 Being chronic in many cases, stones need to be prevented not just removed. That accomplishment, prevention, needs the skills, efforts, and cooperation of two people. I am writing this for the one who makes the stones, and my purpose is to promote success: No more stones. I have never known physicians who do not want successful treatment for their patients. It is the ultimate satisfaction. But they are time pressured, as are we all in this hectic world, and you can help by doing before and after a visit all that you can do to make the visit time count – to waste as little as possible, and put to use as much as you can get by way of treatment. I have cared for thousands of patients with stones. Here are things patients do that help me with their care. If you do them before and after your visit for stone prevention things might turn out even better than they would have otherwise. This article is meant to complement my other one on the Five Steps to Stone Prevention.
Being chronic in many cases, stones need to be prevented not just removed. That accomplishment, prevention, needs the skills, efforts, and cooperation of two people. I am writing this for the one who makes the stones, and my purpose is to promote success: No more stones. I have never known physicians who do not want successful treatment for their patients. It is the ultimate satisfaction. But they are time pressured, as are we all in this hectic world, and you can help by doing before and after a visit all that you can do to make the visit time count – to waste as little as possible, and put to use as much as you can get by way of treatment. I have cared for thousands of patients with stones. Here are things patients do that help me with their care. If you do them before and after your visit for stone prevention things might turn out even better than they would have otherwise. This article is meant to complement my other one on the Five Steps to Stone Prevention.
PREPARE FOR YOUR FIRST VISIT
Gather Your Materials
THE HISTORY
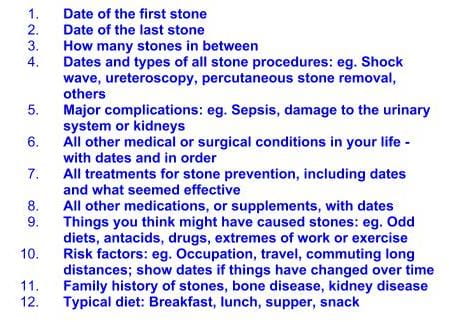 Click on this outline and it will open as printable or downloadable as an image. This will help you make your document. Type your history neatly. These headings are designed for a kidney stone patient and are not meant to cover all aspects of health care. Because this will be a focused visit it is best to keep the history on target. The dates of stones are often only to the nearest year, and that is alright. For procedures the best source is old bills which are dated and name the procedure, or, even better, old medical records. Complications and urinary tract damage usually require medical records for documentation. The same for your other medical conditions and past surgeries apart from stones. Medications can be confusing, Try to focus on prescription drugs, and mention what they are or were for. Supplements, herbs, health food concentrates can cause stones, so be as specific as possible: What, how much, how long. Because idiopathic hypercalciuria and low calcium diets can both cause bone disease, your diet and family history of bone disease matter. About your own diet, besides calcium intake, critical components for stones are protein and sugar intake, oxalate intake, and fluids.
Click on this outline and it will open as printable or downloadable as an image. This will help you make your document. Type your history neatly. These headings are designed for a kidney stone patient and are not meant to cover all aspects of health care. Because this will be a focused visit it is best to keep the history on target. The dates of stones are often only to the nearest year, and that is alright. For procedures the best source is old bills which are dated and name the procedure, or, even better, old medical records. Complications and urinary tract damage usually require medical records for documentation. The same for your other medical conditions and past surgeries apart from stones. Medications can be confusing, Try to focus on prescription drugs, and mention what they are or were for. Supplements, herbs, health food concentrates can cause stones, so be as specific as possible: What, how much, how long. Because idiopathic hypercalciuria and low calcium diets can both cause bone disease, your diet and family history of bone disease matter. About your own diet, besides calcium intake, critical components for stones are protein and sugar intake, oxalate intake, and fluids.
REPORTS
Do not be shy. By law your medical record belongs to you and you are entitled to reports and DVDs of your radiographs. Usually there is no charge. Resist attempts to have them sent to your doctor. They may not get there even though everyone means well and tries hard. Do not believe that electronic medical records will have your information. They may well not. What you will have is what you bring in your own hands.
- All stone analyses – bring actual reports
- Prior records related to stones
- kidney stones you have in your dresser drawer. It is important to analyse all stones.
- CDs of most recent CT, or other radiographs or ultrasound images for stones
- Recent blood measurements, bring actual reports: Serum calcium, phosphate, creatinine, potassium, chloride, total CO2 are most important
- All 24 hour urine kidney stone tests to date – bring actual reports not summaries
24 hour urine test results can be complicated to get. Vendors send the results to your physicians but a lot can go wrong. Electronic transfer to electronic medical records can be unreliable. Faxed reports are sometimes lost. Get the reports sent to you, and bring a full copy with you. If the laboratory cannot release the report to you – some states have laws about this – call the vendor and get the report faxed there. Call the physician’s office and be sure that it has arrived.
Do Your 24 Hour Testing Well
- 24 hour urine testing is essential for prevention, and only you can assure the tests are useful.
- Be sure testing is done by one of the large national laboratories, not a local hospital laboratory. The latter is often not properly equipped to do this kind of work. All national vendors in the US are fine.
- Do the tests before your visit; without them, the visit will be vague and incomplete.
- Read what Jill Harris says about collecting urines – I repeat some of her ideas here
HOW TO COLLECT THE 24 HOUR URINE
All of the vendors provide containers and instructions; follow them exactly. If you think you have made an error, discard the whole collection and call for a new kit. Never try to ‘fix’ an error – you cannot do it and the results will be an expensive and misleading mess.
WHEN TO COLLECT
Do two 24 hour urines so one can be on a weekend and one during the week. The latter should be during a regular work day if you work outside the home. Two samples are very important because even though results on one day are well correlated with results on another day there is a lot of spread between them, and that spread is useful to your physician in planning treatment. The two samples need not be continuous but it is preferable if they are.
HOW TO BEHAVE WHILE COLLECTING
Never show off; never make collection days special. You are selecting 2 frames from a movie that is life long, two days out of thousands. Make the two days represent you as you are in general, as you usually eat and drink, work out, work, and get around. Just go about life as if you were not collecting. Especially, drink as you always do. The large container often goads one into trying to fill it. If you see the jug is almost empty at the end of a full 24 hours, it means you do not drink enough, but don’t choose that moment to reform and correct matters. It was like this you made stones, let your physician see the chemistries as they were.
What To Bring To Your Visit
It is folly to believe anything can be sent to a physician, and folly to believe ‘it will all be in the computer’. In my life, at least, nothing ever comes by mail, and computers are as unreliable as rural mailmen on horseback in 1790. What you bring with you, in your own hands, will be there. Do not give anything up until you reach your physician. Hand the materials to him or her. Here is my list:
1. A TRUSTED FRIEND OR FAMILY MEMBER
The time will be limited, and the information dense and fast coming. Even if you are young and brilliant, you will have trouble because it is you who will be the object of attention. The other person can keep facts straight, write things down, ask questions you may miss on the moment. I shall call this other person your advocate.
2. ALL OF YOUR REPORTS AND EXTRA STONES
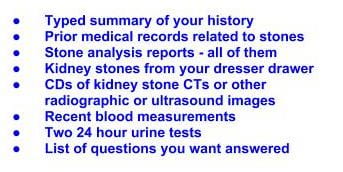 The master list. As I did for the history, this is an image file you can print or make into a card for a reminder. It summarizes everything up until now in a compact form.
The master list. As I did for the history, this is an image file you can print or make into a card for a reminder. It summarizes everything up until now in a compact form.
Plan Your Visit Carefully
WHO WILL BE SEEING YOU?
Sometimes a primary care physician who knows you well will undertake prevention. This has the advantage that history taking is abbreviated and a relationship is already established. That will leave more time for the details of stone management. Urologists often practice stone prevention, and it may be your surgeon you will be seeing. That also has the advantage of pre-knowledge. Surgeons often schedule very brief visits, but can be expert in this particular kind of medical care. Sometimes you will have been referred to a nephrologist or other physician who is expert in stone prevention but does not know you. The advantage of specialization is balanced by a greater time required to become familiar with your situation.
HOW WILL THE TIME BE USED?
You are purchasing time for yourself, and you need to make that time work well for your care and fit into what your physician needs to do. Find out how long you will have with the physician. Since it is all about time, how much will you have? Each of the three physician archetypes I have mentioned have specific time issues: The better you are already known the less total time is needed for background the the higher fraction available for the specifics of stone prevention. Usually physicians have allocated a fixed amount of time to a first visit for kidney stone prevention, so you need to know the usual practice. Typical times for busy medical practitioners can be short – 15 to 20 minutes total with at least 2 – 3 minutes used up for the computer. This generally leaves about 12 to 17 working minutes. Surgeons often have no more than 5 – 7 minutes for a visit but use nurses with advanced training to help and, being surgeons, tend to a high level of organization and accuracy. Review your history with your advocate so you can present it to your physician efficiently. He or she has to produce a legal medical record, and may need to type it into a computer. All this takes time. Go over your questions, and your list of what you want to leave with.
The Usual Sequence of a Visit
First is the history which you have made as convenient as possible. Next your physician should want to view your DVDs. The most important part is to count how many stones are already in each kidney – this is your baseline for treatment. If you pass a stone during treatment, it may well be one already present at this initial visit, and that is not a cause to change treatment. But if new stones appear on a subsequent CT, or you pass stones and the numbers on a subsequent CT are unchanged it means stone disease is ‘active‘, you are producing new stones, and treatment is not yet successful. This initial tally of stones is a crucial event for you. Be prepared to ask how many your physician sees, and write it down, left and right side separately. Although physical examination is a central part of clinical medicine, I have found over decades that the yield of findings that affect kidney stone prevention is minimal. I believe most physicians have found the same. Done or not is simply a matter of time left for what comes next. That next will be a review of your serum and 24 hour urine tests, and your physician will no doubt interpret them to you in terms of what seems to be causing your stones and what can be done about it. The laboratory results are always interpreted in relation to the composition of your stones which are from the stone analysis reports. The last part, and most crucial for you is your treatment plan and follow up routine.
Plan to Facilitate Each Part of the Visit
HISTORY
Being written down, and accompanied by old records, laboratory reports, and medication lists, the history taking should go smoothly. Avoid introducing extraneous stories or minor details. You are seeing a physician who is trained especially in history taking, and will lead the conversation. As much as possible, follow that lead and try to add details you are asked about. Here is where your advocate is most helpful if a spouse, family member, or very close friend.
REVIEW OF CTs
I hesitate to mention the matter, but possibly not all physicians will personally view the CTs and count stones. As best possible bring this matter forward. Without this baseline matters will become foggy during treatment. I have been impressed that official radiologist reports of CT scans are often not quantitative about the numbers of stones in each kidney.
REVIEW OF LABS
The review of labs is central. You and your advocate need to follow as best is possible, and at least one of you write things down for later. Ask questions, do not let things go by you do not understand. The review is for you, and what you do not understand has not been presented well enough. Serum lab results are critical, along with your medical history and past records for diagnosis of systemic diseases that might be causing your stones. I have tabulated the commonest ones for you, and their main laboratory abnormalities. You cannot evaluate systemic disease diagnoses yourself but you can cast a critical eye on your own lab results and ask questions. I have written two articles that enable you to read your own 24 hour urine lab reports intelligently – I mean by this with enough knowledge and expertise to understand the numbers. If you know your stone type review the article for that stone type: Calcium stones; Uric acid stones.
TREATMENT PLAN
Management of Stones Already There
You should expect an assessment of the stone disease to date – numbers of stones, evidence of kidney injury if any, amount of the stone burden – how many stones, how large, risk to the kidneys if any. Most important, is there a need for more surgery or can the stones be left in place? My view is that stones do not need surgery unless they are producing obstruction, significant pain, substantial bleeding, perpetuate significant urinary infection or are a threat because some abnormality of your kidneys or urinary tract will make passage especially hazardous. If surgery is recommended, here is the time to ask why. Just being there is not enough for me, most of the time.
Cause of Stones and Approach to Prevention
Your serum and urine testing should permit an overall analysis of what causes the stones, what you might have done in the past to foment stones, and in general what will lead to prevention of more stones. This is a most crucial area. Make notes, and think through any part of the presentation that is not clear. This is where your advocate can be helpful. Do not let this moment go by without understanding what has been said. Sometimes, the cause of stones will be tracked to a systemic disease, and that will shift matters from fluid prescription, diet, and medications to alter urine chemistries to the management of that disease. In that case, it is critical to understand the basis for the diagnosis, further testing, and treatments that may be used.
Treatment Plan for Prevention When Systemic Disease is Not Present
Apart from the uncommon situation of systemic diseases, prevention is always about fluid prescription, diet, and medications. Fluid prescription should consider urine abnormalities including supersaturation, and also the realities of your life, work, and when relevant limitations such as incontinence and sleep disorders, the one posing a problem for high fluid intake by day the other by night. Review your present urine volumes and how much of an increase is needed. Diet will seek to correct problems observed in your 24 urine studies. Ask to see the abnormal laboratory results you are treating, and compare your results to the normal values and to goals you are to achieve. Common abnormalities are high urine calcium, oxalate, sodium, or uric acid, or low urine citrate. Ask about priorities: It is hard to change everything; can you focus on some of the problems at first and others later? Medications for common stones are potassium citrate and thiazide diuretics. The former is for prevention of calcium stones or uric acid stones. The latter is to lower urine calcium excretion in idiopathic hypercalciuria.
Follow up Plan
There is no sense to treatment without follow up. If you are to change your fluid intake, diet, or add medications, you need to be rechecked with 24 hour urine testing to be sure the desired changes have occurred. If this is not mentioned, ask about the matter and have a plan. In general it is best to wait until changes have been made and followed for some weeks to be sure they can be tolerated and maintained. Be clear about how new testing will be arranged. Although the new results can be communicated by phone or mail, it is best to review things at least once in person.
Your Questions
You can see the problem. If you have special questions, they will tend to be squeezed in at the end, and may not get fully answered. Have your list in hand, and fit them when possible into the flow of the conversation. If some are really urgent, let your physician know and set time aside for them.
IMPLEMENT THE TREATMENT PLAN
Begin Right Away
While things are fresh in your mind, increase your fluids, make diet changes, and begin meds if prescribed. If you can, compare what you are doing with what your advocate heard at the visit, and consult your notes. If you are confused, call the physician’s office, or email, and ask if a nurse or the physician can clarify matters. If some things are impossible, likewise. Do not wait for the follow up visit to say that, for example, your job involves so many long meetings you cannot maintain the desired urine flow, or that a higher calcium diet is being limited by intolerance to dairy products. Use every means possible to create the program in real life that your physician proposed to you, and try to make it work most of the time.
Follow the Treatment Cycle
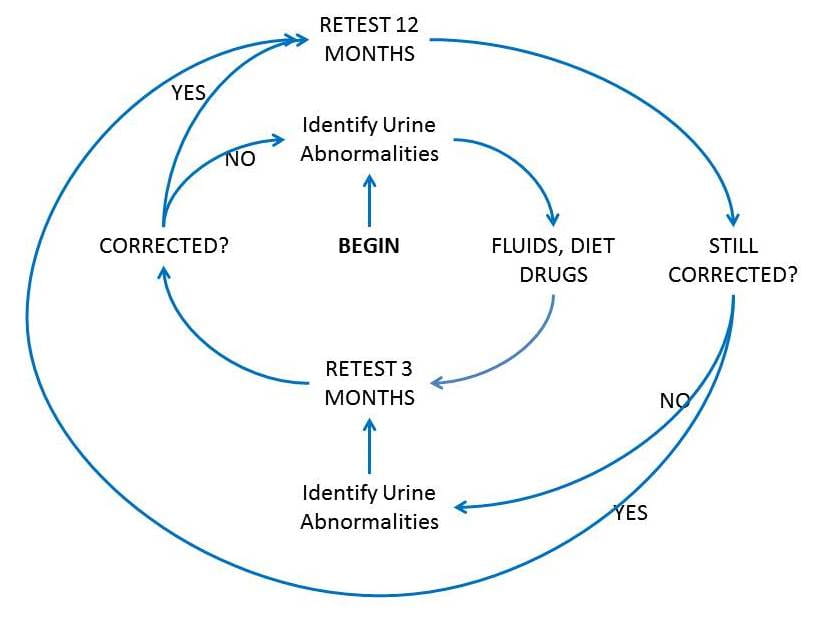 Being chronic, often a reflection of genetics, stone formation is not so much cured as managed, by fluids, diet, and drugs. Lacking cure your physician and you need to stay in the loop together, a loop I call the treatment cycle. The inner ring is a three month cycle to get urine chemistries into line. The outer ring is a yearly maintenance cycle once things are stable.
Being chronic, often a reflection of genetics, stone formation is not so much cured as managed, by fluids, diet, and drugs. Lacking cure your physician and you need to stay in the loop together, a loop I call the treatment cycle. The inner ring is a three month cycle to get urine chemistries into line. The outer ring is a yearly maintenance cycle once things are stable.
THE INNER RING
You already began, when your physician identified stone forming abnormalities in your urine and prescribed fluids, diet, and possibly medications. That is you, just to the right of the bold ‘BEGIN’ sign. The secret to success in preventing more stones is retesting to be sure the right things happened, and I have always preferred 3 months as an interval. There are only two outcomes. Success means the abnormalities are corrected. You leave the inner ring and retest 12 months later. Failure means not all are corrected, so you stay in the inner ring, work with some new combination of fluids, diet, and possibly drugs, then retest again in 3 months. You should review the new tests with your physician. One day you will achieve control and go out into the outer ring, yearly testing.
THE OUTER RING
It is here things fall apart. The yearly cycle is insurance that changes in you or your life have not altered urine chemistries enough to recreate the stone forming condition you came with. It is burdensome, and costs money, but even one shock wave treatment is thousands of dollars, often requires a stent procedure, and therefore far more of a trial. For the yearly testing, be sure and review results with your physician. Sometimes physicians will review results, find them perfect and just send a note. Sometimes email or a phone call is enough. If results are very abnormal or remain abnormal on repeated testing, a visit is preferable.
Stone Attack or Bleeding Despite Good Control
Write down the date and indicate if you think you know why it happened – eg. 6 hours at a soccer game with no fluids; a flight to Asia and back. Perhaps there is no inciting cause. Because you are being treated ‘successfully’, any event is important to understand. Did you have many stones at baseline? Did you have none? At some point a new CT may be needed to count stones and determine if you are still actively forming them. This is a complex medical decision, so your physician is key and needs to be informed. I have already pointed out the issue with continued stone activity despite treatment, and will repeat myself here. Ultimately stones are made of crystals, crystals obey physical laws, and the key law is that supersaturation is necessary – if not sufficient – for crystals to form and grow, and even to remain stable and not dissolve. Whatever the status of treated urine abnormalities, the net aggregate summary of your urine chemistries is supersaturation with respect to the crystals in stones you are forming. If you are actively forming new stones your urine supersaturation with respect to their crystals is too high and needs to be reduced further even if all of the individual components of stone risk in your urine – volume, calcium, oxalate, phosphate, pH, citrate, uric acid – are all within normal ranges. How your physician chooses to lower that supersaturation is likewise a complex medical matter, and you cannot do it alone.
I HAVE NO PROOF MY CYCLE WORKS
No prospective, randomized, double blind trial supports my cycle, and never will, because it is not a treatment but a way of using the components of treatment. We have one trial of fluids, and multiple trials for potassium citrate and thiazide diuretics. So the components work. But, they do not work without a structure. The trials had a structure, after all, even if it was simply to assure the drugs or water were being used. My cycle is much the same, except it assures as best one can that the treatments being used are doing what was intended.
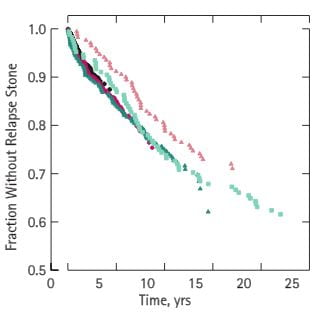 However, I do have long term observations, and though they do not prove what I do will work for you they demonstrate what I accomplished with patients in my practice who stayed in the cycle. Here are five cohorts of stone patients who entered 0-5, 5-10, 10-15, 15-20, and >20 years ago. All five of these life tables are similar – they do not differ significantly from one another. The five year cohort – black circles was >85% stone free by 5 years, the longest possible follow up interval. All of the 5 cohorts showed a gradual decay into new stones, but even for the longest observations – >20 years – 60% had been stone free. Even those not stone free did rather well. In the paper we show the numbers of stones per patient before and during treatment. Before treatment patients in the five cohorts formed between 1 – 2.5 new stones adjusted for the duration of the pre treatment stone interval. During the years in treatment, rates adjusted for duration of treatment ranged from 0.04 – 0.14 stones per patient, a fall of over 10 fold.
However, I do have long term observations, and though they do not prove what I do will work for you they demonstrate what I accomplished with patients in my practice who stayed in the cycle. Here are five cohorts of stone patients who entered 0-5, 5-10, 10-15, 15-20, and >20 years ago. All five of these life tables are similar – they do not differ significantly from one another. The five year cohort – black circles was >85% stone free by 5 years, the longest possible follow up interval. All of the 5 cohorts showed a gradual decay into new stones, but even for the longest observations – >20 years – 60% had been stone free. Even those not stone free did rather well. In the paper we show the numbers of stones per patient before and during treatment. Before treatment patients in the five cohorts formed between 1 – 2.5 new stones adjusted for the duration of the pre treatment stone interval. During the years in treatment, rates adjusted for duration of treatment ranged from 0.04 – 0.14 stones per patient, a fall of over 10 fold. 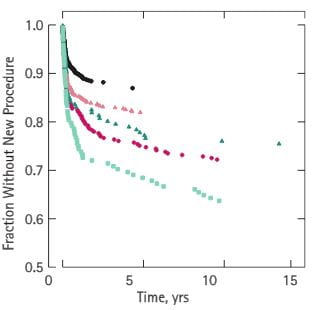 Rates of procedures fell even more dramatically. Procedures were frequent at the beginning for all cohorts. That is why the curves of procedure free state fell sharply from 1 to 3 years. Thereafter, all five cohorts showed a plateau, and after 15 years we had no procedures to count – thus the graph ends beyond that point. So what few stones did pass caused little by way of surgery. There is much in this observational paper to quarrel with. The successful patients are those who stayed in the program, but what happened to the many who left? Why did so many leave? Perhaps those who stayed were otherwise remarkably vigilant, or perhaps blessed with a finer biology than those who left and the latter continued to make stones despite my treatments. Probably many who left also left off treatment. I say all of this is correct and maintain only that can say what happened to those who chose to stay, and it is as this graph shows – imperfect but not bad. I could also say I am not unjustified in recommending my cycle to others, physicians and patients, because it is sensible to treat and look, adjust and look again, and be watchful when new stones keep coming. Likewise it is sensible to stay in partnership with your physician, or with your patients if you are the physician.
Rates of procedures fell even more dramatically. Procedures were frequent at the beginning for all cohorts. That is why the curves of procedure free state fell sharply from 1 to 3 years. Thereafter, all five cohorts showed a plateau, and after 15 years we had no procedures to count – thus the graph ends beyond that point. So what few stones did pass caused little by way of surgery. There is much in this observational paper to quarrel with. The successful patients are those who stayed in the program, but what happened to the many who left? Why did so many leave? Perhaps those who stayed were otherwise remarkably vigilant, or perhaps blessed with a finer biology than those who left and the latter continued to make stones despite my treatments. Probably many who left also left off treatment. I say all of this is correct and maintain only that can say what happened to those who chose to stay, and it is as this graph shows – imperfect but not bad. I could also say I am not unjustified in recommending my cycle to others, physicians and patients, because it is sensible to treat and look, adjust and look again, and be watchful when new stones keep coming. Likewise it is sensible to stay in partnership with your physician, or with your patients if you are the physician.
I DO NOT PRACTICE AS I HAVE DESCRIBED HERE
I have described my own practice on this site, and anyone who reads that description could say I have been disingenuous here. Not so. My practice is within a university, designed to support research as well as treatment of patients, and therefore subsidized by society and disconnected from the travails and limitations of real life. I set out to gather and retain data from every patient, so I work most slowly and take more time than physicians can who pay office rent, a nursing staff, and need to support their families from the proceeds of medical care. But I could practice excellent stone prevention within the common limits of clinical life if patients were willing to organize things as I propose here. I have not proved this assertion, but after so long a time at this one task will you not accept my judgment is probably reasonable?
I HAVE A SECRET
Diet change is maddeningly difficult and no one has enough time or skill to do all that needs to be done within a clinical visit. I work with Jill Harris, who offers diet counseling via the internet. She has often succeeded.
USE THIS SITE FOR EDUCATION
Physicians evaluate and treat people, but educated patients can help themselves and their physicians in so many ways. I have made links throughout for that general purpose, and the site has quite a bit about the causes and treatment of stones. When you have your diagnosis, treatments, laboratory abnormalities, feel free to browse here and read about what is being treated, or what has been found. Knowledge may not improve your treatment outcome, but it cannot do any harm.


Very informative and eye opening. I wish I had this information 20 years ago. I have some work to do and one of the areas on my list is to find a new doctor. I am in the western suburbs so would prefer one in this area. Is there a doctor that you could recommend ? One that approaches the treatment of kidney stones in the same manner as you? ( right now I would describe my treatment as crisis management- with little or no discussion on prevention.) Thank you again for taking the time to share your knowledge and expertise. It is very much appreciated
Hi Kim, Perhaps I could help but I do not think this public a place is proper for discussion of individual physician referrals. I have emailed you privately. Regards, Fred Coe
I very much enjoyed reading this article.
Hi Linda, I am glad you liked it. In fact you have lived it and very well indeed. Best, Fred
Love all your articles, very informative. Anything new with Cystine kidney stones?
Hi Cathy, I am pleased you like them. Nothing new. You would know if I had anything more. Best, Fred
Thank you. After 38 years of suffering calcium oxalate stones and the pain that accompanies them, I will keep better track of things from now on. Your article was enjoyable and really made me think. At this time I have 6 total stones with a 6mm causing hydronephrosis. Only once in 38 years have I known my kidneys to be stone free. I’m so lost. Thanks again.
Hi Laure, I am glad the article helped you. I hope that after all this time you have had proper blood and urine studies and are receiving treatments directed against the causes of your stones. I really do not think that calcium oxalate stones need to recur over so long a period. Regards, Fred Coe
It would be extremely beneficial for every ER to hand this important document to stone patients. Every Urologist and Nephrologist should send this out to patients prior to their first office appointment. Here’s to stone prevention – Cheers!
Hi Dr Coe,
How long does it typically take to form a calcium oxalate kidney stone (of size around 2 or 3 mm). Is it a matter of hours, days, weeks or does it take months?
Hi Pascal, It is certainly a matter of weeks to months. If I had to guess, months. But, that is a guess. Regards, Fred Coe
Hello everyone, it’s my first pay a visit at this website, and post is genuinely fruitful in favor of me, keep up posting
these content.
Dr. Coe,
Thank you for your research and devotion in the work you have done and are doing.. You are a jewel in the crown.
I had hyperparathyroid surgery last year. I do have osteoporosis. I would appreciate it if you could recommend a physician in my area. Matthew, NC (Charlotte, NC) I am most grateful if you could.
Thank you, Florence W
Hi Dr Coe,
I had a very big calcium oxalate/phosphate kidney stone (>5 cm) taken out of me after 3 surgeries, and I am working on stone prevention. With the results from the 24 hour urine analysis, even with some measurements that seem high, she concluded that she thought I just need to increase fluid intake. However, at the end of the appointment, she also threw in a diuretic (Indapamide 1.25mg) and said come back for a checkup in 6 months. I had a bad reaction to this drug and had to stop it after 3 days, and personally I would like to not use any medication, if possible. I communicated this to her team, haven’t gotten response, but I am wondering if I should get a second opinion on the proper prevention measures?
Hi Diana, I suspect your urine abnormalities were a high calcium excretion and high urine pH. Given calcium phosphate stones I would agree you should do as much as possible in treatment. The big issue is lowering calcium phosphate supersaturation. You are someone who should – if you have time – become familiar with supersaturation and how important it is. Low oxalate diet will only help with part of your problem, the other is to lower urine calcium and raise volume – both. If you cannot use a diuretic drug to lower urine calcium low diet sodium is the trick. Try for more than 2.5 liters of urine volume, steady throughout the day. Regards, Fred Coe
I’ve followed mother’s idea that big pharma-trained M. Ds. Have little respect for natural nutrition, preferring quick fix symptom drugs in place of actual cause-correcting natural nutrient application, so in my 71 years I stayed far from any Dr., aa i’ve had almost perfect health.
However. Switching from olive oil to sunflower my prostate reacted, and in ten days completely blocked all urine. Searching “is sunflower oil toxic,” it is blamed as prime cause of u. S. Cancer!
This lws to a permant catheter placement, and no naturopath physician with access to lab monitoring tools to watch diet effects on the swelling, and no M. D. will talk to naturopath physicians!
Now I have severe calcification in my bladder, forcing surgical removal of the last catheter. A suprapubic catheter was placed.
Question: how do I continue mother’s excellent health regimen, reverse calcification and prostate swelling with conflicting food forms for each malady, and, find a lab to work with my naturopath that accepts poverty level medicare and medicaid?
I live within public transit of Seattle. Having a clue where to direct my search ans reseaech will naturally be so much appreciated. My vitality and strength are years younger than my calendar years. People are amazed when I say my age, as I have younger appearance, vitality, and I do constant research on natural nutrient health, nytrient-dense garden soil production, and other interests.
Thank you, Dr. Coe, for the single most informative laymen treatise about common sense calcification knowledge and remedial avenues, expectations, and HOPE!
Hi Claude, Prostatic outflow obstruction often leads to bladder stones because of residual – retained urine. Is there a reason you do not have a prostate surgery? Modern laser techniques are excellent. With a chronic catheter it is very hard to stop bladder stones. Let me know, Regards, Fred Coe
Dr. Coe,
Thank you for your highly informative website – the best I have sourced to-date. After a recent kidney stone, a metabolic work-up revealed the following results outside reference ranges:
Calcium,U24Hr – 9.2 mmol/d – (Ref 2.5 – 7.5)
Oxalate,U24Hr – 616 umol/d – (Ref 100 – 440)
Urate,U24Hr – 4.7 mmol/d – (Ref 1.5 – 4.5)
Urea,U24Hr – 644 mmol/d – (Ref 170 – 580)
Sodium,U – 30 mmol/L – (Ref 40 – 200)
Anion Gap – 14 mmol/L – (Ref 3 – 13)
Phosphate,S – 0.6 mmol/L – (Ref 0.8 – 1.33)
Vit D – 65 nmol/L – (Ref 75 – 250)
All other measures were within reference ranges including pH,U (5.5), citrate,U24Hr (2.5 mmol/d), sodium,U24Hr (108 mmol/d), sodium (138 mmol/L), calcium (2.35 mmol/L) and potassium (3.9 mmol/L). Urine volume output was high/good (3.6L/d) and stone composition was calcium oxalate, mirroring that of stones from two previous episodes.
A fit, late forties male with no major health issues or medication requirements, I workout regularly, consume 2.5+ L of liquids/day (primarily filtered water) and generally eat a healthy, balanced diet moderate in protein. Minor health challenges include common digestive upset (at meals), lactose intolerance and adverse affects on sleep due to increased fluid consumption.
I have questions regarding the best prevention protocol and will be seeing a specialist next week to confer, however in preparation would greatly appreciate any thoughts or exchange of dialogue regarding my metrics – online or via email – to gain another perspective.
Thank you in advance for your follow-up should you be able to accommodate a reply.
Hi MIchael, You appear to have a very high urine calcium despite a reasonable urine sodium of 108 mEq/day, a high oxalate excretion, and assuming a normal blood screening you would be the common idiopathic calcium oxalate stone former with genetic – idiopathic – hypercalciuria. I have reviewed the treatment trials for your kind of patient. You might check out this approach to prepare for your visit. Things should go well. Regards, Fred Coe
Ironically, calcium,U24Hr was within reference range (6.9 mmol/d) in a full metabolic completed sixteen months ago after a calcium oxalate stone episode.
A few questions in follow-up should you have time for a response:
– is a bone density/disease test recommended for someone with idiopathic hypercalciuria?
– is low Vit D a factor in stone production and should it be remedied via diet/supplementation?
– with citrate supplementation, does the type matter (ie. potassium vs. magnesium vs calcium)?
– are the benefits of lemon juice consumption (citric acid) akin to that of citrate supplementation?
– are pro/prebiotics and digestive enzymes beneficial in influencing intestinal oxalate absorption?
– if 200 mg/day), what is the conversion factor to mmol?
Thank you kindly.
The last point in the prior reply was cut-off and should have read:
Finally, so that I may understand some of the measures noted in your website (eg. IH = >200 mg/day), what is the conversion factor to mmol?
Oh, I see; it is mg/day of calcium as the lowest detectable point of increased stone risk. Given the atomic weight of calcium as 40 mg/mmol that would be 5 mmol of calcium element. Regards, Fred Coe
Hi Michael, It is not rare for urine calcium to vary, especially with urine sodium or with diet. A bone density is a very good idea as bone disease is known to occur, Low vitamin D is not a cause of stones but is not healthy for bones and other organs and should always be corrected. Citrate supplementation is best with potassium, but is only important when needed – you have our writings on this. Lemon juice is a variable source of citrate; if the juice is too acid too much of the citrate molecules will be citric acid itself that confers no benefits. Probiotics etc are speculative as treatments and need trials. I do not know what the 200 mg/day means except perhaps diet total oxalate content; given an approximate molecular weight for oxalic acid of 90 mg/mmol 200 mg would be 2.22 mmol. Warm Regards, Fred Coe
Can you kindly expand on your response, “lemon juice is a variable source of citrate; if the juice is too acid too much of the citrate molecules will be citric acid itself that confers no benefits.”? If lemon juice acidity varies, is there a level that is considered ideal and most beneficial? Lemon juice concentrate (eg. Realemon) is said to provide 1.1 g of citric acid per ounce (versus fresh lemon juice at 1.44 g/oz) and according to the FDA, lemon juice from concentrate must have “a titratable acidity content of not less than 4.5 percent, by weight, calculated as anhydrous citrus acid.” Would lemon juice from concentrate be considered a more standardized level of acid content and therefore a better alternative than fresh lemon juice? If so, can high consumption pose any health risks from the added preservatives (ie. sodium benzoate, sodium metabisulfite and sodium sulfite). From what I have researched, ingesting 4 ounces per day of fresh lemon juice appears a good adjuct to diet changes. Thank you kindly.
Hi, I think this was duplicated on another day. Regards, Fred Coe
Can you kindly expand on your response, “lemon juice is a variable source of citrate; if the juice is too acid too much of the citrate molecules will be citric acid itself that confers no benefits.”? If lemon juice acidity varies, is there a level that is considered ideal and most beneficial? Lemon juice concentrate (eg. Realemon) is said to provide 1.1 g of citric acid per ounce (versus fresh lemon juice at 1.44 g/oz) and according to the FDA, lemon juice from concentrate must have “a titratable acidity content of not less than 4.5 percent, by weight, calculated as anhydrous citrus acid.” Would lemon juice from concentrate be considered a more standardized level of acid content and therefore a better alternative than fresh lemon juice? If so, can high consumption pose any health risks from the added sulfite preservatives. From what I have researched, ingesting 4 ounces per day of lemon juice appears a good adjuct to diet changes. Thank you.
Hi Michael, Reasonable issues, but the information is not there for us. It is the pH that determines the fraction of citrate as the anion vs citric acid. Lemon juice mostly has a low enough pH that most of the citrate is citric acid. The titratable acidity is of no value as it is a function of the total proton receptor molecules in the solution – not just citrate – and the pH. Concentrate is equally unknown. One needs the total citrate and pH of the finished beverage to figure out the citrate availability. Regards, Fred Coe
When taking the 24 hour urine test, should you eat and drink like you did when you first knew of the stone, to replicate what your urine was like then? Or should one continue to drink lots of fluids and eat in ways that prevent stones? Seems if you do the latter, you won’t really know what it was in your urine that caused the stone in the first place.
Hi Lee, What a fine question! To me the latter is right – do as you did, so one can tell what happened. Some do this, others changed their ways a while before coming in to see me, and would not want to go back. Usually there is enough wrong beside diet and fluids traces remain, but not always. But we have the history, too, so the original issues can be reconstructed. This area of medicine is very scientific and quantitative but people are not which makes things various. As to your question and what I would most like: Collect at first as things were, if possible. Regards, Fred Coe
What a nice article! Awesome information and suggestion!
I think Urinary Incontinence (UI) is world’s most unbearable and shameful diseases.
Basically, this disease is more danger for the employer women. Like as Cherry 🙁
Hi Cheery, Thank you. I wish I could write a site for UI but alas it is beyond me. If you have stones as well, the article is very useful. In fact, it is useful for any patient in terms of helping their physicians help them. Regards, Fred Coe
Question: I was put on Potassium Citrate to prevent kidney stones from one nephrologist. My new nephrologist says that potassium citrate is prone to cause uric acid stones and gout. Is this true? That is not what I read here or anywhere else. Is he mistaken? If so, why did one kidney doctor put me on K to prevent stones and the other wants to take me off of it? Thank you in advance.
Hi Gina, I do not know why your physician believes that potassium citrate will cause uric acid stones – it can not do that. As for gout, Likewise. I believe he/she simply did not make him/herself clear enough. You misheard. If not, that physician has the facts wrong. Regards, Fred Coe.
Can you recommend a major hospital to be tested at in Canada, as all we have here in Victoria, BC are local hospitals. Would UBC be okay, as they do a lot of research there of all types?
Hi Jeanne, UBC is an excellent place. I have no idea if they do stone prevention well but they will certainly be aware of what is happening internationally and are your best bet. Regards, Fred Coe
I have just had a CT scan reveal several stones in both kidneys. The last 90 days, I’ve been on Prescribed Anti Fungal meds for a toe fungus. I developed a fever, UTI, my DR said, and was put on antibiotics 3 times, finally the CT scan, kidney stones. Is there any connection to fungal 90 day meds in regards to the production of stones, sorry, I’m sure it sounds absurd, but these are 2mm 3mm and one is 6mm, so recent SOMETHING was going on. Thank you1
Hi Annette, I do not know how the medication would cause stones. But something caused them. Here is my newest article about what to do. Regards, Fred Coe
When I attempt to post a comment I get
The requested URL was rejected. Please consult with your administrator.
Your support ID is: 7339711674694711209
Hi, I am sorry. I am sending my programming colleague this material. I suspect our elaborate firewall did it. Thanks so much for sending this! Regards, Fred
Apparently you used ” signs that the firewall took as an injection threat. Comments cannot have ” in them. Best, Fred Coe
I’ve had repeated occurrences of calcium oxalate stones; and have been treated with K Citrate, and chlothalidone plus 50 mg Vitamin B for the past 10-15 years, mostly successfully. A recent bone density scan shows I have severe osteoporosis, and I’m only 62 years young. I’m supposed to research medication options and report back to my primary care physician. I have no idea if I have hypercalcemia…. Many osteo prevention medications mention they should not be taken if a person has this condition. Blood lab tests show calcium is in normal range, is this my answer? I’m at a loss on how to balance strong bones with a low calcium, low oxalate and low vitamin D diet. suggestions or advice welcome. Or are there questions you might suggest I ask during my follow up visit. thank you.
Hi Janis, I would guess you have idiopathic hypercalciuria and perhaps a low calcium diet. To know you would have had 24 hour urine tests and blood tests cannot detect this. The ideal would be low sodium high calcium diet, if so. Most important is a proper evaluation – here is a good plan. Best, Fred Coe
Greetings Dr. Coe.
Your website has so much great information, I have been re-reading it numerous times. I am looking for a lab where I can send a stone to be evaluated. Do you have a recommendation?
Hi Linda, We use Beck Labs in Indianapolis. It seems reliable. Regards, Fred Coe
Thank you so much for all the information! I have sarcoidosis, determined by a lung biopsy. I also have recently had 2 kidney stones, a 5 mm I passed and a 7 mm that they used shock wave therapy on. Both were 80% calcium oxalate and 20% calcium phosphate. I still have a 3 mm one in my other kidney. My urologist scheduled me for a CT scan in a year to see if that one has grown or if I have developed new ones. I have read what you have written here about idiopathic calcium stones since I have been unable to find anything specific on treating these in a person with sarcoid. I was wondering if you would treat these the same in my case as you would for those with idiopathic calcium stones. I have had blood tests, the last one where everything except creatinine fell within the reference range. That was 1.0 mg/dL and reference range was 0.5-0.9. My GFR was 57.61, which I know is low. I am 74.
I had a 24-hour urine test in which these were the results that were not in the threshold range:
High risk for stones:
Urine calcium 460 reference range mg/d <200
supersaturation CaP 2.14 reference range 0.5 – 2
24 Hour Urine pH 6.830 reference range 5.8 – 6.2
Urine Phosphorus 0.906 reference range g/d 0.6 -1.2 g/d
Calcium/Kg 7.6 reference range mg/kg/d <4.00
Calcium/Creatinine 420 reference range mg/g 550
Supersaturation Uric Acid 0.04 ref. range 0 – 1
Urine Uric Acid 0.460 reference range g/day <0.750
I have been on a low sodium diet for years, due to my Meniere's, and the nephrologist has suggested I also go on a low oxalate diet, which I have started. As previously stated, I drink lots of water throughout the day.
From what I've read, thiazides should be tried for this type of stone. However, I was previously on a thiazide 3 years ago for Meniere's and it caused hypercalcemia where I want to the ER and was told my kidneys were ready to shut down, so I cannot use this type of medication. My nephrologist is trying potassium citrate, starting at 5 MEQ tablets twice a day in order to try to bring down the calcium in my urine. She will see me again in a month, take a blood test, and if things go well, wants to up the dosage. I know this is also something you have suggested. However, I am having a difficult time with the potassium citrate as it is causing pain and nausea even though I am taking it with food and drinking a glass of water before and after the meal and am still on a low dosage. I am wondering if this will go away as my body adjusts to it and, also, if you have any other suggestions for a person with sarcoidosis, which my urologist believes is the main cause of my stones. Do you think the Crystal Light, etc. would work instead of the potassium citrate in my case? Thank you so very much for any help you may be able to provide since I just haven't been able to find anything on treating kidney stones in people with sarcoidosis.
Hi Connie, You do indeed have marked hypercalciuria and sarcoidosis may be the cause. High calcium from sarcoidosis is itself from increased levels of 1,25 vitamin D that can be measured. Because of the high 1,25D serum PTH is suppressed. Can you tell if you have such information? Having sarcoid and high urine calcium does not mean the sarcoid caused the high urine calcium. You say you follow a low sodium diet; what was the urine sodium in that sample? If you provide more I can try to be more helpful. As for potassium citrate, is your urine citrate low? It is not useful in general, only when needed. Regards, Fred Coe
My urine sodium in the sample was 98 with the reference of mmol/d 50 -150 and my urine citrate was 738 with a reference range of mg/d 550. I do not have my level of 1,25 vitamin D and don’t think I’ve ever been tested for that but my urologist told me not to take any vitamin D supplements. I had been tested for plain vitamin D, which came out low. My PTH was 27.9 pg/ml. with ref. range of 15.0 -65.0. Hope that helps.
Hi Connie, Given a normal citrate there is no basis for taking citrate. Your PTH is normal, not low as expected when sarcoid raises urine calcium. Your urine sodium is not low, it is at the US tolerable upper limit. 1500 mg is ideal, and at least try to get there as a way to lower urine calcium. Ask your physicians about this remark and be sure they agree. Regards, Fred Coe
In one of your articles you mentioned potassium citrate pills should be for people with calcium stones and a urine citrate excretion below 400 mg/day despite the kidney stone diet. In this same article you state you understood you have one trial of the agent in people with substantially more urine citrate. As my urine citrate is considerably higher than the 400 mg/day, I was wondering if you have any information on that trial. Thank you.
Hi Connie, All the information on all the trials is in the articles. Here is the best of them. The citrate article is here. I believe one trial did include patients whose urine citrate levels seemed adequate, and I wondered at it. In fact only two citrate trials have been significant, they are in the first of the two articles. I hope this is not too vague an answer. Some trials were done before the relationship between stone risk and urine citrate was established. Regards, Fred Coe
I did find these test results on vitamin D so I guess I did have this test. Hope this is what you need:
Component My Value Standard Range
Vitamin D, 25-Hydroxy 24 ng/mL 30 – 100 ng/mL
I could not find any other vitamin D tests, so I did not have the 1,25 vitamin D test. Is this a test I should have?
Hi Connie, you do need a 1,25 D as the very hallmark of sarcoid hypercalciuria is a high level of that hormone. Over production of that hormone is the actual efficient cause of the high urine calcium. Speak with your physicians about measuring it. Perhaps they have done so. Regards, Fred Coe
Thank you so very much for your replies, help, and suggestions. I have scheduled a test to measure 1,25 D, as it had not been done and I will follow your suggestion on discussing the urine sodium count with my physicians. I have tried to follow the 1500 mg of salt a day but I must not have been doing a very good job. I never add table salt to anything and do check labels of foods I buy. Guess I’ll have to do an even better job. Thank you again so very much for sharing your knowledge with us.
Dear Connie, Let me know. Regards, Fred Coe
I received the results of my 1,25 D test. It was in the normal range: Vitamin D, 1,25-Dihydroxy 62 pg/mL 18 – 78 pg/mL
So does this mean that my sarcoidosis is not what is causing my kidney stones but my high urine calcium level is what is causing them? Other than a low sodium diet (1500 mg) and drinking lots of fluids, do you have any other suggestions on lowering my urine calcium? I am already drinking lots of liquids and am on a low sodium diet, trying hard to maintain the 1500 mg a day, so I am frustrated and confused as what to do now. Also, I have osteopenia, so is it okay for me to take vitamin D supplements after all? Thank you!
Thank you.
I had a brother with kidney disease and wonder about the familial relationship. I do not use western medicine, but have been treating with a DC/homeopath and have been told that I am dealing with kidney issues. I have been put on 20 drops of phosphorous to drink in water throughout the day to break up stones. I have not passed any stones. Is there a way to test with urine, what type I may be dealing with?
Hi Jody, Whether Eastern, Western, or Homeopathic the medical care needs to respond to the physics of crystallization that control stone formation. Unlike most diseases stones arise from physical laws that precede biology and always hold. Phosphate in any form has no ability to improve stone disease as it will not defend against crystals. Proper 24 hour and blood testing will reveal the usual causes of stones, and in most cases diet changes specific to those causes can do a lot. I would hope you might consider doing that. Urine testing can give clues to the stone type and x ray images as well. Stones are highly familial, as you asked. Regards, Fred Coe
Dr. Coe,
I have lost about 30 pounds after taking Jill’s prevention course. I had a Roux En Y surgery 6 years ago to remove a GIST tumor from the Antrim of my stomach. I passed a calcium oxalyte stone about 4 months ago, but my latest CT scan showed no new ones had formed since last year. My calcium urine levels are in the 700s range, with very high output urine. Can you please look at the results I sent Jill and advise me on ways to keep calcium in my bones? I’m allergic to sulfa, and I also gave her my parathyroid tear results, which appeared to be in the normal range. I’m truly at a loss of what to do next and with my surgery, I’m a pretty unique case. Thanks in advance!
John O’Neill
Hi John, I have your results, and Jill is with me. You do indeed have a very high urine calcium level as well as a gastric GIST that has been resected. I cannot find any serum calcium or PTH levels, but they are crucial. These tumors can raise serum calcium and thereby raise urine calcium. The problem is so complex your physicians are totally the ones who need to work with it. The tumors can raise blood calcium via hormonal pathways including PTHrP. Given the complexity I cannot offer much more. Regards, Fred Coe
Dr. Coe, my calcium serum levels were 9.9 mg/dL (range 8.6 – 10.5 mg/dL is normal). My PTH levels were 20 pg/mL (range 9-77 pg/mL is normal). The PTH was intact, according to my urologist. I requested a Calcium Ionized Test, which I am to go get soon from reading way too much about things I do not understand completely. My tumor was removed, and I spent about 8 months on Gleevec to prevent recurrence, and it was considered to be successful, as 98% do not recur after a one year follow up for GIST. My largest concern is the calcium leaving my body via urine, as I am allergic to Sulfa. My urologist is also leaving town to take a new opportunity, so I want to ensure I have everything I need from an information perspective for a new urologist. My former urologist states that since I’m not forming new stones since last year, based on a recent CT scan, I should just continue with the low sodium diet, high water intake, etc. But I also read an article you wrote which states I should treat myself as an idiopathic calcium stone former and that I might need to find an appropriate diuretic to prevent the continued calcium leaching. I appreciate any further commentary, and I cannot thank you and Jill enough for all of your exceptional advice and prevention tips. You give so many stone formers hope for better days ahead!
Hi John, so the very high urine calcium is not due to obvious hyperparathyroidism or even hypercalcemia. I did find with cursory search an abstract and associated articles suggesting bone and mineral abnormalities with imatinib, your drug. I did not find urine calcium levels in the brief report. But I would bring the matter to my oncologist and perhaps the drug is affecting bone and raising urine calcium so. If this were my case I would do more research, but at this distance that would be intrusive. Best to mention to your physicians and see what they make of the matter. Regards, Fred Coe
Hello Dr. Coe
I am a 40 year old male that has had poor health ever since given a combination of drugs to treat a suspected prostatitis 15 years ago at age 25. The first drug was Ciprofloxacin which towards the end of the course was switched to Bactrim because of severe flank pain accompanied by Vioxx and Prednisone.
I soon then suffered permanent nerve and tendon damage. And many other issues in several organs. Something known as Floroquiolone Toxicty Sydrome.
I had a CAT scan 5 months ago which revealed a Right 2cm negative for hormone excreting adrenal mass and a 2.7 mm right kidney stone.
Left kidney has “increased interstitial densities within the left perinephric fat upper pole present representing chronic inflammatory stranding.” ???
Also bladder is distended with wall thickening suggesting cystitis.
I have recently been experiencing symptoms of kidney stones with frequent urgent sometimes painful urination and pain in kidneys and urinary system.
I am now allergic to antibiotics steroids and anti-inflammatory medication ever since my adverse reaction years ago.
Apparently Bactrim can cause the kidneys to retain the other drugs for too long and cause kidney problems.
I’ve also heard from many other people in the fluoroquinolone toxicity syndrome support group claiming to have kidney stones.
There is no family history at all of anyone having kidney stones for me.
One theory is that a specific gut bacteria Oxalabacter that is responsible for regulating oxalates in the body may have been wiped out by the Cipro and causing oxalate toxicity and kidney stones.
I’m not sure how to proceed with out being able to take antibiotics.
Hi Mike, I am sorry you developed that problem with Cipro – it is well known indeed. Oxalobacter deficits are a highly theoretical idea concerning a cause of high urine oxalate. But you do not know if you have high urine oxalate. Here is what I would do. Get proper 24 hour urine kidney stone testing and find out what is causing your stones. Here is a reasonable plan to follow. Then when you know what is wrong, act. Regards, Fred Coe
Hi Dr. Coe,
I meant to say in my last post that I have had four kidney stones removed. Thanks
Karen
Dr. Coe –
I so much appreciate your site. I have a history of kidney stones, passing my first one in 1995 which made me initially aware of them, and another also requiring an ER visit in 2016. Any imaging (related or unrelated) since that first in ’95 shows multiple stones in both kidneys. Nothing was ever done because they were just sitting there not obstructing.
Last winter, I had a several-days episode of gross hematuria (no pain). This led to the usual workup, with the final assumption being the stones as the cause, and chronic microhematuria. I was told I could have lithotripsy but it was up to me. In the meantime, I have developed front right targeted sharp abdominal pain which comes and goes upon physical exertion and have been found to be continually anemic. Sometimes the pain goes away for several days. Again, doctors don’t seem to be too concerned about this apparent stone moving around or other stones since the pain is intermittent and tolerable (for now).
My question is, can a stone which keeps jogging about for weeks or months cause damage?
Hi May, Your pain could be from the stone, but possibly not; the anemia is not from the stones, and should be understood better and perhaps treated. A stone that obstructs the kidney can destroy it, but your stones do not seem obstructing. Prevention is not mentioned – it is time to get it in place. Take a look here. Regards, Fred Coe
Dr. Coe – I was a patient of yours back in 2000, had a full workup with urine/blood collections, and it was determined that my stones were due to lifestyle and diet (not enough weight bearing exercises to drive excess calcium into my bones, stress (I had only gotten stones living in IL, near my family), high sodium foods, and low water intake). I did my yearly collection/labs until I moved to NJ in 2006, and enjoyed many years stone-free. I have recently been having several stones on a yearly basis, and decided to find a urologist and see if anything has changed. I’ve done one 24 hr collection and blood test, and was told to increase urine output, follow a low oxalate and low calcium diet (advised to avoid all dairy), and to start Potassium Citrate. I told the Dr that I wanted to make dietary changes first before going on any meds, and I am repeating labs in a few weeks, but wanted to know if it’s possible to ‘sign up’ again as a patient under you, and to be evaluated yearly long distance (I am still in NJ).
Hi Jennifer, Oh my! I am so concerned about low calcium diets = we all have bones, and these diets raise urine oxalate so we try to eat low oxalate diets. You were my patient, and I see no reason we cannot renew our prior medical relationship. Just call my secretary Kathleen Dineen, 773 702 1475 and she can help. Regards, Fred
Hi!Dr Coe.I am from the Philippines!your article is a must-read.I was diagnosed with kidney stone last 2013. It was accidentally known because i have chronic UTI. I suggested an ultrasound I was advised to removed it because it was quite big.I undergone nephrolithotomy on that year!I thought all were removed by the surgeon.Unfortunately after a series of ff-up check ups it was founf out that there are still stones not removed.i was prescribed with potassium citrate and allopurinol 100 mg. Way back 2015 i was advised to undergo shock wave lithotripsy.But the doctor postponed it due to low hemoglobin and hematocrit count.due to my pre menopausal.Despite taking medications the stone is still in my right kidney.I admit sometimes my lifestyle is a culprit especially on my diet. I did not visit my doctor again because i am struggling with my anemia. But is not persistent.Only if i have heavy periods..A month ago,i was awakened at 1 am due to severe right flank pain with prompted an ER visit.I was given Tramadol for pain and Ciprofloxacin.utrasound results showed that i had multiple stones
Hi Karen, You need to know what the stone is made of. What did the analysis show when it was removed. If it is magnesium ammonium phosphate – struvite – it is from infection and can recur and grow – a major urological issue. Urine culture is important looking for urea splitting organisms. If it is calcium based you need 24 hour urine testing and treatment directed at the cause. Shock wave lithotripsy is not an ideal solution. For the new stones flexible digital ureteroscopy would be ideal. You need your surgeons to do all this, as I am just a sideline commentator. Meds without knowledge of stone type is not a good idea, low likelihood of success. Regards, Fred Coe
Stones sizes are 7.1 mm, 1.3 x 0.67 cm and 1.5x 0.2 cm.2 days ago i had right flank pain again with UTI again as revealed by my urinalysis CBC results.I had high fever for 2 days with chills.My concern is about how to be stone free, free from stone formation woes and recurrent UTI which is very unsual since i have asymptomatic before.What amaze me in your article is about 24 hour urine testing which was not mentioned to me by my doctor.i truly wish you will reply .Thank you very much in advance doctor!
Hi Karen, The stones will probably need ureteroscopy as I mentioned. I know the Phillipines are lacking 24 hour urine testing right now, as I lectured there in November to about 1000 physicians, in Manila and Cebu City. Be sure about the urine infection: are the organisms capable of hydrolysing urea to ammonia? Typical examples are proteus, Klebsiella, pseudomonas, and enterococcus; the cultures will show this. Regards, Fred Coe
Hi Dr Coe,
I found out about you and this website through a Facebook Page I am a member of. I was diagnosed with a 4 cm kidney stone which was deemed 100% Carbonate Apatite in nature. I had surgery in January of last year (holmium laser stone ablation) They removed majority of the stone, inserted a stent and I was put on antibiotics to flush out the dust that remained post surgery. Fast forward to April of this year, and my Xray showed the stone had returned and was growing. I don’t feel anything and have no symptoms of any kind. I just had another Xray done today and seems the stone is there (not sure about if it has grown in size or not). I am seeing a Nephrologist in July to see if he has any suggestions. Considering how all this started with recurring UTIs back in 2017, what do you suggest I do? Any help you can provide will be greatly appreciated.
Thanks
Hi Sakshi, Carbonate apatite is a calcium phosphate stone that was removed by dusting. It has recurred or perhaps some residue of crystals simply grew. You need a proper evaluation for cause of the stones, and then treatment directed against those causes. X rays are mediocre for finding stones and useless for counting them, so consider a baseline ultra low dose CT. The infections probably played no role. Regards, Fred Coe
How is long distance travel a risk factor for stones. I’m flying to the mideast next year from the USA. A long flight. Anything I should do/know?
Thanks in advance!!!
Hi Morris, If you are not a stone former, and follow the usual precautions of flight that include hydration new stone onset is not a high likelihood – I do not have real data on this. If you are a stone former, discuss with your physician what abnormalities cause your stones and what specific changes you need to make during the flights and the general disruption of routine travel imposes. Regards, Fred Coe
Many months ago I described how my family experiences frequent stones that begin in childhood.-You had said you couldn’t find anything about this in rare disease databases: we have Silver-Russell Syndrome
(See also Beckwith-Wiedemann Syndrome)
Research is ongoing and stone formation and constantly high urine oxalate levels are common in my family but not well studied. The phenotype of these children is easy to see while harder to detect in adults (if one survives- they kinda grow into their large heads….). I currently have my son’s stones/ oxalates under control – mostly via treating digestive issues and leaky gut – once gut is well it is necessary to eat a high oxalate diet b/c this disorder is treated via the folate pathway. I think this is important because stone formers are told to avoid the very foods that are crucial to maintaining health in this syndrome. In those that are not recognized as having Silver-Russell syndrome, the commonly recommended stone diet could lead to a worsening of their illness and rapid health degeneration. Thanks for all your hard work in this area!
Hi Rebecca, In this reliable review of BWS hypercalciuria is identified as a factor in causing nephrocalcinosis. Silver Russell does not include nephrocalcinosis or stones, or hypercalciuria and appears quite distinct from BWS at a genetic level. Neither disease is especially associated with multiple stones in childhood but BWS is complex enough, and inclusive of hypercalciuria, so childhood stones seem plausible. A search of PubMed for “Beckwith-Wiedemann Syndrome AND kidney stones” yielded only two articles One concerned the increased frequency of hypercalciuria in the syndrome. Thus far oxalate has not been mentioned as a cause of stones. Before embarking on diet treatments I would hope that 24 hour urines are being obtained to determine the reason for stone formation – it is always urine chemistry that mediates the final crystallization events, so far as one now knows – and also that stones are all analysed as calcium phosphate stones would be indifferent to oxalate. Regards, Fred Coe
Hello Dr.Coe
I had CT urogram and ultrasound. A stone measuring 17 x 7 x 7 mm in the left UPJ proximal ureter. There is no other stone. A doctor said that I need to do surgery. Do I have a chance if I follow a low oxalate diet to reduce my stone? Is it dangerous to make a surgery? it can be some complications after surgery? I’m very afraid to do surgery.
Hi Svetlana, That is a very large stone and unlikely to pass. It could obstruct the kidney. Shock wave lithotripsy or ureteroscopy both are reasonable. Neither is very dangerous. Regards, Fred Coe
I have been diagnosed with distal RTA recently. I was on Temodar for about five years for my metastatic melanoma. It’s been at least 12 years since I got off of it. I am concerned that I am doomed. Does having this diagnosis mean that I will have to have dialysis or a kidney transplant? Can it be managed and not progress? Mary
Hi Mary, I believe I answered this. Fred
I am 47 years old I am three time operated kidney stones now at present stones reformation tell how to know reformation stop
Hi Prince, this is the ideal place to begin. It will take you to all the things you need. Regards, Fred Coe
Dear Dr Coe,
My brother had his first surgery at age 39 in jul 2015 for stent placement followed a month later for flexible pyeloscopy and laser. The stone was 11mm calculus in the lower pole of the left kidney with a partial staghorn appearance. He had never had an operation before, his medical history; insulin diabetic since age 19 and vasculitis since early 20’s which was dormant for over 15 years, he was on immunosuppressants and still to this day. The kidney stone was first discovered in 2006 during health check of kidneys for diabetes management, it was 10mm calculus in the lower pole of left kidney.
He began feeling that something was not quite right a few months after surgery, in May 2016 a CT KUB reveals multiple calculi located in pelvis and lower pole collecting system varying in size up to 13.5mm. On 4 September 2016 he has a procedure to place a stent. On 9 November he presents to emergency and passed large fragments which were sent to pathology. A Ct KUB on 10 November revealed 37mm calculus . PCNL was performed in November . The pathology results came in 21/11/16 revealing : magnesium ammonium phosphate, calcium phosphate, calcium carbonate and also Staphylococcus Epidermis – Heavy growth. Unfortunately his Doctor did not discuss the staph epidermis and there was no treatment plan for this infection, his Dr continued to treat my brother as a kidney stone former, and to date he has had over 20 procedures and recently after the last 2 surgeries in May and July has now been diagnosed as having recurrent life threatening urosepsis, He was only informed by another doctor in May that he has a staph infection in his stones. For the past 4 weeks he has been on Vancomycin via picc line which he travels to Canberra hospital every day to have changed, and they are scheduling him for a nephrectomy of left kidney. Many doctors have been consulting on his case these past couple of months trying to kill the staph bug and save the kidney however he also has a piece of metal leftover surgical material in the kidney and Doctors believe the staph may be attached to this and inhibiting their chances of ever killing the bug. The differential renal function performed on 28/7/20 was right kidney 65% and left kidney 35%. Dr Coe, I would greatly appreciate your thoughts regarding his case, and if you might offer your opinion on what impact the staph infection may have had regarding the rapid growth of stones my brother has experienced. Thank you kindly for your time. Regards, Renaee
Hi Renaee, I am afraid the situation is altogether too clear. Your either formed his stones originally for one or another common reason and they because infected, or possibly his impaired immune state led to kidney infection. In either case his bacteria contain urease that hydrolyses urea to ammonia and produce thereby the struvite stones. His surgeries have not been as ideal as possible given the retained metal, yet that kidney still has 35% of function. Being diabetic he is at high risk for diabetic kidney disease, so loss of kidney tissue is a shame. He needs help from the best surgical center possible and all effort should go to preserving kidney tissue. His physicians might want to consider acetohydroxamic acid at least short term as it inhibits urease and stops struvite formation. The drug is nasty and ridden with side effects, but he is in narrow straights. It might keep his kidney stone free if he can get full surgical removal of all stones from a definitive procedure. Of course antibiotics alone are futile, and being driven by living bacteria stones grow with horrifying speed. Regards, Fred Coe
I have been diagnosed with distal RTA recently. I was on Temodar for about five years for my metastatic melanoma. It’s been at least 12 years since I got off of it. I am concerned that I am doomed. Does having this diagnosis mean that I will have to have dialysis or a kidney transplant?
Hi Mary, A brief look on PubMed failed to get me any papers on renal tubular acidosis from Temodar. If you have developed it, that does not mean eventual kidney failure. Here is my best on RTA and stones. If your blood levels are abnormal your physicians will want to use alkali to bring total CO2 content to normal. High urine volume can help stave off stones, but a better approach is 24 hour testing to look for any specific factors. Urine pH will be high, citrate low, as in the article. A CT scan to look for tiny stones is a good idea. Regards, Fred Coe
Dr. Coe, thank you so much for your dedication and work…this website is soooo helpful!! Could I get your perspective on my case? I’m a long time stone former (first stone in 1999 at 36yrs old) who has been told in the past to not take calcium supplements and to drink more water. After 22 years and 3 stone events (with corresponding procedural action of external shock wave and ureteroscopy, I’m finally getting some attention in the prevention ways you have outlined – my most recent event in 12/2020 divulged multiple bilateral stones in the 4-6mm range with one lodged at bottom of ureter sized 11 x 4mm. 1/2021 Ureteroscopy to lithotripsy/basket all. Unsure of what still remains as fragments have been passing. *Regarding the blood tests I should be getting, my urology team has not ordered them. My PCP ordered a routine fasting blood draw (for my annual physical which occurred a few days before my last 12/2020 stone event), that measured all those you list above except phosphorus. Could you direct me to how to read the measurements? What levels are optimal and what’s concerning? All fall within standard norm ranges, but some are on the low end, some on the high end. I’ve asked my urology team about blood work, but no one is moving to order anything. I could pursue a private lab for the blood work, if you could tell me what to have measured. My clinical profile: I have very manageable UC (no drug treatment for past 35 years), diagnosed at 17 (I’m 57 now) have been vegan for 1.5 years which has helped my colon — colonoscopy in 2020 was beautiful (as opposed to 2018 that showed some irritation, small ulcer, and removal of an adenomatous polyp. Both parents and brother have/had stones. I have completed the 24 hr urine collection (Litholink) early this month and have obtained my report. Now I’m trying to construct my risk picture. 2 stones analyzed from procedure in 1/2021 are 70% CaOX monohidrate + 10%CaOx dihydrate + 20% caPhosphate (hydroxy-and-carbonate-apatite) Dietician consult a few days ago recommends increased fluids due to low urine volume, increase/normalize calcium intake at every meal for hyperoxaluria due to diet high for oxalate (she comments that urine oxalate is far from elevated), and to cease vitamin C supplementation. Follow up in 6 months. Any urine composition info you’d like…just let me know 🙂 Thank you, thank you Dr. Coe!!
Dear Cheryl, I gather your stones are calcium oxalate + 20% calcium phosphate. You have inactive UC without GI symptoms – it would seem. Here are several articles to help people read their 24 hour urine results. This one is an overview. This is a general introduction. Let me know if there are still some unanswered questions. Regards, Fred Coe
I’m glad there are fixed times for your first visit to prevent a kidney stone. I have heard they are awful. So I’d do anything to prevent them.
Dr. Coe, What is the CPT code of the 24 hour urine test that you suggest? My provider is currently ordering just creatinine 24 hour urine and calcium 24 hour urine tests and I know that much more is needed. Thank you for all that you do!
Hi Teresa, SIngle ordering is not helpful. Litholink is the best US vendor for complete 24 hour urine samples. It is a branch of LabCorp but run in its own facility. I founded it in 1995 but sold it in 2006 and have no stock in the company – therefore know it well and have no conflicts about saying it is the best around. Fred
Dr Coe, was wondering if you will be willing to do a online consultation I am a stone sufferer I have passed over 40 Uric acid stones in the last 5 years I have seen 4 different urologist I currently have 3 stones at the moment. Please I need this to stop. I am located outside the US.
Thank you,
John Paul
Hi John, I do telehealth through my university and I believe we have no special problem with international patients. My secretary is Banita Williams, US: 773 702 1475. She can arrange things for you. Regards, Fred Coe
Hello, Dr. Coe.
First, allow me to say thank you for providing so much helpful information online regarding kidney stones. I have learned quite a bit from detailed information you have shared.
I have passed more than a dozen kidney stones over the past 30 years. I recently passed another. This leaves me resolved to revisit options for prevention of future stones and options for breaking down existing stones (x-rays show several yet in my left kidney).
Rather than guessing and experimenting with dietary and lifestyle changes, I agree with your perspective that stone analysis and urinalysis are the proper starting point – to identify what type of stone is being formed and then the best course of treatment. My concern, though, is that the average urologist may not be as focused or as interested in being this thorough. (Admittedly, I am biased, based on past experiences with urologists who did not seem to provide good guidance or information.)
As I begin this process, should I aim to be working with a urologist or a nephrologist? And any other hints on how to get started on this journey to be kidney-stone free? (Or kidney-stone-light, if that is the best I can hope for.)
Hi Jerry, Among the more charming and thoughtful comments I have received! Stone prevention is an acquired taste, some urologists I have known are superb, some nephrologists – I say some because not all pursue it. Think about golf, some are really good. Here is an article on what to do – have done. Pick your best guess and see if she/he is enthusiastic. If you tell me where you live I can try to find someone I know who likes stone prevention. Best, Fred Coe
Hi Dr. Coe – I recently had a 5mm kidney stone removed. The crystallographic composition report I received back read:
No Nidus observed in the specimen
The stone is composed of:
Calcium Oxalate Monohudrate 85%
Calcium Oxalate Dihydrate 15%
I tried to find out what these percentages actually mean in reference to my diet and what to change but was unable to find anything online. I made an appointment with a nephrologist but will be unable to see them until the end of July and would like to figure out how to avoid any future stones by changing my diet. Any suggestions would be appreciated. Thank you, Patrick
Hi Patrick, COM is usually from high oxalate, low urine volume or some combination. COD is usually when urine calcium is high so crystals are forming with a great excess of calcium above oxalate. But I would recommend you get fully evaluated as to cause and not guess because random diet change is apt to fail. Regards, Fred Coe
I have not had a kidney stone in nine years because we cured my UTI, but my doctor still has me taking potassium citrate three times a day. At 75 years old and no other prescriptions, and no other illnesses, I would like to get off potassium citrate What is the purpose of potassium citrate?
Hi Lynn, I cannot say given no 24 hour urine testing information and no stone analysis. So I would have to offer a lot of ‘ifs. For example if the stone was uric acid, then potassium citrate is forever. If you provide more information I am happy to help. Otherwise, you will have to ask your prescribing physician who may have all of your information. Regards, Fred Coe
I’m having trouble finding an answer to this. I had a 6mm stone removed in April. 10 weeks later, an US found 3 small stones. 2 L, 1 R. I don’t know if they were there originally. I assume they may cause pain at some point. I am reluctant to run to the ED every time I experience flank pain, especiallyin the absenceof other symptoms. I get that fever, blood, vomiting accompanying pain is a reason. But, do I need to keep going to the ED?
Hi Kim, Given stones in the kidneys obstruction from stones is a risk. If you develop pain that might be a stone, a routine ultrasound is important – this need not be in an emergency room. Ultrasound is very insensitive to stones, so a baseline CT might be advisable. Regards, Fred Coe
Ok. I get that. Guess my next question is how soon? The ED is immediate, obviously. Outpatient takes a couple weeks.
Hi Kim, I guess for the time the ED is the only reasonable site. Stones can obstruct, cause pain, remain obstructing and the pain vanish but the kidney is damaged over time. You do have an important reason to consider removal of the remaining stones, or else busy yourself getting ultra sounds in the case that stone pain recurs. If the outpatient could be really no more than 2 weeks it is probably safe. More, not so much. Regards, Fred Coe
Dr. Coe,
It seems I am a chronic stone former, and have produced three stones so far. The first, a 4-5 mm stone, I passed without issue. Same with the second..I gave my GP a fragment of it (it too was supposedly 4-5 mm but I grew tired of straining my urine after a week and never captured it). The composition of the second stone was 85% dahllite and 15% struvite. I don’t know about the first because it went to my urologist and he didn’t share the info with me. I had my first stone about three years ago, my second back in March of this year, and the last one hit me in early August and is stuck in my left ureter. It is 8mm X 6mm and I have received one round of lithotripsy with zero success. I neglected to mention that a uretal stent was placed due to swelling in my kidney in early August as well. It has caused me extreme discomfort, nausea and subsequent weight loss—none of which are really being addressed by my doctor. I have been scheduled for another procedure on 9/13—what, I didn’t know until I logged into my “patient portal”…another round of lithotripsy. I personally feel that the doctor should utilize urteroscopy instead given what I have read on your site and others. I am so upset over the fact that I may have this stent in for who knows how much longer because of the fact that doctor doesn’t want to perform a more complicated procedure. Don’t I have I right as a patient to ask for a different procedure? Especially when SWL has already been done once and not only didn’t break the stone but failed to even move it?
I thank you for your opinion in this matter. I have tried to have my case sent to another doctor, but it seems no one will take a case once a medical device has been implanted.
Respectfully,
Lucy Peistrup
Hi Lucy, you are forming calcium phosphate stones which can grow rapidly and pose special issues. As I am not a surgeon and I have no direct knowledge of your particular situation I hesitate to make any comments about the choice of stone surgery. But I can say that in general, in a majority of cases, URS does seem preferable to SWL. Given your predicament, one useful help might be referral to a university stone program if your location so permits. I do agree that this kind of stone and the problems you have encountered might well benefit from a second opinion. Regards, Fred Coe
Hello, Dr. Coe,
Thank you for all the info. Some of it is not easy to digest, but I keep coming back and over time, I think, I get better understanding.
The ‘cookie cutter’ approach for prevention from my primary care and two urologist, I met, is disturbing – “Drink more water, don’t eat these foods” (gives a faded print out). I am awaiting nephrologist referral for 7 months now… Would you be able to recommend a prevention specialist in Toronto, Canada?
I am also unable to figure out how to test supersaturations in Canada.
Thanks a lot.
Hi LK, Cookie cutter approaches in medicine never make me satisfied. Unfortunately Canada does not have any vendors that provide 24 hour urine testing with SS values included. This despite brilliant scientists and physicians. There was an outstanding stone/mineral group in Toronto at the main university, but I have lost track of its present work. I found this center in Toronto, perhaps it is what you might want. I do not know the people. This site also looks promising, and mentions St Michaels which is where I used to know stone experts. I hope some of these leads pan out. Regards, Fred Coe
Hi Dr. Coe, I reached your site after finding the Kidney Stone Diet information from Jill Harris, and I’m happy to have found the invaluable volumes of information that you two have shared. I have passed 10 Calcium Oxalate stones over 35 years, and the rate accelerated recently. As it turns out, I believe I caused that through recent dietary changes. In an effort to improve my heart health and lose weight, I eliminated almost all meats except chicken, almost completely eliminated dairy, dramatically reduced sugar, and incorporated foods that I thought were heart healthy: green leafy veggies like spinach and kale, olives, olive oil, dates and figs, carrots, potatoes, popcorn, nuts including almonds, quinoa, beans and lentils, trail mix, V8 juice, tea. I even had a brief courtship with corn grits. You can probably imagine what happened. I passed another stone on Thanksgiving Day and found several more in my kidneys for the first time in my life. It appears based on the info I have been reading on your sites that I adopted a diet so friendly to stone formation that my kidneys could be listed on vacation sites as the Ritz Carlton for kidney stones, a place where they would be welcomed with open arms and continuously fed until they are fat and happy and eventually opt for an excursion through my inner trails. I was very surprised to learn that Calcium intake is so important, especially since my Urologist of 20 years simply said “Drink more water, and good luck”. So now I have completely shifted my diet to hit targets that Jill outlined for oxalate, calcium, salt, sugar and potassium, and I am in search of a good local Urologist who is interested in and knowledgeable about stone prevention. If you know of someone in the metro Detroit area, I live in Farmington Hills, MI and would very much appreciate your referral. I know that good doctors know other good doctors. Thanks in advance.