 The aims of stone prevention are to reduce the number of new stones formed, and to reduce the growth of stones in kidneys by lowering supersaturation. This means we gauge our success by counting and measuring stones.
The aims of stone prevention are to reduce the number of new stones formed, and to reduce the growth of stones in kidneys by lowering supersaturation. This means we gauge our success by counting and measuring stones.
Mostly, radiologists measure and we count.
That is why I wrote this article. Ultimately, physicians are responsible for counting, but patients can help a lot.
Moneylender and his Wife (Quentin Massys, 1465 – 1530), painted in 1514, hangs in the Musee du Louvre, Paris. Massys was ‘…the first important painter of the Antwerp school.’
How To Count New Stones
New vs. Pre-existing
A stone passed or removed or found in an image, and not present on a prior image, is a new stone. Therefore all such stones prior to the first available image are new. Subsequent ones must be counted against changes in the numbers of stones on subsequent images and counted as new or preexisting.
In patients with a massive stone burden, one may not be able to tell if a stone is new. I always assume it is, and work to lower supersaturations as much as possible.
What Does Active Mean?
Stone activity means new stones are forming or preexistent stones are growing. Obviously, any new stones means at some time or other the stone disease was active. But we use stone counts and growth to determine the need for and achievements of prevention efforts. So active or not is always placed in time, of which I can distinguish three periods: Remote, pre-treatment, and during treatment.
Remote Active Disease
Remote means we no longer believe prevention worthwhile. It is subtle. For example, decades ago seems reasonable, but I have no proof. A decade is perhaps reasonable. A few years ago is not remote. So this is pure judgment based on what the patient thinks, how severe the prior stones were, whether we have excellent reasons to believe we know why they occurred, and what has changed in the years between the last new stone.
Pre-treatment Active Disease
New stones have been forming in recent years, recent enough patients and their physicians believe prevention warranted. This level of activity is what we are treating against. We aim to reduce new stones below pre-treatment, ideally to 0.
In-treatment Active Disease
This is a reason to change things.
How to Quantify New Stone Activity
Stone Formation Rate
Stone formation rate is the number of new stones formed / years from last count or from the first stone(s) formed.
Both are of value.
The latter is like an overall average. The former tells about more recent changes, especially during treatment.
Because we cannot know when the first stone(s) formed, we cannot calculate from it a stone formation rate.
Inter-event Interval
This is the time between new stones, which means one requires successive images.
For example, if 1 new stone appears between successive CT scans, or if 10 appear, the measurable interval is the same. Likewise, if 1 or 10 new stones are passed or removed at a single ER visit or surgery and new images show one or more of these were new, it is still one event. So stone counts and inter-stone intervals are not necessarily the same.
If an event of stone passage or removal has no new stones in it, the event is not a new stone event and it does not count. The inter-event interval remains the time since the last new stone event.
Examples
Example 1. A women passed her first stone 10 years ago; her CT showed no stones in either kidney. She passed another stone 3 years ago, which had to be new, giving 1 new stone in 7 years. Her second CT 2 years ago showed 4 stones, 2 on each side. She has had 5 new stones in 8 years. A routine follow up CT one week ago showed 3 stones on the left and 2 on the right, meaning she had added one additional new stone, making a total of 6 new stone in 10 years, with a lifetime total of 7 stones. The bolding of ‘new’ is to emphasize that the first stone is of unknown duration, whereas the ones thereafter are new within a known period, of 10 years. She has obvious active and accelerating disease.
Example 2. A man passed his first stone 10 years ago, and his CT showed 4 stones, 2 on each side. He has formed 5 new stones, but when he formed them is unknowable. One year ago he passed two stones in a single event. His new CT shows 2 stones on the left, none on the right, and his pain was on the right. We presume he passed two old stones. New stone rate, 0/10 years. Since the event was null, without new stones, he has an inter-stone interval of >10 years. Because he has a stone burden, we would treat to reduce or prevent stone growth.
Example 3. A woman formed her first stone 1 year ago, and her CT showed no stones in either kidney. She has had no more stone events and a new CT shows no stones in either kidney. Her new stone rate is 0, her inter-stone interval is >1 year. Being a single stone former, we will choose prevention given reasonable information that untreated she has a significant risk of more stones.
Example 4. A woman with massive bilateral nephrocalcinosis had episodes of stone passage monthly, on average. One cannot detect if the stone burden is changing. Because we cannot be sure, we err on the side of ‘best for patient’ which means assume stones are forming – on old stones, perhaps – and therefore that these are indeed new stone events. Reduction of supersaturation is the only reasonable approach, coupled, perhaps, with surgery to reduce stone burden and therefore morbidity and rates of surgery for stone passage. Her rate is 12 stones/year, inter-event interval 1 month.
Side of Passage and Counting
Example 2 illustrates the importance of records or clinical history. Suppose he had passed his newest stone from the left, not the right. Then, it would have been a new stone as the number of stones on the left remained at 2 before and after stone passage. Patients can help a lot here by keeping careful track of which side pain was on, and from which side stones were removed.
Stones During Treatment
In each of the four examples, stone counting has given us a baseline against which to evaluate the effectiveness of treatment. In example 1 we need to lower stone rate below 1/7 years – her baseline lowest rate -, and lengthen interstone interval above her baseline of 7 years. For example 2, we have little activity, and will treat to prevent new stone growth – not a matter we detail here. Example 3 should not form new stones, ideally, for many years, given only 12% relapse at 5 years of mere increase in fluid intake. Example 4 has very frequent stone events, perhaps new, and we would hope to lengthen the interval between events from the baseline of one month.
How To Count Stones in Kidneys
From everything I have just written, it is apparent that new stone counting depends utterly on the images we have and how well we read them.
Kinds of Images
Nothing Compares to CT Scans
I am devoted to CT images for stone work. Modern low dose instruments much reduce risk by reducing radiation exposure to below 3 mSv. Nothing comes close to a CT scan for counting stones. So whenever possible I get them and use them.
Flat Plates are Mediocre.
Simple flat plates are very hard to use. The bowel overlays the kidneys, stones show as faint white spots, or not. Ribs can be in the way. I squint at the image and try to figure out where, and if, stones are. If one is highly experienced and careful, they are of modest sensitivity. I say this after having read thousands of these images over decades of practice. A recent review gives a sensitivity of 57% vs. 95% for low dose CT, and a specificity of 76% vs. 98% for low dose CT. This means that nearly 1/2 of stones will be missed.
Renal Ultrasound
In the most expert hands ultrasonography has a sensitivity of 84% vs. 95% for low dose CT, and a specificity of 53% vs. 98% for low dose CT. This means that ultrasound can misclassify nearly 1/2 of suspicious objects as stones.
Errors From Changing Image Types
Imagine the first image for a patient is a flat plate showing 1 stone on the right. Several years later, a stone is passed from the right and a CT shows 2 stones on the right and 3 more on the left. What do we make of this? New stones or change of technique?
To me these are not new stones because a flat plate has poor sensitivity compared to a CT. But we cannot be sure, can we?
Imagine another patient with 3 stones in the right kidney seen on CT. After ureteroscopic removal of 3 stones, a flat plate shows no stones. One year later, a new CT shows 2 stones on the operated side. One presumes they are new, but the flat plate could be insensitive and the surgeon unable to see several stones during the surgery. Or, possibly, the ‘stones’ are tissue calcifications not seen during surgery. With ultra low dose instruments, perhaps a majority of such images will be CTs.
How I Record The Count
I list the number of stones in each kidney vs. date of the images and the image type. I draw the stones in on little kidney outlines so I have a record of what I could see at the time.
Value of Surgical Observations
During PERC or ureteroscopy surgeons can estimate numbers of ‘stones’ that are actually tissue calcifications. These will not pass, cannot be removed in most cases, and need to be subtracted from the stone count.
Renal Colic and Hematuria Without Passage or Removal
Quite apart from conventional new stone counting, we have patients who have attacks of pain with hematuria due to either stones too tiny or fleeting to visualize, or to passage of crystals. For them, activity is simply the numbers and spacing of attacks. But the larger problem is to identify these attacks as against the large complex of pain syndromes found among stone formers.
The key is renal colic, a peculiar pain produced by stone passage.
Colic is unique enough that we can use it as evidence for passage of a stone, or of crystals, even if we fail to find the stone or crystals by direct visualization. The details of the pain are discussed a bit later in this article, but right now I want to use it, so assume I will shortly tell you how to identify it.
Small Stones or Late or Insensitive Visualization
Not rarely, an attack of typical colic with hematuria is unaccompanied by a stone. Perhaps it passed unnoticed. Perhaps it was small and only ultrasound or flat plate available. Often, one finds on CT ‘stranding’ around the kidney on the same side as pain, indicating a recent obstruction, or even dilation of the renal collecting system. To me all of these are stone attacks until proven otherwise.
Crystal Passage Attacks
An attack of renal colic with hematuria and no obvious stone or obstruction or stranding is, to me, likely the passage of crystals, and I encourage physicians to look for them. Crystalluria/hematuria is very well known among children with idiopathic hypercalciuria and treated with stone prevention measures to lower supersaturation. I have seen it among adults but never published the cases.
Example 5. An 18 year old man had 3 attacks of renal colic with hematuria during the past 2 years. A single urological investigation shows no reason for bleeding, and a CT shows no stones. Calcium oxalate crystals have been found on one occasion. His second attack was 6 months after his first, his third was 8 months later.
Crystalluria/hematuria attacks should be investigated as to cause and then treated. Such attacks are disturbing and disruptive to the patient, even if no stones can be found. Example 5 has an inter-event interval averaging 7 months. Successful treatment would ideally bring these attacks to a halt or at least increase the interval markedly.
Special Problems
Crystal attacks not rarely reflect drugs, especially antivirals. Their prevention concerns drug management, not stone prevention, and is beyond this site at present. One diagnoses the drug crystal attacks by knowing about the drug and demonstrating the crystals.
Sometimes, bleeding from a tumor or other cause produces clots that pass and cause renal colic. For this reason we always need urological assessment to be sure bleeding has no obvious cause. Uncommon ‘matrix’ stones composed of only urine protein can form and pass causing colic. I always advise these patients to void through filters in hopes of tiny stones, matrix stones, even masses of crystals.
Specifics of Renal Colic
I promised to tell about the special properties of renal colic, and here they are. Mike Borofsky did a very fine article on this. I have only to elaborate from a more clinical and descriptive viewpoint.
I Assume Experienced Patients Can Tell
If my patient has had at least one certain episode of stone passage with pain, I accept their opinion about subsequent episodes of pain as being from a stone or not. The pain of stone passage is odd. It has a foreign, peculiar character. Patients recognize it, and I trust them to know.
When patients are not sure, from inexperience or otherwise, the traits below are very useful. I have found them so for all of the thousands of instances during which I struggled to sort out stones from everything else.
Beginning
The pain begins suddenly. Often it is not so severe as startling, and ominous.
I think the onset is sudden because pain arises from acute obstruction of a kidney. It is ominous because peculiar enough patients recognize it for what it is and experience immediate dread.
I should say, this pain is indifferent to its cause. A blood clot or sloughed renal papilla will feel the same as a stone. It is the acute obstruction that causes the pain.
Location, Course, Associations, Severity
Certainly at the beginning, the pain lies vaguely in one flank or the other most of the time. But I have examples of a midline upper abdominal beginning that only lateralized to one flank over an hour or so and was initially thought a myocardial infarction or gall stone. As it becomes more severe, the pain will eventually find its way to one side, unless stones are passing from both – a dreary and worrisome event.
Pain rises to a plateau of severity over some minutes to a few hours as the obstruction leads to increasing dilation of the urinary system with urine. It is indifferent to movement – bending, turning, walking, lying still. Being visceral, arising from an internal organ, it has a vague flank location and myriad internal reactions – nausea, vomiting, diarrhea, sweating, and changes in pulse rate or blood pressure.
Severity is famous, and terrible.
Character
Among my patients have been poets, significant writers, passionate athletes well acquainted with their bodies, and to them as to most I have posed the question of character – what the pain feels like. All agree it is odd, unmistakable once you have known it, and the oddness has nothing to do with its severity as the pain seems odd even when mild.
Some call it burning, some boring – like a drill. Some combine the two – a hot piercing object. Many just stare, unable to find similes, but say it is like no other pain – strange, foreign, alien, and altogether evil.
Radiation and Movement with Stones
In men, stone pain can radiate to the testicle on the same side as the stone, in women to the labia.
If the obstructing stone moves down the ureter, pain usually follows it downward, along the path your fingers might make if spread out over the abdomen, the thumb hooked just below the lowest rib.
Magical Disappearance
Most important, if obstruction ceases – the stone passes, ceases to obstruct, for example – pain ends abruptly, magically. No pain of such consequence in all of clinical medicine has this property except if from a stone. I have observed it in retained biliary and common duct stones as perhaps my only other examples.
To detect this trait, be careful of what you ask for. Soreness and a general sense of ill dissipate over an hour or more, but the real pain – the one patients know as evil – that pain ceases with surprise, a sense of amazement. Even if pain meds have been used, this odd ending is evident.
Pain with Chronic Obstruction
If a stone fails to pass and obstructs for days, pain may get better. It does not so much magically disappear as fade. If under surveillance, physicians will tend to the problem. Sometimes, colic will gradually subside, no images made, and things simply go by with missed obstruction. This can destroy a kidney. So, if pain seems like a stone, one needs a physician to oversee matters. They will do images – perhaps ultrasound – and keep things safe.
Confused with Other Pains
I am rarely confused, nor are patients. Renal colic, gallstone passage, acute pancreatitis, and myocardial infarction can seem alike at the beginning. So physicians and patients need be careful. But in all my decades of work, colic had more or less always been stone passage.
If lodged at the junction of the bladder and ureter, a stone mimics infection – urinary frequency, urgency, burning. This is not typical stone pain, but may well lead to an image that discloses the stone.
Back Pains of Other Sorts
Back pain that is not renal colic is not a clue to a stone event per se but often to pathology caused by stone burden, stone events, surgery, and infection.
Stones in Kidneys
We know that many people who have significant stone burdens have back pain that is not typical of stone passage but severe and often disabling. Most of us believe it is from the stones but we lack trials to prove surgery helps. For this not uncommon situation we need trials to determine what characteristics of pain or stones justify surgery. Stone prevention efforts may be worthwhile to reduce new stones that could possibly worsen matters.
If pain is on the same side as a kidney with even one stone, questions arise as to be benefits of surgery. Lacking trials, this becomes a difficult balancing of risk to benefit.
No Stones in Kidneys
If there are no stones in either kidney pain is not presently due to stones even if it is due to spasms and inflammation from prior stones.
But not rarely, pain altogether unrelated to stones, because in the flank, or back, or groin associates itself with stone pain in the minds of patients and physicians, and misleads. Here, physical medicine experts can help. Likewise, this maxim: If the pain responds to posture, movement, exercise, it may well represent long term effects of stone events on the back muscles but not pain from the immediate effects of stones themselves.
Events vs. Stones
One cannot help but see by now that events and stones are not the same. Events are when we have a chance to count and there is indeed at least one new stone. Counts are what we make at each event. So an event can have anywhere from one to many new stones.
Here are some of my own results. Joan Parks and I used all events and stones from 371 men to make this picture.
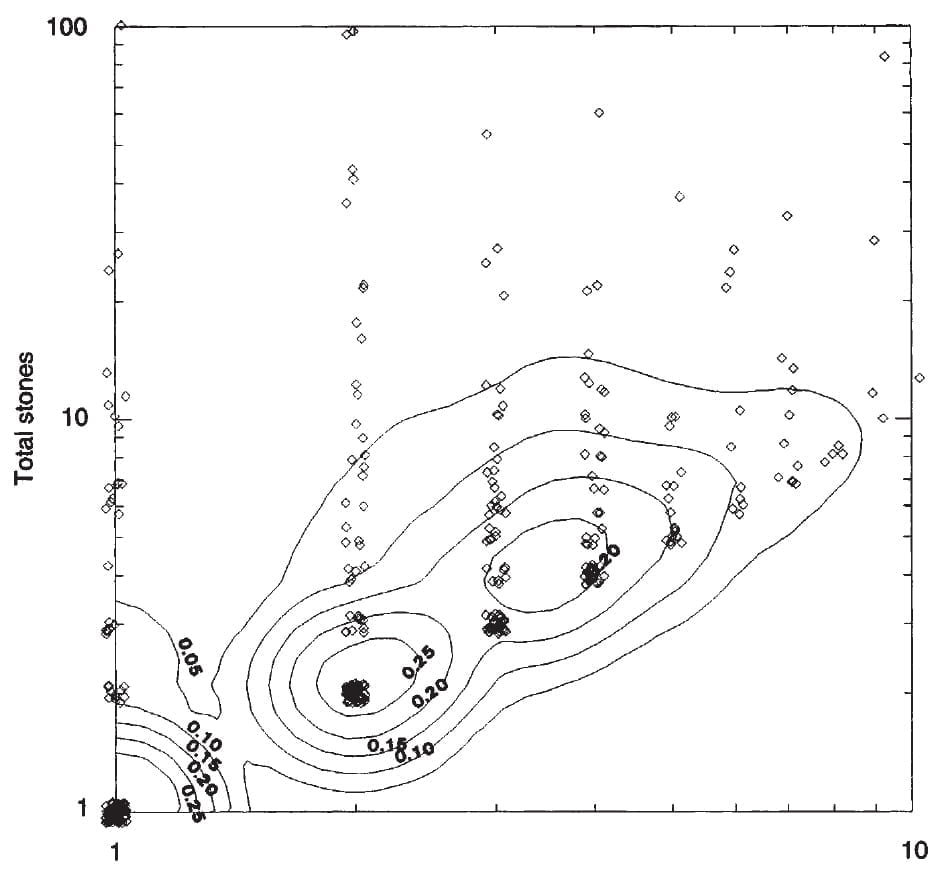
On the horizontal axis are the number of events for each man (shown as a single circle). On the vertical axis are the number of counted stones for all events that patient had.
To make each point visible, I jittered them randomly. That is why some lie just outside the graph borders.
One event, one or more stones
For example, many men clustered at the bottom left corner each had one event with one total stone. But many had one event and 10 or more stones. One man had 100 stones in his one event (upper left corner of the graph).
Two events, two or more stones
Another large group of men had 2 events each. They are centered above the second tick mark from the lower left corner. Many of these men had only 2 stones, one in each event. They form the ball of points. But a large number had many more than 2 stones. Once again several had 100 stones in their 2 events.
Three or four events
Given our limited number of cases, we could identify obvious clusters only for 3 and 4 events, easily seen on the graph. As in the other events, many men had equal event and new stone counts, many had more than one stone on average per event.
The Contour lines
The overlay of contour lines gives a sense of how many points are in an event space, as if they were showing the heights of hills viewed from directly above. The 1 and 2 event spaces have separate contours, meaning they are truly separate. The 3 and 4 are bounded by a single contour meaning that as the numbers become smaller these mounds are more like little hills filled in between.
What This Means
It means the stone counts can be astronomical but clustered in a few events. It can also mean that many events yield only few total stones. The two are not closely related. Of the two, the sturdier is event number. How many stones in an event was determined here because for decades we had the luxury of time to question our patients and pursue old records to get stone counts in an event.
Events vs. Time
The Longer You Wait, the More Events
From the same study, we were able to calculate the event rate (number/year) and the number of events in relation to the duration of
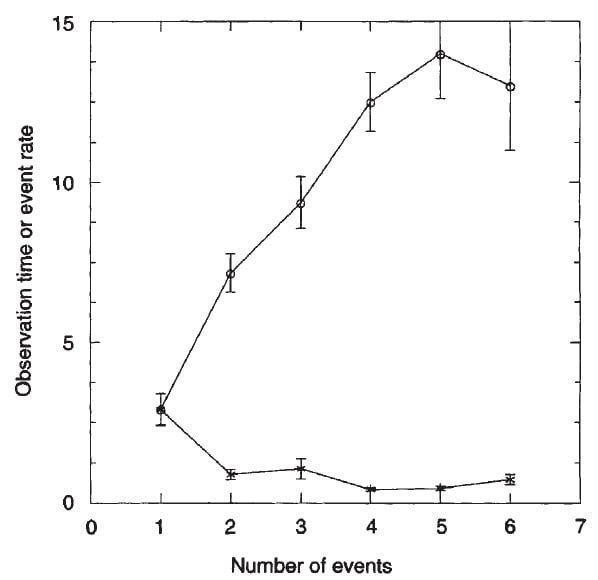
observation from first stone. On the graph, number of events is on the horizontal axis. Stars show the event rate, plotted on the vertical axis. Circles show the time of observation from the first stone, in years, also plotted on the vertical axis.
For example, one event had a mean observation time of 2.5 years from first stone, and a rate of 2.5 events/year.
There is no way you can miss the meaning of this graph. The more years that have elapsed from the first stone, the more events. This is what it means to wait once stones have begun. The common reward is more stone events, meaning more stones.
Event Rate Does Not Change
Because the number of events rises more or less with the time patients are observed, the event rate/year – plotted here – is more or less constant at a mean of about 1 – 1.5 event/year.
You might see an apparent error on this graph. For example, with 2 events and a mean observation time of about 7 years, one expects events/year to be 2/7 events per year, not about 1. But the mean of the ratio can depart greatly from the ratio of means, as is the case here because the means arise from a large distribution of observation times skewed left – downward. So many values would have been 2 events in a lot less than 7 years.
Events vs. Relapse
Everything in the figures arose from before treatment. But we then treated everyone as best we could and observed if relapse – new stones – occurred. We found something very important.
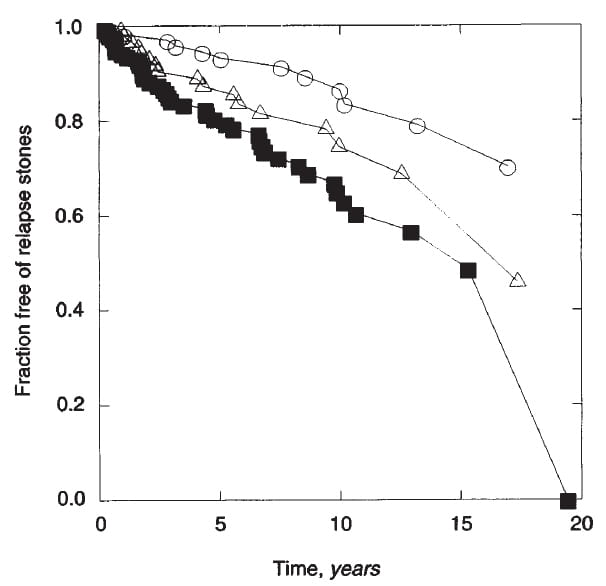
The vertical axis shows the fraction of patients free of relapse vs. duration of treatment (yrs) on the horizontal axis. Those with 1 event before treatment (circles) did best; at 10 years over 80% were free of new stones. Those with 2 events (triangles) did less well, and those with 3 or more events did worst of all (black squares) with less than 60% stone free.
Of course, though prospective, these are observations not a trial. Moreover, the patients were all men, as we lacked sufficient women, then, to make our distribution graphs.
But using only trial data, I have shown the very same phenomenon. During all of the randomized controlled trials we have had in stone disease, the percent of patients who relapsed during treatment with active drug rose with the number of stones formed prior to the trial. In other words, waiting treatment for more events means treatment gives a poorer outcome.
Avoid Confusion: Count
Confusion leads careless shopkeepers into bankruptcy, and distracted pilots into the sides of mountains. Counting tells us who to treat, and counting tells us how well we are doing.
All we do relies on counting well.
Good Prevention Can Look Bad
To count stones new when they are not makes treatment folly.
Like a mariner lost for want of proper charting, we despair of successful prevention which, present all the while, we cannot recognize because we counted wrong. And we, in consequent, regardless flailings, may undo what was a simple triumph.
Bad Prevention Can Look Good
To count stones old when they are new creates delusion.
Caught up in a fantasy of achievement, physician and patient await, unknowing, what nature will present them – in the act. What could have been and what will be are not a joyful pairing.
Pain Does Not Assure Active Stone Disease
Chronic pain is serious, important. It needs to be understood and treated. But pain need not mean active new stones are forming. Stone burden may cause pain that stone prevention may not abolish. As I have said, we lack trials to know if surgery benefits it.
Chronic pain without stones in either kidney may have nothing to do with stone disease. It requires astute evaluation on an individual basis. It requires treatment, and is a very important matter. But it need not denote active stone disease.
Renal Colic is a Good Indicator of Stones
On the other hand, renal colic is so distinctive it marks some kind of stone or crystal activity. While colic does not have the certainty of a passed or removed stone, it denotes a need for treatment – crystals, bleeding from some non stone related cause, tiny stones we are not imaging.
What Patients Can Do
Keep track.
When were stones passed or removed? How many stones did the radiologist report on each side and what kind of image was it? Did you fall into the trap of changing image sensitivity – flat plate after surgery shows no stones, CT one year later shows 5, and who knows what really happened?
This is not to suggest patients do without physicians. Physicians count new stones and read images more skillfully than patients can – they are trained to do it. But their time is limited, and most lack support people to help keep track of dates and events. They must do it all in the brief minutes allowed for a modern clinical visit.
Careful patients, who have their information at hand and good reasons to devote considerable time to the matter, can help immeasurably.
True, they must be very careful and accurate, but most should be so. We calculate our taxes, we make our budgets. We do a lot of dated quantitative counting work. What could be more important than to help clarify the state of our own disease?
I want to thank Dr John Asplin for reading this article and pointing out important confusions in the examples which I believe I have corrected. His help has been and is indispensable to me in running this site.


Anyone in Ontario seen Dr Sener at University Hospital, London? His credentials look amazing. I am booked June 24th as referred by my urologist. (Who wanted me seen sooner than later) The dilemma…reconstruct my left ureter or robotic nephrectomy to remove my kidney which is currently functioning at 20% has 3 stones (the biggest 6mm) and is not draining properly even with a stent and no visible obstruction. My next question (which I will call my urologist)…since my ureter has closed twice should I have a stent placed in the mean time? (Last stent was removed March 13 because of a UTI and 2 weeks of cipro. Incidentally of which I asked my urologist about because every procedure plus 2 UTIs since June I have been given cipro….I had my right wrist give out twice and unable to grasp items for 2 or 3 days each time….I have read the horrors of cipro and was told they usually worry about kids??!?
First stones 25 yrs ago…lithotripsy
No issues until one got stuck June 2018..3 uteroscopy…cystoscopy…5 stents…stones removed both sides….kind of afraid of what my future holds…calcium oxalate and phosphate stones…following duet for both types since June admittedly was a coffeeholic and loved salt and sweets
Hi Kim, While Dr Sener is clearly outstanding, his main emphasis is in transplant, whereas your problems are complications from stones. Dr John Denstedt is a world famous expert in kidney stone surgery and I would consider him as a better alternative. I imaging Dr Sener would agree with me. Regards, Fred Coe
With MSK,,. I am unable to count stones,as each CT scan shows bilateral calcifications in the medulla and multiple bilateral renal calculi. Six months after the last CT scan shows the same along with identification of an up to 5mm,and a 3mm in the other kidney as of 3/19. In mid February,I passed 7small calcium oxalate stones in 11days with no symptoms except hematuria. My 4/19 24urine came back the best it’s been in 1 1/2 years. My nephrologist is satisfied with how I am doing and feels the meds(allopurinol,hydrochlorothiazide,ketoconozole tablet,and Tums w/meals),diet,and fluids are working. Since I can’t count stones on a CT,I base my progress on stone production needing intervention,which has decreased from 3procedures annually to 1 every 1 1/2 years approximately. I see the urologist in July to discuss the 5mm stone. The nephrologist has graduated me from 3month interval visits to 6 month. Am I correct in as to how I am evaluating my kidney stone prevention plan since it cannot be done via CT? Every radiologist I have seen comments that they have never seen so many stones.
Hi Elan, Yes. With so many all you can do is could stone passage events and procedures. Regards, Fred Coe
Hi Dr. Coe – Thank you for all of your helpful information about kidney stones. I am especially interested in your mention of “long term effects of ( past) stone events.” My daughter, who has chronic kidney stones as a result of Crohn’s disease, has passed numerous stones as well as having lithotripsy and basket stone removal. Her ureters are particularly narrow and even small stones become stuck easily. Several of these procedures have caused pain off the charts for her especially after stents have been placed. Two years ago she began having chronic abdominal pain that seems to be located on both the left and right sides of her abdomen similar to where her ureters are. She has had every imaginable test of her digestive tract done because at first we assumed the pain was Crohn’s related but her Crohn’s is apparently under control with a double dose of Humira. Finally a month ago she was diagnosed with abdominal neuropathy by a pain specialist at the University if Southern California. Could this pain – which can be very severe and even interferes with her ability to eat – be caused by nerve damage related to the dozens of past stone events she has endured? She also continues to have stones in both kidneys and has several currently. But I guess my main question is if her neuropathy could have been caused by past stone activity and procedures that caused much inflammation and pain off the charts. Thanks, Mary Wuestefeld
Hi Mary, Abdominal neuropathy is a generic term but not particularly useful. Visceral organs have massive innervation and visceral neuropathies are not rare, the main cause being diabetes. Here is the best reference that came up in PubMed using the term abdominal neuropathy. It is all about diabetes. Possibly the stones are causing pain, a not uncommon problem as yet not well researched. I am not familiar with procedures causing pain apart from obvious stricture or damage to the ureters. Regards, Fred Coe
Thank you for your response. I guess I would like to know what you meant specifically by “the long term effects of past stone events” – what long term effects are you referring to?
Hi MAry, Every stone passage event has some element of obstruction, usually brief, but in some cases prolonged over days. Every surgery involves some element of infection, or transient obstruction – from stents etc, of modest trauma to the renal collecting system, of use of multiple and appropriate medications and anaesthetics etc. None of this is at all dangerous in most cases, but in aggregate amount to minor renal stresses that when ample can have less than ideal effects. In other words it is more than non stone formers encounter. Regards, Fred Coe
Hi – I recently asked a question on here – I am hoping it can be answered soon. Thanks!!
Hi Mary, I did answer, and my answer is on the site at the top of the posts for the ‘counting’ article. I wrote: “Hi Mary, Abdominal neuropathy is a generic term but not particularly useful. Visceral organs have massive innervation and visceral neuropathies are not rare, the main cause being diabetes. Here is the best reference that came up in PubMed using the term abdominal neuropathy. It is all about diabetes. Possibly the stones are causing pain, a not uncommon problem as yet not well researched. I am not familiar with procedures causing pain apart from obvious stricture or damage to the ureters. Regards, Fred Coe” The original posting is superior as it has all of the links that did not copy. Please take a look and see. Fred
So many things to comment on. I passed 12 stones during a 6 week period this past Sep/Oct with very little discomfort. Three were >10mm. My most recent KUB indicates 8 more stones (all 200 miles per week, am definitely not overweight, no alcohol or tobacco. My local urologist thinks I’m unusual because of passing large stones painlessly (my record is 12mm), but not unusual enough to create interest in the research community. I am tired of being a stonemaker.
Any thoughts?
Thank you.
Hi Paul, I gather you are making and passing multiple stones, and from that I would say prevention is your priority. One of these days a stone may not pass. This whole site is about prevention, and here is a good doorway into the problem. By all means get evaluated and treated so these stones stop. Regards, Fred Coe
Dr. Coe,
I have msk and frequently pass stones for 27 years. In the pass few years it has become increasingly debilitating. My urologist does not understand my frequent pain without an obstruction especially when I have a long episode passing many stones. I receive no help with my pain if there is no obstruction. I want my life back. I’m normally very active but when stones pass and then imaging shows no obstruction and then I pass more stones it’s frustrating and totally debilitates me. I’m at my wit’s end. This disease not only affects me physically but also mentally and spiritually. I don’t know what else to do anymore. I have seen urologist in California, Colorado, and South Carolina. I drink tons of water and do a low oxalate diet. I have tried potassium citrate and unfortunately it makes me very sick. I’m not sure what else I can do on my part. Counting stones is nearly impossible for me to do without my drs help. I just create to many stones. If you could advise me on what coarse of action I could do I would greatly appreciate it. Thank you
Hi Jennifer, Given you are actively making stones, the main issue is more targeted prevention. Have you had a proper evaluation? If so, do you know what is causing your many stones? If not, they will continue and that is not necessary. Stones in such numbers are almost always preventable. Regards, Fred Coe
Hi Dr. Coe,
Thank you so much for the time you dedicate to help all of us in this ‘kidney stone’ journey. Your work is very appreciated. I’ve recently undergone a lithotripsy for stones in both kidneys as well as had an obstructing stone removed. I see that you mention “low dose CT scans” and was wondering if these scans are standardly offered or if we must go to a specific imaging center that offers them. I had an abdominal CT scan prior to my surgery and my urologist has now requested one with contrast (triple phase). I am a bit nervous about this, as I worry about the radiation and also that the contrast is probably not very helpful to my kidneys (that may already be a bit frail after the lithotripsy).
Hi Carol, Ultra low dose scanners are now very common – it is really that modern instruments can be run in a low dose manner so CT can be used freely to track stones. One does not need contrast CT scanning unless your physician is worried about either kidney damage, obstruction, or some other abnormality. To could post operative stones one just needs the plain CT images. Regards, Fred Coe
Thank you for your response Dr. Coe. He ordered it after my ultrasound came back stating: “No overt bilateral hydronephrosis. Mild dilatation of the proximal left ureter remains persistent on postvoid imaging. Finding could be chronic and/or relate to recent lithotripsy/stent placement”. Do you think this warrants a CT scan with contrast? I’m just so nervous about all this radiation exposure. Thank you.
Hi Carol, I imagine your surgeon is concerned about the dilation and wants to be sure of what is there. From a distance and without seeing your images I would be unfair to offer any more specific answers. But I think I see the rationale, and above all your physician is probably trying to protect against any obstruction that could impair the kidney. Regards, Fred Coe
Hi Dr. Coe,
I am a chronic calcium phosphate stone former (apatite/brushite included). I have the typical alkaline urine and low urine citrate. dRTA has been ruled out as well as hyperparathyroidism. When I was in my early 20s my stones were primarily calcium oxalate. I understand the stone composition can change over time as it has in my case. I drink plenty of fluids but am aiming for 100oz/daily. I am trying to follow a low phosphorus diet and this, as you know, can be very difficult. Many foods have added phosphorus. Do you have any low phosphorus diet plans that may be effective? I’m wondering what the maximum daily intake should be for phosphorus as well. Lastly, are you currently involved in any studies using phosphate-binding medications in CaP formers? Thank you for any help, it is much appreciated.
Heather
Hi Heather, I cannot recommend low phosphate diet. If effective it will increase production of active vitamin D (1,25D) which will increase GI calcium absorption and also possibly promote bone mineral loss. I would avoid this approach and focus on lowering urine calcium with reduced diet sodium and a thiazide diuretic at a low dose. Regards, Fred Coe
Good afternoon. Three years ago I had 23 stones, Randall’s plaques and crystals. Passed 2, 4 removed clean out procedures. I take Allupurinol for high uric acid( calcium oxalate stones) and vitamin D for low D started at 21 now 42. No new stone attacks. I have a yearly KUB . The stones I have left are tiny and embedded. How often would you do a CT as plain films and ultrasound show none. Would a low dose CT say ever three years be resonable? I made sodium, water and less protein changes. I follow Jill. Thanks
Hi Karen, Sans symptoms, a CT every three or four years seems reasonable. The KUB is so insensitive I would avoid them. Often radiation approaches what a modern CT scanner provides – you can check with your radiology provider. Regards, Fred Coe
Hello Dr. Coe,
I form pure/100% calcium phosphate stones. Regarding the count, after reading my CT report that did not include a number of stones, I was told bey my urologist you have “a lot” . I asked him to please request the radiologist give us a number of stones. He told me “the number of stones doesn’t matter. Whether you have 15 or 50, is irrelevant.” I then reached out to the CT scan department requesting they revise the report to include number of stones, and also disclose their location (whether upper pole/lower pole, etc) and they said only a doctor can request the report be revised. The urologist refuses my request for reasons I don’t understand. He then said at an appointment, “you have too many to count- like 50” when I replied, “50? That is a lot” he replied, “it could be 30, it could be 50, it could be 20, again, WHY are you so focused on the number of stones?”
I am now quite simply confused. He thinks stone count is irrelevant if you have more than 5 stones. So I now hope to get your opinion. Is stone count only for people who have less than 5 stones?
I recently had surgery to hopefully cure the hyperparathyroidism that was causing the stones. Yet, the stones are still there because I’ve had no surgeries or procedures to remove, because I wanted the formation to stop first. In summary, my questions are:
1. Does stone count matter if you have more than 5 stones? (my doctor thinks I’m “too interested” in wanting a detailed CT report with stone count & location)
2. Which type of surgery or procedure do you think has less risk for injury/complication for stones made of 100% calcium phosphate (every stone I’ve passed has been 100% bone mineral /pure dahllite) which makes me wonder will these stones be harder to break up or navigate through during surgery. My goal is if possible an injury free surgery with no added complications, and considering my urologist seems to be not detail oriented, I worry will he even consider stone “type” when deciding which procedure is best for removal. Maybe this matters not, but that’s why I’m inquiring with you. Thank you for any help or thoughts. I appreciate.
Hi DB, Most importantly, having had parathyroid surgery, are you really free of stone risk? We have reported and I put on this site, that after cure of PHPT many people remain hypercalciuric. Are you sure your PHPT is cured? Is your blood calcium level normal?? If so to both, and you really did have PHPT, and produce calcium phosphate stones, and no longer have high risk of more stones (24 hour urine supersaturation with respect to calcium phosphate is <1) the question is what to do about residual and apparently significant stone burden. I have to agree with your physician in that once the stone count in a kidney exceeds 5 – 10 stones it is truly hard to get a good count – tedious indeed, and if there are 20 or more ‘stones’ in a kidney the calcifications are likely to me a mix of stones and tissue calcifications. Certainly ureteroscopy is best, to me who is not a surgeon – because he/she can sort out stones from tissue calcifications and give you the best chance at a stone free kidney. Usually I am slow about recommending surgery in the absence of pain, bleeding, infection, or obstruction as tiny stones may pass with little fuss and surgery has its risks. Regards, Fred Coe
My wife’s GP ordered a CT on 5/9/22 which found the below results.
“KIDNEYS/URETERS/BLADDER: 1.4 x 0.7 x 1.4 cm (AP, TRN, CC) calcification located at the junction of the le! renal pelvis and proximal le! ureter, previously in the mid to lower pole infundibulum. Four additional, small, nonobstructing calcifications in the le! renal collecting system. Single tiny nonobstructing calcification in the right renal lower pole collecting system. Unenhanced appearance of the kidneys within normal limits.”
Refered to Urologist who performed a procedure to remove the stone on 6/6/22 using a laser to breakup the stone and removed the larger pieces . Two weeks after the procedure to remove the stone a ultrasound was performed on 6/29/22 with the below findings.
“Renal cortical thickness: Preserved.
Renal cortical echogenicity: Preserved.
Hydronephrosis: None identified.
Renal calculi: 0.8 x 0.9 x 1.2 cm lower pole nonobstructive nephrolithiasis.”
Ambiguous feedback from surgeon and office. My novice reading of the literature is that when the stone is listed with 3 does it is to reflect the stones size. We were told that the 3 dims actually describe to cumulative area(volume) of a cluster of stones.
Can you provide clarification/guidance on this matter. How is a stone defined dimensionally and how is a cluster to stones defined dimensionally.
My wife pain is unchanged for her initial visit to the GP.
Hi Richard, I assume the new US is of the left kidney from which a large stone was removed. I presume these are either some of the prior stones or fragments from the removal efforts. The dimensions are the three available for a solid L x W x height but of course it is of irregular shape. If you multiply 0.9 x0.9×1.2 you get a volume of 0.86 cm^3, or very roughly 0.9 ml of volume if it were water. Clusters are interpreted, if at all as the sum of volumes, but one usually does not do this. She needs full evaluation and prevention. The stones need analyzing. Regards, Fred Coe
I had my first lithotripsy surgery in my twenties, (30 years ago). I’ve had four more progressive stone removal surgeries since then. Five surgeries in 30 years.
I had the basket surgery to remove stones in January 2020. Recovery time was two weeks due to infection.
Twenty months later I had a stone event that required a trip to the emergency department for IV meds to stop the pain and vomiting but no surgery required.
Seventeen months later, on Tuesday, Feb 1st, I was in the emergency department again for stones. One passed at home, two others passed the next day. I’m expecting more.
I have multiple stones in both kidneys. I also have one stone in my gallbladder, the size of a goose egg. 17 months ago I was told there were multiple stones in my gallbladder. How is it that I have one large stone now? Will this happen with my kidney stones?
I anticipate another stone event in 14-18 months.
At this point, every time I pass a small stone or two (twice a month now on average), I worry that the dam will break and many more stones will come out that require surgery. I can’t handle many more surgeries. I’m a 56 yo woman. BMI is 23.
I have such an understanding of my stones, I can tell exactly where they are and can guess their size within one mm.
I joked at the hospital, before the MRI scan, that I was expecting twins. Lo and behold! Two 4mm stones. If it had been just one, I could have endured it. I passed one at home before going to hospital. The pain from the two additional stones caused intractable pain, repeated vomiting over 4 hours.
I would describe the pain of kidney stones as your body constricting around a shard of glass. Every time the stone moves, it feels like a knife slicing or stabbing your ureter. Imagine handling a shard of glass, rubbing it for hours between your fingers; getting it stuck under a fingernail. The pain, the blood, the smell. Now visualize the delicate spot where that kidney stone leaves your body.
What happens when I have more stones than kidney? Is that possible? I’m tired of hearing they’ll get me “fixed up”. There is no fixing, only periods between medical intervention.
Hi Linda, You really need testing to determine the causes of all your stones, beginning with analysis as to what they are made of. I suggest this be done promptly and predict causes will be evident and treatable to prevent more. Regards, Fred Coe
Hi Dr Coe!
Thank you for sharing your knowledge and your wonderful website. I am a big fan!
I am a brushite stone former who has had 5 stone surgeries. My last was in 2018 – a 1cm stone in the left kidney. After this surgery, I “discovered” your site and began the kidney stone diet and advocated to my doctor to put me on 1/2 chlorthadone and 10 meq potassium chloride daily to manage stones given my high urine ph and high urine calcium post diet.
My doctor here manages stones through annual KUB scans. Although I did have a CT scan in 2022 due to a kidney stone scare. This showed a .2cm stone on right kidney and .3cm and .1cm stones in left kidney. This year 2023 the KUB showed no stones and the 2023 ultrasound report indicated multiple stones up to .4cm in the left and a .6cm stone in the right. Doctor said “You don’t have a kidney stone.” Believes the US to be only reliable for detecting hydronephrosis and if I had a stone it would have been corroborated by the KUB. He said any stone growth is insignificant to prompt a change in medication. He said I am doing good as it has been 5 years with no stones. My US report said I had “mild” hydronephrosis reported in 2022 and 2023 which he says is ok as it is consistent. In his after visit report, I noticed it says “no hydronephrosis” – which must mean mild isn’t anything noteworthy.
Question is this: KUBs expose one to radiation and also unable to detect small stones and possibly some larger ones. US can misclassify suspicious objects as stones about 50% of the time according to your site. My KUBs have all been stone free over the past 5 years but I had some findings on a 2022 CT scan (above) and on the 2023 ultrasound (above). In my opinion I don’t have strong evidence my prevention methods are working as I could have small stones, growing stones, bigger stones missed by KUB and/or maybe the US stones are indeed real as it is 50/50. This process does not seem proactive. Instead I feel like I am subjecting myself to annual radiation on the KUB (often 2 films at one appointment) waiting to to find a stone large enough to “maybe” detect on the KUB and then react. I would like instead to monitor growth in a reliable effective way and then tweak my medicine and diet to PREVENT a stone large enough to be detected on the KUB.
Trying to determine what an annual follow up should look like for a chronic stone former. Is it reasonable to expect a low dose CT scan annually until we figure out if the medicine/diet is working? Then after we determine it is working only have them every 3 years. That seems like a good idea to me but that is not the process here. Please let me know what a reasonable follow up method (kub,US,ct scan) and timeline is to aspire to monitor stones in a person like me that is not symptomatic. Also, should I advocate for a CT scan this year given my kub/us results or wait a year?
Thank you for your time and consideration!
Traci
Hi Traci, You embody and common and serious problem. CT is the gold standard and what it reported in 2022 is surely true. KUB is much less sensitive and US is as you mentioned. Given brushite stones are nasty and grow rapidly I would personally opt for ultra low dose CT every 2 years in place of KUB films. As for the hydro I cannot say as sometimes the urinary tract is a bit dilated because of its natural conformation. But if there is any question isotope renograms are very sensitive to even slight obstruction. Of course this is all abstract as I do not know your real medical situation, and your physicians do and are responsible. Regards, Fred Coe
Also I should mention I am going to Africa in January 2024 which is why I am a bit anxious about the .6cm stone possibility.
Hi Traci, perhaps a CT is in order before, although I cannot imagine why it would stop your traveling – except for undisclosed obstruction. Regards, Fred Coe