You might say this article culminates the two years this site has been on the web.
It is about treatment of the most common stone patients, treatment to prevent more stones, and therefore the topmost important matter for patients and their physicians.
The topic is so important I plan three versions. This one is primary, and has not only references but linked documents so original materials are available to everyone. The next will be a video that offers the material in a more fluent if less documented format. Finally Jill Harris has promised to coauthor with me a version in her lovely and popular style.
I present all of the treatment trials in the context of the supersaturation hypothesis for stone formation and in the light of what we know about urine stone risk factors. The entire site thus far concerns these matters, and was in fact created to support this article which is the capstone of the site to date.
This article draws importantly on three other articles that describe the kidney stone treatment diet. As things have turned out, the 2015 – 2020 US recommended diet more or less exactly matches the needs for stone prevention in idiopathic calcium stone formers. The scientific reasons for this are well established. Therefore this article is meant to be read in parallel with the above three diet articles.
It also draws on our articles on thiazide, potassium citrate, idiopathic hypercalciuria, the idiopathic calcium stone forming phenotypes, and regulation of oxalate excretion, and these links are embedded in the text.
The beautiful picture is Hidden Lake, Bearhat Mountain, Glacier N.P., near Kalispell, Montana. I had thought to use Ansel Adams but this one is by Howie Garber, a modern professional and I think wonderful photographer who had this print on his site.
WHO ARE IDIOPATHIC CALCIUM STONE FORMERS?
They are people who form calcium stones in the absence of any causal systemic disease. I have listed the more common such diseases in another article. Of course, this requires stone analyses be done, hopefully for all or a large majority of stones from a patient. Patients whose stones contain uric acid, cystine, struvite or drug crystals are not included here, being special cases.
Although the idiopathic calcium stone formers come in three separable groups, for the purposes of prevention all three are treated much the same way, with a few exceptions. The most common, calcium oxalate stone formers, have certainly predominated in all of the trials by force of numbers. The hydroxyapatite calcium phosphate stone formers have surely been part of most trial groups but have not been reported separately. The uncommon brushite stone formers may or may not have been in trials but are scarce enough their numbers would be too slight to alter final results and their particular outcomes from a given treatment impossible to gauge looking back. Therefore I do not exclude brushite stone formers having no real reason to do so.
THEORETICAL STONE RISK FACTORS
Determinants of Urine Supersaturation
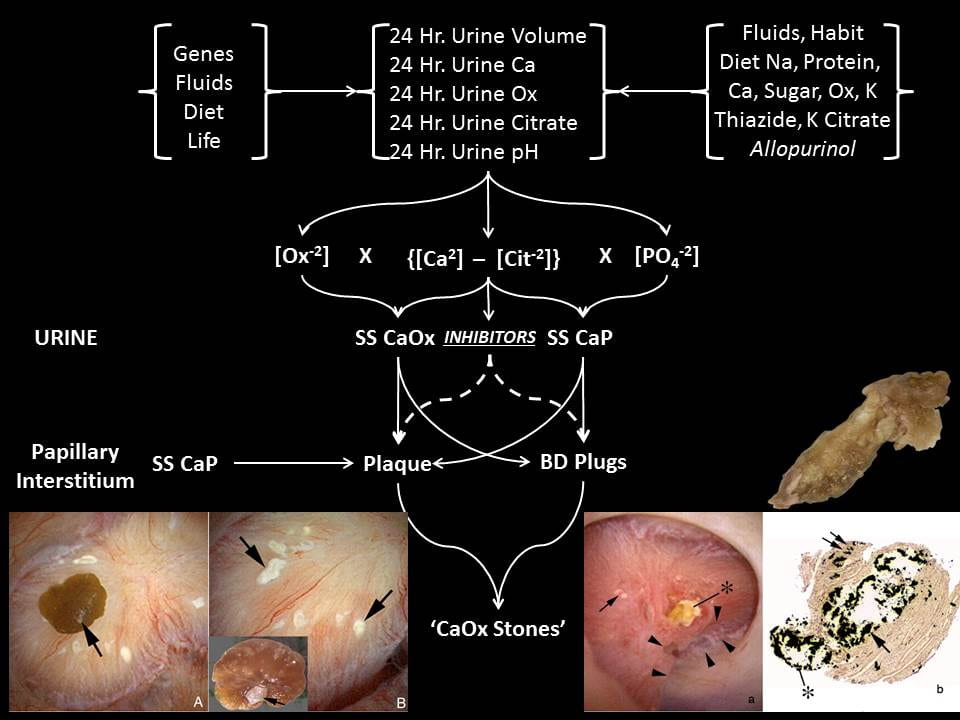
In a schematic sense, the two relevant supersaturations SS CaOx and SS CaP are approximated by the products of calcium and oxalate and calcium and divalent phosphate ion, respectively. The calcium free to combine with oxalate or phosphate is crudely the difference between the calcium and citrate concentrations in mEq/l, because citrate binds calcium in a soluble complex. The divalent phosphate is controlled by the
phosphate molarity and urine pH – higher pH, higher abundance of the divalent form. The oxalate is mostly just the oxalate concentration.
 EQUIL 2, the common computer program used to calculate supersaturations, in fact calculates in this way but considers all possible ion associations.
EQUIL 2, the common computer program used to calculate supersaturations, in fact calculates in this way but considers all possible ion associations.
Therefore the main factors causing stones via supersaturation are the excretions of water, calcium, oxalate, and citrate, and urine pH (Figure at left). These are controlled by genes (idiopathic hypercalciuria and perhaps oxalate and citrate and pH), fluid intake, diet oxalate, calcium, sodium, and acid load. Over it all is life itself that determines not only the daily totals but their variability. We measure using 24 hour urine collections, but relative excretions of water, calcium, oxalate, and citrate and urine pH change throughout the day, so supersaturation may have many peaks and valleys.
Inhibitors – The Inaccessible Quotient
Molecules that Inhibit Crystals
It is not so much that we do not know any urine crystallization inhibitors as it is we can name too many. Urine contains about 1,800 identifiable proteins among which are many anionic species easily able to attach to calcium based crystals and slow their growth or even nucleation. The link concerns stone associated proteins as they are more likely than not to have attached to crystals. The proteins that matter in terms of stone forming propensity, hundreds, perhaps, lie hidden amongst the hordes of proteins, so we do not know which proteins really have large effects and are important for us to measure.
Citrate stands out as the one we can and do measure. It can disrupt calcium crystal growth at concentrations far below those in urine. Just as the unbound calcium is that free to create crystals, the unbound citrate is free to inhibit crystals, so the calcium – citrate molar difference would be predicted as a critical factor in inhibition.
Citrate and The Ostwald Limit
Wilhelm Ostwald was born on September 2, 1853, in Riga, Latvia. Among his famous pupils are Arrhenius (Nobel Prize 1903),Van ‘t Hoff (Nobel Prize 1901), Nernst (Nobel Prize 1920) – taken from the Nobel Lectures. He won his Nobel in 1909 and died in 1932.
The Ostwald limit is the supersaturation at which crystallization begins in a given solution. It can be measured in human urine, and if supersaturation is the floor the limit is the ceiling. That distance, between supersaturation and the limit is smaller in stone forming patients than in normal people, especially for calcium phosphate. Variation of urine citrate concentration in the range found in urine of between 0.5 and 5 mmol/l seems to account for 1/2 of the elevation of the limit above supersaturation. Therefore as a risk factor and as a treatment citrate ought to be very important and perhaps mysterious, too, for it affects supersaturation – via calcium binding, inhibits those crystals supersaturation would produce, and therefore has a role in setting the upper limit of metastable supersaturation – that privileged space between supersaturation and the limit in which a solution remains clear of crystals.
Anchored Tissue Calcifications
Most stones form over anchored tissue calcifications: Interstitial HA crystals, plaque, and terminal collecting duct of Bellini (BD) plugs.
Plaque
On the left of the intra-operative image panel that is itself at the bottom left of the figure above you can see white plaque with a CaOx stone growing on it (arrow) – the removed stone (inset) has a central white CaP anchor site which attached this stone to the plaque. The big arrowhead points to where it was attached. I have made a video that may help clarify this process. Urine CaP SS can create the initial layer over interstitial plaque that becomes exposed to urine when the urothelial boundary gives way.
Plaque itself presumably arises from supersaturations in the papillary interstitium, not the urine, and these cannot be measured at the present time. Some theory exists and has been partially tested. It suggests that idiopathic hypercalciuria may foster plaque but this idea is too untested to affect clinical practice.
Plugs
Urine CaP SS can cause plugging of terminal collecting ducts. A long plug is shown in the right lower panel of the above figure. The shaft is HA and filled the duct. The rounded end arose from the urine over the exposed plug. The OVergrowth can be CaOx stones, CaP stones, or both depending on the urine supersaturation balance that is conditioned by the five factors I have already mentioned: volume, calcium, oxalate, and citrate excretions, and urine pH.
THE SUPERSATURATION HYPOTHESIS
The Separate Roles of CaP and CaOx SS and of Citrate
Urine CaP SS is what must drive formation of the initial HA overgrowth on plaque, and urine CaOx SS must drive subsequent formation of the CaOx that makes up the bulk of the stone. Urine CaP SS is what must drive plugging of BD, and urine CaOx and CaP SS will then determine the relative amounts of these two crystals over the open end of the plug facing into the urine. Urine citrate is crucial in two ways. By binding calcium it lowers both CaP and CaOx SS. By inhibiting CaP and CaOx SS it contributes to the ULM for each and presumably protects against overgrowth on plaque, plugging, and overgrowth on plugs. Since only free citrate can so act, the molar difference between calcium and citrate ions is presumably a crucial determinant of the inhibition effect. This latter point has not been critically tested. Apart from urine citrate, we do not know enough about inhibitors and local tissue factors to use them in stone prevention, but we do have a powerful prediction from the physical chemistry of crystallization.
The Clinical Meaning of the Supersaturation Hypothesis
GIven that stones depend on crystal production, and given that supersaturation is a necessary factor in crystal production, one can say that: The urine supersaturations of an active stone former are too high in relation to the crystals in stones forming. By too high I mean simply high enough that, all things considered – inhibitors, tissue regulation of crystallization – crystals are being formed. Because CaP SS may indeed have a dual role – in forming the plaque attachment site for CaOx stones and being the main crystal in plugs, even when stones have little HA one might conclude the CaP SS is too high.
One immediate deduction from this formulation is that prevention of new stones requires that urine supersaturations with respect to the crystals in stones forming be lowered, and that lowering needs to come from alterations of those urine factors that control supersaturation. As well, even when stones are CaOx, CaP SS should be lowered.
Another deduction is that empirical urine stone risk factors will in fact be mainly those very factors that most influence SS: urine calcium, oxalate, citrate, volume, and pH.
EMPIRICAL STONE RISK FACTORS
Elsewhere I have presented the important work of Gary Curhan, and do so again here. They are in fact those predicted from the primacy of supersaturation because all of them affect supersaturation in a direct manner.
Urine Calcium
 The light red and blue (female and male) bars are plotted downward from the relative risk of becoming a stone former to the lower 95th percentile of that relative risk. The solid bars fill in the space between the end of that 95th percentile and 1, the point of no relative risk increase.
The light red and blue (female and male) bars are plotted downward from the relative risk of becoming a stone former to the lower 95th percentile of that relative risk. The solid bars fill in the space between the end of that 95th percentile and 1, the point of no relative risk increase.
For urine calcium (upper left plot) relative risk with respect to less than 100 mg/day rises progressively in the two female and one male cohort. Between 100 – 149 mg/day the lower 95th percentile crosses 1 meaning the relative risk it not significantly above 1. In the next hexile relative risk is almost certainly significant and thereafter it certainly is. Of crucial importance there is no knife edge; urine calcium is a smoothly graded risk factor.
Urine Oxalate
Urine oxalate behaves similarly except the magnitude of relative risk (with respect to <20 mg/d) does not rise as far as it does for calcium excretion.
Urine Citrate
Urine citrate opposes supersaturation, so one expects that relative risk will fall as its excretion rises, which is a well known clinical maxim that the Curhan data gives a proper experimental foundation. In this case relative risk is plotted upward from below 1 in most cases, and the upper 95th percentile is in the red and blue solid bars. Significant risk exists at values below 400 mg/day. Notably the change in risk seems modest compared to that of urine calcium or oxalate, but partly that is because the available range is only from 1 to 0. Perhaps a lot of the protection from citrate arises from direct crystal inhibition which is rather complete at concentrations below those in urine. I have narrowed the y axis range to make the progression more obvious.
Urine Volume
Urine volume is like citrate; relative risk falls markedly as volume rises, but in some cohorts the upper bound of risk ratios are above 1 until volume reaches above 2 liters – solid bars above 1. I have narrowed the vertical axis range to make the progression of risk reduction more obvious.
Urine pH and Other Factors
Urine pH would have a predictably complex relationship to stone risk, in that low values would cause uric acid stones and high values CaP stones. So one might have predicted a U shaped curve. In fact, if you inspect table 3 from his main paper such a pattern is perhaps present in the first of the female cohorts, relative risk (with respect to <5.5) fell between 5.5 and 6 then rose again; this was also true in the second female cohort but not the male cohort in which risk rose with urine pH.
Urine phosphate is very plentiful compared to oxalate or calcium so pH would presumably control the abundance of the divalent form and therefore stone risk. In two of the three cohorts relative risk (as compared with <600 mg/d) was higher at higher phosphate excretions.
I showed observational data decades ago that reducing urine uric acid excretion with allopurinol reduced calcium oxalate stones, and a double blind randomized trial substantiated this fact, but in the Curhan studies stone risk did not rise and, in several cohorts fell as urine uric acid increased.
These data all arise from one publication. Here is a link to a spreadsheet with all of the data I extracted from Table 3 of the paper. Links to the paper online and to a PDF are in the spreadsheet.
THE SPECIAL CASE OF URINE URIC ACID
Long ago, I published observations from my clinic that some calcium oxalate stone formers excreted a lot of uric acid in their urine (>750 mg/d and >800 mg/d women and men, respectively) and I had decided on purely clinical instincts to see of lowering it with allopurinol might reduce new stone production. Among 21 patients observed for an average of 1.85 years only one had a single recurrent stone, whereas prior to treatment all had been very active stone formers.
The work was meant only to begin a conversation about the possibility that uric acid had some role in calcium oxalate stone formation, and the paper called for a proper trial to determine if the matter was worth pursuing.
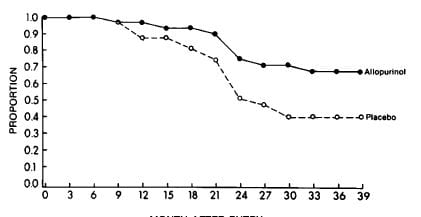 Bruce Ettinger performed such a trial. In a randomized, prospective double blind trial lasting 39 months 31 placebo treated patients had 18 new stones and 29 allopurinol treated patients had 9 stones (X2=3.4 p=0.035). His life table analysis showed a highly significant (p<0.01) treatment effect with 42% placebo stone free and 69% treated stone free.
Bruce Ettinger performed such a trial. In a randomized, prospective double blind trial lasting 39 months 31 placebo treated patients had 18 new stones and 29 allopurinol treated patients had 9 stones (X2=3.4 p=0.035). His life table analysis showed a highly significant (p<0.01) treatment effect with 42% placebo stone free and 69% treated stone free.
Decades of bench research have failed to provide a mechanism by which these treatment effects might be brought about. So we have reasonable empirical evidence for an phenomenon whose cause is not known. I mention allopurinol as a treatment alternative in later sections of this article but do not pool the allopurinol trial with those for diet, thiazide, or potassium citrate.
RISK FACTOR MODERATION REDUCES STONES
Our evidence arises from such stone prevention trials we have available, and although they do not satisfy professional trialists they satisfy me as a scientist. Their message – treatments work – is very unlikely to be wrong.
I have compiled the main data for all of the trials. Here is a link to the spreadsheet of the data. On the sheet are links to PDF images of the publications as well as PubMed links.
Water for Stone Prevention
In patients who had formed a first stone, Borghi (1996) compared a high water intake to minimal treatment. Stones appear to have been mainly 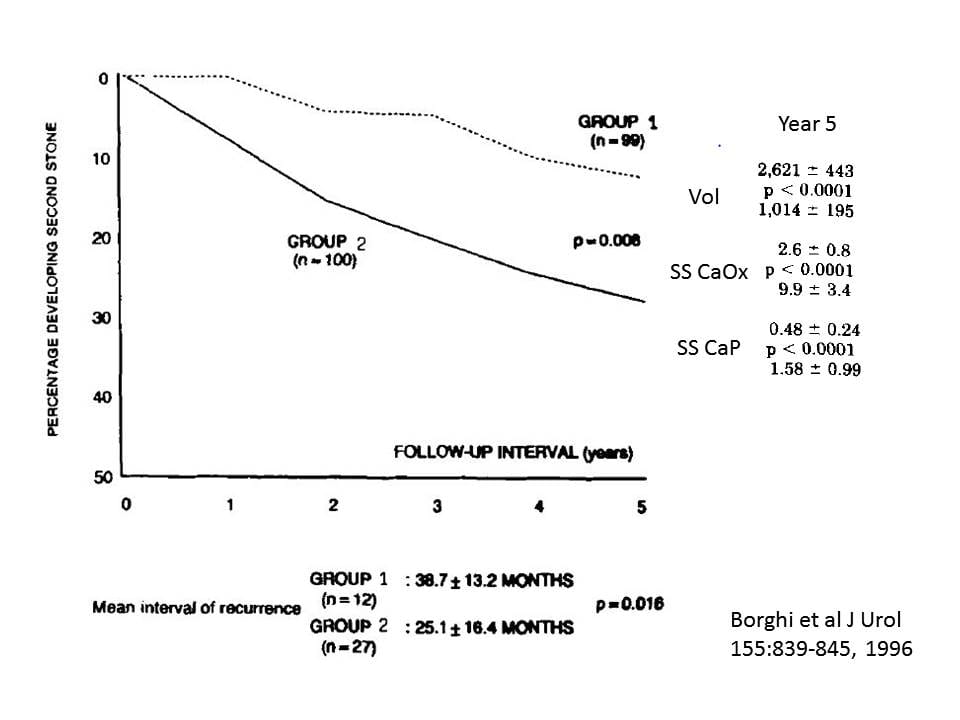 CaOx. Patients with hypertension, retained stone fragments in their kidneys, or ‘other metabolic pathology’ were excluded.
CaOx. Patients with hypertension, retained stone fragments in their kidneys, or ‘other metabolic pathology’ were excluded.
Of note, these patients had low baseline urine volumes (ml/d): 1,057 vs. 1,401 and 990 vs.1,239, patients vs. controls, male and female, respectively, P<0.001 for comparison of patients to controls within sex. This baseline urine volume would carry a high stone risk using the Curhan findings shown above. Urine calcium averaged 244 and 266 mg/day in Groups 1 and 2, respectively, also posing risk. The sex ratios in the two groups were about the same – 60-70% males; average age was 41 years.
Whereas the treated group was aggressively encouraged to raise urine volume, measure volume at home, and bring in a collection every year, the controls were told that ‘…since it was an isolated stone episode, it was not necessary at least at that time to follow any special procedures.’
At the end of five years, 12 of the 99 patients who raised their urine volume had formed a new stone vs. 27 of the 100 who did not (X2 = 6.9, p=0.008). The time to first stone was longer in the high fluid group as noted below the figure.
The urine SS values for CaOx and CaP were much lower in the treated vs. the placebo group as well (Year 5 data shown).
This trial indicates that at least for first time calcium stone formers a urine volume of about 2.6 liters daily will reduce but not abolish new stone formation. This is consistent with the supersaturation hypothesis as the treatment group had both less stones and lower SS than the controls. It also fits well with the Curhan data, in that less stones occurred when urine volume was above 2.5 liters.
Diet for Stone Prevention
Diet Sodium
If you have read about idiopathic hypercalciuria, the main reason calcium stone formers have rather generous urine calcium excretion rates, you know that diet sodium and protein are powerful controllers of urine calcium losses, and that diet calcium cannot be low for long without risk of bone disease.
I and Elaine Worcester compiled these data from a mixture of publication. This spreadsheet contains the data I  used to make this picture along with links to the PDF images of the articles.
used to make this picture along with links to the PDF images of the articles.
In the figure, red are normals, blue IH, circles are experimental and triangles observational data.
The message is clear: Urine calcium is powerfully influenced by diet sodium intake – which is urine sodium in the stable state. IH is, howsoever achieved, a condition in which urine calcium is unduly dependent on diet – and therefore urine – sodium.
That the slopes really do differ was tested in a general linear model with urine calcium as dependent and urine sodium and type – normal vs. IH – as independent. The slopes differed by type (cross product p<0.0001). The slope for IH was 1.396 vs. 0.380 for normals). The overall regression captured 75.6% of the variance around urine calcium. The effect of type on the intercept of the two regressions was NS.
That sodium dependence of calcium excretion is so much more dependent on sodium in IH than normal must reflect mechanisms for the pathogenesis of IH. In my detailed analysis of IH, I show, using data Elaine Worcester and I obtained, a similarly increased dependence of urine calcium on filtered load of calcium, all pointing to reductions of tubule calcium transport.
Diet Protein
Increasing diet protein intake will raise urine calcium excretion. At one time it was thought that protein increased urine calcium by imposing an acid load, but that has proven untrue. Given with enough alkali to offset the acid load protein increased urine calcium. The mechanism of protein induced hypercalciuria is a mixture of increased glomerular filtration and reduced tubule calcium reabsorption. I have reviewed this problem in a another detailed article.
Diet Calcium
Because idiopathic hypercalciuria is so common among idiopathic calcium stone formers and can result in bone mineral loss, a high calcium diet is generally recommended. Such a diet has another value in that high diet calcium reduced oxalate absorption and therefore urine oxalate excretion.
A Low Sodium and animal protein, High Calcium Diet Reduces Stones
Only one trial has concerned reduced diet sodium and it has the fault and benefit of being more inclusive in that diet protein and calcium were also modified. Note that ‘high’ and ‘low’ refer to diet changes from current habits. As detailed in multiple other articles on this site, US government recommendations now favor 1,200 mg calcium, less than 2,300 mg sodium, less than 10% total carbohydrates as refined sugar, 0.8 mg protein/kg body weight, and 112 mEq/day diet potassium from fruits and vegetables. By current standards this is a high calcium, low sodium, low sugar, low protein, high potassium diet.
The 120 subjects all were men with idiopathic hypercalciuria diagnosed by the older research criterion of above 300 mg of urine calcium daily in the absence of a systemic disease. All had at least two CaOx stones.
The trial compared a low calcium diet to a low sodium, controlled protein, high  calcium diet, 60 men in each diet arm. The low sodium diet was 50 mEq/day sodium, a low value, 1,200 mg (30 mmol) of calcium, and 93 gm of protein, 50 gm from animals and 40 gm from plant sources, and oxalate of 200 mg daily – not a low oxalate diet. The contrast group ate a low calcium diet – 400 mg/day (10 mmol) and were told to avoid high oxalate foods. Sodium and protein were not specified. By the end of five years, 12 men in the low sodium group and 23 men in the low calcium diet group had formed at least one new stone (X2 = 4.88, p=0.027).
calcium diet, 60 men in each diet arm. The low sodium diet was 50 mEq/day sodium, a low value, 1,200 mg (30 mmol) of calcium, and 93 gm of protein, 50 gm from animals and 40 gm from plant sources, and oxalate of 200 mg daily – not a low oxalate diet. The contrast group ate a low calcium diet – 400 mg/day (10 mmol) and were told to avoid high oxalate foods. Sodium and protein were not specified. By the end of five years, 12 men in the low sodium group and 23 men in the low calcium diet group had formed at least one new stone (X2 = 4.88, p=0.027).
Reduced Stones Associates with Reduced Stone Risk Factors
Individual Factors
Urine calcium levels were not different, presumably because the higher calcium intake was opposed by low sodium diet. But urine oxalate was lower in the high calcium low sodium group: 422, 411, 422, 433, 411 vs. 344, 322, 333, 333, 333 umol/day years 1 – 5, low calcium vs low sodium diet; all 5 differ as to change from baseline. So oxalate induced risk was lower. Urine volumes were the same – all about 2 liters/day or more. Urine citrate was not presented.
Low diet sodium is the likely reason a high calcium diet resulted in urine calcium levels no higher than found on a low calcium diet, and the high calcium diet presumably lowered urine oxalate as high calcium in food is known to do. So low sodium diet presumably lowered urine calcium and permitted a high calcium intake which will tend to lower urine oxalate.
Supersaturation
Only CaOx SS is presented and not in an ideal form. It was measured using EQUIL at baseline and one week but thereafter calculated by a regression formula. Even so, it was lower in the high calcium low sodium diet group: 7.3, 6.8, 6.7, 4.8, 4.7 vs. 5.1, 4.7, 4.5, 3.7, 3.5, years 1-5, low calcium vs. low sodium diet, respectively; all five differ as to change from baseline. So, despite some weaknesses, SS as estimated was lower.
Diet Oxalate
It seems odd that we have trial data on sodium, calcium, and protein but not on diet oxalate, Nevertheless to date no trial has been mounted. I believe it will fail unless the trial incorporates both high calcium intake and reduced diet oxalate together, because one needs to reach diet oxalate  levels of under 100 mg daily unless diet calcium is high.
levels of under 100 mg daily unless diet calcium is high.
Evidence for this statement is a set of studies I have summarized on this one graph. The symbols are scaled to the diet oxalate intake between 200 to 50 mg/d, and the studies are labelled by who I think of the main investigator involved. The original data are in the linked spreadsheet.
More or less independent of diet oxalate (size of symbols) urine oxalate (y axis) falls with calcium intake (x axis) and by about 1,000 mg calcium intake values more or less pack between 25 – 35 mg/d. In the small upper right box, Hess have a diet of 2,000 mg oxalate with 1,000 mg calcium – upper left point at 80 mg/d of urine oxalate, which fell to 30 mg/d when diet calcium was raised to 4,000 mg/day. The point of this exercise is that even the most remarkable oxalate intake can be balanced by a correspondingly high calcium intake.
Medication for Stone Prevention
Thiazide and Potassium Citrate
These treatments are aimed at reducing supersaturation and, in the case of citrate, increasing urine levels of a powerful inhibitor of crystallization. Both agents reduce new stones, although the trials are perhaps less that perfectly ideal. I have already mentioned the spreadsheet that has all of the key data. Likewise I have presented these trials in a more detailed fashion in two other articles – Thiazide and Potassium citrate.
In the figure, triangles are randomized, prospective, double blind trials, circles are not double blind, and size is scaled to time. The largest symbols 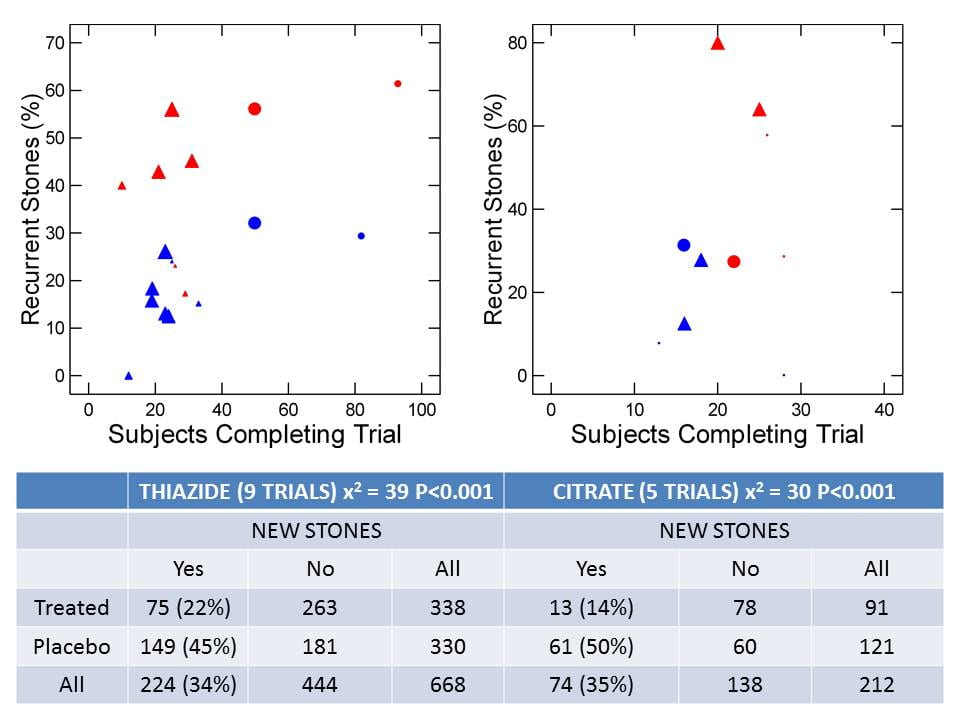 represent 3 years, the next size 2 years, the third one year and tiny points barely visible less than a year. These latter concern formation of new stones after surgery as judged radiographically. Red are control and blue treatment arms. Two randomized double blind thiazide trials had one control for two treatment arms, thus the five blue and three red large triangles.
represent 3 years, the next size 2 years, the third one year and tiny points barely visible less than a year. These latter concern formation of new stones after surgery as judged radiographically. Red are control and blue treatment arms. Two randomized double blind thiazide trials had one control for two treatment arms, thus the five blue and three red large triangles.
The vertical axis plots the fraction of patients who concluded the trial that formed a new stone, against the number of subjects who completed the trial on the horizontal axis.
The table sums up all 9 thiazide and all five citrate trials in terms of numbers of subjects finishing and number with and without new stones.
A total of 668 patients finished the 9 thiazide trials. Of these 22% formed a new stone. Among placebo patients 45% relapsed; the p value for a simple X2 test is shown. Corresponding values for the 5 citrate trials give a similar picture.
Any one of the trials can be and has been faulted. They are small, some too brief, and there is significant patient loss in some which was not perfectly accounted for. But in the aggregate thiazide treated patients had about one half the number of new stones, as those untreated, adjusted for the numbers of cases: 22 vs. 45%. For citrate the difference is more marked.
Synergy Between Diet Sodium and Thiazide
Reduced sodium diet alone will lower urine calcium – I have already shown that above. Thiazide lowers urine calcium by increasing proximal
tubule reabsorption of sodium and water, and secondarily of calcium. High sodium diet can partly overcome that effect so urine calcium does not fall as much as it might with less sodium, and, as is well known, potassium will be lost in excess in many people.
The Borghi diet and thiazide trials provide data on urine calcium vs. urine sodium with and without thiazide. I have compiled their data in a spreadsheet for those interested.
In the trials urine calcium fell with  urine sodium in the control arms of the diet and thiazide trials (red and blue circles, respectively). and in the low sodium high calcium arm of the diet trial (blue triangles). But thiazide (black triangles) lie below all other points at corresponding urine sodium levels. This means that thiazide and low sodium diet are synergistic.
urine sodium in the control arms of the diet and thiazide trials (red and blue circles, respectively). and in the low sodium high calcium arm of the diet trial (blue triangles). But thiazide (black triangles) lie below all other points at corresponding urine sodium levels. This means that thiazide and low sodium diet are synergistic.
Effects of Potassium Citrate On Stone Risk Factors
Potassium citrate has the potential to reduce calcium stones by reducing urine calcium and by increasing urine citrate itself which binds calcium in a soluble salt complex and is an inhibitor of crystallization. Therefore one might expect a more complex relationship between stone prevention and the single index of supersaturation.
Trial Data
Unlike the thiazide trials, the citrate trials offer only scattered urine chemistry data that do not lend themselves to the kind of pooled analysis I provided for thiazide. All I can do is consider each one as a separate experience. Each header below links to the PDF of the trial report.
Ettinger trial. Of the three long term trials, only that of Ettinger provided data on urine calcium before and during citrate treatment, and the treatment citrate data do not include corresponding urine sodium data so I could not plot them as I did on the preceding graph. Patients had active recurring stones (>=2 within the prior 5 yr and >=1 in the past 2 yr) and stones were >50% CaOx. Treatment was 63 mEq citrate/d, 21 mEq Mg and 42 mEq K, given in 3 divided daily doses for 3 years. Diet for placebo and drug arms was restricted in salt, sugar, oxalate, and animal protein with no more than 2 servings of dairy product – a low calcium diet.
Mean baseline citrate excretions were 549 and 587 placebo and treated groups, respectively, and corresponding treatment values were 548 and 769 mg/d. Urine SS was not altered for CaOx or CaP nor were there differences between placebo and treated groups. Given that stone rates fell (stone data in stone spreadsheet) without a change in supersaturation, the best possible hypothesis is that the increase of urine citrate increased inhibition of calcium crystallization.
Barcelo trial. Patients had 2 or more stones in 2 years and ‘low’ (less than 2 mmol/d) or low normal (less than 3.4 mmol/d) urinary citrate. Given a MW for citric acid of 192 mg/mmol these are 384 and 652 mg/day as selection criteria. Stones were calcium oxalate, alone or mixed with calcium phosphate – amount not specified. Mean urine citrate in the normals used by the lab was 3.36 mmol/d or 645 mg/day. Mean urine citrate was 347 and 370 mg/d at baseline in the treatment and placebo groups, respectively. With treatment urine citrate rose to 633 mg/day in the active arm but remained at 384 mg/d in the placebo arm. Urine calcium is said to have not fallen – no data presented. Supersaturations were not measured. So in this trial patients were initially low enough in urine citrate to pose risk, and treatment reversed that risk by raising urine citrate appreciably. Stone recurrence indeed fell (stone data in stone spreadsheet).
Hofbauer trial. Patients were ‘idiopathic calcium oxalate’ stone formers. Urine citrate at baseline (mg/d) was 243 and 249 and, at end, 282 and 438 mg/d, placebo and treated groups, respectively. There was ‘a marked decrease in the 24-hr urine calcium…’ but the data are not shown. Citrate dose was individualized to maintain urine pH between 7-7.2 so there was no double blinding. Dietary restrictions were imposed on everyone, but not specified. So the patients had low enough urine citrate to pose a risk of stones, and treatment increased urine citrate and lowered urine calcium but stone recurrence was identical in both groups (the red and blue circles on the trial figure, stone data on the linked spreadsheet). In fact both groups had rather low stone rates at the end, comparable to those of the treated arms of the other two long trials. So although stone risk should have differentially fallen, stone formation did not show a differential response.
Soygur Trial. Patients stone free or not after SWL were given 60 mEq/d potassium citrate in 3 divided doses and new stones or growth of fragments noted at 12 months. Stones were CaOx. Details are in the spreadsheet. About half of the patients had urine citrate excretions below 320 mg/day – their cutpoint for ‘hypocitraturia’. In the 20 citrate treated hypocitraturic patients mean urine citrate rose from 234 to 525 mg/d and from 343 to 718 in the remaining 26 who were not hypocitraturic. So reduced stone crystal formation – as one might put it – associated with increased urine citrate excretion.
Lojanapiwat Trial. Post SWL or PNL 76 patients were followed over 1 year for new stones or growth of stones. Stones were ‘calcium containing’ but I could not find more detail. Of these, 39 received potassium sodium citrate 81 mEq total citrate in three divided doses. Mean urine citrate was 304 vs. 259 mg/d and 305 vs. 405 mg/d, control vs. treated groups, baseline and at one year of treatment, respectively. So reduced stones were associated with an increase of urine citrate.
rSummary of the tials. The Hoffbauer trial poses real problems because urine citrate rose yet stone formation did fall. Better put, stone formation fell alike in treated and untreated patients. In the other trials, stone risk and stone rates fell in tandem. If I had to choose between more thiazide and more citrate trials I would vote for the latter because results are more variable.
Synergy Between Diet Sodium and Potassium Citrate
The trials offer no insight into the effects of potassium citrate on urine calcium, as opposed to urine citrate, and whether a synergy exists between diet sodium and urine calcium. We would expect potassium citrate to lower urine calcium by offsetting diet acid load.
 Among 197 patients selected only as consecutive studies in our kidney stone clinic, 32 had been prescribed potassium citrate (open circles on graphs) the rest no drug treatments. Those given potassium citrate had a higher urine excretion of potassium, higher pH, and lower urine calcium excretion, evidence for use of the agent. This link leads to the complete statistical analysis of these data.
Among 197 patients selected only as consecutive studies in our kidney stone clinic, 32 had been prescribed potassium citrate (open circles on graphs) the rest no drug treatments. Those given potassium citrate had a higher urine excretion of potassium, higher pH, and lower urine calcium excretion, evidence for use of the agent. This link leads to the complete statistical analysis of these data.
Urine calcium varied with urine sodium (Upper left panel). Those people taking potassium citrate (open circles) had significantly lower urine calcium excretion rates at corresponding urine sodium excretions – dashed line (detailed analysis in the linked document).
From the few clinical trials that provided both sodium and calcium excretions with and without potassium citrate treatment (upper right panel) those on the agent had lower urine calcium (open circles, statistics on page 9 of the link) and the lower urine calcium was statistically significant adjusted for the urine sodium. These data come from trials beyond those considered in this article.
The bottom two figures will be of interest only to a few scientists. They show urine calcium vs. the delivery of calcium out of proximal tubule and also delivery as a function of urine sodium, left and right panels, respectively. The analysis is on pages 4 and 5 of the linked document. Potassium citrate reduces urine calcium at any delivery but the p value is borderline (0.058). Potassium citrate reduces distal delivery adjusted for urine sodium (lower right panel of figure, page 4 of linked document) p=0.003. So potassium citrate reduces urine calcium and in part does so by increasing proximal tubule reabsorption.
The clinical message is this: Although data are incomplete and a proper trial needed, it would appear that reduced sodium intake and potassium citrate act independently to reduce urine calcium excretion, so they are synergistic, as are reduced sodium diet and thiazide. But the trials are not sufficient to confirm these as hoc observations.
Observational Data – Urine Supersaturations
Citrate can reduce urine calcium and raise urine citrate which would lower supersaturation, but will also increase urine pH which would increase CaP supersaturation. Once again, the trial data – shown above – are very limited. From our 197  observational points, however, we have some idea of what will happen clinically.
observational points, however, we have some idea of what will happen clinically.
Urine SS CaOx (upper left panel) is significantly reduced by K citrate, but the reduction for SS CaP (upper right panel) is not significant. SS CaOx does not vary significantly with urine sodium excretion with (dashed line, open symbols) or without K citrate treatment (lower left panel). It is much lower with K cit than without (6.63 vs. 3.72, sodium adjusted p<0.001. CaP SS varies strongly with urine sodium (F=6.2, p=0.014) and the sodium adjusted value for SS is lower in K Cit treated subjects (0.73 vs. 1.13, p=0.03). The details of the GLM are at the end of the linked document.
I suspect these shards of observational data will hold up in a prospective randomized trial. Differences are significant with only a few treated subjects, and the distribution of points is reassuring. So for the moment these data can be pressed into service as a guide to treatment pending a formal trial.
A STRATEGY FOR PREVENTION
Here is, so to speak, the payoff for all this reading and analysis. Essentially I offer my own clinical practices, but have offered the reasons my practices are as they are. I have based them on the analyses you just read, and you are free to inspect the data themselves and come to your own conclusions.
Before Treatment
Be Sure Stones are Active
I cannot say this often enough as nothing can prevent old stones passing. One needs to know what is there at the start and that new stones are forming in the kidneys or stones are passing not previously seen in the kidneys.
Be Sure You Know The Stone Crystals
Our purposes are to stop crystals from forming stones and given this purpose what could be more unfortunate than ignorance of those crystals. Old analyses are no guarantee for the present time. Things change. Stone analysis is not very expensive compared to unnecessary surgeries.
Be Sure the 24 Hour Urines Represent Life as Lived
How else to say this but that urine collecting is burdensome and people like to do it while at home whereas they live a majority of life elsewhere, on the go, working, and doing all those things we call real life. Likewise, once treatment begins, collections have to represent what is being done every day, not simply on collection days. When collecting urine, patients must not drink especially well, or follow diet guidelines especially well. Physicians cannot assure that urine samples represent life, but patients can and need to.
Use Fluids and Diet First
Raise Urine Volume above 2.25-2.5 l/d or more
I do not scruple or demur about fluid intake; no amount up to 5 liters a day is too much in an otherwise healthy person. Too much can make life unacceptable, so one compromises. But I try for the most a patient is willing to achieve.
The water trial achieved about 2.6 liters of urine volume, the diet trial about 2.1 liters – but there were other treatment measures. My own studies of supersaturation vs. urine volume point to about 100 ml/hour or about 2.5 liters daily, and the Curhan data place the minimum for absolute safety about 2.25 liters. So water intake to achieve 2.25 – 2.5 liters of urine flow will be perhaps 3 to 3.25 liters in a routine environment. It is a high goal that many will achieve perhaps only some of the time. Hot environments and extra physical activity require more water. Like every physician I remind patients that when their urine looks dark and concentrated it is concentrated, and crystals do not sleep.
What I say here about water and other treatments concerns idiopathic calcium stone formers without systemic causes of stones and without important systemic diseases that would affect such treatments as water loading, low sodium diet, potassium loading, or thiazide diuretics. I mention this here because patients can and should read this article and those with any significant medical concerns must always seek the opinion of their physicians in regard to treatments.
Prescribe The Kidney Stone Diet = US 2015 – 2020 Diet Recommendations
The recent US diet recommendations more or less exactly match the needs of our patients: Intakes are Sodium below 2,300 mg/d, Calcium 1,000 to 2,200 mg/d, protein 0.8 gm/kg/d, refined sugar below 10% of total carbohydrates, and potassium intake 112 mEq/d from fruits and vegetables. Other articles on this site detail the diet and the correspondences between it and the needs for stone prevention. Given vast resources have been spent to vet the science behind the health benefits of this diet for such major diseases as osteoporosis, obesity, diabetes, and hypertension, there is no need to scruple about its use in any idiopathic stone former unless one has some serious additional diseases.
Lower Diet Oxalate
GIven the evidence that 1,200 mg calcium intake markedly reduces urine oxalate, it may prove less arduous in practice to control urine oxalate than with the present much lower calcium intakes. I estimate that diet oxalate intakes between 100 and 200 mg/d will be adequate for most patients. Our oxalate lists are as reliable as we could make them thanks to the efforts of Dr. Ross Holmes and the basic excellence of the Harvard lists we started with. Our article culls out the highest oxalate foods, so pruning the food choices can be easier. The arduous nature of diet change is perhaps lessened by the wide variety of foods still available.
Because oxalate is an issue for stone formers and not for people in general, the need to place high calcium foods into meals that contain appreciable oxalate must be brought to our patients separately from information about the diet in general.
Test the Effects of Diet Change Before Prescribing Drugs
Effects on Subsequent 24 Hour Urine Collections
My approach is to make the changes in hydration and diet, and see what happens to urine stone risk factors – urine supersaturation especially. If things are changing for the better, and there seems some room for more fluids or more diet change, patients are probably well advised to make those changes and measure again so as to achieve the most that they can achieve.
The caveat is that the urine collections be realistic reflections of life as lived. This means that the diet and fluid changes are universal not simply reserved for days of collection. If fluids and diet changes lower supersaturation well below what it was when stones were active, the use of a drug is hard to justify unless patients say they cannot or will not pursue these measures long term or despite lowering of supersaturation stones continue to form. This latter simply means that relevant supersaturations are still too high.
Effects on New Stone Formation
Many patients form no more than a stone every year or so, and if fluids and diet lower supersaturation in multiple samples I am in favor of waiting to see if more stones in fact appear. But this is said with reservations in all dimensions. Patients have their own desires as to level of protection vs. risks and troubles of medications. There are innumerable subtleties – single kidneys, kidney damage, many kidney stones in place, very high rates of stone formation, special risks from stone passage, job or other life situations that make another stone a special problem, pain medication issues that are better served by promptness. Even so, I push back against prescribing drugs at first in hope of the best control as a baseline on which to add medications – sodium, water, sugar, calcium, and oxalate.
In this matter of achieving the best from conservative measures and best timing of medications resides the very soul of medical practice. That is why I cannot put what I do on the page in a simple manner, and why I despise stepwise guidelines that pretend to substitute for real encounter with the complexity of human goals and of life as lived.
When Should Fluids and The Kidney Stone Diet Begin?
It is Best Begun After One Stone
 In 1994 I reviewed our experience with the outcomes of treatment in patients – all men, I am afraid, because of limitations of numbers – to the number of stones that patients had formed before treatment was begun.
In 1994 I reviewed our experience with the outcomes of treatment in patients – all men, I am afraid, because of limitations of numbers – to the number of stones that patients had formed before treatment was begun.
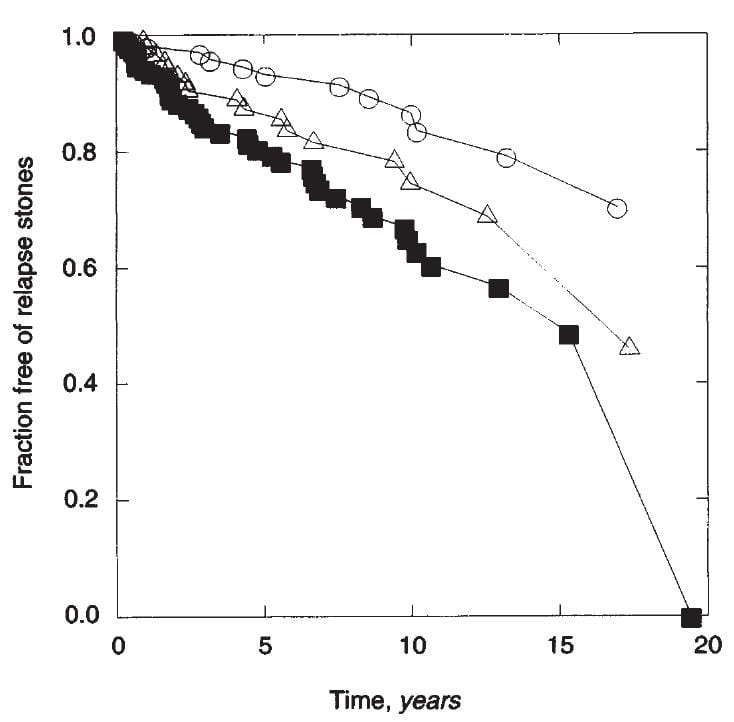
Although these are not trial data, merely observations, we had a long time of treatment – along the horizontal axis. Also treatment was never one thing but whatever mixture of fluids, diet, and medications that seemed right – I was taking care of patients not doing research about that care.
The people who had formed only one stone before treatment (open circles) were about 85% stone free at about 10 years 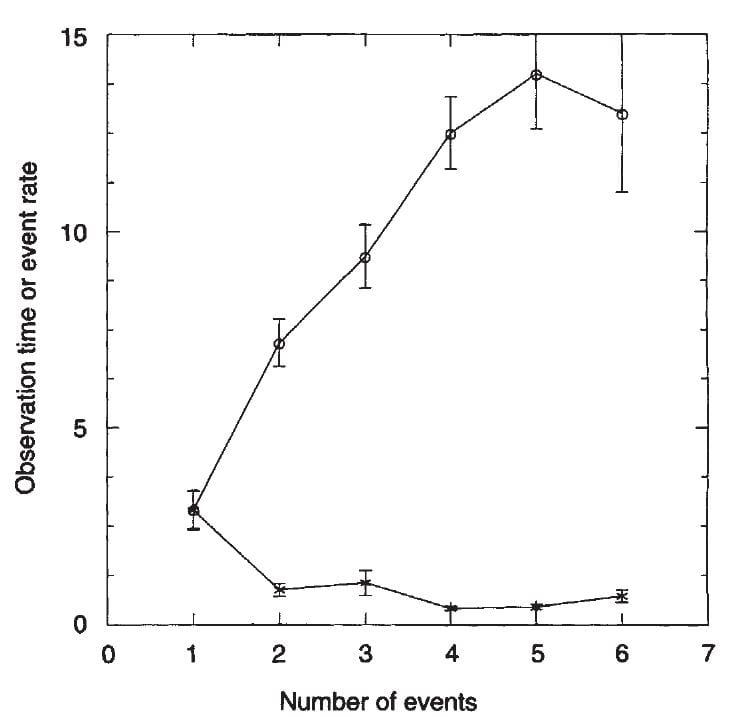 (about 15% had relapsed). Those with 2 stones (as we counted this would have been two clear stone episode periods each of which might have contained more than one stone) were less responsive to treatment, with about 25 – 30% relapse at 10 years. Those with many stones – 3 or more dated episodes and as much as 10 or more stones did least well, about 40% relapsed at 10 years. As this is a life
(about 15% had relapsed). Those with 2 stones (as we counted this would have been two clear stone episode periods each of which might have contained more than one stone) were less responsive to treatment, with about 25 – 30% relapse at 10 years. Those with many stones – 3 or more dated episodes and as much as 10 or more stones did least well, about 40% relapsed at 10 years. As this is a life
table, there are a lot of statistics, and they are in the paper.
Among these same people we could reconstruct the time course of stone formation before we
ever saw them clinically, using our detailed records. The graph to the right plots time of pretreatment observation (gray circles) and rates of stones/year against the number of events.
A rising number of dated stone events was associated with a longer time
between the first stone and entering our program. For example those with one episode came only 2.5 years after the first stone. This graph means the obvious – if you wait more stones may form, and more stones implies a less ideal outcome from stone prevention efforts. That the rate remained flat means the same: Stones formed over time at a more or less constant rate.
This was all observation, so I analysed the trials that I have already summarized for you earlier in this article and asked if the fraction of patients who relapsed despite treatment rose  with a larger number of pretreatment stones. This was not easy because it was not always clear just what was the pretreatment stone average – individual data were impossible to find in most cases.
with a larger number of pretreatment stones. This was not easy because it was not always clear just what was the pretreatment stone average – individual data were impossible to find in most cases.
On the vertical axis I placed the percent of treated patients who relapsed. I had no interest in the placebo cases for this analysis because my question is whether more pretreatment stones prejudice the outcome of treatment efforts. On the horizontal axis is my best estimate of the average number of pretreatment stones in the treated group. I emphasize this is very hard to be sure of, so the graph is an approximation.
Even so the results are remarkable. Relapse despite treatment tends to rise with an increasing number of pretreatment stones. The three points marked ‘Mulit’ are from my paper. I knew the numbers of pretreatment stones exactly. The points at 1 stone are my single stone formers and the single stone formers from the Borghi trial. The others are labeled with the treatments used. The axes are logarithmic because of crowding in the lower ranges,
I cannot use this kind of data to test a scientific theory – too indirect, but I can use it to ask whether the kidney stone diet is worthwhile early on.
It Is Appropriate for Family Members
Stone formation is highly familial. One reason may be the marked tendency for hypercalciuria in the immediate relatives of calcium stone formers which we have documented in children. Because the kidney stone diet is essentially identical to what is recommended for all American people – absent the high fluids and specific attention to oxalate – we certainly should advocate for it in relatives of calcium stone formers.
Add Medication To the Best Fluid and Diet Control Possible
Thiazide
In the absence of other compelling reasons, I add thiazide when stone activity continues despite increased urine volume, reduced urine sodium to below 100 mEq – 2300 mg sodium intake, and I have come to believe I cannot lower relevant supersaturations further with more fluids or less sodium intake or reduction of sugar or animal protein loads. Or, as I just said, when patients are not willing or able to maintain diet and fluid changes.
I strongly avoid adding thiazide when sodium excretion is above 100 mmol/d because it will be less effective and potassium wasting a common problem. I also cannot justify thiazide when urine calcium excretion is already low, below the Curhan lower limit for risk of 200 mg/d.
My own preferences are for indapamide or chlorthalidone as opposed to hydrochlorothiazide. The latter is short acting and has been tried mainly in twice a day dosing which is less convenient for patients. Personally, as opposed to the trials, I begin with 12.5 mg of CTD in most cases and often achieve good lowering of urine calcium and supersaturations. This is because I try to control diet sodium before using the drug.
Potassium Citrate
The US diet calls for 112 mEq of potassium from fruits and vegetables, which is about 60 mEq/d more than present diet averages. For this reason, actual use of the diet should raise both urine potassium – a sign of proper usage, and urine citrate. This latter is because potassium from these food sources will generally be with organic anions that are metabolized in their acid forms. This means a proton is taken up with metabolism, so new bicarbonate will be produced in the blood and such bicarbonate may commonly reduce NaDC1 transporter rates and increase urine citrate.
Potassium citrate pills should therefore be for people with calcium stones and presumably a low enough urine citrate excretion to make such treatment worthwhile – below 400 mg/day despite the kidney stone diet. I understand we have one trial of the agent in people with substantially more urine citrate.
From our observational data, low sodium diet is synergistic in lowering urine calcium and therefore should lower supersaturation. Likewise, although it increases urine pH, potassium citrate lowered urine CaP SS in our observational patient cohorts. Of course, I use this agent for potassium replacement for thiazide hypokalemia. My typical starting dose is 30 mEq/d in three divided doses.
Choosing Between Thiazide and Potassium Citrate
I do not think of this as a matter of taste. Thiazide seems appropriate when urine calcium remains above the Curhan risk limit despite all that can be done with diet, and either supersaturation is not lowered at least by half from baseline, or it has been but new stones are forming. I mention again, because names are confusing, that hypercalciuria used to be defined as against the distribution of values taken from non stone forming control populations. This is fine for physiology research but no longer tenable given the real nature of the urine calcium – stone risk relationship. Therefore the old statement that thiazide is a choice in even ‘normo-calciuric’ patients is misleading; most may have had urine calcium levels above 200 mg/d.
Potassium citrate seems appropriate when urine citrate excretion is below the Curhan risk limit despite diet. Because citrate action is complex, on urine calcium and as an inhibitor of crystallization, a low value seems to call for correction. When urine citrate is already above the risk threshold I am willing to use the agent to correct hypokalemia from thiazide, and usually do so. Because potassium depletion lowers urine citrate, the agent is often appropriate for that reason.
This reasoning means that from time to time I use both agents in an independent manner – for higher urine calcium and for lower urine citrate. No trials have explored their combination.
Calcium phosphate stone formers pose a special theoretical issue. Potassium citrate will increase urine pH and unless sodium is controlled urine pH increase will tend to increase urine CaP SS. No trials have tested this agent for CaP stones per se. I use it but with low diet sodium and attention to whether urine citrate and CaP SS increase and try to make a best judgment.
Allopurinol
I personally do not use this drug in my own work even though I am indeed the person who first put forth the idea that it might prevent stones. In principle, for patients who cannot take thiazide or potassium citrate, have recurrent stones, and all other treatments have proven unsuccessful I would use it at 200 mg.day. In his trial report Ettinger mentioned that it was unlikely the drug would work only when urine uric acid excretion was high, but he had no more reason for this comment than I do in these comments. We have the one trial which is sound, and a treatment that lacks a mechanism and so is difficult to endorse. But although a mere empiric remedy it can have its uses.
What if You Need Help Getting the Diet to Work?
In my practice I find it very difficult indeed, and I know lots of physicians find the same. As for patients and their families, diet is hard to change and even harder to maintain over time. My writing partner, Jill Harris, provides help via the internet, and if you would like to have some here is where to find her: Jill Harris’s Kidney stone diet site



Dr. Coe, thanks for continuing these studies an articles. I do look forward to them, and since moving from
Chicago 2 months ago, I follow that low sodium, higher food calcium, high water intake that you have
prescribed for me. I have been able to keep the stones that are in my kidneys from getting larger, and
have been satisfied that the lower sodium that I am careful about has been a positive influence. Thanks
Hi Midge, I hope you are happy in your new home and I am very happy that your stones are under some control. Stay careful, and perhaps their days are numbered! Best, Fred
Thank you for the Kidney Stone information. I think it will be some good bed time reading….
A little background info: I started having my first kidney Stones in 1974. my stones are always Uric Acid with an aver
af=gwIt all started, like you flicked on a light switch. The ripping & tearing intense Painit was instanous instanious At that time
Hi Michael, Some of your comment just never got through but the big part did. If your stones are entirely uric acid they should have never continued and can be stopped now. Just take sufficient potassium alkali – your physician knows all about this I am sure – to raise your urine pH above 6 and uric acid cannot crystallize. If there is a calcium component that is a separate issue and here is a good way to think about prevention for it. Regards, Fred Coe
DEAR PROFFESOR
WHAT ABOUT THE INFECTION STONES ??? THE CURRENT TREATMENT CONSIDER METABOLIC ACTION??
I presume you are Dr Vasquez; The question is very important and I have not at all done justice to it. But it is true that metabolic stone formers can become superinfected and form both calcium oxalate and struvite stones and present a dual treatment problem. I hope to have something about this sooner than later. Thank you for bringing the topic up. Warm regards, Fred Coe
Dear Dr. Coe, is there a benefit to knowing blood oxalate levels as well as urine levels? I am asking because my Calcium oxalate stones began when I suffered symptoms of IBS I am trying to understand the connection between bowel inflammation and oxalate, and does the bowel play a role in oxalate absorption. My urine oxalate level was very low when tested, but I was wondering if oxalate should could exist in blood and cause bone problems or stones?
Hi Nancy, I believe I already answered this for you in another string concerning low oxalate diet. Serum oxalate levels are not useful for any stone disease except possibly primary hyperoxaluria where such values have a specialized role not so much in stone prevention but kidney disease monitoring. Since you report a low urine oxalate level such serum measurements would be of no value to you. As well, diet oxalate is not of real interest and your stones would likely be from some other cause. Regards, Fred Coe
This is a handy explanation of may things to help with calcium stones, thank you! I am saving it for future reference!
Have you any experience with or opinion of magnesium oxide and B6? A study from 1974 showed it reducing stone recurrences from 1.3 stones/year to 0.1 sones/year (the only text of it I can find is here: https://www.researchgate.net/publication/18750548_Magnesium_oxide-pyridoxine_therapy_for_recurrent_calcium_oxalate_calculi ), and a more recent study from 1993 showed the changes in the urine chemistry as “leading to a significant (P<0.01) decrease in CaOx risk index from 0.09±0.04 at 0 day to 0.05±0.02 after 120 days of treatment." ( http://link.springer.com/article/10.1007/BF00571844 ) It's not clear to me what the "CaOx risk index" is, but a nearly 50% reduction in that from the 1993 study and a 92% reduction in the incidence of stones from the 1974 study look more impressive than the roughly 50% reductions in the various other treatments discussed in a 2012 AHRQ report ( https://www.ncbi.nlm.nih.gov/pubmed/22896859 ). Interestingly, however, that article claims that magnesium didn't seem to help (or at least that any evidence about magnesium was weak), but the only study using magnesium in that book was as a monotherapy (without B6), used magnesium hydroxide (which seems to have low bioavailability) and was underpowered (RR, 0.65 [CI, 0.37 to 1.16], n=1 trial), in addition to the report's authors seemingly being unaware of the earlier studies on B6 and Mag oxide.
Hi, Your reading of the literature is very astute and I agree with it. The earliest report of magnesium – not a formal trial – was encouraging, and magnesium lowers calculated CaOx saturations so it should be useful. The risk index was a composite of saturation and growth, not very pure. But there are no real trial data comparable to the thiazide and K citrate or even plain water. Sometimes I think people made a mistake not doing a real magnesium trial, sometimes I think it is high risk of low effect size and poor publishability. The old articles are very hard to get, too. So, everything you say seems right to me, and I agree. Perhaps I should review all these papers on the site for completeness – now that you bring the matter up. Warm regards, Fred
Thanks for your thoughts!
I’ve been recommending the B6 and magnesium (usually not oxide, but a better absorbed form) for years and have seen very few recurrences of stones, but my volume of people with stones is so low that it’s hard to draw much conclusion from my experience.
Thank you Dr. Coe for this series about diet and renal stones.
I have had two CaOx stones about 8 years apart. A CT at the time of the first showed 3 additional renal stones/calcifications. No follow up or US since then.
The 24 hr urine (abbreviated) done with this most recent stone:
CALCIUM UR 47 mg/24hrs <250 mg/24hrs
OXALATE UR 124 mg/24hrs 320 mg/24hrs L (just barely)
PH UR 5.7 5.5 – 7.0
TOTAL UR VOLUME 2.08 L/d >2.00 L/d
SODIUM UR 91 meq/d <200 meq/d
The urologist's advice; fluid, low Na, reduce oxalates, and no mention of Calcium, but suggested the possible addition of Urocit-K. I have increased Ca intake and fluid, and reduced high oxalate foods and Na intake.
Is there any reason to take the K citrate, especially since the one or so daily Ca supplement (~200mg Ca) is in citrate form, about 10meq per tablet.
Is ingested Calcium lost to the body in the process of blocking/reducing absorbtion of dietary oxalates? What is its mechanism of action?
Thanks
Hi Les, The urine data are out of order. I think the oxalate is 47 mg/day which is high and the calcium is 124 mg/day which is low. The pH is high at 7. I would use high calcium foods to lower the urine oxalate and redo the measurement. The urine sodium of 91 mEq/day is good. Regards, Fred Coe
I muddled that a bit though the Ca and Oxalate were as reported. Does the citrate or CaOx value offer any additional indication that the reported Ca and Oxalate may have been incorrectly reported by the lab? The values below are copied and pasted as reported along with the lab normals.
Range
CALCIUM UR 47 mg/24hrs <250 mg/24hrs
OXALATE UR 124 mg/24hrs 320 mg/24hrs L
PH UR 5.7
VOLUME 2.08 L/d >2.00 L/d
SODIUM UR 91 meq/d <200 meq/d
CALCIUM OXALATE 1.49 <2.00
Hi Les, The urine calcium is very low. The oxalate of 124 milligram (mg)/day is very high but as the normal is given as 320 mg/hour I think the units are micromole – that would be 32 mg/day roughly. Whereas your urine value could be anything the range of normal cannot and the upper limits for urine oxalate are order of magnitude 30 – 40 mg/day not 300 mg/day. Check the units. If you are in the US mg/d is usual, in Canada and UK it is mmol. Let me know. The low calcium is often low calcium diet, vitamin D deficiency or bowel disease – I cannot tell from just numbers. Regards, Fred Coe
These values did not transmit correctly: Oxalates were 124 with the normal 320mg
Sorry for the multiple emails but there seems to be some problem with formatting, the following was omitted:
And Citrates at 319 with normal of >320mg.
Is citrate good for stones that contain uric acid, cystine, struvite
Hi Steve, Potassium citrate is specific for uric acid stones that are prevented by an alkaline urine pH. It plays a modest role in cystinuria and none at all for struvite stones. Regards, Fred Coe
Dr. Coe,
What would you advise to be included in a nephrology work-up for a post-menopausal woman with IH, osteoporosis but no stones to date – but who has a family history of calcium oxalate stones? Also, I’m confused about the degree to which I should be minimizing oxalate consumption as part of your advised overall diet/H20/salt program.
Many thanks for your invaluable postings!
Mary
Hi Mary P., Your most likely problem is estrogen loss coupled with idiopathic hypercalciuria. Treatment is very low sodium and high calcium intakes. Oxalate means nothing given no stones. High fluids likewise. Best, Fred Coe
Thank you, Dr. Coe! I was making myself somewhat crazy avoiding oxalates and drinking water. Would you recommend a nephrology consult for me?- and, if so, with what labs? I’m having blood work and a 24 hour urine for an upcoming 6 month bisphosphonate evaluation anyway, so could see a local nephrologist about possibly adding to those orders.
It’s unfortunate that our system is not more prevention oriented; can you imagine how much suffering your advice has alleviated?
All the best,
Mary
Hi Mary P, I do not see what a nephrologist would add. Look at your 24 hour urine calcium – your bone physician will, too – and consider low sodium diet as an addition to the bisphosphonate. Also you need a lot of calcium, so be sure and eat at least 1000 mg = with your meals. Essentially the kidney stone diet sans oxalate precautions and fluids is fine. Regards, Fred Coe
Thanks again, Dr. Coe! I finally feel I have clarity about how to proceed. Perhaps this information is helpful too for the many osteoporosis patients with underlying IH.
All the best,
Mary P.
Hi Dr. Coe
I am 31 years old and had my first stone at age 18 which required blasting because it was large. This is my 3rd time now with stones. I have 3 siblings, 2 of my siblings and both parents have had multiple stones. I have been diagnosed with hypercalciuria and my calcium levels read about double the upper limit. My stone analysis reads calcium, oxylate and phosphate. I have increased my fluid intake, I try to take calcium with meals, and take vitamin b6 200mg/day. Would you recommend taking b6, i was told by my doctor that it would reduce stone formation? I was wondering if I should be supplementing calcium and is tums and adequate form. Also would you recommend potassium citrate, also would lemon juice be an adequate substitute for postassium citrate? Thank you.
Hi Shane, You have raised your diet calcium but I hear nothing about sodium. The plan is three way: lower urine calcium – to 1500 mg or so; raise diet calcium – bone protection, lowers urine oxalate; raise urine volume above 2.5 liters/d. You need to do new 24 hour urines and see if all the changes occurred: higher volume, lower sodium, lower oxalate. B6 has no role. Potassium citrate or thiazide is used when you cannot control things with diet and fluids. Check out the latter parts of the article – this one you have written to. Regards, Fred Coe
Hi Dr. Coe,
I am a 29 year old female, and I just had my first and hopefully only kidney stone. Both of my parents and all 3 of siblings have had them. I believed it to be their lifestyles causing them, however now I’ve had one and am unsure. I have a high water intake (2-3 liters a day), and low meat intake (once a week if that), and I dont add salt to things but I definately am going to keep track of that better and make sure it’s low.
My lab results for the 2mm stone were 50% Calcium Oxalate dihydrate & 50% Carbonate apatite.
My question to you is, how important is genetics when it comes to these types of stones?
More importantly, will a supplement/vitamin with Calcium suffice for appropriate Calcium intake? I’ve read that they can cause more harm than good as opposed to getting Calcium from food. Which doesn’t make sense to me because i was taught that a body will use molecules as needed regardless of origin.
Thank you for this very helpful website.
-Kasey. …..now a stone sufferer
Hi Kasey, You form calcium phosphate stones ( the high carbonate apatite), and really need to pursue prevention. Genetics matter but we cannot treat them, so we do what we can. The article you read is one my favorites and gives the rationale for the high diet calcium – to block oxalate intake. Here is a more detailed article about that – the timing of the calcium to match larger meals matters. For prevention we are best with the entire kidney stone diet – Meds are add-ons and sequential 24 hour urine testing essential. Regards, Fred Coe
Dr. Coe,
Thank you very much for your help. That article was very helpful indeed. I’m looking forward to reading more of your articles.
Gratefully,
-Kasey
Hi dr. Coe,
Thanks for such a comprehensive article.
My 24h urine calcium = 6mmol
Oxalate = 678 umol
Citrate= 1 mmol
Urate = 4.8 mmol
Urine output daily is around 3-3.5l on average , water intake is around 2-2.5l daily.
Other than reducing oxalate foods and sodium and getting more calcium (I don’t get anywhere near 1000mg). Should I be trying to increase citrate? If so , can consuming a couple of medium sized lemons a day (after meals) be helpful in my case?
The other urine results were normal as were the blood results.
Many thanks !
Ray
Hi Ray, It is no one thing but all parts of the kidney stone diet that matter: high food calcium timed to where oxalate is, low sodium as noted, high potassium anion from fruits and veggies, low refined sugar, care with diet oxalate, fluids. The goal is to lower supersaturations – as in the article. If citrate will not rise with 5 servings of fruits and veggies, one might want to raise it, if supersaturations are still high – not reduced by half. I love the article you read, it is my best on on the topic. It does not mention lemons because focus on any one fruit is poor – most fruits have potassium anions that convert to citrate. Note, your urine volume exceeds your fluid intake by a lot – I suspect you drink more than you say; water from metabolism rarely is so large. Regards, Fred Coe
Many thanks dr. Coe, I will take on board all your advice, specifically the timing of calcium and fluids to match oxalate. I start a new 2l bottle of water each day and usually don’t go much over this, I do urinate quite a lot naturally even when I don’t drink much , is this a bad thing ? My urine pH is usually a bit on the higher end e.g 6. Thanks Ray
Hi Ray, It is a good plan; the trials are decent. Good luck with it. Regards, Fred Coe
Dr Coe,
My daughter is 4 years old and was born with classic Bladder Exstrophy. She has been cared for by Dr. Gundeti at Comer since the day she was born. Over the last two years she has had rapidly occurring bladder stones. She had her 6th procedure in 18 months for removal this past March and is already showing signs of stone formation again. Her most recent stone report shows 7mmx8mmx5mm stone (1 of 5) 100% Calcium Carbonate Phosphate (carbonate apatite). She is currently being treated with Diuril and Hiprex as well as Nitrofurantoin and Gentamicin bladder flushes. We also try to push more fluid, but it is difficult with a 4 year old.
Here are some of her latest 24hr urine results:
-SSCaOx – 4.54
-Ca 24/KG – 7.1
-pH – 6.863
-Cit24 – 251
-Volume – 1.2L
We are not sure where to go from here and cannot have procedures done every three months. Can you offer any advice or point us in the right direction?
Hi Pat R, As it happens Comer is the hospital for Children where I work – University of Chicago. Her physicians can contact me directly and I can try to help with stone prevention. She is forming calcium phosphate stones and one can try to prevent them, although the work is technical – that is why perhaps her physicians could contact me directly. Regards, Fred Coe
Hi! I need to know if its ok to have a cloudy urine when it is alkaline (ph 8-9)…when I add a drop of vinegar it instantly turns clear. I read that this might be phosphorous crystals that form in an alkaline urine that dissolve when acidified with vinegar? But is this harmful? Does it need treatment? I’ve asked 2 Doctors about this and they didn’t seem to care once urinary infection was ruled out… but it concerns me… Please let me know if this is harmful, why it happens, can this be a sign of stones?
Hi Kristina, your’s is a most intriguing note. Of course you form calcium phosphate crystals but no stones, I gather. It may be a sign of genetic hypercalciuria, a trait that predisposes to calcium stones and bone disease because of high urine calcium losses. Your physician can order a 24 hour kidney stone urine panel – LabCorp/Litholink is very good for this. Your physicians can identify the crystals by microscopy, as well. It might be worth a simple flatplate xray looking for stones – not likely. Regards, Fred Coe
I forgot to mention the cloudy phosphate urine occurs 1-2 hrs after a meal that contains calcium ( lots of cheese/dairy )… this cloudy urine is always alkaline (9). All acidic urine is clear. I’ve stopped consuming dairy to avoid any problems from this and I’m able to avoid the cloudy urine, but if I have a high calcium meal and alkaline urine it reoccurs. The cloudiness becomes clear when vinegar is added to the cup.
Thank you for your time and knowledge!
Hi Kristina, your experiments confirm my suspicions that you have genetic hypercalciuria. Take a look at my prior answer. If so, low calcium diet can raise risk of eventual bone disease and is not an acceptable alternative. Read about the condition and consider getting tested. Above all do not limit diet calcium. Regards, Fred Coe
Thank you very much for the reply it is most informative! I’m grateful for your warning about limiting calcium and bone disease, I had not even considered it before.
I have a question, if I take a calcium supplement or eat calcium rich food to prevent bone disease -would keeping my urine acidic after the meal with cranberry juice help prevent calcifications from forming inside the kidney? Or the crystals I see in cloudy alkaline urine form only once they reach the bladder?
Also please tell me which type of calcium supplement is preferred when avoiding kidney calcification. Do you suggest Calcium citrate/carbonate/phosphate or other? Magnesium?
I am very grateful for your articles and answers, many many thanks!
Hi Kristina, the key is to lower diet sodium, so you need not this or that but the whole proper diet – all of it in one unit. Acid is not the treatment; the diet will do it if you do the diet. Supplements are my last resort, I dislike using them and rarely have to. Regards, Fred Coe
CT scans and X-rays have determined that I have a 5 mm stone in my right kidney. It has been there for many months.
My lab tests are showing 3+ urine hemoglobin and 51-100 RBC’s and have been for multiple months. I am concerned
because I test my urine at home every day with Siemens Hemastix and every day I show from 3+ on early morning specimens to a trace to 1+ later in the day when I have been ingesting large amounts of fluids. Shouldn’t this daily slow
bleed for multiple months be a concern? My Urologist does not seem to be concerned and has only recommended diet
changes similar to what you advocate a long with Urocit K. I am worried that my kidney could be damaged by this
daily slow bleed over multiple months.
Hi Kurt, One presumes the stone causes the bleeding. But proper practice for urologists is to investigate to be sure it is not something more. Let your urologist know about the 3+ urines so s/he can be sure you are not bleeding and also have a stone. The blood need not mean kidney damage, but your physicians need to be sure of that – there are kidney diseases that cause bleeding. Regards, Fred Coe
Dr Coe,
Can the initiation of dietary changes and K Citrate ever reduce the size of established stones?
Thank you
Howard Kaplan, MD
Hi Dr Kaplan, Only uric and cystine stones ever shrink, in my experience. That’s why I seem preoccupied with prevention. Warm Regards, Fred
Dr,I have 4mm stone in right kidney,If I drink lemon juice will it dissolves the stone,Pls suggest me a natural remedy to dissolve the stone.
Hi Raja, No, lemon juice will not dissolve your stone unless it is uric acid – your physician can help decide if you have had a CT scan. For the common calcium oxalate stone, the ideal diet is indeed natural, and will do a lot but you have to have 24 hour urine testing to really organize and monitor your treatment. This article is the best one concerning prevention, and I would recommend reading it and trying to follow the advice in it. Here is another one that is perhaps less technical. Regards, Fred Coe
I started having issues with oxalate stones 10 years ago, the CT scan showed a dozen at that time. I started drinking more water and started taking the following 2 times per day: 160 mg of magnesium citrate, 99 mg of magnesium citrate and 300 mg of calcium citrate (plus 1/2 of Greek yogurt at lunch). I thought those measures had worked as follow up yearly x-rays for 3 years indicated no stones. Three years ago I started suffering occasional bouts of extreme bloating and stomach pain every few months but did not feel like it was a kidney stone. No issues were found with an ultrasound, colonoscopy, or endoscopy. Then January of this year when I know I passed a stone and a second one a few months later. A recent an x-ray showed I now have 5 , the largest is 4 mm. I drink over 2 liters of water daily and I have been trying to reduce my high oxalate diet. I have upped my calcium intake to 1000mg daily with 600 mg of calcium carbonate/citrate taken in the morning and 400 calcium citrate at lunch, then I take 400 mg of magnesium carbonate at dinner. The magnesium carbonate is what is in my powdered multi-vitamin (I would have preferred mag citrate). I want to add citric acid powder or capsules to my diet instead of using additional mineral supplements just to get the citrate and would like to know how many mg of citric acid you would recommend and how often? Do you have any other suggestions. Thank you very much for your help.
Hi Linda, I am not sure if you are forming new stones or not. You had dozens of stones on CT 10 years ago but perhaps your new x rays are not CTs but simple flat plates that have very low sensitivity. Were your interim x rays misleading and your newest one another CT? If you are indeed forming new stones despite these questions, then the article you are reading has in it my best on prevention. I see you are eating calcium, which can help with oxalate, but I see nothing about sodium; the magnesium has no proven role at all. Likewise I see no 24 hour urine monitoring. Might I suggest you review the article – here is another one from a different perspective – and see if you can make a better pattern of prevention for yourself. Regards, Fred Coe
There has been no CT scan since 10 years ago. Since the recent kidney stone episodes I started going to a urologist again.The X-ray last month that showed the multiple kidney stones was digital kidney, when they were doing the follow up x-rays 7 to 10 years ago they were not digital. The new urologist did a 24 hour urine analysis and my oxalate level was 62mg. I have always eaten a low sodium diet and avoid fast food and processed foods. I was looking at the Harvard Goggle Spreadsheet List posted by J. Harris this morning, it lists “Stevia Sweetener” as 42 grams per tsp, I think I read something last week where you said processed stevia does not have oxalate, it that right? I use about 3 tsp a day.
Hi Linda, Processed stevia has no oxalate and your high oxalate suggests low calcium diet and/or other sources of oxalate. What else did your urologist find? What kind of stones do you form? Regards, Fred Coe
I need to correct my oxalate urine level, I double checked my lab results and it was actually 52 mg, not 62. . The large stone that was analyzed when I was first diagnosed was oxalate. I weigh 127 lbs so I think my water consumption is very good. My recent 24 hour urine analysis had a total urine volume of 3500 ml. The test results were:
Calcium 263 mg
Oxalate 52 mg
Uric Acid 665 mg
Citrate 948 mg
I was previously taking calcium citrate capsules twice a day for a total of 600 mg, and 1/2 cup greek yogurt at lunch. Since the urinalysis I now take 800 mg of calcium, along with 1/2 cup of greek yogurt at lunch, which puts me close to 1,000 mg. I just began taking 1/2 teaspoon of citric acid with every meal. I used to eat 20 almonds at lunch and 20 more after dinner, along with a few bites of dark chocolate. I have started soaking the almonds and draining the water off since I have read that helps remove some of the oxalate and I am eating at total of between 10 to 20 per day now. I have cut back on eating high to moderate oxalate foods by at least 25%, but I still eat 1/2 cup of blueberries with my yogurt, I cut out the raspberries & blackberries. I am trying to avoid taking large doses of citrated minerals such as potassium just to get the citrate. Do you think taking the 1/2 teaspoon of citric acid with meals containing oxalates, like potatoes, etc. will help prevent stones? If so am I taking enough? Thanks for your advice, I really appreciate it.
Hi Linda, Food oxalate concentrates like almonds are a problem. Try to eat them with dairy product to block oxalate absorption, and the same for blueberries or other berries. It is all about timing calcium to go with the oxalate loads. As you coordinate this, if urine oxalate stays high you will need to reduce the high oxalate foods. Citric acid is of no use at all; it is eliminated in urine unchanged and does nothing to help with stones. So, stop it. Regards, Fred Coe
Thanks for your help! I double checked my 24 hr unine analysis and need to correct my oxalate level, it was 52 mg, not 62. My volume was 3500 ml, uric acid 665 mg, citrate 948, and calcium was 263 mg. I have been cutting way back on oxalate foods and I have started taking 800 mg of calcium a day, plus another 200 mg from yogurt. I also just started taking 1/2 tsp of citric acid with meals since it is impossible to completely avoid oxalate. Do you think the 1/2 tsp is a good dose as a replacement for drinking lemon or orange juice (with too much sugar) ?
Hi Linda, I answered you already about this. Please check your other query. Regards, Fred Coe
Hi Dr. Coe,
I haven’t had a kidney stone and ultrasound looks clean, but I have idiopathic hypercalciuria and osteoporosis. Non-drug methods (Na, Ca, etc) failed to reduce Ca/urine but 12.5 HCTZ cut it approximately 50% to 165.
So, here’s my question: if Ca “binds” with oxalates to reduce stone formation, does that “use up” some of the calcium that would be available to blood and might otherwise come from bone? Obviously, it’s best to reduce oxalates to the extent possible, but wondering if that’s an effect (i.e. stealing a little from the bone column to mitigate the stone part of equation)
Thank you!
Hi Mary, No; oxalate has nothing to do with you. You need as low a diet sodium as possible, 1000 mg or more of calcium as food, and the thiazide can be helpful. Low sodium <1500 mg is ideal. The usual problem is too high a urine sodium. Remember, a low urine calcium from low calcium diet will not benefit your bones. Regards, Fred Coe
I was diagnosed with kidney stone upon Xray and microscopy test revealed i had calcium oxalte present and did chemistry and found out that i had cratinne of 1.4mg/dl. Please what drug will i to get rid of the stones and further prevent its reoccurence?
Hi Austine, I gather the stone is calcium oxalate, and that you have an increased serum creatinine. This latter can signal loss of kidney function. Your personal physician needs to understand why your kidney function is reduced. One possibility is a very high urine oxalate level, and that is very important to test for using 24 hour urine collections. Prevention depends on cause; here is a good overview of how to go about it. Regards, Fred Coe
Hi, I am a 43 y.o. woman with a healthy low sodium diet. Started getting ca phosphate stones 4 years ago (discovered w/ infected 10mm stone trapped in kidney). At that time I was taking topamax at moderate doses for migraines. Quit that and urine ph is down from 8.5 to 7 but still have had multiple stone removals (4+ times) or just sent home to pass stones. Tried citrate tabs and sol’n 3 yrs ago but couldn’t tolerate bec. of gastroparesis and stomach pain.
Now I had ct scan of chest last June that also showed multiple 4mm kidney stones. I have an orphan collagen disease called sticklers syndrome and terrible arthritis. Know I don’t drink enough water when painful which seems to set off renal colic. I have been having bilateral flank pain/ renal colic for a month and they said I had uti with wbc in urine and a questionable skin flora cultured out 2x, 10,000-50,000 cfu/ ml.
I’m wondering if these smaller stones in kidneys are getting colonized by bacteria? Or if they just hurt in there. Treating w/ my other meds Zofran and tramadol. Or wondering if my cartilage breakdown could be affecting my kidneys? I have a pretty good diet but was encouraged to eat more animal protein due to anemia. I still don’t eat that much for an American. Have you any advice? I have worked to better my malabsorption issue, traced to wheat, but still the stones return.
Hi Anna, Certainly the drug would be prime suspect in starting your stone disease. I presume the stones are apatite, but you did not say. If infected with e coli, you may be getting pain in your kidneys, but that would neither raise urine pH nor promote more stones. If infected with organisms that hydrolyse urea to ammonia that would raise urine pH and ammonia, both, and your 24 hour urine testing surely reveal the problem. Likewise, the stone type could convert to struvite. The skin flora give no useful clues to the urinary tract that I know of. Stickler’s is a collagen gene variant, as you know, and has not been associated with kidney stones or kidney disease that I know of. I did review it on OMIM for this response. I would suggest your and your physicians review the details of your 24 hour urines and serums looking for any clues to why stones keep forming, and do this in the light of repeated stone analyses because after all you need to know what crystals you are trying to eradicate. From here, I cannot say much lacking almost all details. That you have enough pain to need narcotics makes the situation rather urgent. Regards, Fred Coe
Thank you for your reply. The stones are almost pure calcium phosphate which I know is unusual. My urine ph has changed from very high 4 yrs ago (8.5? 8?) to normal at last testing. But I continue to have symptoms of renal colic, nausea, loose bowels, flank pain after supposed resolution of the uti/kidney infection. I have been told the cause of stone formation may be a metabolic disorder. Kidney function is great. I do tend to be dehydrated because I don’t feel well.
It has not been my experience that drs consider severe pain to be urgent. I have terrific joint pain much of the time and that’s not adequately treated either. I’m thinking my high pain tolerance makes evaluators think I’m ok (for example, when in ER for that infected 10 mm kidney stone, the nurse didn’t believe I was sick but after opioids. Examining dr. cleared that up and said “you rate pain that takes your breath away as a 6? Wow.” I’m feeling like too complicated a case so they throw up their hands.
I will go back to the UW urology, having cleared up my ibd by eliminating gluten. Perhaps they’ll do another 24 hr urine study. I just wish they would take my pain seriously as I’m not one to cry or throw a fit. It’s rotten to be young and in pain all the time.
And yes, they’re apatite stones. Suggested renal tubular acidosis but why yet another medical problem is the question.
Hi Anna, RTA is often suggested in younger women with calcium phosphate stones. I doubt it. Urine pH is high because of other factors. Right not these are not amenable to direct clinical treatment, but you might want to bring the article to the attention of your physicians. It concerns normal women and men, but stone formers are the same – paper not yet in press. What usually makes the stones is a high urine calcium from idiopathic hypercalciuria, easily treated. Regards, Fred Coe
Hi Anna, Pure calcium phosphate is not unusual in younger women with stones, it is in fact common. Dehydration sounds like a major issue as it can perpetuate stones despite all forms of treatment, so the bowel issues need fixing. Regards, Fred Coe
I Looked back at 24 hr supersaturation test from 3 yrs ago. The abnormal values were 0.76 DG brushite, 5.69 DG hydroxyapatite. Vol 1.875 L. Nml Ca oxalate, nml Na, Ca, Mg, Cl, K, Ph, sulfate, nml oxalate and oxalate 2, nml Uric acid, creatinine, osmolality. Sodium urate 0.88 dg.
Last urinalysis (12.20.18, before 2nd antibiotic ) much improved from 12.4.18, pH7.0, everything nml/ neg except trace leukocyte esterase, wbc 5-10/ hf ; before 1st antibiotic ph 5.5 and wbc 10-30/ field and 2+ leukocyte esterase, very concentrated urine, too.
Don’t know if that’s at all helpful. I think I need another 24 hr study. I’m working on drinking 2+L per day and eliminating foods that cause intestinal difficulties/ diarrhea. Thanks for your patience and tolerance and advice, of course you are not obligated to further reply. But I would surely appreciate any insights.
Hi Anna, ‘Normal’ has a fictive element as urine ranges are so large. I would indeed get another 24 hour urine, and perhaps you might mention the actual urine values for calcium and oxalate excretion, citrate as well. Multiple stones usually have causes one can detect and alter. Regards, Fred Coe
I have had my first stone. I show several tiny stones in both kidneys. My 24 hour urine test shows pH 7.3, calcium 281.8, sodium 84.8, citrate 1006mg/24 hours, magnesium 121.5mg/24 hours, oxalate 40.0.
My physician recommends low sodium diet and high fluid intake. I do have osteopenia.
I have to admit I am scared. Im trying to increase my calcium directly from foods in my diet. I did talk with Jill, she’s wonderful and Im currently enrolled in the kidney prevention course. My parents are no longer alive, Im not sure if this is hereditary. I really don’t want to be medicated. I live in a small rural community, medical experts are very busy with little time. I do have another 24 hour test ordered, but not until June. Is there anything I can do nutritionally to lower my calcium levels in my urine. My maternal grandmother was diabetic and my mother died at 63 from kidney cancer. I am now 63.
Thank you! I appreciate your time!
Melody
Hi Melody, You have hypercalciuria, and that is a cause of both stones and bone disease. Idiopathic hypercalciuria is detailed in this article, and links point to the primary article from there. It is indeed inherited so if you have children still living with you a high diet calcium low diet sodium is important. Reducing diet sodium will lower urine calcium a lot, and if it is not complete one can add medication. Jill has already given you a diet sodium goal, and she is really expert. Regards, Fred Coe
Hi Dr. Coe.
I have a question about side effects of potassium-citrate therapy (as a matter of fact, potassium-magnesium citrate – 4K2+:2Mg2+:2Cit-3) (7 + 3.5 + 10.5 mEq/caps)). I prescribed 3-4 capsules/day to a patient with a first episode of bladder stones (removed by percutaneous suprapubic cystolitholapaxy), most likely secondary to a bladder outlet obstruction, of pure uric acid (normal serum UA and an average of 500 mg/day in the urine) to maintain a urinary pH between 5.7 and 6.5 plus high fluids. After a couple of months he complained of severe heartburn and an upper GI endoscopy revealed several gastric ulcers and an extensive area of gastritis, Helicobacter pylori negative. Biopsy showed acute gastritis. It is important to note that the patient has no prior history of gastric problems. Treatment with a PPI and stopping the pills resulted in a complete resolution after about a month, as demonstrated by another endoscopy.
Have you seen such a side effect of potassium-magnesium-citrate treatment? I am missing something?
I thank you in advance and commend you and your collaborators for an outstanding work on this important subject.
Yous truly.
Hi Dr Saldanha, The magnesium version of potassium citrate is not marketed in the US so I have used only the plain potassium citrate. With that product I have never seen something quite so bad, but lots of patients develop upper GI symptoms. You need alkali, of course, and perhaps sodium alkali is a good fallback. If your patient is hypertensive or otherwise not a candidate for more sodium, you can use my favorite which is a very low dose of a long acting diuretic like chlorthalidone 12.5 mg daily to help get rid of it. Warm Regards, Fred
Hi Dr. Coe
I am a 60 y/o W female Jill Harris zealot , who follows the diet very closely. Alas, I have IH and recently had a DEXA scan that shows osteoporosis. My question is about Vit D levels and optimum absorption of calcium. My level drawn in the summer ( with total calcium intake through food of 1200mg daily), was 27 which my urologist said was just fine-no supplement needed. I am wondering if I should be asking for more specific blood work to further assess if supplementation would help my poor bones? I am trying to understand all the factors involved in bone health and keep my risk for further kidney stones down. I worry that no one specialty really can incorporate the two problems and give me good advice. I live in Minneapolis and think Dr. Borofsky is a gem. Not sure if an endocrinologist would be advisable or stick with my urologist thoughts. Thanks for taking the time! Sincerely, Barb
Hi Barb, IH causes bone disease, variably, and often in a patchy manner. Partly it is because of renal calcium losses with inadequate diet calcium, partly there is something wrong with bone itself. If you are postmenopausal and bone mineral is at the fracture risk level a bone directed drug is appropriate. Thiazide, which is also a first line stone prevention, can stabilize bone mineral if diet sodium is indeed low. If that is not working then one needs to move on to the next agents – usually a bisphosphonate. Regards, Fred Coe
Hi Dr Coe,
Firstly, thank you so much for publishing these guides online. I have read much of this book and even reread many parts because some of this information is complex and is difficult to absorb with only one read. Please realize your work is positively affecting many of us suffering from stones and it is much appreciated. I am a brushite former and I started my diet of 1500mg sodium a day based upon your recommendations so thank you for encouraging a diet change (my baseline litholink showed sodium at 130-150 mmol/d and calcium loss at 300 & SSCaP 2.1, PH 6.8, UUN 24 = 10). I am hopeful my new diet will improve my urine calcium and show a corresponding decrease in SSCaP. Anyway, in your chapter discussing treatment of idiopathic calcium stones you said “I strongly avoid adding thiazide when sodium excretion is above 100 mmol/d because it will be less effective and potassium wasting a common problem.” I am trying to understand why a thiazide is less effective with sodium excretion above 100 mmol/day such that you feel strongly enough to avoid prescribing it in these circumstances. Would you be so kind to expound on this? If I cannot sustain my diet long-term this will be relevant to me. My interpretation of this is I must change my diet because if I can’t or won’t thiazide is not a viable option given my urine sodium. I was under the impression thiazide decreased urine calcium nevertheless.
Hi Traci, urine calcium varies with urine sodium in a very strong positive way, more so in hypercalciuric people like you than in normals. The link arises in the basic physiology of the kidney. Thiazide diuretics do not alter the slope of the calcium to sodium relationship but do shift the whole curve downwards by about 100 mg/d of urine calcium at any urine sodium. So, if you lower urine sodium – which is diet sodium – you bring urine calcium down along the slope, and then thiazide lowers it by that extra amount. If you leave sodium higher, you lose the sodium benefit. This means you will need more thiazide dose to get a given fall in urine calcium than you would have needed given a lower diet sodium. Given that thiazide has side effects and lower diet sodium has benefits – lower blood pressure, for example, I always try to lower diet sodium first. As for potassium, thiazide causes kidneys to waste it in proportion to diet sodium – also a consequence of how the organs work. So overall, you can use thiazide without controlling diet sodium, but you will use more than with a lower diet sodium, and have a higher risk of potassium wasting. I hope this helps. Regards Fred Coe
Hi Dr. Coe. I am primarily a brushite former and have had 3 stones in last 10 years all requiring ureterscopy. My Urine sodium is 110, Calcium 320, SS CaP 1.8, SSCaOx 3.26, citrate 448 and 516 on my last urine test. PH ranges 6.8-7.1 in all my 24 hour urine tests. I am on the 1500mg sodium diet. I have an appointment coming up and I would like to ask to be on 12.5 mg of chlorthalidone. Two questions: 1. Wondering if I should also ask to be on one 1080mg potassium citrate pill a day given my citrate is a bit lower than the 550 recommended or would it be best to not be on potassium citrate at all due to my higher PH ranges? I was previously on 4 1080mg potassium citrates daily and my citrate rose to 928 so I figure each pill must raise me about 100. 2. If my serum potassium is too low after being on the 12.5 mg of chlorthalidone, would it be best to supplement with amiloride or potassium citrate given my propensity for calcium phosphate stones. As far as the high PH goes, I have a digital PH meter and I am in the early stages of identifying reasons for these huge swings. It appears it occurs when I depart from my diet and over consume red meat but I don’t have enough data to make any judgement. Thanks!
Hi Renee, I think chlorthalidone is a good idea given what you say, and I see little benefit from potassium citrate as no trial has ever been done testing if for CaP stone formers, brushite or apatite. If your serum potassium falls I would be happiest with potassium chloride and, if needed, amiloride. Meat can raise urine pH, incidentally, because it contains considerable metabolizable anions as the potassium salt. Regards, Fred Coe
Thanks Dr Coe! Appreciate your insight and time. Also, greatly appreciate this site. Just curious about the potassium chloride. Do you recommend that in my case because it does not raise urine PH or is there another reason you prefer that to potassium citrate? I can’t find any information on the benefits of potassium chloride for CaP stone formers.
Hi Renee, the potassium chloride is a way to maintain normal potassium balance without raising urine pH as happens with potassium citrate. The latter can raise calcium phosphate supersaturation as it raises urine pH. No trials have studied effects of this agent ini calcium phosphate stone formers. Be sure your physician is aware of my remarks, and approves, if you should act on them, because she/he is entirely responsible for your care and I am an outsider without real knowledge of your situation. Regards, Fred Coe
Thanks I will tell him and appreciate your time. Lastly, I am also confused as to when is the best time to follow up with a potassium check for a person in good health like myself and on no other meds. One urologist put me on 25 mg chlorhalidone and followed up in 5 days with a potassium test. After 5 days, my potassium plummeted to 2.8 and they really seemed to panic and scared me and I completely went off the medication. Five months later a new urologist put me on 12.5 mg chlorthalidone with no potassium supplement (above) and will not test my potassium for a month. Given I had such a large seemly dangerous dip before, is a month too long to check potassium with a 12.5 mg dosage or is that standard practice and time a healthy persons body needs to adjust? Both approaches appear vastly different. I want to be safe and at the same time I do not want not be prescribed unnecessary potassium by checking and reacting too soon.
Hi Renee, Thiazide agents cause potassium wasting in almost everyone but in some people the effect is very marked. So whatever the dose I would check serum potassium soon. If it is low oral potassium can help as can amiloride – an agent that reduces kidney potassium loss. Your physician may want to consider these remarks. The lower your sodium intake, the less your potassium loss. Regards, Fred Coe
I am confused. Under the heading “Empirical stone risk Factors” at the Urine Volume paragraph – wouldn’t risk factor fall as urine volume INCREASED rather than FALL? I am getting a lot of information from your writings having just been DX with first stones by a renal stone CT and high urine Ca Ox levels subsequent to new onset and pain. Thanks, I plan on studying every article as I plan my diet changes.
Hi Judy, How Lovely! A real mistake by me and you are kind enough to catch it – no one before you have mentioned it although perhaps many have been amused. Of course a fall in urine volume will raise risk. I will edit the post today. Warm regards, Fred
Dr Coe, I make a mix of calcium oxalate and calcium phosphate stones. Wondering what urine ph does a person start favouring/producing calcium phosphate vs calcium oxalate stones? What minimum urine ph is needed to form calcium phosphate stones? I am concerned about medication raising my ph and flipping my stones to more phosphate in nature.
Hi John, pH above 6.3 begins to favor calcium phosphate stones. Potassium citrate has not been proven to cause conversion, but also no trials have shown efficacy in CaP stones, either. Regards, Fred Coe
Dr. Coe, I’ve had kidney stones (calcium oxalate) since 2008 (I’m now 46 yrs). I never sought treatment as the stones, in the beginning, occurred maybe once a year. Until about 2015, I started getting them more frequently. My PCP advised me to lower my sodium and referred me to a urologist, but I didn’t go. In July 2018, I had bariatric surgery, Duodenal Switch. Yes, this anatomy change made me a “stone factory”. I had to have surgery in Oct 2019 for a stone that was stuck in my distal ureter. I did a 24 hr Urine Analysis in early December 2019, and my urine has calcium, oxalate, low citrate. Have you heard of oxalobacter formigenes as a treatment, which is said to reduce the oxalate in the gut? or VSL#3 as a treatment? My urologist has lowered my calcium supplement to 1000mg/day (i was taking 1500mg/day – due to my malabsorption), lower my Vitamin D (was taking 100,000 IU/day – and even with this high amount, my bloodwork showed my D to be at 47 in early Dec) to 50,000 IU/day, suggested i drink 100 oz of lemon water, prescribed Potassium Citrate (10 mEq, 2xday), lowered my sodium to 3g/day (this was high in my urine) and to follow a low oxalate diet, which has me here at this site. I am concerned about him lowering my calcium dosage. Everything I’ve read online, here included, says NOT to lower calcium (my urologist thinks I have calcium in my urine due to my high sodium intake, BUT ALSO because i was taking 1500mg of calcium and the extra calcium my body wasn’t absorbing was being excreted in my urine). I’ve incorporated some of the low oxalate foods into my diet over the past two weeks, and have cut out many of the high oxalate foods (I’m going to miss chocolate). I’m wondering if my dosage of the citrate needs to be adjusted to take into account my malabsorption, and same for my calcium, which I think shouldn’t have been lowered. I’ve also read that since I only absorb 20% of the fat I eat, the remaining fat also binds to calcium, which could also be a reason why my oxalates are still high. Any guidance you can provide is helpful.
Hi Molly, I imagine you have increased urine oxalate, and that is promoting stones. Oxalobacter is not a treatment that works. Low citrate is known after surgery, especially in women. Treatment for someone like you is really complex, and you need to be at a center that has specialized skills in both the surgery and stones. This article says some things about the condition. This one tells about what can happen if physicians are not careful. Because of the complexity, I cannot safely help with details of your treatment. Regards, Fred Coe
Hello Dr COE,
I AM PROPERLY DIAGNOSED WITH mask and CaOx stones. I have had many stone attacks, with varied symptoms and levels of pain. Slightly more than a month ago, I felt activity of a 3 mm stone. It stopped and over the past two weeks,I have had minimal pain,but I do feel it moving. With fluids,meds,and staying active, I am hoping this strategy will allow it to pass soon. Since it is so small,am I wise to give it more time to pass since it has not caused the usual issues (UTI,moderate-severe colic,nausea,backache) for me?
Hi Elan, MSK is a chronic and potentially nasty problem. You are doing the right thing to minimize stone risk so as to reduce new stone formation, but the cysts cause stagnation of urine which abets crystallization. Of course, one hopes to minimize surgery that poses risk of infection. REgards, Fred Coe
Dear Dr. Coe,
We have a 12 year old autistic grandson who held his urine for unknown reason at the time to where we now have a mitrofanoff to drain him. He first had a suprapubic cath but it kept clotting off due to brushite formation. The mitrofanoff did not resolve that. He has been passing stones manually thru his penis until I asked his doctor to go in and clean his bladder out. The pediatric urologist was in shock at the amount of stones. Dare I say several 100 in that they came up to the 10ml mark on a specimen cup. They came back 100% dicalcium phosphate. I would love to send you the pic. We had been giving him pot citrate 10meq bid. His diet is awful due to sensory issues with eating. His urine output is 800 to 1200ml per day and often depends on how much pain he is if he drinks good or not. He weighs 90 lb and is 57 inches tall. Their is discussions of putting a g-tube in to increase his output. We are scared of putting him thru another surgery and it not being the answer. We have heard the tubes are painful and its already a task just to drain him. What are your thoughts and recommendations. Thank you for reading Joe Davis (grandpa)
Hi Joe, Massive brushite stone formation is usually of obvious cause, and 24 hour urine collection is the way to figure it out. As he has a drain process it is easy to collect the urine, and I would advise you use Litholink as the testing vendor. Once the urine chemistries are available the cause will be obvious, and treatment as well. Regards, Fred Coe
Dr. Coe,
We ve done all that. Not getting any help no matter where we turn. But thank you for your time
Hi doctor
Can I ask you something please
What happened when I eat something with high oxalato and drink a lot water and lemon juice straight way ?
The stones will be form any way or will be dissolve it?
My last stones was 100% calcium phosphate
9mm right kidney and four small on left kidney
2 surgeries in 4 weeks time
I’m still recovering
Thanks
Eduardo
Hi Eduardo, Your stones are 100% calcium phosphate so oxalate is of zero interest. What causes phosphate stones is too alkaline a urine pH and too high a urine calcium. Lemon juice is not a good idea as it raises urine pH. You need 24 hour urine testing with serums to figure out why you do this. Treatment is specific to what is found. Regards, Fred Coe
Hi Dr. Coe- I have done three 24hr urine collections in the past six months. I was recently diagnosed with osteoporosis and have had one calcium/oxalate stone about 13 yrs ago. My endocrinologist is concerned about increasing my calcium supplements due to having a excess of calcium loss showing up in my urine which could cause a kidney stone. The most recent urine collection indicated 404 mg for calcium in urine/6.651 urine PH/1.93 for SScaP. My sodium is low at 84/my protein is low/Citrate was 1262/Oxalate was 26. My urine volume was 2.86. I have a mostly vegetarian diet, however I eat at least 3-4 eggs per week, and fish about once per week. My doctor wants me to lower my calcium supplement to bring down the calcium in my urine. I’m currently only taking about 600mg per day, and probably only getting about 400-500mg dietary calcium. My very first urine collection (of the 3) I was taking about 1000mg of calcium and my urine calcium was actually lower 275.. I’m a bit confused as to whether the added calcium supplement is good or bad for my urine calcium losses? I’m reading extensively on your site about how to accomplish results with my diet. Optimum calcium for my bones without getting another kidney stone. Are calcium supplements not utilized by the body as well as dietary calcium? Also, how do I accomplish getting my PH to be less alkali when I have a vegetarian diet? Do I need to increase my citrates, and how? Thank you In advance for any insights.
Hi Kelli, Your urine calcium is rather high – 404 mg/d with lowish sodium – 84 mEq/d. The urine is alkaline perhaps because of your plant diet, perhaps because you are losing bone mineral at a high rate, which adds alkali to the blood. I presume your fasting morning serum calcium is normal (10.1 mg/dl or less). If so, I would suggest even lower diet sodium and a low dose of chlorthalidone, 12.5 mg daily, to help retain calcium in your bones. OF course your physicians are entirely in charge and may know things that make this suggestion inappropriate. Regards, Fred Coe
Thank you so much for answering my question. My endocrinologist just ordered some new bloodwork. My fasting calcium came in at 9.5, my sodium was 142, potassium – 4.0, Phosphorus 3.6, everything else was with normal range. My Parathyroid was 41. Vitamin D was 45. My doctor wants to start me on a low dose of Thiazide which I believe to be the same medication that you suggest. Hopefully it will not affect my blood pressure too much as I typically run about 105/70. I have expressed this concern to my doctor as well. Of course I’m also concerned about keeping my potassium within normal range. I am also currently taking Actonel for my osteoporosis. Will likely be doing another urine collection in a couple of months to see if Calcium numbers improve. Your website has been so helpful as I am learning so much about my condition and determined to increase my bone density and stay stone free. Oddly enough my first and only kidney stone was a calcium/oxalate stone in 2007. Was told back then to stop taking calcium and eat no oxalate foods. Clearly that was bad advice. Live and learn. Thank you again for so much excellent information.
Hi Kelli, You can try lowering diet sodium a lot and see if urine calcium falls. One can go as low as 1500 to even 1000 mg of sodium a day. If it is not enough, the dose of diuretic can be vanishingly small, so potassium wasting is not a problem. This article you post on shows evidence for this strategy. Regards, Fred Coe
Am 62. Was diagnosed with CKD 3b several years ago. Have had three small stones (2-3mm) in the last twenty years, the last one being two weeks ago. Comprised mostly of calcium phosphate. Dad was a stone producer. Here’s my big question: Who’s better at dealing with the issue of stones….my neph or a urologist??? Love your articles, btw. Thanks!!!
Never mind. I see that you’re a neph, so I guess that answers that question. I’ve been seeing N. Soifer that last three years. 😀
Hi Marvin, calcium phosphate stones in a man are a bit less usual. Nephrology is the right field to see you and he/she needs to be witty and sharp about what might be the cause of calcium phosphate stones and its relationship to the CKD. Dr Soifer and I know each other, and I am sure he is perfect for you and for the task at hand. You might comment to him about our recent paper on CaP male stone formers. Best, Fred Coe
Thank you for sharing your knowledge dr. Coe, I highly appreciate it.
I’ve got a question: if it is the citrate in the potassium citrate that does the good work, could I also use magnesium citrate instead?
Hi Belinda, It causes GI symptoms, and is not ideal. Be sure K citrate is the best choice for you. The article is my best on if you have common calcium stones. Regards, Fred Coe
Hello Dr. Coe,
Would Vitamin C supplements lower urine PH for people with high PH and phosphate stones? I did read that they can increase oxalate but would that be an issue for people that have low oxalate in the urine? Because fruits and vegetables make the urine more alkaline should phosphate stone formers be on the lower end of the recommended daily allowance of 5-9 servings or do they not raise the urine PH significantly?
Thank you for this site!
Hi Lisa Marie, it is not an ideal approach and I would advise otherwise. No trial, and uncertain effect. A better approach might be to be sure your diet protein is about 1 gm/kg/d and otherwise balanced in regard to protein and veggies. Phosphate stone formers have a basic defect in acid base management we have discovered, but we are not clear what to do about it. Here is the actual article, and I really need to review it on the site. It is true that veggies raise urine pH because they contain potassium alkali so diet balance as above is worthwhile. But more important hypercalciuria is common in phosphate stone formers and can be treated. Regards, Fred Coe
As the composition of my kidney stone is 80% calcium oxalate dihydrate and 20% calcium oxalate monohydrate could you please recommend the most effective diet that I should consider ?
Thanks.
Hi John, The article you have posted on is actually my best for treatment. But perhaps in search for more diet specifics, here is one that focuses on the key links between diet sodium, calcium, and oxalate. The crucial step is achieving the low diet sodium, which makes everything else work. regards, Fred Coe
Good Day, Sir!:
As a medical clinician all my life, I have had relatively great health!
However, due to parental, hereditary conditions, I have developed the last 13 years, renal calcium oxalate stones. I had extensive surgery three instances last year and to my amazement, this autumn I develop one addition renal calculus. I started the half-dosage of Potassium Citrate this past August, 2020. I consume an entirely gluten-free diet and limited 93% hamburger protein intake. I am awaiting a ESWL procedure to remove the stone, but not looking forward to the renal stent placement.
Please, Sir, what can I do to further enhance my assurance that NO further stones form in my future years? Your….. time…….feedback…….advice………are GREATLY appreciated and thanked!
Dr. Don, MD., FAAD.
Hi Doctor Don, It is unusual to begin these stones much later than 50 – it does occur, though. Here is something on stones later on in life that might help. You posted on my best treatment article, and seem to have ended up with K Citrate, so I presume diet did not control supersaturations. Are you sure about new stone activity – counting stones is tricky for me, for everyone. Let me know it there is more. Regards, Fred
Dr. Coe, my husband recently had surgery to remove a 6 cm stone. The doctor told him that he was very acidic and hyper- calciuric. He prescribed one Hydrochorothizzide, 12.5 MG tablet per day, but did not tell him the make up of the stone, or recommend any kind of diet. My question is; Can my husband take a Potassium Citrate, 99mg supplement each day while also taking Losartan 100 mg per day? Thank you so very much! Sandra
Hi Sandra, The 99 mg of potassium is an OTC product and the amount of potassium trivial, so it is safe. But perhaps you might ask the physician why he/she did not tell the kind of stone, or offer diet advice. The dose of losartan is very high, and perhaps a reduced diet sodium intake might allow a lower dose, perhaps adding thiazide might permit a lower losartan dose. Home BP measurements might make all this clear to your husband. Here is an article on BP management in general and in stone formers. The dose of thiazide is lower than that used in the trials, so followup 24 hour urine measurements are important to be sure urine calcium has fallen. If urine is very acid, uric acid stones might form (have formed?) so perhaps a medicinal dose of potassium alkali (1080 mg 2 – 4 times a day) is important. Obviously in saying all this I am ignorant of the details, and offer the comments as just a general set of ideas his physicians might choose to ignore – they are in charge and responsible for his care. Regards, Fred Coe
Hi Dr. Coe,
My stone type is of calcium oxalate. I read your articles and I understand that low supersaturation is the goal. In my own case, by practicing what you and Jill have informed us, I do have low SS in my lab results, with SS CaOX consistently under 2, SS CaP about 0.15, and SS Uric Acid about 0.6. However, my citrate level is relatively low and is around 245 and that’s the only problem shown in the lab reports. I tried to increase my citrate level through food, but in my case it did not give rise to any significant change. My question is: Given the goal of low SS has been achieved, do I really need to take K citrate to address my relatively low citrate level as far as stone prevention is concerned? My doctor prescribed K citrate, but I have experienced side effects from taking other medications. As a result, I have become more and more wary of taking medications, particularly when the medication needs to be taken not many days, but many months and years and even for the rest of my life. With respect to this, if you recommend taking K citrate at all, I was wondering whether it would mean that I need to take it for the rest of my life and, if so, whether long-term use of K citrate would cause any side effects you are aware of.
Thank you so much for all your great altruistic work done for stone formers!
Best regards,
Dynas
Hi Dynas, Given your stones are calcium oxalate and SS is so low, I would not think you need more unless your personal physician knows something special about you, or follow up imaging shows new stone formation. Food – veggies and fruits will raise citrate in your kind of stone former but enough of it may be burdensome. Citrate does inhibit calcium crystallization and that is beneficial but as above it may not be needed. Regards, Fred Coe
Thank you so much, Dr. Coe! I very much appreciate it.
Best regards,
Dynas
Dear. Dr. Coe,
You recommend not taking calcium supplements between meals—would this also hold true for not eating a high-calcium snack, such as yogurt, between meals? Is your general rule to only eat high-calcium foods at mealtimes?
I am following the recommendation to drink 4-6oz. of lemon juice per day to raise my citrate levels and thus inhibit crystal formation. A recent review of studies on KSD patients found that, although lemon juice raised urinary citrate levels and despite orange juice raising oxalate as well as citrate levels, orange juice was the more protective—perhaps because it was more alkalinizing? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8625077/
My last question, also about raising citrate levels—have you ever seen stones shrink or break up after a patient has significantly increased their urinary citrate?
Thank you for being an intellectual safe haven for those wandering in search of trustworthy help!
Amanda Ray
Hi Amanda, I wrote a reply but believe it went astray so I am writing again. Calcium with meals blocks oxalate absorption. Lemon juice is an inefficient way to raise urine citrate. Is your urine citrate low? If not, raising it will not prevent stones. The article is not about protection but about response of urine citrate, so the same question: do you need a higher urine citrate, or pH? The only stones that dissolve reliably with alkali are made of uric acid, and it is not the citrate but the pH. In the event that you have a low urine citrate, and that you want to use lemon juice, be sure to measure 24 hour urine before and while taking the juice to prove it raises urine citrate to the desired level. Regards, Fred Coe
Thank you for those clarifications. But did I misread that citrate interferes with or blocks the formation of calcium oxalate crystals in supersaturated solutions?
Also, does this mean you do not recommend in-between-meal snacks with high calcium? (I know I should eat it at mealtime.)
Hi Amanda, Citrate does indeed inhibit calcium oxalate stones. It has so many actions. It binds calcium and lowers supersaturation. It slows growth of CaOx crystals by adsorbing onto the crystal surfaces. It inhibits formation of brushite – the earliest urine crystal – which serves as an initial nidus for CaOx stones. The last two actions require very low concentrations of citrate compared to calcium binding, incidentally, so no one really knows how much citrate treatment affects them. As for calcium between meals I have no qualms, but I do like to save it against oxalate in main meals. No trials for this homily, so please be free to ignore me. Regards, Fred Coe
Dr, Coe,
In this article you mention keeping refined sugars below 10% of carbs, if someone eats their breads and crackers white rather than whole grain and it states there are no added sugars or very little on the label is that fine? Is it just added sugars to worry about regardless if you eat several white carbs a day, I know not to go over 25 added sugars a day.
Hi Lisa, the 10% concerns added refined sugar, not starch in food. Regards, Fred Coe
Dr. Coe,
I’ve found the info on your website very informative and it’s helped me so much on being educated on kidney stones and be an advocate for my health. I wouldn’t have otherwise discovered how much calcium I’m spilling in my urine as no one had ever recommended a 24h urine test, so thank you!!! I am concerned about calcium phosphate stones. My 1st stone in 2012 was CaOx, but pH has since gone up to 7.1.
On 11/29/22 CT Urogram showed I had 3mm stones (was asymptomatic, but had hematuria in my urine). 1/24/23 ultrasound showed 6.8mm. Do stones form that fast?! I’ve been straining my urine since December, but no stone has come out, so can’t test it. The urologist I have focuses on surgery and doesn’t seem to care about prevention. In convo with PCP about chlorthalidone. Do you think I would need to be on this med for life? Any chance supplements could be causing my issues? How often to repeat 24h urine / check potassium levels? How to lower phosphates? It’s also odd to me that the left kidney no longer has any stones (numerous stones 2 mo prior). Can one clear calculi that fast? Any thoughts or suggestions would be most appreciated. Not confident in the care I’m getting. 24h urine, serum CA, PTH and Vitamin D were requested by me.
52 female, postmenopausal since 51, Sjogrens, SLE, urine is regularly cloudy, often with white sediment, no family history of stones. 6th stone event since 2012, with the previous event almost 5 years ago. Since 12/1/22 I’ve followed yours and Jill’s recommended kidney stone diet including keeping sodium under 1500mg/day.
24h urine: Ca 496, Ox 19, Uric Acid 549, Citrate 1193, ph 7.1, volume 2.95L, Na 25, phosphate 245, Mg 174, K 63, creatine 1124, sulfate 10, CaOx SS 1.28, brushite SS 2.29, sodium urate SS 0.17, uric acid SS 0.08.
(On the day of collection I ate: 33g meat protein (54g tot prot), 4g added sugar, 1289mg Na, 75mg oxalate, 88oz h20, 1177mg of Ca, 497mg Mg, 2284mg K ), with similar values the day before.
Non fasting bloodwork (17 days after 24h urine): CA 9.8, PTH 35, Vit D 57, Na 142, glucose 111, Bun 10, uric acid 2.6, potassium 4.3, chloride 102, bicarbonate 31
11/29/23 CT urogram: numerous tiny 1-3 millimeter calcific densities in the bilateral kidneys. An approximately 3 mm stone in the midportion of the left ureter with mild hydronephrosis and hydroureter. There is mild prominence of the right renal pelvis and proximal ureter most likely secondary to a slight kink of the proximal ureter. BLADDER: No significant abnormality.
1/24/23 Ultrasound: Few right renal calculi, with the largest measuring up to 0.68 cm in the inferior pole. Mild hydronephrosis; Left kidney: No hydronephrosis. No nephrocalcinosis nor renal calculi; BLADDER partially contracted.
Hi Jen, You have a very high urine calcium with normal serum calcium and PTH and despite a very low urine sodium. Urine pH is 7.1 and citrate is very high at 1193. Blood TCO2 is high at 31. I notice diet data showing 1177 mg calcium and 497 mg Mg and 2284 mg (57 mEq) of potassium. I wonder if any of the calcium is a supplement? Everything looks like hypercalciuria with diet alkali loading that raises the urine pH and citrate but does not lower urine calcium. The white crystals in the urine are surely calcium phosphate. Of course I cannot figure this out from far away but perhaps you have rapidly progressive bone mineral loss adding to genetic hypercalciuria? Sjogren causes renal tubular acidosis but citrate is high not low. Treatments for SLE are not mentioned – steroids? Serum phosphate is not mentioned, perhaps it is low suggesting a gene variant for the phosphate transporters. Serum 1,25D is not given, perhaps it is high from a CYP24a1 defect. This complex will not be figured out unless your physicians consider referral to a stone center. Perhaps you live near a university medical school. Possibly I could help via telehealth but I favor something more near at hand for you. Regards, Fred Coe
Hi Dr. Coe,
Thank you so much for your response and insight. Serum phosphate wasn’t tested. What could one do about low serum phosphate or high TCO2? The white sediment seems soft. Is this submittable for stone analysis? I have to admit I’m discouraged diet changes haven’t been enough and wonder about the care I’m getting. Much of the testing I had was thru my requests. I’m in Santa Clara, CA. The potential for fast growing stones or osteoporosis is very worrisome.
Kaiser stone prevention group (group of HMO pharmaD’s) has put me on indapamide 1.25mg (b/c of tendency towards prediabetes) and I’m supposed to run a potassium test 2wks after start. I had already been following KSD diet to a tee for 1mo prior to 24h urine test. Despite me asking multiple times about the phosphates and the cloudy urine, they don’t seem knowledgeable or concerned. Urologist says the ultrasound must be wrong and a stone wouldn’t grow that fast. He and PCP aren’t concerned about the cloudy urine either. Stone program said to repeat 24h urine in 4mo; surprised it’s not sooner to see if the med is working. At Kaiser, stone prevention group works with you, but doesn’t follow you after that. After the potassium test and 24hr urine, unless there’s a problem, no repeating and no followup. Their recommendations were less restrictive than KSD and they don’t consider sugar. Urology said they only deal with surgery, nephrology is for dialysis; talk to PCP. It doesn’t seem like they’re too concerned or have continued annual checks etc…
On the day of the test I had 1 Kirkland calcium citrate (250mg) & the rest from eggshell powder, both with food (plus 1 magnesium citrate & 1 mag glycinate. no citrus fruits). I have since stopped cal cit and eggshell powder and get 1200mg from 2 cups Kirkland skim milk and vegetable sources. Urine still has white sediment and is sometimes cloudy but less so? after indapamine, dairy switch, limiting protein to 3oz at a time, even more water. Vitamin D, 1,25 was 57 when tested with the PTH and non fasting calcium.
I’m not on any meds for SLE as I’ve managed to be healthy in that regard thru diet & lifestyle, just biannual bloodwork which they say is good. No meds except the indapamide right now. I do take 1 omega 3, 1 multi, 1/2 Pure Encapsulations K2D (500IU Vit D, 120uG K2 Mk7), 1-2 Magnesium Citrate (120mg) (or mag glycinate) to help with overnight muscle/foot cramps and balance out all that calcium intake.
CYP24a1: rs2762926 G/T, rs2585413 G/G, rs2762929 T/T (don’t know how to read this). In 2008, Vit D was 25ng/ml and doc put me on supps. Have some Vit D from above K2D capsule since I avoid the sun – (autoimmune hives & melasma).
Dexa scan on 11/21/22 was normal (1st one; requested b/c of low BMI, Asian, mom had osteoporosis in mid-late 50’s (Graves). I’m more subclinical hypo.)
lumbar: BMD= 0.998 g/cm2; tscore=-0.4; zscore=+0.4
left hip: BMD= 0.889 g/cm2; tscore=-0.4; zscore=+0.4
left femoral neck: BMD= 0.776 g/cm2;
tscore=-0.7; zscore=+0.2
frax 10y maj=2% hip=.1%
Hi Jen, I cannot decipher the variants you list for CYP24a1 as they do not show up on a PubMed search, but the report should give the significance and references. A serum 1,25D is important as if it is very high one might want to aim treatment there. Low serum phosphate is a clue to abnormal phosphate transport in kidney which also leads to high 1,25D. The white material is easily analysed by a kidney stone lab, and may well be calcium phosphate. I would suggest seeing the stone group again and asking if they can dig a bit deeper into the cause of your high urine calcium in hopes of more effective treatment. Nothing may come of it, but there is some chance. Regards, Fred Coe
Dr. Coe, we all know we need to have our calcium with oxalates to reduce urine oxalate excretion but how much is needed at a meal? For instance if I ate a high oxalate dinner that had spinach would a half cup of milk that would have approximately 150 mg calcium be enough or do you need much more calcium for a very high oxalate food?
Hi G, The idea is to eat about 1000 mg as food, distributed among the day’s meals. That will generally reduce oxalate loss in urine. There are no data one can use to titrate food calcium against food oxalate as a realistic approach. Regards, Fred Coe
Hello Dr Coe,
Your website and information has considerably helped me understand my kidney stone disease. I just want to say I really appreciate all that you have contributed first of all.
I have obtained all my medical data and I’m a very fast calcium phosphate stone former. (stone analysis is mainly carbapatite 90%). I’ve tried many things such as big doses of potassium citrate but I mostly get undetectable citrate readings.
I have always had Phosphate SS above 1.3 but recently I’ve managed bring down my level to under 0.75 which is good.
If you could be so kind to explain if I will make stones with my readings.
As you can see I have no citrate with high PH but my calcium and sodium and potassium are within normal levels.
Would I still be at risk of fast stone formation given I can keep my Phosphate SS at below 1 at all times. This was achieved by high urine volume and pottasium citrate of 6g per day.
Thank you Dr Coe.
Urine Citrate concentration <0.10
Volume 3.787L
Bicarbonate 25.4mmol/L22 – 29
Estimated GFR (CKD-EPI) 64mL/mi
Sodium 139mmol
Potassium 4.1mmol
Creatinine *127umol/L
Albumin 43
Calcium 2.32mmol/L
Corrected Calcium 2.30mmol/L
Inorganic Phosphate *0.73mmol/L
Total Bilirubin 10umol/L
Alkaline Phosphatase 71IU/L
Alanine Transaminase 28IU/L
Urate 224umol/L
PH Urine – 7.0
Hi Jonathan, The very low urine citrate + high pH + CaP stones point to distal renal tubular acidosis. But your serum phosphate is low and that is not part of RTA but of other kinds of kidney problems. So you seem very complex medically and your physicians might want to obtain consultation at a medical center stone problem geographically convenient to you. Very likely your care could be improved by gene testing so one knew what was really wrong. Regards, Fred Coe