
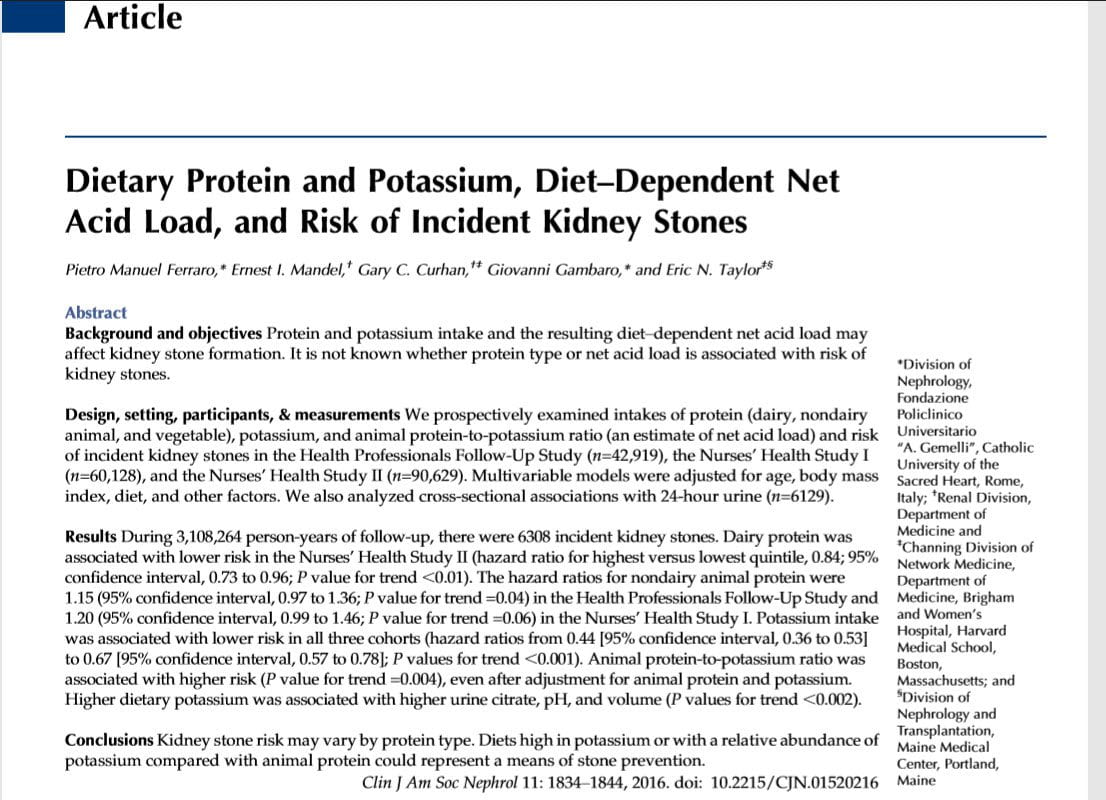
 Gary Curhan and Eric Taylor have given us many insights into how diet might influence kidney stone risk. I think this new article by them and their colleagues a great opportunity for close reading and practical use of a high quality research paper remarkably germane to the practice of kidney stone prevention.
Gary Curhan and Eric Taylor have given us many insights into how diet might influence kidney stone risk. I think this new article by them and their colleagues a great opportunity for close reading and practical use of a high quality research paper remarkably germane to the practice of kidney stone prevention.
What They Want
We all know that science is about discovery that enables us to do something, or know how nature does something. As a consequence, most of us ask what kind of science a paper is about – doing or knowing. But we also all know that this dichotomy is false because almost every scientist is after at least some of both. Likewise, that a paper lies between the two poles of doing and knowing – that, too is false. Far better to say any fine research has two separate gauges of new discovery: one about doing and one about knowing.
What about this one?
Do Something Research
Certainly diet is a massive factor in stone formation and prevention. Protein is a main player because it raises urine calcium excretion, some say because cystine and methionine are metabolized to acid. This has made physicians worry that too much animal protein worsens stones. This new work says no – it does not, but so long as it is within reasonable limits 0.8-1 gm/kg/d, or so.
Likewise for potassium in foods. Whether in plants or animals, potassium’s counter ion is not chloride, but rather anions that we metabolize to bicarbonate. So foods rich in potassium can act like potassium citrate pills, to put things in a crude if direct way.
Alkali loads lower urine calcium and raise urine citrate – good for preventing calcium stones. Acid loads the exact opposite.
Given these antinomies, one wants to know how food protein and potassium affect stone formation, so we can better use diet in stone prevention. Plants usually have an overabundance of potassium alkali over acid producing amino acids. Food protein of animal origin also has potassium – cells store it, but acid production from amino acids usually overbalances alkali production from potassium anions. So this class of food provides not an alkali but an acid load – the opposite of potassium citrate pills.
That is not all. Dairy foods come from animals but unlike meat have large amounts of calcium that can lower urine oxalate and reduce stone risk.
Since we can do something about diet, this certainly is ‘do something’ research. Given their differing proportions of acid and alkali generation, these three food sources may indeed affect stones and offer a chance to reduce stone risk by altering their relative proportions in the diet.
Know Something Research
The investigators also want to know something. All agree that protein metabolism gives rise to an acid load, or seems to, and likewise agree that acid loads increase urine calcium, lower urine citrate, and therefore raise kidney stone risk that varies with both. But not everyone agrees about protein and urine calcium. Some find that protein feeding raises urine calcium even when it imposes no acid load at all.
If protein raises urine calcium independent of acid load, potassium alkali from plant sources would not directly null its effects on stone risk, but only do so indirectly by lowering urine calcium and raising urine citrate from the action of alkali.
Perhaps, they reason, the balance between diet potassium – an alkali source, and diet protein – an acid source, might itself influence stone formation. If so, that would bolster the ‘protein as acid’ school of thought concerning stone risk. Although as we state the proposition one can see some difficulties with this test of the acid theory.
What They Already Know
Prudent scientists make sure they know what has already been discovered before setting out to discover something new. The authors are mandarin scholars.
The Main Facts
Curhan and Taylor – the architects of this work – do skilled epidemiology using three well established cohorts of women and men followed, by now, over decades. From their own studies they know that protein intake per se, not separated as to source, has a weak and variable association with becoming a stone former. Likewise, they know that increasing food potassium intake associated with progressive fall in risk of stones, but only in two of their three cohorts – so it has seemed not as vigorous an association as some others – urine calcium, oxalate, and citrate excretions, as examples, and urine volume itself.
Their Hypotheses
They imagine that diet protein raises stone risk by imposing an acid load that can raise urine calcium, lower urine citrate and perhaps cause other effects as yet to be defined. When evaluated by source, animal protein will most strongly associate with risk of stones because it imposes the largest acid load. Vegetable proteins offer very much less acid load, and dairy proteins somewhere in between.
They also imagine that with more observations, such as they now have, the potassium effect will be significant in all three cohorts because potassium alkali must raise urine citrate, a powerful defense against stone formation.
Because acid load is envisioned as stone producing and alkali load the opposite, they envision that the play between intakes of animal protein and potassium should strongly influence stone risk via modulation of net acid load.
Their Deductions
From this they must have deduced three necessary outcomes were one able to somehow assess effects of proteins and potassium on risk of kidney stones:
- Animal protein will associate with increased stone risk, vegetable protein will not, and dairy protein perhaps somewhere in between.
- With more observations, diet potassium will strongly associate with reduced stone risk
- The relationship between animal protein and potassium intake – the ratio of the two as they propose to test the idea – will strongly associate with stone risk.
What They Did
They did what they always do: Highly sophisticated epidemiology.
They have information from three cohorts, two of women (NHS I and II, nurses) and one of men (HPFS, physicians) followed for many years. Among them, some became kidney stone formers, most did not. All had filled out elaborate and well calibrated food diaries at least once before forming any stones. As well, the scientists collected 24 hour samples from the stone formers and a properly selected parallel set of well matched people who never formed a stone. From comparisons of diet intake and urine values between the two groups, and using a highly elaborated mathematical technique they extract the relative risk of becoming a stone former from various intake levels of the three protein sources.
Elsewhere on this site I have presented their work showing the effects of urine calcium, oxalate, volume, and citrate on this relative risk.
What They Found
Like most professional scientists, this group presents their answers in dense tables from which I have extracted and graphed what seem to be the key results related to their deduced outcomes.
Protein Intake

Animal Protein
Each bar shows the the mean relative risk at its top, and at its bottom the lower 95th percentile for that risk. For clarity, values above 1 (the dashed horizontal line) are lighter, those below deep red.
Contrary to prediction, risk does not vary significantly with animal protein intake. I show here the pooled values for all three cohorts, but results are essentially the same for each one taken separately. At the highest quartile of animal protein intake the bottom 95th percentile does not go below 1, so the relative risk is significantly increased. But increasing amounts of animal protein do not create increasing risk of stones (p=0.2).
I plot their multivariate corrected pooled values adjusted for BMI, presence of diabetes or hypertension, use of thiazide diuretics or supplemental calcium, and for intakes of fluid, sodium, potassium, fructose, oxalate, phytate, alcohol and all other types of protein.
As they do not give intake quartiles for pooled values, but values in the three cohorts differed only by small amounts, I used those for the NHS II cohort because they lay closest to the bottom of the table above the pooled values.
Vegetable Protein
Vegetable protein had no effects, so I omit graphing them from the supplemental tables.
Dairy Protein

Because in general this form of protein lowered risk slightly, I plot the mean risk ratio at the bottom of each lighter bar and the upper 95th percentile at the top.
The highest quartile of intake has an upper 95th percentile below 1 and therefore is significantly protective, but overall as a trend, rising amounts of dairy protein did not confer progressive amounts of protection as is obvious from the graph (p=0.06 for the trend).
As in the prior graph I have plotted the fully adjusted values from the pool of the three cohorts. This time I used diet intake quartiles from the male HPFS cohort – for variety. Note how much smaller are intakes of dairy than animal protein – about 4 fold.
Their Protein Hypothesis
Falsified by Their Data
Their experiment falsifies a necessary prediction of their hypothesis that protein intake – especially animal protein intake – raises kidney stone risk. None of the three protein sources had a robust effect on stone risk. Within the actual ranges that dominate the populations they studied that effect cannot be demonstrated.
When Is No Really No?
Karl Popper founded the philosophical groundwork for ‘no’ as the only sure guide to a form of reliable truth. Put simply, and poorly, a hypothetical idea cannot be universally true if even one of its necessary predictions proves false. But this leaves open the question of domain – can an idea be useful within one domain yet fail elsewhere?
Great Protein Excess May Pose Risk
The very highest animal protein load did seem to have some baleful effect. So massive protein loading from concentrates, or even from very large meat intakes, could pose risk. They did not specifically set out to test that idea, and it may prove false if tested with more vigor.
The Common Intakes Create No Risk Gradient
But over the ambient protein intake ranges of people in numbers and over time they detected no effect of protein on stone risk. So their ‘no’ pertains to a specific but large and practical domain, and also to the techniques and methods they used to measure effects.
Falsification Has Practical Value
Because among people in numbers and over time protein intake scarcely alters stone risk, in the commonplace business of stone prevention protein intake need no longer attract our interest. This is a powerful statement for physicians to make to their patients. It is one burden to lift from them, one complexity they can ignore, for the most part, in perfect safety. We need only caution against excesses, and even there we have no proof as yet.
Does Not Test the Acid Load Hypothesis
The negative result does not invalidate the idea that protein can promote stones via acid load. But it does demonstrate that the acid loading from actual ranges of protein intake are not sufficient to vary kidney stone risk. In other words, they have tested the relevance of protein under common conditions in relation to stone risk, but not the underlying mechanism of acid load promoting stones as a basic physiology.
Potassium
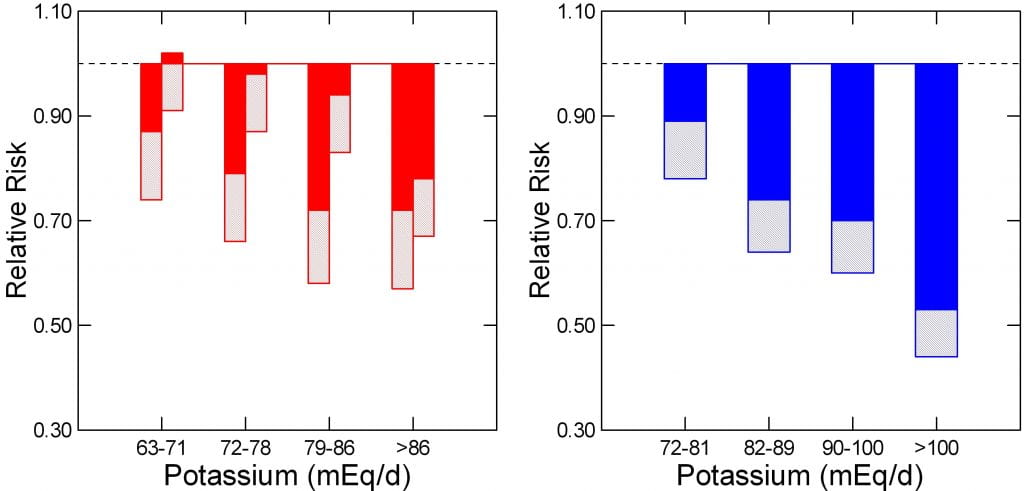
Because women and men differ in size, I cannot plot them over one set of intakes, so the two female cohorts (red) are on the left, the male cohort (blue) on the right of this two plot. For female quartiles I chose those of NHS II.
I converted all intakes into mEq/d because this site has preferred that unit. One multiplies by 39 (the atomic weight of potassium) to get household units of mg/d.
As potassium intake rises, relative risk of becoming a stone former falls markedly and progressively in both sexes, and the upper 95th percentile of the risk is far below 1 (upper ends of the lighter bars). Compared to the reference ranges, below 63 and below 72 mEq/d, women and men, respectively, the protective effects are evident and significant in the first quartiles, with the exception of one of the female groups (red bar extends above 1).
Their Potassium Hypothesis
Quite opposite to protein, this food component has a powerful effect, and therefore physicians can have confidence in recommending high potassium foods to their stone patients. Because some have significant oxalate contents, we need to choose with some care and use diet calcium as an offset. Several articles have detailed this approach. More generally, the kidney stone diet, like the US recommended diet, is a whole food plan that includes high diet calcium, reduced sodium, and ample servings of fruits and vegetables. The latter provide much of the potassium load.
When is Yes Really Yes?
In a way, forever. These data will hold, no doubt indefinitely, as will the negative data concerning protein. Others may find differently among different people, in different places, with different techniques. But those who repeat what Curhan and Taylor did will almost certainly find what they found. If not, will ensue the scientific homologue of disagreement as to simple facts, thus calling for more repeated work that inevitably discloses some final consensus.
But what will inevitably fall is the idea underlying this study, that alkali protect against stones, acids promote stones, and the one can offset the other – in other words, the mechanistic vision this work arises from. Given the history of science, these mechanistic visions of how nature does things rarely last but are – as it were – overlain by revelation presently unthought of.
Even so, while we wait for their inevitable demise, these two formulations have met various tests and remain viable explanations for what we can observe. This makes them useful, still, as generators of new research.
Correlates of Diet Potassium
As a kind of gift, the data of excellent science often enough give us useful or at least eye opening glimpses of how things work. Here are four urine measurements central in kidney stone diagnostic evaluation plotted as a function of diet potassium intake – that means veggies and fruits for the most part. The authors tell us that stone formers and controls scarcely differed, so they offer the pooled values.
In all four plots, the big blue dots are medians, the lines the 95% confidence limits. All four trends were significant at p<0.001.
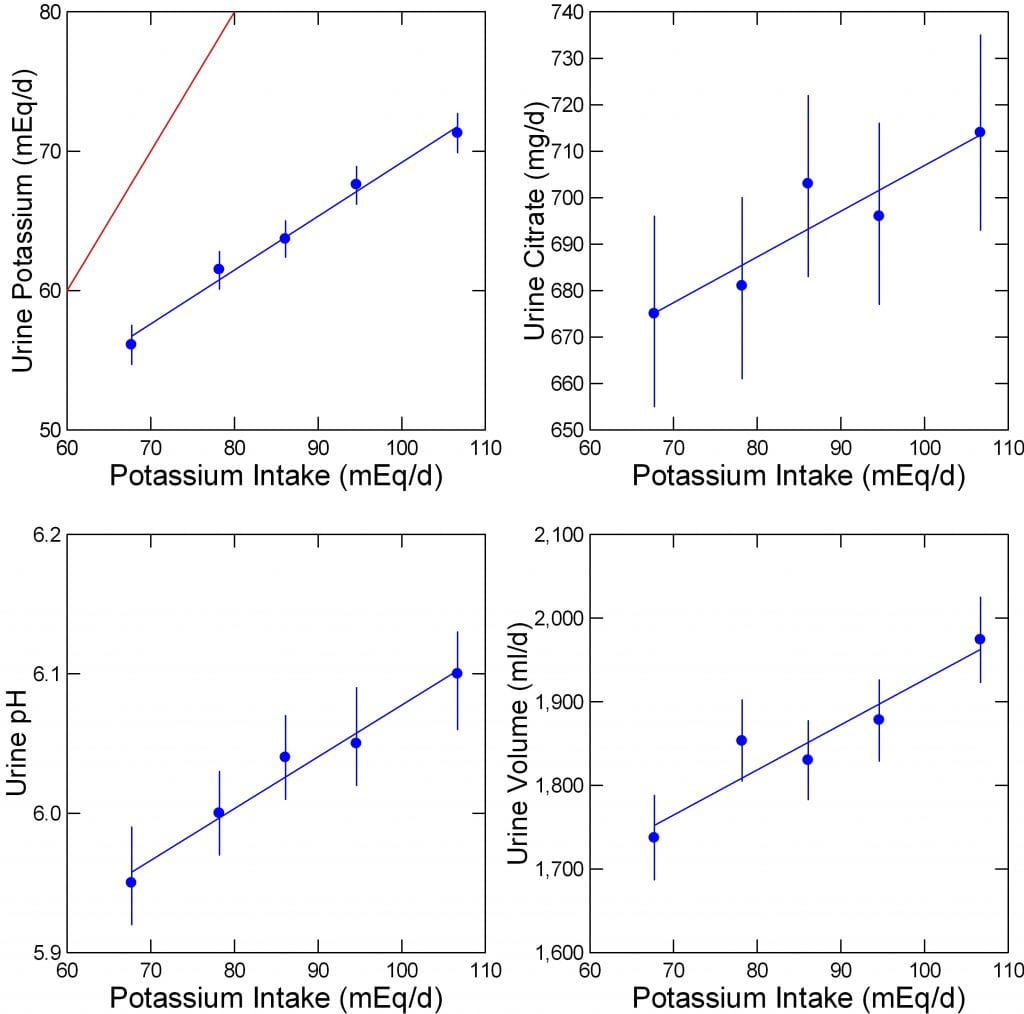
Urine Potassium
Indeed, as diet estimates show higher values, actual urine potassium rises in excellent accord. The excellent correlation makes clear how well the diet estimates gauge potassium intake. The red line of identity lies far above, as only a fraction of ingested potassium is absorbed and lost in the urine.
Urine Citrate and pH
Food potassium is mainly as the salts of anions that can be metabolized to bicarbonate – put crudely. This should raise urine citrate and pH.
Urine Citrate
Urine citrate, rises in a haphazard and rather sluggish way, from about 675 to 710 mg/d over the wide range of potassium intakes. This is true even if we take the lower 95% boundaries of the confidence intervals. The three cohorts had high average citrate excretions, as it were, and the effect of potassium intake is small. Therefore the expected protective effects of citrate from diet potassium would seem likewise small.
Urine pH
The latter rises in fine progression with potassium intake, and over the range in which calcium oxalate stones will predominate. Even the outer boundary of pH for the highest pentile of diet potassium is below the region where calcium phosphate will predominate in stones. I view this as important. We can tell patients to eat their fruits and veggies without fear of provoking calcium phosphate stones as a general rule. Of course people do vary, and prudent physicians measure to be sure.
Urine Volume
This rose with more vigor – to my eye – than did urine citrate, presumably because fruits and veggies contain a lot of water. The CaOx supersaturation fell (5.8 to 5.1 over the whole range of intakes) with rising potassium intake, perhaps because of this volume increase, and that may well explain at least part of the marked stone risk reduction from increasing potassium intake. Although the change in supersaturation does not seem so marked, we have as yet no data from this group about its effects on stone risk, which may be very powerful indeed.
Animal Protein to Potassium Ratio
Rationale
Even though animal protein had no effect on stone risk, but potassium intake had a powerful effect, one might imagine that when the latter was low and the former high one might see an effect of the ratio even after adjusting for the total intakes of both. Put another way, the combination of high animal protein and low potassium intakes might foster stones even when total intake of one (animal protein) was itself not a driver of stone risk because the other (potassium intake) was.
The reason for suggesting this rather counter intuitive idea is not the obvious and rather debatable one that given no effect of the numerator (animal protein intake) and a powerful effect of the denominator (potassium intake) the ratio must show a strong relationship to stone risk. It is, I suspect, that individuals will vary in this ratio so that those with high ratios will become stone formers even if one corrects for total intakes of both animal protein and potassium – as they did.
Result
Indeed, this prediction proved true for the males and for one of the two female cohorts. The pooled results for all three cohorts likewise showed a significant trend of increasing risk with rising ratios. For those with sufficient technical insight I recommend consulting the table of data in the original paper, and giving the matter some thought.
Clinical Meaning
Clinically, I cannot see how this will help patients overly, as we want high diet potassium intake and that will, when successful, place most of the ratio effects on just animal protein intake, which latter has little effect by itself. To ask patients both a reduction of animal protein and increase of diet potassium seems excessive once we know the former has no independent effect. Every thing we ask of patients by way of change takes energy from them, and we need to focus on where risk most varies – in this case diet potassium in a spectacular manner.
Mechanistic Meaning
Obviously this ratio derives it intellectual force from the food acid – alkali antinomy. As plant alkali – potassium – neutralizes animal acid, meaning as the ratio falls, the theory predicts a fall in stone risk, which was found. But, although this is a necessary prediction of the acid base theory, a positive result has enough alternative explanations to make it a weak confirmation.
If animal protein acid were, in fact, irrelevant, as some have said, and if potassium alkali were in fact a powerful protection via increase of urine citrate and reduction of urine calcium, those who chose a low potassium intake would have increased stone risk whether or not animal protein acid had any independent effect.
So the acid – alkali formulation has passed a necessary test and was not falsified, but the test lies far shy of support for the animal acid portion. This is especially true because protein whose entire animal acid load has been neutralized with alkali still raises urine calcium.
Thus does debate over theory inevitably roil one more than disagreement over fact. This group always has its facts right, and no group ever gets its theories accepted but by mighty effort.
What Do We Have For Our Patients?
Eat Your Fruits and Veggies
As usual with results from the Curhan/Taylor group we have something very excellent. Diet potassium increase seems an unmitigated benefit and of great value. The upper end of the range, about 100 mEq/d, or about 4,000 mg/d, is at the US recommended ideal. So this research about stone disease more or less coincides with the massive research upon which a generation of scientists have based diet recommendations for the whole of the American people.
Apart from massive support for what everyone’s mothers have long urged, we have a crude yet tolerable estimator of diet intake from urine potassium. More or less, an ideal intake should give us somewhat over 70 mEq/d of urine potassium, and from their data as I have graphed it, one can estimate – albeit most crudely – about where a given patient might lie in terms of eating.
Past Fears of Animal Protein Seem Bogus
No one questions that massive protein excess can raise urine calcium. So, enough protein – 0.8 gm/kg/d and not too much – no more than 1 gm/kg/d seems as prudent for stone formers as for the rest of the US, which matches the general US recommendation for us all.
As for the protein in milk products, it is not any risk at all.But either way, from acid or not, within the range of large numbers of people over long time periods these investigators find no support for animal protein intake per se as a cause of stones. That dairy proteins may have minimal protective effects could be related to the calcium that accompanies it, or perhaps other factors in milk products; but the effects are small.
Dr Eric Taylor kindly read this article, at my request, and accepts my account as accurate. I thank him personally for going to this effort. Since his reading, I have slightly modified the logic of the first several sections with regards to their testing of the acid theory of protein stone genesis, but the main lines of this review remain unaltered.

Hi Dr. Coe,
When you refer to “dairy” – are you referring to milk products exclusively. I assume eggs would be in the animal protein category, correct?
And your recommendations of limiting to 0.8-1.0 gm/kg/day – this is based on IBW if the patient is overweight, correct?
Some of my patients like to take protein supplement drinks – any thoughts on this?
Lastly, you are talking total protein for this number, correct? Not just animal protein. I generally encourage patients to limit animal protein (I do not include milk products in this) to 3 oz at lunch and dinner, 1 oz at breakfast, ~50 gm/day.
Thanks for another great article!
Hi Marilyn, I gather you are a physician but cannot be sure, so my manner of address is informal. Dairy is all products made from milks as opposed to proteins from eating the animals themselves. The per KG is as best as possible ideal weight – reality does intrude here, doesn’t’ it? I despise protein drinks instead of food unless there are medical special needs; but I have no evidence. As for the protein total, the sum of dairy and animal is what I had intended – more or less what you seem to be saying. Regards, Fred
Hi Dr. Coe., I have been reading many of the papers on kidney formation and they all point out to animal protein intake as one of the main causes for kidney stone formation, do you think is different the case for people who follow a high non-animal protein diet? Since I couldn’t find any paper where they make this distinction, although, they are all explicit about the source of the protein being animal.
Also, do you think that trying to keep an alkaline PH can help to reduce the chances of kidney stone formation?
Thank you very much
Hi Sebastian, The article you write on summarizes the lovely research by Taylor and Curhan showing more or less no kidney stone risk from protein, animal or not. Plants seem to reduce stones, perhaps because of the potassium alkali they contain – same article. I do not know why people have always believed animal protein causes stones. The potassium alkali from vegetables does not reduce stones because of increased urine pH but I presume because of increased urine citrate. Regards, Fred Coe
Dr. Coe, Thank you for the great overview and information. I have had kidney stones for most of my life, not knowing exactly what was causing so much pain and discomfort until in my thirties, when large stones started passing. In the past two years, they have become more pronounced and sharper and have caused more damage when passing. Urologists have encouraged greater water consumption, but I am also looking at increasing my potassium intake. My question is do potassium and magnesium supplements work as effectively as natural food consumption in the prevention of stones? Also, are bananas good sources of non-oxalate potassium? Lastly, what non-oxalate vegetables are recommended for potassium intake?
Thank you.
Hi John, Given so many stones I would advise you get fully evaluated for their cause and base treatment on what is found. Here is my best on the subject. Mere water is not a good idea, too limited. Food sources are fine but only when your testing discloses their proper role and re-testing shows food is doing what you need. Food oxalate rarely is a main cause of stones, although it is an important factor among many. Get tested, treat abnormalities. Regards, Fred Coe
Dr. Coe, Thank you. I will look at what you sent and get tested. I did have one of my last stones tested, and it was calcium oxalate. Appreciate it. And Happy New Year! Regards, John
How do i make an appt with the renal stone clinic at University of Chicago? Thank you cb
Please call our coordinator at 773 702 1475. She will do everything you need. Regards, Fred Coe
Hi Dr. Coe,
Following the thread of Marilyn’s comment regarding protein, when recommending limiting animal/dairy protein to 0.8 mg per kg of IBW. This appears to be in the context of patients at risk for calcium oxalate stones, but would it apply also to uric acid stones also? Is the plant potassium/ animal based proteins ratio in addition to a diet low in oxalates? What are your thought regarding protein restrictions in low-purine diets? There is so much conflicting information out there it seems, that it is hard to make heads or tails out of it all.
Hi Charlotta, I see no role for low purine pr low protein diet in uric acid stones. The entire problem is from too acid a urine and that is almost never due to diet but to defects of renal acid handling. More abundant fruits and veggies should be enough to raise urine pH, but I have never succeeded with diet and invariably need potassium citrate or, when potassium loading is a problem, sodium alkali. I think the failure of diet to prevent uric acid stones reflects a real kidney defect, perhaps of ammonia production, or a problem with GI alkali absorption. As for calcium stones, this very article makes clear that diet protein, if a risk at all, is one only at the very highest intake level. Their data do not support 0.8 gm/kg/day protein intake for calcium stones, but only far higher levels – their highest one. Regards, Fred Coe
Dr. Coe, I was blessed several years ago by finding your site soon after my first stone, which was and will be my last. I write today also to share information with you that you may not have had access to due to your medical role. I work with a man who regularly passes stones, which he was informed are calcium oxalate when tested over ten years ago; however, this man does not feel it worthwhile to take dietary or medicinal steps to prevent further stone formation and has come to withstand the pain of passing stones, which he does once very 2 or 3 months, without great emotional or physical pain. He says your ureters get used to it, maybe stretched out. He has brought a bloody stone with him when returning from the bathroom once even, to my amazement, and reported that he had to pull it out of the tip of his penis when urinating because it got stuck (the stone was that large). He does not see doctors for his stones anymore, except when one is so large he feels instinctively that he cannot pass it, in which event he has a scan taken and subsequent ultrasound crushing of the stone (sorry for the improper terminology). In short, I just wanted to share with you that there are some people out there who prefer to make only the absolute minimal life changes to prevent further stone formation and instead opt to “get used to it,” something I could never do, or rather, would never choose to do.
Yours,
David
Hi David, what an awful story! Of course everyone is free to do as they like, but stones can cause a lot of trouble beside pain. I hope co-worker is lucky and does well despite dismissing prevention. Thanks, Fred
Thank you very much for sharing the information through this article. My trainer recently advised me to start using bcaa and whey protein supplements for improving the strength and muscular strength during workouts. But I was conscious about the authenticity and quality. I always used to wonder if there are any side effects of using these supplements. Hoping to see the benefits of bcaa supplements as listed by you.
Hi Kashish,
We are not advocates of supplements unless they are warranted by your doctors.
Best, Jill
Hi Dr. Coe,
Thank you very much for your recently updated article on CaP stone formers! I found it very relevant.
You have written here about the effect of acid load from sulfur containing proteins on Ca 24, Cit 24, and stone risk.
Can you please share your thoughts on whether acid load has the same or different kind and magnitude of effects on CaP stone formers with high ammonia excretion and high pH 24 (7.0 or higher)?
Kind regards, Al
Hi Al, I do not know, but suspect that acid loads will raise urine ammonia and lower urine pH. We did not try that experiment. Warm regards, Fred
Hi Dr Coe!
I am brushite stone former and am on the low sodium 1300-2000mg kidney stone diet and was just placed on 12.5mg chlorthalidone per day. I also have been intentionally eating at least one banana per day. After taking 12.5 mg for 10 days days my blood potassium was at 3.3 mol/liter. My 24 hour urine PH is 6.9 and citrate is 350-424. I have a low anion gap of around 5 but doctor says nothing to worry about. I plan to ask for 10 Meq per day of potassium chloride from my physician as I don’t want to overmedicate and it took 10 days for the decline so thinking this would be enough although thinking it will further reduce anion gap. In your opinion, would 10 meq be enough or will I need to take 20 meq per day? How does a person know how much they need to offset effects of chlorthalidone assuming a fairly good low sodium diet?
Hi Carrie, Although seemingly small, that is a lot of chlorthalidone, and some people lose quite a lot of potassium on it. I have found it takes 40 or more mEq/day of potassium chloride to maintain blood calcium levels, and often have had to add amiloride – a sodium channel blocker – as well. I presume the drug lowered your urine calcium. Another factor – the lower the diet sodium the more effective the CTD to lower urine calcium, so I aim for 1500 mg of diet sodium. This will reduce potassium loss, and you may need even less of the drug. It has a 23 hour 1/2 life and can be taken every other day if one needs a lower dose. Regards, Fred Coe
Thanks Dr Coe! I did try the 12.5mg chlorthalidone every other day and I didn’t need any extra potassium. However, my urine calcium ranged from 230-250 and that was on a very strict 1200-1500 mg/day diet. My physician thought that was good enough but I wanted to try to get it lower so he allowed me to try 12.5mg every day. Of course, we all want urine calcium as low as possible but do you think the 230-250 urine calcium was good enough? If I just take the 12.5 every other day then I won’t need to take potassium and potentially amiloride too. It is hard to decide what is best given all the trade offs.
Hi Carrie, If your 24 hour urine sodium was below 1500 mg (65 mEq) and calcium 230 – 250 despite chlorthalidone you probably are as far as you can go along this path. What’s next? Stone type – is your urine supersaturation < 3 (calcium oxalate stones ) and CaP SS <1 (all calcium stones). If so, perhaps things are alright. If not, one goes on until both (or just CaP SS <1 if your stones are calcium phosphate ) are achieved - more urine volume, lower urine oxalate if relevant, more care about diet protein if very high, sugar. Regards, Fred Coe
Dr. Coe
Thank you so much for this website. I have two questions. 1. I find it hard to get in 1200 mg of calcium a day in food (btw I am a vegetarian), could you think chewing calcium carbonate tabs with food will work?. 2. Do you suggest Potassium citrate pills? I had a 100% Ca Oxalate monohydrate stone in 2008. Other than a half hearted attempt at increasing fluid intake I have not dome much. A recent US showed one 5mm stone in the R kidney and a few smaller stones there. Ty again
Hi Ravi, You need to know what actually caused your stones. Here is a good approach to evaluation. Citrate is useful when urine citrate is low, but you only know that from testing. Find the abnormalities, and treat them. Regards, Fred Coe
I have ammonium hydrogen urate stones, mainly, along with lower amounts of calcium oxalate, phosphate stones. I am 23 years old and have Duchenne’s muscular dystrophy. My dietician and doctor seem to be at a lose concerning the diet that I should follow. I am now having these stones frequently with stones large enough that led to having procdures to remove them twice so far this year. Currently, I am experiencing pain along in the kidney area with nausea once again. Do you know of any connections between muscular dystrophy and kidney stones? Thank you
Hi Sinjun, This rather rare kind of stone arises when urine ammonia is too high – GI diseases, diarrhea of any kind, special high protein diets, especially with supplements. The 24 hour urine testing used for all stone disease will show exactly what is happening and what to do about it. Diet is useless unless you know the chemical conditions in the urine. Regards, Fred Coe
Dr Coe,
I’m trying to understand what Anion Gap blood test means? Does this have anything to do with kidney stones? I also have seen the term GI Anion Gap, are these the same thing?
Hi Lisa, the blood anion gap is the difference between serum sodium + potassium – serum total co2. The anions are mainly sulfate but also other anions (negatively charged molecules) from our cells and diet. Increased AG occurs in kidney diseases. GI anion is calculated in the urine and reflects the amount of potential alkali in our food. These are rather deep and technical issues, and if you want more please let me know. Regards, Fred Coe
Dr Coe,
1) Can drinking large amounts of water in itself cause a lower Blood Potassium level?
2) If you have a lower Blood Potassium level does that correlate with having a Lower Urine Citrate Level or no connection?
3) Is Potassium Gluconate OTC a Potassium Citrate or a Potassium Chloride or neither and will that raise your Blood Potassium or even your Urine Potassium?
Hi Diane, water will not lower blood potassium unless there is some other reason. Lower potassium will lower urine citrate. OTC potassium gluconate has about 2 mEq of potassium in a dose, way too low to replenish body stores. Your physicians need to figure out why your serum potassium is below normal, which is not obvious to me at the moment (your prior notes (7 in all) are not immediately visible on this platform as I write this, a major deficit). Regards, Fred Coe
Your writing is the clearest I’ve ever read from an academic, partly because it doesn’t sound “academic.” It’s amusing sometimes, even. THANK YOU.
I gather than potassium supplements aren’t a good idea? I track key nutrients in what I eat with MyFitnessPal, and I cannot see how anyone ever reaches 4700 RDA of potassium or even 3600. One can eat only so many sweet potatoes and avocados. Am I missing something?
Hi Judith, How lovely to say! I am an academic at a school notable for academic behavior – dressed down, hemmed in, almost think we should be communicating is Latin, or Ancient Greek. IF you read my publications (for the academics) you would understand why I so much like this public facing site where I can speak normally. As for potassium citrate it is intended as a prevention for some stones in some people, not a supplement in general. But I think your concerns are diet in general. Given the atomic weight of potassium is 39 mg per millimole 4700 mg of potassium is 120 mEq (to make it like sodium) and we are happy to eat 150 mEq of sodium. Ideally we would eat 50 mEq of sodium and 140 mEq of potassium. The problem is fruits and veggies – very high in potassium and more trouble to shop for, prepare and eat than, as an example, a steak. I am the same as the world here. You do not need sweet potatoes and avocados, none of us do, but it is tiresome to think about the fruits and veggies in quantity. Harmless, healthy, bulky, possibly drab looking compared to – need I say?. SO we are missing something, yes. Not so much missing it as – how shall I say this? – looking the other way. Regards, Fred
appreciate this article very much!!
I’m a classic diet-induced stone creator. After 55 stone-free years, i finally got control of my high-triglycerides & low HDL via a restricted carb diet…very dramatic results & never felt better in my life. But eating “metric tons” of almonds, cashews, peanuts, raspberries and spinach, as well as Vitamin D & C supplements for COVID health, must have led to my matching 4mm stones in each kidney. One passed in a week, while the other one is just hanging out. Stone chemistry was classic Calcium Oxalate Mono. I just finished my pee collection today.
I’m very happy that normal meat consumption and even-high consumption of dairy looks to be OK, because I have to match low oxalate foods with low carb foods to keep my lipids in good shape without generating stones. I never liked spinach anyway, but I’ll miss the nuts.
Your website is a godsend for high information patients like myself.
Hi Tim,
You can still eat nuts in moderation. There is lots of diet help from my site but it sounds like you have it together!! Good for you! kidneystonediet.com/start
Jill
Hi Tim, when you get your 24 hour studies be sure and scan for possible remaining causes of stones. Howsoever suspicious the prior diet, things may lurk that need treating. Regards, Fred Coe
Once again, thank you thank you for this rich resource! I can’t tell you how much I appreciate your diligent work in helping to educate both patients and practitioners. I am a stone former and I just learned (with no help from my doctors unfortunately) that as a person with cystic fibrosis I may have higher urine calcium excretion than normal people. This could be the result of genetics, predominantly. It would explain why have higher urinary calcium and I form stones even though my daily oxalate intake is very low (I form calcium oxalate stones). A few questions:
1) You write here that taking high dose potassium is protective, even in the case of high-normal protein intake. But elsewhere you have written that this actually doesn’t reduce urine calcium excretion – can you please clarify? My doc is afraid to let me have too much potassium citrate due to risk of calcium phosphate stones. But here you say this is not a real risk. I am recommended to take only 600mg of potasium citrate daily. According to what you’ve written here this seems way too low. Also, my urine pH is always 6.5-7.5 no matter what I eat (I test regularly), and I’m guessing this is too high, probably due to the excess (genetic?) calcium excretion. If I took more Potassium citrate, do you think I can offset that calcium excretion perhaps?
2) In the last two months I’ve started eating more protein, about 100g daily, and most of it is animal based. Now that I read this article, this seems too high and potentially risky. So I’d like to get half of that from plant sources (pea protein powder) ideally, for you say plant protein has close to zero stone forming risk. This would put my animal protein intake under 62g threshold for risk. My question is: are some animal proteins more risky than others? I’m wary of dairy because my baseline calcium excretion is so high (and sometimes when I eat dairy it seems to make my urine cloudy… increasing calcium excretion?). Dairy aside, is there any difference in acidic impact comparing red meat vs. poultry vs. fish? I know for uric acid specifically, poultry is the lowest of these in purines. But is it the same for acidic impact generally?
Thank you so much for this work!
Hi Mica, Here is a nice review of prevalence of stones in CF – about 6%. A modern article on the CFTR defect clarifies that the defective transporter is not in kidney, so there is no link between CF and abnormal kidney mineral handling via abnormal kidney function per se. Most experts propose that the intestinal and pancreatic abnormalities lead to fat malabsorption which in turn raises urine oxalate. This is a probable reason the stones tend to be calcium oxalate. So your higher than normal urine calcium is presumably from another cause, perhaps genetic hypercalciuria. I gather your urine oxalate is not high? It is not clear what was found in the 24 hour urine samples. If your urine citrate is low, then alkali are indicated, and I would not be concerned with transformation to calcium phosphate stones if citrate actually rises with treatment. The problem I have with all this is that I do not have enough information to be more than very general, whereas your physicians have all of your data and are in a better position to help you. As for protein intake and diet in general, that is often complex in CF because of malabsorption. Put another way, given CF, your physicians might wish to refer you to a convenient stone center at a university where this rather uncommon problem is more familiar. Regards, Fred Coe
Thank you Dr. Coe. I will read about a possible genetic hypercalcuria but it’s strange because if that was the case I would have expected to get stones all throughout my life, but it’s only been a serious problem in the last three years even though my diet has been very strict to limit oxalates. I’m still trying to find the cause and my nephrologist has not been helpful in this regard (though I just switched to a new one so maybe she will actually investigate possible causes).
Basically, my problem is that my urine citrate is always low but if I increase potassium citrate supplement my pH gets too high. I recently upped my potassium citrate dose to 1200mg daily and it led to a rise in my urine pH to about 8. I assume this is too high and therefore risky? What pH is of concern to you? I am surprised that eating a high protein diet does not drop my pH down much, maybe the potassium citrate and magnesium supplements explain this? Thank you.
Two more questions: I eat a diet high in salt. CF people are advised to eat high salt diets due to CFTR channel dysfunction. My nephrologist said he’s not concerned about the amount of salt I’m eating because my urine sodium is consistently normal (110-130 range). Do you agree with this? Or could my sodium intake be too high even if the urine level is normal?
I’ve ready studies that show supplementation with the oxalate-degrading bacteria Oxalobacter formigenes is extremely effective at preventing stones (this is a bacterium we’ve lost in the Western gut due to modern living and eating). Why is this not available for patients? I cannot find anything available on the market for it. Any updates you have on this would be appreciated.
Hi Mica, Urine sodium must match net intestinal sodium absorption – losses from sweating. It would appear that your net balance is in a common level, and there may be no good reason to change it. Oxalobacter does not work because it needs oxalate, so one must feed oxalate or it is overwhelmed by the normal bacteria in colon not burdened with oxalate nutrition. It is not useful for treating human stones – tried and failed. I am not interested enough in the matter to write about it, even though some wonderful basic science is being done aiming to use the bacterial machinery as a way to increase intestinal oxalate secretion out of blood. Best, Fred Coe
Hi Mica, pH of 8 is about the upper limit of what kidneys can do – urine is bicarbonate buffered at high pH and such a buffer actually cannot go above pH 7.9. Os you have a problem with citrate transport, and I do not know if CF does that as it is not my disease. If your urine pH will not fall from any mechanism, perhaps you have a form of renal tubular acidosis, a matter I do know a lot about but lacking real detail about you hesitate to pursue here. I found a single case report of both conditions in one person, but it seems as though they are simply two separate problems. Regards, Fred Coe
Thank you so much for this info. I will do further investigation and raise these things with my docs. Much gratitude!
I am 54 year old male, who played sports during my adolescent years through college. After graduating college, I continued working out religiously (5 to 6 days a week – 1 hour of anaerobic work and 50 minutes of aerobic work). When I turned 40 years old, I would periodically suffer debilitating muscle cramps in my hamstrings to the point of passing out (after being rushed to the ER and a complete workup because of an episode, it was determined I suffer vasovagal). At that time, I was drinking a gallon of water per day, but I was told this was depleting my electrolyte levels and contributing to my cramps. It was suggested that I drink low sugar Gatorade (G2), so I started intaking an average of 64 ounces per day. I’ve always had a high animal protein diet mostly comprised of poultry and fish limiting red meat to once a week. My carb intake is comprised of both starchy and fiberous carbs throughout the day, but probably not enough fibrous ( I definitely don’t eat enough fruit). Fast forwarding 13 years, I developed calcium oxalate stones; and my urologist instructed me to stop drinking G2 and go back to drinking a gallon of water a day. Almost 2 years later, I haven’t had any additional stones, but my muscle cramps are becoming more frequent again. My blood work came back as normal with the exception of low Vitamin D levels, so my family physician has me taking 5000 IUs of Vitamin D/day. To avoid debilitating hamstring cramps and passing out, I started taking potassium gluconate, which seems to help. However, I was worried this strategy would cause additional kidney stones; but after reading your article, I do not think it will. I am not the sharpest knife in the drawer, so I don’t mean to over simplify or incorrectly deduct the conclusions in your article; but I would appreciate your input and/or advice. If I should do more medical workup, who should I consult: my family physician, my urologist, my hematologist (I ended up developing a DVT for the 2nd time and 2 PEs 3 months after my stones, the bloodwork confirmed I do NOT have any genetic abnormalities, and I am on bloodthinners for the rest of my life), and/or a sports medicine physician? Thank you.
Hi Rick, Potassium repletion as potassium chloride or citrate or gluconate should pose no kidney stone risk. Sodium rich drinks can increase urine calcium and stone risk, although whether or not they do so in you is unknown. If potassium helps your symptom I would think it safe. Regards, Fred Coe
Dr. Coe,
Thank you for this interesting article. I think I’m getting a little confused by the statement “As for the protein in milk products, it is not any risk at all”.
When thinking about total daily protein intake to achieve the 0.8-1.0 kg/d guidance in the kidney stone diet, are you saying one should still count the total protein (animal + plant + dairy) for the basis of calculation? Or, as part of the total calculation you would omit the dairy (just counting animal + plant) to determine how much protein intake is appropriate for myself to acheive the 0.8-1.0 kg/d range?
I have regularly been exceeding the 1.0 kg/d range for a number of years a part of a high protein diet, not realizing the increased risks as a stone former and for bone disease, and am working to implement the kidney stone diet to lower urine calcium. Thanks kindly!
My apologies, I mean to say 0.8 gm/kg/d – 1.0 0.8 gm/kg/d range !
Hi Sam, Thanks for clarifying. But my comment below does answer to you. Fred
Hi Sam, Good reading. In a way, yes indeed. Milk protein seems irrelevant to stones. Frankly the article points out that protein in general is not of a problem unless it is much more than needed. So strictly from a stone point of view one wants 1 gm/kg/d of protein excluding milk products. I must say that WHO and other diet authorities point out that above 1 gm/d/kg of protein from all sources is more than normal people need, even it is without harm. Regards, Fred Coe
I find this discussion on the relationship between diet, protein, potassium, and kidney stone risk quite enlightening. It’s crucial to understand how our dietary choices can impact our health, especially when it comes to conditions like kidney stones. The insight that protein might not necessarily worsen stone risk within reasonable limits is reassuring. Additionally, the role of potassium-rich foods in mimicking the effects of potassium citrate pills for stone prevention is intriguing. It’s great to see researchers delving into this area, as it offers hope for better stone prevention strategies through dietary adjustments. For more information on optimizing nutrition, you can also visit Optimizenutrition.ca for the best Omega 3 supplements. It’s always beneficial to stay informed about our dietary choices and their potential impact on our health.
Hi, my husband just received the following dietary instructions for his type of kidney stone (Calcium oxalate mono hydrate):
Calcium Oxalate Dietary Instructions
Your kidney stone was primarily made up of Calcium Oxalate. Following these suggestions may help prevent future stone formation.
– Take a B-Complex vitamin or 100mg vitamin B6 daily.
This helps decrease oxalate
– Take a Magnesium supplement of 300mg daily
Magnesium binds to oxalate in the same way that calcium does but is more soluble. Magnesium will take the place of calcium when binding with oxalate and be less prone to form stones.
– Increase urinary citrate by squeezing one lemon in your water every day.
– Drink at least twelve 12oz glasses of water every day.
– Decrease your intake of sodium to 2500mg maximum.
– Decrease phosphorus (soda) and caffeine.
*—>- Limit meat and roasted nuts to 2-3 times per week.<——-*
– Females – Eat 3 servings of dairy per day or take a Calcium supplement. Try not to exceed 500mg per day
– Males – Eat 4 servings of dairy per day or take a Calcium supplement. Try not to exceed 750mg per day.
I understand the need to avoid or limit nuts, but not the protein restriction. Your article says animal protein is ok as long as it in the normal range ( .8 – 1.0 g/kg/d), so is there any reason to limit animal protein to only 3 times per week?
Do the other recommendations seem sound, or are some outdated?
Hi Jamie, I inveigh against pro forma advice when proper means of evaluation exist and are not overly costly – given the great expense of stone surgery. A full evaluation is appropriate here and treatment based on what is found.