 Pieter Bruegel the Elder (1530-1569) painted ‘Children’s Games’ in 1560. It resides in the Kunsthistorisches Museum, Vienna.
Pieter Bruegel the Elder (1530-1569) painted ‘Children’s Games’ in 1560. It resides in the Kunsthistorisches Museum, Vienna.
On the Rise
If you read the many reviews that abound (Pediatr Ann. 2017;46(6):e242-e244; Bowen D K Urol Clin N Am 45 (2018) 539–550; Evaluation and Medical Management of Kidney Stones in Children 2014) they mostly all say the same things.
Stones are becoming more frequent among children and adolescents. Generally children form calcium stones, as do adults. They benefit from the same surgical procedures as adults but their smaller size demands specialized skills. Genetic causes of stones tend to manifest earlier in life and are therefore enriched among children.
What seems unique to children is their stone risk factors, and therefore I detail them here.
Stones Children Form
All of the reviews emphasize that children form mostly calcium stones. Of course cystinuria often shows up in childhood, being hereditary so that stone type is not rare. Calcium phosphate may be more prominent in children than adults given that urine pH falls with age. But with the exception that uric acid stones are uncommon in children, their stones are not very different from those in adults with idiopathic calcium stone formation.
Counting Stones in Children
One can assess new stone formation only by systemic medical history combined with CT images. Ultrasound is highly insensitive and non specific. The advent of ultra low dose CT scanners makes use of CT for children more reasonable as the radiation dose can be very modest. Even so, one wishes to hold radiation to the barest minimum. This certainly means that history and careful inspection of past treatment records should play the main role when possible.
Crystal passage with pain and hematuria is well known in adults and children. The syndrome is not uncommon as a presentation in children. I do not view it as separate from stones, and believe that it mandates serum and 24 hour urine testing to find the cause of the crystals.
Genetic Causes of Childhood Stones
I intend to write about these in greater detail in another article. I have already detailed renal tubular acidosis, and Anna Zisman cystinuria. Primary hyperoxaluria often causes childhood stones and kidney disease, and the site needs an article on it. A wide range of very uncommon genetic disorders cause hypercalciuria and likewise should have their own article.
So this topic exposes some real gaps on the site, and I will try to fill them in over time.
Idiopathic Calcium Stones Predominate
I put this large header here to emphasize that in general children form calcium stones without harboring systemic diseases as a cause. What follows concerns this vast majority of children and adolescents with idiopathic calcium stones.
Stone Recurrence in Children
 They recur, and as rapidly as in adults.
They recur, and as rapidly as in adults.
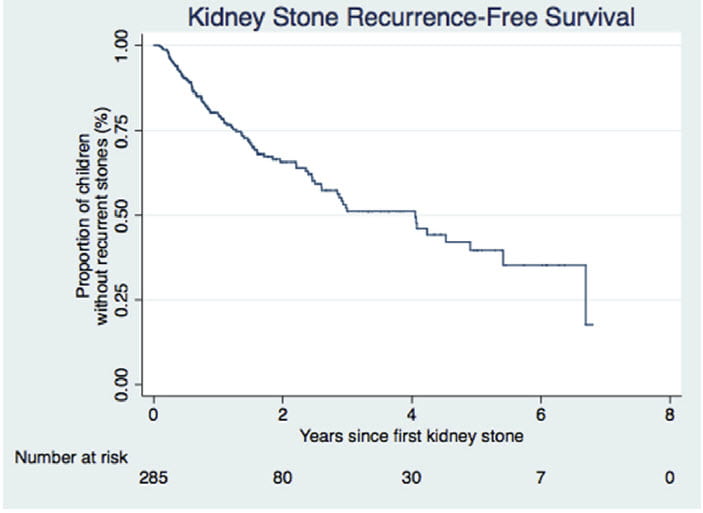
Here, 285 children, median age 14 were followed after a first stone. By three years after that first stone, about 50% had formed at least one more stone, and thereafter new stones kept coming.
24 Hour Urine Testing Reduces Recurrence
The scientists ordered 24 hour urine testing in all of the children, but only 161 got it done.
Those who did the urine testing had a lower rate of new stones. Partly they might 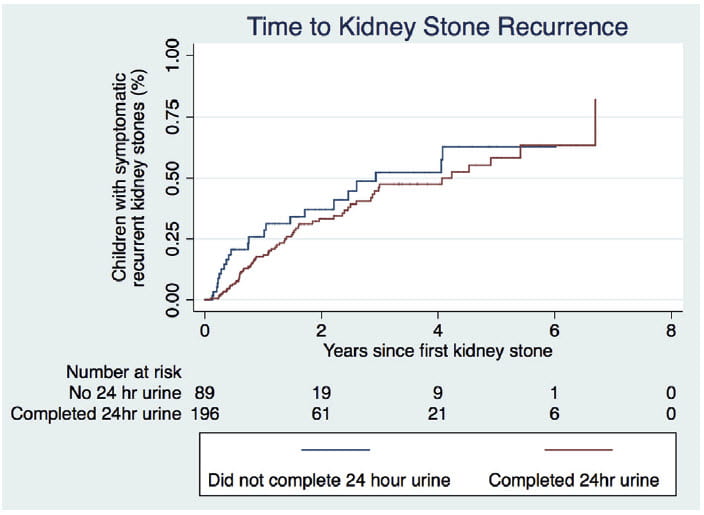 have been better about fluids and diet. Partly, those who did the urines got increased thiazide and potassium citrate.
have been better about fluids and diet. Partly, those who did the urines got increased thiazide and potassium citrate.
On the left, the lower of the two lines is from those who collected the urines. Being lower means fewer recurrent stones. The difference between the two lines does not look as impressive as it is. When the authors calculated the risk of another stone it was reduced by 60% in those who got urine testing.
Even more, when patients got treatments but no urine testing their risk of recurrence did not fall – random treatment was useless. Children who were tested and treated had less recurrence and are the reason for the lower placement of the recurrence line.
This tells us that 24 hour urine testing of children really helps. Random treatment without 24 hour urine testing did not reduce stones. Treatment after testing did reduce recurrence of stones. Children with stones need 24 hour urine testing.
Urine Stone Risk Patterns in Children
When I owned Litholink, we won NIH grant money to do a national survey of 24 hour urine stone risk in children. Six practices in the US collaborated with us to obtain 417 children age 6-17 years old.
Of these, 129 (73 girls) formed calcium stones. As controls we enrolled 105 siblings (46 girls) who formed no stones, and 183 (86 girls) non stone forming children who had no family history of stones but, arise from these same practices and lived in the general areas of the stone forming children and their families. We were able to study everyone in the absence of any medications that might influence 24 hour urine findings.
Urine Calcium
The Raw Data (Left Panel)
The left hand panel of this figure shows each child as one point. Urine calcium excretion – a main stone risk – is on the horizontal axis, and the fraction of children with each excretion rate on the vertical axis.
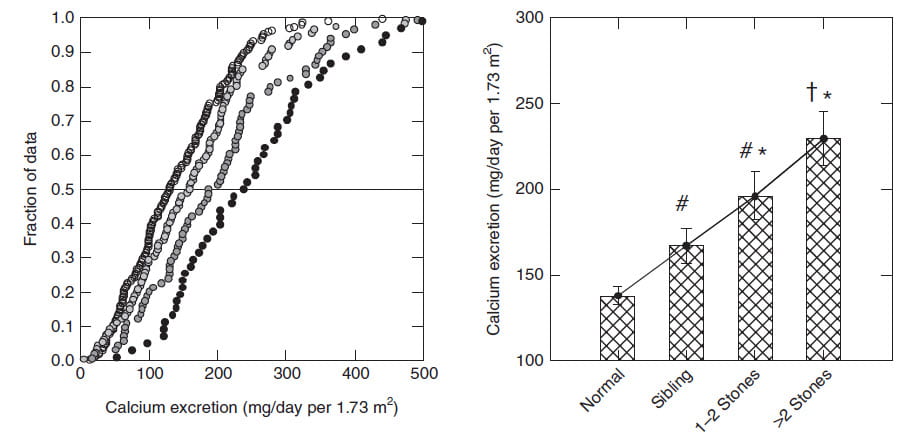
The leftmost curve is children without stones and from families with no history of stone forming. Their median urine calcium – the value at 0.5 or 50% – was about 100 mg/d. Only about 15% were as high as 200 mg/d, the beginning of stone risk from urine calcium.
The next curve is non stone forming siblings of the children who made stones. To their right are their brothers and sisters who made 1-2 stones, and the rightmost curve is children with more than 2 stones.
You can see how urine calcium excretion rises progressively as one goes from normals, to siblings – who share family stone risk but do not make stones – through to stone formers.
The Mean Values (Right Panel)
The right hand panel shows the mean values for each of the four groups. Siblings of stone formers were significantly above those of non stone forming children from families with no stone history (thence the # sign). Those with 1-2 stones were higher than the siblings, and those with >2 stones even higher – above all the other three bars.
Idiopathic Hypercalciuria Raised the Urine Calcium
This is perhaps the most dramatic illustration I know of how genetic (idiopathic) hypercalciuria works. Of course it runs in families, we proved that decades ago. But here its magnitude correlates not only with being a stone former but with the numbers of stones formed. This latter is a version of the much larger and more powerful epidemiology by Dr Gary Curhan who showed how urine calcium excretion is a graded stone risk factor.
Other Stone Risk Factors
How about oxalate, citrate, volume?
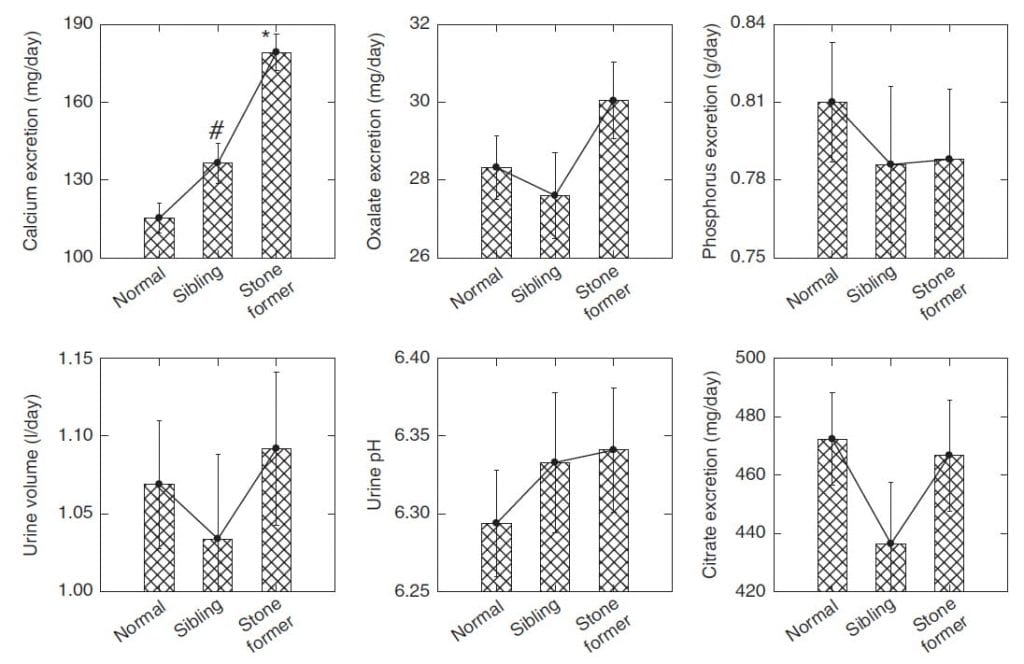
These rank with calcium as general stone risks.
But not here; they did not differ among our groups.
The calcium graph is copied at the upper left of this figure for reference. Siblings exceed normals, stone formers siblings.
For oxalate, which is in the upper middle panel, none of the bars differ. The same for urine volume at the lower left and citrate at the lower right. Urine phosphate, at the upper right and urine pH – bottom middle – are thrown in for good measure. None show anything.
In the paper we have another figure showing calcium, oxalate and citrate by sex and over age to see if oxalate or citrate perhaps might be different in stone formers from normals here and there. They are not.
So, only urine calcium, of all the four main factors – calcium, oxalate, citrate, and volume – stands out as a putative cause of calcium stones in children.
Supersaturations and Upper Limits of Metastability
Supersaturation is a powerful risk factor for calcium stones and the site has many presentations about it. The upper limit of metastability (ULM) is the supersaturation at which crystallization begins in a given urine.
Whereas supersaturation is calculated from the many ionic and molecular interactions in a given urine, the ULM must be measured by adding calcium or oxalate and determining when enough has been added to get crystals. From the amount added one can recalculate the supersaturation at that point, which is the ULM.
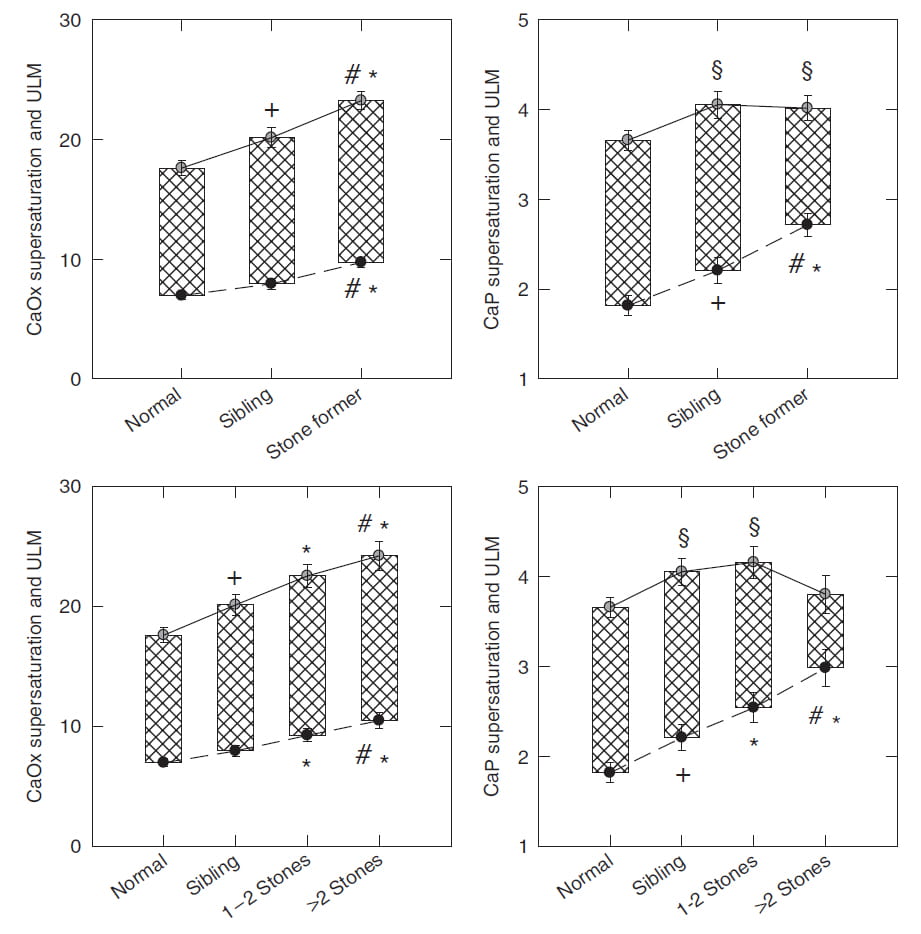
Put another way, if SS is the floor, ULM is the ceiling. So safety is when the SS is far from the ULM, danger is when they get closer together.
The ULM is not usable clinically because it is too expensive to produce for commercial testing. This work was supported by federal grant money that allowed us to make the measurements.
I have already shown you the supersaturations. These are the bottoms of the bars in each panel. As before, they rise from controls, through siblings to stone formers for both calcium oxalate (left panels) and calcium phosphate (right panels).
For calcium oxalate, the ULM values rise with supersaturation, so the distance between them stays reasonably constant. We found this years ago and have published the fact.
For calcium phosphate, the ULM does not rise with supersaturation as much in stone formers as it does in normals and siblings, so the ceiling is closer to the floor – greater danger. When you consider those with >2 stones – lower right panel – the effect is dramatic: the bar shrinks a lot meaning at the SS of the urine one is rather close to crystallization.
It is not oxalate nor pH nor urine phosphate, nor urine volume that causes these supersaturation in the stone formers. I showed you none of these differ between the groups of children. The effect is entirely from the higher urine calcium excretion.
How the ULM rises with calcium oxalate supersaturation and not with CaP supersaturation is not known. I have estimated from other data that the CaP ULM arises from urine citrate and perhaps inorganic pyrophosphate. But urine citrate is not different between stone formers and normals here, and pyrophosphate was not measured.
As Children Age Protection Wanes
Urine inhibits the formation and growth of calcium crystals. Part of the effect is from citrate. A large part is from proteins and other large molecules. We rarely speak about large molecule inhibitors on this site because they cannot be commercially provided as a clinical test. 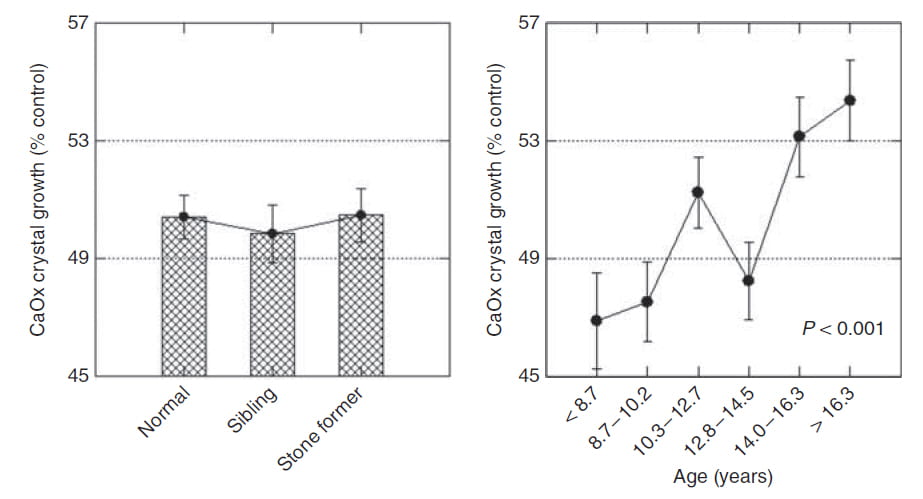
But in this grant supported work we measured the ability of urine proteins to inhibit the growth of calcium oxalate crystals and asked if it differed between groups of children and with age.
Crystals are added to a simple solution containing calcium and oxalate, and the rate of crystal growth measured continuously by increase of optical density at 37o. Control solutions had no protein, experimental solutions had 20 ug of dialysed urine protein.
Results for both panels are growth rate of pre-formed calcium oxalate crystals as a percent of control – no added protein. Higher values mean less inhibition.
The left panel makes clear that normals, siblings, and stone formers are all alike. Protein from urine of each group inhibits to slow growth to about 50% of that without added urine proteins.
But we had the chance to see what age can do.
On the right, we plot the effects of urine proteins from all children against their age. The youngest inhibit the most, to about 47% of control. The oldest, who are nearing adult life, do no better than about 55%. The p value refers to the significance of the increases in the means from youngest to oldest – age has a real effect.
I suppose this makes it easier for younger children to resist the supersaturation from hypercalciuria, and predicts that stone onset increases with age.
As for how protective inhibition wanes with age, nature is wonderful and I leave the problem to future scientists.
What Do We Do?
Exclude Genetic Causes of Stones
Serum and 24 hour urine studies can detect clues to most genetic causes of stones. Astute pediatricians are needed, however, to be sure subtle clues do not go unnoticed. Any genetic cause of stone in a child must be detected and managed properly. Once excluded, this will leave most children as idiopathic stone formers presenting early in life.
One might say idiopathic hypercalciuria is a genetic disease causing stones, but so far it is more of a trait than a disease. It can cause stones and also bone disease, but it would appear that proper diet management may be sufficient treatment against both. Unlike many of the other inherited causes of childhood stones hypercalciuria does not progress to kidney disease or involve other organs of the body – apart from bone.
Treat Most Children with Diet First
All children with stones need 24 hour urine testing, and most will need treatment directed at idiopathic hypercalciuria.
The kidney stone diet, with its low sodium, high calcium, low refined sugar, high fruits and veggies is ideal as a diet, healthy for children, and good for everyone. Especially children will benefit both from stone prevention and learning a good diet for a lifetime. Siblings and parents share risk for idiopathic hypercalciuria, so the diet is excellent for the entire family.
Attention to diet oxalate should always follow increase of diet calcium and reduction of diet sodium, to minimize food restrictions. But the very highest oxalate foods are not necessary for childhood health and should be avoided.
Add Drugs When Necessary
If diet cannot control the urine calcium, and stones continue, then thiazide or potassium citrate are reasonable additions to the diet. This strategy is essentially the same as for adults but more important in childhood. A good diet has multiple values for childhood stone formers and their families, and it seems unwise to abrogate diet efforts by an early use of drugs unless stone recurrences demand them.

Thank you so very much for this information. My daughter recently had a right nephrectomy due to a large kidney stone (2cm..not mm) developing and getting stuck in her ureter. We were uncertain as to how long it had been there, but there were additional stones in her right kidney. The damage was so severe to the kidney and ureter ruined that the best decision was to remove both the kidney and her ureter. Since that time, we have heeded the kidney stone diet and are anxious when the time comes to do another 24 hr urinalysis to see if her left kidney is free of stones.
I am always interested in reading about kidney stones in children, as I have yet to meet another mother who has had a child suffer through the experience. Thank you for your research and sharing your information.
Hi Melody, You are right to do everything possible to prevent more stones. The reason for the initial stones does not seem clear, nor what they were made of. All that matters a lot. Best regards, Fred Coe
Hi,
My 5 year old daughter has several gallstones and also 2 kidney stones, and produces some white urine at the start of every wee which her hospital have said is lots of little tiny stones. She is currently under investigation so we are hoping for results soon but thought I would share the results of the white stuff caught in one of her urine samples in case you had any ideas?
Sample
Type:Calculus
Calculus specimen site Bladder stone
PLEASE NOTE: Calculus analysis is a semi-quantitative method
and percentages represent the approximate
composition of mixtures of minerals.
Minor components <10% are not numerically
reported because of imprecision at this level.
Weight 12 mg
Macroscopic appearance Crushings/Fragments
Colour Off white/cream
Consistency Hard
Microscopic appearance Crystalline and granular
Calcium phosphate 61 %
Magnesium ammonium phosphate 39 %
Hi Nicola, The crystal composition is typical of kidney stone and there is certainly a cause lurking that requires expert care. I am sure her physicians will soon or already have disclosed the cause and plan treatment. Fred