 Unfortunately producing stones means higher risk of hypertension and kidney disease. But most of the diet changes and even first line medications for stone prevention also lower blood pressure. Here is how that works.
Unfortunately producing stones means higher risk of hypertension and kidney disease. But most of the diet changes and even first line medications for stone prevention also lower blood pressure. Here is how that works.
The featured painting, Vincent Van Gogh, The Starry Night. 1889. Oil on canvas hangs in The Museum of Modern Art, New York. Somehow, to me, the whorles of color bring blood pressure to mind. Some say the yellow halos about objects came from digitalis excess, from his physician.
My Sources
From time to time, quantitative scholars produce ‘guidelines’ about diagnosis and treatment of disease. Recently, a band of such have compiled results from the large literature on blood pressure treatment and given us this new compendium. For those with a taste for ‘primary’ sources’, here is the full version. I plodded through this turgid swamp, this winding endless bog, and gathered for you the wildflowers one commonly finds in such places. Here they are: the nuggets of gold left in the pan.
Blood pressure
There Are So Many in a Day
The heart is powerful and quick. Every left ventricle contraction stretches and distends our blood vessel walls with the blood pumped into them. They relax for a moment on the diastolic, between beats, while the left ventricle refills from the lungs through the left atrium. Given 70 beats a minute, and 1,440 minutes in a day, each day brings 100,940 separate systolic pressure peaks and diastolic troughs to bear on our arteries.
Pressure Itself Causes Disease
Evidence from masses of trials would have it that it is these pressures themselves that directly cause stroke, heart failure, and presumably heart attacks. Other factors interact with pressure to worsen the damage elevated pressure can cause. Diabetes and chronic kidney disease, certainly. Age and being male also enhance risk from high pressure. There are more, less compelling factors as well, like blood lipids. But the one thing we can most easily change is the pressure itself.
What Raises Pressure?
Your genes certainly play a role. Next come factors you can control like obesity and high sodium intake. Other things that seem to foster high pressure are a sedentary life style and inadequate potassium from fruits and veggies. Likewise for smoking and excessive alcohol intake. All of these factors are what we alter when we want to lower blood pressure and are not yet at the point of adding medications.
We Need Multiple Measurements
We are diagnosing and treating numbers – systolic peaks and diastolic troughs. But think about the miserable sample we have – a few beats measured with a cuff by your physician, or a few more measured by you at home. From this meager glimpse, a few frames out of a movie that runs all day and night all your life long, we need to judge and plan.
What can we do?
A single measurement by a physician or nurse can be very accurate, but poorly represent the average of all those heartbeats. One can wear an ambulatory blood pressure monitor that makes frequent measurements, but present models are clumsy. Repeated filling of the cuff every 10 or 15 minutes is tolerable for perhaps a day or so.
Home Blood Pressure
This leaves home blood pressure monitoring. The guidelines recommend it, and I long have asked my patients to do it if high blood pressure seems a problem. Common sense favors them – a cheap way to get a lot of measurements. Experts find they predict cardiovascular outcomes better than office pressures from physicians. Commercial, cheap digital devices reduce measurement to pushing a button.
But there are some things to watch.
Machines
Buy a good machine. Use arm cuff models. Shun wrist monitors as potentially inaccurate.
Cuffs
The cuffs are specific to either the left or right arm. You cannot switch a left arm cuff to the right arm or the opposite. So buy the side you want. The cuff needs to go around your upper arm with a good length to spare and be wide enough to cover the upper arm. So if you are large, or overweight, or a muscle builder, get a large cuff. They come in sizes. If you are thin, or not too muscular, or just small, you want a cuff that fits, so choose for you. Some cuffs, notably those from the preferred manufacturers listed below, can accommodate a standard to large arm, but be sure the one you buy will fit you.
Which Machines are Good?
Although 195 pages long, the guidelines fail to give us the names and model numbers of reliable instruments.
But Consumers Reports (CR), usually a very reliable source, has rated them. Only four of the 14 arm cuff units they studied in their lab, showed excellent accuracy.
Their top unit was Omron10 Series BP786N. However, as good as it seemed in their laboratory 3 of 10 recent reviews found it inaccurate. Most criticised its bluetooth connectivity. Next was Rite – Aid BP3AR1-4DRITE. For it 13/18 reviews were scathing – inaccurate mostly. The third, A&D Medical UA767F had only 3 reviews, two of which complained about faulty construction. Accuracy did not come up, but so few! The fourth, ReliOn, from Walmart had 5/9 reviewers complain of inaccuracy. The unit is made by Omron, incidentally.
Why Are So Many Users Dissatisfied About Accuracy?
How can CR find uniform accuracy and users not?
CR buys units at retail outlets.
Here is their measurement protocol: ‘Accuracy is based on how the model’s readings compared with those taken on a mercury sphygmomanometer used by two trained testers.’
The users had comparisons made at their physician’s offices. Possibly, the users encountered less able comparisons in those offices than those made in the CR labs – ie, the physician office testing is problematic. Possibly, units vary. Possibly, cuff placement makes a big difference, but in a physician office this is presumably supervised by a nurse. Possibly, most users are happy, comparisons at physician offices are fine, and they do not bother to write in.
Bottom Line
Possibly this, possible that: what do we do? Bring the machine to your physician, get it checked. Take note of how CR did it (just above) and see if the nurse will duplicate those tests – 2 comparisons, i.e. four measurements.
Procedure of Measurement
No, it is not just ‘put on the cuff, push the button, done.’
When
Mornings before taking any medications and/or evening before supper. Never after a meal. Likewise, never until at least 30 minutes after smoking, caffeine, or exercise.
Experts say to sit quietly at rest for at least 5 minutes before the measurement. Frankly, that is a long time. I don’t see nurses taking that much time in physician offices. Probably a nice long contenting rest gives better – more stable – results. But if we ask too much, we may end up quitting.
I say 2 minutes or so is reasonable.
At the beginning, for the first few weeks, measure in the morning and in the evening before supper to see if there is a big difference. If there is, then make all your measurements at the higher time. If not, then pick the one most convenient and stick to it.
Technique
Sit in a straight chair – no slumping.
Put your feet flat on the ground and uncross your legs – pooling of blood below the knees is not ideal.
Put on the cuff as the instructions show – there is usually an arrow to align it with your elbow. It should be snug.
Support your lower arm on a desk or table. It – your forearm – will be below your heart, but your upper arm – from the elbow to the shoulder – will be more or less along the course of your heart.
Let a few minutes go by as you think about something nice.
Push the button.
I think two readings are ideal, about a minute apart. The system memory will record them.
Get Trained and Checked
If you are neither a physician or nurse, here is a time to use your physician’s office in a cost effective and unquestionably valuable way. Schedule a time, bring in your machine, and let a nurse show you how to use it. She can check your reading of you against her own reading with your machine – they must match. Likewise, she can check her measurement of you with your machine against her measurement of you with her machine – usually more expensive and accurate than yours.
Although CR used classical mercury manometers, the automatic machines your doctor has in the office are usually a lot more expensive and more accurate than anything you would buy, and good enough to check your machine against.
Records
All this fuss – let’s keep the numbers straight. Personally I like a spreadsheet – free from so many sources now. I put the systolic, diastolic, and pulse rate in three columns, and the dates on the rows. If you make morning and evening measurements, use six columns, 3 for each time. But some paper will do if you have no spreadsheet, or the will to make one.
Should we record the first and second measurement as two rows for a single date, or average them to one row? I like the latter. Average: add the two together and divide by 2. Your phone calculator will do it just fine.
Name The numbers
You have made your measurements. Now, what do they mean? Who has ‘hypertension’? Who needs treatment for it?

BP Categories
Their Names
Below 120 and below 80: Normal. This is the far left bars on the chart. Red are diastolic blue systolic ranges. I set the lower end of the normal ranges rather arbitrarily. The keys are the tops of the bars.
120-129, and below 80: Elevated. The red bar does not reach 80, the blue bar is above the 120 line.
130 to 139 OR 80-89: Stage 1 hypertension. I labeled as stage 1 (D) when it is the diastolic pressure that makes the diagnosis, and stage 1 (S) when it is the systolic value.
Above 140 OR above 90: Stage 2 hypertension. Likewise I labeled the bars for whether the diastolic (D) or systolic (S) value made the cut.
When both systolic and diastolic values create the stage 1 or 2 hypertension, treatment is the same. But perhaps one should worry more and act with dispatch.
All of these blood pressure names refer to the average of two or more measurements made on two or more occasions.
At the Borders
What about 120 and 80? Elevated, of course. The systolic pressure is above the threshold.
But this is a game of razor edges! No one can tell blood pressure to one mmHg. One can best say that around these border values one makes a kind of judgement. How else to proceed?
Power of Numbers
If you really do measure a lot of blood pressures at home you can get an increasingly accurate average of your pressure, and that kind of average probably reflects well your ‘true’ average – the average of all 100,000 heartbeats a day over many weeks or months.
Special Problems
In a well ordered world, blood pressure grade is more or less the same using office blood pressure and home blood pressure measurements. For example, if values indicate high blood pressure in both settings one refers to the condition as ‘sustained’ hypertension. On the other hand, when normal in both settings one says simply ‘normal’
White Coat Hypertension
But what do we say when measurements in physician offices exceed those made at home?
Personally I detest wearing a white coat. They never fit well and make me look faint and ghostly. Because they are so ugly, I wear real clothes, almost never color white. But historically, and even now, some doctors show up in their white cotton and poorly tailored coat – like garments, and apparently raise blood pressure either because they are doctors or because patients detest their coats as much as I do.
When office blood pressures are consistently above home blood pressures by more than 20 mmHg systolic or more than 10 mmHg diastolic, one considers this diagnosis. It matters because, in trials, white coat hypertension fails to predict increased all cause mortality, so adding medications or advancing medication levels would be futile, simply add side effects and complexity without benefit. One uses the home pressures as the guide. Sometimes, when matters are unclear, daytime ambulatory monitors help clear things up.
Masked Hypertension
Here things are opposite. In the office, no hypertension. At home, hypertension. Unlike the white coat variety, this ‘masked’ hypertension predicts a risk of cardiovascular and all cause mortality twice as high as when blood pressures are normal. So your home pressures can be critical. Likewise, here, ambulatory measurements for a day or two can help.
Secondary Hypertension
Most hypertension is genetic – primary. But here and there diseases raise blood pressure and we treat those diseases as a primary aim. This is completely analogous to the distinction between idiopathic kidneys stones and stones arising from systemic diseases, but diseases that cause hypertension are a much lower fraction of the hypertensive population.
I shall not review screening for and documenting secondary causes of high blood pressure. It is a deep area of clinical medicine, and not one in which I publish as a professional clinical researcher. Whereas for stone diseases I am such, and correspondingly bold in reducing medical details to a public medium, here I demur, but out of courtesy not fear. For I could do well as a summarizer of the blood pressure causes, perhaps better than some who represent themselves as blood pressure experts. But should I not leave to them their own demesne without my footprints on the lawn?
The Importance of Physicians and Good Measurements
It is for your physician to screen and document, as I said.
There is more. If you are on treatment, or not, and if you have increased risk factors for cardiovascular disease or not, physicians can elaborate on my simple explanations in regard to risk and urgency of treatment. One needs to rely on their physician and use what I say as background.
The physician who is treating you for stone prevention is an excellent one to do all this. Stone prevention uses multiple office visits, and time efficiency benefits from stone physicians also seeing to blood pressure.
But obviously, home blood pressures really matter. So do what I said. Get trained, and check your machine.
Likewise, make lots of measurements. They are free. You cannot tell me that life permits no five minutes a day before supper to measure and record. No risk, no cost. Pure benefit.
Risk Factors
Risk of cardiovascular death, heart attack, or stroke is higher in people with at least two of these vs. those with only one. Risk factors help set the threshold for use of medication in lowering blood pressure.
Relatively Fixed and Fixed Risk Factors
Fixed
Family history of cardiovascular disease. Increasing age. Male sex – biological maleness. What can you do about these?
Relatively Fixed
Chronic kidney disease (CKD). Obstructive sleep apnea. Low socioeconomic conditions of life. I know the second and third are always potentially remediable, but the guidelines I am parsing for you say otherwise. Frankly, for sleep apnea the best message is that if you suspect it is present get a sleep study and fix it. As for the last of the three, I am far beyond my expertise.
Fixing May Not Help
Psychosocial stress
Modifiable Risk Factors
Smoking; diabetes; lipid abnormalities; obesity and overweight; too much alcohol; physical inactivity or low fitness; poor diet. All of these are remediable and should be remediated. Why not? Stop smoking. Get your blood glucose as well controlled as possible. Diet, and exercise properly. Easy to say? Sure. Crucial? Sure.
Special for Kidney Stone Patients
Having crystals in your kidneys, and being prone to repeated obstruction from stones, virtually all stone formers might best consider themselves as having CKD even if glomerular filtration is not reduced. Stone formers are at increased risk for both high blood pressure and overt kidney disease. So when you do your addition of risk factors, add 1 up front because you form stones.
That means your go into the higher risk bracket with only one other. If you are male, or older, too bad. You are already in a high risk category.
This is a powerful argument for all stone formers to attack every modifiable risk factor with zeal and impudence. Why tolerate any of them if exercise, a good diet, and restraint can eliminate risk factors you do not need? And, as for blood pressure, insist on the best possible outcome.
Goals
Lesser Goals Are Recommended
By the way, have I mentioned what are the blood pressure goals?
According to official doctrine of the Guidelines: Below 130 mmHg systolic pressure and below 80.
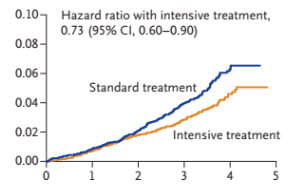 But, in the most recent SPRINT trial, below 120/80 mmHg as a goal gave better cardiovascular outcomes.
But, in the most recent SPRINT trial, below 120/80 mmHg as a goal gave better cardiovascular outcomes.
So why the higher official goal from the Guidelines, this massive pool of experts. One reason is a higher incidence of a serious side effects: Acute kidney injury 4.1 vs. 2.5% total over the entire 5 year trial.
But against this, put the real message: Heart attack or acute coronary syndrome, or heart failure or death from cardiovascular event – 2.25 vs. 2.9 events per year.
This little snippet from the trial shows the lower hazard for death – any cause, with more intensive treatment aimed at below 120 and below 80 mmHg.
What, then, is the other reason, since the acute kidney injury cannot suffice? It is that the lower goals have not been tested per se in their own trial, using ‘hard’ endpoints such as death.
The Bugaboo of Evidence Based Medicine as Practiced
Here, is why I have trouble with the ‘evidence based medicine’ school of thought. This is quoted, in context, from page 169 of the big swamp: ‘The combination of epidemiological data showing a graded relationship between BP and outcomes, particularly above a BP of 120/80 mm Hg, and the results of the SPRINT trial showing benefit of more comprehensive treatment to a target BP of <120/80 mm Hg, suggests that a lifelong BP below that level will substantially lower CVD and CKD incidence. This is especially the case for younger individuals, those with DM, and those with high lifetime CVD risk based on the presence of multiple risk factors, including high BP. If hard, cardiovascular outcome clinical trials remain the sole driver of evidence-based guidelines, then determining the full benefit of earlier intervention may not be possible because of the cost and length of time needed for intervention.’
Need Conservative Mean Lesser Benefit?
What, indeed, is this mass of words telling us? They suspect, in all their wisdom and pride of knowledge, that below 120/80 is better but cannot say it lacking ‘…hard, cardiovascular outcome clinical trials…’. They cannot say it and so revert to higher – almost certainly less beneficial – blood pressure goals.
Why not revert to the lower ones that seem better?
While we wait for more trials that may never prove practical, what keeps these experts from supporting lower blood pressure goals? Obviously from their own words, they lack the evidence. But they also lack evidence in the other direction. No evidence says 130/80 is better than below 120/80.
My Own Uneducated View
Being no devotee of ‘evidence based medicine’ as presently practiced, I simply propose we ignore their niggling preposterous suggestion, and always go for below 120 and below 80. If our patients experience lightheadedness, we know to back off. We know to move slowly toward our goal. And we know that it makes no sense to offer the lesser quality outcomes from a higher goal blood pressure, waiting for some long off trial to ‘prove’ it is lesser, while our patients lose the benefits of an obvious better choice – obvious to these experts who nevertheless cannot say so until they have ‘hard’ evidence.
Remember, that ‘hard’ evidence must be more cardiovascular events in the over 120/80 group than in the under 120/80 group. Is this an ethical stance?
Physicians Are Not Simple
There is also judgment. If someone has kidney disease, is old or frail, or has cardiovascular disease, we know cautions exist. Patients know, and so do their physicians. Treatment needs monitoring, labs as well as blood pressure measurements. The guideline authors cannot admit that physicians – and patients, too – have not only agency but wit, and thought. As much as I have published reams of numbers lifelong, and performed my own abstruse calculations, I never once have believed they are medical practice – merely its shadow.
Non Drug Treatments
We have our goals: Below 120 and below 80, if possible.
The Kidney Stone Diet
Sodium, Potassium, Sugars, Protein
Low in sodium, high in potassium anions from veggies and fruits, low in refined sugars, moderate in protein – it is ideal for blood pressure reduction. That is one reason why the US task force on diet recommends more or less the very same for all Americans. Unlike the rather vague diet plan in the long and involved guidelines, the stone diet goals are crisp and spare. You can use them with confidence for blood pressure and stones together.
We have become accustomed to low diet sodium advice. High diet potassium is of equal importance. Here is a remarkable review of the topic my partner Dr Elaine Worcester pointed out to me. Physicians who are reading this article surely will want to read the reference. Some patients, too.
Here are predicted blood pressure changes (reductions) from the guidelines:
Sodium <1500 mg/d or 1000 mg/d below your present value – 5 to 6 mmHg systolic and 2 -3 diastolic.
Increase of potassium intake to 100 mEq/day, 4,000 mg/day: 4 to 5 mmHg systolic and 2 mmHg diastolic.
The whole ensemble of low sodium, high potassium, embedded in a DASH type diet: 11 mmHg systolic, 3 mmHg diastolic. This is about what one gets from adding the sodium and potassium reductions together.
Fats
The guidelines continue the low fat recommendation and I am in no position to argue. But given the main effect of refined sugar to raise triglycerides and other noxious lipids, and the long saga of sugar money corrupting science via a deflection of blame onto food lipids, I may sing in the low fat choir but in a soft and muted voice, mouthing the words, impatient for the song to end.
Dash and Me
Dash diet is a kind of veggie, fruit and nut, grain and milk, spare protein and meat variety of the stone diet. I do not favor all the nuts, as being gratuitous oxalate for stone formers. Likewise, the diet has been brutally commercialized with people making money off of innumerable Dash books. That repels me so, I cannot recommend their products.
The US Diet Website
Free, colorful, and filled with diet advice, I much prefer it. I have made more than clear how the kidney stone diet and the US diet guidelines say almost the same things. Only regulation of diet oxalate below 200 mg/d, a matter irrelevant to blood pressure control, differs.
Weight Loss
The kidney stone diet when properly exercised will reduce excess calories. Because it matches the US diet guidelines, and they offer elaborate portion guides, adherence to the stone diet should permit gradual weight control. But high blood pressure adds a significant special meaning.
Lowering weight to the ideal can get you a reduction of 5 mmHg systolic and 2 to 3 mmHg diastolic. This should add to the changes from diet.
Exercise
If you get 90 to 150 minutes a week of aerobic exercise at 65 to 75% of your maximum heart rate (every gym posts these) you get 5 to 8 mmHg systolic and 2 to 4 diastolic. Alternatively, you can do dynamic resistance exercise at 50 to 80% of your maximum for 90 minutes/week. This will get you 4 mmHg systolic and 2 diastolic. Isometric resistance exercises in 3 sessions a week over 10 weeks involving hand gripping to 30 to 40% of maximum gets you 5 mmHg systolic and 4 mmHg diastolic, respectively.
Put together, about 1.5 hours a week of exercises get you about 4 – 5 mmHg systolic and 2 – 4 mmHg diastolic. This should add to diet and weight loss.
Alcohol
No more than 2 drinks a day for men, one for women. A drink means 14 gm of alcohol, or 12 ounces of regular beer, 5 ounces of wine, or 1.5 ounce of distilled spirits. No actual values shown for BP change.
Summary from Diet and Exercise – So called Lifestyle Changes
Diet sodium less than 1,500 mg/d or 1,000 mg below usual – 5 to 6 mmHg systolic and 2 -3 diastolic
Diet potassium 100 mEq/day, 4,000 mg/day – 4 to 5 mmHg systolic and 2 mmHg diastolic
Dash (kidney stone) diet – 11 systolic but only 3 diastolic; so the systolic parts add more independently than diastolic.
Weight Loss – 5 mmHg systolic and 2 to 3 mmHg diastolic
Exercise – 4 – 5 mmHg systolic and 2 – 4 mmHg diastolic
Put these together and even though they may not add up independently we are talking about as much as 11 + 5 + 4 = 20 mmHg systolic from sodium, potassium, weight loss, and exercise alone. This is massive, and without any risk or side effects apart from loss of fun, and facing the gym.
Medications
If you cannot do the diet, the workout, the weight loss, or do them but find you need more, it is meds. But the meds are the same as we use for kidney stone prevention. How fortunate is that?
Staging
People with really high blood pressures, above 160 systolic and/or above 100 mmHg diastolic need medication without delay. Otherwise, why not do all four lifestyle changes, and see where you are?
Depending on BP Levels and Risk Factors
Normal Blood Pressure
Normal blood pressure is not treated with medications even if you have risk factors – like being male, or older, for example. This is true if that pressure was that way or became that way with diet, exercise, weight loss, and reduced alcohol.
Because you are a stone former – who else is reading this blog? – you want the kidney stone diet even with a normal blood pressure, of course. This may well lower your blood pressure within the normal range. If so, that is fine.
Elevated Blood Pressure
Elevated blood pressure is treated without meds, by diet, weight loss, exercise and reduced alcohol. The diet would be needed for the stones. The exercise, weight loss, and exercise are extra, necessary for blood pressure.
Stage 1 Hypertension
Because all stone formers can be considered as having a form of kidney disease, it is safe to say every stone former has at least one risk factor. That means even one more prompts use of meds on top of the weight loss, diet, exercise, low alcohol complex.
Given mere age or maleness will do, the guys sort of lose. Likewise anyone with diabetes or a family history of cardiovascular disease. Naturally, anyone with established cardiovascular disease will be on treatment, or get treated.
Stage 2 Hypertension
More or less, everyone in this class needs medications.
Prefered Medications
Thiazide Type Diuretics
Here is a kind of good news. These are the first of the primary agents, and the ones that are known to have saved the most lives and the most morbidities. And, of them, my favorite – chlorthalidone – is most prefered: long half life and best trial evidence. The doses we use for lowering urine calcium, 12.5 to 25 mg daily are exactly those for blood pressure control. Thiazide like drugs are proven in three trials to reduce new stone formation.
For those who want an alternative, indapamide 1.25 to 2.5 mg is ideal, being long acting. Hydrochlorothiazide 25 – 50 mg daily is also usable.
One uses these agents on top of the kidney stone diet and, for blood pressure, on top of exercise, weight loss, and reduced alcohol. The low sodium of the diet permits a greater effect of the drug on blood pressure and urine calcium lowering, and reduced potassium wasting.
Potassium Citrate
Citrate is very valuable in stone prevention, and often the first choice medication. For those with hypertension who need potassium citrate for their stone prevention, I always wait and see if the extra potassium lowers their blood pressures enough to obviate other medications. A standard dose is 40 – 60 mEq daily, but if combined with the kidney stone diet this will amount to 140 to 160 mEq/d of potassium.
Most stone formers, although they have CKD risk and often some kidney damage, have no limit on renal potassium elimination. By contrast to the situation with more severe forms of CKD, one rarely has concerns about potassium use. Even so, if eGFR is reduced I always check a serum potassium after one week of potassium treatments.
If thiazide lowers serum potassium, potassium citrate is an ideal replacement. In fact, I often begin both potassium citrate and chlorthalidone together to avoid a fall in urine citrate from mild potassium depletion.
ACE or ARB
Angiotensin converting enzyme inhibitors (ACE) or angiotensin receptor blocking agents (ARB) are preferred as either a primary first drug or a second drug to use when thiazide is insufficient. For me, ARB is preferable, as ACE can cause coughing in not a few patients. Unlike thiazide that has a main role in stone prevention, these drugs are entirely separate.
Three Drugs or More
If potassium and thiazide and ACE/ARB fail to reach goal blood pressures, we are in a different universe, and I do not want to extend this article into it. Nephrologists regularly treat with multiple agents, and I am one of them. But the issues are more complex and this article already long enough. Interestingly, given stone prevention uses the diet and potassium citrate, I wonder how many patients who really use the diet and also exercise and lose weight will really need three drugs or more.
Sum It Up
Stone formers are more apt than others to become hypertensive. Likewise, they are at risk for kidney disease. This means that blood pressure levels are critical in any kidney stone prevention program. Any hint of even borderline measurements prompts me to get home blood pressures, in profusion, and do what I have written here.
My treatment goals using diet, weight loss, exercise, and moderation of alcohol, are below 120 and below 80 mmHg.
It is very easy to combine stone prevention and hypertension treatment. One diet suffices for both. One of the main stone prevention drugs – chlorthalidone – is an ideal first line treatment for high blood pressure when a drug is needed. Another, potassium citrate, has a potential to lower blood pressure and may be sufficient, with the kidney stone diet and exercise and weight loss, to achieve goal pressures.
Being more prone to kidney disease and hypertension, stone formers are best off always aiming at lean body weight, exercise, moderation of alcohol, and the kidney stone diet. Stone prevention should aim at all of this for all patients.
Kidney stones can portend hypertension, CKD, and bone disease. All of us have to treat our patients, not just their stones. Always, and in the least burdensome manner possible. All patients with stones should expect this from their physicians.

As usual, your articles are so informative. Right now, I’m struggling with hard to control hypertension and am a long time kidney stone former. I have now reduced sodium greatly, begun a healthy diet to lose many extra pounds, walk 25 mins per day and I’ve always drank a lot of water. I am one of those on multiple medications for bp control. Hctz 25 mg, lisinopril 20mg, amlopadine 5 mg and atenelol. I just went to my internist after reading what you wrote about chlorthiadone and she wrote me a script for 25 mg and I will try my best to split them. My high bp is ALWAYS in the morning and goes down during the day. The morning bp can be 155/90. I’m hoping that by changing my thiazide with it’s longer mode of action, it helps to keep my bp lower during the night. I am also a type 2 diabetic and 57 year old woman. I use basaglar long acting insulin and metformin. How long will I have to wait to see if chlorthiadone works? Also, if not should I go back to 25 mg of htcz in the morning and 12.5 in the evening. I’ve never gone that high. I take just regular potassium and magnesium supplement daily with 99mg of potassium twice daily. Thanks.
Hi Michele, A key step is to measure your 24 hour urine sodium to know what you are really eating. Dropping it can make all the difference. You do not have to split the chlorthalidone, it is very long acting. Just take the 25 mg in the morning. But stop the OHCTZ, do not take both together! I bet you will find your urine sodium is high, and if you do and lower it you may get a marked improvement. Regards, Fred Coe
Thank you so much, Dr. Coe. I was splitting the chlorthalidone and not seeing a reduction in my morning numbers so switched back to hctz, 12.5 mg morning and evening. If that isn’t sufficient I’ll try the 25 mg once in the morning. Always afraid of losing too much potassium and magnesium. I supplement but need to eat more potassium rich foods. 11 lb weight loss so far! Thanks again.
Hi Michele, One can always reduce potassium loss with amiloride 5 mg one or two a day. Mention this to your physicians. Low sodium intake is crucial as it lowers blood pressure and also lowers potassium wasting. Regards, Fred Coe
Forgot to add that I think I’ve successfully lowered my sodium to 1500 per day. Hard to figure out sometimes as I don’t eat a lot of processed foods but for this salt lover, it’s been quite an adjustment.
Hi Michele, measure the 24 hour urine sodium and creatinine to be sure you really lowered salt intake. We always deceive ourselves. Regards, Fred Coe
Male age 48.
I too have been a kidney stone maker. Have had at least 6 in last 15 years. I also developed hypertension. Take 10mg lisinopril exercised more and have lost 20lbs. My Bp numbers have dropped and am now told to take potassium citrate by my urologist after urine test revealed high acid / phosphorous levels.
I began to think my kidneys were to blame recently as I began to feel “off” and have recently struggled with slight depression, anxiety & higher BP numbers. Hoping to feel normal soon.
Hi Eric, Weight loss, low sodium, and extra potassium: a good combination. For stone prevention, be sure your treatment fits your test results. Here is a good review of the matter. Regards, Fred Coe
After conscientiously following the Kidney Stone diet, reducing salt, sugar, fat, etc, and loosing 40 lbs, no new stones, etc., I still had too high urine calcium so urologist prescribed 25mg HCTZ, which helped–tho urine calcium could still be lower. Six months later, my cardiologist was concerned about slightly low blood potassium, so prescribed 10 meq Potassium Chloride. Levels improved to normal, but I need stay on it. What is the difference between potassium chloride and potassium citrate especially related to the issues in your article?
I do take BP med, 25 mg Metoprolol, and BP typically is below 120 sometimes as low as 99, but really varies depending on all the things you mentioned above re testing.
Hi Martha, The fall in serum potassium is common with OHCTZ and potassium chloride is a perfect remedy. Potassium citrate would also work but is more expensive. I worry your diet sodium is too high – this will worsen potassium loss – check your next 24 hour urine and be below 1500 mg/d. Always check the urine concerning diet changes as few of us really can judge what we eat. Regards, Fred Coe
Thanks to you and Jill, most of my numbers are pretty good now. On my first 24-hour urine test 2 years ago, Na 24 was 109, its highest, and now it is only 40. (Actually cut back salt years ago!) I sometimes wonder if I get enough! I do not add any, and eat almost no processed foods. Aim for 1500, seldom have a problem going over that–usually it is less. Originally SS caOx was 10.39, now only 2.91. Ca24 was 396 now is 270. I do love dairy, try to count carefully, so I don’t get too much! Dietary potassium is a hard one since the best sources are high oxalate.
Hi Martha, do not worry, no amount of sodium is too low – below 1000 mg is fine unless you have an underlying heart or kidney or liver disease. Get the extra potassium, if you eat the right amount of calcium – 1000 mg/d – and use that calcium with meals that contain oxalate, urine oxalate will not rise much. Regards. Fred Coe
Hi Dr.!I just want to ask what is the best anti hypertension meds.for me,my bp is sometimes 130/90 but lately i had 140/100 and when i take catapres 75mcg it will become 120/80 in the morning i take losartan 50 mg but in the evening my bp increases again to 140/100,i was diagnosed with small kidney stones.what shall i do doc?thank you and God bless
Hi Phoebe, Treatment of high blood pressure is a lot more than meds. Take a look here, and see if you do not get better results. Regards, Fred Coe
Hi Doctor Coe. I will be taking potassium citrate . Can I also eat potassium Rich foods? I also take vasotec. Also which form of potassium citrate is more gentle to the stomach? Pill, powder or liquid? Thank you so much for all of your information.
Hi Holly, yes, the foods and the pills without concern. Vasotec (enalapril) does reduce kidney potassium removal efficiency but your physician has prescribed the potassium with knowledge that your kidney function is adequate to the task. As for the stomach, the pills are slow release so are least likely to be a bother. Regards, Fred Coe
Dr Coe, I am trying to figure out how much protein to eat. I am 5’1″ and 93 pounds. Is there a calculator somewhere I can use?
Hi Kristie, you want about 1 gm/kg body weight per day; a pound of weight is about 2.2 kilograms, so it is 93/2.2 or 42 gm/day. The amount of protein in uncooked meats varies; here is a reliable US government website. Regards, Fred Coe
Dr. Coe,
Thanks very much for the helpful information on your site. I am 73 and have had moderate hypertension for about 20 years. I get lots of exercise, try to reduce sodium and sugar intake and reduce weight, and take Lorsartan 50 mg per day. I also have BPH and take Alfuzosin 10 mg / day. This all helps keep my blood pressure at normal. This spring a started passing small kidney stones (about 3 mm) , diagnosed as uric acid stones. I started drinking about 2 liters of homemade lemonade sweetened with stevia a day and passed about 35 stones in a month. My urologist prescribed potassium citrate 10 MEQ tabs 3 times per day. I raised a concern about whether this amount of potassium (with the Losartan) might be a problem and he said not to take the potassium citrate and continue the lemonade. I did so for a month or so and passed only two more stones. I became concerned about the acidic lemonade eroding tooth enamel, and have tapered off while still drinking 1 – 2 liters of that or water and using straws to keep the lemonade away from teeth. My pharmacist said that taking 1 tab of the potassium citrate a day should be okay so I have also done that for a couple of months. Two more stones passed and blood pressure somewhat lower still (about 110/70). I will see my urologist later this week. I welcome any comments you may have about combining Losartan with Potassium citrate, concerns about tooth enamel and lemonade, and any other related matter. Thanks.
Hi Richard, Uric acid stones form when urine pH is too low and potassium citrate is a perfect cure. The original dose of 3/day was fine even with losartan, and in fact 4 a day would be better. If your kidney function is reduced, your physician can check serum potassium after one week of treatment. All this beverage activity is unsuitable. If you take in enough potassium citrate from beverages to raise urine pH it is still the same potassium load as from the pills, and less reliable. Regards, Fred Coe
Hi Dr. Coe. I am in a real pickle. For the 2 years since getting off Metoprolol Succinate 100 mg i have been stone free and my blood pressure has stayed around 135/.82. I also have psoriasis and psoriatic arthritis which I do not take any prescribed medications for, but do utilize CBD oil which helps tremendously. Previously, I used to get around 20 stones a year with at least one requiring surgery. In the last 2 weeks, I have started to get some chest pain and my blood pressure has started rising. I restarted the Metoprolol and my blood pressure has dropped and the chest pain has stopped. Howevre, I am scared to death that Metoprolol was causing the kidney stones. I am already on low sodium intake, no gluten, dairy or sugar and very little red meat. I am overweight, but losing. I try to exercise but the psa really doesn’t help, but the CBD has at least gotten me able to be able to work full time.
I’m so grateful you lend your knowledge to us. I have been having stones since my last pregnancy 16 years ago. I had no idea about the stone/bp correlation until I read your article, though my bp issues started at the same time. I have had several basket extractions and 2 lithotripsy (did not break up stone either time). I’ve only had analysis twice and I know that I form different stones (including uric acid). My most recent is below. My new uro wisely told me that I have a kidney disease and therefore need to see a kidney dr. Waiting on that appt. After reading your article about MKS, I have no idea if I actually have it or not. Is the particular diagnosis important? What can you tell from my test results? TIA, truly.
Kidney stone breakdown:
1st Constituent:
RESULT: 60% Calcium oxalate monohydrate
2nd Constituent:
RESULT: 20% Calcium oxalate dihydrate
3rd Constituent:
RESULT: 20% Calcium phosphate (apatite)
CT before surgery:
1. Left obstructive uropathy related to a 5 mm stone at the left UV junction.
2. 2.3 mm stone in the distal right ureter, which is not associated with hydronephrosis; however, mild hydroureter is noted.
3. Bilateral medullary sponge kidneys with extensive medullary calcifications.
Hi Patti, Radiological diagnosis of MSK is most unreliable. SUffice that you have lots of calcifications, and produce calcium oxalate/ calcium phosphate stones. You need a proper stone prevention program and also blood pressure management. Ideally the kidney stone diet can help both so unless the pressure is very high I would pursue diagnosis for cause of stones and see if the kidney stone diet lowers blood pressure. Regards, Fred Coe
Hello sir,
I have 3 stones in my right kidney size 3mm and one in left kidney size 3mm . I am experiencing hypertension 150/90 . I am taking medicine for hypertension . Do I need to take hypertension medicine for life long..
Hi Bapu, proper diet – in the article you have commented on – can lower blood pressure and if that is not enough drugs are added. If you need a drug you need it life long. Regards, Fred Coe
Hello sir,
I am vishal 19 years old since 1 month my blood pressure is 170/90,160/90.Did some blood tests but everything is normal in it.they said i have 4mm stone in my left kidney.Docter said that there is no relation to kidney stone and high blood pressure. they me tablets for high blood pressure.
What should I do?
Hi Vishal, Your blood pressure is very high and stone formers indeed have increased risks of high blood pressure. Given your youth and high pressure your physicians will want to be sure as to why it is high – is there some underlying disease causing it. Diet is also important. I do not know anything about your real situation so all I can say is that your physicians need to be very thoughtful as what you have is uncommon and needs careful attention. 24 hour urine testing for cause of stones might disclose reasons for your high blood pressure. Regards, Fred Coe
Hiii doctor i am 27 years old i have 5 stones on my right side kidney the doctor said that they are in the urinary tracs im having high blood presure and the medication i giving me alot of side efect like dizinies hight heart rate and diarrhea i been eating well and doing exercise and the high blood pressure still high and i dont want to take the medication what i can do thank you in advance
Hi Jose, You appear to have two problems. One is stones, and they need their own evaluation. The other is high blood pressure, and that begins with diet and exercise – as in the article, and failing that one adds medications. Your physician needs to see to the diet and also the nature of the medications given you have having side effects. From here, knowing nothing in detail, I cannot add anything particular. Regards, Fred Coe
Thank you so much..it is really useful for me..
I have a question..one of my friend have 2mm kideny stone nd blood pressure is around 175/130..he is on medication of thaizide..
Will he be okay after removal of stone??..or blood pressure still remain the same??
Hi Kajal, That is a very serious blood pressure, and beyond the scope of my article. If this high pressure is because of the acute pain from stone passage, it usually is brief and blood pressure falls rapidly with pain meds. If it is his usual pressure, there is serious risk and care is urgent. Regards, Fred Coe
I have 2 inactive stones. I had BP of 140/65 with medication. My BP suddenly rose to 220/90, can the stones have something to do with this? My doctor is on vacation.
Hi Fried, If the stones are not causing pain or obstruction, the marked changes in blood pressure are not likely due to them. Your long term pressures seem too high, as modern data call for systolic pressures below 130 mmHg. Such very high spikes as you now mention are potentially serious and your physician needs to intervene. This site was not intended to accommodate such levels of pressure but rather offer to patients, and remind physicians, about present conventions and guidelines. Let your physician know, and get the pressure controlled. Regards, Fred Coe
I have had stones since my first pregnancy 7 years ago. I have had three surgeries and both kidneys and two sets of stints. I have passed over 20 stones at home between surgeries one the size of a small pea but usually between 5-6mm. The entire urology clinic where I live have seen or treated me at some point but now are saying they will only see me if I need surgery and they can’t help me. I am lost at what to do I now have four young children and feel like I could die at times I’m so backed up from stones and kidneys retaining fluid. My BP has scared enough to try and get a doctor to help me again. Can you suggest anyone reliable who will listen to me in the Northwest? I live in Missoula Mt. I feel helpless. The last 2 CT’s I had the doctors here evaluated me as having no stones in my uritors but I passed them only days later and they were enormous! I’m in constant pain and pain meds do not work so I almost always go through this with no help. I could go on and on about the last 7 years but really I just need someone to help me figure this out so I can be here in another ten years watching my babies grow up.
Hi Ashley, I gather you have pain, stones, and high blood pressure, and I see from the map that you live – actually – nowhere. I found a University of Montana Medical School not too far away. That may be your best bet. Regards, Fred Coe
Hello Doc,
I had kidney stone in ureter which passed and 3 more stones in Kidney.My diastolic pressure in normally around 100 and I feel perfectly alright but today it shot up (last 3 days) and I had to rush to the doctor (Systolic-192,Diastolic-123). I am not sure what is going around.I have no tension issues,no sleep issues.But,yes do have recurring kidney stones.Can you please advise.
Hi PSAHI, You do indeed have a significant problem. Sudden increases like this are unusual and your physicians need to find out the cause, as I am sure they will. Pheochromocytoma is a not rare cause of this kind of remarkable variability, and they know this. Stone pain can raise pressure a lot, but you say this occurred in the absence of stone passage or pain. How did you know your BP had increased?? Did you have symptoms? I would consider the BP problem separate from the stones for the moment and hope your physicians can figure out why and how to treat it. Regards, Fred Coe
Hello Doctor,
I am a stone former, big time. 61 year old female, at ideal weight, and otherwise healthy.
I passed my first stone about 15 years ago, but in recent years everything has intensified. An ER visit 5 years ago, revealed 19 stones in my right kidney and 12 in the left. A good doctor surgically removed 9 from my right kidney, one by one, basket style (9 were left, somewhat “embedded”). I’ve since passed numerous stones, some at home with intense pain, others at ER with excruciating pain.
My blood pressure had always been very good, even low. But with one stone passing I experienced much blood in my urine, then intense pain, and my blood pressure sky-rocketed. Although it pretty much normalized after I passed that stone, my urologist discussed hydrochlorothorazide as a means to prevent stone formation. He did explain that he didn’t see my diet as an issue, but more that I have medullary sponge kidneys, whereby urine “pools in pockets” and crystals form. I’ve been told that I have calcium oxalate stones. They are definitely dark, some smooth, some jagged (ouch!).
I am trying to drink more water, recognizing this is an issue for me, as I rarely experience thirst. I did move to Florida from Canada 10 years ago, and understand this can be a factor. Perhaps this explains the sudden increase in stones? I’ve wondered why, if my condition is congenital, didn’t I experience more stone formation in my younger years. The only other factor that I see different in my life, besides the move to FL, is perhaps my morning chai latte. But I’ve not read anything to believe that is a factor with kidney stones.
A few months ago I had my gallbladder removed (many stones) and my issues of bloating and daily discomfort seemed over. However, the kidney stone passing and intermittent kidney pain continues.
I was very discouraged a few months ago where a scan revealed 16 stones in my right kidney and 3 in my left kidney. Although it’s an improvement in the left kidney, it’s obvious a major problem with the right kidney. Most of my pain and passing stones occurs on the right side.
I was reluctant to start with hydrochlorothorazide because my father (who died at age 65) was told that his systemic lupus may have been triggered by his long-term blood pressure meds. But I have been taking HCT now for almost a year.
I take no other meds. Almost in desperation, I do take chianca piedra (tincture drops in water) and tamsulosin (Flomax) at the onset of throbbing kidney pain. Sometimes it lessens and nothing happens, but often it intensifies, then lessens, and I will pass a stone.
With this chronic condition, I am growing fearful of any travel, never knowing when the next stone passing will happen. I almost lost the realtor course I took, passing a stone just an hour before class. And of course, it’s very costly going to the ER, so I do my best to manage stone passing at home. I would guess that I’m passing about 4 stones a year now. Perhaps more, smaller ones that I don’t actually “catch”?
My doctor has been reassuring, but he has also used the terms “dangerous kidneys” and “kidney disease” in recent discussions.
Do you have any advice for me?
Hi Sue, First I would be sure about what is happening. Are the stones really calcium oxalate? Have you seen the actual analysis reports? If calcium phosphate, things would be different. The embedded stones: where they really in sponges or just in the tissue? If the latter I begin to suspect calcium phosphate stones. What do your 24 hour urines really show: High calcium, high oxalate, low citrate, altered pH, volume? Some combination? Are your pain attacks from actual stones, or are the attacks pain with bleeding but mostly no obvious stone is passing? The high blood pressure from stone pain is not significant, as pain will raise BP in anyone. What matters is your pressure when you are otherwise well. Is it in a good zone – below 130 mmHg systolic? Check out all of this, and see if things become clearer. Regards, Fred Coe
sir, i have right kinday middle calyx and lover calyx 8mm and 9mm stone . no pain . but my bp rise suddenly 200mmhg to140mmhg . how can my bp reduce .
Hi Patel, Such large variations in blood pressure are serious and not likely due to the stones. Your physicians need to find out if this is from a systemic disease or not, and treat it promptly. Unless the blood pressure increases are during stone passage I see no relationship between them and your blood pressure. On the other hand people with severe hypertension may have uric acid stones, and that is also something for your physicians to consider. Regards, Fred Coe
Hi Fredric,
First of all, thanks a lot for such a nice article. It is very useful to me. My doctor diagnosed me with severe hypertension around 170/110mm of Hg a year ago. Since then I am taking medicine a Telma-H 40mg in the morning. He diagnosed with small kidney stone 2mm and mild hydroneuphrosis problem. I am on DASH diet now. Now the size of stone becomes 4mm recently with pain. Is my hypertension due to stones? Is it possible to reverse my BP to normal without meds after removing stones? Eagerly waiting for your suggestion.
Regards
Sathya
Hi Sathya, The small stone did not raise blood pressure, it is that people who form stones appear at risk for high blood pressure perhaps because of intolerance to the modern high sodium low calcium low potassium diet. I do not think removing the stone will lower blood pressure, but it may be best to remove it if it is causing infection, pain, bleeding or obstruction. Regards, Fred Coe
Thanks Fredric,
I have ureteral obstruction at lilac level on right side of kidney and I feel pain too nowdays. Suggest me some natural ways to dissolve my stones.
Which is the best way to remove stones either medications or surgery? Do I need to take BP medicine for my lifetime if it is due to sodium intolerance?
Regards
Sathya
Hi Sathya, Given obstruction, blood pressure can rise, so you the main issue is relieving the obstruction. This is going to happen if the stone passes or is removed. Dissolving stones is very limited – to uric acid stones. Even if this one is uric acid, obstruction is bad for a kidney so removal is best. Prevention depends on the composition of the stone and blood and urine testing. Blood pressure treatment is best undertaken when the stone is out. Regards, Fred Coe
Thanks Fredric,
I have ureteral obstruction at lilac level on right side of kidney and I feel pain too nowdays. Suggest me some natural ways to dissolve my stones.
Which is the best way to remove stones either medications or surgery? Do I need to take BP medicine for my lifetime if it is due to sodium intolerance?
Regards
Sathya
Hi, I believe I answered this just below. Fred
Thanks for the great article! My husband has kidney stones and recently started hypertension treatment. He is currently on Chlorthalidone and amlodipine, and he also takes potassium citrate for the stones. The BP has improved but the diastolic pressure is still in the mid 80s to low 90s. We know that telmisartan and other similar drugs are an alternative if his pressure does not improve further (besides him losing weight and exercising more, which is something he struggles with). However, we also read that Telmisartan can increase the potassium levels even further when given together with potassium citrate. Is this something that causes trouble in practice or just a theoretical interaction?
Hi Rafael, Given chlorthalidone causes renal potassium wasting I imagine a sartan will be safe. Of course his physician needs to be in charge and make appropriate followup measurements of serum potassium. I do agree exercise and weight loss are far better than any meds, and should be used as fully as possible, and I am sure his physician will agree. Regards, Fred Coe
HBP 199/90, how can I lower?
age 86 stress test ok
HBP 199/98
stress test and ct to check earth ok
kidney gfr 59
createene 1.3
1 kidney stone
age 86
how can I lower the BP
THANK YOU
Hi Peter, This is very high blood pressure. Given a creatinine of 1.3 I would think your eGFR might be even lower than you note. At your age and with this level of pressure you must have a nephrologist take care of you. As well, you need that now, because the pressure is high enough for worry. Management is complex for you, and needs highly trained physician help. Please do this right away. Regards, Fred Coe
I was diagnosed by a nephrologist with Gitelman’s disease approximately 3 years ago. Multiple trips to ER with low potassium while already receiving potassium chloride 20meq daily. I am currently 50 years of age. Until age 30 blood pressure ran 90 /60. With birth of my first child and pre-eclampsia blood pressure was never that low again. Now I have severe hypertension. I am taking diltiazem 360 LA and Bystolic 20 mg daily. Blood pressure still not controlled. So as a last resort I was placed on valsartan 80 mg qd . I have had kidney stones for 35 years. I went 14 years without needing one to be treated. Then last summer I had one which was a size 8. After being on valsartan and gabapentin for less than a week I have formed a confirmed size 6 stone. I crave salt all the time and my legs are swollen most of the time. In referencing articles it does not say why ARB’s and Ace Inhibitors are to be avoided. I tried clonidine patch, but after being on it for 7 days it decreased sodium levels. any suggestions.
Hi dewanna, I gather that your diagnosis was 3 years ago, but presume low potassium and magnesium and blood pressure were always present. It would seem that your episode of preeclampsia has overlaid the electrolyte disorder with kidney disease causing high blood pressure. Given stones for 35 years is very confusing in that Gitelman’s much lowers urine calcium so stone formation would be very unlikely. Given the confusing findings, can you clarify if your potassium wasting was present all or much of your life or a recent matter perhaps after your preeclampsia. Just on the surface, you do not seem to have Gitelman’s syndrome but perhaps some other problem. Regards, Fred Coe
I had kidney stone in 2009 (and then 2009, 2012, 2020 now) when I faced pain, went to hospital, did ultrasound which confirm there is stone (sometime not) and they told me to increase water to pass which I reckon did work. One reason I don’t understand why they keep coming back (maybe I don’t keep with precautions). But bad thing I got high BP during this and start BP medicine in 2019. I asked doctor whats the reason for High BP and they never mentioned Kidney stone ever once. I hope I can improve this condition and maybe can reduce some of my BP or BP medicine intake. Thanks for this article doctor. Much appreciated
Hi Hardeep, In addition to lowering blood pressure try to get fully evaluated for the causes of your stones using stone analysis and serum and 24 hour testing. Prevention can be very effective and some of the diet changes and even meds also help with blood pressure. Regards, Fred Coe
I am 44 male and in decent shape. I have produced oxcelate stones since I was 19. I roughly pass 4-5 a year. Worst year was over 100. I have been diagnosed with hypertension since age 25 and have been on meds since. My currents doctor states that kidney stones wont raise my blood pressure. I have been having bouts of increased BP and it has directly correlated to fighting a stone before it drops into my bladder. Currently I am feeling the discomfort of another stone and my BP spikes at different times of the day. Any suggestions on treatment?
Hi Matthew, Stone formers do have increased risk of high blood pressure, and stone passage raises blood pressure, but this should be transient. With multiple stones a year, perhaps spikes in BP you describe associate with stones. Effective stone prevention is an important alternative. Yours cannot be effective as stones persist. Perhaps your physicians will want to pursue better prevention. Home BP will help sort out if BP is high apart from stone passage, an important point. Regards, Fred Coe
Dear Dr. Coe,
I had my first episode of kidney stones in 2005. The next one was in late 2015. But since 2019, I’ve had three episodes (that I’ve felt the pain of).
Particularly alarming is my elevated BP—especially my diastolic pressure, which is truculently above 85, and shoots up to the high 90s often. My systolic is often in the 130s, but with meditation, deep breathing, and exercise I can get it down to the 120s, and even 1-teens. After aerobic exercise, both my numbers drop. My systolic drops by a whopping 30 points often (from the 140s to 11x, and diastolic by about 10 points. And they stay that lowered for several hours after exercise.
No matter how far I’ve searched, I haven’t been able to find peer-reviewed journal articles (or even regular WWW articles) discussing the connection between diastolic pressure and kidney stones.
A more recent symptom is tinnitus.
I lowered my sugar intake long ago. But my cholesterol has been elevated (in the 240s as of a year ago). I’ll make a serious effort to change the remaining suboptimal aspects of my diet as well, based on some of the recommendations on your page on the kidney-stone diet.
My father used to suffer from gout, but never had kidney stones.
I wonder if you have any insight on how to attack the diastolic pressure, and whether you know of any connections between tinnitus and kidney stones, BP, cholesterol.
Medicine is not my expertise, but I *am* able to parse through journal articles and make sense of them, in case that helps you point in me the right direction.
Many thanks,
Babak.
Hi Babak, I suspect you are on the younger side during which diastolic pressure rises in proportion or even out of proportion to systolic pressure. In general with age the systolic pressure is high the diastolic low. But either one is hypertension and treated in the same ways. The article walks through the non drug and drug approaches and I endorse them all. Aerobic exercise, loss of visceral fat as much as possible, low sodium diet – 65 mEq – 1500 mg/d is ideal, and the 24 hour urines for stone prevention show the sodium. If all of these do not bring both pressures into a decent range (shown in the article) then one adds meds. One choice is a long acting thiazide type drug like chlorthalidone 12.5 to 25 mg/d. Another is an A2 receptor blocker like losartan 25 mg/d. Central to everything is daily home BP before eating, I suggest before supper is usually convenient – put the results into a spread sheet so you can track the trends. Of course get a personal physician who will be responsible for your care. Hypertension with stones is odd only because both share many common treatments, both use 24 hour urines to advantage, and stones promote high blood pressure. Regards, Fred Coe
Dear Dr. Coe,
I thought I had submitted an acknowledgment reply to you, but I must have done something wrong in posting it, because I don’t see it.
Thank you very much for your quick and thorough reply.
I wish I were as young as you guessed; I’m a male and in my early 50s.
I’ll heed your advice and implement the lifestyle changes and use some of the diagnostic tools you suggested. And I’ll read the other pages on your site more carefully to get more details and assemble a more thorough picture.
Many thanks for the generosity of your time and knowledge..
Regards,
Babak.
Hi,
I found this article interesting and relevant to me.
I am a 36 year old female, this is my story:
Always in good health, I never had any health or medical issues until February 2018 when I woke up suddenly in extreme pain on lower left side. Long story short I had an 8mm stone obstructing my left ureter. I had a ureteroscopy, stone was completely removed intact and I had a stent put in which was removed 10 days later.
In July that year I had a CT scan which showed up multiple small stones in both kidneys but my urologist at the time said it was nothing to worry about so just left it.
I had no further issues until July 2019 when I was 5 months pregnant with our 4th child and had a sudden extremely painful attack in my left kidney. I had an ultrasound which vaguely showed a largish stone in my left kidney but not much could be done due to the pregnancy so I suffered through weeks of pain until it eventually subsided. I gave birth to our son in November and eveything seeed fine until 2 weeks postpartum I experienced some frightening symptoms and went straight to my GP who tested my blood pressure which was roughly 177/102. (Throughout 4 pregnancies my bp was always completely normal, Inhad never had any high bp problems.) She tested several more times and it was similarly high. She prescribed labetalol and told me to monitor my bp with a machine at home that I had borrowed.
Again, long story short I ended up in hospital twice for 3 days each time in the following month with very high bp and feeling awful. Was put on enalapril by physician which I am still taking (11 months later.)
Numerous tests haven’t showed up any other health problems however a recent CT scan showed a large stone in left kidney and multiple smaller stones in both.
My bp had been stable for months and I was slowly coming off the enalapril but bp has suddenly spiked again 4 days ago. I am fine during the day but bp is in 140s/90s in the afternoon/evenings and I feel terrible.
Do you think this sudden spike is kidney stone related?
Hi Sara, You are describing a really complex problem and I am far away and cannot dare to say much. In general post partum high blood pressure can be renal in origin, but if your stone is partly obstructing that can raise blood pressure, too. You should have a nephrologist and she/he work with your urologist to decipher what is causing this problem. I am not evasive, but concerned that I lack the information to be of real help and could be a source of confusion. If your physicians are themselves in favor, perhaps you and they might wish an outside consultant to help. Regards, Fred Coe
So pleased I came across your website. I am 65 years old with a duplex kidney, and have had kidney stones on and off for 7 years. Drinking the juice of freshly squeezed lemons 2-4/day reduced the size, until now. I stopped drinking the lemon juice for a few years, and now at present I have a stone 20 mm long and 5 mm wide. That was a very big surprise. I have never had excruciating pain so I didn’t worry much about it, until now. I have developed high blood pressure 170-150/90-80 quite suddenly. I also have increased my fluids to 4 quarts/day. My eGRF and electrolyes are normal. My doctor has never known me to be hypertensive and feels that I am just too stressed about the surgery I must have to eliminate the stone. He has put me on Tamsulosin and told me to relax. Other than this problem I am in excellent health with normal weight, liver function and my dietary intake is full of fresh good food with no processed items.
Do you think that drinking excessive fluids can raise my BP that significantly or is it the stone which has become a problem now? I do have slight hydro nephrosis.
Thank you so much.
Beth
Hi Beth, Do you have uric acid stones? It sounds like it. If so, potassium citrate is a lot better way to prevent growth and new stones than lemon juice. Your blood pressure is high and perhaps from stress or something else. I would be concerned enough to suggest you do home blood pressures – as in the article you have posted on. Fluids will not raise blood pressure. Perhaps your physicians might want to be sure about your kidney function and possible obstruction from the stone. In any event if pressures are high much of the time they may wish to take steps to reduce it. Regards, Fred Coe
I have a h/o kidney stones, 4 episodes over 49 years. Ct with contrast had an incidental finding of staghorn calculus R kidney. Watchful wait/no treatment. Lacunar stroke Janyary this year, ace inhibitor/statin/anti platelet. Stabilised over a few weeks then acute hypertension 185/110 ish for several hours, loin pain. Calcium channel blocker introduced, weary/nauseous since. I’ve spoke nwith primary care several times, hoping for referral to urology, gasn’t happened. Any thoughts?
Hi Gordon, a staghorn is a very large stone, and if the kidney is otherwise working its removal is reasonable. Was the very high BP due to pain from the stone?? I would not favor waiting long as your pain might have been obstruction from stone fragments – you need rapid attention. Regards, Fred Coe
I am a 67 year old woman with a 20+ year history of hypertension. For most of those years I had significant “white coat” spikes of BP in medical settings, but it has now progressed to having spikes anytime there is great stress or anxiety. My spikes can go as high as 200/100 with pulse sometimes over well over 100. This is a huge source of stress and worry for me, as anytime I go to a doctor or have a medical procedure, I have these huge spikes, which causes everyone great concern. This past year I have now developed palpitations (PAC’s), and a recent echo showed mild thickening in the left ventricle. I have been on Amlodipine 10mg and Losartan 50 mg (2x day), plus 10mg Rosuvastatin for a number of years. My BP is well controlled at home (consistent home monitoring), but still spiking very high during anxiety or stress. I recently started seeing a hypertension specialist and he just changed my meds to Amlodipine-Olmesartan 5-40, and lowered my statin to 5mg. I started these new meds yesterday. I developed my first kidney stone in 2019 and my second in late 2020. I had never had a kidney stone before that. I read that this new medication, Amlodipine-Olmesartan can reduce urine output, which is concerning for me now that I am at risk for more kidney stones. My doctors have never discussed with me the correlation between hypertension and kidney stones, but I am concerned that hypertension meds are, in part, causing my kidney stones. Are there BP meds that do not increase risk of kidney stones?
Also any advice on which doctor is best to oversee and treat hypertension? I have a PCP, cardiologist and hypertension specialist (internal medicine with a hypertension specialty – only deals with hypertension). All three sometimes give differing advice, or make med changes the other hasn’t, etc. I would also like to see a nephrologist for kidneys, but I understand they also deal with blood pressure. How does a patient know who to really listen too when there are so many doctors, each with their own specialty? Help!
Hi Deb, Very complex, and for this reason my comments are just that – I do not know all the facts about you. In general, the sartans work a lot better with either very reduced diet sodium or with a thiazide type diuretic. This is because either measure makes blood pressure dependent on angiotensin – which the olmesartan blocks. This might be a reason your BP is not easily controlled. Your drugs should not cause stones, but if they are uric acid stones I would not be surprised as urine becomes acidic with prolonged high blood pressure. Given your reactions to stress your physicians might want to consider a low dose of a beta blocker, but with the thickening of your heart muscle that approach is complex. You are right, your situation is very complicated, and one can only hope that one of your physicians takes the lead and gets your pressure controlled. Regards, Fred Coe
Hello Dr. Coe,
I appreciate this blog very much and have been following it for quite some
time after history of 3 calcium oxalate stones over the last 10years – I am 40 now, and have been do following all the dietary recommendations. After my last stone (in 2019) I seem to have developed elevated BP. I’m have ‘white coat’ but monitor at home (although also have very marked anxiety at home during measurements) – my measurements are usually around 110-115/83-86. I guess this is stage 1 hypertension, even though systolic is pretty low.
Would you treat this BP with medications?
I exercise regularly (several miles running/walking per day + yoga and sodium <1500). Trying to keep sugar to a minimum + potassium through food (although it’s hard to get enough potassium on a low oxalate diet). Have been doing lifestyle interventions for 2 years now, and no change to the BP.
My doctor does not think my BP necessitates medication yet.
Thank you!
I forgot to mention that ultrasound found one 2mm stone in right kidney in lower pole. It’s just been left there and they said no treatment was needed unless it became symptomatic.
Could this be a contributor to the isolated diastolic? What tends to cause isolated diastolic in active, Middle Aged women of regular weight, non-smoker? My GP does not think I need a referral to cardiology or nephrology at this time.
Being in this gray area gives me a tremendous amount of anxiety and stress, especially after 2017 guidelines updates. I am wondering if I should more actively push for meds, or just try and relax without checking so frequently (hoping less anxiety might bring diastolic down), generally.
Thank you kindly!!
Hi Lien, I answered below before seeing this. Daily measurements allay measurement anxiety – every day at some fixed time, never after eating or exercise. Elevated diastolic is expected in young middle age, so the elevation is not ideal – if it is really there. Fred
Hi Lien, Be sure about the sodium intake by checking 24 hour urine excretion – 1500 mg daily is hard to achieve. As for measurement anxiety, the best cure is measurement every day – after a while physiology begins to dissociate from psychology and you will get a true reading. The slight diastolic elevation is not ideal, so attend to the 24 hour urine sodium and of course any extra abdominal fat. Eventually, one’s physician has to decide. Regards, Fred Coe
Hi Dr. Coe,
First, I really enjoyed reading your article – never thought I would get a chuckle out of something about blood pressure and kidney stones. I was just wondering if having two stones within the span of a year is normal (more or less). I had one stone that passed during a visit to the ER (I think it was 4-5mm) and then a year later had to have a 1 cm stone removed via laser lithotripsy. I’ve also recently been diagnosed with high blood pressure (3 months after the second stone). Is it typically the case to be hit kind of back-to-back? Thank you!
Hi Beth, the lithotripsy is suspicious for causing BP to rise, and no – I am not surprised. I would do all the things in the article to lower BP and be sure and measure it at home – I think daily measurements are ideal because boredom sets in and anxiety dies out so you get a clear measurement. Regards, Fred Coe
My current situation is that I have very high blood pressure. Averages 150-160. I did not take it that seriously for years now, and was not getting good medical advice. I was on Lisinopril and Amlodipine, and frankly wondered if they were doing any good because my BP numbers were all over the place, infrequently as low as 140 or the high 130’s and sometimes as high as 170. I never felt I had a problem and my eye doctor said I have no sign of eye problems caused by HBP. I am 5’9″ and weight 235 and I know I am unhealthy because I feel terrible. My life is a disaster, and I want a life back. I am working now to exercise as much as possible, brisk to fast walking 5 times a week for 5 miles, usually takes me about 1hr 45min. After walking I feel great, but when I urinate it comes out brown like strong tea, and for the first time I have noticed solids or sediments in my urine.
Now I have a new medical practitioner and I went off the Amlodipine now for 3 weeks, because of edema … my feet were swollen over time and I did not notice it happened so gradually. Every time I got out for a long walk now I realize I come home and my urine is incredibly dark. I never noticed if I had this problem before, but it is like strong tea. If I drink a lot of water it goes away, but now after those walks I am seeing small solids in my urine for hours after I have walked. I have for a years now had difficulty urinating, frequent urination and very small volumes, 1/4 to 1/2 cup I would estimate. It also interferes with my sleep. I don’t feel I drink enough water, and have started making sure I drink at least 3-4 12 ounce bottles of water each day … but this is very hard for me for some reason. For some reason the seriousness of my health just has not hit me until recently, probably because I have mostly felt healthy, but not any more.
My diet now is mostly plant-based, but I also eat meat, but if animal based it is mostly fish, canned salmon or sardines when I do. I don’t really know how I let this situation get so bad other than a lack of energy or depression, and I am determined now to turn this around – I have to.
The walking I have been doing for about the last month, and the dark urine I just noticed by urinating into a clear plastic cup, so I don’t know how long it has been. I am fearful that I could possibly have bladder cancer, and the more I read the more I scare myself. In addition I have also had difficulty urinating, slow start, slow stream, and stop and starts for so long in my life that I just assumed it was normal. My diet for many years was very full of sugar, but I have almost completely cut that out now.
My immediate goal is to try to figure out how to find out confidently where I am and what my priorities should be, should I be lucky enough not to have a terrible or life-threatening illness. I feel like there are multiple issues and that I will be lucky if all of them are not serious. The more I read the more my mind spirals. Previously my doctors told me my issue was being over-weight and that if I lost weight my blood pressure would probably go down, but I have lost 10 pounds now and my BP is going up, I have also gone off the Amlodipine and the doctor is considering a different medication. My anxiety level is high, and it is hard to maintain a positive outlook as my medical insurance is not very good. I guess I am wondering if anything I am saying either raises red flags, or is something that can tell you what I should do and check off and in what order? What can or should I do? Can you please help me with some advice? I read a lot of good information above, thank you.
Sorry, I forgot to mention I did have a calcium kidney stone once about 20 years ago after an hours long bicycle ride in the hot sun. Never had a recurrence of that, but I am not sure what those solids are in my dark urine after my long walks lately … which is what brought me here.
Hi BPK, Have the material analyzed, that will help clarify matters. Fred
Hi BPK, You should collect some of the sediment and have it analyzed. It may be crystals. A good way is to urinate through a coffee filter held in a funnel, let it dry and ask your physician to have it analyzed by a kidney stone lab. Your physician can look at your urine and see if it is blood. As for blood pressure, you do not mention any attempts to lower diet sodium – a very beneficial aid to make drugs more effective. Regards, Fred Coe
Hello I would love some advice about my situation.
History: Kidney stones 22+ years ago found to be from prenatal vitamins (calcium) during summer (dehydration). Uncontrolled hypertension on and off since 24+ years (since first pregnancy). 3 years ago heart attack NSTEMI. 1 year ago diagnosed Hyperaldosteronism. Was switched from Triemetrene HCTZ to Epleranone (I also take Statin, Aspirin, Carvedilol, Amlodipine).
Epleranone causes extreme thirst for me and I am constantly drinking fluids and wake up 3-4 times per night for bathroom. Also feelings of dehydration such as dull headache. After starting Epleranone I gained 10 pounds within 3 months (saw nutrionist after Heart Attack my diet is very good more mediterranean style very low salt). Although I have elevated Aldosterone (maxed at 30), my Renin is extremely low which makes my PRA exteremly high. My doctor had me increase Epleranone to 3/day to try to push up the Renin. Within a month I had kidney stones which i thought was a coincidence (I had recently had a salt loading test and thought maybe that caused it.) When my Renin was still too low he raised my Epleranone to 4/day. I got kidney stones again within 1 week. When I reported this to my doctor’s office I was informed that “Epleranone does not cause kidney stones”. Perhaps not, but something did and it was too much of a coincidence for me (meanwhile even at maximum dose my Renin just barely made into normal range and the PRA still flagged extremely high. I went down to 2/day Epleranone and feel better. Finally saw Urologost (6 months after event) who scheduled me for a CT scan.
Should I get the scan now, or go back to 4/day Epleranone (which doctor wants) for a few weeks and then get the scan? I fear the scan now will show nothing but I hate to put myself though that again.
What can I/doctor do to raise Renin? Even when my Aldosterone was medicated well within normnal range, the PRA was still sky high due to the Renin.
I see a Cardiologist, Endocrinologist and now Urologist. Do I need a Kidney specialist? I thought the Urologist would help me with the Renin problem.
Note: HA is pretty rare and my Engocrinologist has only seen this 3 times in practice including me. I am willing to drive further but do not know how to find someone with extensive experience.
Hi Melissa, I presume you have bilateral primary hyperaldosteronisn – not surgically curable – and thence must rely on drugs. Failure of EPH to raise renin has been reported, and a newer agent worked, so perhaps this will be of use to your physicians. In a trial setting EPH caused little symptoms vs. amlodipine, and I suspect your weight gain may be from the latter agent. Specifically thirst and weight gain are not reported from EHP. As your physicians have not treated many primary hyperaldosteronism patients they may need to do a web search on PubMed to become familiar with the nuances of this complex system. In this limited venue I cannot provide a really proper review. Regards, Fred Coe
Hi Dr. Coe,
I need advice as to which type Dr. should be managing my care, or a RD? I aready have high BP, under control with 80mg Valsartan. I had my first and pray my only stone, last month. ER/hospital and then treated with lithotripsy. They took a CT scan in the hospital, then xrays. I passed what was left of the stone which the urologist tells me was 100% calcium oxalte. How do I know if I will get another one? They did not do a post lithotripsy CT, only x-ray. I did the 24 urine test–Dr. told me my citrate is low and prescribed 500 mg calcium and postassium citrate. They tested my blood, not parathyroid disease (don’t even know what this means). He told me no vitamin C and to eat a low oxalate diet. I have had foot surgery (couple months before the surpise stone) and am pretty sedentary right now, with the other foot to follow as soon as the first one heals (long story, it’s going slowly). I don’t know what to do–cannot really exercise, am struggling to adopt the low oxalate diet because I don’t have enough information–I asked about combining milk with (spinach) for example and Dr. laughed at me and said that wasn’t how it worked. I also take levothryoxine every morning which I absolutely need to function, and directions say no calcium for four hours after taking, so I am struggling. Any advice? I am trying to eat healthy, cut sugar, alcohol, salt etc. I am pretty sure I did this to myself by drinking 6 cups of tea a day for 30 years, along with a rather bad chocolate addiction. So I am trying to change those habits as well, so far so good, but it is hard. Should I go to a dietician? I can’t stand my urologist–not going back to him.
Hi KLE, postoperative simple x ray is common. Usually there are fragments left behind after lithotripsy, many of which will pass over some weeks. So a CT at one month or so is a reasonable idea. Low citrate is common among women with CaOx stones so the K citrate is a reasonable idea. The extra calcium is to reduce urine oxalate – if you take it with meals that contain oxalate that effects will be most beneficial: calcium in the GI tract reduces oxalate absorption. Hyperparathyroidism is diagnosed from blood and urine testing. The main criterion is high serum calcium which I presume you do not have. As for putting milk into spinach it is not a silly idea, but you are better off without that particular vegetable. Here is our low oxalate diet paper. Here is something much better – a proper diet for stone prevention. As for physicians, perhaps a nephrologist might be better suited to stone prevention. Also, given telemedicine is not chic you can get consultation from anywhere. Regards, Fred Coe
Thank you for your advice, I appreciate it. I’ve ordered a cookbook online for low oxalate eating, and am integrating the calcium and potassium citrate into my day. Onward and upward!
Dr. Coe, thank you for such a informative, understandable article. My husband has had cystine stones since childhood and has always had slightly above normal BP, but recently (likely due to COVID lockdowns and a distinct decrease in physical activity) his blood pressure has risen. Do you have any specific advice for someone with cystine stones?
Hi Kim, Cystinuria is a serious stone problem as you know, and needs very expert medical treatment. Higher BP and even reduced kidney function are common. BP treatment is the same as in all patients, just as outlined in the article you are writing on. But prevention of cystine stones is very difficult, drugs are available and not easy to use. Regards, Fred Coe
I have kidney stones because my body is not absorbing calcium so it’s going into my urine and forming stones. My doc put me on 3 different types of thiazide meds and potassium. With or without potassium, I experience horrible heart palpitations all day. It feels like I’m having a panic attack, so I cannot take those meds. My blood pressure is good, so I think the meds are negatively impacting my BP and causing intolerable side effects.
You mentioned ACE or ARB. Are there any other options?
Thank you!
Hi Tim, The thiazide are to lower urine calcium. This article helps explain the best approach to lowering urine calcium in idiopathic hypercalciuria – which I presume you have. The ACE and ARB drugs are to lower blood pressure which is for you irrelevant as you say your BP is normal. Regards, Fred Coe
Hello Fred. Could I ask does Kidney stones cause High Boood Pressure?
My husband jss always had kidney stones and the past 6 months his blood pressure has been sky high . Before it would go up but then go down. Now it’s continually high. He has been put on blood pressure Meds today. Will this help his stones at all ?
Hi Lisa, Indeed stone formers have increased risk for high blood pressure. The linked article is ideal for him as it points to the value of home BP and also presents current approaches to treatment, both drugs and diet + lifestyle. Regards, Fred Coe
Dearest Dr. Coe,
I was a patient of yours referred by Dr. Joseph Nuzzarello (Wheaton, IL) about 20 years ago with cystine stones. I subsequently have had surgeries, have passed several and currently have 3 stones in my right kidney. My major problem right now is high blood pressure. I have been on captopril 75mm 2x a day but I am stalling at high 140s/90s with high spikes as well. I am 58 years old and hope there is a “blood pressure cocktail” that I can refer my primary doctor to research. Also, should my blood pressure be brought up/treated by my urologist or remain with my primary care physician? I have to thank you for truly saving my life all those years ago. Meeting you and consulting with you gave me and my little family a new lease on life. You are my hero! Thank you! Lisa
Dear Lisa, The captopril is a dual purpose blood pressure medication that can bind cystine but is itself not ideal for blood pressure. Your blood pressure is best treated by a nephrologist because with cystinuria there is always some risk of loss of kidney function. Likewise, it sounds like management of your cystinuria has been less than ideal and should be bettered. This, too, is done by nephrologists with an interest in stone disease. If your personal physicians desire it, you might benefit from consultation at a center – as you did when I saw you years ago. With telehealth that can be remote. Regards, Fred
Having low blood pressure and stones in kidney and back pain very much And having tensions and what is solution required to solve this problem
Hi Manojj, Having a low blood pressure is usually a good thing unless your physicians have found something worrisome in your particular case. Pain and stones are never good, and prevention is workable. Here is my best effort at an introduction. Regards, Fred Coe
Hello Dr. Coe,
I had a stone pass in Dec., 2017. Subsequent ultrasounds since then have shown many small stones still present as of 2020. In fact, a very large stone was detected in my kidney which my urologist attempted to surgically remove, but couldn’t. So it remains embedded in that kidney.
I just recently had an appointment with a new primary care doctor (we moved to another state) and he felt that because of my high blood pressure readings (168/80) a diuretic was necessary. So, he prescribed Amlodipine-5mg. However, I questioned that choice because of reading that Amlodipine might add to the problem of kidney stone formation. So I had read your article suggesting Chlorthalidone as a high blood pressure med.
My problem is that some 50+ years ago I had a sulpha reaction (from an antibiotic). I cannot remember what that reaction was, specifically, so it must not have been more than a rash or itching of some sort.
Consequently, it seems that the Chlorthalidone would not be something I should take. So my problem is….with me being a stone former AND having had a reaction to sulpha,…what diuretic would you recommend for me?
Thank you!!
Hi B Felsecker, Things are a bit confused here. Amlodipine is a calcium channel blocker and suitable for lowering blood pressure. It is not a diuretic at all. CHlorthalidone is a diuretic and most of them have a central ring structure common to the sulfadiazine drugs. There is little cross reaction, however. But is everyone certain that a drug is needed for your stones? In the article my point was that when it was the diuretic would serve two purposes. Take a look at another more general and stone focused article and see if you have been evaluated fully and if so what is causing your stones. As for amlodipine causing stones, there is this article. For nearly two decades the stone field was infected by multiple animal experiments in which ethylene glycol was given to produce calcium oxalate crystals and this ‘model of human stone disease’ used to explore mechanisms of stone production and prevention. It was flawed as rodents given ethylene glycol in no way modeled common human stones. So I make of the linked article on amlodipine a a cause of human stones exactly what it is worth for that specific question: Useless. Regards, Fred Coe
Hello. My wife had stones and recently a hypertensive crises. Went to ER with BP of 200/130. They sent her home with Amlodipine and Lebetalol. Approx 3 months on meds so far and she’s lethargic, pressure normal ever since, but she just passed a new stone and is dealing with intense pressure. Saw ER, cat scan neg, passed blood but calcium still not really elevated…could this be the meds?
Hi Clayton, Her BP is very high and her meds advanced. The cause of the hypertensive event needs to be understood. Was it a panic attack, or one of the uncommon but important medical causes – her physicians know how to separate one from the other and diagnose the medical causes. Passing blood without stones – I think that is what you imply – could mean crystals are forming. Most important is the cause of her stones. A proper evaluation should reveal it. Her lethargy may be from her medications, so they need expert review as to need and dose – this is far beyond what I can comment on from a distance, but I might wonder if her physicians might not wish for consultation at a convenient medical school center as an additional aid to diagnosis. Regards, Fred Coe
I am a kidney stone producer with hypertension, pre-diabetes, and mild congestive heart failure. My cardiologist prescribed chlorthalidone 25 mg but would not prescribe the potassium citrate. Fortunately my primary care physician was willing to prescribe it. You mention to take the Chlorthalidone in the morning. I find that it makes me a little sleepy when I first take it so I have been taking it in the evening before bed. Is that the wrong way to take it?
Hi Genee, Are the stones calcium or uric acid. If the latter you need alkali. Perhaps it cannot be potassium based. Regards, Fred Coe
Hi Dr. Coe,
I was recently prescribed pantoprazole in addition to aspirin and clopidogrel following PCI with stents. I thought proton-pump inhibitors increase the risk of kidney stones, but the doctor told me pantoprazole does not. Is pantoprazole ok? If not, are any acid reducers ok to take? I have idiopathic hypercalciuria and have had calcium oxalate stones, but haven’t had any in more than 10 years. I take chlorthalidone and potassium citrate to help prevent stones..
Thank you,
Laura
Hi Laura, pantoprozol is a proton pump inhibitor. The drug is strongly associated with reports of reduced blood magnesium and potassium and calcium, acute renal injury and kidney stones. Here is a recent reference which is public. Short term use seems not unreasonable but not long term. Read the paper yourself. Regards, Fred Coe
Dr Coe, What an amazing article. I currently have 5MM stone partially blocking left ureter at top. And per the CT scan have a 3 or 4 more smaller stones inside my right kidney. I am currently on 100MG of Losartan, 5MG of Norvasc. Current BP taken 3 or 4 times a weeks is around 135/84. Also during CT they spotted a 1.7 cm right adrenal adenoma. (That was why I got the CT and finding the stones was a bonus). The puzzling part is, while not on your diet (yet) I am on a fairly good diet. I log everything I eat in a calorie app I am using for weight loss. I have brought sodium down probably over 2000MG per day and am average 1800. The part that is puzzling to all doctors and specialists is: My Serum Potassium was average about 2, over three to four test spread over a month. Doctor put me on 4MEQ of Potassium Chloride which has brought up potassium to bottom of normal at 3. I have been tested for hormone levels for adrenals and everything is normal. My potassium urine 24 hour test is normal range as well. Just seems like I need a lot of extra potassium. Sorry so long. Maybe you offer consultations for a fee over the phone? My docs have left me with little to no solution.
Hi Russ, I gather you have high blood pressure and a low serum potassium and that combination led to a CT to look for an adrenal adenoma as a cause, and stones were found incidentally and likewise an adrenal adenoma. Although I do not know the details of your situation and am an outsider, somehow your serum potassium was low and you are not taking a diuretic (I presume). If you are not taking a diuretic, and have not been taking a diuretic, how does one imagine the serum potassium was so low? There is also the stone obstructing your kidney. That needs attention as obstruction can damage kidneys. So the stone has priority. In terms of evaluating the function of the adenoma in lowering your serum calcium, it is not possible when serum potassium is low because low serum potassium itself lowers aldosterone secretion. One must replete the potassium, a time consuming business. Then, one needs to measure urine and serum also, renin, angiotensin 2, etc along with 24 hour urine sodium to decide if there is surplus aldosterone secretion. It is a subspeciality within speciality so your physicians may need to consult for specific details. In saying this, I am an outsider, know only what you have told me, do not know if you have been on diuretics so the whole potassium matter is moot -etc. Your physicians are entirely responsible. But perhaps my outsider remarks may be helpful. Regards, Fred Coe
Hi Dr Coe!
Your very special to offer such great advice and in my case I have a 9mm left lower pole kidney stone that’s been giving me bad lower back ache for many years so after failed Lithotripsy that was agony I’m scheduled for lazer treatment, I’ve now since 8 days had a double j stent and it’s excruciatingly painful when I urinate, my BP has always been high but I checked my omron tested machine and it’s 190/ 110 sometimes higher and this morning was 169/ 99 I should take Losartan 50 mg daily but I don’t so now at 70 yrs I need to start being less of a reble! So I took lasartan today and I keep doing so..After stent my BP was 210/ 115 I go lazer soon so not long now..this stent is no joy ride Dr as you can imagine, I have potassium citrate but not took any, im not constipated but was 5 days after stent, I am not dizzy or light headed but am lying flat in bed since stent but after lazer I guess I get another stent so I must man up to get through this..I do have strong oxycodone 10mg I’m just concerned there might be a reaction with losartan? Water I’m drinking enough..any advice most welcome Dr Cole..sincerely Steve
Hi Steve, Stents are horrid for everyone and pain raises blood pressure – a lot. Right now I would let my physicians know and let them manage things. When the stent and pain end, your BP will come down and you may well need meds. Do not omit them if prescribed. Home BP are very excellent and continue them. Losartan is fine in later life, incidentally. Best, Fred Coe
Hello doctor, its a great article wish i had read it in 2019.
I am 30 years old, 140lbs, 5’6”, had a history of kidney stones from almost 11 years. 5 years back(2019) to treat the 11mm stone in the lower ureter and hydroureteronephrosis, i had URSL. during my discharge my BP was 140/100, i was told its due to surgery. after that i never checked for 2 years.
in may 2021 , my bp was 118/72
in july 2021, my bp was 110/66
but when i checked on nov 2021 after the workout it was 172/107, i thought it was due to heavy workout
then i got checked for stones in feb 2022, i was told i have 6.5mm stone and 5mmm stone with hydroureteronephrosis, i passed both of them on april 2022 and august 18th 2022
then on august 31st 2022 i checked my bp it was 130/76.
in oct 2023 i went to doctor to check the headache and cough, at the time my bp was 160/120, 188/124, 150/90, i was told to measure in home for the next 14 days. it appears around same, so doctor put me in lisnopril 10mg.
with medication now my bp is around 120’s/80’s
in April 2024, i went to urologist for kidney stone checkup ( i do this checkups when i visit my home country generally once a year), i have a stone of 9.5mm in the mid ureter and hydroureteronephrosis) surprisingly i have no pain.
after learning that i have 9.5mm stone and hydroureteronephrosis, i started going all my health records and found that my bp is inconsistent and high when i have stone blocking the ureter.
can i expect my bp would became normal after URSL without medications?
Hi Lovely, obstructed kidneys can raise blood pressure, and it sounds like you do not always know when obstruction is present. As time goes on this repeated obstruction can injure the kidneys so it is crucial to find out the cause of the stones and prevent more. Basically, and put another way, your care is not ideal as is and prevention is the proper direction. Regards, Fred Coe
Thank You Doctor,
I asked for 24 hours urine and serum analysis, doctor told me once the URLS surgery is done i can do that.
My main concern is whether my Bp is permanent or temporary due to the obstruction that i am having now.
Hi Lovely, Measure your blood pressure at home and if it does not go down (systolic below 130) your physician needs to help reduce it. Regards, Fred Coe
Hi sir this is Hasib from Pakistan and i am 31years old now i have done my URS procure but my blood pressure level is not going down and there are two more stones in my kidney is this why the blood pressure level increase or in addition another reason too.
Hi Hasib, I think pain from surgery and stents can raise blood pressure a lot, so check it when you have fully recovered. If still high your physicians can control it with diet and medications. Regards, Fred Coe
Hello Dr Coe, Your article was very interesting. My husband has been diagnosed with a 14mm renal stone in the left kidney by CTKUB scan recently. This was after pain from a 4mm stone in the proximal ureter which we presume has passed as the pain has resolved.
My two questions are: 1) can ACE inhibitors and/or beta-blockers cause kidney stones?
2) if he has lithotripsy as planned, how can they ever analyse the stone fragments so we know whether they are formed form uric acid salts or calcium salts? (he has gout but cannot take preventative treatment due to allergy to allopurinol, and contra-indication to taking feboxustat (on apixaban for AF).
I am very keen he does not develop impaired kidney function as he is lucky to have normal kidney function being in remission from multiple myeloma.
Thank you again,
Susie
Hi Susie, ACE and beta blockers do not cause stones. I am suspicious his urine is too acidic and he forms uric acid stones. He needs a proper evaluation which will give the information needed for prevention. Regards, Fred Coe
Hi Dr. Cloe, My ckd 3a has been stable for over 8 years. I am on telmisartan 40 mg and potassium citrate 30 meq? should I be concerned of hyperkalemia? My potassium was within normal range after being on telmisartan and potassium citrate. Thank you.
Hi Elizabeth, No. Your level of renal function, dose of potassium, and drug pose no such risk apart from remarkable circumstances like extreme dehydration. Best, Fred Coe
I have the following conditions: hypertension, ckd 3a, and kidney stones. I am on telmisartan 40mg and potassium citrates 30 meq. I had a normal potassium level after being on these medications for one week. Should I worry for hyperkalemia?
Hi Elizabeth, I believe I answered this already: No. Fred