the first time I have pass stones. My urologist is stumped as to why I am doing this and they are so big 5-7mm stones and 1-2 on both kidneys. I have short gut syndrome and a full permanent Ileostomy. It was caused by a server infection of diverticulitous.
My nutritionist is having me drink a sodium based (Gatorade watered down) electrolyte drink and I am consuming about 96-120 oz a day.
My question is would this article help explain to my doc why I am getting these stones. I am his only patient ever with a Ileostomy.
Thanks
Greg
Hi Greg, Your physician might well find the article useful. It is written at a high level and has references. Regards, Fred Coe
I am a urologist in Georgia and have a patient with recent ileostomy for benign disease. No prior history of stones, but now two months after ileostomy, bilateral stones. Plan to start sodium bicarb, how do you dose and administer?
Hello, Doctor Gilbert; I use sodium bicarbonate because these people are usually sodium depleted. I start with 2 ten grain tabs (14 mEq) 3 times a day, timed with meals if needed for symptome, and recheck pH and citrate. Often I need more, sometimes much more. FLuid replacement is critical, of course, and I find that sport drinks with glucose may work better than plain water. If your patient cannot stand the pills you can use oral sodium citrate as a liquid supplement – I find it expensive and most people hate it. Regards, Fred
I have a long time ileostomy patient and have recently been diagnosed with stage 3 kidney disease. My 24 hr urine calcium was so low it could not be determined and the 24 hr citric acid/citrate was also very low. In the past I passed some sand like crystals that were determined to be uric acid stones but I’ve never had any large stones and haven’t noticed the sand in over a year now. Is this what is causing my kidney disease?
Hi Vicki, Ileostomy causes stones because of low urine volume and acid urine. So, indeed the gravel would occur from it. Your physician might want to add some alkali to prevent uric acid crystallization. This can occur in the kidneys and perhaps contribute to some reduction of kidney function. Besides, loss of alkali from ileostomy causes systemic acidosis that possibly injures kidneys and surely reduces life quality. Since all ileostomy patients have reasonably low urine sodium losses, sodium bicarbonate might be a reasonable and cheap approach. But only use it with your physician’s agreement. Regards, Fred Coe
Hi Dr Coe,
I shared your article with My nephrologist and she found it very interesting. I am going to start on the soda bicarbonate as you suggest. My Dr wondered if sodium citrate would be better? More expensive tho and not covered by insurance. I wondered what your thought are on this? It it more effective given I have little to no urine Citric acid? Thank you so much for your help.
Hi Vicki, I favor sodium bicarbonate because ileostomy causes sodium alkali wasting. If your serum or 24 hour urine potassium is also low, then you could use potassium chloride as an inexpensive substitute for potassium citrate whose price has been raised excessively by profiteering companies. The sodium bicarbonate will raise urine pH, give you needed alkali, and cost almost nothing. Be sure and measure serum and 24 hour urines to check the dose is right for you. Regards, Fred Coe
Hi, could I just check that it is this type of tablet you are suggesting? I am in the UK so any help much appreciated. ,(if anyone has suggestions for a UK supplier that would be helpful) Thanks, Jo https://safrel.com/products/safrel-sodium-bicarbonate-antiacid-650-mg-10-grain-1000-tablets-for-relief-of-acid-indigestion-heartburn-sour-stomach-upset-stomach-value-savings-pack
Hi Jo, sodium bicarbonate is ideal for ileostomy as the fluid loss is precisely that. Regards, Fred Coe
Fredric Coe, My husband has a permanent ileostomy for 8 years now. He has been having problems with kidney stones, passing more then 100 now since 2015. He was just hospitalized for an 8 mm stone in his ureter and a 9 mm stone in his kidney. They are saying that the stone is uric acid and not calcium. He is also listed on the discharge papers from a recent hospital visit as stage three kidney disease. We had not been notified until this weekend that stones and ileostomies go hand in hand. What is the best thing for him to drink as Gatorade causes him to form stones. He tries to drink plenty of water however this does not seem to be the answer either. The doctors did start him on sodium bicarbonate this weekend. Hoping this will help, but want to know if there is a way to improve kidney function and what he should be drinking.
Thank you!
Hi Kristin, I am afraid ileostomy is indeed a terrible risk for stones. Given uric acid, alkali seem crucial and as the article posits sodium bicarbonate is the most obvious and safest form. Of course his physicians are in charge here as ileostomy and CKD both require expert care. I see his physicians have begun this treatment and the goal is a pH above 6 in the 24 hour urine. Voiding urine pH dipsticks are a help here. Regards, Fred Coe
I have had an ileostomy for 20 years and had 2 large kidney stones in the last 6 years. Would drinking the O.R.S.hydration tablets help prevent them.
Hi Charlotte, a brief Perplexity search says these tablets are per tablet sodium (about 277mg), potassium (~193mg), glucose (~3.27g), and sometimes vitamin B2. Dissolved in water they should be excellent except there is not a lot of alkali. Ileostomy losses include alkali loss. SO the pills are alright but your actual hydration should be more balanced and this is what your physicians need to supervise so as to maintain a urine pH near 6 and a blood bicarbonate in the normal range. Best, Fred Coe
Dear Dr. Coe,
Thank you for this information. When will your book be available for purchase?
This is a new arena for me and it helped give context to see that there is a connection between having an ileostomy and kidney issues. I stumbled across your site tonight and I’m going to forward the link to my doctor. I have an ileostomy and recently passed my first (and, I hope, only!) stone. The urologist explained that my stone analysis showed I had a calcium oxalate stone that was large enough that I was lucky to pass instead of needing surgery. I had no idea I had a stone before suddenly experiencing the pain of passing it. And, to my bewilderment, the doctor said that I needed to hydrate more and change my diet, including eliminating broccoli, spinach (two of my favorite foods), chocolate, beer & red wine. I eat a very clean diet, rarely drink alcohol, and am a huge water drinker. I asked the urologist if having an ileostomy might affect my conditions for creating another stone since my fluid absorption is compromised, I drink a ton of water, and often still feel dehydrated. He said yes and recommended lemonade. Do you agree? Will your book include any dietary/hydration recommendations? I also take Imodium every day and am wondering if there could be a connection. Thank you and please let me know if you need any other participants for your research.
Hi Sharon, as the article points out, urine oxalate is low in ileostomy so low oxalate diet is not useful. I would advise treatment as in the article, sodium alkali will be ideal and could be simply sodium bicarbonate pills OTC. But your physician has to see to things and do periodic testing as ileostomy is serious. As for the book, I have not planned to make it into a free standing item. I have done a lot of books, all for physicians. But perhaps you are right and I should pull this one together. In any event try to pattern your treatment as the article says – it is a pretty good review of what is known. REgards, Fred Coe
Thank you so much! Perhaps you could make it easier on your end to publish and sell as an ebook? In any case, I am grateful for your contributions.
As Dr Coe mentions, I am not sure why the doc is recommended a low oxalate diet here. Do you still have a colon? My experience is not all docs know the subtleties that Dr Coe is aware of.
Yes, no colon no elevated urine oxalate. Fred
Thank you for your reply to my previous question. Next question: will it help my kidneys, in the mean time, to drink a glass of water with tbsp. Baking soda?
Hi Michaele, Yes; in ileostomy sodium bicarbonate pills OTC variety will do, can raise urine pH. Because you probably lose considerable sodium from the GI tract, the extra sodium load is not likely to be a problem. Of course your physician is in charge, so be sure S/He approves. Check urine pH to be sure it is in a good range – above 6. Regards, Fred Coe
I am finding what feel like small, sand-like crystals in my iliostomy bag. My urine output is minimal, often days with no output and I have a continually swollen lower leg/ankle/foot. Could the crystals I find in my iliostomy bag be from my kidneys?
Hi Lynn, They are probably from your kidneys. You sound terribly dehydrated, and having no urine for a day is alarming. Be sure your physicians check your blood levels, soon, and get far more hydration. With ileostomy high sodium fluids – soups – and lots of water are needed. Sodium bicarbonate tablets, too. If your description is accurate, your physicians need to intervene. Regards, Fred Coe
Wow, I hope you are still with us Lynn. The two times in my life that I went for a day unable to urinate it turned out I was in renal failure. I had to spend weeks in the ICU coaxing my kidneys back to life, and at first it didn’t look good at all. Do not mess around with these symptoms! Best hopes and wishes, Frank
Dear Dr. Coe,
I’ve had an ileostomy (with rupture and peritonitis) since age 13. I’m now 66 and kind of surprised I’ve made it this far. Since my mid 30’s I’ve had a steady stream of calcium oxylate stones. I’m half way through getting the largest stone ever, about one inch diameter, removed right now. It’s taking two procedures with a ureter stent in for about a month and a half. (Yuk.) I assume it got so large because it was firmly attached and never really bothered me, over almost two decades. Then there’s a half inch stone waiting in the other kidney. It’s a terrible process to go through. My question is this: I get wildly divergent advise concerning dietary calcium. Some say it has absolutely no effect on stone growth while others say it is downright deadly for me. Do I really need to completely avoid calcium? I love my dairy products. Thank you, Regards, Frank
Hi Frank, as the article points out, ileostomy reduces urine volume and pH, fostering CaOx and uric acid stones. Alkali to raise pH is valuable because it can raise urine citrate which inhibits stones. Diet calcium has little role in that urine oxalate usually is low, and calcium loading will not lower it further. Of course increased volume is important, and if you use sodium based alkali the sodium will help absorption of fluids that contain glucose. So one might want to use such fluids and alkali. The article details all this. Low calcium diet has no place at all. But I say all this without having seen your particular data, which may not follow the common pattern. Your physicians have done so, and their opinions weigh far more than mine. Regards, Fred Coe
My husband has an ileostomy for 6 months now. 2 months after his ileostomy his kidney function went way off with high creatinine , low eGFR and high blood calcium. His BUN was just above higher normal. He had protein in urine. They put him in the hospital for a week and gave him lots of IV. His levels became normal after that and stayed normal for few months. Now we tested his kidney function again and creatinine has again gone back up and eGFR has reduced. He usually drinks 3-4 liquid IV’s for electrolytes.
Will taking sodium bicarbonate help him? Before his ileostomy surgery his kidney function was always normal.
Hi Smitha, After ileostomy risk is high for acute kidney injury. Some is from uric acid crystallization in the kidney and potassium or sodium alkali is very valuable to prevent this. Some is from profound dehydration, especially if NSAIDS – like Motrin – are being used for pain. His physicians are no doubt taking all precautions to avoid more episodes as they do threaten kidney function. So, yes, sodium bicarbonate is a very good idea to discuss with his physicians. Regards, Fred Coe
What great info! Thank you so much. I am a clinical nutritionist (MS, CNS) who had my lower ileum and all of my colon removed due to volvulus last year. Recently, some signs of kidney issues have raised their head so this article is very timely. Consistent with most of the research I have seen, I tend to prefer the WHO-based oral rehydration solution (ORS) over the high sugar things like gatorade (of course some glucose needed to help carry the sodium into the cell but too much just promotes diarrhea). Recently. I also started adding partially hydrolyzed guar gum (PHGG) to the ORS per this article https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5026008/ . In addition, PHGG has been shown to benefit a number of conditions including those involving the small intestine https://www.sciencedirect.com/science/article/abs/pii/S0022346819305883. I should note the use of PHGG is my personal experiment and I may be off base in considering- that said, I thought it was worth a try. I also get IV hydration at a local infusion center once/week.
Hi Rosemary, Thanks for the information. I have not included it in my ileostomy article. Usually things adapt with time so you will not need IV hydration. I hope so. Supplemental sodium bicarbonate is very useful because low urine pH really promotes uric acid stones. It should be easy enough in that ileostomy causes massive sodium depletion. Ask your physicians. Be sure and get a kidney stone 24 hour urine study to assess risk. Regards, Fred
Dr Coe- Please note I am a CNS-candidate not a CNS. Still a ways to go for that.
Thanks so much for suggestion re: 24 hour kidney stone study. Will discuss with my GP. The GI specialists and surgeons don’t seem very engaged in this regard. Really have to be proactive!
And, of course, thanks for researching this topic
Hello. I Have had a permanent ileostomy due to alternative colitis since age 23. I am now 72. Recently diagnosed with stage for kidney disease and frequent stones. However my stones are ammonium. Would your advice also apply to these stones?
Hi Nancy, Ileostomy can promote ammonium urate stones, and the best treatment is adequate sodium bicarbonate to neutralize the acid load caused by alkali loss from the ileostomy. Acid loads cause the kidneys to produce a lot of ammonia, and this promotes such stones/ Sodium bicarbonate pills are OTC and cheap and a usual dose is 2 10 grain pills 2 – 3 times a day. This is, of course, for your physician to decide about, as I do not know your situation, so perhaps you might mention this to her/him and do what she/he things best. Likewise, one does not use this approach without preliminary 24 hour urine testing to determine exactly what is in the urine. Of importance, given some kidney disease, neutralization of the acid load is likely to protect against progression of more kidney damage. Regards, Fred Coe
Hi Dr Coe: I am curious regarding the timing of the sodium bicarbonate dosage. Is that best before, during or after a meal? Also, if some one eats more often (for example, I do better with a snack in late afternoon to keep weight up so have 4 meals/snack), would you perhaps spread the dosing out?
Hi Rosemary, Given the sodium bicarbonate is to neutralize loss of bicarbonate from the ileostomy it is best to take it throughout the day, maybe 3 or 4 times a day as needed. Needed means enough to correct the urine ammonia and pH to normal. Regards, Fred Coe
Thanks so much. This is very helpful to know.
Hey Dr Coe. Sorry for all the questions. What are the implications for taking sodium bicarbonate in terms of HCL and its role in digestion and antimicrobial functions. Could it interfere with those functions by neutralizing HCL?
Hi Rosemary, It could, but only briefly as the material is rapidly absorbed. I would not worry about this. Regards, Fred Coe
Thank you. Sorry to post the question twice.
Hi Dr Coe: I was just wondering if the oral ingestion of sodium bicarbonate could interfere with hydrochloric acid (HCL) and its role in protein digestion and as an antimicrobial in the stomach. With that in mind, I have been using a bit after meals but would love your thoughts on it. Thanks
Hi rosemary, I think I answered this. Perhaps you might want to move the pills away from your meals, which is fine for their effect. Regards, Fred Coe
Hi Dr. Coe. I’ve had an Ileosomy since ’97. Starting getting symptoms of kidney stones in ’02. Started passing Uric Acid stones in ’06. Have had multiple series of them since then, with 15+ plus stones per series. Also my weight has ping-ponged between 220lbs and 170lbs while going through these series. (I lose weight and form stones. Lots of fluid loss. Doesn’t matter if I guzzle water all day. The more I drink the higher the bowel output. Output resembles chicken broth in consistancy and color.) Have had 3 Lithotripsies and a Perc.
Was proscribed K Citrate in 2013 and felt like I was losing my mind after a few months. My bloodwork was fine when taking it, other than elevated Liver Function. Urine is always very concentrated. Was proscribed anti-anxiety meds while on K Citrate in ’13 and ended up having a suicide attempt.
Stopped taking Citrate again until June ’19, after my latest Lithotripsy. Started passing stones and losing weight again. Have passed approximately 20 stones and innumerable sandy particles since July ’19. Largest was 9.4mm and another 7mm showed up on MRI in Jan ’20 which hasn’t passed yet.
Had to stop taking the K Citrate a few months ago. Was getting heart palpatations and feelings of what I can only describe as ‘doom’. Waking up gasping for breath and my heart racing. 30 minutes to an hour after taking it, it feels like my heart starts pumping harder (not faster, just more force per pump) with occasional flutters or skipped beats.
Can’t get a hold of my Urologist because of pandemic. Feel a great pressure to take the citrate again because I feel the stone every day and have been passing occasional fragments.
Wondering if you know of any negative interactions between taking K citrate and underlying mental illness, or if you’ve ever had patients who discribed this sort of scenario before. I had been taking 1 pill daily of Webber 99mg High Absorption Potassium Citrate. Increased to 2 per day in December ’19 because the stone frequency was not dropping. Stopped in Feb ’20. Not sure what to do 🙁
Hi Tony, given an ileostomy and intolerance to citrate, you can use OTC sodium bicarbonate pills. Two 10 grain pills give 13 mEq of alkali, so 2 pills 3 – 4 times a day will raise urine pH enough to abolish uric acid stones. Use pH paper or 24 hour urine pH as your guide, aim for pH 6 – 6.5 and uric acid stones will end. Regards, Fred Coe
Hi Dr Coe. I have a j-pouch and form uric acid-stones, now going on 17 years without much success using potassium citrate. I may have prevented some stones but I have never been able to dissolve existing stones. Potassium citrate with water also contributes to diarrhea which can be problematic for me. I also have ADPKD so I am not sure if I can use sodium bicarbonate. I’m still looking into that option as that is the most appealing.
I believe you mentioned apple cider vinegar can raise urine pH and may be a viable option. In my own experimentation I haven’t seen urine pH rise after consuming vinegar and I wonder if this is a dose-dependent issue. I can’t find much information on this approach, unfortunately.
Are there any other options to increase urine pH besides potassium/magnesium citrate, sodium bicarbonate and lemon/lime juice?
I’m also curious of this is an element of timing at play. With an ileostomy or j-pouch drinking fluids is considered to be a poor practice as it causes GI and diarrhea issues. Would it be ok to take the potassium citrate several hours after a meal? I’m also wondering if it might be acceptable to simply flush the kidneys with potassium citrate 1x per day before bed, as an alternate example.
Thank you for writing this article and for the help. Best, James
Hi James, Usually ileostomy causes so much sodium depletion one can use sodium based alkali, so sodium bicarbonate tablets might be fine, The 24 hour urine is ideal here as it gives net sodium loss which is what your kidneys ‘see’. As for timing, I would generally opt for 2 10 grain NaHCO3 tabs perhaps 4 times a day, assuming urine sodium remains reasonable and your renal function tolerates it. Your nephrologist has to be involved here, and may have reasons to disagree. Always do what she/he advises. Regards, Fred Coe
Hi,
In Feb 2013 I had my colon removed due to Ulcerative Colitis. I had 2 trouble free years. Then in early 2015 I started noticing what looked like hundreds of tiny gold flecks in my pee. And it would burn when I pee’d! That summer I had my rectum sewn shut (real fun). While recovering I had to pee in a container (whole other story). I noticed one day shortly after surgery that there was a large piece of..something in the container. Kidney stone! I felt no pain. And to this day I never have.
Immediately made an appointment with a Urologist. I did a 24 hr urine test. Was told based on the results to start drinking about a gallon of water a day and to add lemon juice. I followed the orders. And have never stopped for the past 5 years.
I had another 24 hr urine test a year later in 2016. The results of this one are below. And an ultrasound which showed 1 tiny stone in one of my kidneys. Advice was the same. Keep drinking the water and lemon juice.
Well, the stones have never stopped appearing in my urine. If I were to skimp on the gallon a day, for even 1 day, I’ll see tons of tiny flecks in my urine. Then after drinking a gallon of water they all seem to clear out. And I may see 1 or 2 tiny ones here and there if I pee into a container to check.
Coming across this article as alarmed me. I don’t know if my Urologist has been treating me with the context of having an Ostomy in mind.
Has permanent damage been done over the last 5 years in spite of me drinking over a gallon a day of water almost every day? I never have felt any pain from these stones. At all. I am 39 and in otherwise great health. Very active.
Would electrolyte packets be of any use? I do add extra salt to my foods but perhaps it’s not enough? I don’t want to link products here but there is one newer product on the market that has 1000mg of sodium, 200mg of potassium and 60mg of Magneisum. Sugar free. You can google “LMNT” to find it. Would something like this possibly be useful? Or dangerous?
I still have stones every single day. But don’t feel them unless I let myself get a little behind on the gallon a day of water. Then it will burn when I pee. But that’s all the pain I feel.
Thanks for reading and sharing your expertise! I have just made a new appointment with my Urologist to discuss this article. I sent it to him and asked him to read.
Litholink Summary results Sept 2016:
Urine Volume: 4.32
SS CaOx: 2.70
Urine Calcium: 397
Urine Oxalate: 26
Urine Citrate: 603
SS CaP: 0.35
24 Hour Urine PH: 5.805
SS Uric Acid: 0.60
Urine Uric Acid 0.870
Hi Douglas, You have very high urine calcium that may be fostering stones, and your urine pH – usually low in ileostomy – is rather decent mid range. But so much is missing I cannot say more. What were the stones made of? Uric acid, calcium oxalate or phosphate? Why is your urine calcium so high?? The high fluids are alright but inefficient because any slip in fluids and stones will come back from the high calcium. That calcium is high enough for concern as to cause, and I would ask your physicians to figure it out and reverse the problem. Regards, Fred Coe
Hi there – I came across this site in hopes of finding some help for my younger sister. She is 37, primary progressive MS. She has had her bladder removed and has both an ileostomy and colostomy. She has been suffering from Staghorn Calculus. She gets severely sick, and is hospitalized. They end up diverting the urine while getting whatever infections popped up with it under control and then remove the Staghorn very carefully. She is back in the hospital today with a new one after just having surgery on the 29th of December. She has a very hard time consuming enough liquids due to swallowing’s issues and intolerance. I just wish there was something they could come up with to help her avoid some of this agony. Any advice would be greatly appreciated.
Hi Amanda, I presume she must have lost bladder control from MS, needed catheters, got infected, and had all of these procedures – this is just a guess. The stone composition is crucial – I guess they are struvite, from infection, but I have seen uric acid make large stones after ileostomy and they can be prevented. If they are struvite, it is in situations like this one sometimes uses acetohydroxamic acid, to stop them. Given the ileostomy and dehydration, one may resort to parenteral fluid replacement, which is workable. Regards, Fred Coe
How do you perform a 24 hr urine on a patient with a illestomy? I pee constantly and am not aware when my appliance fills up.
Hi Darlene, Ileostomy does not involve the urinary tract so the appliance should not contain urine. All of the 24 hour results in the article arose from patients who collected them. Fred Coe
Hi Dr Coe, I had a 4cm x 2cm staghorn stone in my left kidney, removed by pcnl surgery this year (2021). Stone was analysed and found to be Calcium Oxalate Monohydrate.
I also had a small bowel resection in 1992, I was wondering if the stones could be a result of the bowel surgery? If so what can I do to prevent the stones re-occuring?
Hi Stuart, I am rather sure it is the small bowel resection and that you have abnormally high 24 hour urine oxalate, and perhaps low citrate, pH, and volume. You need a full evaluation and treatment to prevent more stones and also because oxalate poses a risk for kidney damage. Here is a good link to where to begin. Regards, Fred Coe
I am 48 and have had a permanent ileostomy for three years. The last two years I have been passing sediment, many small kidney stones, and have had three laser lithotripsy procedures to deal with larger stones. The largest was 12mm. I had a lithotripsy yesterday for my left kidney and I will need to have another laser lithotripsy in a few weeks for my right kidney. My urologist has requested 24-hour urine stonerisk every 3-months for a year. The consistent issue has been low urine volume and pH (as you have noted in your work). I am not a doctor, so I am doing my best in reading/understanding your research. We tried potassium citrate pills, but they came out in the ostomy bag within an hour. I am now adding potassium citrate liquid to water. Getting urine volume up is difficult due to the ileostomy. GI has suggested 6-8 Imodium pills a day to slow output. I see discussions from other comments on this page regarding sodium bicarbonate pills to assist with the pH issue. Is there anything else that can be done? It’s good to know I’m not the only ileostomy patient with this issue, but I am nervous that my life will be 2-laser lithotripsy procedures a year. Any thoughts appreciated.
Hi Eric, Sodium bicarbonate is the best and cheapest way to raise urine pH and stop uric acid stones in your case. Ileostomy causes sodium bicarbonate losses so the pills just add back what has been lost. My usual is 2 10 grain pills (this is the common OTC size) 3 times a day and check a 24 hour urine in a few weeks to see if pH is above 6. The low volume can lead to other kinds of stones, but that is not common. Regards, Fred Coe
Does sodium bicarbonate count towards total sodium intake? In other words. If I am trying to reduce my sodium intake from food to 1500mg a day. And I then take one 650mg pill of Sodium Bicarbonate. Did I just boost my sodium intake to 2150 for the day?
Hi Douglas, a subtle question. Sodium bicarbonate does not raise blood pressure as does sodium chloride, and I do not think it increases urine calcium. On the one hand sodium will increase calcium loss, on the other, and by another mechanism, the bicarbonate will reduce urine calcium loss. So although you would increase sodium – as the bicarbonate not chloride salt – the effect will not be the same. Regards, Fred Coe
Dear Dr Coe,
This is the most informative sIte I’ve come across. I am a chronic calcium oxalate stone former, starting at age 30, but which have increased since having a permanent ileostomy following total colectomy for UC 11 years ago, I am now aged 60.
My local service here in the UK have been overseeing my care but I’m being treated as a normal stone patient with the recommendation made that I increase my citrate intake by drinking lemon juice on a daily basis.
Do you know of a UK physician with a similar in-depth knowledge of the issues pertaining to ileostomy patients such as I that I might be referred to?
Thank you.
Hi Matthew, as you see from the article ileostomy is its own world – GI sodium alkali losses dominate the scene with very low urine pH, low volume, low sodium, and real risk of kidney damage given any dehydration added on to the Ileostomy. I find simple sodium bicarbonate pills are best as your urine sodium will be low, and uric acid eventually shows up in stones from the low pH. Low urine volume is almost always present. Prevention is always expected, however. Regards, Fred Coe (PS, I guess I do not know anyone there right now to recommend, but UK does have a lot of excellent stone physicians, I am sure.)
Dear Dr. Coe, I have had a permanent ileostomy since 2002. In 2015 I discovered I had kidney stones too numerous to count. Since then I have had several surgeries to remove kidney stones but they keep forming. 24-hour urine collections show I have super low citric acid (as of today 52 mg) although I have been taking potassium citrate (in liquid form) for several years. My magnesium and ammonium are also consistently low. I drink lemon water and lemonade every day. Since August 2020 I have had a stricture in my left ureter that will not heal so I have a stent in place all the time, which requires surgery at least every 6 months to replace. Because I have had arthritis since I was 2, I have had numerous joint replacement surgeries so have no veins anymore and a fused neck which makes intubation for operations difficult and risky. My surgeon just finally admitted earlier this year that my ileostomy is the problem (after many years of saying he got all the stones out); I had to suggest that theory to him first. Is there ANY change I can make to my diet that would help? Should I be seeing a nutritionist? I cannot have these constant operations for the rest of my life. Please help! Thanks from a lifelong patient, Allison
Hi Allison, as the article documents, the problems from ileostomy arise from low urine volume and very acid urine pH. Urine Citrate is always low because of the acid load. The ileostomy causes sodium losses so sodium bicarbonate tablets OTC are usually better than potassium citrate – and cheap. Ask your physicians. I use 2 10 grain tabs 3 times a day for most patients. The kind of stone matters a lot. Many are uric acid and will stop when alkali has been taken. Some are ammonium acid urate, and some calcium oxalate – from low volume. See what your physician thinks. Nutritional counseling needs to focus on beverages that are absorbed in the small bowel – these usually have sodium and glucose in them. Regards, Fred Coe
Hi dr coe
Due to having Spina bifida I have had an urostomy since I was 5. I also have been on laxatives since then . Now in my 50s I’m starting to feel aching in my right kidney and most of my life I have had issues with smelly urine. All scans suggest I’m fine but I don’t feel fine.
I have been told I have had high protein in my urine .
I will admit that I don’t drink a lot of water but have started making a more conscious effort to but I do love my coffee and tea which seems to have conflicted information on how healthy that is.
I’m waiting for a specialist appointment but as scans and other tests show no immediate issues I have been waiting months .
I am concerned so I was hoping you may be able to give me some advice at this stage and any concerns I should be aware of until I see my specialist.
I appreciate and look forward to your reply.
Hi Krissie, as scans have shown no stones, it matters what kind of scan. Only CT scans will reliably show sodium hydrogen urate stones, which would be a reasonable guess, or even uric acid stones. If CT scanning shows no stones, one should look for crystals in the urine as a clue – I realize the complexity of this. The urine protein is important – is there also blood?? The latter is a common reason for high protein. I would not hazard any guess apart from the above about what would be useful before seeing a proper expert. Regards, Fred Coe
I have a temporary ileostomy (7 months now). The reversal colon surgery is scheduled within a month. Recent CT scan showed (1) kidney stone (6mm ). No medical expert told me that the ileostomy is culprit for kidney stones. I have STAT appt with urologist next week to work on resolution. Would drinking alkaline water with lemons be helpful for now?
Hi Jan, Ileostomy is a cause for stones. Possibly your stone is uric acid – one can tell from the CT density which your physicians can easily measure. If so alkali by mouth may prevent more and also prevent growth. Alkaline water has no appreciable amount of actual alkali, lemons are a bit awkward. I suggest your physicians determine if it is uric acid and then use clinical amounts of potassium citrate. Regards, Fred Coe
Hi I have a spc.catheter, and a sns neurostimulator for Fowlers Syndrome.and embedded infections and had temp ileostomy for 2.5 years before having whole colon removed and perm ileostomy this year in May. I have suffered with constant stones since just before the first ileostomy and then they increased in occurance so every 2 months I suffer when passing them which can take over a week or two, agonising and my pain meds don’t touch it. Doc and hospital don’t do much just IV fluids as they’ve run out of options they say can’t have ablation due to having the SNS. I have moved docs they seem willing to help.so will share you’re paper with them here in wales, UK. I get the sand and fragments and many very small stones both kidneys more than large stones. I believe to be uric acid formed but not one person has done a 24 hour test so will ask for it to confirm. I cannot tolerate water with ileostomy as high output empty up to 12 times daily and drain approx 4 litres of urine per 24 hours. Water equals severe diarroeah and depletion. So I live on isotonic sports drinks approx 12 plus per day and drink gallons of lemonade when stones around to try and break down. Am I a good candidate to try your solution above, and any recommendations for the pain side of what works best. The stones caused my Fowlers to become painful also and increase my infections and often can get sepsis as result. Feel it’s the only condition of multiple that I can’t find a solution for. Great great paper thanks so much very grateful to have come across this.
Hi Samantha, I understand the stimulator for Fowler’s syndrome but not the ileostomy – which must reflect some additional disease. Ileostomy – as in the article – acts mainly via reducing fluid available for urine so urine volumes are low. Alkali loss creates an acid urine so stones frequently contain uric acid. Oral alkali supplements can help prevent the uric acid stones and are generally a good idea which your physicians might want to consider. I am afraid with so little information there is not much more I can suggest. Regards, Fred Coe
Hello Dr. Coe,
First of all, thank you for this vital information.
I recently had a colectomy this past december and later jpouch (as of May). It is my understanding the risk of acute kidney injury is now reduced due to compensatory mechanisms that occur several months after surgery.
I was curious about my kidney function and wanted to reach out to see if there is anything I can do to prevent kidney related complications due to chronic dehydration. What can I do? What type of specialist can I consult?
Hi Tomas, If there is a university based stone program near enough to attend I would do that. Telehealth is also possible. I agree that colectomy poses real stone problems. If there are no direct means for expert consultation consider the main issues are alkali loss with acid urine and uric acid stones, and fluid loss with low urine volume raising saturations and risk of COM and uric acid stones. Kidney function is assessed in routine practice by serum creatinine level. Regards, Fred Coe
Hi, I have come across your site simply by accident, but am very glad I have done so. Since my ileostomy operation I have had kidney stones and no-one has ever suggested a urine problem, just like many others, I have been told it is diet and to eliminate foods. I have, on Monday, got to go again for lithotripsy treatment and I would really like to discuss starting the sodium bicarbonate, anything to stop stones forming and avoid long term kidney damage. Please have you got a link for the sodium bicarbonate tablets. I live in the UK and can only find these:- https://www.healthleadsuk.com/sodium-bicarbonate-750mg-x-90-capsules.html?gad_source=1&gclid=CjwKCAiAt5euBhB9EiwAdkXWO1-dC5FasRfO7MlWssuZOa3KNTWiNwq2sBOeICenmgwcbdGpd6Pu3BoC3jEQAvD_BwE
Would these be ok or do you have a link that could be shared of the best tablets to buy.
I have one 4mm stone making its way down (which is what I going for treatment on Monday for). But from CT scan i had done this week there are 4 others in my kidneys. Please could you advise if these tablets will break any of the others down and or what I can do to get rid of them. Also what should I be asking my consultant on Monday to do? Urine tests, kidney analysis to see if my kidneys are covered in anything or damaged. Sorry I know there is a lot to answer her but I really would appreciate any advice before I go. Many thanks, Jo
Hi Jo, Indeed these are correct as noted in my other reply. Analysis of the stones is crucial as they can be uric acid or calcium oxalate. Maintaining fluid intake to counter loss is also crucial. Regards, Fred Coe
Dear Dr. Coe, i have crohns disease with an ileostomy & i used to have lots of small uric acid stones I could pass but now they are larger, not passing & i have to keep having ureteroscopies. I can’t take anything acidic due to gastritis & gerd but the drs. tried me on 1 tsp of baking soda a day. unfortunately it gave me nausea & diarrhea. the drug i could try allopurinol is contraindicated as i am on Imuran for the crohns. Is there anything you can suggest? I am 80 & don’t think i can withstand too many more surgeries. there is a great new therapy in trial studies called “burst wave therapy” which uses ultra sound
rather than shock waves, but won’t be available for a couple of years.
thanks so much for all you are doing ! sincerely Lari Doughty
Hi Lari, alkali are the sole treatment for uric acid stones. They are forming because of GI alkali losses. Sodium bicarbonate will cure the whole thing but you have tolerance issues and your physicians need to work with you to get the material to work for you. The 10 grain pills might work (you would need perhaps 6 a day) as each is small and doses can be spread out. Allopurinol is without merit against uric acid stones as the problem is urine acidity. Potassium or sodium citrate might work, one or the other dissolved in water. Potassium citrate is also in wax matric tabs, but these might not provide the drug to your blood. Cure rests on tolerance of alkali and surely this can be achieved. Regards, Fred Coe
Dear Dr. Coe, i have crohns disease with an ileostomy & i used to have lots of small uric acid stones I could pass but now they are larger, not passing & i have to keep having ureteroscopies. I can’t take anything acidic due to gastritis & gerd but the drs. tried me on 1 tsp of baking soda a day. unfortunately it gave me nausea & diarrhea. the drug i could try allopurinol is contraindicated as i am on Imuran for the crohns. Is there anything you can suggest? I am 80 & don’t think i can withstand too many more surgeries. there is a great new therapy in trial studies called “burst wave therapy” which uses ultra sound
rather than shock waves, but won’t be available for a couple of years.
thanks so much for all you are doing ! sincerely Lari Doughty
Hi, I believe I answered you another of your inquiries. Fred
Hi Doctor Coe. I have neuroendocrine cancer which resulted in me getting part of my colon removed. Since the surgery I have suffered with high amounts of oxalate kidney stones in both kidneys. Could this be due to the loss of sodium in my urine? I am thinking about starting on 20 grains of sodium bicarbonate 3x a day as a trial to see if this helps. Do you concur?
Regards,
Mark P.
Hi Mark, I presume it was a carcinoid tumor and the surgeon removed part of the ascending colon and the terminal portion of the ileum. The common outcome is increased urine oxalate because: bile acids are no longer reabsorbed by the terminal ileum but enter the colon where they raise oxalate absorption and also reduce absorption of water and alkali. I would obtain 24 hour kidney stone oriented urine studies and I suspect high oxalate + low urine volumes. The urine can also be overly acid with uric acid stone risk. It is not that sodium alkali is wrong it is that it is likely to be inadequate. Best, Fred Coe
Hello again, Dr. Coe.
You are correct on the surgery and diagnosis of my cancer. So, it’s been 6 weeks since I started on the sodium bicarbonate 20 grains 3x a day. NO STONES. It’s been quite a relief not to have passed a stone during that time, to say the least. I will continue on with this regimen and I will have by bi-annual CT scan in April which will hopefully show a reduction in the stone formation in my kidneys. Thanks much for the insights!
Mark
I had an ileostomy for chronic ulcerative colitis back in 1997. I’m now 73 and in relatively good health. I have had kidney stones – uric acid – for almost all the time since and had 7 lithotripsy surgeries. I had potassium citrate tablets prescribed, but they passed straight on through without dissolving – they only changed color. I read that they were designed to be absorbed in the large colon. Now I’m taking a potassium citrate liquid solution, and I experienced some positive results on the PH levels for about 2 years.
Now the PH blood levels are bad again, and the nephrologist has increased the dosage. Coincidentally, I have been experiencing changes in my bowel movements that are quite different from my relatively normal stools. My trips to the bathroom have about doubled, from 6-8 times a day to about 10 times, they have included a yellowish clear liquid (not ordinary diarrhea), and my bottom is extremely raw and sore. it burns and stings going in and really burns and stings coming out (Taco Bell syndrome).
Here’s my question – could the increase in the potassium dosage be responsible for these quite unpleasant symptoms? Is there an alternative?
Hi Gavin, Indeed. Possibly the GI problem reflects something in the small bowel so you might want your GI physician to weigh in. But certainly ileostomy can be treated with oral sodium bicarbonate pills, OTC and ideal in that they cause no GI issues of consequence. If you need extra potassium it can be supplemental but not the main engine of treatment. Two 650 mg NaHCO3 tabs provide about 14 mEq of base, so 6/d should be enough. Best, Fred Coe