 Of all the knowledge on this site, a tiny nugget of three well established facts has explosive power for patients and physicians. Put to actual use they let you prevent idiopathic calcium stones and preserve bone mineral.
Of all the knowledge on this site, a tiny nugget of three well established facts has explosive power for patients and physicians. Put to actual use they let you prevent idiopathic calcium stones and preserve bone mineral.
If you do not want to read the article, I have made a VIDEO to tell you the story in about 13 minutes (available below). On my iphone the video opens well and looks better horizontal. Please let me know if it does not work well for you.
I have not been shy nor secretive. Article after article speak about the three, but always in context so other facts can distract one, as can superb but unmagical paintings from a few masterpieces hung on the same wall. I know some patients, some physicians, have fully grasped the crucial importance of the three, and put them to use. From the many comments I read weekly, I know many have not. So I am taken with a passion to redress matters.
Les Demoiselles d’Avignon, Picasso, 1907, Hangs in MOMA, NY. It is my choice of masterpiece. I deliberately cropped into the center as I love the abstraction and also want metaphor for limiting attention to a few essentials in the midst of a richness of details.
Because Spring has come to cold Chicago, I used my picture from some Springs ago. Partly it is the green ivy, partly reminiscence.
This is About Idiopathic Calcium Stone Formers
Cystinuria, uric acid stones, struvite stones – all these are to one side. Calcium stones from systemic diseases likewise. Physicians detect these and manage them. My focus is on the vast mainline of patients who form calcium stones without systemic disease.
The Three Essential Facts
Diet Sodium Controls Urine Calcium
If I could I would paint this on the sky, draw it on sidewalks across the world. It has been demonstrated by scientists for at least 70 years,
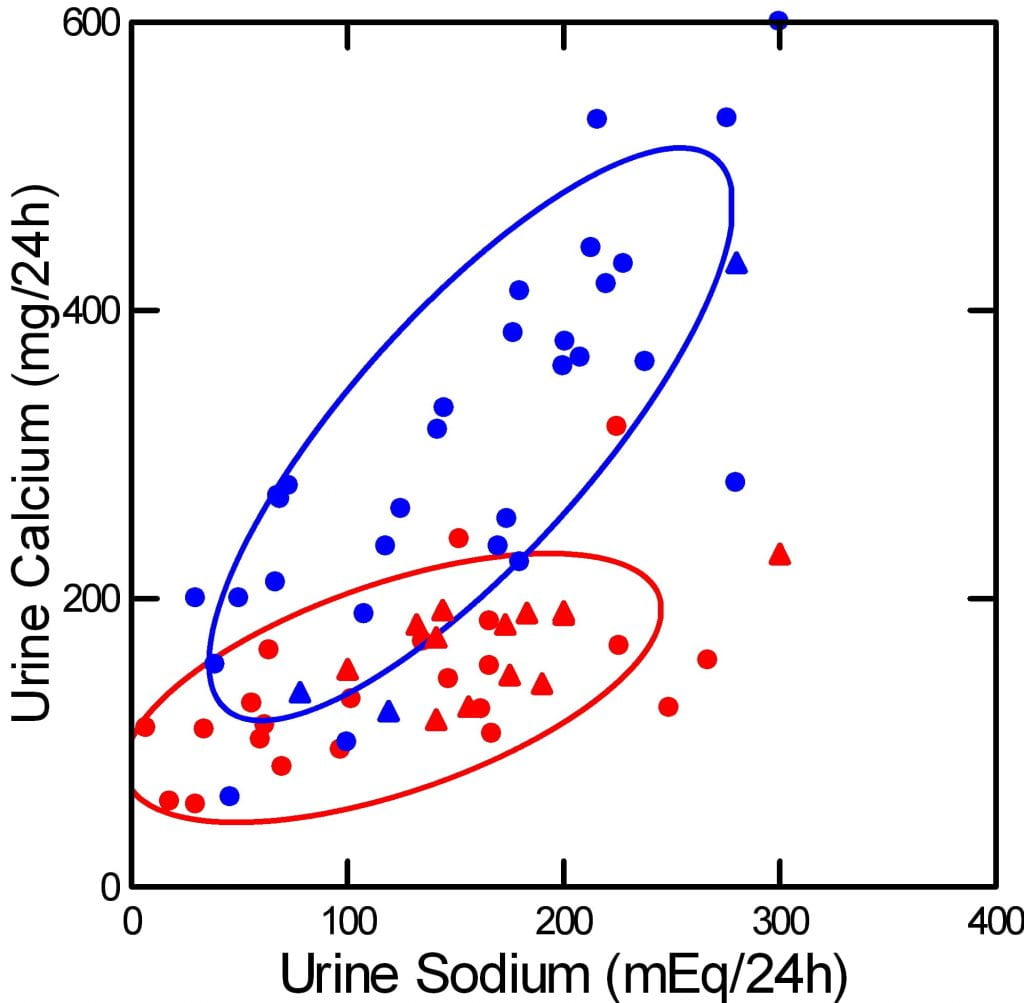
and how it happens is reasonably well known. I made this picture using published data from many sources, and I placed the original data and references within this site. The blue points are from calcium stone formers, the red from normal people.
Urine sodium is diet sodium, because we absorb almost all the sodium we eat, and excrete it in the urine. Urine calcium is not diet calcium. We absorb only 18 – 35% of the calcium we eat, and that absorption is regulated by the intestines, and by hormones like vitamin D.
Stone formers absorb a higher percentage than normals, but that is not why their urine calcium is higher. It is higher because they have idiopathic hypercalciuria and their kidneys do not retain calcium as well. At the heart of idiopathic hypercalciuria is what this graph shows – urine calcium is abnormally sensitive to diet sodium. As you lower diet sodium from the average US value of 150 – 200 mEq ( 3500 – 4600 mg) to the present ideal diet sodium of 65 mEq (1500 mg), their urine calcium (blue) falls into the normal range.
Not rarely my own patients seem disappointed when I begin their treatment with lower diet sodium. It seems so mundane, so like the common nostrum that we all eat too much salt. Many have had multiple 24 hour urine tests, and I make a crude pencil graph of urine calcium vs. urine sodium and show them their own behavior. That works, sometimes. Otherwise, they agree to so alter their food lives, but – I sense this – wonder at coming all the way to a professor for a dull seeming advice. They do not sense the power sodium has, even if I show them this graph – or their own.
Diet Calcium Controls Urine Oxalate

I made this messy but remarkable graph from work other people have done and put the name of the main author below their dots. These were experiments with variations of diet calcium, on the horizontal axis, measurements of urine oxalate on the vertical axis and diet oxalate as the size of the symbols. The smallest symbol means 50 mg/day of oxalate, the largest means 200 mg/d, the middle size is 100. In the main article using this I placed links to the original data.
The data scatter but above 1,000 mg of diet calcium all four authors found only modest urine oxalate, 35 mg/d or less as mean values. Average US calcium intake is about 500 mg/d or less, which permits a much higher swing in urine oxalate.
People with idiopathic hypercalciuria, the reason for high urine calcium in idiopathic calcium stone formers, absorb diet calcium more efficiently than normal, so a higher diet calcium supply will raise urine calcium and stone risk.
But, low diet sodium will offset this, improve kidney calcium conservation, so urine calcium can stay low even though diet calcium is high enough to lower urine oxalate.
This is part of the magic and the peril. You must lower diet sodium first and show it is low by another 24 hour urine. Then you can raise diet calcium to block diet oxalate. If you do it right, and keep the diet sodium low, urine calcium will rise little if at all with a higher diet calcium.
Diet Sodium and Calcium Control Bone Mineral
Only one trial proves this, and only in one kind of person – perimenopausal women. We could use more trials. But this one was so perfectly done, and so dramatic, we can for the moment use it as out guide.
Each woman ate each of four diets, high and low 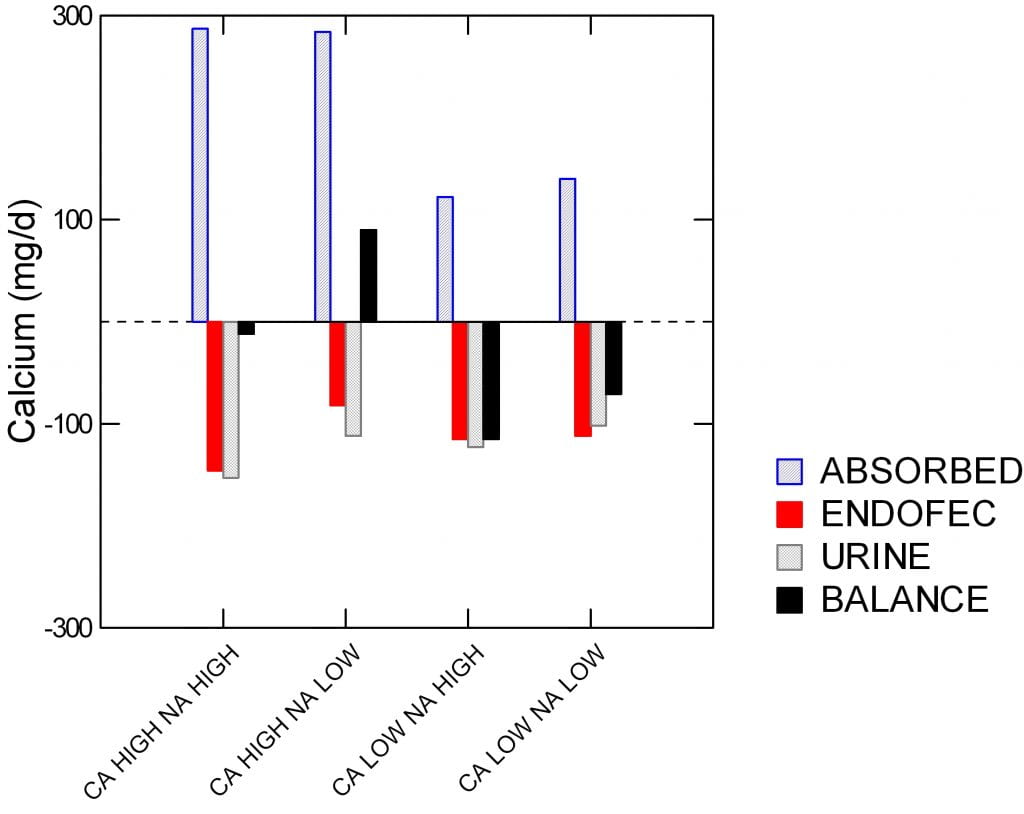 sodium, high and low calcium, and in a random round robin fashion. Specifically, the sodium levels were 1600 and 4400 mg/day, and low and high calcium (518 and 1284 mg/day. On each diet, each woman participated in a full balance study so bone mineral uptake or loss could be quantitated.
sodium, high and low calcium, and in a random round robin fashion. Specifically, the sodium levels were 1600 and 4400 mg/day, and low and high calcium (518 and 1284 mg/day. On each diet, each woman participated in a full balance study so bone mineral uptake or loss could be quantitated.
The four diets are on the horizontal axis. Calcium balance of bone is the black bars scaled on the vertical axis in mg/day, and it can be negative – bones are losing – or positive – bones are gaining calcium.
Absorption is plotted upward, meaning more for bone. Urine and intestinal secretory (‘endofac’) losses downward meaning potential losses for bone,
Balance was positive only with the high calcium + low sodium diet.
The amount of calcium absorbed was higher on the two high calcium diets, of course, and the urine calcium was lower on the low than on the high sodium diets.
As I have already said, the odd term ‘endofec’ means the amount of calcium secreted from blood into the stool by the duodenum, pancreas, and small intestines. This was measured using stable isotopes. If you look close, it was a fall in urine calcium and calcium secretion, both, that created the bone mineral gain from high calcium low sodium diet vs. the high calcium high sodium diet.
Also look close at the urine calcium. The high calcium low sodium diet gave the very same urine calcium as the low calcium high sodium diet. In other words, the women could raise their diet calcium from 500 to nearly 1300 mg/day and yet by lowering diet sodium to 1600 mg/day keep urine calcium unchanged.
The Magic Works for Stones
This is the one trial of the magic formula. Low diet sodium to keep the calcium in the body and thence the bones, high diet calcium to keep oxalate out of the body and thence the urine. It works for bones. Does it work for stones?
Of course, why else would I put it here, and many other places on this site.
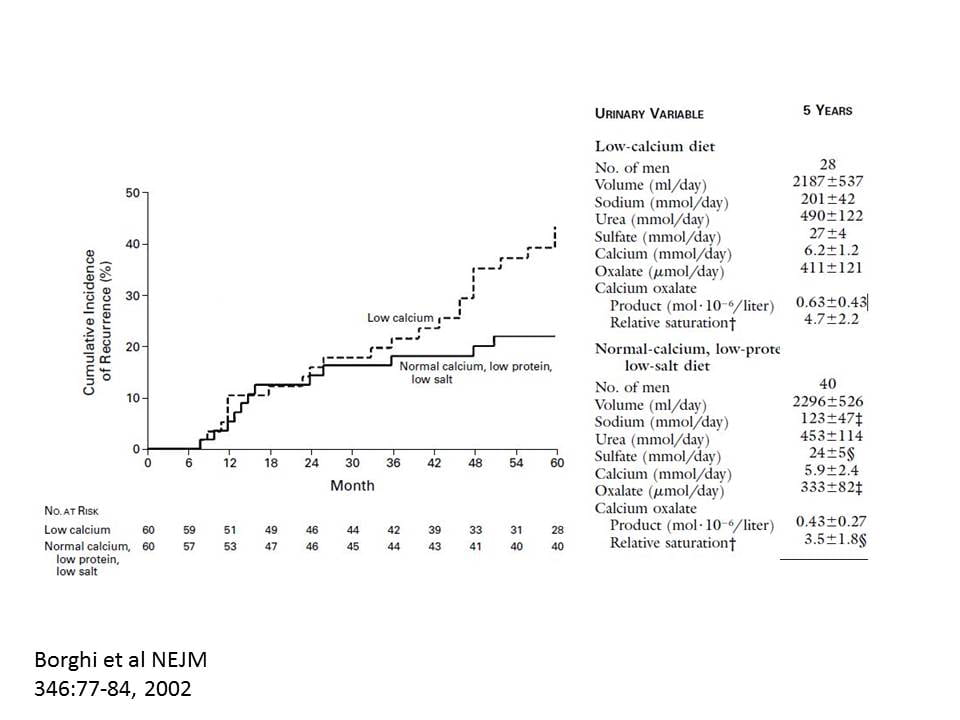
I made the graph very large so your could see the printing in the overlay. The patients were men forming calcium oxalate stones whose urine calcium exceeded 300 mg/d. Low calcium diet was 400 the high calcium 1200 mg/day. The low sodium diet was aimed at 1150 mg, the high at the usual level of about 4000 mg/day.
After five years, stones were fewer in the high calcium reduced sodium group – highly significant statistically.
The why of less stones is exactly what my prior graphs predict.
Of course urine sodium was lower in the low sodium diet group (2,800 vs. 4,600 mg/d, low vs. high sodium, respectively).
Urine calcium of the low and high calcium groups was virtually identical (248 vs. 236 mg/d, low vs. high diet calcium, respectively). Just like for the women in the bone study, one could triple diet calcium yet keep urine calcium the same by lowering diet sodium.
Are you not amazed by this? In two studies one can raise diet calcium three fold and urine calcium does not increase if you also lower diet sodium. Look at the power diet sodium has.
How about oxalate?
Both groups were told to avoid high oxalate foods – walnuts, spinach, rhubarb, parsley and chocolate. The high calcium diet lowered urine oxalate (333 vs. 411 umol of oxalate/d, high vs. low diet calcium, respectively). Supersaturation for calcium oxalate, the proven driver of stone risk, was 3.5 in the high calcium and 4.5 in the low calcium group.
Think about how the threefold magic formula worked. Low sodium diet permitted high diet calcium. The high calcium lowered the oxalate but could not raise urine calcium because sodium was so low.
How to Use the Three Facts
These are magical facts, but they must be used in the right order. It is exactly like casting a magic spell.
Lower Diet Sodium First
Make the change and then be sure you did it by getting a new 24 hour urine. Without the urine test you will never know if you succeeded. Ask yourself if what you did during the collection was like the usual for you and also ask if you really mean to keep the diet sodium as low as during the test. If you get tired of the low diet sodium, and urine sodium rises, all is lost.
Raise Diet Calcium Next
Once you know your diet sodium is low, raise the diet calcium and test again. Is diet sodium (urine sodium) still low? If so, is urine calcium low enough? Low enough is about 200 mg/d of calcium or less.
If so, you are done. If not, you need to keep changing diet sodium and calcium until you get there – high diet calcium, below 200 mg urine calcium.
Some people cannot make do with only diet. Their urine calcium remains too high. For them, we add thiazide to the diet, usually in a very low dose. But for most, this will do. You must keep the low diet sodium, so the thiazide works well at a low dose, and to avoid potassium loss.
Now, Consider Diet Oxalate
With high diet calcium in place, is urine oxalate high enough to raise risk of stones – above 25 – 30 mg/d. If so, it is time to get rid of the highest food oxalate sources. Not all food oxalate, but foods on the high end. I listed some just above. My site has the main ones on a graph. Work from the top down.
Diet oxalate is the last thing to worry about, never the first. One wants to remove what high diet calcium has not removed.
Of course, repeat 24 hour urines are the only way to know if success or failure has attended your efforts.
If You Have Bone Disease
If your bone mineral is deficient, these diet changes are good but you need a physician to be sure they are enough. You may also need medication. Do not rely on just diet. Repeat bone mineral measurements are essential. Be sure your physician is satisfied with your bone health.
If you do Not Have Bone Disease
You may not have looked. Get a bone mineral density. If it is normal, get another some years later. The diet is fine for you unless bone mineral declines. If it does decline your physician needs to manage things. The diet is still advisable, but may not be enough.
There is More but Focus Here, on the Big Three
Diet potassium and protein matter, the former from from fruits and veggies. Diet refined sugars matter, they raise urine calcium. Diet protein matters, too much raises urine calcium. The kidney stone diet accounts for all of these.
Fluids matter. Urine volume should be above 2 liters/d, the point at which stone risk has been reduced. But fluids are never enough.
But the three way magic spell predominates over all else: – lower diet sodium, then raise diet calcium, then consider diet oxalate.
Keep your mind on diet sodium and calcium first, and be sure they are set properly. Then go on, if you must, into the thicket and brambles of oxalate lists. Then control unhealthy sugars, excess protein, and get adequate diet potassium. They matter, I always attend to everything I can.
But always, I urge, stay on the main road. Perform the magic spell and see how far you can get.


Can KCl be used as a substitute for NaCl in IH, or does it also cause Ca loss in the urine? Thanks so much for you work in this area.
Hi John, KCl is not so nice taste wise but some people use it in place of NaCl. For stones, KCl is not a problem. Let your physician know before using KCl to be sure she/he is fine with it. Do not omit that simple precaution. Regards, Fred Coe
Dr. Coe, thanks for this article! It is one of two I have bookmarked and printed and tried to interest clinicians in.
I’ve just been looking at LabCorp’s website and Quest’s (questhealth . com), and neither seem to offer a lab test that includes a 24h urine sodium or calcium or oxalate analysis, at least not one that an individual can order directly. “Ulta Lab Tests” ( ultalabtests . com ) also doesn’t have one for sodium but has one for calcium ($50) and another for “oxalic acid” ($88) — is “oxalic acid” the same as what we want or do we want “calcium oxalate” or just (free) “oxalate”?
So after increasing my urine volume and lowering sodium intake, I seem to be have hit a stumbling block in taking your advice ! I know I’m not the only patient visitor to your web pages to note clinicians’ or insurance companies’ lack of interest in your method and the urinalyses they require, so I know there are others who need to find businesses from which they can directly get the needed urinalyses. Is anyone else having difficulty finding these? Do you know of any you can mention? If there does not yet exist on this website an article I have overlooked that contains links to such direct-to-consumer lab services, perhaps I can help you create such an article if I can eventually find some such services.
Hi Kevin, It should be clear to you by now why I founded Litholink. There are few decent vendors but LL is ideal. Fred
Hello Good Sir!
I enjoyed learning about you and your life’s work. Fabulous site. Clarifying question, please. For the first of the 3 facts, “Lower Diet Sodium First,” I am assuming you are referring to refined table salt, which has been processed and stripped of its naturally occuring trace minerals? Wouldn’t unrefined salt such as Redmond Real Salt and quality Himalayan Salt be different since they contain the full spectrum of minerals, typically 80-ish trace minerals, and no additives?
Thank you kindly,
Victoria
Hi Victoria, I too love good salts – I favor sea salts. But between us, sodium is sodium, an atom, and it will do what sodium does howsoever charmed by added tasties. This is not to argue against tract minerals, but the main atom, sodium, is a villian for stone formers – raises urine calcium if you are prone to hypercalciuria, and can contribute to loss of bone mineral. Best, Fred Coe
Dear Dr. Coe, I have developed four phosphate kidney stones in the past two years. Six weeks after my last surgery, I went to my post-op appointment and learned that I have two more stones. These did not appear in my kidney CT a month prior to my surgery. I need more experienced help with prevention. Is it possible that they didn’t completely remove these stones and that’s why I’m getting regrowths? Can you recommend the name a doctor and center in the Phoenix/Scottsdale Arizona area please? Thank you.
Reply
Hi Sherry, calcium phosphate stones, especially brushite, can grow rapidly. Mayo has a branch not too far from you and I would recommend it as an excellent choice. Regards, Fred Coe
Great information thank you! How long should you focus on the low sodium before retesting to see if you are ready to increase calcium?
Yes, Rachel, an excellent deduction. I really should take a look and see if I made this clear enough. Thanks, Fred
hi!
I did a 24 hour and the only 2 standouts were high Calcium at 347 and sodium 144mmols.
I have stopped adding any salt and have been watching any other intake in an attempt to lower sodium, as recommended. Hoe long should i wait to retest to see if it’s working before i increase my dietary Calcium?
PS I do not eat ANY calcium because i don’t eat dairy, could this be the problem?
Also, i read somewhere (can’t find it now) that increased dietary Lysine can create stones, are you familiar with this? I was using a lot of lysine to counteract my dietary arginine for cold sore prevention, wondering if i caused stone with that???
Hi Cara,
Your lack of calcium can very much be adding to your stone problem. My website has so many articles on how to get calcium without using dairy. Go to kidneystonediet.com/blog
Also change your diet over the next couple of months and then do the follow up urine collection to see how much you lowered your urine calcium. Don’t forget to do all the kidney stone diet goal, which you can find here: kidneystonediet.com/start.
The Lysine is less of an issue. Don’t overdo any supplement is a great rule of thumb and only use those that you are deficient in.
Jill
My calcium in urine is 314 and my sulfur is a little high. Could it be that I’m eating too much protein and beef? Will this high calcium and sulfur combo create a stone? I’m drinking 12 cups of water daily with 2 cups lemon juice I read that stones can’t form in diluted urine
Hi Matt, High protein can raise urine calcium. The protein catabolic rate can help – values above 1.2 usually raise urine calcium enough to matter. The high calcium could in principle cause stones, but this major study did not link protein intake to increased stone risk. Regards, Fred Coe
Dear Dr Coe,
I follow you for your kidney stone advice and I also look to the University of Texas SW to see what they have to say about Stage 3 Kidney Disease and to other sites. But some use different measurements.
I have doubts about my ability to figure out certain equivalents so as to be able to relate the various reports.
If one is taking so many mg of potassium citrate, I know that the amount of elemental potassium in mg is 38.3%. Does that mean that the other 61.7% is all citrate?
Can you please tell me what the mmol and the meq of 1mg of citrate is?
Your truly,
Michael
Hi Michael, For the commonplace 10 mEq potassium citrate pill, which has 1080 mg of potassium citrate crystals, it contains 10 mEq of potassium and 10 mEq of citrate. It is not easy to parse the milligrams of potassium vs citrate, nor necessary. Hope this helps, Fred
Dear Dr Coe
Potassium Citrate neutralizes the acid load in the kidneys. Does Potassium Citrate also neutralize the stomach acid? Would it prevent the calcium in cheddar cheese from being available to the body? Should a calcium food be eaten at a different time from when one takes Potassium Citrate?
Thank you.
Yours truly
Michael
Hi Michael, No. Potassium citrate is absorbed and the citrate is metabolized as citric acid thus taking protons off of the blood buffers. The agent has no known effects on absorption of food nutrients. Regards, Fred Coe
Dr Coe. My 24 hour Lithoink urine calcium is 231mg and my Urine Oxalate is 45mg. My citrate is slightly low 503. My sodium is 71mmol/24hr. I now better understand that I need to keep a low sodium diet, replace animal protein with plant protein, eat lots of
fruits and vegetables to raise my citrate. Is 71mg a reasonably low sodium diet or should it lower? I’m concerned because my dr. now wants me to take Inda[amide l.25mg daily. What is the best dietary calcium to take to sufficiently raise my calcium …..while not robbing it from my bones?
Hi Kay, Youe urine sodium is excellent for lowering urine calcium which is still hefty. As for fruits and veggies, they are an ideal source of potassium and alkali. I presume your physician wants to use indapamide to lower urine urine calcium further. As for diet calcium 800 to 1000 mg is generally ideal for bones and will lower urine oxalate if taken as food and with meals that contain oxalate – plants. Regards, Fred Coe
I am 60 year old female following the Kidney Stone diet and am taking Fosamax for osteoperosis. My urine calcium is still high at 308. I cannot seem to tolerate even low does of Hydrochlorithiazide (extreme dry eyes). Do you think it would be worth trying another thiazide (do they have the same side effect profiles)? My bone density did improve on Fosamax and my CTX is good at 236. I would love to correct this hypercalciuria to save my bones especially when I have to stop taking the Fosamax. Fortunately, I have never had a kidney stone.
Hi Shelly, Your high urine calcium despite thiazide and fosamax makes one wonder about cause. Are your physicians sure you have no other condition – primary hyperparathyroidism comes to mind – and there are others as well. What has been done by way of testing and what found? Perhaps you will be as some patients I have studied – high urine calcium, bone disease despite a bisphosphonate, no apparent reason and a woman. If I were to consider research on the problem it might aim at loss of estrogen effect on the kidney cells. Practically your physicians might want to be certain about established causes of bone disease and hypercalciuria besides menopause. Regards, Fred Coe
I need assistance interpreting my 24 hr urine results. These are the levels out of range. What does this mean?
Calcium Oxalate Saturation 3.86
Calcium, Urine 365
Calcium Phosphate Saturation 2.41
pH, 24 hr, Urine 6.970
Sodium, Urine 181
Urea Nitrogen, Urine 14.38
Protein Catabolic Rate 1.6
Calcium/Kg Body Weight 5.8
Calcium/Creatinine Ratio 330
Hi Angela, You have a very high urine calcium and a very alkaline urine (pH 6.97) which can foster calcium phosphate stones. The high calcium is in part due to massive protein excess (PCR 1.6 gm protein/kg body weight/day vs 1.0 as normal). The high pH can be normal in young women, or perhaps you have other diet issues or take supplements. Your physicians probably have already recognized these issues, and plan remedy. If not they should want to. Regards, Fred Coe
I really appreciate all the imformation you have provided. I have learn alot. I have had stones on and off for years. I am 69 yr female. I take 200 mg calcium citrate and Vitd D 1000mg daily.
My recente 24 hour urine panel shows the following and I would like some guidance on interpreting the results and knowing what dietary changes I should make. Three months prior I had done the same test the only difference being that I increased water intake and did not take the clacium cupplement. Those resutls are in () :
Cal. Oxalate Sat. 5.88 (4.00)
Cal. urine 248 (235)
Oxalate 26 (26)
Citrate 765 (672)
Calcium Phosphate Sat 0.43 (0.36)
ph 5.623 (5.832)
Sodium 87 (89)
Potassium 51 (48)
Creatinine 996 (912)
Two of my siblings also have stones. 1 year ago I had my PTH checked and it was fine.
I am willing to make dietary changes before using medication.
Thank you,
Nel
Hi Nelida, Your urine calcium is high enough to raise calcium stone risk, and your urine is acid enough to raise uric acid stone risk. I presume you produce calcium stones though you do not say. Likewise you do not show the urine volume, but I guess it is not very high because your SS CaOx is nearly 6 with an oxalate of only 26. Purely guessing you stones are CaOx and your urine volume has been low, but I do not have enough here to be helpful. Regards, Fred
Can you eliminate my full name from the previous comment?
Nel
Hi Nelida, I do not know how. But I will try. Fred