Unlike Zeus, or Athene, Janus did not come to Rome from Greece but from myths about a person living early in Roman history and later deified. Janus – deity – presides over beginnings and endings, gateways and doors, invariably dual in nature.
For the Full Video – 19 Minutes
For the Shorter Version – 11 Minutes
What is dual here?
Calcium stone formers are dual. A minority arise from systemic diseases we must screen for. Each systemic disease has its own universe of causes and treatment decisions. A majority are “idiopathic”, systemic causes have been excluded.
Idiopathic calcium stone formers are dual. They have no systemic cause of calcium stones. Most form calcium oxalate stones. A minority, more women than men, form calcium phosphate (CaP) stones.
Idiopathic calcium phosphate stone formers are dual. Most have hydroxyapatite (HA, like bone mineral) as their stone calcium phosphate. Some have brushite (Br, calcium monohydrogen phosphate) in their stones. These latter have more kidney damage than HA CaP stone formers, and are a special high risk group of patients.
Both kinds of CaP stone formers need special attention. That is why I have written this article for them.
Basic Facts about Phosphate Stone Formers
Phosphate Stones Damage Kidneys
Phosphate stones, HA or Br, can grow faster and larger than calcium oxalate ones. Calcium phosphate crystals invade kidney tissue – so called tubule plugs. Tissue damage is common, as is Nephrocalcinosis from plugging – often misdiagnosed as medullary sponge kidney. Kidney tissue damage is worse with Br than HA stones. Potassium citrate, a common stone prevention, may not be appropriate as a treatment because it raises urine pH.
Alkaline Urine Causes Phosphate Stones
Stone phosphate replaces oxalate when urine is too alkaline. Kidney and GI tract physiology raise urine pH, especially in women. Diet is not the cause of higher urine pH. Diet will not reliably lower the pH, and we have no specific drugs to do it, either. So although treatment uses the same tactics as for the more common calcium oxalate patient, it must follow a different strategy.
How Stone Analysis Distinguishes CaP from CaOx Stone Formers
Only CaOx and HA Present
If the average stone mineral composition of all available stones for a given patient is above 50% calcium oxalate, the patient is considered a calcium oxalate (CaOx) stone former. If the average calcium phosphate content is above 50% the patient is considered a calcium phosphate stone former.
The average must be computed using 0 – for example, given CaOx/CaP percentages of 100/0, 0/100, 40/60, the correct classification is 140/3 vs 160/3 or 46% CaOx vs 53%, and so a CaP stone former.
Uric Acid, Struvite, Cystine Also Present
If uric acid, struvite, or cystine are present we name the patient for that constituent. A patient who forms mixed stones – for example, 60% calcium phosphate/20% struvite 20% CaOx is called a struvite stone former. The reason is that these stone types have special causes and treatments.
Any Brushite Present
Brushite is very uncommon in human kidney stones, and associates with large tubule plugs and more severe tissue damage. So when any stone contains brushite we classify the patient as a brushite stone former even though brushite is a minority of stone mineral.
Sex and Age
Single Clinic Experience
Percentages of Cases
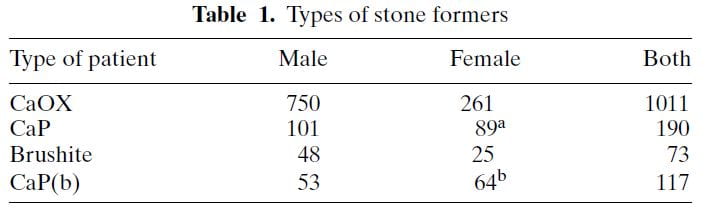 The table shows ‘CaP’ as cases where HA or brushite was the stone phosphate crystal (in early years we did not distinguish). CaP(b) are CaP stone formers with only HA, no brushite in any stone.
The table shows ‘CaP’ as cases where HA or brushite was the stone phosphate crystal (in early years we did not distinguish). CaP(b) are CaP stone formers with only HA, no brushite in any stone.
CaP predominate among females (a and b superscripts denote outsize high frequencies). Brushite does not show this difference a statistical level of significance. CaOx stone formers predominate among the total of all cases. Brushite patients are least common.
Sex vs. Percent CaP in Stones
The same study furnished this nice graph showing the sexes as the percent of stone CaP increases. The bulk of patients have very little CaP in stones (tall bars at the left of the graph). These are the common CaOx stone formers, mainly men (% female, dots, right axis about 25%). But when CaP percent is 20 – 50% in stones, women and men are nearly equal.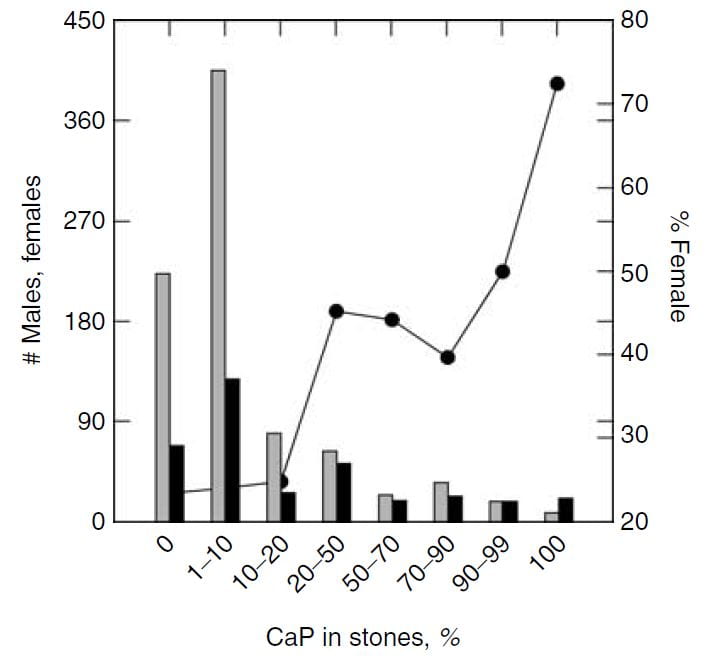
This graph blurs the sex distinction because we used stone CaP% from both brushite and hydroxyapatite. Today, I would have left the brushite to one side, which would have made the female preponderance among those with high stone CaP% more marked – because the sex ratio for brushite stone formers is closer to 1.
National Laboratory Findings
The Mayo Clinic kidney stone analysis laboratory analyzed 48,446 stones in 2010, and of these 43,545 were the first submitted to the lab for that person. From these stones, they report the distribution of stone type by sex and age. I have made a graph from Table 2 of their publication.
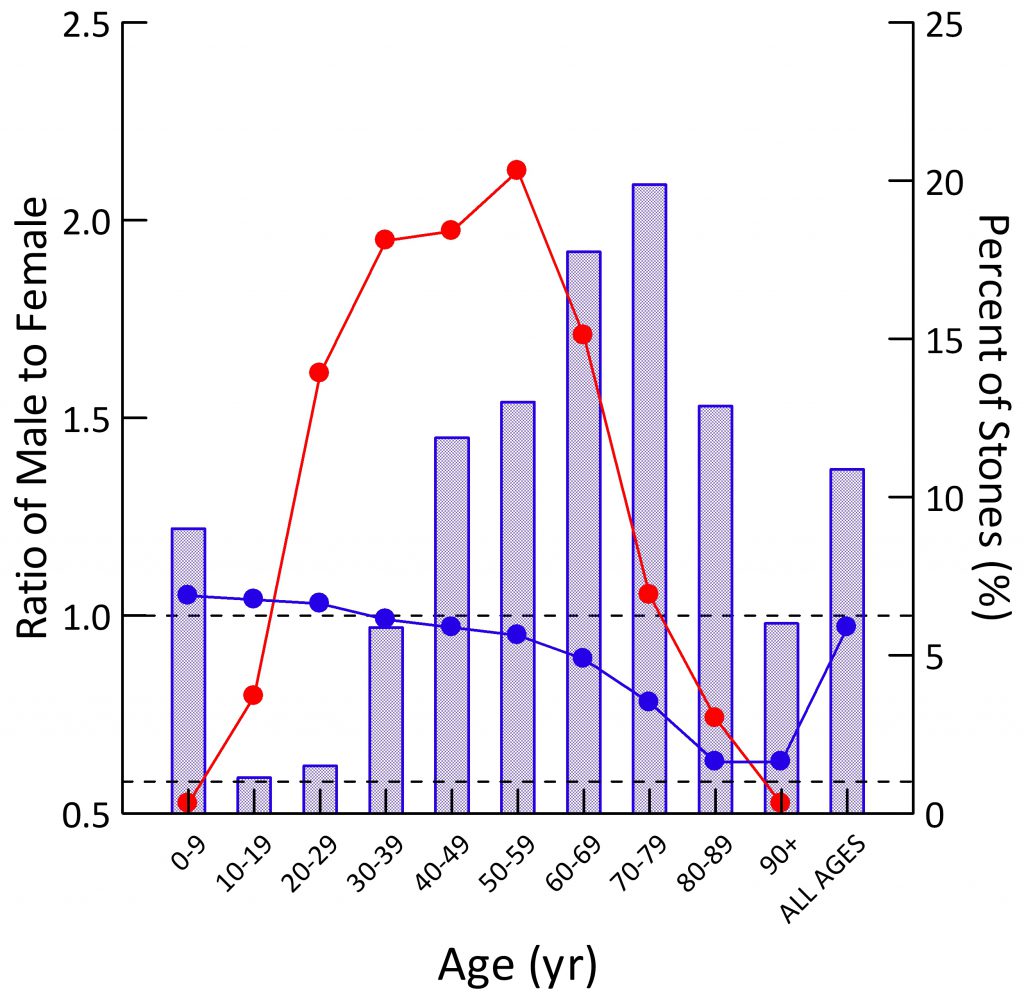 Population Sex Ratio
Population Sex Ratio
The general population contains more males than females at younger ages (blue dots). By age 30-39 the two sexes are present in equal numbers. Thereafter, as men predecease women, their blue dots slump downward.
For all ages combined, the ratio of men to women is just under 1 (last blue dot at right).
Stone Former Sex Ratio
The blue bars show male to female ratios among stone formers. Remember this is counted from the sex of the person whose stone was analyzed. A survey based on symptomatic rates of stone passage, by contrast, might give different results altogether.
In childhood, men have slightly more stones than women (blue bar is above 1.0). In the teen years and up to age 39, women predominate over men (blue bars are below 1.0). After age 40 men predominate, until at age 90 and more, in this and perhaps most things, the sexes come into a near perfect alignment. Averaged over all of life, men have more stones, which appears to be because of their midlife excesses (Height of the ‘ALL AGES’ bar above 1.0).
The fraction of all stones formed (red dots; scale along the right axis) for both sexes combined is highest from age 20-69, with only a small fraction in childhood or old age.
Types of Stones
The men are on top, women on the bottom of the picture to the left.
Stones were classified using the system I have used on this site. Uric acid in any amount meant the stones were classified as uric acid stones, and likewise for any struvite or cystine.
CaOx stones preponderate among both sexes over all ages, except in women between ages 20 – 39 stones were about half CaOx and HA. With age, HA stone frequency fell in both sexes, so that most men, and most older women (over 40) have CaOx stones.
Brushite stones, in both sexes, are very uncommon. You can see them as triangles along the bottom of both graphs.
Over age 50, uric acid stones become a significant concern in both sexes.
Struvite stones, which always arise from infection with bacteria that possess urease, are more common in women than men, a fact known for ages.
The Mystery of Brushite
Brushite stones are rare but should be rarer still. I have written a whole article on brushite because it is so important and yet so evanescent. It forms first of all crystals in human urine. If pH is not too high, oxalate steals away its calcium atoms so it vanishes. If pH is high, HA does the same, and brushite vanishes.
Why, then, are there any brushite stone formers?
I do not know nor does anyone I know of. It is an open question that seems obscure but whose answer might well lead to some new understanding of how stones form.
The Importance of Brushite
Being the first crystal to form, brushite supersaturation is crucial for stone prevention, a fact not intuitive but worthy of special emphasis. Rare in stones, vanishing in most urine, yet brushite supersaturation is foremost in importance for clinicians and patients. The goal is a supersaturation below 1, so brushite cannot form. For those who want to know more about why, please look at the parent article.
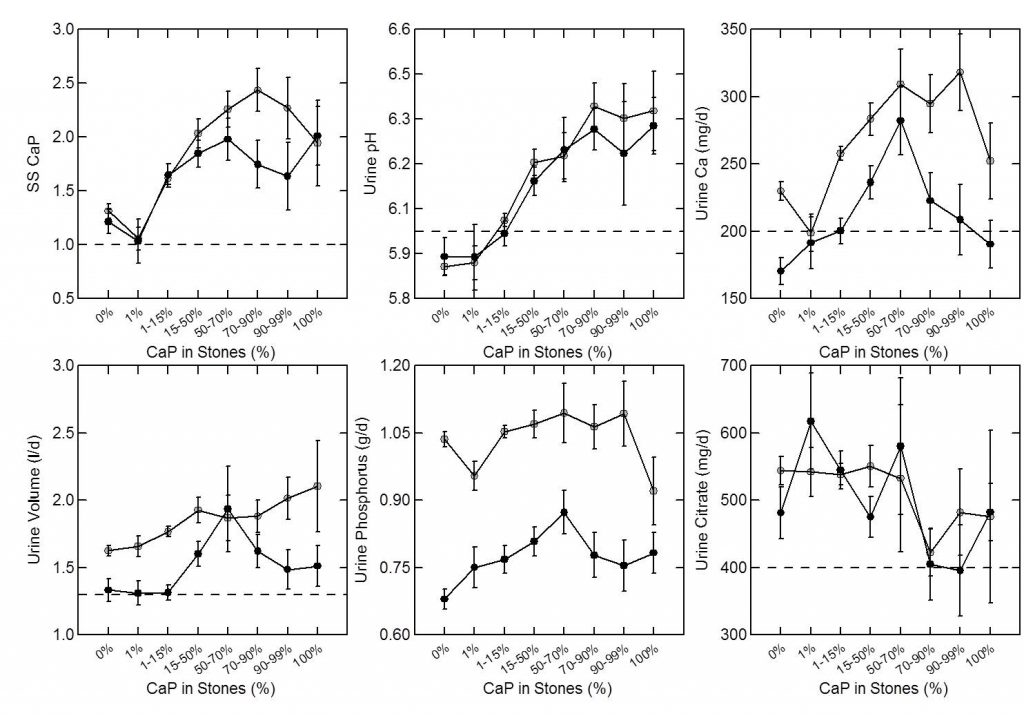
Time and Shock Wave Lithotripsy
We (left hand figure below) and others have noted an increasing percent of CaP in stones over the past 30 years. In women (black dots) CaP percent is always higher than in men, but it has risen in both. For those of a quantitative bent, the time trend of stone CaP tested by ANOVA with post hoc contrasts was significant for both sexes, and women were higher than men throughout.
In the publication, we found a relationship between CaP 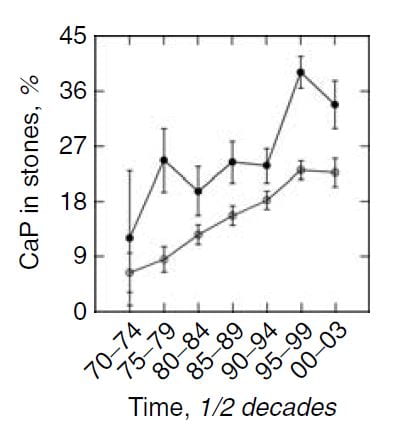 percentage and numbers of shock wave lithotripsy procedures. Use of potassium citrate, however, did not seem to increase stone CaP.
percentage and numbers of shock wave lithotripsy procedures. Use of potassium citrate, however, did not seem to increase stone CaP.
The number of shock wave procedures per patient adjusted for the number of stones and the years of stone disease rose with the percent of CaP in stones (Panel A of the figure below to the right) and the percent of CaP likewise adjusted for number of stones and duration of stones and sex rose progressively with the number of shock wave procedures (Panel B of figure to the lower right).
Not shown here, but of interest, the number of shock wave treatments was higher among BRSF than HASF suggesting a link between shock wave treatment and brushite stones.
One might infer from this set of graphs that the advent of shock wave lithotripsy caused the increase in phosphate stones, and there is nothing to contradict the idea. In fact, the very physiology of phosphate stone formation and the effects of shock waves on kidney 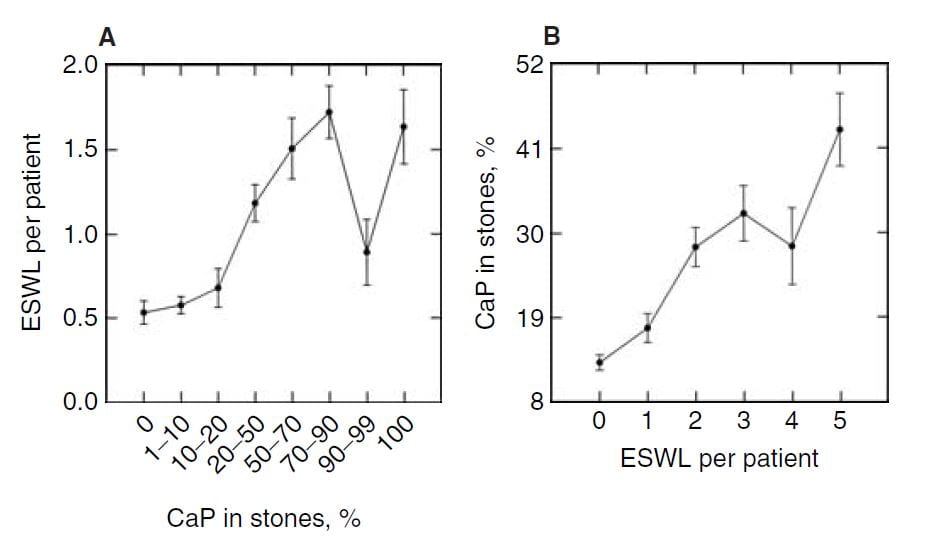 function strongly support that idea as I shall show you.
function strongly support that idea as I shall show you.
Mechanisms of Phosphate Stone Formation
High Urine pH
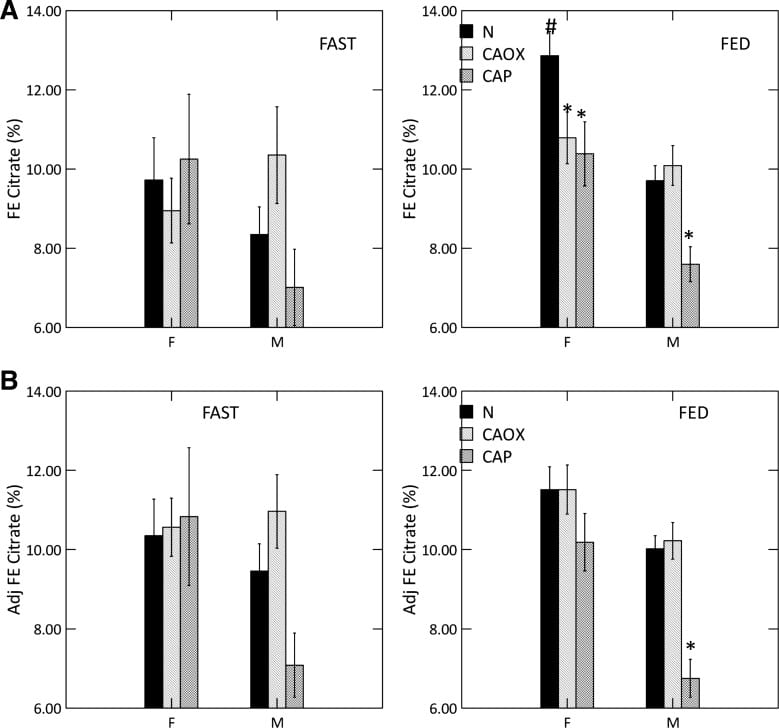
As expected, percent CaP in stones (upper left panel of the figure below) rises with CaP SS. I have shown elsewhere on this site that stone crystals parallel urine supersaturations.
Because CaP SS depends powerfully on urine pH one expects and finds (upper middle panel) that urine pH tracks very closely with stone CaP percent. Urine calcium, volume, phosphate, and citrate excretions (remaining panels) had no important relationship to stone CaP percent.
But take a look at the urine calcium excretions (Upper right panel). They are very high on average. This is because a high fraction of all calcium stone formers have genetic (idiopathic) hypercalciuria. Risk for stone forming begins at a urine calcium of 200 mg/d in both sexes.
So you can think of CaP stones as a two hit model.
Genetic hypercalciuria promotes calcium stones, and urine pH controls the fraction of phosphate in the stones. High CaP SS and CaP stones require a urine pH significantly above 6 as shown in the upper middle panel.
Kidney Tissue
Plaque and Plugs
CaOx stones can be produced as overgrowths in interstitial HA deposits, called plaque.
Idiopathic CaP stone formers, and patients with stones from bowel disease, ileostomy, renal tubular acidosis, and primary hyperparathyroidism, form stones on plaque but also on plugs of HA that fill and damage the last millimeter or so of the nephron, the inner medullary collecting ducts and ducts of Bellini.
Although we are not certain, I think it is fair to say that the plugging of CaP stone formers is because more CaP crystals form in urine and can produce plugging. In a recent article I trace out how calcium phosphate actually forms, how it is a rapid process compared to calcium oxalate, and therefore more able to make plugs during the short times it takes for urine to pass out of tubules into the renal pelvis.
Distinctions Among the Three Idiopathic Calcium Stone Formers
We have 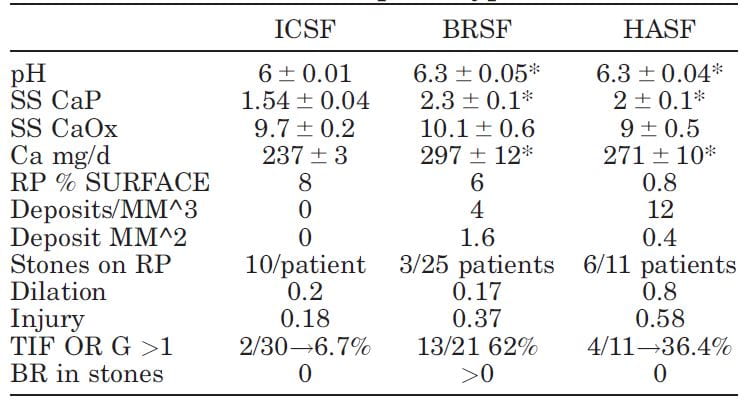 published selected laboratory and tissue findings of CaOx, brushite and HA stone formers, in an attempt to clarify differences in how stones form, and amounts of tissue injury.
published selected laboratory and tissue findings of CaOx, brushite and HA stone formers, in an attempt to clarify differences in how stones form, and amounts of tissue injury.
Numbers are small because each patient had been studied with intra-operative imaging of the renal papillae and papillary biopsy: 11 CaP (HASF), 25 BR (BRSF), and 30 CaOx (ICSF) stone formers.
As expected, urine pH was higher in the BRSF and HASF than in the ICSF, as was supersaturation (SS) for CaP. Incidentally, urine calcium (Ca) was also higher in both CaP groups than in the ICSF.
Mainly CaOx and BR stone formers formed plaque, and mainly CaOx SF form stones on it. About 8% and 6% of papillary surfaces were covered with plaque in ICSF and BRSF but only 0.8% among the HASF. CaOx stone formers had an average of 10 stones/patient attached to plaque, vs. only 3 plaque stones in 25 BRSF and 6 in 11 HASF stone patients: 10/ CaOx patient vs 0.12/brushite patient and 0.54/HA patient. These are 80 and 18 fold differences, respectively!
Plugging (‘deposits’ in the table) was absent in ICSF, but common in BRSF and HASF. Plug size averaged 1.6 mm2 in BSRF but only 0.4 mm2 in HASF – a 4 fold difference. The number of plugs was 3 times higher in HA vs. Br patients: 12 vs. 3/mm3 of tissue volume. BRSF formed fewer but much bigger tubule plugs.
Calyx dilation (a abnormal finding) estimated during surgery was higher in HASF than in the other two groups, and papillary injury (papillae are the parts of kidneys inside calyces) higher in both phosphate groups than in ICSF.
In the kidney cortex, far from where stones form, many CaP stone formers had scarring (TIF, tubular interstitial fibrosis) vs. very few CaOx patients. Brushite patients had most cortical damage.
So phosphate stone formers have injury involving the papillae and cortex, whereas CaOx stone formers have almost none.
Why is Urine pH High?
Being Female
I wrote a whole article on how women raise their urine pH. They do it by absorbing from their food a higher fraction of its alkali content. No sense copying all that here, it is better to read the article. High GI alkali absorption is not easy to treat. Those alkali are nutrient – anions that cells metabolize to get energy.
Being Young
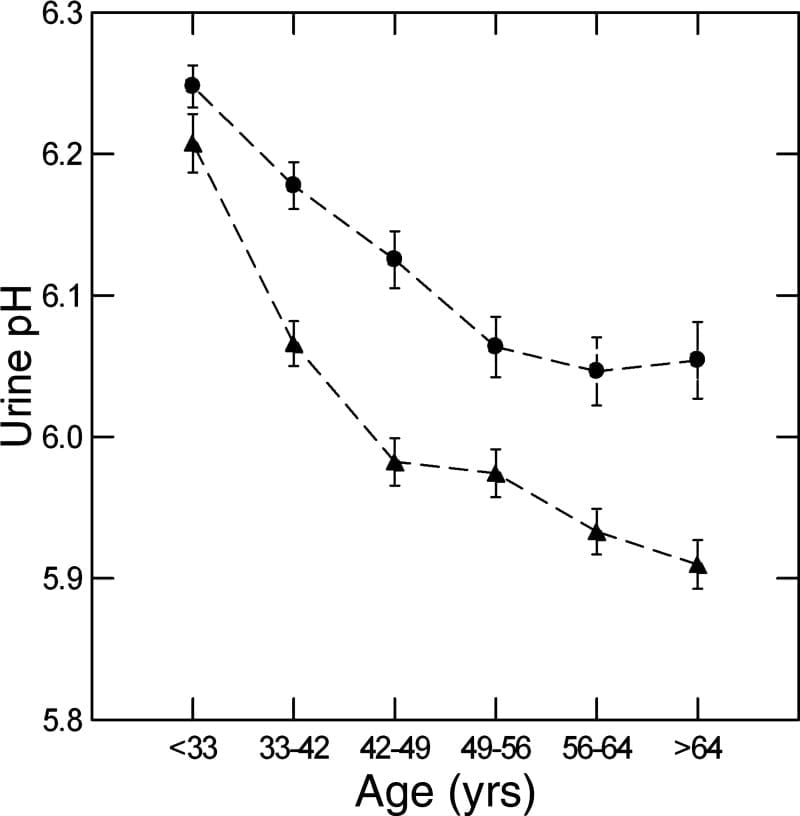
We used a massive database of kidney stone formers to ask what happened to urine pH in men and women with age. The answer is it falls, in both sexes (women are circles, men triangles).
Why is a long story. We could exclude gain in BMI, loss of kidney function, and GI alkali as reasons, but could not find the reason itself. In fact, GI anion absorption rose with age, as if to offset the falling pH.
Here the important fact is on the graph – higher pH in women and in youth are an obvious cause of more CaP stones.
Shock Wave Lithotripsy (SWL)
No practical experiments permit us to measure effects of SWL on urine pH in humans.
For these reasons we turned to an animal model: The farm pig whose kidney is much like that of a human, and likewise is similar in size.
In these animals we could shock one kidney, and then compare the treated to control side at time intervals after the treatment, the untreated side being a perfect control as both kidneys are bathed by the same blood.
SWL Raised Urine pH.
Urine pH from the treated kidneys was 0.18 pH units higher than the control, meaning SWL had increased urine pH (first line of table under ‘Basal’).
SWL Damaged Kidney Tubule Function
There was a lot more.
Urine flow, and excretion of bicarbonate, potassium, chloride, sulfate, calcium, magnesium, sodium and oxalate all were higher from the treated side (bolded). This means that shock wave treatment affects tubule handling of multiple molecules, presumably because of injury.
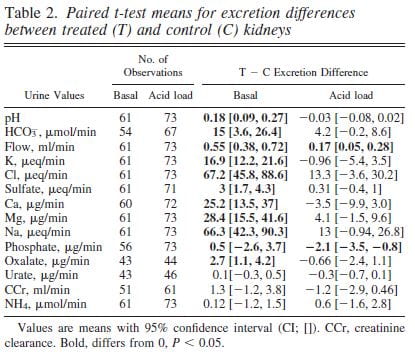 We could find these abnormalities up to 90 days after shock wave. The control kidney reduced its losses in compensation so blood remained entirely normal.
We could find these abnormalities up to 90 days after shock wave. The control kidney reduced its losses in compensation so blood remained entirely normal.
Bicarbonate Losing Raised the pH
The higher urine pH could have been due to damage of final urine acidification in the collecting ducts or to high delivery of bicarbonate from higher up in the nephron so that acid secreted lower down was neutralized by a flood of bicarbonate.
To tell these apart we gave the pigs an acid load that lowered their blood bicarbonate and therefore filtration and downstream delivery (‘Acid load’ columns). Acid load brought urine pH and almost all other measurements to equality between the shocked and control kidneys (loss of bolding).
The tissues from the pigs showed widespread injury to the thick ascending limbs, and you can read the paper for details.
SWL Can Raise Urine pH by Damaging Kidney Tubules
The meaning of the work is clear.
After shock wave treatments the treated kidney may excrete excess calcium and produce a urine of higher pH than it would otherwise do. The effects are precisely those needed to produce calcium phosphate crystals. From the bladder urine, which mixes urine from both kidneys, one could never know this was happening.
It is possible that the advent of shockwave lithotripsy has contributed to the rise in CaP stones, and I hope that further science sorts out whether this hypothesis is false or true.
High Kidney Ammonia Production
 Ammonia Production Regulates Urine pH
Ammonia Production Regulates Urine pH
Kidneys excrete acid by making ammonia that can carry acid (protons) into urine without lowering urine pH. They also excrete acid by titrating urine phosphate, which does lower urine pH. If ammonia production goes down, from kidney disease, for example, urine pH has to fall so acid can be lost on phosphate.
Ammonia production relates itself to body acid load – from food and metabolism – so that the average urine pH is just around 6. But what would happen if regulation were abnormal so more ammonia than normal was made for a given bodily acid load?
Urine pH would rise.
CaP Stone Formers Make More Ammonia
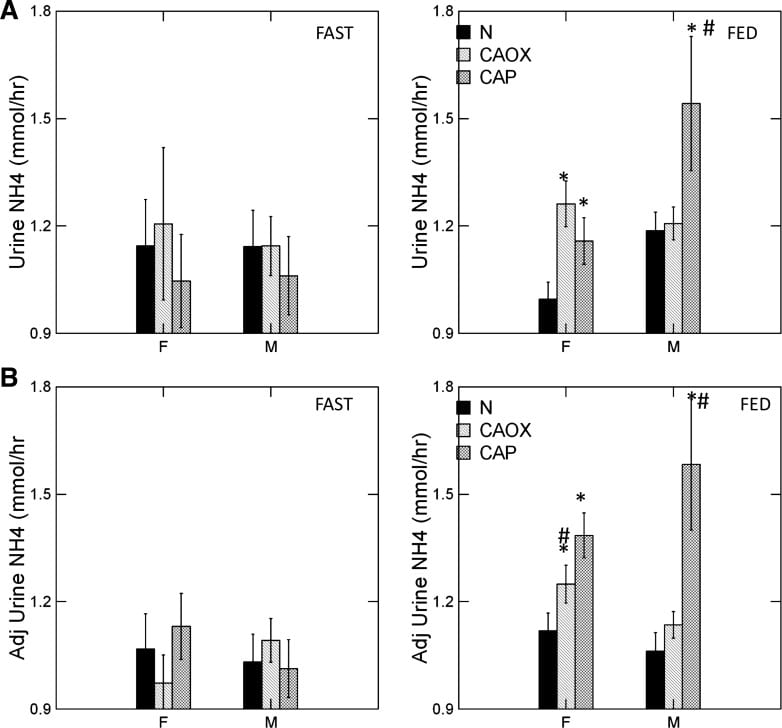
The graph shows urine ammonia excretion from normals, and CaOx and CaP stone formers studied eating the exact same diet in a research center.
Fasting, all three groups are the same (left panels). Food increased urine ammonia in male CaP patients (#). Fed, the female CaP stone formers produce more ammonia than female normals (*, top right panel). So do the female CaOx stone formers. Ammonia production is governed by body acid load, which we measure as GI anion and urine sulfate – a residue of metabolic acid production. When we adjust ammonia for acid load (lower right panel) CaP stone male and female stone formers remain high compared to same sex normals.
We suspect the high urine pH that causes CaP stones arises in part from high ammonia production, perhaps an inherited trait.
Low Urine Citrate
Many articles on this site explore the powerful effects of citrate to bind calcium and inhibit calcium crystal growth. In these closely
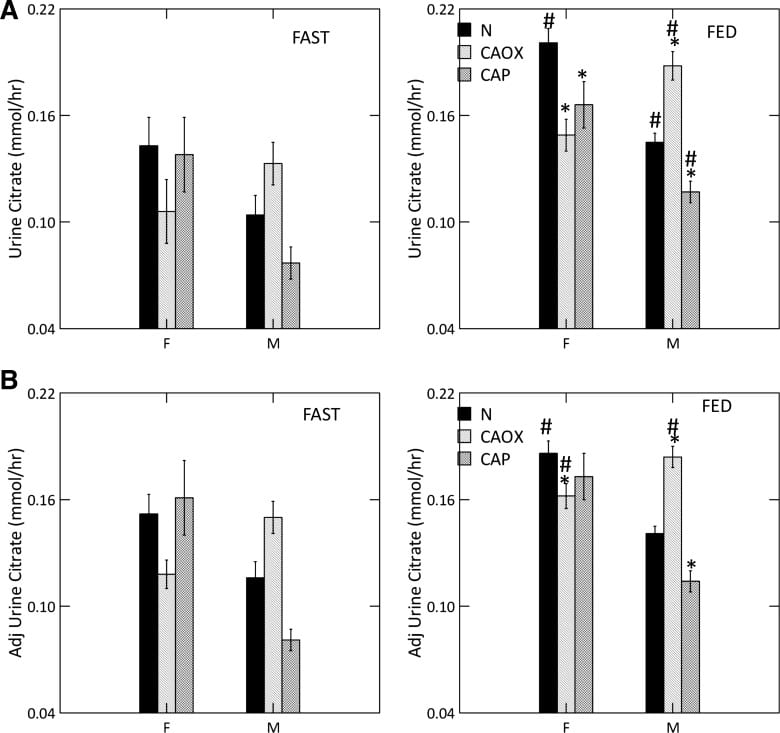
studied men and women we could document a uniquely low urine citrate of CaP stone formers vs. normal people.
Low Citrate in CaP Stone Formers
Food increased urine citrate is normal women and all three male groups (#). With food, CaP stone formers of both sexes have urine citrate excretions below their same sex normal counterparts (*, upper right panel) as did female CaOx stone formers.
As is well known, citrate is lower in normal men than women (compare black bars; we did not choose to compare the sexes statistically).
Adjusted for GI alkali and urine sulfate, (lower right panel) low citrate is concentrated among male CaP and female CaOx stone formers. Normal men remain below normal women.
Male CaOx stone formers have abnormally high urine citrate with and without adjustment for systemic acid balance.
Abnormal Kidney Cell Citrate Handling
Alkali loads, most famously potassium citrate, raise urine citrate and is an established stone prevention. Citrate also raises urine pH, because the alkali appears in urine as bicarbonate. That is why potassium citrate is not an ideal treatment against CaP stones, and why we have for decades needed a controlled trial to see if it works or makes things worse.
But here we have a high urine pH coupled with low urine citrate, in male CaP and female CaOx and CaP stone formers. That points to something wrong with kidney cell regulation.
We measured serum citrate and glomerular filtration so we could calculate the fraction of filtered citrate excreted (FE Citrate), shown in the upper right panel of the graph at left.
FE citrate is low in female CaOx and CaP stone formers and in males with CaP stones. This means that CaP stone formers are reabsorbing abnormal amounts of citrate back from the filtrate. It is used by kidney cells to produce metabolic energy.
Adjusting for GI alkali absorption (lower right panel) removes the female abnormalities but makes the male one even more prominent.
That male CaOx stone formers have abnormally high urine citrate excretion with normal FE citrate is because their serum citrate concentration is higher, a fact for which we had no explanation.
CaP Stone Formers Have Proximal Tubule Abnormalities
Citrate reabsorption and ammonia production are linked in the proximal tubules of the kidneys as part of overall kidney regulation of bodily acid base balance. In general alkali loads raise urine pH and urine citrate, and reduce ammonia production, whereas acid loads do the opposite.
Here we have high pH and high ammonia production coupled with low urine citrate, more marked in male CaP patients but detectable among the women as well.
It is as though the cells perceive a need to produce more acid excretion (ammonia) and conserve potential alkali (citrate is metabolized to bicarbonate), but there is no need. So urine pH rises and converts calcium stones to their phosphate forms. The cause(s) of these proximal tubule abnormalities are not known.
Incomplete Distal Renal Tubular Acidosis (dRTA)
A Questionable Disorder
Some have proposed that CaP stone formers have high urine pH and low citrate as part of “Incomplete renal tubular acidosis”. In proof, when given extra acid they may not reduce urine pH as low as normal people. In my primary article on dRTA, I present contemporary evidence that acid loading creates a continuous spectrum of urine pH responses, even among normal controls, so it is not a good basis for diagnosis. It seems better to say that CaP stone formers have abnormal proximal tubule functions, and make those the focus of new science.
Heterozygotes of Familial dRTA
With one exception, hereditary dRTA arises from gene disorders of the main proton transporters or of carbonic anhydrase itself, and these disorders are in general recessive. They are recessive because you need two defective genes to knock out a transporter whereas one good gene copy will maintain function.
Of course dRTA causes massive CaP stones and kidney disease. But heterozygotes – meaning one good and one defective gene – from families with dRTA if studied in detail, may not lower urine pH normally. These might be diagnosed as ‘incomplete dRTA, because in fact that is what they are.
CaP Stone Formers are Not Like Incomplete dRTA
Unlike our CaP stone formers, urine ammonia is low in dRTA and heterozygotes from families of dRTA, when compared to their acid load – urine sulfate. Urine ammonia is never high. I suspect that some CaP stone formers have high urine pH because they are indeed heterozygotes of dRTA. Low ammonia may be a way to separate them from the high ammonia of routine CaP stone formers.
Risk of Conversion From CaOx to CaP Stones
Some patients gradually increase their stone CaP percent, often enough to alter their classification to CaP stone former. The opposite, conversion from CaP to CaOx stones must be very uncommon, as we have no cases to report. We wanted to know how to detect risk of conversion.
Who We Studied
From 4767 patients in our program, we collected all CaOx stone formers who had two or more stone analyses and clinical follow up data (445 patients). From these we selected all who had a last stone CaP% at least 20% higher than that of the first stone (62 patients). Men and women were combined because we had so few cases.
Of these 62 cases, 26 had had three initial (pre-treatment) 24 hour urine studies before they passed the stone whose CaP percent was at least 20% higher than their first stone. We labeled these transformers with prior laboratory work – labs before they transformed – as ‘TP’.
For controls we chose 181 patients whose first stones were >90% CaOx and who increased their stone CaP percent <20% between the first and last stone.
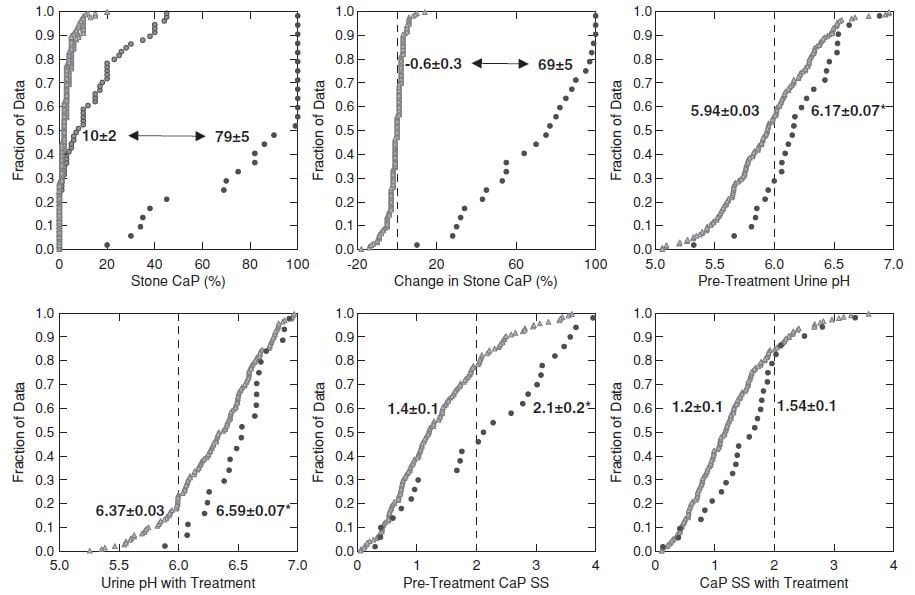
This figure shows the 26 TP cases and the 181 controls.
CaP% Was High at the beginning
Even though their initial stone CaOx percent was >50%, the 26 TP cases (black circles, upper left panel) had an average stone CaP of 10% before treatment, whereas it was much lower in the controls – who never added significant CaP.
During follow-up (upper left and middle panels) the 26 TP (black circles) increased their stone CaP markedly (average 10% to 79%, top left). The controls (gray triangles) hardly changed (-0.6% for controls, 69% change, for TP, upper middle panel).
Higher Urine pH Increased CaP SS
Urine pH and CaP SS before treatment and before conversion (upper right panel and lower left panels) and during treatment (lower middle and lower right panels) were higher in TP (black circles) than controls. CaP SS rose because we used potassium citrate as part of our treatment program.
SWL May Have Played a Role
ESWL associated with conversion: 112 of the 136 total cases with no ESWL procedures were controls, whereas only 21/41 cases with >2 ESWL were controls (X2=17, p<0.001). Furthermore, a predominance of ESWL procedures preceded the final stone (not shown here but shown in the paper), meaning ESWL could have been a causal factor.
Who is at Risk?
When stone CaP is above 10%, average 24 hour pH is as high as 6.3, or CaP supersaturation is above 2 before treatment risk of increasing stone CaP may be high. More than 2 ESWL procedures likewise. Given these risk factors in a CaOx SF perhaps one is prudent to treat as if CaP stones were already forming, so as to possibly prevent further stone CaP accumulation.
Prevention of Calcium Phosphate Stones
The objective is to lower CaP SS – reported with respect to brushite – below 1.
The main modifiable factors are urine volume, and calcium and citrate excretion. Because we cannot lower urine pH, the most crucial factor, we have to use what is left to achieve our goal. Likewise, because citrate regulation is abnormal in CaP stone formers, use of potassium citrate may not raise urine citrate so much as it raises urine pH, and therefore this otherwise valuable treatment can be ineffective.
Fluids
Relative calcium stone risk falls to 1 (no excess risk) at about 2.3 l/d of urine volume. Given the limitations of our treatments, I usually strive for 2.5 l/d spread out over the waking hours. This is an achievable goal if patients understand why it is important for their stone prevention.
Reduced Calcium Excretion
Genetic hypercalciuria is very common among calcium stone formers. If we understand that relative risk of stones rises above 1 at a urine calcium of 200 mg/d, both sexes, our goal is to reduce urine calcium to or below that point.
Reduced Diet Sodium
Multiple articles on this site detail the power of diet sodium to control urine calcium and bone calcium balance. The US diet recommendations for sodium are 100 mEq (2300 mg)/day as a tolerable upper limit, and 65 mEq (1500 mg)/day as ideal. These values concern blood pressure and bone rather than kidney stones. But if we achieve an ideal diet sodium it will lower urine calcium as well as defend blood pressure and bone mineral. So I have no reservations about promoting the ideal diet sodium, but also am prepared for compromise in this fast food dominated world.
Reduced Diet Sugar
As for diet sodium, I have written extensively about sugar as a factor that raises urine calcium, abruptly after the sugar load and with proven increase in supersaturations. Once again, US guidelines call for reducing sugar intake, and there is no benefit to anyone from eating refined sugar in any form. So I am shameless in my zeal to encourage patients to eat as little of it as possible.
Thiazide
Drugs of this class lower urine calcium about 80 to 100 mg/d below the level predicted by sodium intake. They act in part to increase proximal tubule calcium reabsorption. They are trial proven agents to reduce calcium stone recurrence. We have shown thiazide drugs lower urine pH, a possible benefit.
I have often argued to use diet as much as possible before adding thiazide to avoid drug side effects. But phosphate stones are not easy to prevent, so far as I have observed, and they damage kidney tissue. Moreover, we have no trials – none. These patients may have been in trials but are doomed to perpetual minority status unless specifically a focus.
So I am not shy about adding thiazide after perhaps only one to two efforts at diet control, should CaP supersaturation remain above 1.
Why NIH has yet to fund a calcium phosphate stone prevention trial escapes me. I cannot imagine how this has not been a priority.
Potassium Citrate
This drug will lower urine calcium below the level predicted by diet sodium intake. It may raise urine citrate excretion. But It may also raise urine pH.
Being as it is therefore able to raise or lower CaP supersaturation, I do not so much avoid using it as view it with a cold eye.
If thiazide is not attractive to a given patient I will try citrate and watch the effect on CaP supersaturation. CaP supersaturation is the final resultant of whatever changes it induces in urine calcium, pH, and citrate. If it indeed lowers CaP supersaturation, I am prone to use it but with appropriate 24 hour urine followup and an inextinguishable skepticism.
Reduced Diet Oxalate
I am aware that calcium oxalate in stones matters, and that even high phosphate stones often contain that crystal. If urine oxalate is high enough to confer risk – above 25 mg/d in both sexes – I make appropriate diet recommendations.
But patients cannot do everything all at once, so I generally put most emphasis on the calcium phosphate side. The exception is when urine oxalate is quite high – above 40 mg/d, for me – whereupon I do what I can with diet.
Monitoring Treatment
The objective is to lower CaP supersaturation below 1 in the 24 hour urine, and that is what I aim to achieve.
If fluids are enough, so be it. If not I add more treatments more or less as in the paragraphs above. Lacking trials, this is the best we can do. I watch supersaturation for calcium oxalate as a secondary endpoint, and if it is high enough to promote risk – above 3 – I attempt to lower it by reducing diet oxalate.
Monitoring is crucial. What we try to do may not be done because patients cannot or will not do it, so we have to know when to try another approach.
Put another way, for stone prevention, especially calcium phosphate stones, deliberation is reality.
I wish to thank Dr John Asplin for his careful reading of this article and suggestions for improvement.




Hi Fredric, I’m just getting to this article now. One thing I did note though at first brouse, is where you stress that duct pluggings are made of calcium phosphates, apatite and/or brushite. From what I’ve read Randall’s plaque or nephrocalcinosis is also made of hydroxyapatite, on top of which CaOx stones may form depending on whether a patient suffers from hyperoxaluria, my sister Laura does not.
Just one question for now, in your opinion, what do you think MSK tubule ductal stones are made of? If not calcium phospates (apatite/brushite)? I’ll be back! Thank you.
Hi Celia, Duct plugs all seem to be made almost completely of apatite, with brushite or calcium oxalate growing on them. A few have traces of brushite or CaOx in the plug itself, but mostly these are growing over the open end of the plug where they make new stones. MSK ductal stones are calcium oxalate and very different from plugs. They are very tiny round stones, like microscopic BBs, they do not attach to the walls of the ducts the way apatite plugs do, and they do not harm the lining cells whereas plugs destroy the lining cells. There is no inflammation around the MSK ducts. In general MSK patients form calcium oxalate stones, and have few if any tubule plugs. Warmest regards, Fred
Hi Fredric, I found many different interesting things that I’d like to comment on, I’m afraid this will be long, hope you don’t mind! 🙂
You say you put in one place all ICSF with over 50% CaOx, no cystine, uric acid or struvite (from infection). I’ve always found curious the fact that we have so few MSK members with struvite stones with bacteria and infection (only 1 that comes to mind but yet doesn’t suffer from UTIs!) yet so many with chronic UTIs and recurrent pyelonephritis and no struvite stones? (or at least their stone analysis doesn’t show struvite!).
You say that Ca stones are more a disease of men than women! that males surpass females in younger ages but by ages 30/40 the sexs are equal. I find it curious that we only have a handful of men members (perhaps 10 out of 1000?). Could this mean they also suffer like all our members but are too shy or suspicious of FB support groups?
About types of stones, I believe we have a predominence of CaOx stones in our MSK group.
Referring to CaP% stones and Lithotripsy; most of our members have had inumerable ESWL procedures for stones including my sister who was initially diagnosed with CaOx stones then at some point her stones turned to CaP.
Reference to mechanisms in Phosphate stone formation; urine suppersaturation of CaP depends on urine volume, calcium excretion, phosphate excretion, low urine citrate, high urine pH: many of our members have these same conditions!
Regarding “Physiology Post SW Kidneys” interesting the fact that all levels increased including urine pH after ESWL and that this procedure is known to affect reclamation due to tubule cell injury! (which could cause inflammation and trigger crystalization and calcifications?)
Referring to High bladder urine pH a trait in CaP stone formers; I wonder if this high pH could have anything to do with IC which so many of our MSK members suffer from?
Referring to dRTA, I believe we could have many members who suffer from this form of RTA although they have been only been diagnosed with generic RTA and no definition. Most members have low citrate, low potassium. Concerning the hereditary form of dRTA due to gene disorders, I believe many could have this form but majority of nephrologists treating MSK don’t do gene testing for a proper diagnosis? Including my sister’s, I wonder why?
I find it interesting that you suspect some CaP SF have high pH due to Heterozygotes dRTA, some due to crystals damaging kidneys AND that urine pH cannot be safely lowered because “acid loads” cause bone disease! the same bone disease already known to be caused by MSK as well. But you say “whatever the cause” the treatment remains the same “increase urine volume and lower urine calcium loss”!
Referring to the difference in plaque and nephrocalcinosis, I’ll have to get back to this topic!
Thank you so much for listening and appreciate your patience, I’m trying so hard to understand!
Dear Celia, You certainly are my most careful reader. Many shock wave treatments do indeed associate with phosphate stones, and I suspect may raise urine pH and actually cause conversion from oxalate to phosphate stones. With modern ureteroscopes the use of SWL will no doubt wane. I think the high urine pH of phosphate stone formers is from their kidneys as it is in the kidneys we find the high phosphate stones – very often. And, it is the kidneys whose tubules are plugged with phosphate crystals. Finally I think many of your members have calcium phosphate stones and that is why they often report the findings you note above. Even so, prevention is very successful, and worthwhile for them. Warmest Regards, Fred
Hi Dr. Coe,
Thank you so much for another extremely pertinent and valuable article! The section on Incomplete dRTA is particularly timely because I have been trying to research the known causes of innate high pH, but had found little. Also, my recent stones have been 80/20 CaOx/HA.
As we have discussed, my baseline supersaturation test had pH of 6.8, Ca 24 of 431, Cit 24 of 570, and SS Cap of 2.01. My doctors have done a range of blood tests including NTX, a urine culture, a CT scan with contrast, and a DEXA scan and found no recognizable systemic causes, infection, or disease other than osteopenia with the characteristic osteoporosis in one vertebra – and, of course, strong IH.
I’m hypothesizing that rather than simply IH, the ability of my kidneys to excrete acid might be somewhat impaired as a result of a genetic defect or tissue damage – and that is forcing my body to steal Ca from bones to compensate. It seems like that could potentially explain the osteopenia, hypercalciuria, high urine pH, and perhaps family history in one fell swoop.
I had $99 genetic testing for health and ancestry info done a few years ago, but unfortunately they did not appear to sequence the gene in question. However, I have several clues: My pH seems highest in first urine when I would expect it to be the lowest as a result of normal acid purging during sleep for animal protein consumed during the day. My father and I both have had chronic issues with hypercalciuria, bone loss, and unexplained chronic tight muscles. However, my citrate seems normal at 570, not low as seems to be expected for Incomplete dRTA. And as strange as it sounds, potassium citrate seemed to elevate my Ca 24 when tried (20, and 40 mEq across three SS tests.)
I’d really like to reach a diagnosis for a number of reasons even if that would have little impact on treatment today. But I’m concerned about the safety of an acid loading test – specifically whether that may send my Ca excretion, SS Cap, and stone risk through the roof for the three days of the test. I wonder if serum bicarbonate and pH (not yet tested) might yield some clues.
Question – Do you have any suggestions of possible safe ways to research/test the hypothesis of an impaired ability to excrete acid? Or maybe you have a more likely hypothesis?
Appreciate your time and anything you might offer.
Best regards, Al
Hi Al, Idiopathic hypercalciuria is a cause of bone disease, and I suspect you are an example. The elevated urine pH and 20% stone CaP put you in the higher risk category for conversion to CaP stones. I would try to use very low sodium diet – 65 mEq (1500 mg) sodium daily or less, and if that does not lower urine calcium to below 200 mg and SS CaP below 1, add a thiazide type diuretic like chlorthalidone 12.5 to 25 mg daily to the low sodium diet. OF course a urine volume above 2.5 liters daily is important. Regards, Fred Coe
Hi Dr. Coe, Thank you for your reply. I have taken your hypothesis and recommendations very seriously – I would be a fool not to. Reducing sodium has worked reliably for countless thousands of stone patients.
That said, I have been optimistically testing it very methodically. Unfortunately the data seems to consistently indicate that sodium is not my dominant factor. And logically, reducing even to zero (impossible) would not get my Ca 24 even close to 200 unless the effect were exponential. That’s a bold statement, so here’s some data from a pair of SS test showing one step of significant reduction of sodium with constant Ca intake:
Dates: 8/27/15 and 2/22/16
Reduced Na 24 from 173 to 125 mEq (-48 mEq = -28%) ,
AND Added 37.5 mg Chlorthalidone and 20 mEq Potassium citrate
AND Reduced PCR from 1.6 to 1.4
AND Increased volume from 3.41 to 3.99 liters
But all of these together only reduced Ca 24 from 378 to 347 (-8%). Even if we are extraordinarily generous and attribute 100% of the improvement to sodium reduction, it barely makes a dent.
I have also tested 65 mEq sodium intake on a short term basis. And based on your recommendation I have also reduced poultry/meat by 1/3, and also reduced other protein, as well as sugar. Every little bit is worthwhile and helps, but I have only seen more small incremental improvements in the latest tests. My doctor’s opinion is that I have been eating a very healthy, balanced diet. Of course, I will continue collecting more data through the year.
So, in light of these data, can we please expand the discussion beyond salt/protein/ thiazide? My doctor apparently only has one other patient like me, so we’re in uncharted territory. Litholink flags high pH is my single greatest risk factor in many tests. Naturally I want to learn as much about that as possible – and try to make sure it doesn’t get any worse. This leads me back to my original question (please see above.) No hurry though. This is a marathon, not a sprint, of course.
Best regards, Al
Hi Al, so with reduction of urine sodium to 125 mEq/day did not reduce urine calcium. The chlorthalidone is in a high dose as 25 mg is usually enough, and that did little. Your protein intake is still very high at a PCR of 1.4 and some studies have shown quite an effect of protein on urine calcium; are you willing to lower that? The high urine pH is relevant to calcium phosphate stones – are these your variety? Ultimately all hypercalciuric conditions can be controlled, but yours is a bit pesty, I agree. Even so with all the water I would imaging supersaturations are low, and new stones will be sparse in the interim. Regards, Fred Coe
Al, I see your comment here, not visible while editing. Your stones are CaOx with a hefty amount of phosphate so the high pH is important. I would focus on the urine calcium, however, and my suggestions are unchanged – try lowering the protein, too. PCR of 1 is good. Fred Coe
Hi Dr. Coe,
Thx. Oh yes, I am working on PCR 1.0 with lower salt, but no data yet. I have also reduced unintentional excessive Ca intake from 1300mg/day to 1000, and Ca 24 dropped from 325 to 299. Then the interim step of reducing PCR from 1.4 to 1.2 nudged it from 299 to 291.
I really don’t want to be a pest, yet I can’t escape the need to know more about my high pH. Based on our discussion from March on the FOOD page, I understand that animal and plant protein will have the same effect on Ca 24 for a normal person. The acid will just be excreted.
But my pH is not normal. If my high pH, highest in 1st AM urine, were high due to a somewhat impaired ability to excrete acid, may for example, the acid cause more Ca to be stolen from my bones to neutralize it and then that Ca be excreted? O/W it seems I should favor animal over plant protein for my allotment in order to reduce my pH and CaP SS – the opposite of a normal.
Email if easier. Best Regards, Al
Hi Al, the high pH is presently a research issue, and the initial manuscript is being written. It is too early to write about the matter, but we are working on it. Best, Fred
That’s very encouraging. Thank you! Your research helps so many people. Years ago all doctors had to offer my Dad was a low Ca diet – and as you would expect, the results were grim. Best Regards, Al
P.S I found the notes on SWL in this article very interesting too even though I’ve never had it.
What do you recommend for recurrent CaPhos stone formers with persistently alkaline urine and normal to high serum bicarbonate (not on diuretics, no emesis/eating issues) and no sig hypercalciuria? Another neph rec ammonium chloride. I have never given that in attempt lower urine pH on a chronic basis. In the very few patients I have had who have been tested for incomplete dRTA w NH4cL load they all had GI side effects.
I enjoy your very informative site immensely.
Hi, These are a major issue. Given high serum bicarbonate and no systemic issues the high pH may come from diet peculiarities that are in the normal range. As you know well, diet contains a lot of potassium anion that is metabolized to bicarbonate, and the main sources are fruits and vegetables. Some people make smoothies or other concentrates which raise urine pH a lot. Another cause is low protein diet – check the PCR. Then, there are those in whom I have not been able to find a diet cause at all but I am not convinced by the incomplete RTA proposition – I have not written on it as yet. One reason for scepticism is that I often find high or normal urine citrate in these cases. When I am stuck with high pH I work around it. How high is CaP SS? WHatever it is I lower it with water and low sodium, the latter to bring the urine calcium down as much as I can. If the SS CaP gets below 1, stones usually become inactive whatever the pH. If that is not enough I add thiazide to the low sodium high fluid regimen. That usually is enough. I know there is no trial here, but in the meantime I get good results. Warm regards, and thanks for the question. Fred
Dr. Coe,
Results just in, and before f/u conversation with urologist is this an calcium oxalate or calcium phosphate stone?
50% calcium oxalate monohydrate
10% calcium oxalate dihydrate
40% calcium phosphate (hydroxy- and caronate-apatite)
Thank you so much.
Hi Scott, strictly speaking, calcium oxalate, but with so much phosphate I would treat you as a phosphate stone former. Assuming there is no systemic disease causing your stones, this has a few subtle details. Take a look here. Regards, Fred Coe
Thanks, one more note: (Can’t see my urologist til Nov. 8). A second test result just appeared in my online record. I think it was for “residue” on the stent my urologist saw upon stent removal after implantation for 6+ weeks and also sent for analysis. It shows: 10% CaOx and 90% monohydrogen phosphate dihyrdrate…perhaps confirming your instincts to go the phosphate treatment route? That would inform new research on my part prior to seeng my urologist. Thanks again for your time…
Hi Scott, You are I think forming calcium monohydrogen phosphate – brushite – stones, a stubborn and worrisome kind. Above all you need prompt and efficient urological case and then serious prevention efforts. My best on the latter is here. Regards, Fred Coe
Hi Dr. Coe, I read your paper on patients that convert from CaOX to CaP stones over time with great interest. What I am wondering is if their baseline pH was already elevated as concluded (rather than the conversion being a result of citrate therapy), why did they initially form a majority CaOX stone? Is there an initial mechanism that inhibits CaP nucleation, that fails after passage or removal of the initial CaOX stone?
Thanks for your time, Stan
Dr. Coe,
Thank you for all of your research you have done and continue to do on, for me, what is a horrible condition. My name is Paul R. Doherty and I am an average 57 year old middle class man. College educated, hard working and have a life like most, other then many, many kidney stone episodes. I could detail all of my medical information for you, but that would take pages upon pages of information. I will share with you my most resent episodes;
9 months ago stones were removed from both kidneys in one procedure. I can, and will have all on my medical information sent to you if wanted or needed… Last January I found myself driving to the local ER again in that pain only a kidney stone patient can relate to. This incident was a difficult one as far as pain goes… I knew in my soul I was having ANOTHER stone attack, but could not understand how it was even possible, just having stones (6) removed 9 months previous from both kidneys! That procedure of removing stones from both kidneys- my choice not the doctor’s- was a horrible experience for me… I was diagnosed with stones again in both kidneys at the ER in January! Leading up to this it should be noted I was treated for two UTI by my primary care doctor. Several weeks later I had one removed from my right kidney by the scope procedure and all went well. I am scheduled to have my left side done on April 17 at MGH. This stone is NOT like any I have ever had! It is a 2.7 cm staghorn calculus in the left renal pelvis that will have to be removed by making an incision in my back and kidney. First time this has had to be done in what is my 8th or 9th stone episode. I am being treated by Dr. Brian Eisner out my MGH in Boston. I have been to the ER three times now for pain management and on a list of meds that is insane, both for pain management and other reasons… The pain with this stone has, at times had my hair on fire! I take several different pain meds daily- which I am concerned about, but need at times just to get through my day and work.
Needless to say I am at a point of hopelessness. This has affected my life in so many ways. I need some help and I am desperate. I consider myself a pretty smart and educated person, have read countless pages of information, articles, and reports on this. What I am finding in all of my research is there is no real answers why this happens to people like me and really what the proper treatment is? I am so depressed over the affects that this is having on my quality of life, work and mental health I don’t know what to do any longer. Any help or advice that you, our your peers can provide would be greatly appreciated and if any of my medical information can help you, or your peers in their research I will gladly and willingly help in any way I can.
Thank you for listening and your work.
Sincerely,
Paul R. Doherty
PRD031@AOL.COM
Hi Paul, As you know, I answered you in a personal email. Your present physicians and institution are so excellent, I am sure they will resolve your issues by finding a mode of stone prevention. Warm regards, Fred Coe
Hi Fredric, your website is a life saver to me!
I would be very glad to hear your opinion on my case. I’m 27, otherwise healthy male.
In December I had an ultrasound because had pain around gallbladder from some magnesium powder or sunflower seeds (had eye tick). Everything was fine.
For this year my sports goal was to make my abs show. So I calculated my calories and made sure I get at least 1 g /kg protein, so around 80 g. I’m pretty sure I never ate more than 200 g a day. My main source was lentils, 200 g a day (54 g protein). I ate them almost every day. I also used some complete meals, like Soylent (vegan), for a few weeks, some shakes and enjoyed peanut butter. Around 15/03 I noticed that I don’t have any erection and after drinking a shake, or a complete meal it got terribly worse. So I stopped and then noticed that went overboard and had very low fat level and was used to eating low fat. Weighed the same since mid February, that’s why got confused. Started eating also fatty foods and got back erections.
Then had kidney sand, first time I remember was 14/04 after coffee; don’t drink it usually. Went to my physician due to erection loss, he made blood and urine tests, everything was fine. On 23/04 asked for an ultrasound because had strong 2 hour characteristic pain after eating spinach. In the ultrasound there was a 3 cm black spot between the right kidney and adrenals. The physician told me to schedule an appointment with an internist and thought it was a cyst, but was not sure. Got it only on 23/05. Had more kidney stone symptoms, went to urologist, he suggested a CT. On 02/05 my first 3-5 mm stone left. Was sharp and blueish, didn’t catch it. CT didn’t see anything afterwards, wrote that this black thing is an old cyst (ha!) in the adrenal. Symptoms were also gone. Then the next week had like 3 stones in 4 days after eating lentils with buckwheat for two days in a row, the next after whole grain pasta and the last after muesli with milk. Had a panic attack for 2 days that I cannot eat anything, overdrank water. Got massive swellings in feet and hands, was afraid to go to sleep. Next day ate salt. Usually don’t salt food when I cook. Then finally got my internist appointment. He has a good ultrasound and said that that cyst is still in the kidney and is filled with stones and has calcified walls. I managed to collect my second stone, again 3-5 mm, very smooth. The internist said it’s CaP with Ca HA. 24 h urine is OK too, but after my terrible week I’m trying to eat low oxalate and make sure to eat 1000 mg calcium; I’m lactose intolerant and definitely ate too little. Now get only kidney sand symptoms and sometimes stone symptoms but only at the bladder-ureter passage. The urine flow is not straight most of the time, but sometimes it is. I hope that with enough calcium and low oxalates I’ll just lose all crystals as sand.
My town has a university hospital, should I ask for an appointment in the nephrology section there? I’m getting another ultrasound on 18/06, I hope it’ll show that I’m moving in the right direction.
Some other symptoms I had: after only eating vegan foods like lentils, beans etc for a few days have an alkaline taste in my mouth and later on joints cracking, but in a different manner than the usual tendon moving. That was also the case when I had stones falling like crazy. The taste can be offset with eating meat, pork seems to be the best. After lots of meat have the usual acidic taste. Now with the moderate diet taste seems normal, joints as well.
I get tingling in my arms or numbing when I sleep, could be just because of sports, nerve flossing seems to help.
During the panic, I noticed that I was overdrinking for at least 3 years. All socks left huge marks, waist size went from 32 to 36 although now have barely any fat, could not sit for too long, skin got burnt much easier, was sweating way too much. Try not to drink more than 3 litres now; 24 h collection was 2.7 L first day and 2.7 L second day in 10 hours. Was one of my hopefully last overdrinking days.
I would like to thank you very much. Without your blog I’m not sure what would have happened to me, I most certainly would have been way much worse off than I am now.
Hi George, I think your idea of consulting at a university is wise. You appear to be forming hydroxyapatite crystals and perhaps stones, and have crystals forming in a cyst – to me, your diet swings may be part of the problem. Things are so variable and complex, I would let a university consultant help sort them out for you. These collections of presumed calcium phosphate are not a good thing, so I would hope that with proper advice you will stone them. Regards, Fred Coe
Hello Dr. Coe ! Could you please advise as to WHAT type of diet I need to be on for stones that are : 40% calcium oxalate monohydrate, 10% calcium oxalate dihydrate and 50% calcium phosphate hydroxy-and carbonate-apatite ?!
Hi Christina, I can offer an approach to stone prevention. Here is my best article on this subject. The kidney stone diet is not one thing, but a group of changes toward what is advised for all Americans. Take a look. Regards, Fred Coe
HI Dr Coe… I have been a stone former for many years. Most recently the stones are now showing up as brushite. Given that Calcium carbinate can precipitate into calcium phosphate…
https://link.springer.com/article/10.2478/s11532-009-0063-6
And one of my favorite medicines for my acid stomach is pepcid – which has calcium carbinate as one of it’s active ingredients and My intake of pepcid has grown as I have gotten older….
Is there a relationship between brushite stone formation and the use of calcium cabinate as an antiacid?
If i stop taking pecid – will my stone formation go down or will I just have calcium oxalate stones instead of calcium monohydrogen phospate dihydrate stones?
Or the fun question… since they are not oxalate stones – can I eat chocolate.. Cheers
Hi Michael, Alkali calcium loads could certainly help produce brushite stones. Pepcid alone would not do so. You need a full evaluation for the cause of all this – probably high urine calcium – and definitive treatment. Brushite stones are nasty. Here is a pretty good plan for your treatment. Regards, Fred Coe
Hi Dr. Coe, I’am a 47 years old Woman, I’ve been having kidney stones for over 7 years, at least once a year I get them removed. The composition of the last stones removed was 98% of Calcium Phosphate. Any advice please.
Hi Concetta, Calcium phosphate stones are important to prevent. You need to get fully evaluated and treatment based on what is found. Here is a good place to start. Regards, Fred Coe
Hi Dr. Coe,
I just sent you a question about my calcium phosphate kidney stones.
I said they were 7 cm. Correction,
7 mm. Other than that, I saw after I sent it that my smart phone had done it’s own strange editing, but I think it is still decipherable.
Anne
Hi Anna, I am sorry to be a bit late; we have had some trouble with the comments reply pages this past week or so. I believe I answered you as best I can. Regards, Fred
Why do I not see my comment posted? Did I miss something?
Anne Danahy
Hi Anna, Once again, I am sorry about the timing. I did answer you. Fred
Hi! thank-you for all the amazing information! I have been passing kidney stones for the past 15 years. For a long time it was just 1 every couple years, but in the past couple years it has been picking up pace. Now it is at the point where I am passing them monthly. I passed 2 already this month and have another stubborn one trying to pass now again already. I just turned in the 2 I passed this month and got my results today: 40% calcium phosphate (apatite), 30% calcium oxalate monohydrate, and 30% calcium oxalate dihydrate. Waiting for results from my 24 hour urine collection still but my blood work they took when i turned in my stones this week looked normal.
Potassium, S 4.1 mmol/L
Chloride, S 99 mmol/L
Calcium 9.1 mg/dL
Sodium, S 140 mmol/L
Bicarbonate, S 26 mmol/L
Anion Gap 15
Any input from this info while I am impatiently awaiting my appointment with the specialist? I had a couple tiny blood clots in my urine this month too which I have never seen before. Is this something you have seen before? and everytime I end up in the ER I have very low elevated WBC count which they bring up every time but it seems too low for infection. And last of all, I was curious if any of these kidney disorders you have mentioned had the symptom of a face rash? maybe its not related but it is another weird symptom i have been getting the past months too. it is a defined red rash on cheeks and nose and sometimes goes up on forehead and it burns! It comes on suddenly for an hour or so and then disappears. Again maybe not related but just with the increase in urinary/kidney issues I was thinking maybe it was all tied together. I live in a smaller town and we don’t have the best doctors all the time so it is all making me nervous. Any input would be appreciated. Thank-you!
Ok now got my 24hr urine results back and they seemed really bad. i dont get why they are so off but my blood levels are normal. For example my urine calcium was over 500! Also elevated was my Chloride (314 mg), Uric Acid (1200 mg), Creatinine (2415 mg), Urea Nitrogen (21.4 g), Sodium (282 mg), Potassium (84 mg), protein catabolic rate (159 g). and Ammonium (only by a couple mg). There is also a list of random crystal – calcium oxolate crystal, brushite crystal, hydroxyapatite crystal, uric acid crystal, sodium urate crystal. These results showed up on my online patient account and said they were computer generated, and now since its the weekend I have to wait to until atleast monday to talk to the doctor. Mixed with how horrible i am already feeling, it is making my anxiety go through the roof. I would appreciate any feedback. Thank-you!!
Hi Katie, I guess the 24 hour urine results are indeed helpful. Your urine calcium is indeed high, and this may be in part from your very high sodium intake, but also your collection seems out of range. Urine creatinine arises from muscle, and most women do not have 2415 mg a day – usually about 1/2 of that. Perhaps this was a 48 hour collection? Even if I correct your urine calcium by dividing through by your creatinine, it is very high, about 200 mg calcium/gm urine creatinine, and so I suspect you have idiopathic hypercalciuria (your serum calcium was normal, 9.1). You do not give your urine volume, oxalate, or citrate, all important, so I cannot say much more. But I am sure the hypercalciuria can be easily corrected. Regards, Fred Coe
Hi- I was just reading through this and am not a doctor, just a patient. The rash you describe sounds a lot like a butterfly rash of lupus. You may already know or have eliminated that as a possibility but just in case, I wanted to share. Hope things get better for you. Many blessings.
Hi Katie, without the 24 hour urines one cannot say or do much. Are you taking any medications? Some promote stones. Given the increasing pace, has anything changed in your life? The rash is not so obvious a clue, nor the white blood cell count. If you like, post the 24 hour urine results – I bet they help. Regards, Fred Coe
Hi Dr. Coe,
I am a 60 year old female who has been having kidney stones for the last 10 years. My medication list is as follows: flecainide for A-fib.,
gabapentin for neuropathy,
cholestyramine for irritable bowel syndrome,
fosamax, along with a calcium supplement and vitamin D for osteoporosis.
My blood work is all in the normal range.
The results from my 24 hour urine test are as follows:
calcium oxalate urine-: 1.52 Delta G
Calcium Hydrogen Phosphate dihydrate: 0.34 Delta G
Hydroxyapatite : 6.15 Delta G
Urate Urine: -5.14 Delta G
Sodium Urate: 0.10 Delta G
Sodium: 103 mmol
Potassium: 27 mmol
Calcium:189 mg
Magnesium: 63 mg
Chloride: 76 mmol
Phosphate: 399 mg
Sulfate: 8 mmol
Citrate: 611 mg
Oxalate: 0.23 mmol
ph urine: 6.8
uric acid: 378 mg
creatinine: 1050 mg
Osmolality: 218 mOsm/kg
Ammonium: 25 mmol
urea nitrogen: 4.9 g
protein catabolic rate: 56 g
My urologist has told me to drink 2 quarts of lemonade a day, increase fluids and eat a low sodium diet, which I have been doing , but I am still getting stones. I was wondering if you had other ideas of what I can do to aide in the prevention of these stones.
Thanks so much for your time,
Brenda
Hi Brenda, You do not mention the type of stone but the high pH suggests calcium phosphate. Your urine has some odd features in that your sulfate is low compared to your urine ammonia, this suggests potassium depletion, or some odd diet patterns. You do not mention the volume of the 24 hour urine, was it in fact 2 liters as you suggest? With a lot of gaps, I cannot be much help, but perhaps you could fill in the volume and stone type. Regards, Fred Coe
I had a GSW to abdomen with a partial whipple, partial R Nephrectomy, and had some small intestine removed. I actually have hypoparathyroidism; just under the low mark by several points. I have had kidney stones for over 20years and am now suffering CKD. Creatine 1.5 and GFR fluctuates in the 50’s. I am 48. I need a really good doctor to help me figure this out. So far, all I can manage to get from my doctors, and I have seen many, is the same thing…treat me then send me home. My stones have gradually increased from Calcium Oxalate to 50/50 oxalate/phosphate. I am in Florida near Tampa. I have many stones in the kidneys and they are difficult to treat. Horseshoe kidney makes things a bit more complicated; at least for some doctors. I even had one send me home with a referral from ER when I had a complete obstruction with a rising creatine. He didn’t want to touch me. I am at a loss and very frustrated. I would even travel to Chicago or anywhere to receive the right treatment.
Many thanks,
Gerald
Hi Gerald, You indeed have a very complex problem. I know of no facilities in Tampa, but there is a fine kidney stone group at the university in Gainesville. Chicago seems harder to get to but if you wish to come up here we can arrange for the consultation you need. Let me know what would be easiest for you. Regards, Fred Coe
I am going to have another 24hr urine and all relevant bloodwork done; as well as a ct. May I send the results to you. Perhaps I can arrange with your office for a consult. Having had the opportunity to see the results of the tests and records, I am hoping you can shed some light on this. I am scheduling soon to have my kidney stones dusted and kidneys cleaned out. I just do not want to do so and not have a clear plan for future prevention. I have to save my kidney function
Hi Gerald, Medicine is a very complicated space. On a site like this I can offer information, even up to specific ideas for patients to think about and bring to their physicians. But if it comes to a review of medical records and tests for the purpose of practicing medicine, that is structured. Presently, my institution permits me to provide care for patients who come to see me. Telemedicine is not as yet available as a member of the UC medical staff and as a professor of medicine. If your physician wants me to review your records and report to him/her about my opinion, we can arrange that. Of course you would receive whatever is sent. Absent our meeting I cannot review your records and tell you how I think you need to be treated, that is improper practice of medicine. Please let me know what you might like within this framework. Regards, Fred Coe
I would gladly make an office visit with you if you can provide whom to contact.
Hi Gerald, That is the easiest way to do it. My secretary is Karen Niswander, 773 702 1475. She can make all arrangements. Regards, Fred Coe
These articles are so very helpful. I am a 35 year old female with 15+ years kidney complications, urethral pain, flank pain, stones, and hematuria (consistent 2015-present) without identifiable cause. CKD Stage 3 at 50 GFR diagnosed at age 28 that I managed to improve now testing between 60-78 GFR the past year. Age 27 diagnosed with Dysautonomia including Chronic Migraine, Sensory Disturbances, Postural Orthostatic Tachycardia Syndrome and Suspected Mast Cell Activation Syndrome (MCAS). MCAS presentation includes falres of wide spread itching skin rash inconsistent with urticaria pigmentosa, bilateral eye watering, swelling, abdominal distention, GERD/SERD, Elevated PGF2a and cyclic vomiting. Cystocopy unremarkable, Endoscopy and Colonoscopy biopsy revelaled borderline (20-25 Mast Cells per/HPF) Hiatal Hernia, otherwise unremarkable. Highly sensitive to most medications and food additives but no identifiable allergy.
There is speculation kidney disease is an underlying condition leading to Autonomic Dysfunction/Dysautonomia and MCAS symptoms closely resemble symptoms of poor kidney filtration. Family history of Lupus and X-Linked Alport Syndrome (Confirmed I do not have the Alports mutation)
Below are my 24-Hr results which I notice are elevated for Brushite but I’ve not found the reference level in my results on the graphs provided in the articles I’ve read so far and am not sure what to make of this information. Unfortunately I cannot see Nephrology until September. To note the say after providing my 24-hr urine sample I broke out in widespread spots 3″ x 3″ +/- itchy and felt as though my entire body was sunburned. Very curious if Brushite or it’s cause may also explain the bigger picture:
Component Your value Standard range
SPECIMEN VOLUME 24 HR URINE 1.15 L/day >2.00 L/day
PH, 24HR URINE 6.7 5.5 – 7.0
CALCIUM RATE, 24 HR URINE 510 mg/day <250 mg/day
OXALATE RATE, 24 HR URINE 25 mg/day <45 mg/day
URIC ACID RATE, 24 HR URINE 726 mg/day 320 mg/day
SODIUM RATE, 24 HR URINE 188 mEq/day <200 mEq/day
SULFATE RATE, 24HR URINE 16 <30
PHOSPHATE RATE, 24 HR URINE 867 mg/day 60 mg/day
24HR URINE AMMONIA RATE (UMOL/24HR) 24 mEq/day 14 – 62 mEq/day
POTASSIUM, 24 HR URINE 50 mEq/day 19 – 135 mEq/day
CREATININE RATE, 24 HR URINE 1479 mg/day 600 – 1800 mg/day
CALCIUM OXALATE INDEX, 24HR URINE 3.17 <2.00
BRUSHITE RELATIVE SUPERSATURATION 12.89 <2.00
SODIUM URATE RELATIVE SUPERSATURATION 7.97 <2.00
STRUVITE RELATIVE SUPERSATURATION 20.04 <75.00
URIC ACID RELATIVE SUPERSATURATION 0.60 <2.00
CRYOGLOBULIN, , QUALITATIVE NEGATIVE
RHEUMATOID FACTOR <10 IU/mL <=14 IU/mL
C3 173 mg/dL 90 – 180 mg/dL
C4 36 mg/dL 10 – 40 mg/dL
PROTEIN, URINE, QN 10 mg/dL <=11 mg/dL
CREATININE, URINE 131 mg/dL mg/dL
PROTEIN/CREATININE, URINE 0.08 <=0.19
GLUCOSE, UA <30 (Neg) mg/dL Negative mg/dL
KETONES, UA <10 (Neg) mg/dL Negative mg/dL
SPECIFIC GRAVITY, UA 1.015 1.005 – 1.030
UA HGB 1.00 (3+) mg/dL Hb Negative mg/dL Hb
PH, UA 6.5 5.0 – 8.0
PROTEIN, UA <10 (Neg) mg/dL <30 (1+) mg/dL
NITRITE, UA Negative Negative
LEUKOCYTE ESTERASE, UA Negative Negative
UROBILINOGEN, UA, QL 0.2 (Neg) mg/dL Negative mg/dL
BILIRUBIN, UA <0.5 (Neg) mg/dL Negative mg/dL
Hi Nichole, Your stones surely arise from the extremely high urine calcium level of 510 mg/day. The urine is alkaline with pH of 6.7 and that is why your stones are brushite – calcium monohydrogen phosphate. You have a very high sodium intake of 188 mEq/d and scanty urine volume of 1.15 liter/day. So you need treatment aimed at much higher urine volume, low diet sodium, and probably a medication to lower urine calcium. Here is a good article close to what you have. I urge you speak with your physicians about the possibility of pursuing treatment as prevention seems obvious and very likely. Regards, Fred Coe
Hi, had several small stones removed with Lithotripsy, then 16 months later had enormous stone form … 27 mm in same kidney, it is calcium phosphate. I agree with your findings.
Hi Lanie, Be sure you have full evaluation for cause with 24 hour urine and blood testing and go on a proper regimen for protection against more stones. Phosphate stones can form and grow rapidly and are often caused by high urine calcium and pH. The former is not hard to treat, the latter is not directly treatable. Regards, Fred Coe
I’m 34 yr old female and had my first kidney stone with a 97%CaP content
Waiting for the urinalysis
And I have no other symptoms – where can I find details about high % stone formation?
Hi Waheeda, This article speaks precisely about you. Evaluation and treatment are in the article and very important for you to follow. Regards, Fred Coe
I have had four stones all large requiring surgical intervention. The earlier ones were calcium oxilate and the last 1.2 cm stones was 100% brushite. My urine calcium is 350, urine volume 2.7 liters, citrate 400, SSCap is 2.1, PH 6.8. I am wondering what I should be on: 1. Chlorthalidone 12.5mg/day and try to not supplement with potassium citrate since my super saturation of calcium phosphate and PH are rather high. However, it will not reduce calcium as much or 2. High dose of chlorthalidone at 25mg a day plus potassium citrate (since my potassium will surely go down).
Hi Traci, Brushite stones are always a problem, often large, numerous, and hard to disrupt with with lasers or shock waves. The treatment approach to your high urine calcium begins with sodium, which often solves the problems you mention. You want to lower diet sodium to below 1500 mg/d if you can, and see how far down that takes your urine calcium. Then you add chlorthalidone on to the diet in the lowest dose that is workable. Here is a good review of the process of combining diet with meds effectively. Regards, Fred Coe
I had my first kidney stone aged 59. It comprised 50% calcium oxalate and 50% calcium phosphate. Prior to this I had been suffering from persistent heartburn. My GP prescribed taking Gaviscon Advance four times daily for a few weeks which I did. Could this be the cause of this stone?
Hi Colette, Gaviscon is aluminum hydroxide and magnesium carbonate, so it will make your urine more alkaline and perhaps foster the phosphate part of your stone, but the calcium oxalate is not from the drug. Also you took it for only a month. You have stones in mid life and it is probably something else. Here is a good source about this very subject. Regards, Fred Coe
Hi Fred,
I recently had a stone analyzed that was Carbonate Apatite (Dahllite) 90% and Calcium Oxalate Dihydrate (Weddellite) 10%. I am still unclear what this means.
Hi SC, It means you produce calcium oxalate stones richly admixed with calcium phosphate. The article you write on is pertinent to your situation as urine pH will be high and treatment has some special features as in the article. Regards, Fred Coe
I had kidney stones that were 100% calcium phosphate. My doctor is saying it’s rare and he’s not sure how to help me with these. Is there any treatment?
Hi Alyson, They are not uncommon in women, and need the same 24 hour and serum evaluation as for calcium oxalate stones, and prevention as well. Perhaps your physicians see fewer kidney stone patients than I do, a reasonable situation as I specialize in them, but I am sure they can and will see to prevention for you. Regards, Fred Coe
I am a calcium phosphate former & I never stop forming them. I pass stones / sediment every 3-4 weeks. I was diagnosed with a “leaky kidney” & put on a diuretic, that I am unable to take because of my bodies reaction to sunlight while on the medication. Are there other solutions? Any nutritional advice?
Hi Sean, I imagine you have genetic hypercalciuria, and diet may suffice. Take a look at the article on that topic. If you reduce diet sodium enough you might need no drug or only a tiny dose. IDIOPATHIC HYPERCALCIURIA (IH)Regards, Fred Coe
I have my 70% calcium phosphate stone and 30% calcium oxalate on stone analysis. I’m taking potassium citrate but it promotes high alkaline environment suitable for phosphate stones to strive in . I’m confused , should i continue with potassium citrate or not ?
Hi Khansa, An astute remark. Is potassium citrate actually appropriate for your situation. Be sure that you have been fully evaluated using 24 hour urine studies and blood as well. Usually phosphate stone formers have genetically high urine calcium excretion and treatment is other than potassium citrate. Regards, Fred Coe
Yes I’ve done my 24 hour urine analysis and had high calcium in urine with mild proteinuria and low citrate . I’ve raised parathyroid hormones too but no adenoma found on parathyroid scintigraphy and ultrasound . Dr just prescribed me calcium and vitamin D supplements to lower it . Please mention in comment the treatment plan for such case . I’m mistreated and misdiagnosed by many doctors wrong . Thanks for your informative article .
Hi Khansa, Low citrate high calcium and – you did not mention it – high urine ammonia are what we find in CaP stone formers. The proteinuria sounds like kidney problems your physician might want to consider. High PTH with normal serum calcium may be secondary, perhaps to even slight reduction of kidney function or perhaps low vitamin D. Again, your physicians need to help with this. PT imaging is usually not very informative in the absence of high serum calcium – I presume your serum calcium is normal. If it is high, that is an entirely different matter. Regards, Fred Coe
Dr. Coe,
Love your work, a great source for me being Calcium Phosphate stone former. I’ve worked hard using your site and think I have accomplished some work and very compliant to make any changes needed. Drink 10-12 liquids daily, mostly all water( 12 oz coffee and milk other) and limit diet sodium and here are my 24 hour urine changes in last year.
2019 = Cal 324, ox 23, uric acid 513, citrate 350, PH 7, volume 2.73, sodium 95, phosphorus 871, Mag 87, Ca Ox Sat 1.33,
Brushite Sat 4.39, Sodium Urate Sat .62, uro potassium 48, uro creat 1054
2020 = Cal 237, ox 35, uric acid 461, citrate 325, PH 7, volume 3.72, sodium 73, phosphorus 915, Mag 85, Ca Ox Sat 1.22,
Brushite Sat 2.38, Sodium Urate Sat .25, uro potassium 41, uro creat 977
I get all my calcium from diet, mostly dairy and my next step was to increase that to get to 1000-1200 mg day. Leary on calcium supplements but will take them if you advised to make up the difference. No problems eating dairy and like.
Other questions, is there anything I can do to get my PH down on my own such as cranberry juice daily, Vit C, or other? I know increasing urine citrate helps with crystallization for stone prevention but was thinking it wouldn’t be advised for me to drink lemon juice because it would increase my PH or does the citrate outweigh the PH in stone formation? What is a good 24 hours urine citrate number to have? Uro Phosphorus number? Also am I okay not to worry too much about oxalate foods on a whole, I eat pretty healthy and have wheat in my diet daily from healthy cereal and bread and my biggest oxalate would be 2 measured TBS of peanut butter a day that I love and use for some protein. Is that an issue? Working hard on decreasing sugars since I use to eat too much with snack foods and chocolate. Eat lots of fruit and veggies a day and proteins are from eggs, tuna, dairy (milk, cheese, yogurt) mostly with some turkey lunch meat and very little red meats on occasion only. I find it hard to keep the protein in range for a 120 lb 50 year old woman when I don’t eat much meat! If I go by your website I’m getting that I should only have total protein under 50g a day, I tend to have in the 70’s or 80’s with my diet and little meat. Been tested for primary hyperparathyroidism and endo doc says I don’t have or any other metabolic reason for my stones. I have been studying this since I developed stones in 2018 with new R stone 2019 US and now new L stone 2020 US, one ureteral stone removed 2019 that was 70% phosphate(hydroxy and carbonate apatite) and 30% oxalate. I need guidance on what to do next since urologists locally don’t have time to educate which I understand with their schedules. He did not believe I needed meds because of their side effects and the potassium citrate raising PH.
Thank you for your valuable time,
Carol
Hi Carol, Even with a lowered urine sodium urine calcium is generous and SS for brushite – calcium phosphate – is above 1. If you are forming new stones, then either you may have to lower diet sodium even further or use a thiazide diuretic along with the diet. As for diet calcium, it is raised to lower urine oxalate but your SS CaOx is very low so a normal calcium intake in the range of 800-1000 mg from food is reasonable. The problem here is that I am not in a position to really direct your care – only your real physicians can do this, so whatever I say needs to be alright with them. If stones continue, you might want to obtain a separate consultation, which can direct your care. Regards, Fred Coe
Dr Coe,
In your years of research have you found any info about long term use of oral contraceptives (33 years long) on stone formation or affect on 24 hour urine values?
Why doesn’t my 24 hour urine have urea nitrogen, chloride, sulfate, ammonium, and protein catabolic rate? Is this a separate urine test and how should that be ordered? I’ve seen these in reading articles from other patients.
I don’t understand my bone density from 2 years ago at age 49. AP Spine T score -1.6 Z score -1.2 Total left dual femur T score -1.4 Z score -1.0 Total right dual femur T score -1.8 Z score -1.3 Left Forearm T Score -1.0 Z score -1.0. Three different providers told me three different things. Is this normal?
Thanks and learned so much from you,
Lisa
Hi Lisa, About stones, I do not believe OCT promotes them. I suspect if estrogen use extends into menopause urine calcium will remain lower as bone mineral is better preserved. Your 24 hour urine is not from a kidney stone lab vendor as urea chloride sulfate and ammonia are needed to calculate supersaturation. Your physician may have ordered from a routine lab. I prefer Litholink as a vendor – no financial interest. At age 49 spine t = -1.6 femur t = -1.4 forearm -1; this is all from one test and one provider, just different parts of you. The T score measures deviation from peak bone mass for sex in SD units, so -1 means your value is one standard deviation below the mean for normal young women – about 67% low, a mild fracture risk. In your spine and femur risk is a bit higher than in your forearm; the first two have a higher fraction of trabecular bone the arm is cortical – outer shell of bone. Given these modest values just be sure you get enough vitamin D and diet calcium, weight bearing exercise. Regards, Fred Coe
Good morning Dr. Coe,
I have had 2 very large stones in my right kidney in the last 2 years (first was 11.65mm and second was 9.46mm) they were both broke up with Lithotripsy and after many passing of stones 4mm and below I was told I have a lot of “gravel in the bottom of my kidneys. I had a 24hr urine culture for stones and found out I have Hypercalciuria, supersaturation index – Brushite (Ca phosphate) .
my 24 hour StoneRisk Urinalyses profile levels we as follows:
Total urine volume – 2.92
pH Urine – 6.8
Calcium – 325
Oxalate – 29
Uric acid – 517
Citric Acid – 660
Sodium – 162
Sulfate – 8
Phosphorus – 940
Magnesium – 90
Ammonia – 29
Potassium – 43
Creatinine – 1266
Calcium oxalate – 1.29
Brushite – 3.14
Sodium urate – 0.89
Struvite – 2.12
Uric Acid – 0.14
This all stated after I turned 40 and had a life altering change due to a Trauma which caused PTSD and Severe Anxiety. Physically I lost 60lbs and started working out daily after being over weight for most of my life. Since the first stone I have been Hyperaware of my diet and water intake. I have been on the gallon challenge for over a year. I try to drink a gallon of water spaced out from 7am to 9pm daily. I have just learned that I am Hypercalciuric with high Brushite. I have already changed my diet to reduce my intake of beans and nuts however I do not eliminate leafy greens just try not to intake a full serving.
Do you know of anything I can do to help prevent or limit the forming of the large stone?
Hi Alicia, You do not say what your stones are made of, but I presume calcium phosphate from the article you have posted on. In that article is all I have to say about treatment for reduction of new calcium phosphate stones. Here is a more general article on stone prevention that may help more – essentially with high urine calcium and pH, which you have – treatments begin with diet and move on to meds as noted. If you are still perhaps a bit confused, here is my best introduction to how a stone former might want to proceed. Regards, Fred Coe
Dr. Coe, I’ve seen ionized calcium test mentioned, should all stone formers have that tested and what benefit is ionized over a regular calcium blood test? Also since my lab does not show on my 24 hour urine PCR, ammonia, sulfate, chloride, and urea nitrogen can they be figured out from the supersaturation values that are listed on my 24 hour urine? I can only use this lab because of insurance and Quest but I’ve read that Quest doesn’t show many of the values either. As long as the supersaturations are listed along with other routine values like calcium, vol, ox, citrate, etc is it okay to not have those others listed above? Thank you for your valuable time.
Hi Lisa, Ionized serum calcium is sometimes used in diagnosis of primary hyperparathyroidism.It adds little. The article discussed the crucial problems of fasting morning samples and a need to make many measurements if the values seem high. As for QUEST, their stone product is mediocre, and there is no way to get the missing information. Lacking them, at least try to keep total protein intake to about 1 gm/kg body weight/day, which is what PCR tells us. I am not sure about the SS values either, but you want them as low as possible. Regards, Fred Coe
Hallo Dr. Coe
I see only few patients with recurrent CaP (mostly apatite) kidney stones in our clinic.
If those patients have nephrocalcinosis additionally,we search for hereditary diseases of calcium and phosphate metabolism.
But, in the literature there is sparse information on the stone composition in such diseases. So it is not clear if those patients have CaOx or CaP stones (or both)
Do you have information on stone composition in hereditary hypercalciuric/hyperphosphaturic diseases?
Do you think it makes sense to screen for hereditary diseases of CaP metabolism in patients with recurrent CaP stones and nephrocalcinosis?
Kind regards
Christoph
Hi Dr Schwartz, Phosphate stone formers form tubule plugs that can mount up to look like nephrocalcinosis on CT. Images during URS are the most reliable, for me, in assessing stones vs plugging. Our most recent – small samples, immense detail – of CaP stone formers show what appears to be a dysregulation of renal NH4 production with an associated increase of citrate reabsorption – higher urine pH lower citrate. I suspect this is heritable. There is a sex difference as well, men CaP SF having the more marked NH4 disorder. All of the patients we have studied in detail have idiopathic hypercalciuria, which is genetic and polygenic enough no one has as yet even found workable clinical gene markers. As for the less common single gene diseases, in my own work I rarely find them. I do family history in everyone and in a few instances have uncovered forms of dRTA but our clinic does not have routine genetic screening. Best, Fred
Dr. Coe,
Given that potassium can have an effect on glutamine metabolism, whereby potassium depletion augments its metabolism to ammonium and bicarbonate, I wonder whether the alalkaluria, hypocitraturia, and increased urine ammonium could be a response to real or “inappropriate sensed” potassium deficiency? And I say potassium deficiency as opposed to hypokalemia as we know that serum potassium measurements are not a true reflection of total potassium content. Thanks.
Hi Steve, You are a mind reader – I have had the same thought. I wonder if KCl would lower HH4 production and urine pH. Fred
Dr. Coe,
1) My 24 hour urine does not show Ammonium. Can that be ordered as a separate urine test?
2) What is the test to measure GI Anion Gap, is that the same blood test that is in the routine chemistry with the result range of about 4 mEq/L – 14 mEq/L?
3) In regards to Urine Anion Gap, is that suppose to be in a 24 hour urine or is that a separate urine test or called something different?
4) Lastly, How do you measure Bicarbonate? I see that a lot in articles, is this the same as CO2 in the complete blood count?
Thank you for your time.
Hi Carol, It is always best to get 24 hour urines for kidney stones from a vendor that specializes in it. Litholink is the best of breed, but most large labs have kidney stone 24 hour urine packages that include it. The GI anion is calculated: urine sodium + potassium + 2*calcium +2* magnesium -(1.8* urine phosphate + urine chloride). Calcium, magnesium, and phosphate have to be calculated in millimoles, the others are already reported that way. The factors of 2 and 1.8 convert to their charged form. No present vendors calculate this – it is just emerging into clinical practice, mainly because of our publications. Serum TCO2 is measured in blood and is presented in all routine blood panels – it is CO2 in the label. Regards, Fred Coe
Dear Dr. Coe, In 2018 I had cystolitholapaxy and in 2019 had 2 of the same procedure. In 2020 I had an open procedure to remove 1.5 lbs of bladder stones and for a simple prostatectomy to core out a 170 gm prostate. Three months later (Jan. 2021) I had another cystolitholapaxy to remove a small stone fragment that was left in a bladder diverticuli. This is was suppose to be the ‘final’ stone related event. Approximate 2 weeks ago I passed two small grainy stones in two separate events. The initial analysis of the stones in 2018 were “80% calcium phosphate (brushite) and 20% calcium phosphate (apatite)”. The current urologist has recommended another cystoscopy to evaluate for any stone recurrence. I have not been on Thiazide but have in the past, on the recommendation of the previous surgeon taken potassium citrate (800 mg, BID). I am inquiring as to find out if there are any dietary recommendations or clinical suggestions for future testing, evaluations, etc. My sodium intake is very low but my sugar intake in moderate. I do not smoke (never have), do not drink (have never had a taste for ETOH), age = 68, height = 6′, weight = 167. Do not eat red meat, drink green tea regularly. I “Thank you” for your time and would be happy to pay for your comments. John Espy…
Hi John, Brushite is an uncommon stone type and often recurrent. Most people have high urine calcium and pH>6.3 on a 24 hour basis. Brushite itself is a probable starting crystal for all calcium stones. I would take a careful look at the 24 hour urine studies and blood to be sure all causes of stone were being controlled via diet and meds – of especial importance brushite supersaturation below 1. Potassium citrate raises urine pH and may or may not be ideal for brushite stones, no trial data exist. Regards, Fred Coe
Dear Dr. Coe, If I may I would like to add one aspect that I left out. Do to the number of the bladder stones and the time they were in my bladder I have also developed numerous bladder diverticuli. Part of the current thinking is that even though I have had a simple prostatectomy that I am still not fully emptying my bladder and therefore urine is collecting in the pockets and producing stones. Again, I thank you and appreciate the value of your time. My best, John
Thank you again…
May I ask if you see the bladder diverticuli as being problematic with regard to my previous posts. Thank you, John Espy
Ho John, Diverticulae can harbor crystals till they grow to worrisome size that normally are swept away as particles too small to recognize. Regards, Fred Coe
Thank you again for your willingness to take the time to answer questions regarding these difficult medical situations. Please forgive my bad manners in taking so long to say, “Thank you…”
I just received test results of:
10% calcium oxalate (monohydrate and dihydrate), and
90% calcium phosphate (hydroxy- and carbonate- apatite).
INTERPRETIVE INFORMATION: Calculi (Stone) analysis
I am trying to make sense of this before I return to the doctor tomorrow. Any help would be greatly appreciated!
Hi Ryan, You are writing on the article that is about you. Higher urine pH, almost always high urine calcium, lowish urine citrate. You need complete 24 hour and serum testing and treatment of abnormalities. Phoshate stones can grow faster and larger than oxalate stones, so prevention is a lot more crucial. Regards, Fred Coe
Dear Dr Coe,
I wonder what is your plan of management for patients with hypocitraturia and Ca phosphate stones secondary to treatment with carbonic anhydrase inhibitors such as topiramate and Zonisamide. Do you tend to treat them with potassium citrate? Dose? urine pH target? how effective it could be? Many thanks
Hi Dr Zouwail, I am afraid they are intractable, because they inhibit CA. The bicarbonate distal nephron delivery is perpetual because either the kidney replenishes bicarbonate losses via acid excretion, or we do with alkali supplements, so tubule fluid and urine pH are too high. Likewise citrate is a problem – I do not think the problem is systemic acidosis as citrate almost never responds to systemic alkali normally. I think it is the inhibition of NHE3 function from CA inhibition, and some imbalance of chloride to bicarbonate limiting SLC26a6 which links to the citrate transporter NADC1. So I stop the CA inhibitor and get another drug to do its job. Regards, Fred Coe
Hi Dr. Coe; I just want to thank you for all of your hard work and generous sharing of same with us kidney stone patients. My first stone, that I’m aware of, was in Feb 2012. Since that time it has been multiple stones, chronically, at great expense and loss of work, eventually disability, worst of all my time spent enjoying my grandchildren. Recently, your PTH article seemed to “jump out at me”, so I asked the PA at my urologist to please consider a blood test. I’m happy (which may sound strange) to find everything falls right into the guidelines. Along with stones, I also have high blood pressure and a very bad case is osteoporosis – to the odd extent of crumbling teeth of recent. I’ve been referred to a local endocrinologist, Priyanka C. Iyer, MD with my first consult on June 9th. My NMRIS15 test begins on June 22nd. I am So Very Excited! My osteoporosis has gone from my first dexa scan in 2012 to my recent in Feb 2021 to dropped -8.8 left fewer , 7.5 right, and 5.3 for spine and there is now IV medicine to actually re-build bone strength, sounds like a God-send to me, and with many remarks on my tests stating “supersaturation” the thought of possibly reducing the frequency of kidney stones is a miracle to me! As you can clearly tell I know little if anything regarding the medical science of this, your specialty, but it is your name I’ve enjoyed following and just cannot Thank You enough for your dedication and hard work spent helping us, those plagued with these inconvenient and expensive annoyances. Best of all, I look forward to more time spent enjoying my 2 year old granddaughter, Madilynn, something my 16 yr old granddaughter I wasn’t so fortunate to enjoy (we scarcely know one another!). My numbers aren’t too bad, PTH 78.3, Calcium 10.0 phosphorus 1.03 creatinine 1014 and magnesium 101. I have Every symptom but heart problems with my son having noticed my mental loss first and quite concerned. My GFR no-black (I’m half Japanese half Caucasian) has been up and down drastically for decades but fortunately changes each month. BUN is 61 Chloride 110. I hope I’m not boring you unnecessarily with these numbers, I clearly don’t know what they mean. But You have given me hope, that one day fairly soon I just may be clear of all this and can enjoy my senior years. Thank You Dr. Coe, sincerely and with all my heart. If you suggest a different endo you have more faith in, believe me your input is more than welcome. And if these numbers have caused you to suspect otherwise, your input is and will be greatly appreciated. (My referred to endo is due to having financial assistance. Healthcare is not cheap in the USA but I am very grateful for it and have been following your articles faithfully, despite my struggle to comprehend. I just want to thank you for the hope you’ve given me and the appreciation and gratitude to those like you who have dedicated your lives for our improved lives. My sincere and deeply felt thanks! MaryAnn Roberts My Best Wishes to you and yours Always!
Hi MaryAnn, Given your bone disease and stones and estimate that stones began in midlife I would consider primary hyperparathyroidism – your single blood calcium was 10.0 which is at the border of high, your PTH is high but your kidney function is reduced which can raise PTH. I would suggest repeated fasting morning serum calcium measurements to be sure if the values are really in the 9- 10 range or generally 10 or higher. If the latter your may benefit from removal of an enlarged parathyroid gland. The other issue is your urine calcium that you did not mention – was it high? Regards, Fred Coe
Do non obstucting(lower left pole) kidney stones cause pain? And why is there continued sediment in urine despite a bladder washout in.a patient with kidney stones? Should these stones be removed?
Hi Helga, small stones not rarely associate with pain and research has not disclosed why. But passing crystal sediment will cause cause pain and bleeding. You need to collect this sediment and have it analyzed so you know what the crystals are – I bet they are calcium phosphate. If so, your urine is supersaturated with respect to that crystal and steps to lower the SS will stop the crystals and perhaps your pain. Regards, Fred Coe
Hello Dr. Coe,
I had my first stone two years ago with surgery and it consisted of 6.5 mm stone Calcium hydrogen phosphate (brushite 10%) CoD (Weddellite 20%), CoM (Whewellite 55%) and CaP (Apatite 15%) next stone 10mm was CoD(Weddellite 25%), CoM (Whewellite 45%) and CaP (Apatite 30%) and my last 9.8cm calcium oxalate dehydrate 40% and Calcium phosphate (hydroxy- and-carbonate-apatite 60%)
24 hour urine collection results: Urine Volume 1.3, SS CaOx 10.23, Urine Calcium 394 Urine Oxalate Urine 22, Citrate 663, SS CaP 2.38, PH 5.84, Uric Acid 0.86 Urine Uric Acid 0.448
All three where stent surgeries and ER visits, and I do not want anymore. If you can help, I would really appreciate it. before the 24 hour urine collection I was taking fish oil daily and before the third stone I added Calcium citrate to my diet. Of course I am drinking 50-90 oz of water too. Thank you in advance, Maria Johnson
Hi Maria, you have a very high urine calcium and a very low urine volume and urine oxalate, so you are making mixed calcium oxalate calcium phosphate stones. Surely your physicians want you to nearly triple your urine volume – 2.5 liter/d would be a basic goal, and will want to help lower your urine calcium level. Given so many stones, and so much phosphate in them, I would think a few years of a thiazide would be desirable – that is their concern and responsibility. Regards, Fred Coe
Hi, Dr. Coe… thank you for putting these wonderfully informative articles on kidney stones online. My kidneys were unremarkable until this year. I had 3 stones (5mm, 4mm, 2mm) removed last week… my first kidney surgery ever. I am a 70 y.o. Female, non-drinker, non-smoker, and my stones were 10% calcium oxalate mono hydrate and 90% calcium phosphate, hydroxy & carbonate apatite.
My fluid intake is 2 liters a day minimum (water), sodium always less than 2000mg/day. Since I eat a low carb diet, my Protein is slightly more than your recommendation, but not excessive. However, I have minimal calcium intake due to severe lactose intolerance and calcium supplements cause GI problems.
No doubt I need to add more calcium to my eating plan. I am adding rice milk and tums for calcium until I meet with a nephrologist in four weeks.
However, in the meantime, i wonder if my two Prolia injections for osteoporosis a year ago may have contributed to the formation of these fast-forming stones??
I stopped the Prolia after two treatments because I developed intense itching after injection two. The kidney stones were identified a year after the first Prolia injection. Symptoms started out of the blue with intense pain, nausea, vomiting. When I awoke, I also had other symptoms that seemed “sepsis like”: body temp of 95.2, extreme lethargy, feeling as ill as I ever felt in my life. Basically I went to sleep feeling well, and I went to the ER just after midnight.
Stones were confirmed that morning in ER by a CT scan. Again, the kidney stone CT scan was a year after the first Prolia injection (which a bone scan showed did help my bone mass significantly).
Your comments about Prolia and/or other osteoporosis meds in relation to calcium phosphate kidney stones would be much appreciated.
Again, thank you for publishing this valuable kidney stone info. It’s a very complex topic, and we patients as well as our Primary Care physicians need to have a much better understanding of how various stones form… and what can be done to prevent them.
Hi Dee, I looked up several references – effects of prolia with or without extra calcium and vitamin D and one showing effects on kidney function but no one shows 24 hour urine calcium that I could find. Since the monoclonal antibody to RANK reduced bone osteoclasts the expected effect is a fall in urine calcium and stone risk. So, I think the cause of your stones lies elsewhere. Regards, Fred Coe
My blood & urine tests show that i have high phosphorus levels of 6.4 in addition to low PTH levels of 6.6 showing that i have calcium phosphate stones. My dr told me that i need further checkups. However, upon reading further on the topic, i noticed that i can do dietary changes already. i realized that based on my test results, i need to eat more calcium concentrated products and limit animal proteins. I would love to know your suggestions, whether nutrition-based or others.
Hi Majd, I cannot clearly understand your post. Serum PTH seems too low to measure, urine phosphate of 6.4 is uninterpretable as there are no units. If you can clarify matters, I would try to help. I have allowed your post as a courtesy despite what seems a linked in form I would usually block. Regards, Fred Coe
Dr Coe, I have Ca Phos Stones and no signs of high oxalate on 24 hr urine. Made changes to diet that I log daily including 25 added sugars, 800-1000 Calcium, protein 55-65g, sodium 1000-1500 and 13 cups of water. Got my urine sodium down to 61 mEq, Brushite SS down to 2.08 from 4 and still considered high but my urine Ca is 249 from the 300’s and still not down enough. Uro oxalate is 32mg/day and Oxalate SS is 1.13. Of course high PH. My question is should someone who doesn’t have an oxalate issue but has Phos Stones keep their calcium intake to the lower end of the scale around 800? I know we need to have lots for our bones but if we are still losing in the urine what good does more do for us? Plus from what I read if you are over 50 you need 1200 mg of calcium and I would think that much would raise urine calcium even more. Thank you very much-
Hi Diane, oxalate is no more important for your stones than moonlight. What matters is pH, volume, calcium and citrate. Low sugar and sodium will help lower urine calcium. Given you have brought down your calcium and SS CaP is really too high, how about more urine volume – maybe 3 liters a day? Potassium citrate might do more harm than good – raises pH, might raise citrate. Thiazide is next – it will lower urine calcium, and at least chlorthalidone will lower pH. Regards, Fred Coe
Dr Coe, Thank you for the advice. My 24 hour urine volume was 3.76L/day. Will it help to go even higher?
Not much. Perhaps a low dose of thiazide would be most prudent. You might ask your physician what she/he thinks. Fred
Hi!
23 yr old female
80% CaP 20%CaOx Stones
Ive passed about 8 in the last 3 years and they are becoming more frequent.
2.8L urine output, 250 Urine Calcium, 450 citrate, 7.2 urine PH 3.5 SSCaOx 1.5 SS CaP
Taking 50 MEQ potassium citrate (prior PH was 6.5 before starting citrate, and citrate was 160)
I am getting stones more frequently since starting the citrate and am wondering if it would be better to stop taking it and see what happens. My PH and citrate are the issue here. Whats the better evil? Any other suggestions on reducing my stone risk?
Hi Jessica, so your calcium is hefty but not remarkable, your urine citrate was very low – 160 and pH 6.5, and rose to 450 (still low for a woman) but pH is not really high. Stones are not better, maybe worse. I would think to stop the K citrate and use chlorthalidone 12.5 mg a day with KCl replacement – better pH and the drug will lower urine calcium. Of course, you have a citrate problem – not enough without K citrate but it seems that replacement of citrate is not making things better. A caution – I do not know your real medical circumstances, so my remarks are just that, and your physician is in charge. Best, Fred Coe
Hi Dr Coe,
You haven’t mentioned the role of infection so I assume that it is a lesser cause. However, that has always been cited as the cause of my son’s kidney stones. He has Cerebral Palsy and, as a result of having Harrington Rods implanted in his back in 2002, at the age of 15, he has a paralysed bladder (and bowel). He has had an indwelling suprapubic catheter since then and has had numerous kidney stones since he was 17. He’s had open surgery twice, lots of lithotripsy, laser treatments, stents, etc. He’s also been seriously ill with misdiagnosed total blockage of one kidney twice. I am always searching for ways to stop this happening to him. I was recently told that his stones are of the Calcium Phosphate type.
So, he drinks 4 litres of liquid a day, mostly water. I get up in the middle of the night and give him about 250ml of water. He loves dairy and only has a very small portion of meat once a week. He has no sugar except for what is naturally occurring in the approx. 400ml of fruit juice that he has each day. I guess he gets a fair bit of salt in the cheese that he wants every day. I hadn’t thought of that. I have control over what he can choose from but he chooses what he will eat so there’s things that he won’t even try, like fruit. I give him Cranberry, D Mannose, Vitamin C,D,E and K2 and he is on Hiprex and Potassium Citrate 1000mg a day. He was started on 2000mg at first but that was reduced after blood and urine tests and the Dr is happy with his test results now. He is also on Propranolol and Pariet to protect his oesophageal varices (neonatal hepatitis). He’s been on them (or equivalent) since he was 4 so I presume they wouldn’t cause kidney stones.
Everything seems OK. He hasn’t had a problem stone for over 2 years and hasn’t been sick with a UTI for years but there’s always sludge in his drainage bag, sometimes gravel, sometimes blood. His urine always smells, unless he is on an antibiotic, but the smell comes back within a few days of going off the antibiotic. His catheter is changed every 4 weeks and his urine is usually better for a few days to a week but it always goes back to smelly, a bit dark and sludgy. Urine tested from his catheter (not the bag) usually doesn’t show any infection. I’m always trying to do my best for him but never know whether I am or if the next day will see us in hospital.
Oh, as an aside, his father had one kidney stone when he was 26 and one of his sisters had one in her mid-thirties. Maybe there is some minor genetic predisposition. If there is, surely it can’t be a bigger reason than having an indwelling catheter.
I’d really appreciate your thoughts even though our problems may be slightly to the left of your focus.
Thanks,
Marilyn
Hi Marilyn, The smell must be ammonia like, and infection present with proteus, enterobacter, or pseudomonas or the like. These convert urine urea to ammonia and lead to struvite stones – magnesium ammonium phosphate + calcium carbonate which co-crystallizes. I would have the gravel tested again. So I suspect it is indeed infection. In a chronically catheterized person infection is impossible to eradicate. He may also have calcium phosphate stones from high urine calcium losses from immobilization – if so that can be helped perhaps, but we are in a very complex area. You do not mention his urine chemistries. Regards, Fred Coe
Hello Dr. Coe,
Can high Ammonia in the urine come from sulfur foods/dietary proteins or is it mostly an unknown, hereditary, or a problem in the tubules. I know people with Ca Phos Stones tend to have higher ammonia and PH. Just wondering if it can be high due to excess of certain foods that could raise it.
Hi Lisa, Smart question. Acid loads raise kidney production and urine losses of ammonia but urine pH is low and stones are never phosphate. In your situation, ammonia is regulated improperly – too high – so acid excretion is a bit more than needed and urine pH rises. Foods that raise urine ammonia are acid loads. Fred
Hi!
23 yr old female
80% CaP 20%CaOx Stones
Ive passed about 8 in the last 3 years and they are becoming more frequent.
2.8L urine output, 250 Urine Calcium, 450 citrate, 7.2 urine PH 3.5 SSCaOx 1.5 SS CaP
Taking 50 MEQ potassium citrate (prior PH was 6.5 before starting citrate, and citrate was 160)
Hi Jessica, The potassium citrate is raising your urine pH and risk for calcium phosphate stones. We have no trial evidence that this agent is effective against calcium phosphate stones. I would consider lower diet sodium to lower urine calcium + higher urine volume in hopes of lowering CaP SS below 1. If you have repeated stones, a thiazide diuretic will lower urine calcium and CaP SS, and will not increase urine pH, but is a medication with side effects. The low urine citrate is – unfortunately – the rule in CaP stone formers – mechanisms not so clear but possibly inherited. Regards, Fred Coe
Hi Dr. Coe,
Thank you for all your years of extensive research you have dedicated to help the stone forming community. We really appreciate it! I have had two calcium phosphate stones surgically removed in the past 1.5 years. About two years ago I got off taking diamox for IIH that was in remission. I was on the diamox for about 3 years total. I never had an issue with kidney stones until the diamox. Is it possible the diamox had changed something to make me still form calcium phosphate stones two years after stopping it? (I will be submitting a 24 hour urine test tomorrow to my urologist). Thanks so much! Laura
Hi Laura, I am afraid Diamox is a very powerful cause of calcium phosphate stones. It causes a form of renal tubular acidosis and is of highest likelihood the cause of your stones. Your urine test will no longer register its effects and may be normal. Avoid the drug and any other inhibitors of the carbonic anhydrase enzyme. Regards, Fred Coe
Hello,
Since many Ca Phosphate stone formers have high urine ammonia I was wondering if it can be controlled at all by eating lower sulfur foods? Also does the excess urine volume we need “wash out” citrate at all with that being low with these kind of stones? Thanks for your time.
Hi Geo, I am afraid that urine ammonia excretion and citrate, too, are controlled by a vast biological system. If we lower food methionine and cystine intake – source of acid from sulfate – urine ammonia will go down, but remain high in relation to the lower acid load. As for citrate, urine flow is without effect. Regards, Fred Coe
I’ve been passing stones several a year for the past 5 years. 2 lithotripsy and 1 ureteroscopy to remove one that was stuck. I’m told all my stones which currently number more than 10 in each kidney are now passable 10 stones in each one). My question is can simply having the stones in my kidney be causing the right flank seemingly kidney pain? My urologist has referred me back to my PCP for the pain saying that he doesn’t think that it’s urological. Anyway just looking for some answers or guidance. I should also note that I am a 42 year old woman otherwise healthy and normal weight (5’8″ and 135lbs) . I’ve given birth to 5 children…the kidney stones were discovered and started causing the problems during my pregnancy with baby #4 at age 36.
Hi Tara, Multiple calcium phosphate (I assume this is your stone type) in the kidneys can cause pain, even without obstruction. Right now we do not have real trials or basic science but I suspect inflammation plays a role. Of course your physicians want to look for and treat any infection – all stones can become infected. As well I would do all I could to reduce causes of stone as new crystal formation can cause pain. This latter means serum and 24 hour urine testing as in the linked article. Regards, Fred Coe
Hello Dr and thank you for a great article. Do you have any recommendations in treatment for CPPD in a patient with metastatic renal carcinoma (left nephrectomy 7 hrs ago) stable Mets and an eGFR 41 pre CPPD arthritis episode (severe inflammation CRP 24 previously 3.4) Both prevention of another episode and is there any chance of removal of crystals and repair of inflammatory assumed lesions systemically ? Also do you do private consults for a fee?
Hi Amal, I am not sure but presume CPPD is calcium pyrophosphate crystal mediated arthritis (often called pseudogout). It is not uncommon with reduced kidney function and the crystals are not removable at this time. Here is a recent review of treatment options. If you search through PubMed (where this link will take you) many more articles abound there. It is not my main clinical area, so although I do telehealth consultation as part of my work at this university I do not generally try to aid in management of CPPD. Regards, Fred Coe
Dr. Coe.
I am a 53 year old woman who has been forming stones for the past 20 years. Over the years, I have had 3 lithotripsy procedures and 2 uretoscopies with laser lithotripsies. In my earlier years the stones were calcium oxalate. However, the last stone I was able to have analyzed was calcium phosphate [10% calcium oxalate dihydrate,
70% calcium monohydrogen phosphate dihydrate (brushite), and 20% calcium phosphate (hydroxy- and carbonate- apatite).] My last 24 hour urine showed low citrate, high 24 hour calcium, high supersaturation CaP, and a pH of 6.313. I am now forming stones at an alarming rate. I had a uretoscopy 6 months ago to address a problem stone and have already formed many new stones including one that appears to be 12mm based on a recent ultrasound. I continue to work on raising my fluid intake (which is a significant challenge as I am a teacher and can’t often run out to the bathroom at will). My doctor is kind of at a loss for what to try next. He is suggesting trying potassium citrate, however, I am concerned it will further raise my pH and cause more problems with the calcium phosphate stones. What do you think? Any suggestions you might have would be very welcome.
Hi Jane, Conversion to brushite does this – more stones, more frequent. I would talk to my doctor about thiazide to lower urine calcium. Your condition is serious. K Citrate is not a good idea, it may not raise your urine citrate and will raise urine pH. Thiazide will help even if your urine calcium is not so high. I usually use chlorthalidone 12.5 mg to start. Regards, Fred Coe
Dr. Coe. Thank you so much for sharing your expertise. I am hoping you will answer three follow-up questions regarding my calcium phosphate (brushite) stones. First of all, do you have any thoughts on taking IP6 for stones? Secondly, would cranberry extract help to lower my urinary pH? Finally, is there anyone in the country who is focused on these types of stones that sees patients. Thank you so much.
Hi Jayne, IP6, inositol hexaphosphate, has no role in stones. This decent enough public information website appears to show no proven use for it in any condition. It can alter clotting so be careful of drug interactions. It may reduce calcium absorption from food which is a possible bone hazard especially in stone formers who are abnormally prone to bone disease. So overall I cannot endorse its use. Regards, Fred Coe