Diagnosis of MSK is Increasing
Urologists and nephrologists specializing in the treatment of kidney stones seem to encounter patients with medullary sponge kidney (MSK) far more often than one would predict given the fact that this disease affects less than 0.5-1% of the general population.
One potential explanation is the high frequency of stones in such patients, nearly 70%. Stones call attention to themselves. Even so, referrals for MSK seem to be occurring at ever increasing rates, out of proportion to the prevalence of the disease.
Another explanation is that we can see more because of dramatic improvements in CT scanners and endoscopic equipment we use for stone removal.
Latest generation, thin slice CT scans can isolate tiny stones as small as a millimeter in size. Meanwhile, modern flexible endoscopes not only visualize every crevice of the renal collecting system but are able to do so in high definition. Consequently we can identify previously unrecognized variations in the appearance of stone forming kidneys, of particular interest here nephrocalcinosis on CT and tubular plugging on endoscopy.
But diagnostic capabilities may be progressing faster than our ability to comprehend the significance of what we see. As a result, one can misclassify patients as having MSK when the correct diagnosis is another more common finding such as nephrocalcinosis or tubule plugging.
For example, a urological surgeon performing ureteroscopy with a modern high resolution digital instrument notices “hundreds of tiny stones,”, “abnormal papillary architecture” or “stones located under the urothelium” and proceeds to label the patient with MSK. Or, a patient with urologic symptoms such as renal colic, recurrent urinary tract infections, or microhematuria has a CT scan showing ‘nephrocalcinosis’ and is labeled as having MSK.
In both instances, the true likelihood of actually having MSK is, by a recent small study, only 4/15 (25%), but physicians are not generally aware of the differences between MSK, nephrocalcinosis, and tubule plugging because these are new areas of knowledge which have not been proliferated widely.
This article is one way we hope to make the diagnosis of MSK, a unique and complex disorder of renal development, clearer for physicians and their patients.
What Is MSK?
Our collective understanding regarding the development and pathophysiology of MSK is rather sparse even though G. Lenarduzzi first described it in 1939.
The Cause of MSK
The exact mechanisms that produce MSK are unknown. It is believed to be a result of abnormal renal development in utero. More specifically, scientists believe the ureteric bud – which will give rise to the ureters – interacts abnormally with the metanephric blastema tissue in the embryo which will produce much of the kidney substance.
There appears to be a genetic component to the disease. Recent evidence is that about half of patients diagnosed with MSK will have at least one relative with some degree of similar affliction. This kind of familial clustering can suggest an autosomal dominant gene expression or the actions of multiple genes giving that impression. The review of the above link is an excellent recent treatment of the matter of development and genetics which we highly recommend.
The Anatomy of MSK
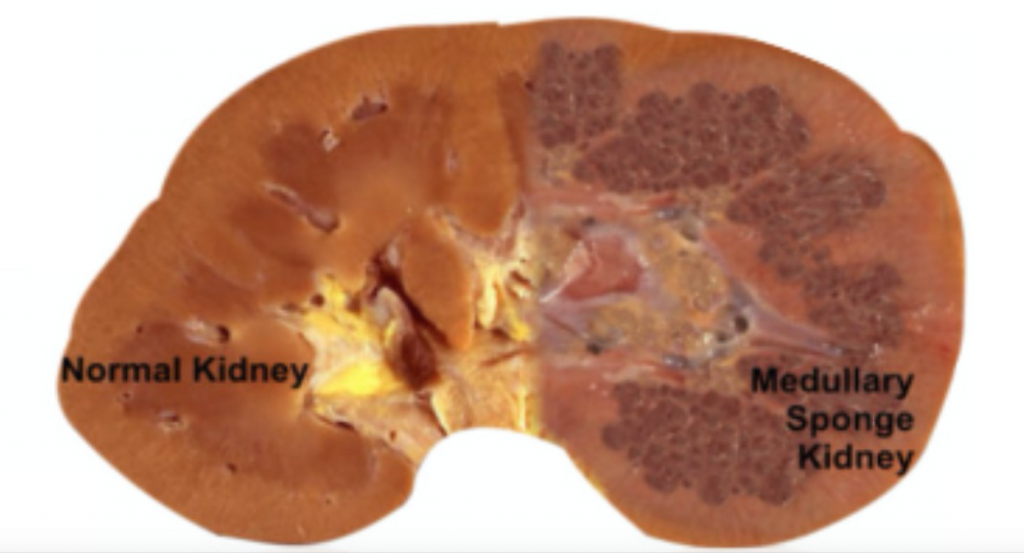
MSK, as its name implies, is characterized by sponge like, cavitary regions within one or both kidneys (Figure 1).
Figure 1 – A normal appearing kidney (left) compared to MSK kidney (right).
More specifically, the dilations occur in the inner medullary (precalyceal) collecting ducts. These collecting ducts are the terminal region of the nephrons, the individual functional units of the kidney.The inner medullary collecting ducts (IMCD) have the job of delivering urine to progressively larger ducts (ducts of Bellini) that deliver the final urine out of the renal papilla into the minor calyces (Figure 2) which connect into the renal pelvis and thence into the ureter to the bladder.
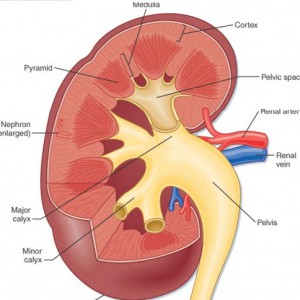
One way to think of the IMCD is as a collection of streams merging and forming a river (duct of Bellini) which leads to a delta (minor calyx) and then a lake (major calyx) and ultimately an ocean (renal pelvis) (Figure 2).
Figure 2 – Anatomic depiction of kidney and collecting system
The IMCDs are not visualized in Figure 2 but if you scan down to Figure 3 just below several human nephrons which were microdissected from an MSK kidney show what is really wrong with them.
In MSK, some IMCD are dilated markedly and have outpouchings (cysts): blind sacs which begin at the IMCD lumen but go nowhere – like a hallway someone walled off at one end. It is at the ends of these hallways one finds the stones, free floating and probably trouble. Other IMCD are not dilated and do not have cystic outpouchings.
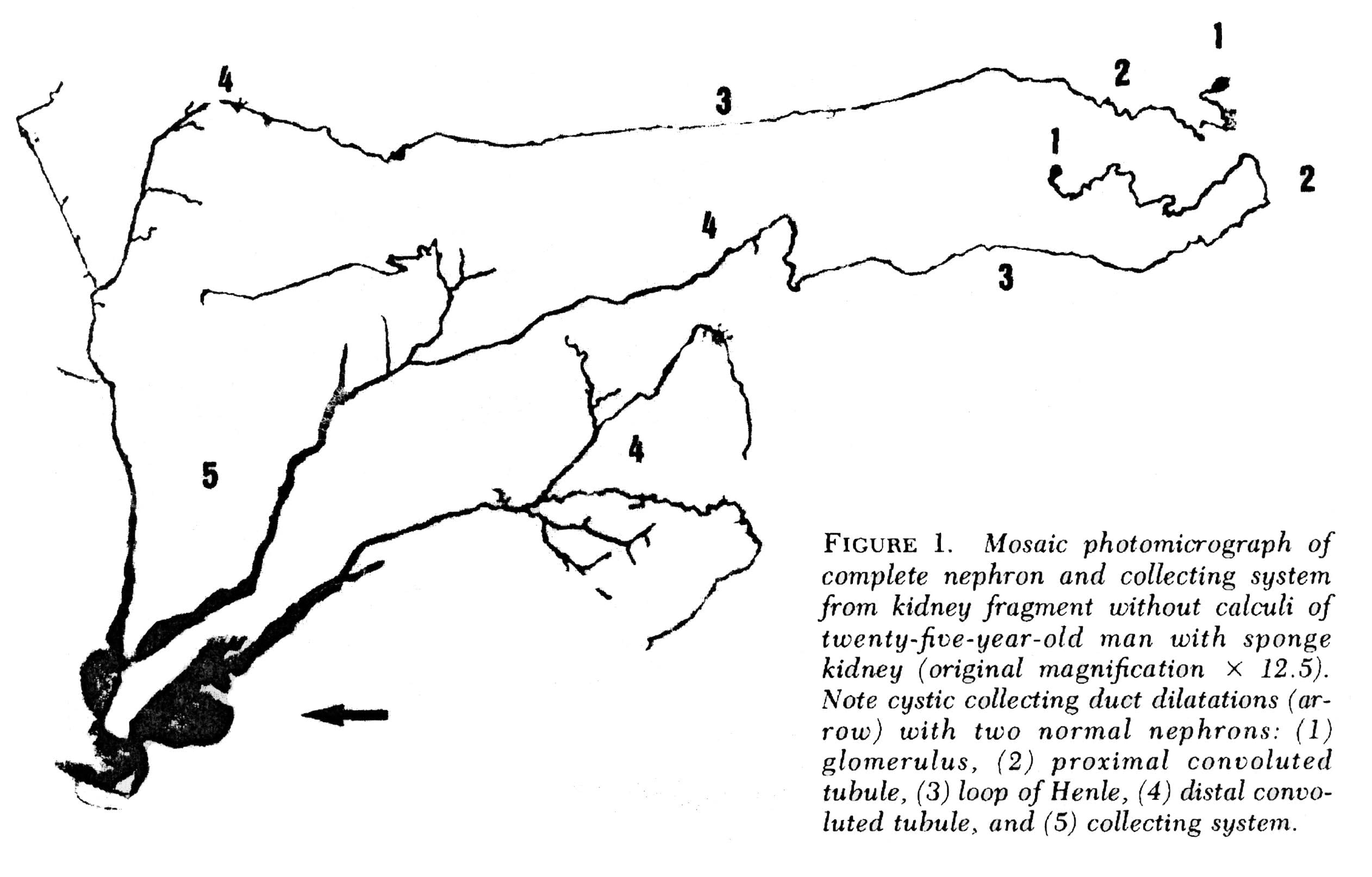 Figure 3 – Microdissection of complete nephrons from MSK. Irregular dilation of the IMCD is present. Cystic outpouchings are present, of varying sizes. The blind ends are obvious. It is in these cysts that tiny stones are found.
Figure 3 – Microdissection of complete nephrons from MSK. Irregular dilation of the IMCD is present. Cystic outpouchings are present, of varying sizes. The blind ends are obvious. It is in these cysts that tiny stones are found.
Quite apart from the IMCD dilatation and cysts, the kidneys of MSK have two other abnormalities which mark it as a specific disease. Those IMCD which are not dilated nor cystic have a multilayered epithelial lining, whereas a normal undilated IMCD lining is one cell layer thick. The interstitial cells of the renal papillum – the cells between the tubules and vessels – are more numerous than in normal kidneys, and have an immature appearance much like is seen in fetal kidneys.
Why Stones Form in MSK
Elsewhere on this site we have pointed out that supersaturation is a force, a source of energy directed at forming solid phases such as stone crystals. The kinetic retardants in urine, which include citrate, stave off crystallization but can never prevent it: A supersaturated solution will eventually collapse into two phases, crystals and a residual solution precisely at the solubility point, devoid of extra free energy.
The stagnant flow as a result of the dilated MSK IMCD, and particularly the static conditions in the fluid filled blind ended cysts, are the probable reason those innumerable tiny stones form which end up packing the ‘sponges’ with masses of crystals. How MSK patients produce larger stones, big enough to block the ureter is unknown. It is not true that MSK patients have remarkably high urine supersaturations or other physiologic abnormalities such as hypercalciuria and hypocitraturia. Possibly the tiny stones somehow leave their cysts and enter the urine where they act as nucleation centers.
Other Associations
Other common associations with MSK include urinary tract infection, microscopic and gross hematuria, and impaired renal function. Perhaps the stagnant flow in dilated IMCD and particularly in cysts, predisposes to infection. But since the papillae are abnormal in other ways it seems likely that these intrinsic abnormalities themselves must be clinically important, and more work needs to be done on the problem.
Making the Diagnosis of MSK
Of course, when we speak of what is wrong in the MSK kidneys, and how it affects people, we base everything on knowing that a given patient has MSK. If you have a kidney from such a patient and can show the dilated IMCD, the cysts, the tri-layered IMCD epithelium, and abnormal interstitial cells, diagnosis is certain. But what can we do when we are dealing with a patient?
Radiological Studies
Intravenous Urography
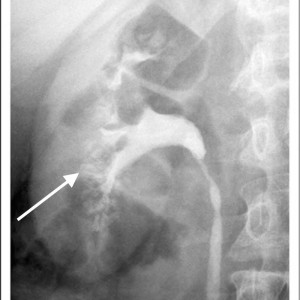
Historically, the diagnosis of MSK has been made on intravenous urography (IVU). Radiographic contrast is administered and x-rays of the kidneys, ureter, and bladder are taken periodically as the contrast is absorbed and later excreted by the kidneys through the urinary tract.
The delayed phase image is essential for diagnosis. This is when contrast material fills the masses of dilated IMCD and cysts which make up the sponge.
The masses of dilated IMCD filled with contrast material produce a characteristic ‘papillary blush’ which appears like flames on the outer edges of the papillae. When particularly large it can mimic a bouquet of flowers peripheral to the collecting system.
Figure 4 – IVU image of medullary sponge kidney. The arrow designates the papillary blush in the mass of dilated IMCD space.
CT Scans and Other Imaging
Over the past 10-15 years, noncontrast CT scans have replaced IVU as the imaging method of choice for stone formers. While these scans are more sensitive in detecting small stones, the lack of contrast limits the ability to accurately diagnose MSK and has raised concerns regarding the potential for under-diagnosis of this disease.
CT does have the capability of making this diagnosis when contrast is given and CT urography is performed; though this is not used as a first line choice for stone imaging and is generally reserved for specific indications such as hematuria and concern for urinary tract injuries.
Figure 5 – Demonstration of papillary blush (small arrows) on CT urography for patient with medullary sponge kidney.
Use of other imaging modalities have been investigated as well though they have proven suboptimal in their diagnostic capabilities. Ultrasound has poor sensitivity to detect dilation of the collecting ducts and MRI has the potential to delineate detailed renal anatomy but can not detect stones or calcification.
High Definition Endoscopy
State of the art high definition endoscopes have allowed investigators to make observations at the time of renal endoscopy correlating the appearance of the renal papillae and collecting system to specific types of diseases and metabolic derangements associated with stone formation. Because endoscopy is now being performed as a common and often preferred way to manage stones, this kind of detailed imaging of kidneys will be available more and more in the course of regular patient care and permit physicians to diagnose the exact kinds of disorders in the kidneys of stone formers.
Medullary sponge kidney in particular has an entirely unique appearance unlike any other type of stone related disease, making endoscopy a particularly exacting diagnostic procedure. Detailed anatomic descriptions from twelve such patients each with evidence of MSK on biopsy were recently described by Evan et al.
The Papillary Malformations Seen Via Endoscopy
In stone formers the papillae often appear abnormal, a concept that merits its own post and which we can only briefly summarize here.
Plaque
The renal 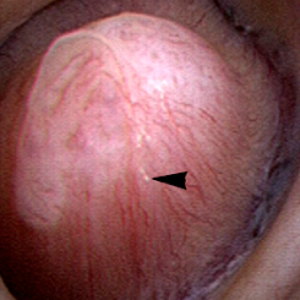 papilla is the anatomic subunit of the kidney where the IMCD merge together into the terminal Bellini ducts which empty into the minor calyx. Normally, it should have the appearance of a smooth walled mound or mountain without much if any calcification (plaque) along its surface. The link is to a detailed post about plaque by Dr Andrew Evan.
papilla is the anatomic subunit of the kidney where the IMCD merge together into the terminal Bellini ducts which empty into the minor calyx. Normally, it should have the appearance of a smooth walled mound or mountain without much if any calcification (plaque) along its surface. The link is to a detailed post about plaque by Dr Andrew Evan.
Figure 6 – Healthy appearing renal papilla with a minimal amount of Randall’s plaque (arrowhead).
Ductal Plugging
Another common abnormality identified in many papillae at the time of endoscopy are plugged ducts. The physiologic mechanisms for this process are currently unclear; 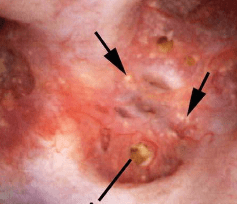 however, we believe it is a reflection of injury that begins a potentially disastrous chain of events for stone formers.
however, we believe it is a reflection of injury that begins a potentially disastrous chain of events for stone formers.
Figure 7 – Abnormal papilla in a patient with severe ductal plugging. Yellow mineral deposits (arrows) can be seen protruding from dilated ducts of Bellini.
Our present assumptions are that once crystals begin to form within a duct, they damage the lining cells and the duct loses its ability to make acidic urine. This in turn raises the local pH level and leads to the growth of more calcium phosphate mineral deposits which are favored by high pH.
Unclear is what begins this process. Since these ducts contain fluid which is very close in composition to the final urine, we suspect it is high supersaturation with respect to calcium phosphate. This occurs in those patients with both high urine calcium excretions (hypercalciuria) and higher urine pH levels – above 6.2. Such patients often form stones high in calcium phosphate composition and plugging is strongly associated with formation of such stones.
The mineral deposits subsequently grow and we believe can even act as a nidus for stone formation. The corresponding papillae can look markedly abnormal and the dilated ducts are easily evident. Remnant dilated ducts left behind after the mineral is spit out or surgically removed (Figure 8) show dilation without the mineral plug.
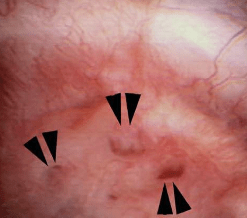 Figure 8 – Evidence of abnormally dilated ducts (arrowheads) at the surface of a papilla.
Figure 8 – Evidence of abnormally dilated ducts (arrowheads) at the surface of a papilla.
MSK
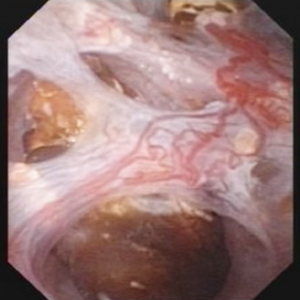
The findings in MSK are comparable in some ways to ductal plugging; however, rather than the papillae having one or several abnormally dilated ducts, the entirety of the papillum is markedly abnormal.
Therefore MSK and plugging type papillae look remarkably different.
The MSK papillae are excessively round, enlarged, and billowy (Figure 9).
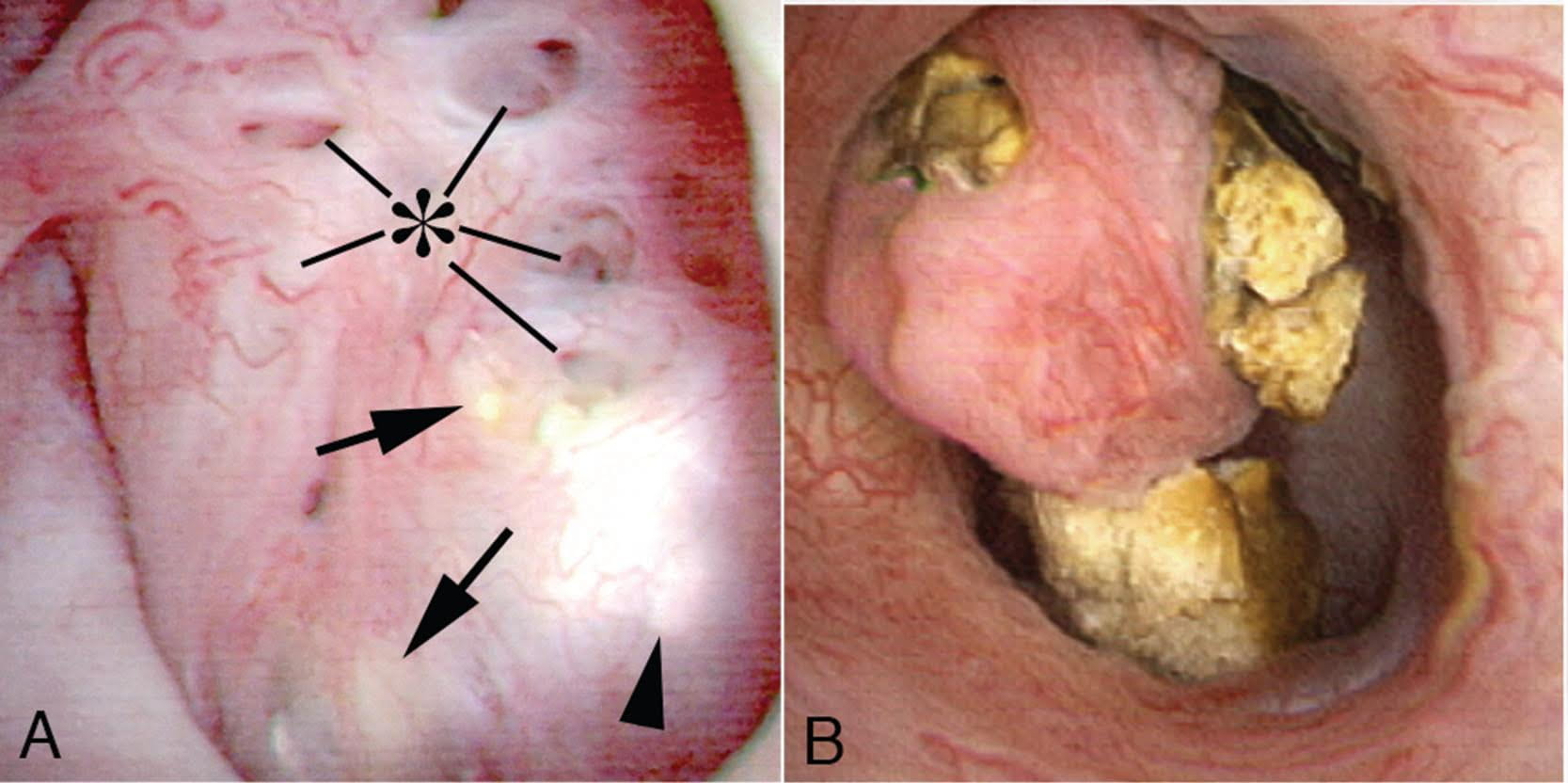 Figure 9 – A papillum in a patient with medullary sponge kidney. The papillae are rounded and enlarged with a billowy appearance. The papillary tips are blunted. No other kind of papillary disease is known to present this appearance which is therefore pathognomonic of MSK. Panel a shows dilated Bellini duct openings at asterisk; the arrows show yellow plaque – plugging of IMCD completely separate from the stones which fill dilated IMCD, the arrowheads show traces of white plaque. Panel b shows the billowy papillum with a blunted tip surrounded by calyceal stones.
Figure 9 – A papillum in a patient with medullary sponge kidney. The papillae are rounded and enlarged with a billowy appearance. The papillary tips are blunted. No other kind of papillary disease is known to present this appearance which is therefore pathognomonic of MSK. Panel a shows dilated Bellini duct openings at asterisk; the arrows show yellow plaque – plugging of IMCD completely separate from the stones which fill dilated IMCD, the arrowheads show traces of white plaque. Panel b shows the billowy papillum with a blunted tip surrounded by calyceal stones.
In the majority of such cases, these changes are seen diffusely throughout each kidney, though segmental sponge findings are present in a minority of patients.
The differences in appearance are well demonstrated in the post by Dr. Evan and the following video. With ductal plugging the bulk architecture of the papilla is intact though many ductal plugs are seen. Note the way the ductal plugs are adherent to the lumen.
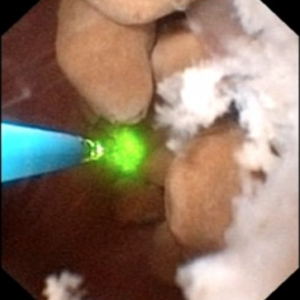
In MSK on the other hand, the papillary architecture has and unique, billowy appearance with massively dilated ducts and freely mobile stones within them. The following video is from a patient with MSK. A duct of Bellini is massively dilated and numerous tiny stones which are free floating pass out of it during the visualization as the opening is enlarged with a laser. You can see stones bouncing within the duct because of movement of the irrigation fluid.
Clearly neither papillum is “normal” and one can imagine the tendency to misdiagnose a plugging patient as a MSK patient unless the two patterns are clearly in one’s mind.
The ductal deposits themselves are an important clue. In all plugging diseases but cystinuria ductal mineral plugs are fixed within the ducts because the crystals adhere to the lining cells and often destroy them. As the lining cells are destroyed crystals fix themselves to the basement membranes, the collagen shell on which the lining cells once grew. Inflammation follows such injury with scarring and loss of the tubule segments. Deposits therefore never float free from a dilated duct except in cystinuria and in MSK. Cystinuria is usually diagnosed directly from stone analysis and urine cystine screening.
Perhaps because the tiny stones in MSK do not attach to the epithelium of IMCD there is no evidence of cell injury or inflammation, in marked contrast to all of the plugging diseases. Even in cystinuria injury occurs, not from the free floating distal cystine plugs but from calcium phosphate plugs which form in the IMCD.
Stones may cause pain in MSK despite the lack of ureteral obstruction and inflammation and cell injury. Possibly distention of the dilated ducts by masses of tiny stones could be a factor. Consequently, laser unroofing has been postulated as a potential treatment option in both disease states: those with plugging and MSK.
The video may not make it easy for everyone to visualize the stones and cavities of MSK. The 4 still pictures below show much the same thing for clarity.
Figure 10 (a-d) – Example of laser unroofing of sponge cavity full of freely floating stones. The massively dilated MSK bellini ducts are seen in Panel a; the white speckles at 9 o’clock are tiny stones in dilated IMCD or cysts. Panel b shows a holmium laser fiber being used to open dilated IMCD or cysts. Panel c shows masses of tiny stones free in dilated IMCD or cysts which float out as the surface is incised with the laser. In panel d, the remnant sponge cavity can be seen now free of stones.
Nephrocalcinosis and MSK
Strictly speaking, nephrocalcinosis refers to the presence of calcium deposits in the kidney tissue. Of course, this includes ductal plugging and the masses of tiny micro – stones inside cavities produced by numerous dilated IMCD in MSK. However, the word ‘nephrocalcinosis’ is also used as a radiological diagnosis which is far less specific.
Limitations of Radiology
When radiologists speak of nephrocalcinosis they can mean large numbers of calcifications within the collecting system or kidney tissue, because they cannot differentiate reliably between tissue calcifications and stones. When urologists speak of nephrocalcinosis seen during high resolution endoscopy they can specify if it refers to tissue calcifications, stones, or both, and will reserve the term for that component arising from tissue calcifications.
MSK is one of several disease states that is commonly associated with extensive nephrocalcinosis observed by radiologists. Other common conditions are stones caused by renal tubular acidosis and primary hyperparathyroidism. Calcium phosphate stone formers without any systemic disease can also produce sufficient combinations of ductal plugging and stones that nephrocalcinosis is diagnosed radiologically.
In a recent study of 67 idiopathic calcium stone forming patients undergoing percutaneous nephrolithotomy, rates of nephrocalcinosis ranged from 18-71% depending on the type of associated stone.
Figure 11- X-ray example of patient with MSK affecting the left kidney. Extensive nephrocalcinosis is seen.
Because radiographs cannot reliably distinguish tissue calcifications from stones adjacent to tissues, the very word ‘nephrocalcinosis’ needs to be re-defined.
In particular, the situation with respect to diagnosis of MSK has worsened as radiological techniques have changes. When IVU was the first line imaging modality for stones, contrast enhanced urographic phase imaging gave additional clues to MSK – the papillary blush illustrated in a prior section.
Nowadays since a single non-contrast CT series is all that is typically performed, the papillary blush effect cannot be seen, and diagnosis of MSK must rely more on the presence and pattern of nephrocalcinosis itself, which is not very specific to MSK. This means that the diagnosis of MSK by radiology has become unreliable.
The Power of Endoscopy
Differentiation of Nephrocalcinosis from Stones
During endoscopic procedures, stones and tissue calcifications can be directly identified and told apart. For example, in the images below, some of the calcifications were identified as stones. Others were tissue calcium deposits such as plugging or extensive plaque.
This has led to the notion that kidneys should only be labeled as having nephrocalcinosis once confirmed visually on endoscopy.

Figure 12 (A-C) – Evidence of increasing degrees of nephrocalcinosis confirmed visually at the time of percutaneous nephrolithotomy. In each image a nephrostomy tube (not calcification) is depicted by an arrow. The remainder of the images have increasing degrees of calcification (bright white) within the kidney. Ignoring the nephrostomy tube, one can clearly appreciate a minimal but very present degree of accessory brightness (calcification) in panel A, a moderate amount in panel B and a severe amount in panel C.
Diagnosis of MSK
Of course, all of the problems of nephrocalcinosis are compounded when it comes to MSK. Stones and tissue mineral are easily mistaken for one another in CT scans, and ‘MSK’ affixed as a label to patients who do not have it. Endoscopy will easily identify the remarkably abnormal papillary shapes and dilated sponges, so MSK patients are properly diagnosed.
Tips for diagnosing MSK
1) Confirmation with flexible renal endoscopy can make a definitive diagnosis in patients suspected to have MSK and can be diagnostic as well as potentially therapeutic in terms of stone removal.
2) Consider urographic phase imaging either with IVU or CTU to confirm MSK suspicion in cases where renal endoscopy is not clinically indicated.
3) MSK should not be confused with ductal plugging as these are distinct clinical entities.
4) Nephrocalcinosis is more common than previously appreciated and does not necessarily indicate systemic disease or the specific developmental disorder of MSK.
A Final Word on Treatment
MSK is a true disease and deserves more attention and research efforts to help clarify its etiology and optimize treatment strategies. Because diagnosis by CT scanning is unreliable, the condition is easily overdiagnosed, a problem which leads to many kinds of confusion, clinical and research.
Alternative diagnoses to MSK, such as severe ductal plugging, are not benign and require their own treatment in order to prevent progression. Very often patients with plugging have multiple and severe abnormalities of urine chemistry which can be treated with diet and medications. Proper classification of patients is therefore especially important as different disease states may require unique treatment strategies.
In the event that an accurate MSK diagnosis is made, the tendency to give up on treatment and surrender to the inherent challenges of the disease should be avoided. In fact, these are the patients where metabolic evaluations and attempts at stone prevention are most critical.
Moreover, just because many of these patients tend to have extensive nephrocalcinosis on imaging does not mean they can’t form symptomatic stones in the collecting system as well. In fact, for such patients the clinical history is especially important as visualizing new stones in the setting of extensive nephrocalcinosis can be quite challenging.
Oftentimes when there is a high index of suspicion based on clinical factors, the optimal approach is ureteroscopy as this can be both diagnostic and therapeutic.
That being said, realistic surgical goals should be established. Clearing all stones from such kidneys is rarely feasible, though unroofing those pockets closest to the collecting system or largest on CT imaging offers a good place to start.
MSK is a complex and poorly understood disease that can manifest uniquely from patient to patient. In that respect what works for one person may not be appropriate for another and treatment strategies should thus be organized on a patient to patient basis.







I live in the four corners area. No dr seems to think I’m in pain and I can’t get relief 🥺
Hi Stacie, Your best is in the University of Colorado health system, but I looked at both medical schools – colorado and ft collins and not one professor listed kidney stone prevention. Even so I would call either and ask. Regards, Fred Coe
Hoy le diagnosticaron MSK a mi esposo el doctor solo dijo tienes esta enfermedad no te preocupes te veo en 6 meses y tenemos tantas preguntas y mucho miedo vivimos en NY gracias
Hi Nivram, I do not speak Spanish, but I get the idea. If you are in NY Dr David Goldfarb at NYU is an authority on MSK. Regards, Fred Coe
What recommendations for a urologist or nephrologist do you have in Colorado? Thanks
Hi, I would use the university medical school. Strangely I found none listing kidney stones! But surely some urologists there specialize in that problem. Regards, Fred Coe
Hello Dr. Coe, are there urologists who practice according to your teaching in the Dallas area? I was diagnosed with MSK in January 2020, both kidneys are full of calcium oxilate stones.
thank you,
Janice
Hi Janice, At UT SW in Dallas, there are outstanding physicians who I consider experts in stone disease. Perhaps Dr Peggy Pearle is a good person to start with. She is a brilliant surgeon and researcher. Feel free to let her know I mentioned her to you. Regards, Fred Coe
Hello Doctor,
What is Severe Bilateral Medullary Calcinosis.m.i recently went to the ER for heartburn presenting as chest pain and by happenstance the scan revealed this with my Kidneys. Can I reverse this? Will herbs and diet help? What kind of doctor do I need? It sounds very serious.
Hi E R, The condition means crystal deposits in the deeper regions of your kidneys and should be evaluated carefully. MSK is possible. Likewise it can arise from multiple other causes. It is unsafe for me to speculate here in the absence of information, but I would begin with a full evaluation for stone forming conditions – here is a good start. But I am sure your physicians are quite concerned as to cause, and are already working on a diagnosis. Herbs and diets are not appropriate, you need to know what is causing the problem and have that treated. Your personal physician is a good place to start. Regards, Fred Coe
Hello i am in florida and looking for a specialist in msk can you recomend any
Hi Stephanie, The only group I can personally recommend is at University of Florida, Gainesville – they have a terrific kidney stone program, and MSK is in their line of expertise. Regards, Fred Coe
I have been diagnosed with MSK and have been taking PPI (nexium specifically) for over 5 years now. I am concerned about the health of my kidneys. I recently had an ultrasound when I was pregnant with my daughter that showed a lot of built up fluid. Should I see a nephrologist? Any recommendation on specialists in northwest Arkansas? Thank you!
Hi Rebecca, The PPI is not ideal long term as you note and your physicians can find alternatives. I do not know where the fluid was nor what your physicians meant by it. When pregnant the urinary system dilates so perhaps that is their meaning – a normal part of pregnancy. If your kidney function – eGFR calculated from serum creatinine – is normal and you have no excess protein in your urine I cannot imagine why you would need a nephrologist. Ask your physicians. As for MSK, as the article says it is often over diagnosed. You have some form of stone disease and should be fully evaluated for cause and treated. Here is a good place to start. Regards, Fred Coe
I was diagnosed with MSK back in 1978 when I was only 16yrs old. I had an IVP test done. I am now 56 and I am really started to have problems with calcification in my left kidney that has been in there for over 20 yrs. I recently found out that I also have 1 in my right kidney but it is 1cm. I am trying to see a kidney dr to get some kind of relief. My left kidney doesn’t hurt so I’ve left it alone. I don’t have any burning or pain with a UTI until my back starts hurting. Some of my family members have it. An aunt and uncle both got cancer of the urinary tract from kidney to bladder. My right kidney is giving me problems and also right under the right side bottom rib cage has had sharp pain. The CT scan showed that everything was good but 1 cm kidney stone in the right kidney.
Hi Pamela, MSK is often overdiagnosed but certainly you have some important problem with stone formation. Be sure you have been fully evaluated as to the cause of the stones – prevention can matter a lot to avoid even more deposits in your kidneys. As to the pain, your urologist needs to decide with you if surgery will help, and especially if there is infection causing symptoms. Regards, Fred Coe
I have MSK and have have over 20 kidney stone surgeries and 4 within the past 8 months. Some of the surgeries require a stent in the ureter which cause great discomfort. My urologist says I can take Aleve for the 4 days of having the stent. My GP doesn’t advise taking Aleve due to MSK. It there any medical suggestions or findings on taking Aleve short terms with MSK. Thanks
Hi Marlena, Aleve does not have a bad record in relation to kidney damage, so it is not necessarily worrisome. But your physicians are totally responsible for your care and may know things about your situation that make this drug inadvisable – I would use their advice. In this case your urologist and PCP seem to disagree, and given that fact, I would ask them to come to some joint decision. I do not mean to be vague or evasive, it is just that drug use after surgery is a very complex matter, and I have no real knowledge of your personal situation. Regards, Fred Coe
Hi my daughter is 24 diagnosed with MSK. Can you please help with finding a Dr that specializes in this. We have called many and most are not aware s of this disease. We are in Greenville South Carolina. She has been throwing up and excruciating pain for 4 days now. They finally gave her fluids at the hospital yesterday. Put her on dissolvable Zofran which isn’t helping because she is constantly throwing up. I would appreciate any and all help you can give me. We have ran out of options now. Thank you so much.
Hi Linda, I do not know any particular physician in your state. However you do have the University of South Carolina Medical school and here is the head of the kidney disease section there. He is highly trained and certainly can point you to the right person at his school. I would call his office, say I sent you, and see who he has to offer. Regards, Fred Coe
(This is rather breathy, and I apologize)I have been searching everywhere (literally), to try and find anyone that might possibly have any answers, resources, or anything really.
Backstory-my issues started at the age of 16 (now 34), and I was not diagnosed until I was 27. For me, it started with a cyst on the left kidney, a kidney stone coming from the right kidney, and a cyst that had burst on my right ovary. In the 18 years since I have had surgery (both lithotripsy and Ureteroscopy) approximately 5 times; and around maybe 4 or five kidney infections between 16 and 33. Last year at the age of 33, I experienced my first complication; I almost died from Urosepsis.
Before the surgery that caused my Urosepsis, I had a count of about 40 stones between my two kidneys; he did clear the two I was moving and proceeded to clear my left kidney-and I got septic 36 hours later. (I know this is a lot and you’re probably wondering why I’m so winded-I’ll get to it). Fast forward to today, exactly one year from my two week stay in the hospital, I have had SIX Kidney infections; and recently was told by one doctor that I was moving another stone. Because of the COVID-19 pandemic, I had to fight to get into the urologist; (the urgent care doctor did start the normal treatment for a stone) the night before they called to set up the appointment I started showing signs of Urosepsis again (mainly the horrific pain). They scheduled CT, and when I went to the Urologist they told me there was nothing they could treat; even though I explained to them the pain. After the appointment, my urine was straight blood, my legs, hands, and feet were swollen; and I have a multitude of other symptoms as well-and I can’t get anyone to put any pieces together but me. Frankly, I’m getting tired of fighting; and I have a new found respect for people I work with that have chronic illness.
My question with all of this is-is there any chance this has progressed into something more than just MSK; and is there anyone in Iowa that you could recommend?
I know that you cannot diagnose or anything of that nature; but I am so desperate for help from ANYONE. None of my doctors are listening to me (except my Ophthalmologist); I need resources, someone who can help me-literally, anything. Is this MSK or something else; or has it progressed? I’m tired of not being able to do anything because I don’t have the energy-or I am just in too much pain.
Thank you, for listening (should you make it through this lol).
Hi Aislinn, Given so many stones, you may have MSK or just massive calcium accumulations in your kidneys. That you have had so many stones is not so rare as I have reported many such patients. You have been infected because of procedures – almost inevitable when one has so many. If you were septic, physicians would have been able to determine it: Sepsis is more life threatening than Covid by far! The best resource in Iowa is the medical school. It is a very fine one. I would make inquiry there for kidney stone expertise. You will have to wait, but quite possibly they will do your initial evaluation via telemedicine – we are beginning to do that here. Regards, Fred Coe
Have you been tested for candida? (It’s a simple urine test but requires a request for it.) If you have had too many antibiotics, you can get it. It happened with me.
I have a question, what types of pharmaceutical therapies have been successful in reducing the amt of calcium excreted into the urine (hypercalciuria)?
The amt has been increasing, and no therapy we have tried appears to be helping.
thank you
Hi Renee, Here is my best article on genetic hypercalciuria – it tells about how it is treated. Here is another that shows the interactions between medications and diet sodium. I believe between them you will have what you have asked for. Please let me know if you need more. Regards, Fred Coe
I was diagnosed with bilateral MSK about 15 years ago (around 22 yrs old). Until 2018 I hadn’t had any major complications except for constant UTI’s and sporadic pain (that’s tolerable). However, starting last year, pain (more in my left kidney) has increased significantly and occurs more often. I’ve had two lithotripsy surgeries (the last one was just a few days ago).
When I explain to my Urologist how much pain im in I feel like im not being heard. I cannot tell you how many times I’ve been told, “it’s in your head” or “you shouldn’t be experiencing that much pain”.
My question is this- How is treating a patient with pain that has kidney stones different than a patient that has kidney stones but also diagnosed with MSK (or is there a difference). Do you have any advice?
Also, do you have any recommendations for a good Doctor or Medical facility in California?
Respectfully,
Regina
Hi Regina, If you have MSK shock wave lithotripsy is not likely to help much. In southern California, Dr Clayman is a famous authority; In Northern California at UCSF, Dr Stoller is brilliant and has a remarkable team. Let me know if one of these excellent specialists helps you. Regards, Fred Coe
I have been dealing with MSK for over 30 years now. After 24 operations and passing hundreds of stones, I figured out how to stop making stones about 8 years ago, (with huge change in diet and bifido bacterium lactis). My difficulty now is that I had an undiagnosed kidney infection that infected the stones and after many too many antibiotics, I how have candida in those stones. Two weeks ago I had my 4th operation to try to remove the infected stones and it was pretty successful. Alas, I still have the Candida infection in the kidneys. Do you have any suggestions? Who are the country’s leading doctors with medullary sponge kidneys? Do you recommend any hospital in particular? My doctor has been great but at this point, he is not solving this issue and I have had fevers, exhaustion and pain for 3 and 1/2 years now.
Hi Carole, If I knew where you lived I could try to identify a place. Perhaps you might want to email me and I can offer suggestions fredcoe@gmail.com. Fred
Hi I was diagnosed with msk 6 years ago but started when I was 16(now 27). I deal with constant pain with fever and nausea with UTI’s every 3-6months. Along with both kidneys being infected. After reading some of the comments I’ve never had to have any surgeries thus far, and I feel now lucky for that. I was wondering if you have any recommendations for doctors here in Arizona. I have kinda given up hope and I am tired of the pain. If you have any advice that would be great. I hope to here back thank you for your time.
Hi Loretta, I found that the University of Arizona planned a stone clinic some time ago and perhaps it is now running. Medical schools are best given so many problems, and I confess to rather little knowledge of who practices in your state. Regards, Fred Coe
Dear Dr. Coe, Thank you for the fine article and your kindness in offering guidance! I would like to give a little synopsis of my diagnosis with MSK so I can know how to proceed with what I am dealing with at present. I am 56 years old, and about 15 years ago I had my first kidney stone that had to be removed by basket retrieval. It was 6mm and determined to be calcium oxalate. About 5 years later, I passed another on my own. I began to have a nagging pain on my right side under my ribs that felt like it continued down to my groin. I thought it was another stone trying to pass, but after finally getting US and CT scan, I was told I indeed had a stone but it wasn’t moving so wouldn’t cause pain, but I was told I had MSK. I dealt with the uncomfortable pain for a year. I moved and went to another doctor whom ordered a CT with contrast, and again I was told I had MSK. Finally, the stone began moving and became obstructing and was again removed by basket retrieval. While there, the urologist did a clean out of my right kidney, confirming a diagnosis of MSK. I felt better for a while, but after a couple of years I again have the nagging ache on the right. I used to say if you cut me in half my left side would be perfect. Well, recently my left side started, and I felt like I had a UTI. Went to gynecologist and had blood in urine, put on Cipro, culture came back negative. Kept having pain and was sent for US…5mm stone in left, 3mm in right. Was told I could opt for lithotripsy because I was going out of town to help move my elderly in-laws and was afraid I would pass a stone while gone. I decided to wait and try to deal with it. The UTI feeling came back and worsened so that I had to stop at ER on the way home (July 4th) as I wanted to make sure I was not getting an infection. Same thing-blood in urine. I was prescribed Toradol to help with inflammation till I got home, but I only took one as I am afraid of side effects. Here is my question-should I arrange to have the stones removed? If the pain is going to be a constant feeling of starting a UTI, I don’t know how long I can handle it-(it is a feeling of fullness in kidney with a sensation of a clothespin on my lower ureter; no burning on urination but a need to go often because of the sensation). Perhaps I should try to find a doctor that is familiar with MSK? I live in Fairhope, Alabama, but would be willing to travel if not too distant. Thank you for any guidance you can give.
Sincerely, Amy
Hi Amy, You need special care in Alabama. Fortunately you have a world famous stone expert in town. He is himself a superb surgeon and runs a brilliant stone program – among the best anywhere. He is also a friend of mine, so you can say I sent you. Do this. Regards, Fred
can some one help me please
Hi Alesha, Sure – can you tell me a bit about what is wrong? Regards, Fred Coe
I am a 61 year old male, and I passed my first kidney stone when I was 8 yrs old (1966). I did not have a diagnosis of MSK until I was 28. I have passed many hundreds of pieces of stones. Is there any practitioner in the Atlanta area that specializes in MSK? I have a decent Urologist, Nephrologist, and Pain Management Specialist. Even though they try to help, their focus is on the run of the mill patients, and I am an oddity. If you could help i would greatly appreciate it.
Regards – Mark McDonald.
Hi Mark, Emory is your best bet. I went through the faculty in Urology and did not recognize any names, but I would call and ask who specializes in stones. In renal medicine, I noticed Dr Robert Hoover who is not a stone person but a friend of mine and he might point you in the right direction. Regards, Fred Coe
Thank you very much for your advice Dr. Coe.
I have another question, I am completing a Living Will. and would like to know if the University of Chicago (your department) would be interested in the donation of my kidneys to your MSK research after I pass away. If the University is interested, what do I need to specify or to place in the Living Will to ensure it occurs?
Regards – Mark McDonald
Hi Mark, I believe I replied to you personally. Your thought is generous. I believe you need only specify it in your will, and that is the legal force involved. The world is better for people like you. Fred
I was diagnosed with MSK 25 years ago. I have passed many large stones on my own. I am seeing a new Urologist and he has suggested PCNL to remove all my stone. Is that a successful treatment for MSK?
Hi Ann, If you really have MSK there will be a lot of stones and they will be removed by opening the sponge cavities. Usually that is done because of severe pain. PCNL is usually because of a very large stone burden or very large stones, which I presume you have. Knowing nothing more about you I cannot say more that would be useful. Regards, Fred Coe
I was diagnosed with bilateral MSK in 2003. I have passed multiple stones over the years. Do you have any recommendations for a “stone specialist” in Buffalo NY? Rochester, NY and Cleveland would work as well.
Thank you!
Hi Giana, In Rochester, Dr David Bushinsky is very skilled in stones, and he has several partners with similar skills. I would advise you go there. Regards, Fred Coe
Hello, I really hope that you get this message as I am in desperate need of some help. My doctor does not take this condition seriously and refuses to provide me any medication that is adequate to treat the pain. She does not believe that I am experiencing pain. I just went through a 14 week experience where I called her weekly to tell her that something was wrong, that something was different and not right and got no Assistance until I ended up in the hospital, septic with a fever of 107 and a heart rate of 365 with a blood pressure of 80/40, I almost lost my life! She still refuses to take it seriously! When I tried to talk to her about it today she told me that she had other patients to deal with and disconnected the call. I really need someone who’s going to take this seriously! This is affecting my daily life and the pain is making it unable for me to maintain a normal job or social life. I just went through a 14 week experience where I called her weekly to tell her that something was wrong, that something was different and not right and got no assistance until I ended up in the hospital, septic with a fever of 107 and a heart rate of 365 with a blood pressure of 80/40, I almost lost my life! She still refuses to take it seriously! When I tried to talk to her about it today she told me that she had other patients to deal with and disconnected the car. I really need someone who’s going to take this seriously! This is affecting my daily life and the pain is making it unable for me to maintain a normal job or social life. Are there any good doctors in Atlantic Canada that specialize in this or have knowledge of this disease? Thank you in advance!
Hi Jessica, I am very sorry for all this – sepsis is so dangerous and scary. I found this physician at Dalhousie University in Eastern Canada. She has trained in stone disease and is the only one listed for stones there. I would try to see her. Regards, Fred Coe
I was diagnosed with MSK in 1965 while passing blood in my urine. The passing of blood continued for the next 7 years; no stones, no pain. I was monitored every 6 months to make sure I was not becoming anemic. The next lengthy constant showing of blood started again in 2015. In the interim years, my problem would pop up for days, or weeks or a couple of months. Once again, no pain and no passing of stones. In spring it started again and occurred daily for 8 months. I was referred to a urologist by my PCP, had a cystoscope and conversation and she was convinced I didn’t have MSK and was absolutely amazed when it just disappeared again. Last December I had an ultrasound which indicated that I now have kidney stoner which have not caused me any problems. I had occasion to confer with a urogynecologist within the last week and when she read my history she told me I do not have MSK but that it was the kidney stones that probably caused the blood. My sister has had a few “episodes” like mine, passing blood for several days with no pain or stones and also been told that it is not MSK. We are both in our early 80’s. I would be interested in your comments. Your article was wonderful.
Hi Carol, I suspect you both may form crystals. Probably you both have genetic hypercalciuria, a common cause, but that is a guess. 24 hour urine testing might show the high urine calcium. Your physicians might look for crystals when bleeding occurs. Regards, Fred Coe
Hello Dr. Coe,
My story is almost identical to the above stories. I live about an hour north of Seattle. My last ER visit had me hospitalized for 5 days with a kidney infection. Very scary! I thought I was just going into the ER for a “normal” kidney stone attack The urologist that I’m with is new and doesn’t seem to believe that I’ve been diagnosed with MSK in the past, nore does he give any credit to it. I’m 54 yo now and have been dealing with this 25 years. Do have any great references for urologist, north of Seattle, that can help with my MSK? Sincerely Anna
Hi Anna, My best guess is at the university kidney stone program. This doctor there seems best suited. She is a nephrologist not a surgeon but may be more interested in prevention. Regards, Fred Coe
I have been diagnosed with genetic MSK. I’m looking for a referral in Greenville SC. I can’t believe it took four years to be diagnosed.
Hi, There is a kidney stone program at the medical university of SC. At Emory, in Atlanta, they have a large renal and urology program. I do not know any of the physicians, but Dr Jeff Sands at Emory is brilliant and if you email him he would know who at his university might actually have the expertise you require. He is unlikely to care for you personally. Regards, Fred Coe
Hi there. This is a fantastic and informative article. I am going to print this off and place with my medical records. I was diagnosed over 2 yrs ago and seem to live in constant pain with frequent stone passing. My biggest concern is finding a Nephrologist and a Urologist that specialize in MSK. I have been to more than 10 specialist (Nephrologist & Urologist) and cannot get help. The Nephrologist says they will see me 1x yr while the Urologist wants nothing to do with mr unless I have an actively passing stone. I am in the Kansas City Metro area. Can you recommend a specialist?
Hi Crystal, I found two physicians at the university, but neither seem specialized to kidney stones. If telehealth will do, one of us here at U Chicago could consult for you in terms of prevention, or perhaps the same at another US stone prevention center. Our number is 773 702 1475. Regards, Fred Coe
I have MSK and Nephrocalcinosis in both kidneys. I need help getting pain management as I am in constant pain. I live in Oklahoma if you know of someone who can help. Thank you
Hi Susan, I do not know anyone personally. There is a medical school and the renal program seems to include a kidney stone clinic, That would be your best bet. Regards, Fred Coe
I was diagnosed with MSK 20 years and and just this past week was diagnosed with Polycystic kidney Disease but i cant find any information on having both diseases. I am starting iwth a nephrologist next week but would like some information sooner to calm my worries. Can anyone provide information on have these diseases simultaneously?
Hi Shasta, MSK is not directly related to adult onset PCKD. If you have the latter it is a significant but manageable condition I am sure your nephrologist will tend to. The MSK itself is benign apart from stones and increased infection risk. Regards, Fred Coe
Hi,
Thanks for the article. I was diagnosed this past week with sponge kidneys only by an ultrasound. They also found nephrocalcinosis. Should I be asking for a more specific test to confirm this finding?
I also have Rheumatoid Arthritis and am on max dose of Methotrexate. Is there any risk to having the above and the excretion of Methotrexate?
Hi S, I am always skeptical of MSK diagnoses – are your stones calcium oxalate or calcium phosphate? If the latter, you may well not have MSK at all. RA can lead to an abnormal high urine pH and calcium phosphate stones, so the question is very pertinent for you. Regards, Fred Coe
Hi I was diagnosed with msk and nephroptosis 20 years ago. My quality of life is poor and my pain is unmanageable. Constantly at doctors with zero solutions.
Hi April, I gather it is multiple non obstructing stones and pain, not at all rare. Surgery is not as yet tested as a remedy. Infection can be a part of the problem, and perhaps your physicians can see about it. I wish I had more to offer. Regards, Fred Coe
I was diagnosed a few weeks ago. I have calcium pocketed stones. This has been really tough for me. I’m in constant pain an constantly throwing up. They put me on citrate pills an a crazy diet 😭😭
Hi Summer, I presume you have either medullary sponge kidney or form calcium phosphate stones. Rather than just take citrate and a special diet, take a look at a good introduction to what is needed and be sure you have been tested and your treatment is directed at the causes of your stones. I imagine both are true, but reading about things will help you understand what is needed. Regards, Fred Coe
I was hoping the comments that someone has found hope. I was in and out of surgery since July 4th with for stents and still I am in daily pain. At this point the stones are not moving which makes us fall under the general rule well if the stone isn’t moving its not painful. Which even going to the ER for pain management doesn’t even help because I am not the normal kidney stone case that has a stone stuck. Is there any doctor the understand MSK in California or Nevada that can help me?
Hi Melissa, Persistent pain always raises the question of obstruction. Be sure your surgeon has checked that no stones are obstructing any portions of the kidneys. Another reason for pain is infection, also what your physicians can look for and treat. Regards, Fred Coe
Reading so many comments about others in constant, severe pain at least makes me feel that I’m not alone and that the pain is not “all in my head” as some physicians have indicated. I had stone issues for years (1999-2015) before finally getting diagnosis of MSK.
Every doctor I see say I’m a very “complex” case. I am on long acting opiates for pain control but I still struggle with breakthrough pain and especially when passing a stone. If I go to my local ER, they see me as “drug seeking” (wish they would distinguish between drug seeking and “pain relief seeking”). Acute pain, and even the thought of it makes me very anxious and I’m sure I have mild PTSD from so many hospital visits of not receiving proper pain management. I get they can’t give me “too much” opiates and they all agree it is the most painful thing to be passing a stone… yet it’s extremely difficult to receive proper treatment.
Hi Leeann, You may have MKS or calcium phosphate stones. In either case you are one of many with a lot of pain from stones that are not obstructing the kidney in an obvious way or infected, so far as physicians can tell. It is a not uncommon frustrating situation and the only idea I have is to seek an opinion from a kidney stone center that is convenient to where you live. If you say, I can try to identify one for you. Regards, Fred Coe
Reading so many comments about others being in severe, chronic pain at least makes me feel not as alone or that the pain isn’t “all in my head” as many physicians have tried to make me believe. The thinking that kidneys have no nerves, therefore we shouldn’t be having pain unless a stone is active or obstructing, is extremely outdated and causes us to face many challenges in properly managing our pain. I am lucky to be on a good long acting opioid for my chronic pain but I still struggle with acute flair ups, especially when actively passing a stone.. many of us, myself included have been labelled as drug seeking which hampers our care. It’s time to distinguish “drug seeking” from “pain relief seeking”. I am sure I have at least mild PTSD from being very under treated for my pain on several occasions at mostly my local hospital.
Hi Leeann, Indeed kidneys have nerves, and produce pain. Fred
My daughter has been diagnosed with MKD and hyper calcium. They cannot determine why she is hyper calcium. She is in daily pain with excruciating flare ups. She is presently at Mayo. She is on Norco which is definitely not enough and leaves her bedridden during flare ups. She has been told if she goes on long acting opioid that her flare ups will be worse. Only option she is given is to try renal denervation which there is no information on with kidney stone patients. She has done every procedure offered. She also is treated as a drug seeking addict when she goes to ER. She lays in bed for a week in excruciating pain. Please offer any advice.
Hello. I’ve been diagnosed with MSK and I have several kidney stones in both kidneys. They aren’t obstructing the urine but I sometimes feel pain in my kidneys. When I go to the er they assume I must have past a stone because my ureters have hydro and I have blood in my urine. I also have frequent utis that have scarred my kidneys. Would opting to have surgery to remove the stones be the best option? They haven’t determined if the stones are in my tissue or free floating. I live near Portland Oregon if you have any suggestions of where to go?
Hi Alexis, as the article points out MSK is often a diagnosis in error when calcium phosphate stones are the real problem. The medical school in Portland would be ideal for you. I would contact them. Regards, Fred Coe
Trying to find a doctor who understands what I’m going through has been almost nonexistent. I’ve been diagnosed with MSK and am “full of stones”. Yet I keep being told there’s nothing they can do. I just have to pass them and that they don’t cause pain unless they’re traveling. I’m still peeing blood 7 days after being on antibiotics for a kidney infection. Why is this being brushed off as no big deal?
Hi Jessica, Given MSK is so often over diagnosed, I would be sure it is not something else which means stone analyses and 24 hour urines and proper blood testing. If it is something else, treatment may be a lot different and more effective. Rgards, Fred Coe
Hello. I am 60 years old. Yesterday, for the first time in my life, I had an abdominal CT scan with contrast. Kidneys conclusion: there is BLUSHING OF THE RENAL TUBULES WHICH SUGGEST THE POSSIBILITY OF MEDULLARY SPONGE KIDNEYS.
I should worry and be examined further or continue to live without paying attention, since this pathology is most likely of a congenital nature. Renal markers are normal.
Hi Olena, at age 60, if you indeed have MSK, it has been kind to you in not creating stones – the CT would have shown them. There is nothing for you to do based on any science. Perhaps you might want to ensure a reasonable hydration, or at least avoid dehydration, and look forward to a normal renal life as you have already had. But, why the CT in the first place? Was it bleeding or pain?? Regards, Fred Coe
I have been diagnosed with msk. My dr doesn’t do much. He orders lots of KUB X-rays and tells me if they get larger he can treat but otherwise there is nothing he can do. I live in Las Vegas. Is there a dr here that specializes in patients with msk?
Hi Andrea, As the article points out, you probably have calcium phosphate stones, not MSK, but in either case you should try to get expert help. I found a medical school in Nevada and tried to find their kidney stone program – failed. Here is the link to the school, and I would call and ask if they have anyone there who is expert in MSK. I wish I knew more about your state. Regards, Fred Coe
Hi ~
I was diagnosed with MSK in 2000 and have seen multiple doctors regarding it since, including Nephrologists, but have yet to find one who seems to FULLY understand MSK. IF you happened to have an MSK familiar doctor you would recommend in the Seattle area, I would greatly appreciate it. No worries if not, but you sound like you are in the know so I thought I would just ask and see if you did. Thank You. This article was very through.
Hi Leslie, The university has a stone program, and one nephrologist who is specially interested in the problem. I would use that resource. Regards, Fred Coe
I was diagnosed years ago from an IVP that I have MSK in my left kidney. I’m plagued with uti’s and they are now always present. I’m on antibiotics every day and recently had a kidney stone on my left side. My bladder has been damaged from all of the uti’s, so now I’m told I have interstitial cystitis. Can this cause severe uti’s which require multiple antibiotics to be taken? Are you familiar with doctors in the Virginia area who can help me? I’m in my 60’s and the infections have been in my life since my 30’s. Thank you.
Hi Maureen, The University of Virginia has a kidney stone program, and would be your best bet. They list four physicians, two in nephrology, and I would consider starting with one of them. I do not know the people and therefore have no recommendations. Regards, Fred Coe
Hello Fred, In 2018 a pregnancy ultrasound showed “Nephrocalcinosis” on my kidneys. I am now seeing a Nephrologist who has diagnosed MSK. Although now I have read this article (thank you) I am not certain the right techniques have been used to determine I do have MSK. I will show him the article and now raise that question with him. I am doing 3 – 6 monthly 24 hour urine tests and showing hypercalciuria. I will be seeing my Nephrologist this week to discuss beginning to take a thiazide diuretic to combat the hypercalciuria. I have not suffered from kidney stones as yet, but I believe continued hypercalciuria is likely to lead to that? I would love to hear any advice about what I should ask of my Nephrologist at this point? Also, do you know of any doctors in Melbourne, Australia that have in-depth knowledge of MSK diagnosis/treatment? Thank you,
Andrea
Hi Andrea, I suspect you have a high urine pH as well as hypercalciuria and have formed calcium phosphate deposits. Thiazide is a good idea. I looked for a stone program at the medical school in Melbourne and could not find a kidney stone program, but I would enquire as that is usually where the experts hang out. As for MSK, stones are usually calcium oxalate – a clue. You are wise to think your problem will seem strange and foreign to most doctors, because it is. Try to keep urine stone risk down (supersaturations for calcium oxalate and calcium phosphate) and avoid procedures as best you can. Regards, Fred Coe
Thank goodness we have you Dr Coe! You are so appreciated!! I have been reading your articles and website for several years. When I was diagnosed by IVP in my twenties after my first stone, they told me it was just a benign condition and I would never have to worry a out. Several procedures and painful years later I finally found a doctor who recognized this is a real chronic condition. Unfortunately, my doctor just retired. Can you recommend a specialist in the DC/MD area familiar with MSK? Everyone seems to have a kidney stone center these days… And I don’t want to waste time with doctors who see this as benign. Also do you think it is better to work with a nephrologist or urologist? Or should I have one of each? Thanks in advance for your help!
Hi Jen, Brian Matlaga at JHU is a brilliant stone urologist and surely has a partner nephrologist. I have known him for years, feel free to say I sent you. Fred
I was diagnosed with MSK when I was 18. Now 49, and starting to significantly lose kidney function. I have had 20 to 30 procedures to remove stones throughout my adult life. Constant UTI, which I am on prophylactic antibiotics for. Hospitalized multiple times with kidney infections, and after most of my stone removal procedures, I become septic. MSK has dominated my life! My question is, I am in a constant state of dehydration, no matter my fluid intake, and my potassium levels are impossible to stay within the normal range, even with supplements. I have had more medical test than I can count, and more procedures than anyone should have to. I have, what I think are good doctors. Both urologist and neurologist, but now that my kidneys seem to be failing, I’m wondering if there is something they or I are missing. As of now I am in stage 3 renal failure. Is it the MSK? The procedures? The infections? Or all of the above? I feel like I am fighting a losing battle. One that is going to kill me. I am at a loss of what to do next.
Sincerely,
Kat
Hi Kat, You need really expert care. I wonder if you have MSK or form phosphate stones, you do not mention stone type. I suspect the many procedures, sepsis, and renal infections may have damaged your kidneys. The fact that your serum potassium falls – I presume you are not taking a diuretic – is important. Do your physicians know why that is happening? If I had more information, I could try to be more helpful. Regards, Fred Coe
In 2003 I was diagnosed with MSK in both kidneys and was told the condition was benign – no long term kidney damage to be concerned about – and best managed through diet to discourage stone formation and UTIs. Fast Forward to 2021 and my latest ultrasound came back showing some alarming things in relation to cortical thickness, etc. Are there any programs/doctors in the Los Angeles area whom you would recommend having a better understanding of MSK and its long term effects?
Hi Natalie, UCLA is the most likely place to find high level talent, but I do not know anyone specially I can single out. What you want is a skilled renal physician who is specialized in kidney stone management and research, but I looked up the renal faculty there and no one indicates any special interest in stones. At Cedars Sinai a search for kidney stone prevention as a service in medicine yielded no results. You may have to default to telehealth as an option. Regards, Fred Coe
Dr. Coe
Thank you for being willing to answer questions. You truly are a kind doctor
I’m 65 years young and suffered my first major stone attack at age 14 (I’d been experiencing ischemic events since my early childhood and was known to have some sort of kidney issues) . I live in the St. Louis Missouri area and am lucky to have the Washington University Medical school here, where I’ve received treatment. I was diagnosed with MSK by Dr.’s Elsbeth MacDougall and Ralph Clayman when I was in in my mid twenties. I was told that I had one larger and one much smaller kidney, and a “significant” amount of kidney stones. Since that time I’ve been cared for by a number of other rotating doctors through the medical school while I passed hundreds of stones and and had 70+ scope operations to remove blockages. Eventually one kidney was removed due to function being less than 3% in a hope to eliminate constant pain. As the scope operations continued, the ureter to the remaining solitary kidney formed scar tissue causing it to shut with regularity with the resulting agony and no ability to urinate. Finally, a resection of the ureter was done to remove the scar tissue, but not before I had a stroke during one of the surgeries, leaving me blind, deaf and numb on one side of my body. I still endure constant pain in my remaining kidney and live on antibiotics to try and keep my ongoing UTI’s under control. I caught (developed?) a fungal infection in my kidney that turned my urine white that lasted for over 3 painful years, and included a trip to the Mayo clinic looking for a solution, before another doctor, an infectious disease specialist at Barnes Hospital in St. Louis agreed to treat me, eventually curing it by giving me anti fungals via a PIC line for months, but not before the first dose sent me into anaphylactic shock, necessitating a change in the treatment drug. I’ve endured dozens of stents, as well as a half dozen nephrostomy tubes after surgeries. I currently hover in lower stage 3 renal failure, but am thrilled to not be on dialysis. I have been told by so many doctors so many times that kidney stones can’t and don’t cause pain unless they are moving. I need to share with my doctors information from another source, as indeed they must cause pain as I have “hundreds” of inoperable embedded stones and feel like I’m having a kidney stone attack with the least amount of physical movement. A big bump while driving feels like a knife in my kidney. Are you aware of my research about pain from stones that aren’t moving? Can anything be done to resolve the constant ache and intermittent sharp pain from all of these “razor blades” in my remaining kidney? Are the embedded stones truly inoperable? Many thanks!
Hi Bob, You are at an excellent university and despite that have had a really difficult time. Infection is a cause of pain like you describe, and I also know from many stone websites that non obstructive pain is a common complaint. Even uncomplicated stones associate – and probably cause – inflammation in the kidneys, and inflammation itself may cause pain – some investigators are interested in this problem. My comments reflect the genuine lack for hard knowledge in this area, for which I apologize. Of all available, infection is the only one with any current practical interest and perhaps it should be sought for. Regards, Fred Coe
Hi!
I currently see a nephrologist for MSK, but no longer a urologist, as he retired 3 years ago. Do you recommend seeing one specialist over the other or both? I live in Ohio and have been really struggling with constant daily kidney and flank pain for the last month, which usually means I’m building up to a major episode and my current nephrologist never seems too concerned that my potassium and calcium are consistently through the roof. I have been in the process of changing doctors, but wasn’t sure if I should reconnect with a urologist again or just continue with a nephrologist?
Thank you so much for any help in this matter!
~Becky
Hi Becky, Cleveland Clinic is exceptional, if you can use it. You should have a urologist for your stones, and someone to take care of prevention – a nephrologist or endocrinologist is often interested. I do not know what you mean about your calcium – if it is your urine calcium that is high, one can treat that. If it is your serum calcium, that is a serious matter and also treatable. Regards, Fred Coe
Can you recommend a specialist in Upstate SC or Western NC that can help me with Medullary-sponge-kidney? The urologist I have seen in SC is not helpful and my previous doctor is retired.
Hi Sherry, I have had trouble doing this before – UNC says they are founding a program and so does Wake Forrest. North Carolina has great medical schools but probably too far away. You do not have obvious kidney stone experts for me to point to. Sorry, Fred Coe
I was diagnosed with medullary sponge kidney during my last pregnancy at age 35. I am currently 65 and have managed the disease without medical intervention. Passing stones along the way that were quite large with old fashion natural remedies. I am noticing more frequent blood in the urine than before but am also more physically active walk g an average of 5 to 10 miles per day and exercising at a cross fit gym? I live in Western Pa. I did once consult with a great doctor Sunil Soi however, he is no longer in the area. Which facility would you recommend if I ever need a consult. If necessary I could travel to Cleveland Clinic.
Hi Lou Ann, Penn has a program in stones. I do not know any of the surgeons listed but I am sure they will be excellent given the fame of the university. Cleveland Clinic the same. Regards, Fred Coe
Hello, I have been a long time member of the stone passing club (about 20 years), unsuccessfully managed through diet, medication, and procedures to remove stones. I was diagnosed with medullary sponge kidney about 10-12 years ago, (by military docs – maybe they got it wrong??) from an ultrasound, but no other testing. Over the years imagining always noted “Medullary sponge kidney versus medullary nephrocalcinosis. Lobular contour with cortical volume loss at the lower pole consistent with developmental cleft or old scar”, however no provider ever addressed these findings, they would just remove the stones. My newest CT shows “No hydronephrosis. There are multiple (greater than 10) renal calculi bilaterally, left greater than right. Suspect medullary nephrocalcinosis. On the left, largest in the lower pole measures 1.1 x 1.2x .8 cm. On the right, largest calculus in the lower pole measures 9 x 8 mm. Since 2019, there has been increasing confluence of stones in the right lower pole although decrease in size of stones within the left upper pole. Lumbosacral transitional anatomy with the left L5-S1 pseudarthrosis. Impression: Suspect medullary nephrocalcinosis with bilateral nonobstructive renal calculi as above. Overall stone burden is similar to past imagining, increased in the right lower pole although decreased in the left upper pole.”
I currently am looking for new provider(s)- are any doctors/programs in Southeast CT that you would recommend having a better understanding of MSK and its long term effects?
Thank you in advance,
Jennifer
Hi Jennifer, The confusion is with multiple calcium phosphate stones so stone analysis is crucial. In MSK stones are almost always mainly calcium oxalate. That would be my first step. 24 hour urine testing is always a good idea as high urine risk factors for crystal formation can increase any form of stone disease. As for southeast CT, does that include New Haven – Yale is always excellent. Regards, Fred Coe
I am a 66 year old woman, diagnosed with MSK at age 20 via the UCSF renal clinic. I have been quite well with the exception of chronic hematuria and anemia, but no big deal. I recently had my first routine bone density exam and I have severe osteoporosis! Followed that with a renal ultrasound that showed cysts, one stone and angiomyolipomas. I think that’s a disturbing combo of stuff and want to see a nephrologist. They are refusing to see me because it’s all “benign “. I don’t think they know what they’re talking about. Where do I go from here?
Hi Karen, The bone disease certainly warrants care. Angiomyolipomas (with cysts) have gradually changed in meaning, and may possibly imply significant serious potential. Certainly a urological surgeon at UCSF with experience in potentially malignant diseases would know about this article and scattered others. Most likely you have utterly benign problems, but one would want to be sure. As for MSK and stones, I have found many cases to be calcium phosphate stones with mislabeling to MSK. MSK produces calcium oxalate stones. I am disappointed that university nephrologists would not undertake your care, and surprised as well. I would contact the Urology group there, and perhaps they might find you a ‘worthwhile’ patient. The institution is superb. Regards, Fred Coe
I am 38 and diagnosed with MSK a couple years ago. I have constant Sodium Oxalate stones and have never had them removed. Is there a certain kind of doctor I should see to help me prevent further stones from forming? I do have a Urologist I see yearly that prescribed potassium citrate with hasn’t worked. I started taking it 3 months ago. I live in the Seattle, WA area. Thanks!
Hi Melissa, Indeed calcium oxalate stones can result from MSK and removal can be problematic as well. The university medical center in Seattle is excellent. I would suggest it as a reliable source for you. Regards, Fred Coe
Hi doc, I have recently been diagnosed with MSK at the age of 60. I have had two large stones stuck in the bottom of my right kidney for decades. I was told to leave them be since they don’t get in the way. However, recently, I have been getting multiple UTI’s that have become antibiotic resistant. I have been told by urologists and nephrologists that I should have these stones removed due to the infections. I also recently learned that my right kidney is not working at 100%. Renal scan showed left at 79% right at 21%. Apparently my right kidney is filled with scar tissue. I have been told that I may lose function of my right kidney eventually. Should I even bother getting surgery on it if it’s low functioning anyway? I don’t believe I will get any more function out of it even with surgery. However, I may avoid infections in the future.
Hi Debbie, you do indeed have a very complex medical /surgical problem. I urge your physicians consider consultation for you at a university kidney stone program. WHether or not to do more for your right kidney is not a simple matter as every surgery presents risk of a general nature. Regards, Fred Coe