 Do you need a low oxalate diet?
Do you need a low oxalate diet?
Who does?
Who does not?
How can you tell?
I chose the gorgeous painting by Raphael that hangs in the Musée Condé Chantilly because three surpasses one.
Who Needs Low Oxalate Diet?
Most of all, those whose stones contain calcium oxalate crystals and urine oxalate enough to promote such stones.
Less so those with systemic diseases – bowel disease, malabsorption syndrome, bariatric surgery, and primary hyperoxaluria – that raise urine oxalate. Their diseases require many treatments, only one of them low oxalate diet.
Therefore, I write here for only patients without a systemic cause of stones.
Do Your Stones Contain Calcium Oxalate?
If your stones contain little or no calcium oxalate crystals, and urine oxalate itself poses no danger to your kidneys, low oxalate diet is silly.
On the other hand, if your stones do contain calcium oxalate crystals, how much? Traces of the crystal, less than 10 percent, hardly bring it to the foreground. Even 20 percent is marginal. Above 10 or 20 percent calcium oxalate crystals in stones, consider lowering urine oxalate if high enough to raise risk of stones.
If you do not know what crystals make up your stones, struggle to find old analyses. Send all new stones for analysis. Stone prevention means crystal prevention. Stones are made from crystals. How can you prevent what you do not know?
But if all this fails, assume your stones contain calcium oxalate crystals because they are the most common kind. Even then, keep trying to get a stone analysed; you have built your treatment on a rickety foundation because a guess is just a guess.
Does Urine Oxalate Raise Your Risk for Stones?
It Does in General
In Gary Curhan’s wonderful study, the three bars represent two female (red) and one male cohort observed for decades. Some became stone formers, most did not. Twenty four hour urine samples drawn from both groups permit calculation of the risk from urine oxalate.
When below 25 mg/day urine oxalate poses no increased stone risk vs. even less than 20 mg/d. Thereafter, risk 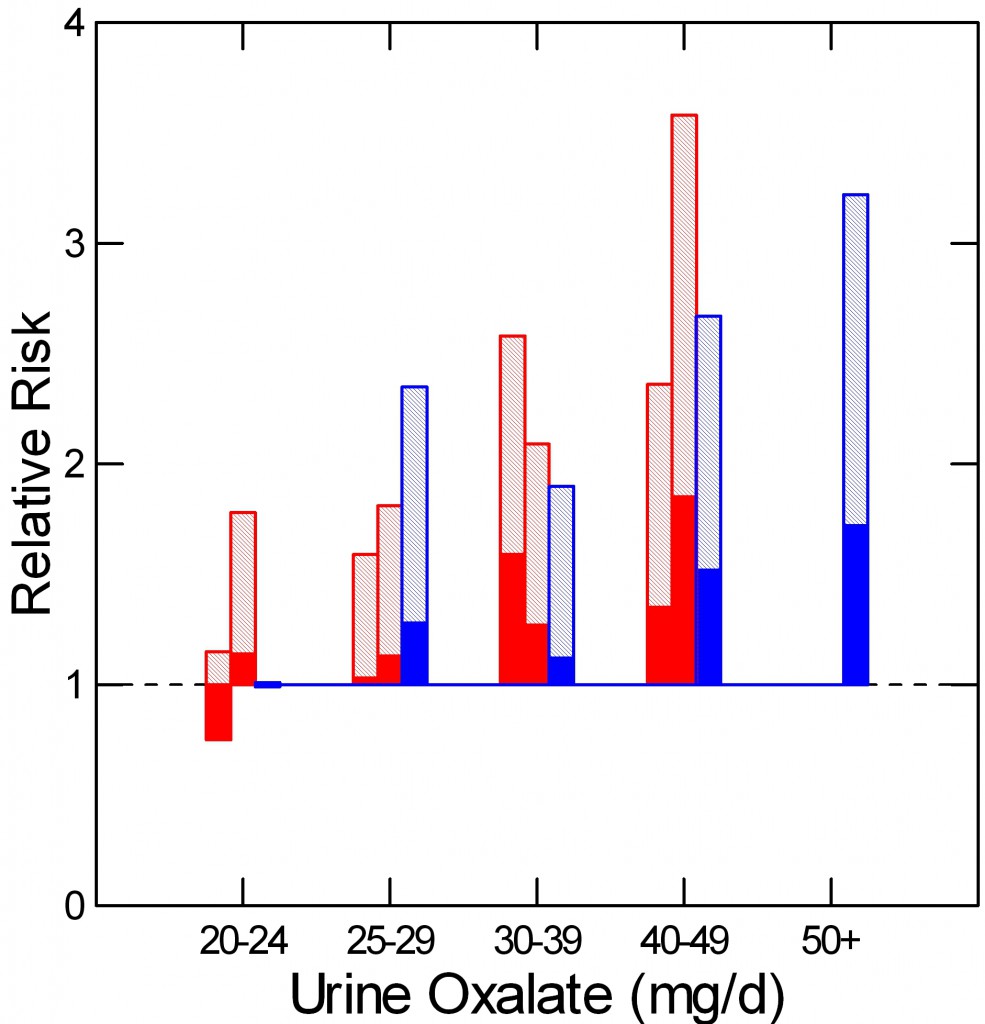 rises with urine oxalate, and low oxalate diet can contribute to stone prevention if stones contain significant amounts of calcium oxalate crystals.
rises with urine oxalate, and low oxalate diet can contribute to stone prevention if stones contain significant amounts of calcium oxalate crystals.
Although Curhan had no stone analyses, calcium oxalate – being most common – would have predominated by chance. This is why if you do not know what your stones are made of, and your doctor has no clue either – from seeing them, or from observations during surgery, you can make the same assumption Curhan made and guess calcium oxalate predominates.
It May In You
Avoid circularity. That urine oxalate levels exceed, for example, 30 mg/day, does not raise the probability that calcium oxalate crystals comprise a majority of your stones.
It is when calcium oxalate crystals make up a significant proportion of your stone crystals – over 20 percent as a first approximation, or when you have no idea what your stones are made of but employ the Curhan conjecture favoring calcium oxalate that urine oxalate excretion matters. When above 25 mg/d you have a reason to lower it.
Be careful here. Follow the logic. Keep that oxalate list in the drawer for now and think about what you just read. If the trail of ‘ifs’ lead you on to urine oxalate as a suspect and you are in the right group – no systemic diseases, no kidney risk from oxalate according to your physician – continue reading.
Raise Your Diet Calcium
Here, I am repeating material that is in another article that has its own video. I do this to integrate that material with the richer treatment of diet, stone analysis, and urine oxalate analysis presented here. The linked article details how to best manage diet calcium and sodium, the present article gives the details in a larger context.
Diet Calcium Lowers Urine Oxalate
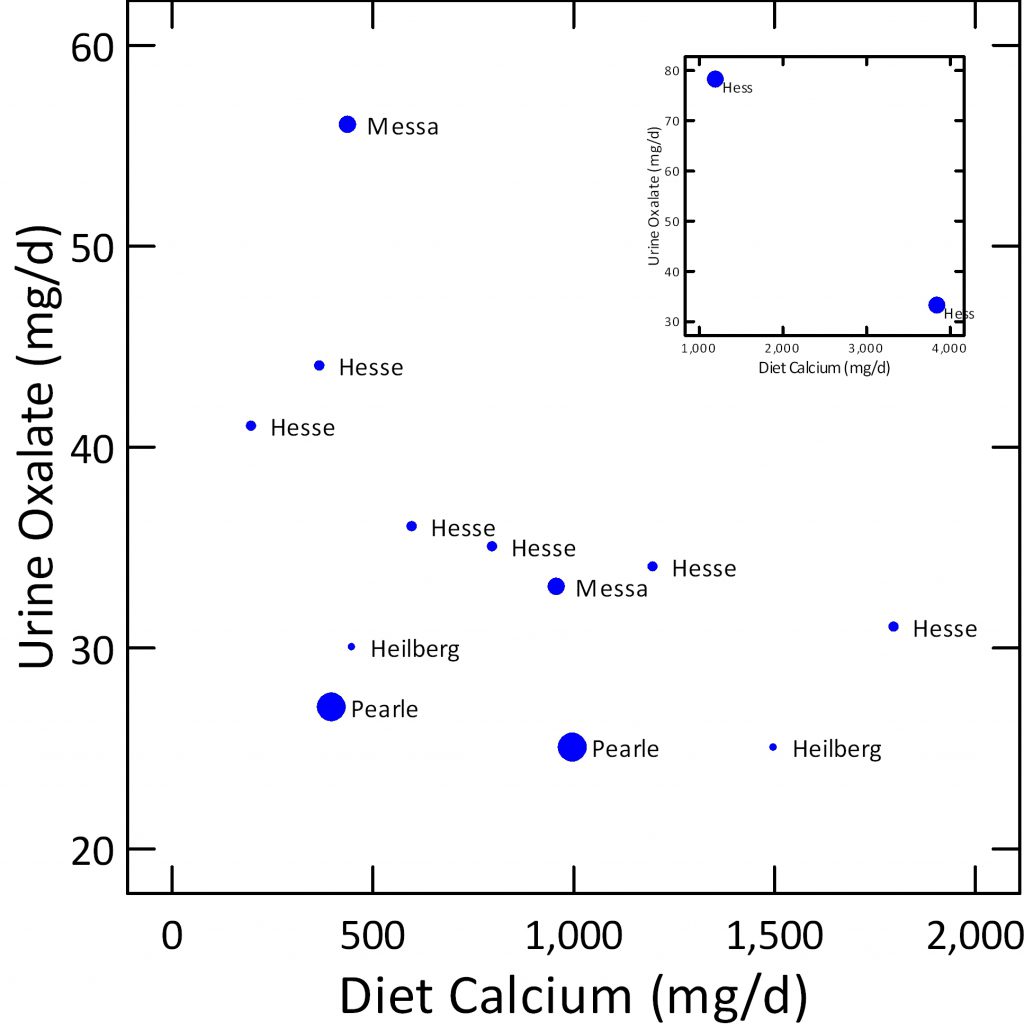
To illustrate the effects of diet calcium I have gathered average urine oxalate and diet calcium figures from multiple research papers named by senior author.
Dot size shows mean diet oxalate – the largest 200 mg/day, smallest 50, and middle 100 mg/day.
In each study raising diet calcium lowered urine oxalate. Diet oxalate itself had little effect.
The small box at the upper right shows an extreme experiment. Eating 2,000 mg/d of diet oxalate and 1,200 mg of calcium, subjects excreted 80 mg/d of oxalate. Despite the massive diet oxalate, enough diet calcium – 4,000 mg/d lowered urine oxalate to 30 mg/d.
Be careful. No one wants to eat that much calcium. The experiment simply aimed to make a point. My point is you eat 1,000 to 1,200 mg of diet calcium, and be done with it.
In other words, for any reasonable range of diet oxalate, diet calcium strongly controls urine oxalate. For that reason, measure the urine oxalate during high calcium diet and decide if low calcium diet remains important.
Diet Calcium Protects Bone Mineral
Even without stones we should want abundant diet calcium. Based on thorough reviews of mineral balance USDA and its scientific advisors recommend 1,000 to 1,200 mg of diet calcium daily for all US people as a benefit to bone health.
Because idiopathic hypercalciuria affects a majority of calcium stone formers they benefit especially from high calcium diet. Some people with IH cannot maintain bone mineral balance even on the high calcium intakes recommended for normal people. Less than high calcium diet poses risk of bone disease in later life.
Diet Calcium Should Come From Food
Like most people, stone formers without systemic diseases do well with just dairy products and need no supplements. Industry makes them sans lactose, sans fat, in all the forms diet restrictions require. One might say the 1,000 or 1,200 mg of diet calcium best comes by parts in all the meals. If so, diet oxalate will encounter diet calcium by chance most of the time, so calcium can reduce oxalate absorption and thence urine oxalate excretion.
What About Supplements?
Like with high calcium foods, calcium from supplements lowers absorption of oxalate when they meet during a meal. No meal, they serve no purpose. Worse, they can raise urine calcium and risk of stone.
Lower Your Diet Sodium
If high urine oxalate raises risk of stones, so does high urine calcium. Both count. But raising diet calcium can raise urine calcium. So if all you do is eat more calcium you may not stop forming stones. You need to do one other key thing.
 The trick, the smart move, the center of the center: Keep diet sodium as low as possible.
The trick, the smart move, the center of the center: Keep diet sodium as low as possible.
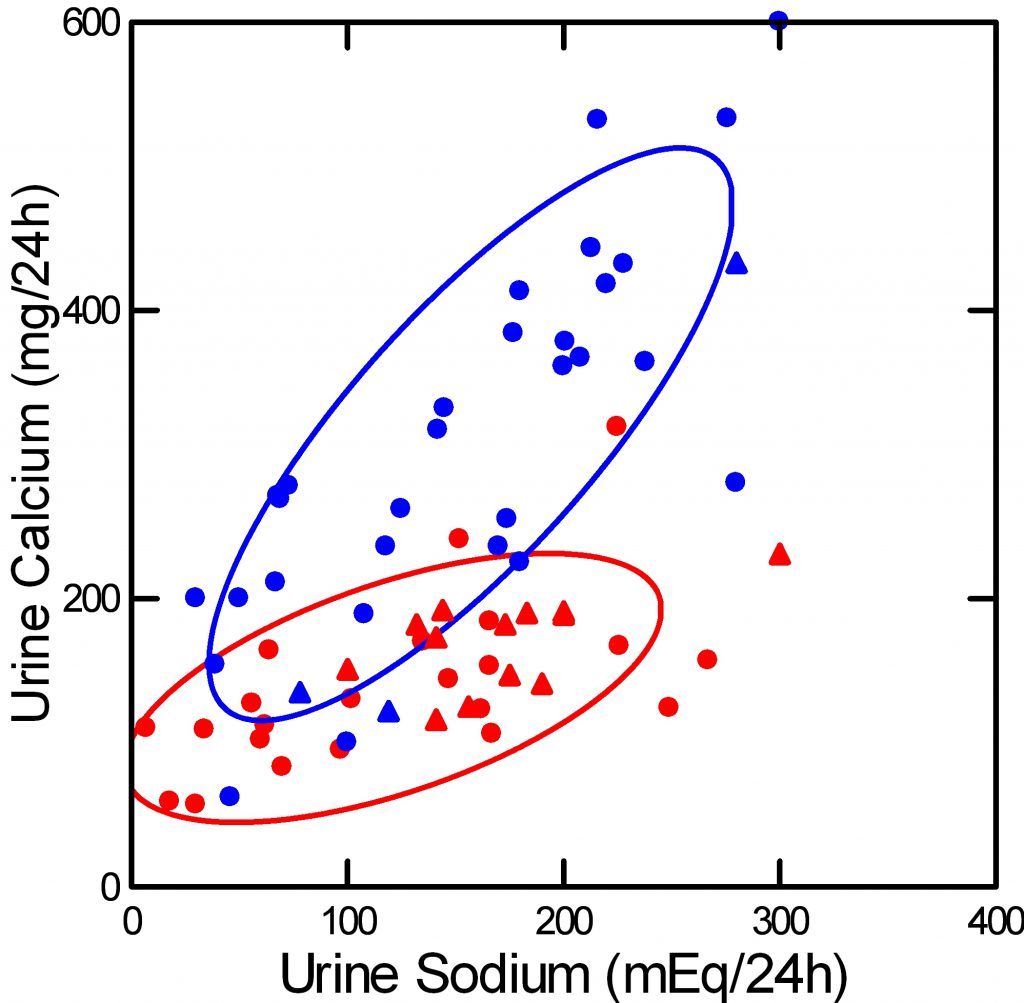
Red dots are normal people, blue stone formers with idiopathic hypercalciuria. For both, urine calcium rises with urine sodium, and urine sodium – more or less – reflects diet sodium intake. Each dot represents an entire published study group.
Modern diet recommendations for US people consider 100 mEq/d (2,300 mg) of sodium the tolerable upper limit. These diet guidelines do not concern stones but rather high blood pressure and bone disease, but even so fit well with our needs. You would want to lower your diet sodium below 2,300 mg/d even if you formed no stones, for your blood pressure and general bone health.
In fact, the ideal diet sodium is far below 2,300 mg, at 1,500 mg – or 65 mEq if you prefer.
With care for diet sodium, high calcium intake need not raise urine calcium and certainly will lower urine oxalate. Lower urine oxalate without any rise in urine calcium means a fall in stone risk and therefore fewer stones long term.
Low Oxalate Diet Seems Easier
What?
He tells me to obsess about my stone crystals, raise my diet calcium, and lower my diet sodium. Two diet changes!
Why not just lower diet oxalate in the first place and be done?
Low Oxalate Diet Serves Only One Purpose
Low oxalate diet provides no health benefits apart from stone prevention. The highest oxalate foods, some dark green leaves, have good nutritional value. No data support diet oxalate as cause of any significant diseases apart from kidney stones. If you need to rely only on low oxalate diet to lower your urine oxalate then the diet may need to be very strict and restrictive of otherwise good foods. Higher diet calcium makes it easier and allows for greater variety.
Low Oxalate Diet Has Never Been Tried as a Stone Prevention
No one has yet published evidence that low oxalate diet itself prevents calcium oxalate stones. At most, trials of other agents or diets have specified some restrictions of diet oxalate.
High Calcium Low Sodium Diet Prevents Stones
US diet recommendations favor low sodium and higher calcium to prevent hypertension and bone disease. One formal trial proved this kind of diet prevents calcium oxalate stones.
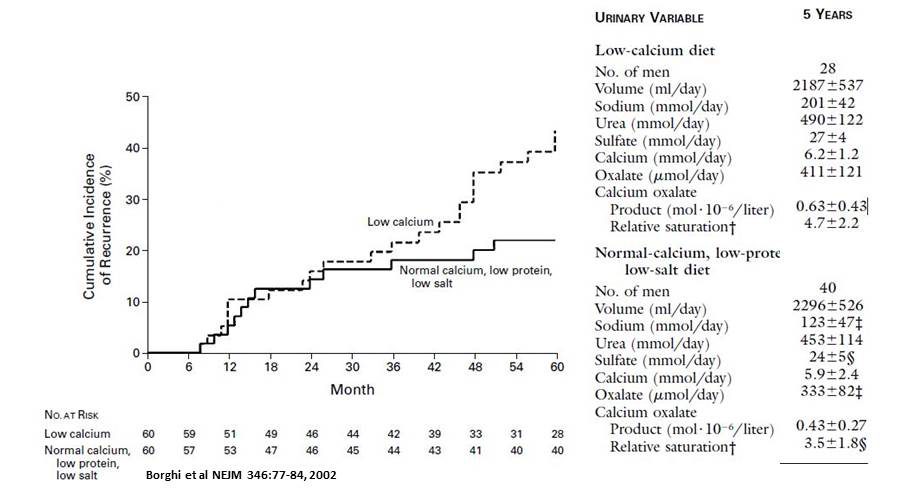 That trial showed that a high calcium, low sodium diet reduced calcium oxalate stone recurrence in men with idiopathic hypercalciuria.
That trial showed that a high calcium, low sodium diet reduced calcium oxalate stone recurrence in men with idiopathic hypercalciuria.
Over five years, stones were less (solid line) in men asked to eat 1200 mg of calcium, 200 mg oxalate, 65 mEq of sodium compared to men eating 400 mg/d of calcium, unrestricted sodium and oxalate (dashed line). The 200 mg of diet oxalate in the high calcium group was achieved simply by excluding very high oxalate foods like spinach and nuts.
Although diet calcium was twice as high, urine calcium in the low sodium group was the same as that of the low calcium controls (5.9 vs. 6.2 mmol/d). Even though diet oxalate was 200 mg/day, not very low, urine oxalate was lower in the high calcium group (333 vs. 411 umol/day – about 35 vs 43 mg/d) and it is this reduction that reduced supersaturation and presumably new stones.
So low oxalate diet has no trial but high calcium, low sodium diet has one trial, a positive one at that.
Low Oxalate Diet is Not Easy to Follow
I know that from the many comments on this site, from decades of practice, too. One can lower diet oxalate. Those who form calcium oxalate stones are well advised to be wary of high oxalate intake. But why strive to go below 200 mg of diet oxalate when you can just eat more calcium and less sodium which helps your bones and your blood pressure? Let us make that diet – higher calcium, lower sodium our goal. With it, you need not so much a ‘very low’ as a moderately low – 200 mg – oxalate diet and that may be enough.
An Important Oxalate Authority Recommends a Lower Goal
Despite the one trial, Dr Ross Holmes favors somewhat less daily oxalate.
He wrote on this site: ‘Hi Dr. Coe. I think you have been too cavalier in setting 200 mg oxalate as an appropriate target oxalate intake. Several studies in individuals eating controlled diets with adequate amounts of calcium have shown that the average amount absorbed is 8% with about half of that occurring rapidly in the small intestine. That is about 8 mg of oxalate that will flood the kidney within an hour or two after ingestion. Those great studies of Dr. Curhan that you have often mentioned show that this amount of oxalate in urine will substantially increase the risk of forming stones.’ (italics added for clarity).
Essentially Ross makes this point. The immediate inflow of oxalate from a 200 mg/day diet – if all 200 mg were eaten in one meal – could flood the urine with as much as 8 mg of oxalate in an hour or two (1/2 of 8% of 200 mg). That flooding could produce transient high urine oxalate concentrations. High diet calcium might not prevent such a happening. A lower goal of 100 mg offers what he might call an extra margin.
Ross is a wonderful scientist whose work has informed oxalate research for decades. So I tend to respond to what he says.
The transient flooding – stone risk mechanism presumably affected the Borghi trial. Flooding would matter less if one avoids eating all 200 mg of oxalate in one meal. But even so, I accept his comment and suggest that 100 to 200 mg is perhaps preferable to a simple 200 mg goal- with care to avoid eating all of it in one meal.
Let Us Focus Elsewhere and Better
High calcium, low sodium, and moderate oxalate seems the best plan. There is a trial of it. Three separate factors all point at stone reduction. Two of them, low sodium and high calcium confer health benefits beyond stone disease. As part of a threesome, diet oxalate lessens in intensity. The ‘list’ needs contain only the highest oxalate foods. The budget of 200 mg/day is large enough to permit considerable freedom.
More important than everything I have said so far. Do not begin with a reach for the oxalate list. The list at best adds value for some patients. You may not be that patient. You may not have an oxalate problem at all. If you do, higher diet calcium and lower sodium may solve your problem with a minimal effort toward diet oxalate.
Put your money on the high cards, on the best horses, the best teams.
In case you wonder about the three goddesses, it is for the three fold plan: Higher diet calcium, lower diet sodium, moderate diet oxalate. Not so pretty as they are, but good enough.


Thank you Dr. Coe, I was getting ready to go crazy on lowering oxalates…So , before my last kidney stone episode ( and first!) I had been researching the benefits of cocoa – not the sugarared kind, just raw cocoa – and had been making these wonderful smoothies with frozen bananas, cocoa, a small bit of honey, a little bit of milk or yogurt. After the kidney stone, I quit all cocoa, as well as avocados and walnuts and almonds…And no more spinach , all favorites for me. I thought since my first stone was at age 60 the culprit was the cocoa…But from reading this, maybe not? If the cocoa is with plenty of milk or yogurt, does it cancel out the bad?
Thank you so so much!
Debbie
Hi Debbie, The message is simple: Lots of diet calcium with meals and as little sodium as possible will get you a lower urine oxalate and controlled urine calcium with a net gain. Be sure to retest on such a diet and be sure things are as you expect – diet is tricky. Smoothies are a common problem because they concentrate too much into too little. Try eating your foods as they come. As for cocoa with milk it should be fine – do it and check out the urine if that is to become a habitual snack. Regards, Fred Coe
Check the urine for what?
Hi Lillis, in stone disease it is most efficient to obtain a 24 hour urine that includes all of the measurements relevant to stone prevention.They are sold as a recognized panel. Regards, Fred Coe
Hi Lillis, in stone disease it is most efficient to obtain a 24 hour urine that includes all of the measurements relevant to stone prevention.They are sold as a recognized panel. Regards, Fred Coe
Thank you Dr. Coe. Very informative. I am working with my doctor on getting a handle on Calcium Oxalate and Acid Stones. Putting together a diet is tricky. Is there a book you can recommend?
Thank you again. Ron
Hi Ron, Try this article about treatment. It links well elsewhere, too. Regards, Fred Coe
Hi Dr. Coe…You answered my biggest question about oxalates. Aiming for 200 mg/d oxalates with high calcium of 1200 mg/d and 1500 mg/d sodium answers my questions all in one equation. It fills in the last part for me. Love your article. Thank you for all you and Jill have done for stone sufferers. We need you both!
Thank you!
Kathleen
Hi Kathleen, I am glad this works for you. Regards, Fred Coe
I tried a low oxalate diet and was miserable. I’m also diabetic and had some restrictions. Now I eat all foods in moderation and try and drink a glass of milk or eat cheese with foods high in oxalate. I eat nuts but not daily, olives and chocolate and I’m sure a million other moderately high oxalate foods. I don’t eat spinach or anything else from the high list except for nuts and chocolate which I’m not prepared to give up, so I limit them.
Hi Michele, Just be sure to do all three – the high calcium and low sodium; both may benefit your other conditions as well as control urine oxalate. Regards, Fred Coe
Hi Dr Coe,
I would be lost without your and Jill for sure!!
I have all the figures for Sodium, Water, Oxalates and Calcium, but is there one for Sugar? I have read women should not have more that 6 teaspoons of sugar a day. That is A LOT. I know sugar is bad for Calcium Ox stones, but is there a low figure amount we could have that would be safe?
Also, it is all quite overwhelming as to have to count all this stuff. Is there anywhere on your website that would list sample menus for breakfast, lunch and dinner and snacks that WOULD be safe for us??
It would be sooo much easier for us to be good if we could just follow along. At least to even get a look at what is safe without having to look up all the values each time of everything we are eating.
There are Paleo, Gluten Free, Low fat and tons more cookbooks out there, but I have never seen a Kidney Stone cookbook. It is MUCH needed.
Thankyou so much,
Renee
Interesting article, but I am confused. I had symptoms of burning after urinating. My first urine analysis showed microscopic traces of blood and raised level of calcium oxalate crystals. I was given a list of things not to eat and sent on my way, and made to believe I probably have kidney stones. This was in December and my symptoms still come and go, but I have never experienced renal colic (thank God) or had any significant pain. I think I may have passed one stone, but not sure. I have seen black flecks in the toilet bowl sometimes, and a couple of grains of what looks like sand. But that is all. I recently went back to my doctor and this time my results show no blood or crystals, but slightly raised urinary calcium. I am awaiting oxalate levels from a 24 hr test. If that comes back high what would you recommend? And should the calcium test have been done over 24 hrs to? I really am confused and quite worried.
Hi Alison, I guess your confusion is reasonable as so much is not known. Do you have stones? So far nothing says so. When some grains of sand next appear collect them and get them analysed – even tiny ones can be analysed successfully. The tests needed are 24 hour urines that contain oxalate and calcium and all other measurements together in one place so one can tell what is going on. Given no stones, however, are your physicians sure you need treatment?? Regards, Fred Coe
Hi again. Thanks for replying. I got the results of my 24hr urine analysis today – it shows a normal oxalate level of 28.1mg/24hr – higher level is 31mg/24hr. Weirdly my symptoms were a little better while I was doing the collection. The calcium level was not done over 24hrs, but rather was a morning sample and was slightly elevated. I also had an ultrasound and they found no stones. I guess I need to go back with my results and see what my doctor says. The food list I was given included all the ‘high oxalate’ food but also dairy products. A bit confused, that’s for sure!
Hi Alison, I wish you would get all your numbers from 24 hour urines – it is hard to estimate sodium and calcium otherwise. Oxalate is clearly not your problem, not perhaps calcium is, or citrate. As for an oxalate list, it seems beside the point. Take another look at the article and see how low sodium high calcium is the best bet. It is hard to know much without 24 hour urine testing as a guide. Regards, Fred Coe
Hi Alison, I wish you would get all your numbers from 24 hour urines – it is hard to estimate sodium and calcium otherwise. Oxalate is clearly not your problem, not perhaps calcium is, or citrate. As for an oxalate list, it seems beside the point. Take another look at the article and see how low sodium high calcium is the best bet. It is hard to know much without 24 hour urine testing as a guide. Regards, Fred Coe
Hi Dr. Coe. I think you have been too cavalier in setting 200 mg oxalate as an appropriate target oxalate intake. Several studies in individuals eating controlled diets with adequate amounts of calcium have shown that the average amount absorbed is 8% with about half of that occurring rapidly in the small intestine. That is about 8 mg of oxalate that will flood the kidney within an hour or two after ingestion. Those great studies of Dr. Curhan that you have often mentioned show that this amount of oxalate in urine will substantially increase the risk of forming stones. I like Michelle’s comments above. Avoid the high oxalate foods and limit those favorites you enjoy. I think 100 mg is easily achieved without much sacrifice and the need to count oxalate values.
Hi Ross, I took the number from the one trial – Borghi’s – that was successful. Gary Curhan’s data are based on 24 hour urines and one cannot extrapolate from them to what happens transiently after an oral oxalate load. But, I so much respect your own terrific work on oxalate that I will amend the article to include the issue of transient loading and suggest the lower value of 100 mg might be more prudent. What we need is another trial of calcium and sodium management with perhaps 2 levels of diet oxalate. Thanks for the comment; look for the changes in a few days. Regards, Fred
Hi Fredric, you ask “Who Needs a Low Oxalate Diet?” answering your own question, “Those whose stones contain ca/ox and have high urine oxalates … accept for those who suffer from systemic diseases like bowel disease, primary hyperoxaluria”.
As you know we have many members in our MSK support group who make calcium oxalate stones, many suffer from bowel disease. As far as I know none have been diagnosed with primary hyperoxaluria yet, can I ask what the testing for this disorder is? By gene testing or are there other tests available? Thank you!
Hi Celia, The primary hyperoxaluria patients have very high urine oxalate – over 80 mg/day – that does not respond to change of diet calcium or oxalate and is not due to bowel disease or other causes. Gene testing is useful once those facts have been ascertained. Organic bowel disease can produce considerable increase of urine oxalate and needs special care – I have not written about these conditions yet. Warm regards, Fred
Thanks Dr Coe, I feel better already!
Hi–is there a downside to taking, say, calcium citrate supplements with meals in lieu of dairy? Dairy can be inflammatory and I had cut it out of my diet in favor of 4 x 200 mg calcium citrate tabs taken strictly with meals each day. I have IH and osteoporosis. Unfortunately, while on 25 mg chlorthalidone and observing appropriately low Na (<750 mg/day) and protein restrictions (about 45 g/day), my last urine Ca was 388. Horrified and wondering if (a) it's the supplements that are doing it and (b) if so, whether that adversely affects calcium balance and bone loss, or whether the bones aren't being hurt. I have never formed a stone, oddly enough.
Hi jenny, I am concerned, too. Was the urine sodium really low as you say? Was the PCR – protein intake – around 0.8? Do you really time the supplements with the food. If so, I would stop the supplements and repeat. Regards, Fred Coe
Hi Dr. Coe, thank you for addressing my comment on the Crystal Light page. I enjoyed reading this one as well.
Here is an article http://www.bestchinanews.com/Health/7301.html , regarding drinking Tea with Milk as a means of reducing its Oxalic acid absorbability (although another article mentions that Black Tea is not very absorbable in the first place). I wonder if the English across the pond who incessantly drink Tea with milk in, have increased their calcium intake significantly enough to reduce kidney stones on a national level in comparison to the US. The article also states, “Intestinal probiotics can degrade oxalic acid”.
I also liked to share with everyone this article https://www.researchgate.net/publication/308962080_Addition_of_calcium_compounds_to_reduce_soluble_oxalate_in_a_high_oxalate_food_system
Another article mentions that high oxalate foods differentiate in their absorbability which I think could hint to a more honed approach to eating oxalic acid rich foods. This is the list of foods that the University of British Columbia stated had oxalates that were absorbable “peanuts, pecans, wheat bran, spinach, rhubarb, beets and beet greens and chocolate. While other foods are considered high in oxalic acid, studies have not shown that the body readily absorbs their oxalate content. These include soy foods, sweet potatoes, black tea, berries and other dark leafy greens, like Swiss chard and collards.” http://healthyeating.sfgate.com/oxalic-acid-foods-8447.html
Yet another interesting article calls for the modification of our crop growing methods by which it proved it could reduce the oxalic acid in spinach by 2/3rds, which would increase the calcium bioavailability from spinach. http://www.techbriefs.com/component/content/article/ntb/tech-briefs/bio-medical/498
Lastly, here is an article that states that a study on the low oxalate diet shows it reduces the risk of kidney stones by 14% while the DASH diet reduces it by 35%.
Thanks again Dr. Coe.
http://www.belmarrahealth.com/kidney-stone-risk-may-be-reduced-with-a-dash-diet-plan/
Hi Sheldon, The effects of calcium intake on urine oxalate are much more accurately documented on the site, as I actually compiled the data from the only available experiments into a usable graph. The graph is in the article to which you have appended this very note!
The material about low oxalate diets and stones are not as you say. They are not trials but epidemiological associations between remembered diet intake and new onset of stones. No trials exist for low oxalate diet.
As for bioavailability of food oxalate, my only authority is Dr Ross Holmes who did much of what we have available, and he does not agree that these foods are indeed more safe.
Best, Fred Coe
Thank you Dr. Coe for your insight and help. Could you help me find the list of foods which Dr. Holmes deems less bioavailable in regards to oxalates and maybe also the ones that really bad for you. Thank you, Sheldon
Hi SHeldon, The food lists in this article are graded from bad to better. I would advise avoiding those in the top 20 – look at the graph in the article that shows the worse 89 foods. Perhaps the top 30. Then, recheck your urine and see if your oxalate is still above the stone risk of 25 mg/day. If so, go down 10 more on the graph. Regards, Fred Coe
Thank you for the link and the advice. I’ve read of the high oxalate content of date fruits and its listed as 24 in just one date. I wonder if it was a specific variety being tested. As I understand it, there are a multitude of varieties. The two I’ve been exposed to on the market are Mejdool dates & Deglet Noor dates. They are easy to eat, high in fiber & potassium and have other benefits. I wondered which type were tested. I found a pdf, which I’ll provide, that tested 8 different varieties which I’ve never heard of but one, Deglet Noor, which they recorded as “Total oxalate (g/100 ml) 0.432±0.038”. In the opening paragraph of the paper it stated that the 8 date varieties they tested were low in oxalates. I don’t understand the values they attributed to the Deglet Noor variety. Are they in fact low in oxalates? If the values are low, can the source of the study, in your opinion, be trusted? https://www.ajol.info/index.php/ajb/article/download/80650/70891
Hi. This is interesting news and a relief for my adolescent daughter who doesnt have kidney stones but suffer pain in urination and burning skin, particularly after nuts, dates or a smoothies(spinach). I will try calcium, low sodium and be more mindful of levels without depressing her further with a new ‘diet’ where she feels overwhelmed what she cannot have. thank you
Hi Genna,
IS your daughter having an allergic reaction to these foods? If so is she using any type of inhalers or other allergy medications. These sometimes can cause pain on urination as a side effect.
I have Kidney stones, I had them treated by lithotripsy 7 years ago. But they are back, i have one that is 10mm. I looked through my medical file and I can not find any urine test for oxalates. Can you tell me what the name of the test should be. And would it probably be the same here in Canada.
thank you
Hi Donald, The test name would be urine oxalate. I am not sure the measurements are at all the same in Canada as I have seen some results that are too low to believe. But that is what to look for. Regards, Fred Coe
Thank you. I am starting the test tomorrow. Appreciate the info
Dear Dr. Coe,
Thank you so much for your informative site. I am 63 y/o female who just passed my first ever stone – the analysis showed it was 85% oxalate. My urologist now informed me that I should go on a low oxalate (<50mg/day) diet. I'm a scientist myself, and after reading your site and the literature, I think your advice to increase dietary calcium and lower sodium, with moderate oxalate, is the way to go. How do I explain this decision to my urologist? Is there a position paper or review that I can give to him as evidence?
Thanks again. Your column is a beacon in a sea of confusion about dietary oxalate.
Anna
Hi Anna, The web article is linked out to the source papers that are on PubMed. For example, the data on effect of diet calcium on urine oxalate come from the main article on treatment of idiopathic calcium stone formers. The graph is shown there and the text has a link to the original data sets. Here is the link. The references are linked on the sheet. The combination of low sodium, high calcium and moderated oxalate is the Borghi trial that is in the article you are commenting on. It links back to the treatment article that has a link to the original trial paper. But even without that, the figure is from the trial paper and has the reference in it. So, the web article is referenced enough and the URL would be fine. Put another way, although this is a website it is referenced like a textbook or review. Regards, Fred Coe
Dear Dr. Coe:
I have diagnosed with hyperoxaluria and as to cause was told “No, the cause is unknown. You just have it. ”
*Is there a class of hyperoxaluria with no known cause?*
Age 61, stone history.
Diet restrictions did little; nor additional calcium; no symptoms of other disorders and now seen 2-3 metabolic experts, as well as regular urologist. No sign of genetic Primary Hyperaxaluria.
Since 2014, 24-hour urine UrOx:
162 | 160 | 668 * | 56 | 65 | 86 | 133** | 51 | 112 | 46
*668 is probable error
**133 is only one done with Litholink
All other urine/serum values normal, including Calcium and Citrate; uric acid controlled by Allopurinol.
Thanks for any thoughts.
Hi Jim, Given that your urine oxalate can be as low as 56 and 46, I wonder about diet calcium. Likewise about your diet. If you use extra food calcium to achieve 1200 mg daily, and be sure the high calcium foods come with the main meals, perhaps the urine oxalate will stay at the lower end of your range. Primary hyperoxaluria does not go as high as 160 AND fall to 46. I suspect food calcium was not synchronized to the main meals. If you do increase calcium as noted, urine calcium may well rise a lot, whereupon low sodium will reduce it again. As for HOX, no it never has no cause. You do not ever just have it. Try what I suggest and let me know. Regards, Fred Coe
Thank you.
Due for another 24 hour urine soon; will check back.
note:
–Calcium supplement began with 4th test (56) and is taken with meal ONLY when no dairy (usually plain yogurt) with meal. Calcium Citrate (20% element calcium) .
–Low sodium diet for many years (not perfect)
The 56 urine Ox was with calcium AND “low Oxalate diet” (impossible diet!)
Urine calcium never high; once low.
–Will check back. Thanks for your writings, very helpful.
Hi Jim, I am not sure I understand, but guess the urine oxalate was 56 even when you used high calcium diet of 1000 to 1200 mg daily eaten with main meals that had your oxalate in them; also a low oxalate diet. That does seem a bit unfortunate, and perhaps you have some reason for such a high persistent oxalate. I gather you are now adding calcium, but try to stay within 1200 mg daily as a total. Regards, Fred Coe
“high persistent oxalate” – yes, this is my understanding. Even with Calcium supplement and lot of yogurt. 56 was on low-oxalate diet (ie counting mg oxalate)
For completeness, here are urinary and serum calcium numbers for the 24-hour labs (since 2014)
Several doctors (in Portland, Ore) have reviewed, but can identify no cause:
162 | 160 | 668 * | 56 | 65 | 86 | 133** | 51 | 112 | 46 (urine oxalate)
169 | NA | 150 | 146 | 175 | 58 | 78 | 188 | 257 | NA (urine calcium, 24)
9.5 | NA | NA | 9.6 | 9.5 | 9.9 | 9.3 | 9.8 | 9.7 | NA (serum calcium)
Hi Jim, What catches my eye is the variability in urine calcium. I propose this as something you and your physicians can consider. Perhaps try a true 1200 mg calcium diet using real foods, seeing to the calcium with meals that might contain oxalate. Keep a diet diary for the days before and during the collection. Be attentive to urine creatinine so collections match. Since the lowest oxalate values 46, 51 are mundane, I deeply suspect diet calcium as too low or the calcium not matching the oxalate intake times. But I may be wrong, thus the suggestion. If you were nearer by we have had an open CRC project for years that could have settled this, but it is closing and you are distant. Let me know, and best regards, Fred Coe
I’ve been as Bangkok for treatment! Can you send me link to CRC project? I will review with my doctors. Know Hyde Park well (grad school) and eager to ‘settle’ this if possible. Have all diet records.
Thanks.
Hi Jim, I have forwarded your email to Elaine Worcester who is running the research protocol. She will no doubt be getting back to you. eworcest@bsd.uchicago.edu Best, Fred
I will forward this to her. I reviewed the whose correspondence and sent her a copy. Either way, with our protocol or not, a high calcium diet may benefit your situation. Obviously this would require a corresponding reduction of diet sodium. Have you discussed this possibility with your physicians?? Fred
I am looking for a recent update oxalate count list can you help me please
Hi Le Ann, Here is ours, and it is very good. Regards, Fred Coe
Chives and radishes are high in oxalic acid, but they are also highest in calcium among vegetables. Isn’t that a paradox and do we still need to avoid them?
Hi Thomas,
Sometimes the calcium is just not good enough to combat the extra oxalate. Like spinach. As far as chives, I would think the portion you use is not going to be big enough to make a difference in either category….but then maybe you are a chive-a-holic… my point is portion is key with most product.
Best,
Jill
Hi Thomas, Not a paradox if you think about the plants. They use oxalic acid as an energy store as it is essentially a two carbon fatty acid. Packing it in their tissues as calcium oxalate crystals can be very efficient. So we often see oxalate and calcium together. I do not know the oxalate bio availability of these two foods, perhaps no one has measured it. I would suggests getting your calcium elsewhere and not using these overly much. Regards, Fred Coe
According to testing preformed by Dr. Michael Liebman’s lab at U of Wyoming:
Red radishes contain only 1.7 mg ox/ 100 gm (published 2012 by VP Foundation) and chives contain only 7.2 mg/100gm (published 2014 VPF). Both of these foods are very low in oxalate. The problem with the low oxalate diet is that doctors, researchers, and dietitians are unconcerned about the inaccuracy and other short comings of their lists.
Hi Sally, We are indeed concerned. The lists here arose at Harvard and have been curated by Dr Ross Holmes, a world authority on food oxalate. We know Dr Liebman, and he knows Dr Holmes. Unfortunately Dr Liebman often fails to publish his results in open source journals, as his site and materials are held commercially, so we often do not have access to the data themselves or to peer review of them. I will write to Dr Holmes about you note and see what we can do. Regards, Fred Coe
Hello Again, Sally, I wrote to professor Holmes and he replied. Rather than select here is his entire text: “Hi Fred,
I appreciate the concern over these issues. Let’s look at Sally’s notes. Values for both chives and radishes are published in the “Low Oxalate Cookbook; Book Two” published by the VP Foundation in 2005. Chives are listed as 4 mg/100 g, red radishes as 1.7 and white radishes as 0. Both values attributed to Honow and Hesse in Food Chemistry, Vol 78 (2002) 511- 521. Most importantly, no one is going to eat 100 g. Thus, Both items contribute next to nothing and Sally should be reassured she has nothing to worry about with these items.
I am working on buying an Ion Chromatograph specifically for food analyses and to employ a summer student to do assays over the summer, firstly addressing the most discordant in published databases starting with those with the highest contents.
I would suggest recommending that if individuals want to determine their oxalate intake from tables to aim for 75 mg per day and ingest 1000 mg of calcium spread throughout the day. Don’t focus on foods with low amounts and eaten in small quantities and drink plenty of fluids.
Hoping to help resolve this some time soon,
Regards,
Ross.”
About oxalate we are clearly still in the midst of gathering more data. About radishes, I hope you are not more at ease. However, I do not think one has to restrict so much as to 75 mg/d of food oxalate if one really eats that much calcium – timed with meal oxalate. Regards, Fred Coe
Hi Doc,
Would a multi-vitamin with 250 mg. Calcium Carbonate/Dicalcium Phosphate be a problem? I’m now incorporating milk and kefir into my “post-stone” diet as well-
Many thanks,
Rob Lewis
Raleigh, NC
The vitamin is fine – use it with a meal so it can reduce oxalate absorption. But get evaluated as below. Fred
my level of oxalic acid from 24 hr test is 117. its been high for the last 4 years that i have been tested. i have many stones. i have changed my diet. i looking into vitamins herbs apple cider vinegar.
Hi Ed, That is high. The usual cause is low calcium diet or high intake or bowel disease. This needs fixing and your physicians need to do it. The level is too high for safety and the cause can always be found. Herbs and vinegars are not the best idea. Let me know, Regards, Fred Coe
Hi Dr. Coe,
Does one that has a uric acid stone (low urine ph) adhere to an alkaline diet as much as possible? with potassium citrate?, not seeing this on your site…
Thank you!
Hi Gail, Given the chemistry and the complete prevention from medicinal alkali I do not much favor changing diet. But I do favor it if obesity or insulin resistance or diabetes are causing the low pH. Regards, Fred Coe
I have had 3 kidney stones over the past 25 years, 2 before being Vegan and once since. I would like to continue my Vegan lifestyle but am not sure how. I love beans, potatoes, etc. I have eliminated spinach, beets and have switched to coconut milk from almond. I love tofu but see that’s not a good option. Really don’t know how to move forward or if it’s even feasible to continue eating a plant based diet. My cheeses are usually made with cashews. Can you help with meal suggestions as far as the calcium intake being Vegan and how to eat this way if possible. Thank you.
Hi Judi, I will ask Jill to answer this one. Regards, Fred Coe
Hi Judi,
You need detailed help. Perhaps think about contacting me on my website to set up a personal consultation.
Best,
Jill
I so appreciate the information you’ve gathered here, and I especially appreciate the art and how that relates to the medical advice. My girlfriend and I have been searching the net for guidance on kidney health, and yours is the best one we’ve found so far. Thank you so much!
Thank you, Claire; I am happy the site is useful to you both. Regards, Fred Coe
Where can I get a more thorough analysis of my stones? Here in Canada, labs only report if the stones contain oxalate etc., they do not report the percentage.
Hi Jason, Offering percentages is a debated topic. Usually IR spectra are used to analyse stones, and they do give percentages but rather approximate. My concern is when calcium phosphate is predominant, even when it is above 20% or more, because it suggests plugging of kidney tubules and makes prevention more urgent. Perhaps if asked the lab can give you more information. Within Canada I do not know which lab does what, unfortunately. You could send stones to the US and pay yourself; it is not very expensive. Regards, Fred Coe
My lab results here in Canada only stated that my stones are mixed calcium oxalate and phosphate, but what does this really mean? Which is more predominate or does it really matter?
Hi Jason, THe other fraction may be calcium phosphate. I cannot tell. But whatever it is, prevention requires more than the stone analysis. Here is a reasonable starting place. Regards, Fred Coe
Do you know if drinking apple cinder vinegar provides any benefits for kidney stones? Also thank you for the information on this site it’s very helpful
Hi Alandra, I know of some interest in it but no data. I cannot recommend it. Regards, Fred Coe
I have been told that potassium citrate, magnesium, and b6 taken together helps break up stones and also lowers the acidity in urine. My urine tests always shows high acidity no matter how much I drink. And so far have had two Uric stones. Have you heard of this helping. This site is the best and helped my husband with his calcium oxalate stones. Thank you for all your time and effort helping people. Your a blessing.
Hi Gail, Since you have uric acid stones and low urine pH potassium citrate is indeed your only real treatment. Here are articles on uric acid stones, one fancy and one simple. Magnesium has no relevance at all. Get on treatment and uric acid stones must stop. Regards, Fred Coe
I formed my first stone after cutting out dairy from my diet because it makes me constipated. I have tried to re-introduce it with no success. I’m thinking of taking calcium citrate with my meals. thoughts? Thanks!
Hi Jennifer, High calcium is part of a good diet for stone prevention. Here is the entire diet, as just more calcium by itself may not be ideal. Regards, Fred Coe
Dear Dr.Coe,
Thank you for this great information. While I am not a kidney stone former, I have Polycystic Kidney Disease with normal renal function. It is my guess, that there won’t be human studies most likely, in my lifetime, that will produce a diet that may help people like me. There are very promising lab results in animal studies that you may be familiar with. So far, learning about a lower oxalate diet your information seems the most helpful.
Hi Diane, There is something important to do about APCKD: Very high fluid intake to suppress the hormone vasopressin, which has been improved using a recently approved drug. I would suggest you try to find physicians near you with a special interest in this condition. Oxalate seems of little importance, so far as I know. Regards, Fred Coe
I’ve read contradictory info on the oxalates in both broccoli and blueberries. My nephrologist said yes to broccoli and no to blueberries. Your list says raspberries are far worse than blueberries. I eat broccoli every night. Thank you.
Hi Nikki,
I’ve read much the same. On this website https://www.arizonadigestivehealth.com/low-oxalate-diet/ it says that Zucchini, blueberries, brocolli, brussel sprouts and oatmeal are all very high whereas Jill Harris’ book says they’re all very low. What’s going on. Help, I dont know what to eat i’m going crazy.
It seems like you’re missing the point of the article. Namely, oxalate is NOT nearly as important as low sodium and correct calcium. Stop worrying about oxalate, unless you’re still having stones after getting your sodium and calcium (and 2.5+ liters of liquids) correct.
Oxalates diet info is very confused. Raspberries have lots of oxalate in the seeds, but few people chew the seeds so it is irrelevant.
Hi Robin,
Yes, it is all confusing. Watch this from my YouTube channel and you will be clear. https://www.youtube.com/watch?v=RfMnRhiiKx4&t=92s
Jill
kidneystonediet.com
One thing that confuses me is that those who advocate high calcium from dairy and also advocate low-protein never address the fact that increasing dairy also means increasing protein, which in turn increases urine oxalate. Also, as an alternative to dairy, I started taking a modest amount of plant-based (marine algae) calcium with oxalate- rich meals and my calcium level on a 24 hr test shot WAY up, presumably increasing my risk. No binding with oxalate in the gut the way it’s supposed to??
Hi Joe, milk protein is rather a good actor in that oxalate does not seem to rise with it. Partly, the protein composition is not like meat and fish. Partly there is a lot of calcium per the amount of protein. As for algae, I do not know the form of the calcium. Perhaps it is as the carbonate which would be rapidly absorbed whereas milk calcium is absorbed more slowly because milk contains a lot of both protein and fat but also phosphate. Regards, Fred Coe
I read that the oxalate comes specifically from glycine rather than protein in general, and then only if B6 is deficient. So agreeing with Dr Coe here.
Dear Dr. Coe,
Would you please tell me if these two ingredients are high oxalate:
1. soy lecithin
2. cocoa butter
Thank you very much.