
Let me put the main points first, so you know what you are going to read about. Kidney stone formers have increased pregnancy risks for prematurity, need for C-section, low birth weight newborns, gestational diabetes, and preeclampsia.
To write about all this I did a PubMed search: “Pregnancy AND kidney stones” which yielded 357 papers published between 1962 and 2021 – a surprisingly small collection. Many are reviews, guideline statements, or specialized beyond the uses of this article.
From the lot, I selected 25 with original data, of which I use those few that concern risks to mothers and their fetuses. I use additional references about preeclampsia risks unrelated to kidney stones.
The detail from the gorgeous Arnolfini Portrait, Jan Van Eyck, 1434, a tempera and oil on oak panel, 82.2 x 60 cm (National Gallery, London) is copied here from a study by Dr. Lane Eagles.
To the few and privileged contemporary eyes that might have seen the image, she would not have seemed pregnant – it was in poor taste, then, to depict pregnancy – but posed demurely, a hand at the girdle of her elaborate dress. Yet those same eyes would have understood that pregnancy was the usual condition of premenopausal women, and a grace that costume and gesture would happily imply.
Insurance Claims Study
Population
Analysis of the Optum® claims database identified 1.43 million pregnant women of whom 11,260 (0.8%) had kidney stones diagnosed during pregnancy. Quite apart from pregnancy, the stone formers had higher frequencies of diabetes, obesity, high blood pressure, gout, kidney disease and hyperparathyroidism. This last four have well known associations with stone disease.
Maternal Complications
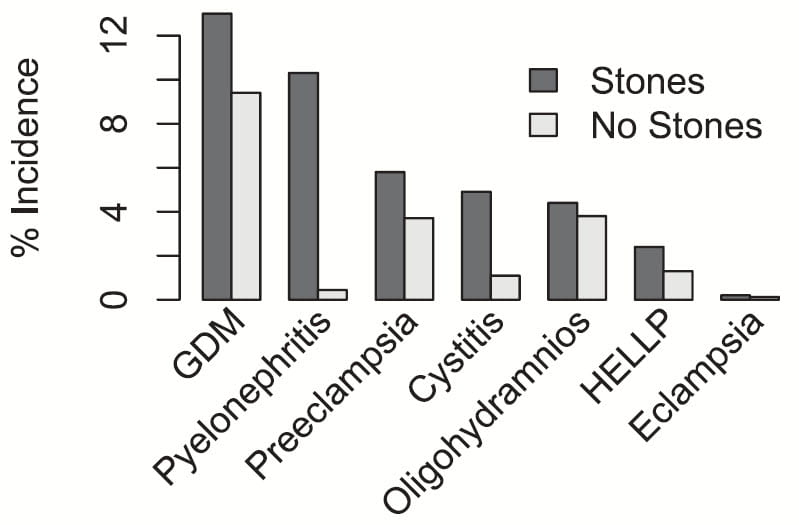
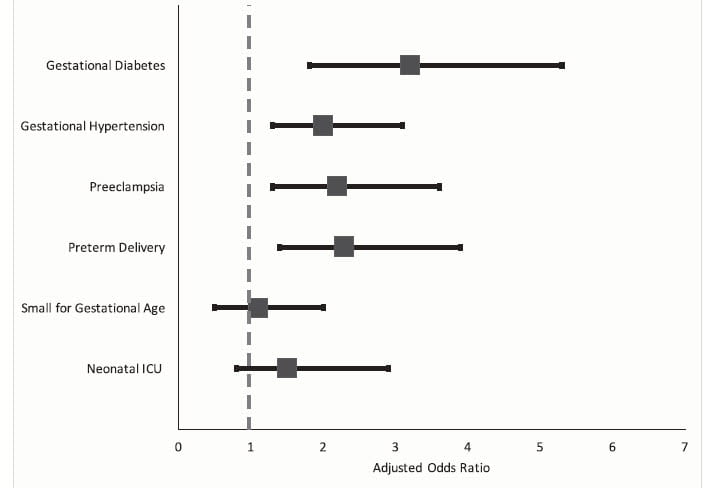
In this figure, all differences between the “stone” and “no stone” pregnancies are highly significant, p<0.001.
Stones were associated with increased gestational diabetes (GDM), kidney infection (pyelonephritis) and cystitis. The last two associations are well known from smaller studies.
Preeclampsia is a serious pregnancy complication that includes high blood pressure, increased loss of albumin in the urine, reduced kidney function, and risk of very severe kidney disease and fetal loss. Mostly it can be managed well with modern approaches. Women who have had preeclampsia have higher risk of stroke in later life. (relative risk, 3.79; 95% CI, 1.24-11.60).
Eclampsia, very uncommon, is a life threatening extreme of preeclampsia. Oligohydramnios is a deficiency of amniotic fluid. HELLP is a combination of hemolysis (red blood cell injury), liver injury as manifested by increase of serum levels of enzymes normally inside liver cells, and a fall in blood platelet levels.
Fetal Outcomes
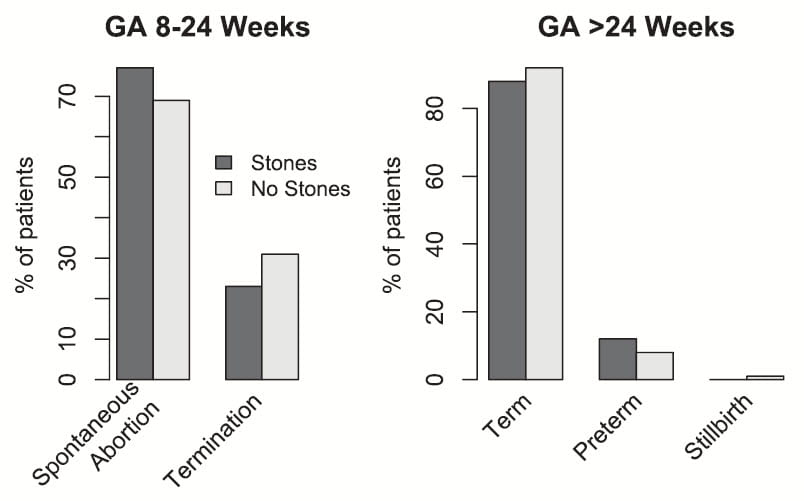
Among non-viable pregnancies, gestational age (GA) less than 24 weeks, spontaneous abortion was higher in stone formers (left panel of the figure}. Of viable pregnancies (GA>24 Weeks), stone formers had a higher rate of preterm deliveries (right panel of the figure). Even so, rates of fetal death (not shown on the graph) were not different (0.4% vs. 0.5%).
Since urinary infection and preeclampsia both cause premature delivery, these are not surprising results.
Ontario Population Study
This province has an administrative health care database system and a very low rate of emigration. There were 1.39 million pregnancies between 2004 to 2014 of which 2863 (0.2%) were associated with kidney stones. The authors matched each stone pregnancy to up to 6 non stone pregnancy to achieve its set of 17,171 matching controls.
Adverse Outcomes
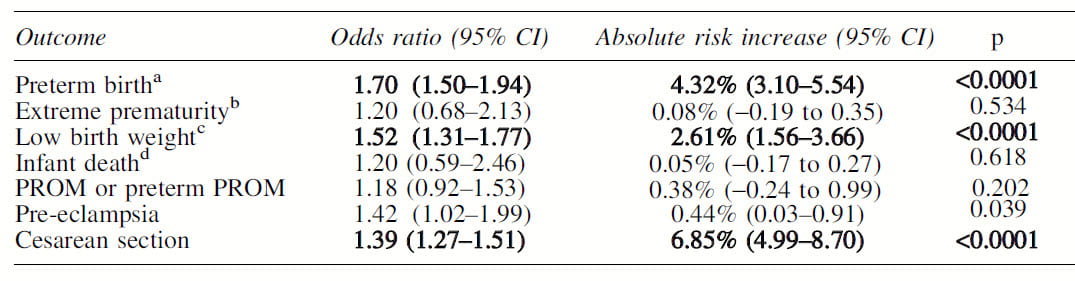
Three adverse outcomes predominated in pregnancies complicated by stones. They are bolded, have p values <0.0001, and include preterm birth, low birth weight, and need for Cesarean section. PROM, not significant, means premature rupture of amniotic membranes.
These results agree with the insurance study noted above, but include C section data not in the prior study. The two studies also agree on higher rates of pre-eclampsia but the effect here is far more modest even though the populations are about equal in size. The Ontario study did not find an excess of gestational diabetes or of kidney or urinary tract infection.
Effects of Procedures
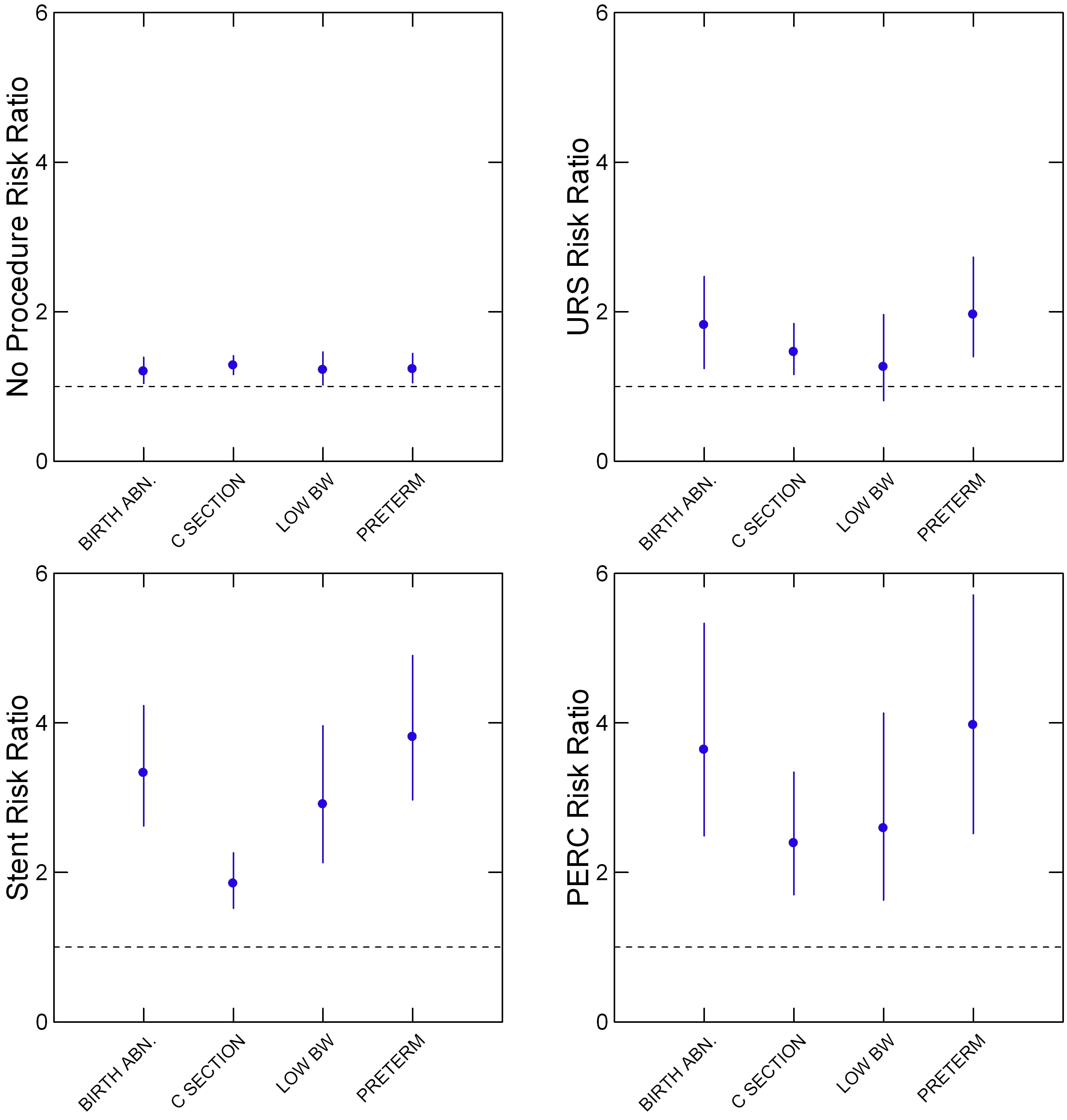
Procedures for stone management associated with birth abnormalities.
From Table 3 of the study I have graphed the four adverse outcomes whose risk was significantly increased. By significantly I mean the mean risk ratio (circles in my graph) – vs. the non stone pregnancies is above 1 and has a lower 95% confidence limit (line downward from the circle) that does not go below 1.
For example, among women who had no procedures for stone management (upper left panel) all four mean (circles) risk ratios for a birth abnormality were above 1, and the downward pointing lines that end at the 95th percentile are also above 1. But the increases are very modest.
Each ratio is independent, so, as an example, the ‘C-SECTION’ ratio in the ‘no procedures’ panel is slightly higher than the total of all birth abnormalities (BIRTH ABN).
Risks were generally higher in pregnancies that required ureteroscopy (URS), upper right panel) and considerably higher in those that required stents or percutaneous nephrolithotomy (PERC).
These are all associational data, so it is not as if we knew URS, Stent, or PERC caused the adverse birth event. For example, a large stone that required PERC or URS might have led to obstruction and infection of a kidney, and infection or obstruction, not the procedure, caused an abnormal birth event.
I presume that infection lurks within these procedures, and may have additionally raised risk for these adverse pregnancy outcomes.
Massachusetts General Hospital Study
This has all of the advantages and limitations of a single center report.
From 2006 to 2015 the authors found 14,994 singleton (no twins or triplets) pregnancies in women without hypertension, diabetes or kidney disease. Of these 1430 had pre-pregnancy CT studies, 166 showing stone disease and 1264 without stones. They had an additional 14,878 without kidney stone disease by history but lacking CT proof. The main contrast was between the 166 vs. the 1264 CT proven cases.
The key findings are in the figure to the left. Gestational diabetes, hypertension, preeclampsia and preterm delivery were all significantly higher in the women with prior stones vs. those without prior stones.
This generally agrees with the insurance claims and Ontario study, but adds a crucial point: stone passage did not complicate these pregnancies, it is just that the women had documented stones on prior CT scans.
We are looking, therefore, at the increased risk during pregnancies of being a stone former. Having had prior stones seems to confer these increased risks. In this, the study is most like those showing that people with stone disease are abnormally at risk for fractures, high blood pressure, and kidney and cardiovascular disease. All but the first of these raise risk for preeclampsia.
There were no obvious ill effects for the newborns, as noted.
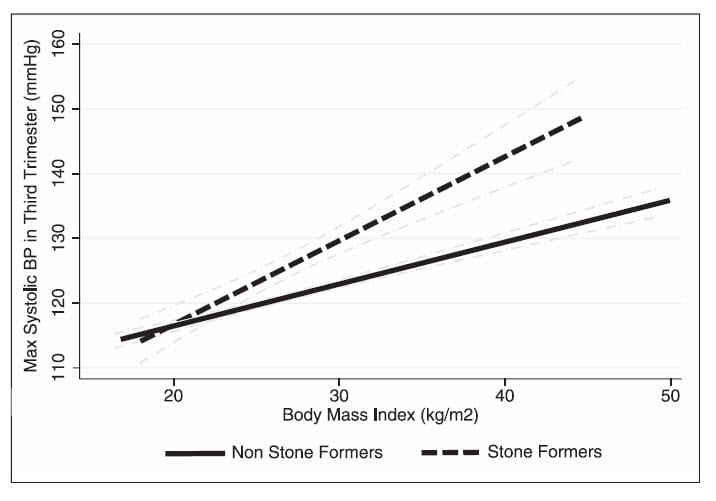 During the third trimester of pregnancy systolic blood pressure tends to increase as a function of BMI. Using commonplace modeling techniques, the investigators calculated the slopes of systolic third trimester blood pressure as a function of BMI for those women with and without prior stones.
During the third trimester of pregnancy systolic blood pressure tends to increase as a function of BMI. Using commonplace modeling techniques, the investigators calculated the slopes of systolic third trimester blood pressure as a function of BMI for those women with and without prior stones.
As the figure to the left shows, the slope was higher for those who were stone formers prior to their pregnancies.
This work as well as the insurance claims study all accord with higher rates of hypertension and renal and cardiovascular disease found in non pregnant kidney stone cohorts.
NHANES Association of Pregnancy with Stones
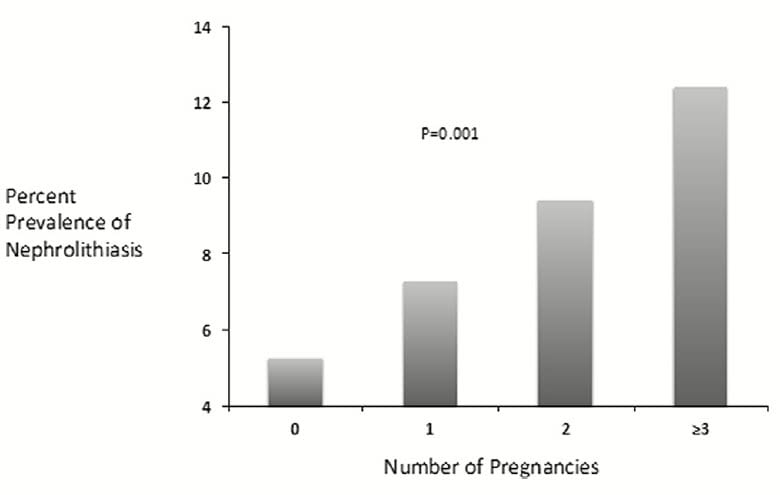 The 2007 – 2012 National Health and Nutrition Examination Survey (NHANES) includes a question about having stones. This permits association between pregnancies and stone disease.
The 2007 – 2012 National Health and Nutrition Examination Survey (NHANES) includes a question about having stones. This permits association between pregnancies and stone disease.
This graph more or less sums up the findings. As the number of pregnancies per woman increases the fraction of women with kidney stones rises from about 5% to above 12%. Moreover, there is a steady rate of increase, which is what ‘p=0.001’ refers to – the increase of stone frequency with rising pregnancies is not likely from chance, but a real phenomenon.
The reason for the association is not known, but probably reflects the remarkable changes in mineral metabolism pregnancy creates.
Why Pregnancy Causes Stones
Years ago, Drs Marshall Lindheimer, Patsey Maikranz, Jean Holley and I along with my long term coauthors Joan Parks and Yasushi Nakagawa studied 11 women through all three trimesters of their normal pregnancies, and 6 – 8 weeks after delivery. We made all of the serum and urine measurements commonplace on this site including supersaturations.
Urine Calcium
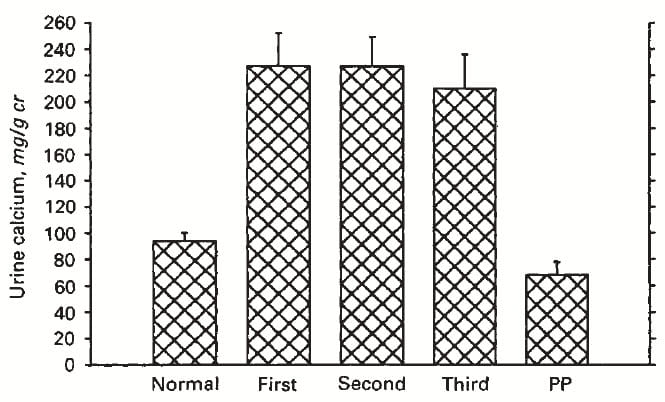 Compared to normal women, urine calcium was elevated by the first trimester of pregnancy and remained so until delivery. Post partum, it was well within the normal range.
Compared to normal women, urine calcium was elevated by the first trimester of pregnancy and remained so until delivery. Post partum, it was well within the normal range.
We know this increase derives to a great extent from increased GI calcium reabsorption, itself driven by a great increase in serum 1,25 vitamin D. Mineral supplements are common during pregnancy so GI absorption rates can be much above normal.
Although urine calcium losses are abnormally high, the main purpose of higher calcium absorption is the fetal skeleton, so maternal bone mineral is frequently mobilized for this purpose.
Urine pH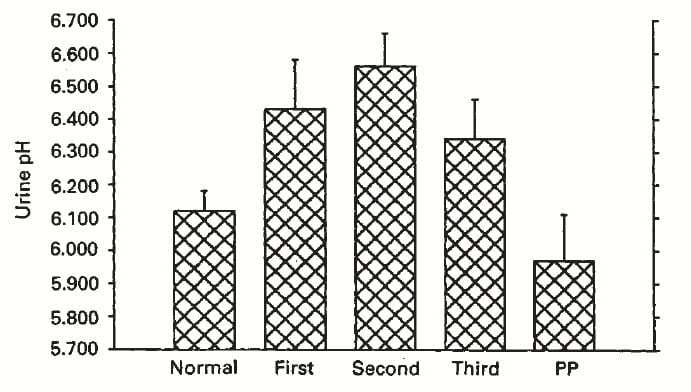
Urine pH determines which kind of calcium stone will form. Higher pH values, above 6.3, foster calcium phosphate stones. We have already noted that stones during pregnancy are generally calcium phosphate in composition.
Normal women have a mean urine pH of 6.1, which would favor calcium oxalate stones. By the first trimester urine pH was already 6.4, and remained at 6.3 or higher throughout. Post partum, urine pH fell to below 6.
Urine Citrate
Urine Citrate Normally Rises with Urine pH
Citrate is the saving grace of high urine pH. Most of the time, when urine pH rises so does urine citrate, protective against stone formation – because it binds calcium in a soluble complex, and inhibits crystal formation and growth.
But high urine citrate does not always accompany high urine pH. For example citrate is not increased in calcium phosphate stone formers even though their urine pH is high.
Urine Citrate Does Not Rise Normally During Pregnancy
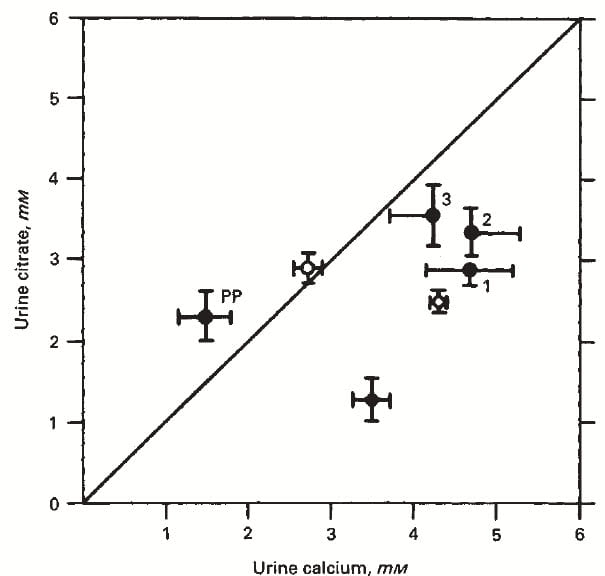 The same in pregnancy. The graph to the right shows urine citrate concentration (vertical axis) plotted against that of urine calcium.
The same in pregnancy. The graph to the right shows urine citrate concentration (vertical axis) plotted against that of urine calcium.
Post partum (PP) and in normal women (open circle left of the line of identity) citrate concentration equals or exceeds calcium concentration. This is the normal situation.
In the three trimesters of pregnancy, labeled 1, 2, and 3, citrate concentration is below calcium concentration – it does not rise as much as calcium does.
The disproportion between citrate and calcium during pregnancy is much like that found in non pregnant women with calcium oxalate stones (open circle right below trimester 1) but not as severe as in non pregnant women who form calcium phosphate stones ( closed circle at the bottom of the graph to the right of the slanting line).
Supersaturations
Calcium Oxalate
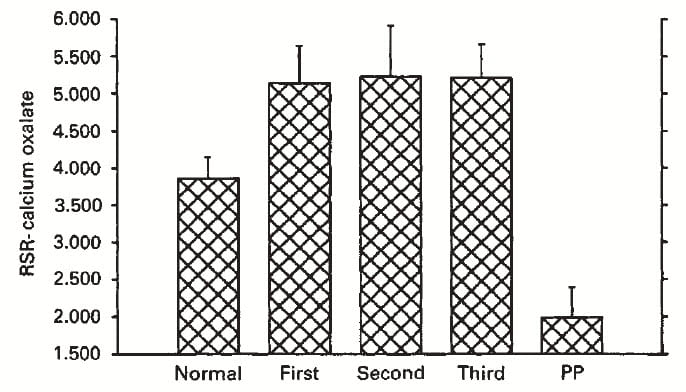
Calcium oxalate supersaturation rose above normal throughout the pregnancies. It fell below normal, to a very low level after delivery. ‘RSR’ is an old term, relative supersaturation ratio, shown on the graph because we did the work so long ago.
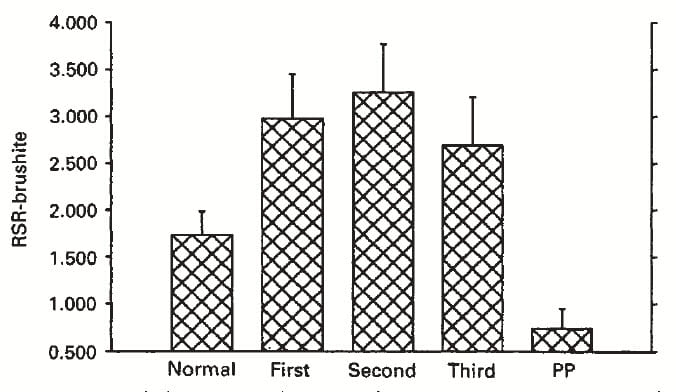
Calcium Phosphate
CaP supersaturation – graph below and to the right – goes up just like that for calcium oxalate, and stays up until delivery.
Many articles on the site present the importance of calcium phosphate (CaP) supersaturation in calcium oxalate stone formation. Brushite, among the earliest calcium crystals to appear in urine can give up its calcium to oxalate forming calcium oxalate. It also converts to hydroxyapatite, the main crystal in calcium phosphate stones.
Pregnancy is a Major Stone Forming State
We presume that the NHANES link between more pregnancies and more stone disease arises in part at least from the marked increase of stone risk from hypercalciuria, high pH, abnormal calcium to citrate balance, and high supersaturations.
Stones may form rapidly enough to manifest during a pregnancy. Tiny seed crystals may form during pregnancy and manifest months or years later as they grow to clinically important size.
Calcium Balance in Pregnancy
Given high urine calcium losses, and a need for calcium to make a fetal skeleton, what happens to maternal calcium balance? Does the mother’s skeleton need to lose a lot of its mineral for the fetus? Is absorption from food and vitamins so high that her skeleton is spared?
Measurements
Scientists measure total body calcium balance as the difference between diet calcium absorbed (horizontal axis on the graph below) and calcium lost in the urine. Net calcium absorption is the difference between calcium eaten and that lost in the stool. A single balance requires about 6 days in a clinical research center, so balance measurements are a precious legacy.
I gathered available balance data for pregnancy, children, hypercalciuric stone formers and normal men and women form the original research papers – a never again effort! Although unforeseen events damaged the collection, I salvaged figures made from the original data sets.
How to Read a Balance Graph
Being the difference between diet calcium intake minus stool calcium loss, net calcium absorbed can be above or below 0 the vertical line. The double horizontal line at 300 mg/d of urine calcium represents a very high stone forming value.
The slanting line marks identity between net calcium absorbed and urine losses. To the left of that line, urine calcium exceeds calcium taken in through the intestines – bone mineral loss. To the right of the line, net absorption exceeds urine loses, so bone has gained mineral.
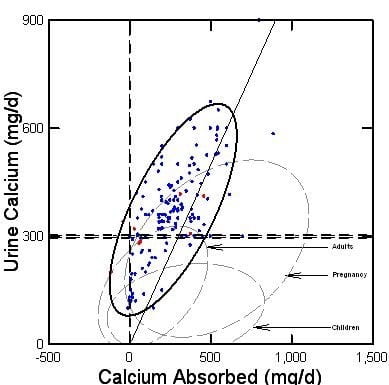
Normal Adults
The dashed outline at the arrow labeled ‘Adults’ is the 95% ellipse of containment for the data points for normal adults (the points are not shown to preserve visual clarity).
The line of identity bisects the normal ellipse, because normal young – midlife adults neither lose nor gain bone mineral on average so their points will scatter about the line of identity – zero mean change in bone mineral.
Hypercalciuric Stone Formers
Because idiopathic hypercalciuria has always been my main emphasis, I filled in all the data for this group. The dark solid outline is the 95% ellipse of containment. Data points for women (red) and men (blue) fall mainly above normals, and to the left of the line of identity meaning urine calcium exceeds total calcium intake and bone is losing calcium on average. This is one probable reason why stone formers are at abnormally high risk for fracture.
Pregnancy
The 95% ellipse for pregnancy (labeled by an arrow) bulges upward and to the right of the line of identity, showing that urine calcium is higher than in normal adults but GI absorption is so much higher that most of the women are in positive calcium balance – only a small part of the pregnancy ellipse is left of the slanting line of identity.
The positive balance of pregnancy is mainly calcium retained in the fetal skeleton. Maternal bone balance cannot be isolated, and can be negative of positive depending on calcium intake.
Children
Children are remarkable for their very low urine calcium losses given net absorptions that exceed normal adults and rival pregnant women. Bone actively takes up calcium as it grows.
What Links Stones to Preeclampsia?
Although the various studies list gestational diabetes, preeclampsia, oligohydramnios, preterm delivery, HELLP and eclampsia, all but gestational diabetes are part of what one might call the preeclampsia syndrome of linked abnormalities.
Main Risks for Preeclampsia
Obesity and Pre-gestational Diabetes
A large survey of all preeclampsia risk gleaned individual risk ratios from between 1 and 40 different studies, often involving millions of people (3 – 5 million for BMI, 6 million for hypertension, just under 1 million for CKD).
Of the main risks, overweight (BMI >25<31) risk ratio (RR) was 2.1 (95% CI, 2 – 2.2) and obesity (BMI>30) 2.8 (2.3 – 3.1). An extensive modern meta-analysis, gives a similar ratio for overweight 1.71 (1.52 – 1.91) and obesity 2.48 (2.05-2.90).
Diabetes is powerfully linked to preeclampsia RR is 3.1 (3.1 – 4.3).
Hypertension and Chronic Kidney Disease (CKD)
In the same large survey, chronic high blood pressure RR was 5.1(4.0 – 6.5) and chronic kidney disease (CKD) was also significant – 1.8 (1.5 – 2.1).
Kidney donors also have increased preeclampsia risk. Among 85 donors vs 510 normals during an 11 years median followup, donor age 29, incidence of preeclampsia was 11.5% in donors vs 4.8% in controls, RR 2.4 (1.2 – 5), p<0.01. This is not remarkably different from the value in the large survey of 1.8 for CKD.
Kidney Stones Associate with high blood pressure and Kidney Disease
Several articles on this site document that kidney stones associate with high blood pressure, and with kidney disease. The causes of these linkages are presently unknown. One is tempted to say that both reflect the association between kidney stones and obesity and diabetes, detailed just below. But I think that recurrent stone obstruction may also play a role, as each such causes what amounts to single kidney acute renal failure.
Likewise, the odd high density of papillary tissue may be an important – and overlooked – clue because it is present in stone formers even before stones begin and is certainly abnormal.
Kidney stones Associate with Obesity and Diabetes
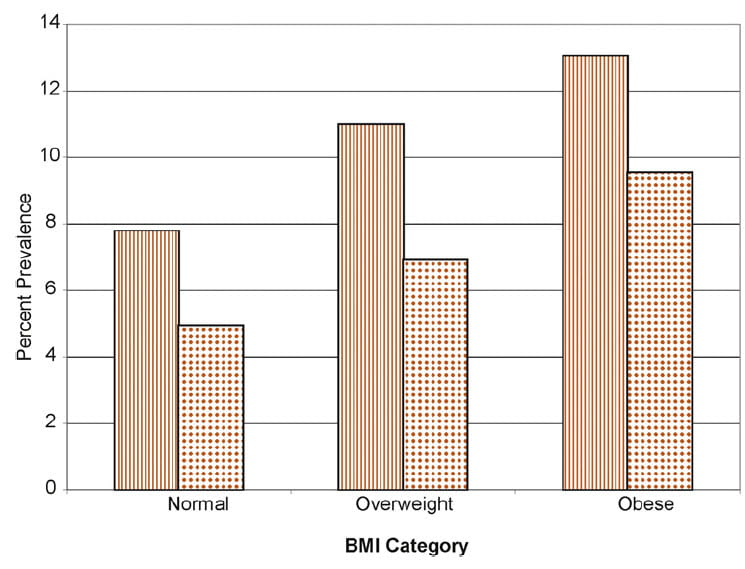 Using NHANES as in the prior analysis of the link between pregnancy and stones, Scales and colleagues found a clear link.
Using NHANES as in the prior analysis of the link between pregnancy and stones, Scales and colleagues found a clear link.
Among men (vertical stripes) and women, the percent prevalence of stones in the population sample rose progressively with overweight and obese categories vs. normal BMI. If normal BMI is taken as the reference, the RR for overweight is 1.29 (0.96 – 1.72, p=0.088) and for obese is 1.55 (1.25 – 1.94, p<0.001).
Diabetes raised risk as well, multivariable RR was 1.59 (1.22 – 2.56, p<0.001) as did gout RR = 1.92 (1.44 – 2.56, p<0.001). But complexity lurks here as gout is likely to relate to uric acid stones, and reduced kidney function.
A recent review expands this one report by adding all such up to 2018 and presents much the same results I do not detail here.
The study of Taylor et al deserves detailed review as it arise from prospective observations of three cohorts, 2 female, and is perhaps the most compelling of its kind.
Among men, given a referent of BMI at 21-23, a BMI of 21 had a stone RR of 0.73 (0.52 – 1.03). Between BMI of 25-27 the RR was 1.1 (1.02 – 1.41); between BMI 27-29, RR was 1.24 (1.03 – 1.5) and for BMI of 30 or more RR was 1.33 (1.08 – 1.63). For women, same ranges of BMI, values were higher: BMI 25 – 27, RR was 1.34 (1.13 – 1.59); BMI 27 – 30, RR was 1.75 (1.45 – 2.1); for obese, BMI >30, RR was 1.9 (1.61 – 2.25) – I used only one of the two female cohorts, as the other was much the same.
Another set of data one must detail is from the Women Health Study. Given a referent of BMI 18.5-24.9, overweight RR was 1.3 (1.17 – 1.44), obese RR 1.62 (1.43 – 1.83) and BMI >35 RR was 1.81 (1.57 – 2.10). These are very close to the NHANES and Taylor results.
In every study stones follow obesity like a shadow.
Summary
Hypertension, CKD, obesity, and diabetes are prime risk factors for preeclampsia and all four are associated with kidney stone disease.
One must presume it is this series of associations that links stone forming to an abnormally high risk for preeclampsia. The mechanisms between these major diseases and stones have had far too little research thus far, and too little attention – in my opinion – from NIH funding agencies.
Stones that manifest during pregnancy cause problems that are easier to understand. Infection and need for surgical stone management are clearly causes of premature delivery and low birth weight infants.
What Should Stone Formers Do Planning Pregnancy?
Stone formation should not hinder any woman from undertaking pregnancy. But they and their physicians need to be careful about gestational diabetes, kidney and urinary tract infection, spontaneous abortion, preterm delivery, and preeclampsia.
Since all are the familiar territory of obstetrics practice, none should pose special issues for management. But even so, one may take away from this article that patients need be aware of their increased risk and work with their physicians to minimize adverse outcomes.
Bring BMI As Close to Normal As Possible
One can argue strongly for efforts to keep BMI in a healthy range in all people, but perhaps especially in stone formers planning pregnancy. High BMI raises risk of preeclampsia. Because on average BMI is higher in stone formers, they might want to pay especial attention to this matter.
Lower Blood Pressure
Weight loss to normal BMI lowers blood pressure. So does low diet sodium (ideal is 1500 mg/d) and high diet potassium (ideal is above 4000 mg/d from foods). Aerobic exercise lowers blood pressure. You train for marathons, why not train for pregnancy? Go in as fit as possible.
Minimize Stone Events During Pregnancy
One can also make the case that management of existing stones may be affected by planned pregnancy. Depending on the circumstances, one might elect to time needed stone removals before pregnancy occurs. Certainly, stone prevention is of highest benefit before pregnancy to minimize risk for forming new stones that might pass during the pregnancy.
Minimize Urinary Tract Infections
Stone formers have a lot of pathways to UTI. No one paragraph, no one article can cover all the possible issues, but an outstanding cause is stone surgery.
So, stone prevention seems paramount. Stones you do not form are stones that do not require a surgical procedure.
Planning pregnancy: Do everything possible to prevent new stones – everything.
If infected, ask your physicians to do their best to eradicate it promptly.
Infected stones are probably best removed before pregnancy, though I know of no trials to support this point.
What Should Stone Formers Do During Pregnancy?
Never Miss Routine Appointments
Blood and urine testing, and blood pressure testing need to be done on schedule in all pregnancies, but especially when risks are higher than normal. This is almost too obvious a point to make.
High Calcium Intake
Calcium balance in pregnancy depends on high calcium net absorption, so there is no case to be made for limiting calcium intake while pregnant. Urine calcium will be high during pregnancy and cannot be lowered. All modern pregnancy care employs proper calcium supplements, and they are appropriate for stone forming patients. Evidence exists that high calcium intakes during pregnancy may reduce risk of preeclampsia and not increase risk of stones.
Be Wary of Obstruction
Stones obstruction can damage kidneys if left unattended. Pregnancy causes a lot of background aches and pains and distractions, in the midst of which subtle symptoms of an obstructing stone might be missed. Ultrasound is safe and effective diagnostically in pregnancy, and can be done after any hint of an obstructing stone. Experienced stone formers know stone pain even when mild. Specialized MRI urography can help distinguish stone obstruction from the normal pregnancy dilation of the urinary tract
Not only is obstruction a danger to the kidney, but loss of function of a kidney might cause other special problems in pregnancy such as rising blood pressure.
Maintain Hydration to Prevent New Stones
Pregnancy is a stone forming state, as I showed in this article. Any new stones from a pregnancy can raise risk during subsequent pregnancies.
Within the limits imposed by pregnancy a good urine volume, above 2 liters daily, is about the only stone risk reduction available. Changes in diet, and diet restriction may not be safe, and should be undertaken unless supervised by the physicians responsible for the pregnancy.


Dr. Coe, Since pregnancy can increase urine calcium and PH do you think the long term use of oral contraceptives could also increase urine calcium and PH? I just wondered if there is a connection since both pregnancy and OC’s are hormone related. Thank you-
Hi Diane, No. It is pregnancy. Fred
Can K Citrate be continued during pregnancy?
Hi Bernard, It would not be ideal in most cases as the rise in urine pH is not likely to be balanced by a rise in citrate so CaP SS will probably rise. I know of no contraindication to K citrate during pregnancy. Fred
Dr. Coe,
Could you comment on the use anti-calciuretics (such as thiazides and/or ENaC inhibitors) and citrate pharmacotherapy during pregnancy for those stone formers on these meds pre-pregnancy (ie continuing the meds) or a new stone former during pregnancy that may have other indications to start these medications (such as gestational hypertension)?
Thanks.
Hi Dr Knohl, Thiazides are labeled Class C during pregnancy – poor data, possibility of harm. Potassium citrate should be benign, and I do not know of any guidelines concerning it. Regards, Fred
Dr. Coe, postpartum women are advised to continue taking their pre-natal vitamins after giving birth, especially if breastfeeding. Since prenatal vitamins have high concentrations of calcium, should women who formed stones during pregnancy discontinue taking prenatal vitamins? Does the advice change if the woman does not have a history of stone-forming (stone in pregnancy was first)?
Hi Sarah, NO, they should not. It is after pregnancy that calcium absorption falls, so you need a lot of calcium to rebuild bone. If breast feeding it is even more important – all the calcium in the milk has to come from what you are eating or from your bones. Take the supplements. Regards, Fred Coe
Hi Dr. Coe, my stones started during pregnancy. 100% carbonate apatite — bilateral and recurrent. I’ve had 2 litholinks and I have decreased my sodium as you recommended on another thread. I have included my most recent LithoLink “Interpretation” section as I am pretty lost. My current Nephrologist is not recommending any further testing despite these results. What are your thoughts? Thank you!!!
Section Level 1/21/23 5/19/22
Summary Stone Risk Factors
Urine Volume 3.25 2.24
SS CaOx 1.65 3.21
Urine Ca 137 246
Urine Oxalate 21 22
Urine Citrate 667 518
SS CaP 0.87 2.08
24hr Urine pH 6.656 6.806
SS Uric Acid 0.15 0.13
Urine Uric Acid 0.884 0.789
Dietary Factors
Na 24 113 247
K 24 66 96
Mg 24 84 82
P 24 1.094 0.958
Nh4 24 25 23
Cl 24 95 252
Sul 24 33 39
UUN 24 10.72 9.89
PCR 1.1 1
Normalized Values
Cr 24 1434 1223
Cr 24/Kg 19.9 15.9
Ca 24/Kg 1.9 3.2
Ca 24/Cr 24 95 201
Interpretation of Results from LithoLink Directly:
Urine pH remains very elevated. Despite high urine pH, calcium phosphate stone risk is not elevated. High urine volume is protective and should be maintained.
Uric acid excretion has risen moderately. is significantly elevated, and can promote calcium oxalate stones (was 0.789 and now is 0.884 g/d). Hyperuricosuria almost always arises from high intake of animal protein that contains purines fron DNA and RNA in tissues. Our records do not report that allopurinol has been prescribed. Protein intake is not high enough to explain persistent hyperuricosuria; PCR is less than 1.3 (1.1 g/kg/d) and urine sulfate excretion is less than 70. Consider unusual high purine food sources such as nuts and seeds. Medical nutritionist help might be of value in this unusual situation. Rare hereditary causes of uric acid over production need consideration, as do states of increased DNA turnover from cell proliferation (e.g. lympho-proliferative and myelo-proliferative states).
Hi Britt, Your urine calcium varied with your urine sodium (diet sodium) and the higher value is high enough to raise stone risk. SO you should keep your diet sodium closer to the low than the high value. YOur urine uric acid is rather high and so is your protein intake and the latter can raise urine calcium but not stone risk. Phosphate stone formers have their own issues but in your case pregnancy supplements and underlying genetic hypercalciuria might have started things off. Right now your stone risk is low when your sodium is low, which is presumably why your physician is not doing more. Regards, Fred Coe
For a recurrent stone former who wants to be pregnant, what do I tell her about her risk of kidney stones during pregnancy? Will it be higher in the 2nd or 3rd trimester?
Hello Dr, I could find this information when I wrote the article. Because urine calcium rises very early in pregnancy I would suspect stones can occur throughout. Of course the main complications occur in the later pregnancy – prematurity, preeclampsia, etc. Regards, Fred