Diagnosis of MSK is Increasing
Urologists and nephrologists specializing in the treatment of kidney stones seem to encounter patients with medullary sponge kidney (MSK) far more often than one would predict given the fact that this disease affects less than 0.5-1% of the general population.
One potential explanation is the high frequency of stones in such patients, nearly 70%. Stones call attention to themselves. Even so, referrals for MSK seem to be occurring at ever increasing rates, out of proportion to the prevalence of the disease.
Another explanation is that we can see more because of dramatic improvements in CT scanners and endoscopic equipment we use for stone removal.
Latest generation, thin slice CT scans can isolate tiny stones as small as a millimeter in size. Meanwhile, modern flexible endoscopes not only visualize every crevice of the renal collecting system but are able to do so in high definition. Consequently we can identify previously unrecognized variations in the appearance of stone forming kidneys, of particular interest here nephrocalcinosis on CT and tubular plugging on endoscopy.
But diagnostic capabilities may be progressing faster than our ability to comprehend the significance of what we see. As a result, one can misclassify patients as having MSK when the correct diagnosis is another more common finding such as nephrocalcinosis or tubule plugging.
For example, a urological surgeon performing ureteroscopy with a modern high resolution digital instrument notices “hundreds of tiny stones,”, “abnormal papillary architecture” or “stones located under the urothelium” and proceeds to label the patient with MSK. Or, a patient with urologic symptoms such as renal colic, recurrent urinary tract infections, or microhematuria has a CT scan showing ‘nephrocalcinosis’ and is labeled as having MSK.
In both instances, the true likelihood of actually having MSK is, by a recent small study, only 4/15 (25%), but physicians are not generally aware of the differences between MSK, nephrocalcinosis, and tubule plugging because these are new areas of knowledge which have not been proliferated widely.
This article is one way we hope to make the diagnosis of MSK, a unique and complex disorder of renal development, clearer for physicians and their patients.
What Is MSK?
Our collective understanding regarding the development and pathophysiology of MSK is rather sparse even though G. Lenarduzzi first described it in 1939.
The Cause of MSK
The exact mechanisms that produce MSK are unknown. It is believed to be a result of abnormal renal development in utero. More specifically, scientists believe the ureteric bud – which will give rise to the ureters – interacts abnormally with the metanephric blastema tissue in the embryo which will produce much of the kidney substance.
There appears to be a genetic component to the disease. Recent evidence is that about half of patients diagnosed with MSK will have at least one relative with some degree of similar affliction. This kind of familial clustering can suggest an autosomal dominant gene expression or the actions of multiple genes giving that impression. The review of the above link is an excellent recent treatment of the matter of development and genetics which we highly recommend.
The Anatomy of MSK
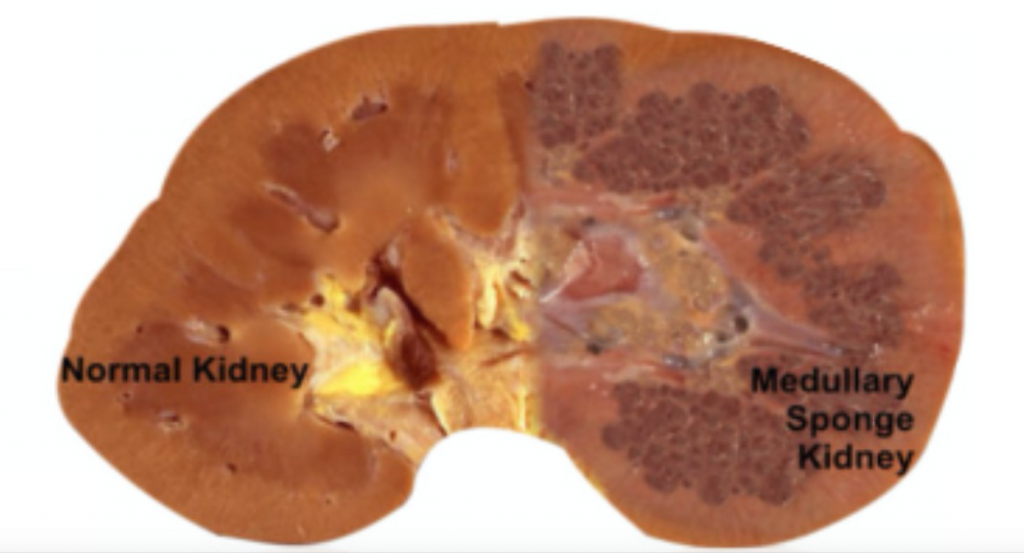
MSK, as its name implies, is characterized by sponge like, cavitary regions within one or both kidneys (Figure 1).
Figure 1 – A normal appearing kidney (left) compared to MSK kidney (right).
More specifically, the dilations occur in the inner medullary (precalyceal) collecting ducts. These collecting ducts are the terminal region of the nephrons, the individual functional units of the kidney.The inner medullary collecting ducts (IMCD) have the job of delivering urine to progressively larger ducts (ducts of Bellini) that deliver the final urine out of the renal papilla into the minor calyces (Figure 2) which connect into the renal pelvis and thence into the ureter to the bladder.
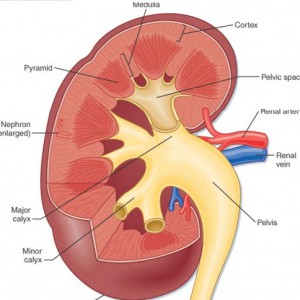
One way to think of the IMCD is as a collection of streams merging and forming a river (duct of Bellini) which leads to a delta (minor calyx) and then a lake (major calyx) and ultimately an ocean (renal pelvis) (Figure 2).
Figure 2 – Anatomic depiction of kidney and collecting system
The IMCDs are not visualized in Figure 2 but if you scan down to Figure 3 just below several human nephrons which were microdissected from an MSK kidney show what is really wrong with them.
In MSK, some IMCD are dilated markedly and have outpouchings (cysts): blind sacs which begin at the IMCD lumen but go nowhere – like a hallway someone walled off at one end. It is at the ends of these hallways one finds the stones, free floating and probably trouble. Other IMCD are not dilated and do not have cystic outpouchings.
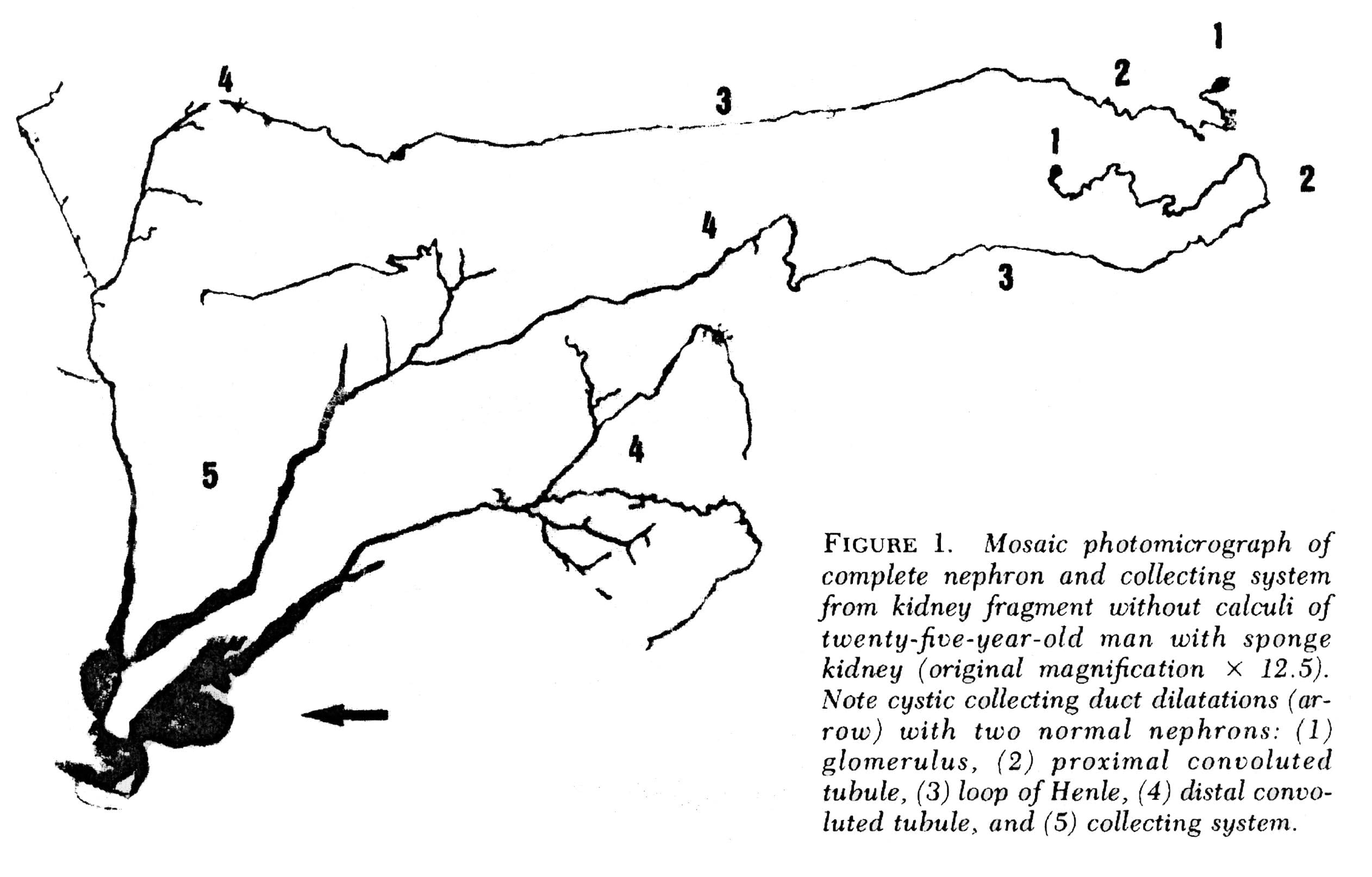 Figure 3 – Microdissection of complete nephrons from MSK. Irregular dilation of the IMCD is present. Cystic outpouchings are present, of varying sizes. The blind ends are obvious. It is in these cysts that tiny stones are found.
Figure 3 – Microdissection of complete nephrons from MSK. Irregular dilation of the IMCD is present. Cystic outpouchings are present, of varying sizes. The blind ends are obvious. It is in these cysts that tiny stones are found.
Quite apart from the IMCD dilatation and cysts, the kidneys of MSK have two other abnormalities which mark it as a specific disease. Those IMCD which are not dilated nor cystic have a multilayered epithelial lining, whereas a normal undilated IMCD lining is one cell layer thick. The interstitial cells of the renal papillum – the cells between the tubules and vessels – are more numerous than in normal kidneys, and have an immature appearance much like is seen in fetal kidneys.
Why Stones Form in MSK
Elsewhere on this site we have pointed out that supersaturation is a force, a source of energy directed at forming solid phases such as stone crystals. The kinetic retardants in urine, which include citrate, stave off crystallization but can never prevent it: A supersaturated solution will eventually collapse into two phases, crystals and a residual solution precisely at the solubility point, devoid of extra free energy.
The stagnant flow as a result of the dilated MSK IMCD, and particularly the static conditions in the fluid filled blind ended cysts, are the probable reason those innumerable tiny stones form which end up packing the ‘sponges’ with masses of crystals. How MSK patients produce larger stones, big enough to block the ureter is unknown. It is not true that MSK patients have remarkably high urine supersaturations or other physiologic abnormalities such as hypercalciuria and hypocitraturia. Possibly the tiny stones somehow leave their cysts and enter the urine where they act as nucleation centers.
Other Associations
Other common associations with MSK include urinary tract infection, microscopic and gross hematuria, and impaired renal function. Perhaps the stagnant flow in dilated IMCD and particularly in cysts, predisposes to infection. But since the papillae are abnormal in other ways it seems likely that these intrinsic abnormalities themselves must be clinically important, and more work needs to be done on the problem.
Making the Diagnosis of MSK
Of course, when we speak of what is wrong in the MSK kidneys, and how it affects people, we base everything on knowing that a given patient has MSK. If you have a kidney from such a patient and can show the dilated IMCD, the cysts, the tri-layered IMCD epithelium, and abnormal interstitial cells, diagnosis is certain. But what can we do when we are dealing with a patient?
Radiological Studies
Intravenous Urography
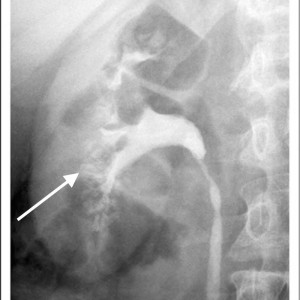
Historically, the diagnosis of MSK has been made on intravenous urography (IVU). Radiographic contrast is administered and x-rays of the kidneys, ureter, and bladder are taken periodically as the contrast is absorbed and later excreted by the kidneys through the urinary tract.
The delayed phase image is essential for diagnosis. This is when contrast material fills the masses of dilated IMCD and cysts which make up the sponge.
The masses of dilated IMCD filled with contrast material produce a characteristic ‘papillary blush’ which appears like flames on the outer edges of the papillae. When particularly large it can mimic a bouquet of flowers peripheral to the collecting system.
Figure 4 – IVU image of medullary sponge kidney. The arrow designates the papillary blush in the mass of dilated IMCD space.
CT Scans and Other Imaging
Over the past 10-15 years, noncontrast CT scans have replaced IVU as the imaging method of choice for stone formers. While these scans are more sensitive in detecting small stones, the lack of contrast limits the ability to accurately diagnose MSK and has raised concerns regarding the potential for under-diagnosis of this disease.
CT does have the capability of making this diagnosis when contrast is given and CT urography is performed; though this is not used as a first line choice for stone imaging and is generally reserved for specific indications such as hematuria and concern for urinary tract injuries.
Figure 5 – Demonstration of papillary blush (small arrows) on CT urography for patient with medullary sponge kidney.
Use of other imaging modalities have been investigated as well though they have proven suboptimal in their diagnostic capabilities. Ultrasound has poor sensitivity to detect dilation of the collecting ducts and MRI has the potential to delineate detailed renal anatomy but can not detect stones or calcification.
High Definition Endoscopy
State of the art high definition endoscopes have allowed investigators to make observations at the time of renal endoscopy correlating the appearance of the renal papillae and collecting system to specific types of diseases and metabolic derangements associated with stone formation. Because endoscopy is now being performed as a common and often preferred way to manage stones, this kind of detailed imaging of kidneys will be available more and more in the course of regular patient care and permit physicians to diagnose the exact kinds of disorders in the kidneys of stone formers.
Medullary sponge kidney in particular has an entirely unique appearance unlike any other type of stone related disease, making endoscopy a particularly exacting diagnostic procedure. Detailed anatomic descriptions from twelve such patients each with evidence of MSK on biopsy were recently described by Evan et al.
The Papillary Malformations Seen Via Endoscopy
In stone formers the papillae often appear abnormal, a concept that merits its own post and which we can only briefly summarize here.
Plaque
The renal 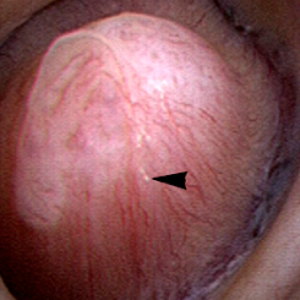 papilla is the anatomic subunit of the kidney where the IMCD merge together into the terminal Bellini ducts which empty into the minor calyx. Normally, it should have the appearance of a smooth walled mound or mountain without much if any calcification (plaque) along its surface. The link is to a detailed post about plaque by Dr Andrew Evan.
papilla is the anatomic subunit of the kidney where the IMCD merge together into the terminal Bellini ducts which empty into the minor calyx. Normally, it should have the appearance of a smooth walled mound or mountain without much if any calcification (plaque) along its surface. The link is to a detailed post about plaque by Dr Andrew Evan.
Figure 6 – Healthy appearing renal papilla with a minimal amount of Randall’s plaque (arrowhead).
Ductal Plugging
Another common abnormality identified in many papillae at the time of endoscopy are plugged ducts. The physiologic mechanisms for this process are currently unclear; 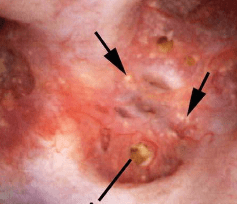 however, we believe it is a reflection of injury that begins a potentially disastrous chain of events for stone formers.
however, we believe it is a reflection of injury that begins a potentially disastrous chain of events for stone formers.
Figure 7 – Abnormal papilla in a patient with severe ductal plugging. Yellow mineral deposits (arrows) can be seen protruding from dilated ducts of Bellini.
Our present assumptions are that once crystals begin to form within a duct, they damage the lining cells and the duct loses its ability to make acidic urine. This in turn raises the local pH level and leads to the growth of more calcium phosphate mineral deposits which are favored by high pH.
Unclear is what begins this process. Since these ducts contain fluid which is very close in composition to the final urine, we suspect it is high supersaturation with respect to calcium phosphate. This occurs in those patients with both high urine calcium excretions (hypercalciuria) and higher urine pH levels – above 6.2. Such patients often form stones high in calcium phosphate composition and plugging is strongly associated with formation of such stones.
The mineral deposits subsequently grow and we believe can even act as a nidus for stone formation. The corresponding papillae can look markedly abnormal and the dilated ducts are easily evident. Remnant dilated ducts left behind after the mineral is spit out or surgically removed (Figure 8) show dilation without the mineral plug.
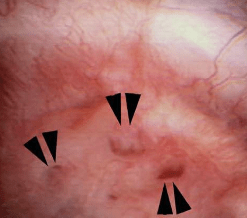 Figure 8 – Evidence of abnormally dilated ducts (arrowheads) at the surface of a papilla.
Figure 8 – Evidence of abnormally dilated ducts (arrowheads) at the surface of a papilla.
MSK
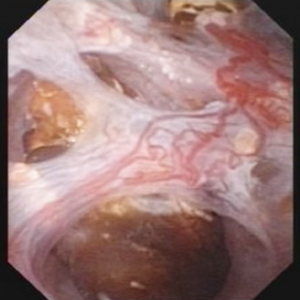
The findings in MSK are comparable in some ways to ductal plugging; however, rather than the papillae having one or several abnormally dilated ducts, the entirety of the papillum is markedly abnormal.
Therefore MSK and plugging type papillae look remarkably different.
The MSK papillae are excessively round, enlarged, and billowy (Figure 9).
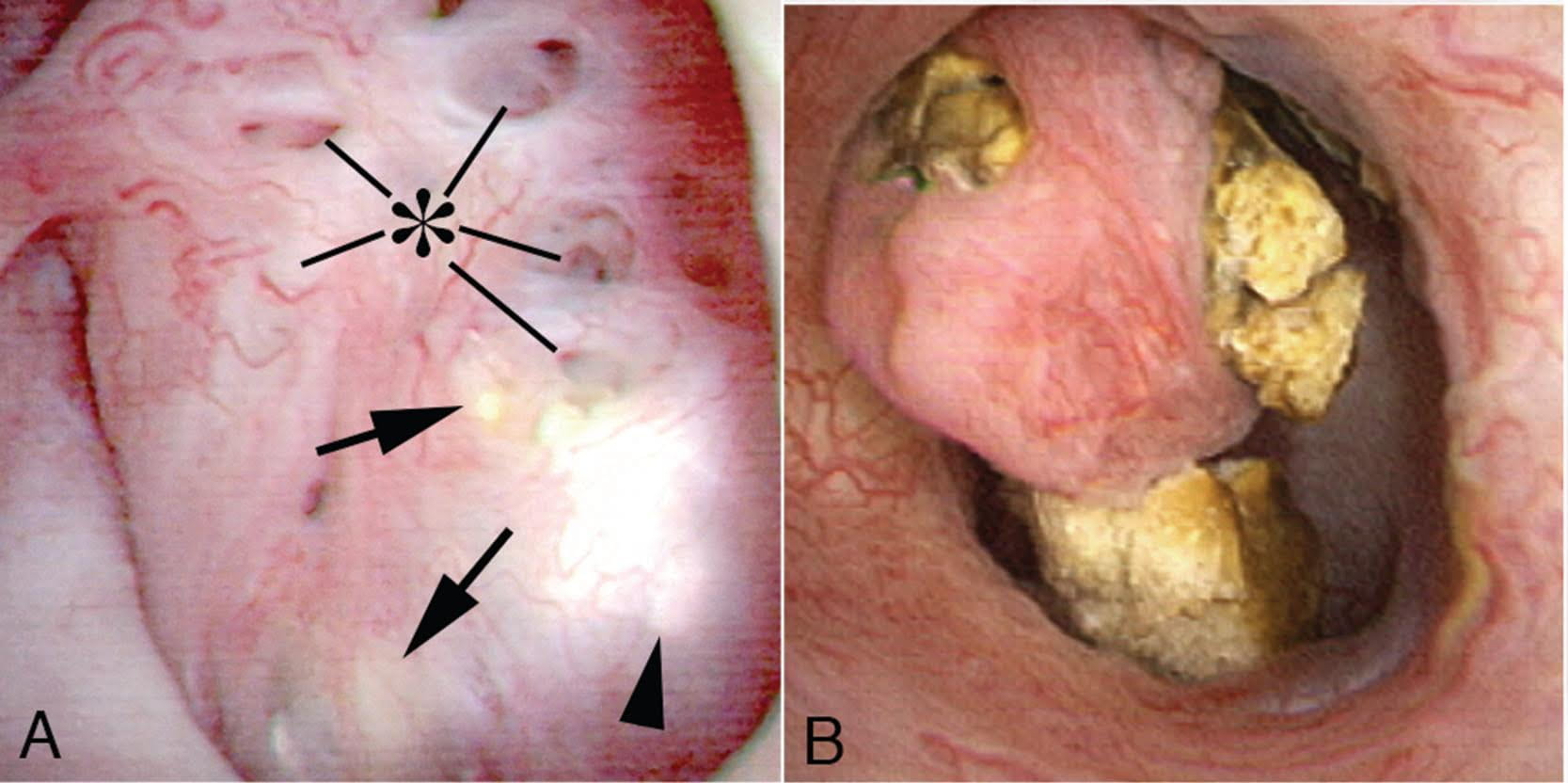 Figure 9 – A papillum in a patient with medullary sponge kidney. The papillae are rounded and enlarged with a billowy appearance. The papillary tips are blunted. No other kind of papillary disease is known to present this appearance which is therefore pathognomonic of MSK. Panel a shows dilated Bellini duct openings at asterisk; the arrows show yellow plaque – plugging of IMCD completely separate from the stones which fill dilated IMCD, the arrowheads show traces of white plaque. Panel b shows the billowy papillum with a blunted tip surrounded by calyceal stones.
Figure 9 – A papillum in a patient with medullary sponge kidney. The papillae are rounded and enlarged with a billowy appearance. The papillary tips are blunted. No other kind of papillary disease is known to present this appearance which is therefore pathognomonic of MSK. Panel a shows dilated Bellini duct openings at asterisk; the arrows show yellow plaque – plugging of IMCD completely separate from the stones which fill dilated IMCD, the arrowheads show traces of white plaque. Panel b shows the billowy papillum with a blunted tip surrounded by calyceal stones.
In the majority of such cases, these changes are seen diffusely throughout each kidney, though segmental sponge findings are present in a minority of patients.
The differences in appearance are well demonstrated in the post by Dr. Evan and the following video. With ductal plugging the bulk architecture of the papilla is intact though many ductal plugs are seen. Note the way the ductal plugs are adherent to the lumen.
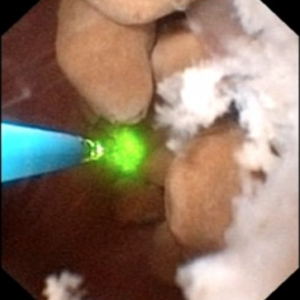
In MSK on the other hand, the papillary architecture has and unique, billowy appearance with massively dilated ducts and freely mobile stones within them. The following video is from a patient with MSK. A duct of Bellini is massively dilated and numerous tiny stones which are free floating pass out of it during the visualization as the opening is enlarged with a laser. You can see stones bouncing within the duct because of movement of the irrigation fluid.
Clearly neither papillum is “normal” and one can imagine the tendency to misdiagnose a plugging patient as a MSK patient unless the two patterns are clearly in one’s mind.
The ductal deposits themselves are an important clue. In all plugging diseases but cystinuria ductal mineral plugs are fixed within the ducts because the crystals adhere to the lining cells and often destroy them. As the lining cells are destroyed crystals fix themselves to the basement membranes, the collagen shell on which the lining cells once grew. Inflammation follows such injury with scarring and loss of the tubule segments. Deposits therefore never float free from a dilated duct except in cystinuria and in MSK. Cystinuria is usually diagnosed directly from stone analysis and urine cystine screening.
Perhaps because the tiny stones in MSK do not attach to the epithelium of IMCD there is no evidence of cell injury or inflammation, in marked contrast to all of the plugging diseases. Even in cystinuria injury occurs, not from the free floating distal cystine plugs but from calcium phosphate plugs which form in the IMCD.
Stones may cause pain in MSK despite the lack of ureteral obstruction and inflammation and cell injury. Possibly distention of the dilated ducts by masses of tiny stones could be a factor. Consequently, laser unroofing has been postulated as a potential treatment option in both disease states: those with plugging and MSK.
The video may not make it easy for everyone to visualize the stones and cavities of MSK. The 4 still pictures below show much the same thing for clarity.
Figure 10 (a-d) – Example of laser unroofing of sponge cavity full of freely floating stones. The massively dilated MSK bellini ducts are seen in Panel a; the white speckles at 9 o’clock are tiny stones in dilated IMCD or cysts. Panel b shows a holmium laser fiber being used to open dilated IMCD or cysts. Panel c shows masses of tiny stones free in dilated IMCD or cysts which float out as the surface is incised with the laser. In panel d, the remnant sponge cavity can be seen now free of stones.
Nephrocalcinosis and MSK
Strictly speaking, nephrocalcinosis refers to the presence of calcium deposits in the kidney tissue. Of course, this includes ductal plugging and the masses of tiny micro – stones inside cavities produced by numerous dilated IMCD in MSK. However, the word ‘nephrocalcinosis’ is also used as a radiological diagnosis which is far less specific.
Limitations of Radiology
When radiologists speak of nephrocalcinosis they can mean large numbers of calcifications within the collecting system or kidney tissue, because they cannot differentiate reliably between tissue calcifications and stones. When urologists speak of nephrocalcinosis seen during high resolution endoscopy they can specify if it refers to tissue calcifications, stones, or both, and will reserve the term for that component arising from tissue calcifications.
MSK is one of several disease states that is commonly associated with extensive nephrocalcinosis observed by radiologists. Other common conditions are stones caused by renal tubular acidosis and primary hyperparathyroidism. Calcium phosphate stone formers without any systemic disease can also produce sufficient combinations of ductal plugging and stones that nephrocalcinosis is diagnosed radiologically.
In a recent study of 67 idiopathic calcium stone forming patients undergoing percutaneous nephrolithotomy, rates of nephrocalcinosis ranged from 18-71% depending on the type of associated stone.
Figure 11- X-ray example of patient with MSK affecting the left kidney. Extensive nephrocalcinosis is seen.
Because radiographs cannot reliably distinguish tissue calcifications from stones adjacent to tissues, the very word ‘nephrocalcinosis’ needs to be re-defined.
In particular, the situation with respect to diagnosis of MSK has worsened as radiological techniques have changes. When IVU was the first line imaging modality for stones, contrast enhanced urographic phase imaging gave additional clues to MSK – the papillary blush illustrated in a prior section.
Nowadays since a single non-contrast CT series is all that is typically performed, the papillary blush effect cannot be seen, and diagnosis of MSK must rely more on the presence and pattern of nephrocalcinosis itself, which is not very specific to MSK. This means that the diagnosis of MSK by radiology has become unreliable.
The Power of Endoscopy
Differentiation of Nephrocalcinosis from Stones
During endoscopic procedures, stones and tissue calcifications can be directly identified and told apart. For example, in the images below, some of the calcifications were identified as stones. Others were tissue calcium deposits such as plugging or extensive plaque.
This has led to the notion that kidneys should only be labeled as having nephrocalcinosis once confirmed visually on endoscopy.

Figure 12 (A-C) – Evidence of increasing degrees of nephrocalcinosis confirmed visually at the time of percutaneous nephrolithotomy. In each image a nephrostomy tube (not calcification) is depicted by an arrow. The remainder of the images have increasing degrees of calcification (bright white) within the kidney. Ignoring the nephrostomy tube, one can clearly appreciate a minimal but very present degree of accessory brightness (calcification) in panel A, a moderate amount in panel B and a severe amount in panel C.
Diagnosis of MSK
Of course, all of the problems of nephrocalcinosis are compounded when it comes to MSK. Stones and tissue mineral are easily mistaken for one another in CT scans, and ‘MSK’ affixed as a label to patients who do not have it. Endoscopy will easily identify the remarkably abnormal papillary shapes and dilated sponges, so MSK patients are properly diagnosed.
Tips for diagnosing MSK
1) Confirmation with flexible renal endoscopy can make a definitive diagnosis in patients suspected to have MSK and can be diagnostic as well as potentially therapeutic in terms of stone removal.
2) Consider urographic phase imaging either with IVU or CTU to confirm MSK suspicion in cases where renal endoscopy is not clinically indicated.
3) MSK should not be confused with ductal plugging as these are distinct clinical entities.
4) Nephrocalcinosis is more common than previously appreciated and does not necessarily indicate systemic disease or the specific developmental disorder of MSK.
A Final Word on Treatment
MSK is a true disease and deserves more attention and research efforts to help clarify its etiology and optimize treatment strategies. Because diagnosis by CT scanning is unreliable, the condition is easily overdiagnosed, a problem which leads to many kinds of confusion, clinical and research.
Alternative diagnoses to MSK, such as severe ductal plugging, are not benign and require their own treatment in order to prevent progression. Very often patients with plugging have multiple and severe abnormalities of urine chemistry which can be treated with diet and medications. Proper classification of patients is therefore especially important as different disease states may require unique treatment strategies.
In the event that an accurate MSK diagnosis is made, the tendency to give up on treatment and surrender to the inherent challenges of the disease should be avoided. In fact, these are the patients where metabolic evaluations and attempts at stone prevention are most critical.
Moreover, just because many of these patients tend to have extensive nephrocalcinosis on imaging does not mean they can’t form symptomatic stones in the collecting system as well. In fact, for such patients the clinical history is especially important as visualizing new stones in the setting of extensive nephrocalcinosis can be quite challenging.
Oftentimes when there is a high index of suspicion based on clinical factors, the optimal approach is ureteroscopy as this can be both diagnostic and therapeutic.
That being said, realistic surgical goals should be established. Clearing all stones from such kidneys is rarely feasible, though unroofing those pockets closest to the collecting system or largest on CT imaging offers a good place to start.
MSK is a complex and poorly understood disease that can manifest uniquely from patient to patient. In that respect what works for one person may not be appropriate for another and treatment strategies should thus be organized on a patient to patient basis.







Can you please comment on whether or not for patients with MSK and normal Cr, there is an increased risk from NSAID use compared to those with the same Cr but without MSK.
Hi Dr Gorbatkin, I know of no increased risk in MSK concerning kidney damage from NSAID. Regards, Fred
Thank you for your research. I’m 35 and was disgnosed with MSK (finally) three years ago after dealing with recurrent stones since the age of 22. I have the “lesser” of the two evils with MSK, according to my nephrologist. I don’t deal with infections, and I rarely have blockages. But at any given time I have 10-20 stones/calcifications in each kidney, mostly “in the meat”, as I’ve been told. My biggest problem over the years has been receiving treatment for the pain. At best, my pain is a constant chronic low level flank ache, like a toothache in my back. At worst, it’s the stabbing sharp pain that kidney stone passers experience, and has landed me in the ER. I can’t tell you the number of times I’ve been treated like a drug seeker in the ER. Doctors treat first, then do CTs. When the CT comes back and shows multiple stones in each kidney, I’m always told that I shouldn’t be in ANY pain, as none are blocking. I’m part of a forum of fellow MSK’ers, and we all share the same experiences in ERs, being labeled as drug seekers, and not having our pain acknowledged. Do you have any theories on how pain manufactures without blockages? My go to is telling the ER doctor “How can you think that carrying around 20 stones in an organ would NOT cause some kind of pain?”, but I’m still often rebuffed. Just curious as to your thoughts. Thanks!
Hi Sarah, Given the description I presume your urologist saw calcium deposits in your kidney tissues; often these are not MSK but calcium phosphate plugs in collecting ducts. I wonder if your stones are indeed calcium phosphate or calcium oxalate. MSK if painful could be treated, by some urologists, via unroofing during ureteroscopy to let out the myriads of small stones. If you have plugging the key is prevention of new tiny stones and crystals that can cause pain and escape notice. If you have more information, please post it and I will try to suggest directions for you and your physicians. Regards, Fred Coe
Why can’t we cure this?? I have a friend who has suffered tremendously for years and years-its not fair.
Hi Carole, MSK is a developmental anomaly so it is not easy to cure. Surgeons are beginning to treat it, but alas no trials. The most important steps we can take are prevention of more stones. Also, MSK is over diagnosed, so be sure your friend really has it and not some other easier to treat condition. Regards, Fred Coe
OH MY GOD YOU SOUND LIKE ME!!! Does anyone have any idea how amazing it is to find this article?! Its like the heavens have opened!!
Please someone help me understand this asap! I’m going in for my 10th lithotripsey in 3 weeks and I’m only 35.
can u have msk, if u only have severe infections, 200+ in 20 yrs, but no kidney stones??
Hi Erin, yes you can. Unfortunately. Regards, Fred Coe
I am new to the diagnosis of MSK and nephrocalcinosis. I’ve only had one UTI and as far as I know, I’ve never passed a stone. However, over the past 4-5 months, renal colic has increased. The nephrologist I see is very quick to say that he doesn’t know much about the disease outside of the textbook. Is there a specialist that is very knowledgeable about this? We are willing to travel and see someone and get a good game plan for treatment. Right now everything is just trial and error as far as diet and medications are concerned. With my urine calcium being high and the renal colic increasing, I’m ready to know exactly what the best plan is. Thank you for all of your detailed information! This is a great read.
Hi Ashley, Let me know where you live and I will try to suggest a suitable center where things can be clarified for you. As an aside, most nephrocalcinosis is not MSK, and most MSK do not have very high urine calcium levels, so that is part of what needs clarification. Regards, Fred Coe
My friend is diagnosed with “Nephrocalcinosis, medullary calcification of kidney, and medullary sponge kidney”. She lives I. Pain for 5 years in & out of the hospital & ER. Any suggestions or help you can advise
Thank you
Hi Jude, small stone pain – I think that is what you are describing is a real problem and opinions about treatment all over the place. My best advice is she seek an opinion from a kidney stone center at a university. There is so much detail one cannot say much from a distance like mine, and physicians who are busy in a wide range of practice cannot usually take the time or hone the skills when the disease gets as bad as you describe. I hope this is possible. Regards, Fred Coe
My friend has “Nephrocalcinosis, medullary calcification of kidney, and medullary sponge kidney”. She lives in pain for the past five 5 years. She is in & out of the ER or hospital. She lives on pain pills. She is 0nly 35. Do you have any suggestions where she can go for help. She has been to Mayo in MN and no help. She lives in MO.
Hi Jude, OOPS, I missed this second note. Mayo is very fine. I looked on a map and she is no further than Mayo to me in Chicago, or even better Dr Jim Lingeman at Indiana University, in Indianapolis. The latter looks closer, actually. Both are university programs, and will do. Let me know, or just see if she can go to Indy. Regards, Fred Coe
I was diagnosed with MSK at age 19 via an IVP. I had a few sporadic stones and UTIs since but I am now 45 and am currently suffering my fifth bout of kidney stones (three stones currently) with hydronephrosis & hydroureter just this year. My uroligist is blaming my MSK but is offering little help beyond giving me flomax & pain meds when I get them. Im curious why this has started all of a sudden and in constant pain in my left kidney. Im near Cleveland-any suggestions on a stone clinic or specialist?
Hi Kim, Dr Manoj Monga at Cleveland Clinic is world famous for stone surgery and knows a lot about prevention. I would suggest you might want to consult with him about prevention and also about any other surgical needs. I know him, and he is an excellent physician. Let me know, Regards, Fred Coe
In search of urologist/nephrologist in Kansas City area that understands MSK can be painful. Looking for preventive treatment to avoid more stones and pain management.
Hi Jane, The University of Iowa seems closest. A close friend who is now emeritus would know who is good at kidney stone prevention. Her name is Dr Vicci Lim victoria-lim@uiowa.edu. Email her and see what she can do for you. Regards, Fred Coe
Hi! I have been in & out of the hospital so often that my husband jokes that he has his own coffee cup that he keeps there! I was diagnosed years ago by the radiologist with MSK. My Urologist seemed like she did not know that that was a real thing! So, could you please recommend someone in the Detroit, Michigan area? Preferably Novi, Michigan.
Also my father has been a long time sufferer of Kidney Stones. He is in Ft Myers, FL. Could you please recommend someone for him?
Thank you so much in advance!
Hi Kelly, You are close to university of michigan in Ann Arbor. Here is their kidney stone clinic notice. I do not know who runs it but the place is excellent. As for florida I am afraid I have no immediate answers. Sorry. Regards, Fred Coe
Hi Dr. Coe,
First, my apologies if this comment posted twice (or more)…
Thank you so much for this website! I have learned so much from it, and feel like I’m gaining more control over my stones now from reading it.
I won’t go into a long personal history, but MSK was mentioned to me by my nephrologist after bloodwork and Litholink 24hr urine results came back with good levels, no red flags. He said that the treatment for stones and MSK is basically the same: increased water intake, lower sodium/higher calcium diet, possibly lower oxalate intake. And because of that, he didn’t seem too concerned about finding out if MSK was a possibility for me because he would prescribe the same “treatment” (my citrate levels are also good). I didn’t think too much about it while we were talking, but have since been reading about MSK.
So, my question is, do you think there is anything to gain on my end by having any testing done? If it was a disease that could be fixed with prescriptions or surgery, absolutely I’d do it. But if it’s going to be managed more by diet and fluid intake and monitoring for new stones, I’m wondering if it’s worth knowing if I have MSK or not. Also, I am adopted and have no way to find out if this runs in either of my families.
Thank you again for your amazing work!
Amy
Hi Amy, I removed your duplicates and saved the last of the three. MSK is diagnosed during ureteroscopy or by CT scan with infused contrast agents. Usually multiple calcifications are present without contrast. Stones are usually calcium oxalate. If you have MSK or not treatment is indeed the same except surgery is more complex should you need it. But ‘normal’ Litholink results mean nothing as the normals used were lab normals where stone risk arises from considerably lesser deviations of urine chemistry. Here is a good review of all this. So, no; no reason to pursue MSK as a diagnosis. Regards, Fred Coe
Hello, excited I ran across this article. I have MSK. I have had 14 lithotripsies in the past 6 years. Also a couple basket retrivals. My last litho was in Feb. Six months later several stones on each side. I am 38, busy working mom of three active kids. Surgeries every 3-6 months and then stents are not working. The cost of these is debilitating as well. I am on pottasium citrate and amiloride. Any suggestions? I live in mid Missouri. I told my husband I want to go to Mayo or anywhere that can help me. Thank you!
Hi Meghan, You may not have MSK – it is an overused diagnosis. You need a proper evaluation and prevention program. Here is my basic approach. If you can travel, we can see you at university of chicago. I avoid mentioning this as the site is not intended to attract patients, but I and my colleagues regularly see patients for prevention of new stones. If you would like to come, my secretary is Kathleen Dineen – 773 702 1475. Likewise you can email. Regards, Fred Coe
Hello,
I am worried that my latest nephrologist is jumping to an MSK diagnosis without proper testing. (The first was a “you will die if you don’t change your ways” guy, second was way too “everything is fine”, so I am now on my third.) I have been given so many different diagnoses over the last few years it makes my head spin; papillary necrosis, incomplete dRTA, nephrocalcinosis, idiopathic stone former, and just recently MSK.
Background:
I have passed small calcium/oxalate or calcium/phosphate stones or some combination of the two types since I was 18, at a rate of a stone every few weeks to months, to date over 100 stones that I have caught. I am now 37. Every doctor that I saw about stones just told me to drink more water and sent me on my way. Largest stone was 11 mm but passed on it’s own, it was extremely painful and triggered an emergency room visit where they did a CT scan. I have had two CT scans without contrast and both showed innumerable calcifications in both kidneys. First radiologist called it papillary necrosis (May 2014), second called it MSK (Oct 2018). The second CT showed a significant increase in the number and size of the calcifications. Blood work over the past 18 months has shown an eGFR of 57-59 using the BUN-Creatinine ratio, eGFR previously was always >60. My creatinine has gone from a 0.7 to a 1.1 in the 4 years of regular labs. My first set of labs done showed a low potassium and Vitamin D deficiency. No other blood or urine tests show any abnormalities, aside from a high urine pH 7-7.5. Highest calcium in a 24 hour urine was 222 mg. All of the 24-hr urine tests looking for stone risk show that my levels are all very good with only the pH putting me at risk of stone formation. I have been taking potassium citrate for 4 years, and hydrochlorothiazide for several months. I have also been on a low sodium (<1500 mg), moderate calcium, and low oxalate diet for 4 years. I drink over 4 liters of water a day. I recently tested 1:2560 positive for Antinuclear antibodies (ANA).
Questions:
Could a diagnosis of MSK be wrong? Could this be an autoimmune disorder that is causing the calcifications? Does diagnosis matter if prevention is not helping???
Hi AJ, Given high pH and calcium phosphate stones, MSK is not probable; more likely you have calcium phosphate stone disease with multiple tubule plugs that along with stones are giving rise to the radiographic images showing lots of renal calcifications. The ANA is interesting in that some immune disorders cause renal tubular acidosis that can produce a picture like yours. You need expert consultation. If you tell me where you live I could try to identify a reasonable source. Regards, Fred Coe
Hello! I have medullary sponge kidney. I have had 14 lithotripsies in the past 5 years and multiple basket retrievals. I just had both sides cleaned out in February and both kidneys have multiple stones again. I am a 38 year old working mother of 3. I am active and this is putting physical restraints on me. Surgery followed by several weeks of stents is not working. Not to mention the cost of surgeries. I am currently taking potassium citrate and amilorhide. I told my husband I would travel to mayo for help. I am desperate.
Hi Megan, I believe I answered this already. Let me know if that is incorrect. Regards, Fred Coe
Would you please comment on whether any type of postural drainage would help prevent the formation of stones in patients with MSK. For example would a daily exercise like yoga where a patient is inverted with down dog, horizontal and rotated side to side with planks, etc help prevent urine from pooling and crystallizing? Obviously this would be in addition to hydration and dietary measures.
Hi Linda, Given the microscopic dimensions of the stones within medullary sponges what you describe is unlikely to help. Likewise, the cysts drain into the collecting ducts, so no amount of external motion can do much to remove them. But, most ‘MSK’ is not really MSK as the article points out, so treatment may be possible. The usual mistake is vs. calcium phosphate stones – uncommon with MSK and capable of producing a similar picture to MSK on CT. Regards, Fred Coe
I’ve had issues with stones for 20 years-I’m 44 now. I was recently diagnosed with MSK after having surgery to remove stones in April. Stone analysis came back as calcium oxalate dihydrate 15%, calcium oxalate mono hydrate 70% and carbonate apatite 15%-could this be a misdiagnosis? My urologist hasn’t explained anything to me about the disease or prevention of more stones. Is a urologist the best doctor to handle MSK or should I be looking for a nephrologist. I am having pain more consistently now and I’m looking for options for relief without pain meds. I live in Elgin, IL. Thank you for your time.
Hi Vanessa, Your surgeon would have seen the inside of your kidney if he did ureteroscopy and therefore knows if there are medullary sponges or simply stones. The calcium oxalate composition is certainly compatible with MSK provided they are not simply growing on plaque. I would ask s/he directly if sponges are there. If so, routine stone workup is right and prevention as for any kind of stone disease with the proviso that the sponges indeed make more stones a higher probability. Regards, Fred Coe
I have msk bi lateral stage one with over 600 kidney stones . We are rarely treated as a patient to patient basis there is no understanding from dr about chronic pain that comes with this disease for most patients. Alot of friends I found online with this disease have ended their own life after being cut off of pain medication that is the only thing that helps with their quality everyday life. Most dr read asymptomatic and think that we are drug seekers thanks to the recent epidemic. This disease is harsh, brutal. Unforgiving, and deserves more attention. There is no where for msk patients to turn which is why so many of us are turning to suicide. This article was one of the best I’ve read. Thankyou for bringing awareness to the seriousness of this disease
Hi Ashley, Suicide is a terrible concept. If you have such pain, perhaps your surgeons might want to open up the sponges surgically. This can be done via digital ureteroscopy. No trials prove efficacy, but you describe a harrowing kind of situation. Regards, Fred Coe
Hi. I want to aploligize right off the bat as I’m sure I’m going to be rambling on. I am 37 years old and I was told about 5 years ago that I have MSK. The 1st Dr. told me that there is nothing they could do that I would just have to change my salt in take. I felt like there had to be more they could do so I found a new Dr. The new Dr. had a lot of ultrasounds done and 1 CT scan done in which they said that both of my kidneys are 1/4 of they way calcified. They didn’t have anything to compare against (as my 1st Dr. just washed their hands of it) to see how fast they had calcified. This was about 2 years ago. I asked if they could do another scan last year to compare and they had no idea what I was talking about as my Dr. who told me my kidneys were completely calcified 1/4 of the way has since moved to a different hospital and my new Dr. isn’t concerned about it. They put me on a regiment of 1 gallon of water with 1 1/2 cups of lemon juice a day. I did this for about 2 weeks until my throat was raw from all of the acid. I have had UTI’s ever since I could remember. I just recently had another where I was told that my body is becoming resistant to the medications and I will eventually have to do IV treatments to treat them. I feel lost and confused. Do you have any recommendations for a great Dr. in the wisconsin area or surrounding states that could possibly help me? Thank you in advance.
Kimberly
Hi Kimberly, Most MSK diagnoses are wrong, so you may have it have another kind of stone disease altogether. Dr Steve Nakada at University of Wisconsin Madison is outstanding and runs a fine prevention center. I know him well and please feel free to use my name as a reference. Regards, Fred Coe
Hi Dr. Coe,
I am very happy to have come across this article. Thank you. I have MSK and am newly diagnosed. I have not passed many stones(though I do have quite a few hanging out) but I have, in my doctor’s words, prominent calcification at the corticomedullary junction of both kidneys(I am not really sure what this means). I am currently in the north suburbs of Chicago but will be relocating soon to the Phoenix area. Can you recommend someone in that area?
Thank you very much,
Megan
Hi Megan, I doubt you have MSK and suspect calcium phosphate stones in stead. Sorry you are moving as I could have helped you here in Chicago. In Phoenix, I would recommend Dr Humphries at Mayo. I see nothing at the local medical school. He is excellent and a friend of mine. Please feel free to use my name as a reference. Regards, Fred Coe
Hi there! I was just seen earlier this year for blood in my urine, lower abdominal pain, and a CT scan showed multiple stones. All of which, I was informed, should be passable. I had a follow up with my primary care provider and he mentioned the report suggested MSK. He rechecked my urine for blood and found nothing. I don’t know if it’s related, but I know when I was a child they had concerns over one kidney being smaller than the other. I’m obviously a bit concerned because I don’t feel like he knew much bout it or gave me much info about it. Should I be worried? Should I push to see a urologist to gain a more in depth understanding of what I have going on? Also, if it is should I be concerned about hyperparathyroidism? I’ve had high T4 uptake before which I’m unsure if that is related to hyperparathyroidism or just hyperthyroidism in general. All in all I’m just worried and not sure what next steps should be or even what I can do to help reduce risks of complications.
Thank you for your time!
Hi Alora, Very confusing. You have stones, for sure, and need a plan for evaluation and prevention. This is a good introduction. Here is another more detailed version. The Kidney Stone Book itself is a good next place to read in. If you follow the general plan in the first two links your physicians can figure out the cause of your stones and help plan treatment. Regards, Fred Coe
Dear Dr. Coe, Thank you for sharing your experience and research through this website. I was diagnosed with MSK 11 years ago and have passed so many stones that I’ve lost count, along with lithotripsy and basket extractions numerous times. I recently changed doctors and I feel we are making progress with diet and medications. I do have a couple of questions that my dr. has not been able to answer. I am hoping that you can.
1. How long does it take to create a stone? On numerous occasions I’ve been told that I was stone free (x-ray diagnosis) and a couple of months later I’ve passed a stone. Of course to diagnose me prior to pain medications the ER wants to do x-rays. I understand their need to correctly diagnose but I need to be my own advocate. I know when I have a stone and do not need an x-ray to diagnose me. The laws have also changed recently and my urology office cannot just call in pain medication without an x-ray diagnosis.
2. Is there any research that ties high blood pressure, preeclamsia while pregnant, and MSK together?
3. Do you know of any clinical trials for MSK?
Best regards, Kristy
Hi Kristy, It takes months for calcium oxalate stones to grow appreciably, but calcium phosphate stones can be faster – these are my experience, I know of no real data. I suspect your stones are calcium phosphate. With many small stones, the xray evaluation depends on the technique. CT scans show most stones, ultrasound about 65% of CT and routine single abdominal film much less. So the last of these can say stone free when the CT would show many small stones. You need prevention. I cannot imagine why not. Take a look here and see if the articles do not help a bit. Stone formers have problems with blood pressure. And kidney disease. I know of no MSK trials. Regards, Fred Coe
Dear Dr. Coe,
I have recently been diagnosed with MSK. I would like to know what changes to make in my diet and what other changes are necessary while I wait for my appointment with a urologist.
I am currently on a waiting list. I want to stay proactive about my health. I am in pain almost all day every day.
Thank you.
M.
Hi Marianne, MSK is treated the same as other calcium stone diseases. Partly this is because prevention is not altered by the sponges and mostly because most people diagnoses as MSK do not have MSK but some other more common condition – the article you posted on makes this clear. So get the blood and 24 hour urine testing and let your physician recommend treatment. Here is a good guide for your visit. While waiting, just raise your urine volume above 2 liters a day. Other so called remedies are usually without value. Regards, Fred Coe
Dr. Coe,
I am reaching out as a chronic kidney stone sufferer and a diagnosis of MSK. I have had 9 lithotripsy surgeries and 2 basket retrievals in the last 5 years. Multiple stents and once again full of stones I am reaching out for help. Currently I am taking Potassium Citrate and Amiloride. I had both sides done 6 months ago and have several stones again. Thanks for any insight.
Hi Meghan, You have certainly had a large amount of surgery. MSK is usually calcium oxalate stones, are you sure those are your stones and that you have MSK and not something else? Potassium citrate and amiloride sound odd by themselves, is there not a diuretic as well?? Have you been completely evaluated for cause? Do your urine tests reveal a cause?? Regards, Fred Coe
Marianne,
I am not a doctor but a lifetime sufferer of MSK. I have had several lithotripsies and passed several other stones without intervention. I have been seeing an urologist for years, but my primary doctor suggested I see a nephrologist. This is the one that helped with the preventative stuff. Like Dr. Coe said, The nephrologist ordered a 24 hour urine with a full blood panel and discussed a low oxalate diet with me (and made sure I understood what that meant). I had been given a stone diet for years, but this is the doctor that explained it. It’s more than just avoiding tea, coke and beef. I hope this helps! And, good luck! There is no way to stop the stones but this has helped slow them down. And, don’t go dairy free. Dairy carries the oxalate out of the body…
“Stones may cause pain in MSK despite the lack of ureteral obstruction and inflammation and cell injury.” THANK YOU FOR THIS. I’ve suffered from what has tentatively been diagnosed as MSK for almost 15 years now (although with this article, I wonder if it’s some sort of ductal plugging instead…?) I was told by my nephrologist (who is very old school) that I have “some kind of MSK”, and the “good” kind of MSK (is there a thing?), the one which I never get kidney or urinary infections, the one where stones rarely become stuck in the ureter, the one where I’ve never actually seen a stone pass; instead, I have the one where I have a chronic flank pain (at best it’s comparable to having sand in my eye–a constant nagging cramping pain on both sides, at worst it’s the sharp unrelenting pain that lands me in the ER for management), low level hematuria, and visualization of multiple bilateral stones on CT. I did the 48 hour urine collection and my stones are calcium oxalate. My pain is unrelenting, but is manageable for the most part. The thing I deal with most is when it isn’t, and I wind up in the ER. I can’t tell you how many times I’ve been treated like a drug seeker because the CT shows no obstruction. “Nothing is obstructing, so you shouldn’t have any pain.” is a phrase I’m told, often condescendingly. I usually reply with “Do you think having an organ packed full of 20 stones would NOT be painful?”. Most ER doctors are not up on current research and will argue with this. My kidney function has always been fine, like I said, no infections or large stone passing. I’ve had four ureteroscopies over the years to “unroof” stones, as the article put it. My urologist said my stones are mostly “packed into the meat” of my kidneys, but he can go in every few years and “clean out” what he can. Do you think this sounds like MSK, or some other stone disease?
Hi Sarah, You say the stones are calcium oxalate but say it in the context of the 2 24 hour urines. Were actual stones analysed and found to be calcium oxalate?? WHat was found in the 24 hour urines that might lead to stones?? Your pain seems to worsen in attacks, could these be crystal passage events – pain like stone passage, hematuria, no stone seen? Regards, Fred Coe
Hello Dr. Coe,
I was just recently made aware of my diagnosis of MSK and nephrocalcinosis. I’ve had kidney stones since I was 11 years old. However, I had very few stones in my youth compared to now (age 32). I just underwent laser lithotripsy/ureteroscopy for the removal of approximately 30 stones in both the right and left kidneys. This is my 5th stone removal procedure since I was 11. I’ve had several stone analysis procedures and have had different types of stones show up in each study. When I was 11 it was calcium oxalate. In my 20’s my stone analysis showed “carbonate apatite dahlite.” My most recent removals showed a mixture of calcium phosphate and apatite stones. My 24 hour urine tests showed that my urine contained excess amounts of brushite, and is too alkaline. I was on an antibiotic regmine to prevent stone formation, but it did not help. It appears that the stones are increasing in numbers over time. I had approximately 20 stones removed (10 in each kidney) prior to my most recent procedure. I have family members who also suffer from stone disease with the same amount of stones present. My urologist noted that the anatomy of my kidneys did not appear normal, and the colluction ducts were dialated. Is this true MSK or possibly something else? I’m confused about why I can create so many different types of stones.
Hi Marisol, I suspect you have increased urine calcium and pH and have multiple plugged collecting ducts – the typical picture of a calcium phosphate stone former. Treatment is important and usually successful. MSK is not likely here. This article sums up how to evaluate someone like you. Regards, Fred Coe
I was dx with MSK about 8 years ago. I’ve only passed a few stones, which were tested and found to be CaOx. I’ve be advised to stay away from high oxalate foods following several 24hr urine collections due to high oxalate levels in my urine. I haven’t seen a nephrologist in about 4 years. My latest Urinalysis showed a pH of 8. Which is out of the ordinary for myself. I’ve always started developing what I can only describe as constant urtheral pain. Any knowledge of urtheral pain and or a sudden pH shift to alkaline?
Hi Beth, High urine oxalate is not very common in MSK, and the cause needs to be found and treated. THe high pH and urethral pain could reflect infection with bacteria that hydrolyse urea to ammonia – your physicians can tell. Food oxalate is hardly your main approach, rather the cause of the high oxalate: low calcium diet is a common one. Regards, Fred Coe
Just had an U/S return a finding of MSK after a decade of nagging flank pain, hematuria and 2 lithotripsies in the last 3 years. None of my other scans have found this- is it worth pursuing to determine if this result is correct? My urologist says it doesn’t change anything for treatment.
Hi R Lang, It does not matter in that US nor CT can diagnose MSK unless the CT is infused, and that is not worthwhile. But you should pursue prevention. Here is a good place to start. Regards, Fred Coe
I was diagnosed with MSK 27 years ago. I had suffered with reoccuring uti’s sinc childhood. While pregnant with my second child, I became septic, what seemed like overnight. I was hospitali for almost a full week with many tests ran. I had my daughter 1 week later and surgery to clear my uriter a week after that. After all of those test and surgery, my urologist informed me I had something called MSK. I’ve been treated by. Y family physician for years, but he has sent me to a new urologist recently. I’ve only seen the PA, but he told me, he doesn’t think I have MSK, since my kidneys looked pretty healthy on the ct they ordered. I’m just so confused. What has caused me horrible pain, neumorous er visits, and many streams of red torture? I suppose my kidneys looking pretty fair is good news, but leaves me wondering why I’ve had such a rough kidney life.
Hi Carol, If you are confused, so am I in that what is wrong is not clear. Do you have stones? Have you passed any? Are stones visible on your CT. Is it that you have had many urinary infections and no stones but MSK has been diagnosed in the absence of stones? You mention your ureter as if it were once obstructed by stones, but do not mention any stones. It matters a lot. Perhaps you might want to clarify these matters. Regards, Fred Coe
Hi, I’m from Philadelphia area, diagnosed 19 yrs ago IVP MSK. I’m 55 yr old female, passed over 150 stones, both kidneys full of stones, have had no surgeries or treatments. Over the years, several ER visits, most recent was the worst, severe kidney infection. I sufferred four days of bright red urine, severe pain in back, weakness, chills, fever and an unexplained skin tightness/pain I never experienced right before I drove to ER. I am now up to date with CT, KUB, 2 24 hr urine & complete bloodwork. I followed up with several urologists who tell me to go to a Nephrologist only to be told to see a urologist. It’s discouraging, as this has been my ping pong life the past 19 yrs. I have had a very busy life raising children and caring for aging parents that I am now able to 100% focus on myself. I have increase fluids adding Apple cider ving & lemon, cut to low oxalate medium calcium diet, minimal to no salt, increased exercise and losing weight by eating clean diet & focusing on 7-8 hrs sleep. The last few urologist all suggest surgery to remove stones in both kidneys, each of the largest stones are over 2cm, one in each kidney. He told me he would go in my back, 2-3 holes to insert tubes to get to stones, 3-4 hrs for operation. He said I may need 2-3 surgeries to get all the stones out…then repeat the same operation on the other kidney. Need help. I feel good, my tests all came back ok, but Dr said an operation is inevitable. Does that operation sound normal? Can you recommend a team urologist/nephrologist that knows how to handle MSK near Philadelphia? Or, who is doing studies with up to date data on MSK? Thank you for your help.
Hi Mary, You really do need experts in your life. U Penn is the best bet I know about. This doctor is outstanding, and someone I know personally. I would contact him and let him help you. Warm regards, Fred Coe
Hi Dr Coe,
Thank you for your response…What Dr at Univ of Penn do you recommend?
Thanks,
Mary
Hi Mary, The one in the link, Dr Wasserstein. Fred
I am 53 and was accidentally diagnosed with MSK last year. As a teen and young adult I was plagued with UTI and finally thru and IVP Doctors said that there was a nerve where the ureter connected to the kidney that was causing a blockage and they needed to do surgery immediately to repair this birth defect and get the urine flowing again. So at 27 I was cut from my belly button all the way around to the middle of my back on the left side of my body. At 47 they found a stone in the same kidney (my left) the told me it was attached to a suture and they needed to go in through my back to take it out as I wasn’t a candidate for lithotripsy because of the previous surgery and the scarring it may have caused, so they went in through my back took the stone out and I walked around with an 18″ tube hanging out my back for a week then they pulled the tube out and I had pee splashing/;running out my back for about 4 days then it healed. The incidental diagnosis came during a trip out of the Country. I went to the ER in east Africa with severe stomach pain and I have a very high tolerance for pain, when I came out of both surgeries mentioned above and 2 C-sections, I refused all pain meds as I hate the way they make me feel. Anyway, this pain was radiating around my waste and was severe and I was vomiting, they hydrated me and did an CT scan which showed that I had a stone in my right kidney. So I went to South Africa and the urologist there order her own CT scans and found that a case of pancreatitis caused the pain but she diagnosed with MSK and said that my case was classic as my kidneys glowed on CT scan, both kidneys are affected. I was 52 and I have only had two stones in my life or that I am aware of and both of them (well one now) were high in the kidneys. However this did explain my frequent UTI’s (one time I was on preventive antibiotics for a year), and the bright red blood that was frequently in my urine which always seemed to alarm the nurses but not me because it was par for the course for me. I came back to the US and is seeing a nephrologist that put me on 25mg chlorthalidone as he says it should reduce the number of stones I produce, but I’ve only produced 2 in my life?! He also put me on allopurinol because I have high uric acid levels, but no gout, yet. My concern is now that I know that I have MSK what do I do with that diagnosis? Not many Doctors know anything about it…when I tell a PCP they just stare at me…helpless in Georgia
Hi Gee, From your story I suspect your CT showed many small calcifications in both kidneys and this condition is mistakenly labeled as MSK when most of the time it is not indeed because of that specific kidney malformation. My suspicion is calcium phosphate stones because of genetic hypercalciuria, the bleeding from crystal attacks, but that is pure conjecture. Be sure you are fully evaluated for prevention – of more small stones and of their growth! and if a stone is recovered that it is promptly analysed. Regards, Fred Coe
I am 38 yrs old. Been passing dozens of stones for 15 years now. They say it msk. I have had every test, chemical wise, nothing abnormal.i have had lithotripsy 5x. Stints endless uti. Pregnancy is miserable they multiply and are 10x worse. I wish there was a solution.
Hi Erica, I doubt it is MSK as most such diagnoses are incorrect being based on mere CT scans. Perhaps you form calcium phosphate stones and have myriad tubule plugging. I frankly doubt your 24 hour urine and fasting morning serum values all are normal, and suspect you have too high a urine pH and calcium excretion. I would be sure about all this with your personal physicians. There may indeed be many solutions to such extreme stone disease. Regards, Fred Coe
Thank you for this article. Like many who have replied, I’ve suffered since early childhood with UTIs, abdominal pain and flank pain. My pregnancies were difficult with excessive fluid gain and high blood pressure. It was only by a fluke CT scan that my PCP discovered I had MSK in both kidneys. Since that time every ultrasound tech or doctor comments on how “interesting” my kidneys look and how they are so full of little stones. I now take diuretics for higher than normal calcium levels in my urine, however that doesn’t really help with the pain and frequent UTIs. In fact, my doctors are resistant each time I reach out for antibiotics saying my urine looks ok – despite high PH levels, high squamous cells, and other slightly out of range results. The general response is that it is a benign condition and I should just get on with it. It’s really frustrating to have professionals discuss drinking lots of water, hygiene and cranberry juice when I’ve been dealing with this for over 40 years. So my question is this…where are the specialists who actually take this condition seriously and what are the “treatment strategies” because I haven’t found them. Most Urologists seem focused on prostates and Nephrologists with more advanced disease. Any recommendations in Boston? Thank you for drawing attention to this disease. It has impacted my life in a very real way. It would be nice if more MSK research and education was available for physicians. I feel I’ve been under-treated and doubted for many years and fear a “cry wolf” situation each time I seek help.
Hi Katie, Frankly I doubt MSK and suspect you have stones from the high urine calcium. One clue is stone type. MSK is usually calcium oxalate, other kinds of nephrocalcinosis are usually calcium phosphate stones with tubule plugging. Idiopathic hypercalciuria may be why your urine calcium is high, and treatment is more than a diuretic. Pain from small stones is a major US issue right now, incidentally and we need surgical trials to see if removing them helps. Dr Gary Curhan at MGH is an excellent kidney stone expert who might be helpful to you. Regards, Fred Coe
Very interesting read. I’ve been diagnosed 10 years ago. It started with flank pain, blood in urine and UTIs. Later on I had to have my ureter rebuilt due to extensive damage from stones passing (formed scar tissue making my ureter close up). I stopped breathing as a baby 2/3 times. They later on found out it was due to a serious kidney infection. Had one more time in middle school where I fainted when I had to go pee. Otherwise I only started showing symptoms 12 years ago. Pregnancy went well, just had a UTI towards the end but I have a reflux ureter post surgery in 2013. They tested when diagnosed – both kidneys show renal calculi – calcium oxalate. My brother have been diagnosed with same this year. My specialist is however almost 2000kms away from me, and I had a real struggle to find a GP that trusts me (for example, it is known to not have pain if not passing a stone, where MSK patients have contra indicated that). I’m not on any treatment, but I’m doing quite alright.
Hi Tania, I gather you have MSK with infections and ureteric scarring as well as reflux, with many stones seen on radiographs – thence the MSK diagnosis. What seems unfortunate is that you have no physician expert close enough to you to provide ongoing care. Thanks for sharing your experience. As you pose no specific question, I presume you wrote to share – a gracious act. Regards, Fred Coe
Hi,
I really enjoy the in depth articles you are providing.
I have recently done some more 24hr urine tests after undertaking a low sodium diet.
I have been told I have MSK and have analytics done of several stone and they have shown to be calcium oxalate stones. I have passed around twenty stone of various sizes generally increasing over the years. I am currently 31 and started getting them at 18. They were tiny at 18 but the last one I passed was 3&5mm.
Before going on a low sodium and low processed sugar diet my readings were as follows
Urine output 2.6ltrs
Urine creatinine 6
Calcium 4.9
Calcium 24hrs 14.1
Ca/creatinine ratio 0.82
Sodium 95
Sodium 24hrs 285
Potassium 46
Potassium 24hrs 138
Creatinine 24hrs 18
Then with the diet it was
Urine output 3.345
Urine creatinine 4.9
Calcium 2.5
Calcium 24hrs 8.4
Ca/creatinine ratio 0.51
Sodium 13(L)
Sodium 24hrs 43
Potassium 32
Potassium 24hrs 107
Creatinine 24hrs 16.4
So my question is there anything else you would suggest that might help with my diet? And would a fasting 24hr urine and blood test tell me anything more accurately?
I have been told I have MSK based on about 20+ calcifications on each of my kidneys. Most of them are quite small (1mm) but are obviously growing. When I was 18 there was no signs of it.
Your help would be appreciated.
Beau
Hi Beau, With the fall in urine sodium, urine calcium fell remarkably – as expected – but remains high enough to produce considerable stone risk. Fasting urine would tell you nothing useful. I presume your serum calcium is normal. As for MSK, just having multiple stones on a CT says nothing, and I suspect you have more commonplace stones. You might mention to your physician adding a low dose of chlorthalidone 12.5 mg daily to your low sodium diet, to lower urine calcium more. Alternatively, given the stones are not calcium phosphate, you might add potassium citrate 10 mEq twice daily, which may lower urine calcium without the side effects of the drug. Regards, Fred Coe
Thank you, yes serum calcium was normal. Initially the specialists wanted me to go on a drug, I imagine the one you mentioned, but when he mentioned the side effects I said was still quite young and that I’m sure my diet had something to do with it. I went about researching(thanks to your website) I was able to adjust my diet to achieve better results but he is still pushing me towards the tablet (which I’m not against) I just want to do all I can first. It is not my wish to be on a tablet the rest of my life if I can help it. He also mentioned the tablet diuretic/ thiazide also looses its effectiveness over time and would have to be increased the longer I use it, is this correct? Are there any other levels that I can monitor, as in vitamin D, phosphate ect that will effect calcium urine?
Thanks again beau
Hi Beau, This article gives a sequence of steps culminating in a drug. It is reduced sodium, high diet calcium, moderated diet protein, reduced refined sugars, high fluids all together. This diet mimics the ideal US diet. I add the drug to the diet, so the dose can be very low and indeed it can work life long. But see how far the diet can take you, and read the rationale in the article. Regards, Fred Coe
Very interesting article. I was diagnosed with MSK in 2006. My stones have tested as composed of calcium oxalate. Thankfully my stones have remained somewhat unchanged over the last few years without extensive need for surgeries as others have commented. My question is I am currently dealing with elevated parathyroid hormone levels while my calcium remains within normal limits and my Vitamin D levels have dropped below 10. Referral to endocrinologist has me taking a large vitamin D supplement but I question the relation to my MSK diagnosis. Any correlation between MSK and PTH/ Vitamin D issues that you are aware of?
Hi Lori, High PTH with normal serum calcium arises from low vitamin D stores (as you have) and also from low calcium diet. The latter is very bad for bone health and probably for kidney stones as well. This so called secondary hyperparathyroidism is very well known, and should respond to vitamin D and a high calcium diet. Stone prevention should shun low calcium diet, and rather use low diet sodium to control urine calcium while providing for bone. High diet calcium also lowers urine oxalate. The whole package is the correct kidney stone diet – here is a good review of its parts. Regards, Fred Coe
Hi I’m 35 years old and was diagnosis with MSK in both kidneys almost a year ago. My urologist did remove as many stones as possible from both kidneys but was unable to remove them all due to where they were located. I make calcium oxalate and calcium phosphate stones and I have been told my right kidney is becoming calcified. My question is do you know the percentage of patients that have parathyroid problems that relate to calcium oxalate and calcium phosphate plus nephrocalcinosis? My parathyroid level was 38 pg/ml on during my last lab work.
Thank you.
Hi Jennifer, From your description I think you have tubule plugging not MSK, and need prevention. I hope you have been fully evaluated. Serum PTH is not diagnostic of primary hyperparathyroid, it requires that serum calcium be above normal. I am sure your physician wants very aggressive prevention, and I hope you achieve it. Regards, Fred Coe
I’m 54. Disgnosed with MSK on IVP at age 29. Have had only two stones that caused pain five years ago. I’ve never had any treatment or tests done. The last few years my urine has smelled bad and my sweat is so salty it can be seen on my clothes. Are these symptoms I need to be concerned about?
Hi Kelly, when sweat is salty, it means diet sodium is very high. I would consider a more moderate diet. As for the smell, if it is like ammonia I would mention it to your physician who would want to look for the common cause of it – colonization with urease possessing bacteria. Regards, Fred Coe
was diagnosed with MSK 15 years ago, have had over 21 RIRS to remove stones blocking my ureter from both kidneys. I am on Urocit as prevention,
what is the long term solution? i’ve had so many CTs i am worried it is hurting me
Hi A Razak, I am suspicious you have calcium phosphate stones and not MSK, and if that is true you need different treatment. Be sure about the type of stones. Likewise, that you have been fully evaluated and receive treatment based on what is causing your stones. Surely with so much surgery prevention is very important but will not be achieved without a rational method. Regards, Fred Coe
I WAS DIAGNOSED AT 24 WITH MSK I’M 43 NOW I HAVE INCREASED BLOOD VOLUME IN MY URINE WENT FROM TRACE TO SMALL IN THE LAST 6 MONTHS ..AND A UTI AT LEAST EVERY OTHER MONTH AND INCREASED BACK PAIN . AFTER GETTING NEW INSURANCE AND A NEW DR A YEAR AGO AND TELLING EVERY DR EVERY TIME I VISIT I HAVE MSK (HE ACTING AS IF HE UNDERSTOOD WHAT IT WAS ) KEPT ONLY RUNNING KIDNEY FUNCTION PANELS TELLING ME EVERYTHING IS FINE EVEN AFTER I WOULD EXPLAIN WHAT MY CONDITION CONSISTS OF ..IT WAS ONLY YESTERDAY AFTER I MADE HIM GOOGLE IT AND LOOK UP MY RECORDS WITH MY OLD DOCTORS THAT I FINALLY GOT A REFERRAL TO A NEW UROLOGIST NOW THAT HE REALIZED HE DOESNT KNOW A THING ABOUT MSK….I WAS HOPING MAYBE YOU CAN GUIDE ME AS TO WHAT TESTS I MAY NEED TO HELP ME …IM SCHEDULED FOR A ORDINARY CT NEXT WEEK HE WASNT SURE IF I NEEDED CONTRAST ..NOW IM ON ANTIBIOTICS AGAIN AND THE DIET DR DOESNT EVEN KNOW WHAT FOODS I SHOULD EAT OR AVOID TO STAY HEALTHY . ANY POINTERS WOULD BE GREAT AS I NEED HELP GUIDING MY DR .
Hi Carrie, An ultra low dose CT is ideal, without contrast, and your evaluation should be the same as for any other calcium stone former. Any passed stones need to be analysed, too, as you may not have MSK but rather calcium phosphate stones. Regards, Fred Coe
I have been diagnosed with MSK by my urolgist – I have multiple stones in both kidneys last count was around 25, ranging from 4 mm to extremely tiny. One small cyst on one kidney, here are my 24 hour urine results. All of this started only a couple of years ago. I have had no surgeries we are waiting until I have a blockage or complication because the doctor states we would not be able to get all of the small ones anyways. I am told it is not diet related and there is nothing I can do.
Calcium Urine – 181
Oxalate Urine – 17
Uric Acid Urine – 427
Citrate Urine – 659
PH Urine – 7.4
Total Urine volume – 1.27
Sodium Urine – 18
Sulfite Urine – 12
Phosphorus Urine – 478
Magnesium Urine – 79
Ammonium Urine – 14
Potassium Urine – 51
Creatinine Urine – 934
Calcium Oxalate – 1.29
Brushite – 3.92
sodium Urate – 2.25
Struvite – 17.01
Uric Acid – .07
Listed as high PH and urine volume
Hypoparathyroid test negative
I take Hiprex twice daily with Vit. C which has decreased my ph to normal levels, but suffer from recurring UTI’s and have become antibiotic resistant or allergic to most except for 2 antibiotics, which they state they are saving for if and when I go into sepsis. I have been told there is nothing they can do for me and that my “system is infected” so I will always have an infection. I recently read about biofilms and resistant UTI’s and have some hope that I may be battling this as well. I pass a stone about every 6 months, but I feel constantly worn down by the persistent infections. Does this fit the profile for MSK, from what I read it doesn’t my last ultrasound the tech even mentioned except of one spot in my kidney it doesn’t look like MSK. Any insight would be greatly appreciated. I’m 52 and not ready to slow down quite yet.
Hi De Anna, Your urine results are very odd. The sodium is listed as 18, if this is the conventional mEq/d that is remarkably low. The pH is listed at 7.4, that is so high there must be a reason. Potassium is much higher than sodium! I know nothing about you, but am concerned that these numbers are remarkable and require explanation. Your physician may know more than I about what has caused low urine sodium with normal urine potassium and very high pH. Did you have urine chloride in the testing? Was it low or high? From here I can only urge these value find a reason, because the reason may give a clue to the stones. Regards, Fred Coe
Thank you for responding, there appears to be no urine chloride result. But I did notice an error in my above numbers the Sodium Urine result was 98 (not 18) the reference range is < 200 mEq/day. Then there is also a sodium Urate number which is noted as abnormal on the test which is 2.25 with a reference range of < 2.00. Also I see that I left out the urine volume which was noted as low at 1.27 liters. I drink only water all day long upwards of 100 oz per day if not more. The ph of the urine was a conundrum for my urologist and she asked be if I was eating a lot of fruits and vegetables which in fact I was not due to following a more paleo diet regime. My urologist does not seem to know what to do other than to say I am a stone maker. I'm frustrated. I live with constant fatigue, these UTI's and GI problems as well. I had some elevated creatine levels in a blood test awhile back but she said not to worry about it. Any other insight would be amazing, before I go seek another physician opinion, I want to make sure I can work with someone who has some understanding of what is going on with me.
Warmly, De Anna
Sorry I meant to say by Creatinine was low .5. I am also vitamin D deficient and have to take 5,000 mg a day to stay in normal ranges. My PTH test was normal but I have read were you can get false negatives, I’m just trying to get as much information as possible, I feel like I don’t fit perfectly in a box somewhere and it’s frustrating.
Hi De Anna, so low a serum creatinine suggests either very small size or possibly low muscle mass; the vitamin D deficiency needs correcting as it is unhealthy. No one fits in a box; in all my thousands of stone patients none are exactly alike. Regards, Fred Coe
Hi De Anna, So low a urine volume! Perhaps you lose fluids from your GI problems, or perhaps from sweating, but that volume alone poses terrific stone risk.The high pH has some cause, the lack of urine chloride suggests a poor 24 hour urine panel. If you tell me where you live I could try to recommend possible additional physicians who might add to your care. Regards, Fred Coe
Thank You so much Fred, I’ve spent the last few weeks just utterly exhausted and fighting a UTI that an antibiotic does not want to touch. The nutritionist I am working with thinks I might have SIBO, hence the dramatic issues I am having from a GI perspective. I live in Orange County, CA specifically Huntington Beach area, but willing to travel even into Los Angeles or San Diego to work with a more knowledgable clinician. I have suffered from chronic pain which has been labeled fibromyalgia for the last 13 years which limits my ability to be active, I used to run, enjoy spin classes and dancing and now sometimes I can barely walk around the block or open jars and grabs items. My mother also found an old urinalysis from when I was a child that showed increased protein and crystals, my mom stated my urine consistently had elevated protein levels and interestingly enough I also had low amniotic fluid with my last pregnancy that required modified bed rest and drinking a ton of water. My hopes is to also find out if this is genetic so I can see if my daughters will be affected as well. I’m so glad I found this site it has been a wealth of information and given me hope that I can gain some understanding and treatment rather than be told “There is nothing we can do!”
Hi De Anna, Crystals can cause symptoms like UTI so your physician can look for them. You do not mention stones, nor evidence for MSK, so I am a bit confused as to the aims of your medical consulting. Is it fatigue? If so, is there a reason to assume it arises from stones? If you can, perhaps more information might help me offer more to you about possible next steps. Regards, Fred Coe
Yes, I referenced my MSK diagnosis in my first post (perhaps it has gotten messy on the back end of the website) on August 20th along with my stone count which is 25 bilaterally with chronic UTI’s, (brushite/phosphate) My 24 hour urine results are in the above post as well, High PH, Low Ammonium, Low Volume 1.27 liters, low serum Creatinine.. I’m vitamin D deficient (take 5,000 mg perday to have a normal range, fibromyalgia, GI issues ( my nutritionist thinks I have SIBO), multiple allergies to food, chronic fatigue, UTI”S resistant to most antibiotics now and told by doctor’s there is nothing they can do Urologist and Infectious Disease. My stones are too small to remove and I will just make more, my system is infected so as long as I have stones I will be infected and they just hope I don’t go into sepsis. You stated you were possibly going to look at some referrals, given that I should find out why I have such a High PH and Low Volume, I’m in Huntington Beach, willing to go to LA or Orange County. Any help would be appreciated.
Hi De Anna, You have brushite stone disease and certainly not MSK. Brushite stones cause plugging of the ends of nephrons and create multiple calcifications both at x ray and during URS. The cause will be high urine calcium and pH, and low volume will certainly add risk. Sometimes stones do get infected, and any actual stones are best removed via URS, but embedded calcifications cannot be easily removed. Dr Ralph Clayman at UC Irvine is a famous kidney stone expert, and I would consider going there. It is impossible to see serial inquiries using WordPress, as they are not compiled well, so perhaps I appear a bit scattered in terms of details. Regards, Fred Coe
Thank you for the referral to Dr. Clayman in Irvine I see him next week.
Warmly
I have medullary sponge kidney and was born with several other markers of Beckwitch Wiedermann Syndrome. I greatly appreciate your research. Are there any doctors that have expertise in MSK that I could see in the Washington, DC area (or if needed will travel) that I could consult with? Thank you.
Hello, I have been forming kidney stones since I was 15 almost 40 now.Diagnosed @ 27. I mostly pass gravel/crystals. However i recently just passed a stone that had been bothering me for 2 months and had a CT showing a 9.5mm non-obstructing stone that had grown from 4.2 mm in a little over a year. I’m going to see a urologist next week to see what my options are for removal. There were numerous other small stones in both my kidneys. Too numerous to count. This will be the first time I’ve needed to get treatment for a stone. I’ve always passed them on my own. My question is there any genetic testing for MSK? I believe my daughter may have it as well.She’s 12 and she has had a couple UTI’s in her life in addition she has the same dental problem as me. Microdentia. Lack of teeth. Which i believe is related to MSK. In addition is there any research studies available for MSK? I also suffer from Eosinophilic Colitis, which in of itself is rare as well for an adult to have. I look forward to hearing back from you. -Kristina
Hi Kristina, I am not so sure about MSK. I would have thought you formed calcium phosphate stones and the multiple stones on CT are really deposits of crystals in the kidney tubules. What were the stones made of?? MSK has no genetic testing. A search of PubMed using the phrase ‘microdentia AND medullary sponge kidney’ gave back no publications. Spell correction to microdontia with MSK gave none either, nor did a Google search for all of its inadequacies and redundant noise. I found one paper on anodontia – no teeth – and MSK. but do you and your daughter have teeth? If not, then maybe you are a second family. A search on PubMed for Eosinophilic Colitis AND medullary sponge kidney yielded no publications. So, no links, and frankly I believe you have calcium phosphate stones and need specific treatment to prevent them. How about the stone composition? Regards, Fred Coe
My wife was diagnosed passed her first stone in ’97 and three years later was diagnosed with MSK. We went through several rounds of Lithotripsy over a few years. The stone burden always returned quickly. After the last procedure was done back in 2003-2004 she was left in constant pain. The pain gets worse when passing a stone but she has not been pain free for 16 years. After every treatment and doctor possible, we gave up and she has been on pain medication to manage the pain. Now with the political stupidity surrounding opioid usage and what is a first false positive urine test, despite 16 years of responsible and proper use, her pain management specialist has labeled her a drug addict and will not treat her and with a discharge letter stating she violated her care contract we cannot find a new doctor to manage her pain. I know of many MSK patients who suffer in pain, while doctor’s tell them they should not have any pain unless they are passing a stone. I’d like to see more info on the pain associated with many of these cases and what can be done.
Hi Matt, I cannot repeat more passionately than I have that patients with multiple stones do, in large numbers and over a broad range of life circumstances say they experience pain apart from stone passage. By now I believe no one in the field doubts the small stone pain issue is real. At issue is what to do. Narcotics are what they are, surgery has never been tested as to benefit. You do not mention the stone composition but I hazard the guess they are mainly calcium phosphate. If so the rapid return of stone burden may mark incomplete prevention measures, which are the most remediable cause of recurrent pain as you describe matters. Much MSK is actually calcium phosphate stones. Regards, Fred Coe
After reading this article, and many of the comments, I think I’ve spent too much time since diagnosis focusing on events (infections and stone passing) and not management. What would be a better path forward? Would you have recommendations for nephrologists in Ohio (specifically Cincinnati area, but willing to drive…even to Chicago if needed)?
Hi K, In Ohio, Cleveland Clinic is best; Dr Manoj Monga is an outstanding stone expert. If you can come to Chicago, we can provide help with prevention of more stones. Our coordinator can make arrangements: 773 702 1475. Regards, Fred Coe
I have MSK and can’t seem to find a doctor who understands. I’ve suffered with pain for the last 10 years and no one gets it. I have been to Mayo Clinic and brought in this research and was looked at as if I had 4 heads. ER doctors mistreat me on a regular basis. I have gotten to the point of rather suffering then seeking help. My infections are more frequent and my “colic kidneys” has been hurting a lot more then usual. I am a wife, a mother of 3 and work full time and by the time I get home my pain has me worn down. Over the years I have had to learn to deal and tolerate high levels of pain and because of my treatment by the medical professionals I have panic attacks at the thought of seeking relief.
As mentioned in this research MSK is often misdiagnosed, when I brought this up to the doctors and asked for a reevaluation of my condition in hopes that it’s something else that might be fixable I got the run around and nothing was done. I am not one who fits into what the textbooks say is normal. If there is anyway someone with your research center can help me I would greatly appreciate it. I’m at the end of my rope with dealing with people who don’t want to listen or even try to understand. I have done everything the doctors have told me I need to do with regards to diet and water consumption, so I am doing my part to keep myself as healthy as possible.
I want to thank you in advance for your help in this and even if nothing comes from this I thank you for listening.
Sincerely,
Andrea Domeij
Hi Andrea, I have no knowledge of the details, but if you know the composition of your stones and will tell me I can make some suggestions. If you wish to see us at University of Chicago, our clinical coordinator is at 773 702 1475. Regards, Fred Coe
I have been told that I have both calcium, and calcium oxalate stones. Both kidneys are affected but my right side gives me more problems. I have also been told that my left kidney and ureter are smaller then they should be and I am RH negative. I am allergic to IV contrast so it does make broader testing difficult. Thank you for getting back with me. My husband and I will have to discuss the affordability of a visit to your center since we live in Florida.
Hi Andrea, By ‘calcium’ I believe you mean calcium phosphate stones. As I see it there are two problems. One is urological management, and for that rather than our center I would consider – if possible – such physicians as Dr James Lingeman in Indianapolis, Dr Manoj Monga at Cleveland Clinic, Dr Glenn Preminger at Duke University or Dr Ojas Shah Columbia University in NY (I am aiming along the east of the US and not too far north). There are other surgeons of exactly equal skill but this is a good initial list to consider. There have been sufficient problems to warrant a second opinion. We are skilled in prevention, but I think the urological issues are predominant right now. Regards, Fred Coe
I live in Indianapolis and what luck that was, because Dr. James Lingeman performed my kidney stone surgery in December of 2010. He was excellent. They could not tell me how many stones they removed from my kidneys because there were so many of them. I had started having kidney stones and an x-ray and another x-ray with contrast diagnosed me. I have had very little trouble since my surgery. Now I will have a tiny stone pass every year or so and it usually takes about 20 minutes to pass from start to finish. Otherwise I live pain free. Dr. Lingeman is sort of the “rockstar” of the kidney world, LOL. He was great and I highly recommend him!
Hi Ann, He has been my research colleague and is indeed a superb surgeon. Fred
I was diagnosed at 18 years of age with MSK and am currently 42. I can not find a urologist that can/will help me. I’ve had lithotripsy 19 times with uncountable stent placement. My right kidney is my trouble side, but there are stones in the left as well. I live in the Tampa, Fl area, any recommendations?
Hi Valerie, There is a USF medical center in Tampa but I do not know any of the physicians there. Even so, it is likely to be a reasonable place to try. In gainesville, admittedly a bit far away, there is an outstanding stone expert, Dr B Canales. I hope one of these proves useful to you. Regards, Fred Coe
I am writing on behalf of my daughter (age 24) who has MSK and nephrocalcinosis in both kidneys. She produces calcium oxalate and uric acid stones. Furthermore, she suffers from Interstitial Cystitis, endometriosis (including on the ureter), IBS, fibromyalgia, and other autoimmune disorders. We are in central Wisconsin and are having a hard time finding a urologist who understands MSK and how to help her. Do you have any suggestions? Thanks!
Hi Tracy G, Uric acid stones are not found in MSK. A search of Pubmed for ‘MSK AND uric acid stones’ yielded no articles. Calcium oxalate stones are the usual stones, so perhaps she has those with MSK. As the article makes clear, a lot of ‘MSK’ is really something else, so even that diagnosis is not clear. Your daughter would profit from evaluation at a stone center with 24 hour urine and blood testing. The university medical school in Madison WI has an excellent stone program. Some physicians at Medical College of Wisconsin in Milwaukee also are reasonably good at this problem. Looking at a map, Madison would seem most reasonable. Dr Stephen Nakada is the best physician there. I know him and believe he is outstanding. Regards, Fred Coe
My disease has tormented me for 16 years. I am 31 years old, I’ve had over 200 catscans, I’ve had to date 88 kidney surgeries. I create calcium oxalate and calcium phosphate stones. Every doctor will tell you there’s no pain unless it’s obstructing, this is wildly false. I wake up everyday like I have the flu and have been stabbed in my side.
I’ve taken all the medicine citrates to slow the development of stones or try to “melt ” them. Nothing has helped, changing diet hasn’t helped
Nothing helps. Studying a true msk group is hard I get that, but we shouldn’t suffer due to lack of knowledge by doctors. We know our bodies, trust the patient.
Hi Amanda, 88 kidney surgeries is astounding, and too many. You simply must seek alternatives, ideally at a stone center. If you say where you live I could try to identify one for you. Regards, Fred Coe
I’m located in Sacramento CA and I want to find a doctor that knows about MSK because I’m in pain all the time my kidneys feel full and sharp pains. But all doctors tell me the kidneys don’t feel pain only if there is a blockage. I have calcium stones the common ones and nephrosis
Hi Karen, You are nearest to UCSF, and Dr Marshall Stoller is the most interesting and intelligent physician there who studies kidney stone diseases. I strongly recommend him. Regards, Fred Coe
Please recommend a stone center in OKC or Dallas. I need help please
Hi Charlette, The University of Texas, Southwestern Medical School in Dallas has a superb kidney stone program, and you would be best off going there. I know the physicians, and have great respect for them. Regards, Fred Coe
How about a specialist in the Atlanta area.
Thanks.
Hi Frank, I looked at the faculty at Emory and found Dr Jeff Sands who I know and believe is a brilliant physician and scientist. I am not sure if he is practicing kidney stones prevention presently but he surely will know who is the best for you there. Regards, Fred
Can you recommend any knowledgable urologists in the Central Florida region? My wife has seen a number of urologists in the area who have largely been useless. The last one was arguably negligent (prescribed the wrong medicine, told her she had no stones and she passed a giant one 2 days later, took no responsibility for any of that), but the CT he ordered noted MSK. We’d like to see an expert, we’ll travel too if we have to. Thanks for the help!
Hi Randy, At Florida University Gainesville there are splendid kidney stone experts. Call them, make an appointment and go there. Dr Segal specializes in vascular biology and the kidney but is chief of nephrology and an email to his office will be the easiest way to get to the right person for stone prevention and stone surgery. You can say I sent you – via the web. Regards, Fred
Thank you Fred!
Mr Coe
I work in pain management and had a patient today with MSK “spongy kidney disease” I have been researching all evening trying to determine the best plan of care do you know where I could find treatment options. I know she is in pain daily I’m just not sure treating with opioids is appropriate. Thank you
Hi Sherry, Pain with non obstructing stones is a national problem and not solved. Most experts think it is from renal inflammation from the stones, but no one has proved it, and the role of surgery is untested. Everyone is concerned about what to do, and no one really has a proper answer. Regards, Fred
I live in central Illinois and have would like to find a stone/kidney center. Thanks you!
Hi Marly, I think central illinois is not too far from Indianapolis. Dr James Lingeman is outstanding and works in that city. Regards, Fred Coe