
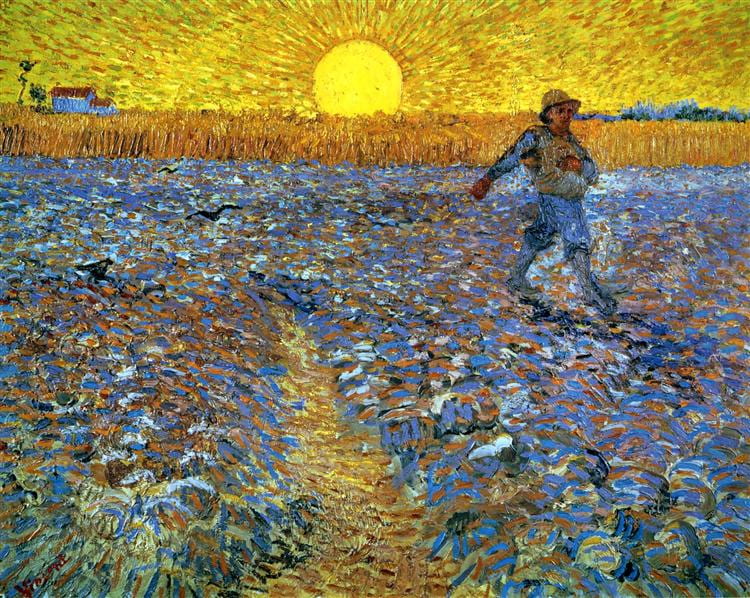
The painting by van Gogh, The Sower with Setting Sun (1888) Kroller – Muller Museum, Otterlo, Netherlands, has no obvious connection to this article unless you have read Nellie Hermann’s essay on the former mining district of Belgium called the Borinage. Writing in the Paris Review, she reminds us van Gogh lived there in the 1880’s amidst active coal mines now long obliterated.
He based his painting on an earlier (1850) painting, The Sower by Jean-François Millet (1814–1875). The artist sold it in 1851 to William Morris Hunt (1824-1879), Boston, where in 1917 Quincy Adams Shaw, Jr. (who inherited it) and Mrs Marian Shaw Haughton donated it to the Boston Museum of Fine Arts where it resides. It seems unlikely van Gogh ever saw the original but only copies.
an earlier (1850) painting, The Sower by Jean-François Millet (1814–1875). The artist sold it in 1851 to William Morris Hunt (1824-1879), Boston, where in 1917 Quincy Adams Shaw, Jr. (who inherited it) and Mrs Marian Shaw Haughton donated it to the Boston Museum of Fine Arts where it resides. It seems unlikely van Gogh ever saw the original but only copies.
Millet painted in France, and van Gogh appropriated the lush fields into this painting that he made in a simple wood house facing an active coal mine.
There are, of course, no mines or mine shafts in either painting, nor a canary, just the brilliant yellow of the van Gogh and the place he painted it in with its dangerous and decaying mines. He wrote “This mine (Marcasse) has a bad name because so many die in it, whether going down or coming up, or by suffocation or gas exploding, or because of water in the ground, or because of old passageways caving in and so on. It’s a somber place, and at first sight everything around it has something dismal and deathly about it.”
Why Write about Canaries, and Mines?
Canaries Signalled Danger
Mine gases – lethal from inhalation or explosion – killed caged canaries before they killed people. So the birds stood as warnings, if ill or dead. The use of canary birds may have originated from the advice of John Scott Haldane who first identified carbon monoxide as a major toxic mine gas.
Stone Forming Seems to Signal Danger from Other Diseases
In a simpler time, when stone formers were just people who formed kidney stones, we had no need for metaphor or simile. They were what we saw them do, and we strove to stop their doing it.
We now know much more.
Stone formers are at increased risk of bone disease, hypertension, kidney disease, and vascular disease.
Almost no one, myself surely, has any reason to believe that for the most part all of this extra burden of disease arises simply from formation and passage of stones. While it is possible that inflammation and injury from stones leads to smoldering kidney disease and thence to vascular disease, even one stone raises risk for hypertension. And bone disease is often found when kidney function departs in no way from normal. Many, myself included, believe idiopathic hypercalciuria causes bone disease when diet calcium is inadequate, but there may be other reasons as well.
A Small Part is Obvious
Systemic Diseases Cause Stones
Well known systemic diseases cause stones and additional systemic diseases. Primary hyperparathyroidism is perhaps the most obvious example. It can evade detection, raise blood pressure, damage kidneys, and demineralize bones. Renal tubular acidosis, and myriads of rare hereditary kidney diseases cause stones, kidney damage, and bone disease. Varieties of bowel disease, including obesity surgery cause stones and can cause kidney disease. Cystinuria causes stones and is, like RTA, a kidney disease in that major transporters are abnormal. Hereditary hepatic enzyme defects cause primary hyperoxaluria that often leads to dialysis and transplantation. Defects of hepatic CYP24A1 can cause extreme hypercalciuria.
We have well established panels of testing for the purpose of screening, and good guidelines to proceed to diagnosis and specialized treatment of all of these important causes of stones. One might say it is unusual for any physician to miss a systemic cause of kidney stones, or to fail of proper treatment. So while systemic diseases might contribute to the linkages between stone forming and kidney, bone, and vascular disease, they are a minor part of the whole, and we have excellent means for dealing with them.
Uric Acid Stones
These occur when urine pH is too low, and very often that low pH arises from diabetes or a complex disorder of acid base balance. Patients are often obese. Older people predominate, and they suffer from the effects of age. So for many reasons, uric acid stones and vascular, kidney, and bone disease would appear to coincide. Even so, uric acid stones represent perhaps 10% of the total stone population, and are not a likely reason for the population wide linkages observed between stone formation and hypertension, and kidney, bone, and vascular disease.
Struvite Stones
Struvite stones arise from infection with urease possessing bacteria, and can injure kidneys because of their large size and the infection itself. They are a minority of stones, and like uric acid stones unlikely to have caused the disease linkages I have already mentioned.
The Large Part Is Not Obvious
It is among the majority of people who form stones, so called idiopathic calcium stone formers, that epidemiologists have discovered links to vascular, bone, and kidney disease, and their discoveries are puzzling and call for new thoughts about mechanisms and what they might mean for patient care.
Stones Seem a Biomarker for Other Disease Risks
One way to respond is surveillance. Those who form stones have called attention to their increased risks, and deserve a higher than usual surveillance for the diseases those risks represent and also whatever we can do to reduce risk. That is a proper clinical response, and I advocate for it.
Perhaps Diet Promotes Stones, and Cardiovascular, Renal, and Bone Disease
A more subtle response might concern why all these risks associate with stones, and what that association could mean. Do all the recent evidences of disease risks, though each one modest, support a new direction of thought concerning what appears to be a manifold of disease linkages?
I have written a lot on this site about how high diet sodium, low diet potassium, excess protein loads, and refined sugars can promote stone formation by raising urine calcium and reducing urine citrate. Likewise, many have put forward substantial evidence that low calcium diet can cause bone mineral loss with especial vigor in people with idiopathic hypercalciuria, a common trait among stone formers.
Other research communities have ample evidence that high diet sodium and low diet potassium contribute to hypertension.
Likewise, obesity is linked by epidemiological data to increased kidney stones, and also to cardiovascular and kidney disease, and to diabetes, itself a major cause of both. While explained by no single cause, the modern acceleration of obesity surely arises in significant measure from population wide increase in fructose consumption from common table sugar, and sweetened beverages. We also know that modern recommendations to increase diet calcium aim at reducing onset of osteoporosis.
In other words, our modern diet predisposes to kidney stones via mechanisms specific to stone formation and to renal, vascular, and bone diseases via mechanisms specific to those diseases. This simply leads one to recommend improved diet for all US people, which is exactly the burden of our government’s message.
Perhaps Not All People are Equally Susceptible
But only some fraction of people who eat too much sodium, too little potassium and calcium, too much refined sugar, or just too much altogether develop any obvious disease. Many escape, meaning they are relatively less vulnerable to obvious risk factors that in other people cause manifest disease. For example, average diet sodium consumption is about 200 mEq/d, double the tolerable upper limit, but large numbers of people do not have hypertension. Likewise, only some people develop osteoporosis despite a population – wide calcium intake viewed as below ideal. Well known, a majority of hypercalciuric people do not form kidney stones. In fact, it is this very remarkable variability that has always made diet recommendations so difficult. If a given diet universally caused disease, diet planning would be far more simple than it is.
Could These Diet Vulnerabilities be Linked?
Presumably, stone formers are more vulnerable to diet than the average person and therefore form stones.
What if that increased vulnerability to diet is linked across stone forming, hypertension, vascular disease, kidney disease, and even diabetes?
In other words, what if stones give an obvious sign of an abnormally high diet vulnerability to more serious, if initially less obvious diseases?
Put as crudely as possible, perhaps stones are a biomarker for increased susceptibility to other far more sinister diseases from our common and unhealthy diet.
If This Were True
Primum Non Nocere
When you combine this enduring precept with my speculation that stones mark for manifold disease susceptibilities from diet, we get a basis for action. If Improved diet for a stone former might help reduce not only stones but an abnormally high risk for a manifold of diseases, to omit efforts at diet improvement for stone formers is, so far as we can presently tell, to do harm.
Harm arises not only because of stones – we possess other treatments to prevent stones. But because we suspect stones mark abnormal vulnerabilities from diet to a wider and more dangerous group of diseases.
Therefore, safest is to alter diet in those directions that decades of research have established as reducing risks for stones and for cardiovascular, renal and bone disease. Here in the US we have remarkable amounts of research available concerning how to eat in a healthy way.
The precept to avoid harming patients is, incidentally, of unknown origin, and appears to have been promulgated mainly orally. Its use in the US originated – according to this scholarly article – in the early 19th century. It is surely not from the extant works of Hippocrates.
Correct the Diet or Get Someone to Correct It
The kidney stone diet, my name for what is in fact the US ideal diet according to the vast assemblage of experts who create the US diet guidelines, can reverse many crucial urine stone risk factors, and has one excellent trial. It is safe, effective, and might well reduce risk for kidney, cardiovascular, and bone disease in this specially vulnerable population.
It Synergizes with Other Stone Preventions
The high diet calcium in the diet lowers urine oxalate markedly, saving patients much of the onerous bother of following oxalate lists to their final detail. The lower diet sodium reduces potassium wasting from thiazides, should they be needed, and the high potassium in fruits and veggies provides potassium repletion.
It Directly Benefits Patients and their Families
High diet calcium helps preserve bone mineral. Of course a high potassium low sodium diet is against hypertension, and the high potassium foods are a source of alkali that functions exactly as would potassium citrate supplements.
Less refined sugar will reduce spikes of calcium, and the Stanhope trial has proved that fructose – 1/2 of table sugar – causes insulin resistance in normal people in only 8 weeks and is therefore a powerful drive toward diabetes.
Moderation of protein can prevent unnecessary high urine calcium levels caused by protein mediated increases of diet calcium absorption and perhaps protein based acid loads.
Given that stone forming is strongly heritable, diet changes in one family member that spread to others around the table may help lower their risks of stones and its associated diseases. This could be especially important for children.
Four Brief Precepts
Here are some ways of making my one point within a few of the common situations we all encounter.
Change Diet First
Because to neglect diet is possibly a harm, always begin with diet change and do as much as possible. High fluids are fine, meds are fine, but to me should be on top of a proper diet, as needed.
Shun ‘Just Drink More’ as a Sole Treatment
It will not do to just push fluids in hopes stones will stop. They may well stop, and even so the patient remains incompletely treated.
A large trial of just water seems inevitable, however odd one might think such an expense of money and spirit. It will of course reduce stones. We must not let that distract us from what else we need to do.
Shun Pills and Remedies as a Sole Treatment
LIkewise for thiazide or potassium citrate or both together. They may work well and, as with fluids alone, risk remain for other disease because we did not correct the diet.
Multiple companies presently plan new drugs to reduce urine oxalate excretion. I hope they emerge from research into practice, and help in stone prevention. But the same for them. Lowering urine oxalate will not by itself correct the diet, and if the diet causes multiple disease it will remain a hazard.
Pills are great, new pills, too, but the diet remains an untreated potential menace the pills may not counter.
Shun Single Diet Changes as a Sole Remedy
The almost universal diet oxalate list will not do either for stones or the disease manifold. Likewise for piecewise suggestions like ‘eat less salt’. As for drinking lemon juice, and all other well intentioned nostrums, consider them just that. We need to change the diet to the US healthy people diet. To the diet we should eat, all of us.
I Know We Lack Proof
I do not write as if I knew that diet is the reason for the many increased disease risks of stone formers. I do not know this. It is speculation at this time.
But the speculation leads to a potentially useful interim approach to stone forming patients that is itself likely to do more good than harm for everyone, patient or not. While we wait on the slow progress of science, we can act toward a larger health aim than stone prevention alone by taking literally the idea of ‘Primum non nocere‘.
I am no therapeutic nihilist, in theory or practice. I do not advocate we give up what we have by way of useful treatments against stones. I merely mean to say that preventing stones per se is not a complete goal in stone formers given what we now know.
Speculation is the Forerunner of Hypothesis
The idea that stone forming marks abnormal diet based vulnerability to a manifold of diseases is speculative, and as such the earliest stage in science. But though early and prone to eventual disproof, the speculation leads to useful suggestions for physicians.
My Speculation Fits What Has Been Observed
In the 14th century, speculate meant intelligent contemplation, a meaning consistent with its Latin root specere – to look at or view, and its Proto-Indo-European (PIE) root “spek” – to observe. Speculation as something ‘mere’ arose a century later, an idea disjunct from the root source.
If we are to remain true to the word, we have to contemplate what we have, and reason accordingly. Right now nothing obvious contradicts the speculation of diet vulnerability to a manifold of disease, so it is a basis for action until we have better.
Hypothesis Surpasses Speculation, but Time Runs On
Hypothesis, speculation’s successor, consists not only in our viewing the world intelligently but in imagining the causes of what we know and can observe and fashioning experiments to test the imagined causes. For example, the brilliant experiments of Kimber Stanhope tested the imagined effects of fructose to cause insulin resistance and de novo increase in hepatic lipid production, two key mechanisms through which sugar can cause vascular disease, obesity, and diabetes.
We need this kind of science for diet change in stone formers, but it will take a while to get it done.
We Can Act While We Wait
Given that diet change has no harms, and lack of change has possible harms, I am opposed to waiting, perhaps for years, until – if ever – we have proof in stone formers of benefit. Decades of study point to proper diet structures, and all I call for is that we deploy them for our patients.
I Know Diet Change Is Difficult
Once people have dangerous disease, physicians expend considerable money and time on diet. For example Stage 4 CKD is a time for concern about diet potassium and phosphate. Dialysis even more so; great efforts are warranted to control excessive fluids or sodium, and especially potassium. When bones fracture from idiopathic hypercalciuria or other forms of osteoporosis, very costly drugs are appropriate, and calcium supplements. For diabetes with nephropathy and retinopathy and neuropathy we spare no amount of time and cost on expensive treatments.
But skill is late. Long before, when organs and tissues function well, that is when we can get the most benefit from diet change. If indeed stone formers have even modest excess risk for these terrible diseases, and the very same diet that can reduce their stones can reduce these other risks, how else can we better manage things than by using diet – whatever the difficulties.
Closing Repetitions for Emphasis
If it is a reasonable speculation that stones mark out those who cannot tolerate our modern diet without increased risk of serious disease, then it is harmful to elide diet efforts, to put away the trouble of diet counseling against new stones. If sensitivity to our modern diet causes stones as part of a manifold of disease, we need to assume that a diet that reduces new stones has the potential to reduce risk of the other diseases in that manifold.
I propose it is proper to use whatever we have to prevent stones, but always to correct the diet in a direction aimed at that same goal – stone prevention, because it may be that other systemic diseases may be avoided or minimized, or delayed through that one therapeutic effort.
I would deny no one my most passionate efforts to improve diet according to what we know presently as sound until science’s superb surprise enlighten us as to the final truth of the matter.

Your warning about connections between stones and other health problems fits my family history.
What specific “healthy” foods would help, considering that so many (eg, leafy greens, nuts, beans, whole grains, berries, figs, etc) are on the oxalate warning lists?
I have had at least 6 painful stones over 19 years; the latest was yesterday.
I prepare almost all meals for my family and me, but choosing my foods has been a big problem.
Hi Susan, The kidney stone diet is our best on this. It certainly does not eschew veggies! Take a look. Regards, Fred Coe
Thanks for writing this excellent article on diet and kidney stones. I have always been a believer that a healthy diet can help you avoid, treat or even heal many diseases. Thanks for reminding us that we have another important tool in our tool box to keep us healthy whether we are stone formers or not.
Hi Kim, Thanks for your lovely note. Fred
Dr. Coe:
Always good to receive and read your emails and articles.
It might be helpful sometime if you would include a link or information on the diet that stone formers should follow.
Thank you very much for your writing and for your work.
Ted
Hi Ted, Thanks for asking. Here is my kidney stone diet. It is very close to the US ideal diet, and frankly all of us should eat it. Regards, Fred Coe
Hi Dr. Coe, I am your patient and have worked with Melanie for my diet. I have been decreasing my protein to 45-60 mg/ day. My protein intake previously was much higher. I understand now that lowering my protein will aid in less calcium loss in the urine. Is there any negative effect of limiting diet protein such as less ability to build muscle?
Thanks
Hi Patti, Not unless you bring it down below 0.8 gm/kg/d and Melanie is not going to do that. As you are my patient, please feel free to also email me personally or through Karen. Best, Fred Coe
What a beautiful & sensible piece you have written here Dr. Coe. As you point out, there are so many things a good diet promotes besides fewer stones. Many physicians are silent on the subject, and have no strategies to offer their patients to help make it easier to transition out of their addiction to sugar & processed food. How do we get the AMA treatment protocols changed? Going “cold turkey” for many people is just too hard – reducing a little at a time and learning how to cook healthily instead of grabbing fast food would be a good first step? Perhaps there are already nourishing healthy frozen dinners with reasonable levels of salt, sugar, protein, etc.? I skip that aisle in the grocery store so I don’t know. Unfortunately, for many people, not having to cook is an important goal. As you know, the big picture is pretty complex, as reducing the chemicals, pesticides, etc. in foods, the soils, etc. may well play also a role for scientists trying to prove healthy diets prevent disease, e.g. research on “red” meat does not usually use grass fed, hormone and anti-biotic free steers. Keep up the good work. We need more voices in medicine such as yours.
Hi KD, thanks for your thoughtful note. The kidney stone diet itself, like the ideal US diet is simple in a way and rather difficult, for many of the reasons your bring up – cooking, shopping etc. Perhaps the best way is to tackle one item at a time. I did sugar, for example. I am lucky in that my wife does not like a lot of salt, nor so I. I have never thought about strategy, and perhaps this one is not bad. Best, Fred Coe
Dr. Coe,
Excellent, relevant, eye-opening paper. I am 6 days s/p double knee replacement. Surgeon “worst arthritis I have ever seen in my career.” Bone on bone. I have had stones for 20+ years. On March 7th, I had a percutaneuous nephrolithotomy for a 2 cm and 1.5 cm stone in my left kidney. Prior to the knee surgery, I sent my 24 hour urine to Litho in Chicago. Normal oxalates with phenomenal urinary Ca++ level (over 500). My stones were Calcium Oxalate. I hope this information is helpful. My hypothesis: arthritis = bone on bone degradation = elevated serum levels, maintained and controlled by kidney function. (Serum Ca++ normal). Your thoughts or FYI.
Hi Karl, The urine calcium is remarkably high and stone prevention obviously not controlling it. Given so many stones, I would surely want it 4 times lower. I do not think the high calcium loss affected your knees because the problem there is cartilage and ligaments, neither responsive to calcium balance. The high urine calcium is either idiopathic hypercalciuria or perhaps Cyp-24 mutations. Try to work with your physicians towards lowering it. Regards, Fred Coe
Last November 14, I went through a major ten hour surgery to reconstruct my lower spine, correct a serious tilt of my spine forward and to the right and stabilize everything with new rods. To do this they had to break through a former fusion, remove a set of rods and carve a precisely shaped wedge out of my fifth lumbar vertebra. Then surgery was successful, but the recovery was long and difficult. Because of numerous drug allergies, I was limited to a regimen of morphine and Tylenol for pain relief. I was on morphine for three months. The effect of high pain levels and morphine was to diminish my appetite to practically nothing. I had to force myself to eat even small amounts of food. I shifted to very simple meals, much less sugar (which became repugnant) and very little salt. Even after I was off of the morphine, my appetite did not and has not returned to former levels, nor has my sugar consumption. The result has been incredibly dramatic. Over the last six months, I have lost 60 pounds, dropping from 282 to 222. I am still slowly dropping, though my primary thinks I am at about the right level, I would like to get down another 10 pounds or so. I way less right now than at any point since I was in my early 30’s. I am currently 74. A Type II Diabetic, I had been using 100 mg of Januvia and 72 units of Basaglar on a daily basis. I am now at 50 mg of Januvia, which we may drop altogether, and at 20 units of Basaglar. My A1c is at 5.6. It had been at 6.8 for several years running. I have been a daily chronic stone former – both Uric Acid and Calcium based stones – for five years, with no breaks from stone production during that time and three surgeries to deal with kidney or ureter blockage during that time. I often passed stones up to 10 mm in length, though much of my daily production was considerably smaller. I’ve incorporated a lot of water and lemon juice into my diet, but it has always been clear that I have a serious malabsorption problem. I have Celiac Disease and Multiple System Atrophy, both of which have impacted the way I absorb nutrients. I also am lactose intollerant – not severely, but enough to limit my dietary calcium intake. Another after effect of the surgery combined with malabsorption was an increase in my chronic anemia, dropping my hemoglobin level from a typical 12 to 8.6. When that did not rebound, they decided to try iron infusions which have raised my hemoglobin level by 1 point so far. Whatever develops on that front, the overall impact of my dramatic change of diet and sugar consumption has clearly had an impact on weight, blood pressure, blood glucose levels and kidney stone production. I still produce stones from time to time – say once or twice in two weeks, but that is a huge difference from hundreds of stones daily. You wrote to me some time ago about working on dietary changes. I was somewhat at a loss for what to do, but morphine and pain did a good job of forcing the issue. I believe you are definitely on to something in terms of diet. Thank you.
Hi Louis, Thanks for the note. Diet does work, but I am sorry you had to do it in such a horrid way. When you are eating better, do consider 24 hour urine testing, and for the uric acid stones especially be careful about urine pH. I hope you fully recover, hemoglobin included, but keep the weight off. Regards, Fred Coe
Thank you for the article as your writing style is always fun to read! I was wondering if the intense focus on diet is the same even though I suffer from MSK?
Hi Cecile, Indeed the same. Firstly, many ‘MSK’ do not have that disease at all. Even those who do need to begin with diet. I would say, Do it. Regards, and thanks for liking my words. Fred
Stopped potassium citrate because potassium number went very high, now on sodium citrate, does this help, in formation of stones?
Hi Anthony, It depends on what you are treating. If it is to lower urine calcium, the sodium salt is not so good. If it is to raise pH to prevent uric acid stones, it should be fine. Regards, Fred Coe
Hello Dr Coe,
I am enjoying your articles and this web site so much. I do not have enough technical knowledge about my health, but can describe what has been my experience. I have been a vegetarian for over 35 years. There is little to no history of kidney stones in my family history. I.am now 55 years old, post menopausal, but struggling significantly with oxalate stones for the past three years. I have received three lithotripsy treatments, changed my diet to eat even more low oxalate foods and decreasing higher oxalate ones like my beloved beans, nuts, oatmeal and tofu. I have tested negative for hyperparathyroiism, and currently undergoing genetic testing for Primary Hyperoxaluria though genetic counseling doubts this possibility. My nephrologist has conducted 24 hr urine testing and the results are the same with high oxalate counts. Even with the addition of Whole Foods based calcium like whole milk, Greek yogurt daily, increased fluids, my urinary calcium increased causing hypercalciuria along with high oxalate. I was again at the ER today with eight new small renal stones, always in my right kidney, though now I am noting an increase in protein in urine, with upcoming kidney function tests to r/o early CKD. In short, I feel that I have been a very healthy person, no history of hypertension, diabetes, obesity, IBS, or IBD. I have hypothyroidism but have been successfully maintained on Synthroid for the past twenty years. In trying to find a cause for these stones, I am at my wit’s end, and maybe my nephrologist is as well! Please help with any suggestions you might have! Also, does your department offer nutrition counseling via internet consultation? It is so difficult to find a nutritionist who knows about oxalate diets.
With all my heart, I thank you for any and all suggestions, Dr Coe,
Christine
Hi Christine, I suspect you have some form of induced hyperoxaluria, either one of the primary overproduction states – PHI PH2 – or occult malabsorption – GI, pancreatic insufficiency. If your renal function is falling and urine protein rising it is urgent to figure out the problem and fix it. Fluids will not protect the kidney against oxalate injury, only against stones. Oxalate injury is far more complex than stones themselves. Here is a case that illustrates the problem – she had high oxalate because of obesity surgery that induced malabsorption, but the same can happen with anything that raises urine oxalate to truly high levels >8 mg/d. Regards, Fred Coe
Hello Doctor, I am a 22/M and about a month ago I went through the excruciating pain of a blockage from my first ever kidney stone. It is estimated to be 5mm and after the first week and then eventual ER visit, it has stopped causing me pain completely, however it remains in my distal ureter just about the UVJ and slowly headed down. My urologist said that Shock Wave therapy can not be performed, and this is really upsetting to me as after researching it is what I would HIGHLY prefer to have done. Do you believe that this is not possible where it currently is? Or do you think another urologist would be willing to try shockwave therapy?
Both the idea of ureteroscopy/stent or the likely return of that unimaginable pain once it reaches the UVJ are honestly really scaring me as all the pain medication they gave me at the ER did not help in the slightest and it continued for 8 hours. Do you believe that same pain will certainly happen again if it reaches the UVJ? Also if this info helps the stone is visible on X-ray, the urologist said the stone hadn’t moved since my last xray 3 weeks ago however the radiologists report said that it had moved 4-5cm down the distal ureter since the last xray and is above the UVJ.
Thank you for any advice you can give me, I really appreciate all the information and work you’ve put into this site.
Hi Dylan, The most important thing here is to avoid obstruction of the kidney while all this is going on. Your urologist is key for this and please do exactly as she/he recommends. If the stone is not obstruction but just moving, be sure and meet all recommended followup exams so its progress and the safety of the kidney are ascertained. If your surgeon needs to do a surgery, do it. Most important, when you are well get evaluated for cause and pursue prevention to avoid more of these things. Regards, Fred Coe
Hello Doctor, Thank you so much for the reply, I appreciate it a lot.
From everything I have researched I have not been able to find any reasoning for why I would not be a good candidate for Litho as I have a stone that shows up on X-ray and a 5mm stone has high success rates, nor have I read that stones in the distal ureter are somehow incapable of receiving SWL. I know you can’t judge or give any medical advice without seeing it all for yourself however generally are stones in the distal ureter capable of being “litho’d” if they are the right size and type? I most likely will try and seek out a second opinion if my doctor again declines the idea. I apologize if it’s a difficult question however I would really value your advice on litho and my situation.
Hi Dylan, You are right. Every stone is its own surgical problem. So in this case you need your surgeons to make decisions and I cannot be of much help. SWL can work in some of these cases, URS and even simpler means also work. But my only advice is your own advice to you: Get another opinion if you have doubts, and then you will be happier with your care. Regards, Fred Coe
Hi Dr. Coe,
I’m a former young (27) male patient of yours that had to unfortunately move away to Florida last August! I just wanted to say that the diet change + increased water intake has reduced stone events and pain significantly (although, I did have one unfortunate ER visit where I passed a stone).
There is an ongoing issue that I mentioned previously that you weren’t certain about during my last visit that maybe you could comment on. Perhaps there is more information now. There are the rare days where I don’t have easy access to water and typically have increased activity (lots of walking). On these days, I have guaranteed excruciating abdominal/flank pain + nausea from pain. If I sit down, the pain slowly subsides over a resting 10 minute period. However, if I start walking again it ramps back up within minutes back to the previous high degree of pain. Is there any possible explanation for this? My stone type when tested with you was Calcium Oxalate. I also had this issue way more frequently (between ages 16 – 25) before your diagnosis + lifestyle changes. Perhaps I have some long-term damage?
Thank you so much for your articles. I direct everyone I can to them when they mention kidney stones! I hope Joan is doing well!
Hi Austin, I suspect it is crystals forming. The posture effect is not obvious as to why, but the setting – Florida, less fluids, lots of walking, is crystal season. Try to take water with you. Lots of attractive water bottles are now on the market and some find them chic. Diet and fluid treatment is ideal but risky for obvious reasons, so do as much as you can to maintain fluids at all costs. Joan is well, and I will tell her you sent regards. All the best, Fred
Dear Dr. Coe,
I am a medical student on the east coast. I have been reading many of your articles. I very much appreciate your detailed writing of topics not otherwise easily approached. A favorite was the article on citrate. Just dropping this note to let you know that your work is appreciated over many distances!
Hi Craig, High praise indeed. The medical students I have taught are a tough bunch, so your note is a special delight. All the best, Fred
Dr. Coe,
They discovered a 1.3 CM stone in my left upper ureter on Feb 2nd causing blockage of my ureter with moderate hydophrenosis. I was in pain for a few days and then the pain subsided on its own. On Feb 21st I had ESWL procedure and passed a lot of fragments over the next week and a half. 167.0 mg of 80% CalOX Mono and CalOx Dihy with one 4.0 mg Uric Acid Stone as well.
I had another xray performed on March 6th that showed the stone was still in the same place and appeared just as large? Hard to believe considering how much I had already passed. Regardless, my doctor wanted to wait 3 more weeks to see if the rest would pass? I guess he did not feel the blockage was significant or still there?
After the three weeks I had another xray done and an ultrasound. Pretty much looks the same and in the same place. The ultrasound revealed cracks in the stone, but it also revealed mild hydroprehnosis. The left ureter jet is showing urine is still flowing past the stone and into the bladder, but the left kidney is retaining a lot of urine. My Dr. wants to act now and I had a complete urinalysis done, as well as BMP Serum, and CBC Auto Diff in prep for ESWL on March 27th. Everything came back normal, but I can’t get anything done this upcoming week due to the hospitals and Stones Clinics in New Jersey are shut down this upcoming week due to CoVid19. I do not know how long they will be shut down?
1. What can I do in the meantime to try to protect my kidney? As I said, some urine is still passing through the ureter jet into the bladder, but urine is backed up in the left kidney.
2. Is the left kidney still working under these conditions? Meaning, is it still filtering and producing more urine even though it is backed up, as the ultrasound is showing urine passing into the bladder via left ureter jet.
3. What is your best advice for me considering this scenario and in light of the closure of surgical centers in NJ at this time. My Dr just tells me if I have pain go to the emergency room.
I appreciate any insight as I am really feeling lost and so concerned as to what to do.
Hi Steve, It is indeed a vexing and serious issue. Your urologist is in a complex position. It is entirely up to him to protect the obstructed kidney, and if he fails to do the best for you it would be unfortunate for you and for him. Non critical surgery is in abeyance most places awaiting Covid to go away and that will not be for many weeks or more. If he believes your kidney is in jeopardy of damage from the stone then you are an urgent case and need surgery – it is then done most places. If he believes the kidney is safe, you and the surgery can wait. I would suggest you might want to have a frank and entirely objective – friendly – conversation about this issue, and I am sure he will act in your best interest. The other kidney always takes up the slack. Regards, Fred Coe
This sums up my frustration. First stone at 70. Don’t want another. Osteopenia x3 years. Overweight. Risk factors for HTN, NIDDM. Pain when walking from a bone spur and sciatica. I know being able to resume walking 2 miles a day would help this situation. . Trying to get PT for that part, but insurance cuts me off just when I feel I’m making progress. I’m working on diet as much as I can, but need sommeone to order the 24 hour urine. I live between Tampa and Orlando with Tampa being more accessible. Can you recommend a doc(s) who will look at this whole picture?
Hi Kim, Stone onset in midlife is a special issue – take a look. You are best off at the University of South Florida which seems nearer to you than other venues. I suspect you may have primary hyperparathyroidism, and it is best managed in a referral center. Regards, Fred Coe