
A Good Place to Start
The videos review the chapter and emphasize the main points. I would start with them.
Salt Ponds
The featured image shows salt harvesting from evaporation ponds.
The sea is salty and like our blood holds its salts in solution. But if you channel the sea into ponds, and balance things so the sun evaporates water faster than new water can enter, the remaining water overloads with sodium chloride. It crystallizes out of solution as sea salt. Workers collect it for us to season our food with.
Is it not an apt picture?
Our Blood is the Sea, our Kidneys Make the Pond
Mostly the Salts Stay in Solution
Our kidneys filter the salts and water of our blood into their millions of fine tubules. Like the sun they take back the water, unlike the sun they also take back much of the salts.
Mostly they are balanced, these takings back, so the final urine can dissolve its salts.
Stones Arise from Imbalances
If you ask me to say what makes stones form, I must answer that something has disturbed the balance, leaving not enough water to dissolve the salts, as in the ponds drying out under the sun.
Which salts, you might ask? After all, we are not ponds and our kidneys remove many small molecules.
Those salts, I would answer, that have made the stones.
Precisely those. Usually calcium oxalate and calcium phosphate.
The 24 Hour Urine is Our Pond
In it we measure losses of salts that can become stones, and the volume of water to dissolve them. We need the full day because things vary, with sleep and food, and all of what we do in life. Each is snapshot of our pond for one day. Which salts, how much imbalance, all this comes from our daily samples.
Abnormal Excretions Cause Stones
In our urine, excesses of calcium or oxalate excretion, or insufficiency of citrate excretion or of water are proven independent risk factors
that predict new onset of stones. Since stones cannot cause these abnormal excretions, and the abnormal excretions can cause stones, this association is equivalent to cause.
By independent I mean that the effect of each is significant when the effects of the other factors are adjusted for mathematically using common statistical techniques.
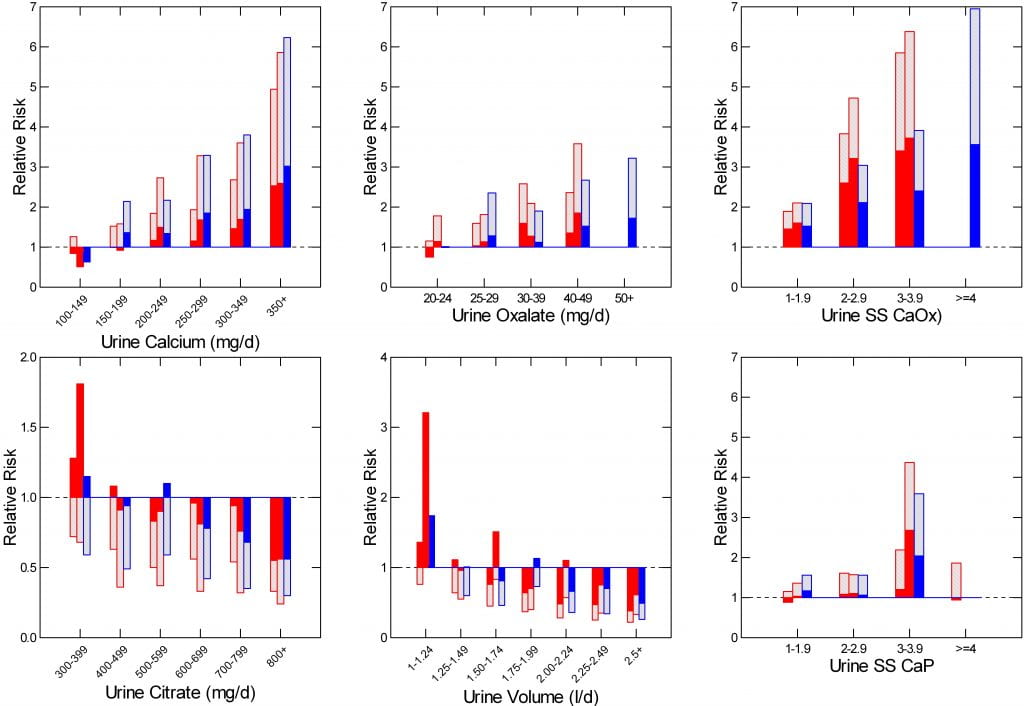
In cohorts of women (red) and men (blue) followed over decades, risk of forming stones rose smoothly with urine calcium or oxalate (upper left and upper middle panels), and fell with increasing citrate and urine volume (lower left and middle panels).
The mechanisms causing high urine calcium and urine oxalate are well known. Means for lowering them, likewise, and such lowering is known to reduce new stone formation.
Risk from low urine volume is most obvious below 1.25 liters per day (lower middle panel), a scanty volume. By 2 liters a day risk from low volume is gone.
Supersaturation is the Word for Overloading the Pond
Crystals produce kidney stones, and supersaturations produces the crystals. Modern laboratories can measure the supersaturations in 24 hour urine collections along with the key components in the urine that control the supersaturations.
As you might expect, supersaturation is a powerful predictor of whether people will become stone forming patients. The two right panels of the graph show how supersaturation with respect to calcium oxalate (top) or calcium phosphate relate to risk of stones. (Note that common supersaturation urines for calcium oxalate are 3.3 times higher than these older style supersaturation ratios. Your report will almost always use the newer units. So risk begins above 3 and rises smoothly up to 12 or more).
Given the stone crystals and the supersaturations you can gauge treatment goals from a simple maxim: In a patient who is producing new stones, urine supersaturation with respect to the crystals in the stones forming is too high.
Ideally one will lower supersaturation by improving all factors that raise it. But one must avoid a common and obvious fallacy. Water alone can lower urine supersaturation – think about rain and the pond. But water alone, without proper testing and as a sole remedy is a poor idea under all circumstances and to me anathema.
Ideal Treatment Improves All Abnormalities
Given a patient may have any one of these four abnormalities, and that they act independently, the ideal treatment strategy will attempt to improve each one to achieve synergy. It is often more practical to partly reverse multiple abnormalities than to rely on improving only one. For example, possibly extremely high urine volume might reduce stones even if urine calcium and oxalate remain high. But lesser volume would be sufficient if these two excretion rates were each moderately reduced.
When treating hypertension, as an example, one tries to achieve some weight loss, some increase in exercise, some reduction in sodium intake, and some increase in potassium intake, and then use medications as needed. The alternative, medications alone, or just exercise, would create a potential for side effects – too tired from exercise, or drug side effects in this case – which synergy would avoid.
Proper Testing Is Essential for Proper Practice
All Stone Formers Deserve Serum and 24 Hour Urine Testing
It is obvious that the only documented risk factors for stone are found in 24 hour urine, so this measurement is the bedrock of stone prevention. Systemic diseases that cause stones often alter serum chemistries, and they must be diagnosed from those alterations.
Inadequate Testing Can be Dangerous
A few causes of stone disease, such as severe hyperoxaluria can destroy kidneys. Others like primary hyperparathyroidism or renal tubular acidosis can do the same. Other rare but dangerous inherited diseases lurk in any kidney stone population. They require both serum and 24 hour urine testing.
Consider that idiopathic hypercalciuria can be very severe and lead to both stones and bone disease. One cannot know without a 24 hour urine collection. Elevated serum calcium can mark for primary hyperparathyroidism, or simply benign familial hypocalciuric hypercalcemia. So one needs a 24 hour urine here as well. Low urine citrate as a cause of stones is simply unknowable without a urine collection.
Arguments Against 24 Hour Urine Testing are Specious
Cost, difficulty, and futility are all common arguments against urine testing, and none of the three convince me. Add to this that all people fear and detest surgery. Surgery is a nightmare one hopes to avoid. If testing can reduce surgery by even a small amount, testing is a virtue.
Surgical Costs Dwarf Those of Proper Testing
A common 24 hour urine with fasting blood sample costs a few hundred dollars – say three hundred for an upper end estimate. A kidney stone surgery, ureteroscopy for example, costs – about eight to ten thousand dollars, to which one must add lost work and the debilitating effects of general anaesthesia, postoperative pain, stents, infections, and postsurgical visits to physicians. Shock wave lithotripsy costs as much or more as shown in the same reference. At these rates, 30 to 40 24 hour and blood testing panels match one surgery discounting the personal losses.
Difficulty of Collection Stops Few Patients
In my decades of managing patients with kidney stones almost none have demurred to collect – pilots, surgeons, busy and successful business people, teachers. I could also point out that modern commercial vendors all provide convenient collection kits and instructions. But no one could make the case better than my partner Jill Harris did in her spirited article on this topic.
Personalized Kidney Stone Prevention
Stone Analysis is Crucial
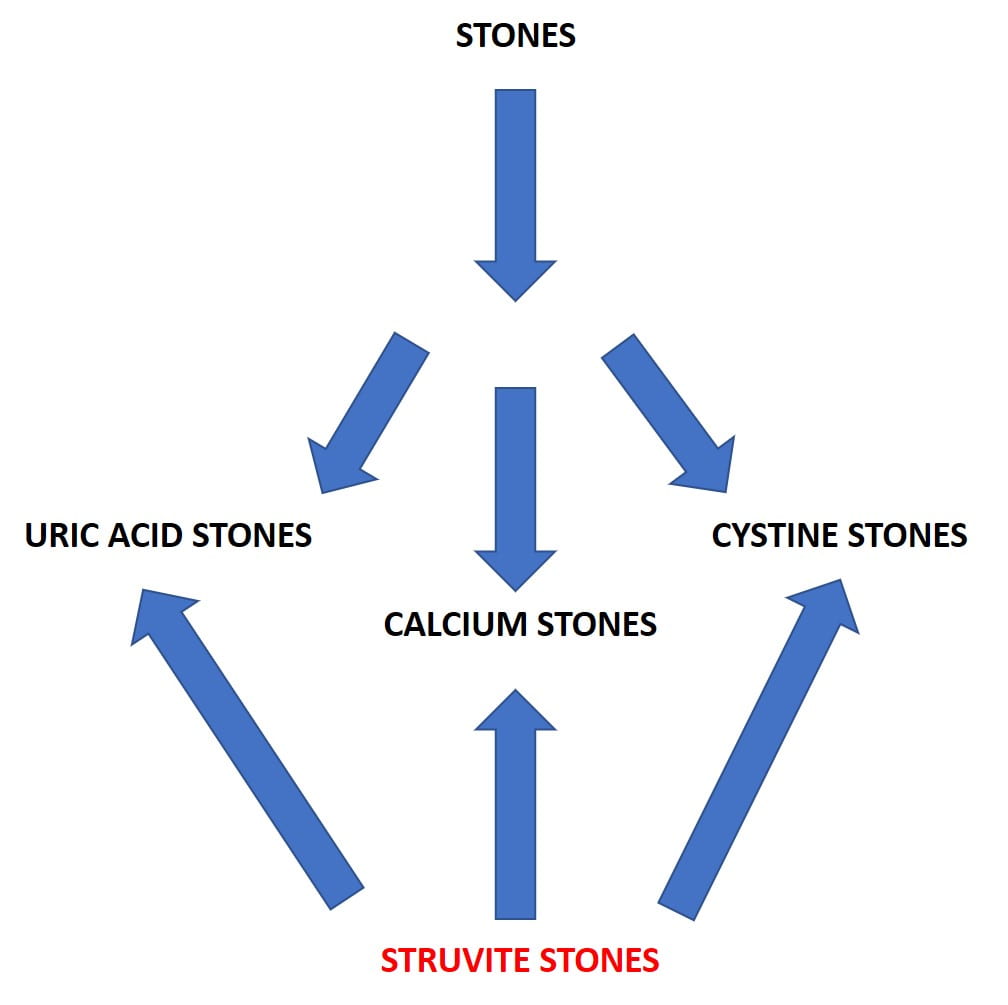 Assuming stones are forming or have formed, everything branches off of stone analysis.
Assuming stones are forming or have formed, everything branches off of stone analysis.
Uric Acid in Stones
Uric acid stones form mainly because an overly acid urine raises supersaturation so powerfully nothing can reliably prevent more stones but alkali to raise pH and make the urine less acid. Uric acid stone can be pure or admixed with calcium oxalate crystals. In either event, treatment must include alkali to prevent more uric acid. If your stones contain uric acid, follow this link.
Cystine in Stones
Cystine stones form only when genetic abnormalities of renal cell transporters allow a vast excess of this amino acid into the urine. Treatment is high specialized. Stones can grow very large and rapidly. Supersaturation can be measured but only in a few laboratories. Like uric acid stones, cystine stones can contain calcium phosphate crystals, but prevention of cystine crystallization is paramount and takes primary importance. If your stones contain cystine, follow this link.
Struvite in Stones
Struvite, magnesium ammonium phosphate, forms in humans only because of infection with organisms that hydrolyse urea to ammonia and carbon dioxide. Struvite can be the only stone crystal or can become part of any stone. Treatment has nothing to do with diet or the usual stone medications. Struvite stones are essentially infected foreign bodies within kidneys, and cure requires a mixture of thoughtful surgical management and use of antibiotic drugs.
Calcium Stones
The mass of patients will form calcium stones unmixed with uric acid or struvite. Out of this mass physicians – patients cannot do this

themselves -must cull the small fractions with systemic diseases that cause stones but produce illness beyond stones and require special and often very complex management.
Serum and Urine Testing
The tubule disorders are recognized from serum abnormalities, sometimes paired with specific 24 hour urine findings. Renal tubular acidosis and primary hyperparathyroidism are particularly related to stone disease. Both require both serum and 24 hour urine abnormalities for diagnosis.
Primary hyperoxaluria, and hyperoxaluria from bowel diseases, dangerous diseases that can cause kidney failure, are diagnosed from high 24 hour urine oxalate excretion and cannot be otherwise recognized. Bowel disease is recognized clinically, but 24 hour urine testing is required to assess both urine oxalate excretion and other secondary abnormalities that can cause stones and kidney disease.
Idiopathic Calcium Stones
Evaluate 24 Hour Urine and Treat Abnormal Risk Factors
Urine Calcium
High urine calcium in these patients arises from idiopathic hypercalciuria, and can be controlled with reduced diet sodium intake, avoidance of excessive diet protein intake, perhaps reduction of refined sugar intake, and, when needed, thiazide diuretic agents. Adequate diet calcium is needed to reduce risk of bone mineral loss.
Urine Oxalate
Urine oxalate above 25 mg/d can be treated with adequate diet calcium, that reduces oxalate absorption, and reduction of diet oxalate intake to below 200 mg/d using lists of high oxalate foods. Of these, spinach, rhubarb, nuts, seeds, and pepper are common offenders. If diet calcium increase does not bring urine oxalate into the desired zone (<25 mg/d is ideal, <30 is acceptable), limiting diet oxalate to below 100 mg/d is a proper strategy.
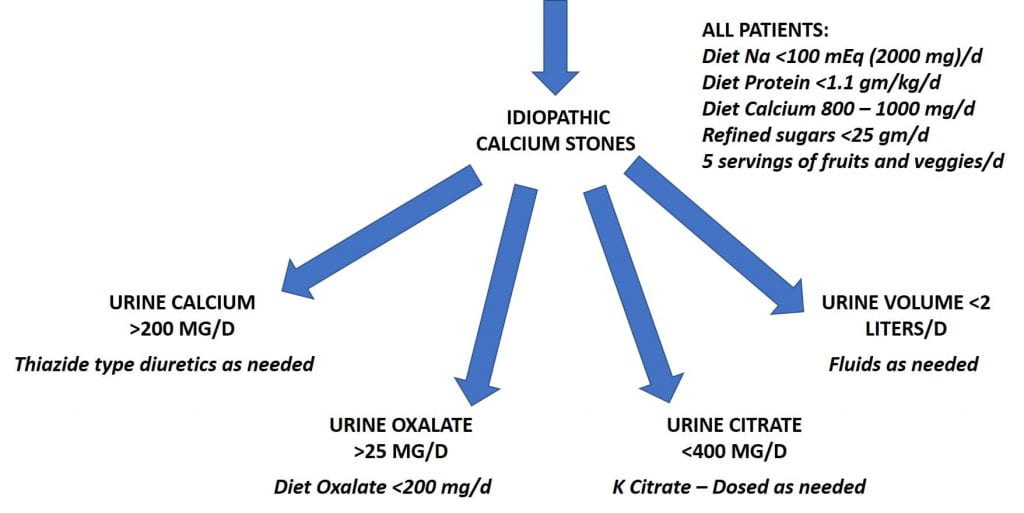 Urine Citrate
Urine Citrate
Low urine citrate, below 400 mg/d raises stone risk because citrate binds urine calcium in a soluble complex and directly inhibits formation and growth of calcium oxalate and calcium phosphate crystals. Five servings of fruit and veggies provides about 120 mEq/day of potassium alkali that can raise urine citrate. If needed, potassium citrate can be added as a specific treatment.
Urine Volume
One hardly need mention that urine volume below 2 – 2.25 liters a day needs extra fluids to achieve that goal.
The Kidney Stone Diet
The elements common to the three main risk factors beside urine volume are reduced diet sodium, sugar, and protein – to permit adequate diet calcium without raising urine calcium, adequate diet calcium for bones and to block diet oxalate absorption, and fruits and veggies to provide diet potassium alkali. These are highlighted in the large upper box.
These five diet elements all correspond to present healthy diet recommendation for all US citizens, and should be advocated by all physicians for all patients unless otherwise limited by underlying diseases. Since idiopathic calcium stone formers are almost by definition free of systemic disease, it is a desired diet in general. The diet has been tested in one prospective trial and more trials are much needed.
Online help with the kidney stone diet is available from my colleague Jill Harris.
Specific treatments, thiazide like diuretics, potassium citrate pills, and low oxalate diet are noted under their respective abnormalities. A strategy for beginning treatment with diet and adding drugs as needed is outlined here.
More is Wrong Than Just Stones
Having stones is burden enough, especially the dreaded surgery they can entail. But epidemiologists have discovered links between stone formation and risk of hypertension, bone disease, stroke, heart attack, and kidney disease including even renal failure and dialysis. The links between stone forming and these other major diseases are not as yet obvious, but the message obvious. Physicians need to treat the patient, nor just focus on preventing stones.
The kidney stone diet, being in line with best present recommendations for all US citizens, is a reasonable choice for all stone formers because aimed at reduction of risk for all of the above mentioned disorders. Even if the problems of stone formers transcend those of normal people, so that a healthy diet does not suffice, it can do no harm, and may do some element of good.
Why Not Just Lots of Water?
Consider the least threatening possible scenario, an idiopathic calcium stone former who has had only one stone – a kind of baseline kidney stone disease. Being such a common and large group why not simply treat them with lots of fluids, do a single 24 hour urine for safety, and save more refined treatment if water fails?
That Has Been Tried
Before you read what follows brush up on supersaturation.
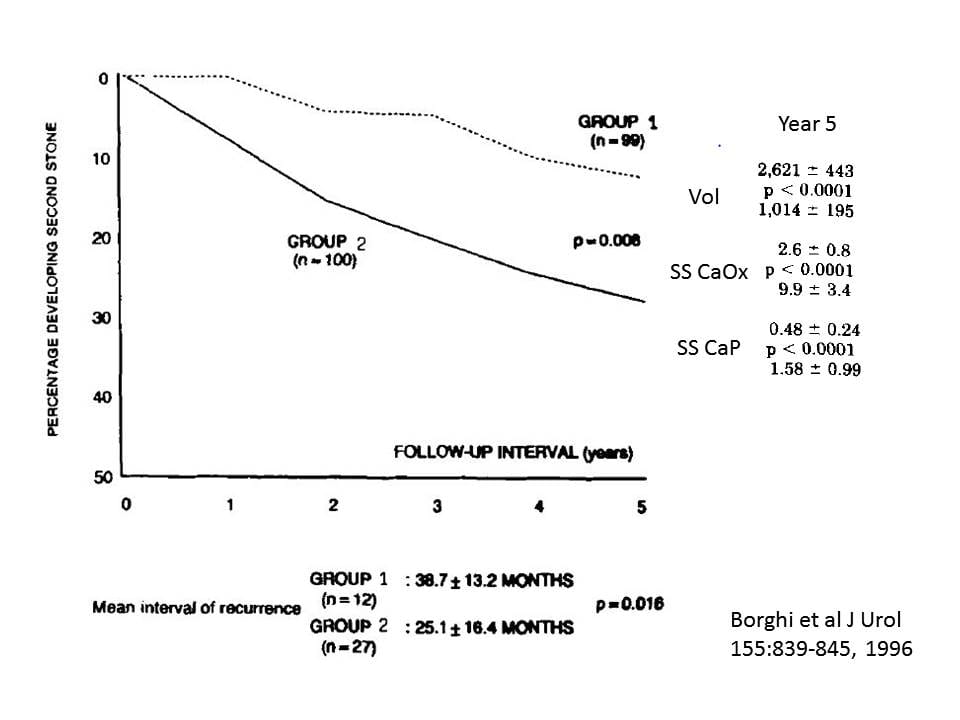
Of ninety nine people who formed one calcium oxalate stone and drank so much they produced 2.6 liters a day of urine, 12 formed one or more new stones in five years (Group 1). Among one hundred more just like them who produced only 1 liter of urine daily 27 formed one or more new stones during the same time.
As expected water reduced supersaturations. SS CaOx was 9.9 in the low flow and 2.6 in the high flow group. SS CaP was 1.58 in the low and 0.48 in the high flow group. Excellent and predictable results.
In passing the authors note that before the trial, at baseline, patients had lower urine volumes than their non stone forming subjects. One might surmise from this that habitual low urine volume played a role in causing their stones. But that is observation, not hypothesis testing.
Water Is Not Enough
Surely water works. Stones were less with lots of it.
But why so many stones? Of one hundred random people 12 people will not make one or more new stones in five years drinking so much water as to achieve a urine volume of 2.6 liters daily. This would be 2.4 percent per year or 24 percent per decade. Even if limited to adult years this would produce stone rates approaching 75 percent in a population of high fluid drinkers.
For the controls, who drank less, the numbers essentially double.
More is wrong than water could right. Given the risk factor studies I have already presented, this is an expected outcome.
In fact, in Table 4 of the water treatment article in the link above, hypercalciuria was at least one of the reasons for higher relapse. Baseline, before anything was done, the urine calcium levels of those destined to relapse was higher than those who did not 233 vs.336 mg/d and 249 vs. 313 in the high fluid and low fluid groups, respectively; p<0.001 for those into statistics. So those destined for a bad outcome had idiopathic hypercalciuria, a well known personal risk factor.
This Was Water Under Ideal Conditions
Above all else, these patients were supervised so that water treatment was as good as it can ever be. The cost of such supervision was underwritten by the grants that supported this trial. Outside the umbra of a subsidized program, adherence to such high fluid intakes will be less ideal.
Multiple Stones Predict Higher Relapse on Treatment
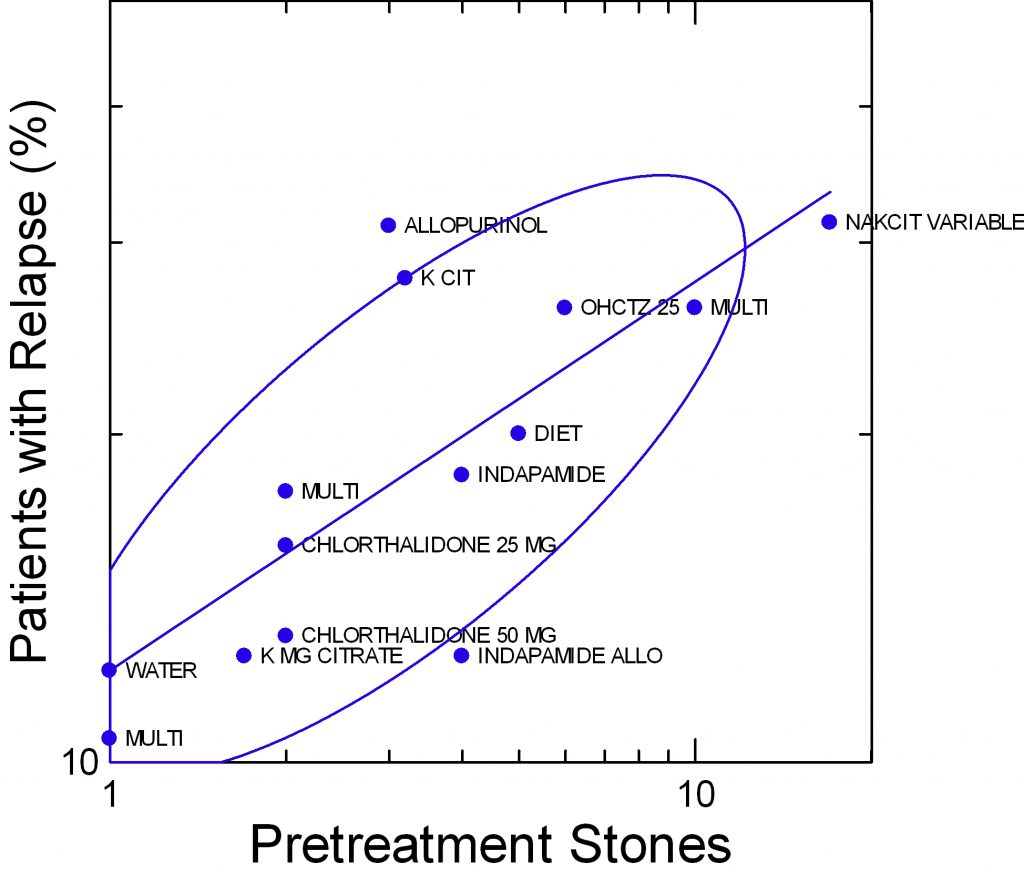 This figure shows the treated patients in a number of published trials. The details can be found in the parent article.
This figure shows the treated patients in a number of published trials. The details can be found in the parent article.
The abbreviations refer to the treatment modalities: K Cit means potassium citrate; chlorthalidone, indapamide are thiazide like diuretics, HCTZ is hydrochlorothiazide; Multi means several medications were used together; allopurinol lowers urine and serum uric acid and proved effective in one major trial against calcium oxalate stones.
As the number of stones produced before treatment goes up, from one to 10 or more (along the horizontal axis), the percent of patients who relapse during treatment rises from 10 – 12 percent to 20 to 30 percent. More or less, the percent who relapse increases proportionally to how many stones had formed before treatment.
Results for the water trial of single stone formers and my own published observations on patients who had formed a single calcium stone are at the lower left of the graph.
Stones Form Steadily Over Time
Waiting to treat a single idiopathic calcium stone former, either by the use of relatively ineffective high fluid intake alone or, in the worst
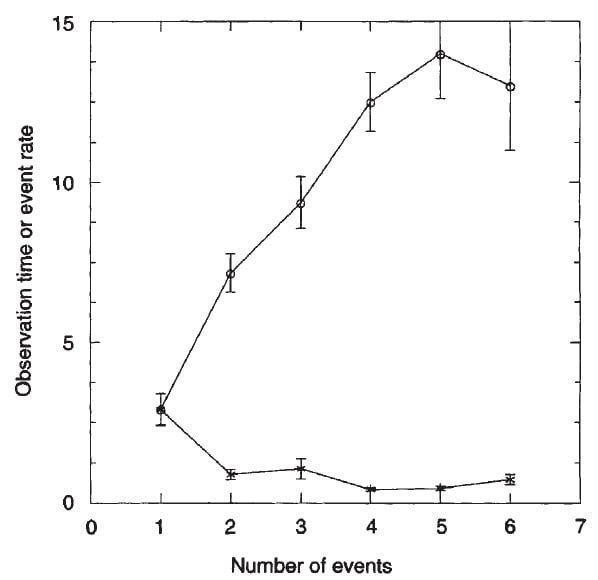
case, doing nothing at all, will on average lead to more stones. On this graph, detailed elsewhere, time is on the vertical axis and the number of countable stone events on the horizontal axis. Squares show the rate of stones per year, a rather constant number. Circles show the inevitable consequence: more time, more stones.
So time wasted, with water as a sole remedy, or no specific treatment, will tend to increase the number of stones, and as that number increases the successfulness of even highly supervised protocol treatment as used in trials will wane.
Never Use Water Alone
I will surely not treat any patients with just water unless 24 hour and serum testing shows me that nothing at all is wrong but low urine volume. Even then I am sceptical.
The reason I am so stubborn about water and waiting is that the main force of treatment for idiopathic calcium stones – those forming in the absence of systemic diseases – is diet change. Not only that, the diet change is in the direction considered most healthy for the US population. Why would anyone force fluids on patients when much of the disordered urine chemistry can be mitigated by a healthier diet?
Maintenance Treatment
Analyse Every Stone
One might think that once we know someone forms, for example, calcium oxalate stones more analyses add little or even nothing to successful treatment. But obvious problems make that thought a poor one.
New Struvite
Every surgery poses risk of infection. As foreign bodies in the kidneys stones themselves offer lodgment to bacteria that may be passing through the urinary system. So struvite can grow over older calcium stones, or even begin on their own. The person ‘converts’ from one type of stone crystal to another. Treatment no longer stops stone growth.
Because rapidly growing, large, and laminar in appearance by x ray, struvite stones will make themselves apparent over time. But larger size means more complex surgery, and perhaps kidney injury or even sepsis from stone infection. So early detection matters.
New Uric Acid
People age, gain weight, develop diabetes and with this urine pH falls. Treatment with alkali that might have stopped uric acid production begins late, when rapid stone growth or large stone size makes uric acid come to mind. But large means harder to dissolve, perhaps impossible. That means surgery. Early detection of uric acid in stones can save future surgery.
Calcium Oxalate to Calcium Phosphate
This happens and probably matters. CaP stones most often arise over tubule plugs which means cell injury in tubules and the tissues around them. By contrast, growth over plaque, how CaOx stones form, appears less invasive. Tissues seem less injured.
My imagination tells me calcium phosphate stones may cause more long term kidney problems than calcium oxalate stones. If this hypothesis were true then mere observation of patients well characterized in stone composition should disclose differences in kidney function, or perhaps urine albumin loss. Perhaps blood pressure rises more. Perhaps someone might have such information.
Quite possibly potassium alkali that work well to prevent calcium oxalate stones do poorly for calcium phosphate stones. After all, they raise urine pH and a higher pH will foster the phosphate stone. No trial addresses this obvious question; one should.
How Good is Kidney Stone Analysis
Less than ideal
What happens if you make a rigorous analysis of stones, divide the sample up into parcels and send them to different commercial laboratories. What will they tell you?
Ideally they will tell you what you already know. But in fact they under reported struvite and calcium phosphate – as hydroxyapatite. They also failed in to identify brushite.
Not Utterly Unreliable
My own work with Joan Parks compared kidney stone content of CaP – as hydroxyapatite to urine pH and supersaturations obtained by 24 hour urine samples. Unlike work from centers that performed their own kidney stone analyses we relied on a multitude of commercial lab reports obtained over decades. Even so urine pH and CaP supersaturations tracked will with these commercial lab results.
A Reasonable Conclusion
As an inexpensive and indispensable tool, all of us need and use commercial kidney stone analysis. What we know prompts wariness about missed struvite – a most important stone diagnosis. But perhaps that argues for multiple analyses – more tries lower likelihood of missing the diagnosis.
Make Followup 24 hour and Serum Measurements
It would seem unnecessary to say, but sometimes this obvious maxum goes unfulfilled. There is no use to changing diet – or trying to – or adding medications if one does not assure that the changes lead to a betterment of stone risk. I think followup urine collections for diet change should be when a patient believes the diet has changed and is tolerable enough to be used long term. With thiazide or potassium citrate, I favor 6 weeks initially. For all patients, followup with testing and a clinical visit should be yearly at least until stones become a thing of the pasts.
Aids for Patients Who Have Formed Stones
I have written several articles outlining the steps to prepare for and do testing, and for obtaining the most from physician visits.
This site has a large volume of articles. This page lists all of the articles by topic.
Chapters 2 – 6 of this book give a lot of background and links to related articles.
Chapters 7 – 12 concern specific stone forming systemic diseases.
Summary of Chapter One
The miserable fragments we call kidney stones have a complex origin in the kidneys. All but one kind contain crystals without which they could not exist. The exception, protein stones, occur rarely and I do not consider them here. Stone crystals form as all crystals form, from a solution overloaded with the crystal material – supersaturated with respect to the crystal of interest.
Many Paths to Stones
Kidneys can supersaturate urine by conserving water or by increasing the amounts of insoluble salt constituents such as calcium or oxalate. They can reduce the excretion of citrate, an inhibitor or change pH. The latter can be downward, fostering uric acid or upward fostering calcium phosphate crystals.
Treatment Synergy Requires Proper Testing
Although effective and obvious, extra fluids do not reduce new stone production completely to the baseline levels of average people. Moreover, above perhaps 2 to 2.5 liters a day of urine becomes difficult to maintain. So ideal treatments employ synergies – increase of fluids and changes in calcium, oxalate, citrate, or pH of urine as indicated in any one patient. Only blood and 24 hour urine testing can tell what is indicated in any one patient, and also what treatment has accomplished.
Stone Analysis is Crucial
Since all treatments but water relate to specific crystals, prevention depends on stone analysis whenever possible. Stone crystals can change over time and I see no reason to discard stones and good reasons to analyse them. Especially, infection or uric acid stones may complicate or even replace calcium stones and be missed without analyses. Likewise for stones from drugs.
Stone Prevention is Precision Personalized Medicine
Stone prevention exemplifies the best features of precision medicine. The crystals arise from specific supersaturations we measure in simple 24 hour urine samples and can reduce with healthy diet changes and a few medications that have proven their worth in trials. No two patients are quite the same, so each needs personalized care – stone analysis and 24 urine testing along with blood tests and clinical assessment to exclude systemic diseases.


I live in the UK and have gallbladder disease. Do you work with patients on a one to one basis? If so can this be done by Skype or phone? What do you charge for a session? Thanks
Hi Mrs Williams, Gallbladder stones are altogether different from their renal cousens, so I am afraid I would be of no help. Usually when troublesome, surgeons remove them via modern minimally invasive instruments. Sorry I cannot help, Regards, Fred Coe
Is there help for a calcium oxalate stone maker with MSK and kidney reflux? I’m eating low oxalate, low salt, low sugar, high calcium and kidneys still full of stones. Passed one this morning. Having a repeat 24 hour urine before my next visit. I also have ckd 2.
Hi Debi, Prevention of new stones is generally effective. Prior stones usually remain or are removed. This latter is often via ureteroscopy. One should always set up prevention prior to removal so new stones do not reform. Regards, Fred Coe
I am pleased to find this information, I have just started reading it. I make stones and I am currently filled with stones in both kidneys (over 20 in each kidney). I pass stones weekly. I have had several lithotripsies, the last one in January. I have never been told as to why or how I can prevent them. I recently received the lab results of my stones. 85% calcium oxalate and 15% calcium phosphate. With this information I believe it would be best for me to try a low oxalate diet. I won’t go back for a follow up KUB till August. Hoping to change my diet and see fewer stones in the future. Thank you for making this information available.
Hi Heather, with all those stones, and calcium oxalate at that, one generally feels that low diet oxalate will be ideal. Usually it is neither sufficient nor necessary. Here is my best on prevention for many stones without – I gather – a systemic disease as cause. No one remedy has as much chance as a fully integrated treatment program. Regards, Fred Coe
My daughter has been diagnosed with MSK for 10 yrs.She is in continual pain to the point of disability.Surgeries too numerous to count,hundreds of seed stones in each kidney.Been to the Mayo Clinic and most Drs say to avoid the “unroofing” procedure.It would cause further issues down the line.What are your thoughts on that? She has no quality of life…
Dear Julie, I can only suggest another opinion from an expert surgeon. Dr James Lingeman at Indiana University, Indianapolis would be by suggestion. Please feel free to use my name by way of introduction. Regards, Fred Coe
Dear Dr Coe, I have Crohn’s Disease diagnosed at age 38, 36 years ago. My first kidney stone was two weeks prior to the full term third live birth. It was not diagnosed as kidney stone. I figured it out when I found a black jagged stone in my underwear the morning after the extreme pain episode. I have had 3 subsequent diagnosed kidney stone episodes many years apart. I participate in high intensity activities in which my fluid intake and output significantly decreases. A urologist determined from a ct scan many years ago that there were multiple kidney stones. The advice was to increase my potassium intake during those activities and saturate myself with water before and after the activities. I have not followed the water intake. I have increased my potassium intake within a safe and reasonable level.
The most recent kidney stone episode was within the last month. It was two episodes each one week apart. No excreted stones were observed. A visit to the ER resulted in a ct scan which identified the location of the present stone and multiple stones in each kidney. A UA was done nothing a UTI. Nothing further was instructed or done.
Two weeks later, I saw my GI doctor at Mayo Rochester. Another ct scan, 24 hr urine and one clean catch plus blood work revealed multiple stones in each kidney, no evidence of UTI, higher than normal level of oxalate in the urine. Instructions were to drink lots of water, eat Tums and follow a low oxalate diet. I chose walgreens brand mint flavor with Ca carbonate 500 mg. Inactive ingredients: dextrose. Flavors magnesium stearate, maltodextrin, starch, sucralose.
Intuition has me uncertain about the evaluation and instructions. What can I change and implement at this time? Do I need a more detailed evaluation?
If so, where do i go? How do I proceed? I live in the Chicago western burbs.
Thank you for any direction. The thought of experiencing another episode in later years leaves me shuttering.
Hi Ellen, WIth Crohn’s disease, malabsorption leads to increased urine oxalate as you have, and treatment does include calcium. It matters how one does all this; the Tums need to be with the meals that contain oxalate – for example, they are worthless with eggs for breakfast – no oxalate to block. Monitoring via 24 hour urine oxalate matters a lot so you know if things are better. Likewise, a more refined approach can include higher calcium foods where possible so not everything depends on calcium supplements. If you like, we can see you at UC (my partner or I) to help. Regards, Fred Coe
Dr Coe, Thank you for your reply. I’ve been trying to figure out the calcium vs oxalate way of eating with some difficulty. About the time I think I have found a list of oxalate dens foods, I find another list that contradicts the previous list. I would like and appreciate some help from either you or your partner. You may contact me at my email address to set up an appointment.
Ellen
Hi Ellen, Use our list, it is curated by excellent people (not just me). I will email you. Regards, Fred Coe
Hello Dr. Coe. I’m 34 and have had one stone about a year ago. I didn’t have it analyzed nor did I have any significant tests done. Unfortunately I have regular anxiety about passing more stones (I know that is likely a mental issue). Is it recommended to find a urologist and go through analysis or is that unnecessary when only one stone in one year has presented? Thank you for your time.
Hi Bob, because treatment is so based on eating a healthy diet, I always begin it with even one stone. Here is my best on the subject – or better said, another view of it as I like the chapter you have written on. Regards, Fred Coe
As an engineer I deduced that stone formation was a crystal precipitate from a supersaturated solution based on my college studies in materials. I was obviously pleased with myself when I discovered your site and found your detailed explanations. One of the best, selfless internet sites I have encountered. Thank you for sharing your knowledge.
Obviously I have Stone Disease otherwise I would not have looked for your site. My work involves the use of data and statistics to solve systemic and often times confounded problems related to automotive power train systems. We like to say that there are two ways to solve a problem; 1) optimize the inputs by reducing the variation or 2) become insensitive to the input variation.
I will try to do both. If a metabolic condition is responsible for the supersaturated condition and a method is available to rectify the sensitivity issue I will certainly pursue it. As for the input variation I have not completed a saturation analysis yet but my urologist has already indicated that that will be the next step but I do have a stone analysis:
1st Constituent: 70% Calcium oxalate monohydrate, 2nd Constituent: 20% Calcium phosphate (apatite) and 3rd Constituent: 10% Calcium oxalate dihydrate.
If I understand your videos, my existing plaque deposits pose the greatest because they can provide the seeds that initiate the crystal growth. I can certainly increase my fluid intake and modifying my diet but what about the plaque? Can you provide additional insight on how to manage plaque buildup? Can I purge the existing plaque in my system? What drives plaque formation and how do I prevent additional plaque growth? Or am I reading more into the video than what is warranted?
Hi Pat, I just put up a new plaque article, one that goes into how it may form. If I am right about that, the treatments that lower urine supersaturation should reduce plaque formation. I do not know how plaque goes away but suspect it may slough off of the tissues. Your stones have considerable phosphate, suggesting urine pH runs a bit high – 6.2 or more. The 24 hour urine and serum studies will give the causes, and treatment follows them. The chapter links to other resources, as I am sure you have already discovered. Prevention is reasonably good, so pursue it. Regards, Fred Coe
Dear Dr. Coe,
My history with kidney stones started in March 2012. I have formed almost exclusively uric acid stones (the most recent was the one exception: 90/10 UA/CO). I believe the change in my metabolism was the result of aggressive breast cancer treatment; the stones started forming vigorously after a few rounds of chemotherapy. Fast forward: I have had two PCNLs, three ureteroscopies and two emergency stent surgeries. I believe I’ve had 3 AKIs and am a CKD Stage 3 patient. I’ve done several 24-hour Urine Collections. The result: take potassium citrate and increase my urine output. Initially, I could barely swallow the pills and gave up. Then I found Effer-K and solved that problem. I believe the reasons it’s important for me to follow this stone prevention regimen. So – what’s my problem?? I have beaten myself up for not being compliant; I always forget why was I having problems staying on this regimen. So, in September, October and November 2018, I was as perfect as I could be and only missed a few doses (four, to be exact) in over 10 weeks. But I remembered why I’ve failed every time: I feel physically ill when I take potassium citrate. I didn’t sleep more than two or three hours at a time for more than two months last fall. I was incontinent all night long; I felt lousy during the day. I started to dread every day and every night. Have you ever had a patient who could not physically tolerate 40 (or 60)mEqs of potassium citrate daily? I don’t believe this is psychological; but, maybe I’m wrong. I gave up, in December, because I could not go another month without useful sleep. I am a professional church organist, and we’re busy in December! But now I’m facing the dragon again; and, in about six weeks, I will be facing my urologist and nephrologist at a stone clinic. Do you have any advice? Is, “stick it out at whatever cost” my only option?
Thank you,
Tacy
Hi Tacy, The uric acid stones occur because urine pH is too low and the only treatment is to raise the urine alkalinity (pH). Potassium citrate does not seem good for you. How about sodium citrate or sodium bicarbonate? If you have high blood pressure and the sodium worsens it, your physician can add a very low dose of a diuretic – like chlorthalidone. You may waste some potassium but can take plain potassium chloride instead of potassium citrate if needed. I have used this workaround for people adverse to potassium citrate. You might use 1/2 potassium citrate, 1/2 sodium citrate – there are mixtures on the market. If effer-K worked, why not use that. Regards, Fred Coe
My dear friend is suffering from Randalls plaque disease, can you please refer her to a urologist who is familar with this horrible disease , she lives in West Palm Beach, Fla.
Hi Michae, I am afraid I do not know who is practicing in Palm Beach – being an academic type I have only a poor knowledge of the practical world. In fact I do not know any stone specialists in Florida, likewise out of ignorance. Apologies, Fred Coe
Hi Dr. Coe,
I had a 7cm stone removed using a stint and lazer. It is 70% calcium phosphate, 20% magnesium phosphate and 10% calcium carbonate. The doctor had a 24 hour urine test done and said I was excretion calcium and potassium into my urine. He prescient chlorthalidone and uro city k, both of which I stopped taking after 2 days. They made my conic diarrea (due to collaginous collitus) and frequent urination significantly worse. After the second day my legs were weak. Is there something I can do with diet? I am already on the low fodmap diet which reduces the gas associated with the collagen ousted collitus.
I welcome any advice you can give me.
Anne Danshy
Hi Anne, I believe I answered this question from another post. Take a look. Fred
Hi, Dr. Coe,
For Calcium Oxalate stones, are Calcium Citrate, Potassium Citrate and Magnesium Citrate helpful or hurtful supplements while following your suggested diet protocols for reducing Calcium Oxalate stone formation?
Regards,
James
Hi James, potassium citrate has several trials and works. Calcium citrate is used as a calcium supplement when food will not provide enough calcium, and has a main role to lower urine oxalate. Magnesium citrate is not used alone for stones, but has been part of a potassium citrate product. You are on the right reading track, so just follow the links, and read along. Be sure of your blood and 24 hour urine results, treat what is abnormal, and things should go well. Regards, Fred Coe
Hi Fred, I am 22 years old and I have been having kidney stone issues since I was 19. Since 2016, I have had 8 kidney stones pass, the biggest and most recent being 8mm.
I have had my stones tested in the past after having Shock Wave Lithotripsy (in 2016) and they were mostly Calcium Oxilate, with a little bit of Calcium Phosphate.
Its now been over 3 years and I’ve passed multiple large stones since. I had the 8mm stone analyzed by a lab and the results say that it is composed of %20 Calcium Oxalate Dihydrate (Weddellite) and %80 Calcium Monohydrate Phosphate Dihydrate (Brushite).
I am passing stones almost monthly and its terrible. I understand that Brushite isn’t known as well as other stone formations..
I am just looking for any type of help or explanation, because my urologist didn’t seem too concerned.
Thank you,
Gage B.
Hi Gage, You have progressed from calcium oxalate to calcium phosphate stones, the latter as brushite – calcium monohydrogen phosphate. Brushite stones are a problem, and need effective prevention. They are all too well known among those of us who do a lot of work with stone formers. Here is a profile of the calcium phosphate type stone former. The crystals tend to plug tubules, so some of the ‘stones’ seen on CT are actually tissue deposits. Shock wave LT is not so good, and I favor flexible digital ureteroscopy. The chapter you have posted on is a fine guide to evaluation and prevention, and I suggest you and your physicians pursue both with high energy and aggression to prevent more stones. Regards, Fred Coe
Greetings Dr. Coe,
In surfing the Internet, and reading all that is easily digestible, I recently found your information and wanted to simply say thank you as it is plentiful and easy to understand; i.e. enough for me to continue my challenge to my urologist with the volume of questions I have … mostly now around how to maintain a proper PH level as I have yet to commit to only low Oxalate foods … rather, with focus on ‘moderation’ and lots of ACV/Lime Juice water. I am also researching (the minor, and unreliable data) on what it takes to break down a stone after it is formed; as we all know when one is forming!
Thanks (again) in advance of my total absorption of your data.
Robert
Hi Robert, stone dissolution is not a very likely event given calcium stones. Uric acid stones can be dissolved. As the chapter points out stone type is crucial, and the 24 hour urine chemistries. Urine pH is a minor player for calcium oxalate stones, too high in calcium phosphate stone formers and not alterable in a practical sense, and too low with uric acid stones and easily raised. I would hope you will get fully evaluated and pursue the steps in the various chapters – they are good, at least until we get more research. Regards, Fred Coe
Hello Dr. Coe,
I just turned 69 and had my first stone back in Dec. 2017. I thought it was a bladder infection and was in a lot of pain and discomfort for about a week before my husband finally took me to the ER where it was discovered I had a stone. It did pass.
Fast forward….I had a checkup with my urologist in February ‘19 and it is now evident there is a 8mm stone in one of my kidneys. He would like to do a ESWL procedure. I have severe osteoporosis but he assures me there would be no problems. Is this 8mm kidney stone too large to use a ureteroscope with a stent, instead?
Hi Barbara, ESWL should not fracture bone, so it is not unsafe. An 8 mm stone can be removed via URS. But your surgeon decides which modality to use, and that choice can be complex. H/She will always act in your overall best interest. Incidentally, pursue prevention, so you do not keep making stones. The article you have posted on is a good place to start. Regards, Fred Coe
Hi i got my left renal stone 2018, 5.2mm and had uti symptoms too. Dr gave me ural and antibiotics for 7 days. I had my ultrasound and ct few months later and it shows no renal stones. I was also diagnose with familial hypercholesterolemia and im taking atorvastatin and ezetimibe but not tolerated thus i stopped against doctors advised. After 6 months i again suffer with on and off flank pain with uti, i was treated with same antibiotic and ural but the symptoms doesn’t go away. Utrasound done and it shows bilateral sand calcification/ renal crystals. Am devastetad and dunno what to do and afraid of my kidney function. Im trying to change diet to vegetarian to low uric acid but seems getting worst
Hi Nerv, Often crystals do things like this are are easily missed. Crystal prevention is just like stone prevention, so you might want to pursue exactly the same testing and treatment options. Regards, Fred Coe
Followed a link in one of your responses in the comments section of Jill Harris’s article.
I just wanted to express my frustration with all of this (recently suffered my second stone attack); low-oxalate diet, more water, etc. Only 1 in 10 of adults will form a kidney stone over a lifetime, and the number of stone experiences is increasing (based on what I’ve read), so once again, the medical establishment is treating instead of finding the true cause. There’s something causing this, what I don’t know. Diets and more fluid intake are just band-aids in my opinion.
Hi Kurt, You and I think alike. I am more than sure that stones arise for the most part because of a mismatch between our evolutionary adaptations to one diet and our consumption of another. In particular I believe high sodium, low potassium, low calcium, high refined sugars are the main culprits. In this I am part of a large group of scientists. This thinking led me to the kidney stone diet, which is really much like the US ideal diet. Diet may well account for the increased occurrence of hypertension, stroke, and kidney disease in stone formers. So I think this may be the ‘true cause’. Regards, Fred Coe
There are a LOT of medications that impact the kidneys and cause stone formation. Many are over the counter medications like Prilosec, and many more are medications for seizures, migraines and psychiatric conditions. Anti-virals can cause stones too. I am sure the list is really long of medications that cause kidney stones in many different ways that physicians do not bother to screen for.
hello Dr Coe.
you are a kind hearted man and i am pleased to have met you here. how wonderful that you give your time and energy to help so many in need. thanks!
Hello Dr. Coe. My name is Mohamed. From Egypt.
My mother is 55 years old, she suffered 4 attacks of ureteric colic with unilateral ureteric obstruction and hydroureter and hydronephrosis, and one attack which was bilateral. all the attacks were relieved in one day with medical conservative treatment. notably, all the attacks were in summer. in July.
Is there a high risk she could develop Chronic kidney disease?
Her GFR now is in the normal range. how many attacks of hydronephrosis could lead to CKD?
The prevention strategies doesn’t seem to work, 3.5 litres of water per day, healthy diet, less salt, some medications like Cystone rowatinex. and nothing seems to work.
What should we do?
How many attacks of Hydronephrosis before she develops CKD?
Thanks.
Hi Mohamid, For your mother as for everyone we need to look at stone composition and at serum and 24 hour urine measurements to determine what seem to be the causes of the stones. More water is always at least of some value, but without a sense of cause it rarely will be sufficient – and has not been for her. As for hydronephrosis and kidney disease, I do not know. If obstruction is promptly relieved and she does not become infected above an obstructing stone, and surgical damage is avoided, one hopes for excellent preservation of kidney function. But multiple episodes create multiple chances for trouble, making prevention of highest importance. I would begin with what the stones are made of and proceed from there. Regards, Fred Coe
Hi Dr Coe,
I am 29 years old and having multiple kidney stones since 2015, had 2 surgeries and recently before 2 months i had a Ureteroscopy to remove a stone, while CT scan showed 2 more small stones in both kidneys, since few weeks i am again having the pain in kidney and lower ureter. Do not know how to get rid of this
Hi Quddus, The article you posted on has a good outline for prevention and links to more detailed articles. Here is another take that is perhaps more specific. Basically you need to know what the stones are made of, and what is causing the stones. Treatment follows logically. Prevention is reasonably successful – thence this website. Regards, Fred Coe
Hello,
I have just had uteroscopy for my third Kidney stone in May. I did not retrieve my previous stones, but my urologist tells me this one is calcium oxalate. I have 3 more stones on my left side with the largest being 1cm (approx) and 2 smaller ones. My urologist is sending me to St Michael’s Hospital in Toronto for shock wave lithotripsy for the larger one. I have asked him for a 24 hr urine but he brushed that off. He’s given me a handout for dietary changes and wants me to take 1/2 cup lemon juice in water daily.Thankfully, I found this website and Jill Harris’ facebook group so I have already implemented lower sodium, sugar, oxalate and increased calcium diet. Should I see if I can get my family doctor to order me a 24 hour urine and bloodwork? I asked my urologist if I can go to the Kidney stone prevention clinic at St. Michael’s but he said to get this bigger stone taken care of first. Just wondering if you have any other suggestions. Thanks so much.
Lisa
Hi Lisa, Jill is a good idea and so for this site. But I think your physicians would want to get proper 24 hour urine studies to find out why you make stones. The kidney stone prevention clinic in Toronto is excellent, I think, and I know a few of the people there to be outstanding investigators. By all means go there and get stone prevention. Regards, Fred Coe
I am an active stone former. My stones have been identified as calcium oxalate. My fluid intake and low sodium intake is exceptional and I avoid high oxalate foods as much as I am able (when traveling that can be a bit tricky). I am asked to have at least 3 servings of dairy (1,000 mg) a day for calcium; calcium in the form of supplements is not recommended. However, I also suffer from IBS aggravated by dairy which not only contributes to fluid loss but also interferes with my daily quality of life. My nephrologist does not recommend calcium supplements and is suggesting lactaid milk (which still upsets my stomach). My urologist is now suggesting I opt for elective Ureteroscopy and lithotripsy with the possibility of a stent (that would be my 6th procedure) instead of waiting to be symptomatic or passing the stones on my own. Are there plant-based forms of getting calcium into my diet??? I am feeling very discouraged that my body continues to produce kidney stones despite all my efforts.
Hi Lynn, There are two problems. Given the GI fluid losses, perhaps your 24 hour urine volume is not large enough, and since you do not mention any 24 hour urines I am left to guess. As well, what did the serum and urine testing disclose as the causes of your stones? High calcium intake is to lower urine oxalate and provide for your bones, low diet sodium is to keep urine calcium low despite high diet calcium intake. But what is your 24 hour urine oxalate, sodium, calcium? As for procedures, URS is my favorite, but do you need it? Are stones causing pain, bleeding, infection, or obstruction? So I guess I do not have enough to offer back real answers. Regards, Fred Coe
Thank you so much for your response. My last 24 hour urine was on 8/1/19. My urine volume was 2.86. My Urine oxalate was 58, urine calcium 134 and Na 99. I have a 4 mm and a 2 mm stone in my left kidney and am not currently symptomatic. Since I have posted, I have decided against an elective URS. I am being asked to increase my calcium intake but I do not want to consume dairy because of IBS. Why can I not take calcium supplements? Thank you in advance.
Hi Lynn, Sure, supplements are workable, but you must time them with meals that contain oxalate. The calcium needs to crystallize food oxalate in the bowel lumen. Usually it is lunch or dinner where the oxalate resides. Be sure and recheck when you have begun the supplements. Regards, Fred Coe
I very much appreciate your time and response. Thank you!
Here is a list of foods highest in calcium. Many are dairy free and you of course know which are lower in oxalate. Scroll down to view whole list; only a sampling is given at the top: http://www.whfoods.com/genpage.php?tname=nutrient&dbid=45
Hi Dawn, The problem is so much oxalate in many of these. But we do have a high calcium /low sodium diet list – what we need – and some of these foods might have been overlooked. Thanks, Fred
Hello, I am seeking advice for my husband who has suffered from large calcium Oxalate stones every year for the last five years. Largest being 11mm and smallest 6 mm. All have caused obstruction and ended with lithotripsy and the first year was PERC for a cluster of stones. He sees an urologist who has had him increase water with lemon juice, low oxalate diet, and have had 24 hr urine studies which did show high calcium but when blood work checked calcium was normal (so parathyroid cause was ruled out). In last year he has been diagnosed with diabetes (A1c was 7.8) and started on metformin and lost 20 lbs but he had severe diarrhea so he stopped the metformin 3 weeks ago. Current A1c is 6.2. Also endocrinologist seems to think stones are caused cuz his vitamin d was super low but has been normal now. Before being seen by PCP to see what to take for diabetes, he now has a 6 mm blocking at junction and a 7 mm and 8 mm formed and he is going to have his fourth lithotripsy on Wednesday. NOW after several thousands of dollars, someone noticed he has ureter renal pelvis stenosis and they said they can trial him on potassium and thiazides and if that doesn’t work —surgery to help with stenosis. My question is why does he keep having all these stones—nobody wants to find out why —just try this and take medication that may or may not work? My husband hates medication and doesn’t want to take something long term. Is thiazides and potassium to be taken forever once started? He is upset and just wants to be free of stones.
Hi Annette, The high urine calcium with normal blood calcium is probably a result of his diabetes or perhaps he has always had high urine calcium because of genetic hypercalciuria. Either way it probably was a cause of stones. Low vitamin D will not cause calcium stones so far as I know. As for the stenosis, perhaps it was caused by prior stone passage events or was there at the beginning, either way it will foster stones via partial obstruction. He needs to consider perhaps some additional consultation. His personal physicians can arrange for that. The high urine calcium needs lowering, and here is how one can do that. But given all of his diseases no outsider like myself, or article as a source can possibly substitute for real expertise for him as a personal physician. For that reason, I suggest the possibility of a second opinion, perhaps at a kidney stone center or major medical school, whatever seems best to his physicians. Regards, Fred Coe
I am working with a personal trainer to loose weight. He is suggesting more protein since the body breaks it down at a slower rate and you do not feel as hungry. Is this safe to do? What macronutrient ratio would be the best daily balance for stone formers?
Hi Sherry, You need to keep the protein within a normal range or it can raise urine calcium and stone risk. A good normal is 1 gm of protein per kilogram of body weight a day, and up to 1.2 gm is still within reason. Beyond that I would be concerned. Best, Fred
One other factor is Granulomatous disease or sarcoidosis. I can take in only small amounts of vitamin D without having cascades of stones–and it isn’t hyperparathyroidism. It is granulomas on my spleen and liver from either Histoplasmosis as a child in the Ohio River Valley OR Epstein Barr at age twenty. I still also adhere to the kidney stone diet now as well, but the thing that helps most is taking in very little vitamin D. When we got my D25 levels to 32 once, my D 125 was around 190. I was terribly ill from hypercalcemia and my kidneys are permanently damaged. The doctors thought I had Multiple Myeloma or Tuberculosis, but it was the granulomas which produce vitamin D–a hormone. Many who have sarcoidosis have this issue–I am in touch with people the world over. This is one reason after WW2 in the UK when cod liver oil was lavishly prescribed–there were deaths–undoubtedly those with undiagnosed sarcoidosis or granulomatous disease.
Hi SHaron, You are certainly right. I did not put the details of the systemic diseases in Chapter one, but do allude there to this chapter that includes them. You seem to be getting thoughtful treatment, which is so important. Thanks for sharing. Fred
Can you recommend anyone in the Clarksville / Nashville TN area? My son suffers from chronic stones, and is just now getting over a kidney infection, and having 3 13ml. stones blasted. We have searched and searched for Dr.’s that will help us, and it feels like we are in a ping pong match. Thank you for any help
Hi Beverly, Dr Hsi at Vanderbilt is someone I know of as excellent for stone urology. Dr Lewis is outstanding for medical prevention. Regards, Fred Coe
Hello Dr.,
Your website is a godsend, thank you so much for it.
I suffer from a complex, multisystem disease (mitochondriopathy, not exactly defined yet, also suffer from pots, mcad, and small fiber neuropathy, I am completely bedbound and 32 years old).
I had a kidney stone (stent was inserted) and no doctor here is really trying to find ways to reduce likelihood for new ones it seems to me, I have a very good primary care doctor though, would you be willing to do a paid consultancy?
Kidney stones for me are very dangerous as anaesthetics and pain medication is very bad for my mitochondriopathy and I lose quality of life persistently with every incidence.
Thank you so much!
Hi Christoph, You are reading the right chapter. You need a full evaluation as to cause as noted in the chapter and then treatment aimed at the abnormalities found. I would gladly try to be of help, but there are restrictions. In what country do you live, and if in the US in what state. That affects what I can do. I agree stones are a large risk for you. Regards, Fred
In your analysis under “Why Not Just Lots of Water”, you may have flipped the percentages of people who formed stones vs those who did not. 12 people formed stones over five years, and 87 did not. This should mean stone rates approaching 24 percent per decade in a population of high fluid drinkers.
Thanks, Narish, I did indeed. Fred
Recommendations for a highly competent nephrologist in Oregon?
Hi Sam, For kidney stones, I know Mike Conlin in urology. Nephrologists are rarely interested in this condition, and if there are such at Oregon U, Mike will know them. Regards, Fred Coe
Dr. Coe , Thank you so much for your very informative videos. I enjoy listening and learning . Your dry sense of humor keeps me smiling.
Hi Carol, thanks for commenting – and smiling. Fred
Can going through chemotherapy treatment cause stones (in someone who has had capsicum oxalate stones)?
Hi Angels, Possibly. It would not be the drugs themselves but diarrhea, vomiting, dehydration all could lead to stones. Regards, Fred Coe
I am 70 years old. Three years ago I had to have lithotripsy for kidney stones. I had to go in again 2 months later for second procedure as my urologist said apparently she hadn’t gotten them all. The pain from the stones was bad enough. But, the stints used after were much harder to endure. The second procedure she used 2 stints. I was “climbing the walls” with bladder spasms/pain. 4 prescriptions to alleviate this did not work. I couldn’t sleep. I was so affected that I developed a weird voice tremor/shaking and change of voice that lasted for months. I begged the doctor to remove the stints earlier than the almost 2 weeks prescribed. So, now my biggest fear of kidney stones is the stint. Can kidney stone removal be done without the stint or is one kidney stone procedure better than another regarding use of stints?
Thank you for the information you have provided here. I have eaten the wrong foods. Aware of some, but not others, unfortunately. I fear kidney stones are there ready to cause problems at any moment. So, stints are are bigger fear than the kidney stones!
Hi Kathleen, Doing without stents is a surgical issue, some surgeons do forgo them in special cases. Stone prevention is your ideal, and you are reading an excellent primer. Get tested, correct the causes of stones, with meds if needed, and stents cease to matter. Regards, Fred Coe
Hello Dr. Coe,
I first want to thank you for such an informative article. Our daughter is 8 and she was recently diagnosed with a 1.7 cm kidney stone. I was curious what your treatment recommendations are for a stone that large in a child (50 lbs) are? It’s probably unlikely, but do you have any recommendations for a pediatric urologist in the Spokane, Wa area? Thank you for your time.
Jill Werner
Hi Jill, Indeed stones in children are a big deal and require expert physicians. Here is our recent article about this matter. The stone is very large and the surgeon needs to be an expert in pediatric stone surgery. I would contact the university medical school and have her work done at a university hospital as it is rather unusual and it might be hard to identify the ideal surgeon in other settings. Regards, Fred Coe
Hi I have suffered from kidney stones for 30 years, just had surgery to laser 3 stones in right kidney 2 weeks ago, one being 12cm, now dr just told me I have to back next week and have it done all over again because he was not able to get all of the big stone. this is a new urologist for me because the last one that I had for 30 years just kept telling me to drink more water, I drink 2-3 liters a day and still form stones. did a 24 hour urine, dr says its fine. why do I keep making stones, every year I have a least 1 surgery, two years ago I had 4 procedures in a matter of 6 months! What can I do to prevent these stones from forming?? Dr’s are no help, at least not for me.
Hi Debra, I am sorry you have all this. More water is a weak prevention – the article you have posted on tells all about that, and also about how to fashion a proper stone prevention program for yourself. I am worried that the article did not make its point better as you ask what you can do and I wrote it to say what you can do. Please take another look and write back if things are not clear enough. As for a repeat procedure, if it is not urgent- stone is obstructing the kidney – I might seek a second opinion. Regards, Fred Coe
5 months ago I was diagnosed with Grade 1 fatty liver, Schatzkis Ring, Few linear erosions in lower end Oesophagus, few erosions in fundus and body of stomach, mild active iletis. Total Bilirubin – 1.6 Direct Bilirubin – 0.3
Weight – 77 kg Height – 170 cm Male Indian
I again got USG abdomen done 3 days ago with CBC and Liver Function Test
My current results are Mild Altered Ecotexture in Liver, 4.5 mm renal Calculus in RT Kidney and 3 mm Renal Calculus in Left Kidney
Bilirubin Total 1.5 , Bilirubin Direct -0.31, Bilirubin Indirect – 1.19, Monocytes – 1, Basophils – 0,
Current Weight – 63 kg
During these 5 months I had totally cut down on mostly shifted to gluten free dairy free vegan diet with an exception of Youghurt.
Kidney stones were a surprise for me and wondering what more tests should I need to get done and which doctor to consult. Whether Urologist or Gastroenterologist
Hi Arpit, Given the complex GI issues, you may have formed calcium oxalate stones from increased urine oxalate. As in the article you post on, you need a full evaluation for causes of stones, and I would urge your physicians consider getting the requisite 24 hour and urine studies. Regards, Fred Coe
Hello Dr. Coe,
I’ve been suffering from intermittent (but increasing) suspected kidney stone pain for 7 years. I have a history of both gall and kidney stones. Due to the pain, I had my gall bladder removed in 2014, but it didn’t resolve the pain. I live in north-central New Jersey and would like to find a local urologist with your perspective. None of the urologists I’ve met with have mentioned anything other than invasive procedures. None have mentioned the tests (analyses) you speak about.
I look forward to hearing from you if you’re able to provide me a local referral. Thank you.
Debi
Hi Deborah, A nephrologist in NY is excellent. I would suggest you call him. Fred
Thank you for your informative article!
I am searching for an alternative for Urocit-K 10 extended release that I was prescribed 3 time daily, after I had my first kidney stone last year. As a senior citizen on a fixed income I am one of those people concerned about the rising cost of all of my medications as I age.
I’ve been looking at bulk (1kg) packaging of pure potassium citrate powder. I can purchase 1kg for 25% of the cost of my monthly prescription. Is pure potassium citrate powder a good alternative. If it is, what size dose and how often should these dosages be spread throughout the day?
Hi Walt, Many have used bulk powder. The usual K Citrate pill is 1080 mg so you would have to buy a scale that can measure that amount accurately and take what your physician has prescribed. Likewise He/She needs to know what you are doing and approve as potassium is safe but the amounts in a dose need to be controlled. Regards, Fred Coe
Thank you for the lessons! I learned more here than I have over the last several months dealing with my UTI. I’m a bit discouraged as I have been fighting proteus marabilis for several months. It clears up and then comes back. Recently, through a CT scan, a significant staghorn calculi was discovered. It appears surgery is the way to remove it, but my concern is, if the bacteria is the cause, will stone forming be a constant problem?
Hi Donna, Proteus can produce struvite stones and they are a big problem. Your surgeon will know about the special management issues with such stones. If it is struvite, it is the bacterial themselves produce it, and prevention is very difficult indeed. I am sorry I have not written an article on the problem – we need it. Best of luck, Fred
Thank you for an excellent article. I’ve had at least four stones in each kidney for several years, based on annual ultrasounds, though each year I’m told that they are basically stable. They are under 5 mm each, though at least one is nearly 5 mm. I’ve never passed a stone. I had severe pain related to gallstones and had my gall bladder removed in 2020, and my pain resolved. Around the time of my gallbladder episodes, my eGFR fell to 57. Later in September of 2020 my eGFR fell to 53. I’d been at a very hot funeral the day before and could have been slightly dehydrated. After hydrating, we repeated the test and my eGFR is now above 60. I’ve had a recent 24 hour urine collection, and I’m going to meet with a diet specialist soon. I’m 67 and petite, about 110 pounds. Around the time of my gallbladder attacks, my blood pressure became elevated (in the past my blood pressure was quite low, around 95 to 110 over 58 to 68.) I am now taking Verapamil. I’ve received conflicting advice from two doctors about switching to HCTZ. One doctor recommends that i switch immediately, while the other recommends that I stay on Verapamil and try to manage the stones with diet. I’m trying to weigh the benefits of HCTZ on stone formation against the potential negative impact on kidney function. I had a previous 24 hour urine collection in 2017, at which time I was told my stones were most likely calcium oxalate. I’ve been trying to follow a low oxalate diet since then. I would appreciate your thoughts.
Hi Debra, The chapter you picked is my favorite and very good I think. When you get your 24 hour urine results, read them in light of the chapter and see where you fit in. Oxalate is much emphasized for historical reasons, overly so in my opinion. So many factors can cause stones! As for blood pressure the best advice from far away is home pressure measurements with a decent machine – usually around $50 – $75 and sometimes covered a bit by insurance. Here is my best on blood pressure in stone formers. Regards, Fred Coe
Hello Dr. Coe, thank you for the informative article and sharing your knowledge with us. I had not heard of 24 hour urine analysis from any of the 3 the urologists I consulted. After having a stone removed, I am looking at all options to prevent a recurrence. This article helps. Regards, Harshad Dixit
Hi Harshad, I am glad you now know, and you should certainly get tested. Regards, Fred Coe
I’ve spent the last week trying to pass a kidney stone after a trip to the ER for the pain. It’s been a bit grueling and to be honest, not sure if I did. Can a 24 hr urine test verify the type of stone even if I do not have the stone in hand?
Hi Lynn, A full evaluation for cause sans knowledge of stone type is still helpful in that most stones are calcium stones. The radiographic density from your CT helps, as well – your urologist will know – in ruling out uric acid. Here is my best on the subject. Regards, Fred Coe
My husband has kidney stones. Would you recommend a urologist in the Columbia, SC area please? Thank you for all of the helpful information you have shared. He is a U of Chicago alumni , so it is wonderful to find you.
Hi Jean, The safest bet is at your university medical center that has a kidney stone center. They do not list their physicians so I do not know if any of them are nationally recognized – I do not know who is there. But most university centers have good people. Fred
I am a 60year old petite female 110lbs. Have been diagnosed 12 years ago with osteoporosis. Which doctors have told me is a result of having kidney stones. They are calcium oxalate stones. Have had many 24 hour urines and blood tests. High calcium in urine but not blood. When I was in my 20s they told me I had something called medullary sponge kidney. Not sure exactly what that is but would this be why I have so many stones. For the past 26 years I have passed stones and have had surgery for some and lithotripsy. Every time I have a cat scan they see multiple stones in both kidneys. I am currently trying to pass a size 4 which is I can usually do but this one is taken longer than usual. My recent cat scan shows approx. 10 stones in each kidney the bigger ones averaging size 3-4. Saw your article and will try low oxalate diet. Do you know anything about medullary sponge kidney and stones?
Hi Patty Jo, Genetic hypercalciuria causes abnormal bone mineral loss when diet calcium is low or sodium intake high, or both. In general, given all of your stones, diet and meds might be a good idea. Here is my best article on what I think is your problem. Diet oxalate is usually a very minor issue. Likewise, with so many stones, be sure they are really calcium oxalate – I suspect they are calcium phosphate. As for MSK, it is unlikely, though possible. Here is my best on that. Regards, Fred Coe
Hi Dr. Coe,
I came to your website in hope of finding a more robust answer to why thiazides prevent stones. What I found instead, was a complete treasure trove of knowledge. I am an M2 at Des Moines University in Iowa, and I am giddy knowing that this resource exists. You have written with eloquence, enthusiasm, and depth, and the interwoven references to medical history and art history captured my attention immediately. Thank you for your contributions to medicine and the medical humanities from a hopeful future educator, writer, and physician.
Sincerely,
Mikayla Brockmeyer
Hi Mikayla, Thank you for the note, and I am happy the site is a value for you. Regards, Fred
Hi Fredric, I’m so interested in your findings. I’m making 80% phosphate (apatite) and 20% calcium oxalate monohydrate stones. I’m confused as how to prevent more. I had my parathyroidectomy as was diagnosed with Primary Hyperparathyroidism in 2014; thought that would cure me; but since then have had at least 3 episodes of 9mm blocking stones. I am at my wits end about what to do? I had shock wave lithotripsy but this made me sicker as my inflammation markers went up and my kidney function went down to 50% so they kept me in Hosp until I got better and then did the laser ureteroscopy. The urologists seemed to be arguing about my receiving the shock wave treatment as one said it was barmy to give me that? I am worried my kidneys are getting damaged as more form? I am 50 and female. Many thanks Angie
Hi Angie, Are you sure your PHPT is cured? In other words, are fasting morning serum calcium values below 10? If so, you have the problems of a routine calcium phosphate stone former, and they are significant. I would avoid ESWL as the stones will not break up easily – ureteroscopy is better. The article outlines prevention but it is tricky, and if you can consult an expert – I do not know where you live, but could try to help find you someone near – things might be simpler. There is also telemedicine. Regards, Fred Coe
Hi Fred, thank you so much for your reply; you’re so kind to respond! I live in the Uk. I have had follow up blood tests which showed my calcium was back to normal levels; but they weren’t fasting morning tests just a normal day routine one. They said I was “ok” regarding my primary hyperparathyroidism; so I accepted that as conclusive. From what you’re saying I need to ask for a morning fasting one? Is that different? I’m worried my PHPT isn’t cured then? Or that I’m just a phosphate former. Thank you for replying I am so grateful. It’s hard here in the UK to get any follow up at all sadly. We are just left alone and scared. Could you tell me what telemedicine is please? I am beginning to think I am a phosphate stone former and I feel very scared about my future.
All the best
Angie
Hi Angie, I believe I answered this (above); if not please reply for more. Fred
Hello Fred
Thank you for your reply; much appreciated. I will ask to have a fasting serum check as not had one: only normal blood tests have been done which say normal calcium. I think I may be a phosphate former, which I’m finding very scary. What is telemedicine please? I am in the UK and our follow ups are non existent so I feel quite lost to be honest and need more investigation which I can’t seem to get here unfortunately. Do you know anyone in the UK I could get advice from ? As I’m so worried about my multiple bilateral stones.
Many thanks
Angie
Hi Angela, For consulting that does not require physical examination, we visit via Zoom, which is a world wide video platform. The only problem is that your insurance is via the national health service which is unlikely to pay my university in Chicago. I no longer know physicians in UK who specialize in kidney stone prevention, unfortunately. The NHS has lots of material; here is there general introduction. I imagine within your region there is an NHS group of specialists. Regards, Fred Coe
Just wondering how you would treat patients with short-bowel syndrome who must drink ORS to maintain hydration. Obviously analyzing the stone would be crucial. Their diets are so limited anyway, it’s difficult to put on more restrictions. I would be inclined to have them avoid the highest oxalate foods, get calcium with meals and possibly add the K citrate regularly? Other tips or specific resources for this? Of course, these are short-bowel patients with colon attached.
Hi Merin, I suspect you are a physician, or other kind of health worker. These are very complex problems. I have found it very hard to lower urine oxalate and suspect hepatic oxalate production may be increased. Calcium additives to bind oxalate, low oxalate diet – none work well. Cholestyramine is poorly tolerated. But overall urine volume is an issue in a lot of these patients and hydration fluids are key – as you imply. I would usually try tot push that as far as possible and be guided by 24 hour supersaturation values. Regards, Fred Coe
“I have found it very hard to lower urine oxalate and suspect hepatic oxalate production may be increased.”
Have you tried increasing vitamin B6? It’s been known (and probably forgotten again) for 60 years that B6 deficiency causes glycine to be converted to oxalate, and addition of B6 stops the oxalate formation. More at Page 184 of Adelle Davis Let’s Get Well.
However, people are recently saying that the problem of “oxalate dumping” is very non-simple, once you have oxalate deposits it doesn’t just respond like a machine you are oiling. Instead there is an effect also found in mercury poisoning detox, that there is a change from “locked down” to “let it flow out”, with the latter confusingly resulting in worse rather than better.
Cheers.
Hi Robin, I usually do not approve posts with advertising for a commercial entity but did in this case. For readers I need to demur concerning oxalate dumping and the like. Absent kidney failure serum oxalate is in the range of 1 – 4 umol/l, so the calcium x oxalate product is an order of magnitude below that needed to form crystals. Oxalate itself is a metabolic end product. So systemic oxalate storage (deposits) is limited to renal failure and the rare primary hyperoxaluria states. Oxalate itself cannot deposit apart from calcium oxalate crystals. Regards, Fred Coe
Hi, are there any over the counter urine tests that can help monitor low urine citrate? Or are there any over the counter tests a calcium oxalate stone former can use as a tool? It’s so frustrating to figure out the magical combination of diet, water intake, etc. with so few tools.
Thanks
Hi Joe, No. But any physician in the US has access to Litholink that produces a fine set of data. I would certainly have it used for your care. You are right about many variables, and they need to be correct and all present at once. Regards, Fred Coe
Dr. Coe, Thank you for providing all of this information – very informative for a first time kidney stone patient. I’m a 58 year old female, 5’6″, 140 lbs with typically lower blood pressure ~101/60 with no history of kidney stones or any kidney issues nor family history. I take 7.5mg of Rosuvastatin for slightly elevated LDL, and 88 mcg of Synthroid since 1996 as a result of radio-iodine treatment of Grave’s disease. I use bio-identical compounded topical and vaginal hormones, use beginning shortly after menopause at 45 yrs. old.
Over the years I’ve had Vit. D absorption issues resulting in the need to take prescription Vit D temporarily 2x and have supplemented 5000 IU for years. On advice of my GP I decreased this to 2000IU then 1000 over the past couple of years. I’ve had low Cortisol results from saliva testing, although recent blood work shows in range. For years I’ve taken Turmeric, fish oil, CoQ10 regularly and the occasional multi-vitamin.
I had a one-time A-fib event in 2008 that was resolved (after many months of cardiac testing) by adjusting Synthroid from 100 to 88mcg. Thankfully that hasn’t happened again!
All this to say that I am completely surprised by the kidney stone that showed up last month unannounced. I consider myself fairly fit, exercising regularly and eating fairly well. I watch sugar (which has been inching up over these past several years – diabetes in the family). I don’t salt anything or cook with salt. I watch fat due to LDLs. Little red meat, not a lot of dairy and a focus on whole grains, veggies, fruit, salads. I probably don’t drink as much fluid as needed.
My 4mm stone, (analysis showed calcium oxilate (80% calcium monohydrate/20% calcium dihydrate), was lodged at the distal end of the ureter at the bladder. Under general anesthesia they did a ureteroscopy and placed a stent for a week. I’m due to follow up in 6 weeks with an ultrasound & blood work. Low oxilate diet has been recommended but no talk of 24 hr. urine testing, no discussion of other possible medical issues/causes. I won’t see doc for 8 weeks post-procedure, which seems like a really long time to not discuss any of this.
I’m really stumped about this stone and how to prevent another. I welcome your thoughts and wonder if you do virtual consultations and have recommendations for Endocrinologist and Nephrologist in the Hudson Valley area of NY.
Apologies on this long-winded post but I am a worrier and have had more than my share of anxiety and fear over numerous things since mid-2019. The pandemic didn’t help. Also wonder if this has contributed to any of this. I appreciate your time and hope you can respond.
Hi Ellen, The calcium oxalate monohydrate is most compatible with oxalate excess or low urine volumes, but I would do a complete evaluation to be sure about the cause. This chapter is my best on that. New onset in mid life has special implications. I noticed the turmeric, a very high oxalate product and perhaps the culprit, but I would not count on that. I do video consultation, but perhaps your personal physicians will be able to help when you have all of your data. If not, my secretary is at 773 702 1475. Regards, Fred Coe
Thank you Dr. Coe.
I had noted that turmeric is high oxalate and I stopped taking it a month ago. Also, in reading Jill’s information and others I see that all of my “go to” snacks (peanuts, almonds, essentially most nuts) are high in oxalate, which I was eating in some form every day, multiple times per day for years now to be heart healthy and cut cholesterol. Also dark chocolate has been a regular – a small bit most days. And very likely not enough fluid intake. When you say “…have all of your data” what do you consider all the relevant data to determine a path forward?
Thank you again.
Hi Ellen, I mean 24 hour urine and blood studies, CT imaging to count stones, and a lists of all meds and supplements. Of course everyone has a different collection of medically related information – all of it can matter. Regards, Fred Coe
Good afternoon,
I need help! I am 58 yo female, 147 lbs with Crohn’s disease/bowel resection and Randall’s plaques disease. i drink one gallon of Simply lemonade a day plus water, take 650mg of Calcium, and a magnesium/potassium/citrate supplement-Theralith XR. I am very careful about what I eat. I keep getting recurrent kidney stones-I have had two 24 hour collections that basically say I am doing the right things. My Physician is at a loss as well as I am. can you offer any help?
Thank you,
Marie
Hi Marie, If the 24 hour urine supersaturations for calcium oxalate and calcium phosphate are below 3 and 1, respectively, and stones are not uric acid, you may be passing old stones or experiencing within day peaks and valleys of stone risk the 24 hour urine blurs. This requires your physicians and you to review your day/diet cycle looking for problem areas. As well, one needs to keep count of stones. Regards, Fred Coe
Hi Dr. Coe!
First off, an excellent resource of information this article is, great work. I’m a frequent stone former at 38/m, I had a 24/hr urine test back in Dec that showed a Urine citrate of 189mg/day which was well below the recommended amount. Quest results says I have “Hypocitraturia”. I’ve been looking at ways to help learn about my own issue as I’ve just learned that I have two more stones in my kidneys, 1mm and 2mm on left/right just this week respectively after having passed one in Aug 22 and two in Mar 21. (they’ve made up shop till they decide to move on to the highway that is my ureter). I’ve been dealing with this since I was 18 and I’m starting to reach the limits of my anxiety. Multiple surgeries, lasered and blasted.
I might forsee my first Lithotripsy in the future given the current homemakers.
Unfortunately, I don’t think I was provided adequate knowledge on “my diet” and recently started to eat “healthier” due to a recent “elevated cholesterol”. I’ve come to realize at least my recent run of stones may have been related to cutting dairy out and loading unknowingly high oxalate foods. With yours and Jill’s articles I’ve become more informed unbeknownst to my current healthcare provider. Unfortunately my doctor seems to just pass around a pamphlet, drink lots of water and out the door I go. I don’t really feel like I’m getting personalized care from my current doctor. Often times even feel like I have to remind them on my own history with them specifically. I’m in Sarasota, FL. Next step is a CT in April too check on things and doctor says (if I recall correctly) Potassium Citrate pills may be in the future if I keep forming stones. Mind you I’ve been going to this doctor since I was 18? I feel like I’ve already reached “the future”. See my point?
Although I don’t have the results to say otherwise, my doctor has mentioned my stones were previously calcium oxalate. I do have my most recent August stone report and it says,
Carbonate Apatite (Dahllite) 90%
Calcium Oxalate Dihydrate (Weddellite) 10%
This may seemingly contradict my supposed previous stones against “today”? Or am I still an Oxalate stoner?
I also wonder with your research/technical advice if something like LithoLyte Powder to add to my drinks is good given my scenario? I’m trying the Lemon drink scenario given my low Citrate but looking for something a bit more manageable with a busy lifestyle too mix with readily available water sources to keep up my intake.
Your thoughts and technical advice on my situation would be very much appreciated. And perhaps any recommendations for local resources to provide a more personalized and caring approach to my kidney needs. I saw you offered a search to another. You’re very kind to do so regardless!
Here are my 24/hr urine results,
STONERISK® DIAGNOSTIC PROFILE
TOTAL URINE VOLUME 2.70
Reference Range: >2.00 L/day
PH URINE 6.7
Reference Range: 5.5-7.0
CALCIUM, 24 HOUR URINE 154
Reference Range: <250.0 mg/day
OXALATE, 24 HOUR URINE 20
Reference Range: <45 mg/day
URIC ACID, 24 HOUR URINE 562
Reference Range: 320 mg/day
SODIUM, 24 HOUR URINE 103
Reference Range: <200 mEq/day
SULFATE, 24 HOUR URINE 15
Reference Range: <30 mmol/day
PHOSPHORUS, 24 HOUR URINE 694
Reference Range: 60.0 mg/day
AMMONIUM, 24 HOUR URINE 35
Reference Range: 14-62 mEq/day
POTASSIUM, 24 HOUR URINE 35
Reference Range: 19-135 mEq/day
CREATININE, 24 HOUR URINE 1219
Reference Range: 800-2000 mg/day
CALCIUM OXALATE 0.66
Reference Range: <2.00
BRUSHITE 1.53
Reference Range: <2.00
SODIUM URATE 0.73
Reference Range: <2.00
STRUVITE 2.72
Reference Range: <75.00
URIC ACID 0.21
Reference Range: <2.00
THE PATIENT HAS:
Hypocitraturia
Hi Blake, Your stones (calcium phosphate) form in alkaline urine and your urine is indeed alkaline with pH of 6.7. Despite the high pH your urine citrate is low at 189. Your urine ammonia is 35 mEq/d (acid excretion) and your sulfate acid load is only 15 mEq. We see this pattern often in calcium phosphate stone formers. Possibly you are a carrier (heterozygote) for one of the gene variants that cause distal renal tubular acidosis). If so that could influence how one treated you to prevent stones. If not, treatment might take another course. Knowing nothing more than the urine labs that is all I should say. I would suggest getting the gene work which is available to you and your physicians through national vendors. If your physicians believe I could be helpful (this is an unusual situation), consultation can be arranged via telehealth. Regards, Fred Coe
Dr. Coe
Can you recommend a Urologist or other Doctor in Ocala, or Gainesville, Fl? My Urologist is saying drink water and little else. I’ve never heard of the urine tests and I have passed 5 stones and have another 4 in kidneys. I appreciate you and any insight you can provide. Thank you!
Hi Greg, I can. Gainesville (U Florida) has a brilliant stone program. Among the best in the country. Go there. Regards, Fred Coe
Thank you! I’m going to see Dr Vincent Bird at Shands.
Hi Getting some confused advice due to my 24 hour results. First stone, 5mm, sitting in right lower kidney lobe
TOTAL URINE VOLUME 2100
PH URINE 8
CALCIUM, 24 HOUR URINE 347
Reference Range: 0-320
OXALATE, 24 HOUR URINE 17
Reference Range: 4-31
URIC ACID, 24 HOUR URINE 428.4
Reference Range: 173.7-902.1
SODIUM, 24 HOUR URINE 144
Reference Range: 39-258
CITRIC ACID 385
Reference Range: 320-1240
MAGNESIUM 94.5
Reference Range:12-293
I can see my Calcium and Na are high. I have greatly increased my water to 3L and greatly reduced sodium. Of course the urologist and nephrologist both said decrease my Calcium intake, but i don’t even eat calcium for the most part, besides what would be in veggies. I eat no dairy. So from my research with you and Jill, i see to increase my Calcium intake, which i have.
What im confused about is if i should take any citrate/lemon juice because my Citrate is normal toy pH is so high, seems like citrate isn’t good for that? is that correct or no?
How do i lower my pH to safer level?
I have no idea what my stones would be made of based on these results.
I WAS eating a ton of almonds, extra salt, not enough H2O, tons of black and green tea
Hi Cara, You presumably have genetic hypercalciuria, assuming a full evaluation has excluded systemic diseases.The high urinie pH cannot be interpreted apart from knowing stone type and urine ammonia – are stones calcium phosphate, are there bacteria that raise urine pH by producing ammonia. Certainly reducing diet calcium poses bone risk, and is not a reasonable approach to stone prevention. Regards, Fred Coe