Thiazide Type Diuretics Reduce Stone Formation
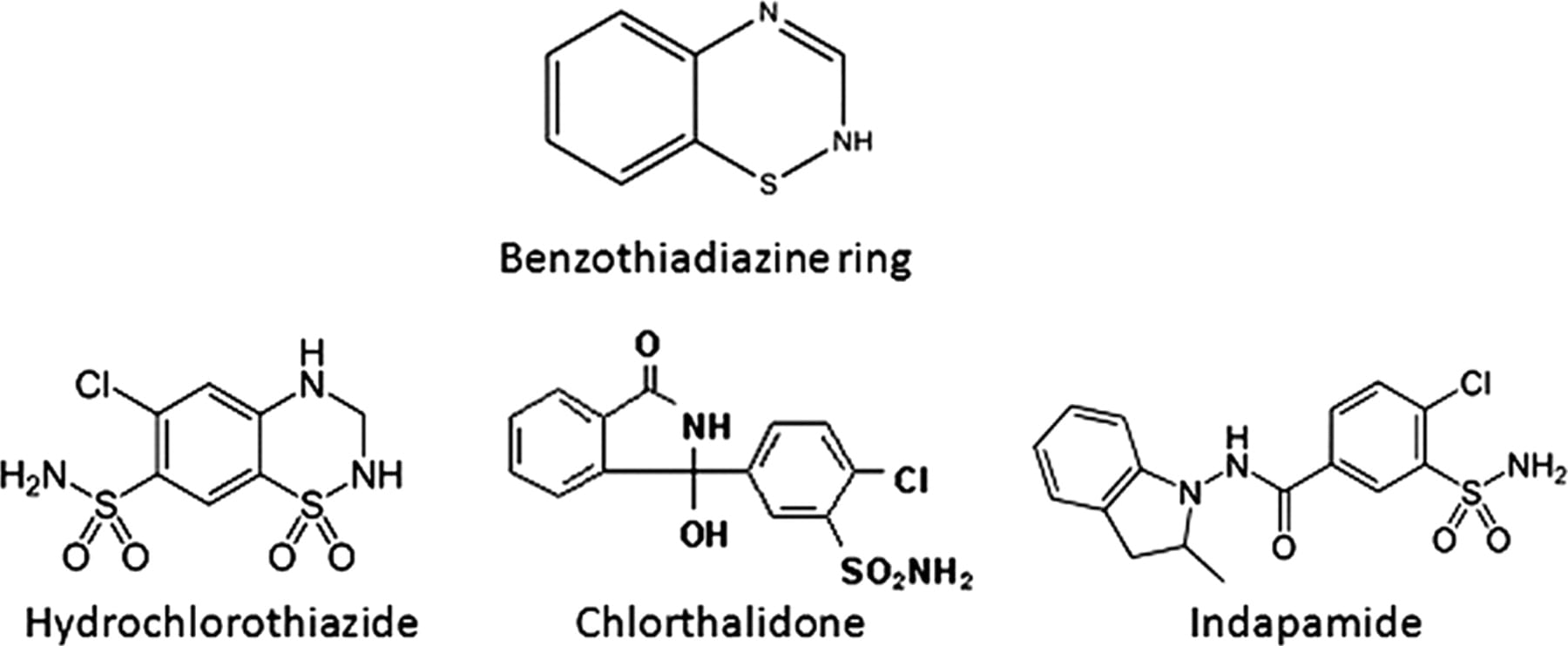
The common thiazide type drugs in use today are hydrochlorothiazide, chlorthalidone, and indapamide. All three have been used in stone prevention trials and shown to have beneficial effects. A nice recent review is also the source for the drug structures pictured above.
I have obtained and studied nine trials. In all nine trials, there was a comparison – untreated – group. This spreadsheet contains links to the trial documents, but you will find it not easy to obtain the original publications unless you have access to a university library system. For this reason I have copied out the key data. Briefly, there were 330 controls, of which 149 relapsed (45%), and 314 treated subjects of whom 72 relapsed (23%), a savings of about half (23%/45%). That is the bottom line for this class of drugs.
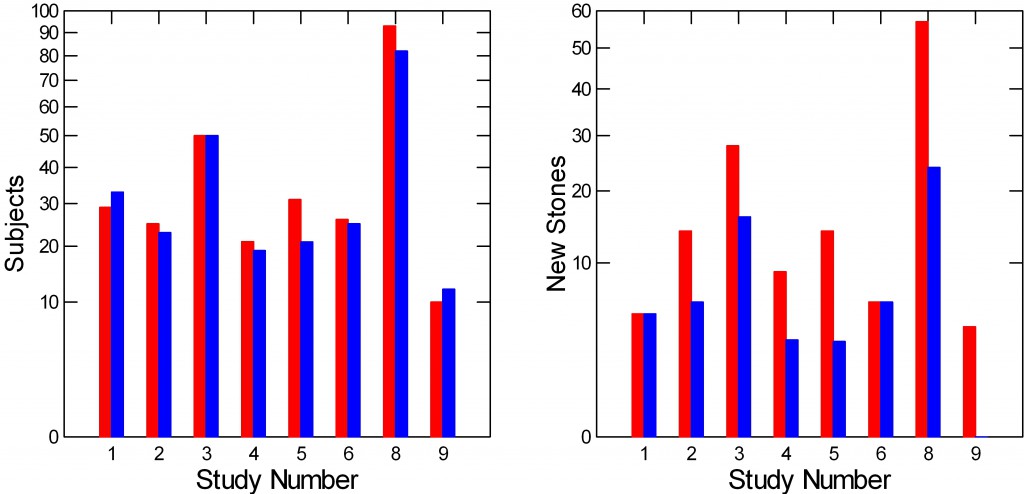
Here is a picture of the 9 studies. For each study the left panel has a bar whose height is how many control – red, and treated – blue subjects it had. The right panel shows how many of the red and blue people made new stones.
It is obvious that there were no differences in new stones between control and treated people (right panel) in studies 1 and 6. These were both brief (see the spreadsheet). In the others, the treated – blue bars – were lower than the red controls. Trial 9 had no relapses in the treated group. (Trial 5 has two drug doses and one control group so the height of the blue bar for 5 on the left panel is the average of the number of subjects in the two dose groups).
By now many of you will want some statistics. The spreadsheet depicts 9 studies each with numbers of treated and untreated people who did and did not relapse. Using ANOVA in which the numbers who relapsed is dependent, treatment or not is a categorical variable, and numbers of total subjects is a covariate, the mean number of relapse subjects adjusted for number of subjects was 16.1 in the control group and 8.3 in the treated group (p=0.008).
A simple X2 test using the four numbers from the bottom line of the spreadsheet: Treated, 72 relapse 242 no relapse; untreated 149 relapse, 181 no relapse gives a X2 of 35.2, p<0.001 (Yates’ correction is virtually identical for those who care).
I have deliberately included all studies that had a control and treatment group without fussing about the ‘quality’ of the trials. Several expert groups have reviewed these trials and a few more I omitted. Fink and colleagues in 2012 reviewed all available stone treatment trials. The same group did a similar review for the American College of Physicians which I did not think much of because of its codicils that seemed inclined to mediocrity – if not folly in practice. Escribano and colleagues authored an outstanding Cochrane review focused on thiazide.
The experts properly quibble about the intricacies of trial conduct and call for more trials. Personally I think more thiazide trials are of marginal importance and little interest. Mine is the untutored opinion of a bystander who does not perform trials as a profession. But I can count, and no one can tell me that the main fact – the pills reduce stone recurrence – will be overturned by trials of increasing ‘quality’. That is very unlikely. So, why do them?
Thiazide is Not Used Alone
Because they can reduce formation of new calcium stones, thiazide type diuretics are co-equal with potassium citrate as a medication physicians can use for stone prevention. Thiazide works differently from potassium citrate, so the two drugs can be used together with additive effects.
But more to the point, diet and lifestyle changes are crucial for stone prevention and need always put in place before writing a prescription.
The goal is to lower supersaturation. Fluids will do this. So will reduced diet oxalate, or raising urine citrate and, in uric acid stone disease, urine pH. Reduced sodium diet will lower urine calcium, and that will lower calcium salt supersaturations. So fluids and diet come first. Aspects of living that promote dehydration are serious obstacles to prevention, and to learn what they are in a given person and some to ways around them is an art of considerable passion and value.
Trials are all about the effect of a pill, and that is a virtue. But no doctor who practices stone prevention with a mere pill can achieves the joyous satisfaction of an accomplished clinician. So all I want or need from trials is to know the pill can reduce stones – presumably by reducing urine calcium, and thereby feel justified to add it into my instruments of practice, which I had done decades ago.
Why Use Diuretics?
It is Not to Raise Urine Volume
Because of the name one might think the drugs work by increasing urine volume, and therefore prevent stones the way water or other fluids might. That is not the case. Diuretics raise urine volume only transiently. Urine volume is set by how much extra water is available for urine loss. After a short while on any diuretic, the average day’s urine volume will be no different taking a thiazide than it would be not taking it.
They Lower Urine Calcium and Urine pH
How they do this is a matter for some detailed commentary, but let us begin by saying they do indeed. When physiologists comment on how this occurs the correct answer is that they lower the urine calcium by stimulating the kidney tubule cells to reclaim back into the blood a higher than usual fraction of the calcium that the kidneys filter out of the blood in the usual course of their functioning. How they lower urine pH is not well known.
But higher calcium reabsorption, though true, could not lower urine calcium for very long any more than reducing the radius of a bathtub drain can lower the flow of water out of the tub whose faucets are open. If you did that, narrow the drain of such a tub, the water would rise until the greater weight of the water column raised outflow back to match the inflow from the faucets or the tub simply overflowed onto the bathroom floor. The amount of calcium in the urine every day is exactly the amount entering the blood from diet and bone. So thiazides have to somehow alter that inflow – either reduce diet calcium absorption or promote calcium entry into bone. It is mainly the latter they do, so they are not without some potential to maintain bone health.
They Must Lower Calcium Salt Supersaturations on Average
This is an old theme on the site. Reduction of supersaturation will lower formation of stone crystals and eventually stones. Given a random variability of urine volumes, and of other key factors that control supersaturations for calcium oxalate and calcium phosphate – eg. excretions of oxalate, phosphate, citrate, and urine pH, a fall in urine calcium from a drug will inevitably lower supersaturations on average unless that drug systematically raises urine oxalate or phosphate excretions, lowers citrate excretion, or alters pH upwards – calcium phosphate. In fact, thiazides can lower urine citrate, probably in part because they deplete body potassium stores and lower the pH inside kidney cells, but that can be corrected by potassium repletion. Lower pH from thiazide will specifically reduce calcium phosphate supersaturation.
How do Thiazides Affect the Kidneys?
Calcium and Sodium
With a brief blush and downward gaze, I choose our own publication as perhaps not unreasonable as a source. Partly I am guilty of favoritism, partly we are the only group to have studied individual stone formers before and during thiazide treatment in a clinical research setting on a constant diet. We did do this, and the results, if perhaps not exactly arising from a multitude, are secure in their precision and in their depth of insights.
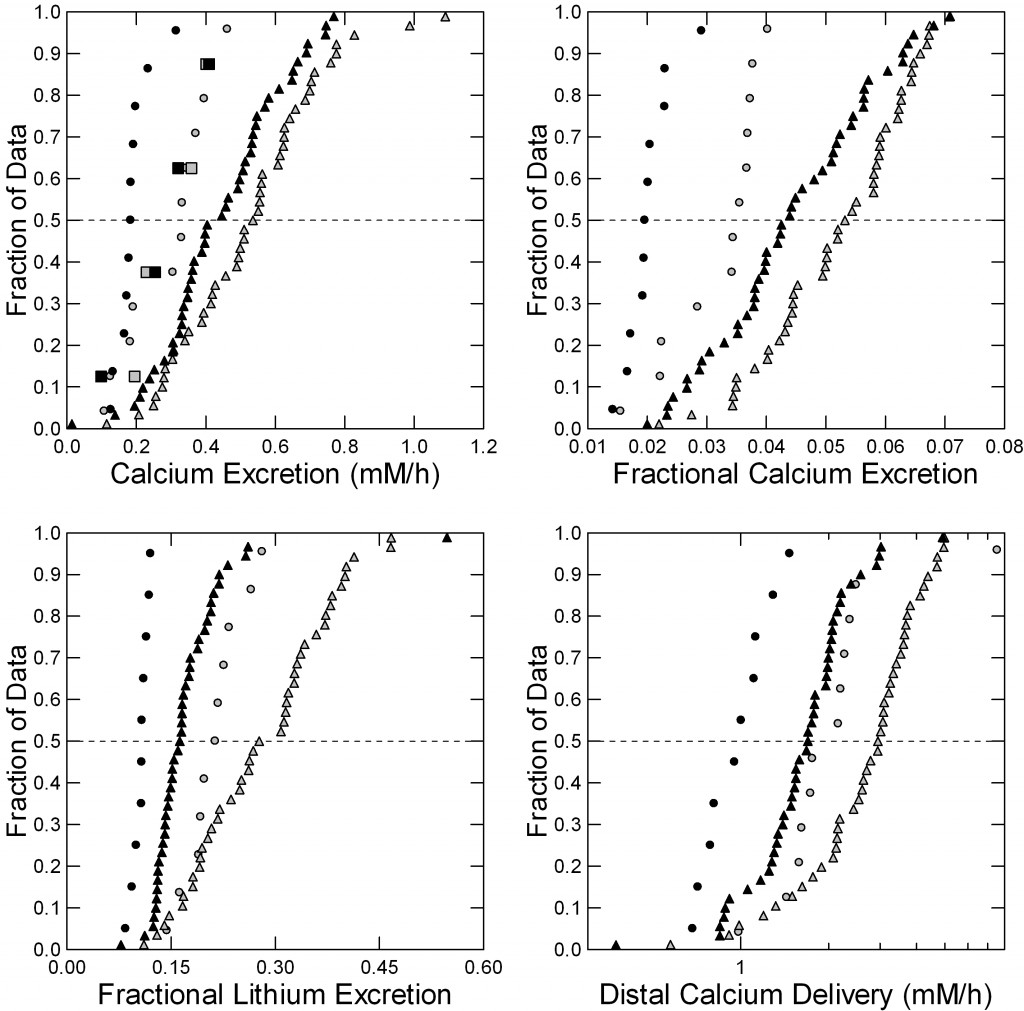 Four men with calcium stones and idiopathic hypercalciuria were studied in our CRC before (gray symbols) and after 6 months (black symbols) of chlorthalidone, 25 mg daily used in treatment for stone prevention.
Four men with calcium stones and idiopathic hypercalciuria were studied in our CRC before (gray symbols) and after 6 months (black symbols) of chlorthalidone, 25 mg daily used in treatment for stone prevention.
We have spoken of filtration and reabsorption elsewhere on this site. The drug had no effects on glomerular filtration, and therefore on the filtration of sodium and calcium. It lowered urine calcium – as expected – but did not change urine sodium excretion.
Fasting (circles) and fed (triangles) but not overnight (squares) the drug lowered urine calcium excretion (Figure to the left, upper left panel) shown here as millimoles/hour. The effect was statistically significant fed because of the large number of observations; fasting it was more marked but we had fewer measurements so formally speaking it was not significant. Overnight there was no change at all.
The fraction of the filtered calcium excreted (upper right panel) represents how the kidney tubule cells alter their reabsorption of filtered calcium – a highly regulated process. Both fasting and fed, that fraction fell markedly with chlorthalidone and both effects were statistically significant. Note that you can make these fractional excretions into percents – multiply by 100 (0.04 = 4%).
Lithium is everywhere, in our water and our food in minute concentrations. It has an odd property. Part of the kidney unit – the nephron -, that part closest to the glomeruli and therefore called the proximal tubule, handles lithium and sodium more or less equally, whereas the latter parts of the nephron do not handle them equally but let most lithium go by into the urine.
This tiny fact lets us sort out where along the nephron thiazides might have their main effects. Fasting and fed, chlorthalidone raised the fraction of filtered lithium reabsorbed in the proximal parts of the nephron so that less went forward into the later parts of the nephron (Lower left panel of the figure).
Here is a fact. Calcium and sodium and reabsorbed along the proximal nephron more or less in parallel. So by knowing the fraction of filtered lithium and therefore the fraction of filtered sodium sent forward, we also know the fraction of filtered calcium (lower right panel), That fraction falls with chlorthalidone. As a result, the early portions of the nephron conserve more calcium with the drug than without, and that is one part of why the urine calcium falls.
My article on idiopathic hypercalciuria is an excellent primer and overview of lithium clearances and proximal vs. distal nephron calcium handling.
Acidity of the Urine
Chlorthalidone, and presumably other thiazide type drugs make urine more acidic. Fasting (upper left panel of figure, circles) the effect is small: Chlorthalidone points (black circles) are just a little to the left – lower pH more acid – than without the drug. But overnight, the four black squares are far to the left meaning the urine is a lot more acidic with the drug. Fed (Upper middle panel) the same.
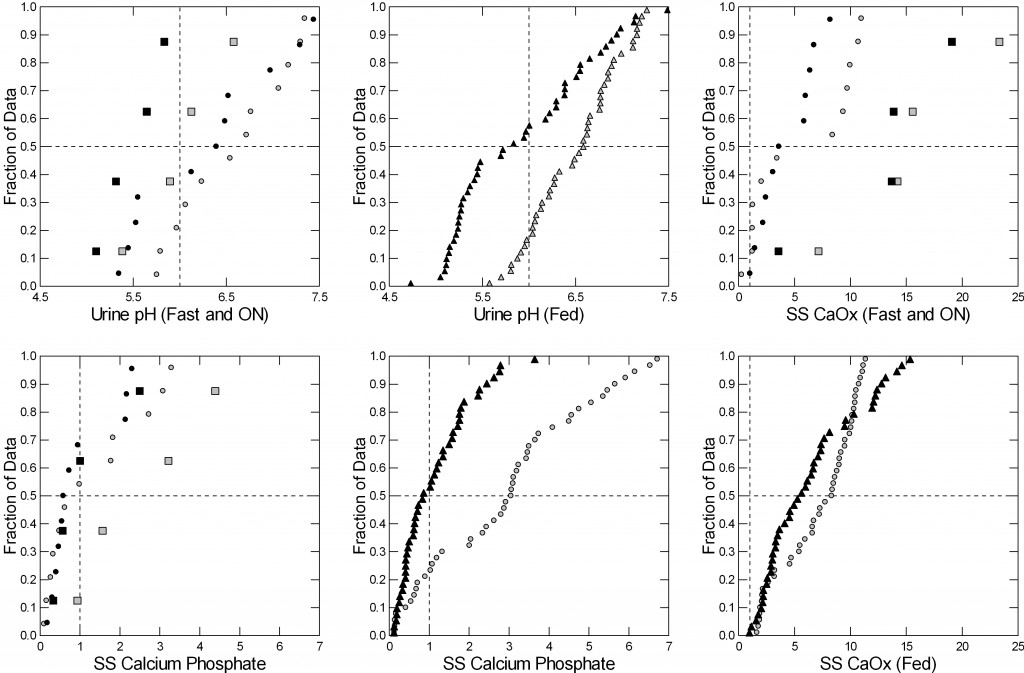 This matters a lot for supersaturation with respect to calcium phosphate, not so much for calcium oxalate. Therefore, although the calcium oxalate supersaturations with and without the drug are barely different (right upper and lower panels) those for calcium phosphate are much lower with the drug (lower left – fasting and overnight and lower middle panel – fed).
This matters a lot for supersaturation with respect to calcium phosphate, not so much for calcium oxalate. Therefore, although the calcium oxalate supersaturations with and without the drug are barely different (right upper and lower panels) those for calcium phosphate are much lower with the drug (lower left – fasting and overnight and lower middle panel – fed).
This makes thiazide type drugs ideal for preventing calcium phosphate type stones and calcium oxalate stones. They can prevent the former because they lower calcium phosphate supersaturation via both reduction of urine calcium excretion and urine pH. Calcium phosphate stones form on plugs of calcium phosphate in kidney tubules or perhaps just in the urine itself, driven by supersaturation.
Calcium oxalate stones are more complex. They form on the surfaces of the renal papillae over deposits of calcium phosphate in the kidney tissue (plaque). A crucial initial step in this process involves the laying down a film of calcium phosphate over plaque. Calcium oxalate then deposits from urine on top of this initial film to make the stone. So thiazide acts in two ways to reduce calcium oxalate stones: by lowering calcium phosphate supersaturation and therefore hampering formation of the calcium phosphate film needed for overgrowth of calcium oxalate on plaque, and by reducing calcium oxalate supersaturation itself.
Note that the nine trials concerned calcium stones, and did not always distinguish between those that did and those that did not contain appreciable percentages of calcium phosphate.
I have not discussed here how thiazide lowers urine pH. That would take us too far afield. The original article points to changes in intestinal uptake of alkali, which seems to be reduced by the drug.
Urine Oxalate
In our paper reviewed above we found no changes in urine oxalate with chlorthalidone, and did not therefore include oxalate data in the tables. In the past we have published a rather large group of patients who were put on thiazide and exhibited no increase whatever in urine oxalate. I do not believe it is likely that thiazide treatment raises urine oxalate.
How Do Thiazides Lower Urine Calcium?
I have said it is not just by acting on the kidneys, for that is to close down the drain – the bathtub will overflow perhaps but you cannot reduce the flow out of the drain for long that way. This is a sometimes overlooked point when people speak about urine calcium losses.
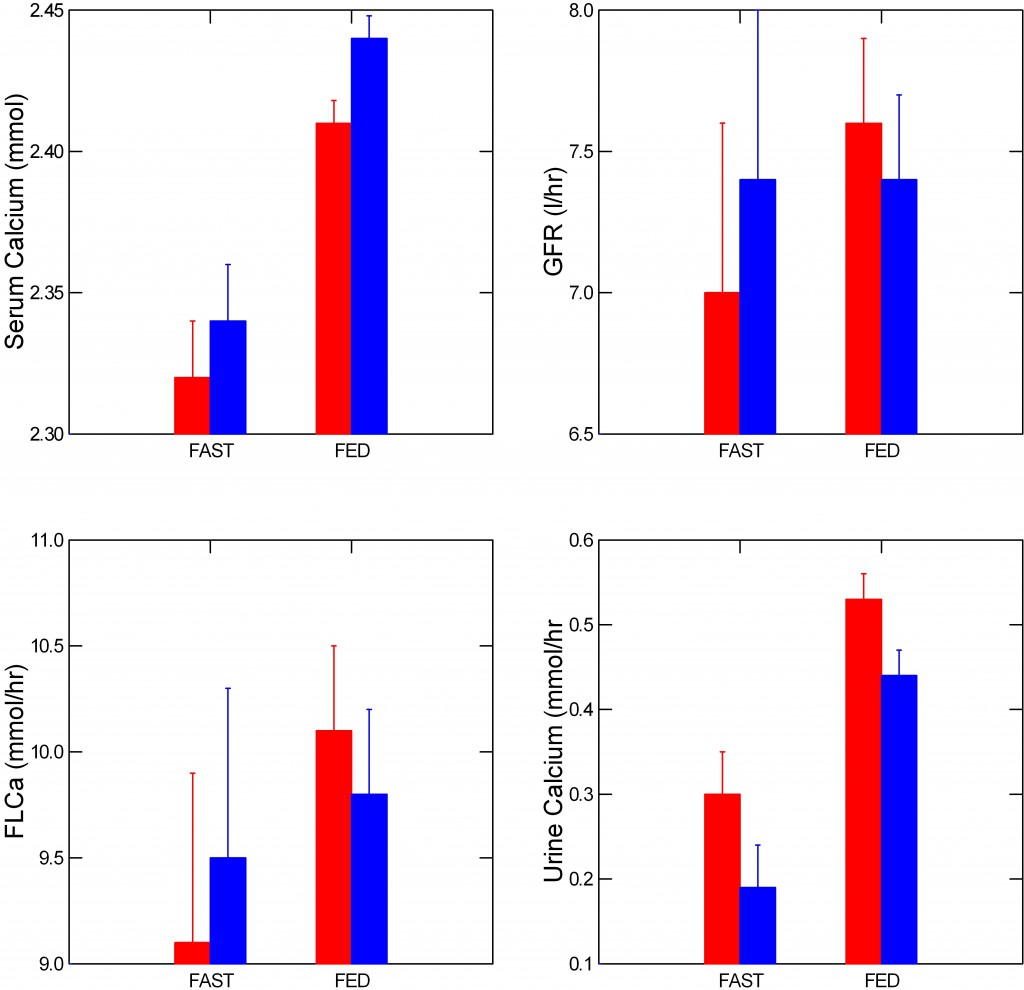 What happened in our patients must have been a fall in absorption of calcium from food, or an increased uptake of calcium into bone, because multiple measurements of serum calcium – the water in the bathtub – were almost unchanged despite a fall in urine calcium.
What happened in our patients must have been a fall in absorption of calcium from food, or an increased uptake of calcium into bone, because multiple measurements of serum calcium – the water in the bathtub – were almost unchanged despite a fall in urine calcium.
But almost is not quite unchanged.
Serum calcium – the upper left panel of the figure, rose significantly with thiazide. The amount of calcium filtered from blood into the kidney tubules (lower left panel) did not change significantly – the error bars overlap -, because filtration itself – (upper right panel) also varied. As I already showed you, urine calcium fell (lower right panel).
So the picture does have in it a bit of the bathtub with a somewhat closed drain – the water level, serum calcium, rose.
Now, I am about to leap into conjecture: Possibly, this increase in serum calcium could promote near instantaneous movement of calcium into bone by sheer physical chemistry.
A body of work that is perhaps more obscure than it should be, edges toward the idea that a portion of bone mineral, brushite in fact, may be in physical chemical equilibrium with blood so that large amounts of calcium can move in and out of bone mineral without any necessary cellular control.
This latter is critical, because bone cell process hours to change in response to hormones whereas urine calcium, as an example, can rise within a few minutes and yet serum calcium remain unchanged or even rise slightly as seen here.
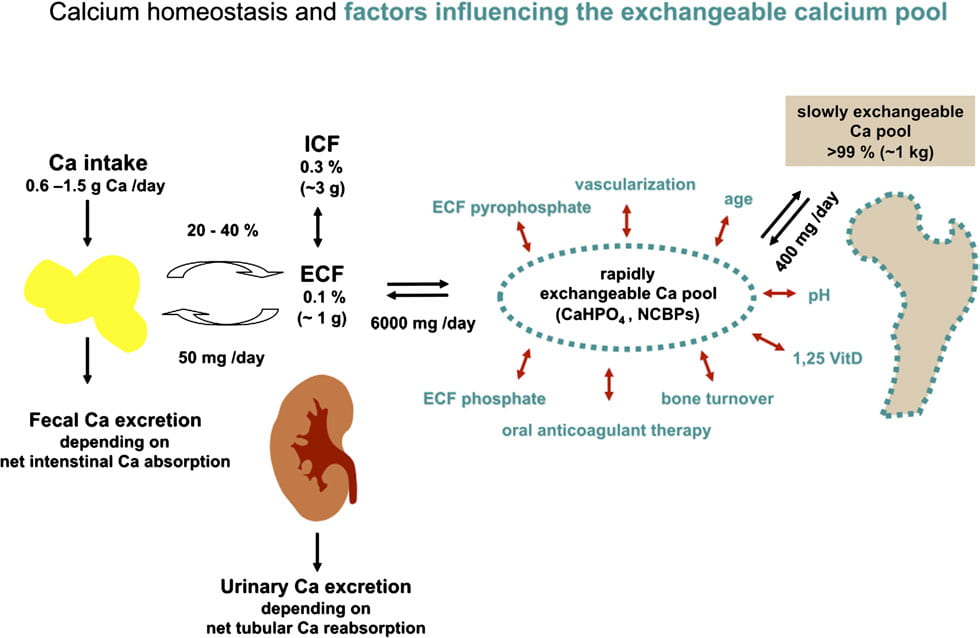
This colorful picture (shown below) is similar to much of what we have often discussed on this site. To the left is diet calcium coming in and leaving, the absorbed calcium entering the ECF or extracellular fluid – we have approximated this as blood. Kidneys can release calcium, as noted.
The big addition is that a large amount of calcium may well be circulating between blood and bone – the 6,000 mg in the middle of the picture. This exchange is affected by serum phosphate, drugs like anticoagulants that alter bone mineral modifiers, and other factors. Of the 6,000 mg of calcium that enter and leave bone every day, only 400 mg go into the slowly exchangeable bone pool which is our familiar hydroxyapatite – the majority of calcium phosphate stones and the principle stiffener of bone.
 What if, when kidney conservation falls – the drain opens – calcium leaves the exchangeable pool so the ‘faucet’ opens. What if, when thiazides raise conservation, the slight rise of serum calcium – from diet inflow perhaps – is just enough to nudge calcium flow into bone?
What if, when kidney conservation falls – the drain opens – calcium leaves the exchangeable pool so the ‘faucet’ opens. What if, when thiazides raise conservation, the slight rise of serum calcium – from diet inflow perhaps – is just enough to nudge calcium flow into bone?
In other words, envision that bathtub. As we eat, the drain opens, the diet ‘tap’ opens, and bone comes into a kind of balancing act: If diet inflow is large enough calcium flows into the exchangeable bone mineral – brushite – pool. If not, calcium flows out. Thiazide clearly tightens the drain, the diet is the same with and without the drug, so possibly diet calcium inflow is raising blood calcium a bit and calcium is moving into bone.
If I were young I would test this idea in humans.
Effect of Thiazide on Bone Mineral Balance
All this raises an obvious question: Do thiazides improve bone health, reduce fractures, increase bone mineral content?
A recent review summarizes a large amount of evidence that they do indeed reduce fractures. The data, from the Danish population, suggest that duration of continuous treatment is more important than dosage in fracture prevention. In particular, fracture risk appeared to increase during the first year of use but then fall progressively. A Cochrane analysis concludes that all evidence to date – 2011 – supported this idea of reduced fractures, albeit there were no prospective controlled trials. Several such trials subsequently confirmed that thiazides maintain or increase bone mineral. Dalbeth and colleagues describe a link between rise of uric acid and bone mineral with thiazide implying a possible causal linkage not otherwise tested.
The overall impression is that one would not win by betting against thiazide as helpful to bone.
By now you might be asking if stone formers are at risk for bone disease. A recent long term followup of nurse and physician cohorts showed an increased risk of wrist but not hip fractures. Our article on idiopathic hypercalciuria summarizes additional information linking it and stone disease to fractures.
How About Salt?
As their prime purpose diuretics cause renal sodium wasting so that for any given intake of sodium the total body sodium stores will be less than without the drug. This is perhaps a main reason why they can reduce urine calcium via increase of proximal tubule calcium retention and also reduce blood pressure.
From this, one might think that low sodium diet might be like thiazide and help with bone mineral balance. In the one really ideal study testing this idea it was correct, and I have summarized that work in another article on this site.
Clinically, reduced salt intake is critical for successful thiazide use. From its basic physiology, high sodium intake will essentially undo the effect of the drug, and raise urine calcium. More, thiazides cause losses of potassium and lower serum potassium, and this is worsened by high salt intakes.
A caution. Thiazides can lower serum sodium levels, especially in older people, and this site advises reduced sodium intake which could increase that risk. In general diagnosis of low serum sodium was made 19 days after initiation of treatment (95% CI 8, 31 days). For this reason physicians invariably monitor serum electrolytes after a few weeks of treatment, and should do so after a few months, and at reasonable intervals, as well.
Is One Drug Better Than Another?
I think so. For example, hydrochlorothiazide has been used 2 times a day in the stone trials, whereas indapamide and chlorthalidone are long acting and needed once a day. People can forget the second dose. It is said that hydrochlorothiazide causes less of a fall in serum potassium but at least in hypertension trials it is less potent so you need more and when more is used it is the same as the other two drugs with respect to potassium, and dosed twice daily.
Dosage
I like to start with lower doses than used in the trials. For chlorthalidone, 12.5 mg (1/2 of a standard 25 mg pill) is enough for most people. For hydrochlorothiazide I like the 12.5 mg pill twice a day – short acting. For indapamide I like 1.25 mg pills. Chlorthalidone and indapamide are long acting so the pill is once a day.
What Have We Learned?
Thiazide drugs can reduce stone recurrence at least in part by reducing urine calcium loss and supersaturation. They act on the kidney but also seem to improve bone mineral balance and reduce fractures. While stone prevention is certainly not accomplished by one pill, thiazide is an important part of what physicians can offer for prevention of stones.


Hi Dr Coe!
I have been reading all your articles and have made progress decreasing my urine calcium by reducing my sodium intake which was initially 130. However, I hit a roadblock. When I achieved urine sodium at 100 and I brought it down to 43 I was not able to get further improvement in urine calcium (see 24 hour litholink data below). My calcium intake was similar during both tests so that couldn’t have affected it and my urine volume is approx 3 liters in all tests. My creatinine really declined too but not sure if it means anything. Do you have any thoughts or ideas? I was stunned my urine calcium didn’t decline further with my sharp drop in sodium intake and a bit disappointed. Unless you have any other ideas it appears 12.5mg chlorthalidone is on my horizon – but please be aware that I am keeping my low sodium diet as this lifestyle is more healthier, I have never felt healthier and have no desire to change back. If you concur with chlorthalidone, should I ask to try to be on the 12.5mg with no potassium and see if my body can handle it or would there be any harm in asking to supplement with at least one potassium citrate to boost my citrate or or even one potassium chloride just so I don’t have to worry about my potassium plummeting if I have a diet splurge now and then? Don’t want to over-medicate but I am a bit anxious about my potassium skydiving and if there is no harm in a little boost it may just make me feel safer. Do most patients need supplemental potassium when only on 12.5 chlortalidone?
Ca Ox Cit SSCaP PH Na UUN Cr Cr24/kg
4/6/20 324 29 440 1.94 6.815 43 9.11 1134 20.5
4/5/20 306 27 372 1.78 6.775 43 8.6 1138 20.6
10/24/19 332 26 448 1.8 7.146 114 9.6 1338 24.6
10/23/19 303 27 516 1.78 7.055 100 9.02 1302 23.9
(By the way I excluded data prior to 10/19 that shows significant improvement with the kidney stone diet in urine calcium and oxalate so please if anyone else is reading this please know that the kidney stone diet really does work – I think there are just limits to how far an improvement different people can achieve.)
Thanks so much for your thoughts! Any advice appreciated. Take care and stay healthy, Dr Coe!
Traci
Hi Traci, I am impressed that your urine calcium shows no dependence at all on urine sodium. Are you sure your blood calcium level is entirely normal (less than 10 mg/dl?). Is it also true that your serum PTH is not suppressed? Urine calcium is remarkably unyielding. CTD 12.5 mg is a good start, but I might suggest even less – 1/2 pill every other day. Given the 23 hour 1/2 life of the medication that is 6.25 mg. Let me know. Regards, Fred Coe
Thanks for responding! My blood calcium was 9.3 on March 8, 2020 and looks like it is steady when I look a prior labs. My serum PTH was 60 on January 17 and I made sure I fasted beforehand. I don’t think I messed up my 24 hour urine test as I was really careful to do everything right so this result is baffling me! Anyway, why do you suggest perhaps 12.5mg every other day (6.25 daily) as opposed to 12.5mg every day? Would I still get a great enough drop in urine calcium? I know a 12.5mg daily dose may yield a 100 mg reduction of urine calcium but what would I expect an every other day dose (6.25 a day)?
Hi Traci, I answered another version of this but am happy to do it again. The starting dose of a diuretic depends a lot on diet sodium. Your urine sodium was low so I think a very low dose may be enough. You will find out through retesting. Too much with low diet sodium can lower blood pressure and cause symptoms. As I mentioned your physician is fully in charge here, so whatever she/he decides is what matters. Regards, Fred Coe
Thanks for responding! My appointment is coming up this week. May I ask why you suggest 1/2 pill every other day? I was thinking I needed a reduction of 100mg urine calcium and the 12.5mg daily would reduce it that much. Are you saying 1/2 pill every other day would give a similar drop in urine calcium and may get me to the desired 200mg urine calcium per day? Sorry to bother you but I just want to understand – this can be so complicated with all the moving parts.
Thanks for your help!
Traci
Hi Traci, With low diet sodium thiazides often have great effects, and I mentioned a very low starting dose for that reason. Of course your physician is in charge here, and she/he may have their own opinion. One can always retest and alter dosage. Regards, Fred Coe
Thanks Dr Coe, Is the 1/2 life of chlorthalidone 23 hours? I was thinking I read somewhere it was like 48 hours but maybe I am confused. Also, can a person just take break the pills in 1/4s and take 1/4 daily rather than 1/2 every other day?
Hi traci, it is 23 hours for 1/2 of the dose to be lost. So at 48 hours one would have – roughly! – 1/2 x 1/2 or about 25% left. The pills are small and fragment, so 1/2 is the least size workable. I believe a pediatric low dose once existed. But to take 1/2 every other day is very little. Regards, Fred Coe
I was put on chlorthalidone a few weeks ago and my doctor asked me to do a 24 hour urine at 6 weeks being on the medicine. Is that timing good to get an accurate test?
Hi Alissa, Yes it is. Fred
I am a fresh gradate medical student from Egypt , your articles are really helpful ,every patient i meet i search for opinion and your studies about am just want to inform you that million around the world get better rbeacause of you ore great prof
Dear Dr Roshdy, You are very kind to say this. Warm regards, Fred
I have Calcium Oxalate kidney stones, I was growing them about 1″ in diameter in about four years, after my second operation my doctor put me on Hydrochlorothiaz (25mg) , for four years I did not have any kidney stones, after my last 2 year check up my x-ray showed I have two stones about 4.7 mm dia. I maybe miss one day a month of medicine. But take them religiously. I also take a potassium pill. It seems lately after urinating my toilet bowl has a oil film on the top. Also if I do not flush my toilet after every time of use, the build up of a brown film on the sides of the bowl grows and after a week or so, I have to use a butter knife to chip it off.
1. Can you explain why my stones came back??
2. Can I increase the amount of Hydrochlothiaz to elimate the stones?
3. My friend in Colorado says I should try Furosemide.
4. I saw a medicine on Amazon called stone breaker, I am sorry I am desperate, will this work to beak up my stones.
PLesae….help…………….thank you………..
Please I am sick of these things, any help would be appriciated
Hi Kevin, Most important, after your surgery 4 years ago, did your surgeon do a CT to see if you were stone free. You found the new stones on a new image but perhaps they are not new but simply were there before. If new, what do your 24 hour urines say? Is your treatment reversing the abnormalities that caused your stones in the first place? Furosemide is not acceptable or useful. The stone breaker is not a proven remedy. A higher dose is not helpful. You need to know if the stones came back or were there, and what your evaluation showed as a cause and if your present treatment has reversed that cause. Fred Coe
Hi Dr Coe! I spoke to my nephrologist and asked him if I could take 1/2 pill every other day. He agreed although he told me he did not think it would have any impact. After 8 weeks I retested and I think my results are wonderful. My urine calcium declined to 220; SScaP .95; SS CaOx 2.95; citrate 359; ph 6.6; sodium 39; PCR 1.5; K24 55. My blood results are normal but sodium slightly low at 134 mmol/L and potassium was good at 5 mol/L. My blood pressure is normal and my heart rate is on the lower side – sometimes 58 at complete rest – maybe has always been low I don’t really know. This doctor only would allow me a one day 24 hour urine litholink as he thought results would be the same on a one day vs a two day test so I chose to take the test on the “off” day when I did not take the 1/2 chlorthalidone for conservatism. Out of curiosity, I am wondering generally how much lower you believe my urine calcium would have been had I taken the test on a day I actually took the 1/2 pill (since my doctor does not have any experience with patients taking only 1/2 pill every other day while on a low sodium diet) . Nevertheless, I am planning on just continuing my 1/2 pill every other day. It would be nice to somehow increase my citrate but not sure how. I certainly value your thoughts and welcome them if you have any other recommendations. Please know I am a huge supporter of your kidney stone diet and I admire, appreciate and marvel at your generosity and time dedicated to educating millions of people across the world on the impact of diet on kidney stone prevention.
FYI Meant to respond to my string dated April 17, 2020 below. Earlier conversation located there for your reference.
FYI Meant to respond to my string dated April 17, 2020 below. Earlier conversation located there for your reference.
Hi Traci, the very low urine sodium is remarkable and no doubt contributed to the fall in urine calcium. The fall in serum sodium is not ideal and perhaps you might not need the chlorthalidone at all. If you stop it, with your physician’s approval, please retest after 6 weeks to be sure the calcium is alright, and the serum sodium, too. Alternatively, you might liberalize the diet sodium just a bit. I imagine your nephrologist noticed the 134 serum sodium and also lifted up an eyelid. Regards, Fred Coe
Hi Dr Coe, I had kidney stones and at the same time my kidney function was decreasing so I went to see nephrologist who suggesting that I take hydrochlorothiazide because he said, the drug can help to prevent kidney stone.
FYI, not only do I have high uric acid (and 2-3 episodes of gout in the past), but also, I passed all of the stones and it was sent to the lab and the result, it was mostly made from uric acid.
That said, my understanding based on your explanation, Thiazide only effective for calcium-containing stones, if so, do you think Thiazide would do any good for me? Should I keep taking the drug? Currently taking 50mg per day.
Hi Nick, I am afraid your nephrologist might have missed the emphasis from the stone analysis. Indeed uric acid stones arise from low urine pH and are cured by raising pH. Often they occur in the context of reduced renal function and gout.So thiazide is beside the point. The two articles tell the whole story. Regards, Fred Coe
Hi Dr Coe,
When I had my first episode of uric acid stone 10 years ago, the urologist at that time told me to do 24 hour urine measurement. There was no discussion about urine pH and I managed to normalize my uric acid by dieting alone at that time. Since then I had no uric acid stone until it came back 5 years ago at which time dieting alone didn’t help to normalize my uric acid level and I started to take allopurinol at 300mg daily. The nephrologist that I have seen 5 years ago didn’t order 24 hour urine measurement.
That said, assuming my urine pH is above 6 (which was maybe why the urologist didn’t mention anything about it), then Potassium Citrate is of no use for me, correct? If so, even though you said: “Sometimes I use a low dose of thiazide diuretic along with potassium citrate” would thiazide also of no use for me?
Hi Dr. Coe,
Not sure if you read my previous reply but you have yet responding to it. So, I now understand that raising urine pH is important and I have took 24 urine collection in the past through 2 different specialist. None of them making any comment about my urine pH. My questions:
1. Assuming my urine pH is normal (which was why the 2 specialist didn’t say anything about it), what should I do?
2. Assuming my urine pH is low, I’m assuming taking a low dose of thiazide diuretic along with potassium citrate is the answer but taking thiazide alone (like what my specialist was prescribing to me) won’t helps as it’s not raising the pH. Is my understanding correct?
Thanks!
Hi Nick, I went on the site and found your comment and my reply from July:
“July 15, 2020 (Edit)
Hi Dr Coe, I had kidney stones and at the same time my kidney function was decreasing so I went to see nephrologist who suggesting that I take hydrochlorothiazide because he said, the drug can help to prevent kidney stone.
FYI, not only do I have high uric acid (and 2-3 episodes of gout in the past), but also, I passed all of the stones and it was sent to the lab and the result, it was mostly made from uric acid.
That said, my understanding based on your explanation, Thiazide only effective for calcium-containing stones, if so, do you think Thiazide would do any good for me? Should I keep taking the drug? Currently taking 50mg per day.
Reply
Fredric L Coe, MD
July 23, 2020 (Edit)
Hi Nick, I am afraid your nephrologist might have missed the emphasis from the stone analysis. Indeed uric acid stones arise from low urine pH and are cured by raising pH. Often they occur in the context of reduced renal function and gout.So thiazide is beside the point. The two articles tell the whole story. Regards, Fred Coe”
Given uric acid stones, urine pH was low and thiazide is not an appropriate treatment. I would suggest you look at your lab results and see if the urine pH is below 5.5, and also check if your stones are really uric acid. If so for both I would discuss the use of potassium citrate for uric acid stone prevention. Of course I am not your physician, so these remarks are simply to bring to the attention of your physicians who are responsible for your care. Regards, Fred Coe
Hi Dr Coe,
First of all, my stone is uric acid stone and based on my blood test which was conducted 1.5 months ago, my urine pH was 5.0.
Second of all, I had discussion today with specialist about potassium citrate and the specialist is against it due to the following reasonings:
1. We can’t objectively measuring urine pH because it keeps changing in seconds due to the many various elements affecting the pH. That said, even if I’m taking potassium citrate, we won’t know how much is the true urine pH level
2. Potassium citrate is expensive (I’m in Canada, is it cheap in the US?)
3. Potassium citrate can affect kidney
4. The ultimate key to prevent uric acid stone is by maintaining the uric acid into normal level which is what allopurinol is supposed to be doing and therefore, knowing I don’t have any stone in the past 5 years while taking hydrochlorothiazide and allopurinol (and unless the situation is changing), potassium citrate really has no use (or overkill at best) to prevent uric acid stone in my particular case
The specialist suggested to keep continuing my current regimen with hydrochlorothiazide and allopurinol. The specialist also said that one of the function of hydrochlorothiazide is to prevent uric acid stone but he believe hydrochlorothiazide is optional and less important than allopurinol.
Any chance you can comment or confirm if what this specialist is saying is true?
Hi Nick, Here are my two articles on uric acid stones. This one is a general review, this one more detailed. I am afraid that what you are saying is not true. Urine pH may indeed vary rapidly but crystallization is integrative and so stone crystals tend to follow average pH values such as we measure in 24 hour urine samples. As for objectively measuring urine pH, glass electrodes have done this for about a century, and its regulation spans thousands of scientific papers – essentially the urine buffer system is very strong so pH is very easy to measure and stable over long time, especially when on the low side. No one has any data pointing to kidney damage from potassium citrate. No one with a reasonable scientific background would state that crystallization of uric acid crystals depends more on total 24 hour urine urate excretion than on urine pH – it is not chemically correct. Thiazide diuretics have no effect on uric acid crystallization. I rarely respond so directly, but you may read the two article which are referenced out to PubMed and make up your own mind. You are free to show my note to your physicians, and I am perfectly willing to respond. Regards, Fred Coe
Hi Dr Coe,
I met with another doctor, a family doctor, who seems willing to listen to me. This doctor said, after her meeting with me, she did research about potassium citrate and I would like to confirm with you some of the thing that this doctor said to me.
There are 2 points that this doctor made:
1. Potassium citrate has serious side effect + I’m stone free in the past 5 years, therefore the risk outweighs benefit.
2. Potassium citrate is not a common treatment in Canada.
My questions:
1. Is it true that potassium citrate has serious side effect and to monitor the side effect, according to this doctor, I have to do ECG, blood test for renal function, plus something else that I don’t remember right now, every 4 months.
2. I currently lives in Canada, but I was diagnosed with high uric acid and uric acid stone in 2010 and met with a urologist while I was living in Boston. The urologist didn’t pay attention to my urine pH much less prescribing potassium citrate at that time. Is potassium citrate a common treatment in the US?
Hi Nick, Potassium citrate to raise urine pH for prevention of uric acid stones is basic medicine. Uric acid crystallization depends on urine pH – the science is over 100 years old by now. I do not know what happened in Boston. The articles I have on uric acid stones go over the pH matter – the main research group is Dallas, and they would be as surprised as I am by your physician. I believe failure to raise urine pH to treat uric acid stones would possibly be inadequate practice by a urologist or nephrologist here in the US – at best it would be marginal behavior. Take another look at the two articles on uric acid stones: clinical, research. Now, that said, perhaps you have reduced kidney function of a magnitude that makes potassium itself, the atom, dangerous – that is a common problem in older people, especially. For them we use sodium alkali. The lack of chloride prevents worsening blood pressure. As for potassium citrate having malign effects apart from potassium as noted, there is no evidence. Regards, Fred Coe
Hi Dr. Coe.
I am at my wits end, After starting on Dithiazide 12.5mg 10/12 ago I thought I finally had an answer/treatment. Unfortunately I had another attack 2 weeks ago and was able to get my 12 month followup moved forward. Ultrasound yesterday showed many large stones, previously calcium oxolate. some up to 8mm. I just wanted some advise before I see my Urologist next week. I have had many lithotrypsy/ureteroscopy/laser in the past and I wish there was something else I could do. Thanks for any advise Regards Julia
Hi Julia, First, is this a new stone or passing an old one – complex arithmetic you and your physician need to do. Second, do you have high urine calcium as the cause of your stones and have you done all you can with diet to lower it before using thiazide? Given many stones medical prevention needs to be orderly and as complete as possible. Regards, Fred Coe
I am a 59 yo female currently under treatment (at your clinic) with genetic hypercalcemia as a participating factor of multiple 4-8 mm sized oxalate kidney stones (and some uric acid as well) — have had 6 pass naturally and 5 removed surgically a year ago that were lodged in a ureter. I saw this article and use your references but had a question. I have been on Losarten w hydrochlorthiazide 100/25mg daily for prevention and has been looking good. However, i have had some significant leg swelling and sob due to weight gain and a run of high sugars and my cardiologist has suggested an additional dose of Lasix of 20 mg every other day. I seem to have better reaction cardia wise from Lasix vs. hydrochlorthiazide but was concerned we would lose the thiazide benefit if we switched to Lasix all together. Would I be ok removing the hydrochlorthiazide and just using Lasix since stronger or does that risk stones coming back? I hesitate to just take more hydrochorthiazide because of past issues with it. Does Lasix do anything for stone prevention at all? I don’t want to reduce liquid intake which helps take the load off the heart when it was recommended to increase that for the kidneys – seems like they sort of work against each other to cut the edema and the high blood pressures and sugar. Thank you.
Hi Darice, As you are a patient at University of Chicago Stone Clinic, we need to review matters directly and see to the issues you raise. Please call our clinical coordinator Banita Williams 773 702 1475 and let her know you need to talk with one of us about all this. Addition of lasix to hydrochlorothiazide in a stone former is a complex matter and whichever of us is your physician – I do not remember if I am indeed one of them – needs to be personally involved. Please call Banita today. Regards, Fred Coe
Hi Dr. Coe,
A question about chloride…
I started taking 25 mg Chlorthalidone 5 years ago. Oddly, both blood and 24-hr urine test levels of chloride have been consistently down ever since. I don’t seem to be able to tolerate enough KCl liquid to bring them back up, so we’re going to try 12.5 mg.
(Note, it seem like a big change: Blood Cl dropped from 99 to an average of ~94 with CHD.
Urine Cl 24 dropped from 203 to an average of ~133.
Also, urine pH 24 actually increased from ~6.8 to ~7.3, and there is some metabolic alkalosis too. We’re trying to balance so many different factors.)
Would you please try to shed some light on what ranges for Blood Cl and Urine Cl 24 levels are good and bad for (1) bone health, and (2) stone prevention, and why?
Many thanks,
Al
Hi Al, by reducing extra cellular volume and producing mild cell potassium losses thiazide type drugs cause metabolic alkalosis so serum total CO2 rises and chloride falls. The result is a fall in chloride filtration and urine chloride and ultimately a rise in urine pH. You are an observant person. Thiazide rather benefits bone and is a proven benefit for stone reduction. Best, Fred Coe
Thank you very much, Dr. Coe.
To clarify, are you implying that blood chloride levels somewhat below the normal range (e.g. 90-94 mmol/L) are expected with Chlorthalidone, and not generally considered harmful for general health, bone health, or stone risk in otherwise healthy individuals?
Kind regards, Al
Yes, Fred
Hi Dr. Coe,
I am a 39 yo male who produced CaOx stones. I believe my stones are under control (no new stones for at least a couple years). I have been on a thiazide for about 4 years. I have only learned how to follow a proper diet over the last 2 years, following your site and Jill Harris. I would like to potentially get off of my thiazide and just stick to my new diet, if I can do so safely. Of course, I don’t want the only feedback to be a stone event. So, I was hoping to taper off the thiazide and see how much my SS CaOx increases. Even on (lower dose) thiazide, low sodium, and low sugar diet my Ca 24 is in the 3-400 range, but SS CaOx is below 4.0. How do I know I have enough margin of safety to safely come off the thiazide? Is there a magic SS CaOx number to stay below, or is it just much more complicated?
Also, do you agree that a higher calcium number is not concerning so long as I can keep my SS CaOx down with hydration, oxalate reduction, and proper oxalate + calcium timing? My hypothesis is that my thiazide is not really helping my SS CaOx levels as much, now that I have cleaned up the rest of my dietary habits. So, I was hoping that SS CaOx should be my prime / sole focus.
Thanks for all you do!
-Tad
Hi Ted, Thiazide lowers urine calcium by about 100 mg/d below that predicted by urine sodium. All of the stone vs. risk data are using multivariable analysis to isolate individual effects, so strictly speaking urine calcium, oxalate, citrate, and volume and SS can be considered independent. But in terms of crystallization SS is the one single measure of free energy available for solid phase transformation and I favor it. Apart from one trial by Borghi we have no diet trials sans thiazide, although that one was positive. So I have to say stopping the drug is neither unreasonable nor fully supported by trial data – it is a matter of weighing one thing against another and you are judge and jury. If you asked me technically I would have to say success is better left alone, but that is mere chatter from the sidelines. Your physicians have a stake in the game, and I would be sure to seek their opinions. Regards, Fred Coe
Dr Coe,
1) In this article it states Thiazides lower urine PH. Am I misinterpreting your response to “Al” on Sept 18 that says:
Hi Al, by reducing extra cellular volume and producing mild cell potassium losses thiazide type drugs cause metabolic alkalosis so serum total CO2 rises and chloride falls. The result is a fall in chloride filtration and urine chloride and ultimately a rise in urine pH. You say a rise in urine PH??
2) Since Thiazide can lower sodium levels in some does that happen frequently or in someone 51 years old? If a person keeps their diet sodium between 1000-1500 with no problem doing so is that an issue if they are ever put on Thiazide?
3) Do lowest dose of Thiazides raise blood calcium and if so does the drug have to be stopped or is that the new norm for someone on them?
4) Can very low dose Thiazide be used alone for Ca Phosphate Stone Former if they always maintain low diet sodium of 1000-1500 because the potassium citrate would cause a rise in urine PH for this type of stone former?
I’ve learned so much from your site and piecing all the parts together for prevention and I thank you.
Hi Lisa, Potassium depletion from thiazide can raise urine pH, but the drug absent potassium depletion lowers urine pH. So when we want to lower urine pH thiazide is a reasonable possibility and KCl the potassium replacement of choice, not potassium citrate. Thiazide will lower body sodium stores unless diet sodium rises – any age. Blood calcium can rise from thiazide, not clinically important so far as I know. Thiazide is reasonable for CaP stones, especially with low diet sodium, and potassium chloride, not citrate, as replacement. Regards, Fred Coe
Hi there,
Just started following your articles and am finally feeling like I have some solid information. Recently saw an endocrinologist for the first time as I have been diagnosed with fairly severe osteoporosis. All of my blood work and 24 hour urine were normal except the calcium in my urine at 286. My vitamin D was slightly low at 26. I also have several kidney stones in my left kidney. At any rate, the doctor was only interested in getting me on bone meds immediately, either forteo or actonel which I’m not crazy about but will probably try. My next trip is to the urologist as my endo didn’t seem interested/knowledgeable about the stones. My question is: would it be safe and effective to take actonel along with the Thiazide and potassium citrate? Thank you!
Hi Marjorie, Genetic hypercalciuria causes stones and can cause loss of bone mineral, too. Actonel, a bisphonate goes well with a low sodium high calcium diet, which is good for bones. Thiazide, if diet is not adequate, helps preserve bone mineral. Potassium citrate, if otherwise desirable, is an alkali load and those help bone mineral maintainance. So, to your question: Yes. Regards, Fred Coe
Hello Dr. Coe,
I have learned the most about my idiopathic hypercalciuria by browsing this website. It has been a great resource! Thank you to you and your colleagues for putting it together.
I am curious what treatment, if any, is advisable for someone who has both idiopathic hypercalciuria and low blood pressure? My blood pressure is typically around 100/60. My parents also have low blood pressure. It has never posed a challenge until now.
I have been unable to take either chlorthalidone or hydrochlorothiazide because of its impact on my blood pressure. I even tried 6.25 mg of chlorthalidone once a day. Both drugs lowered my urine calcium to around 300 mg/24 hours, but I felt lethargic most of the time and sometimes experienced lightheadedness.
Earlier this year, I tried the higher calcium/lower sodium diet from the post-menopausal women study. I consumed 1,200 mg of diet calcium and limited my diet sodium to 1,600 mg. I did this for a couple weeks. It brought my urine calcium down to 325 mg/24 hours. But I experienced the same symptoms of when I was on the low dose chlorthalidone or hydrochlorothiazide. At times my blood pressure was 95/50. So I ended up increasing my diet sodium to 2,000 mg and diet calcium to 1,400 mg. As expected, I felt better and my urine calcium went up to 425 mg/24 hours. I was just retested last week. The low 400s seems to be my baseline.
Until today, I did not know Indapamide was an option so I may try that but I am not confident I will be able to tolerate it. The only other treatment I can think of is keeping my diet calcium at 1,200 mg – 1,400 mg, limiting my diet sodium to 1,200 – 1,500 mg, and taking a medication to raise my blood pressure. While this would be unorthodox, I am confident this limited amount of diet sodium would get my urine calcium to under 300 mg/24 hours. Still not ideal but in my situation, perfection (200 mg/24 hours) is the enemy of good.
The stakes are quite high because even though I am only in my 30s, my bone loss is severe. Depending on the area scanned by the DEXA, my z-scores from last summer were from -2.4 to -3.3.
Best,
Matt
Hi Matt, Is your serum PTH, by chance, below normal? Is your serum calcium borderline high? Is your serum 1,25D high? Obviously you have a genetic variant of IH, with early bone disease, and perhaps bone directed medication – even a simple bisphosphonate – might lower urine calcium remarkably and possibly stabilize your bones. I think you warrant deeper study than is usual, and perhaps more unusual treatment. Regards, Fred Coe
Hi Dr. Coe,
Thanks for the reply. I went back through my medical records from May 2018. This is when I was diagnosed with IH before beginning any treatment. Below are the results. Aside from the vitamin D, everything else was within normal. I have had normal but borderline high calcium serum results a couple of times, but its been 3-5 years. I have also had these tests repeated at least once a year and everything has come back normal (I started taking vitamin D3).
vit D 25.9
PTH 26
calcium serum, 9.6
Ionized calcium 4.82
The only reason I was diagnosed with IH is because while at the podiatrist, I had x-rays on my feet. He came back and told me the bones were extremely thin and that I should have a DEXA right away.
I also found the results from my first 24 calcium urine: 502. At the time, I suspect I was consuming no more than 500 mg of calcium per day (either through diet or supplements).
Thanks to following the principals laid out on this website, I am now consuming 1,400 mg calcium per day and yet my urine calcium is usually 75-100 mg lower. I of course do not have to tell you, but I think its all because I am very careful with my sodium consumption. It’s my hope over the long run this will build back my bone or at the very least stop the bone loss.
As mentioned in my original post, my most recent 24 urine calcium was 425. What I did not mention is my 24 hour sodium was 94. Based on the chart on https://kidneystones.uchicago.edu/three-essentials-to-reduce-calcium-stones-and-preserve-bone/, my urine calcium should be well under 300. But I think my situation is unusual.
I am going to give the number a call on https://kidneystones.uchicago.edu/about/ and see if I can get a virtual appointment with a member of the medical team sometime this summer. I am also going to be seeing nephrologist at Indiana University Health for input soon. Hopefully, I will be able to develop an effective treatment plan.
Thanks for the suggestion of the bisphosphonate. I will pass that along to the endocrinologist who is currently treating me.
Best,
Matt
Hi Matt, At IUPUI Dr James Lingeman is a famous stone surgeon – but you do not speak of stones. As for virtual appointment, I do them and the number will get you to my secretary. Regards, Fred Coe
Dear Dr.Coe
My son has osteoporosis due to Idiopathic Hypercalciuria.
He is taking 1400 mg calcium per day, HCTZ 25 mg, Vitamin D and no bisphosphonate.
Bones have been improved a little within last 15 months but still his 24 hours calcium is high (385 mg).
Shall he change HCTZ to Chlorthalidone?
Thanks in advance
Hi Dr Sharifi, His urine calcium is indeed high – is his urine sodium perhaps very high? How old is he? If very young I would be concerned about a genetic cause. Can you tell me the calcium/gm creatinine as an index?? Regards, Fred
Hi Dr. Coe,
I’m am a 39 y/o male with idiopathic hypercalciuria. I have tried different thiazides and indapamide seems to lower my calcium the best (per urine testing). However, lately I have been having some side effects of muscle spasms, weakness, and numbness tingling – mostly in my hands but other places as well. My metabolic panel came back with all normal results, though. I’m worried this might be something neurological causing this. I have an appointment to see a neurologist, but it isn’t for a while unfortunately. So, I was hoping you could clarify if the side effects can still happen with normal blood work? I will most likely go off the thiazide temporarily, or try going back on HCTZ.
Thanks for all you do!
-Tad
Hi Tad, This drug is not known to cause neurological disease but can cause spasms and numbness as you describe at higher doses. The lowest dose (below 2 mg) is not known to cause these and perhaps will be enough. Regards, Fred Coe
Thank you Dr. Coe. Would these symptoms still potentially exist with a normal blood workup, though? Or would they only exist if my electrolyte balance was off?
Hi Tad, Indapamide is said to cause some of these symptoms and there is no mention of a linkage to blood chemistry measurements. I presume you might want to use the drug at the lowest dosage. I should mention that low sodium intake – below 1500 mg/d – can lower urine calcium and permit use of lower doses of drug. Regards, Fred Coe
Hi there,
My son has Dent disease and is currently being treated with ramipril (2.5mg), hydrochlorothiazide (6.25mg) and potassium citrate (40meQ per day). His last three ultrasounds (May, June and August this year) all detected renal calculi but it is unknown whether they are calcium oxalate or calcium phosphate stones. The largest ones measure approximately 0.2 cm. I was hoping you could weigh in on his treatment plan. Recently he was sick with a cough so we withheld giving him the thiazide for a day and a half as he wasn’t up to drinking as much as he usually does and I noticed his urine PH was higher when he didn’t take the thiazide (which is what we were trying to achieve with the citrate). Any thoughts would be appreciated!
Hi Drina, Dent disease is really complex, so I presume his treatment is at a major academic center. Here is a link to a government site. It was updates in 2016. I should not comment on treatment complexities in this kind of complex condition but do note that thiazide can lower urine pH If desired I could try to help via telehealth (Banita Williams, 773 702 1475) but Mayo Clinic has a rare disease program and should be an ideal source. Regards, Fred Coe
Dr Coe, I am 72 and have a long history of Calcium Ox stones. Ureteroscopy in
2009 and 2017. In 2017 I was informed that ultrasound was incorrect and instead
of multiple stones that randalls placque was present and fewer stones were found.
Based on your website I got my first thyroid test in 2018 and it resulted in parathyroid surgery. I hoped this would finally stop stone growth as my calcium levels
improved from 10.2 to 9.4 Many litholinks and ultrasounds later, today, my ultrasound shows some small stones and 13mm left kidney and 9mm stones in right side.
Last October they showed 7 and 5mm. My only diet change was psylium wafers-2 daily and
12 oz of oat milk. Also, I use polyglycol powder several times thruout the month-GI issues
I follow a low sodium and oxalate diet and have for some years now with discipline.My family
Doc says psyllium and glycol piowder is equivalent to eating spinach and likely responsible
for this doubling stone growth. I am unable to find any data to substantiate this and am a bit
incredulous.
I would like to be a patient and have your input on what may be happening. My GI history
and Fathers medical past may be helpful . How do I proceed. I live in Pa and hope that you
see patients virtually ongoing. Also, very willing to meet initially if required.
Thanks, John
Hi John, You have indeed a complex history. I do telehealth – Sect. Banita Williams 773 702 1475; bwilliams15@bsd.uchicago.edu. She can arrange a visit. Please bring together all of your prior documents, including stone analyses, 24 hour urine testing and the operative report for your parathyroid surgery. Regards, Fred Coe
Hi Dr. Coe
My urine calcium has remained stubborn in low 300’s despite my rigorous following of the kidney stone diet (Thanks you Jill Harris). I am on cholorthaidone 25mg, 2000 IU Vitamin D daily and 3 KCL tabs per day. Is it worth trying Indapaminde? My PTH is normal, Vitamin D level is 28. all other indices are good on my litholink testing. why is my urine calcium so stubborn?
Hi Barb, I believe I answered this on your first comment. Fred
Dr Coe, I’m 58 y.o and have been having calcium stone problems for the last 2 years. The first culprit was my vitamin D was deficient, which had my PHT and my blood calcium off. I went to an endocrinologist and was given a vitamin prescription for a while and have been taking 4,000 IU per day since. No stones for about 15 months. Then I started getting stones. 8-9 in 6 weeks. I did a Litholink, PTH, blood calcium and vitamin D test. All tests other than the Litholink tests were normal. The Litholink test showed my calcium was 702…yes 702. My citrate was 1497, oxalates 18.5, sodium 120, urine 24 hour output 3 liters. I had been taking Potassium Citrate twice a day. My new urologist ( I moved) prescribed 25mg of Chlorthalidone and quit the potassium citrate. He says this will fix my issue. I’m concerned with my calcium number being so high, it won’t fix it. Is there something else I should be doing? Thank You!
Hi Joe, I presume your blood calcium was normal – below 10 – on multiple occasions. Likewise that your serum PTH is not pathologically low – below 15 or so. You are right, that urine calcium is very high. Are you very large, perhaps. Are you an early diabetic? Is your serum vitamin D level above 50? Your urine citrate is very high, which gives one ideas that more is wrong than the calcium. Repeat the test to be sure it is not misleading. Regards, Fred Coe
Dr Coe, In your response here to Joe you asked if his serum vitamin D level was about 50, does that cause high urine calcium if vitamin D is above a certain level in the blood?
Hi GF, Actually no, unless the levels are clearly above normal to s significant extent. Regards, Fred Coe
Thank You Dr Coe! My blood calcium level was 9.8 in November and below 10 last year after the vitamin D was corrected. The PHT was 57 in November. My vitamin D was 75 in October and I continue to take vitamin D every day. I am around 6’1″ and normally weigh in the upper 180’s. My blood sugar is usually at the top of normal or a little high. There is a history of obesity and diabetes in my family so I try to keep my weight in check. I exercise vigorously about 3.5 hours each week. I’ll have my blood calcium checked again after the new year and let you know the results. Happy Holidays!
Hi Dr. Coe,
I’m a 55 year old female, I follow the kidney stone diet. My sodium intake is around 1500mg daily. I drink approximately 4 liters of water daily and get 1200mg of calcium. I was put on Chlorthalidone 25mg and KCL 40meq daily about 2 years ago. Ever since then, my urine calcium has continued to increase (from 250 to current level of 470). My PTH is normal. I have not made any new stones, but my bone disease continues to get worse. Why would the Chlorthalidone increase my urine calcium instead of decreasing it? Should I even stay on it especially since it’s causing my glucose and cholesterol to increase.
Thanks,
JoAnn
Hi JoAnn, Thiazide does not increase urine calcium, so there must be more to the story. Possibly your bone disease has been accelerating and causes the high urine calcium, and if so that is a separate problem. If it is the cause you would want to be taking a bone directed drug – bisphosphonate is a common choice. WIthout more detail I am afraid I cannot add much more. Regards, Fred Coe
Hi Dr. Coe,
I am 41 years old calcium phosphate stone former from northern Scandinavia with 20 years history of having kidney stones.
I got my first Hydrochlorothiazide medication in July 2022 with daily dose of 50mg Hydrochlorothiazide + 5mg Amilorid (Diuramin 5mg/50mg)
I got persistent rash to both hands in March 2024 and
in April 2024 I was diagnosed with superficial facial melanoma which was removed in a surgery (I have never had any chronic skin issues before 2024 in my life)
I don’t tan and I have been using SPF 50 when in sun to avoid sun burns.
Are some of the diuretics more skin friendly than Hydrochlorothiazide?
Should my daily dose be adjusted after recent symptoms?
Hi Tommy, thiazide type agents can cause photosensitivity and also skin issues unrelated to sunlight. I imagine your physicians will want to stop the thiazide and see if the problem goes away. Best, Fred Coe
Hi Dr Coe,
Could you guve me your thoughts on taking Hydroxy Citrate for calcium oxalate stones. Thank you
Hi Chris, a theoretically great idea, available OTC, but no trial. What more can I say?? Fred
Hello Dr. Coe, What are your thoughts on using a thiazide diuretic in pts with unknown stone type who refuse 24 hour urine collections.
Dr. Coe: I would like your opinion on the recent clinical trial published March 2nd in the new England Journal of Medicine that reported no benefit on kidney stone prevention from HCTZ in doses ranging from 12.5 to 50 mg/day. How do you explain these results that contradict previous studies?
Hi Dr Feldman, Of no significance. There is already too much thiazide trial data for this one to change practice. This one used a short acting drug none of us in the business rely on, and I suspect it was their main problem. As well stone counting was complex. I plan a serious review of the trial perhaps as my next article. So take this as my best right now. Regards, Fred
Dr. Coe,
Do you have any thoughts on vitamin k2 for its reputed effects on bone health and its possible relevance to the calcium metabolism of stone formers?
Thank you so much.
Richard
Hi Richard, A PubMed search ‘vitamin K AND kidney stones’ restricted to humans, turned up 16 articles. As rule the paradigm was that vitamin K dependent proteins containing gamma carboxy glutamic acid (GLA) inhibit crystallization so low vitamin K increases and high vitamin K decreases stones. The best clinical test of this idea was essentially negative but now enough to falsify the entire idea. No data support supplemental vitamin K as a prevention (a trial, for example). Good question, good idea, unproved. Regards, Fred Coe
For someone that has low to normal blood pressure but needs to lower calcium in urine, like myself, would hydrochlorothiazide be a better choice.
Hi Lori, Low sodium diet is always a best first stop – try for 1500 mg/d. It may be enough. As for the short acting OHCTZ it is not my favorite choice. One can use very low doses of chlorthalidone – for example 12.5 mg every other day – and get reduced urine calcium reliably. Regards, Fred Coe
I offer my experience as merely one case history regarding the use of HCTZ to stem kidney stones. Thirty yrs ago, followiung my third painful bout with stones, my PCP suggested there had been studies showing HCTZ at 12.5 mg/day might reduce or eliminate stone formation (and lower blood pressure). I’ve been taking it religiously ever since and have had no reoccurrence of stones. I don’t drink as much liquid as I “should.” And I have no idea whether that plays into my outcome but I am a faithful user of HCTZ
Hi Joel, it is not that OHCTZ does not help prevent stones, it is that is is relatively weak in that regard as noted in the trial. I am happy for your excellent outcome. Best, Fred
Hi Dr. Coe,
Are you familiar with K-Phos (a.k.a. potassium acid phosphate) as a way to lower urine PH? Would K-Phos offer any advantages or disadvantages compared to potassium chloride?
Thank you,
Richard
Hi Dick, Very complex issue. KCl is used when potassium depletion has led to increased urine ammonia excretion and increased urine pH. It is the specific treatment and KPHOS would be wrong. Now in some patients urine pH is higher than one would like for reasons not at present known. The value of KPHOS is not known. On the one hand urine pH might fall due to the acid load, But urine calcium might rise for the same reason. So no one knows if it is a good idea. Regards, Fred Coe
Hi Dr.Coe,
Have been following your research for 5 yrs! Thank you for all you do. I’ve been diagnosed with neophrocalcinosis & osteopenia 5 yrs. Tried all dietary means as per your research including 3L water/day; 24hr calcium remains stubborn at 300mg/day, and 24 r phosphate >24.7mmol/day (lab range 8.1-22.6), even with low sodium diet (24h sodium 117 (lab range 55-220mmol/day) and 24 hr urine citrate level around 480mg/day. Vit D level 30+. PTH, serum calcium normal. Oxalate 24 urine 166 (lab range 40-340umol/day).
Last year, doctor prescribed 1.25mg/day Idapamide and 24/urine calcium fell to 168mg/day for the first time! However, without potassium citrate supplement, serum K fell too low at 2.9mmol/L (lab range 3.6-5). 30 meQ potassium citrate/day was added. However, 9 months into it, I started producing calcium phosphate stones (passed 1-2) and the doctor decided to stop thiazide and potassium citrate due to high urine PH (8) and he does not know what the next option is. Would you be able to give us some clues on what to try? Potassium options that don’t affect PH? Would a Bisphosphonate be a good option for idiopathic hypercalciuria? What type would be preferable if that’s the case? Looking forward to your thoughts!
Hi Connie, Indeed your urine calcium seemed to fall nicely with indapamide and only the potassium is holding things back. Possibly the high alkali load and high pH led to phosphate in your recent stones. I would replete potassium using potassium chloride, not citrate, and adding back the indapamide with KCl. The lower you keep your diet sodium, the lower the dose of indapamide needed and the less potassium loss. A sodium of 117 is not low, it is just a bit above the US upper limit of recommended (100). A better goal is 60 mEq or less which is not ‘low’ just lower than our present society favors. Of course I am writing to your physicians who may choose to ignore me as being utterly uninformed about your overall health issues and therefore at best a chatbox, at worst a trouble maker. Regards, Fred Coe
Hi Dr.Coe! Thank you! Would you suggest a lower indapamide dosage than my previous 1.25mg/day? Have you observed lower dosage work on some patients, assuming they take a low-sodium diet? I would love to try KCL as a potassium add-back alternative, assuming that would not have an effect on urine pH? Much appreciated for your sharing as always.
Hi Connie, I would indeed. Sorry to be so late! Fred
Thank you for your previous thoughts. We’re still managing nephrocalcinosis due to hypercalciuria with calcium phosphate stones whilst on 1.25mg indapamide (KCl add-back 40 mEq). Despite a lower-sodium diet (24hr sodium 75 mmol/day), 24hr urine calcium rebounded to 240 mg/day (same calcium intake), with elevated 24hr phosphate at 844 mg/day, 24hr citrate at 360 mg/day, and urine pH ~6.8-7, 3L water intake a day. Blood serum levels (all mid-range of normal), including PTH, are normal. Our physician is at a loss for further steps after years of attempts. We’d greatly appreciate your insights on potential next steps to consider. Much appreciated as always.
Hi Connie, Your physicians might consider increasing the indapamide dose and adding amiloride 5 mg to avoid the inevitable potassium losses. That is a mere guess as I do not know all the details of your situation. Best, Fred Coe
Dr Coe; I am a 72 year old male with history of calcium/oxylate stones. I’ve been taking HCTZ 25mg for a couple years now. Also have restricted dietary sodium to 1,200 mg or less and drink 2.5 liter of fluid per day. I have low body mass (150 lbs) The last two annual 24 hour collections have shown no supersaturations and no new stones from CT scans. Recently however, blood tests for a different condition found low sodium levels (133). Previous serum sodium levels were within the normal range. This was a period from Feb. 2024 when sodium was in the normal range to June 3rd when it was at 133. Around March, 2024, I developed insomnia which has progressed to become chronic and severe. Could this level of hyponatremia cause increases of cortisol, adrenaline, etc and the insomnia? If the answer is possibly yes, then what would you suggest I do?
Hi Robert, Chronic low blood sodium is not a good thing and can cause neurological symptoms. OHCTZ + low sodium diet can cause this condition. I would discuss with your physician lowering your dose of thiazide and – personal observations – switching to a longer acting one. At your age you might do well with a very low dose of chlorthalidone – 12.5 mg every other day – and low diet sodium. Your physician is responsible for your care and needs to be in charge. Regards, Fred Coe
Thanks so much Dr Coe; I think I will pursue making that switch.
Hi Dr.Coe,
We have added 5mg amiloride to limit K/Mg loss from 1.25mg indapamide, but as a Ca-phosphate bi-lateral nephrocalcinosis stone former it pushed urine pH to 7.4 (from baseline 6.7). On indapamide 1.25 mg, urine calcium dropped (340→260 mg/day), but I still need ~50 mEq KCl + 300 mg Mg daily to keep blood serum stable. Any thoughts on lowering urine calcium further without driving pH higher, or substantial K/MG/Phosphate loss?Your thoughts are much appreciated.
Sincerely,Connie.
Hi Connie, This is a tricky issue in details of management. I should not hazard an opinion without reviewing your data entire. Perhaps I could say that the real treatment goal is lower urine SS with respect to calcium phosphate (usually shown as brushite SS). pH volume calcium citrate all enter in and it is their SS outcome not the position of any one of them that matters. Best, Fred Coe
Hello! I have a 14 year old son with Spinal Muscular Atrophy (a neuromuscular disease) who has been diagnosed with kidney stones. His LithioLink shows high calcium, magnesium and phosphate in his urine (likely due to immobility). His urine sodium is also high but his dietary sodium is very low. Nephrologist is recommending chlorthalidone treatment to prevent calcium stones. Do you have experience with pediatric neuromuscular patients and use of thiazide diuretics to treat stones? Would you recommend the 12.5mg starting point? And should KCL also be started with it or only if labs indicate so? Thanks!
Hi Ashley, Immobility raises urine calcium via loss of bone mineral and will raise urine pH as well as bone mineral dissolution releases alkali as well as calcium, magnesium, and phosphate and sodium. I do not practice pediatric medicine but I wonder if bone oriented medications that reduce bone loss – bisphosphonates – are acceptable during skeletal growth. That is beyond my knowledge. Any kind of exercise that has weight bearing would be valuable, but I presume that is already being considered. As his problem arises precisely from loss of weight bearing, such treatment would reverse the basic problem. Regards, Fred Coe
Thanks for the reply. Do you think Chlorthalidone would be helpful in his situation? Thanks!
Hi Ashley, I could not find your prior note on this post, so I cannot answer your question. Can you remind me about what you wrote before, and where? Best, Fred Coe
Your website is invaluable and thank you for that. It has been a site that has helped me tremendously.
I post this one to present my experience with this condition:
At the age of 26 and as a young medical doctor myself, I found out about my hypercalciuria of around 350-400mg/d, small kidney stones and comorbid low bone density of around -2.5 t-score in LS, otherwise healthy.
Been on thiazides since then and the latest I’ve been using is indapamide SR 1.5mg OD. My experience is that indapamide did a better job than HCTZ probably due to its pharmacokinetic profile. Along with the addition of citrates, and rigorous weightlifting t-score went from -2.5 to -1.1 in lumbar spine, while femur didn’t have such a robust response (increase of about 5-6%). Kidney stones remained the same and some couldn’t be detected at later U/S tests.
Whats interesting with this condition and my experience is that once I lowered the weightlifting intensity (due to Covid and unfortunate disc trauma) the t-score has been returning rapidly to its probable baseline of about -2.5 t score. I conclude that:
1. once there is a strong stimulus, osteoblastic activity can overcome any resorption processes in the background due to the disorder, however once the stimulus is either saturated or stopped, the bone density is not sustained.
2. LS site as literature documents is metabolically more sensitive. Femur BMD remained high of about tscore: -1 after the stop of the stimulus (femoral neck -2.0). Probably due to high cortical ratio.
In terms of hypercalciuria indapamide in the first 1-2 years showed good response of about 180-250mg/d. 6-7 years later and the excretion is creeping up to 280-330mg/d which could be a probable factor of the BMD decline. I am thinking of either increasing the dose 1.5×2 so there are higher blood concentrations during steady-state, or take a drug-holiday while risking further decline in BMD during this time period. How long should the drug-holiday be in your opinion? I would love to hear your insight and what approach would you take. I want to notice that I take full responsibility of any decision I make, so I would love to hear your honest opinion even if it is an off-label approach (i.e. increasing indapamide).
Finally, I’ve been following the IH literature closely and I’ve been noticing more and more data on probable cardiovascular effect of this condition. So while kidney stones and bone density are in the highlight, I have a feeling cv system should be taken into consideration, especially if you take into account that thiazides have a mildly unfavorable metabolic profile. I wonder if thiazides or/and especially biphosphonates ultimately help with the cv risk as there is less bone tissue activity and could result in less arterial calcification. Thus following early on with a more aggressive approach to this condition (for instance, biphosphonate therapy without the osteoporosis criterion necessary) would be the gold standard in the future.
Thank you alot.
Hi Doctor, The bone problem in your case probably needs direct attention. Bisphosphonate is reasonable. Thiazide effects on urine calcium do not wane with time but diet sodium can rise or – as you say – bone mineral loss. Perhaps urine calcium will fall with the BP. Guidelines do not point to bisphosphonates sans OP but I have used it for years. Regards, Fred
Dr. Coe, thanks a lot for taking the time to read all that and respond. Your contribution to approaching this condition is invaluable.
Biphosphonates are indeed a reasonable treatment in such cases as you have already mentioned in your articles, as they seem to actually contribute to lowering the urinary calcium and lowering stone formation risk.
However, there’s a limitation in this category of drugs as far as I know and that is, unlike thiazides, they cannot be used indefinitely. Long term use could deteriorate bone microarchitecture due to long term pausing of bone turnover (thus the atypical fractures and other adverse effects). In a cases of younger patients, who are in their 30s/40s/50s, would you choose to use biphosphonates that early on, or wait for a more mature age to start them? Considering there’s a time-limit which you can be using these medications. Could you share your thoughts on this please?
Thank you alot.
Hi Steve, I gather you are a physician. Usually I use them in older people who are more likely to lose bone. When hypercalciuria is significant in younger people and does not respond well to conventional treatments I more and more do gene testing for high 1,25D states like CYP 24 and NaPi 2-c defects. Best, Fred
Dr. Coe,
Thank you alot, I appreciate your valuable insight. Indeed I am, but not in the domain of Urology or calcium homeostasis, so your articles are always an excellent read and dive into the beauty and complexity of nature and human biology.
In your opinion, in the hypothesis that IH (or some subtype) could be driven by increased expression of VDR (or high sensitivity to calcitriol) on bone, which could be causing increased bone resorption, is it reasonable to keep 25OHvitD serum levels on the lower end of range (for instance near 20-25 ng/ml) instead of higher ones? This in theory, could lead to less calcitriol concentrations, which would balance the higher affinity/tissue sensitivity.
Just for the curious mind, Ι increased indapamide 1.5mg SR to 3mg daily, it indeed decreased uCa to 193 (from 230-270), with UNa at 29meq/d and protein at 1.3gr/kg most of it dairy. I was expecting a much lower value, considering I had achieved 190mg/d once over the decade, with 1.5mg indapamide daily and UNa 67meq/d.
Finally, just for piece of mind, would you please take a look at some Ca-PTH pairs I’ve collected over the decade?
Ca-PTH:
10.5mg/dl – no PTH (age 25)
1.32mmol ionized( 1.27mmol being the upper limit) – no PTH
9.9 (with normal measured ionized Ca) – 39.5
10.1 – 21
9.8 – 34
9.7 – 15
9.6 – 40 (age 28)
10.3 – 38
10 (with normal ionizedCa) – 28
9.9 (with normal ionizedCa) – 31
10 – noPTH
10.2 – no PTH
10.3 – 36
9.9 – no PTH
10.1 – no PTH (age 30)
10.2 – no PTH
10.1 – no PTH
9.8 – no PTH
10.4 – 26 (age 32)
10 – 25
10.3 – 33
10.1 – 30
10.3 – 23
10 – 30 (ionized 4.73mg with range 4.1- 4.9)
10 – 28 (ionized 4.89mg with range 4.1- 4.9)
10 – 20.4(ionized 4.79mg with range 4.1- 4.9) (age 36)
Whats bothering me is I am always at the upper limit. ( and this must be independent of thiazide use. I remember having a 10.7 at the age of 20 years old). On the other hand, from what I’ve read, younger ages can sometimes have higher Ca values). My endo I’ve been seeing is insisting the values are not indicative of PHPT. The clinical image is looking alot like PHPT though, but so do IH sometimes.
Thank you alot.
Hi Doctor, No. I would not want low 25D levels as bone senses both 1,25D and 25D. IH is a state of increased vitamin D activation. For example we showed that CaSR activity is increases, no doubt from VDR action. I published evidence for increased peripheral blood monocyte VDR in IH some years ago. The borderline PTH values sans thiazide are compatible with IH as in any state of vitamin D activation at the tissue level. I have also published clinical observations that IH can give way to PHPT, and that post surgical cure of PHPT IH is not rarely left in its wake, so the two are somehow allied. In your case I would just measure and if and when PTH begins to rise stone thiazides and remeasure. Should PHPT appear, it is curable, and probably IH will remain. I should add all the above papers here but this program does not offer easy access to PubMed and you can easily find them. Best, Fred
I was put on chlorathidone 25mg. for too much calcium in my urine after 24-hour testing(400mg) My blood pressure dropped and I had a headache all day. The dr. reduced the dose to 12.5. After being on the 12.50 dose for over a month my chloride which averages 104 was 97 dropping a little below normal and carbon dioxide which is normally averages around 27 was a little higher than normal at 33. My white blood cells which are typically on the low side of normal (5.38) was 3.7. I have an appointment with my PCP but I was wondering if you thought I might be sensitive to this drug. My potassium was 3.7 within the normal range with my average being 4.1. The endocrinologist wants be to up the dose to 25mg and I feel a bit hesitant. Your thoughts would be appreciate.
Hi Antoinette, The fall in potassium, rise in CO2 and fall in chloride are expected from thiazide. The low potassium is best remedied with potassium chloride your physician can prescribe. Usually the low dose will lower urine calcium enough for stone prevention, especially if you lower diet sodium to about 1500 mg. Best, Fred Coe
Thank you Dr. Coe. I have one last question. Have you ever had a patient’s WBC affected by Chlorathiadone. My blood work has always been normal but this time my WBC came back at 3.6 and the only change has been the addition of the diuretic.
Hi Antoinette, The drug can cause a fall in WBC and given the fall you should stop it immediately. Here is a link to a Perplexity review of the subject.Of course your physician is entirely responsible for your care, but I suggest you hold the next dose and speak with her or him immediately. Best, Fred Coe
Thank you Dr. Coe. You are the best.
Hello Dr Coe, if needed how much Potassium Chloride do you normally prescribe for someone that you put on 12.5 of Chlorthalidone if they have Calcium Phosphate stones? I have a low sodium diet from 1000-1500mg.
Hi CG, I wait and see how much serum potassium changes, and when and if. If it does I usually begin with 20 mEq twice a day, but that is not exact science. Some people and very small, and some very large. Best, Fred Coe
Dr Coe,
I was put on Chlorthalidone 12.5mg four weeks ago and had blood work and as expected my potassium dropped to 3.3 and I notified the doctor to see what to do and the nurse stated the doctor didn’t think that was too low and said increase potassium foods. I already eat 10 fruits and vegetables a day plus dairy. I eat a banana a day already which they mentioned. Do you think it’s safe to have a level of 3.3 for very long? Any suggestions since they didn’t want to put me on potassium right away?
Thank you!
Hi C, I am afraid that I have to disagree here; a serum K of 3.3 is not ideal and calls for some potassium chloride supplements – I would think perhaps 20 mEq twice a day. Food will not do it. Best, Fred Coe